#dna repair
Explore tagged Tumblr posts
Text
Sunburns and aging skin are obvious effects of exposure to harmful UV rays, tobacco smoke and other carcinogens. But the effects aren't just skin deep. Inside the body, DNA is literally being torn apart. Understanding how the body heals and protects itself from DNA damage is vital for treating genetic disorders and life-threatening diseases such as cancer. But despite numerous studies and medical advances, much about the molecular mechanisms of DNA repair remains a mystery. For the past several years, researchers at Georgia State University have tapped into the Summit supercomputer at the Department of Energy's Oak Ridge National Laboratory to study an elaborate molecular pathway called nucleotide excision repair (NER). NER relies on an array of highly dynamic protein complexes to cut out (excise) damaged DNA with surgical precision. In their latest study, published in Nature Communications, the team has built a computer model of a critical NER component called the pre-incision complex, or PInC. PInC plays a key role in regulating DNA repair processes in the latter stages of the NER pathway. Decoding NER's sophisticated sequence of events and the role of PInC in the pathway could provide key insights into developing novel treatments and preventing conditions that lead to premature aging and certain types of cancer.
Continue Reading.
80 notes
·
View notes
Text
Word Sound Power
#the mc#new day#todays a new day#cymatics#hip hop#jamaican rapper#rap#affirmations#morning motivation#morning meditation#self talk#chakras#dna repair#music therapy#healing tones#Spotify#dope#bars#lyricist
5 notes
·
View notes
Text
Why we don't all have skin cancer from going outside
What is sunburn? Why does tanning give you skin cancer? The answer has to do with how UV rays fuck up your DNA.
There are three types of UV light: A, B, and C. UVC is absorbed in the atmosphere. UVA and UVB are what sunscreen protects against because they do the damage to your skin. Why do they do damage? UV light has a lot of energy, which can cause the bonds between molecules to change.
Onto DNA. This is the instructions for how to make you. It's made of nucleotides, four of them: Adenosine, Guanine, Cytosine, and Thymine. Thymine and Cytosine are what we call pyrimadines (the other two are called purines). Normally, in double-stranded DNA (that beautiful helix) a pyrimadine on one strand is paired with a purine from the other to make a "rung on the ladder" of dsDNA. (A goes to T and C goes to G).
What happens when UV light penetrates the skin and hits DNA? A pyrimadine dimer. So what this means is that two pyrimadines (usually Thymines) on the same strand have disconnected from their purines and bonded to each other. This creates a weird knob on the strand, and is a type of DNA lesion. Lesions can induce other mutations in the code. The dimer cannot be read by enzymes correctly either. This is all very bad, and can lead to cancer. Cancer = mutation
How do we fix this? So this is happening all the time. 100x per cell per second that your skin is exposed to sunlight. But we aren't all riddled with skin cancer because of Nucleotide Excision Repair. This is a form of DNA repair where the shitty nucleotides (the two bonded pyrimadines) are cut out. DNA polymerase synthesizes a new segment of DNA, and DNA ligase attatches it all back together. Now your DNA is fixed.
What happens when NER doesn't work? Very bad things. One condition where this repair pathway is impaired is Xeroderma pigmentosum. These people cannot repair damage from UV light and develop severe sunburns from only minutes in the sun. They will also get skin cancer and cataracts. Historically, people with this disease have been referred to as vampires, as they can only go out at night. Just shows how important your DNA repair mechanisms are and how much work they do around the clock.
#med student#medical school#medicine#biology#med school#med studyblr#xeroderma pigmentosum#uv light#sunburn#sunscreen#tanning#dna#dna mutations#mutations#dna repair#nucleotide excision repair
4 notes
·
View notes
Text
Brain cancer "going APE": here is its way to resist TMZ and leave DNA repair BEReft of options
In spite of intensive research, glioblastoma remains one of the most lethal types of brain cancer. Despite there are several available medications, temozolomide (TMZ) is the front-line drug in its treatment; while TMZ effectively penetrates the brain and targets tumors, its success depends on the tumor cells attempting to repair the DNA damage caused by the drug. Unfortunately, glioblastomas…
#APE-1#base excision repair#brain cancer#cancer cells#cellular aging#DNA polymerase#DNA repair#glioblastoma#temozolomide
2 notes
·
View notes
Text
The team believes that gars have an unusually strong DNA repair apparatus. This allows the fish to correct somatic and germline mutations. They found that the gars’ DNA consistently evolves up to three times more slowly than any other major group of vertebrates.
2 notes
·
View notes
Text
A recent study reveals the crucial role of the CDK9-55 protein in regulating DNA repair during cell division, which helps prevent mutations that can lead to cancer. The research highlights how CDK9 interacts with other proteins like CDC23, offering new insights for developing targeted cancer therapies aimed at improving DNA repair and slowing tumor growth

0 notes
Text
432 HZ Frequency Pure Tone • Raise Your Vibration • Deep Healing for Body & Soul • DNA Repair
youtube
432 HZ Frequency Pure Tone • Raise Your Vibration • Deep Healing for Body & Soul • DNA Repair
432 Hz is often regarded as one of the most harmonious and natural frequencies, sometimes referred to as the “heartbeat of the Earth” due to its connection to the Earth’s frequency, also known as the Schumann resonance. This frequency is known for its calming and healing properties, promoting mental clarity, emotional balance, and a sense of universal connection. While 432 Hz does not traditionally correspond to any single chakra, it is frequently associated with the Heart Chakra (Anahata) because of its ability to foster inner peace, emotional healing, and a sense of unity.
