#FA Nutrition
Explore tagged Tumblr posts
Text
Experimenting
Male!Vampire Scientist x Fem!Experiment Reader
Bunni’s Monstertober Event
Oct 18th
Oct 17
Oct 19
summary: when a vampire needs a source of unlimited blood, he turns to science. You’re his experiment, and a bit spoiled…
warnings: blood drinking, cock warming, male lead is a bit manipulative
a/n: shut up if I have any spelling mistakes 🙏 I’m trying to catch up

You let out an annoyed whine as he poked his head into your room. You were in the middle of a movie, eating a snack.
“Darling~”
He walked in, throwing his lab coat aside and jumping into your bed. The man had a habit of coming to you after a long day in the lab, being clingy and over baring.
“H-hey, don’t jump in my bed before you wash up!”
You pouted, squirming as he pulled you on his lap and rubbed his cheek against your neck.
“Oh, don’t fuss my dear… you know I just adore you, it’s hard to stay away for long.”
Before you could whine anymore, he moved his hand between your thighs, pressing against your wet panties.
“Don’t you remember who saved you? Who’s spoiled you rotten?”
You did remember.
Before you had been living on the street, hungry and barely hanging on. One night you were caught in the middle of a shoot out, and nearly died from blood loss,
He found you curled up in an alleyway, buried beneath trash and filth. You had already died, not even turning you into a vampire could bring you back…
So he used the knowledge he had gained from his research so far from both science and witchcraft to give you life.
One of the side effects was that you overproduce blood, and had to be drained daily. It was a happy surprise, and he decided to keep you for himself as his blood bag.
You were kept in a sterile section of his lap, your bed a plain cot and your food some sort of nutritional mush.
It was hardly the place for a girl… but it would do. You were just an experiment, after all.
That had been his idea at first, to keep you in his laboratory and feed from you every once in a while… but he grew fond of you quickly.
A room was decorated with your interests in mind, and he made sure you were comfortable and had everything you could ever want.
You were almost like his doll, something he could play with when he was bored. He dressed you up, kept you in a pretty room… you were his perfect, pretty little doll.
That’s what he told himself. In all reality, he truly cared for you. Once you bring someone back from death and care for them for months while they recover, you become fond of that person and want to see them thrive.
As he thought this over, your memory was a bit different.
You reached out for him to help you, and he carried you back to his lab himself, not caring that you were dirty and smelled of decay.
Your spirit watched as he carefully cleaned and stitched up your broken body, his hands gentle and caring. Even though you were simply a corpse, he still dressed you and placed a pillow under your head while he researched ways to save you at his desk.
When you woke up in your body, you were in something much softer than the ground you slept on every night. Every day you ate until you were full, and always had energy to walk around.
You weren’t hungry or cold or dirty anymore… that was enough for you, but he gave you even more! A room just for you, dressed and games and books and all the attention and love you could ever ask for…
But it was so hard to accept all of this, to really give in to being spoiled. Especially when you were crushing this hard on him…
His fangs brushed against your neck as he slipped the silk panties he bought for you aside. Lately his affections had turned from platonic to sexual, and he had been toying with you a lot.
Experimenting.
“I see… this is how wet you get when I rub here, hmm?”
He licked along your neck, eyes on your fat cunt as he flicked your clit, causing you to yelp and your hips to buck.
“H-hey…”
His cock hardened when you squirmed, your plump ass moving against his hard on. “That hurts…”
You were pouting, your face warm and flustered.
“So cute…”
He lifted your hips with ease, his cock rubbing against your cunt before he slowly lowered you into it.
Though you’d never taken cock before, he had been slowly stretching you out for weeks now, pumping his fingers in and out of you, getting you ready to take him.
You could only whine and whimper, embarrassed that it felt so good. You attempted to move, but he kept you still, his fingers toying with your clit.
“Relax, love…”
His fangs sunk into your neck, causing you to wiggle and writhe in mild discomfort, which made his cock twitch inside of you. The man continued to stimulate your clit as he fed from you.
Your soft body felt warm against him, and having your blood flowing through his felt intimate. You were connected in a way no one else could be.
As he finished up his feeding, he began lightly bouncing you, letting you ride out your orgasm as his cum spurted into your womb.
Afterwards you were tired and a bit cranky from the blood loss, so he carried you to a bath and washed you up before tucking you into bed.
Why did he do so much for you? He wasn’t sure… but you knew.
He loved you, his little experiment had become his mate and he hadn’t even noticed yet.
want more of this? my commissions and kofi are open!
