#Caspase 8
Explore tagged Tumblr posts
Text
Caspase 8 Market Overview, Competitive Analysis and Forecast 2031
0 notes
Text
Retinal and choroidal vascular drop out in a case of severe phenotype of Flammer Syndrome. Rescue of the ischemic-preconditioning mimicking action of endogenous Erythropoietin (EPO) by off-label intra vitreal injection of recombinant human EPO (rhEPO) by Claude Boscher in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Background: Erythropoietin (EPO) is a pleiotropic anti-apoptotic, neurotrophic, anti-inflammatory, and pro-angiogenic endogenous agent, in addition to its effect on erythropoiesis. Exogenous EPO is currently used notably in human spinal cord trauma, and pilot studies in ocular diseases have been reported. Its action has been shown in all (neurons, glia, retinal pigment epithelium, and endothelial) retinal cells. Patients affected by the Flammer Syndrome (FS) (secondary to Endothelin (ET)-related endothelial dysfunction) are exposed to ischemic accidents in the microcirculation, notably the retina and optic nerve.
Case Presentation: A 54 years old female patient with a diagnosis of venous occlusion OR since three weeks presented on March 3, 2019. A severe Flammer phenotype and underlying non arteritic ischemic optic neuropathy; retinal and choroidal drop-out were obviated. Investigation and follow-up were performed for 36 months with Retinal Multimodal Imaging (Visual field, SD-OCT, OCT- Angiography, Indo Cyanin Green Cine-Video Angiography). Recombinant human EPO (rhEPO)(EPREX®)(2000 units, 0.05 cc) off-label intravitreal injection was performed twice at one month interval. Visual acuity rapidly improved from 20/200 to 20/63 with disparition of the initial altitudinal scotoma after the first rhEPO injection, to 20/40 after the second injection, and gradually up to 20/32, by month 5 to month 36. Secondary cystoid macular edema developed ten days after the first injection, that was not treated via anti-VEGF therapy, and resolved after the second rhEPO injection. PR1 layer integrity, as well as protective macular gliosis were fully restored. Some level of ischemia persisted in the deep capillary plexus and at the optic disc.
Conclusion: Patients with FS are submitted to chronic ischemia and paroxystic ischemia/reperfusion injury that drive survival physiological adaptations via the hypoxic-preconditioning mimicking effect of endogenous EPO, that becomes overwhelmed in case of acute hypoxic stress threshold above resilience limits. Intra vitreal exogenous rhEPO injection restores retinal hypoxic-preconditioning adaptation capacity, provided it is timely administrated. Intra vitreal rhEPO might be beneficial in other retinal diseases of ischemic and inflammatory nature.
Key words : Erythropoietin, retinal vein occlusion, anterior ischemic optic neuropathy, Flammer syndrome, Primary Vascular Dysfunction, anti-VEGF therapy, Endothelin, microcirculation, off-label therapy.
Introduction
Retinal Venous Occlusion (RVO) treatment still carries insufficiencies and contradictions (1) due to the incomplete deciphering of the pathophysiology and of its complex multifactorial nature, with overlooking of factors other than VEGF up-regulation, notably the roles of retinal venous tone and Endothelin-1 (ET) (2-5), and of endothelial caspase-9 activation (6). Flammer Syndrome (FS)( (Primary Vascular Dysfunction) is related to a non atherosclerotic ET-related endothelial dysfunction in a context of frequent hypotension and increased oxidative stress (OS), that alienates organs perfusion, with notably changeable functional altered regulation of blood flow (7-9), but the pathophysiology remains uncompletely elucidated (8). FS is more frequent in females, and does not seem to be expressed among outdoors workers, implying an influence of sex hormons and light (7)(9). ET is the most potent pro-proliferative, pro-fibrotic, pro-oxidative and pro-inflammatory vasoconstrictor, currently considered involved in many diseases other than cardio-vascular ones, and is notably an inducer of neuronal apoptosis (10). It is produced by endothelial (EC), smooth vascular muscles (SVMC) and kidney medullar cells, and binds the surface Receptors ET-A on SVMC and ET-B on EC, in an autocrine and paracrine fashion. Schematically, binding on SVMC Receptors (i.e. through local diffusion in fenestrated capillaries or dysfunctioning EC) and on EC ones (i.e. by circulating ET) induce respectively arterial and venous vasoconstriction, and vasodilation, the latter via Nitrite oxide (NO) synthesis. ET production is stimulated notably by Angiotensin 2, insulin, cortisol, hypoxia, and antagonized by endothelial gaseous NO, itself induced by flow shear stress. Schematically but not exclusively, vascular tone is maintained by a complex regulation of ET-NO balance (8) (10-11). Both decrease of NO and increase of ET production are both a cause and consequence of inflammation, OS and endothelial dysfunction, that accordingly favour vasoconstriction; in addition ET competes for L-arginine substrate with NO synthase, thereby reducing NO bioavailability, a mechanism obviated notably in carotid plaques and amaurosis fugax (reviewed in 11).
Severe FS phenotypes are rare. Within the eye, circulating ET reaches retinal VSMC in case of Blood-Retinal-Barrier (BRB) rupture and diffuses freely via the fenestrated choroidal circulation, notably around the optic nerve (ON) head behind the lamina cribrosa, and may induce all pathologies related to acute ocular blood flow decrease (2-3)(5)(7-9). We previously reported two severe cases with rapid onset of monocular cecity and low vision, of respectively RVO in altitude and non arteritic ischemic optic neuropathy (NAION) (Boscher et al, Société Francaise d'Ophtalmologie and Retina Society, 2015 annual meetings).
Exogenous Recombinant human EPO (rhEPO) has been shown effective in humans for spinal cord injury (12), neurodegenerative and chronic kidney diseases (CKD) (reviewed in 13). Endogenous EPO is released physiologically in the circulation by the kidney and liver; it may be secreted in addition by all cells in response to hypoxic stress, and it is the prevailing pathway induced via genes up-regulation by the transcription factor Hypoxia Inducible Factor 1 alpha, among angiogenesis (VEGF pathway), vasomotor regulation (inducible NO synthase), antioxidation, and energy metabolism (14). EPO Receptor signaling induces cell proliferation, survival and differentiation (reviewed in 13), and targets multiple non hematopoietic pathways as well as the long-known effect on erythropoiesis (reviewed in 15). Of particular interest here, are its synergistic anti-inflammatory, neural antiapoptotic (16) pro-survival and pro-regenerative (17) actions upon hypoxic injury, that were long-suggested to be also indirect, via blockade of ET release by astrocytes, and assimilated to ET-A blockers action (18). Quite interestingly, endogenous EPO’s pleiotropic effects were long-summarized (back to 2002), as “mimicking hypoxic-preconditioning” by Dawson (19), a concept applied to the retina (20). EPO Receptors are present in all retinal cells and their rescue activation targets all retinal cells, i.e. retinal EC, neurons (photoreceptors (PR), ganglion (RGG) and bipolar cells), retinal pigment epithelium (RPE) osmotic function through restoration of the BRB, and glial cells (reviewed in 21), and the optic nerve (reviewed in 22). RhEPO has been tested experimentally in animal models of glaucoma, retinal ischemia-reperfusion (I/R) and light phototoxicity, via multiple routes (systemic, subconjunctival, retrobulbar and intravitreal injection (IVI) (reviewed in 23), and used successfully via IVI in human pilot studies, notably first in diabetic macular edema (24) (reviewed in 25 and 26). It failed to improve neuroprotection in association to corticosteroids in optic neuritis, likely for bias reasons (reviewed in 22). Of specific relation to the current case, it has been reported in NAION (27) (reviewed in 28) and traumatic ON injury (29 Rashad), and in one case of acute severe central RVO (CRVO) (Luscan and Roche, Société Francaise d’Ophtalmologie 2017 annual meeting). In addition EPO RPE gene therapy was recently suggested to prevent retinal degeneration induced by OS in a rodent model of dry Age Macular Degeneration (AMD) (30).
Case Report Presentation
This 54 years female patient was first visited on March 2019 4th, seeking for second opinion for ongoing vision deterioration OR on a daily basis, since around 3 weeks. Sub-central RVO (CRVO) OR had been diagnosed on February 27th; available SD-OCT macular volume was increased with epiretinal marked hyperreflectivity, one available Fluorescein angiography picture showed a non-filled superior CRVO, and a vast central ischemia involving the macular and paraoptic territories. Of note there was ON edema with a para-papillary hemorrage nasal to the disc on the available colour fundus picture.
At presentation on March 4, Best Corrected Visual Acuity (BCVA) was reduced at 20/100 OR (20/25 OS). The patient described periods of acutely excruciating retro-orbital pain in the OR. Intraocular pressure was normal, at 12 OR and 18 OS (pachymetry was at 490 microns in both eyes). The dilated fundus examination was similar to the previous color picture and did not disclose peripheral hemorrages recalling extended peripheral retinal ischemia. Humphrey Visual Field disclosed an altitudinal inferior scotoma and a peripheral inferior scotoma OR and was in the normal range OS, i.e. did not recall normal tension glaucoma OS . There were no papillary drusen on the autofluorescence picture, ON volume was increased (11.77 mm3 OR versus 5.75 OS) on SD-OCT (Heidelberg Engineering®) OR, Retinal Nerve Fiber (RNFL) and RGC layers thicknesses were normal Marked epimacular hypereflectivity OR with foveolar depression inversion, moderately increased total volume and central foveolar thickness (CFT) (428 microns versus 328 OS), and a whitish aspect of the supero-temporal internal retinal layers recalling ischemic edema, were present . EDI CFT was incresead at 315 microns (versus 273 microns OS), with focal pachyvessels on the video mapping . OCT-Angiography disclosed focal perfusion defects in both the retinal and chorio-capillaris circulations , and central alterations of the PR1 layer on en-face OCT
Altogether the clinical picture evoked a NAION with venous sub-occlusion, recalling Fraenkel’s et al early hypothesis of an ET interstitial diffusion-related venous vasoconstriction behind the lamina cribrosa (2), as much as a rupture of the BRB was present in the optic nerve area (hemorrage along the optic disc). Choroidal vascular drop-out was suggested by the severity and rapidity of the VF impairment (31). The extremely rapid development of a significant “epiretinal membrane”, that we interpreted as a reactive - and protective, in absence of cystoid macular edema (CME) - ET 2-induced astrocytic proliferation (reviewed in 32), was as an additional sign of severe ischemia.
The mention of the retro-orbital pain evoking a “ciliary angor”, the absence of any inflammatory syndrome and of the usual metabolic syndrome in the emergency blood test, oriented the etiology towards a FS. And indeed anamnesis collected many features of the FS, i.e. hypotension (“non dipper” profile with one symptomatic nocturnal episode of hypotension on the MAPA), migrains, hypersensitivity to cold, stress, noise, smells, and medicines, history of a spontaneously resolutive hydrops six months earlier, and of paroxystic episods of vertigo (which had driven a prior negative brain RMI investigation for Multiple Sclerosis, a frequent record among FS patients (33) and of paroxystic visual field alterations (7)(9), that were actually recorded several times along the follow-up.
The diagnosis of FS was eventually confirmed in the Ophthalmology Department in Basel University on April 10th, with elevated retinal venous pressure (20 to 25mmHg versus 10-15 OS) (4)(7)(9), reduced perfusion in the central retinal artery and veins on ocular Doppler (respectively 8.3 cm/second OR velocity versus 14.1 mmHg OS, and 3.1/second OR versus 5.9 cm OS), and impaired vasodilation upon flicker light-dependant shear stress on the Dynamic Vessel Analyser testing (7-9). In addition atherosclerotic plaques were absent on carotid Doppler.
On March 4th, the patient was at length informed about the FS, a possible off label rhEPO IVI, and a related written informed consent on the ratio risk-benefits was delivered.
By March 7th, she returned on an emergency basis because of vision worsening OR. VA was unchanged, intraocular pressure was at 13, but Visual Field showed a worsening of the central and inferior scotomas with a decreased foveolar threshold, from 33 to 29 decibels. SD-OCT showed a 10% increase in the CFT volume.
On the very same day, an off label rhEPO IVI OR (EPREX® 2000 units, 0,05 cc in a pre-filled syringe) was performed in the operating theater, i.e. the dose reported by Modarres et al (27), and twenty times inferior to the usual weekly intravenous dose for treatment of chronic anemia secondary to CKD. Intra venous acetazolamide (500 milligrams) was performed prior to the injection, to prevent any increase in intra-ocular pressure. The patient was discharged with a prescription of chlorydrate betaxolol (Betoptic® 0.5 %) two drops a day, and high dose daily magnesium supplementation (600 mgr).
