#and the chronically ill genes that allow me to be fine after it passes
Explore tagged Tumblr posts
Text
ibuprofen how could you
#betrayal#woke up in severe stomach pain#like seriously considering going to the hospital bad#holy hell that SUCKED#god bless tums#and the chronically ill genes that allow me to be fine after it passes#anyway#EAT SOMETHING WHEN YOURE TAKING NSAIDS#DONT BE AN IDIOT#A PIECE OF BREAD IS ALL YOU NEED#JUST DONT TAKE IT ON AN EMPTY STOMACH
3 notes
·
View notes
Text
A Deeply Personal Post about Suicide
A very personal and dark post about depression, its relapse, and suicide**
*you have been warned*
**A post with a whole lotta trigger warnings~ STAY AWAY if you can’t, or if you must. Otherwise, thank you for taking your time reading. This is not clickbait, and definitely not for the faint-hearted. You have been warned. Don’t blame me for any negative effects**
Yes, there, I have said it. I always had the urge to write this down but I kept getting depressed over and over and I really can’t write it if I’m still in that dark, constricting place. But I am so far OK so I shall be posting this stuff. If this post prevents at least, or even just one person from taking their own life and gets a new lease in life then my broken and torn heart will have its peace. It’s harder to live and easier to die. But if you’re spiritually awakened, then the commitment to stay alive is even more pressing. I salute you for staying alive. You can do it!
OK, that’s enough cheery stuff for now. Anything beyond this point can turn dark and ugly in a manner of letters so again, if this is a strongly-triggering topic for you, and you can’t face it, that’s ok. Just stay away, till you think you can handle this. Also I wrote this on the morning of August 28, 2019 but I also had to purge the energies on this post so it would be healing more than destructive, so it pops up a day later as a queued post.
Edit: accidentally clicked POST instead. Not that I mind, I was gonna anyway. Divine realm kept nagging me so.. here you go. 😆
I *MAY* HAVE BEEN BATTLING DEPRESSION AND SUICIDAL THOUGHTS SINCE I WAS A CHILD
I don’t think I have the need to completely spell out what depression is because again, the internet can do that for you. I will just focus on how it was, and is still manifesting in my life. But how did it materialized in my life then? Well... Mostly I just internalized all of my demons. If I was angry or upset or I feel envy or jealousy, I just sucked it all in. My household growing up was a battlefield of emotional suppression, thus I can’t cry, throw a tantrum, even laugh out loud for being too happy. What’s even more ironic is that I am actually a very emotional person, which made a whole lot of sense once I understood my natal astrological, human design, and gene key charts. So even if my sun was in Gemini and my ascendant in Libra, I pretty much have all the water signs in my chart as well, along with having a strong sacral center that thrives on generating emotionally-charged energy, and that’s where the waterworks come from. Thus the fact that I’m a Gemini cry-baby who gets too-emotional at just about anything makes perfect sense now.
But back to the subject at hand: Emotional Suppression caused my mental instability and depression. Because each time I had to stop expressing what I feel deep inside, I feel like I kept killing a part of me. Each time I kill a part of me, a gaping hole in my heart and soul would grow even larger. Like literally I feel chest pains as a child, which of course don’t show up on laboratory exams and thus I have been deemed healthy, a lot. I already started wanting to kill myself around 7 years of age, because I was forced to grow up quickly so I could take care of my siblings and myself. I really hated myself and the world a lot because I can’t do what I want and I can’t have anything I want, among other things. I mostly play alone, which was fine until the thoughts of wanting to die keep coming up. Maybe for some people these things are nothing, and they’ll start bragging about their own difficulties and that’s OK, I mean, what you feel will always ring true to you, no matter what the world tells you. The brain can lie to you, but your heart and your emotions never will. Feelings and emotions are always true, and what you feel is always valid. If something hurt you or made you happy, it’s because you have those things inside you. If people trigger you deliberately, then that’s on them. If you get triggered by other people, well that’s a whole other matter... BUT, whatever you do when acting under that feeling or emotion is entirely up to you, and you cannot blame other people for making you act in certain ways. Remember, YOU ALWAYS HAVE A CHOICE IN YOUR ACTIONS, THUS THE CONSEQUENCES ARE ALSO OF YOUR OWN DOING. The bottomline is: PLEASE FOR THE LOVE OF GLOB DON’T PLAY DOWN WHAT I AM WRITING HERE AND SAY THAT I’M IN THE WRONG. This entire thing is a personal account, and it’s mine. I get to write this thing because the whole thing is based on what I have experienced. *see? I told you I easily get emotional lol*
I got sidetracked, I apologize. OK, now back to regular programming
Anyway, thoughts of killing myself got even more intense, especially with not meeting parental expectations as well as neglect, abandonment, and rejection issues that popped up as time went on. To be honest though, I was, and still am a bit surprised that I haven’t taken my own life then, and up to this point. Either it’s because I am highly-sensitive to pain *my pain threshold is quite low*, or because I am still trying to find ways to kill myself without the hassle or pain. Basically I fear pain more than death. I guess that’s one of my major motivators for not choosing to end it yet. I just hate physical pain in all forms, even more so right now. So even if it kills me inside, I try to live one day at a time. Back then, I had to live because my siblings need me to cook their food, and I had to do my sister’s homework (she has autism spectrum disorder, which my parents just chose to ignore because they have no idea how to interact with special needs).
How is depression connected with suicide? Well, for one thing the hopelessness, helplessness, feeling worthless, or thinking that living is not worth it can just push a person to the edge. I am quite familiar because I have lost a sizeable number of people ranging from relatives to friends, to classmates and even a work trainee from suicide. I haven’t even counted those who died from natural deaths, those who got killed either in combat or by rebels, or through illnesses. The suicide-related ones just affect me so much because I felt survivor’s guilt, because I haven’t ended my life yet and these “seemingly-happy” people did. My stomach got all knotted up right now, just thinking about it. Especially when I recalled the trainee that killed themselves due to depression. I didn’t mentor them personally but I sorta felt that this person had depression and again, I didn’t reach out. Even then when I was already aware of being an empath and all that jazz. I just gave myself a break after sometime because to be honest, I had no idea how to heal others back then. So... Yeah. But still, survivor’s guilt is real.
RELAPSE ISSUES CONCERNING SUICIDAL THOUGHTS (HOW I HAD THEM)
This is the part where I will be explaining based on my own experiences why some people who were openly-depressed that “seemed” to have gotten a lot happier and brighter suddenly end their own lives with no warnings. Not sure about other people’s ideas, living or dead, but for me, it’s all about the relapse.
Depression relapse, that is. You may be much more familiar with alcoholics or drug-addicts who went to rehab, got all better *or so it seems* but then goes to relapse and either ends up getting even more addicted or worse, having an overdose and dying. Well, again, this is based on my own experiences but for me, because I am not on any kind of medication for my chronic depression so naturally, despite all my conscious efforts on fending it off, it comes back, with a vengeance. All the pain that I feel, all the thoughts that consume what small speck of happiness I have left become even stronger than before, and whatever I did to relieve myself of the pain just stop working no matter how many times I do it. Everything just feels sucky and my pains do not get relieved. I just cry and cry and let the wave pass, allowing a bit of relief, but then they just come back in waves of endless and bottomless anger and feelings of doom and gloom. It feels like I’m forever falling into the abyss of nightmares and frankly, the only solution I see clearly at that point is again, killing myself. Again, because I’m scared of pain, I did whatever I can to escape the pain, thus me ending up learning a lot of bankable and unbankable skills that, quite frankly amused some people I meet once the depression has been controlled somewhat and I got to socialize again.
If I survive long enough to at least raise my happiness levels a bit, I can continue to live, even for a day. I just tell myself “Well, I guess I’ll just have to die another day.” For each time that I tried to escape my pain and my urge to kill myself, I find something new to experience, learn, and have fun with. Thus, the skills I have, the dumb experiences I had, the movies and shows I gave so much of my love to, the ties to people I hold dearly, were not only borne out of a small curiosity, but mostly to prevent myself from ending my life right now. I don’t know how people will react to that, but for me, my hobbies, my passions, are not just due to the fact that these things are worthwhile. For me, these are my LIFELINES. If I didn’t have them, I MIGHT HAVE DIED A LONG TIME AGO. These are also the reasons why despite how many people or the public would shame other people for having weird hobbies or passions, I just let them be happy. I like seeing passionate people, because not only do they look so happy and pure, but also because for me, that might also be their lifeline. So that they CAN STAY ALIVE, because LIFE SUDDENLY HAS MEANING. And who am I to tell them what they or what they cannot do? *unless it’s illegal or hurts other people deliberately, or both. I have limits*
And... Unfortunately, for some of the people who took their own life out of their own accord they may not have been fully aware of it, but when they got out of the funk, they might have thought that YES I AM NOW FREE FROM ALL THAT GUNK. I’M GONNA BE HAPPY, I CAN LOOK FORWARD TO THE FUTURE, ETC. ETC. but noooope, depression is pretty clingy. It comes at the most inconvenient time, right about the time when you thought you’re almost at your goal, or at the time when you feel like you’re about to have that breakthrough. Once anybody who has been recovering from depression falls back into it, the urges, the pain, everything just gets even worse. Everything sucks maybe a hundredfold compared to last time, maybe a million times more. Everything just feels so overwhelming, and heavy, and it cuts through your entire being. The way out just got caved in and now there is no way out other than suicide. THAT FEELS AND SEEMS LIKE THE ONLY WAY. And for some of these people who actually take the plunge and succeed, this is the part where their loved ones who were left behind would comment things like “But I thought they were happy.. They were looking forward to the future.. They had so many plans.. They weren’t showing any signs...” etc. etc. Of course they won’t, and they probably had plans. If anything, they probably wanted to get out of the funk for the rest of eternity. BUt DEPRESSION IS ONE CLINGY F****R my friends, seriously. It is. It will slam everything in your face if it isn’t properly handled, either though holistic means or modern medicine methods, it will certainly choke out the light of any person who just do not have the means to fight it, let alone keep it at bay. Especially when it gets pushed aside. A lot. Each time you succeed at pushing it away or dealing with it, if it creeps into your being, even through just a small crack, it comes to you with a force stronger than a wrecking ball. It’s more of an avalanche. And it will bulldoze anything away till the entire path has been completely covered. Still scary as heck. Thus with each round of its return, it gets more and more strong, thus the need for better ways of fending it off. Or better yet, just facing it head on by all means necessary.
FACING (MY) DEPRESSION HEAD-ON (BY ALL MEANS NECESSARY)
Disclaimer: Again, before I start this section, I will remind everyone that this entire post is all my personal experiences as well as my own opinions on this matter, so please do not take this as a medical or health advice. You can take this as a spiritual advice and you can even ask me about it. I’m glad to help. Other than that, please seek professional help. BY ALL MEANS NECESSARY. I am not responsible for any losses of any kind due to following my own personal methods here, any bodily harm or mental injuries sustained by the end user are done of their own accord, and I am not liable for such losses. Everything here with regards to methods are RISKS. YOU HAVE BEEN WARNED.
OK. Now that’s out of the way, I will now write here how I deal with my own depression and suicidal thoughts,assuming that I’m still here. I’m not saying that I will not kill myself yet, but I am fully aware that other things can kill me and therefore those won’t count. Also, I haven’t watched the entire Fantastic Beasts franchise yet, and my need-to-watch anime and series lineup is still long, plus Avatar The Last Airbender is gonna be on Netflix next year so nope, I still need to live.
Kidding aside, here is what I USED TO DO whenever the relapse comes in full-swing:
Binge-watch anything I’m interested in
Binge-read whatever is available
Binge-doing whatever activity I’m into at the moment (drawing, reading Tarot cards, learning Japanese, cooking weird food, etc.)
Binge-like anything on my tumblr feeds
Get super-obsessed with the canon and headcannon biographies of fictional characters (Hi wikia and AO3 lolol)
Cry and cry and cry even if I don’t know why (It doesn’t even matter how hard I try lolol did you sing that part in your head lol kidding I am trying to lighten up things here)
Of course, after doing all of these, I eventually end up wanting to die because the problem or the cause of my depression remains unsolved. Notice that I didn’t put “contacting close friends” or “connecting to loved ones” there. Because I don’t. I was never raised to ask for help, I was raised to do shit alone. And that also killed a huge part of me because quite frankly, I know that I need help but whenever I tried to reach out I get put-out or shushed, so eventually I never bothered to ask for any help. I just stuck it out all alone. While this method is typically great for doing GROUP PROJECTS by yourself (and cursing the other members out loud or in your head), this is definitely NOT ADVISABLE when dealing with mental health issues. Of course I didn’t know these back then, there was no internet, I didn’t have friends or relatives to talk to, plus I had no idea (or the people around me for that matter) that I was actually depressed. At 7 years old. Maybe 6. Around that time. This was in the early 90s.
