#Respiratory Virus
Explore tagged Tumblr posts
Text

side-eyeing all the anti-vaccine, anti-masks, "get back to normal," "the kids will be fine" fucktwats hella hard right now. fuck everyone one of you.
#COVID#brain health#cognitive deficits#memory problems#brain inflammation#brain aging#brain volume#brain structure#COVID-19#SARS-CoV-2#long COVID#brain damage#dementia#autopsies#respiratory virus
91 notes
·
View notes
Text

Very high COVID levels were detected in 7 states in the US. Doctors continue to urge people to get up-to-date COVID-19 vaccinations, especially if they are in higher-risk groups.
https://ktla.com/news/california/very-high-covid-levels-detected-in-californias-wastewater-first-since-winter/
CDC’s Respiratory Virus Guidance
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
4 notes
·
View notes
Text
#Human Metapneumovirus (HMPV)#HMPV Symptoms#Metapneumovirus Infection#Respiratory Virus#HMPV Causes#HMPV Transmission#HMPV Treatment#HMPV Diagnosis#Respiratory Illness in Children#Seasonal Respiratory Viruses#HMPV in Adults#Bronchiolitis and HMPV#HMPV vs. RSV#Upper Respiratory Infections#Lower Respiratory Tract Infection#HMPV Pneumonia#HMPV in Infants#HMPV Risk Factors#HMPV in Older Adults#HMPV Complications#HMPV Treatment Options#Antiviral Medications for HMPV#Supportive Care for HMPV#HMPV Prevention#Vaccines for HMPV#HMPV Testing#HMPV in Immunocompromised Individuals#HMPV Pathogenesis#HMPV Epidemiology#HMPV and COVID-19 Coinfection
1 note
·
View note
Text
"No Reason to Worry," Says India after 7 HMPV Cases
Seven instances of the Human Metapneumovirus (HMPV), a respiratory virus that recently attracted attention following an epidemic in China, have been reported from India. According to the Center, “there is no reason to panic” because the HMPV is already “circulated” throughout the world. Have a look at few developments on HMPV There have been two new HMPV cases reported from Nagpur, Maharashtra.…
#bronchopneumonia#featured#India#respiratory virus#sciencenews#Severe Acute Respiratory Illness (SARI)
0 notes
Text
What is Human Metapneumovirus (HMPV)?
What is Human Metapneumovirus (HMPV)?
Human Metapneumovirus (HMPV) is a respiratory virus that can cause a range of symptoms, from mild cold-like signs to severe respiratory distress. It was first identified in 2001, making it a relatively new addition to the family of viruses known to affect humans. Despite its relatively recent discovery, HMPV has since been recognized as a significant contributor to respiratory illness worldwide, particularly in young children, the elderly, and immunocompromised individuals. Understanding the nature of HMPV, its symptoms, transmission, treatment, and prevention measures is essential to managing its impact on public health.
What is HMPV?
HMPV belongs to the Metapneumovirus genus, which is part of the Paramyxoviridae family. This family also includes other well-known respiratory viruses such as the measles virus, mumps virus, and respiratory syncytial virus (RSV). HMPV, however, is genetically distinct from these other pathogens and has its own set of characteristics.
The virus primarily infects the upper and lower respiratory tract and is a leading cause of respiratory infections in infants and young children. However, adults, particularly those with weakened immune systems or underlying chronic conditions, can also be affected. In fact, similar to other respiratory viruses, HMPV is known to circulate in seasonal patterns, with outbreaks often occurring in the fall and winter months, peaking around the same time as influenza and RSV infections.
Symptoms of HMPV Infection
Infection with HMPV can present with a range of symptoms, which may vary from mild to severe, depending on the individual’s age, immune status, and any underlying health conditions. In children, particularly those under five years of age, HMPV is one of the leading causes of respiratory illness, including bronchiolitis and pneumonia.
The symptoms of HMPV infection can include:
Upper Respiratory Symptoms:
Nasal congestion
Runny nose
Coughing
Sore throat
Lower Respiratory Symptoms:
Wheezing
Shortness of breath
Rapid breathing
Chest tightness
General Symptoms:
Fever
Fatigue
Headache
While most individuals recover from HMPV infections within a week or two, some may develop more severe respiratory complications. The elderly, infants, and those with weakened immune systems or preexisting lung diseases such as asthma or chronic obstructive pulmonary disease (COPD) are at greater risk for developing serious illness.
