#Signs and Symptoms Of Stem cell
Explore tagged Tumblr posts
Text
Stem Cell Transplant in India

Stem cell transplant (SCT) in India has reached new heights with constant advancements in the medical industry. Many life-threatening diseases, such as leukemia, lymphoma, and some immune disorders, can be treated after undergoing a stem cell transplant in India.
#Stem cell transplant (SCT) in India#Signs and Symptoms Of Stem cell#Types of Stem cell#Diagnosis and tests Of Stem cell#Stem cell transplant Cost in India#Success Rate of Stem cell transplant in india#Risk Factors Of Stem cell#Stem cell transplant Hospitals in India
0 notes
Text
MS Mysteries Unlocked: Early Clues, Lifespan Secrets, and a Radical Cure?
MS Mysteries Unlocked Multiple Sclerosis (MS) is a complex and unpredictable disease—but what if we could crack its code? From strange first symptoms to groundbreaking stem cell treatments, here’s what science reveals (and what still remains a mystery). The Weird First Signs of MS Your Doctor Warned You About MS doesn’t always announce itself loudly. Instead, it whispers through bizarre…

View On WordPress
#"Multiple Sclerosis#autoimmune neurological disease#best MS clinic#best treatments for relapsing-remitting MS#can MS be cured#demyelination and nerve damage#Disease-Modifying Therapies for MS#DMTs for MS#does MS shorten life expectancy#early signs of MS in men#early signs of MS in women#how effective is HSCT for MS#how long do MS patients live#HSCT for MS#is stem cell therapy safe for MS#MRI diagnosis for MS#MS and vitamin D connection#MS disability progression#MS fatigue management tips#MS flare-up triggers#MS heat sensitivity#MS numbness and tingling causes#MS specialist near me#MS support groups#MS symptoms#MS treatment options#MS vs fibromyalgia differences#natural remedies for MS symptoms#neuroinflammation treatment#new breakthroughs in MS research 2024
0 notes
Text

10 Early Warning Signs Of Autism In Your Child - You Should Not Ignore
Discover the crucial early indicators of autism in your child with these 10 warning signs that demand attention. Don't overlook these key signals for early intervention and support.
#signs of autism disorder#autism symptoms#autistic child behaviour#autistic child behavior problems#Stem Cell Treatment
0 notes
Text
Old news, but something people should remember
Never let them tell you "We didn't know covid was so bad" or "It's mild for kids." We knew.
Also preserved on our archive
By John Anderer
PHILADELPHIA, Pa. — The news about coronavirus and children just got a lot worse. A troubling study by researchers at the Children’s Hospital of Philadelphia reports a “high proportion” of children infected with SARS-CoV-2 show elevated levels of a biomarker tied to blood vessel damage. Making matters worse, this sign of cardiovascular damage is being seen in asymptomatic children as well as kids experiencing COVID-19 symptoms.
Additionally, many examined children testing positive for SARS-CoV-2 are being diagnosed with thrombotic microangiopathy (TMA). TMA leads to clots in small blood vessels and has been linked to severe COVID symptoms among adult patients.
“We do not yet know the clinical implications of this elevated biomarker in children with COVID-19 and no symptoms or minimal symptoms,” says co-senior author David T. Teachey, MD, Director of Clinical Research at the Center for Childhood Cancer Research at CHOP, in a media release. “We should continue testing for and monitoring children with SARS-CoV-2 so that we can better understand how the virus affects them in both the short and long term.”
The complex connection between kids and COVID It’s fairly well established at this point that most children who contract coronavirus experience little to no symptoms. However, a small portion of young patients develop major symptoms or a post-viral inflammatory response to COVID-19 called Multisystem Inflammatory Syndrome in Children (MIS-C).
TMA in adults has a connection to more severe cases of COVID-19. Scientists believe the component of the immune system called “complement cascade” helps to mediate TMA in adults. The complement cascade is supposed to enhance and strengthen immune responses when a threat is present, but it can also backfire and lead to more inflammation. Up until now, the role of complement cascade during childhood TMA hadn’t been investigated.
To research the topic of “complement activation” in kids with SARS-CoV-2, researchers analyzed a group of 50 pediatric COVID-19 patients between April and July 2020. Among the group, 21 showed minimal to no symptoms, 11 experienced severe symptoms, and 18 developed MIS-C.
To search for complement activation and TMA among each patient, researchers used soluble C5b9 (sC5b9) as a biomarker. Scientists have used this substance for quite some time to assess the severity of TMA after stem cell procedures. In brief terms, the higher the level of sC5b9 in a transplant patient, the greater their mortality risk.
No symptoms doesn’t mean there’s no problem Study authors discovered elevated levels of C5b9 in both patients with severe COVID-19 and MIS-C. While this didn’t surprise researchers, they did get a shock from seeing high levels of C5b9 among even asymptomatic youngsters.
Some of the lab data regarding TMA had to be obtained after the fact. This meant researchers didn’t have a complete dataset to work with for all 50 studied patients. Among 22 patients researchers did have complete data for, 86 percent (19 children) were diagnosed with TMA. Every child had elevated levels of sC5b9, even those without TMA.
“Although most children with COVID-19 do not have severe disease, our study shows that there may be other effects of SARS-CoV-2 that are worthy of investigation,” Dr. Teachey concludes. “Future studies are needed to determine if hospitalized children with SARS-CoV-2 should be screened for TMA, if TMA-directed management is helpful, and if there are any short- or long-term clinical consequences of complement activation and endothelial damage in children with COVID-19 or MIS-C. The most important takeaway from this study is we have more to learn about SARS-CoV-2. We should not make guesses about the short and long-term impact of infection.”
The study is published in Blood Advances.
Study Link: ashpublications.org/bloodadvances/article/4/23/6051/474421/Evidence-of-thrombotic-microangiopathy-in-children
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
55 notes
·
View notes
Text
disabled children and their parents - part 1
this post will be about babies born with disabilities, and part 2 will be about Susan Mullocks.
Call the Midwife has quite a number of families that are surprised to learn that their newborn has something going on that will make their lives different. Understandably they go through shock and adjustment periods and have to face difficult decisions. We will take a look at some examples in the third part of this post.
In a few cases the parents know before birth that there could be something that endangers their babies life and/or wellbeing.
One of the cases where the parents worry because of an older sibling who has a problem is the Sands family with Elaine. The girl shows symptoms of delayed development and starts having fits, due to phenylketonuria. Fortunately her baby sibling is fine. Elaine will need a special diet all her life to manage her condition and it is unclear how much she will be able to catch up on development. Both her parents are educated by medical staff and do their best. s10e5
Another family who has health concerns is the Aidoo family: first diagnosed in expecting mother Flora, they learn that her son and husband also have sickle cell disease. With both parents afflicted, it's a big concern that their newborn could also have it. Knowing what it is that will make their own and their children's lives harder, the family adjusts with the help of the Nonnatuns. Sickle cell disease remains a huge challenge for families and the health care providers worldwide - one thing people anywhere can do to help is sign up as a stem cell donor and maybe one day donate healthy blood stem cells to a patient. s8e2
In one case it was the grandmother who worried, because she knew about the family history with haemophilia. Hoping her daughter, Lorna Pryce, would have a baby girl, she did not mention that her husband died of the blood disorder. When the baby boy is born, it becomes apparent quickly that something is not working well and he needs hospital care in his first days of life. Probably not for the last time. His grandmother's experience may be helpful in managing his condition. s12e3
Kinda worried: The Reed family. Achondroplasia is making some things a challenge for Peggy and Derek Reed. The doctors fear that the baby they are expecting is going to have the condition as well - which would be likely, and the parents know what life would bring for their child. The other worry is that the child may not live, which would be very hard to bear. In the end the child is well and of regular size for a newborn. The new worry of her parents is that she will outgrow them soon - and they will indeed have to make adjustments again and again, like all parents have to. s6e3
Very clear example of a couple who has plenty of reasons to be anxious: another father called Derek, who has served in the army and was exposed to radiation during his time, is suffering even years after. What he did not expect is that the radiation poisoning would affect his children. When his wife Audrey gives birth, their son Christopher only lives for a few hours. Christopher's body did not develop in a way that made survival possible. The damage his father had endured on a genetic level caused Christopher's legs to be only half formed and more anomalies less visible caused his death. A deep shock for his parents. s10e1
A year later, after collecting information about similiar cases, Audrey is pregnant again. They trust the Nonnatuns to help again with the birth, but their fear that the new baby might also have problems is throwing a shadow over their excitement. Luckily their baby girl is well and lives. s11e1
Another example from an earlier season: (s3e5) in this episode mainly the baby's grandparents and the medical staff are worried that it might have a genetical condition: Sally Harper, a young woman with Down's syndrome, is pregnant. The baby's father, Sally's boyfriend Jacob who also lives in St. Gideon's, wants to marry her but is refused because he has a disability, too. Their baby is born too early and does not survive. We do not learn if it had Down's Syndrome. Sally and Jacob are separated, her parents would rather forget about everything. Jacob is sent to a different institution and does not get to say goodbye to Sally or to their child.

let's stay a while on the topic of babies who die from their disabilities.