But in this day and age, thanks to the internet, more and more information can be shared. Even better is that support groups are actually available, and you can join forums too, so people get to share so many stuff. Of course, I tried that, and it worked for about 6 months before I realized that in most groups I joined in, they weren’t exactly dealing with the depression in the most empowering way, so I got stuck in the victim mentality for a very long time. And the cycles of off-on depression mode kept getting worse each time. That’s when I decided to do things differently, and again, without drugs. FACING THE DEMONS IN MY HEAD is what I call it.
These are currently my go-to combination of methods when dealing with a depression relapse:
Shadow Work - Originally by Carl Jung, the principle is basic: identify the parts of yourself that you rejected due to external pressure, and heal them by understanding why it was rejected and suppressed, releasing the emotional charge by crying it out or something to that effect, and accepting that rejected part fully and without any regret. These aren’t the exact steps by Jung, but I just modified the method for myself. It’s pretty harsh because you need to face past trauma without any emotional attachments, and well, it can also do more harm than good. Only recommended to be done with a professional. Unless you’re a masochist. Just search the internet for Carl Jung and Shadow work for more info, I’m sure it’s quite famous.
Inner child healing - same as previous, but this time focusing more on the inner child (duh). Usually anything that persists for me, I would readily attribute to inner child issues so I would go to that part of myself and relive the trauma. Then pat my inner child and hug her till I stopped crying. By the way, crying is definitely included in almost every step. It’s soothing and also is a great way to transmute trauma. Provided that you’re fully aware of how the trauma happened and you’re able to release it fully. Again, if symptoms persist, consult a professional.
Kundalini Yoga and Meditation - amazingly there are many methods or kriyas and some are for dealing with depression. I call this method “killing two birds with one stone”, mainly because you get a real hard-core workout especially the upper body, and you lift your spirits up. Just search the internet for various methods, but I think 3HO is the one-stop shop for binge-reads. Again, crying is very much a part of this method because at some point, it will all just flow out.
Sound therapy - crystal singing bowls, gongs, tingshas, binaural sounds, isochronic music, subliminal messages, the works. I usually go to Youtube and just binge whatever I need at the moment. Sometimes I feel at peace, other times I just randomly cry. It just happens.
Energetic healing - again, there are numerous methods. I usually go for Reiki since it works for me, and because I can channel a bit more energy either from the original video or music, or on my own. Crying is again, an optional but very helpful step.
Emotion Code - This is the latest method I have learned, and tried. Created by Dr. Bradley Nelson, this method allows suppressed emotions, those you experienced yourself as well as the ones you inherited to be released from your body. You only need this chart, a fridge magnet, and determination. Also crying, if you can.
The stuff in my WHAT I USED TO DO list. - Seriously, self-healing depression is a very tiring and exhausting activity. Please, by all means, make yourself happy. In fact, YOU HAVE TO CHOOSE TO BE HAPPY TO SURVIVE THIS GRUELLING ACTIVITY. Whatever means necessary. Don’t worry, I won’t judge.
Other methods I tried in the past:
Parts work - It is like Shadow Work, but the rejected parts of your self have different age groups. I discovered it before Shadow work and for a while I tried my best to do it, but I still didn’t mesh with it after 2 months so I did Shadow Work instead. Maybe I’m just not cut out for it. I recommend the late Pete Gerlach’s website for more info and even methods and stuff. Super-educational, with some drawbacks. Still it maybe useful for others so please take a look.
Diet adjustments - Some say that food and nutrition affects moods,and maybe yeah, because many foods do create metabolites that become converted into chemicals that eventually become hormones. But for me, it didn’t work as well as the other methods. I mean, I eat a lot of veggies and fruit even before I was depressed and spritually awakened, and quite frankly nothing in this area changed me so I don’t include this in my list.
Again, note that I still haven’t included talking to other people in my list. Because again, I just can’t accept help properly, and I still want to do things on my own. HOWEVER, I tell the people I care for the most and also care for me that I HAD a depression relapse. I tell them after I won the battle, even for that moment. It kinda helps a lot. But this time I don’t want to energetically tie myself to others, I have to transmute my own shit so people won’t have to get mine. I also shield myself so their stuff won’t stick to me. It’s how I understand how karma should be worked out of our systems, it’s a DIY thing. Otherwise you just add more karma on top of your own.
Well, I don't know how to end this post, apart from the fact that this is still an on-going process for me. Case in point, honestly I am literally crying right now as I type this last part out. It took me 5 hours to type and it's a post worth almost my entire life so far, but I hope it's all worth it, for anyone who needs help in any way. I am not glorifying depression or suicide or even addictions here, I am putting this out there as information. This post has been at the back of my mind since the Lion's gate but I relapsed and I just got back so I could write it as orderly as I can. So please, I hope this post won't be misquoted or skewed or even be taken out of context. Again, this is mostly for educational purposes only. Especially when you feel like you're in the dark night of the soul.
Anyway, I hope this was helpful in any way possible. If you need any help *spiritual and/or energetic only, not a doctor guys* just shoot a comment or a message, and I'll see what I can do.
I hope you find the healing you seek. In love and hugs from Source above.
Mikazuki
三日月
**Special Note: While this whole thing is free to heart, share, attach a link-back of the original html (href, if you know what I mean), and to cite in any style (APA, MLA, Turabian, etc.) around 10-20% of its content, please, under any circumstances, FOR THE LOVE OF GLOB DO NOT COPY AND PASTE AND DECLARE THIS AS YOUR OWN. These are my own personal experiences, basically these are parts of myself that I need to transmute in order to heal. However, as this is already an output it is now included in the do-not-steal-entirely-or-else sections of the internet. Especially for people who just simply steal other people’s work as their own. I used to work as an editor and even now I do my best to cite sources, or at the very least insert links to sources that I actually used. Be respectful of content creators, large or small. Don’t take away from us the things that we made with all of our hearts. Those are the only things that help keep us up. Also, because you have no right do that you know. And just a reminder, Karma is a real b****. Just saying. Thank you very much for understanding. PS. If you found the information in this post to be very helpful, insightful, and of great value to you and your own personal journey, please feel free to reblog, share and heart/like, or if you feel super-generous, energetic exchanges are welcomed! Please click here and use this email address: [email protected] you so much and be blessed!
#suicide post#a post about suicide#a post about depression#depression post#suicide#depression#relapse#also a post on why seemingly-happy people suddenly kill themselves#to put it lightly#why happy people commit suicide#why seemingly-happy people commit suicide#my personal experience#my personal experience on being suicidal#my personal experience on depression#how is depression connected to suicide#how is relapse connected to suicide#how is relapse connected to depression#some suggested ways of dealing with depression#but first seek medical help#seriously#spiritual awakening and depression#spiritual awakening and suicide#depression and suicide
2 notes
·
View notes
Text
Paradise - Chapter Thirteen
A.N. - Hi guys, I would like to let you know this is the last update of 2017. My health has not been great the last few weeks and my writing has slipped. I write a few chapters ahead so I knew it would get posted but I am struggling to finish the latest chapter. Calling it writer's block is the easiest solution. I am planning on taking a few weeks off to catch up on my Bill writing and also allowing my body to heal from the latest flare-up.
This applies to my Stranger Things fanfic as well. But there is a Dacre/OFC coming up in the new year.
Happy Holidays and Best Wishes for the New Year.
Love Z xx

WARNINGS - SWEARING & SMUT
September 27th - Stockholm, Sweden
Bill’s POV
~~~~~~~~~~
She looked breathtaking. Her black dressed hugged her curves perfectly, the v-neck showing just a hint of cleavage. The dress didn’t have sleeves so her tattoos were on full show. The heels she was wearing made her already long legs even longer. The group of men sat in the booth by the doors stared at her as she walked towards our table. She slid into the booth beside me and pressed a kiss to my cheek. The waitress was over almost immediately.
Eva smiled up at her. “Hi Ellie, I believe Vinnie left me a bottle of Robertson behind the bar.”
Ellie smiled. “Of course, I'll bring it over. How many glasses?”
“Two’s fine. Thank you.”
“I thought you can’t drink,” Eija asked. Eva just winked at her.
Sam smirked, “You really know everyone don’t you.”
“Dimitri has been on the door since we came here for my 21st. Well I met Vinnie through his wife, she suggested me for a party he was organising when he just started here. Olivia has been here as long as Vinnie. And sweet Ellie, I rescued her from a handsy drunk on her third shift here.”
Ellie appeared with two glasses in her hands. “Watching her knockout four grown men was amazing. It’s the top one moment in my life and I have three kids.”
We laughed at her comment. The barman placed the stand in front of the table, in the centre so no one could trip over it. The bottled was nestled in the ice.
Ellie handed me the flute. “I won’t insult you by asking if you want me to open it.”
Eva laughed. “I think I'll be alright.”
I watched as she began to unravel the pink foil and twisted the cage off the cork. We all scooted as far away as possible waiting for the champagne to burst out of the bottle.
She rolled her eyes. “Jesus guys I know what I'm doing.”
With a twist, the cork popped but the liquid didn’t explode out of the bottle. She I filled both flutes before putting the bottle back on the ice. One of the glasses she pushed towards Eija.
“Try it.”
She took a sip then a larger one. “It’s good. Not too sweet or tart.”
“Want to know the shocker… there's no alcohol in it.”
She was surprised. “Really?”
Eva showed her the bottle label.
“Oh my god. You’d never know.”
Eija passed her glass around the table letting us all try it. She was right you couldn’t tell the difference. It tasted like normal champagne just slightly sweeter.
Eva leaned back into the booth, I stretched my arm along the back of the booth behind Eva’s shoulders.
She sipped her drink. “I think it would be hilarious to give a bottle to your dad.”
Valter snorted. “Don’t you’d kill him.”
Eva smirked, “I think that if he didn’t see the label he wouldn’t know.”
Alex leaned over the table. “You willing to bet on it?”
Eva held her hand out towards him. “Deal. We betting in dollars or krona?”
He shook Eva’s hand. “Dollars. $200.”
She had a naughty look on her face. “Deal.”
“I liked what you did with Valter.” Sam
Alex and Gustaf sniggered.
Eva shook her head, “Okay, what did I miss?”
Valter smiled. “They were insulting your work?”
“Hey! No, I wasn’t!” Alex exclaimed.
Eva laughed. “To be honest, out of all of you lot he’s the second easiest to dress.”
I nudged her, “Am I really that bad?”
“No. It’s just you don’t have a certain style, but you’re particular about what you wear. Valter knows what his style is, his wardrobe is simple but classic.”
Gustaf leaned over me. “Does that mean I'm the easiest?”
Eva raised an eyebrow. “You’re easy that's for sure.”
We all laughed while Gustaf pouted.
“If you really want to know Eija is the easiest to dress.”
She looked surprised. “Me? Why?”
Eva sipped her champagne. “You know your style and what you like wearing, but you’re still open to trying new things. I suppose that comes from the modelling side.”
Eva and Eija clinked glasses. “Us girls need to stick together.”
“Are you looking forward to going home?” Sam asked Eva.
She smiled, “Yeah. I can't remember when I was home last. Definitely, before filming started on IT. You guys are going to love it.”
“I'm looking forward to the food. I love Italian.” Valter rubbed his belly.
“Dad's cooking is the best.”
“Does your mum cook?” Eija asked Eva.
Eva burst out laughing. “Mum can burn boiled eggs.”
I smiled. Eva had definitely inherited her father's gene for cooking.
Eva sighed. “Dad does the cooking, we do the chores and mum look after the babies. Mum works from home, she turned the detached garage into her workshop.”
“Workshop? What does she do?” Alex asked.
Eva smirked. “She’s a metalsmith and carpenter. It was just her, my uncle and my grandpa that completed the build of our home.”
“Shit. Talk about role reversals.”
Eva nodded fiddling with her glass. “We were never a normal family.”
I turned to Eva, “Did you bring any cigarettes?”
She smiled at me and showed me her clutch, inside was her antique silver cigarette case.
“Come on let’s go.”
Eija joined us as we stood on the terrace looking out onto Stockholm. We took it in turns using Eva’s lighter. It was the colour of antique brass and had a tree etched onto the front. She’s had the lighter for as long as I could remember.
