#and if they come back without a diagnosis i have to get a colonoscopy and endoscopy
Explore tagged Tumblr posts
Text
I HATE EBV!!!!!!!!!
#i want to cry straight up i played 2 rounds of beat saber with my brother like three days ago#and my leg muscles still hurt so bad even when im laying down not using them#my doctor told me not to do exercise that isn't mild and low impact because my mitochondria are damaged by my viral infection#and my cells can't power themselves efficiently right now#idk man i thought beat saber would be fine :( it WAS fine while i was doing it but a couple hours later it hurt badly to walk#i haven't dealt much with muscle pain before this. before the EBV reactivation i had back pain and joint pain and poor CV health#but i never felt like my muscles were just dissolving themselves like this. i feel weak and helpless.#also i'm trying to get a diagnosis for my GI issues right now and the lab lost 4 out of the 6 vials of shit i gave them for a stool sample#so i have to do that again. for the third time in like two weeks.#and if they come back without a diagnosis i have to get a colonoscopy and endoscopy#my health is just a wreck right now and i feel so useless spending 20 hours a day in bed most days#but what the hell else can i do. i just gotta wear my brave face and try to preserve my dignity#i want to stop being nauseous and in pain and so so so exhausted all the time. im so tired.
1 note
·
View note
Text
Gonna dump everything from my appointment yesterday here so I can remember it.
Rheum wanted GI to switch me to Rinvoq after positive RA diagnosis in November. GI doesn’t want to switch me off Stelara because it seems to be working, even though the last couple months have been a little rough. We looked at my injection schedule against my notes on when I started getting sick again each month and determined that I am metabolizing Stelara quickly and would benefit from moving my doses to every six weeks as opposed to eight weeks. So we’re going to see if insurance will allow that. Basically, I’ve already been through two of the strongest biologics for Crohn’s, and the doctor doesn’t want to prematurely take me off Stelara until we’ve exhausted all my options with it bc once I’m off it I will build up antibodies. He would much rather see me add in methotrexate, hydroxychloriquine or plaquinel rather than disrupt something that is actually working for me. Which I agree with - and I actually had huge reservations about Rinvoq. I was willing to try it, but I would have been disappointed had it come to that bc I really don’t want a daily oral medication and the side effects - mainly severe acne and sun/heat sensitivity- made me nervous.
Honesty, I’m relived we aren’t giving up on Stelara. I do think I came off the Humira too quickly, even though I think ultimately I would have had to do it anyway regardless. The fact that I had injection site reactions every time wasn’t good, even without factoring the major joint pain. But I was at the point where I would do anything to avoid that shoulder pain, so I didn’t hesitate to stop.
So yeah. Stelara every six weeks if insurance will approve it. Need to get back to rheum to see if I can get an RX over the phone for the RA or if I will have to wait until my next appointment in June. GI also told me that if a joint locks up again I can go to the ER for injections to help it unlock and pain killers, and that an ER visit would likely help me get into rheumatology sooner. They’re scheduling me for another colonoscopy, and honestly I am stoked, lol. Post colonoscopy is the only time I’ve ever felt truly “cleared out” and I am a very data driven person so I will be happy to have something to compare the colonoscopy from 2022 to. I had labs yesterday and they all came back within the normal range. Have to take in a stool sample this week. Honestly, things went as well as they could have, I think.
7 notes
·
View notes
Text
Mild objections and some clarifying points
Hi Em. Long time follower, first time caller here. Its okay if you don’t want to post this, but I just wanted to clarify some thoughts I had about the most recent post about doctors and the medical system (in the U.S., I assume) from the view point of a doctor (if you were interested). If not, feel free to scrap this. I am sorry it got so long.
1. Doctors should be put through an extremely extensive relicensing process every 10 years
Agreed. That was the board exams are for. I am not certain why doctors without board certification are allowed to practice at all to be honest, but it is easy enough to find out if your doctor has re-upped their credentials or not. We usually have additional initials after the MD which stand for “Fellow of your-specialty-here.” If not, there are plenty of ways to check online. Certificationmatters.org is a decent starting point.
In addition to recertification board exams, most healthcare employers in the U.S. require us to have a certain number of CME (continued medical education) credits that are obtained through conferences and other educational events/activities meant to keep us up to date. If you don’t have these, you likely won’t be hired. I think the only people who get away without these might be some doctors doing solo private practices. At the very least, if you work for a hospital, hospital affiliated practice, or university, there is no way to get hired unless you do a certain amount each year.
2. Doctors should have their knowledge scrutinized against current medical research…
Agreed. To the maximum extent possible, we doctors should be practicing evidence based medicine. It drives me nuts when some of my older colleagues just say, “I don’t believe in X.” That shouldn’t be a thing. It’s like thinking the sun will go away just because you decide it doesn’t exist.
3. …and be de-barred at even the tiniest discrepancy
This wouldn’t really be possible, not really. Medicine has come a long way, even in the last 50 years, but we still don’t have all the answers. As much as medicine is touted as a science, the reality is much more wishy washy. The truth of the matter is that we don’t 100% understand how the body, mind, or disease works. Hell, we still don’t even know how some of the most commonly used medications work (example: Tylenol). Some things we understand better than others. Some we don’t understand at all and are still basically guessing. One of the most poignant pieces of advice one of my mentors gave me in medical school is a reminder that about half of what I know about medicine now will be proven as fallacy in 10 years.
So yes, I would love to stick and practice only what has been studied and proven. But the reality is there is so much that has not been studies and human bodies are so diverse, I am often flung into managing people and conditions for where there is no evidence based treatment or testing or algorithm for me to fall back on. I don’t get the option of cherry picking my patients and I don’t want that option. If someone is hurting and coming to me for help, I am going to dang well try to help them, to whatever ability I can.
To that point, when a patient comes to see me, sometime all I have is a really good hypothesis. Most of the time, it is a pretty good hypothesis based on my own exam and the patient’s description of what they have noticed, but it is still a guess and I could still be wrong. It is incredibly hard to prove or disprove a diagnosis definitively. Frankly, a lot of the things required to “definitively prove” a diagnosis are painful and invasive, if they exist at all, and are unlikely to change management (treatments overlap). Why put my otherwise healthy 30 year old patient through a colonoscopy and risk an intestinal puncture (which is a horrifying and incredibly deadly) to prove that their constipation isn’t a result of cancer in the absence of any other symptoms indicating cancer (weight loss, blood in the stool, fever, chills, etc.)? Decisions regarding treatment or testing outside the scope of what has been studied is a combination of medical gestalt (which takes years to develop, hence why we are one of the few professions left with an apprenticeship system) and weighing benefits versus risks.
When I don’t know the straight answer, I am upfront about this with my patients. I explain what I think it is and what I think we should do, but I am also clear that there is not straight right or wrong option. I often leave it up to the patient to make the final decision. I hate how some doctors make patient’s feel cornered like they don’t have a choice or option. It is one of the chief reasons I myself hate being a patient. Medical schools are trying to push away some of that paternalistic training, but it is still a work in progress.
4. Too many people are told their problems are nothing and come back in a year or more
Agreed, this is a problem. The medical system in the U.S. is not set up to facilitate appropriate follow up correctly. It can take my patient months to get an appointment with me and it frustrates me so much, because a lot of these things need to be followed up sooner. I would not want that 30 year old patient from my earlier example to follow up in a year, because if after a month of treatment, their constipation hasn’t gone away that necessitates further evaluation. But visits are stupidly expensive even with insurance and there are so many patients that finding a slot is a nightmare. As of now, I am booked out for 3 months. The dermatologists in my city are booked out for 8 months. The gastroenterologists (the ones who do colonoscopies such as for my poor constipated patient) are booked out until mid 2023.
I would love it if I had the ability to call everyone of my patients back after an appointment to follow up but there is no time. I work close to 70-80 hours a week between seeing patients, paperwork, and answering virtual patient messages. If I go home and do more patient work, I will crumble. I would burn out and be utterly useless to anyone in that state. I need to sleep and eat and play and be well if I am to take care of anyone. Nurses and auxiliary providers help with some of this burden, but frankly there just isn’t enough of us to go around.
5. Doctors are just like “lol everyone makes mistakes”
No. Just no. I don’t like using absolutes, but I have never met a physician who was blasé about a patient dying, regardless of how they may appeared to the patient family. I remember the name of every patient who has died in my hands. I remember the look on their family’s faces when I had to tell them their loved one passed or is going to pass. I have grieved for every single one and pored over the events that led to it over and over in my mind. Even when no mistakes were made, sometimes patients still die and I have never walked away from that unaffected.
That said, I can’t always show or process that in front of a patient or their family. I don’t get the luxury of asking for time off. I still have to turn around and take care of the other patients under my care. Sometimes that means in the moment, I have to lock down my emotions and reactions and act as it if didn’t bother me until later. It’s not a great thing to do and likely actively damaging to the psyche, but I am not given any other choices - we are almost always short staffed and asking for time off to grieve isn’t usually an option (other than a nominal one). Most hospitals have gotten better about doing debriefings and root cause analysis after a catastrophic event, but they are still business and a lot of this is oriented towards legal liability things.
6. Quite frankly, the problem is bad doctors. A person can have all the right information and fill out a test perfectly but that doesn’t mean shit if they aren’t willing to apply that information in practice.
Preach, sibling of unknown gender. Fun fact: A patient recently informed me that the gender neutral term for child of you sibling is called a “nibling” - isn’t that adorable?
7. But there would be so many fewer mistakes if more doctors would actually fucking listen to their patients. What we truly need is more doctors to acknowledge that all of their expert medical knowledge doesn’t change the fact that the patient is the expert on their own body.
I fully believe in this. Patient are experts of their own body and when they something is wrong, something is wrong. Of course, they may not always be accurate about what in specific is wrong, which is where we come in to help them figure it out. For example, I had a patient last week who came in because she though she was having kidney trouble. She then proceeded to point to her left thigh and tell me this was where her “kidney” was and that it was hurting. I explained the kidney does not exist there in the human body and we (the patient and I) are still working together on figuring out what is going on in her leg.
8. We also very much fucking need insurance companies to stop practicing medicine without a license.
OH MY GOD - THIS! Aetna recently purchased or took over some smaller insurance companies and has been suddenly refusing to pay for any of the (very cheap to manufacture, by the way) medications my patients have been stably on for years! I am ready to strangle the bastards on the board or whoever makes their stupid decisions (those terrible spawn of Wall Street Bankers and Orcs).
~~~~~~
In reference to this post
I’m really glad you sent this in!! I’m always happy to hear first-hand perspectives. And thank you for clarifying all the points that I didn’t in my original comment - you’ve explained it all way better than I could.
25 notes
·
View notes
Text
long, long health update - tw in tags please read them
I am going to speak very frankly about suicidal ideation; please don't read further if this is triggering for you ;3; but please know that I love you I had my follow-up appt with my neuropsych on monday to go over my results and whatnot. it was virtual, and I was in the middle of a head episode and I told her I wasn't doing well, but within about 5-10 minutes, she was saying I should probably go to the ER lkajflaj I guess it looked pretty bad lmao anyway I told her all the reasons I couldn't. medical trauma, being dismissed b/c I have doctors who manage my headaches, and I know it's not life-threatening even if it is 10/10 agonizing, so why are you here. they're so dismissive. she said that they have medication to possibly help break the cycle of constant migraines but I've been treated with those before and they didn't do shit migraines are secondary to iih. it's the iih that needs to be fixed ._. she said I still deserved to not suffer and that the ER is very strict about keeping covid patients away from other patients and I didn't have the heart to tell her they intubated a covid patient 10-15 feet away from me last time I was in an ER 😭 anyway so the results. she said she wasn't worried about anything going on that was concerning or indicating something wrong in my brain. I DID score quite a bit lower for someone my age on information processing (which is exactly what I said I was struggling with to my two neuros who were both like ehhh) and some issues with memory but they weren't super specific and so it could be something neurological, could be my migraines and constant agony lmao, could be my Emotional State. could be all of them at once, I suppose ;) she went into more detail about some of these things but it was the two questionnaires I filled out that were HNNN. so once all the data is entered from like 300 questions it shows a good look into my personality and perceptions and all that and it makes a cool little graph (OR SO I THOUGHT). the kind that looks like mountain peaks. so she points at the one that is waaay higher than the rest and nearly touching the top of the box and she's like 'do you see this one' me: yeah 😬 her: this is your feelings and ideations about suicide me: 😬 😩 😬 her: when I see a score this high, I stop what I'm doing and I call the police to have them escort you to a hospital me: 😬😬😬😬😬 her: but I didn't do that. because when we spoke in office you told me you felt this way and why you don't do it. you told me it's something you've lived with for a long time and the pain you are suffering is what makes it so bad. and I trust you me: 😭😭😭 okay her: do you see this line down here? this is people who have suicidal ideation recorded on this test. you scored 98% higher on suicidal ideation compared to people reporting suicidal ideation HNNNNNN. she said it probably wasn't surprising to me and asked me if I was safe again and all that. I assured her I was and said in my previous appointment; I've had suicidal thoughts since I was like 12? maybe earlier. there have been very few times in my life not surrounded by abuse and trauma so I'm never really free of it. I've had four traumatic incidents causing increasingly horrible episodes of ptsd in nine years. all through my 20s. still here woo, lol and she said she knew that and had a patient not long after my first appointment who had similar circumstances in their life. and they told her it's almost a comfort having it. cause I was saying it's in the back of my mind at all times and I won't do it, but yeah, it's always there. anyway she said they said the same thing; it's always there, always in the background as 'hey I'm an option!' even though we aren't going to harm ourselves. it's a comfort knowing there is an option even if we plan on never using it? idk it just spoke to me and I felt it in my soul we talked about some emotional stuff after and I cried and it was a thing. it felt really good to speak to a psychologist who, just as she was in the first appointment, seemed genuinely concerned and wanted to help
me. I told her I was ready for therapy and she said she'd already looked for therapists for me lkasjdlkja and gave me a group that I emailed yesterday. I don't think they'll take my insurance but she said to message her through the portal if they don't and she'll try to find someone who does I don't remember if I mentioned it, but since she knew about the head shit before I met her, she dimmed her office lights without asking if I needed it and like as soon as we started the virtual visit, she leaped up and dimmed them and said she should've thought about it before the appt 😭 (I keep my brightness really low on my computer and use the warming feature 24/7 on comp and phone and my apt is really dimmed but it still helped a lot when she did it) she kept saying 'you did nothing wrong. it was the choice of others to do what they did. you don't deserve to carry their choices. you deserve to be able to hand it back to them. you don't deserve to be in pain. you did nothing wrong. you deserve to be free of what they did and you deserve to not suffer in such physical pain' I'm so wary of doctors but I really like her and I feel fortunate to have been referred to her ;3; speaking for a long time and especially emotionally is hard for me, so I might try to do two sessions a month once I find a therapist and see if I'm ok with that. trying to keep everything virtual while delta is out there I read her report and her official diagnosis is uhh really strong for major depressive disorder, severe. and severe ptsd with disassociative symptoms so!!! I claimed both of those on my disability application and the person handling my claim told me when I had this appt to call and let her know because she wanted the info. I signed a release the day I was there when I told my neuropsych that cause MH stuff is different than other medical records. she said she faxed it to the woman handling my disability application but I was gonna call her and ask if she received it and also tell her I have a new neuro so she will probably request his stuff too I called today and her voicemail box is full so lol try again later today's been awful. last night was horrible. got a bill for over $800 from my colonoscopy/endoscopy even though I asked numerous times if insurance was covering it and was told yep, every penny. so I was on the phone with insurance and the surgery center for 45 minutes. insurance seemed confused af but the agent I spoke with got some help from people who handle this stuff I guess finally she told me not to pay it, they're going to send them a letter to get it sorted (idk if this means I won't have to pay it at all or if they're going to try to make it that way. but I think govt insurance, which is what I have, works differently. like doctors kinda have to follow what they say vs. the other way around) and not worry about it for the next 30 days. I'm still gonna worry about it lmao they used a nice scare tactic on the bill that this was the 'LAST AND FINAL NOTICE' despite the fact they've never sent me anything else. my mom and the insurance agent said nah that's just what they do to scare people into paying fuckin love america <3 land of the free. the american dream! greatest country on earth 💜🖕💜 I just don't want it to go to collections and have to fight credit bureaus to get it off my credit so it's not destroyed |: anyway my head hit like 10/10 bad while I was on the phone cause of the talking a lot and trying to PROCESS INFORMATION and stress and also the fucking hold music, which I have to hear in some way b/c I gotta know when they're back on the line hnnnnn bad day. it's 1pm and bad, bad, bad day. bad month all around. I want this shit to stop anyway. I'm sorry about the suicidal ideation talk, but it's important to talk about that stuff. it can get severe but it can also get better. it does, eventually, even if it comes and goes. it always does get better I'm sorry, I also really needed to get this down somewhere. feel like I'm going to explode emotionally AND physically and I need to talk about it. hopefully
soon I'll have a therapist to talk to so I can get a lot of this stuff worked on. got my whole life to chat about so it'll probably take a long time but I'm willing to let it lmao therapy doesn't usually work for me anymore but idk I've had a lot of shit happen in less than two years so maybe it will this time I'm trying! I really am trying if you read this rambling monster, thank you. love you all and please stay safe
#vtforpedro personal#tw suicidal thoughts#tw suicidal ideation#tw suicide#tw mental health#tw depression#tw anxiety#tw mental illness#personal#medical#also she is obligated by law to report suicide risks and right now that's to the police so I can't blame her for that#we desperately need crisis intervention rather than fucking asshole cops but that's just what it is right now
14 notes
·
View notes
Text
Stress-based sickness, psychosomatic disorders, and the F word. Fibromyalgia.
Read up or listen up @t-mfrs.com (podcast available wherever you stream.)
