#Chronic subdural hematoma
Explore tagged Tumblr posts
Text
Spontaneous Disappearance of an Arachnoid Cyst after appearance of chronic subdural hematoma by M.Hammoud in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Background: Arachnoid cysts are benign extra axial lesions, most commonly located in the fronto temporal region and account for 1% of all intracranial masses. They may remain stable or they may grow in size over time. Reports of spontaneous disappearance of arachnoid cysts are rare.
Case Report: We report the case of a 1-year-old boy with a middle fossa arachnoid cyst revealed by convulsive seizures, managed with anti epileptic drugs, 13 months later, the patient had one seizure episode, the cranial computed tomography Scan showed nearly total disappearance of the arachnoid cyst and the appearance of subdural hematoma. No surgical intervention was performed. Follow-up CT scans 1 month after admission, showed total disappearance of both the arachnoid cyst and the subdural hematoma.
Keywords
Arachnoid Cyst, Subdural hematoma, Spontaneous Resolution
Introduction
Arachnoid cysts are rare benign congenital extra axial lesions, which consist of collection of cerebrospinal fluid (CSF) surrounded by normal arachnoid membrane.
They account for approximately 1% of all intracranial space-occupying lesions, with a higher prevalence in the first 2 decades of life [1].
Most arachnoid cysts are quiescent and remain asymptomatic throughout life.
They are incidentally detected on CT or magnetic resonance images [2].
The cyst may progress, stabilize, or spontaneously regress [3,4].
Spontaneous regression of an AC has been rarely reported in the literature [5,6].
In our knowledge, this is the second reported case of spontaneous disappearance of cerebral arachnoid cyst in less than 2 year [7].
Case report
A 1-year-old boy was admitted to pediatric emergency department for two episodes of non-febrile generalized seizure. On clinical exam, there was no focal neurological abnormality, cranial nerve deficit or papilledema. His head circumference was normal.
Brain magnetic resonance MR imaging showed a well defined, no enhancing, extra-axial cystic lesion in the right frontotemporal region, between the tabula interna and the insula. The lesion is isointense to CSF on T1 and T2 weighted images (Figure 1). This fluid collection suppresses completely with FLAIR and shows no restriction on DWI. The diagnosis of a right frontotemporal arachnoid cyst was made.
We decided not to operate the patient; he was putted under antiepileptic drug,
At 2-months follow-up, the patient was doing well and was seizure-free.
13months later, the patient was presented with another seizure episode; there was no cranial trauma. The neurological examination was unremarkable.
Unexpectedly, the brain CT scan showed a subtotal resolution of the arachnoid cyst with a subdural hematoma on the same side.
We decided to observe the patient without surgical intervention.
At 1-month follow-up, the CT scan control showed total disappearance of both the arachnoid cyst and the subdural hematoma.
Discussion
First described by Bright in 1831 [8]. ACs are benign cystic lesions, which consist of CSF collections between the two layers of arachnoid membrane, by definition three criteria are required for a lesion to be considered an AC: 1/ it must be enveloped by an arachnoid membrane, 2/ it must contain arachnoid mater cells, and 3/ it must contain CSF [9].
They can be congenital or acquired after surgical trauma, infection, or hemorrhage [10].
In most cases, ACs are asymptomatic, the diagnosis is an incidental finding. When they are symptomatic, they are resulting of the direct compression of surrounding structures, ACs are relatively rare. The reported incidence accounts for only 1% of intracranial space- occupying lesions [11].
On CT, ACs manifest as extra-axial cysts with the density of CSF, it does not enhance after injection. MRI signals are similar to CSF in T1- and T2-weighted imaging with no enhancement on gadolinium.
Diffusion-weighted MRI has proved to be very useful for differential diagnosis that includes other cystic lesions [12].
Arachnoid cysts may remain stable or they may grow in size over time, in rare cases ACs may resolve spontaneously [7]. AC disappearance is a rare phenomenon that can occur spontaneously or after an inciting event.
The mechanism of spontaneous disappearance of ACs has not been described in the literature. Probably Communication between an AC and the subarachnoid space may be direct transport through the cyst wall or it may be a valve-like mechanism [13].
Although, the cyst wall rupture and CSF flow perturbation theories seem to be the most applicable pathophysiological mechanisms in triggered AC resolution(18).
Rupture of arachnoid cyst associated to subdural or intracystic effusion or bleeding is a rare complication. It occurs mostly after a head injury [14].
In this case, there was no history of head trauma, the cyst resolved spontaneously with the appearance of a subdural hematoma SDH. In the literature, there are only 11 cases reported in the literature of spontaneous SDH complicating an arachnoid cyst [15,16].
The management modality of asymptomatic ACs is not clear. However, surgical treatment is suitable for large or symptomatic ACs [17].
SDH associated with ACs spontaneously or due to traumas should be treated in an individual-based manner that is specific to each case, either conservatively or surgically [17,18].
In our case report, based on the clinical assessment no intervention was required.
Conclusion
The present case and the few reported cases of spontaneous disappearance of ACs suggest a more conservative approach in patients without asymptomatic ACs. Thus, we report highlight the interest of regular follow up of patients with known ACs.
#Arachnoid Cyst#Subdural hematoma#Spontaneous Resolution#jcrmhs#Journal of Clinical Case Reports Medical Images and Health Sciences predatory#Clinical Images submissions
3 notes
·
View notes
Text
Leo's injuries in my fic I'm making
Over 35 injuries (my boy's going through it 😞)
*All recovery times will be less than stated, due to Leo’s mutant healing factor.
Ruptured eardrum. Will heal within 3 - 6 weeks. Take antibiotics + ear drops.
2. Scrapes on feet.
3. Bruising on tailbone + lower back. Recovery time: 4 - 6 weeks.
4. Skidded knees.
5. Bloody nose.
6. Bruised face.
7. Scratched arms, legs, hand, knees, and plastron.
8. Scraped Shell + Arms.
9. Broken Ankle (Lateral malleolus fracture). This is the most common type of ankle fracture. It is a break of the lateral malleolus, the knobby bump on the outside of the ankle (in the lower portion of the fibula). Recovery time: 8 weeks. Boot for the last 5.
10. Cuts and scrapes on the left side of the body, bruising from around there.
11. Broken ribs on his left. Recovery time: 6+ weeks.
12. Bruising surrounding said ribs.
13. Mild bruising and scratching on shoulder.
14. Black eye.
15. Dented top-middle shell.
16. Concussion from whiplash.
17. Shell punctures from claws and surrounding cracks.
18. Broken shell. Recovery time: 1+ yrs. Drill small screws into the shell on either side of the fracture and then wrap wire around the screws, tightening the shell down almost like opposing tissue during suturing. Apply fiberglass patch and resin. Wrap with sterile gauze to help stabilize any broken shell pieces that may be present.
19. Fractured clavicle (collarbone). Recovery time: 6 - 8 weeks. Sling.
20. Fractured temporal skull. Recovery time: 5 - 7 weeks.
21. Broken femur (thighbone). Recovery time: 4 - 6 months.
22. Punctured lung. Recovery time: 6 - 8 weeks.
23. Neck bruising.
24. VERY skinned knees and lower legs.
25. Back of arms + shell got cut by claws.
26. Broken humerus (upper arm bone). Recovery time: 4+ months. Needs temporary splint extending from the shoulder to the forearm and holding the elbow bent at 90 degrees.
27. Broken scapula (shoulder blade). Recovery time: 6-12 weeks. Needs short-term immobilization along with motion exercises to prevent adhesive capsulitis, also called frozen shoulder.
28. Fractured vertebrae. Recovery time: 3+ months. Would need a brace, but with his shell, it won't happen.
29. Fractured orbital bone (eye socket). Recovery time: 3+ weeks.
30. Pneumothorax (collapsed lung). Recovery time: 1 - 3 weeks. Needs chest tube (but how will THAT work?).
31. Bruised liver (minor). Recovery time: 1 - 2 weeks.
32. Stomach bleed. Will lead to vomiting blood, yay.
33. Fractured sternum (breast bone). Recovery time: 6 weeks. Sternal injuries can usually be treated conservatively involving rest, restrictions of activities and painkillers, or occasionally through some form of intervention including targeted physical therapy.
34. Mild brain bleed. Recovery time: 6+ months. Surgery needed to drain blood from the brain Draining the fluid that surrounds the brain creates room for the hematoma to expand without damaging brain cells. Drugs are used to control blood pressure, seizures or headaches. Burr hole surgery is the main treatment for subdural hematomas that develop a few days or weeks after a minor head injury (chronic subdural hematomas). During the procedure, one or more small holes (the size of dimes) are drilled in the skull and a flexible rubber tube is inserted to drain the hematoma. Will drain within 2 - 3 days.
35. Second degree burns on his front. Recovery time: 1 - 3 weeks. Treat with antibiotic cream and wrap if the skin is raw, if the blisters open, or if there is risk of infection.
Homeboy will also deal with some other stuff, see my other post about it.
Credit to bellflowering and her ROTTMNT injuries masterpost!
#rise of the teenage mutant ninja turtles#rottmnt#rise of the tmnt movie#rottmnt movie#rise movie#save rottmnt#rottmnt fanfiction#rottmnt fanfic#rottmnt au#rottmnt fandom#rise leonardo#rottmnt leo
12 notes
·
View notes
Text
HSH Febuwhump Day 7 - Alt: Soft Words
“Made to Watch” wasn’t inspiring me tbh. I typed out like maybe 100 words about two of the guys being captured and the usual interrogation scene of making one of them watch the other being hurt. But like, it wasn’t really doing it for me. Soft Words didn’t really inspire me either but it fits this better.
Also I won’t lie - I did just want to follow up from yesterdays story. I am not sorry.
-----
Hyrule watches the screen intently.
With every hum of the MRI another layer of tissue is revealed. Hyrule stares at the red and yellow imaging, eyes narrowing at the lighter contrasts that grow between the brain and the dura. His colleague, a young Gerudo neurosurgeon, scribbles something in her notes.
