#Nephritis
Explore tagged Tumblr posts
Text
Doctor: Do you have any questions about the exam?
Student: What was the answer of the nephritic syndrome question? We discussed among ourselves and none of the alternatives made any sense.
Doctor: Crap, it was supposed to be about nephrotic.
59 notes
·
View notes
Text


Nephritis is inflammation of the kidneys and may involve the glomeruli, tubules, or interstitial tissue surrounding the glomeruli and tubules. It is one of several different types of nephropathy. Wikipedia
0 notes
Text
Locked up in The Hospital
Nephritis confined me in the hospital during the summer break when I was in the fourth grade living in Kyoto, Japan. Although I didn’t feel so sick, the doctor ordered me to be inactive all the time. Inside a six-bed pediatric ward and a hallway between the nurse station and the hospital kitchen was the allowed portion for me to move around. When I needed to go beyond it, a nurse put me in a…

View On WordPress
#child#fear#girl#horror#hospital#Japan#Japanese#Kyoto#nephritis#nurse station#pediatric Ward#summer break
0 notes
Text
Lupine Publishers | The Early Treatment of a Bodybuilder with Symptomatic Chronic Renal Failure with Intestinal Dialysis: A New Recommendation for Intestinal Dialysis Enhancement
Abstract
Background: Dietary therapy aiming primarily at reducing the generation and accumulation of urea through protein restriction is the most important non-dialytic therapeutic intervention in the management of chronic renal failure. The use of a urea lowering agent “acacia gum” with protein restriction has been increasingly used as a new form of dietary dialysis which has been increasingly known as intestinal dialysis. Just like in other forms of dialysis, the use of conservative dietary and pharmacological measures is also necessary in intestinal dialysis.
Patients and methods: The early treatment of a bodybuilder with symptomatic chronic renal failure with intestinal dialysis is described, and the relevant literatures were reviewed with the primary of identifying the evidence that can contribute to enhancing intestinal dialysis.
Results: At about the age of 50 years (March, 2022), a professional bodybuilder who presented with progressive symptomatic uremia associated with nausea, vomiting, pruritus, and mild anemia. His weight was about 100 Kg, and before his current illness he reported that his bench press single maximum repetition was 140Kg. On the 19th of March, blood urea level was 162 mg /dL and serum creatinine was 6.2 mg /dL. Renal ultrasound confirmed the chronicity of renal failure and showed small kidneys. The conservative dietary (Acacia gum supplementation plus very low protein diet) and pharmacological managements were prescribed according to the latest published intestinal dialysis guidelines and included oral iron and folic acid capsule, and calcium carbonate. After two weeks, the patient was asymptomatic and blood urea was lowered to 126.4 mg/dL, and the hemoglobin was increased to 11g/d.
Conclusion: This is just another case to demonstrate that intestinal dialysis is effective in lowering blood urea level and improving symptoms in symptomatic chronic renal failure. There is a convincing evidence to support that the addition of essential amino acids and ketoanalogues in the management of chronic renal failure with intestinal dialysis can contribute to its enhancement.
Keywords: Symptomatic uremia; Intestinal dialysis; Ketoanalogues of essential amino acids.
Introduction
Dietary therapy aiming primarily at reducing the generation and accumulation of urea through protein restriction is the most important non-dialytic therapeutic intervention in the management of chronic renal failure. The use of a urea lowering agent “acacia gum” with protein restriction has been increasingly used as a new form of dietary dialysis which has been increasingly known as intestinal dialysis. Just like in other forms of dialysis, the use of conservative dietary and pharmacological measures is also necessary in intestinal dialysis [1-14].
Patients and methods
The early treatment of a bodybuilder with symptomatic chronic renal failure with intestinal dialysis is described, and the relevant literatures were reviewed with the primary of identifying the evidence that can contribute to enhancing intestinal dialysis.
Results
At about the age of 50 years (March, 2022), a professional bodybuilder who presented with progressive symptomatic uremia associated with nausea, vomiting, pruritus, and mild anemia. He was not havening reduction in urine output, edema or hypertension. His weight was about 100 Kg, and before his current illness he reported that his bench press single maximum repetition was 140Kg. On the 19th of March, blood urea level was 162 mg / dL and serum creatinine was 6.2 mg /dL. Urinalysis showed 2 plus albuminuria and one plus amorphous urate. Blood calcium and serum electrolytes were within normal ranges, but he had mild hyperphosphatemia with serum phosphorus of 4.9 mg/dL (Normal range 2.4-4.4mg/dL). Hemoglobin was 10.7 mg/dL (Normal ranges: 11.5-16.5 g/dL). Liver function tests were normal (Total serum bilirubin 0.8 mg/dL, Aspartate aminotransferase (SGOT) 25 iu/L, alanine aminotransferase (SPOT) 21 iu/L, alkaline phosphatase 284 iu/L).
