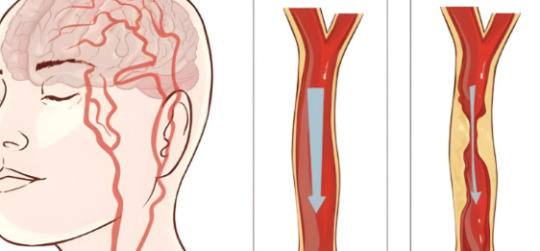
#Plaque in diseased carotid artery
Explore tagged Tumblr posts
Text

#Understanding Brain Stroke:#Plaque in diseased carotid artery#Blood clot (thrombus) breaks off#Blood clot in cerebral artery blocks blood flow#For expert care and consultation#contact Dr. Randeep Jadal (Neurologist) at Lotus Super Speciality Hospital. Call us 24/7 at 896 896 8878 or visit www.lotusneurocentre.in.
0 notes
Text
Some Cardiology Vocabulary

for your next poem/story
Ablation – Elimination or removal.
Annulus – The ring around a heart valve where the valve leaflet merges with the heart muscle.
Arrhythmia – (or dysrhythmia) An abnormal heartbeat.
Autologous – Relating to self. For example, autologous stem cells are those taken from the patient’s own body.
Bruit – A sound made in the blood vessels resulting from turbulence, perhaps because of a buildup of plaque or damage to the vessels.
Cardiac – Pertaining to the heart.
Cardiomegaly – An enlarged heart. It is usually a sign of an underlying problem, such as high blood pressure, heart valve problems, or cardiomyopathy.
Carotid artery – A major artery (right and left) in the neck supplying blood to the brain.
Claudication – A tiredness or pain in the arms and legs caused by an inadequate supply of oxygen to the muscles, usually due to narrowed arteries or peripheral arterial disease (PAD).
Commissurotomy -A procedure used to widen the opening of a heart valve that has been narrowed by scar tissue.
Digitalis – A medicine made from the leaves of the foxglove plant. Digitalis is used to treat congestive heart failure (CHF) and heart rhythm problems (arrhythmias).
Endocardium – The smooth membrane covering the inside of the heart. The innermost lining of the heart.
Infarct – The area of heart tissue permanently damaged by an inadequate supply of oxygen.
Jugular veins – The veins that carry blood back from the head to the heart.
Maze surgery – A type of heart surgery that is used to treat chronic atrial fibrillation by creating a surgical “maze” of new electrical pathways to let electrical impulses travel easily through the heart. Also called the Maze procedure.
Myocardium – The muscular wall of the heart. It contracts to pump blood out of the heart and then relaxes as the heart refills with returning blood.
Palpitation – An uncomfortable feeling within the chest caused by an irregular heartbeat.
Pericardium – The outer fibrous sac that surrounds the heart.
Regurgitation – Backward flow of blood through a defective heart valve.
Septal defect – A hole in the wall of the heart separating the atria or in the wall of the heart separating the ventricles.
Sources: 1 2 3 4 ⚜ More: Word Lists
#cardiology#terminology#word list#spilled ink#writing reference#dark academia#writeblr#studyblr#langblr#linguistics#literature#creative writing#writing inspiration#writing inspo#writing ideas#writers on tumblr#writing prompt#poetry#poets on tumblr#writing resources
81 notes
·
View notes
Text
Best Center for Vascular Surgery: Advanced Care for Healthy Blood Circulation
Vascular health is crucial for overall well-being, as it involves the circulatory system responsible for transporting blood throughout the body. Conditions affecting veins and arteries can lead to severe complications if left untreated. For those seeking expert vascular care, choosing the best center for vascular surgery ensures timely diagnosis and advanced treatment.
Preethi Hospitals, Madurai, is a leading name in vascular care, offering cutting-edge surgical solutions for various vascular disorders. With state-of-the-art infrastructure and ` patient-centric care, it has emerged as a trusted center for vascular surgery.
Understanding Vascular Surgery and Its Importance
Vascular surgery focuses on treating diseases of the blood vessels, including arteries, veins, and lymphatic circulation. Conditions such as aneurysms, deep vein thrombosis (DVT), varicose veins, and peripheral artery disease (PAD) require specialized vascular interventions to prevent severe complications like strokes and limb amputations.
Timely diagnosis and surgical intervention can significantly improve quality of life by restoring proper blood flow and reducing risks associated with vascular diseases.
Why Choose a Specialized Vascular Surgery Center?
When dealing with vascular diseases, selecting a specialized center is crucial. The best center for vascular surgery provides:
Advanced Diagnostic Facilities: Cutting-edge imaging technology like Doppler ultrasound, CT angiography, and MRI scans for precise assessment.
Minimally Invasive Techniques: Procedures such as endovascular surgery and laser treatment reduce recovery time and post-operative discomfort.
Comprehensive Vascular Care: Treatment for a wide range of vascular conditions, from common issues like varicose veins to complex arterial diseases.
Post-Surgical Rehabilitation: Ensuring complete recovery and preventive measures for future vascular health.
Advanced Vascular Surgery Services at Preethi Hospitals, Madurai
Preethi Hospitals, Madurai, stands out as a premier center for vascular surgery due to its commitment to providing cutting-edge treatments. Here are some of the key vascular procedures available:
Endovascular Surgery
Endovascular surgery is a minimally invasive procedure used to treat aneurysms and arterial blockages. This technique involves using catheters and stents to restore blood flow without the need for open surgery. Patients benefit from faster recovery and reduced hospital stays.