“It looks like it’s localized to the cerebellum.” She says, eyes on his clipboard. “The rounded structure indicates it’s clotted. No sign of dead tissue. We need to check the ICP as soon as possible. I’ll have a catheter prepped.”
“If it's a clot we won’t be able to drain it.” Hyrule says, still watching the screen. In the other room, the MRI rumbles to a halt. Nurses pull on gloves and get ready to take the patient back to his room.
“I know. It’s just for monitoring and draining CSF if needed.” She flips through her chart, tongue peeking out in concentration. “I’ll consult the senior director about getting this pushed. For now get him started on 10mg of carbamazepine. He may have compromised motor function so tell him to stay in bed.”
She adds that last bit just as they watch Four try to convince the nurses to let him walk back to his room instead of being wheeled there.
Hyrule can feel his blood pressure rise.
Hyrule thanks his colleague and grabs a copy of the scan. He lets himself into the MRI room and marches up to his small friend amidst the nurses. “Just get on the gurney, Four.”
The doctor doesn’t let Four argue. He practically manhandles the mechanic into bed himself, letting his frustration show on his face. Both the nurses and Four recoil at the look. Legend always does tell him it's the easiest way to get everyone to listen to him.
The trip back to Four’s room is short, just one elevator and a walk down the busy hospital corridors. Hyrule doesn’t say anything and neither does Four. The blonde keeps his head down, cowed by Hyrule’s oppressive aura. His hair hangs loose and hides his face, free of it’s usual headband. Four’s colorful clothing has been replaced by a simple blue hospital gown.
When they get back to the room the only ones in it are Time and Twilight. The rest of the household had been banished at Four’s request. Something about medical privacy. As if such a concept applies to their household. Wind was probably already in the hospital database, waiting for Four’s medical chart to get digitized. The others would know all the details soon enough. But that’s a separate issue. As the patient, Four has the privilege of picking and choosing who’s allowed to be in the room.
Twilight perks up immediately. Time stays where he is, looming in the corner near the door. Hyrule lets the nurses push Four’s bed into position and sets up the MRI scans on the lightboard across from the bed. Twilight, who’s seated in the chair beside the bed, anxiously leans forward at the sight of the scans. Time, on the other hand, remains unmoved by anything and stands still, face stony.
“Thank you, Indrea. Can you talk to Jenni about the pre-op treatment? Doctor Malena has the details.” The Zora nurse nods happily and excuses herself, leaving the Hyrule alone to explain.
The doctor can feel their anxious eyes on him. Time’s gaze is especially heavy. Hyrule takes a breath and flicks on the lightbox, illuminating the scans.
Hyrule doesn’t hesitate. “So, after running a few tests, me and our local neurosurgeon have concluded that Four has a chronic subdural hematoma. It’s an unusual condition for someone young but there have been other cases before. And we do know you’ve suffered an TBI, which is usually a leading factor so that checks out. Right now it’s localized in the posterior fossa-”
“Hyrule, please for the love of the goddess-” Twilight begs.
Right. “Chronic subdural hematoma. That means there’s a collection of blood under the dural layer of your skull.” The doctor points to a lightly colored blob on the diagram of Four’s brain. See this, right here? That's a blood clot. It’s formed from old blood that hasn’t cleared away. Think of it like a bruise but the blood was never reabsorbed back into your body.”
Twilight pales. “In his brain?”
“No,” Hyrule stops that line of thought before anyone panics, “No. Not exactly. It’s bleeding under the skull, but above the surface of the brain.”
He changes slides to show a better diagram to explain. “There’s space between the skull and brain that’s filled with liquid that helps protect the brain called cerebrospinal fluid. That’s where the blood clot is.”
Hyrule looks Four. “The bridging veins in that layer were damaged when you hit your head. We didn’t notice back then because it's chronic as opposed to acute. Meaning it’s a slow bleed. The blood mass has been accumulating with time as the veins kept leaking. This blood mass, which has semi-coagulated, has been growing. Slowly putting more and more pressure on your brain as it fills the space. That’s why your symptoms have been getting worse with time, not better.”
Four grimaces, redirecting his eyes to the board to avoid Hyrule’s gaze. His fingers pick at the hospital sheets.
“And you’re sure this is from Happy’s men?” Twilight doesn’t sound convinced. He glances nervously at his uncle, who remains blank faced. “That was a long time ago. If it’s been bleeding this whole time…”
“Hence the word ‘chronic’. Something like this can go unnoticed for some time.” Or ignored, in this case. And boy, is Hyrule going to yell at Four for this. He’s got a thirty minute lecture already planned out. With excel slides and everything. But it’ll wait until after Four's recovery. He doesn't want to cause any stress before the procedure. “It’s grown large enough that it’s now compressing against your cerebellum. This is probably what triggered the seizure. You’ve also been taking OTC pain meds, some of which act as blood thinners. This may have exacerbated the issue, too.”
“Is this-?” Hyrules eyes flicker to Time when the man cuts himself off. There’s something deep in his eye, a deep well of some emotion he refuses to share. His jaw is tense.
Hyrule can’t be certain, but he’s got an idea of what Time might be thinking.
“It’s treatable,” Hyrule assures him, looking back at Four. “It’s going to require surgery to remove but you should be okay. There’s no sign of brain tissue damage so far and my friend Doctor Malena, your neurosurgeon, is going to push to get this done quickly.”
Time’s shoulders drop minutely.
Four squirms uneasily. His eyes flicker over the scans. He wets his lips, speaking for the first time. “What… What kind of surgery are we talking about?”
“She’s speaking to the department head about it right now, but we’re thinking it’s probably going to be a craniotomy.” Hyrule explains, taking a seat on the edge of Fours bed. “Doctor Malena will explain it more in detail to you later when everything is finalized. But basically it’s when a section of the skull is temporarily removed to give access to the brain cavity. After the problem is fixed, in this case the clot is removed, the bone is replaced and resealed.”
Four recoils, eyes widening. “She’s going to cut into my head?”
Twilight does too, looking particularly pale after Hyrule mentioned removing a section of his skull. “Seriously? Is this safe? Because it doesn’t sound safe.”
Hyrule smiles at them both comfortingly. Bedside manor, Hyrule. You can do it. “It’s not as scary as it sounds, I promise. In terms of head surgery this is actually fairly safe, since we won’t go any deeper than the surface of the brain. No insertions or anything regarding actual greymatter. The most she’ll do is seal up the veins that are causing the problem. But again, that’s not touching the brain.”
“Isn’t there another option? Medication, or something?” This is probably the closest thing to pleading Hyrule has ever heard from Four.
Hyrule pats his arm comfortingly. “Sorry, but we don’t have any good options other than surgery. If we’d caught this earlier then maybe. But as it is, we really can’t wait. We’d be risking real damage if we put it off for too long. And any medication we could give you would be mostly experimental.”
Four groans and drops back into his pillows. He grabs one and covers his face with it. “Fuck.”
-----
I have never watched even one (1) episode of Greys Anatomy idk how doctors talk please be nice to me i had to google ‘medical terms for x’ 1000 times today
WebMd tells me chronic subdural hematomas usually cause fatal problems in weeks, not months. But this is my story and I get to pick the amount of time Four can go without dying.
But yeah, I thought it would be fun to take Four’s change in demeanor into a more physical road, rather than what it probably is. Its also a product of me thinking Stormy said he was having headaches. But it turns out she never said that and it was a creation of my own brain lmao. She just said he was quieter. I might continue this but also maybe not. We shall see.
#HSH au#Townhouse au#HSH Four#HSH Hyrule#HSH Time#poor time feels guilt yet again#also damn tumblr does not like medical terms#half this is underlined in red#Febuwhump 2023
13 notes
·
View notes
Text
Home - but still writing about Egypt
Oct 13, 2024
Greetings all,
I know it has been almost 2 weeks since we returned from Egypt - but “stuff” has gotta in the way of my writing, thinking, and remembering. My vacation “glow” has faded - but today I am going to try to brighten the glow and using my photos, tour book and what is left of my mind, I’m going to finish up our trip.
The “stuff” that has stopped me from writing is big. Before our trip Mark took a little fall on his bike that resulted in a brain bleed (chronic subdural hematoma.) He was hospitalized for a few days and underwent a procedure called an MMA (middle meningeal artery) in which they go through the groin into the brain and put some “glue” near the area of the bleed. Of course that is my layman explanation - but it was a big freaking deal. That caused our travel plans to be modified - but we are flexible.. A few days before we left of our trip, Mark met with this heart Dr and his brain Dr and after another CT Scan they pronounced him in good traveling condition and wished us well. BUT merely as a safety check he was to have another CT Scan the day after we returned from Egypt. So, we got home later Oct 2 and at 8:00 AM October 3, Mark headed to have another CT Scan.
He had felt fine during the entire trip so we expected everything to be fine - but it was not. The CT Scan showed the bleed had continued to "leak" - again - layman speak. The bleed was 3 times the size of the original bleed and he headed to the hospital - this time for a craniotomy. This is major surgery in which a part of the skull is removed to give the Drs access to the “leaking" area. Surgery would last approximately 2 hours, he would be in ICU for 2 days, then in general care for another 4. We were both rattled.
Fast forward. Mark is great.