Waking up, like I didn’t sleep for weeks. Falling asleep after five minutes on my feet. A pounding head. That sense of dread. Sticky sharp pains through in my shoulders and neck. Brain short on energy, missing a few cards from the deck. Waves of nausea and stomach cramps. Chills and sweats, depending on the body amps. Swollen lymph nodes. Muscle weakness poorly bodes. Insatiable hunger but nothing sounds edible - shit, now desire to throw up is incredible. Eyes shriveling, dry, back into my skull. The aches in my legs, pulsing and dull. Foggy thoughts. Racing heart. When will this end, why did this start?
Did I finally catch the ‘rona? Or am I just past my limit for being stressed out again? Well, I just moved, so this time I know that the answer is very likely… stressed.
So who wants to talk about getting sick? Yeah, among this group, the answer might be surprising. A lot of us do.
Why? Not because we love bitching and complaining when we feel less than ideal - spoilers, that’s every day, there’s really nothing left to say about the raging shit storms inside of us after a few years of it. We’re tired of hearing about it, too… just like we’re tired of living it, feeling it, and fearing it.
No, for us, it’s because it feels like there’s always a surprising ailment right around the corner when we least expect it. One that seemingly has no logical basis or reasonable solution. One that no one else understands. One that feels like it’s born of mental illness, somehow, while being very physically present. One that we don’t even bother bringing to doctors anymore, because no one needs to be shamed and shoved out the door again by their flippant disinterest in anything we say after the words, “Yes, I have anxiety.”
Yep. If you haven’t tried to mingle mental health with western medicine before, let me give you a quick disclaimer: unless you’re missing an arm, don’t bother. In my experience, the only thing you’ll get is an eye roll, possibly a prescription bandaid that somehow makes you feel worse, and a bored recommendation to see a psychiatrist - even if you already do.
All of this, of course, has the effect of only making you feel more upset. First, mentally, as you ruminate over the disrespect of essentially being called a liar just because the doctor doesn’t have enough training. Then, physically, as your increased stress and systemic arousal pushes your body into a new level of overdrive.
Oh, was it a mindfuck just to make the doctor appointment, get yourself there, and deal with the social anxiety of a waiting room for 30-120 minutes? I bet it felt great for someone to then invalidate your health concerns, recommend you calm down, and send you out the door without even looking you in the eye. Feeling more upset, now on a highly emotional basis? Enjoy the shame, hypertension, and lost sleep, as if you needed any more of that.
Today, I want to talk about the stress-central area of my health that hasn’t been completely figured out… and the label that I - embarrassingly - just recently learned is highly applicable to my physical condition.
But also, the outrage that I feel over said label, because, well, it explains nothing. In fact, if anything, it probably does all of us a huge disservice after we’re granted this diagnosis by pushing us into the express lane for being written off. It also separates two issues that are poorly explained, rather than combining them into one full picture that might actually yield answers. Oh, and should I mention that I think this is a larger problem of gender bias in the healthcare system? Yeah, why the fuck not. Might as well air all my grievances as a nice lead-in to another upcoming episode; is mental illness diagnosis skewed by gender?
I don’t want to let my pounding head and aching shoulders deter me too much, so let’s just get started.
History of ailments
I’ve talked about this before, but to briefly cover how fucked up this body is… let’s take a trip back to 2013 when my system failed me out of the blue. And by “out of the blue,” I mean that I had chronically overworked myself running on anxiety, obligation, and starvation for 2 years, leading to physiological revolt.
So, looking back, “duh.”
But at the time? This was all-new. It was crisis-inducing and beyond comprehension that I went from a perfectly healthy, physically resilient, surprisingly strong and low maintenance specimen to a chronically pained, systemically ill, digestively impaired, and constantly exhausted sack of wallowing self-hated.
After a lifetime of zero health concerns, I found myself bedridden and obsessed with every weird thing my body was doing to me. Which, as you’ve probably guessed, came hand in hand with the new weird things my brain was doing to me.
After a lifetime of zero health concerns, I found myself bedridden and obsessed with every weird thing my body was doing to me. Which, as you’ve probably guessed, came hand in hand with the new weird things my brain was doing to me.
You’ve probably heard the “What IS CPTSD?” episode by now, so I’m guessing you’re not a stranger to the details about the common emergence of complex trauma symptoms. Yes, that’s based on a lot of research, but it’s also a throwback to my own experience. I was a long time depression and anxiety lurker, first time complex trauma contributor around age 23, when my brain was suddenly uprooted by a series of new social and therapy-based traumas.
My depression became debilitating negative self-regard and stronger suicidal ideation. Suddenly, my social anxiety became agoraphobia. My new health issues became topics of obsessive and intrusive thoughts… you know, when I wasn’t ruminating about my role in every trauma, my worthlessness as a human, and my recently-unsettled childhood memories. My early twenties were a great time.
And with all the mental strain, came the unresolvable insomnia. Which fed right into the health problems. Which circled back to spark more mental duress. Health anxiety is not a fun way to live.
So, to call my illnesses psychosomatic is completely appropriate. But, also, completely insulting when a western medicine practitioner utters the phrase as if it was a turd slowly coming out the wrong end. And that’s exactly what happened every time I tried to seek help.
So, to call my illnesses psychosomatic is completely appropriate. But, also, completely insulting when a western medicine practitioner utters the phrase as if it was a turd slowly coming out the wrong end. And that’s exactly what happened every time I tried to seek help.
To be clear - back in the day I had some very easily detectable physical problems. I understand that doctors have a difficult job when it comes to interpreting the immeasurable inner experiences that their patients detail, but that wasn’t entirely the case here. When your body stops digesting food, well, there’s some evidence to prove that it’s a fact. When a 96oz medical grade laxative used for colonoscopy prep results in zero percent colon cleanse… uh… somebody isn’t doing their duty (pun intended). And boy, did my digestive system just decide that it was DONE doing its only job.
Everything I ate seemed to spark unpleasant physical responses, but moving materials through my guts and extracting nutrients wasn’t one of them. After months of garbage disposal failure, I was basically a walking sewer mixed with a compost pile. I found myself chronically starving, exhausted, puffy, distended, intestinally inflamed, and generally sickly. Your body doesn’t fare so well when it has no sustenance, it turns out.
At the same time, or maybe slightly predating my digestive protests, I started getting ill in weird ways. Things I had never experienced before started popping up, like chronic respiratory tract infections, sinus infections, and gum infections. I was having what seemed like allergic responses to something in my inner or outer environment. I was often covered in hives or my face and stomach were inflating like balloons for no apparent reason. I had near-constant pain in my continually-locked shoulders and neck. My actual skin, itself, hurt, as if I was being stretched to the brink of bursting. My lifelong migraines transformed into something new - disorienting tension migraines that came with horrifying loss-of-vision auras and feverish shakes.
Generally speaking, I was so tired all the time that I could barely get out of bed for more than a few moments before retreating back to my safe place to feel like garbage. My limbs felt like someone had tied weights to them and extracted several major muscle groups. I struggled even showering or washing my face, because both required holding my arms up higher than I was capable of enacting. I was so deliriously tired that I couldn’t see straight, think, or complete basic tasks.
Generally speaking, I was so tired all the time that I could barely get out of bed for more than a few moments before retreating back to my safe place to feel like garbage. My limbs felt like someone had tied weights to them and extracted several major muscle groups. I struggled even showering or washing my face, because both required holding my arms up higher than I was capable of enacting. I was so deliriously tired that I couldn’t see straight, think, or complete basic tasks.
On top of giving up my impressive life trajectory in the aftermath of the physical breakdown - because I was too fucking exhausted to consider the next steps I needed to take for grad school - this is also where I’ve previously mentioned my drive-aphobia coming into play. When you can’t count on your own faculties, you definitely don’t want to be behind the wheel. And suddenly, life gets very restricted.
I gave up my… anything life trajectory at that point. I went from a wildly social and focused student with a fantastic sense of humor about life and stronghold of self-determination to… Hiding indoors. Keeping isolated. Obsessing over my health. Googling the most embarrassing things late at night. Having no answers. Feeling like a crazy person. Hating myself. Fearing that this was the end. Assuming that my future was over. Guilting myself for fucking up my past. Replaying my tragic story of a rapid flight and a crash, after everything I had fought so hard to accomplish. Giving up.
This is riiiiight about where I pull most of my inspiration for talking about living in perpetual “trauma states” from. Being consistently triggered, out of control, and terrified. Having no answers and no one to even ask. Watching mental illness take over my world without the slightest clue of what was happening. And, oh, the perpetual torment of unpredictable physical breakdowns.
Everyday a new surprise. Every moment the opportunity for a shocking change in vitality. Every night a battle of my brain versus my chronic pains versus sleep.
And so it persisted, throughout 2013 and into several later years… despite the fact that I actually came up with an answer for myself that vastly improved a good part of the sickness struggle... but definitely didn’t fix it all.
Finding AN answer
I’m sure I’ve already mentioned this, too… but eventually I found some respite in my health struggles through no help from modern medicine. In fact, I helped myself thanks to familial clues when I decided to exclusion-diet my way into an answer. My grandpa had celiac’s disease long before it was trendy and I decided gluten was a logical place to start. And what do you know? That helped about 60% of my ailments.
So began years of obsessing over figuring out the gluten free life. Which, contrary to popular opinion, fucking sucks. I get that it became a trendy idea at exactly the wrong point in my life, but goddamnit, I hate the question, "Are you ACTUALLY gluten free, or is it by choice?" It is not a dietary walk in the park when essentially every item is contaminated with some form or another of secret sauce and your body is going to flip out at the slightest dusting.
I remember being so distraught over having these drastic dietary considerations to figure out on my own that I would spontaneously break down into tears in all sorts of places - the fridge, the grocery store, restaurants, social contexts when people kindly asked, “how about you choose where to eat this time.” I can’t choose! I can’t eat anything! I would privately bawl to myself. What a fun time that was.
But that was not nearly the end of it.
It turned out, yes, entirely cutting the glutens helped immensely. I also realized that sugar was not my friend. In fact, processed anything was not going to have a great outcome. But then… there was this other weird pattern that I started noticing in my life… sometimes I was pretty healthy and (relatively speaking) happy with the way things were going off-wheat. But sometimes I was just as sickly and digestively screwed when I definitely hadn’t consumed anything questionable. As if other tried and true components of my diet randomly became gluten analogs that upset me just as much.
Plus, there were some ailments that just never seemed to go away. The insomnia was a persistent problem that stretched back to being about 5 years old, but got more severe with time. The aches and pains in my neck and shoulders only worsened, no matter how many tennis balls I rolled on, yoga classes I attended, or muscle relaxers I popped. The exhaustion came and went with connections to my mental health and diet, but not directly related to bready food items. The brain fog didn’t clear up when I had a strictly regimented diet. The tension migraines never fully returned from where they came.
Plus, there were some ailments that just never seemed to go away. The insomnia was a persistent problem that stretched back to being about 5 years old, but got more severe with time. The aches and pains in my neck and shoulders only worsened, no matter how many tennis balls I rolled on, yoga classes I attended, or muscle relaxers I popped. The exhaustion came and went with connections to my mental health and diet, but not directly related to bready food items. The brain fog didn’t clear up when I had a strictly regimented diet. The tension migraines never fully returned from where they came.
I was still finding myself bedridden and ready to give up on the whole idea of living on a semi-regular basis. Sometimes it was every two weeks, sometimes once a month, sometimes a few months apart. But I never knew why, how long it would last, or how to control the system-wide failures.
And if you want to know how western medicine helped me with any of these continued challenges… it didn’t. I tried to get answers for years before I finally gave up. Every doctor turned me away. Every specialist was critically uninterested. Even the Mayo Clinic neglected to listen to what I said or utilize applicable resources, after I was so sure they could solve the medical mystery of my life.
So. I stopped trying at a certain point. I resolved myself to being health anxious and perpetually confused by myself. I realized that I would never know what any day was going to bring, because my discomforts and continued sicknesses seemed to come and go with the tides.
Eventually, after years of this bullshit, it got a bit better. I buckled down with - you guessed it - strict routines designed to circumvent some of the challenges.
Eventually, after years of this bullshit, it got a bit better. I buckled down with - you guessed it - strict routines designed to circumvent some of the challenges.
I realized that my diet needed to be incredibly tight, and by that, I mean “boring.” Beyond gluten, I cut out basically everything sugary, carby, and processed. I noticed that without a certain variety of physical exercise on a regimented basis, everything started slipping. I prioritized finding ways to get to sleep at night, even if it meant being rigid and assessed as “dramatic” by less slumber-impaired humans. I gave up any activities that caused neck and shoulder strain, and tried to be better about things like stretching. I also noticed that dealing with my emotions was a gateway to pain and discomfort relief, which was an uphill battle all it’s own. And, you know, eventually I learned about this Complex Trauma thing that explained a HUGE part of early to mid twenties, including a majority of the physical ailments.
But, although I began to live like an above-averagely healthy human again… I’ve still always had a few mysteries about my health.
Sure, over the course of many years I’ve figured out how to live with a semi-predictable body after long periods of never knowing what tomorrow would bring. But, unfortunately, there are still times when my system throws me a curveball. During those unanticipated spans of health failure, I’m left ruminating on a question or three that haven’t ever been answered consistently.
One of the most common inquiries is coming at you next.
Stress or sick?
So, even after all my life changes and careful modifications. All my sacrifices and seemingly over-the-top regimes. I’ve still had an ongoing health obsession that pops up from time to time when my shit starts to go downhill.
The incrementally-observed question that runs through my head on repeat… “Wait, am I communicably sick, or am I just fucking stressed out again?”
The incrementally-observed question that runs through my head on repeat… “Wait, am I communicably sick, or am I just fucking stressed out again?”
I realized a while back - maybe in my mid-late twenties - that holy hell, I sure felt like I was coming down with the flu more often than it was logical. The thing was, my symptoms only ever progressed to the point of feeling like I was still actively fighting off the sickness as it took hold. I would get the temperature dysregulation, the headache, the muscle pain, the foggy feeling, and oh boy, the exhaustion - that generally serve as your first signs of contagious trouble.
I would be too deliriously tired to get up and do anything. If I made myself go to work, it felt like wading through a dream. Half present, half falling asleep at my desk. My body felt like it weighed a thousand pounds. Even my head was too heavy for my neck to manage the task.
Beyond the energy void, I would genuinely start to experience pre-illness complaints, like swollen lymph nodes, congestion, and the aforementioned shivers and shakes. I would find myself incredibly hungry, as though my immune system was ramping up for a fight. I would get weak, like all my electrolytes were purged from my body. I would characterize the experience as feeling “generally under the weather” in preparation for something much larger slamming into town.
Beyond the energy void, I would genuinely start to experience pre-illness complaints, like swollen lymph nodes, congestion, and the aforementioned shivers and shakes. I would find myself incredibly hungry, as though my immune system was ramping up for a fight. I would get incredibly weak, like all my electrolytes were purged from my body. I would characterize the experience as feeling “generally under the weather” in preparation for something much larger slamming into town.
And I would respond in kind. I would retreat to bed, Nyquil and vitamin C showering over me on frequent intervals, gearing up for the systemic war of a lifetime. I would drift in and out of sleep for a day or two, fending off the weird muscle aches and sweat sessions that come with an emerging fever. Interestingly, many of my old food reactivities would rear up during this period. I would get my neti pot and vomit-bags ready for action.
And then… nothing else would happen. Assuming I chilled out and retreated to a state of forfeit when I actually treated myself with kindness and care, everything would work out. After 1-5 days of being back in my bedridden state, determined that significant contagious sickness was headed my way, it would seem to just disappear overnight. Or, clear up by about 70% overnight, to be more realistic.
It took several rounds of this pattern - I couldn’t tell you how many - before I finally realized… heyyo, my body shuts the fuck down when I’m stressed out. Every time I experienced one of these sudden falls from health, it followed (or ran in tandem with) a period of significant stress, anxiety, and/or depression. And if I let myself relax for a week, it would all be okay. If I tried to push through it because ObLiGaTiOnS, I was signing myself up for a prolonged and far more serious health failure. It happened too many times; I knew it wasn’t a coincidence. Like I had postulated earlier in my adulthood - my health seemed to be drastically affected by my mental state. Particularly, my interpretations of stress, obligations, and fears.
And I can tell you, my health anxiety quieted down for a while in the aftermath of the acceptance. Call it immersion therapy. When you’ve experienced the same event over and over again, but A never leads to B, and C-alming your shit makes condition A disappear back into the ethers... well, eventually you take it for what it is and just stop panicking so much. I think I got tired of preoccupying myself with the whole dumpster fire at some point and preferred to extinguish the flames by letting them run their course.
This is where I’ve lived for the past many years now. Realizing that if I push myself too hard mentally or physically, or if I let too many stress signals infiltrate my brain… I’m about to get fucked up. My health will slip quickly. I will be reactive to essentially every food on this planet. My body will be puffy, inflamed, and painful. Not to mention, so goddamn tired all the time. But that’s it. It won’t last forever. I’m not going to die. Telling myself the opposite makes it all last a lot longer. Don’t pile stress about your stress-induced sickness onto your existing stress, and you'll be better soon.
This is where I’ve lived for the past many years now. Realizing that if I push myself too hard mentally or physically, or if I let too many stress signals infiltrate my brain… I’m about to get fucked up. My health will slip quickly. I will be reactive to essentially every food on this planet. My body will be puffy, inflamed, and painful. Not to mention, so goddamn tired all the time. But that’s it. It won’t last forever. I’m not going to die. Telling myself the opposite makes it all last a lot longer. Don’t pile stress about your stress-induced sickness onto your existing stress, and you'll be better soon.
And yet, when it’s happening, I also never know for a fact that my stress-based illness is definitely what’s going on. The result is getting trapped in a “will I or won’t I” obsessive spiral of anticipating the worst while reassuring myself that it might be nothing at all. There’s a lot of internal and external conversation about it, as people want to know if you’re sick and you want to be able to warn them that you feel like death… but also have to throw in the caveat, “Iunno, you have to realize that this happens to me all the time and it’s usually nothing, though.”