Eija leaned on the railing. “So what are you doing for the rest of the year?”
“Back home for a while. Back here before Christmas shopping, then spend the new year here. It's hard having a party at home when it's full of kids.”
I rested my spare hand on Eva's back.
“And what about you two?”
Eva shrugged. “I've haven't got any film stuff planned for next year. I'll most likely focus on the new lines. That means I can travel anywhere.”
“So you two are going to be shacked up somewhere fucking morning, noon and night.”
I laughed and pulled Eva closer, “We already do that.”
Eija clutched onto Eva’s arm. “4 years and you too haven’t stopped. You must tell me your secrets.”
Eva held onto the railing as she shook with laughter.
Eija cocked her head. “Come on. What’s funny?”
Eva breathed at last. “You think I've kept bill because I'm the one good at sex. Well… it’s the other way around. I’ve made him stay as he’s fucking amazing. There’s nothing better than his face between my thighs.”
Eija’s chin dropped and Eva went back to laughing. Valter appeared at the door.
“We’re ordering another round. What’s up with those two”
Eija turned to her baby brother. “Bill’s secretly a sex god.”
Valter screwed his face up in disgust. “We’ll wait for you.”
He disappeared back indoors. Eva had recovered enough and was trying to put away her case and lighter back into her bag one-handed. It happened almost in slow-mo. Eva’s lighter slipped from her hand. The three of us leant over the railings to watch it drop into the fake plants of the smoking area downstairs.
“Minchia!”
Eija took her hand. “Come on we’ll go down and get it.”
They both finished their cigarettes crushing them into one of the supplied ashtrays
Eva blew me a kiss. “We’ll be back soon.”
“Can you get me another vodka please,” Eija ordered.
Her and Eija linked arms and walked out of the club.
~~~~~~~~~~
Eva’s POV
It took Eija and me awhile to wiggle our way across the packed dance floor downstairs. The smoking area was busy too, but with Eija’s slim frame she squeezed between the wall and two people talking in rapid Russian.
She appeared minutes later my Zippo in her fingers. She handed it to me and I clutched it in my hand.
“Thank god. I love this lighter, I’ve had it since University.”
Eija laughed. “That thing has survived longer than most of my relationships.”
I grabbed onto her hand. “I doubt they were that bad. Let’s get back upstairs, it’s way too noisy down here.”
With my lighter safely tucked into my bra, we headed back through the massive to the stairs by the entrance. As we got closer to the bar I felt someone jostle my shoulder. I turned and saw the person who had knocked me, my apology died on my lips.
“You.”
“Hello, Alida.”
She caught sight of Eija behind me and smirked. “It didn’t take you long to worm your way in did it.”
I sighed. I really didn't want to do this. “You know for a fact it’s not like that. I worked with Stellan years before I met Bill.”
“You’re just a homewrecker”
“Yet again you know that’s not true. You were the one that walked away expecting bill to be there when you’d finished throwing a tantrum. This time he wasn’t.”
“That’s because he was in bed with you.”
Now I was really pissed. This girl didn’t know what to get off the bitch train.
“Look, I came here to spend some time with friends not here listening to you bitch. And for your information, I'm fucking Eija and Alex.” I heard Eija snort behind me.
Alida just stood there like a goldfish, not knowing what to say. “You fat fucking slut.”
I sighed. “There was me thinking girls matured out of schoolyard threats. Look just leave it, you're drunk and have no intention of acting like an adult.”
“So that's why he left because he likes fucking fat cripples.”
“One I'm not fat. I am perfectly in the middle of my BMI range. I try to work out as much as I can a lot more than your normal ‘fat’ person.” I used air quotes on the fat part. “Yes I have a chronic illness and yes it does affect my life. But you need to realise Bill is an adult he can make his own choices. I have not persuaded his choices in any way.”
“The retard can't find a man for herself so she has to steal one.” She said to her group of friends, they all giggled at her words.
You mess with fire you get burnt. I hated the R word with a passion, it's was horrible and derogative. I didn’t bother leaning in so only she could hear. “You can call me a cripple, a retard, fat, a pig, anything under the sun. I have heard it all before. The reason bill left wasn’t because I ‘stole him’. It’s because he couldn’t stand your childish behaviour. That and the sex was really shit. No one likes fucking a corpse.”
I grabbed Eija’s hand and pulled her out of the room and back up the stairs. I paused by the coat check where Olivia was stood. She looked up at the two of us.
“Everything okay ladies?”
Eija went to talk to her as I tried to steady my breathing. I was hanging onto the bannister, I was not going to have a panic attack over her. I saw Olivia talking into a radio. Eija came back over and rubbed my arm.
“I told her someone might try to get upstairs. So they're keeping an eye on her.”
“Thank you. I'm okay now.”
We walked back into V and made our way over to our table.
“You two were ages. What were you doing having a quickie?” Alex joked.
I was sat next to Bill trying to hide my shaking hands. I focused on my glass of champagne, watching the condensation run down the side of the glass.
He noticed and put an arm around my shoulders. “What’s wrong?”
Eija slid in next to Valter. “Your girl just went full-on girl power at Alida.”
“I shouldn't have said anything back to her. I'm now just as bad.” I huffed.
Bill held my chin and made me look at him. “What did she say.”
I squeezed his thigh. “she called me fat, a slut, a cripple, a retard and a homewrecker. I tried to be civil but in the end, I told her that you broke up with her because she acted like a child and was really shit in bed.
Everyone laughed.
Eija smirked over her glass. “They weren't your words.”
I put my hands over my face. “Okay… I said no one likes fucking a corpse.”
Everyone was laughing and had tears in their eyes. Bill took hold of my hands, placing them back into my lap. He pulled me closer, placing a kiss on my temple.
“You didn't do anything wrong. I'm glad she got what she deserved.”
“Yeah, it’s payback for her hitting you.” Alex laughed.
Eija nearly choked on her drink. “She hit you?!”
Bill nodded.
“Well if I knew that I would have let Eva carry on verbally bashing her.”
He sighed. “I didn't want to make a fuss about it. I just wanted her gone for good.”
Eija stirred her drink. “I hate to tell you like this Bill, but apparently Alex and I are sleeping with Eva.”
Alex choked on his pint and Bill laughed. “Yeah, I know. She's a nympho.”
Valter shuddered. “Please, can we stop talking about sex. I really don’t want to know the details about my sibling's sex lives.”
A wicked glint appeared in Eija’s eyes. She innocently stirred her vodka. “Apparently Bill’s got a very talented tongue. ”
Valter flushed bright red then buried his head in his arms on the table. Bill and Gustaf high fived while Alex was nearly crying with laughter. I reached over and patted Valter’s arm.
“With any luck it might it might be hereditary and then every woman you sleep will think you’re a god.”
I saw his shoulders shake with laughter. He sat back up and downed half his beer. “It’s not that bad when you say it like that. But please no more sex talk.”
I sat back in the booth leaning on Bill. Eija caught my eye and winked.
“I’ve always wanted to see you all naked.”
Everyone apart from Eija choked on their drink and began coughing. She just tipped her head back and laughed.
“Let me guess who has the biggest dick?”
I smiled and nodded.
Gustaf held up his hand. “I think I hold that title.”
I snorted. “Yeah right. I know who does.”
I felt Bill poke my side.
I smirked. “Yeah, definitely Eija.”
They all laughed at that. The door to V burst open and Alida flew through the doors. She was quickly followed by Oliva. She stopped at our table and began to scream at us. Oliva was frantically pressing her emergency button on her radio. Out the corner of my eye, I saw Alida reach for Valter’s pint glass. As quick as a flash I grabbed onto her wrist and twisted. She let out a cry of pain. I stood and towered above her. She tried to scratch and kick me, as I held onto her wrist.
“Clear the table,” I ordered.
Everyone grabbed their drinks so the table was free from glasses. I pushed Alida down so her chest was resting on the table. I twisted both arms behind her back so she couldn’t move. She managed to land a kick on my shin. I pulled her up from the table. She thought she could attack me again, trying to land kicks anywhere and trying to headbutt me a few times. That was it.
I swept her legs out from beneath her and dropped her to the floor. Still holding onto her arms behind her back I then knelt on the backs of her knees so she couldn’t kick out. As if by magic. Vinnie and two security guards came through the doors. They took over from me pinning her to the floor.
Vinnie helped me up. “I’m so sorry for this. A fight broke out and everyone had to attend, I now know why. Do you want to press charges?”
I shook my head. “I only did it because she reached for a glass. I didn’t know if she was going to pour it over me or smash me in the face.”
Vinnie squeezed my arm. “She’ll be gone.”
He motioned to the barman. “Give everyone a round of drinks on the house.”
The barman nodded. Oliva held the doors open as Vinnie and the two burly men from the security team carried Alida out of the bar. I sat down heavily back next to Bill, he wrapped his arms around me. His thumb rubbed circles on the back of my tense shoulders.
Ellie slid a small tumbler of whiskey into my shaking hands. She slid handed a glass to everyone at our table. Eija took her glass and smirked over the rim.
“Remind me not to piss you off.”
That did make me laugh. “Wait to we get home and watch my in the ring. My brother and I love beating each other up.”
“The tall one?” Valter asked.
I sipped the whiskey. “Yep. ever since we were little I love to floor him and give him a noogie. Even to this day I still can beat his ass.”
“So have you always done martial arts?” Sam asked.
I nodded. “Judo when I was five, started Kickboxing at 11 and started MMA when I was at uni.”
“Jesus.” Gustaf laughed.
I turned to Bill, “Haven’t you shown them the video?”
Bill shook his head and retrieved his phone. He found the video that had been filmed sometime during Atomic blonde and placed his phone in the middle of the table. During filming I was in the gym every day with Charlize, meaning that I was pretty strong.
Everyone watched as I lifted Bill onto my shoulders. I then lifted him above my head and proceeded to squat multiple times. Bill was trying not to laugh while I held him above my head.
Eija looked up at me and smiled. “I don’t believe it.”
Valters eyes were wide. “Can you do that now?”
I shook my head. “After my hip injury, I had to give up my weights and high-intensity training. It’s still not right now so I've been out of the gym for months. Once I'm better I should be able to get back.”
“I’d love to do stuff like that.” Valter sat back in the booth with his second pint.
“It’s a lot of hard work and a long road. There’s a couple of trainers I know round in Stockholm.”
Sam checked his watch. “What about we have a few more rounds then head home?”
I nodded, “Sounds good.”
Eija held out her glass of Vodka. “Here’s too drunk exs and buff girlfriends.”
We laughed and all clinked glasses.
It wasn’t long till we were the only group left in V. We got talking about dancing, Bill, Alexander and Gustaf knew how much I loved dancing. Not just my burlesque but ballroom and modern dancing as well. Sam didn’t believe me so Oliver the barman, who funnily enough was a competitive dancer, changed the CD and we waltzed around the floor. Eija wanted to have a go at the tango and Oliver was more than happy to comply.
Ellie danced as well and was more than happy to show Valter a few moves after I had convinced him of course. Alex caught my eye and winked, I remember him telling me about Valter being shy around girls. That was back when he was a teenager and he still hasn’t grown out of it. I tugged on Bill’s hand and pulled him onto the floor, the song changed into a slower piece. Over the years Bill had gotten better at dancer but still wasn’t a professional. We were more than happy to sway round in a small circle.
“I saw what you did with Valter.” He mumbled in my ear.
“He’s gotten better at talking to girls. My brother Mikey was like him, sometimes they just need a little push.”
Bill kindly let Sam have a go a dancing. He wasn't too bad, he didn't stand on my toes.
“Is Sanna okay. She looks tired.”
Sam half smiled. “Don't react. She's pregnant. We found out the day after I came to put your cannula in.”
My poker face was solid as a diamond. “I'm so happy for you two. Another boy?”
He chuckled. “You never know. We go to the doctors on the 29th to confirm.”
I grew tired and we all migrated back to our table. Oliver and Ellie pottered around and tidied up, collecting glasses and cleaning tables. They perched on the barstools just in case we needed anything.
It was one in the morning before we decided to head home. While we put on our jackets Olivia radioed for the biggest taxi, from where they parked up the road. She made sure we had all our belongings. The boys started down the stairs.
Olivia pulled me into a hug. She pulled away and held me at arm’s length. “Now you be good and look after yourself. When you’re next in town send me a text and we’ll meet for coffee.”
I smiled at her. “I promise.”
Her radio crackled into life and she listened to someone at the other end, even I didn’t understand what they were saying.
“There’s a slight delay of the taxi but it should be here in five minutes.”
With another quick hug, I made my way down the stairs.
