#Surgery Anti-Rejection Treatment
Explore tagged Tumblr posts
Text
#liver transplantation market#liver transplantation market price#liver transplantation market report#liver transplantation market research#liver transplantation market size#liver transplantation market shape#liver transplantation market analysis#liver transplantation market forecast#Surgery Anti-Rejection Treatment
0 notes
Note
I saw a comment on your blog that says 'the way you eat does not cause diabetes'...are you able to expand on that or provide a source I could read? I've been told by doctors that my pre-diabetes was due to weight gain because I get more hungry on my anti psychotics and I'd like to fact check what they've told me! Thank you so much!
Pre-diabetes was rejected as a diagnosis by the World Health Organization (although it is used by the US and UK) - the correct term for the condition is impaired glucose tolerance. Approximately 2% of people with "pre-diabetes" go on to develop diabetes per year. You heard that right - TWO PERCENT. Most diabetics actually skip the pre-diabetic phase.
There are currently no treatments for pre-diabetes besides intentional weight loss. (Hmm, that's convenient, right?) There has yet to be evidence that losing weight prevents progression from pre-diabetes to T2DM beyond a year. Interestingly, drug companies are trying to persuade the medical world to start treating patients earlier and earlier. They are using the term “pre-diabetes” to sell their drugs (including Wegovy, a weight-loss drug). Surgeons are using it to sell weight loss surgery. Everyone’s a winner, right? Not patients. Especially fat patients.
Check out these articles:
Prediabetes: The epidemic that never was, and shouldn’t be
The war on ‘prediabetes' could be a boon for pharma—but is it good medicine?
Also - I love what Dr. Asher Larmie @fatdoctorUK has to say about T2DM and insulin resistance, so here's one of their threads I pulled from Twitter:
1️⃣ You can't prevent insulin resistance. It's coded in your DNA. It may be impacted by your environment. Studies have shown it has nothing to do with your BMI.
2️⃣ The term "pre-diabetes" is a PR stunt. The correct term is impaired glucose tolerance (or impaired fasting glucose) which is sometimes referred to as intermittent hyperglycemia. It does not predict T2DM. It is best ignored and tested for every 3-5yrs.
3️⃣ there is no evidence that losing weight prevents diabetes. That's because you can't reverse insulin resistance. You can possibly postpone it by 2yrs? Furthermore there is evidence that those who are fat at the time of diagnosis fair much better than those who are thin.
4️⃣ Weight loss does not reverse diabetes in the VAST majority of people. Those that do reverse it are usually thinner with recent onset T2DM and a low A1c. Only a tiny minority can sustain that over 2yrs. Weight loss does not improve A1c levels beyond 2 yrs either.
5️⃣ Weight loss in T2DM does not improve macrovascular or microvascular health outcomes beyond 2 years. In fact, weight loss in diabetics is associated with increased mortality and morbidity (although it is not clear why). Weight cycling is known to impacts A1c levels.
6️⃣ Weight GAIN does NOT increase the risk of cardiovascular OR all causes mortality in diabetics. In fact, one might even go so far as to say that it's better to be fat and diabetic than to be thin and diabetic.
Dr. Larmie cites 18 peer reviewed journal articles (most from the last decade) that are included in their webinar on the subject, linked below.
#diabetes#t2dm#type 2 diabetes#prediabetes#weight science#weight stigma#fat liberation#fat acceptance#inbox
30K notes
·
View notes
Text

A federal appellate court in Richmond became the first in the country to rule that state health-care plans must pay for gender-affirming surgeries, a major win for transgender rights amid a nationwide wave of anti-trans activism and legislation.
The decision came from a set of cases out of North Carolina and West Virginia, where state officials argued that their policies were based on cost concerns rather than bias. The U.S. Court of Appeals for the 4th Circuit rejected that argument, saying the plans were discriminating against trans people in need of treatment.
It’s the second ruling in favor of trans rights this month from the 4th Circuit, a once-conservative court that has become a trailblazer in the realm of transgender rights. The court was the first to say trans students had a right to use the bathrooms that align with their gender identity and the first to recognize gender dysphoria as a protected disability. Earlier this month, the court said a federally funded middle school could not ban a trans 13-year-old from playing on the girls’ track and field team.
LINK
The 4th Circuit has 15 judges, 1 appointed by Reagan, 1 appointed by George HW Bush, 2 by Clinton, 1 by George W Bush, 3 by Obama, 3 by Trump, and 3 by Biden. The newest Biden appointee, Nicole Berner, was only seated just last month. Berner is a Lesbian, famous for among other things suing Israel in 2000 to force the Israeli government to recognize the children of same sex parents as being equally both their parent's child on documents like birth certificates and passports. She's only the 5th LGBT Judge at the Appeals Court level, 3 of whom are Biden appointees. Elections matter.
#Trans rights#trans healthcare#trans hope#court#lgbt rights#queer#trans#news#information#politics#Thanks Biden
217 notes
·
View notes
Text
EDIT: TME/TMA ARE NOT INTERSEXIST TERMS PLS STOP INTERACTING WITH ME IF YOU BELIEVE THIS THANK YOU - sincerely, an intersex person who actually listens to transfems (including intersex transfems) (no not tme people with pcos/ncah/whatever, you know what i mean)
anyways.. here's the original post:
i regularly see people talk about whether pcos should be considered an intersex condition or not.. and tbh, regardless of what you think, pcos (specifically the symptoms they call virilisation) is treated like an intersex condition in practice anyway
even if they don't actually use the word intersex, so many of the symptoms are completely harmless and instead they're defined by the fact that they're "male" characteristics on a "female", if that isn't intersex then idk what is! having the "wrong" sex characteristics according to society is how intersex is (or at least should be) defined
like hell even the term hirsutism on its own literally only exists because of intersexism, the literal definition of it is "male pattern hair growth"... that's literally just it, the only thing that makes it a "symptom" is being the wrong person to have this kind of hair growth
while intersexness does centre around physical traits, imo it's the way society treats us and reacts to our bodies that actually makes us intersex (as an identity and community), if i wasn't treated this way growing up (and still treated this way today!!), i would probably not have identified as intersex, i think it's important to keep this in mind when looking at how people decide what an intersex condition even is
so with that logic, it makes perfect sense for hyperandrogenic pcos to be considered intersex, the only reason why it isn't is because society benefits from having a large group of women to put below other women while still telling them they have a chance to be "normal" like other women, as long as they put the effort into it.. (by making them spend thousands on stuff like hair removal, weight loss, fertility treatments, anti-androgens, surgery, etc!)
them identifying as intersex in any way completely breaks the illusion, it separates the "male" features from the actually bad symptoms, people would start to question why they have to put themselves through so much effort rejecting their bodies just to be seen as normal, and ofc society does not want that, especially because it makes a lot of money to keep things this way
even the way pcos is diagnosed reeks of this, you could easily be diagnosed with it even if your only problem is high androgens and nothing else (i've been told to get checked for pcos for the crime of: simply having more testosterone than average)
if you tell someone their perfectly harmless features are actually part of this scary disorder that needs treatment then it suddenly becomes a lot easier to manipulate them into finding a "cure" for these harmless features, the pathologisation of intersex features is a huge part of what makes intersex an identity in the first place..
not only that, but ncah (a condition that's more commonly accepted as intersex) is almost always misdiagnosed as pcos, if pcos can look almost exactly like an intersex condition, it is probably intersex. i most likely have ncah, not pcos, and it's treated as almost the same especially before it's actually diagnosed as ncah
and if nothing else, if the intersex "symptoms" of pcos could somehow be found out at birth, and could be "fixed" by a surgery, they absolutely would do it (something that so many intersex children have to suffer through), the only reason why they don't is because they can't, if that isn't enough proof on its own that pcos can be intersex then idk what is!!
the experience of being pathologised for having the "wrong" sex characteristics (both primary and secondary) is what makes intersex a community and grouping these "symptoms" in with actually bad symptoms under one syndrome is not by accident!
