#Non-alcoholic fatty liver disease (NAFLD)
Explore tagged Tumblr posts
Text
#Liver disease#Hepatitis#Hepatitis A#B#C#D#E#Chronic liver disease#Liver damage#Cirrhosis#Liver fibrosis#Hepatocellular injury#Liver inflammation#Alcoholic liver disease#Non-alcoholic fatty liver disease (NAFLD)#Liver cancer (Hepatocellular carcinoma)#Viral transmission#Bloodborne pathogens#Contaminated food and water#Unprotected sex#Needle sharing#Vertical transmission (mother to child)#Immune system response#Risk factors for liver disease#Hepatitis vaccination#Liver biopsy#Liver function tests#Viral load#Liver transplantation#Preventive measures for hepatitis
2 notes
·
View notes
Text
The Impact of High Fructose Corn Syrup on Mitochondrial Function
The Impact of High Fructose Corn Syrup on Mitochondrial Function:
Analysis
High fructose corn syrup (HFCS), a widely used sweetener derived from corn, has become a major component of the modern diet, especially in processed foods and sugary beverages. HFCS is composed of glucose and fructose in varying proportions, with HFCS-55 (55% fructose, 45% glucose) and HFCS-42 (42% fructose, 58% glucose) being the most common formulations. While the impact of HFCS on metabolic health has been widely discussed, recent studies have shown that it can also exert a detrimental effect on mitochondrial function. This technical analysis explores the biochemical mechanisms by which HFCS damages mitochondria, contributing to cellular dysfunction and a range of metabolic diseases.
Mitochondrial Physiology and Biochemical Function
Mitochondria are highly specialized organelles responsible for producing adenosine triphosphate (ATP), the primary energy currency of the cell, through oxidative phosphorylation (OXPHOS). This process occurs in the inner mitochondrial membrane and involves the electron transport chain (ETC) and ATP synthase. The mitochondria are also involved in regulating cellular metabolism, maintaining redox balance, calcium homeostasis, and apoptosis (programmed cell death). Mitochondrial dysfunction, characterized by impaired ATP production, altered mitochondrial dynamics (fusion/fission), and excessive reactive oxygen species (ROS) production, is a key factor in the pathogenesis of many chronic diseases, including obesity, insulin resistance, cardiovascular diseases, and neurodegenerative disorders.
Fructose Metabolism and Its Divergence from Glucose
The metabolism of fructose, particularly in the liver, diverges significantly from that of glucose, and it is this divergence that underpins much of the mitochondrial dysfunction associated with HFCS consumption. Unlike glucose, which is predominantly metabolized via glycolysis and the citric acid cycle (TCA cycle), fructose bypasses the rate-limiting step of glycolysis, catalyzed by phosphofructokinase-1 (PFK-1), and is instead phosphorylated by fructokinase to form fructose-1-phosphate. This rapid metabolism of fructose in the liver can overwhelm metabolic pathways and lead to the accumulation of intermediate metabolites such as dihydroxyacetone phosphate (DHAP) and glyceraldehyde, which can be further converted to fatty acids and triglycerides through de novo lipogenesis (DNL).
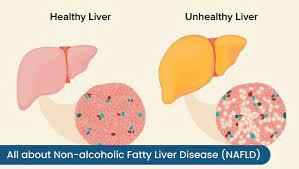
Excessive fructose consumption leads to the accumulation of triglycerides, particularly within hepatocytes, which is a hallmark of non-alcoholic fatty liver disease (NAFLD). The lipid accumulation in the liver, in turn, exacerbates mitochondrial dysfunction and oxidative stress, contributing to insulin resistance and a cascade of metabolic disorders.
Mechanisms of Mitochondrial Damage Induced by HFCS
Increased ROS Production
One of the most significant consequences of excess fructose metabolism is the elevated production of reactive oxygen species (ROS). ROS are byproducts of cellular respiration, primarily generated at complexes I and III of the electron transport chain. Under normal conditions, mitochondria have a robust antioxidant defense system, including enzymes like superoxide dismutase (SOD), catalase, and glutathione peroxidase, which help neutralize ROS. However, when cells are exposed to an overload of fructose, the liver mitochondria become overwhelmed, leading to excessive ROS generation.
Fructose metabolism increases the NADPH/NADP+ ratio, enhancing the activity of nicotinamide adenine dinucleotide phosphate (NADPH)-dependent oxidases such as NADPH oxidase (NOX), which further amplifies ROS production. These ROS cause oxidative damage to mitochondrial DNA (mtDNA), lipids in the mitochondrial membranes, and mitochondrial proteins. Such damage impairs mitochondrial function by decreasing mitochondrial membrane potential, disrupting the electron transport chain, and promoting mitochondrial fragmentation. Furthermore, mtDNA is particularly vulnerable to ROS due to its proximity to the electron transport chain and the lack of histone protection, leading to mutations that impair mitochondrial replication and protein synthesis.