Vinnie was at the bottom of the stairs as usual. He was shaking hands with the boys. He gave Eija and me a kiss on the cheek.
“Anytime you guys want to come back. Just call or send me an email.”
With a wave goodbye, we made our way out of the main doors. There were people meandering out in the courtyard in front of the club. Bill held onto my hand and kept me close to his back so I wouldn’t get pushed around by drunk people, Eija had hold of my other hand and protected my back. I didn’t pay attention to the people around us, I concentrated on my feet and not standing on the back of Bill’s boots. It was loud out the front, people were talking loudly and you could still hear the beat of the music. Most people out here were tipsy, some were blind drunk. People were smoking out here as the smoking areas in the club were always tiny and packed.
We stood on the pavement waiting for our taxi to appear around the corner. Even from a few yards, away Stockholm’s crisp night air was filled with cigarette smoke. I rummaged in my bag for my case and lighter. I ignited the cigarette then past it down the line. Between Me, Bill, Eija and Valter the cigarette was gone in minutes.
There was a loud group of girls back on the other side of the courtyard. Eija turned to look at them I felt her squeeze my hand.
“What?” I whispered.
She leaned in close to my ear so no one would hear. “Alida still here. She’s watching, kiss him.”
I really didn’t want to play games with Alida, it was just lowering myself down to her level. But Eija was right, she really did get off lightly. Attacking Bill could have resulted in her getting arrested, but always the gentleman Bill didn’t want to make anything of it. In my mind this was her punishment, watching Bill be happier with someone else. Thankfully in heels, I was nearly his height. I rested my hand on his shoulder.
“Hey.”
He turned to look at me. Before he could speak I pulled him closer crushing my lips to his. Bill wasn’t shocked as I thought he would be because we didn’t properly kiss in public. He wrapped his around my waist and pulled me closer. I swear I heard Eija laughing and one of the boy's wolf whistle. I pulled away and I rested my forehead on his.
“What was that for.” He asked.
I tried not to smirk. “Payback.”
He laughed. “You are a very naughty girl.”
The taxi brought us home and I paid the driver as I was the only sober one. Getting them all out of the car was like herding cats. I had to keep shushing them while I unlocked the door. The siblings clambered up the stairs.Ragnar who was asleep in the lounge was happy to see me. He and Bill followed me into the kitchen. There was a note on the kitchen table.
Hope you guys had fun.
There are water bottles in the fridge for all of you.
Ragnar was perfect as always
We will try not to wake you in the morning.
Meg & Dad.
True to their word there was a plastic basket with 7 water bottles in the fridge. I let Rangar out quickly while I lifted the basket out of the fridge. Bill took it out of my hands before I had lifted it off the shelf. Once Rangar was in I locked the back door and we climbed the stairs. Bill went to his sibling's rooms handing out the water. I took my makeup off and let my hair down. Bill came back in when I was standing in just black lace underwear, garter belt and heels.
It took his drunk brain a while to process the view. He shut the door and came to stand in front of me staring down at my breasts.
“Is that the set you bought in London?”
I nodded. “Want to take it off?”
His eyes bore into mine. “No. I want you to keep it on. And I want you to ride me.”
He stripped completely and lay back on his double bed. He had been hard since we were on the dance floor. It happened all the time, Bill said it was the feel of me swaying against him that did it. He watched as I stepped out of my heels and slid my panties down over my garters. Rule number two, even if it goes against all rules of being a lady, always wear one's panties over their garters. Rule two came into effect after Bill broke two of my garter belts trying to get them off.
I left my garter belt and bra on, Bill always loved taking them off later. I climbed on to the bed, letting him feel my wetness against his hard length. His hands rested on my hips as always, I began to gently rock against him. I felt his fingers grip me tighter.
“You’re going to kill me.”
I reached down and held him as I slid down all of his length. I watched as his eyes shut and his head tips back. I slowly rode him, dragging out his pleasure. He wet his thumb and tried to rub my clit, I smacked his hand away.
“Bete sig.” {Behave.}
He sat up and pulled me closer to his chest. He tangled his hands into my curls pulling my head back. He scattered kisses up my neck and over my chest. I picked up the pace slightly, rocking my hips. He wet his thumb again and reached down between us. I felt my orgasm build in the pit of my stomach. I clutched on to him my nails digging into shoulders.
I knew Bill wouldn’t last much longer, drunk Bill never did last long. I felt him reach behind me and unclasp my bra freeing my breasts. He latched onto my pierced nippled and bit gently. I gasp and clenched around him making him grunt. He pressed harder on my clit as I started riding him faster. He switched from one breast to the other and back again. Bill was getting near his end, his eyes were flickering shut. I pushed him back down onto the bed, I took over from him rubbing my clit. I knew I could get myself there quicker. I wasn’t fast enough as he got there before me. His fingers dug into my hips and his thrusts became uneven.
He spat out “I’m sorry.” through gritted teeth.
The feeling of him spilling inside triggered my own orgasm. I clenched around him, scraping my nails down his chest. I collapsed onto him unable to hold myself up. Bill slid out from under me and went into the bathroom, coming back with a damp washcloth. He cleaned me gently the warm cloth felt nice against my sensitive skin. Two minutes later Bill came back with my black pouch and a pair of panties from my case. He helped slip them up my legs but left my medication to me, not trusting himself while he was tipsy. He placed the pouch on the bedside table and switched off the light. We snuggled down under the covers, my head resting on Bill’s chest.
“Jag älskar dig, Eva.” {I love you, Eva.}
I smiled. “Jag älskar dig, Bill.” {I love you, Bill.}
#bill skarsgard#Bill Skarsgård#bill skarsgard imagine#Bill Skarsgård imagine#bill skarsgard fanfic#paradise#fanfic#imagine#roman godfrey#hemlock grove#pennywise#it movie 2017
18 notes
·
View notes
Text
2021 Ehlers Danlos Society Awareness Month (Day 9 Prompt: Inclusion)
Inclusion is a difficult topic for me as it's very difficult to feel included. This actually comes hand in hand with discrimination, segregation and inequality, especially being someone with EDS who can’t walk. When it comes to family, I can go into my own house and into my neighbor's house and that's about it. I grew up in the invisible illness community, eventually making me part of the rare disease community. As my symptoms progressed and I was paralyzed, becoming a permanent wheelchair user, then fell into the visible illness community. I will explain my lack of inclusion not only among the community, friends and family but also exclusion I face within the medical system and law enforcement.
I have been excluded by all outings and holidays by my extended family. My aunt likes to have holidays at her house and had a wheelchair ramp installed when her mom got older. Not long after the passing of my grandma, I was paralyzed, going into a chair. Being in a chair and my aunt knowing I cannot walk soon after removing the ramp from her house with little to no consideration of my needs so now when she has holiday dinners at her house I cannot go. I brought up the ramp once and she said “Well I didn't think about you” then later I realized how hurtful and mean what she said was so I sat down asking questions like “So you can't walk at all? “Have you ever tried to see if you can stand up?” “Well what about physical therapy?” “Well, I went to physical therapy when I had cancer and it helped a lot so I don't know why it didn't help you.” Which honestly was even more hurtful because I am not even a candidate for physical therapy after being paralyzed during physical therapy.
With cancer going rampant in my family somehow when family members ask about me and how I've been, they somehow seem to turn the conversation into cancer. “Trust me I know what pain is, I had cancer and if you ever get cancer you will learn what real pain feels like.” of from those older than me saying “You're too young for pain, Wait till you’re my age, then you’ll know what real pain is”, failing to even research EDS, Multiple Neuropathies, Complex Regional Pain Syndrome or any of my other conditions. The McGill Pain Scale has recently been challenged with a study done on a cohort of EDS patients. It was found that EDS is more painful than Complex Reginal Pain Syndrome which originally took the top place on the chart as the most painful condition with Cancer pain hitting around the mid range area of the scale. Some tend to downsize EDS and make it sound like I’m just a wimp for needing medication for my pain. I always hear things like “Me and my daughter were sick and we are both doing great now. Why aren't you getting better? Again, this relates my condition to cancer and other long term conditions that are a lot more common and have treatment and/or surgery that can put them into remission.
EDS has no remission. It doesn't magically go away. I have a gene mutation and as of now, you cannot repair a broken gene so this is forever. There is no remission but society is raised to believe cancer is the worst thing a person can ever go through and cancer is also one of those conditions where there are two outcomes. You go into remission and get better, living life normally or possibly on several meds to keep you functioning well, with the exception of younger children or some adults who have organ systems permanently damaged by chemo but even then they are much healthier and have a much more normal life than they did with active cancer. There's also the other side of the spectrum. You die. There are so many conditions that, depending on the type of cancer or hormonal mutations can easily be much worse than cancer leaving people much sicker than chemo patients but with no chance of remission. Imagine being on chemo for 50 years straight.
I have learned to hate the discussion of cancer when others compare pain and symptoms because many with chronic and/or rare diseases like Ehlers Danlos, Lupus, Muscular Sclerosis, Lateral Sclerosis, Rheumatoid Arthritis, Osteogenesis Imperfecta and many more are also very dangerous, have a lot of serious symptoms and comorbidities, risk the person's life and can very well cause more pain or more systemic symptoms than cancer. I am not saying cancer is not important, I am just saying people with these conditions are also compared with people who have cancer with most people who do this not knowing anything about our condition, just going off of the assumption that what we hear about most in the media, what has the most fundraisers and financial backing and what has the most attention has to be worse. Many more will get offended if you explain or give them information relating to the pain levels found in EDS mad that you would ever compare your own medical condition to cancer even after they just did the exact same thing by invalidating your pain and saying something like "If you think you're in pain now you should experience the pain that comes along with cancer. Now that's real pain" Its as if its okay for them to compare but not you making it automatically wrong for you to stick up for yourself when they try to invalidate your pain. The worst part is when they do this day in and day out without even noticing they are doing it. It gets exhausting and frustrating when someone is always trying to tell you why you are weak and spread the misconception that all cancer patients are much sicker than these other conditions, downgrading you. This leads to a lot of people giving unsolicited medical advice, telling you all the reasons why you aren't getting better knowing nothing about your condition so it really does go both ways and gets old to hear.
Another issue I had with inclusion was when my cousin got married. I have food allergies and couldn't eat anything they were serving. At the time I was a teenager and couldn't drive so my mom told my aunt she was going to go to Wendy's and get me a baked potato because I needed to take my medications and needed to take them with food. We were at the reception and next thing I knew my aunt was literally screaming at the top of her lungs at my mom about how she wishes my dad had never married her, she cant stand her and I’m a spoiled rotten little brat. My mom kept trying to get a word in telling her I have food allergies and can't eat what she has so it has nothing to do with being spoiled and it's not that I don't want what they are eating and honestly would probably rather have what they are eating but that I can’t because before my diagnosis gluten put me in multiple organ failure. My aunt was yelling about how she will not take my mom leaving and coming back and me eating Wendy's at their beautiful wedding and continued saying, if I’m hungry enough I will eat what they have and she needs to quit spoiling me and allowing me to have a different meal than everyone else was eating like I was a picky little kid instead of someone who if I ate what they were serving I can go into organ failure or anaphylactic shock. If she didn't think a Wendy's baked potato fit into her daughter's wedding décor scheme she would have really not been happy to have an emergency squad backed up to the door, a gurney and a bunch of paramedics so my mom, myself and my dad didn't understand why she was making such a big deal out of it. My dad then told my aunt we are going to leave and apologies to my cousin for leaving the reception early. After he did this my aunt started calling my mom and I derogatory terms still yelling while my mom was simply talking and trying to keep it quiet so it wouldn't be a big deal but she started calling me and my mom derogatory names and didn't talk to my mom for two years all over a baked potato and my food allergies.

Outside of the family also have little access to inclusion as I have not one friend with a wheelchair ramp or no steps going into their house so zero access to visiting friends as well as family. The lack of understanding crosses over to friends as well and I have lost most of them. I’m not the best when it comes to visiting friends as my health is so unpredictable and many people take this as me being flakey or not wanting to visit when most of them knew how timely and never canceled on them when I was healthier. I also had two friends who used me and manipulated the situation to make it sound as if I was the reason we never hang out. One of these people, she and her husband did a lot of traveling and it seemed like every time she was out of town she would contact me and ask if she and her husband could come visit me when they came back. I would agree and when she was back in town she would usually ignore my messages until a day or two before leaving again and say “I wish you would have said something sooner. We’re packing up now and about to leave to go to Florida now. They would leave and she would message me saying they were on a Disney cruise but when she comes back they wanted to visit me if I was up for it. Again she would either not tell me when she got home or I would message her that day or a day or two later telling her if they want to visit it's fine with no response and no response until right before they were about to leave again saying something like “Oh, well we're about to go to California. I wish you would have let me know sooner, not acknowledging the message was originally sent a week or two prior. When I finally asked if they really wanted to visit or not and what was going on, she then responded saying, well every time I ask if you want to hang out, you never do which was far from the truth since she would only talk about visiting when on vacation or while packing to leave the state again.