#intersex#actually intersex#queer#lgbtq+#intersex rights#intersexism#interphobia#lgbt#queer issues#intersex awareness#pcos#pcosawareness
49 notes
·
View notes
Text
Thony's Character

I know most find Thony to be an irritating character and believe me when I say I'm one of them, but I do think(or at least hope) that last episode's opening is foreshadowing to her becoming head of the Sin Cara Cartel.
Now I know that makes absolutely no sense given that Thony has not a clue on how to run a cartel, let alone how to be a successful criminal. However, this is a show that had a cardio-thoracic surgeon, who hadn't preformed a single surgery in half a decade, do a pediatric liver transplant on her own. So you know suspend disbelief.
Deadline recently did an article where they spoke on the future of the show. In the article, they mentioned that the show runners pitched some ideas on where to take things without Adan no longer being a part of the show and those ideas were "well received".
I get the feeling those ideas involved a more empowered Thony going forward and with Ramona's health in question I can see the writer's finding a way to place Thony in her position.
*There are some big spoilers under the cut at the veryyyyyyyyyyy end so be mindful* I'll put SPOILERS so you know when to get out!
In a earlier episode this season, Jorge's character did theorize that Thony likes the chaos of crime and that's why she's "there." I'm starting to believe that to be true.
In the beginning, when Hyak, Garrett and Arman were lording over her she did the best she could with the circumstances she was in. Personally, I think that's why Thony's character was more likable in season 1, she wasn't choosing this. However, at the end of season 1 she actively made a decision to stay in America. She wanted to run an illegal clinic at the back of their cleaning shop, all while both she and Luca are undocumented.
Thony not wanting to go back to the Philippines because of Marco made sense, she wouldn't have been able to divorce him given the laws there. To be frank, the show's writing never left me feeling she stayed in America because she was running from Marco, but rather she was running towards Arman. There were no scenes post Marco's death where she toyed with the idea of going back to the Phillippines to resume her career as a high powered surgeon and freely have access to the anti-rejection meds Luca would need for the rest of his life.
I can't remember which episode Arman got out of jail, 2 or 3, but in her first conversation at La Habana she begged arman to ask Bosco to move a couple of boxes through Sin Cara's routes. Thony was now actively choosing to engage in illegal activities even though she could go back to the Philippines where not only she could buy these meds legally, she could go back to work as a surgeon, but most importantly Luca would be much safer and not undocumented.
Thony's circumstances post season 1 are her own fault. I think that's why a lot of watchers are irritated with her character. Watching her judge other people, beg people to help her out of her own mess, shame people for not risking their livelihoods to help her or Luca has grown annoying. Season 2 was the start of that type of character writing, but I do think season 3 has been a bit of an improvement.
I know Fiona going to Russo was stupid, but I can see why she did it. Fiona has lived the entirety of her children's lives in America and no trouble like this has come her way. She kept her head down and focused on providing an education for her children. She wasn't perfect, but she surely didn't get into the crosshairs of criminals along the way lol. I can see why Fiona is on edge. Thony is afterall living under Fiona's roof and driving around in her car. I'm sure they split the bills, but still Fiona and by extension Chris and Jaz will pay the price for Thony's responsibilities. I mean Fiona did get arrested and deported because of the hospital fiasco. A situation that wouldn't have occurred back in the Philippines because the life saving treatment Luca needed was not experimental there. Funny how that works.
Ultimately, my hope is that Thony gets some power in her hands because three seasons of her getting tossed around and blaming other people isn't going to keep the show around. She needs to become more likable. Likable characters aren't synonymous to "decent people", but savvy, humorous, loyal, etc. This recent episode's ending with her and Ramona was a damn good start. I'm just praying that the writer's keep that tone going. I want to see Thony own her situation unapologetically and do what needs to be done. Jorge's line earlier about Thony liking the chaos seems to ne an accurate estimation of her character. Now I need Thony to commit to this life and actively make alliances/choices to protect her family, while she delves deeper into the life.
I know the Russo/Jeremy/FBI bomb is on the table waiting to go off, but I need it to stay ticking until season 4. I'm still praying we get a season 4 and we see Thony switch from working for the Sin Cara Cartel to one of the heads of the snake.
SPOILERS
SPOILERS
SPOILERS
SPOILERS
SPOILERS
SPOILERS
SPOILERS
SPOILERS
I can see Jorge surviving the season. He was in an instagram video with our little Lucas' last scene at Thony's house.

I'm not sure Ramona makes it out because Kate posted an instagram video while they still filming episode 10. that made it seem like she was now working on a new project. Granted my Spanish is not great, but I could make out her asking for well wishes on her new project.
I unfortunately don't think Nadia makes it out, because the actress posted a farewell insta. Then there was that picture that Elodie posted and then IMMEDIATELY took down. Yikes on bikes!

So my prediction is Jorge and Thony are the ones left standing to run the cartel. I saw Jorge's face on Russo's board, so I think moving forward they'll be doing everything they can to get out from under the FBI's crosshairs.
Maybe Ramona takes the fall to protect Jorge and to make sure Violetta has him. Either way, I just DON'T want Thony behind bars. I'm tiredddddddd of her being metaphorically on her back, always fighting to get up on her feet, I want her to end the season empowered. Last season ended that way, but I think given Adan's health coming into the new season they had to pivot.
Sorry for the LOOONNNNGGGGG post :)
#the cleaning lady#thony de la rosa#arman morales#nadia morales#fiona de la rosa#armany#thony x arman#tcl#jorge sanchez#ramona sanchez#kate del castillo#elodie yung#eva de dominici
20 notes
·
View notes
Note
hey there cav. this is sort of a fraught question but. how do I engage with psychiatry when I'm antipsych? I need treatment but I have so much distrust and I feel like it's all bullshit. I don't really have a support system and there's few peer support resources in my area. I can't do this myself but I cant trust this system. soooo... tips for finding therapists that don't suck & getting the most of it? really appreciate your blog and posts, thanks
thank you for entrusting this message to me, I appreciate it! I have answered questions like this a few times before (they're buried somewhere, if you can't find them in my "ask" tag, lmk and i'll try to dig them up!). it's definitely fraught inasmuch as we're never (as people who hate psych but need specific, urgent support that communities aren't by default set up to provide) going to get an answer that we 100% want, but also very not-fraught inasmuch as most of us agree that surviving in this sea of partiality is something we can do together, with love and nonjudgement.