Incidentally the patient developed bradycardia the day after, after altogether instillation of 4 drops of betaxolol only, that was replaced by acetazolamide drops, i.e. a typical hypersensitivity reaction to medications in the FS (7)(9).
Subjective vision improvement was recorded as early as D1 after injection. By March 18 th, eleven days post rhEPO IVI, BCVA was improved at 20/63, the altitudinal scotoma had resolved (Fig. 5), Posterior Vitreous Detachment had developed with a disturbing marked Weiss ring, optic disc swelling had decreased; vasculogenesis within the retinal plexi and some regression of PR1 alterations were visible on OCT-en face. Indeed by 11 days post EPO significant functional, neuronal and vascular rescue were observed, while the natural evolution had been seriously vision threatening.
However cystoid ME (CME) had developed . Indo Cyanin Green-Cine Video Angiography (ICG-CVA) OR, performed on March 23, i.e. 16 days after the rhEPO IVI, showed a persistent drop in ocular perfusion: ciliary and central retinal artery perfusion timings were dramatically delayed at respectively 21 and 25 seconds, central retinal vein perfusion initiated by 35 seconds, was pulsatile, and completed by 50 seconds only (video 3). Choroidal pachyveins matching the ones on SD-OCT video mapping were present in the temporal superior and inferior fields, and crossed the macula; capillary exclusion territories were present in the macula and around the optic disc.
By April 1, 23 days after the rhEPO injection, VA was unchanged, but CME and perfusion voids in the superficial deep capillary plexi and choriocapillaris were worsened, and optic disc swelling had recurred back to baseline, in a context of repeated episodes of systemic hypotension; and actually Nifepidin-Ratiopharm® oral drops (34), that had been delivered via a Temporary Use Authorization from the central Pharmacology Department in Assistance Publique Hopitaux de Paris, had had to be stopped because of hypersensitivity.
A second off label rhEPO IVI was performed in the same conditions on April 3, i.e. approximately one month after the first one.
Evolution was favourable as early as the day after EPO injection 2: VA was improved at 20/40, CME was reduced, and perfusion improved in the superficial retinal plexus as well as in the choriocapillaris. By week 4 after EPO injection 2, CME was much decreased, i.e. without anti VEGF injection. On august 19th, by week 18 after EPO 2, perfusion on ICG-CVA was greatly improved , with ciliary timing at 18 seconds, central retinal artery at 20 seconds and venous return from 23 to 36 seconds, still pulsatile. Capillary exclusion territories were visible in the macula and temporal to the macula after the capillary flood time that went on by 20.5 until 22.5 seconds (video 4); they were no longer persistent at intermediate and late timings.
Last complete follow-up was recorded on January 7, 2021, at 22 months from EPO injection 2. BCVA was at 20/40, ON volume had dropped at 7.46 mm3, a sequaelar superior deficit was present in the RNFL with some corresponding residual defects on the inferior para central Visual Field , CFT was at 384 mm3 with an epimacular hyperreflectivity without ME, EDI CFT was dropped at 230 microns. Perfusion on ICG-CVA was not normalized, but even more improved, with ciliary timing at 15 seconds, central retinal artery at 16 seconds and venous return from 22 to 31 seconds, still pulsatile , indicating that VP was still above IOP. OCT-A showed persisting perfusion voids, especially at the optic disc and within the deep retinal capillary plexus. The latter were present at some degree in the OS as well . Choriocapillaris and PR1 layer were dramatically improved.
Last recorded BCVA was at 20/32 by February 14, 2022, at 34 months from EPO 2. SD-OCT showed stable gliosis hypertrophy and mild alterations of the external layers .
Discussion
What was striking in the initial clinical phenotype of CRVO was the contrast between the moderate venous dilation, and the intensity of ischemia, that were illustrating the pioneer hypothesis of Professor Flammer‘s team regarding the pivotal role of ET in VO (2), recently confirmed (3)(35), i.e. the local venous constriction backwards the lamina cribrosa, induced by diffusion of ET-1 within the vascular interstitium, in reaction to hypoxia. NAION was actually the primary and prevailing alteration, and ocular hypoperfusion was confirmed via ICG-CVA, as well as by the ocular Doppler performed in Basel. ICG-CVA confirmed the choroidal drop-out suggested by the severity of the VF impairment (31) and by OCT-A in the choriocapillaris. Venous pressure measurement, which instrumentation is now available (8), should become part of routine eye examination in case of RVO, as it is key to guide cases analysis and personalized therapeutical options.
Indeed, the endogenous EPO pathway is the dominant one activated by hypoxia and is synergetic with the VEGF pathway, and coherently it is expressed along to VEGF in the vitreous in human RVO (36). Diseases develop when the individual limiting stress threshold for efficient adaptative reactive capacity gets overwhelmed. In this case by Week 3 after symtoms onset, neuronal and vascular resilience mechanisms were no longer operative, but the BRB, compromised at the ON, was still maintained in the retina.
As mentioned in the introduction, the scientific rationale for the use of EPO was well demonstrated by that time, as well as the capacities of exogenous EPO to mimic endogenous EPO vasculogenesis, neurogenesis and synaptogenesis, restoration of the balance between ET-1 and NO. Improvement of chorioretinal blood flow was actually illustrated by the evolution of the choriocapillaris perfusion on repeated OCT-A and ICG-CVA. The anti-apoptotic effect of EPO (16) seems as much appropriate in case of RVO as the caspase-9 activation is possibly another overlooked co-factor (6).
All the conditions for translation into off label clinical use were present: severe vision loss with daily worsening and unlikely spontaneous favourable evolution, absence of toxicity in the human pilot studies, of contradictory comorbidities and co-medications, and of context of intraocular neovascularization that might be exacerbated by EPO (37).
Why didn’t we treat the onset of CME by March 18th, i.e. eleven days after EPO IVI 1, by anti-VEGF therapy, the “standard-of-care” in CME for RVO ?
In addition to the context of functional, neuronal and vascular improvements obviated by rhEPO IVI by that timing in the present case, actually anti VEGF therapy does not address the underlying causative pathology. Coherently, anti-VEGF IVI : 1) may not be efficient in improving vision in RVO, despite its efficiency in resolving/improving CME (usually requiring repeated injections), as shown in the Retain study (56% of eyes with resolved ME continued to loose vision)(quoted in (1) 2) eventually may be followed by serum ET-1 levels increase and VA reduction (in 25% of cases in a series of twenty eyes with BRVO) (38) and by increased areas of non perfusion in OCT-A (39). Rather did we perform a second hrEPO IVI, and actually we consider open the question whether the perfusion improvement, that was progressive, might have been accelerated/improved via repeated rhEPO IVI, on a three to four weeks basis.
The development of CME itself, involving a breakdown of the BRB, i.e. of part of the complex retinal armentorium resilience to hypoxia, was somewhat paradoxical in the context of improvement after the first EPO injection, as EPO restores the BRB (24), and as much as it was suggested that EPO inhibits glial osmotic swelling, one cause of ME, via VEGF induction (40). Possible explanations were: 1) the vascular hyperpermeability induced by the up-regulation of VEGF gene expression via EPO (41) 2) the ongoing causative disease, of chronic nature, that was obviated by the ICG-CVA and the Basel investigation, responsible for overwhelming the gliosis-dependant capacity of resilience to hypoxia 3) a combination of both. I/R seemed excluded: EPO precisely mimics hypoxic reconditioning as shown in over ten years publications, including in the retina (20), and as EPO therapy is part of the current strategy for stabilization of the endothelial glycocalix against I/R injury (42-43). An additional and not exclusive possible explanation was the potential antagonist action of EPO on GFAP astrocytes proliferation, as mentioned in the introduction (18), that might have counteracted the reactive protective hypertrophic gliosis, still fully operative prior to EPO injection, and that was eventually restored during the follow-up, where epiretinal hyperreflectivity without ME and ongoing chronic ischemia do coincide (Fig. 6 and video 6), as much as it is unlikely that EPO’s effect would exceed one month (cf infra). Inhibition of gliosis by EPO IVI might have been also part of the mechanism of rescue of RGG, compromised by gliosis in hypoxic conditions (44). Whatever the complex balance initially reached, then overwhelmed after EPO IVI 1, the challenge was rapidly overcome by the second EPO IVI without anti-VEGF injection, likely because the former was powerful enough to restore the threshold limit for resilience to hypoxia, that seemed no longer reached again during the relapse-free follow-up. Of note, this “epiretinal membrane “, which association to good vision is a proof of concept of its protective effect, must not be removed surgically, as it would suppress one of the mecanisms of resilience to hypoxia.
To our best knowledge, ICG-CVA was never reported in FS; it allows real time evaluation of the ocular perfusion and illustration of the universal rheological laws that control choroidal blood flow as well. Pachyveins recall a “reverse” veno-arteriolar reflex in the choroidal circulation, that is NO and autonomous nervous system-dependant, and that we suggested to be an adaptative choroidal microcirculation process to hypoxia (45). Their persistence during follow-up accounts for a persisting state of chronic ischemia.
The optimal timing for reperfusion via rhEPO in a non resolved issue:
in the case reported by Luscan and Roche, rhEPO IVI was performed on the very same day of disease onset, where it induced complete recovery from VA reduced at counting fingers at 1 meter, within 48 hours. This clinical human finding is on line with a recent rodent stroke study that established the timings for non lethal versus lethal ischemia of the neural and vascular lineages, and the optimized ones for beneficial reperfusion: the acute phase - from Day 1 where endothelial and neural cells are still preserved, to Day 7 where proliferation of pericytes and Progenitor Stem Cells are obtainable - and the chronic stage, up to Day 56, where vasculogenesis, neurogenesis and functional recovery are still possible, but with uncertain efficiency (46). In our particular case, PR rescue after rhEPO IVI 1 indicated that Week 3 was still timely. RhEPO IVI efficacy was shown to last between one (restoration of the BRB) and four weeks (antiapoptotic effect) in diabetic rats (24). The relapse after Week 3 post IVI 1 might indicate that it might be approximately the interval to be followed, should repeated injections be necessary.
The bilateral chronic perfusion defects on OCT-A at last follow-up indicate that both eyes remain in a condition of chronic ischemia and I/R, where endogenous EPO provides efficient ischemic pre-conditioning, but is potentially susceptible to be challenged during episodes of acute hypoxia that overwhelm the resilience threshold.
Conclusion
The present case advocates for individualized medicine with careful recording of the medical history, investigation of the systemic context, and exploiting of the available retinal multimodal imaging for accurate analytical interpretation of retinal diseases and their complex pathophysiology. The Flammer Syndrome is unfortunately overlooked in case of RVO; it should be suspected clinically in case of absence of the usual vascular and metabolic context, and in case of elevated RVP. RhEPO therapy is able to restore the beneficial endogenous EPO ischemic pre-conditioning in eyes submitted to challenging acute hypoxia episodes in addition to chronic ischemic stress, as in the Flammer Syndrome and fluctuating ocular blood flow, when it becomes compromised by the overwhelming of the hypoxic stress resilience threshold. The latter physiopathological explanation illuminates the cases of RVO where anti-VEGF therapy proved functionally inefficient, and/or worsened retinal ischemia. RhEPO therapy might be applied to other chronic ischemia and I/R conditions, as non neo-vascular Age Macular Degeneration (AMD), and actually EPO was listed in 2020 among the nineteen promising molecules in AMD in a pooling of four thousands (47).
#off-label therapy#JCRMHS#anti-VEGF therapy#Erythropoietin#Journal of Clinical Case Reports Medical Images and Health Sciences impact factor.#Primary Vascular Dysfunction
2 notes
·
View notes
Note
Nerd.
LE gasp! I have been discovered.... oh noessss /s
Unsure if this is /aff or /srs
(does this count as first annon hate??? if soo... what a milestone. *sniff sniff, wipes away tear*)
But for both..
YES PROUD NERD HEHEHEHEH
IN FACT
I hath been reseraching things about caspases... I"m SO CLOSE to finishing the article and it has ALLL THE ANSWERSSSS
I SHALL SEND ANNOTATIONS! BE PREPRARED DEAR ANNON!!!





ANYWHOSIES I sent your ask on a discord server because my companions are funnier than I.
this is what one of them said. I found it funny... hope you get a laugh out of it too! <3 <3
"Show your face you wimp. You scrub you runt you idiot with your anonymous name and profile with the sunglasses bcs you’re too scared to look us in our eyes, huh?