——————
NSFW TAGLIST: @sunset-214 @strawberrypoundtown @avalordream @icommitwarcrimes @bazpire @im-eating-rn @anglingforlevels @kinshenewa @pasteldaze @unforgettablewhvre @yoongiigolden @peachesdabunny @murder-hobo @leiselotte @misswonderfrojustice @dij-ology @i8kaeya @lollboogurl @h3110-dar1in9 @keikokashi @aliceattheart @mssmil3y @spicyspicyliving @namjoons-t1ddies @izarosf1833 @healanette @lem-hhn @spufflepuff @honey-crypt @karljra @zyettemoon1800 @exodiam @vexillum-moeru @imperfectlyperfectprincess1 @binnieonabike @enchantedsylveon @mysticranger575 @readeryn68 @danielle143 @kittenlover614 @filthybunny420 @annavittoria-mm @makimamybelovedwife @blubearxy @omglovelylaila @toocollectionchaos-universe-blog @fruk-you-usuk-fans @wil10wthetree @hammerhead96-blog @slightlyusedfloormat
#vampire x you#vampire x reader#vampire x human#vampire smut#vampire boyfriend#monster fucker#monster lover#monster fudger#monster boyfriend#monster fic#ask answered#chubby!reader#chubby reader#x reader#terato#fem reader#teraphilia#terat0philliac#exophelia#female reader#teratophillia#monster smut#monster boy oc#monster fucking#fat reader#monster imagine#monster bf#monster x human#plus size reader
1K notes
·
View notes
Note
🔸hello👋
🔸to all suppourter at the world 🫂
🔸my name is hilda am from gaza🥺
🔸I am pregnant and living in diffic soult conditions here😥
🔸The doctor told me that the baby is small in size due to a lack of nutrition.😭
🔸 We need $30 to $50 daily to ensure the safety of my pregnancy and my family🙏
➡️https://gofund.me/69d9ed7c
🛑💵1 donation last 3 days
✅#am vetted
🟢@gaza-evacuation-funds
🟢@bilal-salah0
🟢@dlxxv-vetted-donatios
🟢@ana-bananya
🟢@khanger
🟢@a-shade-of-blue
#hildanasr5#palestine#free palestine#free gaza#gaza#gaza strip#gaza genocide#gazaunderattack#save palestine#palestinian genocide#gaza gofundme
25 notes
·
View notes
Note
🔸hello👋
🔸to all suppourter at the world 🫂
🔸my name is hilda am from gaza🥺
🔸I am pregnant and living in diffic soult conditions here😥
🔸The doctor told me that the baby is small in size due to a lack of nutrition.😭
🔸 We need $30 to $50 daily to ensure the safety of my pregnancy and my family🙏
➡️https://gofund.me/69d9ed7c
🛑💵1 donation last 3 days
✅#am vetted
🟢@gaza-evacuation-funds
🟢@bilal-salah0
🟢@dlxxv-vetted-donatios
🟢@ana-bananya
🟢@khanger
🟢@a-shade-of-blue
Vetted here as #6 (LOW ON FUNDS)
#palestine#gaza#mutual aid#signal boost#vetted fundraiser#palestine gfm#palestine gofundme#palestine genocide#save palestine#free palestine#i stand with palestine#gaza genocide#free gaza#gaza strip
20 notes
·
View notes
Text
DOVE VA A FINIRE L’ amore QUANDO FINISCE?
- Come faccio - mi chiese -
A lasciarlo andare ? Non vederlo piu’, non sapere piu’ niente di lui .
- perché devi figlia- rispose la curandera guardando verso l’antica quercia .
- vedi , nulla davvero ci appartiene ma chi abbiamo amato ha mescolato con noi il suo corpo astrale .
- che significa?
- che vi siete intrecciati come i rami dell’edera , ma non nel corpo , quello e’ momentaneo, nello spirito .
- ma a me non basta .
Sto male , voglio ancora vederlo e toccarlo e parlargli .
Non ce la faccio .
- non ce la devi fare - rispose sorridendo la donna di cui nessuno conosceva l’ eta’ .
- non ce la devi fare perché non sei tu a decidere : l’amore improvvisamente e senza merito arriva , come un canto di uccelli a mezzanotte .
E cosi’improvvisamente e senza motivo se ne va .
Ma non finisce mai.
Continua in quest’ altra dimensione .
- quale dimensione ?
Chiede la ragazza soffiandosi il naso avvolto dalle lacrime .
- la dimensione dell’invisibile. Dove vivono i maestri, i sacri spiriti, gli esseri di luce e le forze superiori .
I vostri spiriti congiunti e intrecciati salgono su fino a li , fino a diventare impercettibili e tuttavia continuano a vivere .
Vedi cara : l’umano non accetta che cio’ che può vedere e’ pari a un granello di sabbia a confronto dell’oceano.
- sto iniziando a capire ma fa ancora male .
- lo so bambina .
Non scacciare il demone del dolore : ogni volta che il cuore si spacca, si allarga un po’ di piu’ ma solo se lo lasci fare.
Se respingi, fingi , rigetti indietro, ti stordisci con le frivolezze , ritornera’ piu’ forte e ti chiudera’ il cuore .
E un cuore chiuso, e’ cio’ che di peggio puoi dare al mondo .
- gia’ in passato , Signora ho chiuso il mio cuore per non soffrire piu’ ed e’ stato sempre peggio !
