Don't wanna be here? Send us removal request.
Text
the only FDA approved biomarker for traumatic brain injury, the Brain Trauma Indicator™

The Brain Trauma Indicator™ (BTI™) works by measuring levels of proteins, known as UCH-L1 and GFAP, that are released from the brain into blood and measured within 12 hours of head injury. Levels of these blood proteins after mTBI/concussion can help predict which patients may have intracranial lesions visible by CT scan and which won’t. Being able to predict if patients have a low probability of intracranial lesions can help health care professionals in their management of patients and the decision to perform a CT scan. Test results can be available within 3 to 4 hours.
The Brain Trauma Indicator was able to predict the presence of intracranial lesions on a CT scan 97.5 percent of the time and those who did not have intracranial lesions on a CT scan 99.6 percent of the time
A step-wise increase in biomarker concentrations over the continuum of severity from mild to severe TBI was detected. Of the two, only the neuronal biomarker UCH-L1 had the potential to detect acute intracranial lesions, as assessed by CT. Most importantly, both markers were substantially increased in TBI patients with a normal CT. Serum UCH-L1 and GFAP concentrations also strongly predicted poor outcomes
references: (1) https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-first-blood-test-aid-evaluation-concussion-adults?utm_medium=email&utm_source=transaction#:~:text=Press%20Announcements-,FDA%20authorizes%20marketing%20of%20first%20blood%20test%20to%20aid,evaluation%20of%20concussion%20in%20adults&text=The%20U.S.%20Food%20and%20Drug,to%20as%20concussion%2C%20in%20adults (2) https://www.cureus.com/articles/89515-advances-in-traumatic-brain-injury-biomarkers#references (3) Ghaith, H.S., Nawar, A.A., Gabra, M.D. et al. A Literature Review of Traumatic Brain Injury Biomarkers. Mol Neurobiol 59, 4141–4158 (2022). https://doi.org/10.1007/s12035-022-02822-6
10 notes
·
View notes
Text
“jigsaw” depressed fracture

This is a case report of a 13 year old boy who had head trauma with a resultant closed depressed skull fracture (figure a and b). family refused surgical intervention and patient was discharged. after 2 years patient presented to ER with seizure and CT (figure c and d) showed no bone defect with bilateral frontal gliosis.
The depressed broken fragment was displaced such that it fit back in the skull topography such as the pieces of a jigsaw puzzle, hence the term, “jigsaw” depressed fracture was suggested.
Reference: (1) Asian J Neurosurg.2016 Jan-Mar; 11(1): 76. doi: 10.4103/1793-5482.165786
1 note
·
View note
Text
pseudogrowing skull fracture



Reference: (1) Sekhar, L. N., & Scarff, T. B. (1980). Pseudogrowth in Skull Fractures of Childhood. Neurosurgery, 6(3), 285–289. doi:10.1227/00006123-198003000-00011
0 notes
Text
types of growing skull fracture



Reference: (1) Naim-ur-Rahman, Jamjoom, Z. A. A. B., Jamjoom, A. H. B., & Murshid, W. R. (1994). Growing skull fractures: classification and management. British Journal of Neurosurgery, 8(6), 667–679. doi:10.3109/02688699409101180
0 notes
Text
twist drill for evacuation of chronic subdural hematoma
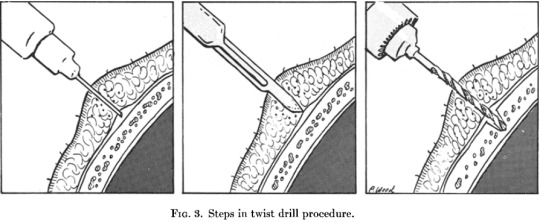

References: (1) Rand, B. O., Ward, A. A., & White, L. E. (1966). The Use of the Twist Drill to Evaluate Head Trauma. Journal of Neurosurgery, 25(4), 410–415. doi:10.3171/jns.1966.25.4.0410 (2) https://www.netterimages.com/craniostomy-for-chronic-subdural-hematoma-unlabeled-neurology-neurosciences-frank-h-netter-1165.html
0 notes
Text
Blood age in MRI





in one study signal characteristics of cSDH on T1- and T2-weighted images were very heterogeneous and that the most frequent pattern was was a mixed signal in both sequences (table)