Another friend of mine since high school did something similar. She would call or text me and ask if I wanted to hang out the next day and of course sometimes I said no but a lot of the times I said sure because it was something low key like she would come over here to visit or just meet at the dog park or something. If I said yes she would say “I know you have good days and bad days and your health can change so if you are still up for it call me at 10:00 in the morning and let me know what you want to do. Well 10:00 am would come around and I would call her and say I was up for hanging out and she would say “well, I’m actually at my sister in laws now so can we do it another time” another time she would call and tell me if I’m up for it call her around noon and I would call her at 11:30 or so and tell her I’m up for it and she would say “Oh, well I didn't know if you would be up for it or not, I actually took my daughter to the park so we will have to get together another time.” Next time she would call me that morning and tell me she was going to be in my area and asked if I wanted to meet her for lunch. I would agree and she said she was going to take a nap and to call her at noon. I would call and she would say “Oh, well I’m at the mall with another friend, can we meet up another day”
Don't get me wrong, she was like this before I got sick and when we were kids where she would cancel a lot but when I got sick and she was calling me at least once a month to hang out and after two years went by and every single one she canceled out on me to hang out with another friend or go somewhere else and only two of those were because you had a doctor appointment or something and declined on your own there's a problem. I asked why she didn’t seem to want to hang out and she said “What's the point because every time I call you say you're not up for it. When I only said I wasn't up for it twice and she canceled more than 20 times in a row, having no problem telling me she was hanging out with a friend from work or someone else making plans to replace the plans she made with me so this is another struggle I have faced since getting sicker.
The people I used to think were my friends who obviously don't like me because I’m boring and can't go out and party, run around the mall for 8 hours or go to the fair and ride all the rides with them but now can only handle the low key stuff like lunch, going to watch a movie, stay here and play cards, go to one of those paint with a friend things or something low key like that and I know the fact is that they don't like these low key activities and think I’m boring to hang out with but don't want to tell me this and I truly believe they don't want to admit to themselves that they don't like me anymore since I’m now disabled so they try to push the blame on me and throw it into the pile of problems I already have lol so friendships just don't work out well for me either.
Now that we have covered inclusion with family and friends let's talk about the community. I have always said, even before I was disabled that the communities that face the most inequality and discrimination are the communities you never hear about when discrimination and inequality is brought up. The Deaf Community, the Disabled Community, the LGBTQ+ Community, the Rare Disease Community and the Invisible Illness Community are the communities who I believe have the most severe lack of inclusion, face the most discrimination, face the most prejudice, endure the most physical, verbal and emotional abuse and have the fewest rights many take for granted. Black Lives Matter has really made me realize how severe these disparities are. Being in a chair I can’t just go to a small town. If we are going on a trip to Cleveland Clinic or the University of Toledo and we are driving through a small town with a lot of small, mom and pop businesses I can't stop and shop at one of those stores. If I have to go to the bathroom they don't have a wheelchair ramp going into their building so not only can I not go into a single store but I am unwelcomed by the entire city.
With ADA being signed in 1990, 21 years later the Columbus Police Department says and I quote “ADA laws aren't real laws and shouldn't be treated as such. Our own police have left me outside on the second coldest day of the year in January when two cars parked illegally in front of both handicap curb cut ramps going down to a parking lot. Instead of enforcing these laws and punishing those who illegally parked in front of these ramps or taking the time to send an officer out to help get me and my chair off of the curb they told me it was my problem and though every building in the strip mall had closed down that it was my responsibility to sit out in the cold with pure autonomic failure and the inability maintain my body temperature indefinitely until someone came back for their car which resulted in me going into hypothermia.
With BLM coming to the surface the disabled are seen as weak and also are essentially the punishing back for the black community now just because we are seen as weak and easy targets to take their anger out on. I have been through the illegal parking issue time and time again. Another time a black man parked in front of the curb cut. My dad kindly asked him to move his vehicle and he told us we had to wait while he finished his conversation with his friend which took about 20 minutes. We were in a bad area of town and my dad and I were the minority so there wasn't much we could say or do or we would be seen as the ones who were racist. This 20 minutes was one of the scariest times of my life as a woman overheard my dad asking him if he would mind moving his vehicle so I could use the ramp. She came up to me and pointed to my dad who is a senior citizen, asking why he can't lift me up in my chair and off of the curb. This area was old and fan down so the sidewalks had been done multiple times so the curb was quite high. It was about 10 inches up from the parking lot so not a little bump I can just back off of and I was 112 lbs., sitting in a 39 lb. wheelchair with a 17 lb. service dog and I didn't understand what she was talking about because she couldn't possibly mean for him to lift all of that weight himself and put me onto the ground plus the wheels spin and even with the wheels locked the wheels will still move so you need two people to lift a person in a chair without flipping it. Anyhow, kind of confused I said “No, I don't think so”
She then went off yelling about how I'm an overly entitled white bitch who thinks she can get whatever I want handed to me on a golden platter. My family probably owned slaves and how I have a lot of nerve to ask a “N word” to move their car so I can use a ramp that belongs to the community and doesn't have my name on it. How he can park wherever he damn well pleases and white bitches like me need to be shot thanking we can get all our NEEDS met when we don't even know what needs are because they “N words” have had to go without their needs for 400 years now calling me multiple swear words and derogatory terms as well as saying multiple times that I need shot. After about 20 minutes of her in my face screaming at me during Covid and me saying please, I have a compromised immune system or I’m sorry, I just can't get to my car the guy finally said he would move his car for us to leave. It was terrifying but things like this happen all the time.


Another incident happened in Aldi near the beginning of the pandemic. The checkout line was massive and stretched ¾ way down the second isle. And there was one of those electric pallet jack things they use that can't be moved because you need a key to start them on the right side of the isle so no space to get through I just waited at the back of the line until it got past the pallet jack so I could get by which wasn't an issue because the line always moves really fast at Aldi and there were only two people with carts in line behind the pallet jack so I got in line behind the last woman in line and locked my breaks. I put my smaller service dog on my lap because the isle was really crowded and I didn't want her to get stepped on.
Next thing I knew there was a black woman coming around the corner yelling everybody move, get out of my way slamming her cart into the back of my nearly new $7000 wheelchair and $7000 smart drive so hard that she shoved me in my chair, with the wheels locked about two feet forward and my foot plate into the ankles of the woman in front of me and kept pushing her cart yelling at me to move. I was still shocked at what was happening so all I could do was say “I can’t” because of course the line ran beside the pallet jack which couldn't be moved so there was only about 4 inches between the edge of the fork of the pallet jack and everyone's cart. The woman let go of her cart and walked up to the side of my chair, grabbing my right side push rims and tires and yelled “I SAID MOVE!” and pulled up flipping me and my service dog out of my chair and onto the ground with my body hitting the shelf to my left and dragging a ton of baking products off the shelf and on top of us. A bunch of people turned around and gasped when she did this and the woman's teenage daughter embarrassingly yelled “MOM NO!” then ran up around her mom and flipped my chair upright.
I was sitting there on the ground so shocked I still didn't know if I was hurt being someone who is prone to dislocations, traumatic brain injuries and having multiple spinal cord manifestations. The woman's daughter was almost in tears from embarrassment and reached down to grab my arm to try to help get me back into my chair when her mom yelled at her to get over there The girl said “but mom” and she said “get your ass over here now” and turned around her cart to start to go around the next isle. The girl then let go of my arm, her eyes still all watery because she was about to cry, she mouthed to me “I’m sorry” and ran around to the other isle where her mom was. Of course I didn't blame her daughter. She tried to help and I felt bad for her too. She tried and proved she was different from her mom.
After they went down the other isle the woman in front of her and the woman in front of me started helping me. I was checking my service dog Maggie to make sure she wasn't hurt and she seemed fine, just had eyes as big as saucers like she was kind of in shock over the whole thing too. The lady in front of me picked Maggie up off of me and held her in one arm while both picked up all of the cake, brownie, cookie and powdered sugar laying on the floor and all over me and put it on the shelf. She then put Maggie down on the floor for a second while they both helped get me back into my chair and then the one in front of me picked Maggie up again and put her on my lap. The Lady in front of me pulled up her pants leg to look at the back of her ankle where my foot plate slammed into her and she was bleeding. I apologized and she laughed sarcastically and said “It's not your fault, trust me, you are not the one who should be apologizing for this.
The three of us started talking with the one in front of her talking about how disgusting it was that she did that to me when right then the woman who slammed the cart into the back of me came up the front of the isle yelling at everyone near the front of the line to get out of her way. She didn't physically assault any of them like she did me but she was yelling at everyone to get out of her way, shoving her way between carts to try to get things off of the shelf and throwing it into her cart. There were only two employees working that day, one ringing people up and one trying to stock all of the shelves that were being picked through faster than she could stock so I can't blame the employees either because they were grossly understaffed.
I have had so many experiences like this since Black Lives Matter took off, a lab core worker talking bad about me because I showed up without an appointment when their door and website says “Walk ins welcome” and I tried to make an appointment but the captcha was down on their website so I wasn't able to confirm that I wasn’t a robot in order to submit my appointment and purposely showed up at 11:30 am because you could see already claimed appointments and 11:00, 11:30, and 12:00 were all open appointments. To make things better, My doctor had already sent the request and I scanned it into the tablet they had there as well as scanning in pictures of my license and insurance so everything was filled out and all I needed was to pick up two plastic, half gallon jugs for a 24 hour urine test.
She was in the back calling me similar names to what the woman did at the eye center when the guy was illegally parked, bringing up slavery and how my grandparents may have been able to get away with whipping “N words” to get them to do what they wanted but I can’t, how inconsiderate I was for walking in and who did I think I was thinking I can just walk in all unannounced without an appointment. She said “I ought to slap that bitch! Girl, you gonna have to hold me back before I slap that bitch” talking to the other phlebotomist. I could hear everything she was saying after she closed the door and she went on and on, came out and asked for my paperwork so she could put it in the system, ripping it out of my hand, kept going on and on saying nasty things about me then finally came back out and nicely said “Oh, I didn't know you already put all of this in the system for me. So you’re just here to pick up the jug?” I said “Yeah, I've done one of these before so I don't need any instructions or anything, just the jugs. She went back and still talking nasty about me came back a minute later with the jugs and said nicely have a nice day but still her body language wasn't nice and you could tell her friendly voice was sarcastic.
That's when I decided to stick up for myself and stopped her before she closed the door again and said, “Did you know your walls aren’t sound proof? I heard every word you said about me while I was back there and just so you know, I tried to make an appointment before I came here. The captcha is down on your website; you know, the little thing you have to click online to prove you’re not a robot? It wasn't working so I couldn't click it to submit my appointment request but it said online and on your door that walk-ins are welcome. I saw you had empty appointments from 11-12. I didn't know if anyone else would be here since the site was down but that's why I chose to come now because I didn't think you would be busy because of Covid and all but I did try to make an appointment. Her facial dropped.
She then started kissing up to me saying “Oh sweetie, you are totally fine, that's what we're here for, come anytime you need to, she walked over to the double doors and opened the first one saying “Let me get that door for you sweetie.” pointed to the floor and said “Do you see that spot right there with no carpet? There used to be a big lip in the door right here and I personally had it removed just for people like you who are in wheelchairs so your wheels won't get stuck on it. Would you like me to get the other door for you?” I said “No, that's okay, It’s not that heavy, I’ve got it” she then said “No, no, no, I insist. I’ll hold it open for you, I’m here to serve you. She then followed me outside where my dad was parked which was awkward and said “would you like me to help you into your car?”
These are the more major examples but I’ve had more minor interactions too such as trying to buy vinyl for my Cricut maker from a black small business owner to be told “Sorry, I only buy from and sell to black people” I had a dental appointment and Medicare and Medicaid is a death sentence for those with rare diseases with only two dentists that took my insurance within a 30 mile radius. I settled for Refresh Dental in Hebron, Ohio which was quite a drive but none that took my insurance were close so I made an appointment. When I called I asked if they were ADA accessible because I’m a wheelchair user and the receptionist said yes. I then asked about Covid and the precautions they take because I’m immunocompromised. She said they are very careful, told me they wear full PPE, mask, face shield, smocks, they have updated their HVAC system and are really clean. She said none of their staff had contracted Covid so I made an appointment.