He is bald - although his hair is starting to grow back. He has a very large incision on his head with 23 staples - kind of a Frankenstein vibe. He spent only 1 day in ICU and then 2 days in general care before he was released to my care.😳. As the grandkids are calling him “Super Grampa” exceeded all expectations. He feels fine and we even attended grandson, Colin’s soccer game the day after Mark was released from the hospital and are looking forward to another game on Tuesday (Go SKYLINE!)

The night we came home from Cairo I unpacked and did laundry and put away suitcases and, and, and, just trying to stay awake. I’m awfully glad I did that - because nothing else has been done since then. Mark is doing better than the doctors anticipated and I’m slowing getting back my rhythm. It is 4:00 AM and I have a load of clothes in the washer and one in the dryer - and they have nothing to do with our trip but they are just part of catch-up on our daily life.
So that is my “stuff” and a legitimate reason for the delay. But I’m going to delve back into the trip because there is still much to share….
Back to Egypt….
I simply adore the opportunities to see a local village and to meet locals and this was a great visit - that I didn’t talk about when it happened.
September 23, 2024 (Day One on our dahabeya.)
This was a long day that started at 3:30 AM as we headed out for our hot air balloon ride. After that we boarded and ship and heading up the Nile. In later afternoon we dropped anchor at a little community called Al Hagz Bahry and we were met by this lovely lady.

Al Hagz Bahry is a large village about 5,000 people but more than a couple of miles from the Nile, which was necessary when the flooding of the Nile was uncontrolled. But since the 1970s smaller “neighborhoods” have sprung up and this is where we were led. Our hostess, whose name I cannot remember - 🤬 - but it might be Asaara, was stunning. Her English was great and she was very proud to tell us that she had learned it from Google. She was funny and generous and gracious. She walked us to her home that she shares with her parents, her two children and her sister.

Her husband works in Cairo and comes home every 6 weeks for a few days. Then she moves back to her in-laws house to be with him, but after he returns to work - she comes back here with her children. She said she had the perfect marriage. No husband for 6 weeks. 5 days of honeymoon and then bye-bye for another 6 weeks. We all cracked up!

She is gregarious, charming and ambitious. She is preparing to give sewing lessons to her neighbors as she makes all the clothes for her family - which are quite lovely - FYI. Her sister is unmarried and a teacher. Notice the paintings on the house. Her father took a plane to Mecca for the Haj a few years ago and others hope to do the same someday. The boat is still a dream - to travel to other lands. The Arabic writing you see are passages from the Quran about family, love and health.
We were served some lovely mint tea - with the mint freshly cut.

She answered all our questions and then gave us a tour of the house. While we were in the house she grabbed Marla, Nora and my hand and pushed us in the bedroom. “I have a surprise for everyone!" she said and she opened the wardrobe and took out clothes. She and her sister selected dresses and headscarves for us and then helped us dress. NOW - I will say that these dresses were lightweight and might have been cool - but we but them on over our regular clothes - you know - layers. Then the headscarves - which are all wrapped differently - and we were hot! BUT it was wonderful. Our hostess was having a great time and so were we. She was so cute - she said to our group - "I want you to meet some lovely Muslim women I just met” and she led us out to the veranda.

One of the things I LOVE about traveling with this company is that they get us INSIDE people’s homes and lives. These experiences shine a light on just how much we have in common. When I think of Egypt years from now, sure I will remember pyramids and temples but I always hold experiences like these in my heart.
I LOVE this Mark Twain quote, "Travel is fatal to prejudice, bigotry and narrow-mindedness, and many of our people need it sorely on these accounts. Broad, wholesome, charitable views of men and things cannot be acquired by vegetating in one little corner of the earth all one's lifetime.”
I think this is so true. When you travel and meet and talk to people who live in the area you are visiting, you are an ambassador for the US and the people you are talking to are ambassadors from their country. It makes it impossible to hate or see “people” as your enemy if you have shared food with them at their home. We spent almost a full month in two Muslim majority countries. We heard the call to prayer 5 times a day. Jordan and Egypt are not Sharia law government countries. BUT what does that really mean? I’m guessing many people reading this have a bad taste in the mouth when they read "Sharia law."
Sharia means “the correct path” in Arabic. In Islam, it refers to the divine counsel that Muslims follow to live moral lives and grow close to God. Most Muslims follow this in their own lives.
Below are the 5 pillars of Islam:

In Egypt and Jordan, people may or may not go to the Mosque to pray 5 times a day. It is not the law. We heard the call to prayer day after day, but shops nor restaurants nor markets closed. People in the streets did not turn into the Mosque. Normal life was not disrupted. For many Muslims praying is personal and although they do not pray 5 times a day at the designated time in a mosque, they do say their prayers at night, after work. Ayman doesn’t tour during Ramadan because it would be physically impossible to have no water and food during the day and keep up the pace he has set for his “ducklings.”
During Ramadan - those who are able - participate in the daily fast that includes abstaining from all food and drink; not even a sip of water is allowed from dawn to sunset before breaking the fast in a meal known as “iftar” in Arabic. Those fasting are expected to also refrain from bad deeds, such as gossiping, and increase good deeds. The elderly, pregnant woman and children are exempt from the fast. The breaking of the fast is a celebration with wonderful food, surrounded by friends, families and neighbors.
Countries with Sharia law see all their civil law through the Sharia lens. We have not been to Saudi Arabia , Iran or Afghanistan- and frankly I don’t want to go - but people we know who have visited tell us that the call to prayer stops everything. Shops close and everyone goes to pray. They have a robust “morality police” making sure people - especially women - are wearing proper attire and doing their required Muslim duties. Jordan and Egypt are not like this. We saw many churches in both countries and people have a right to worship as they wish.
A word of warning to anyone reading this that Christian Nationalism is also “Sharia law.” When one religion demands that the government make laws and restrictions that follow their chosen religion it means trouble. Of course, everyone - world-wide - believes they are correct and have found the one true religion but once the majority religion of a region begins to be intolerant of any other beliefs we have trouble. So Beware!
September 26, 2024
We visited another small village as we cruised by the Nile - and we got there by a little hike down the gangplank, through the woods to a road where Tuk-tuks awaited us. These Tuk-tuks are the Uber of a small village, my friend.

We went to a craftsman’s workshop under a tree.

This man makes baskets for mangos and other things all from the large vein of a palm tree frond. He has been doing this for 52 years. He was charming, friendly and very proud of his craft.
I have two movies to show you can only upload one. DAMN IT!! He was quick, efficient and used his feet. Watch his feet.
He encouraged us to learn his technique. Joe - who is an excellent wood craftsman - jumped right in and did a great job. Joe had a disadvantage right away because he was wearing shoes. Look behind Joe to see the chairs our host also created.

On September 27, we made another stop - this time to the Draw camel market. To get there, we took a boat to the village and then got in the back of pick-up trucks. Wild - huh? People also grabbed a ride as we went from the harbor to the village. Below was our “hitchhiker"

This town is famous for its camel market, where more than 2,000 camels, brought from Sudan in caravans that cross the desert in a 40 day road trip, are sold and bought. Two days a week this small village is flooded with people buying and selling camels. It was NOT market day when we stopped and I think that is a good thing. We visiting with a man who runs a “B&B” - and that has a little different meaning in Draw, Egypt. I think he called it an inn - but is was a place to sleep with food - so I’m going with B&B.
The market participants (buyers and sellers) often want a place to sleep before they begin their long march home - so here are some of the places available. It rains once about every three years here.


And those staying for the night have animals - so there are B&Bs for them as well. Note the marking on the camel - that is his ID.


There were several places for animal and this goat pen was a hit for all of us, especially Mark and Daphne.


Again we were welcomed with kindness like old friends dropping by. The owner explained the market and also the major growth of the city as it has been flooded with people fleeing the Sudan civil war. Since these people are exactly the same people as they are divided only by stupid governments and borders, everyone is pulling together to welcome these people into their community.
Everyone builds up preparing for their son to bring home their wife - but in this community people are building several stories up to house the new emigrants. Atop these taller building are pigeon coops. Pigeon is a common food and is believed to be an aphrodisiac.

I'm stopping here although I have more to report. Hopefully it won't take me 2 more weeks to do it.
Salem
0 notes
Text
Management of acute and symptomatic chronic subdural hematoma
Management of acute and symptomatic chronic subdural hematoma
Let's say rule of 10/5/2 (drowsy/dilated/brainstem compression/Hydrocephalus)