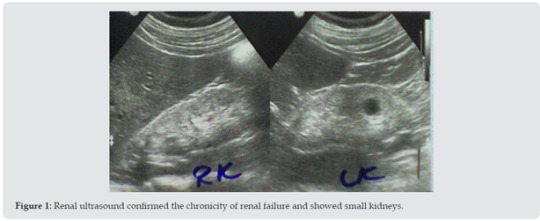
He reported history of episodes of hyperglycemia that in the case of bodybuilders is generally attributed to growth hormone administration in excessive doses. However, the patient was reluctant to provide details about the performance enhancing medications such as anabolic steroids and growth hormone, and he was not confirming or denying the use of such agent. He was simply saying that he was taking protein supplements. Renal ultrasound (Figure 1) confirmed the chronicity of renal failure and showed small kidneys (RK: 8 x 4, cortex 6 mm, LK: 8.2 x 4, cortex 6 mm). The kidneys had hyper-echoic texture with reduced cortical thickness and loss of the cortico-medullary differentiation. There were small cysts on both kidneys, not more than 1.5 cm in diameter. Abdominal ultrasound also showed small polyp in the gall bladder and mild enlargement of the prostate with a volume of 27 cm3 (Normally up to 25). The patient initially required oral prochorperazine 5 mg for two days control the nausea and vomiting, and oral antihistamine plus topical crotamiton 10% to control pruritus. The conservative dietary (Acacia gum supplementation plus very low protein diet) and pharmacological managements were prescribed according to the latest published intestinal dialysis guidelines and included oral iron and folic acid capsule, and calcium carbonate. He also received oral finasteride 5 mg daily for the prostatic enlargement. After two weeks, the patient was asymptomatic and blood urea was lowered to 126.4 mg/dL and the hemoglobin was increased to 11g/d. Ultrasound showed normal prostate size of 20 cm3. Literature review suggested that the addition of essential amino acids and ketoanalogues in the management of chronic renal failure with intestinal dialysis can contribute to its enhancement. Therefore, Ketosteril (Fresenius), was prescribed in a low initial dose of three tablets, and was ordered to be brought to the patient from Turkey.
Discussion
Until now, there is no evidence to support that high protein diet per se can cause chronic renal failure. However, nephrocalcinosis caused exogenous vitamin D intoxication was reported to cause renal failure in a bodybuilder athlete [15]. Therefore, an accurate causation of the chronic renal failure cannot be determined. Carrero et al (2020) emphasized the importance and benefits of fruits and vegetables in patients with chronic renal failure. The intake of fruits and vegetables is associated with a higher fiber intake which can cause a shift in the gut microbiota towards reduced production of uremic toxins. The intake of fruits and vegetables is also associated with lower intake phosphorus, and thus help in controlling hyperphosphataemia [16]. However, the latest published intestinal dialysis guidelines have already suggested intake of fruits and vegetables [17]. The use of Keto-analogues of essential amino acids in the management of chronic renal failure has been reported as early as the 1970s (Walser, 1978; Bauerdick and colleagues, 1978, Giovannetti et al, 1980) [18]. Bauerdick and colleagues (1978) reported the use of nitrogen-free hydroxy and keto precursers of amino acids in the treatment of patients with chronic renal failure with essential amino acid and a low-protein diet was associated with a more positive nitrogen balance [19]. In 1980, Giovannetti et al treated twenty patients with advanced chronic renal failure with a low protein diet (0.2 g/kg/day hour vegetable proteins) and essential aminoacids and ketoanalogues. They reported that treatment was associated with a favorable outcome [20]. In 1981, Barsotti et al emphasized that treatment of chronic renal failure a very low protein diet plus essential amino acids and ketoanalogues is not associated with reduction of creatinine clearance, while treatment with hemodialysis and free protein intake is associated with reduction of creatinine clearance. They treated thirty-one patients with a conventional low-protein diet, and treatment was associated with a linear reduction of creatinine clearance. A thirteen patient treated with hemodialysis experienced significantly accelerated decline of creatinine clearance. However, only one of a twelve patients treated with a very low protein diet supplemented plus essential amino acids and ketoanalogues, experienced continued a continued reduction in creatinine clearance [21].