When we got there we parked at a building that looked like it was about to fall in. Termites had eaten all the way through the window ledge, and you could see the studs behind it. When I went up to the door I was relieved to see a sign saying to go to the white building behind that one, surrounded by a bunch of orange stickers which looked like condemned stickers. Their driveway was gravel and anyone who is in a chair knows, a gravel driveway isn't easy to roll on at all so though it was cold outside I was getting myself into a sweat going back to the building behind it. The first thing I saw was a staircase with about 9 steps up into the building and I was thinking uh oh. I hope they have another door. I went around the building and found another door and this one had two steps into it. It was a door with a step into it, you walked about 5 steps and stepped up another step into a second door. I called the office and no one answered.
I then called my mom who was in the car by the first building and asked her to come over there. She saw the steps and said “You’ve got to be kidding me” and went into the building to talk to them and then came back out and told me what they said. She asked the receptionist if they had a ramp or another way into the building for people in a wheelchair. The receptionist pointed to the door that my mom just came in and said “That's the door our disabled patients use” My mom told her I’m in a wheelchair and called ahead of time and was told they are ADA accessible and the receptionist said “We are ADA accessible.” My mom followed up saying “Then how can someone in a wheelchair get in here? The receptionist said “Can't she just walk in here?” My mom said “No, she’s paralyzed” The receptionist then said “Well we have other patients in wheelchairs and they just leave their wheelchair outside and walk in here. It's only two steps.” My mom then said “So, we just drove 40 minutes here and you’re not ADA accessible?” The receptionist said “Yes, we are” my mom said “but you don't have a ramp?” She said “When your daughter called she asked if we are ADA accessible. We’re ADA accessible, not wheelchair accessible.” My mom said “First of all wheelchair accessibility is part of being ADA Accessible, you don't have wheelchair access you are not ADA Accessible and second of all, she told you she was a wheelchair user so I don't know what else you could have thought she meant by ADA accessible. The receptionist said she had to go speak to another staff member. She then told my mom to have me go back up to the front building and they would bring supplies from this building and meet me over there to see me.
We went back to the first building and I had been sitting out in the cold all this time. We sat outside the building for 20 minutes waiting for someone to come unlock it. I then called their office and this time someone answered and I said “I’m really sorry for bothering you but will it be a while before anyone gets over here? The reason I’m asking is because I have Autonomic Dysfunction so cant maintain my body heat well and was wondering if it was okay if we go back out and sit in the car until someone is ready for us” She said “stay there, she should be there right now” I said okay and waited, finally about 5 minutes later someone came to the door and opened it. The concrete wheelchair ramp was so old that it had sunk about two inches into the ground so I still had to pop a wheelie and push on my wheels while my mom pushed the back of my chair to get up into the door.



When we got in there it was filthy, every surface was covered in dust, dirt, wood chips and dead bugs. It smelled like the moldy basement of my sisters 1890 house. It was so dirty that I put my service dog in my lab because I didn’t want her to sit on the floor. I could see a trail from my wheels and my mom's footprints in the coat of dirt on the floor. The receptionist brought out paperwork for me to fill out and while I did she and the hygienist were flipping breakers to turn on electricity to one of the rooms and were bringing over a laptop, air purifier and some dental tools. I could see them in the room. The hygienist took a dry paper towel and brushed the dirt off of the chair and edge of the countertop onto the floor, not using any chemicals or even moisture to clean anything. The dirt started floating around in the air which was when they brought in the air purifier to suck some of it up. She sat the dental tools straight onto the counter she had simply brushed the dirt and dead bugs off of. I watched them do all of this while I filled out my paperwork and sat in my chair waiting for my appointment. They eventually called me back, now well over an hour after my appointment time. I gave my service dog to my mom because they had to do x rays and went back.
I got in the dirty chair and the hygienist only had a mask on and nothing else. She wheeled in an old x ray machine that looked like it was jimmy rigged to a sawed off IV pole. She put the bite wings in my mouth and tried to take the image and nothing happened. She yelled at the receptionist to hit another breaker and took the first image of the tooth that was bothering me. She then pulled the bite wings out of my mouth and that's when I noticed that they were reusable bite wings and having a lot of medical knowledge I knew those cannot go into an autoclave and was horrified when I saw that they didn’t have the clear sanitary cover bags on them to prevent the spread of disease but at this point I had already had them in my mouth and the damage was done. Having no clue if I had just essentially French kissed a Covid patient while being immunocompromised myself and having a condition that so far no one with it who has contracted Covid has survived it was too late so I didn't say anything. She put it back in my mouth for another image. Once she was done she grabbed a camera made for taking pictures of the inside of the mouth. It also had no sanitary covering on it and she took pictures of my teeth and said we have to wait for the dentist to come over.
I looked around the room while waiting and it was totally empty except for the chair I was sitting in. There were no pictures on the wall, no curtains, no TV, no pedestal where the little sink you can spit in usually is and where the cleaning tools and suction hook up, no chest of drawers with toothpaste or other supplies. They didn't even have any light in the room, just a light fixture with wires hanging out of it. Just a very thick coat of dirt, dust and dead bugs everywhere and a window letting light in. When I looked at the window I noticed there was light coming in around the window where termites had eaten holes all the way through the wall around the window casing. There were brown streaks running down the wall where water had come in the holes which I was assuming explained the moldy smell because if there was water getting all the way inside through the swiss cheese termite walls then there is probably a ton of water and mold behind the walls. I I continued scanning the room while talking to the hygienist about my dry mouth and she told me she was going to give me some jell to trial for dry mouth. Soon after, the dentist came in and was very cold. He said nothing to me at all but said to the hygienist “Cavity on 15 and 16” and left totally ignoring me when I said hi. The hygienist told me to go to the front where the receptionist was to schedule a filling and a second appointment for a comprehensive dental since they refused to do them the same day or do the imaging of my whole mouth when doing the images of the one tooth.
the receptionist had brought over a laptop of her own and tried to schedule my filling for two days after I got the second Covid vaccine and I told her I didn't think that would work because I would get the vaccine less than 48 hours prior to the appointment and I didn't know if it would make me sick or how long your sick for when you get it but I know my nurse didn't feel well for about a week after hers. The receptionists said “You’ll be fine” and scheduled it anyhow making sure to tell me about their cancellation policy and fine which she should know with the vaccine I wouldn't know how it effected me until the cancellation policy had passed. She then went on to tell me that she cant get it because she has a heart problem. I told her I couldn't either at first either but not because of my heart problems but because I'm a high anaphylaxis risk but my doctor came up with a concoction of meds that we can take starting two days before the vaccine, the day of and three days after that has shown to prevent full blown anaphylactic shock in most of us. She said we would have some kind of allergic reaction and still can go into anaphylactic shock but it will reduce the chances so hopefully the allergic reaction is tolerable and we won't need to go to the hospital. So I went that route and got the vaccine at a place close to the hospital. I then said, It's too bad that more healthy people don't consider people who literally can't get a vaccine or are immunocompromised and won't get the full benefit, or any benefit at all from the vaccine before they refuse to get it. She said Actually, I can get it, I just dont think I should get it. My dad got it and my sister and I tried to tell him not to get it but he didn't listen to us and got it anyway but I guess when you're old or sick like you guys are and are going to die sooner than later anyhow you don't really have much to lose.”
I felt like she was throwing me in the grave. She then said “you know that they chop up aborted babies and put them into the vaccine right? I said “Nahh.. that's just a rumor that went viral on Facebook that was originally created by some college freshmen. There's no fetal tissue at all in the vaccine. Where the fetal tissue comes from was in the 70s and 80s two women voluntarily donated their aborted fetuses to science. No other fetuses have been used since then because they have replicated the cells over and over again. Think of cloning. They do this so they won’t need any more fetal cells. The replicated cells aren't used in the vaccine, they are used in the early states of testing potential vaccines before they even start conducting studies on animals and after the hypothesizing stage to see how human and living cells respond to benign injected with the possible vaccine to ensure it doesn't harm the cells and does what its supposed to, which not only saves money because the cells can be replicated over and over again but it also helps save animals because its a way to test the vaccine before moving on to testing on them. Of course a lot more can be found on living animals than just in cells so things can still go wrong in the animal phases but there is no aborted fetus at all in the vaccine, it's simply used as a cell to test the vaccine on.” She said Well I’m a nurse too, not just a receptionist so I would know.
I then thought this would be the perfect opportunity to change the subject and said “Oh, really, I am too. I graduated from Columbus State, where did you go to school?” She changed the subject back saying, I know a lot of nurses and none of them have gotten the vaccine. Only a few people here have gotten vaccinated and this place has been riddled with Covid. Almost all of the ladies have had it at least once and they all are okay now. How many people do you know who have gotten vaccinated? I said “When I called to make this appointment I asked about Covid because of being immunocompromised and the person I spoke to told me no one had gotten it. Why would they lie to me? She said “I don't know who you spoke with but that's not true. This place has been riddled with it” At this point I was letting what she said simmer a bit and sink in, honestly not happy at all that they had lied to me more than once at this point and about very important issues.
She then went back asking me how many nurses I knew who had gotten vaccinated. I said all of them and not even just people I graduated with my home health infusion nurse got hers but she ended up getting Covid too. Idk if you saw on the news about the senior husband and wife that got Covid and the nurse arranged for them to be put in a room together and they died within minutes of each other? Well the nurse who set that up, her name is Mariah and I went to high school with her. Just a fun fact I guess.” She said “Well did she get vaccinated? I said “yeah and right then the hygienist came back with the dry mouth gel so I cut the conversation off and said I needed to go because my mom was out in the car. I couldn’t believe they had a halfway decent office for their able bodied patient but put their patients in chairs into a filthy, condemned building that is moldy and about to fall in from termite damage. If that's not discrimination, I don't know what is. and to top things off, I put the dry mouth jell into my mouth and it tasted awful. I looked at the expiration date and they had just given me and it had expired over a year prior. I saw another dentist and also found out that I never had a cavity at all and my wisdom tooth was coming in.
I do not feel included when it comes to my extended family, friends, community or country. Most things labeled handicap accessible aren't including the Franklin County Social Security Office which slaps a handicap sign on their bathroom stall which the door is so narrow that my tiny wheelchair for my 112 lb. self rubbed the edges of the door trying to get into it, not meeting the 32” door clearance standards listed in the ADA laws nor did it meet the minimum 5’x5’ size limit in order to be ADA accessible so most people in chairs cant use it at all and even those with tiny wheelchairs like mine cannot get their char in far enough to close the door so are forced to use the bathroom with the door open, on their period while people walk past and see everything. It’s disgusting that we live in a society where people in wheelchairs, even if they can hold their bladders are forced to wear adult diapers or map out every public facility, only going to ones they know are accessible enough because here in the US we are so welcomed and marginalized that we don't even have access to about half of the businesses in the US let alone a bathroom that everyone else in the world who is not a wheelchair user takes for granted and when we are lucky enough to find a palace that has a toilet we can use, it's always the filthiest ones, the ones that able bodied people use as their private pooping palace believing that just because it’s two or three feet wider that extra three feet will make their fart inaudible.
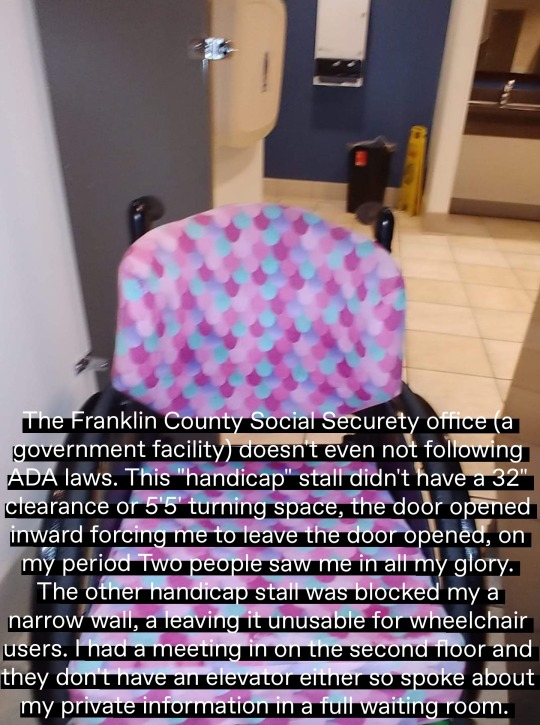
This is a country where an able bodied person can buy a new car for $16,000 and a used one for sometimes less than 2 grand but if you’re disabled your new accessible vehicle costs around $75,000, a used… well many states you can’t insure a van that is more than 5 years old and cannot convert one more than 4 years old and it has to be less than $50,000 miles and fit a bunch of other criteria so used isn't much less. We live in a country where you are not allowed to pay an able bodied worker less than minimum wage yet SSDI comes out to $2.60 less than minimum wage and employers are allowed to pay disabled workers less than minimum wage. We live in a country where ADA laws were passed but police officers don't have to enforce any of these laws. Here in the US they have schools for girls only, boys only, black only, deaf and blind but no special schools for children with physical or developmental disabilities, just life skills training for adults so education is still not equal. A country where if the Black or Asian Americans are brutalized by the police or community members and it is broadcasted on the news even though more than 70 percent of police brutalities in fact occur to those who have physical, psychological or developmental disabilities but this is never mentioned even if the person fits into two minority groups.