Of course, this creates the opportunity for my brain to 1) tell me I’m probably fine, quit complaining, pussy, and 2) compare myself to everyone else on the planet, who doesn’t crumble when their brain interprets times are hard. Because, of course, I have to make myself feel mentally ridiculous for feeling physically horrible. Other people are always happy to help in this regard, too. "You sure get sick a lot. I thought you had the flu last month. Wow, it always seems like something is wrong with you." Mhm, I feel the same on all accounts.
And, Fuckers, that’s why I stopped talking about it or looking for answers a long time ago. Instead, I've just relied on the most logical answer and quit worrying. I’ve done enough research on my own, not to mention all my Animal Science schooling, to know how stress responses work. They’re significant. They have the potential to disrupt your entire body through hormonal dysregulation. And they work differently - as far as we can tell - depending on the organism.
So that’s what I’ve leaned on. Acknowledgement that stress really screws with me. It zaps my energy. It fogs up my brain. It makes me overstimulated. It causes weird pains and immune system responses. It churns up my digestive problems. It also makes me feel like I’m starving but nauseous all at once. Over long periods of time, it can lead to infections. It, obviously, ruins my sleep, which reaaaaally doesn’t help with any of it.
So that’s what I’ve leaned on. Acknowledgement that stress really screws with me. It zaps my energy. It fogs up my brain. It makes me overstimulated. It causes weird pains and immune system responses. It churns up my digestive problems. It also makes me feel like I’m starving but nauseous all at once. Over long periods of time, it can lead to infections. It, obviously, ruins my sleep, which reaaaaally doesn’t help with any of it.
That’s that. Pretty complicated but simple. Try not to stress yourself out and god help you, if you do. Chill for a few days and you’ll be alright, probably. No one knows why it happens. Doctors don’t care. Just watch out for yourself, because no one else deals with this shit.
Unless… they totally do.
So, that’s fibromyalgia
I guess this is where I tell you something that a lot of folks have probably already figured out. Sorry if you’ve been yelling at me through your headphones this whole time - chill, I’m getting to it.
There definitely is a term for everything I’ve described. There are millions of other people who experience it. And, yeah, doctors often still don’t believe it’s real… but the numbers and anecdotal evidence don’t lie.
Ever heard of fibromyalgia?
Of course you have. But have you ever really looked into what it meant? Because… I hadn’t.
Annnnd then a listener and I were chatting on Instagram a few weeks ago. And she mentioned... everything I just mentioned. And her diagnosis had been? Fibromyalgia.
Annnnd then a listener and I were chatting on Instagram a few weeks ago. And she mentioned... everything I just mentioned. And her diagnosis had been? Fibromyalgia.
Via DM, your fellow Fucker started telling me about being tired all the time, mysterious aches and pains that worsen with stress, IBS symptoms, improper temperature regulation, and over-exertion that leads to required days of recovery. My jaw hit the floor.
You know I hopped online and started doing more research of my own. And all of the information was confirmed and expanded upon in a way that drove my mandible straight into the basement.
Hey, you know how fibromyalgia is synonymous with “widespread pain?” Oh shit, if you dig into it, there is a lot more to learn. Here’s a (maybe, complete?) list of the currently known associated symptoms. Keep in mind, I couldn’t find a single comprehensive resource for this information. This list is compiled of information from the the peer-reviewed article I'm going to read from later, the American College of Rheumatology, the CDC, Healthline, and Medical News Today. And if it sounds like a bit of a "catch all" pile, I think you're right.
Pain and stiffness all over the body
Fatigue and tiredness
Depression and anxiety
Sleep problems
Problems with thinking, memory, and concentration, known as “fibro-fog”
Headaches, including migraines
Tingling or numbness in hands and feet
Pain in the face or jaw
Digestive problems, such as abdominal pain, bloating, constipation, and irritable bowel syndrome
Tenderness to touch or pressure affecting muscles, sometimes joints or even the skin
Irritable or overactive bladder
Pelvic pain
Trouble focusing or paying attention
Pain or a dull ache in the lower belly
Dry eyes
Sleeping for long periods of time without feeling rested (nonrestorative sleep)
Acid reflux
Restless leg syndrome
Sensitivity to cold or heat
Problems with vision
Nausea
Weight gain
Dizziness
Cold or flu-like symptoms
Skin problems
Chest symptoms
Breathing problems
Insulin resistance
Wait, wait, wait. THAT’S what fibro is? Because, I’m sorry, I have literally never heard any of that detail before… and although it gets so ambiguous that I suspect these ailments are all the conditions that just haven't been explained before by medical science... this list just described my life. All the way down to the tiniest detail of dry eyes, as I now recall chronically dumping drops into mine for those same years in my 20s. What. The. Shit.
Prior to this research, my symptomatic knowledge of fibro was essentially - pain, of the unexplained and incurable variety. No one ever once has mentioned anything else about the condition to me, or allll the ways that it correlated with my years of health trauma. Not my peers, not my doctors, and not even my amazing, well-informed therapist.
So, maybe I’m really late to the game here, but long story short, my mind was blown when I heard that there’s actually a term for this experience which I had forfeited to processing as a “unique way that my body individually destroys me” for all these years. I thought I was just uniquely uncomfortable all the time and stopped burdening others with my experiences.
So, maybe I’m really late to the game here, but long story short, my mind was blown when I heard that there’s actually a term for this experience which I had forfeited to processing as a “unique way that my body individually destroys me” for all these years. I thought I was just uniquely uncomfortable all the time and stopped burdening others with my experiences.
Maybe that’s why I never had anyone clue me in to the diagnosis - I honestly stopped talking about the cyclical sickness a while back, after recognizing that people didn’t respond favorably to the narrative, “I just get too stressed out to function.” Shutting my mouth and writing off my experiences may have halted my potential for hearing a realistic account of living with fibromyalgia. Oh, how the trauma shame shenanigans never stop royally fucking you.
Of course, based on my own recent education, now I’m wondering if fibromyalgia applies to far more of us in the trauma community. Because if I hadn’t found reliable information on it in all my trauma and inflammatory illness research over the years… how many other people are in the same boat?
And this brings me to my next point. I really hate the term fibromyalgia.
Why I hate the term
There’s actually another explanation for why I never heard about everything that fibromyalgia describes. Uh, you’re going to hate me for this, but I didn’t think it was a “real” diagnosis.
Yep. I’m telling you with moderate guilt that for the longest time, I appraised fibro in the same way that western medicine considers all psychosomatic illnesses - not valid. And I’m unhappy with myself, too. Believe me, I feel like my least favorite kind of person... a hypocrite. But this also points to the systemic issue that undermines so many of our attempts to get help, and that makes me far more unhappy.
Yep. I’m telling you with moderate guilt that for the longest time, I appraised fibro in the same way that western medicine considers all psychosomatic illnesses - not valid. And I’m unhappy with myself, too. Believe me, I feel like my least favorite kind of person... a hypocrite. But this also points to the systemic issue that undermines so many of our attempts to get help, and that makes me far more unhappy.
You see, a number of years ago, as a budding counselor with a few years of experience, my therapist friend mentioned something about fibro. Specifically, that it was a common label granted to more seriously mentally affected patients… and it wasn’t believed to be a real thing. I wish I could remember more detail on the context, but the basis of the story is, someone that I trusted - someone with many trauma patients - told me that in her experience, no one took fibromyalgia seriously. People with intense mental illnesses regularly presented with unfounded complaints of pain, and this is the term they were assigned as a result.
There was no proof of their physical discomfort. The patients tended to have myriad mental and physical health issues. They tended to be more difficult clients. Professionals had doubts about how serious the complaints were. No evidence, no respect. It was just about that simple.
To give more weight to the story, here’s one quick excerpt that is actually validating to read, from an article titled, The management of fibromyalgia from a psychosomatic perspective: an overview.
��People with FM often reported dismissive attitudes from others, such as disbelief, stigmatization, lack of acceptance by their relatives, friends, coworkers, and the healthcare system, that consider them as ‘lazy’ or ‘attention seeking’ people, with their symptoms ‘all in their head’. Such dismissiveness can have a substantial negative impact on patients, who are already distressed, and also on the degree of their pain.”
So… similar to the asshole social associates described above… for years after that, I paid no attention to fibromyalgia. When people brought it up, I nodded and moved on. I didn’t disbelieve that there would be a connection between mental illness and the onset of bodily pains after my own experiences, but the term had also been shuttled to a file in my head that sidled up next to, “seeking prescription pain meds.” This was an incorrect judgement based on incorrect, oversimplified information. But unfortunately, it left an impression.
So… similar to the assholes described above… for years after that, I paid no attention to fibromyalgia. When people brought it up, I nodded and moved on. I didn’t disbelieve that there would be a connection between mental illness and the onset of bodily pains after my own experiences, but the term had also been shuttled to a file in my head that sidled up next to, “seeking prescription pain meds.” This was an incorrect judgement based on incorrect, oversimplified information. But unfortunately, it left an impression.
It took the real life account of someone with the diagnosis to show me all the ways that my previous perception was completely incorrect. I suddenly realized how reductive and insulting the false information had been. Annnd all the ways that I could have really helped myself and a few others a lot sooner if I had just investigated the term on my own, rather than lazily falling back on someone else’s casually-expressed opinion.
So, I’m saying… fuck me. 100%. That makes me really upset with myself. But it makes me even more frustrated with the medical field.
And this is why I hate the term fibromyalgia.
It doesn’t actually explain a fucking thing… and it doesn’t seem like anyone is actually trying to.
At this point, there is no known cause for the development or persistence of the disorder. Fibromyalgia has essentially become more of a label for a grouping of symptoms that we “allow” people to assume when we don’t know what the hell might be wrong with them. I say “allow” very purposely, because it feels like our medical overlords have granted us this word as a way to pacify the uncomfortable masses - not treat them.
At this point, there is no known cause or organic mechanism for the development or persistence of the disorder. Fibromyalgia has essentially become more of a label for a grouping of symptoms that we “allow” people to assume when we don’t know what the hell might be wrong with them. I say “allow” very purposely, because it feels like our medical overlords have granted us this word as a way to pacify the uncomfortable masses - not treat them.
Millions of humans have detailed the same experiences, but science hasn’t yet come up with a way to explain them, so let’s go ahead and give them a new diagnosis that boils down to “Not sure what’s going on, but they say it’s unpleasant and it sounds a little something like widespread pain. Cool, let’s call it a day. Nah, we don’t need to educate the medical community or the public - we don’t need a single list of all the known comorbidities - because we don’t get it, ourselves. Let’s make sure we put that disclaimer right in the definition, so everyone knows it’s a controversial topic."
And implicit in saying that doctors and scientists don’t understand the term, comes a negative connotation of assumed delusion or attention-seeking complaints.
Essentially, what I’m bitching about is the tendency of researchers and practitioners to shuttle things they can’t directly measure to the back of the relevancy line. Despite all of the anecdotal evidence from fibro sufferers that corroborate the same causes, symptoms, and outcomes… we can’t see what they’re talking about and we don’t have an easy explanation, so we put this in the “fake news” stack of information - AKA psychosomatic illness.
Now, it’s also worth mentioning that fibromyalgia is deeply intertwined with trauma. Something like 2/3rds of fibro patients also have confirmed PTSD symptoms, if not higher. Exact numbers depend on which study you trust. Just know, it is a prevalent, accepted, correlation between trauma and the development of fibromyalgia. And of course, no one has determined the causative or affective relationship between the two at this point in time.
Hell, we all know that a lot of mental and physical health professionals don’t even want to acknowledge trauma at this point - or, do so with a smirk and an eyebrow raise, at best. So tethering the two poorly-comprehended disorders together? Oh boy, it’s a sure-fire way to ensure that no one listens to a word you say after honestly answering their background information questions. Might as well throw down your wallet and walk yourself right out of the office at that point.
Hell, we all know that a lot of mental and physical health professionals don’t even want to acknowledge trauma at this point - or, do so with a smirk and an eyebrow raise, at best. So tethering the two poorly-comprehended disorders together? Oh boy, it’s a sure-fire way to ensure that no one listens to a word you say after honestly answering their background information questions. Might as well throw down your wallet and walk yourself right out of the office at that point.
The medical field’s lack of trauma education is a big problem. Making “psychosomatic” a dirty word isn’t helping millions of folks out there. Being invalidated by the people who could possibly help you is another mental health crisis waiting to happen. And all of this is infuriating to me, following my own experiences and thinking about other people’s.
Should we take this one outrage step further? Sure.
You know that a vast majority of fibromyalgia sufferers are… women. Sorry, about to get a tad feminist. Is anyone here surprised that primarily female voices tend to be written off by medical professionals? Ha, ha, ha. No, probably not.
For all of human history, the ladies have been getting the shit end of the stick when it comes to medical care. We all know that women were given amazing explanations for their ailments, such as having “hysterics” or "the vapors" not so long ago.
Furthermore, there is research showing that doctors do not take women’s accounts of pain severity seriously, in particular. Even fellow female doctors and nurses are given different treatment by staff when they go to the ER, versus male counterparts. And if you’re a minority or socioeconomically challenged woman? The data says you might as well take two aspirin and see what happens the next morning, because the medical attention research is even worse for those demographics. Huge surprise.
So, pulling this all together: Considering that the majority of us who receive complex trauma diagnoses are women… considering that implicit in this label, comes the increased likelihood that we’re not economically well-to-do and belong to minority groups one way or another… how do you figure we’ve ever had a chance of receiving real help for our unmeasurable physical conditions?
So, pulling this all together: Considering that the majority of us who receive complex trauma diagnoses are women… considering that implicit in this label, comes the increased likelihood that we’re not economically well-to-do and belong to minority groups… how do you figure we’ve ever had a chance of receiving real help for our unmeasurable physical conditions?
Yeah, we haven’t.
We’ve been given a term - complete with a wink and a nudge - that no one wants to meaningfully research or prioritize understanding. We’ve received a new phrase that doctors will “generously grant us” when we’re drowning in unexplained symptoms and pain. We’re then labeled with a word that essentially amounts to “disregard and humor” for all our future appointments. On top of it all, we’re carrying the burden of traumatic histories, which immediately qualify us for misunderstood diagnoses that more or less equate “ghosts in their blood” - because, hell, we can’t quantify mental illness, either.
The whole ordeal makes me really upset. The fact that I was inadvertently pulled into this biased disbelief makes me more upset. It also serves as quite a demonstration of how powerful or deleterious knowledge can be after it worms its way into your head involuntarily and becomes your only “go-to” piece of data, true or false.
One seemingly-trustworthy person mentioning a negative opinion of fibromyalgia one time in my past somehow infiltrated my thoughts to the extent that I didn’t have a second thought for 5 years? And we're talking about a goddamn trauma researcher - with, what I consider - an otherwise open and connection-happy mind?
The power of assumed authority and truth in opinion is significant. If I can be swayed in this way, how could less mental health informed medical professionals stand a chance in responding differently? That’s frightening and clarifying… though immensely upsetting.
So, since biomedicine hasn’t bothered to find any great information for us, despite the rapidly increasing rate of fibromyalgia diagnoses in the past two decades - how can we make sense of the information to actually help ourselves?
Let’s talk about that next.
What we can conclude
So it kindof blows finding out that you probably qualify for a new medical term… only to find out that we don’t actually know anything about said term. I say this, because if you’re waiting for me to pop off with some sweet research on fibromyalgia… uh… I haven’t found it yet. But not for lack of trying. So far every article I’ve seen has been pretty basic and uninspired.
Does fibromyalgia correspond with trauma? It does. Does stress mediate and moderate fibromyalgia, PTSD symptoms, GI problems, and depression? It does. Does it take a long time and numerous appointments to receive medical help for fibromyalgia complaints? It does. Does the comorbidity of post-traumatic symptoms make fibro more uncomfortable and challenging to overcome? What do you know - it fucking does.
(Wow. So enlightening. Having two debilitating disorders is less fun than having one. Who’s funding these research studies, anyways?)
The first thing I can conclude is, there’s not that much to conclude. This is to say, no one - that I’ve seen, so far - has revealed anything super shocking or thought-provoking about fibromyalgia.
The first thing I can conclude is, there’s not that much to conclude. This is to say, no one - that I’ve seen, so far - has revealed anything super shocking or thought-provoking about fibromyalgia.
Really, the most interesting things I learned from my reading are that
1) insulin resistance is another associated disorder, which explains even more of my baffling life
2) sex hormones are leached from your system under stress, which, refer to point number one... explains another huge chunk of my existence, and
3) the recommendations for treating fibro long term are the same recommendations I’ve given for getting your trauma life re-ordered.
You know how I always push for people to find out what’s manageable on their own through trial and error, rather than approaching trauma recovery with preventable fires burning in every area? Hey - someone agrees.
Namely, it's recommended that in order to manage fibromyalgia you establish routines including strictly nutrition-based eating habits, non-threatening forms of consistent exercising, prioritizing tons of sleep, and controlling your environment as much as possible for stressful stimuli. Doctors can also supplement your rehab with antidepressants, because, again, fibromyalgia is related to the same underlying hormonal imbalances as depression - but the larger health issues are managed best by changing your behaviors. Just like I’ve said.
I suppose this is no surprise, since this entire time I’ve unknowingly been talking, in large part, about how I’ve controlled my own fibromyalgia symptoms. I just thought it was mandatory trauma pains I was dampening. But the word is out! There's a separate phrase for it. The doctors and I agree; stop treating yourself like a turd, and maybe you’ll stop feeling like one. Whatdoyouknow. Sometimes there are reasons for the things I notice experientially, even if they aren’t originally informed by medical lingo.
Secondly, looking at what we can conclude at this point about fibro… Well, it justifies my previous hypothesis that stress is the root of my body’s evil. There’s not much to definitively say about fibromyalgia at this point, but we know for a fact that it is agitated and potentially caused by stress.
Secondly, looking at what we can conclude at this point about fibro… Well, it justifies my previous hypothesis that stress is the root of my body’s evil. There’s not much to definitively say about fibromyalgia at this point, but we know for a fact that it is agitated and potentially caused by stress.
This perfectly aligns with my observations that a terrible work week mixed with a personally challenging month on top of a physically exhausting cleaning marathon will lead to a systemic breakdown every time. And, conversely, those times when life has actually been pretty chill correspond to periods of bodily health and limited upset - the times when I wonder “was I ever really sick at all?” and start to health gaslight my damn self.