Varicose Vein Treatments
Varicose veins are enlarged, twisted veins that often cause pain and discomfort. At Preethi Hospitals, treatments such as laser therapy, sclerotherapy, and radiofrequency ablation effectively remove varicose veins with minimal scarring and downtime.
Peripheral Artery Disease (PAD) Treatment
PAD is a serious condition where arteries narrow due to plaque buildup, reducing blood flow to the limbs. Advanced interventions like angioplasty and bypass surgery at Preethi Hospitals help restore circulation and prevent limb loss.
Carotid Artery Surgery
The carotid arteries supply blood to the brain, and blockages can lead to strokes. Carotid endarterectomy and stenting are performed to clear blockages and reduce stroke risk.
Dialysis Access Surgery
For patients undergoing dialysis, creating a reliable vascular access is essential. Procedures like arteriovenous (AV) fistula and graft placement ensure efficient dialysis treatment.
Deep Vein Thrombosis (DVT) Management
DVT is a serious condition where blood clots form in deep veins, leading to potential complications like pulmonary embolism. Advanced therapies, including catheter-directed thrombolysis, are available at Preethi Hospitals.
Benefits of Choosing Preethi Hospitals for Vascular Surgery
Preethi Hospitals, Madurai, is renowned for its commitment to excellence in vascular surgery. Key advantages include:
State-of-the-Art Facilities: Equipped with advanced operation theaters and diagnostic tools for precise treatment.
Expert Surgical Team: A dedicated team of vascular specialists ensuring comprehensive care.
Personalized Treatment Plans: Customized solutions based on patient-specific needs.
Affordable and Accessible Care: Quality vascular surgery services at competitive costs.
Signs You May Need Vascular Surgery
If you experience any of the following symptoms, seeking vascular consultation is crucial:
Persistent leg pain or cramping, especially while walking
Swelling, redness, or warmth in the legs (possible DVT signs)
Non-healing ulcers or sores on the legs or feet
Numbness, weakness, or cold sensations in the limbs
Bulging, twisted veins with pain or discomfort
Sudden loss of vision or difficulty speaking (potential carotid artery blockage)
Preventing Vascular Diseases: Lifestyle Tips
While medical interventions are available, prevention is always better than cure. Here are some ways to maintain vascular health:
Regular Exercise: Improves circulation and prevents arterial blockages.
Healthy Diet: Avoid processed foods, consume more fiber, and include heart-friendly fats.
Quit Smoking: Smoking damages blood vessels and increases the risk of vascular diseases.
Manage Blood Pressure & Cholesterol: Regular check-ups can help control these risk factors.
Stay Hydrated: Proper hydration supports healthy blood flow and prevents clot formation.
Conclusion
For those searching for the best center for vascular surgery, Preethi Hospitals, Madurai, stands as a trusted institution offering world-class vascular care. With advanced technology, skilled surgeons, and a patient-first approach, it ensures effective treatment and recovery for various vascular conditions.
If you or a loved one is facing vascular health concerns, timely medical intervention can prevent complications and improve overall well-being. Consult with Preethi Hospitals, Madurai, to receive expert care and regain healthy circulation.

0 notes
Text
When To Seek Help: Signs You May Need A Vascular Treatment

The vascular system, often referred to as the circulatory system, plays a crucial role in maintaining the health and functionality of your body. This intricate network of arteries, veins, and capillaries ensures that oxygenated blood reaches every part of your body while carrying away waste products. Given its importance, even minor disruptions in the vascular system can lead to significant health complications. But how do you know when to seek professional help for vascular issues? This blog will explore the key signs that indicate you may need vascular treatment, helping you make informed decisions about your health.
Understanding Vascular Health
Before delving into the warning signs, it's essential to understand the basics of vascular health. A healthy vascular system supports proper blood circulation, which is fundamental for delivering nutrients and oxygen to tissues and organs. Over time, factors like aging, lifestyle choices, and genetic predispositions can negatively impact vascular health, leading to conditions such as:
Peripheral Artery Disease (PAD)
Deep Vein Thrombosis (DVT)
Varicose veins
Aneurysms
Carotid artery disease
These conditions can range from mild discomfort to life-threatening emergencies, highlighting the importance of timely intervention.
Key Signs You May Need Vascular Treatment
Recognizing the signs of vascular problems can help prevent severe complications. Below are the most common symptoms and conditions that warrant professional evaluation and potential treatment:
1. Persistent Leg Pain or Cramping
Leg pain, especially during physical activity, could be a sign of Peripheral Artery Disease (PAD). This condition occurs when narrowed arteries reduce blood flow to the limbs. The pain, often described as cramping or aching, typically subsides with rest but may return upon exertion.
2. Swelling in the Legs
Swelling in one or both legs can indicate venous insufficiency or Deep Vein Thrombosis (DVT). DVT is particularly concerning as it involves a blood clot that can travel to the lungs, causing a potentially fatal pulmonary embolism. Chronic swelling should always be evaluated by a healthcare provider.
3. Non-healing Wounds or Ulcers
Slow-healing or non-healing wounds, particularly on the legs or feet, could signal poor blood circulation due to PAD or diabetes-related vascular issues. These wounds are often accompanied by discoloration, pain, or infection and require prompt medical attention.