0 notes
Text
0 notes
Text
Burr Hole Drainage: A Surgical Marvel in Neurosurgery

In the field of neurosurgery, a variety of surgical procedures are employed to address different conditions affecting the brain. One such procedure is Burr Hole Drainage, a remarkable technique used to treat various neurosurgical conditions. Burr hole drainage involves creating a small hole in the skull to access and drain accumulated fluids, such as blood or cerebrospinal fluid, in a controlled manner. This article delves into the intricacies of Burr Hole Drainage, its applications in neurosurgery, the surgical technique involved, and its impact on patient outcomes.
Understanding Burr Hole Drainage
Burr Hole Drainage is a surgical procedure utilized to relieve intracranial pressure caused by the accumulation of fluids within the skull. This technique is commonly employed in cases of subdural hematomas, chronic subdural hematomas, hydrocephalus, and certain abscesses. By creating one or more small openings in the skull, known as burr holes, neurosurgeons gain access to the affected area, enabling the drainage of fluids, alleviating pressure, and promoting brain tissue recovery.
The Surgical Technique
The Burr Hole Drainage procedure begins with the patient under general anesthesia. Once the surgical area is prepped and sterilized, the neurosurgeon makes a small incision on the scalp, usually over the area where the fluid accumulation is detected or suspected. A specialized surgical drill, called a trephine, is then used to carefully create one or more burr holes in the skull.
The size and number of burr holes depend on the specific case and the surgeon's preference. These holes are strategically placed to access the area of concern and provide optimal drainage. After the burr holes are created, the dura mater, the protective covering of the brain, is carefully incised to expose the underlying fluid collection. The neurosurgeon may also employ imaging techniques, such as intraoperative ultrasound or endoscopy, to guide the drainage process.
Next, a drainage catheter or tube is inserted through one of the burr holes and directed toward the fluid collection. The catheter is connected to a drainage system, which may involve a closed system or a subcutaneous reservoir, allowing for controlled and continuous drainage of the accumulated fluid. The neurosurgeon monitors the drainage process closely to ensure the appropriate amount of fluid is removed.
Applications and Benefits
Burr Hole Drainage offers numerous applications and benefits in the field of neurosurgery. It is particularly effective in cases of subdural hematomas, where the collection of blood between the brain and its outer covering causes pressure on the brain tissue. By draining the hematoma, the pressure is relieved, minimizing the risk of brain damage and facilitating the brain's natural healing process.
The procedure is also utilized in chronic subdural hematomas, which may occur due to minor head injuries, especially in older individuals. Burr Hole Drainage allows for the evacuation of the accumulated fluid, reducing symptoms such as headaches, confusion, and neurological deficits.
For patients with hydrocephalus, a condition characterized by excessive accumulation of cerebrospinal fluid within the brain, Burr Hole Drainage provides a way to alleviate pressure by draining the excess fluid. This procedure may be employed as part of a shunt system, where a catheter is inserted to divert fluid from the brain to another part of the body, such as the abdomen, where it can be absorbed.
In cases of brain abscesses, Burr Hole Drainage allows for the controlled drainage of infected material, providing an essential step in the treatment process alongside antibiotic therapy. By removing the pus or infected fluid, the burden on brain tissue is reduced, aiding in the patient's recovery.
The benefits of Burr Hole Drainage extend beyond immediate relief. The minimally invasive nature of the procedure reduces surgical trauma, resulting in shorter hospital stays, faster recovery times, and improved patient outcomes. Furthermore, the ability to perform this procedure with local anesthesia, when appropriate, offers advantages such as reduced anesthesia-related risks and enhanced patient comfort.
Potential Complications and Considerations
While Burr Hole Drainage is generally considered a safe procedure, it is not without potential complications. Like any surgical intervention, risks such as infection, bleeding, damage to surrounding structures, or cerebrospinal fluid leakage may arise. However, these complications are relatively rare, and neurosurgeons take necessary precautions to minimize them.
Close postoperative monitoring is crucial to detect any signs of complications promptly. Patients are typically observed for changes in neurological status, infection signs, or leakage of cerebrospinal fluid. In some cases, additional surgical procedures may be required to address complications or optimize drainage.
It is important to note that Burr Hole Drainage is not always the definitive treatment for the underlying condition. In some cases, it serves as a temporary measure to relieve acute symptoms or stabilize the patient before considering further interventions, such as craniotomy or shunt placement.
The cost of burr hole surgery can range from approximately $10,000 to $50,000 or more. essential to consult with healthcare professionals, insurance providers, and financial advisors to obtain accurate and personalized cost information based on individual circumstances. They can provide detailed information about the specific procedure, associated costs, available financial assistance programs, or insurance coverage options.
Conclusion
Burr Hole Drainage is a remarkable surgical technique in the field of neurosurgery, offering a minimally invasive approach to address various neurosurgical conditions. This procedure provides effective relief of intracranial pressure by draining accumulated fluids, such as blood or cerebrospinal fluid, and plays a crucial role in facilitating patient recovery. With ongoing advancements in neurosurgical techniques and technologies, Burr Hole Drainage continues to contribute significantly to improving patient outcomes and enhancing the field of neurosurgery as a whole.
0 notes
Text
Can Hemodialysis Cause Seizures
Seizures among hemodialysis patients:
Seizures are common among hemodialysis patients. Seizures in hemodialysis patients can have a variety of causes. Seizures usually occur during or shortly after hemodialysis because of the hemodynamic and biochemical changes that occur during the procedure. This topic discusses the causes and treatment of seizures in hemodialysis patients. The treatment of seizures in patients who do not have kidney failure is discussed elsewhere.
SEIZURE WITH NEW-ONSET:
Causes:
The evaluation of a new-onset seizure is similar to that of non-dialysis patients. End-stage kidney disease (ESKD) or hemodialysis treatment can result in the following complications: uremic encephalopathy, dialysis dysequilibrium syndrome (DDS), intradialytic hemodynamic instability, aluminum-associated dialysis dementia, air embolism, hypoglycemia, hypocalcemia, and hyponatremia.
Other causes of seizures in hemodialysis patients are similar to those in the general population, but may be more common. Cerebrovascular disease (infarction, cerebral emboli [distinct from infarction because dialysis vascular access can lead to infections and septic emboli], haemorrhage, and subdural hematoma) is a major concern in the hemodialysis population. Because of their significantly reduced clearance, patients on hemodialysis are more vulnerable to drug-induced seizures with certain drugs such as carbapenem and ertapenem when compared to patients who are not on dialysis. The following sections go over the most common causes of seizures in the dialysis population. Some are unrelated to dialysis, while others are a direct result of the procedure.
Uremic encephalopathy:
Central nervous system (CNS) dysfunction is seen in patients with severe, untreated uremia but not in patients receiving maintenance hemodialysis unless multiple treatments are missed. Irritability and restlessness are common symptoms, as are seizures, coma, and death. Seizures are most commonly generalised and occur prior to dialysis, frequently prompting the start of emergent dialysis. CNS dysfunction resolves within days to weeks of starting adequate kidney replacement therapy.
Dialysis disequilibrium syndrome (DDS):
Dialysis disequilibrium syndrome (DDS) can occur in severely uremic patients who are starting hemodialysis for the first time, but it rarely occurs in patients on maintenance hemodialysis. DDS is distinguished by a range of neurologic symptoms. Symptoms usually appear during or immediately after hemodialysis. Headache, nausea, disorientation, restlessness, blurred vision, and asterixis are common early symptoms. Patients who are more severely affected develop confusion, seizures, coma, and even death. However, DDS includes many milder dialysis-related signs and symptoms, such as muscle cramps and dizziness that develop near the end of a dialysis treatment.
Toxins or drugs:
Toxins or drugs Many medications in the general population can cause seizures (table 1). Patients on hemodialysis are especially vulnerable to certain drugs due to decreased clearance: 1. Antibiotics such as penicillin, cephalosporins, carbapenem, and ertapenem, especially when given in high doses 2. Meperidine (due to toxic metabolite accumulation, normeperidine) 3. Metoclopramide 4. Theophylline 5. L-dopa 6. Lithium 7. Acyclovir 8. Iodinated contrast material administered intravenously (IV) (in high doses) In dialysis patients, star fruit consumption can result in severe neurologic dysfunction, including seizures and death.
Dialysis dementia:
Dialysis dementia is a progressive neurologic disorder that occurs exclusively in dialysis patients and can manifest as seizures. Aluminum exposure is the root cause. Because of improved hemodialysis water treatment and the use of non-aluminum-containing phosphate binders for chronic hyperphosphatemia management, the incidence of dialysis dementia has significantly decreased.
Immediate management of seizures:
The emergency treatment of seizures in dialysis patients includes the following: • Stop dialysis and begin IV fluid and oxygen infusion if necessary. • Keep the vascular access safe during the seizure. • Ascertain that the patient is in a safe environment and is not in danger of injury (eg, fall risk). Place the patient on their side if possible, during the seizure. During an active seizure, do not put anything in their mouth. • Although most seizures last less than five minutes and spontaneously resolve, (if hemodialysis is performed in an outpatient clinic) or a rapid response (if hemodialysis is performed in a hospital setting) should be called in most cases. • If a patient continues to seize, paramedics or the rapid response team must protect the patient’s airway and stabilise the patient. The first-line treatment is IV benzodiazepines to stop the ongoing seizure activity. A clinician should then evaluate the patient to determine the best course of treatment (eg, with IV antiseizure medications)
Serum levels of glucose, calcium, sodium, magnesium, and other electrolytes should be measured in blood, as significant abnormalities may indicate the underlying cause of the seizure. If hypoglycemia is suspected, IV glucose and IV thiamine should be administered, especially in at-risk individuals (eg, history of heavy alcohol use).
Evaluation:
Once the patients have been treated for seizure and dialysis has been discontinued, the seizure evaluation for patients on dialysis is the same as for other patients. Uremia, subdural hematoma, metabolic disturbances (hyponatremia, hypoglycemia), and drug-induced encephalopathy are all potential causes that should be ruled out. Furthermore, seizure causes that are not specific to dialysis patients must be ruled out.
PREVENTION:
Seizure prevention is directed at specific causes.
Causes specific:
• Uremic encephalopathy – Progressive uremic encephalopathy is a clear indication that dialysis should begin. Seizures are avoided by starting dialysis before the onset of mental status changes.
• Dialysis disequilibrium syndrome – Dialysis disequilibrium syndrome (DDS) is avoided by limiting the reduction in blood urea nitrogen (BUN) per treatment so that it is gradual and spread out over several days. This treatment prevents seizures but may not prevent mild symptoms like headaches and malaise.
• Erythropoietin therapy – Avoiding rapid increases in haemoglobin is the most important measure to prevent erythropoiesis-stimulating agent (ESA)-induced seizures. The optimal haemoglobin target, dosing, and route of administration are all discussed elsewhere.
• Dialysis-induced hypotension – A variety of manoeuvres are used to prevent dialysis hypotension. This is covered separately.
MAINTENANCE ANTISEIZURE THERAPY:
Antiseizure medications are used for the same reasons in hemodialysis patients as they are in the general population. Long-term antiseizure medication therapy may not be necessary if the patient’s seizure is caused by a reversible cause.
Medication selection:
Among hemodialysis patients who are chosen for antiseizure medication, the choice of a specific medication is influenced by a number of factors, and no single antiseizure medication is clearly the most effective or well tolerated.
We usually use levetiracetam for most hemodialysis patients. Levetiracetam is generally well tolerated, inexpensive due to the availability of generic forms, and has few drug-drug interactions. If levetiracetam is used, the recommended daily dose is 500 to 1000 mg, with an additional dose of 250 to 500 mg administered at the end of dialysis.
A variety of other agents are effective. Lacosamide is an alternative that could be used. Lacosamide also has few interactions with other drugs, including immunosuppressive medications.
We generally do not use phenytoin or valproic acid in hemodialysis patients unless the patient is already stable on one of these medications prior to starting hemodialysis. Phenytoin and valproic acid have numerous drug-drug interactions and have a higher rate of side effects.
Dosing:
Dialysis removes many of the newer and more commonly used antiseizure medications. To prevent recurrent seizures in patients receiving a dialyzable antiseizure medication, the dosing regimen must be adjusted to avoid a subtherapeutic plasma level during or after dialysis, which could result in a seizure. Many antiseizure medications require dose adjustments based on the severity of kidney impairment, as detailed in the table for the most commonly prescribed antiseizure medications. The following drugs are removed in varying degrees by dialysis and must be supplemented to maintain therapeutic levels: • Levetiracetam • Lacosamide • Topiramate • Zonisamide • Lamotrigine • Primidone and phenobarbital • Gabapentin • Oxcarbazepine, carbamazepine
We time the doses for patients on any of these agents so that the medication is administered at the end of each dialysis treatment. Another option is to administer an extra dose at the end of each dialysis session.
Dialysis of carbamazepine and oxcarbazepine is minimal. However, even a small amount dialyzed out can cause a decrease in concentration. The strain of hemodialysis, combined with a slight drop in concentration, can lower the seizure threshold.
We do not use long-acting formulations. An extended-release formulation will take longer to achieve a therapeutic concentration if given as a supplemental dose after dialysis.
Some medications, such as phenytoin and valproic acid, are not dialyzed and therefore do not require postdialysis supplementation. As a result, phenytoin and valproic acid are commonly used among hemodialysis patients. However, as previously stated, these agents are less commonly used today in comparison to newer agents.
Serum levels in patients taking phenytoin or valproic acid must be carefully interpreted. Phenytoin and valproic acid are highly protein bound, and the relationship between free and total drug concentrations is unpredictable. There is displacement of the drug from serum proteins with an increase in the volume of distribution in patients with hypoalbuminemia (which is very common in those with end-stage kidney disease [ESKD]).
As a result, the patient has the same concentration of free drug (which has the pharmacologic effect) in serum while having a lower total blood concentration than a subject with normal kidney function and no hypoalbuminemia. If available, free levels should be monitored rather than total levels.
1 note
·
View note
Text
twist drill for evacuation of chronic subdural hematoma
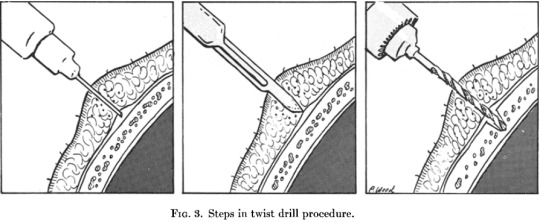

