#HMPV infection
Explore tagged Tumblr posts
Text
What is Human Metapneumovirus (HMPV)?
What is Human Metapneumovirus (HMPV)?
Human Metapneumovirus (HMPV) is a respiratory virus that can cause a range of symptoms, from mild cold-like signs to severe respiratory distress. It was first identified in 2001, making it a relatively new addition to the family of viruses known to affect humans. Despite its relatively recent discovery, HMPV has since been recognized as a significant contributor to respiratory illness worldwide, particularly in young children, the elderly, and immunocompromised individuals. Understanding the nature of HMPV, its symptoms, transmission, treatment, and prevention measures is essential to managing its impact on public health.
What is HMPV?
HMPV belongs to the Metapneumovirus genus, which is part of the Paramyxoviridae family. This family also includes other well-known respiratory viruses such as the measles virus, mumps virus, and respiratory syncytial virus (RSV). HMPV, however, is genetically distinct from these other pathogens and has its own set of characteristics.
The virus primarily infects the upper and lower respiratory tract and is a leading cause of respiratory infections in infants and young children. However, adults, particularly those with weakened immune systems or underlying chronic conditions, can also be affected. In fact, similar to other respiratory viruses, HMPV is known to circulate in seasonal patterns, with outbreaks often occurring in the fall and winter months, peaking around the same time as influenza and RSV infections.
Symptoms of HMPV Infection
Infection with HMPV can present with a range of symptoms, which may vary from mild to severe, depending on the individual’s age, immune status, and any underlying health conditions. In children, particularly those under five years of age, HMPV is one of the leading causes of respiratory illness, including bronchiolitis and pneumonia.
The symptoms of HMPV infection can include:
Upper Respiratory Symptoms:
Nasal congestion
Runny nose
Coughing
Sore throat
Lower Respiratory Symptoms:
Wheezing
Shortness of breath
Rapid breathing
Chest tightness
General Symptoms:
Fever
Fatigue
Headache
While most individuals recover from HMPV infections within a week or two, some may develop more severe respiratory complications. The elderly, infants, and those with weakened immune systems or preexisting lung diseases such as asthma or chronic obstructive pulmonary disease (COPD) are at greater risk for developing serious illness.
Transmission of HMPV
HMPV is transmitted primarily through respiratory droplets when an infected person coughs, sneezes, or talks. It can also spread through direct contact with contaminated surfaces or by touching the mouth, nose, or eyes after touching surfaces that have been exposed to the virus.
Like other respiratory viruses, HMPV is highly contagious, and outbreaks are common, particularly in settings where close contact occurs, such as schools, daycares, hospitals, and nursing homes. The virus can remain viable on surfaces for several hours, making hand hygiene and disinfecting surfaces critical in preventing transmission.
Who is at Risk?
While HMPV can infect individuals of all ages, certain groups are at higher risk for severe illness or complications. These groups include:
Infants and Young Children: Infants, particularly those under one year of age, are more susceptible to severe respiratory symptoms, including bronchiolitis and pneumonia. In fact, HMPV is one of the leading causes of hospitalization in young children for respiratory illnesses.
Elderly Adults: Older adults, especially those with underlying health conditions such as COPD, asthma, or heart disease, are more likely to experience severe symptoms of HMPV infection.
Immunocompromised Individuals: Those with weakened immune systems, including individuals undergoing cancer treatments or those with conditions like HIV/AIDS, are at increased risk of more severe disease.
People with Chronic Respiratory Conditions: Patients with pre-existing respiratory conditions are also more likely to experience complications, including exacerbations of asthma or COPD.
Diagnosis of HMPV Infection
Diagnosing HMPV infection involves assessing clinical symptoms and performing laboratory tests. Given that HMPV shares symptoms with other respiratory infections like the flu, RSV, and the common cold, a detailed medical history and clinical examination are essential for diagnosis.
Laboratory tests that may be used to confirm HMPV include:
Polymerase Chain Reaction (PCR): This test detects the virus's genetic material in respiratory samples, such as a nasal swab, throat swab, or sputum.
Immunofluorescence: This method identifies HMPV proteins in respiratory secretions.
Viral Culture: Although less commonly used due to the time it takes, this test grows the virus from a sample to confirm the presence of HMPV.
In some cases, chest X-rays or other imaging techniques may be used to assess the extent of lung involvement, particularly if pneumonia or bronchiolitis is suspected.