4. Visible Varicose Veins
Varicose veins are twisted, enlarged veins visible just under the surface of the skin. While they may seem primarily cosmetic, they can also cause discomfort, heaviness, or throbbing in the legs. Severe cases may require treatment to prevent complications like blood clots or ulcers.
5. Sudden Numbness or Weakness
Sudden numbness, weakness, or difficulty speaking could be signs of a transient ischemic attack (TIA) or stroke. These conditions are often linked to carotid artery disease, where plaque buildup restricts blood flow to the brain. Immediate medical intervention is critical.
6. Cold or Discolored Extremities
Experiencing cold, pale, or bluish fingers or toes may indicate poor blood flow due to arterial blockages. This symptom can also be associated with conditions like Raynaud's phenomenon or advanced PAD.
7. Family History of Vascular Disease
A family history of vascular conditions, such as aneurysms or blood clots, increases your risk. Regular check-ups and screenings are crucial if you have a genetic predisposition to vascular issues.
When to Seek Medical Attention
It’s essential to consult a healthcare provider if you experience any of the symptoms mentioned above. While some conditions may initially appear mild, they can quickly escalate if left untreated. Delarra Clinic specializes in diagnosing and treating vascular conditions, offering a range of advanced diagnostic tools such as Doppler ultrasound, CT angiography, and vascular lab tests.
Types of Vascular Treatments
Modern vascular treatments are highly advanced and minimally invasive, making recovery faster and more comfortable. Some common treatment options include:
1. Lifestyle Modifications
For mild vascular issues, doctors may recommend lifestyle changes such as:
Quitting smoking
Regular exercise
Healthy eating
Weight management
2. Medications
Medications can manage symptoms and reduce risks, including:
Blood thinners to prevent clots
Cholesterol-lowering drugs
Pain relievers for symptomatic relief
3. Minimally Invasive Procedures
Technological advancements have made treatments less invasive, such as:
Endovascular stent placement
Angioplasty
Laser treatments for varicose veins
4. Surgical Options
In severe cases, surgery may be necessary, including:
Bypass surgery to restore blood flow
Carotid endarterectomy to remove plaque
Aneurysm repair
Conclusion
Vascular health is fundamental to your overall well-being. Ignoring early warning signs can lead to severe complications, making it crucial to recognize and address symptoms promptly. Whether it’s persistent leg pain, swelling, or visible varicose veins, consulting a specialist can provide clarity and treatment options.
At Delarra Clinic, expert vascular care is within your reach. Don’t wait for symptoms to worsen—take proactive steps to ensure your circulatory health. Remember, early detection and timely treatment are the keys to maintaining a healthy vascular system and enhancing your quality of life.
Also, Read: 10 types of facial treatments that will restore your glow
0 notes
Text
Carotid Angioplasty and Stenting in India
Carotid Angioplasty and Stenting
India: A stroke prevention strategy — Carotid Angioplasty and Stenting (CAS)
What is carotid artery diseaseThis disease is characterized by fattening of the arteries supplying blood to the brain. This can cause blood flow to become blocked, raising the chances of stroke. What is Carotid Angioplasty and Stenting (CAS)? Carotid Angioplasty and Stenting (CAS) is a minimally invasive procedure to open narrowed or blocked arteries of the neck, which supply blood to the brain.
Why Choose India for CAS?
India is the latest global hub for health–care with particular focus to heart care. There is a number of reasons for its increasing popularity as CAS:
Expert Hands with Innovative Technology: India has top-notch Interventional Cardiologists, along with High-Quality Medical Facilities.
Affordable Treatment: The cost of CAS in India is approximately 30% lower than in most Western countries, ensuring no compromise on quality.
Less Invasive Techniques: As CAS is a less invasive procedure, fewer hospital stays and shorter recovery times are commonly experienced.
Top-Notch Patient Care: The Indian hospitals are known for their passion toward the healthcare services.
The CAS Procedure
The CAS procedure involves:
Anesthesia: Local anesthesia is given to numb the groin area.
Insertion of Catheter: Insertion of a small, thin, flexible tube called catheter into a blood vessel in the groin.
In Balloon Angioplasty, the catheter is advanced to the constricted carotid artery where a balloon is inflated to crush the plaque.
Stenting: A tiny, mesh tube called a stent is implanted to hold open the artery.
Recovery and Aftercare
CAS does not take long to heal from. Most patients go home one to two days after surgery. Patients will have to refrain from vigorous movements for several weeks after the operation. Periodic visits to a cardiologist are necessary to monitor a stent and general health.
0 notes
Link
0 notes
Text
Carotid Artery Stenosis Treatment Cost in India: Complete Guide
Carotid Artery Stenosis (CAS) is a critical condition where the carotid arteries, which supply blood to the brain, become narrowed due to plaque buildup. This narrowing can increase the risk of stroke, making early detection and treatment vital. If you or a loved one is diagnosed with Carotid Artery Stenosis, you may have several questions, especially regarding the carotid artery stenosis treatment cost in India. Understanding the treatment options, associated costs, and the advantages of seeking treatment in India can help you make informed decisions.

India has become a preferred destination for carotid artery blockage treatment, offering advanced medical care at competitive prices. With renowned specialists such as Dr. Sumit Kapadia leading the field, India is known for providing high-quality healthcare at a fraction of the cost compared to Western countries.
In this comprehensive guide, we will delve into the treatment options available for Carotid Artery Disease, the carotid artery stenosis symptoms, and the cost of treatment. We’ll also explore the reasons why India is considered a top choice for treatment and the role of a vein specialist doctor near me in managing the condition effectively.
