#May-Thurner Syndrome
Explore tagged Tumblr posts
Text
https://showbizsphere.co.in/lauren-boebert-suffer-may-thurner-syndrome/
US Representative Lauren Boebert’s experience with May-Thurner syndrome (MTS) has brought this rare vascular condition into the spotlight. This article dives deeper into understanding MTS, its causes, symptoms, and treatment options.

0 notes
Video
vimeo
(Vascular Compression Syndrome Introduction on Vimeo)
An *outstanding* explainer video about vascular compression syndromes incl. MALS, SMAS, May Thurner, Thoracic Outlet Syndrome and more.
#vimeo#compression syndrome#vascular health#chronic illness#May Thurner Syndrome#MALS#SMAS#Thoracic Outlet Syndrome
2 notes
·
View notes
Text
Republican congresswoman Lauren Boebert has undergone emergency surgery to remove a blood clot after being been diagnosed with a rare vascular disorder. Boebert, well-known for her anti-LGBTQ+ remarks, was taken to a Colorado hospital after experiencing severe swelling in her left leg on Monday (1 April). Her campaign team said doctors found an acute blood clot and inserted a stent; a tube which keeps an artery open. She was later diagnosed with May-Thurner Syndrome.
Continue Reading
5 notes
·
View notes
Text
Deep Vein Thrombosis ST Augustine
Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, typically in the legs. In St. Augustine, specialized medical facilities provide advanced care for DVT, including diagnostics, anticoagulant therapy, and preventative measures. Early detection is crucial to prevent complications. For more details, visit our website.
#may thurner syndrome symptoms#deep vein thrombosis st augustine#end stage renal disease treatment st augustine#superficial venous reflux disease symptoms#critical limb is chemia symptoms
0 notes
Text
MCYT Physically Disabled Week!!

Day 7: Free Day!
Thanks to the mods of @mcytphysicaldisabilityweek for hosting this event!
I chose free day because I gave Tommy what I have, May Thurner/Nutcracker syndrome! Which is kinda a weird one but here's a quick explanation:
May Thurner is a compression of your iliac vein (in your hip) and Nutcracker Syndrome is a compression of your left renal vein (kidney). While many people actually walk around with these conditions and are fine, a teeny tiny percentage of people, like me, suffer debilitating symptom that include swelling, tachycarida, abdominal, back (<- more common with Nutcracker Syndrome), chest, and leg pain, and severe intolerance of walking, standing, and even sitting upright (hence the near-flat wheelchair, which is actually modeled after the one I use.)
It's not a very fun set of conditions, and it's made worse by the fact that having it severe enough to be treated is extremely rare, and thus there aren't many places that treat it. So for this art chommy is just like me: bedridden and slowly loosing social skills.
If you would like to know more about May Thurner or Nutcracker syndrome, please ask!
#art#artists on tumblr#my art#dream smp fanart#dsmp fanart#dream smp art#dreamsmp fanart#tommyinnit art#tommyinnit fanart#tommyinnit#c!tommy art#c!tommy#c!tommy fanart#mcyt fanart#mcyt physically disabled week#can you tell i rushed this a little bit#actually no i didn't rush it#just for the life of me i couldn't get the pose right#disabled artist#disability art#invisible disability#invisible illness#chronic illness#chronic disability
133 notes
·
View notes
Text

Hi, I'm currently drowning in medical debt right now.
I owe nearly $600 in medical debt (ER visit due to torn tendon in foot, cardiologist to rule out May-Thurner syndrome, rheumatologist to refill fibromyalgia meds). Anything helps 🥺
https://www.paypal.me/MorenaZima
I have Venmo and cash app too


12 notes
·
View notes
Text
When time, read: [ ] double barrel wet colostomy [ ] appendiceal cancer [ ] malignant bowel protocol [ ] May Thurner syndrome [ ] Po vs IV vs rectal vs vaginal contrast As always, so, so tired. Last "work" night of 5 weeks with a call shift tomorrow. So the night goes oncology night shift > present research @ 0930 > sleep > graduation @ 1800 > call shift.
