#antiepileptic drugs
Explore tagged Tumblr posts
Text
youtube
#Epilepsy#LEAT#brain tumors#ganglioglioma#dysembryoplastic neuroepithelial tumors#DNET#seizure development#antiepileptic drugs#tumor-associated epilepsy#neuro-oncology#seizure management#surgical resection#epilepsy pathophysiology#diagnostic challenges#low-grade tumors#neurology#quality of life#clinical neuroscience#prognostic factors#emerging therapies.#Youtube
0 notes
Text
0 notes
Text
https://www.pharmanucleus.com/reports/epilepsy-therapeutics-market
#Epilepsy Therapeutics Market#Epilepsy treatment#antiepileptic drugs#seizure management#epilepsy research#neurology#therapeutic options#global market trends#epilepsy medications#patient care#epilepsy therapy
0 notes
Text
Epilepsy: Causes and Symptoms Explained
Epilepsy is a neurological disorder that affects millions of people worldwide. It’s characterized by recurrent, unprovoked seizures, and understanding its causes, symptoms, diagnosis, and treatment options is crucial for both individuals living with epilepsy and their care providers. In this blog, we’ll break down the essential aspects of epilepsy, including its causes and symptoms, explained in…

View On WordPress
#Antiepileptic drugs#Brain abnormalities#EEG (Electroencephalogram)#epilepsy#Epilepsy awareness#Epilepsy causes#Epilepsy diagnosis#Epilepsy FAQ#Epilepsy information#Epilepsy management#Epilepsy prevention#Epilepsy support#Epilepsy surgery#Epilepsy symptoms#Epilepsy treatment#Living with epilepsy#Neurological disorders#Seizure disorders#Seizure types#Vagus Nerve Stimulation
0 notes
Text

Buccal midazolam for epilepsy
6 notes
·
View notes
Text
Lyrica® (Pregabalin): Uses, Safety, and Side Effects
🌟 Discover how Lyrica® helps manage neuropathic pain & epilepsy. Learn about its uses, side effects, dosage, and safety tips. #HealthTips #LyricaGuide 🔗
Lyrica® is a prescription medication that contains pregabalin, a widely used anticonvulsant and pain-relief medicine. It is primarily prescribed for neuropathic pain and epilepsy, offering significant relief to individuals suffering from these conditions. This guide will provide a thorough understanding of Lyrica®, including its uses, safety precautions, dosage, and potential side effects.…

View On WordPress
0 notes
Text
Antiepileptic Drug Market Trends, Analysis and Forecast
The global antiepileptic drug (AED) market is projected to grow at a CAGR of around 2% from 2021 to 2027. This growth is fueled by the continuous development of new drugs and increasing research efforts to produce more specific and effective treatments for epilepsy. According to the World Health Organization (WHO), epilepsy affects approximately 50 million people worldwide, making it one of the most prevalent neurological disorders globally.
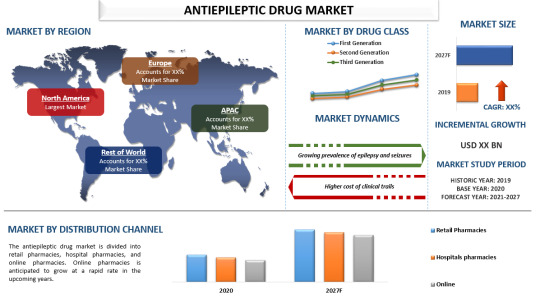
Key Market Drivers:
1. Increasing Prevalence of Epilepsy: With around 50 million people affected globally, the demand for effective AEDs is substantial. The increasing incidences of other neurological disorders and prenatal injuries also contribute to the rising number of epilepsy cases.
2. Advancements in Drug Development: Ongoing research and development efforts aim to create more effective and targeted AEDs. This innovation is crucial for enhancing patient outcomes and minimizing the side effects of existing treatments.
3. Impact of COVID-19: The pandemic has had a mixed impact on the market. While the financial stability of the private healthcare sector was challenged, leading to delays in clinical trials and research, the ongoing need for effective epilepsy treatments remains unchanged, driving demand in the long term.
For a comprehensive analysis of the market drivers, visit https://univdatos.com/report/antiepileptic-drug-market/
Market Segmentation:
1. By Drug Class:
- First Generation: Established treatments with a long history of use.
- Second Generation: Held a significant market share in 2020 due to their efficacy in slowing brain impulses and controlling seizures.
- Third Generation: Represents the latest advancements in AEDs, focusing on improved efficacy and reduced side effects.
2. By Distribution Channel:
- Retail Pharmacies: Traditional brick-and-mortar outlets.
- Hospital Pharmacies: Integral to in-hospital treatment and ongoing patient care.
- Online Pharmacies: Expected to witness significant growth due to the increasing penetration of e-pharmacy platforms and rising awareness of their benefits.
Regional Insights:
- North America: Dominates the market due to the high prevalence of epilepsy, with about 1.2% of the U.S. population having active epilepsy. The region's developed healthcare infrastructure and the presence of major pharmaceutical companies contribute to its leading market position.
