#NLR proteins
Explore tagged Tumblr posts
Text
youtube
#NLRP3 inflammasome#multiple myeloma#inflammation#cytokine release#tumor microenvironment#IL-1β#IL-18#pro-inflammatory cytokines#tumor progression#immune suppression#bone resorption#MM pathogenesis#apoptosis resistance#plasma cells#caspase-1#ASC#NLR proteins#immunotherapy#chronic inflammation#therapeutic strategies.#Youtube
0 notes
Text
Madhuprakash, J., Toghani, A., Contreras, M.P., Posbeyikian, A., Richardson, J., Kourelis, J., Bozkurt, T.O., Webster, M.W., and Kamoun, S. 2024. A disease resistance protein triggers oligomerization of its NLR helper into a hexameric resistosome to mediate innate immunity.

Check the threads by Madhu @JMadhuprakash and AmirAli @amiralito_ on the helper NLR inflammasome-like structure. Animation and much more by Michael @WebsterMichael0 #NLRbiology #OpenPlantNLR https://x.com/KamounLab/status/1803773797130018948
3 notes
·
View notes
Text
Ancient mediators of innate immunity
Bacteria can become infected by bacteriophages and have developed a range of anti-phage immune pathways to counteract these infections. These pathways are often multi-gene systems encoding proteins that sense and inhibit virion production, and efforts to catalog anti-phage signaling systems in bacteria have revealed that some of these genes share homology with components of eukaryotic immune systems. This suggests that eukaryotes horizontally acquired some innate immune genes from bacteria.
Many components have been identified as homologous between bacteria and humans, including bacterial cyclic-oligonucleotide-based anti-phage signaling systems (CBASS) with human cGAS and STING, and bacterial Viperins and Gasdermins with human Viperin and Gasdermin D. However, SBGrid member Aaron Whiteley and other researchers have been searching for other potential components in bacterial anti-phage signaling systems which could be homologous to immune signaling elements in humans. The researchers demonstrate that bacteria express anti-phage proteins containing a NACHT module, which is an important element of the animal nucleotide-binding domain leucine-rich repeat containing gene family called NLRs. These NACHT proteins are widespread in bacteria and contain a C-terminal sensor, central NACHT module, and N-terminal effector component, acting against both DNA and RNA bacteriophages.
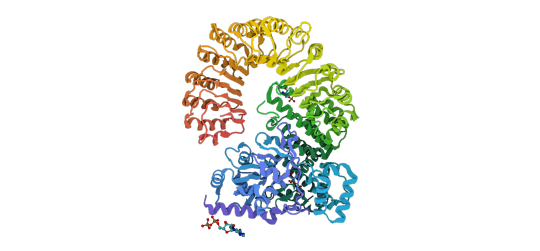
Above: Previously reported structure of NLR family CARD domain-containing protein 4. CC BY SBGrid.
Importantly, they determined that mutations in human NLR which lead to stimulus-independent activation of downstream signaling also activate bacterial NACHT proteins, suggesting that the bacterial and human systems share similar signaling mechanisms. This work identifies NACHT module-containing proteins as ancient innate immune signaling elements and expands our knowledge of homology between bacterial anti-phage immune pathways and eukaryotic immune systems.
Read more about this work in Cell.
#cell#immunology#science#nature#microbiology#sbgrid#sbgrid member research#biomedical research#Biomedical Science
7 notes
·
View notes
Text
The Best Doctor in the World

The Best Doctor in the World
Doctors are the elemental keystone for any country’s healthcare system. It is proved that an established education system in a country is always directly proportional to having qualified doctors. The profession of doctor is one of the noblest occupations in the world. Doctors are respected and considered as they have divine qualities.
The world is pleased to have the wonderful and best doctors. Now, who is the best doctor in the world? So here is the answer Patrick Soon-Shiong is reflected as one of the best doctors in the world. Let’s explore the life journey of the best doctor.
Who is Patrick Soon-Shiong?
Patrick Soon-Shiong, M.D., a physician, surgeon, scientist, inventor, technologist, and philanthropist, has dedicated his career to the fundamental biology driving life-threatening diseases and transforming these discernments into medical innovations with global impact.
Along with his devotion towards his career as a doctor, he also performs his duties as Chairman and Chief Executive Officer of NantWorks, a network of businesses with extensive knowledge of many complicated industries, including physics, data, AI, medical science, communications, and mobility.
Soon-Shiong’s Journey: From South Africa to Medical Innovation
Patrick Soon-Shiong was born on July 29, 1952, in Port Elizabeth, Union of South Africa to Chinese immigrant parents who migrated from China during the Japanese occupation in World War II. His parents were Hakka originally from Mexican District in Guangdong province.
Eventually, Soon-Shiong received a bachelor’s degree in medicine (MBBCh) at the University of Witwatersrand and graduated with flying colors, the fourth in a group of 200 students. After that, he continued his education at the University of British Columbia, graduating with a master’s degree in 1979.
The American College of Surgeons, the Royal College of Physicians and Surgeons of Canada, and the American Association of Academic Surgery all gave him research grants.
Patrick Soon-Shiong: A trailblazing Surgeon
A total of 30 years of Dr. Soon-Shiong’s working experience belongs to medical revolutions. All over Dr. Soon-Shiong’s career, he has introduced therapies for diabetes and cancer, recognized himself as the publisher of over 100 scientific papers, and has taken over 675 patients worldwide for innovative advancements passing over a multitude of fields of medicine, technology, and artificial intelligence.
He was the one who performed UCLA’s first whole-organ pancreas transplant and the world’s first enclosed islet cell transplant in Type 1 diabetic patients he performed this transplant as an Assistant Professor at UCLA in 1993.
He worked at NASA to further his studies in stem cells and nanotechnology during the early 1990s, conducting projects related to the space shuttle program. He was in charge of the California Nanosystems Institute (CNSI) while he was at UCLA.
To incorporate supercomputing data centers and to devise an augmented intelligence for genomic sequencing, NantOmics’ boss, Dr Soon-Shiong, bought the National LambdaRail (NLR) in 2011. This Layer 1 network was further developed by Dr. Soon-Shiong as MOX Networks in 2013.
Patrick Soon-Shiong: Developer of Abraxane
Dr. Soon-Shiong was also the developer of Abraxane, a very pioneered drug, in 1995. Abraxane was the first human protein (albumin) nanoparticle invented to activate a specific receptor on the blood vessels that supply the tumor and this drug was purposed to transform the tumor’s microenvironment and activate the immune system.
Abraxane has been used in different types of cancers inclusive of metastatic breast cancer since 2005, cell lung cancer since 2012, and pancreatic cancer since, 2013 as approved by the FDA.
Patrick Soon-Shong: Business Career
Further on to his medical and scientific career, Soon-Shiong also emerged as an active businessman during the late 1990s, and since the early 2010s, he has grown as an investor.
Already in the period from 1997 up to 2010, Dr. Soon-Shiong was identified as the founder, chairman, and chief executive officer of two public pharmaceutical companies namely Abraxis BioScience, Inc. (NASDAQ: ABII) and American Pharmaceutical Partners Inc. (NASDAQ: APPX) Vista, the parent company of APPX, have inked a biologic supply agreement.
In addition, Dr. Soon-Shiong is the creator of NantWorks, LLC, a business firm whose primary objective is to establish a next-generation pharmaceutical development network and transformative global health information for the safe communication of genetic and medical data, tackling issues of climate change, and changing the characteristics of new media.
The San Diego Union-Tribune and the Los Angeles Times were purchased by Dr. Soon-Shiong in 2018. The process was put into law through the 21st Century Cures Act, and the committee carrying out this policy is the Health Information Technology Advisory Committee, which has a primary duty to provide the government and President with advice on relevant health IT policies.
He was nominated to this committee too. Before this, Dr. Soon-Shiong was a member of Bank of America’s Global Advisory Board and co-chair of the CEO Council for Health and Innovation at the Bipartisan Policy Center.
Patrick Soon-Shiong: Awards and Achievements
Many reputable, prestigious, and honorable awards have been achieved by Soon-Shiong throughout his career. Some noticeable awards include the Ellis Island Medal of Honor, the National Medal of Technology and Innovation, the Horatio Alger Award, and the Ernst & Young Entrepreneur of the Year Award. He has also been acknowledged as one of the world’s billionaires and one of the most influential people in healthcare.
Read More:- Taylor Swift: Redefining Pop Music One Album at a Time
0 notes
Text
Le sindromi autoinfiammatorie: entità prima misteriose, ora hanno un agente responsabile e possibili soluzioni
Le malattie autoinfiammatorie sistemiche (SAID) colpiscono principalmente la risposta immunitaria innata e sono entità patologiche distinte, sebbene possano sovrapporsi in qualche modo alle malattie autoimmuni. Negli ultimi anni lo spettro dei SAID è stato ampliato. I recettori simili al dominio di oligomerizzazione nucleotidica (NOD) (NLR) sono un gruppo specializzato di proteine intracellulari…