Mitch and colleagues (1982) described the treatment of 9 patients who severe chronic renal failure (mean glomerular filtration rate 4.8 ml/min; mean serum creatinine 11.3 mg/dl). They were treated with protein restriction (22.5 g daily of mixed quality protein) plus essential amino acids and keto-analogues of essential amino acids including tyrosine, ornithine, and a high proportion of branched-chain ketoacids, and very little methionine. Phenylalanine and tryptophan were not provided. One month of treatment was associated with significant lowering of serum urea nitrogen. Hyperphosphatemia which was observed in three patients, improved. Treatment was not associated with side effects. The treatment precluded the need for dialysis in patients with severe chronic renal failure who would otherwise need dialysis [22]. In 1983, Barsotti et al described the treatment of 48 patients with chronic uraemia for a maximum of 36 months with low protein diet plus essential amino acids and keto-analogues. Ten patients experienced reduction of renal function and required dialysis.
Eight patients experienced difficulties in complying with treatment and also required dialysis. Three died for causes that are not directly related to renal failure. 27 patients continued with treatment without important reduction in renal function, and enjoyed satisfactory subjective and objective states without evidence of protein malnutrition or unwanted effects [23]. In 1985, Barsotti et al reported that the treatment of men who had uremia with a low protein diet plus essential amino acids and ketoanalogues was associated with restoration of testosterone levels in blood [24]. In 1985, Ciardella et al described the treatment of eighty-five patients with chronic renal failure with a vegetarian low-protein, low-phosphorus diet plus essential amino acids and ketoanalogues. Treatment was associated with marked reduction of serum triglycerides in the 61 men, but the reduction was not significant in woman. When the patients were later treated by maintenance hemodialysis without dietary restrictions, the experienced elevations in serum triglycerides levels which was attributed to the loss of the effect of the dietary restriction on uremic male hypogonadism [25].
Conclusion
This is just another case to demonstrate that intestinal dialysis is effective in lowering blood urea level and improving symptoms in symptomatic chronic renal failure. There is a convincing evidence to support that the addition of essential amino acids and ketoanalogues in the management of chronic renal failure with intestinal dialysis can contribute to its enhancement.
Conflict of interest
None.
For more Lupine Journals please click here: https://lupinepublishers.com/index.php
For more Journal of Urology & Nephrology Studies articles please click here: https://lupinepublishers.com/urology-nephrology-journal/index.php
#lupine publishers#articles#urology#submission#lupine journals#journal of urology & nephrology studies#open access journals#nephritis#nephrology#juns
0 notes
Text
Causes of kidney pain
Pain in the kidneys or in one kidney can be a sign of many diseases. The most important of them include: Renal colic ( nephrolithiasis ) Nephritis Hydronephrosis Kidney cyst Kidney cancer Renal colic Stones or deposits in the urinary tract are what cause renal colic. Urine cannot freely flow because the ureters are no longer open. Renal colic is characterised by the following…
View On WordPress
1 note
·
View note
Text
Hello, my loves 💕.
To be frank, life has been kicking my ass. Sorry, I’ve been MIA. Your girl is just tired and I haven’t had the urge to write anything lately. This has been an…eventful year. Hell, to be honest, it's been an eventful couple of years. Grateful and thankful to be here. Never get that twisted. Life has been smacking me upside the head for quite some time though. All I’ve wanted to do lately is curl up and read.
I’ve also started a bookstagram and booktok, so that’s been getting a lot of my attention as well. I wish I could put into words how I'm feeling mentally and physically but I'm too tired😆😩.
As soon as this lupus flare eases up. Once I don’t have so much brain fog. Maybe I’ll have a desire to write, but until then I hope you all continue to read and engage with the stories available on my masterlist💜.
Honestly, let me be transparent for a moment. I think I can speak for several Tumblr writers. I look at the notes on some of these amazing fics that I’ve read and I'm like, “What the hell? Where are the reblogs and comments?” I’ll say it over and over. The love button is cool, but it’s the bare minimum for that writer. The notes are not matching the constant requests in their asks. That's just the truth🤷🏾♀️. The engagement is just not the same. When we bring it up. Were told to get over it. Mind you this ish is free and we've invested our time creating something that brings joy and entertainment. Engagement shouldn't be so hard to come by. If the facts make you feel a way, ask yourself why that is.
Anywho let me get off that soapbox. I just wanted to drop in and give you all a life update and explain my absence. I hope all my beautiful lovelies are doing okay. To those who aren’t, please know it’s okay to not be okay. You’ll get through it. Just keep the faith. Love you my babies🥹💖.