Disruption of Mitochondrial Biogenesis
Mitochondrial biogenesis refers to the process by which new mitochondria are synthesized within a cell to meet the energy demands. This process is tightly regulated by several transcription factors, most notably peroxisome proliferator-activated receptor-gamma coactivator 1-alpha (PGC-1α). PGC-1α activates the transcription of nuclear and mitochondrial genes involved in energy metabolism, mitochondrial dynamics, and antioxidant defenses.
Fructose consumption has been shown to inhibit PGC-1α expression in both liver and skeletal muscle cells. Reduced PGC-1α levels lead to impaired mitochondrial biogenesis, which limits the ability of cells to adapt to increased energy demands. This is particularly concerning in tissues with high metabolic demands, such as muscle, heart, and liver, where impaired mitochondrial function can exacerbate energy deficits and lead to insulin resistance, fatty liver disease, and other metabolic disorders.
Mitochondrial Permeability Transition and Apoptosis
Chronic exposure to high levels of fructose can lead to mitochondrial permeability transition (MPT), a process in which the mitochondrial inner membrane becomes permeable to ions and small molecules, disrupting mitochondrial function. MPT is typically induced by excessive ROS production, calcium overload, or changes in the mitochondrial membrane potential. The opening of the mitochondrial permeability transition pore (MPTP) leads to the loss of mitochondrial membrane potential, uncoupling of oxidative phosphorylation, and the release of pro-apoptotic factors such as cytochrome c into the cytoplasm. This, in turn, activates the caspase cascade, promoting apoptosis.
In the context of HFCS-induced mitochondrial dysfunction, increased ROS and altered metabolic intermediates, such as ceramides, may trigger MPT and apoptotic pathways, leading to cell death and tissue damage. In tissues such as the liver and pancreas, this can exacerbate the pathological progression of fatty liver disease and insulin resistance.
Fatty Acid Accumulation and Impaired Beta-Oxidation
Excessive fructose consumption induces de novo lipogenesis (DNL) in the liver, leading to an increase in the synthesis of fatty acids, which are esterified into triglycerides and stored within hepatocytes. This accumulation of lipids can overwhelm the capacity of mitochondria to oxidize these fatty acids via beta-oxidation, leading to mitochondrial dysfunction. The accumulation of lipotoxic intermediates such as ceramides and diacylglycerols further impairs mitochondrial function by inhibiting key enzymes involved in mitochondrial energy production.
Moreover, the excess fatty acids can impair mitochondrial membrane fluidity, reducing the efficiency of oxidative phosphorylation. The lipid-induced mitochondrial dysfunction leads to further oxidative stress, creating a feedback loop that exacerbates the metabolic disturbances caused by high fructose intake.
Clinical Implications of HFCS-Induced Mitochondrial Dysfunction
The long-term consumption of HFCS has profound implications for human health, particularly in the context of metabolic diseases:
Insulin Resistance and Type 2 Diabetes: HFCS-induced mitochondrial dysfunction, particularly in liver and muscle cells, contributes to impaired insulin signaling and glucose homeostasis. As mitochondrial function declines, cells become less responsive to insulin, leading to insulin resistance, a precursor to type 2 diabetes.
Non-Alcoholic Fatty Liver Disease (NAFLD): The accumulation of fat in the liver, driven by increased fructose metabolism, leads to mitochondrial damage and dysfunction, which exacerbates the progression of NAFLD to non-alcoholic steatohepatitis (NASH), a more severe form of liver disease.
Cardiovascular Disease: Mitochondrial dysfunction in cardiomyocytes can impair ATP production, leading to reduced contractile function and the progression of cardiovascular disease. The increased oxidative stress and inflammatory mediators associated with mitochondrial damage also contribute to vascular injury and atherosclerosis.
Neurodegenerative Diseases: Impaired mitochondrial function in neurons, driven by high fructose intake, may contribute to neurodegenerative diseases such as Alzheimer's and Parkinson's disease, as mitochondria play a critical role in maintaining neuronal health.