I'm dreading the whole freaking day. My research proposal is not good. My slides are messed up. It's confusing. I think the study itself will be fine, but a 5 week night float was not the time or place to get my shit together for this. I just hope the program coordinator can find it within herself to update my slides in the morning, or else I'm fucked. And then I'm gonna get such LITTLE SLEEP before I have to go to graduation for 4 hrs and pretend to be in a good mood and socialize. At least my call shift right afterwards is normal R2 crap, antepartum/benign gynecology stuff.
To be honest covering the oncology service has been chill enough the past shift-and-half, except for when it's bad it's BAD and probably the worst service to be on. I like onc nights more than days, though, because there's not a lot of extra people and I can just sit in my little work room upstairs and be alone and read through things. It's mostly covering the OR at the end of the day shift, seeing overnight direct admits and transports, and following up vitals and miscellaneous labs, post-op checks, etc. And then sometimes people surgical emergencies, or people crump or straight up die.
So, a medicine service +/- OR time.
My first night I had two transports: a malignant large bowel obstruction iso newly diagnosed HGSOC that is being managed conservatively given its size <13 cm but also her significant neutropenia due to her neoadjuvant Avastin therapy (her prognosis.... isn't amazing), and a "frequent flier" with recurrent vulvar cancer (and the gnarliest genitourinary anatomy I've seen) s/p MULTIPLE resections, EUAs, ablations admitted with c/f sepsis in the setting of a new perirectal abscess. All things considered it went well enough but my presentations were rocky, like I'd expect them to be for a new R2, but I'm almost R3. I was flustered because they both came at the same time and the LBO made me nervous, so I felt rushed trying to get the other transport tucked in so I only had to call the attending once.
Tonight started out with the potential to be a NIGHTMARE. There were two ORs running late, an exlap followed by an EUA with one attending, and a robotic hyst with another, and then I got sign out on four (4) incoming transports, and I also had four (4) post-op checks all due around the same time. I ended up not having to go to the OR because the exlap said I don't need to scrub anyone out, the EUA was cancelled, and one of the transports came at the same time so my R3 said to see that instead of scrubbing her out.
It's a very sad case, though. I mean, all onc cases are sad, but she was with her dad which just tore at my heart. It's a woman <50 yo, no hx cancer, with 3-4 months of back pain who finally had an ultrasound and CT that showed 3 large abdominopelvic masses and widespread mets. :c She's getting omental biopsies tomorrow. We ultimately think it's appendiceal or some other gastrointestinal malignancy because her CA-125 is only about 180, which for a pre-menopausal woman is low. Another one where the prognosis is not very good.
Actually, none of these people I admitted have good prognoses. I guess that's just how gyne onc is. :-/
The other transports probably aren't coming but I'm going to try and prep them in a second. There's a pelvic fluid collection in a woman 5d s/p a hyst with a post-op course c/b May Thurner syndrome and PE s/p extensive thrombectomy now on Eliquis, another vulvar cancer patient whose left drain fell out and now there is c/f infection in addition to just general failure to thrive, and someone who probably won't come who was found to be hypokalemic apparently on outpatient labs. And then some mystery woman in her 80s that may or may not show up on the ED board with recurrent HGSOC and a GTube for gastrointestinal issues.