Overview of Treatment Options
The treatment for carotid artery stenosis typically depends on the severity of the condition and the presence of symptoms. In most cases, treatment aims to prevent a stroke by improving blood flow through the carotid arteries. The key treatments include:
Lifestyle Changes and Medication For those with mild carotid artery stenosis or early-stage carotid artery blockage, the doctor may recommend lifestyle changes, such as adopting a heart-healthy diet, exercising regularly, and quitting smoking. Medications may also be prescribed to reduce cholesterol, prevent blood clots, and control blood pressure.
Carotid Angioplasty and Stenting In more advanced cases, where there is significant narrowing of the artery, a procedure known as carotid angioplasty may be necessary. This minimally invasive procedure involves inserting a stent into the blocked carotid artery to help keep it open and restore normal blood flow. This treatment is especially beneficial for patients who cannot undergo surgery due to medical reasons.
Carotid Endarterectomy For severe carotid artery blockage, carotid endarterectomy is the gold standard treatment. It involves surgically removing the plaque from the artery, allowing blood to flow freely again. This procedure is typically recommended when the blockage is greater than 70% and is associated with a high risk of stroke.
Carotid Artery Bypass Surgery In rare cases, a carotid artery bypass surgery may be necessary. This procedure is used to reroute blood flow around a severely blocked or narrowed carotid artery. It’s typically considered when other treatments are not effective or feasible.
Carotid Doppler Test Before any treatment, a carotid Doppler test is often performed to assess the degree of carotid artery stenosis. This non-invasive test uses sound waves to create an image of the blood flow in the carotid arteries, helping doctors determine the severity of the blockage and decide on the appropriate treatment.
Cost of Carotid Artery Stenosis Treatment in India
One of the primary reasons why many individuals opt for carotid artery stenosis treatment in India is the cost-effectiveness of healthcare services. India offers world-class medical care at a fraction of the cost compared to countries like the US, the UK, and others. The carotid artery stenosis treatment cost in India is generally lower due to factors such as lower labour costs, affordable medical infrastructure, and competitive pricing strategies by hospitals.
While the cost of carotid artery blockage treatment varies depending on the type of treatment required, here is an estimated breakdown of the costs associated with different procedures:
Consultation with a Vein Specialist Doctor Consultation with an expert like a vein specialist doctor near me typically costs around ₹1,000 to ₹3,000 in India. The cost may vary based on the location of the clinic and the doctor's experience.
Carotid Doppler Test The carotid Doppler test cost in India is typically between ₹2,000 and ₹5,000. This test is crucial for diagnosing carotid artery stenosis and determining the appropriate course of action for treatment.
Carotid Angioplasty and Stenting The cost of carotid angioplasty and stenting in India is relatively affordable compared to Western countries. The price range for this procedure is approximately ₹1,00,000 to ₹2,50,000. This cost includes the procedure, stent insertion, and hospital stay.
Carotid Endarterectomy Carotid endarterectomy, the most common surgery for carotid artery blockage, typically costs between ₹1,50,000 to ₹3,50,000 in India. The cost may increase if the surgery involves complications or a longer hospital stay.
Carotid Artery Bypass Surgery In cases where carotid artery bypass surgery is needed, the cost may range from ₹2,00,000 to ₹5,00,000. This surgery is more complex and involves a longer recovery time, so the cost reflects the more extensive nature of the procedure.
Follow-up Care and Medication After the treatment, follow-up visits and medication are necessary to ensure the success of the procedure and prevent complications. These costs can vary, but on average, patients may need to budget around ₹10,000 to ₹20,000 per year for medication and follow-up care.
While these costs may seem high, they are significantly lower than what you would pay for similar procedures in the US or the UK, where the cost can be upwards of ₹10,00,000 for carotid artery stenosis treatment.
Why Choose India for Carotid Artery Stenosis Treatment?
India has gained recognition as a top destination for medical tourism due to its world-class healthcare facilities, experienced doctors, and cost-effective treatment options. Here are some reasons why you should consider India for carotid artery stenosis treatment:
High-Quality Healthcare India boasts state-of-the-art medical facilities equipped with the latest technology for the diagnosis and treatment of Carotid Artery Disease. Hospitals like Apollo, Fortis, and Kokilaben Dhirubhai Ambani Hospital are internationally recognised for their excellence in cardiology and vascular treatments. These hospitals are accredited by international bodies like the Joint Commission International (JCI) and National Accreditation Board for Hospitals (NABH), ensuring the highest quality of care.
Experienced Specialists India is home to some of the world’s most renowned carotid artery stenosis specialists. Doctors such as Dr. Sumit Kapadia, who specialise in Carotid Artery Disease, have years of experience in performing delicate surgeries like carotid endarterectomy and carotid angioplasty. Their expertise and track record of successful surgeries attract patients from around the world.
Affordable Treatment Options The cost of treatment in India is a fraction of what you would pay in developed countries. Whether it's carotid artery blockage treatment or a carotid artery Doppler test, you can expect to save up to 60-70% on medical bills. This affordability, combined with the high standard of care, makes India an attractive destination for those seeking treatment for Carotid Artery Disease.
Comprehensive Care Packages Many Indian hospitals offer comprehensive care packages that cover everything from diagnostic tests to surgery and follow-up care. These packages are designed to make the treatment process smooth, reducing the overall cost and providing a transparent pricing structure.