Irene and Pat Kelly are devastated when their newborn son dies suddenly. Later they learn that he had a problem with his lungs, they were not developed fully and that cut his life very short. There was no sign of a problem right after his birth, and there was nothing that could have been done to help him. The Kelly's can only grieve. s2e2
Valerie's cousin Maureen gives birth to her third child, Warren. At first everything looks fine, then she notices that her son is unusually floppy and quiet. Dr Turner finds symptoms that point to a problem with his heart, and the diagnosis later is that the baby was exposed to german measles in utero. Several problems make it unlikely that he will live long, and his parents are shocked and sad. Then they decide to care for him at home to make his life as comfortable and happy as they can. Maureen attempts to help her older children to cope with the situation and form a bond with their baby brother. Warren dies quietly while his parents and siblings are sleeping close by. This way the family was able to say goodbye in a way they could bear. s9e6

Ruby Cottingham, proud mother of a bunch of boys, is pregnant again and hopes she'll get a girl. She has a difficult labor and needs a C-section, and the doctor is taken aback when he sees that the child is missing all limbs and other body parts. The hospital staff never lets Ruby see her baby, they decide to put the newborn in a side room and let the child die instead of trying to find out how to help. Sister Julienne finds and holds the baby while it is passing away. She is speaking up against a cruel decision, and later delivering the horrible news to Ruby. In the months after Ruby is dealing with her pain mostly alone and when she learns why her child died it is of no comfort. Thalidomide damaged her baby and she lost her child because some complete strangers did not do their work properly and sold dangerous medication. s5e4
Of the parents with disabled babies who lived there are some who will grow up just fine because their problem can be fixed with surgery, medication or other treatments. We'll look at them towards the end of this post. On the other hand, some children will be unwell all their lives and not grow as old as their peers.
Merle and Billy Vickers have two sons with the same puzzling poor health symptoms, and the little one is only saved from choking because his mother ran with him to get help at Nonnatus house. Sister Monica Joans insistence that Dr Turner look into an old textbook that describes their illness helps find the diagnosis "cystic fibrosis" and the treatment that will make the two boys' lives easier. With artificial enzymes they can have less side effects, but they will never be completely fine. s3e1
A newborn with a broken bone needs very careful handling. When Janice and Ray Prendergast have their first baby, Raymond, Sister Julienne discovers two broken bones within a very short time. Afraid that the boy has been assaulted, Dr Turner decides to take him away from his parents and into foster care. When the foster mother brings the baby in with another fracture, it becomes apparent that Raymond has osteogenesis imperfecta, and is therefore likely to suffer more broken bones. Extremely careful handling will protect him somewhat, but his life will be very challenging. s4e5
Two families, Shirley and Ian Dent and Marion and Godfrey Smith, are faced with a predicament like few others: their babies were muddled in the maternity home and each family took home the wrong child. One of the girls, Deborah, has a heart problem and will need surgery to survive. The parents are shocked and worried, and then they learn that the baby they have been caring for is not their own but the daughter of their aquaintances. They suddenly have the option of giving up the responsibility for Deborah. But it is not that easy. They have formed a bond with the sick child and cannot imagine just swapping her for another baby, not even their biological child, Jackie. The question how each family will go forward is unresolved, and we don't know if the risky surgery went well and the girl was fine. s4e7
Also unclear what became of the youngest child in the Lund family. The mother and older sister have Huntington's disease and will suffer increasingly from nerve damage. The hereditary condition could also be present in the baby, with no option of diagnosis as long as there are no symptoms. s7e3
Let's move on to more cheerful stories, shall we?
Remember Kirk? Youngest of six children, born with a cleft lip and cleft palate. Very inconvenient when your only job is sleeping and nursing. Milk gets into the airways and pneumonia will creep in, it's a nightmare. Now his mom Betty is usually a very competent and energetic woman. But with five other children demanding her attention and no husband at home because those sailors tend to sail away all the time, Betty feels she cannot give Kirk the care he needs. Adoption is considered. Until Valerie swoops in, sweeps the school children out the door, smack-talks the oldest boy into taking appropriate responsibility and gives Betty a hand with some of the chores. Kirk has his first surgery, his dad comes home, there's applause and a few years later he gets to be a flower child at Lucille's wedding. s8e3
Also in hospital with some complicated treatment: Clover, daughter of Clover, who now wants to be called Susan again. While the young woman wanted to give birth as naturally as possible, her baby needed immediate intervention because she was born with gastroschisis. Shelagh saves the day with some excellent staying calm skills, and the staff at the children's hospital find a way to put Clover's organs back where they belong. Susan reconciling with her father will also help Clover grow up safe and healthy. s13e2
I did not know that it is possible for a baby to be born with cancer. But apparently it happens often enough to have a name, this quite unlucky genetical mishap. Retinoblastoma. Both of Lindy Webster's girls have it and need treatment. They will be fine. The older girl will have just the one eye, but that's okay. Compared to other parents the Webster family is actually chill and will get through this. s13e5
Stefanie Baxter will be fine, too. More than that, probably, because her hip dysplasia is actually not that rare, the treatment is effective and she will have little long term problems. At first her mom Gillian was out of her depth, learning how to carry and care for a baby that needs to be in a harness and held in a certain way. Her husband Liam helps, as does Phyllis, who was the first to notice Stefanie's problem. Being carried in a baby wrap will help keep her legs in the right position and that is a really cosy way to take your newborn places or calm it down. s13e2
Of all the parents who are surprised by a baby with a disability, the Dellow family has the most happy outcome in my view. Blanche had planned to give her newborn to her childless sister, because her older children are already grown. When baby Robert arrives, he gets the diagnosis of Down's syndrome, and his aunt does not want to become his mother anymore. Blanche meanwhile calmly gets to know the little guy, is appaled by her sister's attitude and decides to keep him. Her husband initially finds it hard to deal with, but a conversation with Fred Buckle about Reggie changes his view. Violet even thanks Blanche for giving her the chance to glimpse a part of Reggie's past, because she never knew him as a baby. A couple of years later Robert is best friends with Reggie and they have the best time. 10e7

I'll close part 1 and wander on to write part 2 with the lovely line from Susan's second episode:
"Children must be loved. There is no rule in life so simple, or so true."
21 notes
·
View notes
Text
Marble Hornet headcanons everyone come gobble em up before they get cold!!! @forgottenporkbun @monszsterz
So my headcanons for MH are a lot less conceret than those for the creepypastas cause ngl, I'm still trying to figure out wtf happened in MH. I haven't read the comics yet so I'm going off the main videos only. I've rewatched them a few times and read the theories but I'm still left with a few questions, and some theories I have fall apart when paired against certain videos SO take everything with a grain of salt. Even WORSE is I'm still playing around with how I want to write these scenarios and dynamics because they change drastically based on what theory I'm going with at the time.
Starting off, I think The Operator (TO) is doing a lot of experimentation. Each person in MH is affected differently cause no two people have the exact same type of TO disease. The closest are probably Jay and Brian, funny enough, because both were infected by Tim. Tim is patient zero for the disease in the sense that he doesn't just have it, he IS IT. Each cell in Tim's body contains a little speck of TO that, when transferred to others, can multiply and spread into a spiritual parasite. It reacts differently to Alex because he's also hand picked by TO. We know Alex had been stalked by him from an early age, maybe his whole life. When he got infected it triggered a sleeper agent type parasite in him. He's a lot more aggressive, violent, and bold. I think the difference stems from where the seed of The Operator has been planted. For Tim its the body, and Alex I honestly think its the soul. I could say mind but I actually think that applies better to Seth (and Ticci Toby but I'm trying not to include creepypastas in this rn). If the disease works through the bodies of Tim, Brian, and Jay it makes sense why normal prescription medication works to stop it. If that's the case why isn't everyone infected and wipes out the world? We were nearly at the end of MH by the time Jay started REALLY showing signs of no return. At almost any point he could have left got some medication, and probably get over it! I mean its like, entry 80 before we see him wandering around in a daze and hallucinating, right? His symptoms always get worse when he's in an infected area or around Tim for a prolonged amount of time. Jessica on the other hand seems to catch it really fast. Like REALLY fast. A single interaction in Rosswood has her just as bad as Jay, who had been on the run for almost two years surrounding himself with this shit. She has also been stalked by TO since a young age. I won't be able to get into her more until I read the comics tho.
I see a lot of people confused as to what Brian's status ends up being with both The Operator and his friends cause me too tbh. His motives are constantly bouncing around. One thing I know is he is still buddy buddy with TO. Some people say he's fighting against him but I don't get that at all from the videos. He's either using special powers he was given or TO is monitoring him and stepping in when possible to teleport him to safety. If TO is wanting followers then it makes sense he'd encourage Brian to lure Tim back into it with him. The issue is Alex is ALSO a follower. The Operator finds himself in a pickle when his girls are fighting one another. This is where I really get thrown off. An easy answer would be The Operator is an inhumane, eldrich, perhaps fae monster with no understanding of how humans really work. This, paired with the fact his followers have NO idea what he really wants them to do, means miscommunication and chaos ensue. When Tim is killing Alex in the final entries TO bounces around BOTH of them to get in their way. We know he's fully capable of tossing Tim off to the other side of the woods, or snatching Alex out of danger, but he doesn't. He's watching....I think he wants to see which style of infection is better. Tim's disease, or Alex's corruption. Which makes a better follower. This falls apart when you remember how close Brian came to killing Alex and he got saved by TO. Again you can sweep this under the rug by saying either A: He wans't done having fun yet or B: It had to be Tim. The OP doesn't give a FUCK about Jay dying, he lets him get shot and then scoops him up for devouring. Same about Brian, he lets him *fall*. They're supplemental to the game. Its all about Tim and Alex.
