#acute renal failure treatment
Explore tagged Tumblr posts
Text
Cutting Edge Methods for Successful Kidney Cyst Therapy
Kidney cysts are fluid-filled sacs on or within the kidneys, often leading to concerns about kidney function and overall health. This article explores various aspects of kidney cyst treatment, focusing on homeopathic remedies for managing creatinine levels, acute kidney injury, and chronic kidney disease.
Understanding Kidney Cysts:
Kidney cysts are typically noncancerous and may not always cause noticeable symptoms. However, they can grow over time, potentially leading to complications such as infection, bleeding, or interference with kidney function. Treatment options for kidney cysts depend on factors like size, symptoms, and the underlying cause.
Conventional Approaches to Kidney Cyst Treatment:
Monitoring and Observation:
Small, simple kidney cysts may require no treatment but regular monitoring to track changes.
Pain Management:
Pain associated with kidney cysts can be alleviated with over-the-counter pain relievers or prescribed medications.
Aspiration:
Sometimes, a healthcare professional may drain fluid from the cyst using a needle, reducing its size and relieving symptoms.
Homeopathic Approach to Kidney Treatment:
Homeopathy offers a comprehensive and personalised approach to treating kidney cysts, focusing on stimulating the body's natural healing mechanisms. Additionally, homeopathic remedies are gaining recognition for their potential to manage creatinine levels and address acute kidney injury and chronic kidney disease.
Best Homeopathic Medicine for Creatinine:
The best homeopathic medicine for creatinine is beneficial in managing elevated creatinine levels. However, it's crucial to consult a qualified homeopathic practitioner for personalised recommendations.
Homeopathy for Kidney Treatment:
Homeopathic remedies for kidney cysts are chosen based on the individual's symptoms and constitution.
Acute Kidney Injury Treatment with Homeopathy:
Homeopathic remedies may be considered for acute kidney injury treatment, addressing symptoms like swelling, pain, and impaired kidney function.
Homeopathic Management of Chronic Kidney Disease:
Constitutional homeopathy kidney treatment, considering the person's overall health and unique symptoms, may help slow the progression of chronic kidney disease.
Conclusion:
In conclusion, kidney cyst treatment involves a multifaceted approach, incorporating conventional medical interventions and complementary therapies like homeopathy. The choice between conventional and homeopathic kidney treatment may depend on the severity of symptoms, individual preferences, and healthcare professionals' guidance. For managing creatinine levels and addressing kidney disorders, a holistic perspective that combines conventional and homeopathic approaches may offer comprehensive care for those dealing with kidney cysts, acute kidney injury, or chronic kidney disease. Always consult qualified healthcare professionals and homeopathic practitioners for personalised advice and treatment plans.
#Kidney treatment by homeopathy#homeopathic medicine for renal cyst#homeopathic remedy for kidney infection#kidney cyst treatment#homeopathy kidney treatment#acute kidney injury treatment#Homeopathic treatment for kidney failure#Homeopathic medicine for high creatinine#Homeopathic medicine for kidney failure#Chronic Kidney Disease#Homeopathic Medicine for Renal Cyst
0 notes
Text
So the info is FINALLY out about the poor kid in Canada with H5N1.
She is thirteen, with a history of mild asthma and was overweight. She "presented to an emergency department in British Columbia with a 2-day history of conjunctivitis in both eyes and a 1-day history of fever. She was discharged home without treatment, but cough, vomiting, and diarrhea then developed, and she returned to the emergency department on November 7 in respiratory distress with hemodynamic instability. On November 8, she was transferred, while receiving bilevel positive airway pressure, to the pediatric intensive care unit at British Columbia Children’s Hospital with respiratory failure, pneumonia in the left lower lobe, acute kidney injury, thrombocytopenia, and leukopenia."
They threw everything at this kid. Intensive respiratory support (was intubated and put on ECMO), three different antivirals (oseltamavir, amantadine, baloxavir), renal replacement therapy as her kidneys failed, plasma exchanges every day for three days (in an attempt to lower the concentration of cytokines in her blood and prevent/lessen the storm). "No evidence of reduced susceptibility to any of the three antiviral agents used in treatment was observed" in samples which were cultured--and honestly, I'm not sufficiently-educated to understand what that means in this case. The drugs we have aren't any weaker against it, and it still took all three? Or did they just hit her with everything because it's Canada, she is a child, and this shit is scary? But what it sounds like to me is "the drugs we have are as strong against H5N1 as they were ever going to be, and it's not enough."
"It is notable that lower-respiratory specimens consistently yielded lower Ct values than upper-respiratory specimens, a finding that suggested higher viral levels in the lower-respiratory tract." So, strong samples from her lungs, weaker samples from throat and sinuses. Nnnnot great.
Notable, but not surprising, is that the virus in her body showed the HA mutation which makes it more adapted to humans. In the serious New Orleans case with a similar mutation, the sick birds he was exposed to didn't show it, meaning it happened inside his body; in this case we don't know where the exposure was, just that it was the same virus type as was present in local birds, but it's probable that it also happened after she was sickened rather than before.
Link to paper below:
33 notes
·
View notes
Text
Can you trust AI Answers about your health?
During the summer of 2020, when the entire world was focused on the pandemic, getting treatment for other health issues became a challenge.
I started experiencing a lot of back pain, but I shrugged it off as an injury and took Advil to cope.
A week later, I thought I had food poisoning.
I tried an at-home service where they pumped me full of IV fluids.
I went to urgent care. They sent me to get scans. I paid hundreds of dollars out of pocket to get them quickly.
The imaging place never sent the scans to the urgent care.
A day later, I had the worst chills. It was July, in Phoenix. Most likely 100 F. I went outside and was still freezing.
At that point, I was taken to the ER. I ended up in the ICU in one of those rooms they zipped up in plastic.
While most of the focus was on COVID, I had something else: a large kidney stone. The kind that doesn’t pass on its own.
I was in septic shock and acute renal failure according to discharge papers.
The hospital stay itself wasn’t too long, but the treatment with specialists took three months to complete.
Surgeries during COVID were extra special because if you tested positive, your surgery was delayed.
Two years later, in 2022, I ended up in the same hospital for the same reason.
And now, I’m a few days into aggressive antibiotic treatment for my kidneys, yet again. Wondering if I make it to the next followup or have to Lyft off to the ER.
So what does this have to do with Google AI Answers?
In 2020 and 2022, I spent a lot of time perusing Google Search results on kidney stones.
Now, I get AI Answers above at the top of SERPs (search engine results pages).
This wouldn’t be a bad thing if one could trust the AI to accurately summarize its sources.
That’s the big if.
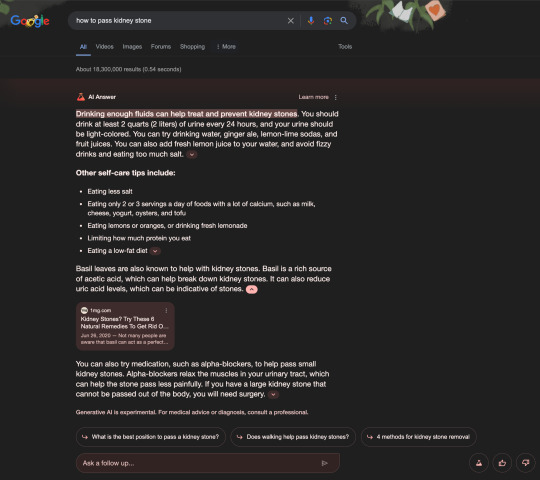
In the first screenshot, you’ll find an AI Answer from Google Search results for the phrase how to pass kidney stone.
The first mistake involved an error with paraphrasing a source with legitimate information.
Because I can assure you after four years of seeing urology specialists, no one has ever suggested drinking two quarts or liters of urine.
The basil leaves suggestion, on the other hand, is suspect. I’ve never come across that as a suggestion. It would have stood out, because I have a lot of basil growing around the garden.
I don’t even remember that website from my previous Google searches. I had to check Wikipedia and other sources to find out what the company even was.
Much like the search quality raters and AI Answer checkers do...