You think you’re so cool like a cold edgy bad boy calling people nerds. You know what you consist of?? What you run based off of?? Cells, caspaces. Next time you’re feeling sick and dying from a disease and you go to the doctor how about you call’em all nerds, yeah? I’m sure they’ll appreciate you so much they’ll give you a special vaccine called kiyoselinopresol, usually shortened to kys.
Didn’t even have the guts to come up with a real insult. “Nerd” yeah yeah very creative I’m shivering in my non-existent boots. What did you expect to get from something like that?? What purpose-less life do you have that drove you to call people enjoying hobbies insults—hobbies that are much more intellectual and meaningful than yours btw, being that yours in to call random people on the internet nerds?
I mean, I congratulate you. Congrats. You called a person on the internet a nerd. You offered no value to society as a whole. I hope you’re proud of yourself. Nerd"
I laughed so hard this is halarious.
ALSO ALSO:
Cassiah is my caspase-3 character and I'm wiritng an entire biology story. I am very much a nerd thank ye thank ye.
Literally this is all for funsies.
Anywho. So i'm still owndering if I should do have the activation for the biostory be through caspase-8 (extrinsic) or caspase-9 (intrinsic) or if I should have the reason for activation be apoptosis or a nonapoptotic need.
Perhapppsss I could have Cassiah attempt to fufill theri thrill seeking life-starved desires through assassining (as you do) and they know that this could lead toward the end of the world, they just want to leave such a mark, live in such a way that they aovid the forgotten death that they will cause.
THE THEMES I'M EXCITED FOR THIS ONE!!
tagging @bonesbeetle. I'm almost done! ANd I shall send my annotatiosn, sotry rambles and make some more thoughts sometime tomorrow or the day after!!
#lobotomy for my brainrot#noorie answers asks#answered asks#biology#science#science side of tumblr#dear annon#we are on the nerd website#i am one of you#heheheh
3 notes
·
View notes
Text
Caspase-8 Monoclonal Antibody
Caspase-8 Monoclonal Antibody Catalog number: B2019650 Lot number: Batch Dependent Expiration Date: Batch dependent Amount: 100 µg Molecular Weight or Concentration: NA Supplied as: Liquid Applications: a molecular tool for various biochemical applications Storage: -20°C Keywords: APG5-like Grade: Biotechnology grade. All products are highly pure. All solutions are made with Type I ultrapure…
0 notes
Text
Cine spune ca albastrul de metilen face minuni in leziunile cerebrale - STUDII
Citeste articolul pe https://consultatiiladomiciliu.ro/cine-spune-ca-albastrul-de-metilen-face-minuni-in-leziunile-cerebrale-studii/
Cine spune ca albastrul de metilen face minuni in leziunile cerebrale - STUDII

Albastrul de metilen utilizat in mod curent ca antiseptic urinar (face urina verde sau albastra), are un rol salvator pentru creier. Citeste mai mult despre mecanismele prin care salveaza neuronii.
Neurological Mechanisms of Action and Benefits of Methylene Blue © Chase Hughes, Applied Behavior Research 2023 16
mitochondria after traumatic brain injury and are protected by cyclosporine A. Journal of neurotrauma, 34(7), 1291-1301. Lee, S. W., & Han, H. C. (2021).
Methylene blue application to lessen pain: its analgesic effect and mechanism. Frontiers in Neuroscience, 15, 663650. Liu, Y., Jin, W., Zhao, Y., Zhang, G., & Zhang, W. (2017).
Enhanced catalytic degradation of methylene blue by α-Fe2O3/graphene oxide via heterogeneous photo-Fenton reactions. Applied Catalysis B: Environmental, 206, 642-652. Matsuda, M., Huh, Y., & Ji, R. R. (2019).
Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. Journal of anesthesia, 33, 131-139. Miclescu, A. A., Svahn, M., & Gordh, T. E. (2015).
Evaluation of the protein biomarkers and the analgesic response to systemic methylene blue in patients with refractory neuropathic pain: a double-blind, controlled study. Journal of pain research, 387-397. Nakazawa, H., Chang, K., Shinozaki, S., Yasukawa, T., Ishimaru, K., Yasuhara, S., … & Kaneki, M. (2017).
iNOS as a driver of inflammation and apoptosis in mouse skeletal muscle after burn injury: possible involvement of Sirt1 S-nitrosylation-mediated acetylation of p65 NF-κB and p53. PloS one, 12(1), e0170391. Ola, M. S., Nawaz, M., & Ahsan, H. (2011).
Role of Bcl-2 family proteins and caspases in the regulation of apoptosis. Molecular and cellular biochemistry, 351, 41-58. Pan, H., Zhao, X., Lei, S., Cai, C., Xie, Y. Z., & Yang, X. (2019).
The immunomodulatory activity of polysaccharides from the medicinal mushroom Amauroderma rude (Agaricomycetes) is mediated via the iNOS and PLA2-AA pathways. International Journal of Medicinal Mushrooms, 21(8).
Neurological Mechanisms of Action and Benefits of Methylene Blue © Chase Hughes, Applied Behavior Research 2023 17 Rojas, J. C., Bruchey, A. K., & Gonzalez-Lima, F. (2012).
Neurometabolic mechanisms for memory enhancement and neuroprotection of methylene blue. Progress in neurobiology, 96(1), 32-45. Shen, J., Xin, W., Li, Q., Gao, Y., Yuan, L., & Zhang, J. (2019). Methylene blue reduces neuronal apoptosis and improves blood-brain barrier integrity after traumatic brain injury. Frontiers in Neurology, 10, 1133. Talley Watts, L., Long, J. A., Chemello, J., Van Koughnet, S., Fernandez, A., Huang, S., … & Duong, T. Q. (2014).
Methylene blue is neuroprotective against mild traumatic brain injury. Journal of neurotrauma, 31(11), 1063- 1071. Tucker, D., Lu, Y., & Zhang, Q. (2018).
From mitochondrial function to neuroprotection—an emerging role for methylene blue. Molecular neurobiology, 55, 5137-5153. Wang, W. X., Sullivan, P. G., & Springer, J. E. (2017).
Mitochondria and microRNA crosstalk in traumatic brain injury. Progress in Neuro- Psychopharmacology and Biological Psychiatry, 73, 104-108. Yadav, S., & Surolia, A. (2019).
Lysozyme elicits pain during nerve injury by neuronal Toll-like receptor 4 activation and has therapeutic potential in neuropathic pain. Science translational medicine, 11(504), eaav4176. Yonutas, H. M., Vekaria, H. J., & Sullivan, P. G. (2016).
Mitochondrial specific therapeutic targets following brain injury. Brain research, 1640, 77- 93. Zhang, D. X., Ma, D. Y., Yao, Z. Q., Fu, C. Y., Shi, Y. X., Wang, Q. L., & Tang, Q. Q. (2016).
ERK1/2/p53 and NF-κB dependent-PUMA activation involves in doxorubicin-induced cardiomyocyte apoptosis. Eur Rev Med Pharmacol Sci, 20(11), 2435-2442. Zhao, M., Liang, F., Xu, H., Yan, W., & Zhang, J. (2016).
Methylene blue exerts a neuroprotective effect against traumatic brain injury by promoting Neurological Mechanisms of Action and Benefits of Methylene Blue © Chase Hughes, Applied Behavior Research 2023 18 autophagy and inhibiting microglial activation. Molecular medicine reports, 13(1), 13-20. Zhu, Y., Wang, H., Fang, J., Dai, W., Zhou, J., Wang, X., & Zhou, M. (2018). SS-31 provides neuroprotection by reversing mitochondrial dysfunction after traumatic brain injury.
Oxidative Medicine and Cellular Longevity, 2018. Zhou, Y., Shao, A., Xu, W., Wu, H., & Deng, Y. (2019). Advance of stem cell treatment for traumatic brain injury. Frontiers in cellular neuroscience, 13, 301.
#abdominala#acasa#Albastru de metilen#Albastrul de metilen#astrocite#astroglii#atac ischemic#avc#Bucuresti#cardiolog#cardiologie#consult#consultatie#Consultatii#doctor#doctor acasa#doctor la domiciliu#doctorul#domiciliu#ecocardiografie#ecografie#EKG#Ilfov#intai#Intreaba#medic#medic acasa#medic la domiciliu#medicala#medicul
0 notes
Text
“Caspase-8 Lymphadenopathy Syndrome“, Victor McKusick, Mendelian Inheritance in Man, 1966. 酪蛋白酶-8淋巴结病综合征。(CEDS).
Here I present: “Caspase-8 Lymphadenopathy Syndrome“, Victor McKusick, Mendelian Inheritance in Man’, 1966. 酪蛋白酶-8淋巴结病综合征。(CEDS). INTRODUCTION. Caspase –8 Lymphadenopathy Syndrome (CEDS) is a genetic disorder of the immune system. It is caused by mutations in the CASP8 gene that encodes the protein caspase-8. The disorder is characterized by splenomegaly and lymphadenopathy, in addition to…
0 notes
Text
Retinal and choroidal vascular drop out in a case of severe phenotype of Flammer Syndrome. Rescue of the ischemic-preconditioning mimicking action of endogenous Erythropoietin (EPO) by off-label intra vitreal injection of recombinant human EPO (rhEPO) by Claude Boscher in Journal of Clinical Case Reports Medical Images and Health Sciences

Journal of Clinical Case Reports Medical Images and Health Sciences
ABSTRACT
Background: Erythropoietin (EPO) is a pleiotropic anti-apoptotic, neurotrophic, anti-inflammatory, and pro-angiogenic endogenous agent, in addition to its effect on erythropoiesis. Exogenous EPO is currently used notably in human spinal cord trauma, and pilot studies in ocular diseases have been reported. Its action has been shown in all (neurons, glia, retinal pigment epithelium, and endothelial) retinal cells. Patients affected by the Flammer Syndrome (FS) (secondary to Endothelin (ET)-related endothelial dysfunction) are exposed to ischemic accidents in the microcirculation, notably the retina and optic nerve.
Case Presentation: A 54 years old female patient with a diagnosis of venous occlusion OR since three weeks presented on March 3, 2019. A severe Flammer phenotype and underlying non arteritic ischemic optic neuropathy; retinal and choroidal drop-out were obviated. Investigation and follow-up were performed for 36 months with Retinal Multimodal Imaging (Visual field, SD-OCT, OCT- Angiography, Indo Cyanin Green Cine-Video Angiography). Recombinant human EPO (rhEPO)(EPREX®)(2000 units, 0.05 cc) off-label intravitreal injection was performed twice at one month interval. Visual acuity rapidly improved from 20/200 to 20/63 with disparition of the initial altitudinal scotoma after the first rhEPO injection, to 20/40 after the second injection, and gradually up to 20/32, by month 5 to month 36. Secondary cystoid macular edema developed ten days after the first injection, that was not treated via anti-VEGF therapy, and resolved after the second rhEPO injection. PR1 layer integrity, as well as protective macular gliosis were fully restored. Some level of ischemia persisted in the deep capillary plexus and at the optic disc.
Conclusion: Patients with FS are submitted to chronic ischemia and paroxystic ischemia/reperfusion injury that drive survival physiological adaptations via the hypoxic-preconditioning mimicking effect of endogenous EPO, that becomes overwhelmed in case of acute hypoxic stress threshold above resilience limits. Intra vitreal exogenous rhEPO injection restores retinal hypoxic-preconditioning adaptation capacity, provided it is timely administrated. Intra vitreal rhEPO might be beneficial in other retinal diseases of ischemic and inflammatory nature.
Key words : Erythropoietin, retinal vein occlusion, anterior ischemic optic neuropathy, Flammer syndrome, Primary Vascular Dysfunction, anti-VEGF therapy, Endothelin, microcirculation, off-label therapy.