Realizing the link between stress and sickness, of course, also begins to explain the correlation to trauma, and particularly, complex trauma.
Now, let me start by saying that there’s some debate over the downstream effects of PTSD - some researchers swear that it decreases system arousal in the face of later stress, others have collected data reflecting that a nervous system hyper-sensitization takes place. From my own trauma involvement, I’ve seen and heard more cases of the latter; we’re quick to upset and easily pushed into stressed territory. I don’t know many, if any, trauma folks who are non-responsive to disturbing life events... but that sounds more like a deep, dangerous, clinical depression symptom to me.
Personally, once I’ve been chronically stressed for a few weeks or months, then I notice the loss of stress response take over. My limbic system gives up, the HPA axis stops responding, and therefore nothing can rattle me. Perhaps you’ve also had the experience of laughing when your car breaks down, because it’s already been 3 months of disaster around every turn and there’s nothing else you can do for yourself. So, sure, people can reach a point where they legitimately don’t respond to the chaos anymore, but I’m not so sure that’s a consistent norm. I think it’s more likely that you turn off your stress reactions if you’ve been adequately prepped to dissociate for the sake of sanity or your chemical balance is so wack that your danger center has powered down.
I can tell you without a doubt that before the point when my stress threshold has been raised sky-high thanks to repeat exposures and wiring disconnections... I’m a rapid-responder when anxiety comes calling. Stimulus - rapid survival reaction - no space in between being startled and shaking from head to toe. And this is the case for basically every Motherfucker I know. I’m no expert, but I think we tend to fall more into the hypervigilant camp surrounding this podcast, rather than the laxadonical one. Always on the lookout, always ready, often bowled over by our own responses.
I’m a rapid-responder when anxiety comes calling. Stimulus - rapid survival reaction - no space in between being startled and shaking from head to toe. And this is the case for every Motherfucker I know. I’m no expert, but I think we tend to fall more into the hypervigilant camp surrounding this podcast, rather than the laxadonical one. Always on the lookout, always ready, often bowled over by our own responses
This nervous system sensitization, as they call it, explains a lot of trauma symptoms. I’ve regularly discussed the hypersensitivity problem it creates, when your brain doesn’t adequately filter out or assess neutral stimuli because it considers basically everything to be a threat. This can also contribute to the ADD and ADHD diagnoses that we receive, when our heads are too busy trying to sort all that data streaming in to direct our thoughts in a steady way. Or, the ways that we’re uniquely thrown immediately into panic mode when we sense a risk. Plus, we’ve probably all had the experience of tiny, secret triggers sneakily upsetting our bodies when the stimulation wasn’t even significant enough to pass through our cognitive recognition centers. These are all caused by the same systemic over-sensitization problem.
In general: yes, we trauma folk are sensitive to our environments - inner and outer. We are easily pushed down survival pathways to fight/flight/freeze/fawn responses. We rapidly catastrophize ambiguous information, which can convince our brains and bodies that the worst has already happened. We’re hyperaware and easily overstimulated, often agitated, and regularly on edge.
I maintain, in the face of controversial evidence, that we get stressed out easily. And our bodies react dramatically.
I feel like I should also state that this is especially true, as most of us have read, when we have unresolved emotional strain floating around in our meat jackets. We can be overstimulated and aroused (in a bad way) from the inside, out. Since the majority of us are not skilled in emotional recognition or resolution, we’re often walking around with a lifetime of hard feelings stored in our guts. And there’s been roughly zero doubt in my head about emotional and environmental stress contributing to dissociation, contributing to a vagal nerve shutdown as a big part of the digestive failure that characterizes fibromyalgia, IBS, Crohns, and so many autoimmune disorders.
On top of the unresolved emotional root of stress, this pings another episode that I've previously released. The one about being overly restrictive in your diet and exercise for the sake of appearance perfectionism. If you physically exert yourself too strongly through caloric deprivation or extreme work outs, you can easily stress your body into a survival response. It can't tell the difference between starvation for bikini season and starvation for lack of food. Running your ass off for your upcoming wedding or running your ass off for your upcoming bear attack. Your danger sensing center is sensitive and it overreacts, much like myself.
Now, considering that all these examples of central nervous system sensitization and physiological survival states that go hand in hand with Complex Trauma and Fibromyalgia, so many weird health mysteries are potentially resolved. But, not exactly the pain component. Or, is it.
Now, considering that all these examples of central nervous system sensitization and physiological survival states that go hand in hand with Complex Trauma and Fibromyalgia, so many weird health mysteries are potentially resolved. But, not exactly the pain component. Or, is it.
Again, the authors out of Italy and Brazil who penned, The management of fibromyalgia from a psychosomatic perspective: an overview, have a potential way to think about that. They state:
“Even if the causes and pathophysiology of FM are not completely known, widespread chronic pain could be explained by a vulnerability due to a perturbation in the central processing of sensory information, named ‘central sensitivity’ or ‘central sensitization’, that amplifies the response of the central nervous system to a peripheral input. Hence, people with FM and/or other central sensitivity syndromes have a lower threshold for interpreting sensory information as noxious. Several factors, such as genetic predisposition, deficiencies in neurotransmitter levels, biochemical changes in the body, endocrine dysfunction, mood states, anxiety, sociocultural environment, psychological trauma and past experiences in general, expectancy beliefs, and catastrophization have been proposed as explanatory mechanisms of patients’ subjective experience of central sensitivity. Current research indicates that abnormal sensory and pain processing is a key factor in the pathophysiology of FM. There is robust evidence that abnormalities in central pain processing, rather than damage or inflammation of peripheral structures, play an important role in the development and maintenance of chronic pain in patients with FM.”
Interesting, huh? I still think inflammatory responses are a big part of the 1000 piece stress puzzle, but I don’t disagree with the idea that our finely-tuned danger detection systems amplify pain and discomfort signals to deafening levels. Putting all the system data together, you can deduce a fairly complete picture of how strain, physical degradation, and pain are all related.
Finally, I have confirmation that being overly stimulated causes everything from my energy drain to my dietary responses, migraines, and autoimmune attacks... all the way down to my temperature sensitivity, random presentation of allergic reactions, and even that occasional sharp pain in my jaw… not to mention all my life-altering functional problems, like being unable to sleep at night, existing with debilitating pain, and living while feeling sedated?
Finally, I have confirmation that being overly stimulated causes everything from my energy drain to my dietary responses, migraines, and autoimmune attacks... all the way down to my temperature sensitivity, random presentation of allergic reactions, and even that occasional sharp pain in my jaw… not to mention all my life-altering functional problems, like being unable to sleep at night, existing with debilitating pain, and living while feeling sedated?
All of my strange health complaints from the past decade have aligned with this new label. And that label corresponds perfectly with my inkling that running on cortisol and overzealous guardsmen have been the major source of my health anxiety sauce. Welp, it’s been validating research for all of my educated guesses, to say the least.
Long story short, there’s not a ton of helpful information about the reasons for developing fibromyalgia or what makes it get worse. But there’s one thing we do know for a fact; stress is the enemy. At least I think it’s comforting to conclude that stress is the root of many of our C-PTSD complaints, as well as depression, anxiety, insomnia, obsessive thoughts, and now… a whole list of common maladies, labeled fibromyalgia.
Whether or not it’s really understood, at least there is a connection between everything. At least there’s something that ties ALL the random, disjointed pieces of torture together. I’m guessing that for many of us, fibromyalgia is similar to complex trauma, again, in that regard.
And, lastly, I can conclude that… I have more questions
More questions than answers
Here’s one last excerpt from the aforementioned article, which is the only one I found that’s worth hearing from.
They state: “FM is labelled, often with a negative connotation, as a ‘functional somatic syndrome’, part of a ‘somatization disorder’, ‘fashionable diagnosis’, ‘idiopathic pain disorder’, ‘non-disease’, ‘psychosomatic syndrome’, dismissing the true suffering of the patients. In the absence of a univocal identified biological cause, subjective reports of symptoms by the patients are often viewed derogatorily and discredited as ‘psychogenic.’”
Like I said, there isn’t a lot of helpful information out there if you’re looking to learn more about this controversial condition. Unfortunately, it has been categorized as a “functional somatic disorder” which essentially means that we don’t have an explanation for the organic basis of the disorder.
Like I said, there isn’t a lot of helpful information out there if you’re looking to learn more about this controversial condition. Unfortunately, it has been categorized as a “functional somatic disorder” which essentially means that we don’t have an explanation for the organic basis of the disorder.
Uh, I don’t know what could be more organic than the endogenous hormones in our own bodies creating downstream health effects, but hey, I’m not a biologist anymore, what do I know?
The fact remains - there’s a lot more to understand about the assorted mechanisms that lead from trauma into depression, generalized stress disorder, and physical manifestations of a biochemical system that’s running off-balance. And this is where I have the biggest questions.
First, I have to get this out of the way. I’m wondering about the known gender split in fibro. The numbers are horrendously skewed towards women as the primary sufferers, and that’s not helping the medical legitimacy case. So, what are the chances that men just don’t have fibromyalgia at the same rate as women? Either they don’t get stressed to the same magnitude or their bodies respond completely differently? It’s possible. OR. Is it something else?
It seems to me like this follows another similar mystery - what are the chances that men just don’t suffer from Complex Trauma at the same rate as women? Pretty poor? Probably more of a diagnostic or seeking-help issue? Yeah, I think so, too. Yet, if you look strictly at the numbers, it sure seems like there are more women hearing about C-PTSD than men.
This analogous labeling issue between the genders makes me think of a few explanations…
1) Men don’t seek help for their physical ailments the way that women do, either because they’re less in tune with their bodies or because they’re shamed for not being tough enough if they complain. Just like C-PTSD.
2) Men don’t hear about fibromyalgia, because it is an engendered diagnosis reserved for dramatic women at this point. Just like C-PTSD. They receive other partial diagnoses, like IBS, that are less controversial. This leads me into a whole spiraling rant about several genital-dependent psychological diagnoses that I feel similarly about, but one of them is…
3) Men don’t receive the same level of fibromyalgia labels as women because men don’t often receive Complex-PTSD labels, which would serve as a hint to their doctors, since trauma is a well-known predisposing factor…
This brings me to the next set of questions.
It’s unpopular opinion time, but, frankly, I don’t know that any of these trauma and fibro issues are really that separate.
It seems to me like we’re talking a lot about one particular problem that splinters off into a thousand different outcomes, depending on the circumstances, the biology, and the human in question. Not separate conditions.
It seems to me like we’re talking a lot about one particular problem that splinters off into a thousand different outcomes, depending on the circumstances, the biology, and the human in question. Not separate conditions.
First comes the trauma, then comes the presentation of downstream physical and mental symptoms. Presentation, magnitude, and personal recognition of these symptoms varies, just like severity of Complex Trauma does. But under both conditions, our experiences are often so similar - the hard part is that we struggle to describe them and often lean on abstract language which can be used in such diverse ways. We focus on different problems, depending on our own life impacts.
So, maybe we notice and report internal events differently, but it’s hard for me to believe that the two disorders aren’t more than corresponding diagnoses - and are, in fact, one and the same.
I could be very wrong, but I’d sure like to find out.
So, to the small percentage of fibromyalgia sufferers who don’t have trauma… you sure? To the depressed and anxious folks who can’t seem to get a grip on their physical health, but never saw their life as traumatic… want to take another look? To all the traumatized folks with Raynauds, food allergies, hypertension, ADD, aches, and migraines… have you really looked into the full definition of fibromyalgia?
ARE these conditions of trauma and fibromyalgia different? Or is this another complication in identifying unseeable symptoms in a population of folks who never learned to name their mental and physical experiences? Is this an artifact from a group who tends to underestimate and under-report their own experiences in light of unhealthy others’ core beliefs? How prevalent is fibromyalgia, really? Especially in the context of Trauma?
ARE these conditions of trauma and fibromyalgia different? Or is this another complication in identifying unseeable symptoms in a population of folks who never learned to name their mental and physical experiences? Is this an artifact from a group who tends to underestimate and under-report their own experiences in light of unhealthy others’ core beliefs? How prevalent is fibromyalgia, really? Especially in the context of Trauma?
Is it possible that everything boils down to one underlying event - trauma - that produces a whole host of other biological adaptations down the line? Did we create a separate term for it, simply based on a lack of standardization?
Or is this an exclusionary problem?
Have all the various ways we’ve learned to categorize and describe our experiences actually separated one full disorder into two half-disorders; one that encompasses the brain and another that covers the body? Is it our societal misunderstanding of the connection between our perceptions and our meaty husks, forcing us to separate the issues of mental and physical health that would be better understood together, as one?
I’m not sure! But I’m definitely thinking a lot about it.
Partially, from personal bias. I always considered my physical issues to be part of my trauma life, not separate from it - and that explanation made perfect sense to me. Where do these disorders really split? Maybe it’s possible to have Complex PTSD without the physical symptoms, but that's really not what I hear from people. The most of us have at least some periods of physical ailments, even if they're not persistent. To me, it seems like a distinction that should be made within the trauma diagnosis - with or without physical wellness degradation - rather than piling a separate, largely-ineffective diagnosis on the vast majority of us who have some variety of said bodily ailments.
I feel like the real issue isn’t “what is fibromyalgia?” The actual problem is a lack of biological understanding in the Psychology field. And a mirrored failure to understand Psychology in the medical field. Then, throw in a reluctance to study the conglomerate of bio-physiology and mental health issues in the scientific research literature because both experiences are difficult to measure or confirm and the studies would be less elegant.
I feel like the real issue isn’t “what is fibromyalgia?” The actual problem is a lack of biological understanding in the Psychology field. And a mirrored failure to understand Psychology in the medical field. Then, throw in a reluctance to study the conglomerate of bio-physiology and mental health issues in the scientific research literature because both experiences are difficult to measure or confirm and the studies would be less elegant.
If more psychologists actually learned system biology and more medical practitioners actually studied abnormal psychology, maybe we wouldn’t have disparate diagnoses that each come with a half-recognition. Maybe we could have one term that encompassed the full experience of trauma. Maybe these professionals could confirm all the details that we don’t understand by working with a more comprehensive approach to how humans work as a whole, rather than organ by organ. Just a fucking thought.
Because, I can tell you, if my therapist friend had the same biological education that I did at the time, I guarantee that she wouldn’t have told me fibromyalgia was a “pseudo diagnosis.” If she had knowledge of the connection between stress hormones and bodily breakdown, plus the trauma physiology that determines our sensitivity to stress - there’s no way she would have been so flippant or insensitive with her words. But under the influence of her counseling peers, the diagnosis became a fallacy.
I think this highlights the danger of the problem at hand. It only took one industry-determined void of knowledge to pass along an unfair opinion that skewed at least my perception for years down the line. And, think about it, how many times has one innocently-baseless comment in the psychology or medical fields probably created a lifetime of bias in an up-and-coming professional?
Maybe this is why we have the self-perpetuating negative connotation of psychosomatic illness in our society that seems to crawl its way towards improvement, while every other disorder makes significant strides. A lack of personal understanding of the biology-psychology connection is easily turned into a respected opinion, and readily transmitted to unknowing people who are eager to learn from their wise mentors. And so, the next generation inherits the same set of half-baked progress-stunting ideas. Over and over and over.
Maybe this is why we have the self-perpetuating negative connotation of psychosomatic illness in our society that seems to crawl its way towards improvement, while every other disorder makes significant strides. A lack of personal understanding of the biology-psychology connection is easily turned into a respected opinion, and readily transmitted to unknowing people who are eager to learn from their wise mentors. And so, the next generation inherits the same set of half-baked progress-stunting ideas. Over and over and over.
Depressing! And enlightening.
And that’s roughly where I stand today, after days of fibromyalgia research and very few satisfactory answers. Depressed and enlightened.
More or less, asking myself more questions about the legitimacy of our entire mental and physical healthcare system and all the lines we draw in the sand. Confident that trauma leads to increased stress leads to increased brain and body trauma. Somewhat happy to know that I’m actually not the only one who consistently apologizes for feeling like shit and questions if it’s “valid” or not because it seems connected to my brain. But also, pretty pissed off that we’ve been given a word that comes with no explanations and a hellofalot of medical field judgement, as if we needed more of that.
Oh, one more factoid to throw into the end of this conversation. There’s a link between low socioeconomic status and fibromyalgia.
Oh, one more factoid to throw into the end of this conversation. There’s a link between low socioeconomic status and fibromyalgia.
Hey, the same link exists between socioeconomic status and complex trauma. Hey, it’s another predisposing factor for post-traumatic stress disorder symptoms’ emergence. Hey, big surprise, if you have a stable and predictable physical and financial environment, you’re less likely to develop the terror-based conditions brought on by earlier trauma.
If you have financial resources, you’re also less likely to be chronically stressed by the demands of life. You’re probably also more likely to receive respectable medical care. Therefore, meaning that you’re both less likely to have enough perturbation to develop over-sensitive nervous system responses and less likely to be dismissed by doctors with a label they don’t believe exists. Plus, probably more likely to have access to mental health care that could prevent the onset of Complex Trauma presentation, and likely fibromyalgia, altogether.
Oh, look, logic explains so many things. Or, fuckit, let’s just choose to believe that poor people are lazy and always want to complain about something, whether it’s in their heads or their bodies. Whatever the rich white men say.
Big issues to think about.
Like I state way too often on this show, it’s the small things in this trauma life that bring you comfort. And monumental societal failures that make you scream. (Okay, I just added that last part today.)
Wrap it
Okay, let me get out of here before I question more beliefs that are way out of my paygrade. Sorry, medical and psychological practitioners. I know that I’m just a critical observer who, like that kid everyone hates in class, perpetually asks too many questions.
At the bottom of all my complaints, I just wish that we could come up with a way to characterize these disorders that actually helped people understand what was happening. If you know how your body is reacting to what stimuli and how the symptoms are all related, that's a lot more powerful than throwing assorted barely-defined titles at them.