- Europe: Significant market share due to advanced healthcare systems and substantial investments in healthcare research and development.
- Asia-Pacific: Rapidly growing market driven by increasing healthcare access, rising awareness, and improving economic conditions.
Major Market Players:
Key players in the global AED market include Novartis AG, GlaxoSmithKline Plc, Johnson & Johnson Service, Inc., Teva Pharmaceutical Industries Ltd., Pfizer Inc., Zogenix, Dr. Reddy’s Laboratories Ltd., Alkem Labs, SK Biopharmaceuticals, and Eisai Co. These companies are engaged in various strategic initiatives such as mergers, acquisitions, and partnerships to develop new and advanced antiepileptic drugs.
For a sample report, visit https://univdatos.com/get-a-free-sample-form-php/?product_id=22772
Conclusion:
The global antiepileptic drug market is set to experience steady growth over the forecast period, driven by the increasing prevalence of epilepsy, advancements in drug development, and the expansion of online pharmacy platforms. Despite challenges posed by the COVID-19 pandemic, the ongoing demand for effective AEDs ensures continued market growth.
Contact Us:
UnivDatos Market Insights
Email - [email protected]
Contact Number - +1 9782263411
Website -www.univdatos.com
#Antiepileptic Drug Market#Antiepileptic Drug Market Size#Antiepileptic Drug Market Growth#Antiepileptic Drug Market Forecast
0 notes
Text
Antiepileptic Drugs Market Size, Analysis and Forecast 2031
0 notes
Text
Antiepileptic Drugs Short Question And Answers
#Pharmacology#PharmaceuticalIndustry#ClinicalPharmacology#DrugsandResearch#Antiepileptic Drugs Short Question And Answers
0 notes
Text
i have discovered that anticonvulsants cause me to have a TC seizure every single time i try to take them. i dont have TCs on a regular basis anymore, but every time i take an AED because im feeling a bit strange and seizurey, i always have a TC later that day
#chronic illness#chronic pain#seizures#epilepsy#tonic clonic seizure#absence seizures#grand mal seizures#seizure disorder#partial seizure#anti epileptic drugs#anticonvulsant#antiepileptic
1 note
·
View note
Text
RIKEN researchers have discovered how the structure of drugs for treating epilepsy allows them to interact with a key protein found in synapses at the junctions of neurons. This knowledge could help to design even better drugs for the condition. Epilepsy is a brain disorder that causes recurrent seizures and can strike without warning. It is thought to affect somewhere between 0.5% and 1% of the population.
Continue Reading.
64 notes
·
View notes
Text
Writing Seizures
Latest installment in Disability Writing Guides! As always, feel free to add something, or come into my ask box with a question, comment, or request.
This post is intended as a writing resource, not medical advice or a comprehensive exploration of seizures or seizure disorders.
Vocab
A seizure is a brief change in normal brain activity. Sometimes this is visible and sometimes not. They can last variable lengths of time and occur with varying frequency depending on the cause. They can be caused by epilepsy, trauma, illness, drug use, or any number of other factors.
Epilepsy is a general term for brain disorder characterized by frequent seizures. A person can have seizures without having epilepsy. Epilepsy is not a distinct diagnosis; there are many different types.
Epilepsy is diagnosed after a patient either has two seizures, or one seizure and an EEG that shows the potential for future seizures.
Again: If a person seizes more than once, they are medically defined as epileptic. A person can be diagnosed as epileptic after only having one seizure if their EEG shows potential for more.
Rescue meds are medications given to stop a seizure currently in progress.
Antiseizure drugs or ASDs, also known as anticonvulsants or antiepileptics, are drugs taken daily to prevent seizures from occurring. These are different from rescue meds.
Status epilepticus is a seizure that lasts longer than five minutes or having a seizure and then seizing again within five minutes without regaining full consciousness. Status epilepticus is extremely dangerous and can cause brain injury or death. Someone experiencing status epilepticus needs immediate medical attention.
Generally speaking, serious intervention would begin before the seizure reached its fifth minute. If someone is seizing past four minutes with no sign of stopping, the people timing the seizure should not wait until five minutes to call 911, administer rescue meds, etc.
A seizure cluster is when a person experiences two or more seizures within a 24 hour period.
A nonepileptic event is an event that may look like a seizure but is produced by a different condition. Examples include ticcing due to Tourette’s or a heart arrhythmia causing a person to pass out suddenly.
Tonic refers to the muscles in the body becoming stiff.
Atonic means the muscles in the body relaxing.
Clonic refers to periods of shaking or jerking in parts of the body.
Myoclonic also refers to short jerking in parts of the body, but is generally more localized/occurring in a smaller area of the body.
Types of Seizures
I’m not going to go through every type of seizure, but I will go over some basics. This is massively simplified, and intended as a general writing resource, not technical or medical knowledge. Feel free to correct if I’m saying something wrong, or add detail.
Seizures are first divided into two overarching groups. Generalized seizures mean that excessive or unusual electric signals are being discharged across the entire brain. Focal or partial seizures mean that excessive or unusual electric signals are being discharged in one specific part of the brain.