View On WordPress
#autoimmunità#citochine#colite cronica#fattore di trascrizione#flogosi cronica#infiammazione#inflammasoma#interleuchina-1#malattia di Crohn#NLRP12#NLRP3#recettore Toll#sindrome autoinfiammatoria#sistema immunitario
0 notes
Text
Free article: A subset of NLRs function to mitigate overzealous pro-inflammatory signaling produced by NF-κB activation. Under normal pathophysiologic conditions, proper signaling by these NLRs protect against potential autoimmune responses. These NLRs associate with several different proteins within both the canonical and noncanonical NF-κB signaling pathways to either prevent activation of the pathway or inhibit signal transduction. Inhibition of the NF-κB pathways ultimately dampens the production of pro-inflammatory cytokines and activation of other downstream pro-inflammatory signaling mechanisms. Dysregulation of these NLRs, including NLRC3, NLRX1, and NLRP12, have been reported in human inflammatory bowel disease (IBD) and colorectal cancer patients, suggesting the potential of these NLRs as biomarkers for disease detection. Mouse models deficient in these NLRs also have increased susceptibility to colitis and colitis-associated colorectal cancer. While current standard of care for IBD patients and FDA-approved therapeutics function to remedy symptoms associated with IBD and chronic inflammation, these negative regulatory NLRs have yet to be explored as potential drug targets. In this review, we describe a comprehensive overview of recent studies that have evaluated the role of NLRC3, NLRX1, and NLRP12 in IBD and colitis-associated colorectal cancer.
0 notes
Text
Oooh, nice! I forgot about acronyms with numbers like that!
I have since learned that a nested acronym is called a "macronym", and the wikipedia article for that suggests "RARS" and "VITAL" as possible contenders:
VITAL -> "VHDL Initiative Towards ASIC Libraries" VHDL -> "VHSIC Hardware Description Language" VHSIC -> "Very High Speed Integrated Circuit" ASIC -> "Application-specific integrated circuit"
VITAL -> "Very High Speed Integrated Circuit Initiative Towards Application-specific integrated circuit Libraries"
Ratio: 93/5 = 18.6 (not good enough)
RARS -> "Regional ATOVS Retransmission Service" ATOVS -> "Advanced TOVS" TOVS -> "TIROS operational vertical sounder" TIROS -> "Television infrared observational satellite"
So RARS -> "Regional Advanced Television Infrared Observational Satellite Operational Vertical Sounder Retransmission Service"
Ratio: 103/4 = 25.75 (better)
There are also apparently a lot of symbols in protein naming, so e.g. the NACHT protein domain technically has a whopping ratio of 39.8, but some of the expansions aren't actually acronyms or initialisms, like HET being short for the "heterokaryon incompatibility protein" domain:
NACHT -> "NAIP, C2TA, HET-E, TEP1" NAIP -> "NLR family apoptosis inhibitory protein" NLR -> "NOD-like receptor" NOD-like -> "nucleotide-binding oligomerization domain-like" C2TA -> "class 2 major histocompatibility complex transactivator" HET -> "Heterokaryon incompatibility protein" (the -E is just a classifier, AFAICT) TEP1 -> "Telomerase protein component 1"
NACHT -> "Nucleotide-binding oligomerization domain-like receptor family apoptosis inhibitory protein, class 2 major histocompatibility complex transactivator, Heterokaryon incompatibility protein E, Telomerase protein component 1"
Ratio: 199/5 = 39.8
But it's not entirely fair to even call NACHT an acronym, since it's not actually short for "NAIP, C2TA, HET-E, TEP1", those are just common examples of things in that domain.
XHR stands for "XML HTTP Request", where XML is the "eXtensible Markup Language" and HTTP is the "Hypertext Transfer Protocol", so the full expansion of XHR is "extensible markup language hypertext transfer protocol request", so those 3 letters expand to 56 letters (62 with spaces), and this got me wondering, there must be acronyms or initialisms with an even greater ratio of "expanded length"/"unexpanded length", but apart from recursive acronyms I can't think of longer examples.
Can anyone else think of any?
270 notes
·
View notes
Photo

Prokaryotic innate immunity through pattern recognition of conserved viral proteins
The innate immune systems of animals, plants, and fungi universally use nucleotide binding oligomerization domain–like receptors (NLRs) of the STAND superfamily to detect molecular patterns common to pathogens. Gao et al. show that NLR-based immune pattern recognition is also prevalent in bacteria and archaea, something that was not known before. In particular, the authors characterized four families of NLR-like genes, finding that they are specific sensors for two highly conserved bacteriophage proteins. Upon binding to the target, these NLRs activate diverse effector domains, including nucleases, to prevent phage propagation. These findings demonstrate that pattern recognition of pathogen-specific proteins is a common mechanism of immunity across all domains of life.
0 notes
Text