INTRODUCTION
Retinal Venous Occlusion (RVO) treatment still carries insufficiencies and contradictions (1) due to the incomplete deciphering of the pathophysiology and of its complex multifactorial nature, with overlooking of factors other than VEGF up-regulation, notably the roles of retinal venous tone and Endothelin-1 (ET) (2-5), and of endothelial caspase-9 activation (6). Flammer Syndrome (FS)( (Primary Vascular Dysfunction) is related to a non atherosclerotic ET-related endothelial dysfunction in a context of frequent hypotension and increased oxidative stress (OS), that alienates organs perfusion, with notably changeable functional altered regulation of blood flow (7-9), but the pathophysiology remains uncompletely elucidated (8). FS is more frequent in females, and does not seem to be expressed among outdoors workers, implying an influence of sex hormons and light (7)(9). ET is the most potent pro-proliferative, pro-fibrotic, pro-oxidative and pro-inflammatory vasoconstrictor, currently considered involved in many diseases other than cardio-vascular ones, and is notably an inducer of neuronal apoptosis (10). It is produced by endothelial (EC), smooth vascular muscles (SVMC) and kidney medullar cells, and binds the surface Receptors ET-A on SVMC and ET-B on EC, in an autocrine and paracrine fashion. Schematically, binding on SVMC Receptors (i.e. through local diffusion in fenestrated capillaries or dysfunctioning EC) and on EC ones (i.e. by circulating ET) induce respectively arterial and venous vasoconstriction, and vasodilation, the latter via Nitrite oxide (NO) synthesis. ET production is stimulated notably by Angiotensin 2, insulin, cortisol, hypoxia, and antagonized by endothelial gaseous NO, itself induced by flow shear stress. Schematically but not exclusively, vascular tone is maintained by a complex regulation of ET-NO balance (8) (10-11). Both decrease of NO and increase of ET production are both a cause and consequence of inflammation, OS and endothelial dysfunction, that accordingly favour vasoconstriction; in addition ET competes for L-arginine substrate with NO synthase, thereby reducing NO bioavailability, a mechanism obviated notably in carotid plaques and amaurosis fugax (reviewed in 11).
Severe FS phenotypes are rare. Within the eye, circulating ET reaches retinal VSMC in case of Blood-Retinal-Barrier (BRB) rupture and diffuses freely via the fenestrated choroidal circulation, notably around the optic nerve (ON) head behind the lamina cribrosa, and may induce all pathologies related to acute ocular blood flow decrease (2-3)(5)(7-9). We previously reported two severe cases with rapid onset of monocular cecity and low vision, of respectively RVO in altitude and non arteritic ischemic optic neuropathy (NAION) (Boscher et al, Société Francaise d'Ophtalmologie and Retina Society, 2015 annual meetings).
Exogenous Recombinant human EPO (rhEPO) has been shown effective in humans for spinal cord injury (12), neurodegenerative and chronic kidney diseases (CKD) (reviewed in 13). Endogenous EPO is released physiologically in the circulation by the kidney and liver; it may be secreted in addition by all cells in response to hypoxic stress, and it is the prevailing pathway induced via genes up-regulation by the transcription factor Hypoxia Inducible Factor 1 alpha, among angiogenesis (VEGF pathway), vasomotor regulation (inducible NO synthase), antioxidation, and energy metabolism (14). EPO Receptor signaling induces cell proliferation, survival and differentiation (reviewed in 13), and targets multiple non hematopoietic pathways as well as the long-known effect on erythropoiesis (reviewed in 15). Of particular interest here, are its synergistic anti-inflammatory, neural antiapoptotic (16) pro-survival and pro-regenerative (17) actions upon hypoxic injury, that were long-suggested to be also indirect, via blockade of ET release by astrocytes, and assimilated to ET-A blockers action (18). Quite interestingly, endogenous EPO’s pleiotropic effects were long-summarized (back to 2002), as “mimicking hypoxic-preconditioning” by Dawson (19), a concept applied to the retina (20). EPO Receptors are present in all retinal cells and their rescue activation targets all retinal cells, i.e. retinal EC, neurons (photoreceptors (PR), ganglion (RGG) and bipolar cells), retinal pigment epithelium (RPE) osmotic function through restoration of the BRB, and glial cells (reviewed in 21), and the optic nerve (reviewed in 22). RhEPO has been tested experimentally in animal models of glaucoma, retinal ischemia-reperfusion (I/R) and light phototoxicity, via multiple routes (systemic, subconjunctival, retrobulbar and intravitreal injection (IVI) (reviewed in 23), and used successfully via IVI in human pilot studies, notably first in diabetic macular edema (24) (reviewed in 25 and 26). It failed to improve neuroprotection in association to corticosteroids in optic neuritis, likely for bias reasons (reviewed in 22). Of specific relation to the current case, it has been reported in NAION (27) (reviewed in 28) and traumatic ON injury (29 Rashad), and in one case of acute severe central RVO (CRVO) (Luscan and Roche, Société Francaise d’Ophtalmologie 2017 annual meeting). In addition EPO RPE gene therapy was recently suggested to prevent retinal degeneration induced by OS in a rodent model of dry Age Macular Degeneration (AMD) (30).
CASE REPORT PRESENTATION
This 54 years female patient was first visited on March 2019 4th, seeking for second opinion for ongoing vision deterioration OR on a daily basis, since around 3 weeks. Sub-central RVO (CRVO) OR had been diagnosed on February 27th; available SD-OCT macular volume was increased with epiretinal marked hyperreflectivity, one available Fluorescein angiography picture showed a non-filled superior CRVO, and a vast central ischemia involving the macular and paraoptic territories. Of note there was ON edema with a para-papillary hemorrage nasal to the disc on the available colour fundus picture.
At presentation on March 4, Best Corrected Visual Acuity (BCVA) was reduced at 20/100 OR (20/25 OS). The patient described periods of acutely excruciating retro-orbital pain in the OR. Intraocular pressure was normal, at 12 OR and 18 OS (pachymetry was at 490 microns in both eyes). The dilated fundus examination was similar to the previous color picture and did not disclose peripheral hemorrages recalling extended peripheral retinal ischemia. Humphrey Visual Field disclosed an altitudinal inferior scotoma and a peripheral inferior scotoma OR and was in the normal range OS, i.e. did not recall normal tension glaucoma OS (Fig. 1). There were no papillary drusen on the autofluorescence picture, ON volume was increased (11.77 mm3 OR versus 5.75 OS) on SD-OCT (Heidelberg Engineering®) OR, Retinal Nerve Fiber (RNFL) and RGC layers thicknesses were normal (Fig. 2). Marked epimacular hypereflectivity OR with foveolar depression inversion, moderately increased total volume and central foveolar thickness (CFT) (428 microns versus 328 OS), and a whitish aspect of the supero-temporal internal retinal layers recalling ischemic edema, were present (video 1). EDI CFT was incresead at 315 microns (versus 273 microns OS), with focal pachyvessels on the video mapping (video 1). OCT-Angiography disclosed focal perfusion defects in both the retinal and chorio-capillaris circulations (Fig. 3), and central alterations of the PR1 layer on en-face OCT(Fig. 4).
Altogether the clinical picture evoked a NAION with venous sub-occlusion, recalling Fraenkel’s et al early hypothesis of an ET interstitial diffusion-related venous vasoconstriction behind the lamina cribrosa (2), as much as a rupture of the BRB was present in the optic nerve area (hemorrage along the optic disc). Choroidal vascular drop-out was suggested by the severity and rapidity of the VF impairment (31). The extremely rapid development of a significant “epiretinal membrane”, that we interpreted as a reactive - and protective, in absence of cystoid macular edema (CME) - ET 2-induced astrocytic proliferation (reviewed in 32), was as an additional sign of severe ischemia.
The mention of the retro-orbital pain evoking a “ciliary angor”, the absence of any inflammatory syndrome and of the usual metabolic syndrome in the emergency blood test, oriented the etiology towards a FS. And indeed anamnesis collected many features of the FS, i.e. hypotension (“non dipper” profile with one symptomatic nocturnal episode of hypotension on the MAPA), migrains, hypersensitivity to cold, stress, noise, smells, and medicines, history of a spontaneously resolutive hydrops six months earlier, and of paroxystic episods of vertigo (which had driven a prior negative brain RMI investigation for Multiple Sclerosis, a frequent record among FS patients (33) and of paroxystic visual field alterations (7)(9), that were actually recorded several times along the follow-up.
The diagnosis of FS was eventually confirmed in the Ophthalmology Department in Basel University on April 10th, with elevated retinal venous pressure (20 to 25mmHg versus 10-15 OS) (4)(7)(9), reduced perfusion in the central retinal artery and veins on ocular Doppler (respectively 8.3 cm/second OR velocity versus 14.1 mmHg OS, and 3.1/second OR versus 5.9 cm OS), and impaired vasodilation upon flicker light-dependant shear stress on the Dynamic Vessel Analyser testing (7-9). In addition atherosclerotic plaques were absent on carotid Doppler.
On March 4th, the patient was at length informed about the FS, a possible off label rhEPO IVI, and a related written informed consent on the ratio risk-benefits was delivered.
By March 7th, she returned on an emergency basis because of vision worsening OR. VA was unchanged, intraocular pressure was at 13, but Visual Field showed a worsening of the central and inferior scotomas with a decreased foveolar threshold, from 33 to 29 decibels. SD-OCT showed a 10% increase in the CFT volume.
On the very same day, an off label rhEPO IVI OR (EPREX® 2000 units, 0,05 cc in a pre-filled syringe) was performed in the operating theater, i.e. the dose reported by Modarres et al (27), and twenty times inferior to the usual weekly intravenous dose for treatment of chronic anemia secondary to CKD. Intra venous acetazolamide (500 milligrams) was performed prior to the injection, to prevent any increase in intra-ocular pressure. The patient was discharged with a prescription of chlorydrate betaxolol (Betoptic® 0.5 %) two drops a day, and high dose daily magnesium supplementation (600 mgr).
Incidentally the patient developed bradycardia the day after, after altogether instillation of 4 drops of betaxolol only, that was replaced by acetazolamide drops, i.e. a typical hypersensitivity reaction to medications in the FS (7)(9).
Subjective vision improvement was recorded as early as D1 after injection. By March 18 th, eleven days post rhEPO IVI, BCVA was improved at 20/63, the altitudinal scotoma had resolved (Fig. 5), Posterior Vitreous Detachment had developed with a disturbing marked Weiss ring, optic disc swelling had decreased; vasculogenesis within the retinal plexi and some regression of PR1 alterations were visible on OCT-en face. Indeed by 11 days post EPO significant functional, neuronal and vascular rescue were observed, while the natural evolution had been seriously vision threatening.
However cystoid ME (CME) had developed (video 2). Indo Cyanin Green-Cine Video Angiography (ICG-CVA) OR, performed on March 23, i.e. 16 days after the rhEPO IVI, showed a persistent drop in ocular perfusion: ciliary and central retinal artery perfusion timings were dramatically delayed at respectively 21 and 25 seconds, central retinal vein perfusion initiated by 35 seconds, was pulsatile, and completed by 50 seconds only (video 3). Choroidal pachyveins matching the ones on SD-OCT video mapping were present in the temporal superior and inferior fields, and crossed the macula; capillary exclusion territories were present in the macula and around the optic disc.
By April 1, 23 days after the rhEPO injection, VA was unchanged, but CME and perfusion voids in the superficial deep capillary plexi and choriocapillaris were worsened, and optic disc swelling had recurred back to baseline, in a context of repeated episodes of systemic hypotension; and actually Nifepidin-Ratiopharm® oral drops (34), that had been delivered via a Temporary Use Authorization from the central Pharmacology Department in Assistance Publique Hopitaux de Paris, had had to be stopped because of hypersensitivity.
A second off label rhEPO IVI was performed in the same conditions on April 3, i.e. approximately one month after the first one.
Evolution was favourable as early as the day after EPO injection 2: VA was improved at 20/40, CME was reduced, and perfusion improved in the superficial retinal plexus as well as in the choriocapillaris. By week 4 after EPO injection 2, CME was much decreased, i.e. without anti VEGF injection. On august 19th, by week 18 after EPO 2, perfusion on ICG-CVA was greatly improved , with ciliary timing at 18 seconds, central retinal artery at 20 seconds and venous return from 23 to 36 seconds, still pulsatile. Capillary exclusion territories were visible in the macula and temporal to the macula after the capillary flood time that went on by 20.5 until 22.5 seconds (video 4); they were no longer persistent at intermediate and late timings.
Last complete follow-up was recorded on January 7, 2021, at 22 months from EPO injection 2. BCVA was at 20/40, ON volume had dropped at 7.46 mm3, a sequaelar superior deficit was present in the RNFL (Fig. 2) with some corresponding residual defects on the inferior para central Visual Field (Fig. 5), CFT was at 384 mm3 with an epimacular hyperreflectivity without ME, EDI CFT was dropped at 230 microns. Perfusion on ICG-CVA was not normalized, but even more improved, with ciliary timing at 15 seconds, central retinal artery at 16 seconds and venous return from 22 to 31 seconds, still pulsatile (video 5), indicating that VP was still above IOP. OCT-A showed persisting perfusion voids, especially at the optic disc and within the deep retinal capillary plexus. The latter were present at some degree in the OS as well (Fig. 6). Choriocapillaris and PR1 layer were dramatically improved.