Tonic-clonic seizures are the kind most commonly portrayed in media. They involve a total loss of consciousness and involuntary muscle contractions and shaking or jerking in parts of the body. This type of seizure may begin as a focal seizure or a myoclonic seizure (more on this later), but a tonic-clonic seizure is always generalized. Also - this type of seizure was formerly known as grand mal, but this is an outdated term and no longer used.
Myoclonic seizures are partial seizures, characterized by the sudden, involuntary twitching of a muscle or group of muscles. People retain consciousness during these seizures, but do not have control over their body or movements.
Atonic seizures, also called drop seizures or akinetic seizures, cause the sudden loss of muscle strength. They’re called drop seizures as they often (but not always!) cause a person to drop to the ground. A person experiencing an atonic seizure generally remains conscious.
Focal, partial, or absence seizures are seizures that do not involve the whole brain. They can involve repetitive movement like muscle jerking, but more often are characterized by being “frozen,” feeling “out of it,” or “staring into space.” It may be difficult for observers to tell that someone is seizing. This type of seizure was formerly known as petit mal, but this an outdated term and is no longer used.
Focal onset aware seizures, formerly known as “simple partial seizures,” occur when someone has a partial seizure and retains consciousness and awareness. Someone can look unaware and still be aware when experiencing this type of seizure. This type of seizure may involve feeling “frozen” or repeated small muscle movements.
Focal onset impaired awareness seizures, formerly known as “complex partial seizures,” occur when someone has a partial seizure and loses consciousness or awareness. This is type of seizure may involve feeling “out of it,” “staring into space,” or a loss of memory.
In describing a seizure (in modern-day America), the convention followed is seizure type, awareness level, and sometimes, where a seizure begins if it is a partial seizure. Thus, you get diagnoses like “Focal onset impaired awareness seizures arising from the temporal lobe,” “Focal onset atonic aware seizures arising in the frontal lobe,” or “General onset tonic-clonic seizures.”
These diagnoses are very wordy, and are sometimes shortened. Drop seizures or absence seizures are typically used as more casual terms. Also, as seizures generally begin in one of the four lobes of the brain, epilepsy is sometimes described by which lobe the seizures arise in (temporal lobe epilepsy, occipital lobe epilepsy, etc.)
Process of a Seizure
An aura is a feeling, sensation, or “warning” experienced by a person who is about to seize. Auras tend to present the same way over and over. Someone may not have auras, or recognize an aura as being a prelude to a seizure. Sometimes, an aura occurs and a seizure does not follow. Basically, there are no real rules with auras, but they are pretty common, and are generally not observable except to the person experiencing them.
Fun fact: people who have migraines also tend to have auras! It is believed that Lewis Carrol wrote Alice in Wonderland while experiencing a pre-migraine aura.
The ictal period refers to the experience of an actual seizure, when electrical activity in the brain is at its most intense. What a seizure itself looks or feels like depends on the type of seizures a person experiences, and y’all should conduct research into that for your characters.
Some people need rescue meds administered every time they seize. Others are only supposed to be given if they seize for a certain amount of time (longer than two minutes, for instance). Meds can be administered as nasal sprays, rectally, or tucked under the tongue or into the cheek. Rescue medications are only injected in hospital settings.
Remember that regardless of how often a character seizes or how long they’ve had epilepsy, seizing for more than five minutes, or multiple times within five minutes without regaining consciousness, is a medical emergency. Rescue meds should be administered and whatever medical intervention is appropriate for your setting should be immediately undertaken.
The post-ictal stage occurs after a seizure ends and lasts anywhere from five to thirty minutes. This is the period when a person is still experiencing after affects from their seizure, like confusion, drowsiness, hypertension, headaches, or nausea. Not everyone experiences post-ictal symptoms, and a person may continue to feel exhausted, irritated, or “out of it” more than thirty minutes after they seize.
Seizure Etiquette
Seizures can be surprising and very noticeable. A person that is seizing still deserves privacy. In your story, they should be given privacy, and good friends/teammates/co-characters could steer other people away or block them from being a public spectacle while they seize.
Do not have anyone put anything in a seizing character’s mouth. Ever. This is not necessary and can be dangerous, as a person can choke, or the person attempting to put something in their mouth could get accidentally bitten.
Do not restrain a person that is seizing. The character seizing or the character attempting to restrain them could get hurt, and the restraints are not going to be helpful whatsoever. Characters can move chairs or place cushions to keep a seizing character from hitting them; do not attempt to stop the seizing character’s body from moving how it will.
If necessary, the person seizing can be placed on their side, otherwise, do not attempt to move them.
If a non-epileptic character seizes, it is an emergency. Epilepsy can arise spontaneously at any age, but seizing with no prior history of seizures is a big deal, and the causes for a seizure need to be checked out to understand what caused it.
If your characters have access to medical knowledge and medical treatment, it would be realistic to have them time the seizure so that they know if a character needs rescue meds or has entered status epilepticus.