This is a country where if you have a service animal that you rely on you still don’t have the freedom of religion because a church can legally turn away a service animal. A country where if you are a drug addict you can get 50 mg of low dose naltrexone free and go to suboxone clinics free of charge but if you are a chronic pain patient you have to pay over 300 for 2 mg of naltrexone to control your pain and stay off of opioids which are oftentimes the only things covered on Medicare but also the same medications being cracked down on not by people who need them for chronic pain but by addicts in turn putting limits on opioids so drug addicts can live and chronic pain patients who are in so much pain they have seizures and go into organ failure to live in agony and possibly even eventually die weather it be suicide because they cant stand the pain or from organ failure that results from the pain.
A country where doctors are taught “if you hear hoof prints on the ground think horses not zebras'' meaning when a patient presents with a symptom consider common conditions that can be associated with these symptoms not rare diseases allowing doctors to abuse and neglect patients and slap psychological diagnoses on them so they don't have to jump into the rare disease realm of medicine or even learn about it in school. This results in more than 250,000 deaths each year from medical neglect alone and that's not even the people like my mom who wake up on life support to find out days of their lives have passed and they are now living with permanent disability. A country where there are still states like ohio where you cannot sue for medical abuse and neglect unless someone died or comes out essentially a vegetable and if this results in disability where you are in a wheelchair or have limited cognitive impairment but can still speak and think to some degree, yet still resulting in permanent disability, it's just too bad, so sad for you because sure you went in for a simple gallbladder removal and came out needing the blood in your body replaced 4 times, going into exploratory surgery with a 5 percent chance of survival, split from your breast to your pelvic bone to have all of your organs removed, your liver repaired which fell apart multiple times in the process of trying to sew back together your liver the other doctor cut open and tried to hide for 9 hours while you bleed to death, sure you came out on life support after being deemed legally dead multiple times and had four brain aneurysms because of this trauma, which resulted in cognitive impairment, missed months of work only to get laid off, now deal with chronic pain, fatigue and weakness for the rest of your life and will never be able function like you once did ever again but you didn't die and you're not cognitively impaired enough so that's on you, the doctor on the other hand can keep operating on people as if nothing ever happened.
America is where people on Welfare, who are poor and in many cases don't want to work, make more money and get more financial benefits than someone on SSDI who is disabled and literally can't work. A country where people on Medicaid who are poor get better healthcare than the sick and elderly on Medicaid and if you qualify for both Medicare and Medicaid you might as well forget it because your insurance isn't much better than having no insurance at all regardless as to what special programs you fit into, where the Medicare formulary trumps the Medicaid formulary and if Medicaid for the poor covers a service but Medicare doesn’t, what Medicare says, goes and you simply don't get coverage for your needs. A country where a president cuts funding to the Orphan Drug Tax Credit, oftentimes the only funding that most rare diseases have to study possible treatments for these diseases while cutting taxes multi billion dollar industries have to pay in taxes such as his hotels and golf courses and every time they send out a relief check during Covid they make up for it by cutting funding to either schools or Medicare, particularly Medicare recipients with rare diseases, removing them from the formulary and allowing them to die to pay for these checks, hitting those with rare diseases because they are just that rare, meaning less people to complain so it's less likely there will be large riots for these people. This essentially reversed the act put in place ensuring those with preexisting conditions can get insurance leaving us so underinsured that many will likely die because they cannot get their medical care covered and can't afford it.

A place where those with disabilities are still not accepted, ADA is not yet being utilized in many areas or even seen as real or legitimate leaving us to be isolated from all aspects of our lives. We have very few rights, access, equality or inclusion more than 20 years after the signing of ADA into law. This leaves a lot of people like me to live lonely lives where we have no chance to succeed or in some cases such as those issues related to Medicare, not even a chance to live. By law an insurance company cannot deny you insurance based on pre-existing conditions however they can deny you coverage of the vital care you need once issuing you a card leaving insurance virtually useless with many rare diseases making survival of the fittest a terrifying reality. Welcome to America. The home of land of the free and home of the brave.
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-15/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-11/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-8/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-7/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-6/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-5/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-4/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-3/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes
Photo

New Post has been published on https://usviraltrends.com/whats-your-risk-of-kidney-disease-heart-attack-or-diabetes-a-single-molecule-can-tell-science-2/
What’s your risk of kidney disease, heart attack, or diabetes? A single molecule can tell | Science
Nate Henry (right), Nick’s identical twin, is healthy. Nick’s high levels of a molecule called suPAR may explain his illness.
Kevin Beasley
By Stephen S. HallApr. 19, 2018 , 12:15 PM
Nick Henry first experienced the symptoms of kidney disease in 2004, shortly after the 19-year-old had a severe reaction to a spider bite. “I woke up one morning, and I was just swollen from head to toe,” he recalls. But doctors managed Henry’s disease, allowing him to return to his unusually active lifestyle—including baseball, softball, basketball, flag football, golf, and fishing—in his northeast Louisiana hometown of West Monroe. Shortly after he witnessed the death of his mother in a motor scooter accident in 2012, however, Henry’s renal health took a dramatic turn for the worse. “It’s almost as if my body went into shock,” he says. “Within a couple months, boom, I started swelling up again.”
That swelling was a sign that his kidneys were no longer working normally. A biopsy confirmed that he had focal segmental glomerulosclerosis (FSGS), a severe form of kidney disease. In FSGS, the kidney’s glomeruli—the microscopic filtration units that sieve excess fluid and waste products from the blood—become overly leaky; essential proteins such as albumin seep out, disrupting blood chemistry and causing fluid to leak from the blood vessels into tissues throughout the body. Henry’s condition deteriorated so rapidly that by July 2014, his doctors in Shreveport, Louisiana, decided to remove both diseased kidneys. The next month, Henry received a transplanted kidney from his identical twin, Nate, who was healthy, even though FSGS can be genetic in origin.
Within a day of the transplant, however, Henry felt like the swelling was coming back. At first, his doctors reassured him that he was doing fine. “Once they checked my urine, saw me spilling a bunch of protein again,” he says, “they realized [FSGS] was attacking the new kidney.” Three days after the surgery, Henry’s doctors conceded that the newly transplanted kidney had already become diseased. His transplant doctor, Neeraj Singh of Louisiana State University in Shreveport, says the recurrence was “one of the most dramatic cases I’ve seen.”
The sudden failure of Henry’s new kidney is a recent chapter in a long-running medical mystery, dating to when kidney transplants became routine in the 1970s. Up to 30% of transplanted kidneys fail in FSGS patients—not because of immune rejection by the body, as doctors first suspected, but because the new organ immediately begins succumbing to the same disease process that ravaged the original ones. As he struggled to cope with that devastating turn of events (and relied on dialysis to stay alive), Henry traveled to Chicago, Illinois, to consult with Jochen Reiser, a kidney disease specialist who is chairperson of internal medicine at Rush University Medical Center there.
Ever since he learned about such transplant failures 2 decades earlier, Reiser has been convinced that “there is something in the blood circulating that attacks the kidney. And we were out to catch that.” What he and colleagues claim to have “caught,” in an elegant but still unfolding story of molecular detective work over the past 10 years, is a protein known as soluble urokinase plasminogen activator receptor (suPAR). When Reiser analyzed blood samples from the Henry twins, the results aligned with the message he has been preaching with evangelical fervor for years. Nate, the healthy brother, had relatively low levels of suPAR; Nick’s were high—a driving force, Reiser believes, of his kidney failure.
Nick Henry had a kidney transplant, but his new organ quickly deteriorated, and he spends his nights on dialysis.
Kevin Beasley
Chronic kidney disease affects 14% of the U.S. population, with estimates suggesting nearly 600 million people affected worldwide. The disease steadily erodes the kidneys’ ability to filter the blood, often leading to cardiovascular disease and premature death. Kidney disease—which can directly attack the filtration process, as in FSGS, or damage the kidney’s support structure—is particularly insidious because by the time the first diagnostic signs appear, patients have irreversibly “burned off” much of their kidney function. Historically, the leading risk factors have been high blood pressure, diabetes, and African-American ancestry. (Several mutations associated with increased risk are more common in African-Americans.)
But research by Reiser and others has dramatically challenged that traditional picture of risk. If suPAR levels are low, people with the high-risk genes are no more likely to develop kidney disease than people without those gene variants, Reiser says. If suPAR levels are high, people are at greater risk of developing the disease regardless of whether they have the mutations.
Molecular studies in animals as well as a growing number of analyses of large human populations associating suPAR with kidney disease have bolstered his confidence—and convinced him the disease could be treated by suppressing suPAR. Some other researchers aren’t convinced, noting that several clinical studies found no clear association between suPAR levels and FSGS. But on both sides of the debate there is widespread fascination with suPAR, a ubiquitous, Zelig-like bystander molecule that, at elevated levels in the blood, seems to presage many health calamities, such as heart attacks, diabetes, and premature death. Whatever suPAR’s precise role in kidney disease, the molecule appears to be a potent signal broadcast by an immune system under siege. It is exquisitely sensitive to inflammation, an accelerant for many diseases.
“What is inflammation?” asks biochemist Jesper Eugen-Olsen of the University of Copenhagen, a pioneer in suPAR research. “It’s the language of cells. It’s how cells communicate with each other. When something is going wrong, the immune system is activated. It produces suPAR … and suPAR is a voice that just shouts, ‘Get on with it! Something is going on!’”
A brash style
In neither background nor appearance does Reiser conform with the public image of the director of a major metropolitan medical center. His 10th floor office at Rush sits just behind a corridor lined with photographs of hospital administrators going back to the 19th century—stern-faced, all-knowing medical patriarchs. Inside, Reiser, 46, sports a stylish striped blue suit, fashionably stubby beard, red socks, and slick dark hair. Known among colleagues as ambitious and scientifically gregarious, he has been eager to collaborate with anyone interested in exploring suPAR biology, and his brash, full-on style extends to the conspicuous display of large-format books celebrating the history of Aston Martins (he owns one) and Porsches on the coffee table in his office. Describing the speed of data collection for a paper that several years ago ended up in The New England Journal of Medicine (NEJM), he says, “It was like going from zero to 200 in no time,” adding sheepishly, “Car analogy.”
Born and raised in the small German village of Remchingen, on the eastern edge of the Black Forest, Reiser got his medical degree and Ph.D. from Heidelberg University and did an overseas residency at Albert Einstein College of Medicine in New York City. Specializing in kidney disease, he went on to conduct research at Harvard Medical School in Boston and became chief of nephrology at the University of Miami Leonard M. Miller School of Medicine in Florida before being hired by Rush in 2012.
Reiser’s arrival in the United States in 1999 coincided with renewed interest in solving the mystery of why up to 30% of FSGS patients who receive transplants see the disease recur in the new kidney. Just 3 years earlier, a group headed by Flavio Vincenti, a transplant specialist at the University of California, San Francisco (UCSF), and Virginia Savin, at the Medical College of Wisconsin in Milwaukee, announced a major clue. They reported in NEJM that they had amassed evidence for an FSGS-promoting factor in the blood of transplant recipients who’d experienced recurrences; they couldn’t isolate the exact protein, but when colleagues later injected an extract of such patients’ blood into rodents, the animals’ kidneys became permeable and spilled protein in the urine. That mysterious “permeability factor” became “the holy grail” of the field, according to Sanja Sever, a molecular biologist who studies kidney disease at Massachusetts General Hospital in Boston.