Transmission of HMPV
HMPV is transmitted primarily through respiratory droplets when an infected person coughs, sneezes, or talks. It can also spread through direct contact with contaminated surfaces or by touching the mouth, nose, or eyes after touching surfaces that have been exposed to the virus.
Like other respiratory viruses, HMPV is highly contagious, and outbreaks are common, particularly in settings where close contact occurs, such as schools, daycares, hospitals, and nursing homes. The virus can remain viable on surfaces for several hours, making hand hygiene and disinfecting surfaces critical in preventing transmission.
Who is at Risk?
While HMPV can infect individuals of all ages, certain groups are at higher risk for severe illness or complications. These groups include:
Infants and Young Children: Infants, particularly those under one year of age, are more susceptible to severe respiratory symptoms, including bronchiolitis and pneumonia. In fact, HMPV is one of the leading causes of hospitalization in young children for respiratory illnesses.
Elderly Adults: Older adults, especially those with underlying health conditions such as COPD, asthma, or heart disease, are more likely to experience severe symptoms of HMPV infection.
Immunocompromised Individuals: Those with weakened immune systems, including individuals undergoing cancer treatments or those with conditions like HIV/AIDS, are at increased risk of more severe disease.
People with Chronic Respiratory Conditions: Patients with pre-existing respiratory conditions are also more likely to experience complications, including exacerbations of asthma or COPD.
Diagnosis of HMPV Infection
Diagnosing HMPV infection involves assessing clinical symptoms and performing laboratory tests. Given that HMPV shares symptoms with other respiratory infections like the flu, RSV, and the common cold, a detailed medical history and clinical examination are essential for diagnosis.
Laboratory tests that may be used to confirm HMPV include:
Polymerase Chain Reaction (PCR): This test detects the virus's genetic material in respiratory samples, such as a nasal swab, throat swab, or sputum.
Immunofluorescence: This method identifies HMPV proteins in respiratory secretions.
Viral Culture: Although less commonly used due to the time it takes, this test grows the virus from a sample to confirm the presence of HMPV.
In some cases, chest X-rays or other imaging techniques may be used to assess the extent of lung involvement, particularly if pneumonia or bronchiolitis is suspected.
Treatment of HMPV
Currently, there is no specific antiviral treatment for HMPV infection. Management is primarily supportive and focuses on alleviating symptoms. In most cases, individuals with mild illness recover with rest, hydration, and over-the-counter medications to reduce fever and ease discomfort.
For more severe cases, especially in young children or high-risk adults, hospitalization may be necessary. Treatment options for hospitalized patients may include:
Oxygen therapy to help maintain adequate oxygen levels in the blood.
Nebulized treatments to relieve wheezing or improve airflow in the lungs.
Intravenous (IV) fluids to prevent dehydration, especially if the individual is unable to drink enough fluids.
Mechanical ventilation in extreme cases, where patients have difficulty breathing on their own.
Antibiotics are not effective against viral infections like HMPV, so they are not used unless there is a secondary bacterial infection.
Prevention of HMPV
Because there is no vaccine for HMPV, prevention relies on reducing the risk of exposure and minimizing transmission. Strategies to prevent HMPV infection include:
Good Hygiene Practices:
Frequent handwashing with soap and water for at least 20 seconds, particularly after coughing or sneezing.
Using alcohol-based hand sanitizers when soap and water are not available.
Avoiding touching the face, especially the eyes, nose, and mouth.
Respiratory Hygiene:
Covering the mouth and nose with a tissue or elbow when coughing or sneezing.
Disposing of tissues immediately and washing hands afterward.
Avoiding Close Contact with Sick Individuals:
Avoiding contact with individuals who are showing symptoms of a respiratory illness, particularly in high-risk settings such as hospitals or daycare centers.
Disinfecting Surfaces:
Regularly cleaning and disinfecting frequently touched surfaces, such as doorknobs, light switches, and toys in childcare settings.
Conclusion
Human Metapneumovirus (HMPV) is an important respiratory virus that can cause a range of respiratory illnesses, particularly in children, the elderly, and individuals with weakened immune systems. While there is no specific antiviral treatment or vaccine available for HMPV, supportive care is effective for most patients. Prevention measures, including good hygiene, respiratory hygiene, and minimizing contact with infected individuals, remain the most effective means of reducing the spread of HMPV. As more research is conducted into the virus, we may gain a better understanding of its behavior and develop better diagnostic, therapeutic, and preventive strategies to manage its impact on global health.