Rescue meds can be very, very expensive. A character will likely not receive rescue medication every time they seize, especially if their condition is largely stable.
It can be scary and emotional to watch someone seize. Feelings of fear and helplessness are common, especially if what’s needed is for characters to stand and wait to see if the seizing individual needs further help. It’s okay for your characters to feel that and react to that.
Things to Know
Epilepsy mostly presents in childhood and in people older than 60, but can arise at any age. Repeated seizures caused by an underlying condition (brain injury, tumors, strokes) are still considered epileptic seizures, and the person that has them, epileptic.
Repeating it once more: If your character seizes more than once, they are medically defined as epileptic.
The vast majority of seizures do not cause brain damage, or any other kind of damage. They can be frightening, distracting, inconvenient, upsetting, confusing - any number of things. But the vast majority do not cause physical harm, besides the bruises or scrapes that may come from muscle contraction or losing awareness.
Some seizures do cause brain damage. If you’re writing this scenario, please do some research into the type of seizure that would cause brain damage and what kind of brain damage that would be. Do not, for instance, have your character experience a tonic-clonic seizure and then come back in a wheelchair with no further explanation.
Sometimes, the muscle contractions of a seizure can cause spit or foam to collect around someone’s mouth. Sometimes, people bite their tongue, and this foam or spit can appear bloody. No internal injuries occur as a result of a seizure. Any bloody foam or spit is a result of a bitten tongue or cheek, and nothing more.
People who are seizing sometimes lose bowel or bladder control. This is not something they have any control over, but can still be embarrassing and is sometimes a reality of living with seizures.
In the United States, driving laws vary from state to state, but generally a person needs to be seizure free for a period of months (usually 3-6) before they are allowed to drive. The restrictions on driving commercially are much stricter.
Someone diagnosed in childhood may grow out of their epilepsy. Some estimates put the number of kids that will outgrow their epilepsy above 50%. If someone is seizure free for 2-5 years, they may begin to lessen their ASD dose, and may continue until they are no longer medicated at all.
Someone diagnosed in old age will not typically have a spontaneous remission of seizures.
Epilepsy can have a genetic basis or it can arise spontaneously. The fact that it can be passed from parent to child has been the basis of discrimination for a very long time. Be aware of this.
For much of human history, having epilepsy has been hugely stigmatized, and people with epilepsy have been routinely persecuted, particularly in the Western world under the banner of eugenics. As recently as the 1970s, many states were still forcibly sterilizing epileptic people. In writing a character with epilepsy, be aware that the diagnosis carries a heavy weight of stigma and painful history.
Though epilepsy and people who have epilepsy have long been stigmatized and persecuted, it has also long been regarded as a mystical illness, closely tied to spirituality and religion. In many places, people who have seizures are considered to be in religious ecstasy, having visions, or are chosen by higher powers. Consider the setting in which your story takes place and if this kind of thinking would realistically occur. Keep in mind that this view of epilepsy and seizures is not necessarily a positive thing.
Accessibility and Treatment
If you are writing a character who only seizes once (and the setting allows for it), proper treatment would consist of visiting whatever medical establishment exists in your universe, and monitoring or testing to determine the cause of a seizure and if another is likely to occur.
Even though your character is not going to seize again and does not have epilepsy, consider how the single seizure may affect your character. What did it mean to them to (perhaps publicly) lose control of their body or brain?
If your character does have epilepsy, their life will change or has always looked different because of that epilepsy. For example, someone with epilepsy may not be allowed to drive, or may have never learned to drive. It is not safe for someone who has uncontrolled epilepsy to live alone. How would these considerations affect your character’s life and independence?
Think about how having seizures would apply to your character and your setting. Do they feel safe swimming? Spending significant time alone? Are there places that they avoid because it’s too dangerous to seize there?
In real life, people who experience tonic-clonic or atonic seizures often take precautions to ensure their safety should they have a seizure. People who have atonic seizures wear padded helmets to protect their heads. People who experience an aura may get themselves to a safe location, or adjust their surroundings so that they won’t hurt themselves while they seize. What precautions might your characters take to protect themselves?
Seizure triggers. Photosensitivity is a very common one, with flashing lights being especially dangerous for epileptic people. Some seizures have clear, specific triggers, while others seem to arise out of nowhere. Though it may be difficult to tell what exactly triggered a seizure, the modern Western medical establishment believes that all seizures have triggers, though the triggers may not be known. Triggers tend to be environmental cues that the central nervous system over-responds to, like the aforementioned flashing lights. A friend of mine has epilepsy that is triggered by anything coming directly at their face, like balls being thrown towards them. Once, a seizure was triggered by a butterfly flying directly at them.
Seizures can also be triggered by sounds, smells, or sensation, not just sight!
What might your character’s seizure triggers be? Your character may or may not know themselves, but if the triggers are known, how does your character avoid them, or plan their life around them? My friend’s seizure trigger meant that they couldn’t play ball sports, even casually, which kind of sucked. But having a seizure sucked more, so.