Tagging a few lovelies so that they get the lovin’ I came to drop off😆💖:
@astoldbychae @darqchilddaydreamz @ravennaortiz @rio-reid-whoreee @percosim @lovedlover @jannavaire @sunshine-flower @phoenixhalliwell @kyletogaz @nobodygetsza @1andonlytashae @novaniskye @thebumbqueen @captainwithoutmakingitlove @kinkiicoils @wroteitbutneverwatchedit @bisexuallyattractivebitch @minton131 @thirtysomethinganduncensored @starrynite7114 @fineanddandy @withmyteeth @prettyyybrownroundd
*if I forgot to tag you sorry in advance. Mama has a lot of babies😆🥰.*
#berberriescorner#checking in#i love my mutuals😍#life with lupus#lupus nephritis#systemic lupus erythematosus#lupus problems#brain fog’s a bish#the biggest bish#i need a nap#slightly depressed#maybe majorly#gotta shake this ish off#i miss yall#writer probs#these books always got me stuck#book boyfriends do it better
48 notes
·
View notes
Text
trying to find any sort of lupus experience on social media is really just
🎶I'm all alone, there's no one here beside me🎶
#I've asked in every disability discord server for lupus nephritis experiences#zero zilch no one nothing
9 notes
·
View notes
Text

little lady
#lupus#lupus warrior#systemic lupus erythematosus#lupusawareness#lupus nephritis#art#illustration#sketch#procreate#disability#disabled#disabilties#chronic illness#arthritis#chemotherapy#doodle#sketchbook#persona#oc#sona
45 notes
·
View notes
Text
A diagnosis
After ten years of being a medical mystery, I was given hope for a diagnosis. Blood tests came back showing positive for ANA which points us towards autoimmune disease.
With a family history of Lupus and Rheumatoid Arthritis, it's not far-fetched to agree. I will still search for a second opinion on my blood work, but I am happy to at least have a direction to move in.
#chronic illness#chronic migraine#migraine#chronic pain#chronic fatigue#invisible illness#lupus#systemic lupus erythematosus#lupus nephritis
17 notes
·
View notes
Text
Hey vaccinate your fucking pets
#watched a dog die of lyme nephritis over several weeks#never got lyme vaccinated#he was a real young golden retriever#this could have been prevented#vet tech life#animal death#by 'watched' i mean we referred them to emergency#then read the reports as she took the dog to several specialists and whatnot until he had to be put down#so now she's spent thousands of dollars and her dog is dead#rather than a single vaccine + prevention every year
7 notes
·
View notes
Text
0 notes
Text
The market for lupus nephritis, which was valued at USD 2.02 billion in 2023, is anticipated to expand at a yearly rate of 6.8%. By 2030, the estimated revenue is expected to have grown by around 3.21 billion USD.
0 notes
Text
Lupine Publishers | Briefly about The Ureter

Abstract
Every man has two kidneys. Each kidney has a ureter, which drains urine from a central collection point into the bladder. From the bladder, urine is excreted through the urethra from the body through the penis in men and the vulva in women. The most important role of the kidneys is to filter metabolic waste products and excess salt and water from the body and help remove them from the body. The kidneys also help regulate blood pressure and make red blood cells.
Keywords: Kidney; Obstruction; UTI; Injury
Introduction
The ureters are tubular structures responsible for the transportation of urine from the kidneys to the bladder. The length ranges from 22 to 30 cm, and they have a wall made up of multiple layers. The innermost layer is made up of transitional epithelium, surrounded by the lamina propria, which is a connective tissue layer. These two layers make up the mucosal lining. The next layer is made of smooth muscle that, as mentioned previously, is continuous with that of the calyces and the renal pelvis. However, one slight difference is that within the ureter, the smooth muscle layer is divided into an inner longitudinal and an outer circular layer. These muscular layers allow peristalsis of urine. The outermost layer is the adventitia, which is a thin layer enveloping the ureter, its blood vessels, and lymphatics. The ureter is often divided into three segments: the upper (proximal), middle, and lower (distal) segments. The upper segment starts from the renal pelvis to the upper border of the sacrum. The middle segment is the part between the upper border and lower border of the sacrum. The lower segment is from the lower border of the sacrum to the bladder.