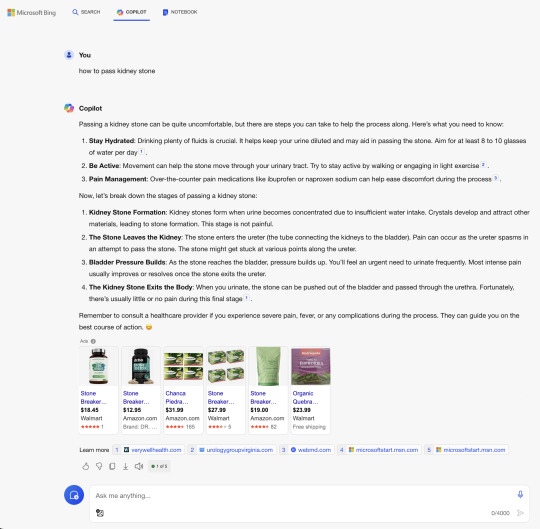
In the second screenshot, Microsoft Bing with Copilot offered ads for supplements and advice from five sources, two of which are the MSN Health Hub.
The hub includes a section where you can Ask a health professional questions.
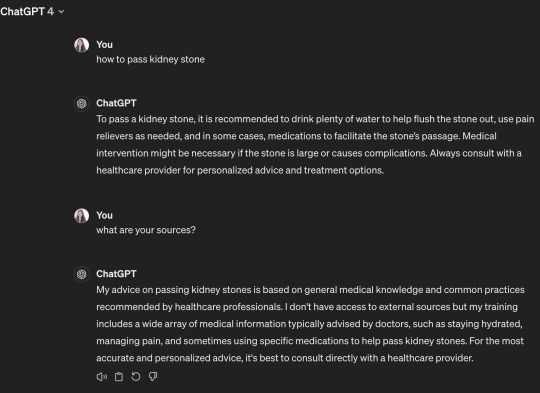
In the third screenshot, ChatGPT using GPT-4 with browsing offered a concise response based on its training data, but claimed not to have access to external sources.
In the fourth screenshot, Perplexity provided the best AI Answer with 19 sources I recognized from my previous research into this health issue.
Moral of the story:
You can’t trust generative AI with your money or your life issues.
But if you do, start with the right AI Answer engine. One that cites sources you trust and doesn’t suggest drinking your own pee.
Think of Perplexity as a better starting point for more in-depth research that you can discuss during your next doctor’s visit.
Not as a definitive answer.
Follow @kristileilani on X for more on AI news, trends, and tools.
35 notes
·
View notes
Text



Leukemia and Lymphoma Awareness Flags!!
This flag was designed by us, as we currently have a family member with Leukemia and wish to bring awareness to this kind of cancer.
color meaning:
#FF2D34: Myeloma
#00DC0E: Non-Hodgkin Lymphoma
#FF8C2E: Leukemia
#D12DFF: Hodgkin Lymphoma
Below is information all about Leukemia and Lymphoma Cancers.
Leukemia and Lymphoma are both cancers that are not associated with a tumor. Lymphomas are cancers that affect the lymph system and start in cells called lymphocytes. Leukemia is a cancer of the early blood-forming tissues, including your bone marrow and lymph system.
There are many types of lymphoma. Some grow and spread slowly and some are more aggressive. There are two main types of Lymphoma:
1. Hodgkin Lymphoma is cancer that starts in the B lymphocytes (B cells) of the lymph system. Your lymph system helps you fight infection and control the fluids in your body.
2. Non-Hodgkin Lymphoma (NHL) is cancer that starts in the lymphocytes anywhere lymph tissue is found:
Lymph nodes
Spleen
Bone marrow
Thymus
Adenoids and tonsils, or
The digestive track.
Leukemia typically involves white blood cells, the cells that are your infection fighters. Leukemia can be divided into categories: fast growing (acute) and slow growing (chronic); and by which white blood cells are affected:
Acute lymphocytic leukemia (ALL)
Acute myelogenous leukemia (AML)
Chronic lymphocytic leukemia (CLL
Chronic myelogenous leukemia (CML)
A screening test is used to detect cancers in people who may be at higher risk for developing the disease. With leukemia and lymphoma, there are no early detection tests. The best way to find them is to be aware of the symptoms:
Swollen lymph nodes which can appear as a lump in the neck, armpit or groin;
Fever
Night sweats
Weight loss without trying, and
Fatigue.
Leukemia can have similar symptoms but also can include:
Easy bleeding or bruising;
Recurring nosebleeds; and
Bone pain or tenderness
Myeloma is cancer of the plasma cells. Plasma cells are white blood cells that produce disease- and infection-fighting antibodies in your body. Myeloma cells prevent the normal production of antibodies, leaving your body's immune system weakened and susceptible to infection. The multiplication of myeloma cells also interferes with the normal production and function of red and white blood cells. An abnormally high amount of these dysfunctional antibodies in the bloodstream can cause kidney damage. Additionally, the myeloma cells commonly produce substances that cause bone destruction, leading to bone pain and/or fractures.
Myeloma cells are produced in the bone marrow, the soft tissue inside your bones. Sometimes myeloma cells will travel through your blood stream and collect in other bones in your body. Because myeloma frequently occurs at many sites in the bone marrow, it is often referred to as multiple myeloma.
Signs and symptoms of myeloma include the following:
Hypercalcemia (excessive calcium in the blood)
Anemia (shortage or reduced function of red blood cells)
Renal damage (kidney failure)
Susceptibility to infection
Osteoporosis, bone pain, bone swelling, or fracture
High protein levels in the blood and/or urine
Weight loss
In 2022, more than 62,650 people are expected to be diagnosed with leukemia. In addition:
Leukemia accounts for 3.6% of all new cancer cases.
The overall 5-year survival rate for leukemia has more than quadrupled since 1960.
62.7% of leukemia patients survive 5 years or more.
The diagnosis of leukemia requires specific blood tests, including an examination of cells in the blood and marrow.
Treatment and prognosis depend on the type of blood cell affected and whether the leukemia is acute or chronic. Chemotherapy and blood and marrow transplant are often used to treat leukemia.
If you wish to read more about Leukemia and Lymphoma cancer, please visit this website!
#leukemia#lymphoma#blood cancer#leukemia and lymphoma society#leukemia awareness#lymphoma awareness#blood cancer awareness#pro endo#pro endogenic#endo friendly
9 notes
·
View notes
Text
“Hafsa Roe,” 33 (Turkey, ~2004)
Abortion laws in Turkey permit abortion for various circumstances before ten weeks, with a clearly stated and unambiguous exception for “life of the mother” cases later in pregnancy. However, even an abortion allegedly done for maternal health can be fatal instead.
“Hafsa” was a lupus patient who had previously given birth to two children. Her chronic condition had been in remission for some time, but during the second trimester she started experiencing symptoms of a lupus flare-up. She was admitted to a state hospital, where doctors documented a butterfly rash on her cheeks, purpura, edema of the legs and acute synovitis. EKG and chest X-ray were conducted, but showed no damage or any other abnormalities. However, extensive lab tests showed indicators for HELLP Syndrome.
Hafsa was admitted to the hospital as an inpatient in the Department of Hematology. She spent an uneventful week there being treated with blood pressure medication and steroids. The “triple test” lab results were normal during this time. An ultrasound and another EKG was planned for the following week. Hafsa was apparently starting to get better.
But despite the encouraging test results, Hafsa suddenly became confused and went into convulsions. She was diagnosed with pre-eclampsia, but her blood pressure was no higher than it was upon admission. Doctors discussed running a CT scan, but decided to delay the scan and transfer her straight to the Obstetric Department instead— even though examination of her eyes showed results that may have benefited from clarification. She had mild papilledema, but there were no exudates and the macula was normal. This is an unusual result and may have been a symptom of pressure on the brain.
Doctors at the OD decided to put Hafsa through an abortion. At this time she was confused and most likely not in a mental state to consent to this. She was put through a prostaglandin abortion at 18 weeks pregnant.
It is worth noting that the compound typically used in prostaglandin abortion is PGF2A. Unlike most prostaglandins, F2A is a very powerful vasoconstrictor. For someone with an eclampsia diagnosis, it was an unsuitable choice— especially since it had been established in medical science for decades that inducing abortion was not helpful for pregnant lupus patients. The treatment for eclampsia is giving birth (typically paired with blood pressure medications), not abortion, and even if Hafsa’s baby wouldn’t have survived birth, there was no medical benefit to ensuring intrauterine death.
Predictably, the abortion did not save Hafsa. It is worth noting that before the abortion, she was breathing independently. Afterwards, she went into respiratory failure and needed oxygen therapy. A catheter had to be placed because of oliguria. She had to receive a blood transfusion of two units of packed red blood cells, 15 ml/kg plasma, a unit of platelets and a 100-ml unit of 4% human albumin. Hafsa was transferred to the ICU, where she would spend her final days of life.