In terms of accessible spaces: The more open space, the better, and the softer the surfaces, the better. For instance, people who have seizures may prefer using an accessible bathroom stall, as they are larger, and the person seizing is less likely to become trapped or hurt themselves if they seize unexpectedly in the bathroom. What kinds of spaces does your character seek out, particularly if they are aware they might seize soon?
A properly medicated epileptic character may still have seizures. Medications are intended to control, shorten, and decrease total number of seizures. Sometimes they entirely eliminate seizures, but a person may still seize and that does not mean the medication isn’t working. A character who still seizes frequently and for long stretches of time likely is not properly medicated. Medications should be taken around the same time(s) every day for maximum efficacy.
Life changes, particularly puberty, can make medication less effective.
Proper medication is life-changing for people with epilepsy, and would likely be life-changing for your epileptic character as well. What does the process of getting medicated look like? How does your character feel upon being properly medicated? What in their life changes, and what stays the same?
Are there any drawbacks to being medicated? Side effects? Cost of medication?
If epilepsy is drug resistant, there are a few other options. I’m only going to discuss two, one because it has a long, fraught, and misunderstood history, and the other because it’s Trendy.
Brain surgery is an option for people/character with epilepsy. This is not the scary ice pick lobotomy of the 20th century. Brain surgery is a necessary tool to help epileptic people that are struggling with frequent, severe seizures that do not respond to medication, or when the side effects of medication are intolerable. Surgery can mean removing part of the brain (resecting), killing specific nerve cells where seizures start (lesioning), disconnecting the hemispheres of the brain (corpus callosotomy), or the implantation of a pacemaker-type device that uses electrical signals to block or disrupt seizures.
If your character is getting brain surgery for epilepsy in a contemporary, futuristic, or fantasy setting, please do your own research and ensure that the type of surgery they’re receiving fits their type of epilepsy and their need. Please frame the surgery accurately and avoid falling back on scary tropes about people coming back with different personalities, no personality, or dying in these procedures.
The last treatment option I’m going to discuss here is the ketogenic or keto diet. You may not be aware, but the diet was originally developed to treat children with epilepsy, and there is limited evidence showing that it does decrease or eliminate seizures in children. This diet is extremely high in fat and as low as possible in carbs. The majority of people who believe they are following a keto diet and are in ketosis (body and brain fueled by fat instead of sugar) are wrong. It is extremely difficult to follow a strict keto diet and is absolutely a major life change.
The diet would typically only be recommended for children between 2 and 12 whose epilepsy is resistant to medication.
Why or how the keto diet works to control epilepsy is not well understood. The fact that the brain is fueled by fat products known as ketones, rather than glucose, is thought to be related. If anyone knows more, feel free to contribute that knowledge.
Rethink
If your character gets brain surgery for their epilepsy, and that surgery is framed as negative, think about why that is. I absolutely understand the long, problematic, real-life history behind lobotomies, and I am not telling you not to explore that. Please do think hard about what beliefs you may have, and what messages you may be sending, about people who get brain surgery.
Characters with epilepsy that gives them visions or confers some kind of power. Yes, there are historical associations between epilepsy and religiosity, but remember the real world people who have epilepsy and how this framing may strike them. This is a common trope, so do a little introspection on what about this narrative is compelling to you and what messages you’re consuming and endorsing.
Seizures that occur to add intensity, drama, fear, or risk to the story. What are your characters afraid of? Why are they afraid of it? As always - what messages are you sending about seizures or the people who experience them? How would it feel to read your portrayal as a person who regularly seizes?
A character who seizes but does not have epilepsy. Related to the above - why is a seizure important to your story, but epilepsy is not a part of it?
A character who seizes twice but is not described as/does not identify with epilepsy. For one, this is medically inaccurate, which you should just be aware of. Secondly - what about this diagnosis is undesirable or unnecessary for your story? Why?
Write what you’re going to write, but understand why you’re writing it, and how it might be perceived. In particular, when writing about a complex, widely misunderstood, and stigmatized condition like epilepsy, understand what stigma you may be contributing to, what inaccuracies you may be presenting, and what complexities you may be ignoring, especially by having a character seize without being epileptic.
Resources
A lot of this is written based on my relationships with epileptic people and personal research. I don’t like to recommend media that I haven’t personally read/watched, just because then I don’t know what I’m recommending, but if anyone else has recommendations, please feel free to add them!
How Evan Broke His Head and Other Secrets by Garth Stein is contemporary novel about a Seattle man with epilepsy who is suddenly thrust into parenting a 14-year-old son he didn’t know existed. I read it a while ago and remember it being pretty good, but nothing special (no offense, Garth Stein). Worth noting that while the author is not himself epileptic, his sister does have epilepsy and he likely has better than typical knowledge of the condition.
The Spirit Catches You and You Fall Down by Anne Fadiman is a creative nonfiction book about a Hmong family, their epileptic child, and the medical saga they embark on as the American medical establishment attempts to treat their child. It is written about a real-life immigrant family and their daughter and was extensively researched over eight years, focusing on cultural differences, and xenophobia, racism, and misunderstanding in medicine.