Last recorded BCVA was at 20/32 by February 14, 2022, at 34 months from EPO 2. SD-OCT showed stable gliosis hypertrophy and mild alterations of the external layers (video 6).
Figure 1: Humphrey visual field at baseline on March 7th 2019, showing an altitudinal central scotoma, an inferior peripheral scotoma with a normal and symmetrical foveolar sensitivity threshold, and a normal visual field OS
Figure 2: Retinal Nerve Fiber (RNFL ) evolution from normal at baseline on March 2019 7th, to development of a superior sequellar deficit that remained stable on last follow-up.
Figure 3: OCT-Angiography at baseline on March 7th 2019, showing perfusion voids OR in the superior superficial retinal plexus and in the choriocapillaris.
Figure 4: OCT en face at baseline on March 7th 2019, showing PR1 layer deficits OR (artefacts in the superior half) compared to OS.
Figure 5: Humphrey visual field follow-ups : at follow-up 1 eleven days after rhEPO intra vitreal injection showing resolution of the altitudinal central scotoma and decrease of the inferior scotoma, and at last visual field follow-up on January 20th 2021, showing residual defects corresponding to the RNFL ones on Figure 2.
Figure 6: OCT Angiography performed on January 7th 2021, at 22 months from EPO injection 2, showing persisting perfusion voids, especially at the optic disc, and within the deep retinal capillary plexus, that were present at some degree in the OS as well.
Video 1 : SD-OCT video mapping OR at baseline on March 7th 2019, showing epiretinal hyperreflectivity and epiretinal membrane with foveolar depression inversion, ischemic edema in the internal and temporal to the disc superior retinal layers, and focal choroidal Haller pachyvessels with reduction in chorio-capillaris/Sattler layers.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_1.mov
Video 2: SD-OCT video mapping OR at follow-up 1 eleven days after rhEPO intra vitreal injection on March 18th, showing epiretinal hyperreflectivity and epiretinal membrane with foveolar depression inversion, ischemic edema in the internal and temporal to the disc superior retinal layers, and development of central cystoid macular edema.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_2.mov
Video 3 : Indo Cyanin Green-Cine Video Angiography OR, performed on March 23, i.e. 16 days after the rhEPO IVI, showing a persistent drop in ocular perfusion: ciliary and central retinal artery perfusion timings were dramatically delayed at respectively 21 and 25 seconds, central retinal vein perfusion initiated by 35 seconds, was pulsatile, and completed by 50 seconds only.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_3.mov
Video 4 : Indo Cyanin Green-Cine Video Angiography OR, performed on August 19, i.e. by week 18 after EPO 2, showing greatly improved perfusion, with ciliary timing at 18 seconds, central retinal artery at 20 seconds and venous return from 23 to 36 seconds, still pulsatile. Capillary exclusion territories were visible in the macula and temporal to the macula after the capillary flood time that went on by 20.5 until 22.5 seconds.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_4.mov
Video 5: Indo Cyanin Green-Cine Video Angiography OR, performed on January 7th, 2021, at 22 months from EPO injection 2: perfusion was not normalized, but even more improved, with ciliary timing at 15 seconds, central retinal artery at 16 seconds and venous return from 22 to 31 seconds, still pulsatile.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_5.avi
Video 6 : SD-OCT video mapping at 34 months from EPO 2, showing stable gliosis hypertrophy and mild alterations of the external layers.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_6.avi
DISCUSSION
What was striking in the initial clinical phenotype of CRVO was the contrast between the moderate venous dilation, and the intensity of ischemia, that were illustrating the pioneer hypothesis of Professor Flammer‘s team regarding the pivotal role of ET in VO (2), recently confirmed (3)(35), i.e. the local venous constriction backwards the lamina cribrosa, induced by diffusion of ET-1 within the vascular interstitium, in reaction to hypoxia. NAION was actually the primary and prevailing alteration, and ocular hypoperfusion was confirmed via ICG-CVA, as well as by the ocular Doppler performed in Basel. ICG-CVA confirmed the choroidal drop-out suggested by the severity of the VF impairment (31) and by OCT-A in the choriocapillaris. Venous pressure measurement, which instrumentation is now available (8), should become part of routine eye examination in case of RVO, as it is key to guide cases analysis and personalized therapeutical options.
Indeed, the endogenous EPO pathway is the dominant one activated by hypoxia and is synergetic with the VEGF pathway, and coherently it is expressed along to VEGF in the vitreous in human RVO (36). Diseases develop when the individual limiting stress threshold for efficient adaptative reactive capacity gets overwhelmed. In this case by Week 3 after symtoms onset, neuronal and vascular resilience mechanisms were no longer operative, but the BRB, compromised at the ON, was still maintained in the retina.
As mentioned in the introduction, the scientific rationale for the use of EPO was well demonstrated by that time, as well as the capacities of exogenous EPO to mimic endogenous EPO vasculogenesis, neurogenesis and synaptogenesis, restoration of the balance between ET-1 and NO. Improvement of chorioretinal blood flow was actually illustrated by the evolution of the choriocapillaris perfusion on repeated OCT-A and ICG-CVA. The anti-apoptotic effect of EPO (16) seems as much appropriate in case of RVO as the caspase-9 activation is possibly another overlooked co-factor (6).
All the conditions for translation into off label clinical use were present: severe vision loss with daily worsening and unlikely spontaneous favourable evolution, absence of toxicity in the human pilot studies, of contradictory comorbidities and co-medications, and of context of intraocular neovascularization that might be exacerbated by EPO (37).
Why didn’t we treat the onset of CME by March 18th, i.e. eleven days after EPO IVI 1, by anti-VEGF therapy, the “standard-of-care” in CME for RVO ?
In addition to the context of functional, neuronal and vascular improvements obviated by rhEPO IVI by that timing in the present case, actually anti VEGF therapy does not address the underlying causative pathology. Coherently, anti-VEGF IVI : 1) may not be efficient in improving vision in RVO, despite its efficiency in resolving/improving CME (usually requiring repeated injections), as shown in the Retain study (56% of eyes with resolved ME continued to loose vision)(quoted in (1) 2) eventually may be followed by serum ET-1 levels increase and VA reduction (in 25% of cases in a series of twenty eyes with BRVO) (38) and by increased areas of non perfusion in OCT-A (39). Rather did we perform a second hrEPO IVI, and actually we consider open the question whether the perfusion improvement, that was progressive, might have been accelerated/improved via repeated rhEPO IVI, on a three to four weeks basis.
The development of CME itself, involving a breakdown of the BRB, i.e. of part of the complex retinal armentorium resilience to hypoxia, was somewhat paradoxical in the context of improvement after the first EPO injection, as EPO restores the BRB (24), and as much as it was suggested that EPO inhibits glial osmotic swelling, one cause of ME, via VEGF induction (40). Possible explanations were: 1) the vascular hyperpermeability induced by the up-regulation of VEGF gene expression via EPO (41) 2) the ongoing causative disease, of chronic nature, that was obviated by the ICG-CVA and the Basel investigation, responsible for overwhelming the gliosis-dependant capacity of resilience to hypoxia 3) a combination of both. I/R seemed excluded: EPO precisely mimics hypoxic reconditioning as shown in over ten years publications, including in the retina (20), and as EPO therapy is part of the current strategy for stabilization of the endothelial glycocalix against I/R injury (42-43). An additional and not exclusive possible explanation was the potential antagonist action of EPO on GFAP astrocytes proliferation, as mentioned in the introduction (18), that might have counteracted the reactive protective hypertrophic gliosis, still fully operative prior to EPO injection, and that was eventually restored during the follow-up, where epiretinal hyperreflectivity without ME and ongoing chronic ischemia do coincide (Fig. 6 and video 6), as much as it is unlikely that EPO’s effect would exceed one month (cf infra). Inhibition of gliosis by EPO IVI might have been also part of the mechanism of rescue of RGG, compromised by gliosis in hypoxic conditions (44). Whatever the complex balance initially reached, then overwhelmed after EPO IVI 1, the challenge was rapidly overcome by the second EPO IVI without anti-VEGF injection, likely because the former was powerful enough to restore the threshold limit for resilience to hypoxia, that seemed no longer reached again during the relapse-free follow-up. Of note, this “epiretinal membrane “, which association to good vision is a proof of concept of its protective effect, must not be removed surgically, as it would suppress one of the mecanisms of resilience to hypoxia.
To our best knowledge, ICG-CVA was never reported in FS; it allows real time evaluation of the ocular perfusion and illustration of the universal rheological laws that control choroidal blood flow as well. Pachyveins recall a “reverse” veno-arteriolar reflex in the choroidal circulation, that is NO and autonomous nervous system-dependant, and that we suggested to be an adaptative choroidal microcirculation process to hypoxia (45). Their persistence during follow-up accounts for a persisting state of chronic ischemia.
The optimal timing for reperfusion via rhEPO in a non resolved issue:
in the case reported by Luscan and Roche, rhEPO IVI was performed on the very same day of disease onset, where it induced complete recovery from VA reduced at counting fingers at 1 meter, within 48 hours. This clinical human finding is on line with a recent rodent stroke study that established the timings for non lethal versus lethal ischemia of the neural and vascular lineages, and the optimized ones for beneficial reperfusion: the acute phase - from Day 1 where endothelial and neural cells are still preserved, to Day 7 where proliferation of pericytes and Progenitor Stem Cells are obtainable - and the chronic stage, up to Day 56, where vasculogenesis, neurogenesis and functional recovery are still possible, but with uncertain efficiency (46). In our particular case, PR rescue after rhEPO IVI 1 indicated that Week 3 was still timely. RhEPO IVI efficacy was shown to last between one (restoration of the BRB) and four weeks (antiapoptotic effect) in diabetic rats (24). The relapse after Week 3 post IVI 1 might indicate that it might be approximately the interval to be followed, should repeated injections be necessary.
The bilateral chronic perfusion defects on OCT-A at last follow-up indicate that both eyes remain in a condition of chronic ischemia and I/R, where endogenous EPO provides efficient ischemic pre-conditioning, but is potentially susceptible to be challenged during episodes of acute hypoxia that overwhelm the resilience threshold.
CONCLUSION
The present case advocates for individualized medicine with careful recording of the medical history, investigation of the systemic context, and exploiting of the available retinal multimodal imaging for accurate analytical interpretation of retinal diseases and their complex pathophysiology. The Flammer Syndrome is unfortunately overlooked in case of RVO; it should be suspected clinically in case of absence of the usual vascular and metabolic context, and in case of elevated RVP. RhEPO therapy is able to restore the beneficial endogenous EPO ischemic pre-conditioning in eyes submitted to challenging acute hypoxia episodes in addition to chronic ischemic stress, as in the Flammer Syndrome and fluctuating ocular blood flow, when it becomes compromised by the overwhelming of the hypoxic stress resilience threshold. The latter physiopathological explanation illuminates the cases of RVO where anti-VEGF therapy proved functionally inefficient, and/or worsened retinal ischemia. RhEPO therapy might be applied to other chronic ischemia and I/R conditions, as non neo-vascular Age Macular Degeneration (AMD), and actually EPO was listed in 2020 among the nineteen promising molecules in AMD in a pooling of four thousands (47).
For more information regarding our Journal: https://jmedcasereportsimages.org/about-us/
For more artices: https://jmedcasereportsimages.org/archive/
0 notes
Text
Silymarin – Chiết xuất Cây Kế Sữa | Cao khô Kế Sữa (Milk Thistle extract) là hoạt chất chính được chiết xuất từ cây kế sữa, hay còn được gọi là cây cúc gai đã được chứng minh lâm sàn là hoạt chất có tác dụng cho gan tôm tốt nhất trong số tất cả những hoạt chất có chức năng tương tự.
1. Silymarin – Chiết xuất cây kế sữa | Cao khô kế sữa (cây cúc gai) là gì?
Silymarin được chiết xuất từ Cây Kế sữa (Milk Thistle) (dân gian còn gọi là cây cúc gai) hay còn được biết đến với tên khoa học là Silybum Marianum (L.) Gaertn). Cây kế sữa là một loại cây có nguồn gốc từ châu Âu và được thực dân đầu tiên đưa đến Bắc Mỹ. Cây kế sữa hiện được tìm thấy trên khắp miền đông Hoa Kỳ, California, Nam Mỹ, Châu Phi, Úc và Châu Á.