Hafsa’s respiratory failure was given the probable diagnosis of Acute Respiratory Distress Syndrome. In the ICU, she continued to receive oxygen therapy and blood transfusions. On her third day as an Intensive Care patient, she deteriorated so badly that she had to be intubated and ventilated. She was producing nearly no urine. Doctors attempted more and more treatments, but nothing was working now.
By the sixth day in the ICU, Hafsa’s respiratory function was worse. The now-abandoned term “lung infiltrate” was used to describe a suspected complication. (This term is no longer used because it was highly vague, but may have referred to post-abortion pulmonary embolism in Hafsa’s case.) She was placed on dialysis for lack of sufficient kidney function, but from day 9 to 11, was noted to remain in acute renal failure. She was still hypertensive and was feverish.
On day 14, doctors performed a tracheostomy. A chest X-ray, which had been normal and utterly unremarkable, now confirmed lung infiltration (see previous notes).
Apparently losing blood, Hafsa went from hypertensive to hypotensive in a few days. Over the course of her hospitalization, she received 20 units of packed red blood cells and “large quantities” of platelets. On day 24 in the ICU, she deteriorated further and developed severe hypotension. Despite aggressive treatment, she died of ARDS on the 25th day.
Hafsa’s family declined an autopsy. However, by observing cases of women with similar conditions who were killed by “therapeutic” abortions, we can draw parallels. First, let’s examine the case of “Molly Roe”, a 21-year-old who was hospitalized for a lupus flare up and put through an abortion that was later denounced by a maternal health committee. In Molly’s case, it was discovered postmortem that the abortion was more of a threat to her health than the pregnancy, and that the instillation abortion (in her case, saline) put a heavy strain on her already-struggling kidneys. Molly suffered kidney failure too.
Next, we examine the case of “Pamela Roe”, a 38-year-old patient who was in the second trimester when she suffered hypertension and pre-eclampsia. Just like Hafsa, Pamela was told to have an abortion instead of the gold-standard delivery. Pamela also underwent a prostaglandin instillation abortion, just like Hafsa did. In Pamela’s case, the powerful vasoconstrictor elevated her blood pressure so dramatically that the blood vessels in her head burst and she bled to death intracranially. (This is a possibility that was mentioned in Hafsa’s case report, but could not be confirmed without a postmortem exam.) If this was the mechanism behind Hafsa’s death, it would explain how she was hypertensive despite needing massive blood transfusions. PGF2A is also a platelet aggregator, which may explain why she needed to receive more.
Hafsa, Molly, Pamela and all women with health conditions deserved better than abortion.
#tw abortion#unidentified victim#abortion is not healthcare#women deserve better than abortion#pro life#unsafe yet legal#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion
4 notes
·
View notes
Text
Okay so, Hemlock, big bad evil man that yoinked our Crosshair.
What I'm intrested in about him, is the Gas that he used in Ep.14, Tipping point. Crosshairs already weak, we can see that, and Resonably so. Before he even gets in the room he's stumbling around, missing shots, he wouldn't have had a chance to handle any sort of Toxin.
Let alone hemlock, a deadly plant that can result in death. And I think that's what the gas is, hemlock.
So hemlock has alot of affects, ingesting it can leave someone experiencing central nervous system depression, respiratory failure, acute rhabdomyolysis, acute renal failure and death. And even when it's just inhaled through a smoke form it can still give someone Central nervous system depression, and respiratory failure.
The symtoms of Hemlock poisoning? From the ones I could see in that animation, Which cannot display alot of the symptoms (High blood pressure, restlessness or confusion, dry mouth etc.) There were still some that Crosshair displayed.
-Mussel weakness, Barley moments into the toxins release Crosshair collapses, yes this could be a symptom of his previous weakness. But prior to the gases release nothing major happened that would have decreased his motor function so quickly, other than the toxins effects. Crosshair is also depicted not long after falling over, trying to push himself up but not having the core strength to do so, this could be argued as respiratory failure. Which he starts to experience, but it's to soon in the prosses to have that much of a hold on him.
-Dilated pupils, From the scene when the gas first entered the room, to the scene where Crosshair had collapsed his pupils had Dilated. (Dialate, for something to expand.)
-Rapid heartrate, even though we couldn't get a visual of this, before the Guard takes him away we can here his hearybeat, and we can here it start to pick up before he fall unconscious (Although the heartrate does slow down right before he loses consciousness, this can be explained by anouther symtom).
-Restlessness and Confusion, I put this down as one of the thing that couldn't be depicted in the visuals, because we can't know if Crosshair feels Confusion in the moment. But I believe a depiction of this, is the way he hears Hemlocks voice while he speaks, the effects on it could be the visual representation of Crosshairs Confusion.
Another thing I want to touch on, is the respiratory failure and central nervous system depression. Although they can't be shown to their full extent in the short time frame, they play a part in the scene.
-Respiratory failure, Very quickly it shows Crosshair struggling to breath, the coughing and short breaths is true to that. The coughing? Not so much, but how short, cut off and quick his breaths become shows a struggle. You can see this in his movements, how after he falls his chest will rapidly rise and fall through the majority the continuing scene, but slow down right before he loses consciousness.
-Central Nervous system depression, The central nervous system depression (CNSD) is a less likely part in how the scene plays out. CNSD is "a physiological state that can result in a decreased rate of breathing, decreased heart rate, and loss of consciousness, possibly leading to coma or death." We see this clearly in afew ways, the loss of consciousness happens quickly, both by his weakened state and by a decreased rate of breathing (Which was touched on in Respiratory failure). However it could also be cause by a decreased heartrate, yes, I had mentioned Crosshairs heartrate picking up during the scene, but I also mentioned how it slowed just before he lost consciousness. This skipping heatbeat could be a symptom of his heartrate decreasing, conflicting with the rapid heart rate symptom. While it could also just be a sign of his lose of consciousness, which is why I don't think the decreased heartrate plays a big role in the bigger picture.
If I could, I'd line up the treatments for Hemlock posioning with what we see of Crosshair in the final episode of S2, But I have no understanding on Starwars medical procedures and wouldn't have a hope of lining that up with the real world methods.
Uh, how do you even end this? It's like school speeches, just copy the introduction and change up the words- But that Dosn't really work when your Intro's 'Big bad evil man'.
Anyway I think that Toxin shown in Ep.14 is some modification of the alkaloid toxins found in actual hemlock plants.
#crosshair#hemlock#the bad batch#bonus points hemlock is the kind of messed up to use this plant with all it's nervous system damaging properties#typo's for the win
22 notes
·
View notes
Text
Understanding The Kidney Infection in Detail

Overview
You’re probably not on the lookout for indicators of a kidney infection all of the time. However, a urinary tract infection (UTI)
can lead to an infection in one or both kidneys, so it’s an ailment to keep an eye on. Once you have been diagnosed with UTI, it’s time to take care of your pair of kidneys. So think twice before skipping any of those antibiotics that your doctor has prescribed. Here is what you need to know about kidney infection symptoms
, where it hurt when you have one, and many more.
What is a kidney infection?
Urinary tract infection is the most common cause of kidney infection that can spread upwards and can affect one or both kidneys. The infection may be acute or persistent. They’re usually painful, and if they’re not treated very away, they can be fatal.
In most cases, the infection is caused by E.coli bacteria.
Pyelonephritis is the medical terminology for kidney infection.
Also, Read — Suffering UTI or Kidney Infection?- Here Is What You Need To Know
How long can you have a kidney infection without knowing?
You will have the symptoms of kidney infection after two to three days after infection. Do not neglect any of the initial symptoms as kidney infection can become deadly, if not treated in time.
Can a kidney infection go away on its own?
A kidney infection can lead to a life-threatening condition. You should seek medical advice
and get it treated. Otherwise, the complications include-
Kidney failure
Kidney damage
High blood pressure
Sepsis
Kidney abscess or pus formation
Also, Read — 7 Best Kidney Transplant Hospitals in India
How to treat kidney infection?
To alleviate the kidney infection symptoms, your healthcare provider
will prescribe
OTC (over-the-counter) pain medications like ibuprofen, and naproxen for the pain
Antibiotics to reduce the bacterial load
Drink as much fluid as possible till the color of your urine become pale. This will flush out the bacteria from your body.
Take ample rest to fight off the infection.
Do not take any medicines (pain killers with aspirin), as this can increase the chances of bleeding.
A serious kidney infection will almost certainly require hospitalization. In this situation, antibiotics and hydration will be administered by an intravenous (IV) injection or infusion.
Conclusion-By simply packing their medical travel in India
, renal treatment can substantially benefit the patient. We also offer a comprehensive range of counseling for coping with emotional challenges to our international patients.
How can we help in the treatment?