- certo! Dimorare nelle tenebre e nella paura non e’ mai bene cara .
Non cercare di capire il dolore , lascia che ti travolga come un’onda, fatti lieve come piuma , lasciato attraversare come burro , ma se chiudi il cuore allora i demoni danzeranno sul tuo petto e ne’ gioia ne’ dolore toccheranno piu’ il tuo ventre .
E questo equivale a morire .
- si , ho capito .
Ho capito che essere forti significa stare 5 passi indietro.
Lo lascero’ andare ...
- domani sera , con la luna piena, da sola , vai in collina e pianta un ulivo .
Le sue foglie argentate saranno nutrite dalla tua leggerezza .
Qualcosa crescerà da questo strappo ma solo se lasci che la luce lo disinfetti .
E cosi sara’ per la pianta .
E la ragazza ando’ .
Con la luna calda di agosto a piantare il suo amore finito tra o cespugli di ginestra .
Scivolo’ dentro se’ per un po’
E la curendera non la perse mai di vista .
Da lontano, la vedeva con l’ occhio interiore e lei inviava ogni sera gli spiriti del bosco a vegliarle il sonno ...
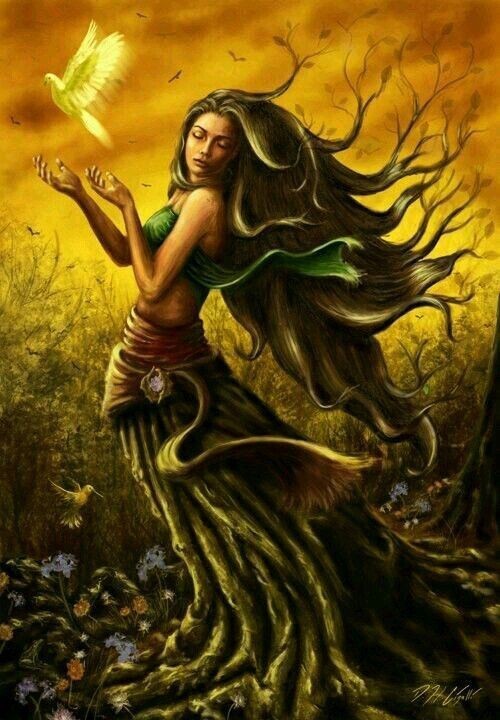
Testo originale di
ClaudiaCrispolti
26 notes
·
View notes
Note
🔸hello👋
🔸to all suppourter at the world 🫂
🔸my name is hilda am from gaza🥺
🔸I am pregnant and living in diffic soult conditions here😥
🔸The doctor told me that the baby is small in size due to a lack of nutrition.😭
🔸 We need $30 to $50 daily to ensure the safety of my pregnancy and my family🙏
➡️https://gofund.me/69d9ed7c
🛑💵1 donation last 3 days
✅#am vetted
🟢@gaza-evacuation-funds
🟢@bilal-salah0
🟢@dlxxv-vetted-donatios
🟢@ana-bananya
🟢@khanger
🟢@a-shade-of-blue
This is urgent! Please don't ignore them! Don't scroll! Reblog, share and if possible donate!
#all eyes on gaza#gaza genocide#free gaza#gaza strip#gaza#free palstine#all eyes on palestine#palestine fundraiser#save palestine#save gaza#palestine
3 notes
·
View notes
Text
Perspective of an ex FA
Trigger warning - mention of disordered eating, depression.
Disclaimer- I do not endorse bullying or body shaming fat people. Bullies need to be shamed and don't deserve any place in the current society.
Coming to my story. I consider myself a feminist who also sways on the left side of the political spectrum. I was very skinny as a kid, but due to puberty-related changes, I gained quite a bit of weight but was still in the healthy range. I started to gain weight in 2019 when my final year of high school hit - due to the pressure of performing well in the exams. Stress made me gain weight and the sedentary lifestyle during 1.5 years of lockdown added to that.
During lockdown, I started being more online in feminist spaces, and while I greatly appreciate the work they do, I couldn't help but notice the growing wave of weight-related content. What was meant as a "Women don't owe you being skinny" or "People shouldn't get bullied for gaining weight" morphed into a "Working out is fat phobic as it endorses skinniness" rhetoric. I fell for that, as a lot of my online friends and influencers peddled that rhetoric. Yes, nobody owes health to anyone but themselves.
I stopped exercising, ate my cravings away and led a very sedentary lifestyle. My anxiety and depression just added to it and soon I no longer felt happy. I felt unhealthy every time I ate greasy foods, I felt like I was hollow from within and that there were deeper issues that I failed to address and instead resorted to binge eating.