so, for context: i was in therapy - first behaviorist OT as a toddler and elementary school child, and, beginning at 7, talk therapy - nonconsensually basically from the time I could remember until adulthood. i likely would never have tried it again, except for the small hiccup of needing letters for Transing Genders. so, this was when i first sought out "trans affirming care," as it were, and i didn't expect much. i went to my college's health center and got a list of possible providers, and ended up getting an excellent PCP, as well as a therapist who was a genuine cis accomplice: she wrote letters for Mad/psych disabled clients whose genders wouldn't typically qualify us for surgery/hormones in the eyes of the M/PsyIC. i did not share with her the things i "ought" to have shared, but she knew I had survived abusive therapy / forced institutionalization, and accepted that, and accepted my cynicism along with it. i was also first genuinely understanding foucault at this time, so rest assured i was quite a little shit (affectionate).
when she left to practice elsewhere, i went to a therapist at the same practice she recommended. she was fine, but not what i needed. by this time, I'd gotten the requisite procedures, so my therapy attendance wasn't required. i basically just ghosted this new therapist around the time covid hit.
when i came to grad school, i initially wasn't looking for therapy, though i had idly considered something for OCD, which I was (and am) managing in part through medication. after getting outright rejected for, essentially, being too crazy for normie OCD therapy, i directed my search specifically for Mad/abolitionist providers. i began by going through some of the archives of places like the National Queer and Trans Therapists of Color Network, and some people who have posted guest articles on Mad in America / The Fireweed Collective -- many are providers seeking to disrupt/abolish the system. That provided some leads, though no openings (there are very few of them, and they are, understandably, in high demand).
I then turned to my community connections: over the years, I've amassed a large number of Mad colleagues in various fields. Many are a half-step from radical/antipsych circles, so I asked them. This time, I asked specifically about a possible therapist who was interested in critiques of "eating disorders" as a category, who had an abolitionist, harm-reductionist, and anti-"health" approach to care, and who, accordingly, refused to cooperate with institutions of psychiatric confinement. I was directed to a list of people, of whom my current and beloved therapist / colleague / comrade was the first to respond.
my trajectory with her has been a steady building of trust through a shared ebbing and flowing of closeness, frustration, enlightenment, and curiosity. it has been close to a year and a half now, and we only began speaking frankly about more "dangerous"/"risky" topics a few months ago. early in our relationship, i did a great deal of boundary-testing, and reacted with anger and shutdown the first time she asked a question that proved risky/activating for me. my biggest recommendation when engaging with ANY provider is to ask them explicitly, repeatedly, and critically about their relationships with your own risk/harm level, their ongoing history wrt patient institutionalization / "referrals" to "higher levels of care". take note about the way they reference past patient situations, as well as their own past experience. take note of how they respond when you choose not to provide the information they seek.
also take note of what info they're willing to provide upfront, including at a consult: what methodologies do they work with, what was their training, how do they feel about said training? what are their politics? ask whoever recommended them to you, too. look at reviews. this is obvious -- what might not be is looking up their work on google scholar. who do they cite? what do they advocate, who do they associate themself with?
i think that it's also a good idea to ask them explicitly about their experience in other/"higher" levels of care - most therapists have done some kind of rotation during their education, often in a hospital, group home, halfway house, similar. if you have ever been institutionalized, you may have even spotted / been abused by some! observe how they discuss these experiences. take note.
if and when you've established this person as someone you want to continue working with, trust notwithstanding, think personally about what you are actually looking for. they will ask you about your goals, surely, but it's a good idea first to think about your own personal goals outside of the verbalized relationship between you two. do you need a confidante, and of what kind? what sort of accountability do you need, and what are you willing to try to figure that out? *what are you paying this person for that you feel others cannot or will not do*? what part of this person's expertise can be of use to you, and for how long?
i think one interesting approach to therapy is to regard the provider as a teacher - they're there to share knowledge with you, and you're free to accept or reject it. they have some kind of training/experience you don't have, and you seek them out because you think it may be of use in your own life, and perhaps even to redistribute that knowledge if and when you gain it. at the same time, you also have knowledge to share with them - not to be extracted, but to be incorporated in their own work and practice. the biggest insight on the practice of good therapy i've gleaned is that, ideally, you're both teaching and learning forever. this is true of all good relationships. there is an exchange of knowledge based on shared trust - values - priorities. once you are in a space where you know that this person shares your general relational orientation (aka, doesn't want to institutionalize, etc. you and people like you) it's possible to begin sharing knowledge in a way that benefits from this imposed structure. the benefit, imo, is that it's okay that you "monopolize" the convo and direct the knowledge-production toward your needs, because that's the service you're paying for!
i guess, to close, i'll return to the classic Mad Pride framing of us as "psych users/consumers." this isn't the perfect term, but i think it's enlightening, as we can and should be able to seek out services that work for us. just like i go to a person who knows wtf they're doing when, say, i need my nails done or my car fixed, so too do i go to an expert interlocutor when i am interested in developing my self-/relational knowledge and/or am seeking support in times of emotional tumult. this doesn't confer them a status as superior to me, just like someone isn't superior to someone else by being a nail tech or mechanic. it simply means that we are entering into a relationship where my needs and their expertise meet. seek a therapist who understands this, and understands themself as someone who can learn from you, too. this approach to therapy, and to care, mean that you can't just throw someone away or lock them up when they say things you don't like. it means that, even in those moments, there is something to be learned, and that the relationship will grow in that process of edification.
#i...this was a Big Boy essay. prepare yourself#antipsychiatry#madness#ask#anonymous#world healing#also i have therapy friday if you want me to ask mine about her connections to ppl#most of which arein California but not exclusively
90 notes
·
View notes
Text
Erin Reed at Erin In The Morning:
Last week, two anti-transgender provisions were quietly added to the National Defense Authorization Act in the Senate. These provisions were included in the “must-pass” budget bill with the help of Senator Joe Manchin, who cast the tie breaking vote to include the provisions in each instance. The bill was then recommended to the full Senate on a 22-3 vote, with many Senate Democrats voting to advance it despite the anti-trans provisions. When asked about the vote by a reporter from The Independent, Senator Manchin expressed confusion about his own vote but then doubled down, expressing support for federal restrictions not just on the military but on all gender-affirming care using funding bills, a major anti-LGBTQ+ Project 2025 policy.
The two provisions in question would use federal funding mechanisms to restrict transgender care for those in the military. One provision would bar the government from paying for transgender surgeries deemed medically necessary for transgender soldiers. Another provision would bar TRICARE, the insurance service for U.S. military service members, from covering any gender-affirming care for those under 18. Both provisions would significantly impact transgender service members and their families, as obtaining care can be difficult for those enrolled in the military without federal support.
Both provisions narrowly passed with a 13-12 vote. Many Democrats on the Senate Armed Services Committee, responsible for the bill, moved it forward despite its anti-trans amendments. Only Democratic Senators Elizabeth Warren and Jack Reed, alongside Republican Senator Tom Cotton, voted against it in the committee. By favorably reporting the bill out of committee, anti-transgender federal funding bans are closer to becoming law than in previous budget battles, where similar provisions were added to House bills but ultimately rejected by the Senate and President Biden.
[...] However, a spokesperson followed up not only defending the vote, but espousing a federal funding ban on all gender affirming care, stating, “Senator Manchin believes that Americans who want to serve our country and can meet the standards should have the chance to do so. However, taxpayer dollars should not be used to pay for any services or treatments that are associated with gender transition.”
[...] None of the anti-trans funding bans targeting health insurance, healthcare research, the Food and Drug Administration, the Department of Education, and more were passed in the budget showdown. These provisions ranged from sports bans to healthcare funding bans around the provision of gender-affirming care. One bill even aimed to defund children’s research hospitals if they provided gender-affirming care. The impacts of such bills would affect health insurance, hospital systems, and doctors providing transgender care nationwide.