References: (1) Rand, B. O., Ward, A. A., & White, L. E. (1966). The Use of the Twist Drill to Evaluate Head Trauma. Journal of Neurosurgery, 25(4), 410–415. doi:10.3171/jns.1966.25.4.0410 (2) https://www.netterimages.com/craniostomy-for-chronic-subdural-hematoma-unlabeled-neurology-neurosciences-frank-h-netter-1165.html
0 notes
Text
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
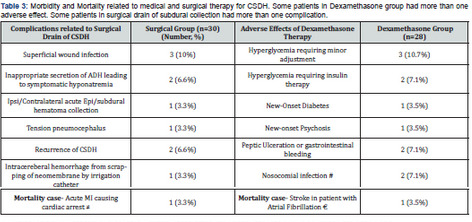
The Role of Dexamethasone in the Era of “Dex-CSDH” Randomized Controlled Trial. A Multicenter, Prospective Study on Specific Subset of Patients with Chronic Subdural Hematoma (CSDH) Treated with Dexamethasone Alone or Surgery
Authored by Abhishek Chaturbedi
Abstract
Background: The efficacy of Dexamethasone as a method of conservative management for CSDH to avoid surgery remains inconclusive even after “Dex-CSDH” randomized controlled trial as almost all patients underwent an initial operation to remove the hematoma. Current study aims to determine the efficacy and safety of Dexamethasone alone therapy in comparison with the surgical drain of CSDH.
Methods: A multicenter, prospective study on mild to moderately symptomatic adult patients with CSDH were performed from January 2019 to December 2020. The patients were enrolled in a 1:1 ratio to receive a 3-weeks tapering course of oral Dexamethasone, starting at 4 mg thrice daily, or surgical drain of CSDH. The patient was assigned to a particular therapy based on their preference. The primary outcome was functional outcome in each group at 6 months determined by mRS, and cure rate (symptomatic relief and radiological resolution of CSDH).
Results: Twenty eights patients were assigned to Dexamethasone group and 30 patients to surgical group. The mean age of the patient was about 62 years in both groups with male predominance (>60%). A favorable outcome determined by mRS scale of 1 to 3 at 6 months follow-up was 25/28 (89.2%) in Dexamethasone group compared to 28/30 (93.3%) in surgical group (difference, -4.1 [95% CI, -6.8 to -2.2], p=0.12). The cure rate was 23/28 (82.1%) in Dexamethasone group compared to 28/30 (93.3%) in the surgical group during index admission (difference, -11.2, [95% CI, -14.3 to -7.6] in favor of the surgical group, p=0.005). Recurrence rate for CSDH was 2/28 (7.1%) in Dexamethasone group compared to surgical group 4/30 (13.3%) which was statistically significant (p=0.01). Morbidity related to medical therapy was not statistically higher compared to surgical group.
Conclusion: Current study exhibits superiority of surgery over Dexamethasone therapy for resolution of symptomatic CSDH. The recurrence rate of CSDH is lower in patients with corticotherapy compared to surgical drain. Patients in Dexamethasone group did not have functional outcome at 6 months or morbidity significantly higher than surgical group. This study strongly puts forward the utility of Dexamethasone as an effective and safe alternative to surgery for CSDH.
Keywords: Chronic subdural hematoma; Dexamethasone; Surgery; Functional outcome; Corticotherapy
Abbreviations: CSDH: Chronic Subdural Hematoma; CT: Computed Tomography; GCS: Glasgow Coma Scale; MRS: Modified Rankin Score; FFP: Fresh Frozen Plasm
Introduction
Chronic subdural hematoma (CSDH) is a common neurological disease prevalent in elderly population and has shown an increase in incidence due to extended life expectancy and use of blood thinners [1]. Burr-hole evacuation of CSDH is simple and easy to perform procedure with low morbidity rate (ranging from 0 to 9%) [2], but a rather variable rate of recurrence (10 to 20%) [3,4]. Surgery remains the mainstay therapy for patients with symptomatic CSDH with acceptable morbidity in medical community which produces excellent outcome and good symptomatic relief. Despite the excellent outcomes obtained by surgery, complications may occur, some of which may be potentially severe or fatal. Furthermore, up to 25% recurrence rate is reported.
Glucocorticoid has been used to treat CSDH [5], with acceptable efficacy and safety profile as stand-alone therapy to avoid surgery or as an adjunct to surgery to prevent recurrence of subdural fluid collection [6,7]. The Dexamethasone for Adult Patients with Symptomatic Chronic Subdural hematoma (Dex-CSDH) trial was a multicenter, randomized control trial conducted in the United Kingdom and published in December 2020 [8]. This recently concluded study aimed to determine the effect of Dexamethasone on outcomes in patients with symptomatic CSDH. It reported that most of patients (>90%) had to undergo surgical drainage of CSDH while on 2 weeks tapering dosage of Dexamethasone drug, which resulted in fewer favorable outcome and more adverse events compared to placebo at 6 months, but fewer recurrence of subdural fluid collection in the Dexamethasone group.
This provided much needed Class I evidence on Dexamethasone therapy to evaluate its effectiveness and its impact on the functional outcome of the affected patients. Since almost all the patients underwent surgery to evacuate CSDH while of Corticotherapy, the true effect of Dexamethasone as stand-alone therapy to treat this disease effectively, safely, with avoidance of surgery and prevent recurrence of subdural collection could not be ascertained by this study. Current study is a multicenter, nonrandomized but controlled, prospective clinical trial to determine the efficacy, safety and functional outcome of patients with standalone 3 weeks tapering dose of Dexamethasone medical therapy compared to surgical drainage of CSDH. Our study aims to add further clarity to the role of corticotherapy in conjunction with Dex-CSDH study in patients with chronic subdural hematoma.
Materials and Methods
Study design
This study is a multicenter, prospective clinical trial that was conducted in 4 different hospitals in Kathmandu, Nepal where the author treated the patients with CSDH. Patients were enrolled in stand-alone 3 weeks tapering course of Dexamethasone or burrhole evacuation of hematoma as the treatment modality based on patient’s preference. To be precise, the decision to perform surgical evacuation of subdural hematoma or conservative monitoring was made by the author following detailed discussion with the patient and patient’s next of kin. Hence it is a non-randomized study but a controlled study. The duration of the study was from January 2019 to December 2020 (2 years). We had almost 1:1 ratio between the two cohorts of patients. Dexamethasone group had total of 28 patients, while there were 30 patients in the surgical group who met eligibility criteria and fulfilled follow-up requisite.
Informed written consent was obtained for all patients who had surgery for CSDH. Verbal consent was obtained and noted in the medical records who preferred stand-alone Dexamethasone therapy as the treatment modality for CSDH. A chronic subdural hematoma was defined as a predominantly hypodense or combination of hypodense with isodense (relative the brain grey matter) crescentic collection along the cerebral convexity on computed tomography (CT) of the head.
Eligibility criteria
Inclusion Criteria: 1) The hematoma has be to be chronic or predominantly chronic with component of subacute blood 2) Glasgow Coma scale (GCS) on initiation of both alternative therapies of 13-15, 3) Modified Rankin Score (mRS) of 1-3 (see below for details on mRS scoring system) 3) Strict adherence to 3 weeks regimen of Dexamethasone as per the prescribed format [see below] 4) Follow-up on a weekly basis for patients on corticosteroid therapy to look for complications or adverse events associated with it 4) Follow-up CT scan every week for patients on corticosteroid therapy and before hospital discharge for index admission of patients with surgical evacuation of hematoma 5) Trauma or spontaneous CSDH were included in the study 6) Patients on anticoagulant or antiplatelet agent when CSDH was discovered 6) Patients who were available for evaluation of their clinical status, functional outcome and repeat CT head at 3 and 6 months follow-up visit after completion of their respective therapies.
Exclusion Criteria: 1) Subdural hygroma 2) Patients on antiplatelet or anticoagulants 3) Asymptomatic patients 4) Patients with poor neurological or functional status as is evident in inclusion criteria, GCS <13 and mRS>3 were excluded as per the pre-fixed study design [explained in discussion part] 4) Contraindications for glucocorticoid use (e.g. uncontrolled diabetes mellitus, recent peptic ulceration or gastrointestinal bleeding, severe valvular heart disease or unstable angina pectoris, active systemic infection, lactose intolerance, had a cerebrospinal fluid diversion shunt, known hypersensitivity to Dexamethasone, had a history of psychotic disorder and patients receiving glucocorticoid oral or intravenous within the last 1 month 5) Patients who failed Dexamethasone therapy and had subsequent surgical evacuation of CSDH were not included in the surgical arm of patients 7) any pre-existing medical condition that precludes surgical drainage of CSDH.
Patients