Reference: (1) https://mriquestions.com/hematoma-overview.html (2) https://doi.org/10.3389/fneur.2022.87266
0 notes
Text
C1 screw

reference: (1) Ma, Xiang-Yang MD, PhD; Yin, Qing-Shui MD; Wu, Zeng-Hui MD; Xia, Hong MD; Liu, Jing-Fa MD*; Xiang, Ming MD†; Zhao, Wei-Dong MD‡; Zhong, Shi-Zhen PhD‡. C1 Pedicle Screws Versus C1 Lateral Mass Screws: Comparisons of Pullout Strengths and Biomechanical Stabilities. Spine: February 15, 2009 - Volume 34 - Issue 4 - p 371-377 doi: 10.1097/BRS.0b013e318193a21b
0 notes
Text
80/20 load-sharing concept

In a normal lumbar spine in the upright standing position, the anterior and middle weight-bearing columns of the spine support approximately 80% of spinal loads while the posterior column only supports 20%. However, with aging and the consequences of the degenerative cascade including dehydration of the nucleus and repetitive annular injuries reducing the height of the disc, the weight bearing shifts such that the posterior column supports a greater percentage of the axial load
reference: (1) Mobbs, Ralph & Loganathan, Ajanthan & Yeung, Vivian & Rao, Prashanth. (2013). Indications for Anterior Lumbar Interbody Fusion. Orthopaedic surgery. 5. 153-63. 10.1111/os.12048.
1 note
·
View note
Text
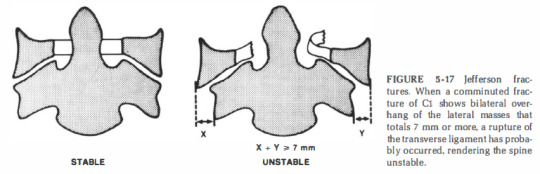
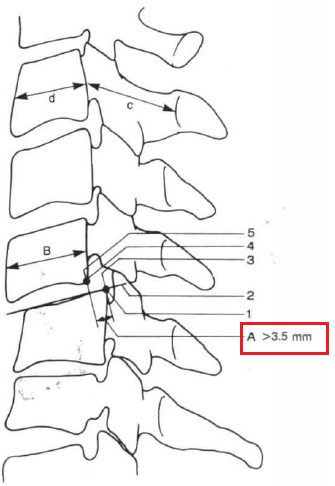
White and Panjabi checklists for spinal instability
A great reference textbook for spine biomechanics is "Clinical Biomechanics of the Spine" by White and Panjabi.
They define "clinical instability": the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain.
physiologic load: are those which are incurred during normal activity -flexion, extension, axial rotation, and lateral bending- of the particular patient being evaluated incapacitating pain: pain unable to be controlled by non-narcotic drugs
White and Panjabi proposed checklists based on their biomechanical data for spine instability
Occipital-atlanto-axial complex (any point should be considered as instability)

the images below explain point in the checklist:


2. Middle and lower cervical spine:

comments on the checklist: 1) anterior elements: posterior longitudinal ligament and all structures anterior to it. 2) posterior elements: all structures behind the posterior longitudinal ligament 3) patients with anterior elements destroyed or unable to function are more clinically unstable in extension, while patients with the posterior elements destroyed or unable to function are more unstable in flexion 4) It is not assumed that the information available on all patients will provide a definitive answer for each item on the list 5) It is recommended that when the evaluation of a given element leads the clinician to a borderline decision that cannot be resolved, the value for that entity should be divided by 2 and added to the other points
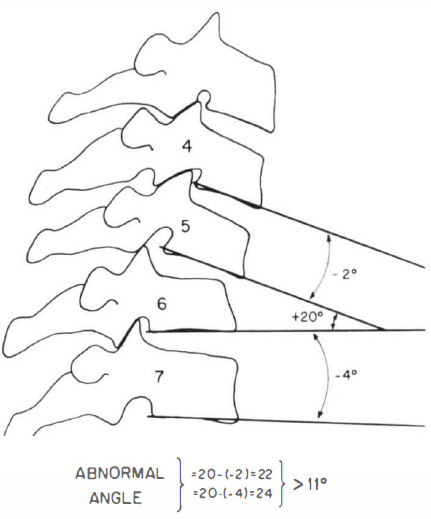
positive angle = kyphotic angle (intersection anterior to spine) negative angle = lordotic angle (intersection posterior to spine)

An abnormal test is indicated by either differences of more than 1 .7 mm interspace separation or more than 7.5 degrees of change in angle between vertebrae, comparing the prestretch condition with the situation after application of axial traction equivalent to one-third body weight.
=> Examples of patients in whom one can anticipate heavy loads are heavy laborers, contact sport athletes, and avid motorcyclists