If you are in search of a kidney transplant treatment in India
, we will serve as your guide throughout your treatment and will be physically present with you even before your treatment begins. The following will be provided to you:
Opinions of expert physicians and surgeons
Transparent communication
Coordinated care
Prior appointment with specialists
Assistance in hospital formalities
24*7 availability
Arrangement for travel
Assistance for accommodation and healthy recovery
Assistance in emergencies
We are dedicated to offering the highest quality health care to our patients. At HealthTrip
, we have a team of highly qualified and devoted health professionals that will be by your side from the beginning of your journey.
HealthTrip — #1 Health Travel & Tour Advisors | Medical Tourism in IndiaExperience the best health trip with a top medical travel company in India. Find the best hospitals, and doctors for medical treatment in India. Best Medical Tourism in India.
Kidney Infection — Symptoms, Prevention, Cause | HealthTripWhere Does It Hurt When You Have a Kidney Infection? — Here is what you need to know about kidney infection symptoms, where does it hurt when you have one, and many more.
4 notes
·
View notes
Photo
Discover the Critical Differences: CRRT vs. Dialysis
When kidneys falter, the body accumulates waste products and excess fluids, leading to a potential health crisis. Dialysis, a well-established treatment, steps in to remove these toxins and regulate fluids. However, for critically ill patients, another option exists: Continuous Renal Replacement Therapy (CRRT). While both CRRT and dialysis address kidney failure, they differ significantly in their approach. Let's discover the critical differences: CRRT vs. dialysis.
Delivery Method: Intermittent vs. Continuous Flow
Dialysis: This traditional method functions in cycles. Blood is diverted through a dialyzer, a specialized filter, for several hours, typically three times a week. The cleaned blood is then returned to the body.
CRRT: CRRT offers a continuous process. Blood is slowly drawn out, filtered, and returned to the bloodstream simultaneously. This gentler approach mimics healthy kidney function, providing a more consistent removal of waste and fluids.
Patient Suitability: Stability is Key
Discover the critical differences: CRRT vs. dialysis in terms of patient suitability. Dialysis is often the preferred choice for patients with stable chronic kidney disease (CKD) and even some cases of acute kidney injury (AKI). However, it might not be ideal for critically ill patients who are hemodynamically unstable (having unstable blood pressure). The rapid fluid removal during dialysis can further destabilize their condition.
360K notes
·
View notes
Text
Myocardial Infarction Minimizing Hospital Readmission Phase 1: EBP for Effective Patient Care Transition Donald, an acute myocardial infarction (MI) patient, has undergone angioplasty, a procedure in which a catheter is inserted into clogged arteries in a patient’s heart to widen them and improve blood flow. To supplement the angioplasty, Donald has had cardiac stents placed to prop the affected arteries open and reduce their risk of narrowing again. Studies have shown that several complications could result from angioplasty procedures and the insertion of stents as in Donald’s case. The most common complications include bleeding or vascular complications (6 percent of patients), acute renal failure (5 percent of patients), and stroke (0.3 percent of patients) (Dunlay et al., 2012). A study analyzing readmission rates among MI patients in Minnesota found that bleeding was the most common complication after angioplasty, affecting 6 percent of patients (Dunlay et al., 2012). The most common form of bleeding was bleeding at the catheter access site, which was shown to affect 62.7 percent of patients. 37.4 percent of patients report complications associated with groin hematoma, gastrointestinal bleeding and bleeding from other sites (Dunlay et al., 2012). At times, the bleeding is just a bruise, but other times, the bleeding may be serious enough to require surgical procedures or a transfusion. To minimize the risk of side effects related to cardiac catheterization, the nurse plans to educate the patient on the potential side effects of the same and what they could do to minimize the risk. This includes availing information sheets explaining the symptoms of retroperitoneal bleeding and hematoma formation at the groin site as well as methods of preventing the same (dunlay et al., 2012). The nurse will also distribute simplified information sheets teaching the patient how to self-hydrate as a way to minimize the risk of renal failure resulting from cardiac catheterization (Lambert et al., 2017). Since the patient’s extended family is nearby, it would be plausible to include them in the awareness-raising as a way of ensuring that they can adequately distinguish between what is normal and abnormal. It is also prudent that the nurse connects the patient with their primary care provider to facilitate constant monitoring of side effects upon discharge (Lambert et al., 2017). Studies have shown that patient education has significant benefits in reducing the risk of renal complications after angioplasty by 20 percent (Lambert et al., 2017). Phase 2: EBP for Prevention of Hospital Readmission Besides the disease-related complications, several non-disease specific factors also influence the risk of readmission. A prominent factor in Donald’s case is that he has not visited his primary care physician for the last 7 months. Given that Donald has been under the observation of a hospitalist during his five days at the hospital, there is a need to involve his primary care physician to ensure sufficient follow-up and post-procedure assessment. According to the Center for Medicare and Medicaid, racial and ethnic minorities are less likely to follow up with a primary care physician or an appropriate specialist after discharge for chronic illness treatment (CMS, n.d.). In this case, the nurse plans to educate the patient, in the simplest terms possible, on the importance of making early follow-ups with their primary care provider (CMS, n.d.). However, the nurse may also need to engage the patient and his family to identify why he has not visited his primary care provider for the past 7 months. This would help the nurse identify whether the problem results from transportation issues, cultural issues, or language barriers. Upon obtaining this information, the nurse will work together with the patient’s PCP to address the problem. For instance, to facilitate transportation to the PCP, the nurse could initiate an informal agreement with both the PCP and community-based non-profits to provide transport services at specified intervals. This form of networking would ensure that the PCP is aware of the patient’s status and can offer constant monitoring for disease progression and potential complications. Donald’s lifestyle choices are relatively poor and although they are not related directly to MI, they increase the risk of readmission indirectly. First, Donald has untreated hyperlipidemia but his diet still contains considerably large amounts of fats from restaurant and cafeteria foods, as well as fast foods. His daily consumption of coke, coffee, and beer during the weekends, coupled with lack of exercise worsens his untreated obesity and the risk of hypertension from his medical history. The nurse’s first plan to minimize the risk of readmission is to provide simplified educational materials to educate the patient on the need to maintain a healthy diet and undertake proper exercise as a way of slowing down disease progression and minimizing their risk of readmission (Jones et al., 2018). Since Donald and his wife are active participants in the church, the nurse will collaborate with the church leadership to organize awareness-raising and sensitization sessions geared at educating members, including Donald, on the components of healthy diets and the benefits of the same on patients with chronic illness. Participants in these sessions could receive t-shirts and recipe books to guide them on healthy diets. To supplement the educational sessions and reinforce participants’ healthy eating habits, participants could take part in competitions that involve preparing healthy diets and bringing the same to church to share with other participants. To encourage healthy eating, the nurse could connect the patients with community-based resources that facilitate home-based delivery of fresh groceries from the nearby grocery store located 0.5 miles from their home. Further, since the patient’s family lives nearby, the nurse plans to engage them by supporting them in developing a daily/weekly exercise plan, where members take turns to jog, cycle or attend gym sessions with the patient. This would be preceded by educational sessions geared at educating the extended family on the benefits of exercise and healthy eating to the patient and their effect on their risk of readmission (Lambert et al., 2017). This would help to encourage the patient while ensuring that exercise is centered on their needs. Phase 3: Hospitalization Prevention Plan The plan for preventing hospitalization for MI patients involves three levels of prevention: primary prevention strategies, secondary prevention, and tertiary prevention. Primary prevention strategies are early interventions aimed at foiling the disease among high-risk individuals before it begins, while secondary prevention focuses on early detection and halting the progression of asymptomatic disease (Karunathilake & Ganedoda, 2018). Finally, tertiary prevention involves arresting, slowing down, and reversing disease to prevent further deterioration and recurrence of symptoms (Karunathilake & Ganedoda, 2018). Studies identify high-risk individuals as those presenting with a family history of MI, and those with diabetes, smoking, hyperlipidemia, and hypertension (Borghi & Ambrosioni, 1996). Primary prevention strategies are mainly lifestyle interventions aimed minimizing these risk factors by reducing blood pressure, serum cholesterol, and blood cholesterol (Borghi & Ambrosioni, 1996). One preventive strategy at the primary level could thus involve educating at-risk persons on the risks associated with smoking and connecting them with the tobacco cessation counseling program, which is co-funded by all states to offer support to individuals pursuing smoking cessation. Studies have shown that smoking