Patients with symptomatic CSDH who were eligible for the study were explained the pros and cons about both forms of treatment modalities. They were explicitly told that Dexamethasone as a stand-alone treatment may not lead to resolution or significant reduction of CSDH, which may ultimately lead to surgical drainage of blood to alleviate the neurological symptoms. This drug has inherited complications/side effects which needs to be carefully monitored during the prescribed period of treatment. The pros and cons of surgical drainage of subdural fluid collection through a burr-hole was also explained along with the complications related to surgical procedure.
Treatment protocol
All patients in this study were enrolled with intention to treat mindset using two different treatment protocol. All the patients under the surgical arm underwent standard single or double burr-hole evacuation of CSDH (based on surgeon’s discretion) with placement of subdural drain to a closed system for 1-2 days in the hospitals with neurosurgical units. The anticoagulant and antiplatelet effect were reversed with fresh frozen plasm (FFP) and platelet infusion if there is urgency to perform surgical drain of CSDH. Otherwise, about 10 days was awaited after discontinuation of blood thinners before performing surgery. Patients who had steroid therapy received a tapering 3-weeks course of oral Dexamethasone at home or assisted living facility (4mg thrice daily on days 1 to 3, then 3mg thrice daily on days 4 to 6, then 2mg thrice daily on days 7 to 9, then 2mg twice daily on days 10 to 12, then 1mg thrice daily on days 13 to 15, then 1mg twice daily on days 16-18, then 1mg once daily form 19-21 days and then stopping the therapy). A proton pump inhibitor was given during corticotherapy to prevent steroid induced peptic ulceration.
Patients who had dexamethasone therapy for resolution of CSDH were evaluated on outpatient basis weekly with fasting and post-prandial blood sugar and blood tests for the presence of newonset diabetes and hypokalemia respectively, steroid induced new-onset psychosis, peptic ulceration and gastrointestinal bleeding, and other gastrointestinal side effects. Adherence to medical therapy was confirmed by reviewing patient’s or next of kin medication records and patient diaries to confirm that the medication was taken at home. Patients who were symptomatic and CT head showed mass effect from persisting CSDH despite completion of 3 weeks of Dexamethasone therapy were given option to undergo surgery to evacuate the hematoma. If agreed upon, these select group of patients underwent standard burrhole evacuation of CSDH with subdural drain.
Outcomes
The author believes that Dexamethasone is a potent antineomembrane and anti-angiogenic agent which is safe and effective treatment for CSDH that positively compares to surgical drain of the subdural collection. The author does not intend to undermine the importance of surgical evacuation of CSDH, but Dexamethasone can be a viable option, especially in specific circumstances, especially in patients with CSDH with minimal or moderate symptomatology and not severely affected neurologically or functionally. In these select subset of patients with chronic subdural hematoma, corticotherpay can be a conservative alternative treatment option in comparison to surgical drain of subdural blood collection.
Ethical issues seems to be a non-entity in this study considering patient or his/her next of kin chose the treatment modality on their own accord which has proven to be effective backed by evidence based medicine and substantial literature on both modalities of treatment for CSDH [8,9]. The modified Ranking scale (mRS) is an ordinal scale to evaluate patient’s functional status with respect to activities of daily living and has wide spread clinical application for several diseases [10,11]. This scale has seven categories: no symptoms-0, no clinically significant disability despite symptoms-1, slight disability-2, moderate disability-3, moderately sever disability-4, severe disability-5, and death-6; in this study, a score of 0 to 3 was used to indicate a favorable outcome.
In lieu with the previous studies of CSDH [12,13], the primary outcome was 1) a score of 0 to 3 on the mRS at 6 months after enrollment in the study, suggesting favorable outcome 2) resolution or significant reduction of chronic subdural collection at the end of index admission for the surgical group and at the end of 3 weeks of dexamethasone therapy for medical group (designated Cure Rate in current study). Resolution of SDH was defined as above 90% reduction in the thickness of the fluid collection with symptomatic relief. Significant reduction was described as above 75% reduction in the thickness of the subdural collection of blood with symptomatic relief.
Secondary outcome was the score on mRS at the end of each respective therapies and at 3 months interval after completion of respective treatment modalities, the number of patients who had to undergo surgical interventions during subsequent admission in the follow-up period. This entails surgery for recurrence of subdural hematoma following burr-hole evacuation of subdural collection in the surgical group or after corticotherapy. Surgical intervention in patients who had corticotherapy and could not effect a cure is also reported in current study. Post-operative recurrence of CSDH was defined as symptomatic re-accumulation of the ipsilateral subdural fluid that was previously evacuated.
Tertiary outcome was mortality at 30 days and 6 months after enrollment of patients in two distinct therapeutic modalities. It also includes morbidity related to both medical and surgical therapies.
Statistical Analysis
The two cohort of patients (surgical group vs Dexamethasone group) were matched for age, sex, GCS on presentation and initial modified Rankin Score. Overall effect was shown with the risk ratio (RR) and its 95% confidence interval (95% CI). Comparisons between Dexamethasone alone therapy versus the surgical drain were made to identify the effectiveness of Dexamethasone therapy. A two-tailed P value < 0.05 set as the level of significance under the assumption of a normal distribution curve in the current study. Statistical significance between two groups was examined by Pearson Chi-Square test or Fisher exact test for categorical variables and Student t-test or Mann-Whitney U-test for continuous variables respectively. Multivariate Logistic Regression analysis models (using the ordinal modified Rankin Scale) [14] were performed to compare variables between two select cohorts.
Results
The age in each group was about 62 years, with male predominance (64% in Dexamethasone group and 67% in the surgical group) (Table 1). The most common cause of CSDH, irrespective to the assigned group for patients with CSDH was head trauma (about 67%), followed by use of blood thinners and spontaneous in nature (14.2% and 18% in Dexamethasone group, and 16.7% and 16.7% in the surgical group respectively). Head, gait instability and cognitive impairment were the most common presenting symptoms in descending order (71.4%, 53.6% and 43% in Dexamethasone group as compared to surgical group (70%, 56.6% and 46.6% respectively). Ischemic heart disease, diabetes mellitus and chronic obstructive pulmonary disease were the most common presenting morbidity in each group (43%, 28.5% and 21.4% in Dexamethasone group compared to 46.6%, 33.3% and 26.6% respectively). The midline shift in brain due to mass effect from ipsilateral CSDH is most commonly in the range of 6-10 mm as evident on CT head (43% and 46.6% in Dexamethasone group and surgical group respectively). The patients who underwent surgery during index admission for surgical drain of SDH mean stay with SD was 5 days ±1.8.
Primary outcome
A favorable functional outcome determined by modified Rankin scale (mRS) score of 1 to 3 at 6 months follow-up was 25/28 (89.2%) in Dexamethasone group compared to 28/30 (93.3%) in surgical group (difference, -4.1 [95% CI, -6.8 to -2.2], p value =0.12). The difference was not statistically significant. The cure rate was 23/28 (82.1%) in Dexamethasone group compared to 28/30 (93.3%) in the surgical group during index admission (difference, -11.2, [95% 95% CI -14.3 to -7.6] in favor of the surgical group, p=0.005). About 18% patients (5/28) had to undergo surgical drain of subdural collection for failure to resolve following full course of corticotherapy.
Secondary outcome
A favorable functional outcome (mRS score of 1-3) at 3 months follow-up was 26/28 (92.8%) in Dexamethasone group compared to 28/30 (93.3%) in surgical group (difference, -0.5 [95% CI, -2.2 to -0.1], p value =1.24 (Table 2). It was comparable between 2 groups at 3 months follow-up. Similarly, at the time of discharge for surgical group during index admission and end of therapy for oral dexamethasone group, favorable outcome determined by mRS was not statistically significant. It was 25/28 (89.2%) in Dexamethasone group compared to 28/30(93.3%) [Point Difference -4.1 (-8.8 to -2.2), p value= 0.08]. Hence at no point in time, surgical group had significantly better outcome compared to corticotherapy group. Only 3 patients (10%) in the surgical group had to undergo repeat evacuation of subdural fluid collection during index admission after first surgery failed to resolve CSDH. Three patients (10%) in the surgical group had subsequent surgery for tension pneumocephalus, contralateral acute subdural hematoma and acute intracerebral hemorrhage (the latter probably due to brain laceration from the subdural irrigation catheter). Recurrence rate for CSDH was 2/28 (7.1%) in Dexamethasone group compared to surgical group 4/30 (13.3%) [Point difference of –6.2 (-4.2 to -8.4)] which was statistically significant (p=0.01).