Pavlov's ratio is a reliable, accurate method for recognizing a developmentally narrow canal without the variables involved in linear measurements. The measurement A is the distance between the midlevel of the posterior aspect of the vertebral body and the nearest point on the corresponding spinolaminar line. The measurement B is seen on lateral x-ray as the anteroposterior distance from the front to the back of the vertebral body measured at the midlevel. The ratio A/B is considered normal if 1 or greater and abnormal if less than 0.8.
=> In patients under 35 years of age, post-traumatic disc narrowing is modestly suggestive of disruption of the annulus fibrosus and of possible instability.
=> A congenitally narrow canal is defined as measuring less than 1 3 mm in its anteroposterior dimension on a lateral radiograph or having a Pavlov's ratio of less than 0.8.
=> if the trauma is severe enough to cause initial neurologic damage, the support structures probably have been altered sufficiently to allow subsequent neurologic damage, and thus the situation is clinically unstable.
=> Evidence of root involvement is a weaker indicator of clinical instability. For example, a unilateral facet dislocation may cause enough foraminal encroachment to result in root symptoms and/or signs but not enough ligamentous damage to render the FSU unstable
3. Thoracic and thoracolumbar spine

4. Lumbar spine
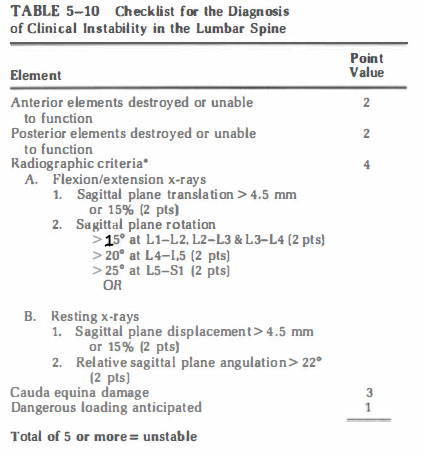
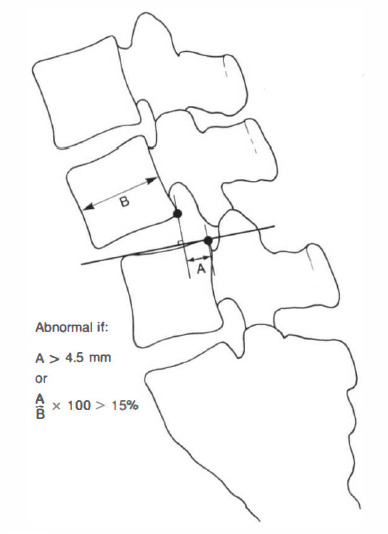
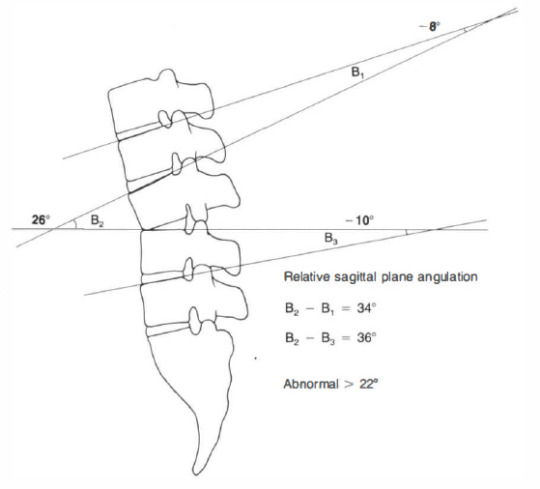
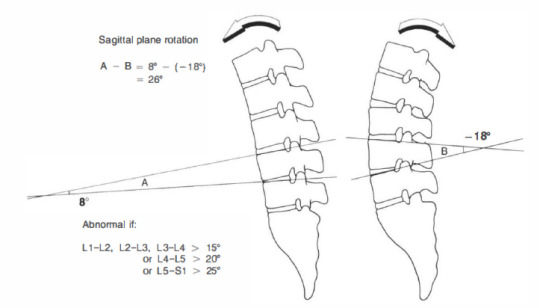
references: (1) clinical biomechanics of spine by Augustus A. White and Manohar M. Panjabi, chapter 5
#spine#trauma#textbook#neurosurgery#orthopedics#spinal cord#instability#biomechanics#medicine#surgery
0 notes
Text
Understanding Fisher's groups of SAH
In 1980 Fisher published an article about 47 patients with aneurysmal SAH to determine if there is a relationship between the distribution of blood detected on CT with the development of vasospasm.
In his study brain CT was done within 5 days of aSAH, angiogram was done during the period when vasospasm was likely to occur between days 7 and 17.
Then he categorized anatomical fissures and cisterns to localized the location of the SAH.