Cây kế sữa được đặt tên dựa trên nhựa của cây như sữa chảy ra từ lá khi chúng bị bẻ gãy. Tất cả các bộ phận lộ trên mặt đất và hạt giống đều được sử dụng để làm thuốc. Silymarin là thành phần hoạt chất chính trong cây kế sữa, đây là chất vừa chống viêm, chống oxy hóa và có tác dụng hạ đường huyết. Hạt giống cây kế sữa có thể bảo vệ các tế bào gan khỏi các hóa chất và thuốc độc hại.
Hợp chất này đã được chứng minh lâm sàng và được công nhận là có hiệu quả vượt trội dành riêng cho gan, là hoạt chất có tác dụng cho gan tốt nhất trong số tất cả những hoạt chất có chức năng tương tự.
Silymarin nguyên liệu có dạng bột có màu nâu và được sử dụng như là một chất bổ sung vào trong rất nhiều các loại thực phẩm, đồ ăn và thức uống khác nhau. Các nhà nghiên cứu khuyến cáo nên sử dụng hợp chất này với liều lượng khoảng 80mg/ngày.
2. Phân biệt Silymarin thường và Silymarin Phytosome®
Silymarin là một Flavonoid (chất chuyển hóa trung gian của thực vật), là một nhóm các thành phần được chiết xuất từ cây kế sữa (cây cúc gai). Trong số các thành phần đó, Silybin là hoạt chất chính, đã được chứng minh lâm sàn là có tác dụng vượt trội dành cho gan, và là hoạt chất có tác dụng cho gan tốt nhất trong số tất cả những hoạt chất có chức năng tương tự. Hiện nay, Silymarin ngoài thị trường sẽ có hai loại chính:
Silymarin thông thường là Silymarin có chứa Silybin được chiết xuất bằng phương pháp thông thường, đây là các Silybin tự do. Ưu điểm của loại Silymarin thông thường này là chúng có giá thành tương đối rẻ, thường được sử dụng để làm nguyên liệu cho sản xuất Thuốc Thủy Sản, Thuốc Thú Y hoặc dùng để phối trộn với Thức Ăn Chăn Nuôi (Thức ăn thủy sản, Thức ăn chăn nuôi gia súc, gia cầm).
Silymarin Phytosome® là Silymarin có chứa Silybin được chiết xuất bằng công nghệ Phytosome, đây còn được gọi là Silybin Phytosome. Công nghệ Phytosomes® là công nghệ dùng để chiết xuất các loại thảo dược, làm cao dược liệu tiên tiến nhất hiện nay.
Công nghệ Phytosome giúp các phân tử Silybin liên kết chặt chẽ với màng photpholipid của đậu nành và giúp cải thiện hoạt tính của Silybin lên mức tối ưu nhất. Chính vì thế, Silymarin Phytosome (hay còn được gọi là Silybin Phytosome) có giá thành tương đối cao, được sử dụng chủ yếu để làm nguyên liệu sản xuất dược như là nguyên liệu Thuốc và Thực phẩm chức năng.
3. Tác dụng của Silymarin trong việc bảo vệ và ph��c hồi chức năng gan
Silymarin đã được chứng minh hiệu quả của nó qua nhiều nghiên cứu lâm sàng khác nhau. Ngoài ra, Indena cũng đã tiến hành nhiều nghiên cứu để kiểm tra dược tính và độc tính của nó để đảm bảo sự hiệu quả và an toàn khi sử dụng.
Liều dùng của Silybin Tế bàoTác dụng của SilybinTừ 5 đến 50 µmol/LTế bào ganỨc chế tín hiệu do trung gian NF-κBTừ 10 đến 100 μmol/LTế bào ganGiảm sự hình thành các chất chứa từ ty thể, tạo phức chelat với kim loạiHepG2Giảm sự hình thành các anion oxy hóaTrung bình: 15 µmol/LTế bào biểu môỨc chế phosphoryl hóa IκBαTiểu cầuỨc chế protein kinaseTế bào ung thưỨc chế c-jun N-terminal kinaseĐại thực bàoỨc chế hình thành leukotrieneTế bào hình saoỨc chế giải phóng cytochrome cHepG2Ức chế phosphoryl hóa ERK, MEK, Raf; ức chế giải phóng caspase 9 và 3, IL-8; ức chế tín hiệu do trung gian PDGF và TGF-beta; giảm MMP2; tăng TIMP2; ức chế sự nhân lên của HCVLiều trung bình có tác dụng được ghi lại: 20 μmol/LTế bào KupfferGiảm sự sản xuất NOTế bào bạch cầu monoDọn các gốc tự do lipodienyl, methyl, trichloromethylTế bào biểu môGiảm nồng độ các hydrogen peroxideTế bào ung thưỨc chế quá trình peroxide hóa lipid màng tế bào
4. Ứng dụng của Silymarin trong việc phục hồi và bảo vệ gan tôm
Hiện nay, chưa có một nghiên cứu hay báo cáo cụ thể nào (kể cả trong nước và ngoài nước) trong việc ứng dụng Silymarin để phục hồi và bảo vệ gan tôm. Tuy nhiên, dựa trên các nghiên cứu về tác dụng phục hồi và bảo vệ gan của Silybin (hoạt chất chính trong Silymarin) lên gan chuột đã bị tổn thương, chúng ta có thể suy ra, Silymarin cũng có tác dụng tương tự đối với gan tôm nói riêng và gan của các loài thủy sản nói chung.
Silymarin đã được nghiên cứu lâm sàng và ứng dụng để phục hồi và bảo vệ gan cho người. Chính vì thế, hoạt chất này rất an toàn khi sử dụng cho thủy sản, đặc biệt là trong việc phục hồi và bảo vệ gan tôm. Một số công dụng chính khi dùng Silymarin cho gan tôm như sau:
Tăng cường hệ miễn dịch cho tôm, tăng cường chức năng gan tôm.
Phòng bệnh và điều trị các bệnh về gan trên tôm như sưng gan, teo gan, vàng gan, hoại tử gan tụy, nhiễm độc tố gan, …
Chữa bệnh sưng gan, phù nề gan thận, nhiễm độc tố gan.
Chống hoại tử gan tụy, giúp lọc máu, chống co thắt đường ruột tôm.
Chống rụng râu, mòn đuôi, đề kháng mạnh khi môi trường có sự biến động đột ngột.
Giảm tình trạng tôm chết đột ngột không rõ nguyên nhân.
Bên cạnh đó, hiện tại chưa có nghiên cứu khoa học nào cho thấy liều lượng cụ thể khi dùng silymarin để trộn cho tôm ăn. Nhưng theo thử nghiệm thực tế của Công Ty Thiên Tuế, liều lượng silymarin khi trộn cho tôm ăn có thể tham khảo như sau:
Tôm dưới 15 ngày: 3 gam cho 1 kg thức ăn.
Tôm từ 15 ngày đến 30 ngày: 6 gam cho 1 kg thức ăn.
Tôm từ 30 ngày đến 45 ngày: 10 gam cho 1 kg thức ăn.
Tôm trên 45 ngày: 15 gam cho 1 kg thức ăn.
Silymarin là một hoạt chất rất mạnh dành cho việc phục hồi và để bảo vệ gan tôm, chính vì thế, silymarin cho gan tôm thường được khuyến cáo là nên dùng định kì, xuyên suốt từ lúc mới thả đến hết vụ. Trong trường hợp tôm bị các bệnh gan, khả năng ăn thức ăn kém, người nuôi có thể hòa tan silymarin với nước rồi tạt thẳng xuống ao để đảm bảo tôm có thể hấp thụ silymarin một cách tốt nhất.
Chính vì những lợi ích cực kì đặc biệt dành cho gan như vậy mà silymarin dần trở thành một trong những hoạt chất cực kì quan trọng dùng trong nuôi tôm nói riêng và trong nuôi trồng thủy sản nói chung. Silymarin hiện tại đang được thương mại ở hai dạng chính:
Một là silymarin nguyên liệu, có nguồn gốc xuất sứ ở Việt Nam, Trung Quốc hoặc các nước Châu Âu như Đức, Ý.
Hai là thuốc thủy sản có chứa Silymarin. Đây là dạng silymarin đã được phối trộn, kết hợp với các thành phần khác để tạo thành dạng thành phẩm, ngoài chức năng phục hồi và bảo vệ gan tôm, các loại thuốc thủy sản có chứa silymarin như thế này thường sẽ đi kèm thêm nhiều công dụng khác dành cho tôm
--------- Follow page Thientue Pharma JSC - Bộ phận THỦY SẢN để đón đọc thêm nhiều thông tin hữu ích về ngành nuôi tôm. Follow page Thientue Pharma JSC - Nguyên liệu dược liệu để ��ón đọc thêm nhiều thông tin hữu ích về sức khỏe con người. #ThientuePharmaJSC #duocphamthientue #congtythientue#aquaculture #thuysan #livestock #channuoi #tpcn #functionalfoods#silymarin #chietxuatkesua #caykesua #caycucgai #sylibin #phytosome --------- Thientue Pharma JSC - Hợp Tác Chân Thành Công Ty Cổ Phần Dược Phẩm Thiên Tuế (Thientue Pharma JSC) chuyên sản xuất và phân phối các loại Cao dược liệu, Chiết xuất thảo dược, Chế phẩm sinh học (men vi sinh, nguyên liệu sinh học) và các hoạt chất nhập khẩu chuyên dụng dành cho thủy sản. VPĐD: 56/30 Tân Thới Nhất 17, KP4, P. TNT, Q. 12, Tp. HCM 71510S ĐT: 028.6267.707
0 notes
Text
https://twikkers.nl/blogs/174365/Caspase-8-Market-Overview-Competitive-Analysis-and-Forecast-2031

Caspase 8 Market Overview, Competitive Analysis and Forecast 2031
0 notes
Text
0 notes
Text
AMPKα1 Rabbit Monoclonal Antibody
AMPKŒ±1 Rabbit Monoclonal Antibody Catalog number: B2019637 Lot number: Batch Dependent Expiration Date: Batch dependent Amount: 100 µg Molecular Weight or Concentration: NA Supplied as: Liquid Applications: a molecular tool for various biochemical applications Storage: -20°C Keywords: Caspase-8 Monoclonal Antibody Grade: Biotechnology grade. All products are highly pure. All solutions are made…
0 notes
Text
lupine publishers|Circ_0001529 Expression Abnormalities Mediate the miR-578 CDC25A Axis Involved in the Growth of Ovarian Cancer
Circ_0001529 Expression Abnormalities Mediate the miR-578 CDC25A Axis Involved in the Growth of Ovarian Cancer

Abstract Purpose: To investigate the effect of Circ_0001529-mediated miR-578-CDC25A axis on the growth of ovarian cancer cells in vitro and in vivo. Method: The expression differences of Circ_0001529 in ovarian cancer tissues and paraneoplastic tissues were first analyzed; Circ_0001529 overexpression plasmids and interference plasmids were constructed and transfected into SKOV3 cells and SiHa cells, respectively, followed by MTT assay, flow cytometry, and immunofluorescence to detect cell growth, proliferation, and apoptosis. The binding relationship between Circ_0001529 and miR-578, or miR-578 and CDC25A was verified by online prediction site and dual luciferase assay, and CDC25A overexpression plasmid and interference plasmid were constructed and transfected into SKOV3 cells and SiHa cells, respectively. qRT-PCR and Western Blot were used to to detect the expression of ACP5, followed by cell growth as well as apoptosis. A mouse xenograft tumor model was constructed, and the growth of ovarian cancer cells in vivo was assessed by calculating tumor volume growth with KI67 and Caspase-3 immunohistochemistry. Result: Circ_0001529 was highly expressed in ovarian cancer tissues and cells; silencing Circ_0001529 inhibited ovarian cancer cell growth and promoted apoptosis in vitro and in vivo. circ_0001529 could bind to miR-578 target, and miR-578 bound to CDC25A mRNA target. Overexpression of Circ_0001529 promotes the expression of CDC25A and promotes the growth and inhibits the apop- tosis of ovarian cancer cells. CDC25A can upregulate the ERK/MAPK signaling pathway, thus promoting ovarian carcinogenesis. Conclusion: circRNA_0001529 promotes CDC25A expression through targeted binding of miR-578, thereby promoting the growth and metastasis of ovarian cancer cells. Key words: ACP5; Circ_0001529; Lung Carcinoma; Kalpan-Meier Analysis; Proliferation; Apoptosis; Erk/Mapk Signaling Pathway
Introduction Ovarian cancer (OC) is one of the deadliest gynecological cancers, with a significant fatality rate. It has a poor prognosis due to late diagnosis and medication resistance [1]. In the treatment of ovarian cancer, it is critical to distinguish between patients who will benefit from primary full cytoreductive surgery and those who will benefit more from neoadjuvant chemotherapy [2]. TK1 could be used as a biomarker to diagnose ovarian cancer. When it comes to differentiating malignant ovarian tumors from benign ones, ROMI outperforms ROMA [3]. The use of cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) has been demonstrated to be effective in a variety of cancers, and it may also provide a prognosis benefit for patients with advanced ovarian cancer [4]. The intracellular signal transducer and regulator of gene expression and protein turnover, Focal adhesion Kinase (FAK), increases tumor progression and is a promising therapeutic target for a variety of cancers, including ovarian cancer. [5] There have been some results suggesting that ERRα may promote ovarian cancer progression and may serve as a promising predictive biomarker [6]. Ovarian Cancer (OC) is a type of gynecological cancer with high mortality rate, and Circ_000152. (PM9 plays an important role in it. However, the clinical significance of circular RNA and its molecular mechanism in OC are mostly unknown. Circ_0001529 (hsa_circAFF4_016), is a circular RNA formed by reverse shearing of AFF4, is a circular RNA newly discovered by us [7] Circular RNAs (circRNAs) are increasingly recognized as important regulators in cancer including ovarian cancer (OC). This work focuses on the effects of circ_0000745 on the OC development of and molecules involved [8]. Imaging intracellular microRNAs (miRNAs) demonstrated an essential role in exposing their biological and pathological functions [9]. The induction of microribonucleic acid (miRNA) in cells is of