Shorter Waiting Times Unlike many Western countries where long waiting times for surgeries are common, India offers quick access to treatment. Once you are diagnosed with carotid artery stenosis, you can expect to be treated promptly, allowing you to avoid the risk of complications like stroke.
Benefits of Treatment Under Dr. Sumit Kapadia
Dr. Sumit Kapadia is one of the leading vascular specialists in the region, known for his expertise in treating carotid artery stenosis and other vascular diseases. Choosing Dr. Kapadia for your treatment offers several benefits:
Extensive Experience With years of experience in diagnosing and treating Carotid Artery Disease, Dr. Kapadia has helped many patients regain their health and avoid stroke. His expertise in carotid artery blockage and related conditions ensures that you are in safe hands.
Advanced Treatment Options Dr. Kapadia stays at the forefront of medical advancements, offering the latest treatments and techniques for carotid artery stenosis. His use of minimally invasive procedures like carotid angioplasty ensures faster recovery times and fewer complications.
Personalised Care Dr. Kapadia takes a personalised approach to each patient, ensuring that the treatment plan is tailored to your specific needs. Whether you require carotid artery blockage treatment or a simpler procedure, he ensures that every step of the process is handled with the utmost care and attention.
Recovery and Post-Treatment Care
After undergoing treatment for carotid artery stenosis, it’s essential to follow a structured recovery plan. Recovery time varies depending on the type of treatment received:
Post-Surgery Care For those who have undergone carotid endarterectomy or carotid angioplasty, the hospital stay typically lasts for 2-4 days. After discharge, patients are advised to avoid strenuous activities for a few weeks. Regular follow-up visits are scheduled to monitor progress and ensure that the artery remains open.
Medications Patients may need to take medications such as blood thinners to prevent clot formation and control cholesterol levels. It’s essential to follow the doctor’s instructions regarding medication to ensure the success of the treatment.
Lifestyle Modifications Adopting a healthy lifestyle, including a balanced diet, regular exercise, and smoking cessation, is critical for long-term recovery and preventing recurrence of Carotid Artery Disease.
Conclusion
Carotid artery stenosis treatment in India offers a comprehensive solution at a fraction of the cost you would incur in other countries. The availability of world-class medical facilities, experienced specialists like Dr. Sumit Kapadia, and affordable treatment options make India an ideal destination for those seeking carotid artery blockage treatment. Whether it’s through carotid angioplasty, carotid endarterectomy, or the necessary pre-treatment diagnostic tests like the carotid Doppler test, you can expect top-notch care and successful outcomes. With the right treatment, the risks associated with Carotid Artery Disease can be managed effectively, ensuring a healthier future.
#carotid artery stenosis treatment cost#carotid artery blockage treatment#carotid artery blockage#carotid artery stenosis#carotid artery stenosis symptoms#Carotid Artery Disease#vein specialist doctor near me
0 notes
Text
Carotid artery surgery, often called a carotid endarterectomy, is a surgical procedure to remove plaque buildup within the carotid arteries. This plaque buildup, known as atherosclerosis, can narrow or block blood flow to the brain, which increases the risk of stroke. By carefully removing this blockage, the surgery improves blood flow and lowers the risk of future strokes. Vein centers in Tampa offer this procedure with skilled vascular surgeons who specialize in safely restoring blood flow in patients with carotid artery disease.
#Carotid Artery Surgery#Tcar Procedure Tampa Florida#Vein And Vascular Institute#Vein Center#Vascular Doctor#Vascular Surgeon#Vein Treatment Pinellas County#Vascular Clinic IN St. Petersburg#Vascular Clinic IN Pinellas County#Vascular Institute St. Petersburg#Vascular Institute Pinellas County
1 note
·
View note
Link
0 notes
Text
Vascular Surgeries: The Key to Healthier Arteries and Improved Blood Flow

Vascular surgeries are critical procedures that address conditions affecting the blood vessels, including arteries and veins. These surgeries help improve blood flow and prevent serious complications such as strokes, aneurysms, and peripheral artery disease (PAD). If you are dealing with vascular issues, finding the right specialist is crucial. With vascular surgeries in Indore, you can restore proper blood circulation and protect your overall cardiovascular health under the care of skilled experts, including the best cardiac surgeon in Indore.
1. Understanding Vascular Diseases
What Are Vascular Diseases?Vascular diseases refer to conditions that affect the circulatory system, including arteries, veins, and lymph vessels. Common issues include blocked or narrowed arteries, weakened blood vessels, and varicose veins.
Symptoms to Watch ForIndividuals with vascular diseases may experience pain, swelling, numbness, or tingling in the limbs. If left untreated, these conditions can lead to severe complications like heart attacks, strokes, or even limb loss.
2. Why Vascular Surgeries Are Essential
Restoring Blood FlowVascular surgeries in Indore are designed to improve blood flow to vital organs and extremities. Procedures such as angioplasty, bypass surgery, and endarterectomy clear blockages and widen arteries to ensure proper circulation.
Preventing Life-Threatening ComplicationsVascular surgeries can prevent serious health risks such as aneurysms and strokes. By addressing arterial blockages or weaknesses early on, surgeons can help patients avoid emergencies and lead healthier lives.
3. Common Types of Vascular Surgeries
Angioplasty and StentingIn this minimally invasive procedure, a small balloon is used to widen blocked arteries. A stent (small metal mesh tube) is then inserted to keep the artery open and maintain proper blood flow.