Accurate estimation of the amount of the SAH on CT was limited due to: 1- irregular dimensions of the cisterns and fissures, 2- inaccuracy in measuring blood densities due to different concentrations, partial volume effect and progressive isodensity with time, 3- in the interhemispheric fissure the falx contribute to the thickness of interhemispheric blood, although the falx itself measures less than 1 mm
Vertically oriented cisterns and fissures (interhemispheric fissure, insular cistern, ambient cistern) were more likely to show measurable layer of blood than were those which are horizontal (sylvian stem and fissure).
Thus, 4 groups are classified: Group 1: no blood on CT Group 2: diffuse deposition or thin layer with all vertical layers of blood (interhemispheric fissure, insular cistern and ambient cistern) less than 1 mm thick Group 3: localized clot and/or vertical layers of blood 1 mm or greater in thickness Group 4: diffuse or no SAH, but with ICH or IVH

Then he grouped and graded vasospasm based on location (ICA, M1, M2, A1, A2, P1) and based on severity (none, slight to moderate, severe). He also recognized the occurrence of delayed ischemic neurological deficit which was corresponding with severe vasospasm and no patient with slight to moderate vasospasm developed the delayed symptoms.
His finding was that in patients in group 3 almost all of the patients (23 patients out of 24) developed severe vasospasm. and all patients with severe vasospasm developed delayed neurological deficit (although in 1 patient it was slight). of the 23 patients, 3 died, 5 had permeant major deficit, 7 had permanent minor deficit.

Studying the location of the vasospasm in group 3 showed the ACA was involved in 20 patients, MCA in 14 patients, basilar artery in 1 patient. and there was a correspondence between site of major SAH and the location of severe vasospasm.
He came to a conclusion that the most important factor in predicting vasospasm is the amount of SAH in the proximal 9-10 cm of ACA and MCA. but not the presence of ICH, IVH or posterior fossa SAH.
Fisher recognized in his article the actual limitation of subjectivity in the interpretation of the CT, especially when we have do decide whether a patient belongs to group 2 or 3!
Komiyama -who was a chief editor in Interventional Radiology Journal- in his article he addressed the misunderstanding of Fisher's Grouping System, especially group 4. He noted that it is more appropriate to use the term "group" but not "grade". because in groups 1-3, the severity in graded in stepwise manner. however, group 4 is defined as diffuse (thin) or no SAH with IVH or ICH. where diffuse here mean very thin and diffusely distributed which might not cause vasospasm such as the thick group 3. So if a patient has thick SAH with ICH or IVH it is group 3. see the example below which is fisher group 3 due to the presence of thick SAH -but not group 5.

The Modified Fisher Scale came to solve the problem of the stepwise scale. Although if a patient has pure ICH or IVH without SAH it cannot be graded using the modified scale.
Then came the article by Frontera et al. where he described the Modified Fisher Scale. In the study CT finding on admission were classified into categories as diffuse or local thin, diffuse or local thick, no SAH and the presence or absence of IVH. No explicit criteria was made for this classification. then the patients were classified into the old fisher's groups and into the new modified groups.

In his study 1355 patients met the inclusion criteria. The risk of developing vasospasm progressively increasing with modified fisher scale. but in the original fisher grade it was highest in grade 3 and then decreased for grade 4.
other predictors of vasospasm are: moderate to severe early angiographic vasospasm (within first 48 hours), MAP ≥ 112 mm Hg, history of hypertension, poor WFNS grade.

It was found that the modified scale has a stronger predictive power for vasospasm compared with the original scale. These results are based on surgically treated patients and may not be applicable to patients undergoing coil embolization.
The last think to talk about is the reliability of Fisher's grading system. which means the consistency in the measurement and the grading between observers.
Svensson et al. studied the reliability of Fisher's grading system by evaluating 59 CT scans according to Fisher's grade by four experienced neuroradiologists.
The proportion of total agreement of the four neuroradiologists was 46% (27/59). the main difference was in classifying grade 3 and grade 4. and it is concluded that the cause of this disagreement in the grading system itself and not the level of experience between the observers. the kappa coefficient was found to be 0.5-0.63. which is moderate to substantial agreement.

