#dysautonomia awareness month challenge
Explore tagged Tumblr posts
Text
Doing the Dysautonomia Awareness Challenge thing because I want to.
1. The type of dysautonomia you have
Pandysautonomia
2. Your diagnosis story
I noticed that I was getting lightheaded after standing for too long, and then I started feeling like I was going to faint. It was annoying but not awful, and I have my plate full with chronic migraine, so it got put on the back burner like every other issue I have that I should be dealing with but don't have the energy for.
And then I was so bad on the way to a family holiday in Malta that I needed a wheelchair to get through airport security. And then I had a fainting spell in the middle of a shop in Malta (luckily, sat down before I could fully pass out)
No idea what was going on, still having migraines, so ignored it. Brought it up with my neuro, 'hey, I've also been getting these dizzy spells?'
My current neuro, the fourth one I spoke to, is fantastic. They referred me over to every clinic imaginable because they suspected POTS, but also referred me to an ENT clinic, just in case.
ENT diagnosed me with vestibular migraine, and Persistent Postural-Perceptual Dizziness (PPPD) and gave me physio before discharging me.
Rheumatologist ruled out EDS and diagnosed fibro (the most tentative lacklustre diagnosis I've ever had)
The neurocardiologist really nailed it down though. I was supposed to have a TTT, but they did an active stand instead, and it wasn't clearly POTS, so that killed me.
THEN I had a battery of other tests (exercise test, ambulatory blood pressure, CT scan, heart scan, something else I can't remember) and my neurocardio confirmed pandysautonomia and POTS.
I challenged the diagnosis, because the active stand results had fucked with my head, and she reassured me that no, I definitely have ISSUES. The TTT is just one diagnostic tool, and the results of my other tests, plus my medical history, confirmed the diagnosis.
I also had a non-dipper profile for my BP, which is a little concerning, but I was having a 9-migraine at the time and didn't really sleep.
I'm still waiting for a gastro appointment, and to drill a little deeper on this pandysautonomia thing, but I feel like I had a pretty easy diagnosis journey comparatively (comparative to other people's journeys and my migraine journey)
My POTS is atypical because I have high blood pressure, not low - anyone else with the combination, hmu, I'd love to hear from you. It sucks having an atypical diagnosis in a 'common' illness.
3. How long it took you to get diagnosed
2-3 years, pretty quick
.
4. Your most bothersome symptom
The fucking TREMORS!
I can handle the fainting pretty well, I get the dizziness, it sucks that I can't get up and do things but I was dealing with that before the pandysautonomia got bad because of my constant refractive chronic migraines.
I went from being inactive to being inactive for more reasons, so there wasn't much difference re: impact in my life
but the TREMORS.
I can't handle them! I can't feed myself properly without weighted utensils, and even then I have to take frequent breaks while I eat because the constant shaking is tiring. It gets in the way of my typing, it makes it hard to do anything that needs even a modicum of steadiness, catching crickets for my tarantulas takes 10x longer and feels bad.
And that's just the ones in my hands! The ones in my legs make me feel like I'm wobbling about like an Ed, Edd and Eddy character. The constant shaking through my skeleton is so uncomfortable and irritating. I just sit there and shake and can't paint or draw or felt or anything. UGH.
end bitching.
1 note
·
View note
Text
7. Your favorite products to manage your symptoms
If by products you mean, like, shit I buy regularly to manage my POTS . . . pedialyte is pretty great bc dehydration exacerbates the POTS symptoms. But besides that, I don’t really buy anything regularly to help me manage it because I don’t think there’s anything I can buy that would help me manage it (also bc I’m poor).
8. Favorite way to hydrate
I get water flavoring powder and add it to my water, then drink that. Sometimes I’ll add salt bc it makes it taste better. If its a really hot day or I’m feeling really dehydrated, I’ll drink a ton of pedialyte. Idk if its hydrating or not but I love juice. Just don’t get it much bc it’s expensive. Hydrations not super important so I don’t have a ton to add to this.
9. Your “saltcuterie board” / salty snacks
I don’t eat a ton of salty snacks. Bread with butter and salt is pretty nice though. I’m beginning to get the sense that this is less of a “dysautonomia awareness challenge” and more of a “neuropathic POTS awareness challenge” tbh bc — from what I can tell — salt is not part of treatment for hyperPOTS and some other forms of dysautonomia.
10. Favorite pair of compression socks
Say it with me folks: “not all dysautonomia is neuropathic POTS”. That being said, I do have some knee length skull pattern compression stockings, I bought them in a desperate attempt for something to help and found that they do alleviate some of my joint pain, but don’t do shit for my POTS.
11. Your mobility aids
I currently have 2 canes (a purple one and a folding blue one), a blue rollator, and a folding manual wheelchair (Offcarr brand, ministar model).
I don’t use anything at home, my apartment technically has enough room for my wheelchair but its so small that its a pain in the ass. I do have a shower stool I use, and I sit on a chair to cook. I used to use my wheelchair around the house when I lived in a co-op.
I rarely use my cane, mostly only to go out and get the mail every so often, but I use the folding blue one to get down the aisle of a plane if I’m flying somewhere. I use my rollator a couple times a week if I’m going on short walks around the neighborhood with my partner or maybe getting something at the grocery store next to my place (have to go up a flight of stairs to get to it, so my bf will pick up my rollator and carry it up the stairs. If I’m on my own, I go the long way in my wheelchair). I also use my rollator for doctors appointments (even though I feel the effects of that poor decision nearly a week later) because I think I’d get judged poorly if I went in my chair. I use my manual chair for pretty much everything else though if I’m leaving the house. Job interviews, going to the library, going to the synagogue, etc.
I’m hoping to get one of those lightweight folding electric wheelchairs soon so I can actually navigate the area around my apartment. Downtown is flat enough that its not tooooo much trouble to navigate in my manual chair, but the area around my apartment and the route I take to the synagogue has so many hills that my partner needs to push me half the time. I know its fucking up my shoulders, so I’m hoping to get a power chair sooner rather than later.
That being said, typically a wheelchair is not good for POTS iirc. I use my wheelchair largely for my other issues, and do my best to avoid deconditioning. If POTS was the only issue affecting my mobility, I would probably just use my rollator most of the time.
12. How you manage a flare
I just lay down and wait for it to be over, which can take a pretty long time.
13. The thing that has helped me the most since diagnosis is
Dealing with the comorbid iron deficiency has been the only thing thats helped the POTS specifically. My doc sucked so my POTS has been untreated this whole time.