Conclusion
High fructose corn syrup exerts a significant impact on mitochondrial function through several interconnected mechanisms. These include the increased production of reactive oxygen species (ROS), inhibition of mitochondrial biogenesis, induction of mitochondrial permeability transition, and the accumulation of toxic lipid intermediates. These disruptions in mitochondrial homeostasis contribute to the development of insulin resistance, non-alcoholic fatty liver disease, and other chronic metabolic diseases. Addressing the widespread consumption of HFCS and reducing dietary fructose intake could be crucial in mitigating mitochondrial dysfunction and preventing associated metabolic disease
#High Fructose Corn Syrup (HFCS)#Mitochondrial Function#Mitochondria#Oxidative Phosphorylation#Reactive Oxygen Species (ROS)#Fructose Metabolism#ATP Production#Mitochondrial Biogenesis#PGC-1α#Mitochondrial Dysfunction#Insulin Resistance#Fatty Liver Disease(NAFLD)#Mitochondrial Permeability Transition (MPT)#Apoptosis#Beta-Oxidation#De Novo Lipogenesis (DNL)#Ceramides#Lipotoxicity#Non-Alcoholic Steatohepatitis (NASH)#Type 2 Diabetes#Cardiovascular Disease#Neurodegenerative Diseases#Fatty Acids#Liver Mitochondria#Metabolic Disorders#Fructose-Induced Oxidative Stress#Cellular Metabolism#Mitochondrial Membrane Potential#Mitochondrial DNA (mtDNA)#Lipid Accumulation
0 notes
Text
If you are experiencing signs of NAFLD or are at risk? If you are concerned about fatty liver disease or need expert care for NAFLD, Dr. Vikrant Kale at Kaizen Gastro Care is here to provide you with the best liver care in Pune. With a focus on early detection, prevention, and treatment, Dr. Kale and his team are dedicated to helping patients achieve optimal liver health.
#Non-Alcoholic Fatty Liver Disease Treatment#NAFLD Treatment#NAFLD Specialist#NAFLD Doctor#Stomach Specialist#Gastroenterologist
0 notes
Text
Non-Alcoholic Fatty Liver Ayurvedic Treatment in India
Reclaim Your Liver Health with Ayurvedic Treatment for Non-Alcoholic Fatty Liver Disease (NAFLD) in India.

The liver is an extraordinary organ, responsible for a myriad of vital functions within the human body. It plays a central role in detoxification, metabolism, and the production of essential proteins. However, an alarming health issue has emerged in recent years, affecting millions across the globe—Non-Alcoholic Fatty Liver Disease (NAFLD). In India, Expert Ayurveda offers a beacon of hope through their specialized Ayurvedic Treatment for NAFLD, focusing on the complexities of fatty liver.
Understanding NAFLD and Its Prevalence in India

Non-Alcoholic Fatty Liver Disease, often referred to as NAFLD, is a condition characterized by the accumulation of excess fat in the liver. Remarkably, it occurs in individuals who do not consume excessive amounts of alcohol. NAFLD is closely associated with modern lifestyles, poor dietary choices, lack of physical activity, and metabolic syndrome. It encompasses a spectrum of liver conditions, ranging from the relatively benign accumulation of fat (steatosis) to more severe inflammation and liver damage (non-alcoholic steatohepatitis or NASH). Left untreated, NAFLDcan progress to advanced liver diseases such as cirrhosis and even liver cancer.
The Ayurvedic Approach to fatty liver Treatment in India
India's rich heritage of Ayurveda provides a holistic approach to health and wellness, including the treatment of liver diseases like NAFLD. Ayurvedic Treatment focuses on harmonizing the body's energies (doshas), bolstering digestion, detoxifying the liver, and promoting overall vitality.
Expert Ayurveda: Your Trusted Partner in NAFLD Treatment
Expert Ayurveda stands at the forefront in India, specializing inAyurvedic Treatment for NAFLD, with an emphasis on addressing the intricacies of fatty liver. Here's why they are the preferred choice for individuals seeking natural and effective remedies:
Ayurvedic Mastery: Expert Ayurveda boasts a team of highly accomplished Ayurvedic doctors and practitioners who possess profound knowledge of NAFLD and its Ayurvedic Treatment. Their expertise ensures that patients receive the highest standard of care.
Personalized fatty liver Solutions: Understanding that NAFLD varies from person to person, Expert Ayurveda provides customized treatment plans tailored to the unique needs and constitution of each individual, putting a spotlight on the management of fatty liver
Holistic Healing: Ayurveda's philosophy is deeply rooted in treating the root causes of ailments, rather than merely alleviating symptoms. Expert Ayurveda's approach is holistic, focusing not only on liver health but also on overall well-being.
Natural Remedies: Expert Ayurveda harnesses the power of natural herbs, dietary recommendations, lifestyle modifications, and detoxification therapies to treat NAFLD. These natural remedies are safe, time-tested, and have minimal side effects, making them particularly apt for addressing fatty liver.