Variable rates of vasospasm corresponding to each Fisher grade have been reported in studies; therefore, the scale should not be used to quote an exact probability of vasospasm or delayed cerebral ischemia (DCI).

The scale does NOT apply to SAH due to trauma, arteriovenous malformations, cavernous angiomas, dural arteriovenous fistulae, cortical or sinus venous thromboses, mycotic aneurysms, or septic emboli with hemorrhagic transformation.
References: (1) Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980 Jan;6(1):1-9. doi: 10.1227/00006123-198001000-00001. PMID: 7354892. (2) Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES Jr, MacDonald RL, Mayer SA. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006 Jul;59(1):21-7; discussion 21-7. doi: 10.1227/01.NEU.0000218821.34014.1B. PMID: 16823296. (3) Komiyama M. Misunderstanding of Fisher's grouping system for computed tomography evaluation of aneurysmal subarachnoid haemorrhage. Interv Neuroradiol. 2019 Dec;25(6):653-654. doi: 10.1177/1591019919856511. Epub 2019 Jun 9. PMID: 31177930; PMCID: PMC6838856. (4) Svensson E, Starmark JE, Ekholm S, von Essen C, Johansson A. Analysis of interobserver disagreement in the assessment of subarachnoid blood and acute hydrocephalus on CT scans. Neurol Res. 1996 Dec;18(6):487-94. doi: 10.1080/01616412.1996.11740459. PMID: 8985947. (5) https://www.mdcalc.com/calc/3836/fisher-grading-scale-subarachnoid-hemorrhage-sah#pearls-pitfalls
#subarachnoid hemorrhage#cerebral aneurysm#aneurysm#neurosurgery#Fisher#brain#brain CT#surgery#neurology#medicine#science
1 note
·
View note
Text
Thunderclap Headache
Definition: severe headache with abrupt onset, reaching maximum intensity within one minute or less
Differential Diagnosis:



Idiopathic thunderclap headache:

references: (1) https://www.uptodate.com/contents/overview-of-thunderclap-headache (2) Dodick DW, Thunderclap headache, Journal of Neurology, Neurosurgery & Psychiatry 2002;72:6-11.
1 note
·
View note
Text
Biomechanics of Head Motion Injuries
Inertia is the resistance to change in velocity. head motion injury also called acceleration injury
Two mechanisms: 1- differential movement of the skull and brain (surface strain): causes localized strain between the skull and dura in relation to the brain thus can cause tearing of bridging veins or by creation of a region of low pressure to cause contrecoup injury. 2- strain within the brain parenchyma (deep strain): causes widespread disturbance in brain function and structure. causes concussion, DAI.

Three Types of Head Acceleration: Translational acceleration: central of gravity (pineal region) moves in straight line. uncommon. e.g, vertex impact, falling down of elevator. surface strain. causes contusions, ICH, SDH. concussion and DAI do not occur.
Rotational acceleration: rotation about the center of gravity. pure rotational acceleration is virtually impossible. highly injurious; surface strain + high level of deep strain.
Angular acceleration: translational + rotational acceleration. center of gravity moves in angular manner. because of neck anatomy, it is the most common head motion. frequently the center of rotation is in lower cervical spine. center of rotation and impact magnitude determine proportion of translation and rotation. as rotation center moves higher up the C-spine, the rotational component is proportionally greater. as rotation center moves lower, translational component is proportionally greater. it is the most damaging mechanism of all. can produce every known type of head injury except for skull fracture and EDH.

Determinants of Acceleration Injury: amount, type, duration, rate. Relationship between acceleration and duration of acceleration (velocity): - high acceleration + very brief duration = very little strain - high acceleration + short duration = superficial strain - high acceleration + long duration = deep strain
References: (1) Youmans and Winn Neurological Surgery, CHAPTER 374 Biomechanical Basis of Traumatic Brain Injury
0 notes
Text
Simultaneous ventriculoperitoneal shunt placement and repair of myelomeningocele
a couple of questions came to my mind when I have read this topic: 1- how it is done? what would be the position? 2- when to do it? 3- what is the outcome compared to two-staged surgery? How it is done? Hubballah et al. described the procedure in 1987: - infant is prone, head turned to the right, neck flexed. - hips rotated minimally to move the right flank into the operative field. - operative field prepared with Betadine and kept to dry. - area of shunt is covered with Ioban, area of MMC is not covered, but has a towel placed over it so that the Ioban does adhere to the exposed neural placode. - a small incision is made over the right lambdoid suture and the right flank and shunt is tunneled between the two incisions. the two incisions are sutured. - the towel is lifted off and the MMC is repaired. - prophylactic antibiotics for 5 days post-op.