cessation could reduce the risk of MI by between 50 and 70 percent over a period of five years (Borghi & Ambrosioni, 1996). Another strategy is to educate patients on the components of healthy diets, the importance of exercise, and the risk associated with alcohol consumption. Besides educating patients, the nurse could help the patients reinforce these strategies into their lifestyles by connecting them with community-based programs such as Alcohol Anonymous programs and nutritionists, helping them develop incremental lifestyle goals, and informing them of apps and other community-based programs that they could use to track their weight and order healthy groceries from local stores. This would ensure that participants not only understand the risk that they face, but also play and active role in implementing the strategies for healthy living. Studies have shown that exercise, healthy diets, and low-to-moderate alcohol consumption could reduce the risk of MI by 45, 55, and 35 percent respectively (Borghi & Ambrosioni, 1996). Prevention strategies at the secondary level focus on halting the progression of asymptomatic disease following an early diagnosis. A crucial intervention strategy at this level is to link the patient with a primary care provider. It is unlikely that patients at this level have a PCP given that they are still asymptomatic. Linking them with a PCP would ensure that risk factors and the progression of disease are constantly monitored (Karunathilake & Ganedoda, 2018). Further, linkage with the PCP would provide avenues for medicinal interventions such as beta blockers and antiplatelet therapy (chiefly aspirin), which help to slow down the progression of the disease. The nurse at the secondary level needs to, if necessary, link patients with programs where they can access statin therapy, a medical program used to manage blood lipids and cholesterol (Karunathilake & Ganedoda, 2018). Lifestyle interventions will also be continued at this stage to supplement the medicinal interventions (Karunathilake & Ganedoda, 2018). Studies estimate that medicinal intervention using beta blockers and antiplatelet drugs reduce the risk of death from MI by 22 percent and 54 percent respectively (Borghi & Ambrosioni, 1996). Tertiary prevention focuses on increasing the life expectancy of MI patients and helping them manage pain (Karunathilake & Ganedoda, 2018). Prevention strategies at this level include insertion of pacemakers, stents, coronary angioplasty, bypass surgery, and defibrillators (Karunathilake & Ganedoda, 2018). These strategies are to be supplemented with the medicinal interventions (chiefly beta blockers, calcium channel blockers, and Aspirin) and lifestyle interventions identified at the primary and secondary levels (Karunathilake & Ganedoda, 2018). Studies have shown that the long-term administration of beta blockers and antiplatelet drugs reduces the risk of recurrent myocardial infarction by 27 percent and 54 percent respectively (Borghi & Ambrosioni, 1996). References Borghi, C., & Ambrosioni, E. (1996). Primary and Secondary Prevention of Myocardial Infarction. Clinical and Experimental Hypertension, 18(3), 547-58. CMS (n.d.). Guide to Reducing Disparities in Readmissions. Center for Medicare and Medicaid. Retrieved from https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/OMH_Readmissions_Guide.pdf Dunlay, S., Weston, S. A., Killian, J., Bell, R. M., Jaffe, A. S., & Roger, V. L. (2012). Thirty Day Hospital Readmissions Following Acute Myocardial Infarction: A Community Study. Ann Intern Med, 157(1), 11-18. Jones, R., Arps, K., Davis, D. M., Blumenthal, R. S., & Martin, S. S. (2018). Clinician Guide to the ABCs of Primary and Secondary Prevention of Atherosclerotic Cardiovascular Disease. American College of Cardiology. Retrieved from https://www.acc.org/latest-in-cardiology/articles/2018/03/30/18/34/clinician-guide-to-the-abcs Karunathilake, S. P., & Ganegoda, G. (2018). Secondary Prevention of Cardiovascular Diseases and Application of Technology for Early Diagnosis. Biomed Research International, doi: org/10.1155/2018/5767864 Lambert, P., Chaisson, K., Horton, S., Petrin, C,…& Brown, J. (2017). Reducing Contrast-Induced Acute Kidney Injury: How Nurses can Improve Patient Safety, a Qualitative Investigation. Critical Care Nursing, 37(1), 13-26. Read the full article
0 notes
Text
[ad_1] We at Sri Ramakrishna Hospital, Department of Urology are equipped with the first and only 100 watts Holmium Laser machine available in the entire Kongu Region. We have done Holmium Enucleation of Prostate (HoLEP) for the prostate size from 90 gm to 260 gm in one endoscopic surgery with excellent results associated with negligible complications. Normally prostate sizes more than 120 gm requires open surgery for complete removal of the prostate. In our hospital one 260 gm, one 160 gm and one 140 gm prostates were successfully operated with HoLEP avoiding open prostate surgery. Open prostate surgery is associated with increased risk of bleeding, post operative pain, long hospital stay, delay in return to work and normal life also leaves patient with lower abdominal scar all these problems are avoided with HoLEP. Patients on blood thinners (antiplatelet drugs) for cardiac, neuro and vascular problems are much benefitted with HoLEP as these drugs can be restarted on the very next day. HoLEP is a boon to the patients with BPH who need surgical intervention. What is Benign Prostatic Hyperplasia (BPH) Prostate is a Male accessory gland of size 20 gm located just below the bladder and around the urethra. Prostate gland enlarges in size after the age of 40 years. Degree of enlargement varies from individual to individual; it is independent of food habits and lifestyle. What are the symptoms of BPH? Patients with enlarged prostate may experience one or many of the below symptoms. Symptoms don't have any correlation with the size of the prostate. What are the complications a patient may experience with BPH? Acute Urinary Retention Sudden inability to pass urine or empty the bladder. A catheter needs to be inserted into the bladder to help drain the urine. Recurrent Urinary Infection Presence of retained urine in the bladder increases the risk of urinary tract infection. Renal Failure Increased residual urine in the bladder increases the pressure in the bladder, ureter and to the kidneys. Leads to a condition called obstructive uropathy, if not treated on time patient will end up in renal failure which may be reversible may not be reversible. Chronic Urinary Retention Patients with BPH symptoms if not addressed early they will gradually accumulate urine in large quantity more than the capacity of the bladder. Eventually the bladder will lose its emptying capacity and will end up in a lifelong indwelling urinary catheter. In those patients surgery for the enlarged prostate may not be helpful. Bladder Stones: One or multiple stones may be formed in the stagnant urine. Holmium Laser Enucleation of Prostate (HoLEP) HoLEP is highly advanced endoscopic surgical procedure done for the patients with enlarged prostate who need surgical intervention. Not all the patients with BPH need surgery. About 70% to 80% of the BPH patients do well with medical treatment which is to be continued for life like wearing spectacle for vision. Approximately 20% to 30% of patients with BPH will need surgery. HoLEP is a type of laser prostate surgery in which anesthesia is given and the patient stay calm and relaxed. Antibiotic given to avoid the risk of infection. A surgical instrument called resectoscope with LASER working element is inserted through the urethra connected to camera which helps to have magnified vision of surgical field. High power Holmium Laser is then passed through the working element and used to detach the entire prostate from its outer shell called prostatic capsule. During detachment of prostate bleeding vessels are simultaneously sealed. Prostatic tissue detached into the bladder. After the laser process a morcellator is used to suck the tissue out of bladder. Once the tissue is removed resectoscope is removed and a urinary catheter inserted into the bladder and then the patient is kept under observation for couple of hours to a day or two. What are the advantages of HoLEP
No Pain No cut No scar No bleeding No Fluid absorption No volume Overload status Quick recovery Early Return to work Early restart of blood thinners (Antiplatelets) Entire prostate being removed and Long term relief These advanced procedures at Sri Ramakrishna Hospital are performed by Urology Experts who are dedicated to providing personalized care while ensuring the best outcomes. With state-of-the-art facilities and a team of experienced professionals, Sri Ramakrishna Hospital ensures patients receive the highest quality care in a comfortable and supportive environment. Individuals experiencing symptoms of an enlarged prostate can seek medical attention while making an informed decision about the procedure. About Sri Ramakrishna Hospital Sri Ramakrishna Hospital has attained an iconic reputation since its inception in 1975. Situated in the heart of Coimbatore city, this hospital has in many ways became a part of medical history. In fact, it has been an integral part of the healthcare revolution of modern India. Established and run by the SNR Sons Trust, Sri Ramakrishna Hospital treats several lakhs of patients each year. From providing the most advanced medical procedures to treatments for everyday ailments, they bring relief to patients from all walks of life using state-of-the-art technology and cutting-edge surgical and medical techniques to deliver outstanding results. !function(f,b,e,v,n,t,s) if(f.fbq)return;n=f.fbq=function()n.callMethod? n.callMethod.apply(n,arguments):n.queue.push(arguments); if(!f._fbq)f._fbq=n;n.push=n;n.loaded=!0;n.version='2.0'; n.queue=[];t=b.createElement(e);t.async=!0; t.src=v;s=b.getElementsByTagName(e)[0]; s.parentNode.insertBefore(t,s)(window,document,'script', 'https://connect.facebook.net/en_US/fbevents.js'); fbq('init', '311356416665414'); fbq('track', 'PageView'); [ad_2] Source link
0 notes
Text
Renal Cysts: Deciphering the Mysteries of Cystic Kidney
The popularity of homeopathy has grown in alternative medicine due to the holistic treatment approach it offers to a variety of ailments. One area in which homeopathy has proven promising is in the treatment of kidney-related problems, which range from cysts and kidney infections to acute renal injuries and sometimes even kidney dysfunction.