Soon the comments from concerned relatives and parents started to pour in and I fell into the victim mindset - I.e. it is their problem and that they have 'internalized fatphobia' thus I shouldn't take care of myself, and instead 'do what my body wants.' I started viewing everyone healthy as "fatphobes" who were missing out on food and it didn't help that the old therapist I had didn't recognize my binge eating (she was an old lady and not very "woke" either). For almost 3 years I believed that I was a victim of fat-phobic people who couldn't see me the way I am. I fully believed that I shouldn't work out or walk or play sports because "it confirms to the body standards."
What was a wake-up call for me was when I noticed that I was jealous of all the pretty girls masked as "they have internalized whatever." I saw girls who took care of themselves and worked out as "weapons of the system" even if they never said anything to me personally. I wanted to look like them but deep down I knew I wasn't willing to put in the effort. What hit me was when I asked myself "Girl, you're depressed. If you listened to your body - you would've jumped off the 13th floor" and that is when the rhetoric started to fall apart. I did courses in nutrition as a part of my curriculum and realized that - obesity is not healthy and that there is a difference between being curvy versus being obese.
I learned the scientific basis of why people with obesity are more prone to getting heart attacks, cancer, strokes and a ton of diseases. It wasn't just an "internet speech" but it had scientific evidence supporting it. It was a harsh wake-up call. Being healthy is not for aesthetics (which comes as a side benefit) but for longevity, for leading a fulfilled life. People don't work out because they want to look good (which is a perfectly valid reason btw) but because having a toned body means reduced unhealthy fats, and a healthy heart, and the body isn't going for an override. There was a saying that my teacher said "Our body works 24/7 for us, we can give it 1 hour of exercise back" and that struck. Once I read about the benefits of exercise for the body machinery, I realized how much misinformation is being peddled and how so many people are being lured into an unhealthy lifestyle in the name of destroying the status quo.
FA's have a modus operandi of cherry-picking scientific information or spreading pseudo-science to push their narrative. "Fat people have decreased risk of a particular type of cancer" while ignoring other types of cancers that you are at risk of if you're overweight. They will weaponize the struggles of people with legitimate hormonal issues into "If you can't lose weight it means you have hormonal issues" or my favorite "People who lose weight gain it back" without going into the reason why they gain it back. They present weight as something you cannot control whereas it is something largely in your control. They make you think that you have hormonal issues, even if that is not the case. The truth is even for people with hormonal issues or PCOS - it is difficult to lose weight, not impossible. It may take them more time to lose weight but they certainly do if they persevere. CICO has been working perfectly fine for me and in a matter of one month I have lost 4 kgs. (I am 5'3 and was 70 kgs - so not obese but overweight). They make you think if you track calories, you are encouraging ED, when in reality being on a severely restrictive diet of less than 1000 calories is ED. A healthy toned body is not the same as the anorexic bodies that were for some weird reason pushed as the beauty standard back in the 1990s.
I realized I no longer wanted to live in a state of self-pity and self victimization because I got concerned comments from people, or my favorite clothes no longer fit me. I no longer wanted to justify my feeling miserable by "owning the system." I wanted to feel like one of those girls and I am willing to put in the effort. I minimized eating out, did workout and strength training, tracked my calories and if I felt like eating junk - I shared the portion with my mom or I ordered half a plate. Because I realized I was craving the taste and not the whole plate of it and a little bit of tasting it(within calorie limits) satisfied my cravings instead of gobbling down the whole plate and feeling miserable. So the moral of the story is - weight is in your control, weight loss can be fun and YOU DON'T OWE BEING HEALTHY TO ANYONE BUT YOUR BODY WHICH IS WORKING TIRELESSLY FOR YOU. Being healthy is being toned, having low body fat, having more than a BMI of 18 and less than 25 and having good stamina.
6 notes
·
View notes
Note
🔸hello👋
🔸to all suppourter at the world 🫂
🔸my name is hilda am from gaza🥺
🔸I am pregnant and living in diffic soult conditions here😥
🔸The doctor told me that the baby is small in size due to a lack of nutrition.😭
🔸 We need $30 to $50 daily to ensure the safety of my pregnancy and my family🙏
➡️https://gofund.me/69d9ed7c
🛑💵1 donation last 3 days
✅#am vetted
🟢@gaza-evacuation-funds
🟢@bilal-salah0
🟢@dlxxv-vetted-donatios
🟢@ana-bananya
🟢@khanger
🟢@a-shade-of-blue
2 notes
·
View notes
Text

Altre cose da fare giornalmente se si pratica yoga: 6. Se viene in mente un’azione gentile, farla Se l’hai pensata vuol dire che è fattibile. Uno yogi non si tira indietro perché “può sembrare brutto o strano”. Yoga è azione. L’azione gentile è un seme nel cuore di chi lo riceve.
7. Rispettare lo spazio che ci circonda Uno yogi lascia un luogo migliore di come lo ha trovato riuscendo a renderlo sempre più bello. Lo abbiamo già scritto, ma ci teniamo a ribadirlo.
8. Pulire spazio ed energia dietro di sé La pulizia di un corpo è igiene. La pulizia di uno spazio è amore. La pulizia dell’energia è un regalo.