Hubballah et al. performed this procedure for MMC patient with overt HCP at birth. he concluded that the benefits of this procedure are: to decrease the damage on the brain from the HCP and to eliminate the danger of wound breakdown, CSF leak, secondary CSF infection. this procedure does not increase the risk of shunt infection.
Chadduk et al. used a similar position to Hubballah and he also concluded that simultaneous surgery decreases the hospital stay, and lessens the expenses.
An article from India by Wakhlu et al. described the procedure by starting with the shunt placement in the supine position the change the position to prone for the repair of the myelomeningocele.
Another article from Barrow neurological institute by Nadkarni et al. described an intraoperative death of a newborn who underwent simultaneous surgery. The patient had overt HCP at birth. Occipital endoscopic shunt placement was done first in supine position, some CSF was lost during the procedure and patient had sunken fontanelles, then the infant was turn prone for repair of the MMC. after the procedure the patient was turned supine and move to the isolette and a blood-stained CSF was noted from the burr hole site. patient had a cardiorespiratory arrest and died. They concluded learned points from this case: The risk of endoscopic shunt placement increases markedly in massive HCP, CSF leakage might be decreased by placing a coronal burr hole for introducing the endoscope, manipulation of these infants after shunt placement should be minimized so the myelomeningocele should be repaired first.
References: (1) Hubballah MY, Hoffman HJ. Early repair of myelomeningocele and simultaneous insertion of ventriculoperitoneal shunt: technique and results. Neurosurgery. 1987 Jan;20(1):21-3. doi: 10.1227/00006123-198701000-00005. PMID: 3808266. (2) Chadduck WM, Reding DL. Experience with simultaneous ventriculo-peritoneal shunt placement and myelomeningocele repair. J Pediatr Surg. 1988 Oct;23(10):913-6. doi: 10.1016/s0022-3468(88)80383-x. PMID: 3236159. (3) Wakhlu A, Wakhlu G, Saxena S, Tandon RK. Single-stage treatment of spina bifida with hydrocephalus based on a prediction rule derived from preoperative cranial ultrasound. Pediatr Neurosurg. 2009;45(4):271-5. doi: 10.1159/000228985. Epub 2009 Jul 17. PMID: 19609095. (4) Intraoperative Death at Time of Endoscopic Shunt Placement in Newborn with Myelomeningocele: Case Report https://www.barrowneuro.org/for-physicians-researchers/education/grand-rounds-publications-media/barrow-quarterly/volume-16-no-4-2000/intraoperative-death-at-time-of-endoscopic-shunt-placement-in-newborn-with-myelomeningocele-case-report/
1 note
·
View note
Text
Findings in various levels of myelomeningocele
what is interesting is that myelomeningocele helped a lot in the study of the nerve root muscle supply by two means: first it gives a unique opportunity for stimulation of motor nerve roots and second to study of motor root lesions.
at least 50% of nerve supply to an individual muscle must be lost before clinical paralysis can be detected
infants born with myelomeningocele and treated conservatively are liable to remain paralyzed or become increasingly paralyzed. among the factors responsible for this deterioration may be traction exerted on the nerve roots passing from the plaque of spinal cord to the intervertebral foramina when the MM sac fools up with cerebrospinal fluid during the first week of life and the caudal roots tend to be more severely affected.
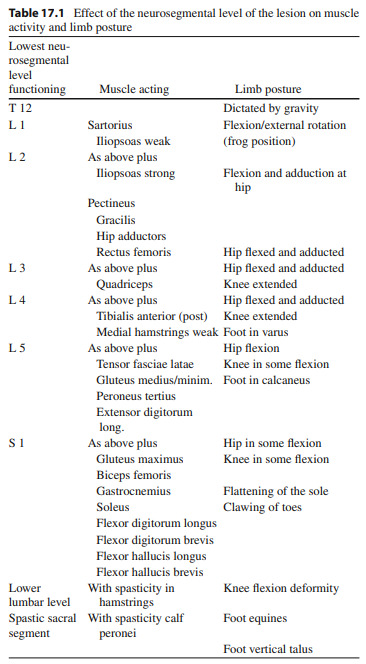
so lets go back to the title of this article, findings in various levels of myelomeningocele.
paralysis below T12: complete paralysis of lower limbs
paralysis below L1: weak to moderate hip flexion + weak sartorius = hip flexion and external rotation