Preventive Measures: In addition to treatment, Expert Ayurveda emphasizes preventive measures and long-term management of NAFLD. They offer guidance on dietary choices, physical activity, and lifestyle changes to help patients maintain optimal liver health, with a keen focus on the fatty liveraspect.
Patient-Centric Approach: At Expert Ayurveda, patient-centered care is paramount. They ensure that patients are well-informed, comfortable, and empowered throughout their NAFLD treatment journey, with a deep understanding of the fatty liver intricacies.
The Ayurvedic fatty liver Treatment Process
Your journey towards liver health with Expert Ayurveda typically involves the following steps, with a strong emphasis on fatty liver:
Comprehensive Consultation: The process commences with a thorough consultation where Ayurvedic doctors assess your condition, medical history, and individual constitution (prakriti), paying particular attention to the presence of fatty liver.
Accurate Diagnosis: Based on the consultation and diagnostic tests, the severity and nature of your NAFLD, including fatty liver characterization, are determined.
Tailored Treatment Plan: An individualized treatment plan is meticulously crafted, incorporating Ayurvedic herbs, dietary recommendations, lifestyle modifications, and detoxification therapies, all designed to specifically target fatty liver issues.
Treatment Phase: You embark on a structured treatment phase, during which you'll receive Ayurvedic remedies and therapies customized to address the fatty liver aspect of your condition.
Regular Monitoring: Regular follow-up consultations and assessments ensure that your progress, especially concerning fatty liver, is closely tracked. Adjustments are made to the treatment plan as necessary.
Lifestyle Guidance: Expert Ayurveda provides detailed guidance on maintaining a healthy lifestyle, including dietary choices and exercise routines. This comprehensive approach is key to preventing the recurrence of fatty liver
Sustained Support: Even after the successful completion of treatment, Expert Ayurveda remains your partner in long-term liver health, offering ongoing support, particularly for managing fatty liver concerns.
Choose Ayurveda for fatty liver Treatment in India
If you're in search of a natural, holistic, and effective treatment for NNon-Alcoholic Fatty Liver Disease, especially focusing on the complexities of fatty liver, Expert Ayurveda is your unwavering ally. Their Ayurvedic prowess, personalized treatment plans, and patient-centric philosophy offer a pathway to healing for individuals grappling with liver health challenges. Take the first step towards revitalizing your liver health by scheduling an appointment with Expert Ayurveda, and embark on a transformative journey towards a healthier and more vibrant life.
For More Information
Dr. Paresh J Thakkar, 32,Raj ami complex, Amin Society,Near swastik school, Sardar patel colony, Narayanpura, Ahmedabad.
+91 9924184234
#Ayurvedic Treatment for NAFLD in India#Non-Alcoholic Fatty Liver Ayurvedic Treatment in India#ayurvedic doctors for liver treatment in india#ayurvedic liver treatment for fatty liver in india#ayurvedic liver treatment in india#fatty liver disease
0 notes
Text
NAFLD and Nursing: Essential Information and Interventions
What is Non-Alcoholic Fatty Liver Disease (NAFLD)? NAFLD stands for Non-Alcoholic Fatty Liver Disease and is one of the most common liver disorders globally. The liver plays an essential role in many body functions, from producing bile that helps digest fats to storing glucose for energy. NAFLD occurs when there is an accumulation of excess fat in liver cells, that is not due to significant…
View On WordPress
#cirrhosis#Diet#elevated liver enzymes#exercise#fatigue#high blood sugar#insulin resistance#liver cancer#liver disease#liver inflammation#medication#NAFLD#NASH#Non-Alcoholic Fatty Liver Disease#non-alcoholic steatohepatitis#Obesity#prevention#triglycerides#weight management
0 notes
Text
New Onset of Acute and Chronic Hepatic Diseases Post-COVID-19 Infection: A Systematic Review - Published Sept 10, 2024
Abstract The SARS-CoV-2 virus caused a pandemic in the 2020s, which affected almost every aspect of life. As the world is recovering from the effect of the coronavirus, the concept of post-COVID-19 syndrome has emerged. Multiple organ systems have been implicated, including the liver. We aim to identify and analyze the reported cases of severe and long-term parenchymal liver injury post-COVID-19 infection. Several databases were used to conduct a comprehensive literature search to target studies reporting cases of severe and long-term parenchymal liver injury post-COVID-19 infection. Screening, data extraction, and cross checking were performed by two independent reviewers. Only 22 studies met our inclusion criteria. Our results revealed that liver steatosis, non-alcoholic fatty liver disease (NAFLD), and cirrhosis were the most reported liver associated complications post-COVID-19 infection. Moreover, complications like acute liver failure, hepatitis, and liver hemorrhage were also reported. The mechanism of liver injury post-COVID-19 infection is not fully understood. The leading proposed mechanisms include the involvement of the angiotensin-converting enzyme-2 (ACE-2) receptor expressed in the liver and the overall inflammatory state caused by COVID-19 infection. Future studies should incorporate longer follow-up periods, spanning several years, for better insight into the progression and management of such diseases.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
22 notes
·
View notes
Text
NASH is now called MASH
metabolic dysfunction-associated steatohepatitis (MASH), formerly known as nonalcoholic steatohepatitis (NASH), which has long been recognized as “the hepatic manifestation of metabolic syndrome.”