great significance for early disease diagnosis and treatment monitoring. DNA is an interesting building material that can be programmed into components with rigid and branched structures and is particularly suitable for intracellular biomolecular imaging or therapeutic drug delivery [10]. Moreover, it has been shown that targeting the hsa_circ_0005785/miR-578/ APRIL regulatory pathway may be a promising diagnostic and therapeutic strategy in the clinical practice of HCC [11]. Similarly, for the ovarian cancer we studied, we combined Circ_0001529 with miR-578 targeting to see if it could promote cancer cell changes and metastasis functionally. Given the importance of silencing Circ_0001529 in ovarian cancer treatment, we aimed to identify an excellent inhibitor and investigate its potential therapeutic effects, thereby knocking down the role of Circ_0001529 expression to promote ovarian cancer cell growth and inhibit its apoptosis. Circular RNA (circRNA) is recently found to participate in the regulation of tumor progression, including ovarian cancer. Methods Tissue samples Eighty patients with ovarian cancer diagnosed and treated in our hospital from September 2012 to June 2013 were selected from surgically resected cancerous tissue and normal paracancerous tissue (at least 2 cm away from the ovarian cancerous tissue), with a median age of 49-79 years and a mean age of (64.9 ± 7.3) years. And all patients were followed up every three months for five years. Inclusion criteria: 1, all patients were diagnosed with ovarian cancer by postoperative pathological examination; 2, all patients did not receive radiotherapy or chemotherapy before surgery; 3, clinical data were complete. Exclusion criteria: 1, combined with chronic systemic diseases; 2, combined with other malignant tumors. The study was approved by our ethics committee and supervised by our ethics committee, and the subjects all signed the informed consent form while enjoying the right to information. Cell Culture Human ovarian cancer cell lines Hela, SKOV3, SiHa, SPC-A-1, L9981 and human normal ovarian epithelial cells
HOSE-1 were purchased from the Tumor Cell Bank of China Medical College (Beijing, China), and subsequently inoculated into cell culture dishes at a density of 1×10 5 cells/cm2 using RPMI-1640 medium containing 10% fetal bovine serum, CM7-1 medium, F12K medium and LHC-9 medium (all purchased from Gibco, Grand Island, NY,USA), and cultured at 37°C , 5% CO2 for 48 h until cell growth was fused to 80%-90%, digested with 0.025% trypsin (Gibco), and passaged. qRT-PCR Total RNA of tumor tissues and cells was used using RNAiso Plus (TAKARA, Otsu, Shiga, Japan) and Trizol LS Reagent (TAKARA, Otsu, Shiga, Japan), respectively. The reliability of the obtained RNA was subsequently verified using formaldehyde denaturation electrophoresis assay to continue the subsequent experiments. Reverse transcription polymerase chain reaction (RT-PCR) experiments were then performed using the PrimeScript TMRT kit (TAKARA, Otsu, Shiga, Japan) strictly according to the instructions. The mRNA expression levels were quantified by standard real-time quantitative PCR methods using SYBR Premix Ex Taq (TAKARA, Otsu, Shiga, Japan). gAPDH was used as a reference gene. The primers for each group are shown in Table 1.
for more information about Interventions in Gynaecology and Women’s Healthcare archive page click on below link
https://lupinepublishers.com/gynecology-women-health-journal/archive.php
for more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
#lupine publishers group#Interventions in Gynaecology and Women’s Healthcare#The reliability of the obtained
5 notes
·
View notes
Text
Going through questions:
After transcription, pre-mRNA (hnRNA, which contains introns and exons) is edited. To become mature mRNA (exons only), pre-mRNA needs to get a 5' methylguanosine cap, have introns removed, have exons spliced together, and get a 3' polyadenine tail. Splicing = removal of introns (non-coding segments). Splicing is done by spliceosomes. Spliceosomes are made of small nuclear ribonucleoproteins (snRNPs). Introns with GU at the 5' splice site and AG at the 3' splice site are removed by spliceosomes. Post-transcriptional modicfication of pre-mRNA: 5' guanosine cap-> 5' cap methylation-> poly A added at 3' end-> introns removed by spliceosomes.
Alternative splicing is when exons of pre-mRNA are spliced together in different ways, which allows for different proteins to be made. E.g., you start off with pre-mRNA containing exon 1, exon 2, exon 3, and exon 4. Alternative splicing allows you to remove and include whichever exons you want in order to make different mRNA strands. So from the pre-mRNA, you could make mRNA that looks like: exon 1--exon 2--exon 3--exon 4 or mRNA that looks like: exon 1--exon 2--exon 4 (removed exon 3). Alternative splicing is basically removing some exons so that you can make different proteins from the same gene.
Some cancer cells can use alternative splicing to avoid detection by the immune system. FasR is a receptor on cells that binds to FasL on cytotoxic T cells. The FasR-FasL interaction leads to programmed cell death (apoptosis). Cancer cells can do alternative splicing to remove the exon that makes the transmembrane part of the FasR, therefore FasR won't be in the cell membrane. If that happens, the cell can avoid apoptosis.
Lol. The Fas receptor (FasR) has "death domains" on the intracellular part of it. When the Fas ligand (FasL) binds to FasR, the death domains cause activation of caspases, which lead to executioner caspases that cause apoptosis. It sounds macabre and funny. I did a question the other day about caspases. They're involved in apoptosis.
Cystathionine synthase deficiency causes homocystinuria; it's autosomal recessive. Pts present with lens dislocation, intellectual disability, marfanoid body habitus (long arms/legs/fingers), and thromboembolism (because homocysteine causes hypercoagulability). Tx: avoid methionine in the diet, supplement cysteine and vitamin B6.
Aminoacyl tRNA sythetase loads the correct amino acid to the terminal 3' OH on the CCA tail of tRNA.
Restriction Fragment Length Polymorphism = RFLP.
Ok, see I was confused about meiosis and the way he talked about in in OnlineMedEd just made me more confused. But this question I just answered makes sense to me. Homologous chromosomes are separated in meiosis I; sister chromatids are separated in meiosis II. Nondisjunction is failure of either homologous chromosomes to separate in meiosis I or failure of sister chromatids to separate in meiosis II. Trisomy = having an extra chromosome; monosomy = losing a chromosome. Nondisjunction-> monosomies and trisomies. In this question, the parents were normal, so they each had 2 bands on RFLP analysis. Their son had trisomy 21, so he had 3 bands on RFLP analysis because he had an extra chromosome 21. I really didn't understand this RFLP analysis, but I got the question right because I remembered from OnlineMedEd that maternal nondisjunction in meiosis I often causes Down syndrome. Anyway, the RFLP analysis showed that the kid had 2 bands from mom and one band from dad, so he got the extra chromosome from his mom. The kid got two different bands from the mom, which means he got each of her homologous chromosomes = nondisjunction in meiosis I (which failed to separate her homologous chromosomes during her egg formation).
Telomerase is the enzyme that prevents shortening of telomeres. Increased telomerase activity occurs cancers. Telomeres at the end of chromosomes have lots of GT repeats.
Endonucleases are needed for nucleotide excision repair, which is the process that fixes DNA that's damaged by UV light (UV light creates pyrimidine dimers in DNA). Without endonuclease and nucleotide excision repair, you get xeroderma pigmentosum. XP is an AR condition where you have impaired nucleotide excision repair, usually due to deficiency in endonuclease.
Never heard of dyskeratosis congenita, but I got the question right because the pt had premature aging due to telomerase deficiency. Telomoerase prevents the ends of the chromosomes from being degraded. Every time you go through cell division, the ends of the chromosomes (telomeres) get shortened. Telomerase adds to the telomeres so that won't happen. Cells that divide frequently need telomerase. The cells include hematopoeitic stem cells, epithelial cells, and lymphocytes. Telomerase is a reverse transcriptase that adds TTAGGG repeats to the telomeres. This protects the chroomosomes from being shortened. Because once the chromosomes are shortened enough, the cells containing them will undergo apoptosis. Without telomerase, pts will have dystrophic nails, bone marrow failure, oral leukoplakia, and pulmonary fibrosis. Cells that don't regenerate don't have telomerase activity--so those cells that don’t regenerate include cardiac cells, CNS cells.
During translation, the first stop codon on the mRNA causes binding of a release factor. The anticodon is on the tRNA. From Wikipedia:
Dyskeratosis congenita (DKC), also known as Zinsser-Engman-Cole syndrome is a rare progressive congenital disorder with a highly variable phenotype.[3] The entity was classically defined by the triad of abnormal skin pigmentation, nail dystrophy, and leukoplakia of the oral mucosa, but these components do not always occur.[3] DKC is characterized by short telomeres. Some of the manifestations resemble premature aging (similar to progeria). The disease initially mainly affects the skin, but a major consequence is progressive bone marrow failure which occurs in over 80%, causing early mortality.
PKU is AR mutation of the gene that codes for phenylalanine hydroxylase. So you need two bad alleles to have the disease.
Hemophilia A and B are X-linked recessive. Probability confuses me, so even if I remembered that hemophilia is X-linked recessive, I still probably would've gotten this question wrong. Anyway, if a woman's brother has hemophilia and one of the parents is a carrier of hemophilia, that means the woman has a 50% chance of being a carrier. The probability of her passing it on to her son is 50%. The probability of her child being male is 50%. So ultimatley, the probability of her child being affected is the probability of the mom being a carrier x the probability that the mom passes it in to her child x the probability that her child is a male = 0.5 x 0.5 x 0.5 = 1/8.
RNA pol I, II, and III are in eukaryotic cells. RNA pol I makes ribosomal RNA. RNA pol II makes messenger RNA, snRNA, and micro RNA. RNA pol III makes transer RNA and 5S ribosomal RNA. I think I made a mnemonic for this a long time ago. RNA pol I = rRNA, RNA pol II = mRNA, RNA pol III = tRNA. The nucleolus in a cell is basophilic, meaning it stains darkly. rRNA is transcribed in the nucleolus. Cancer cells have a lot of rRNA and their nucleoli are dark-staining.
Remember that DNA is made in the 5' to 3' direction, but read by DNA pol in the 3' to 5' direction.
AAUAAA in the mRNA is the consensus sequence that causes addition of the poly A tail, which protects the mRNA from degradation when it goes into the cytoplasm. So it has a bunch of adenine.
Frameshift mutation = addition or deletion of a number of bases that's not divisible by 3-> altered reading frame and premature stop codon.
#Alternative splicing#genetics#snRNP#splicing#Fas#FasL#FasR#apoptosis#caspase#caspases#homocystinuria#homocysteine#telomere#telomerase#xeroderma pigmentosum#nucleotide excision repair#endonuclease#PKU#hemophilia#inheritance patterns#RNA#poly A tail#consensus sequence#hnRNA
2 notes
·
View notes
Text
As shown in Fig. 5A and B, 5- autophagosome cargo degradation and autophagic flux [38,39].