paralysis below L2: strong hip flexion + moderate hip adduction = hip flexion and adduction

paralysis below L3: normal hip flexion + normal hip adduction + normal knee extension = hip flexion and adduction and knee extension
paralysis below L4: normal hip flexion + normal hip adduction + some hip abduction in flexion + normal knee extension + strong dorsiflexion and inversion = flexion and adduction and external rotation of hip + recurvatum of knee + calcaneo-varus foot


paralysis below L5: normal hip flexion + normal hip adduction + moderate abduction + no hip extension + normal knee extension + moderate knee flexion + normal inversion + moderate eversion + strong dorsiflexion + no planterflexion = hip flexion without adduction or abduction + semi-flexed knee + foot calcaneus

paralysis below S1: normal hip flexion + normal hip adduction + normal hip abduction + moderate hip extension + normal hip internal and external rotation + strong knee flexion + normal dorsiflexion + normal inversion + normal eversion+ moderate planterflexion + normal toes extension + strong great toe flexion + no foot intrinsic muscles (except abductor hallucis + flexor hallucis brevis) + weak flexor digitorum longus = clawing of toes and flattening of the skin of the sole of the foot

paralysis below S2: weak intrinsic muscles of foot = at clinical examination it is difficult to detect any abnormality but, with growth development of clawing of the toes.
so this study came with a conclusion regarding the innervation of muscles of the lower limbs