If we can't definitively say that fibromyalgia and trauma symptoms are one and the same, fine. Let there be a distinction. But I think it would be preferable to call fibro something more telling and true to the accepted cause. Call it semantics, but something like Stress Affective Syndrome would be more useful than the made-up word of fibromyalgia. Please, anyone feel free to come up with a better phrase, because I just made "Stress Affective Syndrome" up so I could say "I've got SAS." It already fits the bill.
I guess I’m just up in arms that I’ve tried to find answers for my brain and body health all these years, and turned up completely empty handed until random connections have eventually given me the information I’ve needed after a decade of effort. Maybe if I had my complex trauma diagnosis before I had my health complaints, someone would have mentioned fibromyalgia. Maybe, they would have knowingly smirked and sent me to a psychiatrist. Hard to say.
I guess I’m just up in arms that I’ve tried to find answers for my brain and body health all these years, and turned up completely empty handed until random connections have eventually given me the information I’ve needed after a decade of effort. Maybe if I had my complex trauma diagnosis before I had my health complaints, someone would have mentioned fibromyalgia. Maybe, they would have knowingly smirked and sent me to a psychiatrist. Hard to say.
Even if I had gotten that information about fibro, would it have helped separate from the C-PTSD diagnosis? Honestly, probably not. I would have just been harder on myself for suddenly being too weak in the face of stress. And after reading that medical professionals doubt the validity of fibromyalgia, in the first place? Well that would have been a whole other source of disbelief, anger, and negative self-regard. Maybe a whole new crisis, once my inner critic got a chance to hammer away at my head.
I suppose that figuring out the patterns of my strange bodily conditions actually needed to happen organically for this Fucker, because any semi-questioned diagnosis would have just been more fuel for my trauma fire at that point when I so thoroughly despised myself. Confirming to myself, for a fact, that stress fucks me up may have been a prerequisite for accepting that I might be “one of those fibro people.” You know, the ones who lie about their symptoms. Ha.
And, again, this says a lot about the potential damage that poorly-described labels can do to people… just as much as it says about my own reluctance to be considered a weak-minded over-reactor by outsiders.
All of this being said, I’m so grateful for finally finding out exactly what all fibromyalgia actually entails. It took too long, but honestly, the information came at the perfect time. Two days after I got it, I was stress-sick. Ahhh, it's fibro time. How’s that for irony?
As always, I do think there is some empowerment in the basic root understanding that you aren’t the only one who’s dealt with any of this. The mysterious illnesses, the pain, or the lack of care from modern medicine aren’t individual experiences. Hey, you might even be relieved to know that someone else on this planet routinely asks herself, “Do I have cancer for real this time, or am I just overworked again?”
As always, I do think there is some empowerment in the basic root understanding that you aren’t the only one who’s dealt with any of this. The mysterious illnesses, the pain, or the lack of care from modern medicine aren’t individual experiences. Hey, you might even be relieved to know that someone else on this planet routinely asks herself, “Do I have cancer for real this time, or am I just overworked again?”
After years of nobody I spoke to having a tale that even mildly resembled my autoimmune breakdown, finding anybody who related to my issues was extremely relieving. Not only was it a common experience, but it meant that I hadn’t somehow brought the discomfort on myself - through mental illness, physical shenanigans, or plain old weakness - the ways that I feared.
Furthermore, it proved that I hadn’t imagined it all. Because believe it or not, you’re surprisingly willing to throw yourself under the bus after all the pain has passed. I’ve spent the past decade telling people, “I think I have the glutens, as I call it... but I don’t really know though, it’s never been explained, sometimes other things bother me, and sometimes it’s really not a big deal, I don't know what it is” as an almost-apology. A disclaimer that I, too, doubt my own memories and conclusions because they weren’t properly validated by who I considered authority figures.
Hearing that other people had digestive disorders and autoimmune disasters in the wake of Complex Trauma, via the book The Body Keeps The Score, shocked me into self-acceptance of my prior experiences. Hearing that all of it can be encapsulated by this term fibromyalgia a few days ago - well, shit. This is a more mainstream occurrence than I ever previously thought.
And you know what? It does matter to me that I’m not the only one who falls apart when my brain gets overwhelmed. Even if it doesn’t fix anything. Even if my own postulations for how fibromyalgia is born from trauma feel more applicable than the scientifically proven ones. Even if I don’t believe the term deserves to stand alone as a medical label without further delineation - especially of the connection to and overlap with trauma. Even if I think… it might be inseparable.
And you know what? It does matter to me that I’m not the only one who falls apart when my brain gets overwhelmed. Even if it doesn’t fix anything. Even if my own postulations for how fibromyalgia is born from trauma are more enlightening than the scientifically proven ones. Even if I don’t believe the term deserves to stand alone as a medical label without further delineation - especially of the connection to and overlap with trauma. Even if I think… it might be inseparable.
Now I know. When I feel a physical breakdown coming on, with the suspected cause being stress… I don’t have to apologize for it. I don’t need to tell people that I just can’t handle the pressure with unfettered shame for my own biochemistry. I can rest assured that what I’m going through is common - far more common than we know - and completely valid. Even if there are people ready to tell you that it's not.
But, to be honest, I still probably won’t tell anyone that it’s called fibromyalgia. I’m not proud to say, I wouldn’t want them to think I’m just being dramatic.
UGH.
#cptsd#healcptsd#actually CPTSD#just cptsd things#traumabrain#Complex Trauma#trauma recovery#complextrauma#complexptsd
2 notes
·
View notes
Text
After Hours Medical Advice
As you know, and certain have in mind every day, nursing is a career that carries a huge amount of duty. Be sure to guard your self, especially when asked for advice in an informal setting.
No, Uncle Bob has cornered you within the hallway after Christmas dinner. In trying back, I realize that not as soon as during this experience did anyone INVITE me into a discussion of what could be best for my mother.
She spent two nights in the hospital beneath remark, with IV hydration. Now, admittedly, she has varying levels of dementia even on a good day, but she reached the point of getting severe hallucinations and paranoia.
Having a whole remedy group looking out for you and preparing a discharge plan that is going to set you up for achievement. 90 days of therapy allows for the affected person to work via many of the above mentioned considerations and we treat it using an American Society of Addiction Medicine dimensional assessment.
The general size of keep in remedy that is really helpful is often ninety days. Health safety and prevention is the key to staying healthy for the long haul. From easy blood checks and vaccines now to mammograms and colonoscopies later, your doctor might help you turn into the healthiest model of you.
Although it might appear to be a problem now, one hour in a physician’s workplace now can add years of health to your life. When we have well being questions and considerations, it’s easy to show to good ol’ WebMD for answers. And even though the Internet can be a great well being useful resource, reading about your health points online can usually lead to pointless fear and fear. Remember, you might be unique and deserve a customized evaluation.
So instead of browsing the web for a generic, or even worse, incorrect answer, talk to a doctor in particular person to get the total image—and to cease dropping sleep over your questions (see reason number 5!). While I’ll be the primary to confess that a trip to the gynecologist’s workplace isn’t my favourite way to spend a day, annual pelvic exams are a important a part of any girl’s preventative health care.
Will we have to battle the battle of keyword voids at a grassroots degree, wrangling with the asymmetry of passion by tapping folks to search out these voids and create counter-content material? Do we need to arrange counter-GoFundMe campaigns to pay for ad campaigns that promote real science?
Do not rely on a form’s basic remark that “risks of leaving were discussed with the patient,” he says. That doesn't negate the value of those documents, however they should not be the sum complete of the hospital’s evidence displaying efforts to provide care.
First, the hospital must reconcile any excellent diagnostics, as a result of if any checks had been ordered, the hospital is still liable for checking the results to make certain nothing critical was identified, he says.
Despite our protests, she saved making an attempt to pull out the IV fluid line from her arm and the gizmo , and tugged at her gown. The paper-thin pores and skin on her arms was black and blue from a number of blood attracts. Successful treatment begins with an correct diagnosis, and our experts take the time to get it right.
A team of specialists will listen to your needs and evaluate your condition from each angle to make the very best plan for you. Every year, more than one million individuals come to Mayo Clinic for care.
If witnessed by RN, have them doc the time the patient left in addition to the standing of their IV. If an IV is still in place, first try to contact the affected person after which their emergency contact.
From all the information you've gathered from the Internet and your research, it's time for you to go to your physician with this data and get to know the details. It is important to decide on doctors with whom you're feeling snug.
The level of questioning I got in response to my advice was almost insulting at times. In my head, I advised these callers, “If you trusted me sufficient to name me together with your ailment, why aren’t you trusting my opinion?
Our highly specialized experts are deeply skilled in treating rare and complex circumstances. I actually have been put in this identical position so many times, that I lastly, like you, needed to tell them to contact their supplier or go to the ER/Urgent Care.
I owned a small household follow clinic and some would actually present up there quite than going to their PCP or ER. I do perceive how onerous it is to tell them to go to their PCP’s, but I believe that is the proper motion. We love our family and pals and do not need to see them ill or in ache, however we additionally want them to obtain goal care.
I actually have been practicing as a Nurse and APP for over 15 years now and have found, for me, robust boundaries come with time. You don’t have a look at them as patients, but as whomever they are to you.
YOUR ability to want them to be OK and not be as goal as you'd be with a affected person. Another disagreeable facet effect of trying to assist was the pushback I received.
doctor certification, from the Membership of the Royal College of General Practitioners, and checked performance towards historic outcomes from an independent 2015 examine that evaluated several symptom checkers. symptom checker seems as a chatbot that users can work together with by way of an app or web site. When the consumer varieties out their primary symptoms as a quick sentence or phrase, the symptom checker asks questions about possible related signs.
According to the NIH, 30-40% of Americans report having occasional symptoms of insomnia and 10-15% report persistent issue sleeping—with ladies representing nearly all of those affected.
While you could assume that a poor night’s sleep simply means you’ll need an extra cup of espresso in the morning, chronic sleep problems can actually improve the lengthy-time period threat of hypertension, melancholy, and diabetes. treatment medical disclaimer A physician’s visit can help identify attainable underlying causes for your restless nights—and get you the help you should truly get some zzzs.
Does your family have a history of diabetes, excessive cholesterol, heart disease, cancer, or another significant illness? If so, you could be at risk for these conditions, too—and there are likely issues you can do to decrease that danger. A doctor may help you find out and work with you to determine which screening exams you want.
"Casual" could exit the window, if the individual you advise feels you have triggered them harm; together with your recommendation or deeds. State legal guidelines differ greatly and litigation can truly change the legal guidelines as time passes. So as a nursing skilled, even if your action or advice was justifiable, there isn't a safety from being sued . You might prevail and be discovered "not liable" if sued, but by then you'll have gone by way of plenty of wasted time and pointless stress.
They might help detect vaginal infections, together with sexually transmitted ailments , and should often embody a PAP smear for cervical cancer screening. Although you might have heard about some current adjustments to screening recommendations, the U.S. Preventative Services Task Force nonetheless wants women between the ages of 21 to 65 to get a Papanicolaou test (a.k.a. PAP smear) a minimum of each three years (or more incessantly when you’ve ever had abnormal results).
The lawsuit claimed that Dr M had failed to recognize the patient’s skull fracture and improperly released him when he was intoxicated, and that the delay in treating the fracture was attributable for approximately half of the affected person’s neurological deficits. Later that day, a hospital radiologist learn the affected person’s x-ray and famous a markedly depressed left parietal cranium fracture.
Or will the tech platforms where that is occuring start to grasp that giving legitimacy to health misinformation by way of high search and social rankings is profoundly dangerous? Getting excessive-quality, fact-based well being information shouldn’t be dependent on the result of SEO video games, or on who has extra assets for pay-to-play content promotion. few hours of a newborn’s life, medical doctors administer a vitamin K shot.
This is as a result of infants are born with out sufficient of the vitamin, and the child wants a boost to prevent any potential bleeding. The documentation also should detail the discussion with the affected person regarding potential risks from leaving AMA, Merkrebs says.
The reasons for refusing additionally may be wide-ranging, every little thing from worries about the price to concern about ache or dying, or dislike of being touched, photographs, surgical procedure, or drugs. Once a affected person is examined beyond triage and exams are ordered, a departure at that time could be classified as left without completing remedy , Klauer notes.
Patients leaving the emergency room too soon “are intentionally putting themselves at extra danger for morbidity and even mortality,” Polevoi stated — a degree echoed by other physicians. Ko stated the column will proceed as long as individuals want to study totally different health subjects. Connect with a medical skilled everytime you need one, 24/7, for customized recommendation and prescription, if deemed necessary.
At the end, the symptom checker identifies possible causes and recommends a course of action, similar to reserving a video consultation with a human physician or going to a hospital. The patient and his family consulted with a plaintiff’s attorney who agreed to take the case. Dr M was shocked to find out that he was being sued for medical malpractice.
Within each of these kinds of AMA, there may be further breakdowns when it comes to why the person is leaving, he notes. The affected person might not want any care of any type, or the refusal could also be extra limited — refusing the particular kind of care being provided, as an example, but still willing to be handled.
That's to not say all of the internet is unhealthy, it is okay to make use of Google for health questions when you use a credible supply and if it prompts you to go to your doctor should you could have considerations. Without limiting the generality of the foregoing, the Author makes no representations or warranties with respect to any Information offered or offered within or via the Site relating to treatment of medical circumstances, motion, or software of treatment.
“When sufferers convey themselves into the ED, they are seen in about 5 minutes by a qualified registered nurse and, on common, are seen by a supplier within 30 minutes of arrival,” Thomas mentioned in a press release.
From 2012 to 2017, the variety of emergency room encounters in Fresno County elevated by nearly ninety five,000, or 37%. At Fresno’s Community Regional Medical Center, about 9% of ER encounters ended with a patient leaving too quickly, greater than 3 times the statewide fee.
If no success, contact the police non-emergently to aid in finding the affected person. In this situation, the patient has not but interacted with a doctor. There isn't much to do here as long as the provider by no means met the patient, if so, they might be in a different category.
There are no known instances the place the ED, or ED Providers, have been sued and located to be at fault or responsible for an end result. We recognized people ages with International Classification of Diseases, 9thRevision prognosis codes for infective endocarditis within the National Inpatient Sample, a representative pattern of United States hospitalizations from January 2010 to September 2015.
We plotted unadjusted quarter-year developments for AMA discharges and used multivariable logistic regression to establish elements associated with AMA discharge among IE hospitalizations, evaluating IDU-IE to non-IDU-IE.
The police were notified, and the patient was taken from jail back to the hospital. At the hospital, he was monitored for a number of hours and then taken to surgical procedure where the depressed fracture fragments have been elevated. However, Mr G ended up suffering a brain injury from the fracture which affected his cognitive talents, and which prevented him from with the ability to hold down a job. The police knowledgeable Dr M that the patient, a 24-yr old named Mr G, had been the perpetrator of an assault and in the process was hit within the head with a blunt object by a bystander.
The police had been called, and found him mendacity on the street, clearly intoxicated and with a bloodied head. They took him to the ED, however Mr G was uncooperative and initially refused any treatment. When most individuals hear these words, they're whispered by an overcoated stranger on the bus or a counterfeit Prada peddler gesturing towards the trunk of a car.
1 note
·
View note
Text
WELCOME!!!!
March 17, 2020
Hiiii!!!! My name is Geena. I am 25 years old and I have chronic ulcerative colitis. You all are probably like cool Geena, now why do I care? This is not a blog for you to care or any of that, but if you do, you are an amazing soul already! With this COVID-19 madness,and toilet paper mania, I have decided it is best for me to channel my quarantined energy into informing you young citizens on a chronic illness that I suffer from. They say Shakespeare came out with some great stuff during the plague in his years, so let’s see if we come close!!!
Well, enough with the formal stuff. First things first, I am very goofy!! I will make corny jokes that you guys will not understand! So be ware!!! With that being said, I think I shall call you guys my little assholes *muhahahaha*!!! If you know a little bit about colitis, you will understand that oh so funny joke! If not, welcome and you will be schooled. To make everyone comfortable, I shall introduce myself to you assholes!!!
I said my name so I shall not repeat! And if you already forgot it, get your sherlock holmes on and go search for it again! Anyways, my ADD/ADHD is wanting to creep in!! But we shall stay focused. Anyways, I have been an athlete my whole life, (since three years old)! I also have been Mexican and Puerto Rican my whole life, so you know food is very important in our cultures! I have dealt with stress of sport and home and perfectionism all my life! It was in 2016 that I started to get very sick!! Alright assholes, because I know some of you are going to snooze soon exactly what happened. I can not deny my dramatics but I shall remind you that these are all factual symptoms one does endure. One of my first memories of excruciating pain was when I was hanging out with someone very special to me (intro later to my peeps, sit still and just sip your tea and shut it) when I began to be tumbled over in pain on the bed!! I immediately thought I was going to pass out!!! Now, let's backtrack a little, I have had two major knee surgeries, broken hand surgery, and now after diagnosis, survived 4 colonoscopies (Idk if that is spelled right but we are not here for a spelling bee). With that being illustrated in your guy's head, I want you to understand, it takes A LOT for me to be crying in pain!!! So now after I get up and try and go to the restroom, I see blood in my poop!!! Yup!!! I swear a little gremlin went inside me and committed murder!! I warned you about my ADD/ADHD so stop acting surprised assholes!! To continue with this story, I denied anything being wrong, because well that is just me :))))))))) I also hate doctors, and talking publicly to people unless its for food (sometimes), because I mean FOOD!!!! But then again, PEOPLE!!!!! (SCARY))) Anyways, it was not until after I saw my very special Titi (Aunt), that I realized yeah…. I’m in some deep shit (that is a joke, so laugh or leave)!!!
After getting back home, visiting my GI, and coming to accepting the fact I may have colitis, I underwent my first, terrible colonoscopy at 21 years old…!!! Let me just say, you definitely should never wish a colonoscopy or colonoscopy prep on even your worst enemy!!! Let’s just not!!!