Treatment of HMPV
Currently, there is no specific antiviral treatment for HMPV infection. Management is primarily supportive and focuses on alleviating symptoms. In most cases, individuals with mild illness recover with rest, hydration, and over-the-counter medications to reduce fever and ease discomfort.
For more severe cases, especially in young children or high-risk adults, hospitalization may be necessary. Treatment options for hospitalized patients may include:
Oxygen therapy to help maintain adequate oxygen levels in the blood.
Nebulized treatments to relieve wheezing or improve airflow in the lungs.
Intravenous (IV) fluids to prevent dehydration, especially if the individual is unable to drink enough fluids.
Mechanical ventilation in extreme cases, where patients have difficulty breathing on their own.
Antibiotics are not effective against viral infections like HMPV, so they are not used unless there is a secondary bacterial infection.
Prevention of HMPV
Because there is no vaccine for HMPV, prevention relies on reducing the risk of exposure and minimizing transmission. Strategies to prevent HMPV infection include:
Good Hygiene Practices:
Frequent handwashing with soap and water for at least 20 seconds, particularly after coughing or sneezing.
Using alcohol-based hand sanitizers when soap and water are not available.
Avoiding touching the face, especially the eyes, nose, and mouth.
Respiratory Hygiene:
Covering the mouth and nose with a tissue or elbow when coughing or sneezing.
Disposing of tissues immediately and washing hands afterward.
Avoiding Close Contact with Sick Individuals:
Avoiding contact with individuals who are showing symptoms of a respiratory illness, particularly in high-risk settings such as hospitals or daycare centers.
Disinfecting Surfaces:
Regularly cleaning and disinfecting frequently touched surfaces, such as doorknobs, light switches, and toys in childcare settings.
Conclusion
Human Metapneumovirus (HMPV) is an important respiratory virus that can cause a range of respiratory illnesses, particularly in children, the elderly, and individuals with weakened immune systems. While there is no specific antiviral treatment or vaccine available for HMPV, supportive care is effective for most patients. Prevention measures, including good hygiene, respiratory hygiene, and minimizing contact with infected individuals, remain the most effective means of reducing the spread of HMPV. As more research is conducted into the virus, we may gain a better understanding of its behavior and develop better diagnostic, therapeutic, and preventive strategies to manage its impact on global health.
#Human Metapneumovirus#HMPV infection#Respiratory illness#Respiratory virus#Pneumonia#asthma#health issues#Cold-like symptoms#Viral respiratory disease#RNA virus#Viral load#Diagnosis of HMPV#HMPV treatment#Preventing HMPV spread#Vaccine research#HMPV epidemiology#HMPV symptoms#HMPV mutations and variants#Virus incubation period
0 notes
Text
"Human Metapneumovirus (HMPV) Detection – Get Tested with Agilus Diagnostics"

Experiencing fever, cough, or shortness of breath? Get tested for Human Metapneumovirus (HMPV) with RT-PCR at Agilus Diagnostics. Free home collection available!
Are you experiencing flu-like symptoms that just won’t go away? It could be Human Metapneumovirus (HMPV) – a respiratory virus that causes fever, cough, sore throat, and difficulty breathing. Early detection is crucial, especially for children, older adults, and people with weak immune systems.
🔬 Symptoms to Watch For:
✅ 🤧 Runny nose ✅ 🤒 Fever ✅ 🤕 Sore throat ✅ 😷 Persistent cough ✅ 🫁 Shortness of breath ✅ 🔴 Rash on skin
If you notice these symptoms, it’s important to get tested as soon as possible to prevent complications.
🧪 Recommended Test:
🔍 Human Metapneumovirus (HMPV) Detection by RT-PCR 📋 Accurate & Reliable Results – Detect the virus with precision. 👨⚕️ Doctor Consultation Recommended – Seek medical advice for proper care.
🏠 Free Home Collection Available!
Avoid the hassle of visiting a lab—book your test from home and let our healthcare professionals collect your sample safely.
📞 Call Us Now: +91 98715 34054 / +91 97173 93002
📍 Visit Our Google Business Profile: https://maps.app.goo.gl/bRxSBgK5wmBuweN86
📍 Our Location: B-154/3 near Hanuman Mandir, Vasant Kunj Enclave, New Delhi - 110070
Take charge of your health today. Book your HMPV test with Agilus Diagnostics!
Keywords:
Human Metapneumovirus test, HMPV RT-PCR test, respiratory virus test, flu-like symptoms test, fever and cough test, home collection blood test, Agilus Diagnostics, viral infection testing, respiratory infection screening, shortness of breath test, Delhi home testing, health checkup in Delhi.