This Podcast Will Kill You, which is free on Spotify, includes an hour and forty minute long episode diving into (some) of the etiology and history of epilepsy.
Maintenance Phase is a podcast that is also free on Spotify and has an episode about the keto diet. The main focus of the episode is the keto diet as it is used for weight loss, but it does include some fascinating backstory on the (invented) narrative that the keto diet is a secret that is being kept from the general public.
Please hit me up with questions, comments, corrections, or requests. Happy writing!
#disability writing guide#writing disabled characters#epilepsy#seizures#writing seizures#writing epilepsy#writing characters with seizures#writing characters with epilepsy#disability representation#disability justice#representation matters
426 notes
·
View notes
Text

3 July 2024 // Wednesday
Right now I'm just trying to study atleast some topic everyday cause attending all lectures, clinics and pracs itself is soo damn tiring .
Today's pharmac lecture was on anti epileptic drugs, then for surgery clinics we saw a hernioplasty procedure , it was more interesting because I had read about this topic sooo I could understand atleast something! The we had patho , I zoned put after about 60% of the lecture :')
Then we had psm prac...it was okay.
Then I came home and read antiepileptic drugs and solved past year questions from the covered topics .
#studyblr#productivity#study motivation#study blog#med school#study hard#stdyblr#aesthetic#studtblr#study inspiration#medical student#medical school#medicine#college studyblr#chaotic academic aesthetic#my honest studyblr#heysaher#academia aesthetic#desi studyblr#secondyearmbbs#med student#med studyblr#medical studyblr#study community#study inspo#studyspo#studying#inspirational#daily motivation#study tumblr
44 notes
·
View notes
Text
Been fighting off a migraine for like 18 hours... Christ
My mom has chronic migraines and did for my entire childhood. Genuinely it was one of the biggest factors in ruining my relationship with my mother; she was the breadwinner of the family and so she worked longer hours. She got home from work and often would be too exhausted to interact with me at all. She'd come home two or three times a month, like call out of work, and just be locked in her room for hours, even days. Sometimes I genuinely feel like she was a stranger to me, especially when my dad left. At that point she would come home from work and go straight to her room. Sometimes I wouldn't see her for days. Sometimes even when I saw her she wouldn't speak to me. A lot of that was, in earnest, because she was in a lot of drug trials for migraine preventative medication that turned her into a zombie and left her... frankly, disassociated. I spent so much of my childhood terrified i would end up like her, spending days every month curled up in my room in so much pain and for so much time that my kids were strangers to me. That anything I did to try and improve it would turn me into a zombie. Like she was just always in so much pain and I was so terrified of getting migraines. And then I did, and just like the seizures, they've been escalating as I get older. I didn't have a tonic-clonic seizure until I was like- 27? I never had a migraine before 18. Now I'm averaging one a month. And when i do get them, Jesus Christ they're bad. They're "if I didn't know it would not help and would only make it worse, I would go to the hospital" level. Kidney stone in your brain. I'm really good with pain, but. Still. Doesn't mean I like it.
And the one I had back in May is genuinely the only time I've ever marked something as a 10/10. If I hadn't been home alone I'm sure someone would have dragged me to a hospital, but I was so blitzed out of my fucking mind that the idea of an ambulance sounded like hell and the only solution my soup brain could come up with after id maxed out on acetaminophen, ibuprofen, and finally on oxycodone, was half a bottle of vodka on top of it figuring "either I will feel better or I will die and both are preferable at the moment." Good lord
I probably need to talk to my neurologist about a preventative of some kind... Obviously I'm already pretty unhappy about that idea, especially when I already have to take so many goddamn drugs every day. At least I can be reasonably certain my.migraines are hereditary and not caused by epilepsy since my antiepileptic doesn't do shit to stop them
Ugh
14 notes
·
View notes
Text
Paroxysmal Sympathetic Hyperactivity As A Cause Of Prolonged Icu Stay- Case Report by Arnab Choudhury in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Paroxysmal Sympathetic Hyperactivity (PSH) is commonly described in patients after Traumatic Brain Injury but it can present after an ischemic stroke following a complicated surgery. Usual clinical presentation are tachycardia, tachypnea, hypertension, sweating with seizures and dystonic posturing less likely initial signs. High grade fever and profuse sweating may allude sepsis or epilepsy leading to extraneous administration of anti-epileptics and antibiotics. Suspicion of pheochromocytoma arises in such situations which is ruled out by CECT. Clonidine (α-2 blocker), propranolol (β-blocker) and Baclofen (GABAb agonist) are agents used in treatment. Benzodiazapenes like lorazepam are important part of treatment as discontinuing them can exacerbate PSH attacks. MRI brain with MR angiography usually reveals hyper-intensities on T2/FLAIR in subcortical areas (thalami, cerebellum, crus cerebri) and restricted diffusion with low ADC values. Recurrent PSH episodes can occur due to delay in diagnosing and treatment leading to contractures and difficulty weaning the patient off the ventilator with tracheostomy tube placed. This case presents a scenario in which the delay in diagnosing PSH led to extensive investigations , delay in specific treatment and a prolonged ICU stay of the patient. Mainstay of rehabilitation remains aggressive physiotherapy to improve contractures if any, medications for the autonomic fluctuations and regular follow up.