Now, I think that is enough for my personal introduction to the topic! I want to before getting into any craziness of the topic, say thank you’s. There is nothing in life that we do one our own. I have learned that through many experiences in my life. So to close the first entry of our inauguration, I shall thank people that should be thanked. I will not name people explicitly, for confidential reasons and because I am doing this on a whim. I am going to give them nicknames, that they will surely know!
First off, I got to thank my GI and the monthly visits and his rapid responses to my emails, especially whenever I am losing my mind and my butt! Without his calmness, I would be a case on Law and Order!
Next, of course, my family! Titi and my mom, dad, and siblings, have given me tough love at times for my baby ways, but their endless support and understanding have helped me stay healthy.
Lastly, but not least at all… a very special home and person to me,
“Lil boy”, “peter pan”!!! The very first person I confided anything in, the first person to get on my shit (a joke, but actually), help with my medicine, and the person that helped me change my ways, all around! There are not enough thanks or love to give and share...but if there was an award (I can go for days but this nickname will be mentioned in a lot of stories, just know I am more than grateful), haha you would get it! Always, always, past dirt and earth.
I will close our first blog by allowing any anonymous or un-anonymous questions or proposals of stories or suggestions! I have very funny dramatic stories to tell!! Just ask! I also have very honest stories to tell! At the end of the day, I want to make other people comfortable with acknowledging that they have a digestive issue. I want people to feel they are heard. If you know me personally, you know this is very hard for me to tell publicly, but I think it is time for me to put the shyness behind me, and help people, if not just ONE!! If you have personal questions, on my weight or what I have done to change or anything literally, I will share! I will post the blogs on my Snapchat and if you have any friends or family or know someone who could benefit just from these human and natural processes through my stories...please share!!
Till we have more shit to talk about assholes… SEE YOU SOON!!!! :)
1 note
·
View note
Text
When Shit Got Real - My Journey to Digestive Disease Diagnoses

Greetings everyone! C Here :]
One of the reasons that S and I decided to create this blog is that we both struggle with chronic health conditions. I thought a good place to start would be talking about my journey of how I got diagnosed. In May of 2016, I graduated from my clinical social work master’s program. The previous 2 years had been among some of the most stress-inducing years of my life and I have a feeling that the life stressors, along with genetic predispositions, were significant catalysts to my diagnoses.
I had grown up in the Upper Peninsula of Michigan (s/o to all da Yoopers reading this) and in order to pursue my dreams of attending graduate school to become a mental health provider, I had to move away from my family, friends, and the place that I had always called home.
*Enter huge stress catalyst number 1*
A few weeks before I was scheduled to leave for graduate school, I started to experience some major anxiety about moving so far away from my family and friends and attending school (thanks to the semester that I had taken off). I wasn’t experiencing full blown panic attacks, but my episodes of racing thoughts, rapid heart rate, and shortness of breath were enough to make me ask my primary care provider for anxiety medication. Thank the universe that she was a Doctor of Osteopathic Medicine (DO) and encouraged me to try more holistic ways to manage my anxiety such as going for walks, staying active, and seeking out help from natural supports.
Fast forward to finding an apartment, completing the 400 mile move, and entering graduate school. The first few weeks were pretty difficult, but eventually I made friends and began to somewhat relax. The academic and scheduling demands of grad school were constant and I was experiencing a baseline level of stress at all times (juggling classes, homework, reading, my internship, and a side job). Not to mention, I also pushed myself out of my comfort zone to study abroad in Europe for 2 weeks during the summer between my first and second year. Don’t get me wrong, I was having a blast and the busyness of my new life was exhilarating. But, I was putting my body under months and months of ongoing stress without pause.
Grad school seemed to fly by and before I knew it, it was May of 2016 and I graduated with a 4.0. You guessed it – I’m Type A and a self-proclaimed perfectionist (I’m including my GPA here to illustrate the level of chronic stress that I was experiencing – if you’re a control freak like me, you know this type of stress). A few weeks after graduation, I continued to work my student assistant job as I looked for a job in social work. I was also on the hunt for a rural location so that I could get more assistance with my student loans. Seven applications later and I had gotten a call back from a Community Mental Health agency requesting to schedule an interview.
A few days after the interview, I received a phone call stating that I had landed the job! Praise be! I was so excited that thinking about the stress of finding a new place to live and the 2- hour commute hadn’t even occurred to me. It turns out that they were short-staffed (big surprise in social work, I know) and wanted me to start right away. So, I gave a 2 week notice at my other job and began looking for a place to live. I started working a few days a week at my new job (since commuting 2 hours a day, 5 days a week is enough to make anyone go mad), and was able to able to find a place that was halfway in between my boyfriend’s job and mine. About a week after my boyfriend and I had signed the lease, he was given another work assignment and he would no longer be working at this site – he was now going to be assigned a traveling job where he would have to visit sites all over the country. So here I was. Stuck in a 1-year lease in a town with no friends or family and facing the cold, hard reality of a long distance relationship. Well, shit. I was now going to be separated from my best friend who I had lived with since I was 17 years old.
*Cue mental breakdown*
I tried to stay positive and began my new job with my typical enthusiastic, bright personality. However, your first job as a social worker, fresh out of graduate school, is anything but bright. Don’t get me wrong! I gained some invaluable experience and met the most phenomenal people. But, I’d be lying if I didn’t admit that it was confusing, stressful, and straight up terrifying.
*Enter gut health spiral*
A few weeks into my job, I started noticing some changes in my digestion. If you feel uncomfortable with females talking about their bowel movements, then you may want to stop reading here. Seriously - there’s gonna be a lot of poop talk. As a kid, I’ve always been a 3,4,5 times a day pooper (where’s the poop emoji on this thing?!). My bowel movements always seemed “healthy” and I never had any trouble going. So, it was very strange to me that I was starting to experience constipation.
Huh, that’s odd, I thought.
Too busy to think much of it, I “just kept swimming” with my fast-paced life. After a few weeks of on and off constipation, I started noticing that I had blood in my stools.
Woah. That’s not right.
My mind immediately thought of my older sister. She had been diagnosed with Crohn’s Disease within the last 2 years. My first cousin had also recently been diagnosed with Crohn’s after a major hospitalization and the removal of some of her colon. Naturally, I began to panic. I immediately thought I must have it too and texted my sister. She texted back a few minutes
later –
“You need to go get a colonoscopy.”
So, I went about finding a primary care doctor as I had barely been moved to the area for a month and hadn’t been established with anyone yet. The provider I found was nice enough, but she totally dismissed my concerns as some mild constipation and potential hemorrhoids. I requested that she refer me to a gastroenterologist for a colonoscopy and instead she sent me to a colorectal surgeon.
*eye roll*
Looking back, I wish I would have advocated further for myself. This provider was clearly dismissing my concerns and referring me to a surgeon would get me off of her back. She expected him to examine me and find that nothing was wrong. No, I’m not making a judgment. The next time she saw me I had already been diagnosed and she was genuinely surprised. I should have trusted my gut (see what I did there ;]) and pushed for a colonoscopy right away.
At this next appointment, the provider (who, mind you, was a dude) performed a Sigmoidoscopy. This means that he put a long tube with a camera attached to it up my butt (WHILE I WAS AWAKE) and promptly told me that he was seeing inflammation and I needed a colonoscopy.
NO FUCKING SHIT.
So, after spending an uncomfortable $40 at this appointment, he referred me to a gastroenterologist and said that there’s a potential that I have Ulcerative Colitis. Phew. Anything was better than a Crohn’s diagnosis. Since I had that appointment with the surgeon, I was able to skip right to a colonoscopy without a GI consult prior. I had to call my boyfriend (who was currently across the country in Utah) and ask if he could fly home for a few days to drive me to and from the appointment. Being the supportive angel that he is, he agreed to come home and a few weeks later I had my first colonoscopy.
My new GI doc - a pretty, blonde, and particularly cold woman, explained that she couldn’t figure out if I had Crohn’s or not. Basically, the inflammation in my colon that was causing the bleeding and constipation was so far up in my tract that they needed to try an Esophagogastroduodenoscopy (EGD). Aka go in the other way. She prescribed a mild steroid to help control the inflammation while they tried to figure out exactly what was going on. Thankfully, my boyfriend was home for a week, so I was able to schedule the EGD while he was home. Another round of prep (aka pooping my brains out), another 2 days off of work, and a procedure later and they STILL couldn’t definitively diagnose me with Crohn’s.
So, another procedure was recommended.
“We’ll need to complete a Capsule Endoscopy.”
Aka swallow a giant horse pill that is actually a camera and it takes pictures of your insides while it moves through your digestive tract. Am I actually in an episode of the Magic School Bus? Another day of prep and another day taken off of work to walk around with a giant fanny pack (and not the cute kind) of wires taking pictures of my insides.
Finally, here I sit in an exam room at my new GI’s office - four months later. Anxiously waiting at my GI doctor’s office for her to come in and inform me of the results of the plethora of testing that I had undergone. It had been 6 months since I first noticed the blood in my stool. Six months of labs, procedures, and office visits. If there was ever a drum roll moment, this was it.
My GI doc walked in, greeted me, and said, “Well, it looks like you have Crohn’s.” My heart stopped and ironically, my stomach dropped. Watching my sister endure the complicated symptoms of her Crohn’s over the last 2 years did not give me a hopeful look into my future. She had told me horror stories of having to poop in the woods while on a run because she just couldn’t hold it any longer, extreme fatigue that caused her to feel like she needs 12+ hours of sleep per night, and stomach cramping that was so unbearable it caused her to double over.
I wanted to cry, but I didn’t (see earlier reference to my doctor being cold AF). We discussed treatment options, she prescribed medications, and told me to “eat bland foods like bread, grilled cheese, and rice,” and sent me on my way. I got into my car after the appointment, called my boyfriend, and immediately broke down. The way I saw it, a Crohn’s diagnosis was a “see you later” to my former, happier existence. I couldn’t believe that this was my reality. My next call was to my sister, who I appreciate beyond belief. Because she knew the heartache that I was experiencing at that exact moment.
Okay, pity party over – flash to present day. I’ve now been living with Crohn’s, Irritable Bowel Syndrome (IBS), and Inflammatory Bowel Disease (IBD) for 3 years. Surprisingly, I am doing pretty well. My health isn’t perfect, but I’ve come a long way from 2016. If I’ve kept you entertained this far, I’d like to share more of my journey on how I’ve made my way to this healthier place in my next blog post.
As much as I felt like my diagnoses were a death sentence – I can now see that they were just a beginning to a new chapter in my life. This new chapter includes becoming more aware, mindful, and attuned to my body. In my upcoming blog posts, I’ll share how I have been able to improve my self-care, nutrition, and lifestyle in an effort to lead a more fulfilling, aligned life.
#crohn's problems#crohn's#crohn's disease#ibd#diagnostic#chronic disease#procedures#gi#ibs#inflammatory bowel disease
4 notes
·
View notes
Text
Seven Long Years
I delt with an undiagnosed crippling chronic illness. For most of my life, I had chronic vomiting as a child, but when I turned 14 things took a dramatic turn for the worst. I grew dizzy, I was in pain constantly, I could barely keep food down and when I did I was bedridden for days.
Moving made everything worse. I was basically immobalized. I would have to make choices between eating and on improtant days going to school. Which usually I was only able to tolerate for a MAX of 3 or so hours. I did most of my school work from home. In my bed. Staring out my window and watching my neighbors kids my age enjoy life. I lost most of my friends. On average I was vomiting close to 40 or 50 times a day. The muscle aches from it hurt more then you can imagine. Not to mention the dehydration.
I convinced myself tea was a meal. And lettuce was enough to sustain a person. I could no longer eat what most could. My family did not take my seriously for a long time.
I would research tips for maintaining weight and did my best to keep my weight even.
The doctors visits were horrible. Always told it was stress, or anxiety, or they had to test if I was pregnant, or I was making it up for attention and to get out of class. I lost all trust in medical professionals. Ultra sounds, emergency room visits, xrays, colonoscopys, endoscopies, mri's, being admitted to a children's hospital for nearly two weeks. All with no answers, and no help, and no successful treatments.
Then when I was 16, it got worse. The fainting started, the confusion began, the losing track of things and being able to keep up with minor tasks like remembering the code to the lock for my house. Phone numbers, addresses, chores, conversations began to disappear and wouldn't come back for hours. I was extremely sensitive to light, and could not be in anywhere with florescent lights without becoming violently ill.
And the numbness in my legs, and my arms. It was all horrific and shocking. Motion sickness from turning to quickly. What was already hard to live with became even worse. And slowly it drained my will to live. The depression with it was the worse. I grew to become social phobic, and was diagnosed with both chronic depression, social anxiety, social phobia, generalized anxiety disorder, and had to attempt to attend therapy.
But as things got worse, so did my grades. And I ended up just barely passing highschool.
Now, I am nineteen, and a little over a month ago, I saw a neurologist for the first time. Coming on seven years of being crippled by an undiagnosed illness. I got a new bottle of pills and with some hope I began taking them.
And my world has changed. A diagnosis. Which should not have taken so long to get, with how simple it is. I am now living with my roommates, working a job, supporting my furbaby all on my own.
So what was my magical diagnosis?
Migraines. Or more so aura migraines. Silent Migraines. Migraines without the pain but all other symptoms of horrific migraines. I am now on medication for chronic migraines, and I have bottles of pills for the days when I still get sick and the migraines still come. Things to control the vomiting and pain, coping mechanisms for the dizziness, confusion and numbness.
And I know a month isn't a long time. But heres to hoping this is the diagnosis that saves me from a life of watching from windows.
#chronic migraine#chronic illness#diagnosis#vomiting#numbness#pain#chronically ill#fatigue#confusion#light sensitively
1 note
·
View note
Photo

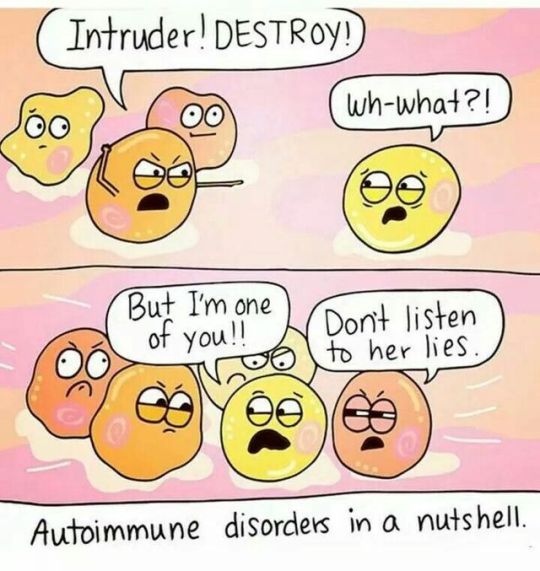
‘In Lockdown’
‘It’s Shingles’ she confirmed in a brusque manner, pulled down my top and then strolled back to her laptop. I inaudibly groaned. ‘I have a compromised immune system’ I squeaked at her, cursing the fact that again my unco-operative and hyperactive body had got too feisty with itself for its own good. She eyed me suspiciously over her glasses and, with all the bedside manner of a bath sponge retorted with a snort, ‘We don’t treat Shingles anymore’. I tried explaining through crossed eyeballs and gritted teeth that I had a chronic health condition and as a result my immune system basically beats itself up and everything else around it on a daily basis, and she again repeated her last sentence, thanked me for coming and ushered me out of the door. I sighed and shuffled out of the door, defeated. Couldn’t have been a cold? A stubbed toe? fungus? But no.... Shingles?! Marvellous.
The last time I had shingles, was two years ago, down my right arm. It made it impossible to grip anything, lift my arm and pretty much ravaged my body for 2 solid weeks and was so painful; I could have quite cheerfully gnawed my own arm off to stop the pain. So I was absolutely thrilled that I was about to go through the experience again. This time the rash was left of my spine, which meant I was looking forward to 10 days of pretty much avoiding all contact with surfaces, backs of settees, taking showers where I would have to wash only half my body, desperately trying to twist myself into some horrible pretzel shape as with bulging eyes, sweaty face and with grinding teeth, try to fold myself in half in order to avoid any water on my back, having to practically levitate or hang from the ceiling like a bat, to try and get some sleep and spend the whole week walking like a crab because I knew I wouldn’t be able to stand up straight. How wonderfully attractive! I am sure my husband was thrilled that he was shortly going to be sharing a living space with a sweaty, irate, scuttling rash covered zombie where he would have to handle me using tongs, whilst wearing a surgical mask. All my plans went to hell as from past experience, I was pretty sure I was going to have to become a hermit whilst I got over it, which meant a week of enduring a week of bloodshot eyes, hair on end, isolation, loneliness and pain. On top of the isolation, pain, discomfort, lack of sleep I was already facing with IBD.
That’s the thing they don’t cover in the ‘this is what you have to deal with when you have Colitis’ guide for dummies. As well as dealing with the annoyance of symptoms like diarrhoea, constipation, and stomach pain, they fail to mention about the rubbishness of chronic fatigue, joints that feel you have mistaken your own for a rheumatic 80 year olds joints, and a brain that feels like you have set yours to maximum speed spin cycle where every day is like you are staring in your very own episode of sesame street.. Today will be brought to you by the letter.... S, T,9, 77, ball, House, crumbs???? and by the number...... 1,4,9,12, Twelfty 7..... house, ball crumbs, testicle.... etc. It makes for very confusing and alarming sentence structure and more than a few raised eyebrows when trying to converse in public. It doesn’t tell you that because Colitis is at its heart an auto immune condition and so now, every day and night is fight night. ‘Let’s get ready to RUMBLE!!!!! Introducing you in the red corner, fighting well .... also..... you, in the blue corner’. Confusing right?