14. Tips for cooking/cleaning with dysautonomia
Do whatever you can sitting. If cooking, gather all the bowls and ingredients and measuring stuff in one go and put it at the workstation so you don’t have to stand up and get shit constantly. I try to also keep most of my cooking and cleaning supplies that I use frequently around eye level so I don’t have to reach up or down to get stuff (both make me dizzy).
15. Managing dysautonomia at work/school
Lmao I dropped out and I’m unemployed so I am very much not the person to be asking about this. I didn’t do anything special to deal with my POTS when I was working and in school, nothing I could do that would help it that I wasn’t already doing for my other conditions. I did make an effort to stay hydrated though, because I was living somewhere pretty hot and dehydration doesn’t mix well with POTS.
Just saw this, thought I might as well do it, can filter out “#dysautonomia awareness month challenge” if you dont wanna see it. might do it in chunks every couple days / every week so that I’m not reblogging it too often (and bc I know there’ll be days I forget)

Gonna do the first couple all in one go bc I’m starting late
1. The type of dysautonomia you have
I have hyperadrenergic postural orthostatic tachycardia syndrome, aka hyperPOTS. POTS is essentially that your heart rate shoots the fuck up when you sit or stand up, which can cause you to feel dizzy, get confused, faint, etc. Also comes with other fun symptoms like brain fog! Why this happens is different for different people, and POTS can be categorized into subtypes based on why its happening. You can often have traits from multiple subtypes at once. The subtype you hear most about in the POTS community tends to be neuropathic / partial dysautonomic POTS, its the most common subtype. There’s also hypovolemic POTS (where you don’t have enough blood in your body I think?) and secondary POTS (where you get POTS because of another condition like diabetes or lyme). IDK exactly how neuropathic POTS works, it think it involves nerves or blood vessels not working right, but I know its different enough that I can’t relate to most of the POTS community because of it. HyperPOTS tends to come on gradually, while neuropathic comes on pretty abruptly. Hyperadrenergic POTS happens directly because of a malfunction in the autonomic nervous system, instead of the ANS malfunction happening because of another cause (which I think is the case for neuropathic POTS?). This “malfunction” in hyperPOTS means that my brain dumps adrenaline into my body. This causes my blood pressure to go sky high whenever I stand up (in most people, blood pressure drops a little when they stand). It also causes my heart to race, causes me to get dizzy, and can cause me to pass the fuck out or fall down. Unfortunately, hyperPOTS is the hardest subtype to treat, and a lot of the stuff you hear as “how you can help manage POTS at home” doesn’t work for hyperPOTS (aka water, salt, compression, exercise). Treatment for hyperPOTS is pretty much just medication, but it can be hard to find the right medication or dosage, and often you need to change the doses over time. Also you’re supposed to avoid SSRIs, SNRIs, and NRIs (which are the classes a ton of antidepressants fall into) but I haven’t heard about this bit very much so idk. (disclaimer: I’m not a medical professional, I’m basing this off of what my doctor/specialist told me and the papers I have read on the subject, I could be wrong. I also don’t engage with the POTS community online at all so what I’m saying could go against whatever the common understanding is of POTS / its treatments / the subtypes / whatever in the community ).
2. Your diagnosis story
For pretty much as long as I can remember, I’ve gotten lightheaded when I stand up. I remember being pretty young and having to lean against walls or sit down pretty frequently because I stood up. I attributed it to my low resting heart rate and low blood pressure (my mom and brother also have low / low end of normal blood pressure and heart rates). When I was maybe 13 my doctor noticed the low resting heart rate and blood pressure, I told him about how I got dizzy standing up somewhat frequently, and he told me to take my time standing up. I was a very active kid who couldn’t be bothered to take 10-15 seconds to go from laying to sitting, and then another 10-15 to go from sitting to standing, and then another 10-15 to go from standing to walking, so I just didn’t. Idk if I met the criteria for POTS back then bc I never bothered checking my heart rate, but regardless. It really didn’t impact my life very much. Fun to note that hyperadrenergic POTS tends to come on gradually and has a genetic component (idk if thats all the time or just some of the time though. I’m the only one in my family who definitely has it, but theres a chance my mom could).
Anyways I started experiencing a host of Mystery Symptoms in the summer of 2020, and they got significantly worse (and new ones started) around fall of 2021. One of the symptoms I was experiencing was that my usual lightheadedness became more frequent and so bad that my body would just give out and I’d collapse onto the floor. Luckily I remained conscious through the whole thing and had just enough control of my body to not hit my head. I went to my doctor about it, she told me to drink more water (throughout the appointment I was drinking out of a large water bottle, I already kept myself pretty well hydrated :/). She ran a couple tests, saw that my iron was a bit low, and told me to take some iron supplements. That helped me get to the point where I wasn’t collapsing nearly as much. However all the other symptoms of Whatever The Fuck was happening still remained, and I was also still pretty dizzy, so she referred me to a specialist.
The specialist was. Not fantastic tbh. However he did test me for POTS, and found that my heart rate shot up pretty high, as well as my blood pressure. For a diagnosis of hyperPOTS, your systolic blood pressure needs to rise by at least 10 mm Hg when you go from laying to standing (+ you gotta have the general POTS criteria). For most people, it stays the same or drops a little. Mine shot up by about 30 mm Hg and I met the other POTS criteria, so it was pretty clearly hyperPOTS.
His theory is that I had hypovolemic POTS (aka not enough blood in my body, which caused POTS symptoms) as a child for a long time and this trained my brain to dump adrenaline into my body whenever I stood up or changed positions in order to keep me upright and conscious. I got older I got my blood volume up to normal, but by that point my brain was so used to dumping adrenaline into my body to keep me going that it just does that permanently. Also long term childhood stress and trauma made my brain learn to dump adrenaline into my body as well. And then stress / catching covid / whateverthefuck was the catalyst that sent it from “mildly annoying and not disabling” to “something I need to account for when doing day to day activities”. I’m not entirely sure thats what happened because I don’t think I had any trouble with blood volume as a child and I don’t think my heart rate shot up as a kid (the way it needs to for a diagnosis of POTS), and also I was experiencing Symptoms with gradually increasing frequency before the Fuckening that was Fall 2021, but who knows.
So he ended up diagnosing me with hyperPOTS as well as something else that I don’t totally agree with. While his knowledge of POTS and the things he was ruling out for me or diagnosing me with seemed pretty extensive, he also sucked at listening to me or actually treating me. But that whole story belongs in the answer to day 20 I think (day 20 is worst interaction with a healthcare provider).