Now my FAVORITE headcanon of all time I use everywhere no matter WHAT...Tim is The Operator's favorite. If we wanna include pre-MH lore about Slenderman, aka his origins in the photoshop contest, then we learn he's been trying to do something like this for a very long time. Tim may be the first person ever directly infected by The Operator to live to adulthood. He may also be the first one to consistently fall back into a state of obedience, aka, a masked state where he's being crazy in Rosswood in the middle of the night. That makes him the favorite child. He is disobedient to The Operator, curses him, openly hates him, and physically fights against him throughout ALL of Marble Hornets and yet Tim never gets killed or devoured. He definitely comes close to both. I think him being teleported around is The Operator's most merciful form of punishment to shake some sense into his first follower. Its basically evil time out lmao. He just ALMOST snags two more followers in Brian and Jay but alas we know how that ends. In most people's "fix it" au, or "no one dies" au, that isn't an issue. My "no one dies" au transfers into creepypastas and the mansion and there is a direct tie in there with Ticci Toby, his similarities to Tim, their relationship, and how The Operator acts. The best way I explain it (and the way that makes me laugh the most) is saying TO is like parents who were cruel af to their eldest child, but by their youngest, they're completely different people and wonderful parents. I wouldn't call Slenderman a wonderful parent even in a very wholesome creepypasta mansion Au but he's definitely BETTER THAN WHATEVER THE FUCK WAS HAPPENING IN MH!!! This results in the younger children (pastas) having no idea why the eldest children (Tim and Brian) fucking hate their parents. Its a very good silly dynamic to wrap up the most gut wrenching, tragic yaoi I have ever watched.
#marble hornets#masky marble hornets#tim wright#mh hoody#jay merrick#brian marble hornets#alex kraile#slenderverse#slenderman#creepypasta#ticci toby
24 notes
·
View notes
Text
Shoulder Pain? Here’s Why You Should See a Top Shoulder Doctor in Austin

Shoulder pain can be debilitating, limiting your ability to work, exercise, or even complete everyday tasks like getting dressed or reaching overhead. Whether the discomfort stems from a sports injury, overuse, arthritis, or a sudden accident, it’s essential to seek professional care. If you’re in Central Texas, seeing a qualified shoulder doctor in Austin can put you on the fast track to relief, recovery, and long-term shoulder health.
Why Shoulder Pain Shouldn’t Be Ignored
The shoulder is one of the most mobile—and complex—joints in the human body. It plays a crucial role in almost every upper body movement. When something goes wrong in this joint, the result can range from mild discomfort to severe limitations in motion.
Ignoring shoulder pain can lead to worsening symptoms, permanent damage, and a much longer recovery process. That's why visiting a shoulder doctor in Austin at the first signs of discomfort is a smart move. A qualified specialist can identify the root cause of your symptoms, recommend appropriate treatment, and help you avoid more invasive procedures down the road.
What Conditions Can a Shoulder Doctor in Austin Treat?
Shoulder doctors, also known as orthopedic specialists, are trained to diagnose and treat a wide range of conditions related to the shoulder joint. Common issues they handle include:
Rotator cuff tears
Frozen shoulder (adhesive capsulitis)
Shoulder impingement syndrome
Shoulder dislocations
Labral tears
Tendonitis and bursitis
Shoulder arthritis
Fractures and trauma-related injuries
An experienced shoulder doctor in Austin will use advanced diagnostic tools such as X-rays, MRIs, and physical evaluations to get a clear picture of your shoulder’s health and recommend a customized treatment plan.
Treatment Options from a Shoulder Doctor
Not every shoulder problem requires surgery. In fact, many patients find relief through non-surgical treatments. A reputable shoulder doctor in Austin will often start with conservative options such as:
Physical therapy
Anti-inflammatory medications
Corticosteroid injections
Activity modification
PRP (platelet-rich plasma) or stem cell therapy (in some cases)
If surgery becomes necessary, you’re in good hands. Austin is home to many board-certified orthopedic surgeons who specialize in minimally invasive arthroscopic procedures and advanced surgical techniques to restore shoulder function and reduce downtime.
Benefits of Choosing a Shoulder Doctor in Austin
Austin is quickly becoming a regional leader in orthopedic care. Whether you’re an athlete, a busy professional, or a retiree, you’ll find top-rated medical professionals who understand the unique demands of your lifestyle.
Here’s why choosing a shoulder doctor in Austin is a smart decision:
Expertise: Many shoulder doctors in Austin are fellowship-trained and have years of experience treating shoulder-specific conditions.
Cutting-Edge Facilities: From imaging to surgery and rehab, Austin clinics and hospitals offer state-of-the-art equipment and technology.
Personalized Care: Unlike larger cities where healthcare can feel impersonal, Austin physicians often pride themselves on providing attentive, patient-centered care.
Convenience: With numerous highly-rated orthopedic clinics throughout the city and surrounding areas, you won’t have to travel far to receive quality treatment.
How to Choose the Right Shoulder Doctor in Austin
When searching for the right doctor, don’t just rely on insurance networks or proximity alone. Here are a few tips to ensure you choose the best shoulder doctor in Austin for your needs:
Look for board certification and fellowship training in shoulder or sports medicine.
Check online reviews to learn about patient experiences and satisfaction.
Ask about experience with your specific condition or procedure.
Schedule a consultation to see if the doctor communicates clearly, listens to your concerns, and makes you feel comfortable.
It’s also helpful to find a doctor affiliated with a reputable hospital or orthopedic group. That way, you’ll have access to a comprehensive care team, from diagnostics to rehab.
What to Expect During Your First Appointment
During your initial visit with a shoulder doctor in Austin, you can expect a thorough review of your medical history, a physical exam, and possibly imaging studies. Be prepared to discuss:
How and when the pain started
What movements worsen or relieve the pain
Any past injuries or surgeries
Your physical activity and lifestyle
After diagnosing the issue, the doctor will explain your treatment options and help you decide on the best course of action, whether it’s physical therapy, injections, or surgical intervention.
Start Your Recovery Today
You don’t have to live with shoulder pain. Whether you’re dealing with an old injury that never healed right or new discomfort that’s interfering with your daily life, a trusted shoulder doctor in Austin can help. The sooner you get evaluated, the sooner you can start feeling better and return to the activities you love.
youtube
Shoulder injuries and pain can disrupt your life—but you don’t have to face them alone. By choosing a qualified shoulder doctor in Austin, you gain access to expert care, innovative treatment options, and a path toward lasting recovery. Don’t wait for the pain to get worse. Schedule your appointment today and take the first step toward a healthier, pain-free future.
#shoulder surgeon austin#shoulder doctor austin#shoulder specialist austin#knee surgeon austin#knee doctor austin#knee specialist austin#ankle surgeon austin#ankle doctor austin#ankle specialist austin#Youtube
3 notes
·
View notes
Text
COVID-19 Vaccines, 20,000 New Eye Disorders Are Reported
These experimental vaccines are designed to cause inflammation throughout the body, by reprogramming human cells to produce inflammatory spike proteins that are derived from the bio-weapon itself. Eye damage is merely a symptom of this inflammation, a sign of more serious problems to come with capillaries and autoimmune issues. The inflammatory conditions caused by the vaccines provide a new revenue stream for various industries within the medical system, including ophthalmology.
With mounting evidence of eye injury post-vaccination, ophthalmologists are ethically obligated to denounce these covid-19 vaccines. The vaccines are causing acute eye injuries at scale and are an underlying cause of inflammation for future eye disorders and other health problems. However, ophthalmologists are not properly trained to recognize, diagnose and report vaccine injury.
When the U.S. FDA issued Emergency Use Authorization for these experimental ‘vaccines’, they did not mention eye disorders specifically. In their fact sheet, they warn, “additional adverse reactions, some of which may be serious, may become apparent with more widespread use of the Pfizer-BioNTech COVID-19 Vaccine.”
In the UK’s Yellow Card System, vaccine-induced eye damage includes 4,616 cases of severe eye pain, 3,839 cases of blurred vision, 1,808 cases of light intolerance, and 559 cases of double vision. These issues were not prevalent until the vaccine was used. Some of the eye issues are mild but could be a sign of more serious issues within the cardiovascular or nervous systems. There were 768 cases of eye irritation, 731 cases of itchy eyes, 788 cases of ocular hyperemia, 459 cases of eye strain, 400 cases of dry eye, and 653 cases of increased lacrimation.
More serious issues of swelling were documented as well, including swelling around the eye (366 incidences), swelling of the eyelid (360 incidences) eyelid oedema (298) conjunctival haemorrhage or breakage of a small eye vessel (236), periorbital oedema (171), and eye haemorrhage (169). The swelling can be indicative of more serious cerebral, spinal, and/or cardiovascular issues. Blood clots and nervous system disorders are a commonly reported adverse event. The eye disorders provide a window of opportunity to understand just how severe the inflammation is. Ophthalmologists are able to identify early signs of vaccine-induced brain swelling, cardiovascular issues and stroke to help patients seek emergency care before the patient becomes another casualty to these horrid vaccines.
One 33-year-old pilot had severe migraines and sudden vision problems following the Pfizer vaccine. The pain migrated down the back of his neck toward the bottom of his skull. The pain lasted for several days and was accompanied by dizziness, nausea, disorientation, confusion, uncontrollable shaking, and tingling in his toes and fingers. He was ultimately evaluated by doctors. The Pfizer COVID vaccine had increased the pressure in his spinal cord and brain stem, rupturing his left inner ear, and damaging his eyesight.
3 notes
·
View notes
Note
Acute radiation syndrome (ARS), also known as radiation sickness or radiation poisoning, is a collection of health effects that are caused by being exposed to high amounts of ionizing radiation in a short period of time.[1] Symptoms can start within an hour of exposure, and can last for several months.[1][3][5] Early symptoms are usually nausea, vomiting and loss of appetite.[1] In the following hours or weeks, initial symptoms may appear to improve, before the development of additional symptoms, after which either recovery or death follow.