But the very worst thing about Colitis, specifically the strain I have which Is Microscopic - Lymphocytic Colitis, (worth 85 points and a triple word score in scrabble) is that not even the professionals have a clue about it. There is so little information about it, especially here in the UK, it’s often misdiagnosed as something else, and the only way it is diagnosed is by biopsy under colonoscopy, which is something you have to beg plead, whine, grovel and cry for, So even though it says very clearly in my medical history that I have MC, the DR who diagnosed the shingles, probably would have had very little knowledge about it because as well as being classed as an invisible illness, it is also completely invisible in the pod of IBD diagnosis. If I said I had any other disease in the IBD family, you would have probably heard of it. Crohns, Ulcerative Colitis are known. Both are devastating. Both are classed as really challenging conditions and also in severe cases classed as a Disability. MC (Microscopic colitis) no one has a clue about. Microscopic makes it sound small and insignificant doesn’t it? Well after living with it for 8 months, It’s not small and its certainly not insignificant. In fact I can state with absolute confidence that it is completely devastating, confusing, maddening, upsetting and every other emotion you would associate with living with any other Long term Chronic disease. There are pages and pages and pages of information about IBD, but it makes me both sad and angry that there isn’t the same kind of profile, support, knowledge or help available for those of us that have MC, making living with it, understanding it and conquering it very sodding difficult.
At the beginning of my journey with MC, I wasn’t informed that I was sharing my body with an autoimmune disease. I had no idea that I would be spending all of my time trying to cajole a hyperactive immune system to stop spinning round in circles, calm down and take a nap. I had no clue, that there were going to be days where I would be in so much pain, I would learn creative new swear words that I would shout into a pillow, while I curl up in a ball, trying to get into any comfortable position that wasn’t hanging from the ceiling by my ankles and taking on the form of a bat. I didn’t know that I would be met with ‘questioning stares and raised eyebrows’ and helpful conversation starters like‘ You don’t look ill’ or ‘ oh well at least you know what’s going on now, just change your diet and everything will be fine’ and certainly not that there would be days I would feel so tired, it would feel like my brain was being submerged under water and I would start imagining people as giant, walking pillows, that I could happily snooze on whether they gave me permission or not. I was ignorant to the fact I would have to give up cake, cheese and all the yummy things I used to love because, by eating them I was turning my bowel into an angry, spiky porcupine, stabbing anything it touched with care free abandonment. Because these are the things they don’t tell you. They just tell you about the joyful toilet troubles. But I promise you. It’s not just that we have to deal with, we deal with a whole cacophony of bloody wonderment, and I wish that every time we had to discuss our disease, the whole process didn’t feel like we have to become a desperate salesmen, but instead of trying to persuade someone to buy a car, we are trying to get help or intervention to give us the best chance to exist harmoniously with this disease.
So, yet again I am enjoying an unwelcome tenant living in my body without paying rent. Yet again I am having to over explain my condition to a professional to try and get any form of treatment for a related autoimmune condition, and yet again I am having to shield myself from the world whilst this butt hole of an illness works its way out of my system. And then after all that fun, go back to dealing with the IBD until another squatter of an illness uses my body as its own personal cave, dwelling there until my body musters up the energy and enthusiasm to squeeze it out again. There’s no room for anything else and I truly worry if something else moves in whilst I am trying to recover from Shingles, I might spontaneously combust. But hey, maybe if I use a dust buster to hoover myself up and present myself as a little pile of dust with eyeballs and shoes in front of the DR, maybe just maybe, she will read my notes, understand my condition, actually show some sympathy and take me seriously instead of hoofing me out of the door. Well We live in hope eh?
1 note
·
View note
Text
Aeisha’s PI Story

My story began just before my 30th when I was planning my big birthday party. I was experiencing strange bloating symptoms where my stomach would go from flat and toned to large and distended for no reason at all. It wasn't triggered by food or anything, just spontaneous bloating. I generally stay fit and lean, so looking like I was 6 months pregnant was an issue for me, especially because my clothes were no longer fitting. It took me many visits to many doctors for them to tell me "it's just hormonal" and "it's no big deal", but I KNEW something was wrong. I know they thought I was just some crazy person coming to their office, but I had to find the answers to my issues.
After visiting primary care doctors and gynecologists who decided they couldn't find anything wrong, I went to a gastroenterologist. Upon seeing him, I broke down in tears letting him know that I wasn't crazy, that I have a great and fulfilling life, that I am not here for attention, but HE NEEDED to take me seriously. After months of tests and consulting with him about my own research and tests I wanted him to perform, we finally did an endoscopy and colonoscopy.

The first thing this doctor said to me was, "You are NOT crazy" since my results showed that my intestines expressed nodular lymphoid hyperplasia (NLH) which simply means they are lined with lumps which prohibits proper absorption of fats and nutrients as well. Though the NLH was seen, no one knew the reason for its existence. It took one of his colleagues to remember seeing this is in a medical book in medical school for him to remember it was linked to a type of blood deficiency.
From there I was sent to get my immunoglobulin levels checked (and a lot of other blood tests) and that is when it was noticed that my IgG and IgM levels presented just outside of the normal range, but my IgA was non-detectable. I was then sent to one of the few specialists in the United States to Mt. Sinai hospital in NY for diagnosis of my condition. She diagnosed me in 2010 with a "Selective IgA Deficiency" and for the next 10 years I managed my gastrointestinal issues by eating clean and removing processed foods. She mentioned that my condition could progress to CVID if my other immunoglobulin levels continue to decline and that I'd have to monitor them over the coming years.
In late 2019, I started to experience spontaneous weight gain in the abdominal area, though I was working out 5 days per week. I was gaining weight so fast that it was uncomfortable to eat or sit up in a chair and breathe. Additionally, I started having strange skin infections on my face and chest. Physically, I felt extremely fatigued and had hardly any energy past 12 noon every day. As someone who works full-time and lives a pretty active life, it was torture. I was too tired to do my normal tasks, I felt awful, and I looked terrible.
I decided to reach out to my gastroenterologist because it had been years since I saw him and I wanted to let him know of the newest issues. My food was no longer digesting, so days of food would sit without leaving my body along with the weight gain and fatigue. He repeated the immunoglobulin tests and repeated the endoscopy and colonoscopy. When my tests came back, the NLH still presented, but all my immunoglobulin levels were drastically low. In addition to treating the gastrointestinal issues, he advised me to find an immunologist who could focus on my condition and decide on my next course of action.
There are very few physicians who are familiar with immunoglobulin issues or physicians who are willing to take on patients with those issues, however, I was lucky enough to find one who was motivated to do extensive research and work with me on finding out what to do. I shared with her my medical files from all the previous years and equipped her with tests and lab results from all my physicians to get her started.
After months of seeing her and doing various tests, she confirmed my diagnosis of CVID and recommended I started immunoglobulin therapy. I went on Instagram and started talking to a few patients who have been using immunoglobulin therapy for CVID and knew what questions to ask her about treatment and the experience overall. Though she seemed sad to break the news, I was ecstatic to know there were options to explore. She set me up with the medication she felt was best for me and the nurses started training me at home in August 2021.

“It has been 7 months since my first infusion and I couldn't be happier with the progress of my treatment and the ease of the pump to do my infusions.”
I quickly learned how to inject my needles and get my infusion going by myself. After the first visit, I was able to do all the steps myself with the nurse on standby for assistance if needed. The first month or so was a bit rough since the infusions seemed to wipe out my energy completely, so when I infused on Thursday, I was in bed the entire weekend in recovery. But after that, I started to feel like Superwoman after my injections. My energy was back and I felt like a brand new me! It has been 7 months since my first infusion and I couldn't be happier with the progress of my treatment and the ease of the pump to do my infusions. Though I still have gastrointestinal issues, I do have more than enough energy to work and workout at the pace that I am used to. I feel as though my quality of life has been restored and I look forward to better days ahead!
- Aeisha W. - CVID Patient
0 notes
Text
Why Do I Need A Gluten Free Diet Regimen?
You've simply listened to the news from your physician. Or perhaps you have actually come to the final thought on your own, perhaps after clashing medical tests and also your unending checklist of signs. Still, this is the moment of truth - you're starting a gluten cost-free diet plan. The kicker is you have no concept what you're doing. Going low-fat? Lower pizza as well as infant back ribs. Going reduced salt? Throw away the salt shaker. Going gluten complimentary? Hmm ... can you repeat the inquiry? That's just how our household was when my husband needed to start a gluten totally free diet. We slightly understood what gluten was, we knew just how unpleasant he felt, yet we didn't have any kind of idea how they were connected. And also when we heard the information, then what? Was this remarkable change really required, as well as would certainly I have to toss out everything in my cooking area to make it occur? It was an obstacle initially, yet we endured it. Let me walk you via the fundamentals of what gluten is, where it hides, what your gastric or gluten level of sensitivity signs and symptoms may resemble, and just how gluten can actually hurt someone who needs to prevent it.
Gluten Free Flour What Is This Gluten Things Anyhow? The initial few weeks of grocery purchasing after my other half's diagnosis were disorienting as well as stressful. Gluten - truly? If it jumped off the active ingredient label and also strike me in the nose, would I recognize it was gluten? Label-reading can be tough because gluten originates from a handful of different grains and also is made right into a million various ingredients not labeled as "this looks a great deal like gluten." It's a healthy protein discovered in wheat, barley, as well as rye. Working bread dough turns on the gluten healthy protein, producing a strong however flexible framework for the bread. Oats do not practically consist of gluten, however it is so typically grown up and also processed near wheat areas that the threat of cross-contamination is respectable. Supposed "tidy" oats are expanded as well as processed in isolated fields, with devoted devices, as well as with constant screening to remove this contamination danger. I Had No Concept Gluten Could Be Because OK, so you ditch the bread, pasta, donuts, and also pizza crust, which huge bag of flour on the back rack. That'll do it, right? Well, it's an excellent beginning, however it's inadequate. A gluten totally free diet plan goes way beyond the noticeable resources. You'll need to split out your reading glasses and get relaxing with food labels from now on. Gluten can be located in malt flavoring (oh no - examine almost any type of mainstream cereal box), "natural flavoring" (one of those nebulous components near the end of many labels), and arbitrary incidents of wheat flour (like some potato chips or nut blends). See what I mean? It's a lot like detecting Waldo in among those books, other than that Waldo often moves around and also alters his t-shirt without telling you. Feeling Sick In A Hundred Different Ways Did you hear something concerning "contamination"? Yes, you did. For some individuals, gluten is basically a poisonous substance. It is to be stayed clear of entirely and continually. Or else, they risk awkward symptoms and potential physical harm. Gluten sensitivity and celiac disease can share very comparable symptoms. However according to current study just gastric condition shows evidence of true intestinal tract damage. These signs can include looseness of the bowels, stomach aches, significant or unexpected weight-loss, a "clouded mind" feeling, headaches, basic fatigue, abdominal discomfort, bloating, joint pain, one more medical condition appearing worse or falling short to boost, depression, irritability, muscular tissue aches, mouth sores as well as other dental troubles. Children may have stunted growth, "failing to prosper", or might show up sickly as well as have a few of the other symptoms defined above. Some have actually found that behavioral troubles and also autism have been linked to celiac illness as well as gluten level of sensitivity. While this is rather debatable and also is not yet definitive, a lot more specialists continue to consider the connections.
Doves Farm Flour The list of possible symptoms is a lengthy as well as winding road, and completion outcome for every individual does not always mean something evident like, "Hey, I have a trouble with gluten!" Some have extremely few, if any type of apparent signs and symptoms, and it's just verified when they get a colonoscopy (often due to a few other recurring clinical treatment or analysis). Others have a vast array of signs and symptoms regularly. You may notice that not every one of the signs and symptoms are digestive system in nature. The key point to remember is that an individual with real unattended gastric condition is likewise experiencing malabsorption of nutrients from their food. Food is available in, yet their body can not get much from it. With time, these symptoms or modifications establish as well as take their toll. Celiac symptoms are typically neglected, misunderstood, abused, overlooked, or lessened for several years before a correct diagnosis is found. As well as who could condemn any person for taking that lengthy to figure it out? With that wide variety of signs, problems might be quickly crossed out as safe problems without link to a bigger picture. It's not reasonable to presume that any kind of arbitrary belly pains or duration of exhaustion is automatically the result of a lifelong medical problem. That sounds over-dramatic, best? When it begins to influence your life in a way you can't neglect, that's generally when the pieces drop with each other. Only when my hubby began shedding a significant quantity of weight did we truly take action to fix the problem. When we obtained the medical diagnosis and looked in the rear-view mirror, we quickly saw the symptoms we 'd misread. Swelling Is A Very Bad Point Here's the largest reason that any person detected with celiac disease absolutely needs to prevent gluten in any way expense - bodily damages from persistent swelling. Bear in mind all that about malabsorption of nutrients? The reason that happens is since gluten triggers an auto-immune reaction in the intestinal tracts, creating a lot of swelling. Generally, the body attacks itself when gluten is about. This unrelenting swelling triggers apparent signs and symptoms like discomfort and pain. It also begins to damage the villi (tiny finger-like projections that line the digestive system) that do all the nutrient absorption. As time goes on, the swelling uses these villi down to a nub. Go into diarrhea, malabsorption, weight-loss, exhaustion, headaches, and basic signs of inadequate nutrition. The good news is, there's a way to restore the gastrointestinal system to its initial function and also structure. It's called ... the gluten totally free diet regimen. Yep, that's it. Now, the total evasion of gluten is the treatment. Medication can occasionally assist the signs and symptoms, or you might require other treatments while recovery up originally. However food is literally your medication once you get a gastric diagnosis. As well as for those wondering about gluten level of sensitivity, you might obtain any of those signs but have no (or really little) proof of damage to your digestive system system. However even so, that wishes to be ill like that at all times? Your body can't operate well if it's frequently reeling from sign episodes and also struggling with inadequate nourishment. Generally, the therapy for any degree of gluten sensitivity is a gluten free diet regimen. Gluten Free Diet Plan - It's Good To Be Healthy and balanced Again The entire goal of a gluten cost-free diet regimen is to assist your body recover as well as keep it healthy. Yes, starting can be complicated and also aggravating. Yes, you will likely miss out on foods you utilized to consume (that's typical and OKAY). Yes, you might have to explain yourself for some time up until people comprehend what you're speaking about. However through all this, you get an invaluable gift - a healthier body for you to utilize and enjoy. If you have other underlying clinical troubles, you might still need to manage those. But opportunities are great you'll handle them much better without all the signs and symptoms, swelling, as well as nutrient malabsorption. It's a new landscape with ups and also downs, however you'll find that you can eat numerous delicious points on a gluten cost-free diet regimen. It's not like you're being told to go survive on the moon (though it might seem like it initially). Every remarkable yummy gluten free food can be located right below on earth.
0 notes
Text
0 notes
Photo


My Story : Steven McCollum and my battle with a Chronic Illness
Why am I cycling 200 kilometres from Dundonald to Dunfanaghy instead of driving? Why am I going to put myself through the ten hours of pain and discomfort of the saddle to help raise money for the gastroenterology unit in the Ulster Hospital?
On 23rd October 2017 as I was being wheeled away to theatre on the hospital bed from the three women in my life, my wife, my mother and mother in law, not knowing if I would see their faces again, the words of Psalm 23 came to mind, “The LORD is my shepherd, I shall not be in want”. As I was pushed through the narrow corridors of the Ulster Hospital I knew my shepherd was leading me and guiding me.
For over eighteen months I was battling a stomach problem, at first not knowing what it was, but as time went on and after numerous blood tests and too many colonoscopies to count, I was diagnosed with Ulcerative Colitis in May 2017. Ulcerative Colitis is a chronic illness that had drained away much joy and happiness in my life. Between March and November 2017 I spent forty four days as an inpatient in the Ulster Hospital, never mind all the day appointments that I had in between.
Although I cannot pin point a start date or the cause of the illness, symptoms began to develop over time. Extreme diarrhoea, abdominal pain and cramping, weight loss and fatigue. At the beginning of 2015 I started to experience symptoms of not being well, so I went to the doctor to get investigations and tests done, but nothing showed up. For 2 years I was able to hide my sickness and persevere through the pain and discomfort without many people knowing apart from my wife Hannah, but things started to go downhill quite quickly at the start of 2017.
The day before my 29th birthday, I headed up to the A&E at the Ulster Hospital to be seen regarding a football injury I got from the weekend before. It had started with a pain in my ankle but then spread up my leg. I lost over a stone in a week, lost my appetite, had extreme fatigue, a really low mood and had no motivation to do anything. If you have ever been at A&E on a Saturday afternoon, you will appreciate how noisy and chaotic it can be, but that day, it didn’t affect me. I was so drained of energy and I lay down and went to sleep on the waiting rooms chairs. I was soon admitted and tests revealed I had 4 clots in my lower leg, clots which were later discovered to be due to severe dehydration caused by the relentless diarrhoea. It wasn’t long after this that I was diagnosed as having an auto-immune disease known as Ulcerative Colitis.
If you have experienced a tummy upset, food poisoning, or the need to rush to a toilet, you will understand a bit of what colitis is. Wherever I went I needed to know where the nearest toilet was, because I wouldn’t know when I would need it. For days upon days, I wouldn’t feel safe enough to leave my own house. I would need the toilet somewhere between 10-20 times a day, sometimes more. For three months, I didn’t have one good night’s sleep, up every hour to go to the toilet, this was draining physically and mentally. With colitis the urgency to go the toilet was unbearable, it came on me so quickly I would need to be at a toilet within a few minutes, sometimes seconds. This along with extreme fatigue made simple daily routine difficult and I ended up having to stop doing the things I enjoyed.
Flare ups could happen at any time or any place, they didn’t discriminate. When I was having an MRI test, I needed to stop the test twice to jump off the machine and go to the toilet.
The joy of driving became difficult. I never knew how a car journey would go, a short 5-minute trip in the car could result in having to pull over. Hannah ended up driving everywhere, because if I needed the toilet on route, I could jump out quickly.
Queues and traffic lights became a source of great anxiety and stress. If the light turned red the stress levels shot up and panic set in as it left me unsure if I would make it to the nearest toilet. On one occasion, Hannah took me to her grandparents for lunch, a 10 minute drive away. A few minutes into the journey the pain started but we were stuck behind a car. There was a queue of traffic behind us so we couldn’t pull in. We phoned her granny to ask her to open the front door so that when we arrived I could go straight in and wouldn’t have to ring the doorbell and wait for it to be opened. Hannah stopped right outside the front door so I could run in. When I came back from the toilet, Hannah was in tears from the stress of those few minutes, from the pressure of having to get me there before it was too late. This illness affected more than just me.