#Human Metapneumovirus test#HMPV RT-PCR test#respiratory virus test#flu-like symptoms test#fever and cough test#home collection blood test#Agilus Diagnostics#viral infection testing#respiratory infection screening#shortness of breath test#Delhi home testing#health checkup in Delhi.
0 notes
Text
Understanding the HMPV Outbreak in China: Cases, Research, and Public Health Response
The outbreak of human metapneumovirus (HMPV) in China is unfolding. Health authorities watch the situation closely. Researchers are also observing developments. HMPV is not a new virus. Still, it has garnered significant attention due to its recent surge
The outbreak of human metapneumovirus (HMPV) in China is unfolding. Health authorities watch the situation closely. Researchers are also observing developments. HMPV is not a new virus. Still, it has garnered significant attention due to its recent surge in cases. This surge particularly affects children and vulnerable populations. Here, we explore notable cases, research findings, and the…
#COVID-19 comparison#epidemiology of HMPV#healthcare system#HMPV#HMPVoutbreak#humanmetapneumovirus#news#respiratory infections#respiratory virus China#ublic health response#winter respiratory illnesses
0 notes
Text

Human metapneumovirus (HMPV) in the Philippines (Jan. 1 to Dec. 21, 2024)
HMPV is tested as part of Panel 2 (expanded panel) for specimens that test negative on Panel 1 (for Influenza, SARS-CoV-2, and RSV). This testing is conducted as part of the Influenza-Like Illness (ILI) and Severe Acute Respiratory Illness (SARI) surveillance programs: DOH
Top 6 causative agents of Influenza Like illness (ILI) (respiratory symptoms: cough, colds, and fever) from 4,921 positive samples):
Rhinovirus (1,257 or 25.5%)
Enterovirus (1,140 or 23.2%)
Influenza A (1,072 or 21.8%)
RSV (560 or 11.4%)
Adenovirus (527 or 10.7%)
HMPV (284 or 5.8%)
#human metapneumovirus#hmpv virus#HMPV in Philippines#respiratory infections#respiratory illness#Influenza Like illness#cough#cold sneezes#fever#respiratory viruses#rhinovirus#enterovirus#RSV#adenovirus#hmpv#influenza a#Influenzaa
0 notes
Text
#Human Metapneumovirus (HMPV)#HMPV Symptoms#Metapneumovirus Infection#Respiratory Virus#HMPV Causes#HMPV Transmission#HMPV Treatment#HMPV Diagnosis#Respiratory Illness in Children#Seasonal Respiratory Viruses#HMPV in Adults#Bronchiolitis and HMPV#HMPV vs. RSV#Upper Respiratory Infections#Lower Respiratory Tract Infection#HMPV Pneumonia#HMPV in Infants#HMPV Risk Factors#HMPV in Older Adults#HMPV Complications#HMPV Treatment Options#Antiviral Medications for HMPV#Supportive Care for HMPV#HMPV Prevention#Vaccines for HMPV#HMPV Testing#HMPV in Immunocompromised Individuals#HMPV Pathogenesis#HMPV Epidemiology#HMPV and COVID-19 Coinfection
1 note
·
View note
Text

O HMPV foi descoberto em 2001 e está associado a aproximadamente 20.000 hospitalizações entre crianças menores de 5 anos nos EUA a cada ano. 🦠
#hmpv#virus#hmpv virus#disease#infection#flu#gripe#infeccao#doenca#saude#health#public health#saude publica#metapneumovirus#human metapneumovirus#metapneumovirus humano#epidemic#epdemia
0 notes
Text
चीन से निकल कर ब्रिटेन, अमेरिका समेत इन छह देशों में पहुंचा HMPV वायरस संक्रमण, जानें कैसे करें बचाव
HMPV Virus News: चीन में HMPV वायरस बहुत तेजी से फैल रहा है. इसके बढ़ते प्रकोप को देखते हुए चीन के कई राज्यों में इमरजेंसी घोषित कर दिया गया है. इस वायरस को कोरोना से ज्यादा खतरनाक बताया जा रहा है. चीन के कई इलाकों में हालात बिगड़ गए हैं. एक बार फिर मास्क वाला दौर फिर लौट आया है. हजारों लोग वायरस की चपेट में हैं. बुजुर्गों ��र बच्चों में तेजी से संक्रमण फैल रहा है. अस्पतालों के बाहर मरीजों की…
0 notes
Text
HMPV Virus : नवीन संकट की अफवा?