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a chronic liver disease that occurs when fat builds up in the liver in people who don't drink much or no alcohol. It was previously known as non-alcoholic fatty liver disease (NAFLD)
3 notes
·
View notes
Text
Is dark chocolate healthy for liver?
Dark chocolate has been hailed as a superfood because of its antioxidant properties, known to benefit Heart Disease and Stroke. Cocoa beans, from which dark chocolate is made, are rich in bioflavonoids, which have the highest antioxidant level compared to other food sources.
Many studies have begun to investigate the potential benefits of dark chocolate on the Liver. It was found that dark chocolate reduces damage to the blood vessels in patients who have suffered scarring on the Liver due to excessive drinking or Liver disease. In addition, dark chocolate reduces blood pressure in the Liver as it contains high levels of antioxidants, which negate the effects of damaging particles from the body.
One study was able to show a clear association between eating dark chocolate and portal hypertension (high blood pressure in the Liver) and the potential to minimize the onset and impact of end-stage Liver disease and Liver Failure.
Cirrhosis is scarring of the Liver as a result of long-term, continuous damage to the Liver. In Cirrhosis, circulation in the Liver is damaged by oxidative stress and reduced antioxidant systems. After a meal, blood pressure in the abdominal veins usually increases due to increased blood flow to the Liver. In Cirrhosis, any further rise in pressure can cause them to rupture and bleed.
Another study found that polyphenols contained in dark chocolate could slow disease progression in Non-alcoholic Steatohepatitis (NASH), the more serious form of Non-alcoholic Fatty Liver Disease (NAFLD), characterised by excess fat buildup in the Liver.
Oxidative stress and inflammation are considered of primary importance in the progression of NAFLD. Consuming dark chocolate can halt oxidative stress and hepatic inflammation seen in NASH, which ultimately leads to Liver failure. Thus, dark chocolate could halt disease progression.
A daily dosage of 30 g of dark chocolate for 12 weeks in patients with NAFLD produced a significant decrease in body weight and BMI, significant risk factors for developing NAFLD. The same study found that HDL cholesterol (good cholesterol that protects the Heart) level increased in NAFLD patients indicating a benefit in the lipid profile. Type 2 diabetes is often found in persons with NAFLD. The antioxidants in dark chocolate help the body use its insulin more efficiently to help control blood sugar. As a result, it helps decrease insulin resistance, the driving factor of type 2 diabetes.
Another interesting finding by a neuroscientist found that a small square of dark chocolate melted on the tongue 20 minutes before eating triggers a hormone that signals a feeling of fullness to the brain so that the meal portion consumed is less. This could again be beneficial in people watching their weight or avoiding the risk of Liver disease.
Notably, chocolates other than dark chocolate contain less cocoa and are not as beneficial. Many dark chocolate brands have over 70% of cocoa, while milk chocolates contain about 20-30% of cocoa solids. So, for Liver health, choose dark chocolates.
2 notes
·
View notes
Text
Investment Surge in GLP-1 Drugs Market: Trends and Future Prospects
Market Growth and Investment Trends
The GLP-1 drugs market has seen substantial investment from pharmaceutical companies and venture capitalists. This is driven by the increasing prevalence of type 2 diabetes and obesity, coupled with the efficacy of GLP-1 drugs in managing these conditions. Key trends include:
Rising Prevalence of Diabetes and Obesity: The global rise in lifestyle-related health issues is fueling demand for effective treatments.
Innovative Drug Development: Companies are investing heavily in R&D to develop next-generation GLP-1 drugs with improved efficacy and fewer side effects.
Strategic Collaborations and Partnerships: Collaborations between pharmaceutical giants and biotech firms are accelerating innovation and market entry of new drugs.