Tertiary outcome
Morbidity related to stand alone Dexamethasone therapy and surgical drainage of CSDH were 17.8% (5/28 patients) compared to 13.3% (4/30) with Rate Ratio of 1.34 (range 0.8 to 1.7) with p value of 0.10. Hence morbidity related to corticotherapy did not reach statistical significance compared to the surgical therapy. The most common adverse effects related to medical therapy (Table 3) was hyperglycemia 17.8% (5/28 patients), followed by gastrointestinal problems including peptic ulceration and nosocomial infection, latter two representing 2/28 patients each (7.1%). In the surgical group, the most common complications were superficial wound infections in 3 out 30 patients (10%) and inappropriate secretions of ADH leading to hyponatremia (2/30 patients, 6.6%). They were managed with appropriate antibiotics and water/fluid restriction. No morbidity related to either therapy were life threatening in this study. There was no mortality at the time of discharge after surgery or end of medical therapy, same applies at 3 months follow-up period. Mortality was 1 patient each in assigned groups at 6 months follow-up, which was not directly related to treatment instituted.
Discussion
Chronic subdural hematoma is a common but retractable neurological disease in the elderly with a noteworthy recurrence rate (up to 25% has been reported in the literature) [9]. The pathophysiology of CSDH has been well elucidated. The process of re-bleeding and breakdown of erythrocytes exacerbated the inflammatory reaction, following by the formation of neomembrane and neo-capillaries. This cycle of the re-bleedingcoagulation- fibrinolysis process eventually led the hematoma to enlarge or recur [9]. Glucocorticoid, a potent anti-inflammatory agent has been found to inhibit neo-membrane and neoangiogenesis [15]. This has been the rationale for the use of Dexamethasone orally or intravenously to treat CSDH.
A review and meta-analysis study on Dexamethasone role for CSDH concluded even though corticotherapy has been used as stand-alone medical therapy, it’s effectiveness as a better alternative to surgical therapy has not been proven [9]. But adjuvant Dexamethasone therapy to surgical drain of CSDH is known to reduce the recurrence of this disease. Trial of Dexamethasone for Chronic Subdural Hematoma (Dex-CSDH) provided much needed multicenter randomized controlled study to elucidate efficacy and safety of Dexamethasone compared to placebo in treating symptomatic CSDH [8]. In this study, almost all patients underwent an initial operation to remove hematoma, no firm conclusion could be drawn regarding the effect of Dexamethasone as a method of conservative management to avoid surgery. However, it did further strengthen the existing literature about the potency of corticotherapy to avoid recurrence of chronic subdural hematoma.
Current study is inspired by anecdotal experience of the author in successfully implementing corticotherapy as standalone therapy for symptomatic CSDH. In his experience, he got better results from 3 weeks of tapering regimen of oral Dexamethasone drug as compared to routinely used 2 weeks of corticotherapy in respect to resolution of subdural fluid collection. This was achieved with acceptable adverse effects related to considerable period of glucocorticoid therapy with strict vigilance of patient during this therapy. When pilot study on Dex-CSDH was published in 2019 with its inception in 2015 [16], the author was enthusiastically propelled to contemplate similar study in the country of his medical practice. The author wanted to conduct a randomized controlled trial comparing the efficacy and safety of Dexamethasone therapy with surgical drain of subdural collection.
Since patient were not keen on randomization and their preference of therapy was paramount, it ended up being a multicenter, prospective, non-randomized but controlled study. The author believed that CSDH patients with poor neurological and functional status should be subjected to surgical drainage for urgent alleviation of their symptomatology and neurological recovery. Hence, mild to moderately symptomatic patients with favorable functional outcome were only enrolled for corticotherapy (GCS of 13-15 and mRS score of 1-3). Being a comparative and controlled study, the surgical group also constituted patients with similar neurological and functional status as Dexamethasone group. All the eligible patients who were assigned to either Dexamethasone group or surgical group were matched for age, sex, GCS score and mRS score at the time of enrollment in the study.
Current study shows that at 6 months follow-up, functional outcome of patients based on modified Rankin Score scale was not statistically significant between stand-alone Dexamethasone group and surgery group. Similar picture emerged for patient’s functional outcome at end of respective therapies or at 3 months following discharge from medical care. However, the cure rate which specified significant or complete resolution of CSDH with symptomatic relief was statistically significantly higher in surgical arm compared to medical therapy (82.1% for Dexamethasone group vs 93.3% for surgery group, P value of 0.005). The recurrence rate for CSDH in Dexamethasone group was lower compared to surgical group which reached statistical significance (7.1% for corticotherapy vs 13.3% for surgical group, P value of 0.01). This is line with most of the studies in existing literature and corroborated by Dex-CSDH study [8].
As shown by various study including Dex-CSDH trial , in this study adverse effects or morbidity related to Dexamethasone therapy was not markedly higher compared to surgical therapy (not statistically significant on analysis). None of the patients in this study had life threatening complications related to respective therapies. About 18% (5 out of 28 patients) in medical treatment group had failure of therapy to resolve CSDH, hence underwent surgical evacuation of the subdural collection. This is in contrast to 2 patients (6.7%) who failed to be cured by surgical evacuation of subdural hematoma at the end of index admission. These two patients had multi-loculated subdural hematoma which prevented from surgical cure. In totality, 3 patients had re-do surgery for removal of residual and symptomatic CSDH during index admission through burr-hole drainage. Three patients (10%) in the surgical group had subsequent surgery unrelated to recurrence of CSDH (e.g., tension pneumocephalus, contralateral acute subdural hematoma collection etc.). There was one mortality among patients belonging to both types of therapies at 6 months follow-up, but probably unrelated to the instituted therapies.
Our trial has limitations, the most important being a nonrandomized trial and small sample size. Another arm of patients with Dexamethasone as an adjunctive treatment to surgery would have added more clarity and substance to this study.
Conclusion
Current study exhibits superiority of surgery over Dexamethasone therapy for resolution of symptomatic chronic subdural hematoma. The recurrence rate of CSDH is lower in patients with corticotherapy compared to surgical drain. Patients in Dexamethasone therapy did not have morbidity significantly higher than surgical group. This study strongly puts forward the utility of Dexamethasone as a viable alternative to surgery for CSDH. It can be a safe and effective stand-alone therapy especially in subset of CSDH patients with initial good neurological and functional status.
For more articles in Open access Journal of Head Neck & Spine Surgery | Please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | Please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf
#Head and Neck Surgery Journal#Chronic subdural hematoma#dexamethasone#surgery#Functional outcome#Corticotherapy
0 notes
Text
Risk factors for developing subdural hematoma: a registry-based study in 1457 patients with shunted idiopathic normal pressure hydrocephalus
Risk factors for developing subdural hematoma: a registry-based study in 1457 patients with shunted idiopathic normal pressure hydrocephalus
J Neurosurg 134:668–677, 2021 Subdural hematomas and hygromas (SDHs) are common complications in idiopathic normal pressure hydrocephalus (iNPH) patients with shunts. In this registry-based study, patients with shunted iNPH were screened nationwide to identify perioperative variables that may increase the risk of SDH. METHODS The Swedish Hydrocephalus Quality Registry was reviewed for iNPH…