9. Dire Grazie Questa parola così piccola e piena di significato è sempre sulla bocca di uno yogi. Qualsiasi cosa accada è un insegnamento. Rafforza le emozioni, il carattere e tutte le relazioni in generale.
10. Lasciare la tecnologia per 10 minuti al giorno Uno yogi vero sa apprezzare un panorama senza doverlo fotografare. Prova a staccarti dagli altri e ricollegarti a te stesso.
Senza dimenticare un’altra cosa da fare se si pratica yoga. Una importante… 11. Mangiare sano Uno yogi si prende cura degli altri, dello spazio, delle relazioni, e tra tutto questo lo spazio interno e la relazione con se stessi gioca un ruolo molto importante. Mangiare sano, quello che ci fa sentire bene ha un alto valore non solo per la salute, ma anche per come ci muoviamo nella vita.
Un radicale cambio di alimentazione per stare meglio porta con sé la consapevolezza dei limiti e delle potenzialità del proprio corpo. Un’alimentazione sana ed equilibrata è componente fondamentale per una pratica olistica come lo yoga: il cibo che fa bene a chi pratica yoga deve dare il giusto apporto energetico ai muscoli coinvolti negli esercizi e, nel contempo, secondo i principi dell’alimentazione ayurvedica, influenzare positivamente le emozioni. eventiyoga.it art by_detelina_ ************************ Other things to do daily if you practice yoga: 6. If a kind action comes to mind, do it If you have thought of it, it means that it is doable. A yogi does not hold back because "it may seem bad or strange". Yoga is action. A kind action is a seed in the heart of the one who receives it.
7. Respect the space around us A yogi leaves a place better than he found it, managing to make it more and more beautiful. We have already written this, but we want to reiterate it.
8. Clean space and energy behind you Cleaning a body is hygiene. Cleaning a space is love. Cleaning energy is a gift.
9. Say Thank You This small and meaningful word is always on the lips of a yogi. Whatever happens, it is a teaching. It strengthens emotions, character and all relationships in general.
10. Leave technology behind for 10 minutes a day A true yogi knows how to appreciate a view without having to photograph it. Try to detach yourself from others and reconnect with yourself.
Without forgetting another thing to do if you practice yoga. An important one… 11. Eat healthy A yogi takes care of others, of space, of relationships, and among all this, internal space and the relationship with oneself play a very important role. Eating healthy, what makes us feel good has a high value not only for health, but also for how we move in life.
A radical change in diet to feel better brings with it the awareness of the limits and potential of your body. A healthy and balanced diet is a fundamental component for a holistic practice like yoga: the food that is good for those who practice yoga must give the right energy supply to the muscles involved in the exercises and, at the same time, according to the principles of Ayurvedic nutrition, positively influence emotions. eventiyoga.it art by_detelina_
2 notes
·
View notes
Text
L'attività fisica i cui benefici per il cervello sono universalmente riconosciuti dagli scienziati è, paradossalmente, la più semplice di tutte: camminare. «Rafforza le connessioni tra i circuiti cerebrali, che sono importanti per l'elaborazione delle emozioni, la risoluzione dei problemi e la memoria», fa notare Nas. La sincronizzazione di queste reti cerebrali è stata associata a una riduzione del rischio di Alzheimer. Secondo un recente studio condotto dal Programme National Nutrition Santé francese (PNNS), 20 minuti al giorno a passo moderato possono addirittura modificare in meglio la struttura del cervello. «Camminare tre volte alla settimana per 20 minuti ispessisce il tessuto che collega la parte destra e quella sinistra del nostro cervello», conferma Nas. «Questo cambiamento porta a un potenziamento della memoria». Una passeggiata di 20 minuti, inoltre, può accrescere notevolmente l'attività cerebrale, l'attenzione e la concentrazione e migliorare i tempi di reazione, spiega la dottoressa Swart, secondo la quale, ogni volta che siamo a corto di concentrazione, dovremmo fare una breve passeggiata, anziché bere un caffè. Infine, camminare ha un effetto benefico sulla salute mentale, in quanto rallenta l'attività delle parti del cervello coinvolte nella risposta allo stress.
Dall'articolo "Mantenere il cervello giovane e attivo? Bastano 2 facili attività quotidiane. Lo dice la neuroscienza" di Marie Bladt
2 notes
·
View notes
Text
annual recurrent flight attendant training day 1/2 [08-19-24]




day 1 of my annual FA training is complete.