ARS involves a total dose of greater than 0.7 Gy (70 rad), that generally occurs from a source outside the body, delivered within a few minutes. Sources of such radiation can occur accidentally or intentionally. They may involve nuclear reactors, cyclotrons, certain devices used in cancer therapy, nuclear weapons, or radiological weapons.[4] It is generally divided into three types: bone marrow, gastrointestinal, and neurovascular syndrome, with bone marrow syndrome occurring at 0.7 to 10 Gy, and neurovascular syndrome occurring at doses that exceed 50 Gy.[1][3] The cells that are most affected are generally those that are rapidly dividing.[3] At high doses, this causes DNA damage that may be irreparable.[4] Diagnosis is based on a history of exposure and symptoms.[4] Repeated complete blood counts (CBCs) can indicate the severity of exposure.[1]
Treatment of ARS is generally supportive care. This may include blood transfusions, antibiotics, colony-stimulating factors, or stem cell transplant.[3] Radioactive material remaining on the skin or in the stomach should be removed. If radioiodine was inhaled or ingested, potassium iodide is recommended. Complications such as leukemia and other cancers among those who survive are managed as usual. Short term outcomes depend on the dose exposure.[4]
ARS is generally rare.[3] A single event can affect a large number of people,[7] as happened in the atomic bombings of Hiroshima and Nagasaki and the Chernobyl nuclear power plant disaster.[1] ARS differs from chronic radiation syndrome, which occurs following prolonged exposures to relatively low doses of radiation.[8][9]
Signs and symptoms[edit]
See also: Effects of nuclear explosions on human healthRadiation sickness
Classically, ARS is divided into three main presentations: hematopoietic, gastrointestinal, and neurovascular. These syndromes may be preceded by a prodrome.[3] The speed of symptom onset is related to radiation exposure, with greater doses resulting in a shorter delay in symptom onset.[3] These presentations presume whole-body exposure, and many of them are markers that are invalid if the entire body has not been exposed. Each syndrome requires that the tissue showing the syndrome itself be exposed (e.g., gastrointestinal syndrome is not seen if the stomach and intestines are not exposed to radiation). Some areas affected are:
Hematopoietic. This syndrome is marked by a drop in the number of blood cells, called aplastic anemia. This may result in infections, due to a low number of white blood cells, bleeding, due to a lack of platelets, and anemia, due to too few red blood cells in circulation.[3] These changes can be detected by blood tests after receiving a whole-body acute dose as low as 0.25 grays (25 rad), though they might never be felt by the patient if the dose is below 1 gray (100 rad). Conventional trauma and burns resulting from a bomb blast are complicated by the poor wound healing caused by hematopoietic syndrome, increasing mortality.
Gastrointestinal. This syndrome often follows absorbed doses of 6–30 grays (600–3,000 rad).[3] The signs and symptoms of this form of radiation injury include nausea, vomiting, loss of appetite, and abdominal pain.[10] Vomiting in this time-frame is a marker for whole body exposures that are in the fatal range above 4 grays (400 rad). Without exotic treatment such as bone marrow transplant, death with this dose is common,[3] due generally more to infection than gastrointestinal dysfunction.
Neurovascular. This syndrome typically occurs at absorbed doses greater than 30 grays (3,000 rad), though it may occur at doses as low as 10 grays (1,000 rad).[3] It presents with neurological symptoms such as dizziness, headache, or decreased level of consciousness, occurring within minutes to a few hours, with an absence of vomiting, and is almost always fatal, even with aggressive intensive care.[3]
Early symptoms of ARS typically include nausea, vomiting, headaches, fatigue, fever, and a short period of skin reddening.[3] These symptoms may occur at radiation doses as low as 0.35 grays (35 rad). These symptoms are common to many illnesses, and may not, by themselves, indicate acute radiation sickness.[3]
Dose effects[edit]
PhaseSymptomWhole-body absorbed dose (Gy)1–2 Gy2–6 Gy6–8 Gy8–30 Gy> 30 GyImmediateNausea and vomiting5–50%50–100%75–100%90–100%100%Time of onset2–6 h1–2 h10–60 min< 10 minMinutesDuration< 24 h24–48 h< 48 h< 48 h— (patients die in < 48 h)DiarrheaNoneNone to mild (< 10%)Heavy (> 10%)Heavy (> 95%)Heavy (100%)Time of onset—3–8 h1–3 h< 1 h< 1 hHeadacheSlightMild to moderate (50%)Moderate (80%)Severe (80–90%)Severe (100%)Time of onset—4–24 h3–4 h1–2 h< 1 hFeverNoneModerate increase (10–100%)Moderate to severe (100%)Severe (100%)Severe (100%)Time of onset—1–3 h< 1 h< 1 h< 1 hCNS functionNo impairmentCognitive impairment 6–20 hCognitive impairment > 24 hRapid incapacitationSeizures, tremor, ataxia, lethargyLatent period28–31 days7–28 days< 7 daysNoneNoneIllnessMild to moderate Leukopenia Fatigue WeaknessModerate to severe Leukopenia Purpura Hemorrhage Infections Alopecia after 3 GySevere leukopenia High fever Diarrhea Vomiting Dizziness and disorientation Hypotension Electrolyte disturbanceNausea Vomiting Severe diarrhea High fever Electrolyte disturbance Shock— (patients die in < 48h)MortalityWithout care0–5%5–95%95–100%100%100%With care0–5%5–50%50–100%99–100%100%Death6–8 weeks4–6 weeks2–4 weeks2 days – 2 weeks1–2 daysTable source[11]
A similar table and description of symptoms (given in rems, where 100 rem = 1 Sv), derived from data from the effects on humans subjected to the atomic bombings of Hiroshima and Nagasaki, the indigenous peoples of the Marshall Islands subjected to the Castle Bravo thermonuclear bomb, animal studies and lab experiment accidents, have been compiled by the U.S. Department of Defense.[12]
A person who was less than 1 mile (1.6 km) from the atomic bomb Little Boy's hypocenter at Hiroshima, Japan, was found to absorb about 9.46 grays (Gy) of ionizing radiation.[13][14][15][16]
The doses at the hypocenters of the Hiroshima and Nagasaki atomic bombings were 240 and 290 Gy, respectively.[17]
Skin changes[edit]
Main article: Radiation burnHarry K. Daghlian's hand 9 days after he had manually stopped a prompt critical fission reaction during an accident with what later obtained the nickname the demon core. He received a dose of 5.1 Sv,[18] or 3.1 Gy.[19] He died 16 days after this photo was taken.
Cutaneous radiation syndrome (CRS) refers to the skin symptoms of radiation exposure.[1] Within a few hours after irradiation, a transient and inconsistent redness (associated with itching) can occur. Then, a latent phase may occur and last from a few days up to several weeks, when intense reddening, blistering, and ulceration of the irradiated site is visible. In most cases, healing occurs by regenerative means; however, very large skin doses can cause permanent hair loss, damaged sebaceous and sweat glands, atrophy, fibrosis (mostly keloids), decreased or increased skin pigmentation, and ulceration or necrosis of the exposed tissue.[1] As seen at Chernobyl, when skin is irradiated with high energy beta particles, moist desquamation (peeling of skin) and similar early effects can heal, only to be followed by the collapse of the dermal vascular system after two months, resulting in the loss of the full thickness of the exposed skin.[20] Another example of skin loss caused by high-level exposure of radiation is during the 1999 Tokaimura nuclear accident, where technician Hisashi Ouchi had lost a majority of his skin due to the high amounts of radiation he absorbed during the irradiation. This effect had been demonstrated previously with pig skin using high energy beta sources at the Churchill Hospital Research Institute, in Oxford.[21]
Cause[edit]
Both dose and dose rate contribute to the severity of acute radiation syndrome. The effects of dose fractionation or rest periods before repeated exposure also shift the LD50 dose upwards.Comparison of Radiation Doses – includes the amount detected on the trip from Earth to Mars by the RAD on the MSL (2011–2013).[22][23][24][25]
ARS is caused by exposure to a large dose of ionizing radiation (> ~0.1 Gy) over a short period of time (> ~0.1 Gy/h). Alpha and beta radiation have low penetrating power and are unlikely to affect vital internal organs from outside the body. Any type of ionizing radiation can cause burns, but alpha and beta radiation can only do so if radioactive contamination or nuclear fallout is deposited on the individual's skin or clothing. Gamma and neutron radiation can travel much greater distances and penetrate the body easily, so whole-body irradiation generally causes ARS before skin effects are evident. Local gamma irradiation can cause skin effects without any sickness. In the early twentieth century, radiographers would commonly calibrate their machines by irradiating their own hands and measuring the time to onset of erythema.[26]
Accidental[edit]
Main article: Nuclear and radiation accidents and incidents
Accidental exposure may be the result of a criticality or radiotherapy accident. There have been numerous criticality accidents dating back to atomic testing during World War II, while computer-controlled radiation therapy machines such as Therac-25 played a major part in radiotherapy accidents. The latter of the two is caused by the failure of equipment software used to monitor the radiational dose given. Human error has played a large part in accidental exposure incidents, including some of the criticality accidents, and larger scale events such as the Chernobyl disaster. Other events have to do with orphan sources, in which radioactive material is unknowingly kept, sold, or stolen. The Goiânia accident is an example, where a forgotten radioactive source was taken from a hospital, resulting in the deaths of 4 people from ARS.[27] Theft and attempted theft of radioactive material by clueless thieves has also led to lethal exposure in at least one incident.[28]
Exposure may also come from routine spaceflight and solar flares that result in radiation effects on earth in the form of solar storms. During spaceflight, astronauts are exposed to both galactic cosmic radiation (GCR) and solar particle event (SPE) radiation. The exposure particularly occurs during flights beyond low Earth orbit (LEO). Evidence indicates past SPE radiation levels that would have been lethal for unprotected astronauts.[29] GCR levels that might lead to acute radiation poisoning are less well understood.[30] The latter cause is rarer, with an event possibly occurring during the solar storm of 1859.