3 h til signout, and then I have about 2-2.5 hr to sleep and practice my presentation. I'm ready for this weekend to be overrrrrrrrrrrr
2 notes
·
View notes
Text
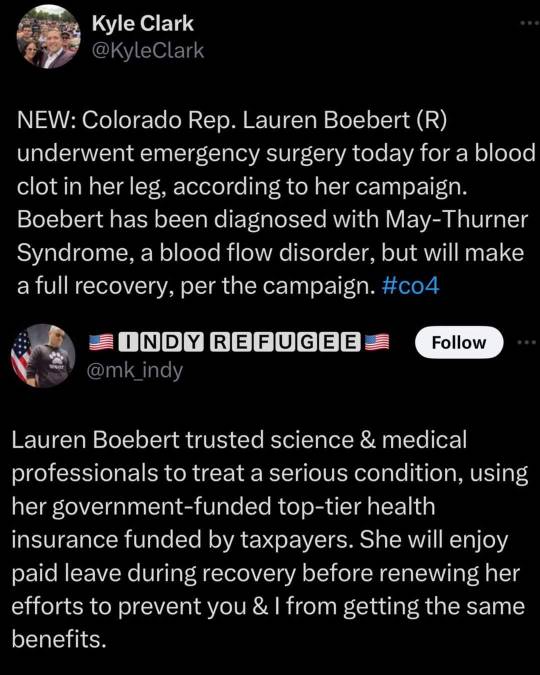
luckily for her, she has excellent healthcare. something she doesn't want you to have
3 notes
·
View notes
Text
hi I'm (24 she/her) new here and I don't really know how to use Tumblr but I downloaded it because I'm feeling very alone and hopeless and don't have any friends to talk to. I have POTS, EDS, MCAS, bilateral May thurner syndrome, IC, chronic anemia, AUB, and endometriosis. I'm currently healing from two surgeries. I had to have 4 stents placed due to severe vascular compression. I'm feeling so depressed and tired of being left on read when I try to talk to friends or group chat vent sections about my chronic illnesses ): Abled body people just don't understand me. I need a new support system. I've tried Twitter but it's a cesspool.
#chronic illness#disabled#pots#invisible illness#chronically ill#disability#dysautonomia#spooniestrong#spoon theory#spoonie
5 notes
·
View notes
Text
Life Update
Today, I got my test results from my CT scan on Wednesday, and it's not great news. I've been diagnosed with Nutcracker syndrome, Median Arcuate Ligament syndrome, May-Thurner snydrome, and possible Ehlers-Danlos syndrome. I will not be very active this coming week as I need time to process this news.
While I'm gone, I will be working on requests to distract my mind occasionally. I apologize for such a long wait, and I appreciate the patience you guys give me during my breaks.
Thank you for sticking around and make sure to take care of yourselves. ~Rory
2 notes
·
View notes
Text
Uterine Fibroid Disease St. Augustine, FL
Suffering from Uterine Fibroid Disease in St. Augustine, FL?If you have uterine fibroid disease and would like to learn more about how UAE treatment can improve your quality of life and help you avoid a painful surgical hysterectomy, give us a call to schedule an appointment today. For more detail, visit our website.
#critical limb is chemia symptoms#deep vein thrombosis st augustine#may thurner syndrome symptoms#superficial venous reflux disease symptoms
0 notes
Text
Understanding May-Thurner Syndrome: Causes, Symptoms, and Treatments
Understanding May-Thurner Syndrome: Causes, Symptoms, and Treatments May-Thurner Syndrome (MTS), also known as Iliac Vein Compression Syndrome, is a relatively rare vascular condition that can lead to serious health complications if not diagnosed and treated promptly. This article delves into the causes, symptoms, diagnosis, and treatment options for MTS to provide a comprehensive understanding of the condition. What is May-Thurner Syndrome? Read the full article
0 notes
Text

God sent Lauren Boebert that Blessed Blood Clot for a Reason!
See how she mocks and denies His divine plan.
May-Thurner Syndrome is a blessing from our Lord, intended to keep non-swimmers out of the gene pool.
Republican hypocrisy is the design.
GOP politicians take and take, then flip and tell others to do without.
4K notes
·
View notes
Text
Why Choose Dr. Kunal Arora as Your Vein Specialist in Mumbai for Optimal Vascular Health?

Say Goodbye to Varicose Veins and Other Vascular Issues with a Leading Vein Specialist in Mumbai: Dr. Kunal Arora
Feeling pain or discomfort in your legs? You might be suffering from a vein condition. If you're in Mumbai, you're fortunate to have access to one of the leading vein specialists in Mumbai with Dr. Kunal Arora.
Dr. Arora is a highly skilled and experienced interventional radiologist specializing in vascular and interventional radiology. He offers a comprehensive range of minimally invasive treatments for various vascular conditions, helping patients achieve long-lasting relief and improved quality of life.
Why Choose Dr. Kunal Arora for Your Vein Treatment?