Mauricio P. Contreras, Hsuan Pai et al.
The nucleotide-binding domain of NRC-dependent disease resistance proteins is sufficient to activate downstream helper NLR oligomerization and immune signaling.
Conceptual image by Andy Posbe @adnroide
3 notes
·
View notes
Text
Data variables-PCS-Covid-19 and pregnancy
The study incorporated Prospective Cohort study design. For the Prospective Cohort study, the explanatory variables, which are the exposures, would be severity levels of symptoms. These levels are separated into four subgroups of cases as asymptomatic, mild, moderate, severe(extreme). These levels can be defined based on measurements of clinical indications of Covid-19 such as leukocyte, neutrophil‐to‐lymphocyte ratio (NLR), neutrophil, lymphocyte, platelet, D‐dimer, C‐reactive protein. The response variables would be maternal and infant mortality rates, premature birth time, fetal birth weight, maternal morbidity, maternal hospitalizations during pregnancy. The maternal mortality cases in this study should only include indirect obstetric maternal mortality cases with underlying disease being exposure to Covid-19 for primary outcome. The secondary outcomes are measured based on ICD-10 codes for Pregnancy, childbirth and the puerperium provided by CDC. The explanatory variables would be distinct values rather than continuous values. All the response variables would be binary values except for premature birth time and fetal birth weight which would be continuous values.
0 notes
Text
Gut microbiota influence host immunity and metabolism during obesity. Bacterial sensors of the innate immune system relay signals from specific bacterial components (i.e., postbiotics) that can have opposing outcomes on host metabolic inflammation. NOD-like receptors (NLRs) such as Nod1 and Nod2 both recruit receptor-interacting protein kinase 2 (RIPK2) but have opposite effects on blood glucose control. Nod1 connects bacterial cell wall-derived signals to metabolic inflammation and insulin resistance, whereas Nod2 can promote immune tolerance, insulin sensitivity, and better blood glucose control during obesity. NLR family pyrin domain containing (NLRP) inflammasomes can also generate divergent metabolic outcomes. NLRP1 protects against obesity and metabolic inflammation potentially because of a bias toward IL-18 regulation, whereas NLRP3 appears to have a bias toward IL-1β-mediated metabolic inflammation and insulin resistance. Targeting specific postbiotics that improve immunometabolism is a key goal. The Nod2 ligand, muramyl dipeptide (MDP) is a short-acting insulin sensitizer during obesity or during inflammatory lipopolysaccharide (LPS) stress. LPS with underacylated lipid-A antagonizes TLR4 and counteracts the metabolic effects of inflammatory LPS. Providing underacylated LPS derived from Rhodobacter sphaeroides improved insulin sensitivity in obese mice. Therefore, certain types of LPS can generate metabolically beneficial metabolic endotoxemia. Engaging protective adaptive immunoglobulin immune responses can also improve blood glucose during obesity. A bacterial vaccine approach using an extract of the entire bacterial community in the upper gut promotes protective adaptive immune response and long-lasting improvements in blood glucose control. A key future goal is to identify and combine postbiotics that cooperate to improve blood glucose control.
0 notes
Text
Neutrophil-to-Lymphocyte ratio in diabetic neuropathy
New Post has been published on https://tattlepress.com/health/diabetes/neutrophil-to-lymphocyte-ratio-in-diabetic-neuropathy/
Neutrophil-to-Lymphocyte ratio in diabetic neuropathy