3. How long it took you to get diagnosed
This is a bit tricky to answer because it depends on what you would consider the “start date”. HyperPOTS comes on gradually, so there was no definitive time I can point to and go “oh if a doctor had seen me at this exact moment they could’ve diagnosed me with hyperPOTS, when they couldn’t’ve the month before.
If its from when I first started having symptoms (and the specialist was right and I had hypovolemic POTS as a kid) then thats over 12 years.
If it’s from when the POTS symptoms started getting to the point where they interfered with my life in a significant way, then only about a year.
I’m still trying to figure if the specialist was right or not about the other thing, and its been over three years since the symptoms started.
4. Your most bothersome symptom
When it was happening, the falling down bothered me the most. It’s hard to know which of my symptoms are hyperPOTS and which are whatever the fuck else is wrong with me, but the constant brain fog and the dizziness + fucked up vision whenever I stand up is not fun.
5. Day in the life with dysautonomia
Tbh the other thing disables me far more than the hyperPOTS does so my average day is far more affected by it. I don’t do the day to day lifestyle changes most people do for POTS because the only treatment for my subtype is medication (compression, salt, water, and exercise don’t help), and I don’t currently have a doctor. I do try to salt my food a good bit and drink a ton of water and exercise as much as I can, but thats just because I like salt and want to be as healthy as possible. Adapting my life around hyperPOTS mostly just consists of being real careful if I’m standing up on a bad day, being careful when I lift my arms above my head (to grab stuff off a shelf, pull the stop request string on the bus, etc), and using a shower stool. I also use a wheelchair whenever I leave the house, which is heavily discouraged for POTS generally because its super important to avoid deconditioning and to make sure you exercise, but the other shit I’ve got going on makes it necessary.
6. Your medication regimen
I’m not on any POTS meds, but I take medications for other stuff. I’ve heard magnesium is supposed to help POTS, I take it to counteract the side effects of a non-POTS medication I’m on. Haven’t noticed it help my POTS symptoms at all though. Probably is supposed to help for neuropathic POTS.
1 note
·
View note
Text
Also preserved on our archive (Daily updates!)
The topmost link includes a video of the news segment
By Destiny Meilleur
Medical researchers at the University of Calgary say a condition affecting autonomic bodily processes — those that occur automatically, such as heart rate, bladder function and sweating — is frequently found in people diagnosed with long COVID.
The condition is known as dysautonomia, an umbrella term for a group of related conditions. Support networks for those who suffer from it are working to raise awareness throughout October, which has been deemed Dysautonomia Awareness Month by the advocacy group, Dysautonomia International.
According to research by Dr. Satish Raj, a cardiologist and expert in autonomic health conditions at the University of Calgary, as many as 30 per cent of long COVID patients also meet the criteria for a condition called POTS, a form of dysautonomia known as “postural orthostatic tachycardia syndrome.”
According to Dysautonomia International, other studies have put the figure at between 70 per cent and 90 per cent.
The challenge is that the symptoms of the condition can be easy to dismiss. “Who likes to sit around and talk about their sweating,” notes Dr. Raj. “No one does that… These are just the background things that are useful for keeping you alive.”
Rashmin Hira, a PhD student at the Universty of Calgary and long COVID researcher, adds, “Unfortunately, a lot of people do get told that it’s just anxiety.”
That’s why raising awareness through events such as Dysautonomia Month are important, says Lauren Stiles, president and CEO of Dysautonomia International.
“(It) is one way that we help people get diagnosed faster,” Stiles says. “It’s also really important to raise awareness so that we can interest government and investors and other people to fund research in this group of diseases.”
When it comes to POTS, symptoms can include lightheadedness, nausea, blood pooling and a high heart rate. The most common treatments include increase intake of fluids and salt and, if possible, recumbent exercise.
But even if the symptoms and treatment of POTS appear subtle, it is nothing to take lightly, Stiles says. Thirty per cent of people with the condition rely on a wheelchair to get around and many others are unable to work.
“There are millions of people who really, really suffer from autonomic disorders,” Stiles says. “We want to build support and compassion for these patients in their communities so that they can get access to the resources that they need.”
Dysautonomia International is encouraging those who want to show support during the awareness month to share information with friends and family, participate in events, raise funds and wear a turquoise scarf.
#mask up#covid#pandemic#wear a mask#public health#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2
15 notes
·
View notes
Text
So I saw this and went back and forth on if I was going to do it. I have decided I want to so to start off strong here are days 1-4.
1. Type of Dysautonomia you have: I have Postural Orthostatic Tachycardia Syndrome or POTs. This is a condition in which upon standing up from laying/sitting my heart rate jumps at least 30 beats per minute OR rises above 120 on prolonged standing.
2. Diagnosis Story: I feel like I had some of the “lesser” symptoms for awhile before this but wasn’t too worried about those. But one day my mom was doing my hair and I passed out. We went to the doctor, then to a Neurologist and a Cardiologist. The neurologist couldn’t figure it out with the tests done, the Cardiologist followed a sneaking suspicion did a tilt table and diagnosed me.
3. How long did it take to get diagnosed: I’m one of the luckier POTs people in that my diagnosis came within 1-3 years of the initial main symptom (passing out)
4. My most bothersome symptom: Probably my Presyncope. Because I have to sit or lay down and stop what I’m doing. And I never know if it’s the day that it will go further and become full syncope meaning I passed out. I’m fine if a pass out but I’m still terrified of it.

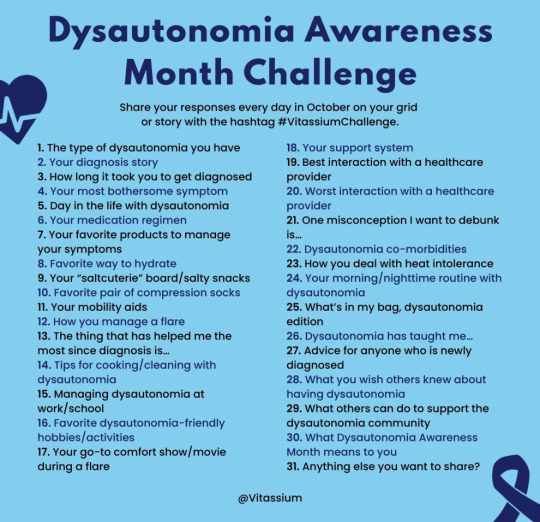
[Image Text: Dysautonomia Awareness
Month Challenge
Share your responses every day in October on your grid or story with the hashtag #VitassiumChallenge.