HMPV Virus : आजच्या घडीला चीनमध्ये ह्यूमन मेटा न्यूमोव्हायरस (एचएमपीव्ही) विषाणूच्या संभाव्य प्रादुर्भावामुळे जगभरात चिंता पसरली आहे. कोविड-19 महामारीच्या आठवणी अजूनही ताज्या असताना, या नव्या विषाणूबाबत जागतिक आरोग्य समुदाय सज्ज झाला आहे. चला या व्हायरसची माहिती, त्याचे परिणाम आणि प्रतिबंधात्मक उपाय यावर सविस्तर चर्चा करू.
#agriculture#breaking news#good omens#marathi#naruto#news#HMPV Virus#Human Metapneumovirus#Respiratory Virus#Viral Infection#Flu-like Symptoms#Bronchitis#Pneumonia#Virus Prevention#Airborne Disease#Virus Transmission#Pandemic Alert#Health Awareness#Viral Outbreak#Respiratory Illness#Winter Virus#Child Health#Vulnerable Groups#No Vaccine#Virus Precautions#China Health Crisis#Virus Similar to COVID-19
0 notes
Text
Understanding Pneumonia in a Post-COVID World
Pneumonia is more than just a chest infection; it’s a potential sign of deeper immune vulnerabilities. Whether it follows a bout of flu, a cold, or COVID-19, it often results from a combination of viral and bacterial factors. The initial viral infection weakens the lungs, making them susceptible to bacterial overgrowth.
In von der Leyen’s case, the timing, just after the holiday season, it raises questions about recent exposure to viruses, possibly including COVID-19. The Christmas period, with its gatherings and travel, often acts as a super-spreader event, creating fertile ground for respiratory illnesses.
The COVID-19 Connection
COVID-19 isn’t just another respiratory virus. Its unique ability to impair immune responses is what sets it apart. By targeting key immune cells like T-cells, B-cells, and natural killer cells, it leaves the body more vulnerable to subsequent infections. This is particularly dangerous in winter, when co-circulating viruses like influenza and HMPV (human metapneumovirus) are already taxing the immune system.
Even mild cases of COVID-19 can have profound impacts beneath the surface, disabling parts of the immune system and opening the door to secondary infections. This “immune freeze” effect, where cells are present but unable to function effectively, may explain why so many people experience lingering illnesses or complications weeks after their initial infection.
3 notes
·
View notes
Text
"HMPV is not like Covid-19, in that it has been around for several decades and there is a level of immunity in the global population from past infections, the experts said. Covid-19 was a new disease which had never infected humans before, driving the pandemic-level spread. 'I don’t think we’re necessarily concerned about a pandemic with this virus, but the surge in cases and impact it’s having are significant,' said Griffin. 'A good lesson can be taken [from the pandemic] to reduce the spread, particularly given we don’t have vaccines or antivirals for HMPV.'”
4 notes
·
View notes
Text
7News spreading misinformation about HMPV
[Transcript: Health officials are raising the alarm over a new virus outbreak in China, which has sparked comparisons to COVID-19. It's a type of respiratory infection which is surging across the country, particularly alarming for young children, the elderly, and vulnerable individuals. And currently there's no antiviral treatment or vaccine available, but remedies, which we're told are under development].
"new virus outbreak in China"
False. This is not a new virus. Scientists have known about this virus since 2001, but research shows that it's been around since the 1950's. Scientists don't know where this virus originated. It was identified in humans for the first time in the Netherlands, and was identified in birds in 1978 in South Africa. However, both times it was almost immediately investigated in other countries and discovered to have already infected their populations. We don't know whether or not it originated in China, and that shouldn't matter. Chinese people aren't inherently dirty, and this is not something that was bioengineered in a lab. Disease is natural. I really don't like the fearmongering and misinformation that has happened in the first line alone.
"surging across the country"
True, but it surges every single year during winter. It's a seasonal outbreak, just like the flu. In Norway, it is estimated that there is almost no one over 5 that hasn't contracted HMPV in their lifetime. According to the World Health Organisation, the rise in recorded HMPV cases hasn't put any strain on hospitals in China. It is being handled as it has always been handled everywhere.