when i catch you i swear。
2 notes
·
View notes
Photo
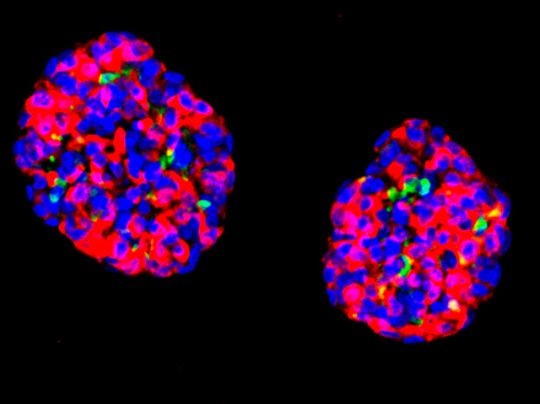
Islet Stand-ins
In type 1 diabetes, the cells of the pancreas that sense blood sugar and secrete insulin accordingly (islet cells) are destroyed. To both fix the problem and avoid immune rejection, doctors are hoping to replace the damaged cells with new ones grown from the patient’s own stem cells. To that end, researchers have grown these insulin-secreting organoids– clumps of cells that mimic the islets. The insulin-producing cells are labelled in red, and other associated hormone-producing cells are green. The organoids were grown from human stomach stem cells rather than pancreatic ones – simply because the cells are similar in nature but more readily retrieved (via endoscopy). Encouragingly, transplants of the organoids into mice with diabetes improved the animals’ symptoms and reversed signs of disease. With no available cure for diabetes, these proof-of-principle transplantations offer encouraging results that suggest such an approach might indeed be successful in the clinic.
Written by Ruth Williams
Image from work by Xiaofeng Huang and colleagues
Division of Regenerative Medicine and Hartman Institute for Therapeutic Organ Regeneration, Department of Medicine, Weill Cornell Medicine, New York, NY, USA
Image copyright held by the original authors
Research published in Nature Cell Biology, April 2023
You can also follow BPoD on Instagram, Twitter and Facebook
10 notes
·
View notes
Text
Stem Cell Transplant Cost in India

The cost of stem cell transplants in India ranges from $6000 to $12,000, with $2000 for each cycle. The price can reach $4000 to $6000 per session, depending on the condition. India offers stem cell transplant at almost one-seventh of the cost compared to countries like the UK and the USA.
#Stem cell transplant (SCT) in India#Signs and Symptoms Of Stem cell#Types of Stem cell#Diagnosis and tests Of Stem cell#Stem cell transplant Cost in India#Success Rate of Stem cell transplant in India#Risk Factors Of Stem cell#Stem cell transplant Hospitals in India
0 notes
Text
Unlocking Glowing Skin: The Surprising Secret Link to Your Gut

Many of us invest heavily in our skincare routines, layering on serums, creams, and treatments in the quest for youthful, glowing skin. We target wrinkles, fight dryness, and try to fade those stubborn age spots. Yet, sometimes, despite our best efforts, our skin doesn’t seem to cooperate. It can feel frustrating when the visible signs of skin aging continue to appear, leaving us searching for answers. What if the missing piece in your skincare puzzle isn’t another topical treatment, but something deeper within your body?
Emerging science points to a fascinating and powerful connection that could be influencing your skin’s health and appearance in ways you haven’t considered. This connection might become particularly relevant after 35, as subtle shifts in gut health and the skin’s natural resilience can sometimes make internal imbalances more apparent externally. As we age, factors like natural hormonal fluctuations, changes in metabolism, and even accumulated environmental stressors can impact our gut microbiome, making the link between internal balance and external glowing skin even more pronounced.
Beyond the Surface: Why Traditional Skincare Has Its Limits
While essential for protecting our skin from the environment and maintaining hydration, traditional topical skincare primarily addresses concerns from the outside. It treats symptoms you can see — the wrinkle, the dry patch, the spot. However, if the underlying cause of these issues stems from internal imbalances, external solutions can only do so much. This is why you might find yourself constantly trying new products with temporary or limited success. For truly healthy skin, we need to look deeper.
Unveiling the Gut-Skin Axis: Your Internal Pathway to Healthier Skin
Get ready for an eye-opening concept: the ��gut-skin axis”. This is the scientific term for the complex, bi-directional communication network between your gastrointestinal tract and your skin. Your gut is a universe of its own, home to trillions of bacteria, fungi, and other microbes collectively known as the gut microbiome. This incredible community doesn’t just help you digest food; it plays a critical role in your immune system, produces essential vitamins, influences inflammatory responses throughout your entire body, and even communicates with your brain. Research continues to explore the intricate relationship of this gut-skin axis, highlighting its significance for overall health and skin wellness.

How the Gut-Skin Axis Delivers on Glowing Skin
Here’s how this intricate connection impacts your skin, based on current understanding:
Inflammation: An imbalance in your gut microbiome, often referred to as dysbiosis (where potentially harmful microbes outweigh beneficial ones), can trigger low-grade, chronic inflammation throughout your body. Studies suggest this systemic inflammation can directly contribute to various skin problems, potentially accelerating visible signs of skin aging like wrinkles, loss of elasticity, and changes in skin tone. This internal inflammation can manifest as increased redness, sensitivity, and even exacerbate conditions like acne, rosacea, and eczema, making the dream of glowing skin elusive. Research also indicates that the gut microbiome is altered in various autoimmune skin diseases such as psoriasis.
Nutrient Absorption: A healthy gut lining is crucial for properly absorbing vitamins (like A, C, E, K, and B vitamins), minerals (like zinc and selenium), and essential fatty acids vital for skin health and repair. If gut function is compromised, your skin might not receive the foundational nourishment it needs to repair damage, maintain its barrier, and look its best for radiant skin. Without these essential nutrients, your skin struggles to regenerate cells and maintain its natural luminosity, impacting your ability to achieve glowing skin.
Hydration: While complex, the gut plays a role in the body’s overall fluid balance. Research suggests that a healthy gut microbiome can help you retain water in your skin, resulting in a more hydrated, youthful appearance. Conversely, an imbalanced gut microbiome can lead to dry, rough-looking skin. Adequate hydration from within is fundamental for supple and resilient skin, directly contributing to that desired healthy glow.
Waste Elimination: A well-functioning gut helps your body efficiently eliminate metabolic waste and toxins. When this process is sluggish or impaired, it’s hypothesized that the body may try to eliminate some waste through other routes, potentially impacting the skin. An overloaded system can lead to breakouts, dullness, and a generally less vibrant complexion.
Essentially, the state of your internal gut environment can significantly impact the health, function, and appearance of your external skin. An unhappy, inflamed, or imbalanced gut can contribute to an unhappy complexion, potentially making you more susceptible to dryness, sensitivity, breakouts, and the visible markers of skin aging we often try to combat with topical products alone. Achieving glowing skin truly starts from within.
Could Your Gut Be Contributing to Your Skin Concerns?
Considering the powerful gut-skin axis, it’s worth reflecting on whether your internal health might be playing a role in the skin changes you’re experiencing, especially if you’re over 35 and finding that external products aren’t delivering the desired results for glowing skin.
Signs that could suggest your gut health might be influencing your skin include:
Experiencing persistent skin issues (like increased sensitivity, reactivity, stubborn dryness, or dullness) alongside digestive discomfort (such as bloating, gas, irregularity, or food sensitivities).
Noticing your skin seems less radiant or resilient than it used to, despite a consistent topical skincare routine.
A history of antibiotic use, chronic stress, or a diet high in processed foods, which can all negatively impact the gut microbiome.
This isn’t about self-diagnosis, but rather recognizing that the body is an interconnected system. Issues in one area can certainly impact another, and exploring gut health offers another avenue for supporting skin wellness and achieving glowing skin.
Supporting Your Gut, Supporting Your Glowing Skin: Actionable Steps
The good news is that you can take proactive steps to support a healthier gut microbiome, which in turn can positively influence your skin’s health and appearance. While individual needs vary, effective strategies often include incorporating natural skincare tips from within:
Dietary Focus: The Foundation for Glowing Skin
Fiber Power: Incorporate a diverse range of high-fiber foods daily. Think fruits (berries, apples with skin), vegetables (leafy greens, broccoli, carrots), legumes (beans, lentils), nuts, seeds, and whole grains (oats, quinoa, brown rice). Fiber feeds beneficial gut bacteria, essential for a healthy gut-skin axis. A diverse fiber intake promotes a robust and varied microbiome, crucial for overall gut health and vibrant skin. Research even suggests that dietary fiber can help protect against allergic skin diseases.
Probiotic Foods: Include fermented foods containing live beneficial bacteria, such as plain yogurt (with live cultures), kefir, sauerkraut, kimchi, miso, and tempeh. These contribute to a balanced gut microbiome. The role of probiotics in skin health is a growing area of research, with promising results.
Prebiotic Foods: Don’t forget foods rich in prebiotics, which act as fuel for probiotics. Examples include garlic, onions, leeks, asparagus, bananas, and oats. Combining prebiotics and probiotics (synbiotics) can offer synergistic benefits for your gut. Studies indicate that prebiotics can help maintain skin’s moisture barrier and ward off signs of aging.
Limit Gut Disruptors: Reduce intake of highly processed foods, excessive sugar, artificial sweeteners, and unhealthy fats, as these can negatively impact microbial balance and promote inflammation, affecting your quest for healthy skin. Ultra-processed foods can adversely impact the gut microbiome by promoting a pro-inflammatory environment. These foods can feed harmful bacteria and contribute to dysbiosis, hindering your journey to glowing skin.

Lifestyle Synergy for Optimal Skin Health
Hydration: Drinking plenty of water throughout the day is fundamental for both optimal gut function (aiding digestion and waste removal) and maintaining skin hydration from within, contributing to radiant skin. Proper hydration helps flush toxins and ensures nutrient delivery to skin cells.