1. The type of dysautonomia you have
2. Your diagnosis story
3. How long it took you to get diagnosed
4. Your most bothersome symptom
5. Day in the life with dysautonomia
6. Your medication regimen
7. Your favorite products to manage your symptoms
8. Favorite way to hydrate
9. Your "saltcuterie" board/salty snacks
10. Favorite pair of compression socks
11. Your mobility aids
12. How you manage a flare
13. The thing that has helped me the most since diagnosis is...
14. Tips for cooking/cleaning with dysautonomia
15. Managing dysautonomia at work/school
16. Favorite dysautonomia-friendly hobbies/activities
17. Your go-to comfort show/ movie during a flare
18. Your support system
19. Best interaction with a healthcare provider
20. Worst interaction with a healthcare provider
21. One misconception I want to debunk is...
22. Dysautonomia co-morbidities
23. How you deal with heat intolerance
24. Your morning/nighttime routine with dysautonomia
25. What's in my bag, dysautonomia edition
26. Dysautonomia has taught me...
27. Advice for anyone who is newly diagnosed
28. What you wish others knew about having dysautonomia
29. What others can do to support the dysautonomia community
30. What Dysautonomia Awareness
Month means to you
31. Anything else you want to share?]
24 notes
·
View notes
Text
Thank you for the post @micah-has-fallen
[Image Text: Dysautonomia Awareness
Month Challenge
Share your responses every day in October on your grid or story with the hashtag #VitassiumChallenge.
1. The type of dysautonomia you have
2. Your diagnosis story
3. How long it took you to get diagnosed
4. Your most bothersome symptom
5. Day in the life with dysautonomia
6. Your medication regimen
7. Your favorite products to manage your symptoms
8. Favorite way to hydrate
9. Your "saltcuterie" board/salty snacks
10. Favorite pair of compression socks
11. Your mobility aids
12. How you manage a flare
13. The thing that has helped me the most since diagnosis is...
14. Tips for cooking/cleaning with dysautonomia
15. Managing dysautonomia at work/school
16. Favorite dysautonomia-friendly hobbies/activities
17. Your go-to comfort show/ movie during a flare
18. Your support system
19. Best interaction with a healthcare provider
20. Worst interaction with a healthcare provider
21. One misconception I want to debunk is...
22. Dysautonomia co-morbidities
23. How you deal with heat intolerance
24. Your morning/nighttime routine with dysautonomia
25. What's in my bag, dysautonomia edition
26. Dysautonomia has taught me...
27. Advice for anyone who is newly diagnosed
28. What you wish others knew about having dysautonomia
29. What others can do to support the dysautonomia community
30. What Dysautonomia Awareness
Month means to you
31. Anything else you want to share?]
October is Dysautonomia Awareness month and Vitassium has a 31 day challenge. And I want to participate but lack consistency so I’ll prob do them in clumps. Anyways here’s a screenshot of the list :)
See y’all in a few days!
(I’m probably doing Inktober too but that won’t be posted here lol, it’ll be the month of consistency challenges)
49 notes
·
View notes
Text
October is Dysautonomia Awareness Month and I'm catching up on the prompt challenge.
Day 1: type of dysautonomia you have
_ I have POTS (postural orthostatic Tachycardia syndrome)
Day 2 and 3: diagnosis story and how long it took to get diagnosed.
I technically diagnosed myself, I've been having symptoms for over ten years (more than half of my life) and I've finally started researching it - finally when I was in nursing school I learnt about POTS and brought it up with my GP. Finally after three years, actively searching for a diagnosis I found a doctor who took me seriously and diagnosed me.
#dysautonomia#dysautonomia awareness month#pots syndrome#ehlers danlos syndrome#postural orthostatic tachycardia syndrome
19 notes
·
View notes
Text
Dysautonomia Awareness Month Challenge Day 4
What’s the most bothersome symptom?
It’s a tie between presyncope episodes, and frequent urination.
I experience both of these multiple times a day, and when my head doesn’t feel like it’s gonna pop off and fly away, due to lack of blood flow, I urgently have to go to the bathroom every 30 minutes at this point.
I have other serious and bothersome symptoms, but I chose the two that happen the most often multiple times throughout the day.
Here’s my heart rate just getting out of bed this morning. I’ve done nothing but stand up.

#chronic illness#disability#pots syndrome#postural orthostatic tachycardia syndrome#chronic fatigue#spoonie#invisible disability#potsie#hypermobile ehlers danlos
20 notes
·
View notes
Text
Hello October
Keep your eyes on the stars, and your feet on the ground.
Wrapping up September and opening October. There are a few things I'd like to cover in this post, so let's get into it!
#1 How did you all fancy the September blog challenge? Seriously all feedback is welcome. I want to hear your thoughts about it.
#2 What kind of challenges would you like to see in the future or just posts in general? How can I change things up to make it more interesting? Again constructive criticism is welcome I want to hear feedback from my viewers.
#3 October is Breast Cancer Awareness month, but it is also Dysautonomia Awareness month and there's loads more of awarneses I'm sure, but I have Dysautonomia so I low key go awareness crazy during that time.
#4 I will be doing another series but this time it will be a journaling prompt series about goals.
I am looking forward to writing this, I hope you all look forward to reading it. I hope you are having a lovely day/night whenever you are reading it.
Until next time Loves💙
0 notes
Photo


[First Image is a blue and white background with the words "October is... Dysautonomia Awareness Month!" on it. A stick-figure girl says, "Make noise for turquoise!" Second image is a blue and white background with the words, "Introducing Potsie's Awareness Challenge!" on it, followed by a list: 1. How dysautonomia effects you; 2. What dysautonomia looks like; 3. Spoonie hack; 4. Your own POTS Problem; 5. The scariest thing about dysautonomia is...] HAPPY DYSAUTONOMIA AWARENESS MONTH EVERYBODY! This month, I'm hosting a special event over on Instagram, but you're all more than welcome to use the prompts to raise awareness here on Tumblr, too! (There's a special bonus if you participate over on Instagram, though... 😬) Also, I would encourage you all to share my comics this month especially--with your help, we can make lots of noise for turquoise! 🎉 Happy awareness raising!