#Human Metapneumovirus#HMPV infection#Respiratory illness#Respiratory virus#Pneumonia#asthma#health issues#Cold-like symptoms#Viral respiratory disease#RNA virus#Viral load#Diagnosis of HMPV#HMPV treatment#Preventing HMPV spread#Vaccine research#HMPV epidemiology#HMPV symptoms#HMPV mutations and variants#Virus incubation period
0 notes
Text
HMPV Virus : नवीन संकट की अफवा?
HMPV Virus : आजच्या घडीला चीनमध्ये ह्यूमन मेटा न्यूमोव्हायरस (एचएमपीव्ही) विषाणूच्या संभाव्य प्रादुर्भावामुळे जगभरात चिंता पसरली आहे. कोविड-19 महामारीच्या आठवणी अजूनही ताज्या असताना, या नव्या विषाणूबाबत जागतिक आरोग्य समुदाय सज्ज झाला आहे. चला या व्हायरसची माहिती, त्याचे परिणाम आणि प्रतिबंधात्मक उपाय यावर सविस्तर चर्चा करू.
#agriculture#breaking news#good omens#marathi#naruto#news#HMPV Virus#Human Metapneumovirus#Respiratory Virus#Viral Infection#Flu-like Symptoms#Bronchitis#Pneumonia#Virus Prevention#Airborne Disease#Virus Transmission#Pandemic Alert#Health Awareness#Viral Outbreak#Respiratory Illness#Winter Virus#Child Health#Vulnerable Groups#No Vaccine#Virus Precautions#China Health Crisis#Virus Similar to COVID-19
0 notes
Text
Respiratory Virus Going Around: Vaccination Updates and Recommendations

https://bestinusafortrendnewssmarthomeandeasyloanadvise.com/respiratory-virus-going-around/
0 notes
Text
The very first time I forgot to wear one while visiting with someone indoors I got Covid. A good well fitting N95 works well. I wear one in indoor public places and at home when visitors come. I have only been sick once since the summer of 2020. It happened in 2024 when I answered the door with no mask and got Covid from an asymptomatic person who had been on a plane unmasked. H5N1 is spread just like Covid. It has been found in wastewater in many places especially in the US. We need to protect ourselves. Respirators like N95's good ventilation, and vaccines all work. The science has proven it again and again.
357 notes
·
View notes
Text

He’s never been sick before.
#chiligerart#comics#loathsome coworkers#darth vader#cc 2224#storm trooper#ensign#vent resident#the head medic#star wars#2224 is a workaholic at the worst of times#i.e. when he’s infected with a virus#Vader’s mostly concerned about himself. his respiratory systems already a mess he can’t afford to be sick#yeeee feels good to draw these doofuses again
1K notes
·
View notes
Note
You're posting a lot about politics for a period drama blog 🙄
Buckle in motherfucker, I'm here all goddamn night
#politics#US politics#Kamala Harris#us elections#I'm on so many pain killers for a respiratory virus I probably won't remember half of this#Prednisone makes me violent#awkward-sultana speaks#Awkward-Sultana#ask#Donald Trump#pinning this in case anyone else has ✨commentary✨
72 notes
·
View notes
Text
Also preserved on our archive
Another perfect example of how masking to help prevent covid keeps us *all* safer from *all* airborne illness.
by Tamara Schneider
Lingering respiratory viruses set the stage for chronic lung disease, mouse study shows
Doctors have long known that children who become seriously ill with certain respiratory viruses such as respiratory syncytial virus (RSV) are at elevated risk of developing asthma later in life. What they haven’t known is why.
A new study by researchers at Washington University School of Medicine in St. Louis may have solved the mystery. The study, in mice, shows that respiratory viruses can hide out in immune cells in the lungs long after the initial symptoms of an infection have resolved, creating a persistently inflammatory environment that promotes the development of lung disease. Further, they showed that eliminating the infected cells reduces signs of chronic lung damage before they progress to a full-blown chronic respiratory illness.
The findings, published Oct. 2 in Nature Microbiology, point to a potential new approach to preventing asthma, chronic obstructive pulmonary disease (COPD) and other chronic lung diseases by eradicating the persistent respiratory viruses that fuel these conditions.
“Right now, children who have been hospitalized for a respiratory infection such as RSV are sent home once their symptoms resolve,” said senior author Carolina B. López, PhD, a professor of molecular microbiology and a BJC Investigator at WashU Medicine. “To reduce the risk that these children will go on to develop asthma, maybe in the future we will be able to check if all of the virus is truly gone from the lung, and eliminate all lingering virus, before we send them home.”