Stress Management: Chronic stress can negatively impact the gut microbiome, potentially altering bacterial composition and increasing gut lining permeability (sometimes called “leaky gut”). Research suggests a close interaction between the gut microbiome and the body’s neurological and hormonal responses to stress. Find sustainable stress-reduction techniques that work for you, such as mindfulness, meditation, deep breathing exercises, yoga, spending time in nature, regular physical activity, or ensuring adequate sleep. Managing stress is a key natural tip for skin wellness and contributes significantly to achieving that coveted glowing skin.

Consider Other Factors: Be mindful of sleep quality, regular moderate exercise (such as brisk walking, cycling, swimming, or dancing), and the potential impact of medications (especially antibiotics, which can disrupt the microbiome) on your gut health. Prioritizing these aspects creates a holistic environment for your gut and, by extension, your skin. Studies have shown that people with insomnia can have an imbalance in their microbiota, and conversely, addressing gut health can improve sleep. If considering probiotic or prebiotic supplements, consult with a healthcare professional to determine the best approach for your individual needs.
Your Journey to Radiant Glowing Skin: Looking Inward
Understanding and nurturing the gut-skin axis is a powerful step in your holistic skin wellness journey. It highlights that true radiance and healthy aging involve supporting your body’s intricate internal systems, not just treating the surface. By focusing on nourishing your gut health through thoughtful diet and lifestyle choices, you’re not only investing in comfortable digestion and overall well-being, but you’re also taking a significant, proactive step towards achieving the glowing skin you desire.
- Natura Radiance.
Disclaimer: This information is for educational purposes only and is not intended as medical advice. If you have persistent gut or skin issues, please consult with a qualified healthcare professional or a registered dietitian for personalized guidance.
#glowingskin#healthyskin#guthealth#gutskinaxis#holistichealth#agingskin#naturalskincare#skincaretips#wellness#naturaradiance
0 notes
Text
Understanding Lymphoma

Lymphoma is a type of cancer that begins in the lymphatic system, an essential part of the body’s immune defenses. It occurs when lymphocytes, a type of white blood cell, grow uncontrollably and accumulate in lymph nodes and other tissues. Understanding lymphoma is important because early detection and treatment can significantly improve outcomes. Although it may sound intimidating, increased awareness and advancements in medical care have made it a manageable condition for many patients. Let’s understand this cancer from our blood cancer specialists in Surat at BCI- Blood And Cancer Institute, so that you are better informed and are able to take timely action.
Types of Lymphoma
There are two main types of lymphoma: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL).
● Hodgkin Lymphoma (HL): This type is marked by the presence of Reed-Sternberg cells, a specific abnormal cell seen under a microscope. HL is relatively rare but often highly treatable, especially when diagnosed early. It commonly affects young adults and has high survival rates with appropriate therapy.
● Non-Hodgkin Lymphoma (NHL): This group includes a wide variety of lymphomas that do not have Reed-Sternberg cells. NHL is more common and can vary greatly in how fast it grows and spreads. Some types of NHL are aggressive and require immediate treatment, while others are indolent and may be monitored without immediate intervention.
Common Symptoms
Recognizing the symptoms of lymphoma early can lead to quicker diagnosis and treatment. Cancer specialist in Surat list its common signs:
● Swollen lymph nodes, often painless, in the neck, armpits, or groin
● Fever without an obvious infection
● Night sweats that soak clothing and sheets
● Unexplained weight loss
● Persistent fatigue and weakness
● Itchy skin that doesn’t go away
● Shortness of breath or chest pain, particularly if lymph nodes in the chest are affected
These symptoms can also result from less serious illnesses, but if they persist for more than a couple of weeks, it’s wise to consult a doctor.
Risk Factors
Hemato-oncologists in Surat lists certain factors that may increase the risk of developing lymphoma:
● Age: Some types are more common in young adults, while others occur more frequently in older adults.
● Gender: Males are slightly more likely to develop certain types of lymphoma.
● Family History: A family history of lymphoma can increase an individual’s risk.
● Weakened Immune System: Conditions like HIV/AIDS, autoimmune diseases, or medications that suppress the immune system raise the risk.
● Infections: Certain viral and bacterial infections, such as Epstein-Barr virus (EBV), Hepatitis C, and Helicobacter pylori, are linked to lymphoma.
● Chemical Exposure: Long-term exposure to certain chemicals like pesticides and solvents may increase risk.
Diagnosis
To diagnose lymphoma, doctors usually start with a physical exam, paying special attention to any swollen lymph nodes. They may then order imaging tests such as CT scans, PET scans, or MRIs to look for enlarged nodes or other signs of disease. A biopsy — removing a small sample of lymph node tissue — is essential to confirm the diagnosis and determine the specific type of lymphoma. Blood tests can assess overall health and identify markers that suggest lymphoma. In some cases, a bone marrow biopsy is also performed.
Treatment Options
Lymphoma treatment depends on the type, stage, and overall health of the patient. Common leukemia treatment in Surat include:
● Chemotherapy: The use of powerful drugs to kill cancer cells throughout the body.
● Radiation Therapy: Targeted radiation to kill cancer cells in specific areas.
● Immunotherapy: Treatments that help the body’s immune system recognize and attack cancer cells, such as monoclonal antibodies.
● Targeted Therapy: Drugs designed to specifically target cancer cell mechanisms, such as proteins or genes driving cancer growth.
● Stem Cell Transplant: In severe cases, patients may need a transplant to restore healthy bone marrow after intensive chemotherapy.
Specialists at blood cancer hospitals in Surat often use a combination of these therapies to achieve the best results. In some low-grade NHL cases, “watchful waiting” is recommended, delaying treatment until the disease shows signs of progression.
Living with Lymphoma
Being diagnosed with lymphoma is life-changing, but many people live long, full lives after treatment. Managing lymphoma often includes:
● Regular follow-up appointments to monitor for recurrence
● Managing side effects from treatments like fatigue, infections, or fertility issues
● Emotional support through counseling, therapy, or support groups
● Maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress management techniques
Survivorship care plans are often created for individuals in remission, providing guidelines for monitoring and maintaining health.
Prognosis
The outlook for lymphoma patients has improved dramatically over the past few decades. Many types of lymphoma respond well to treatment, especially when detected early. Five-year survival rates vary depending on the type and stage of lymphoma, but advancements in therapies and blood cancer treatments in Surat continue to push survival rates higher. For example, the five-year survival rate for Hodgkin lymphoma is about 89%, while many forms of non-Hodgkin lymphoma also have strong survival outcomes.
Final Thoughts
Understanding lymphoma helps demystify a complex disease and highlights the importance of awareness. Persistent symptoms should never be ignored, and seeking medical advice early can make a significant difference. With early detection, proper treatment, and ongoing support, many people diagnosed with lymphoma are able to lead vibrant, fulfilling lives. Staying informed, advocating for oneself in healthcare settings, and building a strong support network are vital steps toward managing lymphoma effectively and maintaining a good quality of life.
0 notes
Text
Best Multiple Myeloma Treatment in India
Top Center for Multiple Myeloma Treatment
BMT Next delivers the best multiple myeloma treatment in India, offering evidence-based and research-driven protocols across all our locations in Gurgaon (Gurugram), Hisar, Faridabad, and internationally through our dedicated unit for Mauritius. Patients trust us for not only our outcomes but also our deep commitment to ethical, patient-focused care.
Our facilities feature highly experienced hematologists, state-of-the-art transplant units, and infection-controlled chemotherapy suites. We focus on integrating autologous stem cell transplant (ASCT), CAR-T therapy, BiTE therapy, and maintenance strategies using lenalidomide and thalidomide to ensure durable remissions in all subtypes of plasma cell cancer. The holistic care we provide includes psychosocial support, pain management, renal support, and long-term rehabilitation. We are a team of best bone marrow transplant specialists.
Understanding Multiple Myeloma: Causes, Risk Factors, and Disease Progression
Multiple myeloma is a hematologic malignancy that originates from plasma cells and disrupts normal blood formation. It can cause severe bone damage, kidney failure, and life-threatening infections. Genetic abnormalities like del(17p) and t(4;14) increase risk and influence prognosis. Environmental exposure to radiation, industrial chemicals, and obesity are also significant contributors to disease onset.
BMT Next incorporates MRD testing, FISH cytogenetics, and regular PET-CT screening to detect disease at early and advanced stages. We actively monitor high-risk individuals such as those with MGUS and smoldering myeloma, allowing for early intervention and improved long-term survival. Trust the best multiple myeloma treatment center in Gurgaon, Hisar, Faridabad and Mauritius.
Signs & Symptoms: When to Consult a Multiple Myeloma Specialist
Patients who experience persistent, unexplained bone pain, repeated infections, fatigue, or symptoms of renal failure may be developing multiple myeloma. Other signs include fractures from minor injuries, frequent fevers, and high calcium levels causing confusion or constipation. At BMT Next, our best hematologists in Gurgaon, Hisar, and Faridabad offer prompt evaluation to initiate immediate diagnostic testing and treatment. We prioritize rapid workup for suspected plasma cell cancer to minimize disease progression. We esnure zero delay, trust us for best multiple myeloma treatment in India and Mauritius.
Types and Staging of Myeloma at BMT Next
BMT Next treats all stages of multiple myeloma, from asymptomatic forms to aggressive relapsed disease. Smoldering myeloma patients undergo close surveillance through light chain assays and bone marrow biopsies. Active myeloma is managed with combinations like VRD or Dara-VRD, followed by autologous stem cell transplant for eligible individuals.
We manage relapsed and refractory multiple myeloma using advanced protocols that include Pomalidomide, Carfilzomib, Elotuzumab, Ixazomib, and access to immunotherapies such as CAR-T therapy and BiTE antibody therapy in India. For high-risk myeloma patients identified by FISH cytogenetics, we use tandem transplants and dual-agent maintenance to reduce recurrence.