While still in Germany, Reiser had trained his research efforts on a unique renal cell called the podocyte (so named because of its amoebic, faintly footlike extensions). That choice turned out to be fortunate. The kidney has about 1 million glomeruli, and in each one, hundreds of podocytes bridge the gap between the bloodstream and the urinary system. Their footlike extensions wrap around capillaries snaking through the kidneys and, along with two other layers of tissue, form a physical mesh of cells, like a three-ply screen door, that allows only small molecules—sodium ions, potassium ions, and metabolic wastes—to pass into the urinary tract. When the podocytes become damaged, however, they essentially lose their architectural integrity. The kidney filters then become leaky, allowing larger essential proteins such as albumin to escape from the blood and pass into the urine.
It’s like a coffee filter, Sever says. “If there are holes in your filter, then you get some coffee grounds in your urine.” Podocyte damage can be reversed early in kidney disease. But, she says, “If you keep losing them, there’s a point of no return. … You are basically walking toward end-stage renal disease.”
An organ under attack
In one scenario for a severe form of kidney disease, a blood-borne molecule called soluble urokinase plasminogen activator receptor (suPAR) disrupts the organ’s filtration units, or glomeruli, which remove waste and fluid from the bloodstream. Other molecules may intensify this attack.
A dangerous immune responseAnimal models suggest immature immune cells in the bone marrow release more suPAR when an organism is under attack. The molecule, an all-purpose marker of ill health, may be directly toxic to the kidney.A HEALTHY FILTERIn each glomerulus, the footlike extensions of cells called podocytes wrap around capillaries, fitting together tightly to create narrow “slit diaphragms.” The slits form a fine mesh that allows only small molecules to escape from the bloodstream into the urine.KIDNEY DISEASEKidneyGlomerulusFunctional unit of kidneyPodocyteGlomerular basement membraneEndothelial cellsuPARsuPARMonocyteImmature myeloid cellNeutrophilPodocyte lost to urinary spaceSlit diaphragmCapillary Albumin leakageBone marrow
What causes such damage? Reiser suspected that the mysterious blood-borne factor disrupts podocytes through receptor molecules on their cell surface. He focused on one: β3-integrin, a molecule whose activation perturbs the shape and motility of cells. When he looked for the molecular key that turned the lock of the integrin receptor, he discovered that oncologists had already been working on one such protein, urokinase PAR (uPAR), a cell surface receptor that plays a role in cancer metastasis. Reiser became even more intrigued when he learned that uPAR can be cleaved from cell surfaces and circulate in the blood—at which point it becomes a soluble cousin known as suPAR. Maybe suPAR was the mysterious kidney-destroying factor.
In 2011, Reiser and colleagues reported in Nature Medicine that in cell culture, suPAR damaged human podocytes through the integrin pathway. The researchers supplemented that evidence with three mouse models showing that rodents with elevated levels of suPAR suffered kidney damage, although sometimes more slowly than in FSGS. With human clinical data suggesting that elevated suPAR levels correlated with the recurrence of FSGS in patients, a picture emerged in which the protein triggers a pathogenic process that ultimately produces holes in the coffee filter, leading to kidney disease.
The findings both electrified and polarized the nephrology community. In a commentary for Nature Medicine, Martin Pollak of Harvard Medical School, who studies the genetics of kidney disease, and nephrologist Stuart Shankland of the University of Washington in Seattle described the findings as “paradigm shifting for our understanding of the pathogenesis of FSGS.”
But some groups could not find the same clinical association between suPAR levels and recurrent disease in FSGS patients, and other groups questioned the protocol and interpretation of the animal models. And regardless of whether suPAR actually destroys the kidney, many nephrologists thought its levels were not very informative—by the time those specialists saw patients with kidney disease, suPAR levels were already high and offered no prognostic value. With Reiser claiming to have found the “holy grail” even as several groups were reporting discordant results, says one source, “People felt very emotional.”
An omen of ill-health
By that point, another key strand of the suPAR story had emerged in Europe. There, the focus was on the molecule as a potential biomarker for a range of diseases.
The first clues came from AIDS patients. In Copenhagen, Eugen-Olsen and others examined blood collected from more than 300 HIV patients in the early 1990s, before life-saving antiretroviral therapies became available. All those patients had died, but a retrospective analysis showed their suPAR levels eerily correlated with disease progression: Higher levels were associated with an earlier death. Eugen-Olsen then spent several years collaborating with a hospital in the West African nation of Guinea-Bissau, testing suPAR levels in patients suspected of being HIV-infected. Again, higher suPAR levels predicted a quicker death among the infected. Surprisingly, however, suPAR also predicted mortality in patients who didn’t have AIDS; many turned out to have tuberculosis. That finding led him to hypothesize that suPAR might be a more general biomarker for chronic inflammation.
In 2001, Eugen-Olsen founded the company ViroGates, which began to manufacture a relatively inexpensive test to measure suPAR levels in the blood. With the test in hand, he and colleagues in Copenhagen began to look at collections of blood samples banked in large-cohort prospective studies. In one called MONICA, which monitored healthy members of the Danish population for about 13 years, elevated levels of suPAR were associated with a higher risk of cardiovascular disease, type 2 diabetes, cancer, and premature death. Two other large European populations, enrolled in the Malmo Diet and Cancer Study and the Danish Inter99 Study, showed similar associations.
The findings caught the attention of researchers at Emory University School of Medicine in Atlanta who had been looking for new and better biomarkers to predict risk of adverse cardiac events in people with heart disease. The researchers had built the Emory Cardiovascular Biobank with serum from several thousand patients. “We draw blood, and we follow them for years,” says Salim Hayek, a physician and research fellow at Emory. When two of Hayek’s colleagues, Danny Eapen and Arshed Quyyumi, delved into the biobank, they found that higher suPAR levels predicted heart attacks and death, as they reported in the Journal of the American Heart Association in 2014. (At the annual meeting of the American College of Cardiology last month, Hayek presented further evidence from the Emory group, suggesting that suPAR is a better predictor of cardiac events including heart attacks and death than any other biomarker in widespread clinical use.)
Jochen Reiser has spent years amassing evidence that suPAR mounts a powerful assault on the kidney.
Rush Production Group
In addition to serving as an omen of ill health, suPAR seems to be a remarkably sensitive indicator of lifestyle insults. Studies have shown that the protein’s blood levels typically rise with obesity and with smoking. (Eugen-Olsen, an inveterate smoker, confesses that he quits when his suPAR levels rise and resumes when they subside again.) “Just looking at the data,” Hayek says, “clearly the environment is a much larger contributor to suPAR than genetics.”
With its links to multiple diseases and environmental stresses, suPAR appears to sit at the nexus of immune signaling, chronic inflammation, and tissue damage. Among the protein’s normal sources are fat cells, immune cells, and endothelial cells, which produce low baseline levels. But a team led by Reiser and David Scadden of the Harvard Stem Cell Institute showed in 2017 that in mice, immature “stemlike” cells in the bone marrow can release a pulse of suPAR when the immune system detects an attack.
Reiser believes suPAR is an ancient and unspecific way for the immune system to send urgent signals to the major organ systems when an organism faces a severe challenge from disease or the environment. Kidney damage, he says, is the long-term cost of that vital signaling mechanism. “As one example,” he says, “you get infected, you release more suPAR, you open your kidneys up, and you can dump the big molecules out into the urine. Almost like a primitive coupling of the immune system to vital organs.” In an acute infection, he says, the body urgently needs to flush out bacterial toxins, relatively big molecules. But if that inflammatory signaling becomes chronic, it takes its toll on kidney function—a trade-off that may have been acceptable earlier in human history, Reiser suggests, but is less so now. “If you live 40 years long, you can burn off the kidney this way, no problem,” he says. “If you live to be 80, 90, 100, you might burn off your kidneys too soon.”
For Reiser, the Emory cardiac biobank offered a chance to put to rest the notion that high levels of suPAR are simply a nonspecific sign of failing kidneys, not a cause. When he saw the 2014 heart risk paper from the Emory group, he had the obvious question: Could the large databank show whether suPAR levels predicted the onset of kidney disease years later? He immediately fired off an email to Hayek.
The Emory-based group quickly agreed to conduct follow-up renal examinations in more than 1300 patients who had no evidence of kidney dysfunction when they enrolled. The team found a strong link between high suPAR levels and the later development of kidney disease. For patients with the highest levels of suPAR, the risk was three times that of patients in the lowest group, and suPAR levels could predict kidney disease up to 5 years before the first symptoms appeared. “The effect was huge,” Hayek recalls.
The association was so robust, he says, that when the group first submitted its findings for publication, “the first response we got from [NEJM] was: ‘How is that association so strong? Is that real? Something is wrong with your cohort.’” But after Hayek and Reiser found the same association in a second, unrelated cohort—the Women’s Interagency HIV Study—NEJM published their findings in 2015. “In that paper,” Reiser says, “we could show that suPAR is the strongest risk factor known in healthy people for new chronic kidney disease. Even stronger than hypertension, diabetes, black race—all of these risk factors that are known to be strong. When you adjust for those, suPAR had the strongest risk.”
In the latest piece of evidence, published last summer in Nature Medicine, Reiser collaborated with researchers at the African American Study of Kidney Disease and Hypertension, based at Johns Hopkins University School of Medicine in Baltimore, Maryland, to compare the influence of suPAR and two gene mutations known to predispose African-Americans to kidney disease. A study of about 600 participants revealed that if suPAR levels remain low, “no notable differences” in kidney dysfunction were apparent between people who had the high-risk “disease genes” and people who did not. Conversely, high levels of suPAR strongly predicted kidney disease in African-Americans, regardless of whether the individual had the genetic variants.
The proof is the cure
Yet nephrologists are still divided about whether suPAR actually attacks the kidneys—and if so, how aggressively. Doubters point to the conflicting clinical results and the slow progress of kidney damage in Reiser’s mice with elevated suPAR levels. The original 2011 animal and clinical data are “as complete as you can get,” Vincenti says. “But at some point, there has to be independent duplication of that data.”
Several unresolved issues might explain the discrepancies. Different forms of suPAR can circulate in the blood, and some variants might be more pathogenic than whole suPAR. And a team led by Minnie Sarwal of UCSF, Dany Anglicheau of Necker Hospital in Paris, and Reiser has shown that in FSGS, a second blood-borne factor, an anti-CD40 autoantibody, works with suPAR to attack podocytes. “Everyone agrees it’s more complicated” than the initial findings in 2011 suggested, Reiser concedes. “But meanwhile, the data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.”
The data gets stronger and stronger that suPAR is the worst toxin you can have for the kidneys.
Jochen Reiser, Rush University Medical Center
The controversy may not be resolved to everyone’s satisfaction until a human trial indisputably shows that removing suPAR cures or slows the progression of kidney disease. Several groups are trying to develop a monoclonal antibody drug that would remove suPAR from the blood. One such group is Trisaq, a company Reiser and Sever founded in 2011. Vincenti said his group also has developed monoclonal antibodies to suPAR for clinical testing. “I was excited to try it in patients,” he says. “But we could not demonstrate, at least in our samples, that suPAR was a biomarker for either FSGS or recurrent FSGS. [That’s] held it back.”
The first human proof may come not from a drug, but from a medical device. Miltenyi Biotec, a company in Bergisch Gladbach, Germany, makes apheresis devices, which remove substances from plasma, and it is developing a technology that would selectively scrub suPAR out of patients’ blood. “The key question,” notes CEO Stefan Miltenyi, “is if suPAR is the cause [of] renal diseases or just a bystander molecule.” Miltenyi hopes to launch a clinical trial in 2019.
For FSGS patients such as Henry, who relies on 8-hour overnight sessions of dialysis to stay alive, a breakthrough therapy can’t come soon enough. But suPAR is already beginning to influence clinical decisions. Singh, Henry’s transplant physician, has used suPAR levels to manage the care of several kidney patients. And since 2013, every patient arriving at the emergency department at Copenhagen University Hospital Hvidovre has undergone suPAR testing to help physicians make triage and discharge decisions.
Reiser often likens suPAR to cholesterol—a key marker and disease-associated molecule that can be monitored and, perhaps, ultimately controlled. But the main lesson of suPAR, he believes, is cautionary in an age of genomics and personalized medicine. Although a huge amount of attention (and government coin) has been devoted to identifying genes associated with disease, the environment can sometimes trump them. “I think that the gene adds to the risk profile—it’s part of the picture,” he concedes. “But the environment is a way-underestimated modifier that becomes way more important, quite frankly, than the underlying gene event. And this is … a beautiful illustration of exactly that principle.”
0 notes