Anatomy
Each ureter lies posterior to the renal artery and vein at the ureteropelvic junction [1]. They then descend anterior to the psoas major muscle and the ilioinguinal nerves, just anterior to the tips of the lumbar transverse vertebral processes. Approximately a third of the way down, the ureters are crossed by the gonadal vessels. They then cross the bifurcated common iliac arteries and run along the anterior border of the internal iliac artery toward the bladder, which it pierces in an oblique manner. It is this oblique entry of the ureter into the bladder, the intramural segment of the ureter that acts as a nonreturn valve preventing vesicoureteric reflux. This valve can be congenitally defective such as that seen in those with short intramural segments, or rendered ineffective as a result of injury, such as surgery or disease, all of which leads to reflux. Many congenital abnormalities of this oblique tunnel are seen in association with a duplex kidney and ureterocoele. In its lower third, the ureters pass posterior to the superior vesical branch of the internal iliac artery also called ‘umbilical artery’. On the right side, the ureter is related anteriorly to the second part of the duodenum, caecum, appendix, ascending colon, and colonic mesentery. The left ureter is closely related to the duodenojejunal flexure of Treitz, descending and sigmoid colon, and their mesenteries.
Obstruction
The diagnosis of obstruction cannot be made on the basis of haematological or biochemical tests [2]. There may be evidence of impaired renal function, anaemia of chronic disease, haematuria or bacteriuria in selected cases. Ultrasonography is a reliable means of screening for upper urinary tract dilatation. Ultrasound cannot distinguish a baggy, low-pressure, unobstructed system from a tense, high pressure, obstructed one, so that falsepositive scans are seen. A normal scan usually but not invariably rules out urinary tract obstruction. If obstruction is intermittent or in its very early stages, or if the pelvicalyceal system cannot dilate owing to compression of the renal substance, for example by tumour, the ultrasound scan may fail to detect the problem. Radionuclide studies may be helpful. If obstruction has resulted in prolongation of the time taken for urine to travel down the renal tubules and collecting system (obstructive nephropathy) this can be detected by nuclear medicine techniques and is diagnostic. Conversely, in the presence of a baggy, low-pressure, unobstructed renal pelvis and calyceal system, nephron transit time will be normal, but pelvic transit time prolonged. If doubt exists, frusemide may be administered; satisfactory ‘washout’ of radionuclide rules out obstruction and vice versa. Relative uptake of isotope may be normal or reduced on the side of the obstruction and peak activity of the isotope may be delayed. In general, absence of uptake of radiopharmaceutical indicates renal damage sufficiently severe to render correction of obstruction unprofitable. Isotope studies may thus provide a guide to the form of surgery to be undertaken. Antegrade pyelography and ureterography are extremely useful in defining the site and cause of obstruction and can be combined with drainage of the collecting system by percutaneous needle nephrostomy. The risk of introducing infection is less than with retrograde ureterography in which technique instrumentation of the bladder is followed by injection of contrast into the lower ureter or ureters. This technique is indicated if antegrade examination cannot be carried out for some reason or if there is a possibility of dealing with ureteric obstruction from below at the time of examination. Ureteral obstruction occurs in 2–10% of renal transplants and often manifests itself as painless impairment of graft function due to the lack of innervation of the engrafted kidney [3]. Hydronephrosis may be minimal or absent in early obstruction, whereas low-grade dilatation of the collecting system secondary to edema at the ureterovesical anastomosis may be seen early post-transplantation and does not necessarily indicate obstruction. A full bladder may also cause mild calyceal dilatation due to ureteral reflux and repeat ultrasound with an empty bladder should be carried out. Persistent or increasing hydronephrosis on repeat ultrasound examinations is highly suggestive of obstruction. Renal scan with furosemide washout may help support the diagnosis, but it does not provide anatomic details. Confirmation of the obstruction can be made by retrograde pyelogram but the ureteral orifice may be difficult to catheterize. Although invasive, percutaneous nephrostomy tube placement with antegrade nephrostogram is the most effective way to visualize the collecting system and can be of both diagnostic and therapeutic value.
Blood clots, technically poor reimplant, and ureteral sloughing are common causes of early acute obstruction after transplantation. Ureteral fibrosis secondary to either ischemia or rejection can cause intrinsic obstruction. The distal ureter close to the ureterovesical junction is particularly vulnerable to ischemic damage due to its remote location from the renal artery, hence compromised blood supply. Although uncommon, ureteral fibrosis associated with polyoma BK virus in the setting of renal transplantation has been well-described. Ureteral kinking, lymphocele, pelvic hematoma or abscess, and malignancy are potential causes of extrinsic obstruction. Calculi are uncommon causes of ureteral obstruction. Definitive treatment of ureteral obstruction due to ureteral strictures consists of either endourologic techniques or open surgery. Intrinsic ureteral scars can be treated effectively by endourologic techniques in an antegrade or retrograde approach. An indwelling stent may be placed to bypass the ureteral obstruction and removed cystoscopically after 2–6 weeks. An antegrade nephrostogram should be performed to confirm that the urinary tract is unobstructed prior to nephrostomy tube removal. Routine ureteral stent placement at the time of transplantation has been suggested to be associated with a lower incidence of early postoperative obstruction. Extrinsic strictures, strictures that are longer than 2 cm, or those that have failed endourologic incision, are less likely to be amenable to percutaneous techniques and are more likely to require surgical intervention. Obstructing calculi can be managed by endourologic techniques or by extracorporeal shock wave lithotripsy.