Introduction
As defective insulin secretion or impaired biological function, chronic hyperglycemia can cause damage to various tissues and systems, especially eyes, kidneys, blood vessels and nerves.1 Most diabetes patients can be divided into two types. Type 1 diabetes mellitus (T1DM), due to the absolute lack of insulin secretion, can usually be identified by serological evidence and genetic markers of islet autoimmunity. Abnormal inflammation and immune responses are associated with the development of T1DM. Recent study have shown that innate immunity and inflammatory mediators play an important and wide-ranging roles, possibly inhibiting β-cell function,2 promoting subsequent apoptotic processes, and leading to insulin resistance in surrounding tissues.
Type 2 diabetes mellitus (T2DM), the more common type, accounts for 90~95% of diabetes, due to the insulin resistance (IR) and inadequate compensatory secretory response. Factors that contribute to impaired glucose tolerance (IGT) and IR include genetic factors, environmental factors, age, obesity, and inflammation. Activation of adipose tissue may lead to the release of inflammatory cytokines associated with IR, such as TNF-α, leptin, IL-6, resistin, monocyte chemotactic protein-1 (MCP-1), angiotensin, endolipids, retinol-binding protein-4, and serum amyloid A (SAA).1,2 Inflammatory factors induce and maintain the inflammatory response and inflammatory damage during the development of diabetes.
As one of the complications of diabetes mellitus (DM), diabetic peripheral neuropathy (DPN) usually develops insidiously and gradually. It can manifest as pain, numbness, tingling, weakness, and balance disorders, leading to ulcers, gangrene, and even amputation. Some patients are asymptomatic at an early stage, which may lead to neglect of the disease. Therefore, early detection and treatment of DPN play an important role in improving disease prognosis and life quality.3 The development of DPN is related to metabolic disorders, such as oxidative stress, increased polyol flux, accumulation of glycosylated end products and lipid changes, and other metabolic abnormalities.4 To date, some hemogram derived inflammatory markers and related metabolites have been found to be associated with diabetes mellitus. Mean platelet volume (MPV) can provide important information on the course and prognosis in many inflammatory conditions.5 Red blood cell distribution width (RDW) is associated with cardiovascular disease, sepsis, and tumors.6–8 Besides, recent studies have shown that NLR and RLR can be used as systemic marker in some inflammatory conditions including cardiovascular disease, metabolic syndrome and malignancies.9–11 Both of them are novel, available, and inexpensive marker of Inflammatory status. Against this background, we aimed to study the association between the occurrence of DPN and related indicators in patients with type 1 or type 2 diabetes, and patients without DPN were followed up to investigate the predictive value of these indicators on newly diagnosed DPN.
Materials and Methods
Subjects
In this study, 225 consecutively hospitalized patients were recruited from August 31, 2018 to October 1, 2019 at the First Affiliated Hospital of University of Science and Technology of China. The inclusion criteria included a diagnosis of diabetes with or without the symptoms and signs of DPN. Diabetes was diagnosed using the revised American diabetes association standards, including fasting plasma glucose [FPG] ≥7.0mmol/L[126mg/dL] and/or postprandial 2h glucose value ≥11.1 mmol/L [200mg/dL].12 Exclusion criteria were as follows: a) a history of multiple nerves due to other causes, such as hereditary, alcoholic, metabolic, inflammatory, and toxic factors; b) a history of tumor radiotherapy and chemotherapy; c) skin damage or swelling which can interfere with nerve conduction; d) active infection and using of medicine affecting the white blood cell counts; e) Complicated hematogenous disease or rheumatic disease; f) a prior history of leg or ankle fractures or surgery. Patients without DPN were followed up in the following 18 months, and patients with new-developed DPN were counted. This study gained approval by the Chinese Clinical Trial Registry’s ethics committee, and informed consent was obtained from all enrolled patients. This study’s clinical registration number is ChiCTR1900026629. This study was conducted in accordance with the Declaration of Helsinki. Due to the limited number of ethical review staff in our hospital, we had to queue for a long time, so we chose to get approval from the Ethics Committee of the Chinese Clinical Trial Registry.
Data Collection
We collected data on patient characteristics (eg, age, type of diabetes, disease course, medical history, height, weight) and inflammatory indicators (eg, levels of NLR and PLR) using the hospital’s electronic medical record system. The included subjects were divided into four different groups, including T1DM with DPN group (T1DPN group), T1DM without DPN group (T1DM group), T2DM with DPN group (T2DPN group), T2DM without DPN group (T2DM group). The diagnostic criteria for DPN were based on the Toronto Expert Consensus.13 Professional doctors (Meichao Chen and Yuanbo Wu) verified the data.
Statistical Analysis
Statistical software SPSS, version 20.0, was used to analyze the collected data. Continuous data and normally distributed data were expressed as the mean ± standard deviation using the Student’s t-test for intergroup comparisons, whereas non-normally distributed data were expressed as the median (1/4, 3/4) using the Mann–Whitney U-test. Categorical variables were expressed as counts (%) using the χ2 test for comparisons. The influence of related indicators levels were assessed using binary logistic regression analysis with significant factors. Results were expressed as adjusted odds ratios (OR) with the corresponding 95% confidence intervals (CI). Receiver operating characteristic (ROC) curves were drawn, cut-off values were determined. The cut-off values and their corresponding sensitivity and specificity were determined using the Youden index. Drew the corresponding box diagram for the indicator with the maximum AUC. P values less than 0.05 were considered statistically significant.
Results
General Data
A total of 70 patients with type 1 diabetes were recruited, including 48 patients with DPN and 22 patients without DPN. For type 2 diabetes, 155 patients were recruited, including 74 patients with DPN and 81 patients without DPN.
Data were compared between the two groups in terms of general patient characteristics (eg, age, disease course), inflammatory indicators (eg, levels of NLR and PLR).
For type 1 diabetes, age was statistically different between the two groups. The age of patients with DPN was generally higher than that of patients without DPN (36.31 ± 15.64 years and 28.32 ± 12.79 years, respectively). For type 2 diabetes, age, disease course and systolic blood pressure were statistically different between the two groups. The age of patients with DPN was generally higher than that of patients without DPN (61.92 ± 11.22 years and 55.90 ± 11.34 years, respectively). The disease course of patients with DPN was longer than that of patients without DPN (11.00 (5.00, 19.50) years and 6.00 (2.00, 10.00) years, respectively). The systolic blood pressure of patients with DPN was higher than that of patients without DPN (144.07 ± 20.60 years and 136.47 ± 17.12 mmHg, respectively). The baseline characteristics of hospitalized patients are shown in Table 1.

Table 1 Baseline Patient Characteristics and Laboratory Results
For type 1 diabetes, levels of platelet counts, indirect bilirubin, total cholesterol, NLR and PLR were all statistically different between the two patient groups, and for type 2 diabetes, indirect bilirubin, triglyceride and NLR were all statistically different between the two patient groups. Notably, the inflammatory indices of patients with DPN were generally higher than those of patients without DPN, as shown in Table 1.
Predictive Value of NLR, PLR and I-BIL
Between DPN group and DM group, ROC curves were drawn for NLR, PLR and I-BIL. The AUCs and cut-off values were calculated according to their specificity and sensitivity as predictive factors.
The AUC of PLR levels was 0.753 (95% CI 0.635–0.871); the sensitivity was 70.80% and the specificity was 77.30% for predicting DPN in type 1 diabetes when the cut-off level of PLR was 97.880. The cut-off NLR level was set at 2.485, with a sensitivity of 38.00% and a specificity of 79.00%, for predicting disease severity, and an AUC of 0.602 (95% CI 0.513~0.691), as shown in Figure 1 and Table 2.

Table 2 ROC Curve Area and Cut-Off Values of NLP PLR and I-Bil for the Diagnosis of DPN

Figure 1 The ROC curves of predicting whether diabetic patients combined with DPN. Subfigure (A) is the receiver operating characteristic analysis (ROC) for NLR, PLR and I-BIL to predict DPN in T1DM. Subfigure (B) is the ROC curve of NLR and I-BIL for predicting whether T2DM is combined with DPN.
Comparison of NLR and PLR in Different Groups
The NLR level in T2DM with DPN group was statistically higher than that of T2DM without DPN group, T1DM with DPN group and T1DM without DPN group. While the PLR level in the T1DM with DPN group was significantly higher than that of T1DM without DPN group, T2DM with DPN group and T2DM without DPN group, as shown in Figures 2 and 3.

Figure 2 The comparison of the PLR and NLR values of DPN for 2 types of diabetes. Subfigure (A) is the comparison of the PLR value between the T1DM with DPN group and T1DM without DPN group. Subfigure (B) is the comparison of the NLR value between the T2DM with DPN group and T2DM without DPN group.

Figure 3 Bar chart of NLR and PLR values for each group. Subfigure (A) is a bar diagram for four sets of PLR values. Subfigure (B) reacts NLR values for four groups; P < 0.05 was marked as “*”, and P < 0.01 as “**”.
Follow-Up Results
General Data
After 18 months of follow-up for diabetes patients without DPN, 9 patients of type 1 diabetes were newly diagnosed with DPN, while 14 patients of type 2 diabetes were newly diagnosed with DPN. We analyzed the data between patients with and without newly diagnosed DPN. The type of diabetes mellitus was a significant factor for the new onset of DPN, and the BWI of patients without DPN was higher than that of patients with newly diagnosed DPN. The results are shown in Table 3.