These bills are key components of the anti-LGBTQ+ provisions found in Project 2025, a Heritage Foundation document outlining a new path for the United States. This document aims to empower the executive branch, remove reproductive healthcare rights, and target LGBTQ+ people nationwide. It seeks to institute an analogue to the Hyde Amendment targeting abortion providers, calling for an end to all “public moneys for transgender surgeries,” though many of the funding provisions in recent fights go even further, targeting all transgender care.
Sen. Joe Manchin (I-WV) has come out in support of bans of federal funding for all gender-affirming care, thereby spitting on the trans community.
#Joe Manchin#Transgender Health#Gender Affirming Healthcare#Transgender#US Senate#118th Congress#Project 2025#NDAA#Hyde Amendment
10 notes
·
View notes
Text
Understanding the Long-Term Effects of Ulcerative Colitis
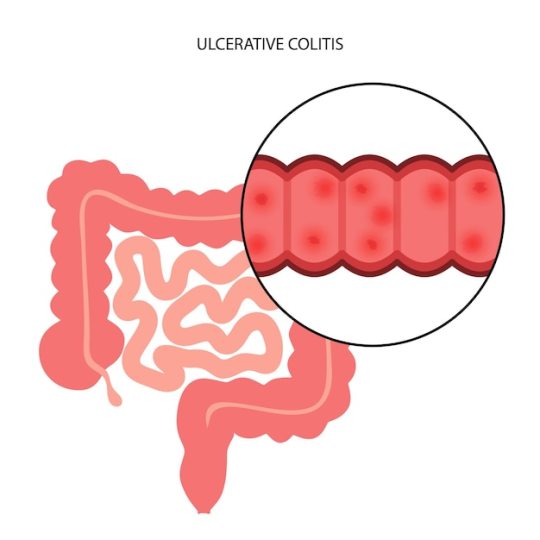
A chronic inflammatory bowel disease (IBD) that affects the colon (large intestine) and the rectum is called ulcerative colitis (UC). Many individuals get treatment to deal with their side effects, this medical condition can have lasting effects that affects many pieces of a person's life. The long term effects of the condition will be discussed in this article, with possible risk and the management techniques.
Effects of Chronic Inflammation
Inflammation over time in the colon causes long-term damage, which is one of the main concerns related to ulcerative colitis.
Risk of Colorectal Cancer: People who experienced UC for longer than 8 to 10 years are more likely to develop colorectal cancer due to ongoing inflammation of the colon.
Tissue Scarring: Prolonged inflammation can result in colon tissue scarring, which can lead to problems like strictures (colon constriction) and restrictive symptoms.
Severe Flare-ups: As UC progresses, a person's colon may enlarge rapidly and more frequently. This can result in challenges including toxic megacolon, a potentially fatal illness.
Effects on the Digestive Systems
Ulcerative colitis can cause major, long lasting changes to the digestive system.
Nutritional Deficiencies: Iron, calcium, and a lack of vitamin D can result from impaired nutrient caused by steady irritation and recurrent diarrhea.
Dehydration: UC patients frequently struggle with dehydration, especially during flare-ups, which can be set on by tireless diarrhea.
Changes in Bowel Function: Many UC patients could require a medical surgery to remove all or a part of their colon, which will modify their capacity to pass stool. The body's ability to control the digestion of water and supplements might be affected by this.
Systemic Health Improvement
Ulcerative colitis doesn't just affect the colon; it can also affect different regions of the body.
Joint pain (Joint Irritation): A great deal of people with UC experience joint inflammation, which brings side effects like joint inflammation.
Skin Conditions: UC can lead to skin issues like difficult red bumps known as erythema nodosum and ulcerative skin lesions called pyoderma gangrenosum.
Inflammation of the eye, like in uveitis and episcleritis, is more common in patients with ulcerative colitis.
Impact on the Brain and Heart
A constant sickness, for example, UC can negatively affect one's mental health.
Stress and Tension: Dealing with a condition with painful and unpleasant side effects that is unstable brings higher pressure and nervousness.
Depression: There is a higher possibility of creating depression because of the chronic nature of ulcerative colitis (UC) as well as expected limitations on everyday activity and interaction with others.
Body Image Issues: Certain people may have issues with their body image because of weight loss, actual look of their condition, or medical surgery, (for example, a colectomy or the requirement for a stoma).
Perspectives Affecting Quality of Life
An individual's personal satisfaction can be affected by UC in various areas of day to day existence.
Physical Restrictions: Exhaustion, continuous bowel movements, and pain during eruptions can cause limitations on actual work and create some issues for social or professional commitments.
Dietary Limitations: To control their side effects, many people with UC should stick to diets that reject explicit things that could cause eruptions.
Surgical Results: A colonoscopy, or the expulsion of the colon, might be important for specific UC patients at some point. This procedure can change a patient's bowel designs and require long lasting modifications.
Extended-Term Care and Therapy
Ulcerative colitis cannot be cured, long-term care can greatly enhance results.
Medication: Immunosuppressants, biologics, and anti-inflammatory meds are habitually used to reduce inflammation and treat side effects for an extended timeframe.
Continuous Monitoring: To follow the course of the condition and identify any possible issues, like colorectal disease, from the beginning, patients should have routine colonoscopies and other diagnostic testing.
Way of life Changes: Reducing pressure, eating a balanced diet, practising habitually, and stopping smoking are great ways of working on the side effects of ulcerative colitis (UC) and reducing its eruptions.
Don't forget to read our next article on''Ulcerative Colitis: Causes, Symptoms, and Key Factors."
There is something else to ulcerative colitis besides eruptions and side effect the board; it is a persistent sickness. Dr Nisarg patel best gastroenterologist in sids hospital surat, will give you the best advice and cure for your IBD issue. Patients and medical care experts can make better designs for decreasing complexities, upgrading personal satisfaction, and deflecting risks by having a better understanding of the disease's drawn out effects. Living with ulcerative colitis can be figured out how to consider a satisfying existence with the right care, checking, and lifestyle changes.
2 notes
·
View notes
Text
How to NOT fix the opioid crisis - refuting a bad podcast episode
I listened to the episode “Fixing the Opioid Crisis ft. Rep. Brittany Pettersen” on The New Liberal Podcast. Pettersen is clearly a crackpot, and the host is oblivious.
My many complaints (a bit rough, only partially cited):
First, the phrase “opioid epidemic” is already misleading and outdated. It frames the problem as caused by the availability of opioids, and frames opioids as bad. For a rejection of the “opioid epidemic” framing, see this Leo Beletsky presentation.
One of the few good things: Pettersen wants better funding models for both naloxone (e.g. via Medicaid) and addiction treatment. I agree.
Pettersen says we should go after “traffickers,” but then it sounds like she wants to crack down on ALL drug sellers. It also sounds like she wants to consider implementing greater mass government surveillance of social media across the board (wtf), to crack down on people buying and selling what I infer are small amounts of drugs (???). This is irresponsibly unclear at best, and probably just stupid and bad.
I note, it has already been shown from multiple convergent lines of evidence that arresting drug sellers increases local overdoses (recent example).