• first aid [practical]
• first aid [written]
• opening/closing exam of the eight aircrafts in our fleet [practical]
• emergency evacuation procedures [practical]
• standard operational procedures exam open/closed book [written]
• location/safety/security aircraft knowledge exam [written]
• fire extinguisher / drager smoke hood firefighting exam [practical]
• unruly passenger restraining exam [practical]
• oxygen bottle & mask application & usage exam [practical]
• medipak usage exam [practical]
all passed 90% or over.
highlights
• have the same training days as a colleague who I got hired with last year, who is one of the funniest people I've ever met. Helped ease any nerves I had
• during first aid in pairs, one of my friends/colleagues was committed to his role of "the injured patient". It was so painfully overly dramatic, I cried tears of laughter
• ran into my role model at the company ! hadn't seen him since 2023 and missed him dearly. he is currently climbing the corporate ladder with no sign of slowing down, was so nice to see him. Had a huge smile on my face the whole interaction
• got the taste of healthy stress again in an educational environment. It is great fuel
• made me that much more excited to go back to college in a couple of weeks
what I ate
• breakfast - yogurt & granola bowl + ginseng stick
• lunch - grilled cheese
• dinner - falafel veggie wrap
final thoughts
overall a packed day, but was happy to get the more difficult exams out of the way. It's a lot easier to be friendly and sociable in a classroom environment, than on the actual job, due to the trainings calm nature.
I am grateful for the way FA training is formatted, and allows me to cram for many exams within one day. It makes going back to college feel a lot less daunting.
I want to do some research regarding how nutrition can positively impact female hormones throughout the day. I always feel lethargic when I have to attend a class after lunch (12:30-3:30), even if I haven't eaten right before. I'd love to converse with people who study these subjects, or possess this knowledge due to their field of study.
I am a bit nervous for tomorrow, because we blend with the pilots for training for "crew resource management". It helps to enhance the quality of communication amongst each other, so we will be able to work together more efficiently. It's a bit intimidating !!
Im going to do my review for a couple of hours, then go to bed early so that I can complete most of my review after a solid rest.
have a good night every one :)
#flight attendant#training#cram#cramschool#college life#study blog#studyspo#studying#study motivation#academia#lifestyle#it girl#healthyliving#nutrition#flying#travel
4 notes
·
View notes
Text




Hello 👋
I am Doaa from Gaza 💔 I live with my elderly parents under very difficult conditions due to the war. With my brothers and my young child, whom I gave birth to during the war, we were displaced to the south and live in a narrow tent. My parents need medical care and medications that I cannot provide due to the current situation. My child needs nutrition and healthy food Please help
👇
Despite my efforts, I was unable to raise enough donations to meet our basic needs. We desperately need your support, and even small donations can make a big difference in our lives.
2 notes
·
View notes
Text
5 Fast-Food Meals That Are High in Protein and Less Than 600 Calories
If you’re trying to lose weight, one of the challenges you’ll face is what to do about those times when you find yourself at a fast-food restaurant. The offerings at these establishments are typically incredibly high in calories. A Big Mac meal at McDonald’s can set you back 1,300 calories. Damn! If your calorie goal for the day is 2,400 calories, that’s more than half your daily calories in a single meal. The typical advice for people losing weight is to just avoid fast-food restaurants altogether. And with some preparing, thinking ahead, and good decision-making, you can accomplish that most of the time. But not 100% of the time. Sometimes, life throws a wrench in your plans. Maybe you’re on a road trip, and your friends decide to stop at Carl’s Jr. for lunch. Maybe your kid’s soccer team decided to go out to dinner to Chick-fil-A after the game. Maybe you’re just really pressed for time and need to grab something fast at a drive-thru on the way from work to another engagement. What to do? Well, what if I told you you don’t have to choose between convenience and your fitness goals? You can have your fast-food burger and eat it too—all while staying on track with your weight loss. When you want to lose weight, you want to choose foods that are lower in calories and higher in satiating, muscle-building protein. Thankfully, most fast-food restaurants now offer options that meet this criteria. With a bit of creativity, you can easily select meals at pretty much all the major fast-food restaurants that will give you 30+ grams of protein (which is a good minimum goal for a meal) and only clock in at around 600 calories. Below, we provide some suggestions for meals that meet these metrics that you can get at five popular fast-food restaurants. One thing to keep in mind is that while you can reduce the calories in your fast-food orders, it’s hard to reduce the amount of sodium. These are going to be sodium bombs. So they’re not great for everyday dining, but they’ll do in a pinch. Whether you’re looking to shed a few pounds or maintain your hard-earned gains, this guide will show you how to navigate the pitfalls of fast-food menus and stay on track with your goals. General Guidelines to Keep Your Fast-Food Meals Lower in Calories Before we get into specific meals, here are some general guidelines to follow that will allow you to keep your meals lower in calories, regardless of the fast-food establishment you visit: * Food tracking apps like MyFtinessPal are your friends. I use the app all the time when I’m at fast-food restaurants. Quickly look up the calorie and macro count of foods and piece together your meal with that info. * Choose grilled over fried meats. * Choose lean proteins. While you can still enjoy a beef burger, protein sources like turkey or chicken breast generally have fewer calories. * Ask for extra protein. Adding extra protein, like extra meat, can help increase satiety while keeping calories low. * Skip the fries. If you’re looking for a side, get fruit or salad instead. Also, hot take: fries aren’t that good anyway! * Skip the high-fat sauces, dressings, and condiments. Ask for lower-calorie options instead. * Load up on veggies. Satiety is premised in part on volume; calorically dense foods won’t fill you up and will leave you feeling hungry. To increase volume and nutrition, add low-calorie veggies to your meals like extra lettuce, tomatoes, and onions. * Choose water or unsweetened drinks like diet sodas. Finally, don’t be afraid to enjoy yourself with a no-holds-barred high-calorie fast-food meal every now and then. I love getting a double cheeseburger on occasion. You can just adjust your macros and calories accordingly and eat less the rest of the day. Or just chalk it up to an anomalous indulgence, and get back to your diet the next day. You don’t have to eat perfectly 100% of the time to still lose weight and stay healthy. Fast-Food Meals That Are 600 Calories or Less With More than 30 Grams of Protein McDonald’s… http://dlvr.it/TBgWkR
2 notes
·
View notes
Text
L'essere femminile è fatto per ricevere, accogliere. Una volta stabile questo, esso si apre come una fontana e nutre in abbondanza. Altrimenti sarebbe malsano, sofferenza.