Table 3 Baseline Patient Characteristics and Laboratory Results on Follow-Up Subjects
For the relative indicator, levels of NLR, PLR, NEUT (%), NC (109/L), LYMPH (%), LC (109/L), TC (mmol/L), TG (mmol/L) and LDL-C (mmol/L) were all statistically different between the two patient groups. For the inflammatory indicators, levels of PLR and NLR were all statistically higher in the group with newly diagnosed DPN. For lipid metabolism-related indexes, TC (mmol/L), TG (mmol/L) and LDL-C (mmol/L) were significantly lower in the group with newly diagnosed DPN. The results are shown in Table 3.
Regression Model
After adjusting for above recorded confounders such as BWI, TC, TG, LDL-C, type of diabetes and NLR were associated with the new diagnosis of DPN in multivariate binary logistic regression analysis. The adjusted OR were 0.091 (95% CI, 0.010–0.799) and 0.060 (95% CI, 0.014–0.258; p ≤ 0.001), respectively. The results are shown in Table 4.

Table 4 Binary Logistic Regression Analysis for Newly Diagnosed DPN in Follow-Up Subjects
Discussion
The neuropathy of diabetes is the most common neurological disorder in the world, and its prevalence increases with the extension of diabetes.14 It affects about half of people with diabetes, affecting their sensorimotor function. And the early stages of DPN can be asymptomatic, resulting in delaying diagnosis. Seeking an effective and convenient screening method can improve the screening efficiency.
Multiple factors contribute to the occurrence of DPN, including endothelial injury, microvascular dysfunction, metabolic disorders, oxidative stress, abnormal cytokines and immune factors, among which inflammatory injury plays an important role. Chronic hyperglycemia can lead to microcirculation disorders. A series of vascular pathological changes can occur, such as vascular endothelial cell proliferation, microvascular basement membrane thickening and hyaline degeneration, which leads to direct narrowing of lumen. The increase of blood viscosity and the disturbance of blood flow aggravate the reduction of blood supply to local tissues. This process leads to ischemia and hypoxia of nerve tissues, stimulating the increase of cytokines, and aggravating inflammatory damage. Besides, hyperglycemia leads to damage through several major, well-characterized biochemical pathways, including activation of the polyol pathway, increased levels of advanced glycation end products (AGEs) and their receptors, activation of protein kinase C (PKC),15 mitogen-activated protein kinase (MAPK), and inducible nitric oxide synthase.16 These biochemical processes can produce oxidative mediators and inflammatory mediators, resulting in local or systemic tissue damage. Abnormal lipid metabolism is also one of the important influencing factors. Adipocytes are important components for inducing and maintaining the inflammatory response. In general, inflammation injury, activated and maintained by various pathways, plays an important role in the development of diabetes mellitus and its complications.
Neutrophil-to-lymphocyte ratio (NLR) represents the balance of neutrophils and lymphocytes in vivo. Neutrophils are closely related to inflammatory responses, and lymphocytes reflect immune regulatory pathways.17,18 They can reflect systemic inflammation,19,20 as well as innate immune responses (mediated by neutrophils) and adaptive immune responses (mediated by lymphocytes).21 The nonspecific inflammatory response caused by hyperglycemia may lead to changes in peripheral blood cell levels, which may explain the abnormal NLR values. Association between inflammatory conditions and elevated NLR has been well-established.22 The reason NLR is reported as a novel marker is that it is very stable compared with the absolute count, which can be altered by various physical, physiological and pathological factors.23 Some clinical studies have proposed that NLR value is related to DM and its complications. Duman et al‘s study has demonstrated that NLR was strongly correlated with age, fasting plasma glucose and HbA1c.24 A Japanese study showed that NLR might be a potential factor for evaluating diabetic patients with a higher degree of albuminuria,25 suggesting that NLR may predict the existence of microvascular complications.26
In diabetic patients, abnormal insulin action may lead to increased platelet adhesion.
At the same time, hyperglycemia also accelerate platelet metabolism and production, exacerbating the imbalance between coagulation and anticoagulation in vivo. This process may play an important role in atherogenesis, thrombosis and microcirculation disturbance.27 PLR is reported to be a prognostic marker of inflammation for many types of cardiovascular disease, including peripheral arterial disease (PAD) and hypertension.28,29 PLR is also reported to have predictive effect about diabetes mellitus and diabetic complications in recent years. A cross-sectional study from Japan demonstrated that PLR can be a marker for high risk diabetic foot and diabetic foot ulcer in patients with type 2 diabetes.30 Besides, Duan et al’s study demonstrated that the PLR was associated with proteinuria and prognosis in diabetic kidney disease (DKD) patients.31
Bilirubin is a product of heme degradation, and recent studies have reported the beneficial effects of elevated serum bilirubin on cardiovascular health and its antioxidant properties at physiological concentrations.32 Research has demonstrated that bilirubin has anti-inflammatory properties in vitro and in vivo. Bilirubin releases eNOS by inhibiting protein kinase C and NAD(P)H oxidase pathways that produce oxidants, and inhibits the peroxidation of lipids and lipoproteins, thereby reducing ROS and protecting nerves from damage.33,34 DPN is associated with inflammatory responses, so bilirubin may have beneficial effects. Kim et al35 demonstrated a significant correlation between low serum bilirubin levels and DPN.
In our study, NLR and PLR were significantly increased in DPN in patients with type 1 diabetes. Through the ROC curve, the area under the curve of PLR was the largest. When the cut-off value was 97.880, the sensitivity is 70.80% and the specificity was 77.30%. PLR could be used to predict whether type 1 diabetes patients were associated with peripheral neuropathy. As for indirect bilirubin, this indicator is negatively correlated with DPN, which is consistent with the research results of Kim et al. According to the antioxidant and anti-inflammatory properties of bilirubin, this is in line with the expected results. For patients with type 2 diabetes, NLR was significantly higher in the DPN group. According to the ROC curve, when the cut-off value is 2.485, the sensitivity is 38.00% and the specificity was 79.00%. NLR may be an independent risk factor for T2DM with DPN, as demonstrated by Siying Liu et al, Xu et al.36,37
Through the analysis of the results of follow-up, we found that the newly diagnosed DPN was related to the type of diabetes, BWI, inflammatory indexes, and lipid metabolism-related indexes. And the result of logistic regression analysis confirmed that the type of diabetes and NLR level were powerful indicators of risk of developing newly diagnosed DPN after adjusted other variables. Compared with type 2 diabetes, patients with type 1 diabetes have a higher risk. While NLR value could be an effective index to predict DPN in the future.
There are some limitations in this study. For the T2DM with DPN group, it has a higher level of NLR compared with the other three groups, while the T1DM with DPN group has a higher level of PLR compared with the other three groups. The relationship between the inflammatory mechanism of diabetic peripheral neuropathy and different types of diabetes is worthy of further study. In addition, there are limitations in sample size, single center, and lack of long-term clinical observation.