Moreover, many anti-drug-dealer laws harm drug users, in a great many increasingly evident ways—see DPA’s “Rethinking the Drug Dealer." She ignores all this. Countless drug users share drugs with one another frequently. They are all at risk of being targeted as “drug dealers.” This is the #1 reason people don’t call 911 when they see an overdose, or why they delay calling 911—they fear police harassment and investigation. (And Good Samaritan laws only cut down a tiny fraction of this problem. Decriminalization, including for low-level dealers, is also needed.) (See parts of the Beletsky video on some of this, as well as DPA.)
Unlike Republicans, Pettersen at least acknowledges that most fentanyl comes into the US through legal ports of entry, not illegal border-crossing. But she proposes no realistic notion of how to meaningfully reduce the fentanyl coming through legal ports. There’s no reason to take this seriously. In practice this sounds like it’s just a less racist version of the same failed drug interdiction efforts that have already been discredited. Only a tiny amount of the fentanyl is ever intercepted successfully. Nobody has ever proposed a feasible way to do it, and she seemingly offers nothing new. Even if they could intercept the fentanyl, other drugs (almost surely drugs on par with fentanyl or more dangerous) (e.g. nitazenes) would take its place, or possibly fentanyl (or other synthetic opioid) production would shift to domestic. For some discussion citing a few drug policy experts, see this Vice article.
She also makes zero mention of the fact that there was no fentanyl crisis until the government cracked down on prescription opioids and heroin. The evidence has increasingly grown over the last decade that these crackdowns made everything immensely worse.
She supports Prescription Drug Monitoring Programs, which have been increasingly shown to cause harm, and there’s basically no evidence they do any good. She thinks ONLY overprescription causes problems (or at least this is basically all she talks about, regarding prescriptions), and totally neglects how refusals of prescriptions, and forced tapering of patients already on prescriptions, has caused devastation to so many pain patients. She wants even MORE punishment against doctors who “overprescribe,” with no acknowledgement of how punishing doctors has already caused devastation and led many doctors to just abandon pain patients, or give Ibuprofen to surgery patients (no, seriously!), and much more. She thinks we can tell a doctor is “overprescribing” if they prescribe more than their peers in the area, which is ridiculous. She is going to make already horrible problems even worse. For some discussion of how deprescribing has caused terrible problems, see linked below (1) Zachary Siegel, and (2) Stefan Kertesz.
At no point does she ever mention policies of other countries. She never mentions Canada’s safe supply movement. She never mentions drug user advocacy for methadone in the Netherlands. She never mentions Finland’s drastic reduction in homelessness. She never mentions Portugal’s decriminalization. She never mentions Switzerland’s heroin-assisted treatment program. If only other countries besides America existed, which we could draw ideas and evidence from!
She seems vaguely friendly to decriminalization, which is better than some other politicians, but she never comes out and says it. I can only assume this reticence is because of political cowardice. Even conservatives and cops tend to say boilerplate stuff like “We can’t arrest our way out of this crisis” these days, but it means nothing if in practice they uphold criminalization. Also she never once mentions harm reduction, except naloxone—nothing about needle exchange, nor supervised consumption sites, nor drug-checking, and certainly no legal regulation. Pathetic.
She says there are no lobbyists on the issue of opioid addiction, nobody who makes money on it. This is a bizarre false statement. Many abstinence-only rehab providers make a lot of money. Many methadone clinic providers make a lot of money (and for many, their financial model would be threatened if the draconian restrictions on methadone access were lifted, so there’s an incentive against helping patients gain access----though I think Petterson might be in favor of making methadone easier to get?). Many people and organizations (often corrupt ones) have been seeking and making a lot of money in the various massive lawsuits against pharmaceutical companies, leading to a bizarre mixture of true and false allegations against the companies, and misuse of funds obtained.
Pettersen says doctors who prescribe drugs need more education on addiction. I agree. But what sort of education on addiction? She doesn’t say. The anti-opioid hardliners who have been extremely influential for the last 10 years often believe ludicrous things, like equating addiction with physical dependence (a mistake prevalent in the anti-opioid-company lawsuits), or they deny the existence of pseudoaddiction. For a pretty decisive case that pseudoaddiction is real, see Scott Alexander's "Against Against Pseudoaddiction."
Pettersen correctly points to lack of adequate access to addiction treatment. But she doesn’t mention the prevalence of pseudoscience and abuse in addiction treatment. Getting more people into pseudoscientific and abusive rehab would do no good—it needs to be good treatment.
More facts she never mentions: Opioid prescriptions have been cut in HALF over the last 10 years. And yet (1) prescription-opioid-involved deaths (which always mostly involved other drugs too—mixtures, not just one opioid, and largely among non-patients) have flattened out, and more importantly (2) total opioid overdoses have skyrocketed to absolutely unprecedented heights. Opioid prescription reduction most likely caused this problem in the first place. And she wants to do MORE of it.
Toward the end, Pettersen and the host pat her on the back for how sane and bipartisan she is. They’re drinking the Kool-Aid. This is just more prohibitionist ideology, in its modern watered-down more politically-correct form. They do not defend drug prohibition with evidence or arguments. They rig the whole framing of the issue, to put serious questioning off the table, so it doesn’t even occur to anyone that something different and better is possible. It’s vile bullshit, don’t be fooled.
4 notes
·
View notes
Text
What To Know: Kidney Transplant FAQ
The kidney transplant process can be long and difficult, with a lot to think about. It is encouraged to get on the transplant waitlist as quickly as possible. Asking questions can help you determine if a transplant is a good fit for your lifestyle.

DO I NEED A SUPPORT SYSTEM?
A kidney transplant is major surgery and a support system plays a vital role before, during, and after transplantation. Both physical and mental support can be provided by a spouse or partner, family, or friends. This is a journey that someone cannot do alone.
WHAT DOES IT COST?
What you are required to pay depends on your insurance coverage. Medicare covers about 80% of costs associated with a transplantation. Private insurance and Medicaid may cover some costs as well. Multiple insurances can be used together to cover more of the expenses. Your social worker, transplant center and financial coordinator will help figure out the exact cost. While it can be an expensive process, transplant are obtainable with insurance.
HOW DO I FIND A LIVING DONOR?
One of the best ways to find a living donor is by sharing your story. Talk to friends, family, or coworkers about what you are experiencing and how they can help. Share your story at work, in your place of worship, on social media or any other place where you can reach others. Your transplant team can assist in what information is and is not beneficial to communicate to others.
WHAT IS LIFE LIKE AFTER TRANSPLANT?
A kidney transplant can feel like a second chance at life. It’s important to know that a transplant is a treatment option, not a cure. You will need to take care of your new kidney with anti-rejection medications and maintaining a healthy lifestyle. Your transplant team will provide directions for how to care for your body after surgery. You’ll likely start returning to normal activities within a month after your transplant, with more freedom to do what you enjoy.
The sooner you start the process to receive a transplant, the better your long-term health outcomes. You can go through this process at one, or multiple, hospitals. See a full list of transplant centers in Ohio here. Watch the Roadmap for Transplantation series on YouTube to learn more.
2 notes
·
View notes
Text
The Role of Immunosuppressive Therapy in Heart Transplants: What Patients Need to Know
For patients who undergo heart transplant surgery, the journey to recovery involves more than just the procedure itself. A crucial part of the healing process is immunosuppressive therapy. This therapy helps prevent the body from rejecting the new heart, which is essential for a successful transplant outcome.