Diagnosis at India’s Best Multiple Myeloma Center
Accurate diagnosis is the first step toward delivering the best multiple myeloma treatment in India. At BMT Next, we offer comprehensive diagnostic services that ensure precise staging, risk stratification, and therapy planning. Each patient undergoes an extensive evaluation process at our centers in Gurgaon, Hisar, Faridabad, and for international patients from Mauritius and other countries. This includes a full clinical assessment, imaging, laboratory evaluation, and cytogenetic profiling to define the subtype and aggressiveness of the disease. We have provided remarkable results across India. Trust the best multiple myeloma treatment center in gurgaon.
We perform bone marrow aspiration and trephine biopsy with immunophenotyping to assess the percentage and behavior of plasma cells. Laboratory diagnostics involve serum protein electrophoresis (SPEP), immunofixation electrophoresis (IFE), serum free light chain assay, beta-2 microglobulin, and LDH. These markers help define disease burden and prognosis. Imaging studies such as whole-body PET-CT scans, MRI spine, and skeletal surveys are essential to assess bone involvement. Our FISH cytogenetic testing identifies high-risk abnormalities including del(17p), t(4;14), t(14;16), and 1q gain.
To track treatment response, we utilize MRD (Minimal Residual Disease) testing, performed using flow cytometry and next-generation sequencing (NGS). This helps us determine the depth of remission and guide maintenance and follow-up plans, allowing us to deliver the most effective and individualized myeloma treatment protocols in India.
Advanced Multiple Myeloma Diagnostic Infrastructure
Diagnostic precision defines success in myeloma treatment. At BMT Next, we perform in-house:
Bone marrow aspiration and biopsy with immunophenotyping
SPEP, IFE, and free light chain testing for monitoring protein levels
Whole-body PET-CT scans and MRI spine imaging for detecting bone lesions
FISH cytogenetics to identify chromosomal abnormalities like del(13q), t(11;14), and gain of 1q
MRD testing using flow cytometry and NGS for minimal disease tracking after therapy
Our integrated labs in all locations, including our international referral network, allow for seamless testing and same-day reporting. We are a team of multiple myeloma specialists in Gurgaon, Hisar, Faridabad and Mauritius.
Meet Our Myeloma Specialists at BMT Next
At BMT Next, expert-led care is the foundation of our reputation. Our experts bring years of focused experience in multiple myeloma diagnosis, bone marrow transplant, and advanced immunotherapy in India.
Dr. Meet Kumar (MD, DM Hematology) leads our myeloma transplant center with more than 20 years of experience in treating complex hematologic malignancies. Dr. Neeraj Teotia is recognized for his expertise in FISH cytogenetics and tailoring therapy for high-risk multiple myeloma patients in India. Dr. Umesh Yadav focuses on supportive care protocols, MRD-based monitoring, and long-term survivorship in myeloma patients. Dr. Sumit Joshi, with over 14 years in hemato-oncology and critical care, brings expertise in managing aplastic anemia, leukemia, and post-transplant complications, and is instrumental in coordinating comprehensive care for adult and pediatric myeloma patients.
Together, this multidisciplinary team collaborates to deliver precision medicine through the lens of global guidelines, ensuring patients receive the best myeloma treatment in Gurgaon, Hisar, Faridabad, and internationally in Mauritius.
Multiple Myeloma Treatment Options at BMT Next
Our treatment strategies vary based on disease stage, patient performance status, and cytogenetic risk.
Initial therapy typically includes triplet or quadruplet drug combinations such as VRD, KRD, or Daratumumab-VRD. Following induction, ASCT is the standard for eligible patients. For those ineligible for transplant, long-term oral chemotherapy protocols with Ixazomib, Lenalidomide, or Thalidomide are used.
Patients with relapsed or refractory myeloma are offered innovative options such as CAR-T therapy, BiTE therapy, or newer immunomodulatory and proteasome inhibitors. Maintenance therapy with Lenalidomide or Ixazomib is tailored using MRD results, ensuring precision dosing and minimizing toxicity. Every patient also receives supportive interventions such as bone-strengthening agents, erythropoiesis stimulants, and nephrology input. We are an expert team of Multiple Myeloma Treatment in Gurgaon, Hisar, Faridabad and Mauritius.
Best Multiple Myeloma Treatment Across India
BMT Next offers the best multiple myeloma treatment in India across all our centers with equally advanced, high-quality care. Our Gurgaon center is internationally recognized for excellence in bone marrow transplant, CAR-T cell therapy, and high-risk myeloma management. It is fully equipped with HEPA-filtered BMT units, MRD monitoring, and advanced diagnostic labs. Choose the best multiple myeloma treatment center in Gurgaon!
Our Hisar center delivers the best multiple myeloma treatment in Hisar, offering the same diagnostic accuracy, chemotherapy regimens, and hematologist-led care. It ensures patients in Haryana and nearby regions have access to cutting-edge therapy protocols and transplant referrals without having to travel far.
At our Faridabad center, we provide the best multiple myeloma treatment in Faridabad, with a strong focus on personalized follow-up, imaging support, and rehabilitation care for patients undergoing or recovering from treatment. Our experts here manage relapsed, elderly, and comorbid patients with precision.
For our international patients, the Mauritius coordination desk ensures full access to the best multiple myeloma treatment in India. Patients from Mauritius and the Indian Ocean region receive direct support for travel, interpreter services, scheduling, and remote follow-up. They are treated on par with domestic patients, with equal access to CAR-T, BiTE, and ASCT therapies offered across all BMT Next centers.
Frequently Asked Questions (FAQs)
1. What is multiple myeloma and how is it different from other blood cancers?
Multiple myeloma is considered a cancer of plasma cells, a type of white blood cell that helps fight infection. Unlike leukemia or lymphoma, it majorly affects the bone marrow and skeletal system.
2. What are the early signs of multiple myeloma?
Early signs include persistent bone pain, frequent infections, unexplained fatigue, anemia, kidney dysfunction, and high calcium levels.
3. How is multiple myeloma diagnosed at BMT Next? We use a combination of blood tests (SPEP, IFE, FLC), bone marrow biopsy, PET-CT or MRI, and FISH cytogenetic studies to confirm diagnosis and risk stratify the disease.
4. What is the role of FISH cytogenetics in myeloma diagnosis?
FISH identifies genetic abnormalities like del(17p), t(4;14), or 1q gain, which help us predict prognosis and customize treatment.
5. Is bone marrow transplant mandatory for all myeloma patients?
No. Autologous stem cell transplant (ASCT) is recommended for eligible patients to prolong remission, but alternatives exist for transplant-ineligible individuals.
6. What is CAR-T therapy and is it available at BMT Next? CAR-T therapy involves genetically modifying a patient's own T-cells to fight myeloma. It is available through clinical access programs at BMT Next.
7. What are the treatment options for relapsed or refractory myeloma?
Options include immunomodulators like Pomalidomide, monoclonal antibodies like Daratumumab, BiTE therapies, and CAR-T cells.
8. How does BMT Next monitor treatment response?
We use MRD (minimal residual disease) testing via flow cytometry or NGS to monitor the depth of remission after treatment.
9. Are there different types of multiple myeloma?
Yes, including smoldering myeloma (asymptomatic), active myeloma (requiring treatment), and relapsed/refractory myeloma.
10. What support services are offered at BMT Next for myeloma patients?
Patients receive nutritional counseling, pain management, physiotherapy, renal care, and emotional wellness support throughout treatment.
11. What makes BMT Next the best center for multiple myeloma treatment in India?
BMT Next offers the best multiple myeloma treatment in India through its expert-led centers in Gurgaon, Hisar, Faridabad, and Mauritius. Our strength lies in bone marrow transplant excellence, MRD-based treatment, next-level FISH cytogenetics, and access to CAR-T and BiTE therapy. Patients across North India and internationally choose BMT Next for high-quality, affordable, and personalized plasma cell cancer treatment.
12. How can patients from Mauritius access myeloma care at BMT Next?
Our international patient desk helps with appointment scheduling, visa support, travel coordination, and follow-up teleconsultation.
13. How often should follow-up occur after myeloma treatment?
Follow-up is typically every 3–6 months with blood tests, MRD monitoring, and imaging when needed.
14. What is lenalidomide maintenance and why is it important?
Lenalidomide is used after transplant or initial therapy to maintain remission and delay progression. It is a cornerstone of long-term management.
15. Are affordable treatment packages available for myeloma at BMT Next?
Yes. We offer cost-effective care across Hisar, Faridabad, and Gurgaon with insurance, CGHS, and EMI support.
Book an Appointment
Your journey to remission begins with one consultation. Let the best hematologists in India guide your path toward recovery and long-term care.
0 notes
Text
Aspergillus Fungus Alert: Inhaling Danger — The Fungus That Eats You from the Inside Out
When we think of deadly health threats, fungi rarely come to mind. But one microscopic organism is gaining serious attention — the Aspergillus fungus — and you might be breathing it in right now without even knowing.
This common mold, found in everything from soil to household dust, is harmless for most people. But under the right conditions, it can cause life-threatening infections by eating away at the body from the inside out — particularly in those with weakened immune systems.

What Is the Aspergillus Fungus and Why Is It So Dangerous?
The Aspergillus fungus includes more than 180 species, but one — Aspergillus fumigatus — is especially dangerous to humans. While most people inhale its spores daily without issue, individuals with compromised immune systems can develop a deadly condition known as invasive aspergillosis.
In these cases, the Aspergillus fungus takes root in the lungs and rapidly spreads to other organs, breaking down tissue and triggering organ failure.