About 27 million people in the U.S. are living with asthma. Many factors influence a person’s likelihood of developing the chronic breathing illness, including living in a neighborhood with poor air quality, having exposure to cigarette smoke and being hospitalized for viral pneumonia or bronchitis while young. Some researchers — López included — suspected that the link between serious lung infection and subsequent asthma diagnosis was due to lingering virus in the lungs that causes ongoing damage, but a direct link between the ongoing presence of virus and chronic lung disease has not been previously shown.
López and first author Ítalo Araújo Castro, PhD, a postdoctoral researcher in her lab, developed a unique system involving a natural mouse virus known as Sendai virus, and fluorescent markers of infection. Sendai is related to human parainfluenza virus, a common respiratory virus that, like RSV, has been linked to asthma in children. Sendai behaves in mice in very much the same way that human parainfluenza virus behaves in people, making it an excellent model of the kinds of infections that could lead to chronic lung disease.
Using the fluorescent trackers, the researchers could observe signs of the virus throughout infection. After about two weeks, the mice recovered, but viral RNA and protein were still detectable several weeks later in their lungs, hidden away in immune cells.
“Finding persistent virus in immune cells was unexpected,” López said. “I think that’s why it had been missed before. Everyone had been looking for viral products in the epithelial cells that line the surface of the respiratory system, because that’s where these viruses primarily replicate. But they were in the immune cells.”
Moreover, the presence of the virus changed the behavior of the infected immune cells, causing them to become more inflammatory than the uninfected immune cells. Persistent inflammation sets the stage for chronic lung disease to arise, the researchers said. Indeed, seven weeks after infection, the mice’s lungs exhibited inflammation of air sacs and blood vessels, abnormal development of lung cells and excess immune tissue — all signs of chronic inflammatory lung damage, even though the mice appeared outwardly to have recovered. Once the infected immune cells were eliminated, the signs of damage diminished.
“We use a perfectly matched virus-host pairing to prove that a common respiratory virus can be maintained in immunocompetent hosts for way longer than the acute phase of the infection, and that this viral persistence can result in chronic lung conditions,” Castro said. “Probably the long-term health effects we see in people who are supposed to be recovered from an acute infection are actually due to persistence of virus in their lungs.”
The findings point to new ways to think about preventing chronic lung diseases, the researchers said.
“Pretty much every single child gets infected with these viruses before the age of 3, and maybe 5% get serious enough disease that they could potentially develop persistent infection,” López said. “We’re not going to be able to prevent children from getting infected in the first place. But if we understand how these viruses persist and the effects that persistence has on the lungs, we may be able to reduce the risk of serious long-term problems.”
Study: Castro IA, Yang Y, Gnazzo V, Kim DH, Van Dyken SJ, López CB. Murine parainfluenza virus persists in lung innate immune cells sustaining chronic lung pathology. Nature Microbiology. Oct. 2, 2024. DOI: 10.1038/s41564-024-01805-8
www.nature.com/articles/s41564-024-01805-8 (PAYWALLED)
#mask up#covid#pandemic#covid 19#wear a mask#public health#sars cov 2#coronavirus#still coviding#wear a respirator#flu#influenza#RSV#respiratory syncytial virus
43 notes
·
View notes
Text




Influenza-Like Illnesses (ILI) is characterized by coughs, colds, and fever, and is commonly due to respiratory viruses.
#respiratoryillness #respiratory #respiratoryhealth
The top 5 causative agents of ILI in the Philippines are rhinovirus, enterovirus, influenza A, Respiratory Syncytial Virus (RSV), and adenovirus.
#Influenza-Like Illnesses#ILI#respiratory#respiratory illness#respiratoryhealth#enterovirus#rhinovirus#influenza a#respiratory syncytial virus#adenovirus#respiratory infections#respiratory virus
0 notes
Text
Ranking suspicious herbal teas that claim to ease cold symptoms
Because all I have been able to eat this weekend is soup and tea Elderflower Spice: 3/10 the flavor of this tea is like if the ghost of toothpaste fucked a teabag that I steeped twenty times. Still better than my previous encounters with elderberry, which is its evolved form
Nettle Leaf: 4/10 I will be honest this is the most tea-like in my current stash of dubious herbs. Fine with enough sugar and steeped to dark brown. Claims to be good for aches and pains, this N of one has seen zero improvement correlated to it.