Perció uomini, esseri maschili, nutrite le vostre donne come regine. Donate voi stessi pienamente.
Non chiedete loro niente. Siete voi a dover dare i vostri frutti, che avete seminato e coltivato con amore.
Loro lo accoglieranno e con amore se ne prenderanno cura.
Sapranno versare il loro amore, nel momento in cui il vostro cuore sarà capace di darlo.
Il nostro amore infinito sgorga dall'interno, se le svuotate chiedendo, pretendendo non resterà piú niente. Soprattutto a loro.
Non si fideranno piú dell uomo, saranno infelici e voi approfitterete di questa debolezza e chiederete ancora di piú e se loro non ve lo possono piú dare perché non c'è, voi lo chiederete a qualcun altro.
Ma se tutti facessero cosí, morireste di fame.
Cari uomini, pensateci prima di voler qualcosa da qualcuno.
Pensate realmente a cosa state facendo.
Se solo siete abituati ad arrangiarvi e a dare piuttosto che a prendere vi accorgerete che molte cose si apriranno al meglio.
Loro non vi devono niente e questo moto innaturale è contro le leggi della vita.
Potreste mostrare un pó di rispetto e con dare non intendo rose e gioielli. Nessun umano si nutre con petali e metallo.
Dare è inteso come aprirsi alle proprie vulerbilità e accettarle come tali, saperle condividere e aprezzare con lei.
Ascoltare con amore e interesse sincero.
Trattare con degna nota il vostro sè, cosí anche la donna.
Perché sappiamo che l'idea media che si ha di una donna è quella che pulisce casa e cucina, fa la madre e si fa in 10 per tutti, ma è proprio questo che deve finire.
A nessuno piace distruggersi per amore degli altri.
Ovviamente sono daccordo che certe donne devono imparare l'amor proprio, ma chi ha mai detto che la donna è questo? La donna è molto di piú di una credenza abituale dettata dagli stereotipi.
Ritrovare il proprio lato femminile, creativo, empatico, accogliente, vi aiuterà ad avvicinarvi a loro e a comprendere quelle cose che disprezzate, temete, non capite, è uguale, sempre stato fa che siete distanti e le donne non sono solo dei gioielli o delle amanti dello shopping.
Potete capire quale potere inestimabile risiede in esse, appunto conoscendo prima in voi stessi quella parte rinnegata, sottomessa e maltrattata da ormai generazioni, millenni, fa parte della storia e della cultura, ma, concepiamo il fatto che, una donna felice nella storia io non l ho vista fin ora.
Quindi cari uomini fate i vostri conti e risarcite i vostri debiti.
Grazie.
Cordialmente
Una donna
8 notes
·
View notes
Text
Una codina di dietro

Gli eucarioti sono quel gruppo di esseri viventi dotati di cellule con all'interno un nucleo contenente il DNA. Noi animali ne facciamo parte, così come le piante, i funghi e molti altri organismi unicellulari. Esclusi i batteri e gli archea, che sono procarioti: organismi unicellulari privi di nucleo. Per cui, nei procarioti, il DNA gira libero nell'intera cellula.
Bene, moltissimi organismi, eucarioti e procarioti, possiedono, almeno in uno stadio della propria vita, cellule che hanno la capacità di muoversi utilizzando una specie di microscopica codina, il cosiddetto flagello.
In moltissimi di questi organismi il flagello, o più di un flagello, è posto anteriormente. Quindi il movimento di questa codina trascina in avanti la cellula.
In un particolare gruppo di eucarioti, invece, ad un certo punto della storia della vita sulla Terra, comparve un flagello che funzionava al contrario, spingendo la cellula anziché trascinarla.
Questo gruppo è stato chiamato Opisthokonta, dall'unione di due parole greche: "opísthios" cioè retro, posteriore, e "kontós" ovvero polo, cioè flagello. Ovvero quelli con una codina di dietro.