Key Aspects of the 432 Hz Frequency: • Emotional Balance and Harmony: 432 Hz is known for promoting emotional balance and inner peace, making it an ideal frequency for relieving stress and anxiety. • Natural Resonance with Earth: This frequency is thought to align with the natural frequency of the Earth, creating a feeling of connection and unity with the world around you. It’s known to promote relaxation and synchronize the body’s natural rhythms with the environment. • Healing and Clarity: 432 Hz is said to encourage clarity, both mentally and emotionally. It can help release tension and restore balance, leading to greater mental focus and emotional stability.
432 Hz and its Association with the Heart Chakra: While 432 Hz is not explicitly tied to any particular chakra, its qualities of emotional healing, peace, and unity resonate strongly with the Heart Chakra (Anahata): • Heart Chakra (Anahata): Located in the center of the chest, the Heart Chakra is associated with love, compassion, empathy, and connection. Since 432 Hz promotes harmony, connection, and emotional balance, it naturally complements the Heart Chakra’s themes of love and unity. Listening to 432 Hz can enhance the Heart Chakra’s energy, helping to open the heart, foster compassion, and create a deep sense of inner peace.
0 notes
Text
youtube
0 notes
Text

TSRNOSS, p 816.
#capillary damage produced by glucose#longevity of women#superoxide dismutase#DNA repair#toxins#malaria#Red Tide#herbivores#cryptobiosis#spores#lngfish#Brownian motion#thermal conductivity of ice#satyendra sunkavally#theoretical biology#manuscript#cursive handwriting#notebooks#diaries
0 notes
Video
youtube
DNA Repair Meditation 432 Hz Binaural Beats
1 note
·
View note
Text
youtube
#Protein arginine methyltransferase#PRMT inhibitors#epigenetics#arginine methylation#gene expression#DNA repair#RNA processing#signal transduction#cancer therapy#neurodegenerative diseases#cardiovascular disorders#targeted therapies#drug discovery#cellular processes#therapeutic strategies#PRMT dysregulation#epigenetic modulation#precision medicine#small molecule inhibitors#biomedical research.#Youtube
0 notes
Text
DNA repair going APE and strand breaks fixing with ATM: please no cash, just redox and contact bases
New research from a team of genome scientists and DNA damage response (DDR) experts breaks new ground in understanding the function of a protein currently limited in clinical trials for cancer treatments. The new investigaton shows how ATM-mediated signaling is induced by DNA single-strand breaks (SSBs) for DNA damage repair – illuminating the distinct mechanisms of SSB-induced ATM kinase and…
#APE-1#chemotherapy#DNA bases#DNA damage#DNA repair#heart failure#oxidative stress#protein kinase#reactive oxygen species#redox biology#transcription factors
0 notes
Text
youtube
MI - 528 Hz | pure tone | Solfeggio Frequency | Transformation, Love and Miracles (DNA Repair)
1 note
·
View note
Video
youtube
528 Hz Healing Frequency: Repair DNA, Inspire Change, Miracle Tone - Pro...
1 note
·
View note
Text
#528 Hz#Love Frequency#Miracle Tone#Sound Healing#Meditation#Solfeggio Frequencies#Chakra Balancing#Green Color#Heart Chakra#Emotional Healing#DNA Repair#Alternative Healing#Spiritual Growth
0 notes
Text
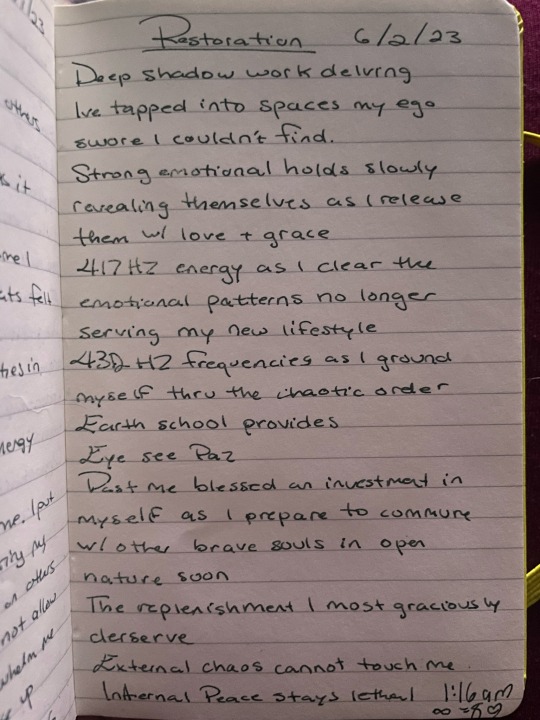
Just for Today, 6/2/23: Present P Power 🌳🌺
Right Now is powerful.
0 notes