UTI
Urinary tract infections (UTIs) are the most common bacterial infection in the paediatric population [4]. The incidence is initially higher in boys, affecting up to 20.3% of uncircumcised boys and 5% of girls at the age of 1. There is a gradual shift, with UTIs affecting 3% of prepubertal girls and 1% of prepubertal boys. The National Institute for Health and Care Excellence (NICE) have defined a recurrent UTI as two or more episodes of pyelonephritis, or one episode of pyelonephritis plus one or more episodes of cystitis, or three or more episodes of cystitis. Diagnostic investigations include urinalysis, which may require suprapubic bladder aspiration or bladder catheterisation in infants. A urine culture and microscopy should be carried out if there is evidence of infection. The role of further imaging is to differentiate between an uncomplicated and complicated UTI, but should also be considered in those with haematuria. A UTI is complicated in the presence of an abnormal urinary tract including upper tract dilatation, atrophic or duplex kidneys, ureterocoele, posterior urethral valves, intestinal connections, and vesico-ureteric reflux (VUR). NICE guidelines recommend an urgent ultrasound of the urinary tract for all those with recurrent UTI under six months. For children six months and older, NICE in the UK recommends an ultrasound within six weeks of the latest infective episode. All children with recurrent UTIs should be referred to a paediatric specialist and have a dimercaptosuccinic acid (DMSA) scan within four to six months of an acute infection to evaluate for renal scarring. European Association of Urology (EAU) guidelines recommend a renal tract ultrasound in febrile UTIs if there is no clinical improvement, as an abnormal result is seen in 15% of these patients. Routinely repeating a urine culture in children treated with an antibiotic based on previous urine culture susceptibilities is not necessary [5]. Approximately 10%–30% of children develop at least one recurrent UTI, and the recurrence rate is highest within the first 3 to 6 months after a UTI. Renal scarring increases with an increasing number of febrile UTIs and with delayed treatment; therefore, parents should be counseled regarding the high risk of recurrent UTI and seek prompt evaluation for subsequent febrile illnesses in their child. Children who had a febrile UTI should routinely have their height, weight, and blood pressure monitored by their primary care provider. Children with significant bilateral renal scars or a reduction of renal function warrant long-term follow-up for the assessment of hypertension, renal function, and proteinuria.
Colic
Urolithiasis represents the commonest cause of acute ureteric colic, with calcium stones accounting for approximately 80% of cases [6]. Ureteric calculi have a prevalence of approximately 2–3% in Caucasian populations, with a lifetime risk of 10–12% in males and 5–6% in females. They are more common in developed countries, in men, in those with a positive family history, and in those with inadequate daily water intake. Ureteric colic typically presents with acute severe loin pain – which patients often describe as unrelenting despite a number of postural changes – and haematuria. Vomiting is often a feature of severe uncontrolled pain. Most patients with renal colic present because of severe uncontrolled pain and do not have signs of overt sepsis. Opiates are commonly given, although diclofenac sodium has been shown to be at least as effective for pain relief, particularly via rectal administration. Despite initial concerns, diclofenac sodium therapy has not been associated with renal toxicity in patients with preexisting normal renal function. Fever, tachycardia, tachypnoea and hypotension suggest sepsis secondary to an infected, obstructed kidney, which represents a life-threatening condition. Immediate management comprises prompt resuscitation, establishment of intravenous (IV) antibiotics, rapid diagnosis and decompression of the obstructed renal system, usually by ultrasound-guided percutaneous nephrostomy. Early involvement of urology and critical care services is essential in such patients. The management of ureteric calculi depends upon factors relating to the stone and the patient. Pre-eminent stone factors are size and site. It has been shown that 71–98% of stones <5 mm will pass spontaneously, whereas rates of spontaneous passage for stones >7 mm are low. Stone passage is also related to location in the ureter; 25% of proximal, 45% of mid and 75% of distal ureteric stones will pass spontaneously. In patients in whom stone passage is deemed likely, a trial of conservative management should be employed. Exceptions include patients with a functional or anatomical solitary kidney, bilateral ureteric obstruction, uncontrolled pain, or the presence of infection. Patients without contraindications should receive diclofenac sodium 50 mg tds, which has been shown to reduce the frequency of recurrent renal colic episodes. Recent evidence suggests that additional treatment with smooth muscle relaxants is associated with increased rates of stone passage over analgesics alone. A recent meta-analysis of studies using either nifedipine or tamsulosin, showed an approximate 65% greater chance of stone passage when such agents were used compared with equivalent controls. Intervention is generally reserved for large stones (>7 mm), conservative treatment failures and those with contraindications to a watchful waiting approach. Options include extracorporeal shockwave lithotripsy and retrograde ureteroscopic stonefragmentation.