View On WordPress
0 notes
Text
Introduction: Dangerous behavior is considered an undesired trait, often attributed to poor training or bad-tempered horses. Unfortunately, horses with progressive signs of dangerous behavior are often euthanized due to concerns for rider safety and limitations in performance. However, this dangerous behavior may actually originate from chronic axial skeleton pain. This case series describes the medical histories and clinical presentations of horses presented for performance limitations and dangerous behavior judged to be related to intractable axial skeleton pain.
...
Fourteen horses that developed severe performance limitations resulting in euthanasia were included. A complete spinal examination and behavioral responses, gait and neurologic evaluations, diagnostic imaging, gross pathologic and histopathologic examinations of the axial skeleton were performed on all horses. A tentative diagnosis of the affected spinal region was formulated using medical records, owner and trainer complaints, and antemortem examination findings.
...
Ten horses showed severe behavioral responses during the myofascial and mobilization examinations. Based on an aggregate evaluation, the cervicothoracic and lumbosacral regions were the most common regions believed to be the primary area of concern. All horses had moderate to severe ganglionitis present at multiple vertebral levels. Subdural and epidural hemorrhage or hematomas were a common finding (71%) in the cervicothoracic and lumbosacral regions.
...
The mean age was 9.4 ± 2.6 years and included eleven geldings and three mares. The breeds included eight warmbloods, four Thoroughbreds, one Quarter Horse, and one Andalusian. Eight of the horses were used for dressage, four for eventing, one for show hunting, and one for barrel racing. The owners' chief complaint and reports of dangerous behavior were recorded. In 12 horses, the time from purchase to euthanasia was 2.5 ± 1.8 years. The other two horses were raised by their owner, and the time from initial complaint to euthanasia was less well-defined.
Related article:
23 notes
·
View notes
Note
Miniscrew, I find the fact that you gave Four a chronic subdural hematoma really funny, because I'm also writing some Four whump, and gave him an acute subdural hematoma XD same condition just a little to the left
Four just has that
Subdural 🧠 Hematoma 🩸 Energy 🥵
No but for real this is sending me 😂 That we just looked at this guy and individually decided that Yeah, this dudes brain is broken.
Anon please let me know when you publish your fic! I’m super interested!
1 note
·
View note
Note
how long can a person survive with a subdural hematoma before it becomes an emergency?
The symptoms of a subdural hematoma can develop soon after a severe head injury (acute subdural haematoma), or very occasionally a few days or weeks after a more minor head injury (subacute or chronic subdural haematoma). Left untreated, it could damage the brainstem, which could lead to coma or death. It’s important that they get treatment for their head injury as soon as possible; the sooner the hematoma is detected and treated, the better the outlook.
67 notes
·
View notes
Text
uhhhhhh discussion of parental stuff/death/medical stuff under the cut so reader beware, you’re in for a scare i guess.
i used to think it would be easy for me to deal with my mom’s death.
i was so sure i hated her. i was so sure i could let go. i was so sure i could just walk away and not feel anything about this. which was ignorant of me of myself, when i know that i feel in the deepest parts of my stupid heart for everyone. when i know no matter how much she fucks up i’m always, always going to care.
and then i realized my mom was just as scared a kid as i was. that we were both horribly stinted people abused into points in our lives that we struggle to move beyond. we talked about the issues we survived involving mark (my sperm donor). we came to an honest consensus. we were going to do therapy as a family. i was going to get a service dog to help me. i was going to find a way to bond with my mom, or find a way to heal some of what’s hurting. we got to talk to each other on terms where we tried to understand each other.
and then it started with a mini stroke. her chronic 20 year neuropathy. her shutdown kidneys. 2 subdural hematomas-- one nine inches and one only two. they sent her home on the day she had fucking brain surgery. she suffered splitting migraines for two weeks where she had to stay in the dark continuously because she couldn’t even look at anything. and then it was what we thought was a stroke. and then she went into a rehab facility and came out completely bedridden because the fucking place treated her like shit, she refused to ‘inconvenience’ them by asking for anything, and they barely moved her.
my mom has been a spoiled, spoiled fuck since childhood. she was raised as ‘the sick child’ and as a result they neglected my aunt and showered her with constant attention, stymied all her opportunities for independence, and then she rebelled so hard she trashed her condition for the rest of her life.
i thought it would be easy to let my mom go. i thought this process wouldn’t hurt me, because she had hurt me so many times. i thought i could walk away knowing i’d be a better parent, a better partner, a better friend than she ever was to anyone, or to me.
she’s downstairs screaming in pain because her colon is severely impacted and my room is directly above hers. yeah, i can put my headphones in and drown it out but.... it’s not going away. my mom’s not going to get better. we know it, it’s obvious.
we were going to do family therapy. we were going to try harder.
i don’t know how to feel. i don’t know what to do. i hate seeing other people in pain. and all i can think about is how mark was terrible to the both of us, and how it impacted my mother to the point of her own trauma. how she’s lived with the depression that led to the cycle of abuse/neglect that she enacts on me. how none of this would be this way if one fucking monster of a man hadn’t acted to his full monstrous capacity, and now he’s somewhere in brooklyn, married and probably lying about me being the ‘awful child who won’t talk to him’. he texted me on my birthday. i wasn’t entertaining that.
i think what i’m feeling is that... everything’s going to end unfinished. i’m angry. i’m angry i’m going to lose my mom before she and i could ever really understand each other. i’m angry that i never really had parents. i’m angry that one of my parents abused me into chronic fear, and everything wrong with my brain now, and the other one, the one i thought was going to be my parent, isn’t going to be around much longer to even make strides toward us being emotionally okay or close. she can’t handle therapy, certainly not now. she can barely answer my questions when i ask her how she’s feeling.
there’s literally no way to make this better.
#negativity /#negative /#death /#parental death /#parental mention /#medical /#hospital mention /#ooc. & that’s when the cannibalism started.#[if you're having a bad day definitely don't click that readmore.#i'm really emotional and i don't want anyone else to feel like shit.#if you're having a bad day you should know: i love you and i'm sending you good vibes for it to improve.]
5 notes
·
View notes
Text
Subdural Hematoma Treatment Market Growth, Analysis, Size and Forecast 2029
Global Subdural Hematoma Treatment Market, By Type (Acute Subdural Hematoma, Subacute Subdural Hematoma, Chronic Subdural Hematoma), Treatment (Anticonvulsants, Diuretics, Corticosteroids, Surgery, Catheter, Physical Therapy, Speech Therapy, Vitamin K Therapy, Others), Diagnosis (CT scan, MRI, Others), Dosage (Tablet, Injection, Others), Route of Administration (Oral, Intravenous, Others), Symptoms (Seizures, Change in behavior, Headache, Nausea, Confusion, Dizziness, Vomiting, Lethargy, Apathy, Weakness, Others), End-Users (Clinic, Hospital, Others), Distribution Channel (Hospital Pharmacy, Retail Pharmacy, Online Pharmacy), Country (U.S., Canada, Mexico, Brazil, Argentina, Peru, Rest of South America, Germany, France, U.K., Netherlands, Switzerland, Belgium, Russia, Italy, Spain, Turkey, Hungary, Lithuania, Austria, Ireland, Norway, Poland, Rest of Europe, China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Vietnam, Rest of Asia-Pacific, Saudi Arabia, U.A.E, Egypt, Israel, Kuwait, South Africa, Rest of Middle East and Africa) Industry Trends and Forecast to 2028.
An expert team performs systematic, object-oriented and complete market research study to provide the facts associated with any subject in the field of marketing via Subdural Hematoma Treatment marketing report. The report has a lot to offer to both established and new players in the Subdural Hematoma Treatment industry with which they can completely understand the market. SWOT analysis and Porter’s Five Forces analysis methods are used wherever applicable, while generating this report. One of the most important parts of an international Subdural Hematoma Treatment market report is competitor analysis with which businesses can estimate or analyse the strengths and weaknesses of the competitors.
Key Players
The major players covered in the Subdural Hematoma Treatment market report are Merck Sharp & Dohme Corp., Northeast Pharmaceutical Group Co., Ltd., Cayman Chemical, Tokyo Chemical Industry Co. Ltd., ,Kaiyuan Hengtai Nutrition Co., Ltd., ChengDa PharmaCeuticals Co.,Ltd., Avanscure Lifesciences Pvt. Ltd., Biosint SpA, Maxsun Industries, MANUS AKTTEVA BIOPHARMA LLP, Huanggang Huayang Pharmaceutical Co., Ltd., Merck KGaA, Viachem Limited and Spectrum Chemical Manufacturing Corp., among other domestic and global players. Market share data is available for Global, North America, Europe, Asia-Pacific (APAC), Middle East and Africa (MEA) and South America separately. DBMR analysts understand competitive strengths and provide competitive analysis for each competitor separately.
Browse More Info @ https://www.databridgemarketresearch.com/reports/global-subdural-hematoma-treatment-market
With the help of credible Subdural Hematoma Treatment market analysis report, businesses can make out the reaction of the consumers to an already existing product in the market. The report includes estimations of recent state of the market, CAGR values, market size and market share, revenue generation, and necessary changes required in the future products. A wide-ranging competitor analysis helps build superior strategies of production, improvement in certain product, its advertising or marketing and promotion for the business. Exhaustive and comprehensive market study performed in the wide ranging Subdural Hematoma Treatment market report offers current and forthcoming opportunities that put light on the future market investment.
Key questions answered in the report:
Which product segment will grab a lion’s share?
Which regional market will emerge as a frontrunner in coming years?
Which application segment will grow at a robust rate?
Report provides insights on the following pointers:
Market Penetration: Comprehensive information on the product portfolios of the top players in the Subdural Hematoma Treatment Market.
Product Development/Innovation: Detailed insights on the upcoming technologies, R&D activities, and product launches in the market.
Competitive Assessment: In-depth assessment of the market strategies, geographic and business segments of the leading players in the market.
Table Of Content
Part 01: Executive Summary
Part 02: Scope Of The Report
Part 03: Global Market
Part 04: Global Market Size
Part 05: Global Market Segmentation By Product
Part 06: Five Forces Analysis
More Reports:
Diuretic Drugs Market
Patient Engagement Technology Market
Healthcare Business Intelligence Market
Chinese Hamster Ovary cells (CHO) Market
Anti-cancer Drug Market
About Us:
Data Bridge Market Research set forth itself as an unconventional and neoteric Market research and consulting firm with unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market
Contact:
Data Bridge Market Research
Tel: +1-888-387-2818
Email: [email protected]
0 notes