We had booked a holiday for September 2017 however as we started to think about what travelling would involve, the long queues for check-in, for security, for passport control, queues which I couldn’t leave and return to, or how I would cope in an aeroplane with only 4 toilets or on the transfer to the hotel where there were no toilets and potentially a language barrier, we decided to cancel our holiday as the reality of travelling with colitis would be more stressful and would defeat the purpose a holiday.
At the beginning of October, only 5 months after receiving the diagnosis of colitis, I had a meeting with my consultant. She advised that after numerous failed attempts to control my colitis through medical treatment, my body was getting sicker and weaker and that surgery was my only option.
On the morning of the 23rd October as I woke from the little sleep I got, the words of Psalm 118 came to suddenly to mind, “This is the day that the LORD has made, let us rejoice and be glad in it”. As I faced surgery that day, I was given a reassurance that this was God’s will for my life. As I had prayed many a night, I prayed that God would grant me a miracle and heal me from my sickness, but that night, I still had the same symptoms, the same lack of rest but God taught me in that moment as I woke that what was going to happen that day, God had foreplaned and I was to rejoice and be glad in it.
The surgery required the removal of my large intestine which was full of ulcers as there was a fear that it could rupture. It brought changes physically with a stoma which has been hard to adjust to and deal with. I have tried to hide myself and cover myself, trying to be as normal as possible. Having this illness has presented and continues to present so many challenges I never thought I would have to face.
Although this is a small insight into life with a chronic illness, I hope you have a greater understanding of what Ulcerative colitis is and how it affected me. Let me thank everyone who has been a real support to me, especially my wife, who through everything was by my side and my constant through everything.
With all this in mind, I wanted to give something back to the unit who cared for me. My consultant, Dr Addley, was amazing, it felt like she had genuine concern for me, not sugar coating anything and was a real help to Hannah through my sickness. Being in a hospital ward as an inpatient can be long, lonely and tiresome. I want to be able to help other people that are/will be in a similar situation to me, so on the 31st August 2019, I will be cycling 200km to Donegal, to raise money for the gastro unit, and hope the money will be of great help to the staff and the patients now and in the future.
Let me finish with a verse that meant so much to me in my sickness. After a long, sleepless night of pain and discomfort, I would read this verse and knew I would been given the strength each morning to face another day “The steadfast love of the LORD never ceases, his mercies never come to an end, they are new every morning, great is your faithfulness.”
0 notes
Text
ABIM: Oncology
ABIM syllabus can be found here Let me know if you find any errors Sources: UWorld, MKSAP 16/17, Rizk Review Course, Louisville Lectures, Knowmedge (free version)
Lung cancer (clinical presentation and diagnosis)
Small cell: associated with hyponatremia/SIADH, Lambert Eaton (like MG but fatiguable); Tx: chemotherapy + whole brain radiation if good response to chemo Non-small cell: CT/PET, MRI brain –> Tx: stage I - surgical, stage II - surgery + chemo, stage III - chemo + XRT +/- surgery, stage IV - chemotherapy alone (1) Squamous cell carcinoma: associated with smoking, hypercalcemia, Pancoast tumors (cause Horner’s: ptosis, miosis, anhydrosis) (2) Adenocarcinoma: not associated with smoking (3) Large cell carcinoma: associated with SVC syndrome (4) Bronchogenic carcinoma: associated with cluster of painless, firm/hard cutaneous metastases *AE of chest XRT is CAD
Breast Cancer
- Screening: mammogram >50yo or >35 with high risk * if palpable mass: ALWAYS BIOPSY (even if not seen by mammo) * if in situ –> no need for LN biopsy * if positive LN –> axillary LN dissection (AE: UE lymphedema) *if >1cm or LN+: give adjuvant chemo * do NOT perform mastectomy if metastized * if mastectomy, add XRT if: (1) dermal invasion, (2) close margins, (3) 4+ LNs - Dx: mammogram/US –> Bx –> ER/PR/Her2neu status - DCIS Tx: lumpectomy + local rads = simple mastectomy (for tumor >5cm) +/- if ER/PR+ –> 5 years of hormonal therapy (1) premenopausal: Tamoxifen (SERM; AE: clots, endometrial cancer), (2) postmenopausal: Anastrazole/Letrozole (AI) +/- if Her2neu+ –> get an ECHO to ensure good heart function, give Trastuzumab (- LCIS Tx: observe or b/l mastectomy (won’t be tested because controversial)
Neoplasm of the head and neck
Thyroid nodules and thyroid cancer: (1) Medullary thyroid cancer: associated with both MEN II syndromes, RET gene; elevated calcitonin –> hypercalcemia; Tx: surgical neck dissection (2) Papillary thyroid cancer: aggressive, associated with BRAF (like melanoma); Tx: surgery + radioiodine (3) Follicular: Tx: surgery + radioiodine (4) Anaplastic: very poor prognosis
Gastrointestinal or hepatic cancer
Stomach cancer: - Dx: upper endoscopy with ultrasound > CT scan - Tx: surgery, chemo, XRT - MALT lymphoma: Tx: PPI and H.pylori Abx Colorectal cancer: - Tx: stage 1-2: resect, III: resect + chemo, IV: FOLFOX chemo +/- resect + Bevacizumab - f/u with CEA Q3-6mo for 2 years, then Q6months for 3 years - f/u with CT chest/ab/pelvis every year for 3 years - f/u with colonoscopy 1, 3, and 5 years post-treatment - Rectal cancer: Tx stage II-III: (1) chemo/XRT –> surgery or (2) surgery –> chemo Pancreatic carcinoma other than pancreatic endocrine tumors: - Trousseau venous thrombophlebitis (migratory VTEs), jaundice, palpable GB - stage I (pancreas) Tx: resection - stage II (duodenum) - stage III (LN) - stage IV (other mets) Tx: Gemcitabine *confused for autoimmune pancreatitis (because of mass); differentiate with biopsy; AIP has elevated IgG Hepatocellular carcinoma: - associated with Hep C > chronic Hep B - if nodule <1cm needs screening abdominal US Q6mo –> if >1cm: contrast CT/MRI liver (arterial phase enhancement) - if AFP>100, don’t have to biopsy –> Tx: resection / liver transplant > EtOH/radioablation > chemotherapy/Sorafenib Other CT abdomen findings: (1) Cavernous hemangioma: early peripheral nodular enhancement with delay in filling from periphery to center; don’t have to treat (2) Hepatic adenoma: associated with OCPs; early rapid loss of enhancement –> resect (3) Focal nodular hyperplasia: central stellate scar –> don’t have to treat
Urologic cancer
Renal clear cell carcinoma: - presents as upper abdominal mass with hematuria; erythrocytosis (elevated Hb), hypercalcemia, and acute varicocele - associated with von-Hippel Lindau (retinal and cerebellar hemangioblastomas and RCC) - Dx: CT ab, pulmonary “cannonball” nodules/mets on CXR, if bone pain: elevated ALP - Tx: nephrectomy Transitional cell carcinoma: - painless hematuria - Dx: cystoscopy - Tx: TURBT –> intravesicular BCG; if muscle invasion: radical cystectomy Prostate cancer: - Dx: exam with elevated PSA –> transrectal US-guided prostate Bx - Gleason >7, PSA >15, large tumor or bone pain –> bone scan and CT ab/pelvis - penetrates prostate capsule Tx: XRT –> f/u PSA and rectal exam Q6-12mo - LN involvement/mets/elevated serum acid phosphatase Tx: total hormonal ablation with 4-6mo Leuprolide (LHRH agonist to be given with antiandrogen Flutamide to prevent tumor flare)/Goserelin –> refractory: Docetaxel Testicular cancer: (1) Non-seminoma (embryonal, teratoma, choriocarcinoma): elevated AFP, hCG; Dx/Tx: inguinal orchiectomy (DO NOT BIOPSY) +/- chemo if spread (2) Seminoma: elevated hCG; Tx: radiation; if disseminated: platinum-chemo
Gynecologic cancer
Ovarian cancer: - may present with bleeding, dyspareunia, ascites (SAAG <1.1, ascites protein >2.5), peritoneal carcinomatosis - associated with HNPCC, infertility, early menarche, late menopause - Dx: pelvic U/S –> stage with ex-lap - Tx: stage I = surgery; stage II-IV: platinum-based chemo –> follow with pelvic exa, and CA-125 Q2-4mo for 2 years (do NOT need routine US) * if BRCA1 or 2+ –> offer oophorectomy at 35yo or after child-bearing * Dermatomyositis (anti-Jo1) is associated with ovarian cancer –> TVUS Endometrial cancer: - Dx: with biopsy - Tx: surgical resection of cervix/uterus/adnexa + XRT +/- chemotherapy; if high risk surgical patient, XRT only Cervical cancer: - Dx: punch bx or colposcopy bx - stage I Tx: LOOP/conization or if finished babies, hysterectomy WITHOUT dissection - stage II-IV Tx: XRT + cisplatin
CNS tumors
GBM: most common and aggressive adult intraparenchymal tumor - ring-enhancing with central necrosis and hemorrhage Meningioma: most common primary brain tumor (extraparenchymal, extradural) - insidious diffusely enhancing, partially calcified +/- dural tail; Tx: observe or surgery if symptomatic Oligodendroglioma: rare, MRI = non-enhancing homogeneous intraparenchymal lesion Schwannoma: benign nerve sheath tumor ~CNVIII (hearing loss/tinnitus) - MRI shows enhancing lesion at cerebellopontine angle vs. Pseudotumor cerebri: headaches worse in the morning + papilledema and visual changes in an obese person on Accutane - Dx: CT/MRI to r/o tumor and dural venous sinus, LP shows elevated ICP - Tx: Acetazolamide, repeat lumbar puncture –> if progressive visual loss: neurosurgery
Skin cancer
Squamous cell carcinoma: preceded by actinic keratosis Basal cell carcinoma: raised pearlescent with telangiectasia Melanoma: Dx: wide excision + if >1mm deep, sentinel LN biopsy; additionally treat with IFN if >4mm or +LN
Hematologic malignancies (see ABIM: Hematology)
Assorted endocrine tumors and endocrine manifestations of tumors (see ABIM: Endocrine)
Malignancy associated hypercalcemia: (1) squamous cell (2) RCC (3) medullary thyroid cancer (elevated calcitonin)
Oncologic emergencies
SVC Syndrome : associated with large cell NSCLC - Dx: biopsy tissue > mediastinoscopy/thoracotomy - if previously untreated: give chemo - if previously treated: XRT +/- chemo Fever and neutropenia: - Tx: with broad spec Pseudomonal abx (Cefepime) until PMN>500 - if no improvement in 2 days, add Vanc - if no improvement in 5 days, add Itraconazole Spinal cord tumors and compression: - Dx: Gad-enhanced MRI - Tx: steroids, surgery, XRT Cardiac tamponade from neoplastic pericarditis: - JVD, tachycardia, pulsus paradoxus - Tx: pericardiocentesis Tumor lysis syndrome: - elevated uric acid, potassium, phosphate - N/V/D, heart failure, seizures, syncope, death - PPx: Allopurinol, Rasburicase Hypercalcemia - elevated Ca, decreased PTH, normal/decreased Vit D3 and Phos - Tx: NS Hyponatremia (SIADH): - associated with small cell - Tx: fluid restrict or if symptomatic, Na<120: 3% Saline + Lasix
Complications of cancer and its treatment
- give Morphine –> translate it to long-acting forms - Palliative O2 not helpful in absence of hypoxemia - Radiation toxicity: CAD, hypothyroidism, lung disease; breast, lung, esophageal cancer - Toxicity bear (borrowed from my Step 1 notes - Second Aid): –> Asparagine: neurotoxicityCisplatin: ototoxic/nephrotoxic; Tx: Amifostine –> Vincristine/Vinblastine: "Christ my nerves, Blast my bones" - Vincristine = peripheral neuropathy - Vinblastine = myelosuppression –> Bleomycin: pulmonary fibrosis –> Doxorubicin: cardiotoxic; Tx; Dexrozoxane (for cardiotoxicity), Dimethyl-sulphoxide (for ROS ulcers) –> Cyclophosphamide: Acrolein = nephro/bladder toxic (Tx: Mesna); also SIADH effects (Tx: Demeclocycline) –> Methotrexate: nephrotoxic (Tx: Leucovorin), myelosuppression (Tx; Filgrastim)

Cancer of unknown primary
- axillary LN? –> biopsy comes back adenocarcinoma –> mammogram –>if neg: MRI breast - high cervical LN? –> PET/CT scan of head and neck - osteoblastic mets? –> PSA test for prostate adenocarcinoma - ascites, peritoneal carcinomatosis? –> ovarian cancer, Dx: ex-lap - young woman with retroperitoneal poorly differentiated mass? –> germ cell cancer; Tx: platinum chemo
Cancer screening (see ABIM: Screening)
#me#oncology#cancer#hematology#onc#internal medicine#im#abim#medicine#medical#exam#test#studying#notes
7 notes
·
View notes
Text
cancer symptoms after hysterectomy
Did you know it's possible to get ovarian cancer even after you've had a hysterectomy? I learned the hard way. My sister, who had a hysterectomy about 10 years ago, simply received a diagnosis for a type of ovarian cancer.
If you have a partial hysterectomy, which removes your uterus, or a total hysterectomy, which removes your uterus and cervix, your ovaries remain intact and you can still develop ovarian cancer, in agreement with the Mayo Clinic.
If, like my sister, you have a total hysterectomy with salpingo-oophorectomy, in which your cervix, uterus and both ovaries and fallopian tubings are removed, ovarian cancer is less likely but still can occur.
The details are confusing--surgeons talk fast and don't like to slow down for patient explanations--but my sister's surgeon says she has primary serous carcinoma, which glances and behaves much like ovarian cancer and likely originated from ovarian cells.
As he clarified it, when the status of women undergoes a hysterectomy and has her ovaries removed, some ovarian tissue may be left behind. Ovaries are not well-formed organs like our liver or kidneys. They are soft tissues that can( and do) come apart when you try to remove them. When parts are left behind, some cancerous or precancerous cells may develop from that tissue. In some females, the ovarian cells moved to the peritoneal field during menstrual cycle before the ovaries were removed and grew cancerous later on. It's also difficult to tell whether the cancer is coming from ovarian or peritoneum cells--and it doesn't much problem. It is treated the same.
My sister's cancer showed suddenly, without warning. Two weeks ago, she started having severe abdominal anguishes. At first she thought it was a stomach virus or food poisoning. But, after two days of worsening indications, her internist cast her to the emergency room. The ER doctor wanted to send her residence with a stool softener, but my sister, being the strong-willed maiden that she is, refused to leave.
When a doctor analyse her the next morning, he found a mass on her colon and are determined to do an emergency colonoscopy. But, the mass was pulping down so difficult on her colon that he couldn't do a colonoscopy. The procedure unexpectedly became disaster removal of her entire colon because the mass had pinched off the tissue and killed it.
Once the surgeon came inside her abdominal cavity, he detected cancer cells throughout her abdomen. As he described them, they were sticky blob of cells that were gluing her organs together. He removed what he had been able to in what was becoming a lengthy and complex disaster surgery.
He was not sure she'd pull round the surgery, but, thankfully, she did. We're still going explanations and are a long way from triumphing the battle against cancer. But we're extremely glad that she's lived to fight it.
I've learned a great deal about ovarian cancer in the past few weeks, and the most important thing I've learned is that it's very important to get an early diagnosis--but there's no screening research for women at norm peril for ovarian cancer.
There are determining factor that would encourage your health care provider( HCP) to be more vigilant in go looking for ovarian cancer, so know your risk factors--and let your HCP know if you have any.
These are risk factors for ovarian cancer:
A "first-degree" relative( mom, sister or daughter) who has or had ovarian, tit or gastrointestinal/ colon cancer
Age; most cases occur in brides 60 and older
Eastern European Jewish ethnicity( Ashkenazi )
Mutation in the BRCA1 or BRCA2 gene
Personal history of heart, endometrial/ uterine or colorectal( colon) cancer
Have never been pregnant or had agitate giving birth
A high-fat diet
Obesity
Endometriosis
Early start for your points( before senility 12) or later-than-average menopause( after age 50 )
Of all determining factor, the most important ones is a family history of breast and/ or ovarian cancer. However, it's important to keep determining factor in perspective. Most women around risk factors for ovarian cancer will never get ovarian cancer. And most women with ovarian cancer is not have any strong determining factor for the disease.
The Ovarian cancer symptoms ( in particular in its early stage) are often not self-evident or intense, but if you have known determining factor, you should definitely talk to your HCP if you show any indications. Ovarian cancer symptoms include:
Pelvic or abdominal anguish, pressing or awkwardnes
Vague but lingering gastrointestinal worrieds such as gas, nausea and indigestion
Frequency and/ or urgency of urination in is a lack of new infections
Changes in bowel habits
Weight gain or loss; specially weight gain in the abdominal place
Pelvic or abdominal grow, bloating or a sense of fullness
Back or leg anguish
Pain during intercourse
Vaginal bleed or abnormal vaginal removal
Ongoing fatigue
If you or your HCP accuseds you may have ovarian cancer, or you have a very high risk of developing it, you may undergo certain diagnostic tests, including likeness tests, biopsy and blood tests.
Your HCP may require a blood assessment that are searching for CA-125, a protein found in the blood of countless women with ovarian cancer. Nonetheless, other conditions, including normal ovulation, endometriosis and pelvic inflammatory disease can also heighten CA-125 positions. And some women with ovarian cancer may have normal levels of CA-125. Because of these problems, the CA-125 measure is not recommended for women at median danger of ovarian cancer.
Because my mother croaked of breast and my sister currently has ovarian cancer, I know that I have significant risk factors. I will talk to my doctor about what measuring is title for me. As with the majority cancers, early diagnosis is the key to survival.
1 note
·
View note