How the Aspergillus Fungus Attacks the Body
Once inhaled, the spores of the Aspergillus fungus can multiply and invade the body’s tissues. It starts in the lungs and may travel to the brain, heart, kidneys, and even the skin. Think of it like a fungal invasion spreading through the body, disrupting vital systems and feeding off weakened tissue.
Common symptoms include:
Persistent fever
Chest pain
Coughing (possibly with blood)
Breathing difficulties
Confusion or neurological issues (if it reaches the brain)
Without quick diagnosis and treatment, invasive aspergillosis can be fatal within days.
The New Threat: Drug-Resistant Aspergillus Fungus
One of the most alarming developments is that the Aspergillus fungus is becoming resistant to antifungal drugs, especially azoles — a common class of medication.
The main reason? Widespread use of fungicides in agriculture, which mimics the effect of medical antifungals. This allows resistant strains to evolve in the environment and make their way into hospitals, where they are much harder to treat.
Drug-resistant Aspergillus infections are rising, especially in ICU settings and among COVID-19 survivors.
Can the Aspergillus Fungus Spark a Health Crisis?
Although the Aspergillus fungus doesn’t spread from person to person like a virus, experts still warn it could cause pandemic-like pressure on global healthcare systems.
Why?
It’s infecting vulnerable ICU patients.
Drug-resistant strains are on the rise.
It’s linked to increased hospital deaths.
Climate change and pollution are making exposure more common.
The World Health Organization (WHO) has named Aspergillus fumigatus a top-priority fungal threat — a clear sign that global health leaders are paying attention.
Who’s Most at Risk of Aspergillus Fungus Infection?
While healthy people are generally safe, the Aspergillus fungus poses serious danger to:
Cancer patients undergoing chemotherapy
Organ or stem cell transplant recipients
Individuals with chronic lung diseases (COPD, asthma)
ICU patients (especially on ventilators)
Immunocompromised individuals (e.g., HIV/AIDS)
Even something as routine as hospital renovations can release fungal spores into the air, creating hidden risks for vulnerable patients.
How Can We Protect Ourselves from Aspergillus Fungus?
To fight back against the Aspergillus fungus, public health experts recommend:
Better diagnostics – early detection saves lives.
New antifungal treatments – especially for resistant strains.
Responsible use of fungicides – in both medicine and agriculture.
Public awareness – people need to understand fungal threats.
Fungal infections are often overshadowed by viruses and bacteria — but the Aspergillus fungus proves that ignoring them could be a fatal mistake.
Final Thoughts: Don’t Underestimate the Aspergillus Fungus
It may be invisible and silent, but the Aspergillus is not harmless. For the vulnerable, it can be deadly. With rising drug resistance, climate-related risks, and growing ICU cases, it’s time to take fungal infections seriously.
While it won’t cause a traditional pandemic, the Aspergillus could still be one of the most dangerous health threats of our time — and it’s already in the air we breathe.
More Blogs That You Should Read
Top 6 Incredible Health Advantages of Apple Cider Vinegar
Is Alcohol and Milk Safe to Drink Together?
Struggling with Acne? – Try These 20 Proven Ways to Get Clear Skin Now!
Managing High Blood Pressure Lowers Dementia Risk
1 note
·
View note
Text
Redefining Modern Medicine: How Innovation Is Changing Patient Care Forever
Medicine is undergoing one of its most significant transformations in history. What was once defined by routine procedures, reactive treatment, and face-to-face interactions is now evolving into a dynamic, proactive, and technology-driven experience. The most recent medical advances are not just improvements in technique—they are entirely reshaping the patient experience, offering new hope, better outcomes, and more personalized care. As science and innovation continue to merge, a new era of healthcare has emerged, one that puts the patient firmly at the center.
The Emergence of Personalized Health Solutions
Today’s patients are no longer just recipients of generic treatments. With the rise of personalized medicine, healthcare is becoming more individualized. Doctors can now use a patient’s genetic information, medical history, and lifestyle data to tailor treatments that suit their needs. This revolutionary shift allows care providers to move away from the “one-size-fits-all” approach that has long dominated traditional medicine.
Through genomic testing and other diagnostic tools, physicians can understand how a patient may respond to a particular medication or therapy before treatment even begins. This is especially impactful in cancer care, where genetic mutations in tumors can be targeted with therapies designed to block their growth or destroy them entirely. In chronic conditions such as heart disease or autoimmune disorders, precision medicine helps reduce trial and error, guiding physicians toward options that are most likely to succeed.
Personalized medicine is not just about effective treatments. It’s about empowering patients with information that can help them make better decisions about their health, manage their conditions more effectively, and, in some cases, even prevent illness altogether.
Digital Healthcare Is Changing the Game
Technology has changed how we communicate, shop, and work—and now it’s transforming how we access medical care. Digital health has exploded in recent years, mainly through the widespread adoption of telemedicine. Patients can now consult with doctors and specialists from their homes, often without long waits or the need to travel.
This digital shift has expanded healthcare access to people in remote or underserved areas. It has also allowed busy individuals and those with mobility challenges to stay connected to their providers. More than just convenience, telemedicine helps catch potential health problems earlier by making it easier for patients to seek help when symptoms arise.
Additionally, online health portals and mobile apps are now used for appointment scheduling, medical records, lab results, and direct messaging with care teams. These tools give patients more control and transparency in their healthcare journey. Remote monitoring, especially for chronic disease management, is also becoming a standard part of care, using smart devices to transmit vital signs and health data to providers in real-time.
Regenerative Therapies Offer New Possibilities
The promise of regenerative medicine is becoming a reality. Instead of simply treating symptoms, scientists and doctors focus on repairing or even regenerating tissues and organs. At the heart of this innovation are stem cells, tissue engineering, and gene therapy—fields pushing the boundaries of what the human body is capable of.
Patients with spinal cord injuries, degenerative joint conditions, or organ failure now have new recovery options. Scientists are using a patient’s stem cells to generate tissues that are less likely to be rejected by the body. In the lab, researchers are exploring the potential to grow organs that could one day replace the need for transplants.
These therapies are still developing in many cases, but clinical trials and early results have shown incredible potential. Gene therapy, in particular, is being used to correct inherited genetic conditions, giving hope to patients who were once told their conditions were untreatable. With continued research and investment, regenerative medicine may soon become a routine part of mainstream care.
Artificial Intelligence Enhancing Clinical Decision-Making
Artificial intelligence is no longer a futuristic concept—it’s already making a significant impact in healthcare. AI systems can analyze massive amounts of data in a fraction of the time it would take a human doctor. These tools assist in identifying patterns, predicting disease progression, and recommending the best treatment strategies.
AI algorithms are trained to detect abnormalities on imaging scans with remarkable accuracy in radiology. In some cases, they can even identify signs of cancer or neurological disorders earlier than traditional methods. By augmenting human expertise, AI helps reduce errors and ensures physicians have the most complete picture when making decisions.
Beyond diagnostics, AI is used in hospital operations to optimize patient flow, reduce wait times, and manage staffing. It is also being integrated into electronic health records to help with documentation and streamline clinical workflows. These improvements free up more time for doctors to spend with their patients, enhancing the quality of care.
Wearable Devices Empowering Everyday Health
Smartwatches and fitness trackers have evolved far beyond counting steps. Today, they are essential health tools that help individuals monitor their vital signs and manage chronic conditions. These wearable devices can track heart rate, oxygen saturation, and sleep patterns and even detect irregular heart rhythms that could signal underlying health issues.
Patients with diabetes are using continuous glucose monitors to keep their blood sugar in check without the need for constant finger pricks. Those with heart disease can receive alerts when their heart rate spikes or drops suddenly, prompting them to take immediate action or contact their healthcare provider.
By gathering real-time data, wearables enable proactive care and encourage healthier behaviors. Doctors can also use the data to understand how a patient is doing between visits, allowing for medication adjustments or lifestyle recommendations without waiting for the next appointment. This real-world, continuous feedback loop transforms how healthcare is delivered and received.
Minimally Invasive Surgery Improving Recovery
Thanks to minimally invasive techniques and robotic-assisted tools, surgical procedures have become safer and more efficient. These advances mean that many surgeries that once required large incisions and long hospital stays can now be performed with smaller cuts, less pain, and faster recovery times.
Surgeons can perform complex procedures with enhanced precision and control using robotic systems. These systems translate the surgeon’s hand movements into minor, precise actions inside the patient’s body. The results are less tissue trauma, fewer complications, and quicker returns to normal activities.
Patients benefit immensely from these techniques, not only physically but emotionally. The reduced pain, shorter hospital stays, and minimal scarring contribute to higher satisfaction and better overall outcomes.
Mental and Emotional Wellness Gaining Recognition
Healthcare professionals are increasingly acknowledging that mental health is inseparable from physical health. Stress, anxiety, and depression can have a significant impact on how patients recover from illness, manage chronic conditions, and even respond to medications.
As a result, many healthcare systems are integrating mental health services into primary care. Patients are encouraged to speak openly about their emotional well-being and offered therapy, counseling, and support when needed. The rise of digital mental health platforms has also made it easier to access care, removing some of the stigma and logistical barriers that have kept people from getting help in the past.
This whole-person approach to treatment ensures that patients receive care that supports every aspect of their health, not just their physical symptoms.
Healthcare’s New Frontier Is Here
The latest advances in medical treatment represent more than just technological progress—they reflect a new philosophy of care—a philosophy where patients are not passive recipients but active participants, a system where care is tailored, timely, and compassionate. With innovations in genomics, telehealth, AI, regenerative medicine, and mental health integration, the future of patient care is already unfolding.
These breakthroughs are more than trends. They are the foundation of a healthcare system built around people—one that listens, learns, adapts, and heals with precision and empathy. As medicine continues to advance, one thing is sure: the future of healing has arrived and is changing lives for the better every day.
0 notes