#dysautonomia#dysautonomia awareness month#pots#postural orthostatic tachycardia syndrome#chronic illness#invisible illness#awareness#challenge#spoonie
213 notes
·
View notes
Text
What You Need To Know
Sjogren’s is an autoimmune disease that can cause a wide variety of symptoms and result in a wide spectrum of severity. It has an overwhelming fondness for women, affecting eight times as many women as men. The average age of diagnosis for women is the early 50s; the average age for men is the late ‘50s, but Sjogren’s can occur at any age. The portion of the general population who have Sjogren’s syndrome is not known; studies vary widely in their findings, from a fraction of 1% to 7% of the elderly population. Better research on prevalence is needed, as is a standardized set of diagnostic criteria. It’s important to note that elderly folks have Sjogren’s 7-8 times as often as do people in their twenties. Sjogren’s can leave patients bedridden, but many patients are very active with only bothersome dryness of their eyes and/or mouth that doesn’t affect their lives significantly. 84% of Sjogren’s syndrome patients are women. One-third of us (including me) have small fiber nerve damage that causes complications in their autonomic body functions. Some I’ve spoken to have damage to organ valves, some even die of the resultant heart or kidney disease. The folks whom I’ve met who bother to talk to other patients online are often very ill, and have become desperate to learn more about their complicated conditions. Please don’t visit a support group and assume you’re going to be just as bad off as the folks online. We are home and online because we’re too sick to do much else. Many complain that their family doctors are ill-informed or that they aren’t giving them enough information. The recent influx of studies on Sjogren’s syndrome and our related conditions make keeping up with the current literature a must for the doctors who care for us. All About Moisture and the Lack of It People with the disorder experience Sjogren’s in various ways. Some are barely inconvenienced, some lives are altered drastically by the profound fatigue that is a major hallmark of the disease (we’ll be talking a lot about fatigue later on). Some of us are in constant pain due to small and large fiber nerve damage, others suffer sporadically with gland inflammation. Some Sjogren’s patients are merely bothered by dry eyes and take a prescription that keeps that issue in check. They may always be able to manage their illness with little difficulty. These people may live and die with barely a hitch in the course of their lives. Others must use artificial tears regularly throughout the day and suck on hard candies or chew gum to keep their mouths moist. There are prescription pharmaceutical remedies for both these issues when over-the-counter remedies are no longer enough. Women with Sjogren’s can experience vaginal dryness that makes it too painful to have male/female sexual intercourse. Pain during intercourse is often described. A lack of ability to perspire can interfere with body temperature regulation. Some of us produce so little saliva that we are unable to keep our teeth from rotting out of our heads no matter how diligently we brush, rinse and floss. Many middle-aged folks in my Facebook support groups already have dentures or tooth implants. Some of us lose their voices due to lack of mouth moisture to lubricate their throats. Singers with Sjogren’s syndrome often notice a raspiness due to laryngeal tissue damage from drying out. Some singers have to give up singing altogether. A few SS patients even completely lose their ability to speak due to throat tissue damage. Wide Spectrum of Central Nervous System Complications As of this post, some small studies suggest that about 30% of Sjogren’s patients have small-fiber nerve disease as found by skin punch biopsy. There is some speculation that small-fiber damage can progress to large-fiber nerve damage; a small, but significant percentage of patients show damage to myelinated large-fiber nerves. Small-fiber nerve damage is common in SS; this kind of nerve regulates the function of autonomic systems; damage to these nerves leads to a wide variety of dysfunction to body processes that occur without our conscious effort. This condition is called dysautonomia. We don’t have to think about each breath, or each heartbeat for them to keep going, or about pushing our blood or food through our digestive tracts or accessing oxygen or glucose or the uptake of trace minerals. It’s worth noting that recent studies show that up to 62% of fibromyalgia patients actually have small-fiber neuropathy to blame for their muscle pain and spasms. Dysautonomia is a health problem caused by our central nervous system’s inability to properly carry out our autonomic functions, which is everything our bodies do unconsciously, that is, without our consciously directed effort. Some autonomic functions include: 1. Breathing 2. Sleeping 3. Digestion 4. Heartbeat 5. Hormone release 6. Body temperature regulation 7. Sweating 8. Balance 9. Sensory feedback 10. Storing memories - that memory loss is an autonomic function is speculative on my part. Emerging research has us closer than ever to a solid understanding of the memory storage process and the physical existence of engrams, the place where our long-term memories are thought to be. Many Sjogren’s patients report memory and cognitive issues (often called “brain fog” by patients). Many patients report losing jobs because of not being able to keep a train of thought or get enough done in a timely manner. Indeed, this was my chief complaint. I could have kept on with school, I could have withstood the muscle pain, dizziness and fatigue if only I was able to think like I used to. But, no, all of me was tired straight through, especially my brain. Even now, I try to do all intellectually challenging things in the morning when I am sharpest. Many Sjogren’s patients also have dysautonomia. We can’t always depend on a regular heartbeat, the ability to swallow smoothly, to be able to sleep well, to properly digest our food, or even to regulate our body temperature. Heatstroke is always a possibility in hot weather and can come on suddenly after even a short exposure to hot, humid conditions. Dysautonomia is related to small-fiber neuropathy, but it’s not clear exactly how. Even taking a shower can be challenging if we try to shower in the warm temperatures we used before we got sick. One woman in my Facebook support group reports that her doctor advised that she not even go outside when the temperature (in Fahrenheit) and humidity together add up to 150 or more. I have heard over and over people say that just the effort of taking a shower tires them out so much that they have to go back to bed. I have been there many times! Talking to Your Doctor If you’re really lucky, you have a GP who is familiar with Sjogren’s syndrome. Unfortunately, there is so much new info coming into medicine, our family doctors may not familiar with recent research on the disease and may still think it’s a rare condition or a condition that only affects salivary and lacrimal glands. For this reason, we may need for our rheumatologists to behave as the doctor who coordinates our various medical specialty needs. Please encourage your rheumatologists and family doctors to become more familiar with this condition as it is still under-diagnosed. Ask whether they would appreciate being updated by you; offer to bring in new research papers. You may not be able to bring in the full studies due to paywalls, but you can bring in the abstract; it will give your doctor enough info to look up the full study if s/he has an account with his university library, Medline or Pub Med, etc. Spreading awareness is important: Early detection can lead to disease-modifying treatment. That is, there are drugs that can prevent further damage in Sjogren’s patients who tolerate it. There is research going on right now that may result in a vaccine for us in just a few years. I