As many patients look for the best care, the importance of choosing a reliable facility, such as the best heart transplant hospital in India, can’t be overstated. Here’s everything patients need to know about immunosuppressive therapy, explained in a simple and friendly manner.
Why is Immunosuppressive Therapy Necessary?
When someone receives a new heart, the body recognises it as a foreign object. The immune system, which usually works to protect the body from infections and harmful cells, may start to attack the transplanted heart. This natural response is called rejection, and without proper intervention, it can harm the new heart and endanger the patient’s life.
Immunosuppressive therapy helps prevent this rejection by “calming down” the immune system. By reducing the body’s immune response, these medications allow the new heart to stay healthy and continue functioning without being attacked. This treatment is lifelong, meaning patients will need to take these medications daily for as long as they have their transplanted heart.
How Does Immunosuppressive Therapy Work?
Immunosuppressive drugs work by lowering the immune system’s ability to identify and attack the new heart. Different medications target various parts of the immune system. Usually, a combination of immunosuppressive drugs is prescribed to provide a balanced and effective response. This combination approach minimises the risk of rejection while lowering the risk of side effects from any single medication.
The main drugs used in immunosuppressive therapy include:
Calcineurin Inhibitors: These are the backbone of most transplant therapies. They prevent immune cells from activating, helping to lower the overall immune response.
Corticosteroids: Often used in the initial stages, these help reduce inflammation and prevent rejection. They may be reduced or even stopped over time to lower the risk of side effects.
Anti-Proliferative Agents: These drugs prevent immune cells from multiplying, making it harder for the body to mount a strong immune attack on the transplanted heart.
Managing Side Effects
While immunosuppressive therapy is necessary, it can cause side effects. Common side effects include increased risk of infections, high blood pressure, weight gain, and weakened bones. Since these medications lower the immune system, patients may become more susceptible to infections.
To manage these side effects, doctors may recommend lifestyle changes, such as a balanced diet, regular exercise, and maintaining good hygiene practices to reduce the risk of infections. In some cases, additional medications may be prescribed to counter specific side effects. Staying connected with the healthcare team and reporting any unusual symptoms is key to managing these challenges effectively.
Conclusion
Immunosuppressive therapy is the cornerstone of life after a heart transplant. While it presents some challenges, it is essential for preventing rejection and ensuring the health of the new heart. By understanding how these medications work, managing side effects, and committing to their treatment plan, patients can focus on recovery and enjoy their second chance at life. Receiving care at the best heart transplant hospital in India can make a world of difference in providing quality support throughout this journey.
0 notes
Text
Kidney Transplant in Pune: A Complete Guide to a Life-Changing Treatment
A kidney transplant is one of the most effective treatments for end-stage kidney disease, offering patients the chance to regain a normal and healthy life. In Pune, kidney transplant services are at the forefront of medical advancements, providing high success rates and improved patient outcomes.

Why Consider a Kidney Transplant?
Kidney failure, often caused by conditions like chronic kidney disease, diabetes, or hypertension, leads to the gradual loss of kidney function. When both kidneys fail to work, dialysis becomes the temporary solution. However, for many, a kidney transplant offers a more permanent and liberating option.
Transplantation allows patients to stop dialysis and lead a healthier, more active life. A successful kidney transplant can:
Restore kidney function
Improve quality of life
Reduce dietary restrictions
Decrease the need for constant medical interventions
The Kidney Transplant Process
Evaluation and Preparation: Before a transplant, the patient undergoes a thorough evaluation to determine eligibility. This includes blood tests, matching for compatibility with a donor, and assessments to ensure the patient is healthy enough to undergo surgery.
Finding a Donor: Kidney donations can come from a living donor, often a family member or close relative, or from a deceased donor. Matching factors like blood type and tissue compatibility are crucial to avoid rejection.
The Surgery: During the transplant, the healthy kidney is placed into the patient’s body. The surgery typically takes several hours and requires a skilled transplant team.
Post-Transplant Care: After surgery, patients need close monitoring to ensure the new kidney is functioning well. Anti-rejection medications are prescribed to help the body accept the new kidney.
Why Pune for Kidney Transplants?
Pune is home to some of the country’s top nephrologists, transplant surgeons, and state-of-the-art medical facilities, making it an excellent destination for kidney transplants. Hospitals in Pune are equipped with advanced technology and a skilled team that ensures the entire transplant process is as smooth as possible.
Benefits of Choosing a Kidney Transplant
Improved Survival: A kidney transplant significantly increases the lifespan of patients compared to staying on dialysis.
Better Quality of Life: Transplant patients often experience increased energy levels, better mental health, and fewer dietary restrictions.
Financial Savings: Over time, a kidney transplant can be more cost-effective than long-term dialysis.
Life After a Kidney Transplant
After a kidney transplant goes well, patients can anticipate going back to their regular lives. Long-term success, however, depends on leading a healthy lifestyle, adhering to prescription regimens, and scheduling routine follow-up appointments with medical professionals.
Conclusion
Patients suffering from damaged kidneys can have far better lives after receiving a kidney transplant. You will receive individualized, excellent treatment from examination to recovery with Dr. Sandeep Morkhandikar’s experience in Pune, guaranteeing the best possible outcome for your transplant journey
Schedule your consultation today at Fertiprotect Superspeciality Center, Pune, and take a step towards better kidney health!
#best nephrologist in pune#dialysis specialist in pune#kidney transplant in pune#Kidney doctor in Pune#Renal specialist Pune#Pune nephrology doctor#Top kidney specialist Pune
0 notes
Text
Dialysis vs. Kidney Transplant: Comparing Costs, Risks, and Benefits

Kidney disease is a life-altering condition that forces patients to make critical decisions regarding their treatment. The patient ultimately suffers from both conditions, whether it is dialysis or a kidney transplant. This raises the patient's curiosity about the potential risks associated with each condition and the differences in treatment costs between them. Each approach, Dialysis vs. Kidney Transplant has its own set of advantages, risks, and financial implications, making it crucial for patients and their families to weigh their choices carefully. In this blog, we will delve into the comparison between dialysis and kidney transplant, exploring their costs, risks, and benefits.
What is Dialysis vs. Kidney Transplant?
Dialysis is a treatment that artificially removes waste products and excess fluids from the blood when the kidneys can no longer perform these functions. People with end-stage renal disease (ESRD) typically undergo it in a hospital or specialised clinic, and it can be a lifelong necessity.
On the other hand, a kidney transplant involves surgically placing a healthy kidney from a donor into a patient whose kidneys are no longer functioning. A successful transplant can restore nearly normal kidney function, eliminating the need for dialysis.
But which option is better? Is a kidney transplant better than dialysis in every situation, or are there scenarios where dialysis might be the more suitable choice?
Costs: Weighing the Financial Implications
Cost is one of the most important factors influencing the choice between dialysis and kidney transplant. Dialysis can be expensive, particularly over the long term. According to The National Kidney Foundation reports, the average annual cost of dialysis in the United States is approximately $90,000. Dialysis is a continuous treatment; these costs accumulate, potentially reaching hundreds of thousands of dollars over a patient's lifetime.
In contrast, the cost of a kidney transplant is front-loaded. The initial surgery, hospitalisation, and follow-up care can amount to approximately $250,000. However, anti-rejection medications, which can total around $10,000 to $20,000 annually, primarily contribute to ongoing costs after the transplant. Over time, these expenses may still be lower than the cumulative cost of long-term dialysis.