Licorice Chamomile Passionflower Valerian: 6/10 I did not read this package before I started drinking it. Valerian actually has some chemical effect on humans, so like. Don't take it as a supplement. There is not enough in this tea to do anything. Tastes pretty good if you like licorice. Licorice and Slippery Elm: 9/10 this one I feel like actually works to make my eustacian tubes not feel like they're being sanded every time I swallow. Docked one point because I don't fucking have any right now, in my hour of need (10 pm)
#Staying home from work for this one#Because I am probably aggressively contagious#and also because I have to pee every hour on the hour#because the medicine regimen so far has been zinc#and as much tea as I can stomach#I have been accused of having colds like a man#but it's my complete lack of tonsils and adenoids#Every virus that comes through thinks my upper respiratory is a fucking music festival
22 notes
·
View notes
Text
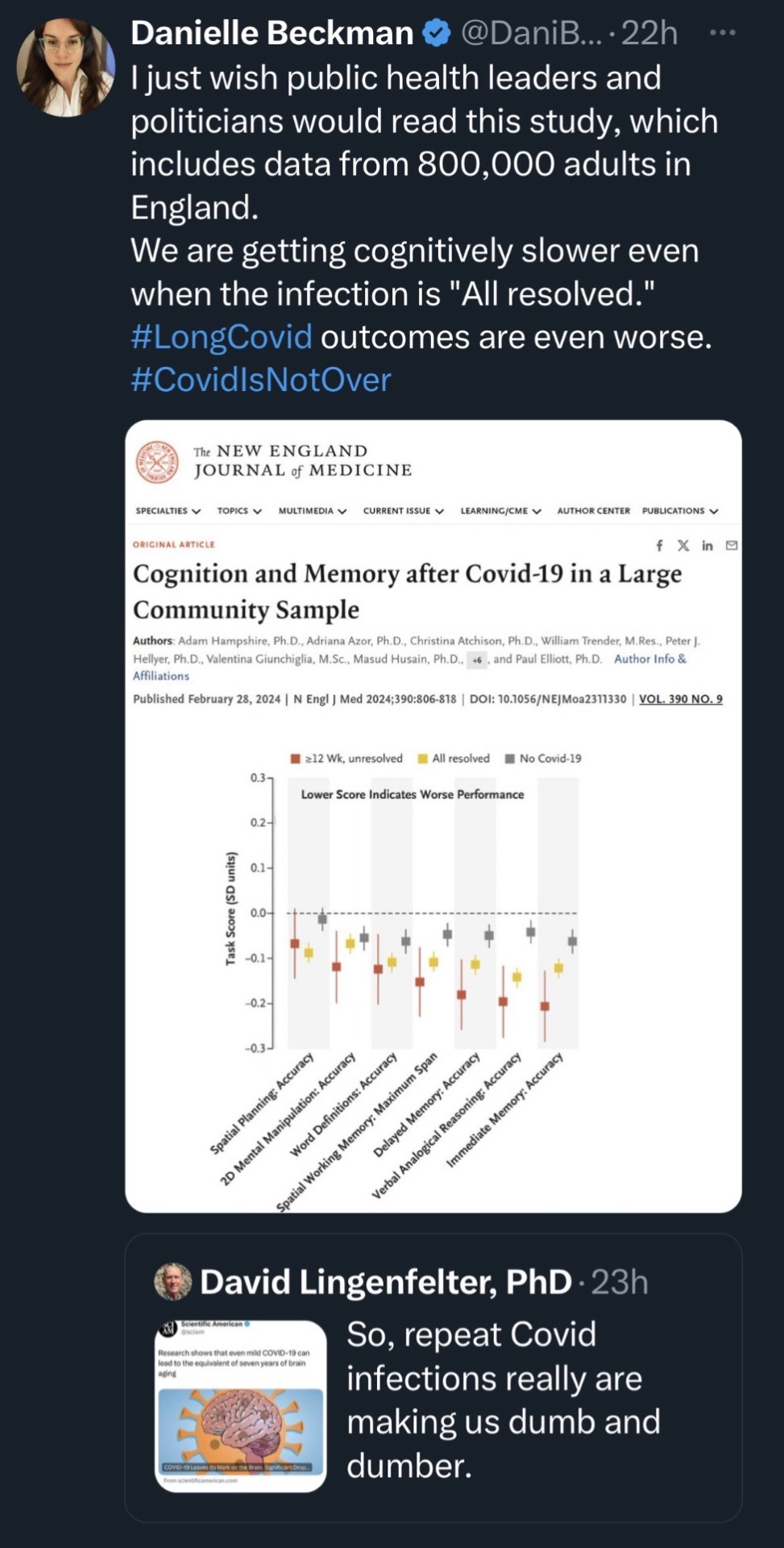
Abstract:
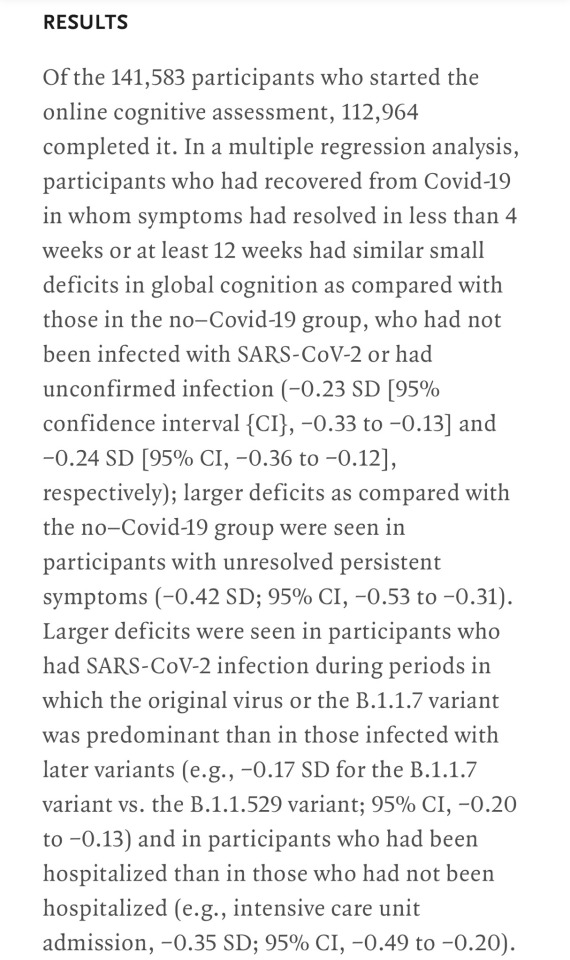
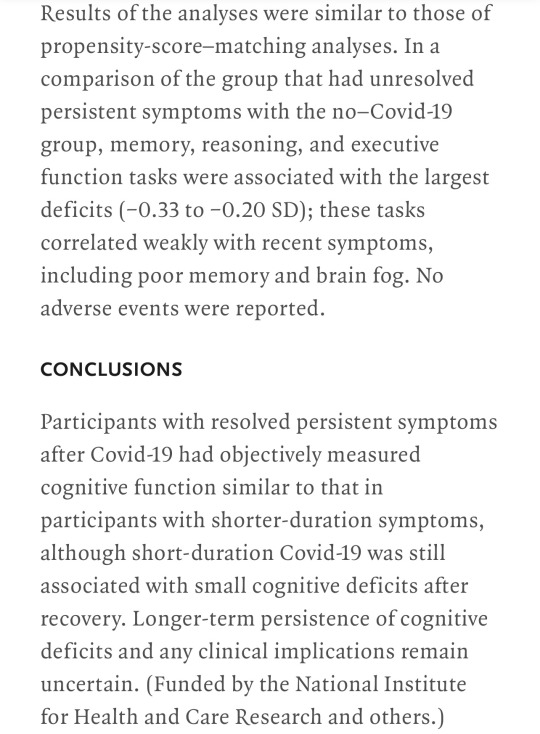
Full article here
#long covid#covid is more akin to hiv than the common cold#as a virus#it affects the nervous system and cardiovascular#and respiratory#and muskoskeletal#it remains in your system years after the initial infection#with cumulative negative effects#and research keeps showing just how devastating the true effects of Covid are#but ppl wanna say it’s just a cold and political mandates are banning masks#????????#how dumb do you have to be#covid 19#covid#covid isn't over#not 1d#public health#turning medicine and health into a political game has done indescribable harm and continues to do so
22 notes
·
View notes
Text
they actually only let you do modern web design if youre skilled in compiling so many javascript elements on one page that all incoming traffic is funnelled behind a ten second wait time for all the stupid little widgets to load. and if you get really good at it the government hires you to make their websites the stupidest and worst working
#is the respiratory virus hub a good resource for tracking covid numbers in ireland? undoubtedly#does it make my laptop go into cardiac arrest every time ? also yes#thanks hse
11 notes
·
View notes