Our results show that the T1DM patients who has a higher level of PLR is more likely to develop into DPN, while T2DM patients who has a higher level of NLR is more likely to develop into DPN. NLR and PLR could be used as predictors to help clinicians screening for DPN in different types of diabetes. In this study, we also found that type 1 diabetes is more likely to develop DPN in the future. For type 1 diabetes, if patients who were without DPN had higher NLR level, the risk of developing DPN in the future will be greatly increased.
Data Sharing Statement
We will share the relevant data of the paper on the website of Chinese Clinical Trial Registry within six months to one year after the paper is published.
Acknowledgment
This study was supported by the Fundamental Research Funds for the Central Universities, No. WK9110000036 (to YBW); Natural Science Foundation of Anhui Province, China, No. 1608085MH209 (to YBW); Fundamental Research Funds for the Central Universities, No. WK9110000114 (to JW).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fukuhara A, Matsuda M, Nishizawa M, et al. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science. 2005;307(5708):426–430. doi:10.1126/science.1097243
2. Steppan CM, Bailey ST, Bhat S, et al. The hormone resistin links obesity to diabetes. Nature. 2001;409(6818):307–312. doi:10.1038/35053000
3. Pop-Busui R, Boulton AJM, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–154. doi:10.2337/dc16-2042
4. King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008;79(8s):1527–1534. doi:10.1902/jop.2008.080246
5. Korniluk A, Koper-Lenkiewicz OM, Kamińska J, Kemona H, Dymicka-Piekarska V. Mean Platelet Volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm. 2019;9213074:2019.
6. Poz D, De Falco E, Pisano C, et al. Diagnostic and prognostic relevance of red blood cell distribution width for vascular aging and cardiovascular diseases. Rejuvenation Res. 2019;22(2):146–162. doi:10.1089/rej.2018.2094
7. Kim YC, Song JE, Kim EJ, et al. A simple scoring system using the red blood cell distribution width, delta neutrophil index, and platelet count to predict mortality in patients with severe sepsis and septic shock. J Intensive Care Med. 2019;34(2):133–139. doi:10.1177/0885066618787448
8. Montagnana M, Danese E. Red cell distribution width and cancer. Ann Trans Med. 2016;4(20):399. doi:10.21037/atm.2016.10.50
9. Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. 2016;14(5):573–577. doi:10.1586/14779072.2016.1154788
10. Buyukkaya E, Karakaş MF, Karakaş E, et al. Correlation of neutrophil to lymphocyte ratio with the presence and severity of metabolic syndrome. Clin Appl Thromb/Hemost. 2012.
11. Diem S, Schmid S, Krapf M, et al. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–181. doi:10.1016/j.lungcan.2017.07.024
12. American Diabetes Association. 2. classification and diagnosis of diabetes: standards of medical care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S13–s27. doi:10.2337/dc18-S002
13. Tesfaye S, Boulton AJM, Dyck PJ, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–2293. doi:10.2337/dc10-1303
14. Iqbal Z, Azmi S, Yadav R, et al. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018;40(6):828–849. doi:10.1016/j.clinthera.2018.04.001
15. Xia P, Kramer RM, King GL. Identification of the mechanism for the inhibition of Na+, K(+)-adenosine triphosphatase by hyperglycemia involving activation of protein kinase C and cytosolic phospholipase A2. J Clin Invest. 1995;96(2):733–740. doi:10.1172/JCI118117
16. Vareniuk I, Pavlov IA, Obrosova IG. Inducible nitric oxide synthase gene deficiency counteracts multiple manifestations of peripheral neuropathy in a streptozotocin-induced mouse model of diabetes. Diabetologia. 2008;51(11):2126–2133. doi:10.1007/s00125-008-1136-3
17. El Kebir D, Filep JG. Targeting neutrophil apoptosis for enhancing the resolution of inflammation. Cells. 2013;2(2):330–348. doi:10.3390/cells2020330
18. Rajakariar R, Lawrence T, Bystrom J, et al. Novel biphasic role for lymphocytes revealed during resolving inflammation. Blood. 2008;111(8):4184–4192. doi:10.1182/blood-2007-08-108936
19. Gibson PH, Cuthbertson BH, Croal BL, et al. Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 2010;105(2):186–191. doi:10.1016/j.amjcard.2009.09.007
20. Tamhane UU, Aneja S, Montgomery D, et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102(6):653–657. doi:10.1016/j.amjcard.2008.05.006
21. Sawant AC, Adhikari P, Narra SR, et al. Neutrophil to lymphocyte ratio predicts short- and long-term mortality following revascularization therapy for ST elevation myocardial infarction. Cardiol J. 2014;21(5):500–508. doi:10.5603/CJ.a2013.0148
22. Moore MM, Chua W, Charles KA, Clarke SJ. Inflammation and cancer: causes and consequences. Clin Pharmacol Ther. 2010;87(4):504–508. doi:10.1038/clpt.2009.254
23. Azab B, Daoud J, Naeem FB, et al. Neutrophil-to-lymphocyte ratio as a predictor of worsening renal function in diabetic patients (3-year follow-up study). Ren Fail. 2012;34(5):571–576. doi:10.3109/0886022X.2012.668741
24. Duman TT, Aktas G, Atak BM, et al. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. Afr Health Sci. 2019;19(1):1602–1606. doi:10.4314/ahs.v19i1.35
25. Kawamoto R, Ninomiya D, Kikuchi A, et al. Association of neutrophil-to-lymphocyte ratio with early renal dysfunction and albuminuria among diabetic patients. Int Urol Nephrol. 2019;51(3):483–490. doi:10.1007/s11255-018-02065-2
26. Fawwad A, Butt AM, Siddiqui IA, et al. Neutrophil-to-lymphocyte ratio and microvascular complications in subjects with type 2 diabetes: pakistan’s perspective. Turk J Med Sci. 2018;48:157–161. doi:10.3906/sag-1706-141
27. Jabeen F, Fawwad A, Rizvi HA, Alvi F. Role of platelet indices, glycemic control and hs-CRP in pathogenesis of vascular complications in type-2 diabetic patients. Pak J Med Sci. 2013;29(1):152–156. doi:10.12669/pjms.291.2592
28. Thomas G, Pichler M, Belaj K, et al. Platelet-to-lymphocyte ratio: a novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. PLoS One. 2013;8(7):e67688. doi:10.1371/journal.pone.0067688
29. Sunbul M, Gerin F, Durmus E, et al. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin Exper Hypertens. 2014;36(4):217–221. doi:10.3109/10641963.2013.804547
30. Mineoka Y, Ishii M, Hashimoto Y, et al. Platelet to lymphocyte ratio correlates with diabetic foot risk and foot ulcer in patients with type 2 diabetes. Endocr J. 2019;66(10):905–913. doi:10.1507/endocrj.EJ18-0477
31. Duan S, Sun L, Zhang C, et al. Association of platelet-to-lymphocyte ratio with kidney clinicopathologic features and renal outcomes in patients with diabetic kidney disease. Int Immunopharmacol. 2021;93:107413. doi:10.1016/j.intimp.2021.107413
32. Stocker R, Yamamoto Y, McDonagh AF, Glazer AN, Ames BN. Bilirubin is an antioxidant of possible physiological importance. Science. 1987;235(4792):1043–1046. doi:10.1126/science.3029864
33. Kwak JY, Takeshige K, Cheung BS, Minakami S. Bilirubin inhibits the activation of superoxide-producing NADPH oxidase in a neutrophil cell-free system. Biochim Biophys Acta. 1991;1076(3):369–373. doi:10.1016/0167-4838(91)90478-I
34. Son SM. Reactive oxygen and nitrogen species in pathogenesis of vascular complications of diabetes. Diabetes Metab J. 2012;36(3):190–198. doi:10.4093/dmj.2012.36.3.190
35. Kim ES, Lee SW, Mo EY, Moon SD, Han JH. Inverse association between serum total bilirubin levels and diabetic peripheral neuropathy in patients with type 2 diabetes. Endocrine. 2015;50(2):405–412. doi:10.1007/s12020-015-0583-0
36. Liu S, Zheng H, Zhu X, et al. Neutrophil-to-lymphocyte ratio is associated with diabetic peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract. 2017;130:90–97. doi:10.1016/j.diabres.2017.05.008
37. Xu T, Weng Z, Pei C, et al. The relationship between neutrophil-to-lymphocyte ratio and diabetic peripheral neuropathy in Type 2 diabetes mellitus. Medicine. 2017;96(45):e8289. doi:10.1097/MD.0000000000008289
Source link
0 notes
Text
So proud of our team's embrace of transparent and early sharing of data, ideas and protocols. The future is bright! #openscience https://asapbio.org/announcing-the-winners-of-the-2024-asapbio-poster-competition