Recent Developments
Several notable developments have occurred in the GLP-1 drugs market:
New Drug Approvals: Regulatory bodies like the FDA and EMA have recently approved several new GLP-1 receptor agonists, expanding treatment options.
Clinical Trials and Research: Ongoing clinical trials are investigating the broader therapeutic potential of GLP-1 drugs, including their effects on cardiovascular health and non-alcoholic fatty liver disease (NAFLD).
Technological Advancements: Innovations in drug delivery systems, such as oral formulations and long-acting injectables, are enhancing patient compliance and convenience.
Browse Press Release
Future Opportunities
The future of the GLP-1 drugs market holds numerous opportunities for growth and innovation:
Expansion into New Therapeutic Areas: Research suggests potential applications of GLP-1 drugs in conditions beyond diabetes and obesity, such as neurodegenerative diseases and inflammation.
Personalized Medicine: Advances in genomics and biomarkers may enable personalized GLP-1 therapies tailored to individual patient profiles, improving outcomes.
Emerging Markets: Increasing healthcare access and rising diabetes prevalence in emerging markets present significant growth opportunities for GLP-1 drugs.
Conclusion
The GLP-1 drugs market is poised for remarkable growth, driven by robust investment, innovative developments, and expanding therapeutic applications. As research progresses and new technologies emerge, GLP-1 receptor agonists will play a crucial role in addressing the global burden of diabetes, obesity, and potentially other diseases, offering improved health outcomes for millions.
About iDataAcumen
iDataAcumen is a global business intelligence and management consulting firm providing data driven solutions to a wide array of business challenges. Our clients are present across major geographies globally and belong to industries ranging mainly from healthcare, pharmaceuticals, life science, biotechnology, medical devices, food industry, chemicals, among others. We have catered to more than 500 clients across these industries.
We aspire to help our clients build a sustainable business by providing them robust business insights that are derived from sound data driven analysis. In today’s ever changing business environment, its become important to look objectively at your own business just as it is important to look at the competition. Technological advancement including but not limited to big data, artificial intelligence, and machine learning are helping industries worldwide to make informed business decisions. Our research process also makes use of some of these advanced tools to uncover valuable insights from vast amount of data to arrive at logical conclusions.
2 notes
·
View notes
Text
I was diagnosed with NAFLD (non-alcoholic fatty liver disease) :(
something i've been thinking about...
in the mornings when Ghost didn't have a deployment, he would get your favourite starbucks drink EVERY morning. you would wake up and walk into the kitchen to find your drink sitting next to him as he read the daily newspaper.
14 notes
·
View notes
Text

Food for removing NAFLD.
NAFLD = Non alcoholic fatty liver disease.
This is my diet chart for NAFLD.
This is not perfectly ideal. But I can manage these foods in my poor economic conditions.
1) smashed papaya.
2) cucumber-tomato-naga 🥗 salad.
3) walnut [akh root].
4) 2 milk thistle supplement. . . .
I wish, I can add extra-vergin olive oil.
#walnuts#nafld#weight loss diet#superfood#usj#utsho_sadhak_joy#bangladesh#india#united states#united kingdom#germany
2 notes
·
View notes
Text
Everyone is being so kind and supportive on my blazed post to find my Prince Sidon figure!
This makes me so happy! So many people are trying to help me, a complete stranger, and wishing me good luck. People are giving me so many compliments and good messages about how Im using blaze, how I approach the proper compensation for artistic work, and how I view supporting tumblr.
I have really been struggling lately. I'm a medical marvek of multiple illnesses, both mental and physical. I've had a really hard year and I'm currently on medical leave working closely with psychiatric services to get my debilitating bipolar disorder under control. I am at a place where medication isn't helping me, and I've been relying strongly on family and friends.
I've never had a bipolar episode so intense, so prolonged, and so debilitating. But that is just the most forefront of my problems right now. I've been struggling to take care of NAFLD, Or non alcoholic fatty liver disease, which is very common in my family and often tied with developing diabetes. I need to change my whole lifestyle permanently to prevent further issues. If any of you have ever tried to quit an addicting processed American diet to a fresh minimally processed-low fat-low sugar-low cholesterol-No red meat-Whole wheat diet, then you know how hard it is. Not just the physical cravings for junk food that are so bad they nearly consume ones thoughts, but the societal and family pressure to socialize and bond through food, the mockery and unwarranted cruelty for refusing "normal" food, staple foods, or red meat.