Homeopathic Remedies for Kidney Infection
Kidney problems, called pyelonephritis, are complex and disrupt your daily routine. Homeopathy has a range of treatments that can ease the symptoms and help support our body's own healing process.
Homeopathic Remedy for Kidney Infection is usually suggested for burning pain when urinating. Patients who can benefit from these remedies typically have the urge to urinate continuously but only pass small amounts every time.
If kidney inflammation is caused by swelling or stinging pain, it may be thought of as. This remedy is renowned for having anti-inflammatory qualities. It is also recommended to treat sharp, throbbing kidney pains which may spread into the bladder. They are believed to aid in helping eliminate kidney stones and ease the discomfort that comes with them.
Kidney Cyst Treatment through Homeopathy
The kidneys are prone to cysts. No matter how complex or straightforward, it causes discomfort and requires careful treatment. Homeopathic remedies seek to target and treat the root cause and improve kidney health. Kidney cyst treatments are usually suggested in cases of the sensation of pain or burning in the region of the kidneys. They can be helpful when kidney cysts are linked to anxiety and anxiety.
Furthermore, if kidney cysts are associated with a feeling of fullness and abdominal heaviness, it could be an indication of. It is believed that they affect the circulation and balance of fluids in the body. Patients who experience bloating and pain caused by kidney cysts, especially on the left side, can find relief through the use of natural homeopathic remedies. The remedy is believed to aid in the function of kidneys.
Homeopathy to treat acute kidney injury
An acute kidney injury (AKI) is an acute and frequently grave condition that requires immediate attention. While traditional medical treatment is vital, homeopathic remedies can be utilised as a complement to aid. If you are suffering from AKI that has a sudden appearance, anxiety, or anxiety, these remedies can be thought of as. It is believed that homeopathy kidney treatment can alleviate the symptoms that are similar to shocks commonly caused by acute kidney injuries. This treatment is usually suggested in the case of AKI, which causes burning and severe weakness. This remedy can be beneficial if there is a need for emotional and physical help during healing.
If AKI occurs, it is often accompanied by extreme sweating, weakness and a feeling of emptiness; some remedies can be considered as a possible natural cure.
Homeopathic Treatment for Kidney Failure
Kidney dysfunction is a situation where the kidneys cease to function effectively. Although traditional medical treatments like dialysis and transplantation are typically required, homeopathy can provide supportive therapy to improve the general health of people suffering from kidney failure.
Homeopathic remedies are frequently looked at by those with kidney problems that cause fatigue, weakness, or anxiety. The treatments are thought to impact the circulatory and respiratory systems. If you feel a sense of despair and hopelessness due to kidney failure, these solutions can be considered. They are frequently suggested for those suffering from mental and emotional stress.
They could be considered if you have a kidney problem and are prone to swelling and retention of fluid. It is believed to improve excellent circulation and ease symptoms of congestion.
Conclusion
While homeopathic remedies cannot be an alternative to conventional medical treatment, they can help support kidney health. It is crucial to talk with a trained professional homeopathic doctor or medical professional before adding these remedies to an overall acute kidney injury treatment plan, particularly for severe kidney problems. Like any other medical treatment, the individual response to homeopathic remedies may differ, and a holistic approach towards kidney disease that encompasses both alternative and conventional treatments could provide the most complete care. Be sure to communicate openly with your healthcare professionals to ensure a balanced and personalised treatment for kidney health.
#Homeopathic Remedy for Kidney Infection#kidney cyst treatment#homeopathic medicine for kidney failure#homeopathic medicine for kidney disease#homeopathic medicine for polycystic kidney#homeopathic medicine for renal cyst#Homeopathic treatment for kidney failure#Acute kidney injury treatment#homeopathy kidney treatment#Kidney Treatment by Homeopathy#Chronic Kidney Disease
0 notes
Photo
Discover the Critical Differences: CRRT vs. Dialysis
When kidneys falter, the body accumulates waste products and excess fluids, leading to a potential health crisis. Dialysis, a well-established treatment, steps in to remove these toxins and regulate fluids. However, for critically ill patients, another option exists: Continuous Renal Replacement Therapy (CRRT). While both CRRT and dialysis address kidney failure, they differ significantly in their approach. Let's discover the critical differences: CRRT vs. dialysis.
Delivery Method: Intermittent vs. Continuous Flow
Dialysis: This traditional method functions in cycles. Blood is diverted through a dialyzer, a specialized filter, for several hours, typically three times a week. The cleaned blood is then returned to the body.
CRRT: CRRT offers a continuous process. Blood is slowly drawn out, filtered, and returned to the bloodstream simultaneously. This gentler approach mimics healthy kidney function, providing a more consistent removal of waste and fluids.
Patient Suitability: Stability is Key
Discover the critical differences: CRRT vs. dialysis in terms of patient suitability. Dialysis is often the preferred choice for patients with stable chronic kidney disease (CKD) and even some cases of acute kidney injury (AKI). However, it might not be ideal for critically ill patients who are hemodynamically unstable (having unstable blood pressure). The rapid fluid removal during dialysis can further destabilize their condition.

snailchicken
book of hours, Bruges ca. 1500
Baltimore, Walters Art Museum, Ms. W.427, fol. 57r
9K notes
·
View notes
Text
[ad_1] We at Sri Ramakrishna Hospital, Department of Urology are equipped with the first and only 100 watts Holmium Laser machine available in the entire Kongu Region. We have done Holmium Enucleation of Prostate (HoLEP) for the prostate size from 90 gm to 260 gm in one endoscopic surgery with excellent results associated with negligible complications. Normally prostate sizes more than 120 gm requires open surgery for complete removal of the prostate. In our hospital one 260 gm, one 160 gm and one 140 gm prostates were successfully operated with HoLEP avoiding open prostate surgery. Open prostate surgery is associated with increased risk of bleeding, post operative pain, long hospital stay, delay in return to work and normal life also leaves patient with lower abdominal scar all these problems are avoided with HoLEP. Patients on blood thinners (antiplatelet drugs) for cardiac, neuro and vascular problems are much benefitted with HoLEP as these drugs can be restarted on the very next day. HoLEP is a boon to the patients with BPH who need surgical intervention. What is Benign Prostatic Hyperplasia (BPH) Prostate is a Male accessory gland of size 20 gm located just below the bladder and around the urethra. Prostate gland enlarges in size after the age of 40 years. Degree of enlargement varies from individual to individual; it is independent of food habits and lifestyle. What are the symptoms of BPH? Patients with enlarged prostate may experience one or many of the below symptoms. Symptoms don't have any correlation with the size of the prostate. What are the complications a patient may experience with BPH? Acute Urinary Retention Sudden inability to pass urine or empty the bladder. A catheter needs to be inserted into the bladder to help drain the urine. Recurrent Urinary Infection Presence of retained urine in the bladder increases the risk of urinary tract infection. Renal Failure Increased residual urine in the bladder increases the pressure in the bladder, ureter and to the kidneys. Leads to a condition called obstructive uropathy, if not treated on time patient will end up in renal failure which may be reversible may not be reversible. Chronic Urinary Retention Patients with BPH symptoms if not addressed early they will gradually accumulate urine in large quantity more than the capacity of the bladder. Eventually the bladder will lose its emptying capacity and will end up in a lifelong indwelling urinary catheter. In those patients surgery for the enlarged prostate may not be helpful. Bladder Stones: One or multiple stones may be formed in the stagnant urine. Holmium Laser Enucleation of Prostate (HoLEP) HoLEP is highly advanced endoscopic surgical procedure done for the patients with enlarged prostate who need surgical intervention. Not all the patients with BPH need surgery. About 70% to 80% of the BPH patients do well with medical treatment which is to be continued for life like wearing spectacle for vision. Approximately 20% to 30% of patients with BPH will need surgery. HoLEP is a type of laser prostate surgery in which anesthesia is given and the patient stay calm and relaxed. Antibiotic given to avoid the risk of infection. A surgical instrument called resectoscope with LASER working element is inserted through the urethra connected to camera which helps to have magnified vision of surgical field. High power Holmium Laser is then passed through the working element and used to detach the entire prostate from its outer shell called prostatic capsule. During detachment of prostate bleeding vessels are simultaneously sealed. Prostatic tissue detached into the bladder. After the laser process a morcellator is used to suck the tissue out of bladder. Once the tissue is removed resectoscope is removed and a urinary catheter inserted into the bladder and then the patient is kept under observation for couple of hours to a day or two. What are the advantages of HoLEP