Final thoughts
If you have a degree in journalism, you learn how to skew people's views, cause fear, etc for people who either lack media literacy or are highly reactive. This wasn't worded this way by accident. It is my belief that this was intentional. Acting like there's another "new Chinese virus" it stirs back up all the conspiracy theories that the Chinese government is out here bioengineering diseases, or pushing the stereotype that as a race, we are unclean, and mistakenly spread disease because of "lack of hygiene" or weird eating habits. Both narratives are (ironically) pushed at the same time, as we saw for ourselves during COVID-19. Anti-Chinese propaganda is being generated again (or perhaps it never stopped).
Please look at the news critically, everyone. Have a good day.
Sources under the cut:
#auspol#hmpv#hmpv virus#hmpv symptoms#stop asian hate#stop aapi hate#racism tw#sinophobia tw#disease tw#sinophobia#racism#7news#australian politics#australia#activism#political#cal speaks
2 notes
·
View notes
Text
2 notes
·
View notes
Text
"Human Metapneumovirus (HMPV) Detection – Get Tested with Agilus Diagnostics"
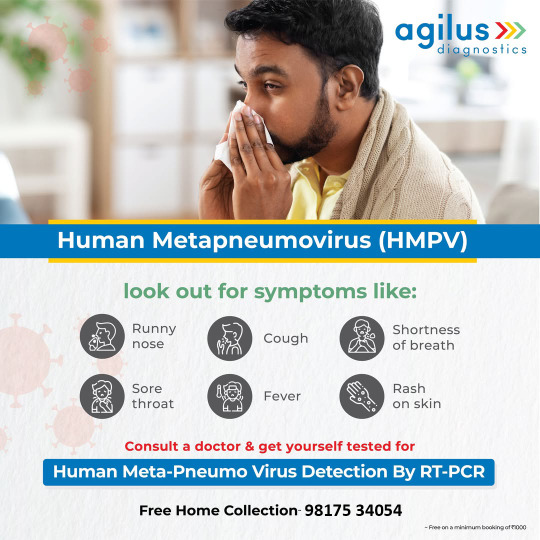
Experiencing fever, cough, or shortness of breath? Get tested for Human Metapneumovirus (HMPV) with RT-PCR at Agilus Diagnostics. Free home collection available!
Are you experiencing flu-like symptoms that just won’t go away? It could be Human Metapneumovirus (HMPV) – a respiratory virus that causes fever, cough, sore throat, and difficulty breathing. Early detection is crucial, especially for children, older adults, and people with weak immune systems.
🔬 Symptoms to Watch For:
✅ 🤧 Runny nose ✅ 🤒 Fever ✅ 🤕 Sore throat ✅ 😷 Persistent cough ✅ 🫁 Shortness of breath ✅ 🔴 Rash on skin
If you notice these symptoms, it’s important to get tested as soon as possible to prevent complications.
🧪 Recommended Test:
🔍 Human Metapneumovirus (HMPV) Detection by RT-PCR 📋 Accurate & Reliable Results – Detect the virus with precision. 👨⚕️ Doctor Consultation Recommended – Seek medical advice for proper care.
🏠 Free Home Collection Available!
Avoid the hassle of visiting a lab—book your test from home and let our healthcare professionals collect your sample safely.
📞 Call Us Now: +91 98715 34054 / +91 97173 93002
📍 Visit Our Google Business Profile: https://maps.app.goo.gl/bRxSBgK5wmBuweN86
📍 Our Location: B-154/3 near Hanuman Mandir, Vasant Kunj Enclave, New Delhi - 110070
Take charge of your health today. Book your HMPV test with Agilus Diagnostics!
Human Metapneumovirus test, HMPV RT-PCR test, respiratory virus test, flu-like symptoms test, fever and cough test, home collection blood test, Agilus Diagnostics, viral infection testing, respiratory infection screening, shortness of breath test, Delhi home testing, health checkup in Delhi.
#Human Metapneumovirus test#HMPV RT-PCR test#respiratory virus test#flu-like symptoms test#fever and cough test#home collection blood test#Agilus Diagnostics#viral infection testing#respiratory infection screening#shortness of breath test#Delhi home testing#health checkup in Delhi.
0 notes
Text
Human metapneumovirus (HMPV) is a respiratory disease that causes flu or cold-like symptoms, but can increase risks or lead to more serious complications like bronchitis or pneumonia, particularly among the elderly, young children, and immunocompromised people.
The disease is in the same family as respiratory syncytial virus (RSV), and has been around since at least 2001 when it was first identified in the Netherlands. Its outbreaks are concentrated during colder seasons.