Thats not all however! I had to have all my upper teeth removed at a young age due to a combination of a genetic defect, poor dietary upbringing, and medications that damage teeth greatly over time. Medications I'll likely be taking for the rest of my life. It took me a few years, but I saved up enough to get the "cosmetic" surgery to have screws implanted in my jaw that teeth could be affixed to. In the time it took to raise the money, the medication and genetic defect caused the reabsorbtion of my upper jaw to the point I barely have any upper jaw bone left. There isn't enough left to have a good chance with a bone graft, never mind enough to put implants in. This news was devastating to me. My face is caved in now, and I'm only in my mid 20's.
Then there's the normal assorted fun bag for my body. Wait list to remove heavy fat deposites that cause strain on my back and hinder my breathing. Migraines I can only try to sleep through as doing anything else is too painful. Shortness of breath and stamina from a sudden dramatic weight gain related to a new medixation. I need new glasses as I can't read the signs in windows with my current ones. Painful cysts on my scalp that I cant get removed yet. A new and very persistent rash that Ive been taking antibiotics for, for a month, while my doctor struggles to figure out what is causing it. Constant fatigue and executive disfunction to the point someone has to wake me up every day, and I barely eat because the effort is so much.
I have very little mental and physical energy. Life is hard. Kindness from strangers and the prospect of having my unconditionally supportive shark friend is invaluable to me right now. I felt good today, and I am so thankful.
3 notes
·
View notes
Text
Top Liver Specialist in Thane: Expert Care by Dr. Rajdeep More
When it comes to liver health, seeking the right care is essential for preventing and managing liver-related issues. If you’re looking for a Liver specialist in Thane, Dr. Rajdeep More is a trusted and experienced expert who provides comprehensive care for various liver conditions. With his expertise, advanced diagnostic tools, and personalized treatment approach, Dr. More is the go-to liver specialist in Thane for optimal liver care.
Why Choose Dr. Rajdeep More as Your Liver Specialist in Thane?
Dr. Rajdeep More stands out as a leading liver specialist in Thane, offering specialized treatment for a range of liver conditions, from hepatitis to cirrhosis and fatty liver disease. Here are several reasons why Dr. More is considered the best choice for liver treatment in the region:
Expertise and Experience Dr. Rajdeep More is highly qualified with years of experience in diagnosing and treating liver disorders. He has a deep understanding of liver diseases and is known for his holistic approach to liver health. Whether it's chronic liver disease, liver cancer, or liver transplantation, Dr. More ensures that every patient receives the most advanced and appropriate treatment.
Comprehensive Liver Care As a leading liver specialist in Thane, Dr. More offers comprehensive care for various liver conditions, including:
Hepatitis (A, B, C, D, and E)
Fatty liver disease
Liver cirrhosis
Liver cancer
Liver transplant consultation and management
Alcoholic liver disease
Non-alcoholic fatty liver disease (NAFLD) Dr. More’s expertise covers both common and complex liver conditions, providing patients with the best possible care and outcomes.
State-of-the-Art Diagnostics and Treatments Dr. Rajdeep More uses the latest diagnostic techniques, including liver function tests, imaging tests (like ultrasound and CT scans), and biopsies to accurately diagnose liver conditions. With advanced technology and up-to-date medical practices, patients benefit from precise diagnosis and effective treatments that address the root cause of liver issues.
Personalized Treatment Plans Dr. More believes in providing individualized treatment plans tailored to the patient’s specific condition and needs. Whether it's lifestyle changes, medication, or surgical intervention, he ensures that each patient receives care that suits their unique situation. His approach focuses on long-term management, ensuring that the liver’s health is restored and maintained.
Holistic Care and Support In addition to medical treatment, Dr. Rajdeep More emphasizes the importance of lifestyle changes, including diet and exercise, to promote liver health. He educates patients about the importance of regular check-ups and early detection, empowering them to take charge of their health.
Services Offered by Dr. Rajdeep More, Liver Specialist in Thane
As a leading liver specialist in Thane, Dr. Rajdeep More provides a wide range of services to treat and manage liver-related issues:
Diagnosis and Monitoring: Accurate diagnosis using state-of-the-art diagnostic tools and ongoing monitoring of liver conditions.
Medical Management: Treatment for conditions such as hepatitis, cirrhosis, and fatty liver, including medications to manage symptoms and improve liver function.
Liver Transplant Consultation: For patients with end-stage liver disease, Dr. More provides liver transplant evaluations and consultation to determine the best course of action.
Liver Cancer Treatment: Expert management and treatment of liver cancer, including chemotherapy, surgery, and other advanced options.
Lifestyle and Dietary Counseling: Dr. More offers personalized dietary plans and guidance to support liver health and prevent further complications.