A stone can traverse the ureter without symptoms, but passage usually produces pain and bleeding [7]. The pain begins gradually, usually in the flank, but increases over the next 20–60 min to become so severe that narcotics may be needed for its control. The pain may remain in the flank or spread downward and anteriorly toward the ipsilateral loin, testis, or vulva. A stone in the portion of the ureter within the bladder wall causes frequency, urgency, and dysuria that may be confused with urinary tract infection. The vast majority of ureteral stones <0.5 cm in diameter pass spontaneously. Helical computed tomography (CT) scanning without radiocontrast enhancement is now the standard radiologic procedure for diagnosis of nephrolithiasis. The advantages of CT include detection of uric acid stones in addition to the traditional radiopaque stones, no exposure to the risk of radiocontrast agents, and possible diagnosis of other causes of abdominal pain in a patient suspected of having renal colic from stones. Ultrasound is not as sensitive as CT in detecting renal or ureteral stones. Standard abdominal x-rays may be used to monitor patients for formation and growth of kidney stones, as they are less expensive and provide less radiation exposure than CT scans. Calcium, cystine, and struvite stones are all radiopaque on standard x-rays, whereas uric acid stones are radiolucent.
Ureteral Stone Disease
Nephrolithiasis occurs with an estimated overall prevalence of 5.2% and there is evidence that stone disease is on the rise [8]. However, many stones in the kidney go undetected because they cause no symptoms or obstruction. Conversely, ureteral stones rarely remain silent, and they have greater potential for causing pain and obstruction. As such, ureteral stones that fail to pass spontaneously require surgical intervention. Although the introduction of medical expulsive therapy (MET, the use of pharmacological agents to promote spontaneous stone passage) has changed the natural history of ureteral stone disease, not all ureteral stones respond to MET. Indications for surgical intervention to remove ureteral calculi include stones that are unlikely or fail to pass spontaneously with or without MET, stones that cause unremitting pain regardless of the likelihood of spontaneous passage, stones associated with persistent, high-grade obstruction, stones in patients with an anatomically or functionally solitary kidney or in those with renal insufficiency or stones in patients for whom their occupation or circumstances mandate prompt resolution (i.e. pilots, frequent travelers, etc.). Once the decision has been made to intervene surgically for a patient with a ureteral stone, treatment options include shock-wave lithotripspy, ureteroscopy, percutaneous antegrade ureteroscopy and open or laparoscopic ureterolithotomy. Although special cirumstances may dictate the application of percutaneous antegrade ureteroscopy or ureterolithotomy (large, impacted stones, stones in patients with urinary diversions or stones that fail less invasive approaches), the two most widely practiced treatment modalities for ureteral stones are shock-wave lithotripsy (SWL) and ureteroscopy (URS). Both are associated with high success rates and low morbidity. However, the optimal treatment for ureteral stones remains controversial because of passionate advocates on both sides of the controversy. Proponents of SWL cite the noninvasiveness, high patient satisfaction and ease of treatment, while URS advocates favor the short operative times, high success rates and short time interval to become stone free.
Cystoscopy
Cystoscopic examination of urethra and bladder should be systematic [9]. The female urethra is only 2.5–4 cm long. Urethral mucosa should be examined for strictures, diverticular opening, or polyps, and the bladder neck is visualised as scope enters and exits the bladder. Base and trigone of the bladder are initially inspected. Trigone lies proximal to the bladder neck; it is the triangular area bounded by the inter-ureteric ridge and the bladder neck at the base of the bladder. One of the most common features of the trigone is squamous metaplasia, present in up to 50% of the women. It is a benign feature with no malignant potential. In staging for cervical cancer, when imaging suggests stage 3 or 4 disease, cystoscopy is indicated. The bladder base and trigone appearance such as bullous edema, inflammatory changes, or infiltration has to be documented, and in case of infiltration, biopsy should be part of the evaluation. Ureteric orifices are slit-like openings easily identifiable by the presence of efflux on either side of the inter-ureteric ridge. The ureteral orifices location, number, nature of ureteric efflux (clear, blood stained), and any anatomical distortion is noted. In a woman with anterior vaginal wall prolapse or an underlying cervical mass, identification of trigone or ureteric orifices may be difficult. In such cases, placing a finger inside the vagina and elevating the bladder base with a finger will be helpful. Blood stained ureteric efflux denotes upper tract pathology and further assessment of the ureter and kidneys is indicated, either by ultrasound or a CT scan of the kidneys, ureters, and bladder (CT KUB). In intra-operative or postoperative ureteral integrity assessment, presence of just ureteric peristalsis does not rule out ureteral injury. Checking for ureteric efflux after administration of methylthionium chloride or indigo carmine (5ml) IV is effective in confirming ureteral patency.