Risks: Balancing immediate and long-term health
When comparing dialysis vs kidney transplant pros and cons, risks play a pivotal role. Dialysis is generally considered a safer option with fewer immediate risks. However, long-term dialysis can lead to complications such as cardiovascular disease, infections, and reduced quality of life.
On the other hand, a kidney transplant comes with significant surgical risks, including infection, rejection of the donor kidney, and complications from anesthesia. The risk of death in the first year post-transplant is higher than for patients on dialysis. However, for many patients, the long-term benefits of a successful transplant—such as improved quality of life and longer survival—outweigh these initial risks.
Learn More..
#sierra leone#best hospital sierra leone#freetown#best hospitals in freetown#cost of a kidney transplant#kidney transplant#Dialysis
0 notes
Text
Organ Transplant: Saving Lives Through Donation and Medical Advancement

The History of Organ Transplant
The first successful organ transplant took place in 1954 when a kidney was transplanted between identical twins in Boston. This groundbreaking surgery paved the way for other transplant procedures. Throughout the 1950s and 60s, doctors continued experimenting with kidney transplants with varying success rates due to the body's natural immune response. It wasn't until the 1980s that anti-rejection drugs like cyclosporine were developed, allowing transplants between non-related donors and recipients to become more widely performed and successful. Types of Transplants
Kidneys are the most commonly transplanted organs, with over 80,000 kidney transplants performed in the United States alone between 1988-2018 according to the Organ Procurement and Transplantation Network. Other organs that can be transplanted include the liver, heart, lungs, pancreas, intestine, and thymus gland. Tissue such as corneas, skin, bone marrow, heart valves, veins and ligaments can also be donated. Organ Donation
For a Organ Transplant to occur, a donor must first agree to donate their organs upon death. In the United States, individuals can register as organ donors through their state's department of motor vehicles or on the Organ Donor Registry. Family consent is also required before organs can be recovered. Once a donor is declared brain dead but their heart is still beating, doctors work to preserve the organs until they can be surgically removed and transplanted into recipients waiting for a life-saving gift. Waiting for an Organ
The need for donated organs far outweighs the available supply. As of January 2020, there were over 113,000 candidates on the U.S. national transplant waiting list according to the Organ Procurement and Transplantation Network. The waiting time for a donated organ varies depending on blood type, organ size match and medical urgency. On average, 20 people die each day from the lack of available organs. Children have a higher mortality rate while waiting, with nearly 5,000 children in need of a transplant. Advancements in Living Donation
While deceased donor transplants remain the standard, advancements have been made to increase living donation options. In kidney and portions of liver or lung donation, a healthy person can elect to donate an organ or parts of organs to recipients in need. The recipient's prognosis is often better when the donated organ is still functioning at the time of transplant rather than being recovered from a deceased donor. Some donors are emotionally motivated to help a loved one, while others choose to altruistically donate to a stranger. Either way, living donation has elevated many from waiting lists to restored health. The Future of 3D Bioprinting and Xenotransplantation
Scientists are exploring new frontiers to close the organ supply gap through bioprinting and cross-species transplantation possibilities. 3D bioprinting uses inkjet-like printers to deposit cells layer by layer, building functional organs. Researchers have printed heart tissue, liver buds and kidney structures, with the goal of fully printed transplantable organs in development. Meanwhile, some scientists are testing the use of organs from genetically-modified pigs, known as xenotransplantation. Pig heart valves and skin are already used as human transplants with promising research underway for whole organs. If effective, bioprinting and xenotransplantation could revolutionize transplant availability in coming decades. The Impact of a Transplant
For recipients who receive that lifesaving gift from a donor, organ transplantation means a second chance at life. Kidney transplant patients can discontinue dialysis treatments and greatly improve their quality of living without being tethered to a machine. Liver recipients are cured of end-stage liver disease and related conditions. Heart transplant patients are no longer constrained by heart failure.
lung transplants restore breathing abilities for people suffering from cystic fibrosis, COPD or pulmonary hypertension. The impact of organ donation should not be underestimated - for both recipients who receive more days with their families, and donors who give the ultimate gift so others may live on. Continued medical progress and donation awareness will help even more individuals overcome organ failure in the future.
Get more insights on Organ Transplant
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)
#Organ Transplant#Organ Donation#Transplant Surgery#Organ Recipient#Donor Organs#Kidney Transplant#Liver Transplant#Heart Transplant#Transplant Medicine
0 notes
Text
Benefits Of Exosome Therapy

Exosome therapy, a cutting-edge regenerative medicine treatment, has gained popularity in recent years due to its numerous benefits. Exosomes are small vesicles secreted by various cells in the body, and they play a crucial role in cell-to-cell communication. This therapy involves using exosomes derived from stem cells to promote healing and regeneration in the body. If you're intrigued by exosome therapy and want to know more about finding the right clinic and hearing success stories from patients, you've come to the right place.
What Is Exosome Therapy?
Exosome therapy is a cutting-edge regenerative medicine treatment that harnesses the power of exosomes to promote healing and tissue regeneration within the body. Exosomes are small vesicles that are produced by cells and contain a variety of growth factors, proteins, and genetic material. These tiny packages play a crucial role in cell-to-cell communication and have been found to have remarkable regenerative and anti-inflammatory properties. When exosomes are used in therapy, they are typically harvested from mesenchymal stem cells, which have been found to be a rich source of exosomes. These exosomes can be administered to patients through various routes, including intravenous (IV) infusion. Once inside the body, exosomes can travel to the site of injury or inflammation and deliver their therapeutic payloads.

Benefits Of Exosome Therapy It has gained popularity in recent years due to its potential to treat a wide range of conditions. Research has shown promising results in the areas of orthopedics, neurology, cardiology, autoimmune diseases, and even cosmetic medicine. By harnessing the regenerative properties of exosomes, this therapy aims to stimulate the body's natural healing processes and promote tissue repair. Related Article: Exosomes IV Therapy - A Revolutionary Approach to Healing
Exosome Therapy Benefits
One of the primary benefits of exosome therapy is its ability to accelerate tissue repair and regeneration. Exosomes contain growth factors, cytokines, and other important molecules that can stimulate the body's natural healing processes. When exosomes are injected into a specific area or administered intravenously, they can target damaged tissues and promote the growth of new, healthy cells. Benefits of Exosomes Promotes tissue regeneration Reduces inflammation Enhances cellular communication Modulates gene expression Improves overall healing Another advantage of exosome therapy is its potential to reduce inflammation. Chronic inflammation is associated with various health conditions, including arthritis, autoimmune diseases, and neurodegenerative disorders. Exosomes can modulate the immune system and suppress inflammatory responses, leading to a decrease in pain and improved overall well-being. - Exosomes can also enhance the efficiency of other treatments. For example, when used in combination with traditional therapies such as physical therapy or surgery, exosome therapy can improve outcomes and speed up the healing process. - Furthermore, exosome therapy has shown promising results in treating various medical conditions. It has been used to address musculoskeletal injuries, chronic pain, cardiovascular diseases, and even neurodegenerative disorders like Alzheimer's and Parkinson's disease. - Exosomes iv therapy, in particular, offers the advantage of systemic delivery. When exosomes are administered intravenously, they can circulate throughout the body, targeting multiple areas and providing a more comprehensive healing effect. Conditions Treated by Exosome Therapy Chronic pain Arthritis Joint injuries Neurodegenerative disorders Cardiovascular diseases It is important to note that exosome therapy is a safe and well-tolerated treatment option. As exosomes are derived from the patient's own cells or sourced from thoroughly tested donors, there is minimal risk of adverse reactions, rejection, or infection. However, it is crucial to seek this therapy from a reputable and reliable exosome therapy clinic. If you are considering exosome therapy, it is essential to find the right clinic that specializes in this innovative treatment. Look for a clinic that has experienced medical professionals, advanced laboratory facilities, and a track record of successful patient outcomes. Reading success stories from exosome therapy patients can help you gain insight into the effectiveness of the treatment and the clinic's credibility.