Here is a link to the poster: Evolutionary diversification of protein-protein interaction interfaces: A case study on an NLR immune receptor network #ASAPbio #openscience https://doi.org/10.5281/zenodo.13365607
0 notes
Text
Biomed Grid | A General Outlook at the Pathogenesis of COPD
Introduction
Chronic obstructive pulmonary disease (COPD) is a pathological disorder characterized by deregulated chronic inflammation of the airways and persistent airflow obstruction [1,2], which lead to emphysematous destruction of lung tissue and deterioration of the pulmonary function [3]. The characteristics of COPD include infiltration of neutrophils, macrophages, B and T lymphocytes, and dendritic cells that release inflammatory cytokines, proteases, and growth factors responsible for the structural changes in the lung. It also comprises mucociliary dysfunction, apoptosis, and structural changes in the airways causing emphysema, and extrapulmonary systemic effects [4], with a calculated prevalence of 10% in over forty years old adults. Clinical features of COPD include persistent pulmonary inflammation, obstructive bronchiolitis, chronic bronchitis, emphysema and loss of alveolar tissue. Conventional therapies work only as palliative treatments. Respiratory infections increase of cardiovascular risk, lung cancer, pulmonary hypertension, and depression are some of the most common complications caused by this disorder. COPD is a significant leading cause of deaths worldwide, and by 2020, it is expected to be the third leading cause of deaths worldwide [5]. Cigarette smoking is the major etiologic and risk factor for COPD [6]. Aging is considered a critical factor in the development of COPD [7]. It’s been shown that the incidence of COPD increases with aging, with a peak observed in patients aged 65-74 years [8,9].
The pathogenesis of COPD remains largely unclear. It is known that emphysema is characterized by the presence of humoral and cellular autoimmune responses against elastin [10], and bronchial smooth muscle cell hyperplasia [11], showing evidence for a role of autoimmunity in COPD pathogenesis, with a prominent role of inflammation. Dysregulated inflammation, dysfunction in airway smooth muscle (ASM), imbalance in the proteolysis/ antiproteolysis equilibrium and in the repair process, and different epigenetic mechanisms –including DNA methylation, decreased levels of histone deacetylases and reduced microRNAs levels– are mechanisms that contribute to COPD pathophysiology [12]. Inflammatory cells influence cell destruction, hyperplasia of smooth muscle cells, and subepithelial fibrosis seen in COPD. It has been hypothesized that inflammatory cells infiltrate the bronchial mucosa and lung parenchyma in COPD lungs, affecting the airway destruction and remodeling by secreting enzymes and inflammatory cytokines or by indirect interference regulating other cellular functions [13], promoting tissue damage and reconstruction. However, the mechanism of participation of different inflammatory mediators is not completely known. Currently, no good biomarkers of remodeling are available, and imaging techniques are not sensitive enough to directly visualize the remodeling changes in the airways.
Cytokines have a controversial and sometimes opposite role in COPD; the elimination of a single one may further deregulate the inflammatory process. Cells and mediators of immunity, and reactive oxygen species (ROS) also contribute to inflammation [14]. Innate and adaptive immune systems are involved in the development of chronic inflammation leading to COPD. The role of innate immunity in COPD pathogenesis has been implicated in the induction and acute exacerbation [15,16], with Interleukin (IL) 1-like cytokines increased in COPD patients suggesting the role of inflammasomes –intracellular multiproteines complexes that activates proinflammatory caspases– in the pathogenesis of COPD that lead to the production of IL-1β and IL-18 in response to pathogenesis [15,16]. Innate immune cells recognize microbial pathogens or damage-associated molecular patterns or recognition of innate immune cells, which activate the inflammasome through several families of pattern recognition receptors (PRRs) expressed in innate immune cells, including Toll-like receptors (TLRs), nucleotide-binding domain leucine-rich repeat-containing receptors (NLRs), C-type lectin receptors, and RIG-I-like receptors [15,16]. TLRs are expressed on alveolar macrophages, lymphocytes, dendritic cells, and bronchial epithelial cells [15,16].
COPD exacerbations are defined as sustained worsening of a patient’s condition associated with respiratory –dyspnea and productive cough– and non-respiratory –fatigue and malaise– symptoms [17] beyond normal day-to-day variations that is acute in onset. Several biomarkers of inflammation can help to identify exacerbations most likely to respond to oral corticosteroids and antibiotics, and patients with a frequent exacerbation phenotype, which requires a preventative treatment [18]. While mild exacerbations can be managed with inhaled bronchodilators, for worsening symptoms, while moderate exacerbations need treatment with antibiotics and/or corticosteroids, and severe exacerbations require hospitalization [17]. The heterogeneity in COPD clinical manifestations, outcomes, and responses to treatment [19] is useful to classify COPD into specific phenotypes. Many exacerbations of COPD involve bacterial or viral respiratory infections [20]. Accelerated cell senescence and insufficient autophagy –significantly deregulated in the cells from COPD patients– increase the accumulation of damaged cells [21]. Cellular senescence has been widely implicated in the pathogenesis of COPD, presumably by impairing cell repopulation and by aberrant cytokine secretion in the senescence-associated secretory phenotype. Autophagy is a process of lysosomal self-degradation that maintains a homeostatic balance between the synthesis, degradation, and recycling of cellular proteins.
Peripheral blood eosinophil count was shown to be a valid biomarker for sputum eosinophil-associated exacerbations [22]. Patients with COPD and evidence of eosinophilic airway inflammation respond well to corticosteroid therapy [23]. C-reactive protein (CRP) is another potentially useful biomarker for predicting which exacerbations may benefit from antibiotic therapy and for selecting those that might resolve without antibiotic intervention [24]. Procalcitonin may not be sufficiently sensitive for use as a biomarker for response to antibiotics in patients with COPD exacerbations [24]. Therefore, the use of CRP as a biomarker could help to avoid unnecessary use of antibiotic therapy that can lead to adverse effects and development of bacterial resistance [25]. In addition to bronchodilators, macrolide azithromycin, taken daily for 1 year in addition to usual therapy, demonstrated a significant reduction in the risk of exacerbations in patients with COPD at increased risk of exacerbation [26]. Furthermore, there is evidence that pneumococcal and annual influenza vaccinations reduce the risk of exacerbation and hospitalization in patients with COPD [27-29]. Other mechanisms further upregulated during exacerbations –triggered by infectious pathogens, air pollution or second-hand smoke– include amplification of inflammatory process.
Conclusion
Inflammation plays a key role in the development of COPD. Other mechanisms such as senescence, autophagy or repair process are dysregulated in COPD. Despite all the current knowledge, there is still a long way to go to further unveil the pathogenesis of COPD, and find useful biomarkers for diagnosis, response to treatments and outcome.