encourage everyone to join The Sjogren’s Foundation (www.Sjogrens.org) to receive ongoing updates on the state of our condition. Patients are best-served when they are being looked after by a good rheumatologist. A good rheumy will know that your Sjogren’s can cause widespread pain from nerve damage as well as deep fatigue. Check the rheumatology staff of your local teaching hospital if you’re having a hard time finding a knowledgable doctor. I’ve found good specialists by seeing who, locally, was publishing research on my condition. I realize that not everyone lives near teaching hospitals, but it can be worth the trek to the nearest big city if you’re only seeing your rheumatologist every 6 months or so, as most of us do once all the diagnostic interaction between you and your doctor’s office is done. Unless a physician has a particular interest in Sjogren’s syndrome, they may not even be aware that it is as widespread as it is now known to be. Recently thought to be a rare disease, Sjogren’s is now thought to occur in 3-5% of the population. That makes it one of the most common autoimmune diseases, only lagging after rheumatoid arthritis. Even less-understood is the complication of small-fiber neuropathy (SFN). Approximately 30% of Sjogren’s patients suffer with it. Patients report that even their neurologists aren’t up on the fact that SFN can cause pain and spasms as this is relatively new information that they didn’t get in medical school. Have a detailed conversation with your general physician about the many aspects of Sjogren’s syndrome and make sure that the two of you are a good fit. Small-fiber neuropathy is painful and can be debillitating; it can impede all physical function because of the wide-spread muscle and connective tissue pain it can cause. SFN is a factor in the disruption in autonomic dysfunction that can lead to serious complications. It’s worth knowing that up to 1/3 of us have SS-A and SS-B negative blood tests. Remember, absence of evidence is not evidence of absence. You are welcome to tell us about your journey to diagnosis or your dissatisfaction with not getting a prompt one. Was it hard for you to get a diagnosis? Please tell us your experience! Sources - I’ve done a whole lot of reading since my diagnosis in February of 2018, but the studies and articles I consulted for this particular blog, are listed below. From Engrams to Pathologies of the Brain - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5383718/ Small Fiber Neuropathy: Disease Classification Beyond Pain and Burning - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5912271/ Sex differences in Sjögren’s syndrome - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4630965/ Small-fiber neuropathy: Expanding the clinical pain universe - https://www.ncbi.nlm.nih.gov/pubmed/30569495 Primary Sjogren’s syndrome with central nervous system involvement: https://pdfs.semanticscholar.org/f2ee/a33c57f84283a4cd882294ad75fcc73e8232.pdf Sjogren’s syndrome disease info - https://www.hopkinsmedicine.org/health/conditions-and-diseases/sjogrens-syndrome Sjogren’s Center at Johns Hopkins - https://www.hopkinssjogrens.org/ Varied prevalence reported in large epidemiological survey - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4122257/ The Sjogren’s Syndrome Foundation - https://www.sjogrens.org #Sjogren's diagnosis#Sjogren's#Sjogren's symptoms#fatigue#deep fatigue#autoimmune#spoonie#chronic#profound fatigue#fatique#small fiber neuropathy#autonomic disorder#autonomic#dry eyes#dry mouth
1 note
·
View note
Text
LOL, that Dysautonomia Awareness Challenge has gone just as I expected - nothing since the 4th.
Anyway, here's Wonderwall
5) Day in the life with Dysautonomia
This one is difficult, not just because dysautonomia is a dynamic condition, but also because I have 500 other things going on that impacts my day in similar ways.
I can tell you that it means I can't stand for very long, even indoors.
I end up sitting on the floor when in conversation with someone, unless there's a chair nearby. If I go out (ha) that used to mean sitting on the filthy shop floor, but now I have a wheelchair. Otherwise I have to hang onto my sister or my mum on short trips outside.
The dizziness and faint feeling makes me feel weak and feeble, which is REALLY annoying. A spell can hit at any time, so I have to either do little projects I can drop in the middle without too much stress, or have someone assisting who can finish the task/get it to a stopping place without me.
Can't eat, tremors. Can't stand, tremors. Can't hold still, tremors.
Can't go in the back garden for any length of time without making sure there's a chair out there or bringing my rollator.
No spontaneity. No independence.
This question is depressing, next!
6) Your medication regimen.
I take a few meds, but the one I take for my dysautonomia is ivabradine. One in the AM, one in the PM, to slow my heart and hopefully help with the palpitations.
Eh, so-so. I certainly get the side effect of light suddenly glaring when I move outside of a dark room.
Otherwise, I used to drink a lot of water, but fell off that wagon. I have compression stockings, but only under the knee because I can't manage the full tights version I was supposed to wear.
All in all, my pandysautonomia isn't really being managed by meds.
7) Your favourite products to manage your symptoms.
Products? Compression socks help, but I hate them. I like Lucozade Sport for electrolyte replenishment, but it's too expensive for me to have a constant supply.
I like 4Head strips for when my temperature regulation goes out of whack.
Uhhhh… it's not really managed, tbh.
8) Favourite way to hydrate.
Pepsi Max.
But no, I like the cute water bottles and all, but I don't have the spoons to wash them out and they get funky and then I don't use them.
Lucozade Sport, again, is good, but, again, it's too expensive for me to rely on that alone.
I got electrolyte salts, but I think they triggered a migraine.
9) Your "saltcuterie" board/salty snacks
UGH, this one pisses me off.
For fuck's sake, dysautonomia isn't just POTS, and it isn't just POTS with low blood pressure, either.
People with high blood pressure, or just all over wacky blood pressure, can also have dysautonomia. Hell, can also have POTS.
And high salt diets are contraindicated for people with high BP and dysautonomia.
I feel like shit like this is just quirkifying dysautonomia into a collection of hashtags and memeable pics.
And what's more, leaves huges groups of people who DO have POTS or other dysautonomic conditions thinking that they can't possibly have POTS because they don't have low BP like the entire internet tells them they need in order for a diagnosis.
Seriously, you can't diagnose this kind of thing online.
You can't 'informed self-DX' dysautonomia.
Can you suspect it? Sure. And if doing all the 'typical' POTS things like increasing salt in your diet and wearing compression socks helps, go for it.
But you'll never know if you actually have POTS or if something else is causing your symptoms, whether it's another form of dysautonomia or something else altogether. Like just having low blood pressure.
And I know that's easy to say, like seeing a doctor for this is simple when it's not, but seriously. Some things you just can't diagnose yourself online.
10) Favourite pair of compression socks
I hate them all. I was supposed to get a pair prescribed, but my GP and pharmacists are all too incompetent and stupid to understand how to do so, so I just bought the right strength myself off Amazon.
THEY SUUUUUCK. I struggle to get them on, they aggravate my dermographia and I can't regulate my temperature properly in them because they make me feel hot all the time.
Sucks.
11) Your mobility aids.
I use a rollator inside the house sometimes, in places like the kitchen where I need to stop and talk to someone but don't want to sit on the cold, hard floor. I use it outside in my back garden so I can walk around a little but not have to crouch or sit in the grass, given that I can't just stand there for very long.