Bypass SurgeryFor severe blockages, bypass surgery creates a new route for blood flow by using a graft. This graft is often taken from another part of the body, bypassing the clogged artery.
Carotid EndarterectomyThis surgery removes plaque buildup from the carotid arteries in the neck, significantly reducing the risk of stroke.
4. Why Choose the Best Cardiac Surgeon in Indore?
Expertise and Advanced CareThe best cardiac surgeon in Indore will offer extensive experience in treating complex vascular conditions. With the latest techniques and a personalized approach, they ensure each patient receives the most effective treatment.
Minimally Invasive OptionsIn addition to traditional open surgeries, many surgeons specialize in minimally invasive techniques. These methods involve smaller incisions, less pain, and quicker recovery, allowing patients to return to their normal lives sooner.
5. Vascular Surgeries in Indore: What to Expect
Comprehensive DiagnosisBefore recommending surgery, specialists will conduct a thorough diagnosis to understand the extent of the vascular condition. This can include tests like ultrasounds, CT scans, or MRIs.
Personalized Treatment PlansEvery patient’s condition is unique. The best cardiac surgeon in Indore will create a tailored treatment plan that addresses individual needs, ensuring the best outcomes for long-term health.
6. Post-Surgery Recovery and Care
Recovery TimeDepending on the type of vascular surgery, recovery time can vary. Minimally invasive procedures generally allow for faster recovery, while more extensive surgeries may require longer healing periods.
Lifestyle ChangesPost-surgery, patients are often advised to adopt healthier lifestyle habits, such as regular exercise, a balanced diet, and quitting smoking to maintain optimal vascular health.
Vascular diseases can have serious consequences if left untreated, but with advanced vascular surgeries in Indore, patients can improve blood flow, reduce risks, and enhance their quality of life. Trusting the best cardiac surgeon in Indore ensures that you receive expert care and access to cutting-edge treatments. Don't wait until symptoms worsen—seek medical attention and take control of your vascular health today!
#vascular surgeries in indore#vascular surgeries indore#cardiologist indore#best cardiologist indore#heart doctor in indore#heart specialist in indore#pulmonologist in indore#chest specialist in indore#best pulmonologist in indore#best heart specialist in indore#heart specialist indore#lungs specialist in indore
0 notes
Video
tumblr
@vascular_lab ما هو تضيق الشريان السباتي؟ يشير تضيق الشريان السباتي إلى تضيق أحد الشرايين السباتية أو كليهما. يحدث هذا التضيق بمرور الوقت ، بسبب تراكم الترسبات داخل الشريان ، وهي عملية تُعرف باسم تصلب الشرايين. مرض الشريان السباتي هو حالة طبية خطيرة للغاية لأنه يمكن أن يمر دون أن يلاحظها أحد ولأن الانسداد في الشريان السباتي لا يزداد إلا بمرور الوقت ويمكن أن يسبب سكتة دماغية إذا تُرك دون علاج. What is Carotid Stenosis? Carotid stenosis refers to the narrowing of one or both of the carotid arteries. This narrowing occurs over time, due to plaque buildup on the inside of the artery, a process known as atherosclerosis. Carotid artery disease is a very serious medical condition because it can go unnoticed and because blockage in the carotid artery only increases with time and can cause a stroke if left untreated. . . #مختبر_اوعية_دموية #جلطات #جلطه #دوالي #شريان #وريد #شرايين #اوعيه_دمويه #اورده_دمويه #أورده_عنكبوتيه #قسطرة #قسطرة_الاوعية_الدموية #التهاب_اوردة #الأورطي #جراحه #جراحه_اوعيه_دمويه #dvt #varicose #varicosities #spider_veins #varicoseveins #varicoseveintreatment #carotidartery #ultrasound #tcpo2 #abi #aorta #vascularsurgery #vascularity #vascular
0 notes
Text
N-Terminal proteomics reveals distinct protein degradation patterns in different types of human atherosclerotic plaques
BACKGROUND: Destabilization and rupture of atherosclerotic plaques is a major cause of acute atherosclerotic cardiovascular events, including heart attack, ischemic stroke and peripheral arterial disease. Plaque destabilization is associated with extracellular matrix (ECM) modification and remodelling involving protease activity. Enzymatic cleavage generates protein fragments with new 'ends' (N-termini). We hypothesized that plaques susceptible to rupture would contain elevated levels of fragmented proteins with new N-termini. Identification of active proteases and their target proteins might allow categorization of plaque stability. METHODS: Plaques from 21 patients who underwent carotid surgery due to symptomatic carotid artery stenosis were examined in an observational/cross-sectional study. The plaques were solubilized, digested, enriched for N-terminal fragments and analyzed by liquid chromatography-mass spectrometry. RESULTS: The above methodology detected 35349 peptides, with 19543 being N-terminal species; 6561 were subsequently identified and quantified. Multidimensional scaling analysis and hierarchical clustering indicate the presence of three distinct clusters, which correlate with gross macroscopic plaque morphology (soft, mixed, and hard), ultrasound classification (echolucent/echogenic) and presence of hemorrhage/ulceration. Major differences were identified in the complement of peptide fragments, consistent with alternative turnover and degradation pathways dependent on plaque type. Identified peptides include signal and pro-peptides from ECM synthesis/turnover, and many from protein fragmentation. Sequence analysis indicates the targeted proteins (including ECM species) and the proteases (including meprins, cathepsins, matrix metalloproteinases, elastase, kallikreins) involved in fragment generation. CONCLUSIONS: This study provides a large dataset of peptide fragments and proteases involved in plaque stability, mechanistic insights into remodelling, and possible biomarkers for improved atherosclerosis risk profiling. http://dlvr.it/T759wh
0 notes
Text
How to Prevent or Alleviate Blockage of Arteries in the Neck?