#biomedgrid#American Journal of Biomedical Science & Research#Journals on Cancer medicine#Journals on Biomedical Imaging#Journals on Medical drug and theraputics#Behavioural medicine journals
0 notes
Text
Animal NLRs provide structural insights into plant NLR function
Animal NLRs provide structural insights into plant NLR function
Since the characterisation of the gene-for-gene concept in plant disease resistance by Flor in the 1940s, resistance (R) genes have played a central role in breeding resistant crops. Gene-for-gene resistance is now known to be the result of the effector-triggered immunity response in plants. Molecular characterisation of R proteins reveals that they function analogously to the intracellular…
View On WordPress
#Avirulence protein#cryo-electron microscopy#crystal structure#effector-triggered immunity (ETI)#leucine-rich repeat (LRR)/nucleotide-binding oligomerization domain (NOD)-like receptor (NLR)#nucleotide binding (NB)#plant pathogen effector protein#resistance protein#three-dimensional structure
0 notes
Text
Graduate position: INRA_Avignon.AphidAdaptation
PhD thesis proposal : Non host resistance and genetic/heritable resistance: how Aphis gossypii, the melon aphid, does adapt? Supervisor Nathalie Boissot INRA-GAFL (Avignon, http://bit.ly/2rmYxWU), [email protected] for more details The paradigm for plant-pathogen interactions is based on the evolution of molecular patterns of pathogens recognized by the plant (1)): pathogens adapt to immune reaction of plants, either the immune reaction concern the entire plant species and act against the pathogen at the scale species, it is non host resistance, or the immune reaction concern specific plant accessions, what we call genetic resistance or heritable resistance. Like pathogens, aphids deliver into the plant effectors via their adapted mouthparts, the stylets. Aphids establish a compatible relationship with the plant when these stylets reach the phloem in which they feed. Does the paradigm for plants/pathogens coevolution portable to plants/aphids interaction as proposed recently (2), especially in the Melon-Aphis gossypii system? An alternate hypothesis is that aphid specializing on Cucurbit and/or adapted to NLR resistance present in melon use the particularity of the phloemic system, which is dual, in Cucurbits (3). (1) Jones D.G., Dangl J.L. ,2006, The plant immune system. Nature 444:323-32 (2) Dangl J.L., Horvath D.M., Staskawicz B.J,2013, Pivoting the plant immune system from dissection to deployment. Science 341:746-751 (3) Zhang B.C., Tolstikov V., Turnbull C., Hicks L.M., Fiehn O., 2010, Divergent metabolome and proteome suggest functional independence of dual phloem transport systems in cucurbits. PNAS 107:13532-13537 WORKPACKAGES 1A / Establish in which phloem of Cucurbitaceous plants feed in A. gossypii clones specializing on Cucurbits. This could be tested on Cucurbits belonging to three genera of Cucurbitaceaous: Cucumis melo, Cucurbita pepo and Citrullus lanatus. 1B / Determine whether the punctures of non-Cucurbits aphids not-specializing on Cucurbits cause clogging of the fascicular and/or extra-fascicular phloem on a non-Vat melon plant. 1C / Determine whether the punctures of the specializing clones on Cucurbits which elicit the Vat resistance (ie avirulent clone) lead to clogging of the fascicular phloem and/or extra fascicular on melon Vat plants. 2A / Characterize the diversity of candidate genes for their involvement in the adaptation of A. gossypii to Cucurbits. Establish the phylogeny and confront it with the membership of the breed of hosts of the individuals analyzed. Seek for the traces of selection in these genes. 2B / Identify the avirulence gene in A. gossypii eliciting the Vat resistance. Characterize its diversity, establish the frequency of the allele (s) conferring virulence in natural populations. METHODOLOGY PROPOSITIONS To determine in which phloem feed the aphids specializing on Cucurbits, adapted or not to the Vat-1 resistance, we will collaborate with the team of Sylvie Dinant at the IJPB (http://bit.ly/2sG1q9t). We will take advantage of the difference in flow velocity in the two types of phloem in Cucurbits, coupled with the use of fluorochromes (Zhang et al., 2010) that can be tracked even in honeydew produced by aphids. We will use the particular phenotype of aphid-elicited resistance to viruses to identify among an established set of candidate proteins the aphid effector for avirulence. Candidate proteins will be expressed in planta via the use of a viral expression vector. If the candidate protein is the elicitor of resistance, replication of the virus will be blocked in Vat-1 melons but will occur in non-Vat-1 melons. This work will be carried out in collaboration with Ccile Desbiez, (http://bit.ly/2rn8fso). We will sample on Cucurbits winged individuals at spring, these aphid populations are known to contain wide diversity (Thomas et al., 2012). Each individual will be characterized on the basis of the 8 SSR markers used routinely in the laboratory and assigned to one of the genetic groups established on the basis of the 2095 genotypes that we have described to date. The candidate genes studied will be sequenced in individuals with non-redundant multilocus genotypes, we will establish phylogenies and selective traces of selection. This work will be carried out in collaboration with Flavie Vanlerberghe, (http://bit.ly/2sFrBwS). Boissot Nathalie via Gmail
0 notes