but newer studies using direct intraoperative nerve root stimulations during decompressive surgery concluded that a significant number of roots innervate a broader range of muscles than expected.
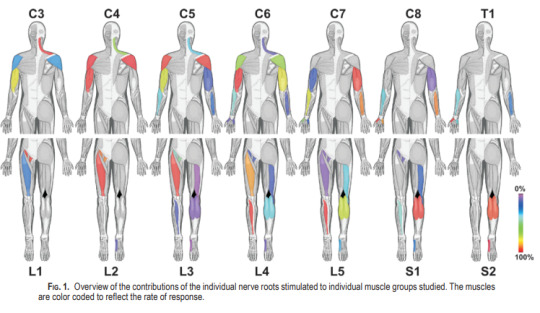
this table summarizes the neurological findings in MM
References: (1) SHARRARD WJ. THE SEGMENTAL INNERVATION OF THE LOWER LIMB MUSCLES IN MAN. Ann R Coll Surg Engl. 1964 Aug;35(2):106-22. PMID: 14180405; PMCID: PMC2311748. (2) Schirmer CM, Shils JL, Arle JE, Cosgrove GR, Dempsey PK, Tarlov E, Kim S, Martin CJ, Feltz C, Moul M, Magge S. Heuristic map of myotomal innervation in humans using direct intraoperative nerve root stimulation. J Neurosurg Spine. 2011 Jul;15(1):64-70. doi: 10.3171/2011.2.SPINE1068. Epub 2011 Apr 8. PMID: 21476796. (3) Graham, H. K., & Parsch, K. (2009). Neural Tube Defects, Spina Bifida, and Spinal Dysraphism. Children’s Orthopaedics and Fractures, 265–286. doi:10.1007/978-1-84882-611-3_17
0 notes
Text
Intelligence Quotient (IQ) in myelomeningocele
A family of a 20 day old patient with a repaired Myelomeningocele visited my clinic and they asked me about the expected prognosis for the intelligence for the child.
(1) A simple answer is that :
- patients with myelomeningiocele, with or without complications, have lower IQ than those without the lesion.
- Hydrocephalous decreases the IQ further in patients with MMC. Early correction of MMC can return the IQ to the MMC without hydrocephalous baseline.
- Shunt complications and revisions and CNS infections decrease the IQ even further.
- Higher lesion in spinal cord associated with lower IQ.
(2) An interesting article in the JNS discussed the neurobehavioral outcome in patients with myelomeningocele:
- MMC affects multiple anatomic levels which will affect neurobehavioral outcome:
. Spinal cord: deleterious effects of amniotic fluid on the neural placode. sensory and motor deficit. greater impact with higher lesions in spinal cord. deficits include weakness, sensory loss, incontinence, musculoskeletal anomalies. thoracic lesion associated with more severe brain anomalies and worse neurobehavioral outcome. motor impairment limits environmental exploration and learning experience.
. Chiari II malformation: in 96% in MMC at T12 and higher, 90% in MMC below T12. pathophysiology: leak of CSF through spinal defect > prevents normal distension of embryonic ventricular system and limits growth of posterior fossa > cerebellum develops in a smaller posterior fossa > downward displacement of the cerebellar tonsils, vermis and brainstem > cerebral abnormalities include corpus callosum hypoplasia, tectal beaking, polymicrogyria, cortical heterotopia > worse neurobehavioral outcome.
. Cerebellum: reduced cerebellar volume in MMC, more reduction in higher lesions. reorganization as anterior portion is larger and posterior-inferior portion is smaller. has a rule in cognition particularly executive functions. deficit in timing and precision of truncal, upper-limb, and eye movement and cognition.
. Brainstem and midbrain: due overcrowding of small posterior fossa and chiari. 65% of MMC have distorted midbrain, e.g, tectal beaking, which is colliculi fusion into a single beak. 70% have elongated and kinked medulla at the spinomedullary junction. deficit in eye movement and attention.
. corpus callosum: abnormality in 70%-90% of CM-II. hypoplasia or hypogenesis (partial formation). abnormalities primarily in posterior part (splenium), anterior part tend to be intact. variable abnormalities, include congenital and acquired (from complications like HCP). deficit severity correlates with abnormality of CC. deficit in cognition.
. Hydrocephalous: secondary to CM-II. pathophysiology: aqueductal occlusion, obstruction of 4th ventricle, eradication of subarachnoid space by overcrowded posterior fossa. HCP in 85%-90% of individuals with MMC without fetal surgery. expansion is posterior-to-anterior direction and cause stretching of parietal and occipital lobe axons around lateral ventricles. MMC with HCP +/- shunt exhibit worse neurobehavioral outcome compared to MMC without HCP. shunt revisions and infections add to cerebral damage.
. cerebrum: less common. gray matter heterotopia in 19% of MMC. seizure in 15%-25% of MMC, related to heterotopia and polymicrogyria. worse neurobehavioral outcome.
- Neurobehavioral profile of MMC
. cognitive deficit in MMC is significantly impacted by environment.
. assembled processing (integration of information) is affected by pathophysiology of MMC. associative processing less affected by MMC pathophysiology and more vulnerable to environmental factors.
. MMC patients have difficulties with
1- intelligence
2- attention
3- executive function
4- language
5- memory
6- visuospatial function
7- motor function
8- academic functions
9- psychosocial and adaptive concerns
References:
(1) Intelligence Quotient in Patients with Myelomeningocele: A Review: 10.7759/cureus.3137
(2) Neurobehavioral outcomes in patients with myelomeningocele: https://doi.org/10.3171/2019.7.FOCUS19445
1 note
·
View note
Text
Gestational age in neurosurgery
a family brought their 20 day old baby boy to my clinic today. He is a case of myelomeningiocele and underwent repair somewhere else. I asked the mother if the baby was a full term and she answered that she had delivered at the first week of the ninth month. and i went blank trying to calculate if the baby was term or not! so this is a review of gestational age:

Reference: Uptodate
GA is calculated in weeks from the first day of the last menstrual period.
So again: >42w postterm 37w - <42w term 34w - <37w late preterm 32w - <34w moderate preterm 28w - <32w very preterm <28w extreme preterm and generally any GA <37w is a preterm
another important note is that the estimated due date is at GA 40w = 280d = 9m + 1w
But she said that she delivered in the first week of the ninth month, how to convert that to weeks. lets put a rule: ‣ 3 months = 13 weeks for example 9 months + 1 week = 13 weeks + 13 weeks + 13 weeks + 1 week = 39 weeks + 1 week = 40 weeks ‣ months x 4.345 = weeks ‣ Google converter "months to weeks" is a great tool to use, keeping this in mind: 0.033 = 1 day in a month 0.23 = 1 week in a month for example: 8 months and 1 week = 8m + 0.23 = 8.23m
after all of that, what is really important to me is to know when a neonate is a preterm, when a neonate is <;37w. 37w = 13w + 13w + 11w = 3m + 3m + 11w = 6m + 11w = 6m + (11x7) = 6m + 77 days = 6m + 61 days + 16 days = 6m + 2m + 16 days = 8 month + 16 days = 8 month + 2 weeks + 2 days
What I really need to know from all of that a baby is term if the GA is equal to or more than 8m+2w+2d = 8.53m = 37w

1 note
·
View note