The carotid arteries are critical for transporting oxygenated blood to the brain, making arterial obstructions preventable. Carotid artery disease can cause strokes and transient ischemic attacks, jeopardizing brain safety. This article describes how to prevent and treat these obstructions. High blood pressure can strain the heart and cause organ damage or a stroke, therefore it's crucial to monitor it on a regular basis. Monitoring blood pressure levels assists in guiding therapy and lifestyle changes.
Checking cholesterol levels is especially important since high cholesterol can promote plaque accumulation in the arteries. It is advisable to take monounsaturated fats like olive oil while limiting trans fats and saturated fats. Diabetes patients must manage their blood sugar because high amounts of glucose can damage blood vessels and raise the risk of heart disease. Annual carotid Doppler ultrasound exams are non-invasive and used to measure blood flow and carotid artery wall thickness.
Taking these precautions can strengthen the carotid arteries and lower the likelihood of arterial blockages, benefiting overall health and avoiding major consequences.
The carotid arteries are vital because they deliver oxygenated blood to the brain. This emphasizes the importance of preventing artery blockages. Plaque development can put key arteries at risk by narrowing once-wide passageways. This is where carotid artery disease lurks, casting doubt on the safety of our brain's safe regions and frequently resulting in strokes and TIAs.
0 notes
Text
Comprehensive Guide to Doppler Ultrasound: Types, Benefits, and Cost Breakdown
Doppler ultrasound is an essential diagnostic tool used by healthcare professionals to assess blood flow and detect vascular abnormalities. From monitoring fetal health with a fetal Doppler scan to diagnosing renal artery stenosis through a renal Doppler test, this advanced imaging technique provides valuable insights into a variety of medical conditions. In this guide, we'll explore what Doppler ultrasound is, its uses, the different types of Doppler tests, and the cost of getting a Doppler scan near me. We will also answer common questions related to this diagnostic procedure.

What is Doppler Ultrasound?
Doppler ultrasound is a non-invasive imaging technique that uses high-frequency sound waves to measure and visualize blood flow in the arteries and veins. By sending sound waves into the body and recording their reflections off moving blood cells, this test provides valuable information about blood flow speed, direction, and any obstructions or abnormalities in the blood vessels.
The primary principle behind Doppler ultrasound is the Doppler effect, which refers to the change in frequency of sound waves as they bounce off moving objects, such as blood cells. These changes are then used to create real-time images or audio representations of the blood flow.
Types of Doppler Ultrasound Tests
Doppler ultrasound is used for a wide range of diagnostic purposes, depending on the area of the body being examined. Let’s explore the different types of Doppler tests that doctors commonly use:
1. Colour Doppler Ultrasound in Pregnancy
A colour Doppler ultrasound in pregnancy is an important test that helps monitor the blood flow between the mother and the fetus. It assesses the flow of blood in the placenta, umbilical cord, and fetal blood vessels. This test can identify complications like intrauterine growth restriction (IUGR), placental insufficiency, or signs of fetal distress.
The colour Doppler technique uses colour to display the direction and speed of blood flow. Red and blue colours indicate blood flowing toward and away from the probe, while the intensity of the colours represents the flow speed. This scan is a non-invasive and safe way to monitor the baby’s health throughout pregnancy.
2. Renal Doppler Test
A renal Doppler test is used to assess the blood flow in the kidneys. It helps doctors diagnose conditions such as renal artery stenosis, which is a narrowing of the renal arteries that can lead to high blood pressure and kidney damage. The test helps to visualize any blockages, narrowing, or abnormalities in the renal arteries, which is crucial for preventing kidney failure.
The renal Doppler test is typically recommended for patients with high blood pressure, kidney disease, or those who show signs of kidney dysfunction.
3. Carotid Doppler Test
A carotid Doppler test is used to evaluate the blood flow in the carotid arteries, which supply oxygen-rich blood to the brain. It is particularly important in detecting carotid artery disease, which involves plaque buildup that can block blood flow and increase the risk of stroke. Using Doppler ultrasound, doctors can visualize the degree of plaque buildup and any narrowing in the arteries.
This test is often performed in patients with high blood pressure, high cholesterol, or a family history of stroke.
4. Penile Doppler Test
A penile Doppler test is used to measure blood flow to the penis and is typically performed to diagnose erectile dysfunction (ED). The test helps determine if poor blood flow is causing the condition, which may be the result of blockages in the penile arteries. It is particularly useful for diagnosing vascular erectile dysfunction.
By assessing the blood flow in the penile arteries, doctors can identify potential causes of ED and recommend treatments such as medications, lifestyle changes, or surgical interventions.
5. Renal Artery Doppler
A renal artery Doppler test is specifically focused on the blood flow to the kidneys through the renal arteries. This test is crucial for diagnosing renal artery stenosis—a condition that can cause high blood pressure, kidney damage, or kidney failure. The Doppler ultrasound allows doctors to evaluate blood flow in these arteries and determine the severity of any blockages.
Early detection of renal artery stenosis can prevent complications such as kidney failure and high blood pressure.