Keywords : Sympathetic, hyperactivity, paroxysmal, brain, episodes
Introduction
Paroxysmal sympathetic hyperactivity (PSH) is a disorder of autonomic function regulation most commonly observed in patients with acute brain injury. It mostly occurs after traumatic brain injury, but it can also occur after non-traumatic brain diseases such as anoxic-ischemic coma after cardiac arrest, intracranial haemorrhage, and ischemic stroke-[1].
The core clinical features include - tachycardia, tachypnea, hypertension, sweating , hyperthermia and posturing-[2]. These episodes are mostly triggered by some external stimuli such as pain , movement , and urinary retention . PSH occurs due to diffuse or focal brain injuries that disconnect one or more cerebral centers from the caudal excitatory centers and the disconnection of descending inhibitory pathways causing spinal circuit excitation.
Tonic posturing during episodes can mimic tonic seizures, and the raised temperature can mimic infection, which can lead to unnecessary investigations, delays in proper management and prolonged ICU stays. Here, we are presenting one such case.
Case Presentation
A 32-year-old woman (gravida 2 and para1) had pain in the lower abdomen at week 31 of gestation for which she was hospitalized and emergency Lower Segment Cesarean Section was performed in view of fetal hypoxia. On the 2nd day post-delivery, she developed multiple episodes of seizures without regaining consciousness in between and was intubated for airway protection. Brain Magnetic Resonance Imaging(MRI) with angiography suggested posterior circulation ischaemic stroke with bilateral narrow caliber of both vertebral arteries and a left fetal PCA. She was started on antiepileptic drugs and secondary prophylaxis for stroke. She was having high-grade fever and, multiple episodes of profuse sweating per day. Blood counts, cultures, and other markers of infection gave negative Results. She had episodes of tachycardia, tachypnea, hypertension, and sweating associated with fever.
The fever episodes created difficulty in weaning the patient from the ventilator.Therefore, she was started on clonidine and later on, propranolol;-however, these episodes continued to occur. Suspecting pheochromocytoma, abdominal contrast enhanced computed tomography (CECT) was performed, but the results were normal. The patient had recurrent episodes of increase in whole body tone (Fig 1) associated with bilateral lower limb tremors, abnormal posturing along with the above-mentioned episodes of fever. Initially, it was assumed that the rigors were those associated with fever, but later,speculating that the rigors were seizures,- the dosage of herantiepileptic medications were increased, and she was administered triple antiepileptics ( valproic acid , levetiracetam and lorazepam). Her brain EEG showed no epileptiform discharges. Despite receiving triple antiepileptics, she continued to show seizure-like activity. Later, these episodes of fever, tachycardia, tachypnea, hypertension , sweating and increase in body tone occurred simultaneously,- and the diagnosis of paroxysmal sympathetic hyperactivity was made.
The patient was administered clonidine, propranolol, and baclofen. Her episodes of sympathetic hyperactivity were controlled . Later, her empirical antibiotics were stopped as there was no evidence of infection and fever was explained as a part of sympathetic hyperactivity. Antiepileptic medications were tapered off to only levetiracetam. However, after discontinuing valproate and lorazepam she again started experiencing episodes of sympathetic hyperactivity. Therefore, lorazepam was reintroduced to control her symptoms. Finally, the patient was weaned off ventilator support and shifted to the ward.
Investigations
Blood parameters: TLC - 10,000 /mm3 ,Hb - 12 g/dl , Platelets - 2.8 lac/mm3
Blood culture - no pathogenic organism grown after 48 hrs of aerobic incubation.
Urine culture - sterile
Endotracheal aspirate culture - no pathogenic organism grown after 48 hrs of aerobic incubation.
High vaginal swab culture - normal vaginal flora grown.
Procalcitonin - 0.29 ng/ml
CSF analysis, - Acellular; sugar,-24 mg/dl; protein,-68 mg/dl; culture,-sterile
Dengue IGM,- negative; ICT and peripheral smear for Malaria - negative , Typhidot IGM,- negative; scrub typhus IGM,- negative.
Ultrasound abdomen:- no significant abnormality.
MRI Brain with MR Angiography –The brain stem appeared bulky and showed T2/FLAIR hyperintense signal. Similar areas with T2/ FLAIR hyperintense signal were also seen involving the thalami, right crus cerebri and bilateral inferior cerebellar peduncles. Many of these areas showed restricted diffusion with low Apparent Diffusion Coefficient (ADC) values. The bilateral (right > left) vertebral and distal basilar arteries appeared significantly attenuated in caliber. The right PCA appeared to be significantly attenuated in caliberas compared with fetal origin of the left PCA.
EEG - Generalized cerebral dysfunction; -no epileptiform-discharges.