Why is HMPV in the news?
Cases have been surging in northern China, particularly among children, according to local authorities. The country’s centre for disease control (CDC) has warned people to take precautions with health and hygiene, but has also pushed back against online claims of overwhelmed hospitals and fears of another Covid-like pandemic.
“Respiratory infections tend to peak during the winter season,” Chinese foreign ministry spokesperson Mao Ning said on Friday.
“The diseases appear to be less severe and spread with a smaller scale compared to the previous year.”
The apparent increase in cases is likely partly due to new technology more easily detecting and identifying HMPV, experts told the Guardian.
Also, “I think we’re just more cautious of outbreaks now”, said Dr Jacqueline Stephens, a senior lecturer in public health at Flinders University in Australia. “Everyone is hypervigilant, and you hear this term human metapneumovirus and it sounds kind of scary.”
How serious is HMPV and what are the symptoms?
The symptoms of HMPV are similar to a cold or flu, and it is one of several viruses often lumped under a broad definition of the “common cold”, said Stephens. It is not a notifiable disease like Covid-19 or influenza.
“There’s a range of others … that are not notifiable because they are very common and lots of people get them. They make us feel terrible for a few days but if we rest and recuperate for a few days then we get better,” said Stephens.
Who is most at risk from human metapneumovirus?
HMPV can lead to more serious illnesses like bronchitis and pneumonia among elderly people, very young children, and people who are immunocompromised.
“It certainly can and does cause severe disease, that’s why I think it’s important that people know it’s out there,” said said Prof Paul Griffin, director of infectious diseases at Mater Health Services in Brisbane.
“The challenge is at the moment there’s not much we can do except educate people [that] it’s around to reduce transmission. There’s no vaccine or antivirals, although there are some vaccines in development,” said Griffin.
How worried should we be about the virus?
HMPV is not like Covid-19, in that it has been around for several decades and there is a level of immunity in the global population from past infections, the experts said. Covid-19 was a new disease which had never infected humans before, driving the pandemic-level spread.
“I don’t think we’re necessarily concerned about a pandemic with this virus, but the surge in cases and impact it’s having are significant,” said Griffin. “A good lesson can be taken [from the pandemic] to reduce the spread, particularly given we don’t have vaccines or antivirals for HMPV.”
What should we do about it?
“For a number of years [during Covid] we were good at precautions for reducing the numbers, now we are doing less, and we’re seeing a rebound,” said Griffin.
“I’m certainly not suggesting we go back to the harsh restrictions of Covid, but staying home, practising good cough and sneeze etiquette, and hand hygiene are so important during the winter season.”
Both experts also urged people not to go to work while sick, and Stephens suggested wearing a mask if you do have to go into the community, to prevent further infecting others, especially those at higher risk.
2 notes
·
View notes
Text








KEEP CALM !
Do Not Panic ! 😌
The World Health Organization (WHO) statement on the increasing trends of acute respiratory infections (ARI), including human metapneumovirus (HMPV) in the Northern Hemisphere, January 7, 2025.
#WashHands 👏 #MaskOn 😷 #hmpvvirus 🦠
https://www.who.int/emergencies/disease-outbreak-news/item/2025-DON550
#hmpv#human metapneumovirus#respiratory illness#respiratory diseases#respiratory infections#acute respiratory infections#northern hemisphere#world health organization#WHO#hmpv virus#wash hands#mask on
0 notes
Text

🚨 Virus Outbreak in China 🚨
China is currently facing a surge in respiratory infections, particularly Human Metapneumovirus (HMPV), affecting children under 14 in northern provinces. 🦠
📝 Key Updates:
HMPV Symptoms: Mild cold-like symptoms but can cause severe illness in vulnerable groups.
Overwhelmed Hospitals: Children's hospitals in provinces like Hunan are experiencing a sharp increase in patients with respiratory symptoms.
Government Response: A pilot system is monitoring pneumonia of unknown origin, aiming to prevent future pandemics.
While experts suggest the risk of another pandemic like COVID-19 is low, public concern is growing. There is no vaccine for HMPV yet, so prevention and symptom management are crucial.
⚠️ How to Stay Safe:
Practice good hygiene (wash hands regularly).
Avoid crowded places if possible.
Seek medical attention if severe respiratory symptoms occur.
Let’s stay informed and cautious. Share this to keep others updated!
#BeAGenius💯 #HealthAlert #StaySafe
2 notes
·
View notes