I used to have a manual wheelchair, but I don't have the strength to push myself, and I don't have the stamina to be able to do so. I go a chair BECAUSE I don't have the stamina to stand, and I wanted to have a little left over when I got back home so that a grocery shopping trip didn't leave me in bed for the next 3 days.
The manual chair wasn't doing that so I switched to a powerchair and it's wonderful. Yeah, there are drawbacks (battery life, dead-end corridors, narrow doorways, manouverability, STEPS FOR NO REASON) but I can go to Tesco or the garden centre and buzz around for an hour or an hour and a half and come home and be tired but still able to sit upright.
12) How you manage a flare
Literally, by dropping to the floor. If I'm having a really symptomatic day, I'll either spend it in one place (my bed or the couch usually) or I'll make really short trips of a few steps at a time and then sit to rest before continuing.
Hate it.
13) The thing that has helped me the most since diagnosis is…
Diagnosis it self has helped with the imposter syndrome A LITTLE.
It's helped me understand what's going on with my body in relation to my other health issues more as well.
I can tell people I have pandysautonomia without uhmig and ahing and adding footnotes to it, and it's helped me when telling benefits that no, I can't stand actually.
14) Tips for cooking/cleaning with dysautonomia
I can't do either. Maybe pick up little bits of rubbish and put them in the little bin in my room, but I can't cook for myself and I can't do any large cleaning duties either.
For smaller tasks, I'd probably say, wait for a day where you've had a rest, where you know you can rest afterwards (for the next day or two), you have no big trips out or mentally draining tasks coming up, etc.
Break the task into small parts and see what you can do while sitting down, leave those for a bad day.
Do little and often, if you can.
Don't expect yourself to be able to complete a task all at once. Make small, achieveable goals.
But mostly, have a carer. IDK how I'd manage without my mum. I'm not going into a rant about the quality of life disabled people have at higher expense in order to just live, I'm not.
15) Managing dysautonomia at work/school
Lol, I can't work like this. I was fired from my job of 10 years for my migraines, and I developed pandysautonomia a few years later. I can barely spend time out of bed and downstairs most days, I physically can't work. What are you, the DWP?
16) Favourite dysautonomia-friendly hobbies/activities
WRITING!
Writing most of all.
Puzzle app on my phone
Plants are good, because they only need a little sporadic care, depending on what you get, and research is sometimes something I can do in a flare, depending on brain fog.
Keeping inverts. Tarantulas are good because they need infrequent feeding and really simple care, bioactive enclosures that don't need deep cleaning like a hamster cage or litter box might.
Inverts of all kinds, really, except the tiny ones that need tiny food because flies are a pain in the butt to work with.
Reptile keeping is also pretty easy, depending on the reptile and how you keep them. Surprisingly low maintainence, but it's also really easy to do in short bursts at infrequent intervals.
I like artistic pursuits, but they're hard in a flare up when the tremors get bad and I stop being able to lift my arms.
At the moment my favourite hobby is planning out my fish tanks, also pretty easy if you've got help for water changes, and really nice if you're having a migraine but can't sleep.
17) Your go-to comfort show/movie during a flare.
Adventure Time.
Generation Kill.
My Neighbours the Yamadas
There are others (Always Sunny, Over The Garden Wall, Inside Man (not the David Tennant one), Knightmare (old TV show on YouTube), Animals of Farthing Wood, Bob's Burgers, Fight Club, various anime) but those are the main three.
#dysautonomia awareness month#dysautonomia awareness month quiz#pandysautonomia#dysautonomia#pots#postural orthostatic tachycardia syndrome#chronic illness#dysautonomia awareness challenge
0 notes
Photo

Since its EDS awareness month I figured I'd give the challenge a go just to raise said awareness... I'm a few days behind so... 1. What type do you have? Hypermobile 2. When were you diagnosed? Pass? Quite a long while ago! 3.What comorbidities do you have? Dysautonomia 4. How bendy are you? 8/9 on the Beighton Scale 5. Are you stretchy? Sort of. In some places my skin is overly stretchy! . . . #eds #ehlersdanlossyndrome #spoonie #heds #edsawarenessmonth #edschallenge #edsformay
7 notes
·
View notes
Text
Dysautonomia post #1 (Days 1-3)
Day 1: The type of Dysautonomia you have
- I don’t yet know what specific type I have yet as I’m still in the official diagnosis phase. But my guess is something similar to POTS.
Day 2: Your diagnosis story
- I’m still in the diagnosis phase. I’ve been experiencing symptoms since age 11 and they’ve progressively just gotten worse and worse. They just ran a one week long heart monitor on me and I’m awaiting those results but itll definitely be a long process. (It took so long to seek help because my mom experiences similar things and really doesn’t want a diagnosis so she didn’t get why I should want one)
Day 3: How long it took you to get diagnosed
- As mentioned before it’s been almost six years fighting to even get to see the doctor. As of right now I’ve been in the official process for about six months. So who knows.

#vitassium#POTS#pots syndrome#dysautonomia#dysautonomia awareness#disability awareness#ehlers danlos syndrome#EHDS#month challenge#NCS#neurocardiogenic syncope
0 notes
Text
10 Ways Yoga Will Improve Your Life
It's an improperly concealed that I have some illness. I was born with a problem called dysautonomia, which suggests my free nerves does not quite work right.
This effects my heart, my mind, my digestion, my energy levels, and also my sleep patterns. For several years I was a miserable accident incapable to do things regular individuals do.
But then I discovered yoga. Yoga has literally changed my life, and also it is as a result of this makeover I do what I do.
I am persuaded I am not the only person that can attain such change via yoga. You don't have to have some hard-to-spell illness to see benefits from yoga exercise.
Here are 10 methods yoga exercise can transform your life.
1. You'll be calmer.
Yoga is understood for its relaxing residential properties and comforting reflections. My favourite component of yoga is the meditation at the beginning as well as completion where I could attach with myself as well as my practice. I have never ever strolled away from yoga exercise stating, 'Male, I'm upset.' I always leave the mat sensation calmer as well as a lot more kicked back than when I took place the floor covering.
2. You will certainly transform into more flexible.
There is a myth that yoga exercise is for super-bendy skinny individuals. I can not tell you the number of times I heard, 'I can't do yoga. I'm not adaptable sufficient.' You do yoga to come to be flexible. A routine yoga method will certainly increase your flexibility throughout the board. If you ever before spent your youth thinking concerning doing divides, begin yoga, and you will work your way up to divides.