CECT abdomen - No significant abnormality
Outcome and Follow-up
The episodes of sympathetic hyperactivity resolved, and the patient was shifted to the ward from the ICU with tracheostomy in room air. She developed contractures owing to persistent decerebrate posturing. Aggressive physiotherapy was administered. In the ward she regained her sensorium and was discharged with a GCS score of E4VTM6 for further follow-up in the OPD.
Discussion
A significant minority of patients who survive acquired brain injury develop sympathetic hyperactivity, which includes episodes of periodic increase in heart rate and blood pressure, sweating, hyperthermia, and motor posturing, often in response to external stimuli, which can last for weeks or more months-[3].Some studies argue that it is common but often unrecognized-[4].Most studies have reported paroxysmal sympathetic hyperactivity after traumatic brain injury. Fewer cases have reported it to be a sequel of brain stroke following prolonged hospital stay.Though commonly seen in TBI, PSH has rarelybeen described in patients with brainstem strokes and anoxic brain injury-[5].PSH may be mistaken for sepsis, which may lead to unnecessary treatment with antibiotics and prolonged hospital stays-[6].Fever is relatively common among patients in the intensive care settings. Although the most obvious and concerning etiology is sepsis, PSH may be the underlying etiology-[7].There are diencephalic structures analogous to the cerebral motor cortex that are capable of producing, when irritated, paroxysmal motor discharges similar to the focal discharges described as epilepsy-[8].PSA may be camouflaged by epileptic seizures, leading to the unwarranted administration of antiepileptics to the patient. Obstetric patients can present with acute increases in heart rate,-BP and the onset of HELLP syndrome mimicking PSH. Epigastralgia, hypertension, and tachycardia necessitate cesarean section, as in our case, with the subsequent development of HELLP syndrome mimicking PSH.An acute fluid shift from the splanchnic vasculature to the central vasculature may have occurred, causing HELLP syndrome as a result of vasospasm associated with sympathetic hyperactivity. Reporting such cases will facilitate in understanding if the reverse is true, that is, if PSH can mimick as HELLP syndrome-[9,10]. Pregnancy is a risk factor for paroxysmal sympathetic hyperactivity exacerbation, and delivery can result in resolution of the condition-[11].PSH is reclassified as a sympathetic storm rather than an epileptic disorder because of its unresponsiveness to anti-epileptics and the absence of epileptic activity on EEG. [12]it is crucial for clinicians to distinguish this disorder from paroxysmal dystonias. [13,14]Sympathetic storms have been linked to dystonia-like posturing (e.g., PAID, i.e., "paroxysmal autonomic instability with dystonia")[15], Antidopaminergic medications are best avoided to minimize the risk of neuroleptic malignant syndrome, which can potentially mimic PSH (dysautonomia). In contrast to delirium‐associated persistent agitation and picking‐like behaviours, PSH movements are episodic, tend to be provoked by touch, and are uniquely associated with increased sympathetic activityIn the management of this disorder opiates, γ-aminobutyric acid agents, dopaminergic agents, and β-blocker pharmacological agents have been studied. There is a lack of recommendations and comparisons of agents for the management of this disorder. There is a paucity of recommendations and comparisons of agents for the management of this disorder. Monotherapy is usually ineffective for the management of paroxysmal sympathetic hyperactivity, and multiple agents with different mechanisms of action should be considered, as in our case .β-blockers have proven to be therapeutic (not as monotherapy) as in our case,α-agonists such as dexmedetomidine have reported therapeautic efficacy in many studies. However, clonidine another α-agonist has shown therapeutic efficacy, as in our case. The effectiveness of physiotherapy in PSH is rarely reported in medical journals; our case strives to provide an example of such therapeutic benefits.
Conclusion
Paroxysmal sympathetic hyperactivity is quite common in patients with brain insult.It can mimic seizures and/or sepsis (due to high grade fever) leading to unnecessary investigations, exposure to higher-grade antibiotics and antiepileptics. Benzodiazepines are beneficial in controlling sympathetic hyperactivity.Non recognition of PSH can lead to difficulty in weaning patients off the ventilator and prolonged hospital stays. Recurrent episodes of sympathetic hyperactivity can lead to significant weight loss and contractures.
#Sympathetic#hyperactivity#paroxysmal#brain#episodes#JCRMHS#Journal of Clinical Case Reports Medical Images and Health Sciences (JCRMHS)| ISSN: 2832-1286#clinical decision making
2 notes
·
View notes
Text
Epilepsy: Causes, Symptoms, FAQs and Treatments
Living with epilepsy can be challenging, but with the right treatment and support, it’s possible to thrive. Our complete guide covers everything from seizure types to treatments, safety tips, and resources for living well. Read more! #EpilepsyAwareness #S
Epilepsy is a neurological disorder that affects millions of people worldwide. It is characterized by recurring, unprovoked seizures that are a result of abnormal electrical activity in the brain. While epilepsy can develop at any age, it is a condition that requires careful management and understanding. In this guide, we’ll explore what epilepsy is, its causes, types of seizures, diagnosis,…

View On WordPress
0 notes