Exosome Therapy
How Does Exosome Therapy Work?
It is a revolutionary treatment that is gaining popularity in the field of regenerative medicine. But how does it work? To understand the mechanism behind exosome therapy, it is essential to first understand what exosomes are. Exosomes are small vesicles that are released by various cells in the body, including stem cells. They contain proteins, growth factors, and genetic material such as RNA and DNA. These exosomes play a crucial role in cell-to-cell communication and regulation of cellular processes. When it is administered, exosomes are collected from a source such as umbilical cord-derived stem cells or mesenchymal stem cells. These exosomes are then purified and prepared for therapeutic use. The exosomes can be delivered to the patient through various routes, including intravenous (IV) therapy. Once the exosomes are introduced into the patient's body, they travel to the target tissues and organs. The exosomes have the ability to penetrate cell membranes and deliver their cargo directly into the recipient cells. The proteins and growth factors carried by exosomes can stimulate tissue regeneration and repair damaged cells. Additionally, the genetic material within the exosomes can potentially modulate gene expression in the recipient cells, leading to therapeutic effects. It has shown promise in treating a wide range of conditions. The regenerative properties of exosomes make them particularly effective in promoting healing and tissue regeneration. Conditions such as joint inflammation, musculoskeletal injuries, and neurological disorders can benefit from exosome therapy. The precise mechanisms by which exosomes work are still under investigation, but the potential therapeutic applications are vast. Patients who have undergone exosome therapy have reported improvements in their condition, faster recovery times, and reduced pain and inflammation. When considering exosome therapy, it is crucial to find the right exosome therapy clinic. Not all clinics have the same level of expertise and experience in exosome therapy. It is essential to choose a reputable clinic that specializes in regenerative medicine and follows strict quality control standards. https://youtu.be/TZ1dWGRxy8s?feature=shared
Conditions Treated By Exosome Therapy
One of the key advantages of exosome therapy is its versatility in addressing different medical conditions. From orthopedic injuries and degenerative joint diseases to neurological disorders and autoimmune conditions, exosome therapy has shown promising results in clinical trials and real-world applications. By harnessing the therapeutic potential of these exosomes, targeted repair and regeneration can be achieved at the cellular level, making it an attractive treatment option for a wide range of patients. Some of the conditions that can potentially be treated by exosome therapy include: - Joint Pain and Osteoarthritis: Exosomes can help promote tissue regeneration and reduce inflammation in the joints, providing relief from pain and improving mobility. - Tendon and Ligament Injuries: Exosome therapy can accelerate the healing process and enhance tissue regeneration, aiding recovery from tendon and ligament injuries. - Neurodegenerative Diseases: Studies have shown that exosome therapy may have the potential to slow down or reverse the progression of neurodegenerative diseases such as Alzheimer's, Parkinson's, and amyotrophic lateral sclerosis (ALS). - Autoimmune Conditions: Exosomes can modulate the immune response and help regulate the body's autoimmune reactions, potentially providing relief for conditions like rheumatoid arthritis, lupus, and multiple sclerosis. These are just a few examples of the many conditions that can benefit from exosome therapy. The regenerative properties of exosomes offer a promising alternative to conventional treatments, which often focus on managing symptoms rather than addressing the underlying cause.
Is Exosome Therapy Safe?
Firstly, it is crucial to note that exosome therapy is a minimally invasive procedure. The exosomes are typically administered through intravenous (IV) infusion, which means there is no need for surgical incisions or complex procedures. This significantly reduces the risks associated with the treatment. Additionally, as exosomes are derived from the patient's own cells or carefully screened donors, the chances of any adverse immune reactions or rejection are minimal. Furthermore, it has been extensively studied and has shown a favorable safety profile. Numerous preclinical and clinical studies have been conducted to evaluate the efficacy and safety of exosome-based treatments. These studies have demonstrated the ability of exosomes to effectively target damaged or diseased tissues, without causing any significant side effects. In terms of side effects, exosome therapy is generally well-tolerated. Some patients may experience mild discomfort at the injection site or transient flu-like symptoms, which are considered normal and temporary. Serious complications or adverse reactions are extremely rare.
Finding The Right Exosome Therapy Clinic
When considering exosome therapy, it is essential to find a reputable clinic that offers expert guidance and safe, high-quality treatments. Exosome therapy clinics should have experienced medical professionals who specialize in regenerative medicine and stay up to date with the latest research and advancements in the field. Additionally, the clinic should have a comprehensive understanding of the specific conditions that can be effectively treated using exosome therapy, such as orthopedic injuries, neurodegenerative diseases, autoimmune disorders, and aesthetic concerns. While searching for the right exosome therapy clinic, it is important to consider the clinic's track record and success rate. Look for patient testimonials and success stories from exosome therapy patients. These firsthand accounts provide valuable insights into the clinic's effectiveness and the experiences of previous patients. Reading about positive outcomes can be reassuring and give you confidence in choosing a particular clinic. Another crucial aspect to consider when finding the right exosome therapy clinic is the availability of tailored treatment plans. Each patient is unique, and their specific needs should be taken into account during the therapy process. An excellent clinic will provide personalized treatment plans that are customized to address the individual's condition, medical history, and goals. This personalized approach ensures that patients receive the most optimal and effective treatment possible. Related Article: IV Therapy NYC
Exosome Therapy Reviews
Many patients have reported remarkable improvements in their health and quality of life after receiving exosome therapy. For instance, individuals suffering from joint pain and arthritis have experienced significant pain reduction and increased mobility. Through targeted injections of exosomes, damaged cartilage and tissues can be regenerated, leading to improved joint function and decreased inflammation. Another example of a success story from exosome therapy involves patients with neurological conditions such as Parkinson's disease or stroke. By delivering exosomes directly to the affected area, these tiny vesicles can help regenerate damaged brain cells and improve neurological function. Patients have reported improvements in motor skills, speech, and overall cognitive abilities. The regenerative properties of exosomes offer hope for individuals affected by debilitating neurodegenerative disorders. Read the full article
0 notes
Text
Rheumatic heart disease after a heart transplant
The main goals of treatment for rheumatic heart disease patients following a heart transplant are to minimize problems related to the underlying ailment and to avoid graft rejection. Immunosuppressive therapy, which usually includes steroids, anti-proliferative drugs (such as mycophenolate mofetil), and calcineurin inhibitors (such as tacrolimus or cyclosporine), is essential to preventing rejection. Lifelong antibiotic prophylaxis is necessary to prevent infective endocarditis given the history of rheumatoid arthritis heart disease. To know more do visit Supreme hospitals, the Heart Transplant Surgery in Thiruporur.
0 notes