Injury
Most ureteral injuries are iatrogenic in the course of pelvic surgery [10]. Ureteral injury may occur during transurethral bladder or prostate resection or ureteral manipulation for stone or tumor. Ureteral injury is rarely a consequence of penetrating trauma. Unintentional ureteral ligation during operation on adjacent organs may be asymptomatic, though hydronephrosis and loss of renal function results. Ureteral division leads to extravasation and urinoma. If the ureteral injury is not recognized at surgery, the patient may complain of flank and lower abdominal pain on the injured side. Ileus and pyelonephritis may develop. Later, urine may drain through the wound (or through the vagina following transvaginal surgery) or there may be increased output through a surgical drain. Wound drainage may be evaluated by comparing creatinine levels found in the drainage fluid with serum levels; urine exhibits very high creatinine levels when compared with serum. Intravenous administration of 5 mL of indigo carmine causes the urine to appear blue-green; therefore, drainage from an ureterocutaneous fistula becomes blue, compared to serous drainage. Anuria following pelvic surgery not responding to intravenous fluids may rarely signify bilateral ureteral ligation or injury. Peritoneal signs may occur if urine leaks into the peritoneal cavity.
Conclusion
The ureter starts from the renal pelvis, descends down the retroperitoneal space of the abdominal cavity and enters the pelvis, where it ends by pouring into the urinary bladder. Therefore, it distinguishes the abdominal and pelvic part. The boundary between these parts is the so-called terminal line. When entering the pelvic cavity, the ureter forms a border curve and in this narrowed part the kidney stone can be stopped. The curvature of the ureter is projected on the anterior abdominal wall in the area of the Hale topographic point. Urinary tracts pass through the bladder wall obliquely. When the bladder wall is stretched, the fold of its mucosa acts as a valve and prevents the return of urine to the ureters and the possible spread of infection from the bladder to the kidneys.
For more Lupine Journals please click here: https://lupinepublishers.com/index.php
For more Journal of Urology & Nephrology Studies articles please click here: https://lupinepublishers.com/urology-nephrology-journal/index.php
#nephrology#lupine journals#open access journals#journal of urology & nephrology studies#nephritis#submission#articles#juns#lupine publishers#urology
0 notes
Text

LUPUS NEPHRITIS
Lupus stands as a prominent name amongst the myriad systemic chronic inflammatory conditions resulting from an individual's immune system attacking their own tissues.
The condition derives its name from the Latin word for wolf because of the characteristic butterfly-shaped rash stretching across both cheekbones that appear like a wolf bite.
Lupus is incurable, the clinical presentation is variable with occasional debilitating flares and complications that could be potentially fatal if left untreated.
Among other organs, Kidneys are a prime target here causing inflammation and patchy progressive scarring in the kidney tissue in around 20-63% of all Lupus cases. This entity is clinically called Lupus Nephritis - a major cause of morbidity & mortality globally.
As a portal dedicated to demystifying nuggets in nephrology, let us walk you through the what-why-how Lupus Nephritis by linking to a lucid article in our website as below:
👇🏻
P.S. : We are mindful of the existence of individual variations that apply to any medical condition. The article attempts to offer a comprehensive insight into the commonly encountered clinical picture in Lupus nephritis.
#chronic kidney disease#kidney#kidney disease#health#health blog#allthingskidney#kidneydisease#kidneyhealth#kidney failure#lupus nephritis#systemic lupus erythematosus#lupus#kidneydiseaseawareness#kidney treatment
0 notes
Text
Conclusions:
This study confirms previous case reports and epidemiologic studies of end-stage renal disease that found an association between kidney disease and exposure to silica.
The epidemiologic data are conflicting on the mechanism by which silica causes kidney disease and are compatible with silica being able to cause kidney disease by both an autoimmune and direct nephrotoxic effect.
Chronic kidney disease should be considered as a complication of silicosis.
#Chronic Kidney Disease#silica exposure#silica nephritis#CKD#autoimmune diseases#silicosis#pneumoconiosis
0 notes