6. Fetal Doppler Scan
A fetal Doppler scan is an important diagnostic tool used to monitor the well-being of the fetus during pregnancy. It listens to the fetal heartbeat and measures the blood flow in the placenta and umbilical cord. The test helps doctors detect signs of fetal distress, growth restrictions, and abnormalities in the fetal heart rate.
By using sound waves, the fetal Doppler scan is a safe, non-invasive procedure that provides important information about the baby’s health and development.
Benefits of Doppler Ultrasound
Doppler ultrasound offers many advantages over other diagnostic imaging methods. Some of the key benefits include:
Non-invasive: Doppler ultrasound does not require surgery, injections, or the use of radiation, making it a safe diagnostic tool for both children and adults.
Quick and efficient: The procedure typically takes 30-60 minutes, and results are available immediately.
Accurate diagnosis: Doppler ultrasound provides detailed and real-time images of blood flow, which helps doctors diagnose various conditions accurately.
Safe for pregnant women: Since Doppler ultrasound uses sound waves and not radiation, it is completely safe to perform during pregnancy, making it ideal for monitoring fetal health.
Versatile: Doppler ultrasound can assess blood flow in different parts of the body, including the brain, kidneys, and reproductive organs, making it an essential diagnostic tool for a variety of conditions.
What to Expect During a Doppler Ultrasound
Here is a step-by-step guide on what to expect during a Doppler ultrasound procedure:
Preparation: In most cases, you will be asked to wear comfortable clothing or a hospital gown. For some tests, you may be advised to avoid eating or drinking before the procedure.
Gel Application: A special gel will be applied to the skin where the ultrasound will be performed. This gel helps transmit the sound waves and ensures clear images.
Procedure: The technician will use a small handheld device called a transducer to send sound waves into the body. The transducer is moved over the skin to capture the images and sound waves that reflect off the blood cells.
Completion: After the test, the gel will be wiped off, and you can resume your normal activities. In most cases, the doctor will provide you with the results shortly after the test or schedule a follow-up appointment.
Doppler Ultrasound Cost
The price of a Doppler ultrasound can vary depending on several factors, including the type of test, location, and healthcare provider.
Factors that affect the cost include:
Type of Doppler test: More specialized tests like fetal Doppler scans or carotid Doppler tests tend to be more expensive than basic tests like renal Doppler tests.
Location: Prices may vary based on your location and whether the test is performed in a hospital, outpatient clinic, or private diagnostic center.
Insurance: If you have health insurance, it may cover part or all of the cost. It’s a good idea to check with your insurance provider for coverage details.
If you’re located in Indore, trusted diagnostic centers like Health Scan Diagnostics provide reliable and affordable Doppler ultrasound services.
Commonly Asked Questions About Doppler Ultrasound
1. What is a Doppler ultrasound used for?
Doppler ultrasound is primarily used to assess blood flow in the arteries and veins. It helps diagnose conditions like vascular disease, kidney disease, stroke risk, and erectile dysfunction.
2. Is Doppler ultrasound safe during pregnancy?
Yes, Doppler ultrasound is completely safe during pregnancy. Unlike X-rays, Doppler ultrasound uses sound waves, making it a non-invasive and safe option for both the mother and the baby.
Conclusion
Doppler ultrasound is a crucial diagnostic tool that provides detailed information about blood flow and circulatory health. Whether you’re undergoing a fetal Doppler scan, renal Doppler test, or a carotid Doppler test, this non-invasive procedure plays a vital role in diagnosing and monitoring various health conditions.
If you’re looking for a Doppler test near me, contact a reputable quality diagnostic centre in Indore like Health Scan Diagnostics for affordable and high-quality testing.
contact us:
[email protected] 78695 24599 451-G Greater Brajeshwari,Near Kerala Bakery,Pipliyahana Road, Pipliyahana, indore, Madhya Pradesh 452016
0 notes
Text
Carotid Angioplasty and Stenting in India
Carotid Angioplasty and Stenting
India: A stroke prevention strategy — Carotid Angioplasty and Stenting (CAS)
What is carotid artery diseaseThis disease is characterized by fattening of the arteries supplying blood to the brain. This can cause blood flow to become blocked, raising the chances of stroke. What is Carotid Angioplasty and Stenting (CAS)? Carotid Angioplasty and Stenting (CAS) is a minimally invasive procedure to open narrowed or blocked arteries of the neck, which supply blood to the brain.
Why Choose India for CAS?
India is the latest global hub for health–care with particular focus to heart care. There is a number of reasons for its increasing popularity as CAS:
Expert Hands with Innovative Technology: India has top-notch Interventional Cardiologists, along with High-Quality Medical Facilities.
Affordable Treatment: The cost of CAS in India is approximately 30% lower than in most Western countries, ensuring no compromise on quality.
Less Invasive Techniques: As CAS is a less invasive procedure, fewer hospital stays and shorter recovery times are commonly experienced.
Top-Notch Patient Care: The Indian hospitals are known for their passion toward the healthcare services.
The CAS Procedure
The CAS procedure involves:
Anesthesia: Local anesthesia is given to numb the groin area.
Insertion of Catheter: Insertion of a small, thin, flexible tube called catheter into a blood vessel in the groin.
In Balloon Angioplasty, the catheter is advanced to the constricted carotid artery where a balloon is inflated to crush the plaque.
Stenting: A tiny, mesh tube called a stent is implanted to hold open the artery.
0 notes
Link
0 notes