No Pain No cut No scar No bleeding No Fluid absorption No volume Overload status Quick recovery Early Return to work Early restart of blood thinners (Antiplatelets) Entire prostate being removed and Long term relief These advanced procedures at Sri Ramakrishna Hospital are performed by Urology Experts who are dedicated to providing personalized care while ensuring the best outcomes. With state-of-the-art facilities and a team of experienced professionals, Sri Ramakrishna Hospital ensures patients receive the highest quality care in a comfortable and supportive environment. Individuals experiencing symptoms of an enlarged prostate can seek medical attention while making an informed decision about the procedure. About Sri Ramakrishna Hospital Sri Ramakrishna Hospital has attained an iconic reputation since its inception in 1975. Situated in the heart of Coimbatore city, this hospital has in many ways became a part of medical history. In fact, it has been an integral part of the healthcare revolution of modern India. Established and run by the SNR Sons Trust, Sri Ramakrishna Hospital treats several lakhs of patients each year. From providing the most advanced medical procedures to treatments for everyday ailments, they bring relief to patients from all walks of life using state-of-the-art technology and cutting-edge surgical and medical techniques to deliver outstanding results. !function(f,b,e,v,n,t,s) if(f.fbq)return;n=f.fbq=function()n.callMethod? n.callMethod.apply(n,arguments):n.queue.push(arguments); if(!f._fbq)f._fbq=n;n.push=n;n.loaded=!0;n.version='2.0'; n.queue=[];t=b.createElement(e);t.async=!0; t.src=v;s=b.getElementsByTagName(e)[0]; s.parentNode.insertBefore(t,s)(window,document,'script', 'https://connect.facebook.net/en_US/fbevents.js'); fbq('init', '311356416665414'); fbq('track', 'PageView'); [ad_2] Source link
0 notes
Text
Understanding Kidney Failure: Causes, Symptoms, and Treatment Options
Kidney failure, also known as end-stage renal disease (ESRD), is a serious condition where the kidneys lose their ability to function properly. The kidneys play a crucial role in filtering waste, balancing electrolytes, and maintaining overall body health. When they fail, it can lead to life-threatening complications. In this blog, we will discuss the causes, symptoms, and treatment options for kidney failure, along with the importance of seeking medical care from the Best Nephrology Hospital in Bhuj.
What is Kidney Failure?
Kidney failure occurs when the kidneys lose their ability to remove waste and excess fluids from the blood. This leads to a buildup of toxins in the body, causing severe health problems. Kidney failure can be acute (sudden) or chronic (gradual), and both types require immediate medical attention.
If you are experiencing kidney-related health concerns, it is essential to visit a Top Kidney Hospital in Bhuj to get a proper diagnosis and treatment plan.
Causes of Kidney Failure
Several factors can contribute to kidney failure, including:
1. Diabetes
High blood sugar levels damage the kidney’s filtering units over time, leading to chronic kidney disease (CKD) and eventually kidney failure.
2. High Blood Pressure (Hypertension)
Increased blood pressure damages kidney blood vessels, making it difficult for them to function properly. Long-term hypertension is one of the leading causes of kidney failure.
3. Glomerulonephritis
This is an inflammation of the kidney’s filtering units, which can lead to chronic kidney damage.
4. Polycystic Kidney Disease (PKD)
A genetic disorder that causes cysts to form in the kidneys, reducing their ability to function.
5. Urinary Tract Blockage
Kidney stones, tumors, or an enlarged prostate can block urine flow, leading to kidney damage.
6. Infections and Autoimmune Diseases
Certain infections and autoimmune disorders, such as lupus, can damage the kidneys and lead to failure.
Seeking early intervention at the Best Nephrology Treatment in Bhuj can prevent further complications and improve kidney health.
Symptoms of Kidney Failure
Kidney failure often develops gradually, and symptoms may not appear until significant damage has occurred. Common symptoms include:
Persistent fatigue and weakness
Swelling in the legs, ankles, and feet
Decreased urine output or changes in urination frequency
Shortness of breath due to fluid buildup in the lungs
High blood pressure that is difficult to control
Nausea, vomiting, and loss of appetite
Confusion, memory problems, or difficulty concentrating
Muscle cramps and twitching
Skin itching and dryness
If you experience any of these symptoms, consult the Best Nephrologist in Bhuj for an accurate diagnosis and treatment plan.
Diagnosis of Kidney Failure
To diagnose kidney failure, doctors perform several tests, including:
1. Blood Tests
These tests measure creatinine and blood urea nitrogen (BUN) levels, which indicate kidney function.
2. Urine Tests
A urine analysis helps detect abnormalities such as protein leakage or blood in the urine.
3. Imaging Tests
Ultrasounds, CT scans, or MRIs help identify structural abnormalities in the kidneys.
4. Kidney Biopsy
A small tissue sample is taken from the kidney to determine the extent of damage.
Getting diagnosed at a Kidney Hospital in Bhuj ensures access to advanced medical technology and specialized care.
Treatment Options for Kidney Failure:
The treatment approach for kidney failure depends on its cause and severity. Common treatment options include:
1. Lifestyle and Dietary Changes
Patients with mild kidney disease can manage their condition through:
A low-sodium diet to control blood pressure
Reducing protein intake to lower the workload on the kidneys
Staying hydrated and avoiding harmful substances like alcohol and tobacco
2. Medications
Doctors may prescribe medications to:
Control blood pressure
Reduce cholesterol levels
Manage diabetes
Treat anemia
3. Dialysis
Dialysis is a procedure that removes waste, excess fluids, and toxins from the blood when the kidneys can no longer function adequately. There are two types:
Hemodialysis: Blood is filtered using a dialysis machine.
Peritoneal Dialysis: A cleansing fluid is used inside the abdomen to remove waste.
Dialysis is a life-sustaining treatment available at the Best Nephrology Hospital in Bhuj.
4. Kidney Transplant
A kidney transplant is the best option for long-term survival in patients with end-stage renal disease. In this procedure, a healthy kidney from a donor is implanted into the patient. The success rate for kidney transplants is high, especially when performed at a Top Kidney Hospital in Bhuj.
Preventing Kidney Failure
While some causes of kidney failure are unavoidable, adopting healthy habits can reduce the risk of kidney disease:
Control Diabetes and Hypertension: Regular monitoring and medication management can prevent kidney damage.
Stay Hydrated: Drinking enough water helps kidneys flush out toxins.
Eat a Balanced Diet: Reduce sodium, processed foods, and excessive protein intake.
Exercise Regularly: Physical activity helps maintain a healthy weight and blood pressure.
Avoid Overuse of Painkillers: Nonsteroidal anti-inflammatory drugs (NSAIDs) can damage the kidneys over time.
Regular Health Check-ups: Early detection of kidney issues can prevent disease progression.
For expert guidance on kidney health, visit Aayush Hospitals for the Best Nephrology Treatment in Bhuj.
Why Choose Aayush Hospitals for Kidney Care?
Aayush Hospitals is renowned for providing top-tier nephrology care. Here’s why we are the Best Kidney Hospital :
Experienced Nephrologists: Our specialists are highly trained in diagnosing and treating kidney diseases.
Advanced Dialysis Facilities: We offer state-of-the-art dialysis units with expert monitoring.
Comprehensive Kidney Transplant Program: We provide top-notch transplant services with high success rates.
Personalized Treatment Plans: Our approach focuses on customized care for each patient.
24/7 Emergency Care: Our team is available around the clock for urgent kidney-related emergencies.
Conclusion
Kidney failure is a serious but manageable condition with the right treatment and lifestyle choices. Early detection, timely medical intervention, and expert care from the Best Nephrologist in Bhuj can significantly improve the quality of life for kidney disease patients.
If you or a loved one are experiencing kidney-related symptoms, don’t delay seeking medical help. Aayush Hospitals, the Top Kidney Hospital in Bhuj, is here to provide comprehensive and advanced nephrology care.
For consultations and appointments, visit Aayush Hospitals today and take the first step toward better kidney health!