Chiaramente ci sono opistoconti unicellulari che possiedono il flagello per tutta la vita, altri che invece ce l'hanno solo in alcuni stadi, come noi e i funghi. Questi ultimi, che quindi sono molto più imparentati a noi che alle piante, possiedono questa codina di dietro quando producono le spore. Noi quando produciamo gli spermatozoi, che tecnicamente non sono altro che la primissima e incompleta fase della vita di un individuo adulto.
I vantaggi di questa innovazione, avvenuta sicuramente più di un miliardo di anni fa, sono stati notevoli. Essere una cellula spinta, anziché trascinata, fa risparmiare energia, aumenta l'agilità, permette un più semplice sviluppo di organi sensoriali e meccanismi di cattura del cibo. Mentre, sul retro, la codina reagisce agli stimoli sensoriali e avvicina la cellula alle sostanze nutritive.
Le innovazioni nell'evoluzione degli opostoconti da quel punto in poi sono state innumerevoli, è chiaro. Ma è bello pensare che, da un certo punto di vista, la storia della vita sulla Terra si può riassumere con la seguente timeline formata da poche fondamentali pietre miliari:
niente codina > codina davanti > codina dietro > scienza aerospaziale.
3 notes
·
View notes
Text
DOVE VA A FINIRE L’ amore QUANDO FINISCE?
- Come faccio - mi chiese -
A lasciarlo andare ? Non vederlo piu’,non sapere piu’ niente di lui .
- perché devi figlia- rispose la curandera guardando verso l’antica quercia .
- vedi , nulla davvero ci appartiene ma chi abbiamo amato ha mescolato con noi il suo corpo astrale .
- che significa?
- che vi siete intrecciati come i rami dell’edera , ma non nel corpo , quello e’ momentaneo, nello spirito .
- ma a me non basta .
Sto male , voglio ancora vederlo e toccarlo e parlargli .
Non ce la faccio .
- non ce la devi fare - rispose sorridendo la donna di cui nessuno conosceva l’ eta’ .
- non ce la devi fare perché non sei tu a decidere : l’amore improvvisamente e senza merito arriva , come un canto di uccelli a mezzanotte .
E cosi’improvvisamente e senza motivo se ne va .
Ma non finisce mai.
Continua in quest’ altra dimensione .
- quale dimensione ?
Chiede la ragazza soffiandosi il naso avvolto dalle lacrime .
- la dimensione dell’invisibile. Dove vivono i maestri, i sacri spiriti, gli esseri di luce e le forze superiori .
I vostri spiriti congiunti e intrecciati salgono su fino a li , fino a diventare impercettibili e tuttavia continuano a vivere .
Vedi cara : l’umano non accetta che cio’ che può vedere e’ pari a un granello di sabbia a confronto dell’oceano.
- sto iniziando a capire ma fa ancora male .
- lo so bambina .
Non scacciare il demone del dolore : ogni volta che il cuore si spacca, si allarga un po’ di piu’ ma solo se lo lasci fare.
Se respingi, fingi , rigetti indietro, ti stordisci con le frivolezze , ritornera’ piu’ forte e ti chiudera’ il cuore .
E un cuore chiuso, e’ cio’ che di peggio puoi dare al mondo .
- gia’ in passato , Signora ho chiuso il mio cuore per non soffrire piu’ ed e’ stato sempre peggio !
- certo! Dimorare nelle tenebre e nella paura non e’ mai bene cara .
Non cercare di capire il dolore , lascia che ti travolga come un’onda, fatti lieve come piuma , lasciato attraversare come burro , ma se chiudi il cuore allora i demoni danzeranno sul tuo petto e ne’ gioia ne’ dolore toccheranno piu’ il tuo ventre .
E questo equivale a morire .
- si , ho capito .
Ho capito che essere forti significa stare 5 passi indietro.
Lo lascero’ andare ...
- domani sera , con la luna piena, da sola , vai in collina e pianta un ulivo .
Le sue foglie argentate saranno nutrite dalla tua leggerezza .
Qualcosa crescerà da questo strappo ma solo se lasci che la luce lo disinfetti .
E cosi sara’ per la pianta .
E la ragazza ando’ .
Con la luna calda di agosto a piantare il suo amore finito tra o cespugli di ginestra .
Scivolo’ dentro se’ per un po’
E la curendera non la perse mai di vista .
Da lontano, la vedeva con l’ occhio interiore e lei inviava ogni sera gli spiriti del bosco a vegliarle il sonno ...
Testo originale di
_ClaudiaCrispolti_
Proprietà letteraria riservata:
NOTA BENE Primo: non ho mai letto la profezia della curandera
Secondo questo racconto breve e’ un Mio pezzo originale scritto nel 2020
Vi prego di NON spargerlo in giro sotto falso nome
I miei post sono firmati e protetti da diritto di autore.
4 notes
·
View notes