There are several reasons why Dr. Kunal Arora should be your top choice for vein specialist in Mumbai:
Expertise and Experience: Dr. Arora is a board-certified interventional radiologist with extensive experience in diagnosing and treating vascular conditions. He stays updated on the latest advancements in vein treatment to provide his patients with the most effective and cutting-edge care.
Minimally Invasive Treatments: Dr. Arora prioritizes minimally invasive procedures whenever possible. These procedures offer several advantages over traditional surgery, including:
Smaller incisions
Reduced pain and scarring
Faster recovery times
Less risk of complications
Comprehensive Treatment Options: Dr. Arora offers a variety of treatment options to address different vein conditions, including:
Varicose vein treatment: This includes procedures like endovenous laser ablation (EVLA), radiofrequency ablation (RFA), and sclerotherapy.
Deep vein thrombosis (DVT) treatment: Dr. Arora may recommend medications, compression stockings, or minimally invasive procedures to remove blood clots and prevent future complications.
Peripheral vascular disease (PVD) treatment: PVD treatment may involve angioplasty, stenting, or other procedures to improve blood flow in the legs.
Compassionate Care: Dr. Arora understands that vein conditions can cause physical and emotional distress. He is committed to providing his patients with compassionate care, taking the time to explain treatment options and answer any questions you may have.
Conditions Treated by Dr. Kunal Arora
Dr. Kunal Arora offers treatment for a wide range of vein conditions, including:
Varicose veins: These are swollen, twisted veins that appear just below the skin's surface, often on the legs. They can cause pain, achiness, fatigue, and swelling.
Spider veins: These are smaller, red or blue veins that resemble spiderwebs near the skin's surface. While typically not a medical concern, they can cause cosmetic problems.
Deep vein thrombosis (DVT): This is a serious condition that occurs when a blood clot forms in a deep vein, usually in the legs. DVT can cause leg pain, swelling, and redness and can be life-threatening if the clot travels to the lungs.
Peripheral vascular disease (PVD): This condition is caused by a buildup of plaque in the arteries that reduces blood flow to the legs. PVD can cause leg pain, cramping, and difficulty walking.
May-Thurner Syndrome: This is a condition that occurs when the iliac vein, a large vein in the pelvis, is compressed by the iliac artery. This can cause pain, swelling, and blood clots in the leg.
Don't Let Vein Problems Hold You Back
If you're experiencing any symptoms of a vein condition, such as leg pain, swelling, or varicose veins, it's important to seek medical attention promptly. Early diagnosis and treatment can help prevent complications and improve your quality of life.
Take Charge of Your Vein Health Today
Contact Dr. Kunal Arora's clinic today to schedule a consultation and discuss your vein treatment options. With his expertise, advanced treatment options, and compassionate care, you can take charge of your vein health and get back to living an active life.
Call to Action
Don't suffer in silence. Take control of your vein health and schedule a consultation with the leading vein specialist in Mumbai with Dr. Kunal Arora today. Call us at 90040 93090 / 90040 93053 or visit our website to book an appointment.
#dr. kunal arora#best varicose treatment#endovascular care centre#vascularhealth#veintreatment#interventional radiologist in mumbai#deep vein thrombosis#varicoseveintreatment#best interventional radiologist in mumbai#healthcare
0 notes
Text
0 notes
Text
this has less of a direct relationship to mental state (although averse physical symptoms can affect someone's mental state obviously) but some things i never see mentioned are adenomyosis and vascular issues/pelvic congestion syndrome
adenomyosis is when endometrial tissue grows inside the uterine wall and can cause many of the same symptoms that endometriosis can (heavy bleeding, severe cramping, pain w/ intercourse, etc.)
pelvic congestion syndrome can cause chronic pelvic pain, painful intercourse, gastrointestinal and bladder issues, and can come with some other symptoms depending on different factors (some people have it secondary to May-Thurner Syndrome or Nutcracker Syndrome)
due to the overlap in symptom profile either of these can be mistaken for endometriosis based on symptoms alone without sufficient diagnostic practice (if they're not occurring alongside it that is)
So many people who get periods are like “Ugh it sucks that having a menstrual cycle makes you almost die every month” like no that’s not normal you need to go to the doctor
56K notes
·
View notes