0 notes
Text
Dr L H Hiranandani Hospital Kidney Care: What Makes It the Best?

Kidney diseases are a growing health concern in India, affecting millions of people each year. As cases of chronic kidney disease (CKD) and kidney failure rise, the demand for high-quality kidney care is more crucial than ever. Among the top medical institutions providing world-class nephrology and renal care, Dr L H Hiranandani Hospital Kidney care services stand out for their excellence, advanced technology, and patient-centric approach.
With a team of renowned nephrologists, cutting-edge treatment methods, and a holistic approach to kidney care, Dr L H Hiranandani Hospital Kidney department has earned a reputation as one of the best kidney treatment centers in India. In this blog, we will explore what makes this hospital the preferred choice for kidney patients and why it remains a leader in renal healthcare.
Comprehensive Kidney Care Facilities
One of the key reasons Dr L H Hiranandani Hospital Kidney care is highly regarded is its comprehensive range of services for kidney patients. From diagnosis to treatment and post-surgical care, the hospital provides end-to-end kidney care solutions under one roof.
1. Advanced Diagnostic Services
Early diagnosis plays a vital role in managing kidney diseases. Dr L H Hiranandani Hospital Kidney care department is equipped with state-of-the-art diagnostic tools, including:
High-resolution ultrasound scans
Kidney function tests (KFT)
Blood and urine tests for creatinine and protein levels
CT scans and MRIs for detailed kidney imaging
These advanced diagnostic methods help in detecting kidney problems at an early stage, allowing timely treatment and better patient outcomes.
2. Kidney Transplant Program
Kidney transplantation is one of the most effective treatments for end-stage kidney disease. Dr L H Hiranandani Hospital Kidney transplant program is recognized for its high success rates, skilled surgeons, and advanced post-transplant care. The hospital follows a strict protocol for donor selection, organ matching, and immunosuppressive therapy to ensure safe and successful transplants.
With a dedicated transplant team, the hospital offers both live donor and cadaveric kidney transplants, making it a reliable option for patients seeking life-saving kidney treatment.
3. State-of-the-Art Dialysis Center
For patients with chronic kidney disease who require dialysis, Dr L H Hiranandani Hospital Kidney dialysis unit provides advanced hemodialysis and peritoneal dialysis services. The hospital ensures:
Use of high-quality dialysis machines
Personalized treatment plans for each patient
Skilled technicians and nephrologists monitoring the process
A sterile and comfortable environment to minimize infections
With cutting-edge dialysis services, patients experience fewer complications and improved quality of life.
Expert Team of Nephrologists and Surgeons
A major reason behind the hospital’s success is its team of highly experienced nephrologists, urologists, and transplant surgeons. Dr L H Hiranandani Hospital Kidney care specialists are well-trained in handling complex kidney disorders and employ the latest treatment methodologies.
Some of the key areas of expertise include:
Management of chronic kidney disease (CKD)
Treatment for acute kidney injury (AKI)
Pediatric nephrology services
Kidney stone removal and laser surgery
Preventive nephrology and lifestyle counseling
Patients receive individualized attention and a treatment plan tailored to their specific condition, ensuring the best possible outcomes.
Cutting-Edge Technology and Minimally Invasive Procedures
Technology plays a crucial role in modern kidney care, and Dr L H Hiranandani Hospital Kidney department is at the forefront of innovation. The hospital utilizes:
Robotic-assisted kidney surgery for precision and minimal recovery time
Laser treatment for kidney stones, reducing pain and hospital stays
3D imaging technology for accurate kidney function assessments
AI-driven diagnostics to predict kidney disease progression and suggest personalized treatments
By integrating advanced technology with expert medical care, the hospital ensures the highest standards in kidney treatment.
Personalized Patient Care and Holistic Approach
Unlike many healthcare institutions that focus only on medical treatment, Dr L H Hiranandani Hospital Kidney care adopts a holistic approach. The hospital emphasizes:
Nutritional counseling for kidney patients to maintain a balanced diet
Mental health support to help patients cope with stress and anxiety
Post-transplant rehabilitation programs to enhance recovery
Regular follow-ups and monitoring to prevent complications
This patient-first philosophy has helped countless individuals lead healthier lives even after undergoing complex kidney treatments.
Affordable and Accessible Kidney Treatment
Despite offering world-class kidney care, Dr L H Hiranandani Hospital Kidney services remain affordable and accessible. The hospital provides financial assistance programs, collaborates with insurance providers, and supports government health schemes to make kidney treatments available to a larger population.
Key benefits include:
Transparent pricing for kidney transplants and dialysis
Financial aid for economically weaker patients
Insurance partnerships for cashless hospitalization
By making high-quality kidney treatment more affordable, the hospital continues to serve a diverse group of patients from across India.
Research and Innovation in Nephrology
The hospital is not only a leader in treatment but also in research and innovation. Dr L H Hiranandani Hospital Kidney research center continuously works on:
Developing new medications to slow CKD progression
Advancing artificial kidney technology
Exploring genetic factors affecting kidney disease
Improving kidney transplant techniques
By investing in research and staying updated with global medical advancements, the hospital ensures that patients receive the latest and most effective treatments available.
Success Stories and Patient Testimonials
Many patients have benefited from the high-quality kidney care offered at Dr L H Hiranandani Hospital Kidney department. From successful transplants to life-changing dialysis experiences, numerous success stories highlight the hospital’s excellence in nephrology care.
Real patient testimonials reflect:
Improved quality of life after treatment
Minimal complications and quick recovery
Professional and compassionate medical staff
These positive experiences reinforce the hospital’s reputation as one of the best kidney care centers in India.
Conclusion
When it comes to world-class kidney care, Dr L H Hiranandani Hospital Kidney department is a name that stands out. With its exceptional team of specialists, state-of-the-art facilities, advanced technology, and patient-centered approach, the hospital continues to set new benchmarks in nephrology and renal treatment.
For anyone seeking expert kidney care in India, Dr L H Hiranandani Hospital Kidney services provide the highest level of medical excellence, ensuring the best possible outcomes for patients battling kidney diseases.
Frequently Asked Questions (FAQs)
What makes Dr L H Hiranandani Hospital Kidney care the best in India?
The hospital offers advanced kidney transplants, dialysis, and nephrology treatments with expert specialists and modern technology.
How can I book an appointment at Dr L H Hiranandani Hospital Kidney department?
You can visit their official website or contact the hospital directly for appointments.
Does Dr L H Hiranandani Hospital Kidney care provide financial aid?
Yes, the hospital collaborates with insurance providers and government schemes to make kidney treatment accessible.
What post-treatment care does Dr L H Hiranandani Hospital Kidney department offer?
The hospital provides regular check-ups, dietary guidance, and mental health support for kidney patients.
With its unwavering commitment to excellence, Dr L H Hiranandani Hospital Kidney care continues to revolutionize kidney treatment in India, offering hope and health to thousands of patients.
#hiranandani hospital kidney transplant#hiranandani hospital kidney#hiranandani hospital powai news#hiranandani hospital kidney care#hiranandani hospital powai#hiranandani hospital powai covid#hiranandani hospital reviews#hiranandani hospital#hiranandani powai hospital#hiranandani hospital kidney tranplant
0 notes
Text
Dr. Keyur Dave: The Best Nephrologist and Renal Specialist

Dr. Keyur Dave is one of the leading nephrologists in India, renowned for his expertise in diagnosing and treating a wide range of kidney-related conditions. With years of experience and a patient-centered approach, he has earned a reputation as the best nephrologist in the field, providing exceptional care for conditions like chronic kidney disease (CKD), kidney stones, hypertension, and more.
As a dedicated renal specialist, Dr. Dave offers comprehensive care tailored to each patient’s unique needs. His clinical expertise covers everything from managing acute and chronic kidney diseases to advanced treatments like dialysis and kidney transplants. His holistic approach focuses not only on treating the disease but also on improving the patient’s overall well-being.
Dr. Dave’s patients consistently praise him for his compassionate care, thorough explanations, and clear communication. He ensures that every patient understands their condition and treatment options, making them feel comfortable and supported throughout their journey to recovery.
In addition to his clinical practice, Dr. Dave’s clinic offers state-of-the-art facilities, ensuring that patients receive the most advanced treatments available. Whether you’re dealing with kidney failure, looking for dialysis options, or seeking preventive care, Dr. Keyur Dave is a trusted expert in the field of nephrology.
For more information or to schedule a consultation, call on +918108167176. With his exceptional expertise and compassionate approach, Dr. Keyur Dave is the go-to renal specialist for kidney health in India.
0 notes