Common Liver Conditions Treated by Dr. Rajdeep More
Dr. Rajdeep More specializes in the treatment of various liver conditions, including:
Hepatitis: Whether caused by a viral infection, alcohol abuse, or other factors, hepatitis is a leading cause of liver damage. Dr. More offers treatment plans to manage and cure hepatitis, depending on the type and stage of the disease.
Fatty Liver Disease (NAFLD/NASH): Non-alcoholic fatty liver disease is one of the most common liver disorders today. Dr. More provides expert care and treatment to reduce liver fat and improve liver function.
Cirrhosis: Cirrhosis is a condition where the liver becomes severely scarred. Dr. More offers advanced treatment options to manage cirrhosis and prevent complications such as liver failure.
Liver Cancer: Dr. Rajdeep More provides expert treatment for liver cancer, offering the latest options for surgery, chemotherapy, and radiation therapy to improve the chances of a successful outcome.
Liver Transplants: For patients with advanced liver disease, Dr. More offers consultation for liver transplants, guiding patients through the evaluation and process.
Why Liver Health Matters
The liver is a vital organ that plays a key role in detoxifying the body, producing proteins, and aiding in digestion. Maintaining liver health is crucial for overall well-being. Early detection of liver diseases and timely intervention can prevent severe complications and improve the quality of life.
With Dr. Rajdeep More, patients can be assured of receiving the highest standard of care to maintain or restore liver health, whether it involves medical management, lifestyle changes, or surgical interventions.
Conclusion
If you are looking for a liver specialist in Thane, Dr. Rajdeep More offers comprehensive and expert care to treat a wide range of liver conditions. With a focus on personalized treatment plans, advanced diagnostics, and holistic care, Dr. More is committed to providing the best possible liver health management for his patients. Schedule a consultation today and take the first step toward better liver health!
0 notes
Text
If you are experiencing signs of NAFLD or are at risk? If you are concerned about fatty liver disease or need expert care for NAFLD, Dr. Vikrant Kale at Kaizen Gastro Care is here to provide you with the best liver care in Pune. With a focus on early detection, prevention, and treatment, Dr. Kale and his team are dedicated to helping patients achieve optimal liver health.
#Non-Alcoholic Fatty Liver Disease Treatment#NAFLD Treatment#NAFLD Specialist#NAFLD Doctor#Stomach Specialist#Gastroenterologist
0 notes
Text
life expectancy with fatty liver disease treatment

Life Expectancy with Fatty Liver Disease & Treatment
The life expectancy of someone with fatty liver disease depends on the stage of the disease and how well it is managed. Proper treatment and lifestyle changes can significantly improve outcomes.
1. Simple Fatty Liver (NAFLD/AFLD - Early Stage)
Life Expectancy: Normal with proper treatment.
Treatment: Healthy diet, weight loss, exercise, and avoiding alcohol can fully reverse the condition.
2. Non-Alcoholic Steatohepatitis (NASH) / Alcoholic Hepatitis
Life Expectancy: May be reduced by 5-10 years if untreated.
Treatment: Strict diet control, managing diabetes/cholesterol, quitting alcohol, and medications to reduce liver inflammation can slow or reverse progression.
3. Liver Fibrosis (Scar Tissue Formation)
Life Expectancy: Shortened by 5-15 years if untreated.
Treatment: Lifestyle changes, avoiding alcohol, and medications can prevent further damage and improve prognosis.
4. Liver Cirrhosis (Severe Scarring & Damage)
Compensated Cirrhosis: Life expectancy of 10-12 years with proper treatment.
Decompensated Cirrhosis: Life expectancy drops to 2-5 years without a liver transplant.
Treatment: Stopping alcohol, medications, regular monitoring, and managing complications can extend life.
5. End-Stage Liver Disease (Liver Failure & Liver Cancer)
Life Expectancy: 6 months to 3 years without a liver transplant.
Treatment: Liver transplant is the only option for long-term survival.
Click here to Read A Blog- Life Expectancy with Fatty Liver Disease
Can Treatment Improve Life Expectancy?
Yes! With early diagnosis, lifestyle modifications, medical treatment, and regular monitoring, fatty liver disease can be stopped or reversed, significantly improving life expectancy.
#FattyLiver#LiverHealth#NAFLD#AFLD#LiverDisease#LiverCare#Cirrhosis#HealthyLiver#LiverTreatment#LifeExpectancy
1 note
·
View note
Text
Liraglutide and semaglutide can be used to treat NASH.
ALT/AST ratio greater than 1 is NAFLD.
Haven't listened to this in a while. Trying to get back into studying. I don't wanna😫
2 notes
·
View notes