3. You will become stronger.
Another justification I typically listen to is, 'I'm not solid sufficient to do yoga exercise.' Yoga exercise positions need a particular quantity of toughness to begin with, yet that isn't really to state they're difficult. You do not need to be Superman to be able to do yoga. You do not even have to have a normal strength-building fitness center routine. Yoga exercise presents can be customized for your present toughness level, as well as the even more you do them, the stronger you become. You will slowly however undoubtedly work your way up from modified slab to full slab to holding chatarunga for 5 minutes.
4. You will certainly discover your internal strength.
Holding chatarunga for an impressively much time amount of time isn't really the only toughness you will plant. You will certainly likewise cultivate inner strength. A normal yoga practice will certainly show you ways to stay with a routine, it will certainly show you self-discipline. You will certainly discover the best ways to do something also if you're uninspired, and also you will certainly discover the best ways to take those lessons you discovered on the mat off the mat. You will find your stamina off the mat as well. There is power as well as self-confidence in understanding, 'I just did crow for 10 seconds longer compared to before.'
5. You will transform into much more energetic.
Studies show normal workout increases your power degrees. ' In contrast to popular belief, working out doesn't make you tired-- it actually creates power in your body. Your body rises up to meet the difficulty for more power by ending up being stronger,' nutritional expert Samantha Heller told WebMD.
Moderate workout, like a 45 minute vinyasa class, can boost your energy levels throughout the day. Make it a routine technique, and also you'll continually have even more energy.
6. You will be much more harmonic with your body.
When you're doing yoga, you must be focusing on your body, breath, alignment, and activity. This focus will certainly affect your perception and awareness off the floor covering. You will come to be more mindful of just what's going on with your body. You will understand if the placement you're attending the sofa isn't supportive. You will certainly come to be much more knowledgeable about the tiny, minute modifications in your body. - Perhaps to a frustrating level. When I began doing yoga a lot more regularly, I started seeing traits in my body I didn't notice previously. A muscular tissue twinge right here or there. It's enough to drive one to hypochondria if one isn't careful.
7. You will begin sleeping better.
Sleep deprivation is typical amongst Americans for a number of factors. Bedtime procrastination, sleeplessness, too much anxiety, a lot of dedications, loud sounds, light, and also many other points can trigger rest interruption. Yoga exercise could in fact aid you get your sleep back on the right track.
According to a research study from the National Facility for Biotechnology Info, yoga was verified to be a secure as well as effective means to boost sleep in older grownups. While I have yet to locate a research that looked into the impacts of yoga exercise on rest top quality for young adults, I also have yet to find any kind of studies that show yoga rises insomnia. Unscientific evidence does recommend those who do yoga exercise on a regular basis sleep better than those who don't.
8. You will certainly boost your posture.
Part of hearing your body includes boosting your position. When you're a regular yoga exercise practitioner, your pose normally enhances due to the fact that you begin to observe when you're slumping over. Yoga concentrates on positioning, as well as if your back isn't really properly aligned because you're dropped over your TPS reports, you'll observe.
You may not notice as quickly as you begin to slouch, however after a couple minutes your body will certainly notice it's not straightened in a helpful means. When you're slouching, it gets challenging to breath. A lightheaded experience is normally the trigger for me that I'm not sitting in a helpful way.
I love having far better pose. I really feel a lot more certain. I really feel stronger, and I even seem like a princess. Who does not wish to really feel like aristocracy?
9. You will certainly learn just how to breathe.
When we are kids we are educated we understand exactly how to take a breath, taking a breath just comes normally. After all, it becomes part of our autonomic nerves. When I first heard this, I didn't think it, and also held my breath as long as feasible, established to confirm breathing is unneeded. (Ends up 7-year-old me was incorrect) But even if breathing is something we do normally doesn't indicate we cannot learn how to do it much better. Yoga exercise instructs you to straighten motion to breath. Pranayama exercises teach you the best ways to manage your breath to lower your heart price, relax your mind, or increase your power. All are powerful abilities to have.
10. You will certainly boost your immunity.
Regular exercise is shown to boost your resistance, although researchers typically aren't specifically certain why. There is a theory that posits exercise sends out antibodies and leukocyte as a result of the body at a much faster price because of a rise in flow. The increased rate of distributing antibodies and blood cells may activate the release of hormones that caution the immune cells of germs as well as infections.
This can extremely well belong to the reason I have not obtained unwell yet this winter months. By January I am generally sick two or 3 times. Maybe yoga exercise has actually saved me from obtaining respiratory disease.
These are simply a few of the means yoga can transform your life. Are you a yogi? Exactly how has yoga altered your life? Let me know in the comments.
2 notes
·
View notes
Text
Dysautonomia Awareness Month Challenge
Day 4: my most bothersome symptom
My most bothersome symptom would honestly be when I have to go from sitting to standing and my heart rate shoots and I have to take a moment to work out whether or not I have to take a seat or if I can keep going (high potential for passing out)
Day 5: day in the life with POTS
I have to change positions slowly (going from sitting to standing). However, this usually isn't an issue, considering I'm standing most of the time for work. I also try my best to stay as hydrated as possible - usually with electrolytes when I'm having a flare up. I also use a shower chair to reduce the risk of passing out in the shower.
Day 6: Medications
At the moment I only take propanalol to control my heart rate
Day 7 and 8: Favourite products to manage symptoms
- ice packs to reduce temperature
- fans/aircon to help with overheating
- hydralyte_electrolytes_ for hydration (this also counts as day 8 - favourite way to hydrate)
- I wear compression socks
- SALT!!! I carry salt packets with me everywhere
Day 9: my "saltcuterie" board
- i love miso soup and eat it quite often
- salt and vinegar chips
- pickels
- popcorn
- toast with hummus, smoked paprika, cayenne pepper and salt
3 notes
·
View notes
Text
Dysautonomia Awareness Month Challenge Day 1
What type of Dysautonomia do you have?
I have Postural orthostatic tachycardia syndrome
Also called: POTS
Postural orthostatic tachycardia syndrome (POTS) is a condition that causes your heart to beat faster than normal when you transition from sitting or lying down to standing up. It’s a type of orthostatic intolerance.
The symptoms of POTS include but are not limited to lightheadedness (occasionally with fainting), difficulty thinking and concentrating (brain fog), fatigue, intolerance of exercise, headache, blurry vision, palpitations, tremor and nausea.
#chronic illness#disability#pots syndrome#postural orthostatic tachycardia syndrome#October#dysautonomia#dysautonomia month#invisible disability#potsie
25 notes
·
View notes