As shown in Fig. 5A and B, 5- autophagosome cargo degradation and autophagic flux [38,39]. We Fuorprodigiosinaloneminimallyinhibitedtumorgrowthcomparedto found that prodigiosin blocked the lysosomal phase of autophagy by that in the untreated tumor-bearing mice. In contrast Cell Counting Kit-8 mw, both tumor increasingaccumulationoftheprecursorcathepsins.Furtherstudiesare weight and volume decreased significantly in the combination tr###http://www M3814 (nedisertib).glpbio.com/simage/GA11233-L-NAME-hydrochloride-4.png####eat- neededtoelucidatethemechanismsofprodigiosin-mediated inhibition ment compared to that in either single-agent group. Furthermore, no of autophagosome-lysosome fusion and cathepsin maturation. significant changes were seen in the body weight of any of the treated Recent studies have implicated autophagy as a mechanism of 5-Fu mice (Fig. 5C). The safety profile of prodigiosin was also assessed in resistanceincancercells[40,41].Furthermore,inhibitionofautophagy terms of the hematological and histological parameters. The serum le- by3-methyladenine(3-MA,anautophagyinhibitor)sensitizesCRCcells vels of creatinine, blood urea nitrogen (BUN), AST and ALT were not towards 5-Fu-induced apoptosis involving cytochrome c release and significantly affected by prodigiosin (Supplementary Fig. 6A), and no activation of caspases [30]. Consistent with these findings, we found changesweredetectedinthemajororganslikeheart,liver,spleen,lung that 5-Fu induced apoptosis and autophagy in CRC cells, and co-treat- and kidney of the prodigiosin-treated mice compared to the controls ment with prodigiosin and 5-Fu activated caspase-3, caspase-9 and (SupplementaryFig.6B).Consistentwiththeinvitroresults,prodigiosin PARP.
1 note
·
View note
Text
Zhao, et al. Cancer Letters 481 (2020) 15–23 (caption on next page)
3xFLAG price. Zhao, et al. Cancer Letters 481 (2020) 15–23 Fig. 5. The combination of Prodigiosin and 5-Fu inhibits the growth of HCT116 xenografts in nude mice. Nude mice bearing HCT116 xenograft tumors were treated with vehicle, prodigiosin alone (1 mg/kg), 5-Fu alone (30 mg/ kg), or a combination of prodigiosin and 5-Fu twice weekly through i.p. injection for 21 days after inocula- tion with cultured tumor cells. (A) Tumor images and tumor weights are shown.Onday21afterinoculation,the mice were sacrificed, and the tumor tissues were imaged, weighed, and de- tailed. Mean ± SD (n = 5); **, P < 0.01 versus control, prodigiosin or 5-Fu alone. (B) Tumor volume was recorded every three days after treat- ment. Mean ± SD (n = 5); **, P < 0.01 versus control, prodigiosin or 5-Fu alone. (C) Body weight was recorded every three days during the 21 day of exposure. No sig- nificant differences were detected be- tween the vehicle and other groups: prodigiosin alone, 5-Fu alone or com- bination of prodigiosin and 5-Fu. (D) Western blotting analyses for LC3B-II and SQSTM1 in the xenograft tumor tissues from the vehicle group (#1, 2, 5), 5-Fu-treated group (#7, 9, 10), prodigiosin-treatedgroup(#11,13,15) and combination-treated group (#17, 19,20).(E)H&Estainingforevaluating the histological morphology and im- munohistochemistry staining to detect c-caspase 3 and SQSTM1 levels. Scale bar = 50 μm. All the immunostaining experiments were repeated in three se- parate mouse tumor tissues and the most typical images are shown 3x FLAG solubility. Acquisition of data (provided animals and conducted western References blotting,qPCR,immunohistochemistryandotherexperiments.):S.Qiu, Y. Peng, H. Xu, C. Zhao. [1] R.L. Siegel, K.D. Miller, A. Jemal, Cancer statistics, Ca - Cancer J. Clin. 68 (2018) 7–30 2018. Analysis and interpretation of data (statistical analyses and [2] F.Bray,J.Ferlay,I.Soerjomataram,R.L.Siegel,L.A.Torre,A.Jemal,Globalcancer biostatistics): S. Qiu, Z. Feng, C. Zhao, H. Huang, Y. Zhou. statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 Writing 3xFLAG PEPTIDE storage, review, and/or revision of the manuscript: C. Zhao, Y. cancers in 185 countries, Ca - Cancer J. Clin. 68 (2018) 394–424. [3] B. Gustavsson, G. Carlsson, D. Machover, N. Petrelli, A. Roth, H.J. Schmoll, Zhou, Y. Nie. K.M. Tveit, F. Gibson, A review of the evolution of systemic chemotherapy in the Study supervision: Z cck8 chemicals. Feng, Y. Nie. management of colorectal cancer, Clin. Colorectal Canc. 14 (2015) 1–10. Performed the experiments: J. He. [4] T.H.Cartwright,Treatmentdecisionsafterdiagnosisofmetastaticcolorectalcancer, Clin. Colorectal Canc. 11 (2012) 155–166. [5] L. Dahan, A. Sadok, J.L. Formento, J.F. Seitz, H. Kovacic, Modulation of cellular redox state underlies antagonism between oxaliplatin and cetuximab in human Declaration of competing interest colorectal cancer cell lines, Br. J. Pharmacol. 158 (2009) 610–620. [6] M.J. O\'Connell, Oxaliplatin or irinotecan as adjuvant therapy for colon cancer: the results are in, J. Clin. Oncol. 27 (2009) 3082–3084. The authors declare no conflicts of interest. [7] N. Mizushima, D.J. Klionsky, Protein turnover via autophagy: implications for metabolism, Annu. Rev. Nutr. 27 (2007) 19–40. [8] N. Mizushima, B. Levine, A.M. Cuervo, D.J. Klionsky, Autophagyfights disease through cellular self-digestion, Nature 451 (2008) 1069–1075 Cell Counting Kit-8 for sale. Appendix A. Supplementary data [9] J.H. Hurley, B.A. Schulman, Atomistic autophagy: the structures of cellular self- digestion, Cell 157 (2014) 300–311. Supplementary data to this article can be found online at https:// [10] A. Kuma, M. Hatano, M. Matsui, A. Yamamoto, H. Nakaya, T. Yoshimori,
1 note
·
View note
Text
Metformin Reduces the Extent of Varicocele-Induced Damage in Testicular Tissue
Authored by: Erkan Erdem*
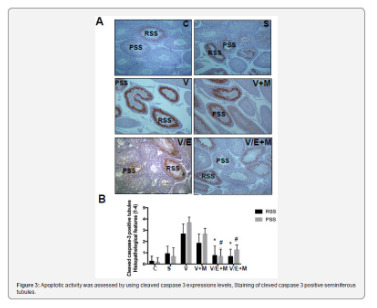
Introduction
Varicocele is an abnormal vascular dilatation of pampiniform plexus, commonly developing at puberty. Although underlying mechanisms remain poorly understood genetic background, anatomical aberrations, incompetence of venous valves, difference between the drainage of left and right testicular veins were suggested in the etiology [1]. As left spermatic vein being longer than the right vein, it is more commonly incurred to increased hydrostatic pressure and dilatation. Compression of the left renal vein between the aorta and the superior mesenteric artery may also contribute to the disturbed intravenous pressure [2].
The prevalence of varicocele varies between 15-20 % in general population and 30-40% in infertile men, and 11-19% of adolescents [3-6]. It was reported that varicocele is a progressive disease and early diagnosis and treatment in youth may enhance fertility potential [7]. Several contributing factors in the pathophysiology of varicocele have been proposed such as higher temperature of testis, the disorder of neuroendocrine system, autoimmunity, accumulation of renal and adrenal metabolites, genetic and epigenetic factors, hypoxia and oxidative stress [8-10].
Varicocele represents a chronic process within the testicle, which is linked to increased reactive oxygen species (ROS) beyond physiologic limits and, subsequently, disrupting sperm membrane fluidity, causing DNA damage and necrosis [11]. Moreover, superoxide dismutase 1, glutathione S-transferase M1 and T1 which are counteracting free superoxide radicals in cells have been reported to be decreased in men with varicocele, that may be important on disturbed sperm parameters [12]. Apoptosis of germ cells was also demonstrated in the pathogenesis of varicocele-related infertility [13]. Clinical findings suggest that surgical repair of varicocele may decrease seminal oxidative stress levels and sperm DNA fragmentation and, thus, may improve sperm quality [14]. Therefore, surgical intervention seems to be a reliable option in the treatment of varicocele-related male infertility, although some controversial reports exist.
Additionally, anti-oxidant medications such as kallikrein, L-carnitine with L-acetyl carnitine, pentoxifylline, coenzyme Q10 have been used to improve the milieu in the testis in men with varicocele [15]. Metformin is a major therapeutic agent in the treatment of type 2 diabetes mellitus as an insulin sensitizer, which decreases hepatic glucose output and increases peripheral glucose uptake. Although its action was not fully elucidated, metformin attenuated intracellular reactive oxygen species and apoptosis in aortic endothelial cells, myocardium, renal tubular cells and testicular cells [16-20].
Aim
Potential effects of metformin on varicocele-induced testicular damage have not been studied in neither humans nor in animal models. Thus, we investigated the impact of metformin on spermatogenesis, testicular integrity, and apoptotic activity in the testis of adolescent rats with experimentally-induced varicocele.
Materials and Methods
Thirty-six male adolescent Wistar rats (6-week-old) were randomly and equally divided into six experimental groups. Surgical procedures were carried out under anesthesia with intraperitoneal injection of ketamine (50 mg/kg). The experimental groups were as follows:
• (C) Control group; no surgical procedure was performed, and testis was examined after removal.
• (S) Sham group, a midline incision was performed, and testis was examined 8 weeks later.
• (V) Varicocele - only group: Experimental varicocele was induced by partial ligation of left renal vein with
Silk suture at the area medial to the insertion of the adrenal and spermatic vein into renal vein as described previously [21].
• (V+M) Varicocele + metformin group: All rats were treated with metformin (300 mg/kg per day by oral gavages) for 8 weeks following induced varicocele.
• (V/E) Varicocele + varicocelectomy group: Varicocelectomy was performed 4 weeks and the examination of the testis 8 weeks after the induction of varicocele. No medication was used.
• (V/E+M) Varicocele + varicocelectomy + metformin group: Varicocelectomy was performed 4 weeks after the induced varicocele. Metformin treatment (300 mg/kg per day by oral gavages) was initiated after the induction of varicocele and continued for 8 weeks. Left testes were examined 8 weeks after the induction of varicocele in all varicocele - induced groups. As maximum apoptotic activity initiates approximately 28 days after the induction of varicocele the procedure of varicocelectomy was performed 4 weeks after the formation of varicocele [22].
Histologic preparation and evaluation
The testicular tissue was fixed in Bouin’s solution (75% picric acid, 5% glacial acetic acid, and 25% formaldehyde) and embedded in paraffin blocks. Sections (5 μm) were formed, deparaffinized, and stained with hematoxylin and eosin. Spermatogenesis was examined in each group using Johnsen’s score (a score of 1-10 was assigned to each tubule regarding epithelial maturation) as described previously [23]. Sections were examined in a random order under a standard light microscope with 10x and 40x magnification by a blinded histologist; unaware of which group each rat belonged to. Histological grading was done by examining approximately 80 randomly selected seminiferous tubules per rat. Thus, a total of approximately 480 seminiferous tubules were scored for each group.
Histomorphometry analysis
A total of 103 randomly selected seminiferous tubules stained with hematoxylin-eosin were analyzed in each group. The presence of round spermatid stage (RSS) and primary spermatocyte stages (PSS) were assessed as described previously and compared among the groups [24].
Immunohistochemical staining for cleaved caspase-3 and ImageJ analysis
Cleaved caspase-3 was used for immunohistochemical staining. Testicular tissue samples were immediately fixed in 10% neutral-buffered formalin, embedded in paraffin, and sectioned (5 μm). Sections were deparaffinized and blocked for endogenous peroxidase activity with methanol containing 3% H2O2 for 10 m. Ultra V Block (Lab vision, Freemont, CA) for 7 m at room temperature. Cleaved Caspase-3 (#9664, Cell Signaling, U.S.) was applied at a dilution of 1: 500 and incubated overnight at +4 °C in a humidified chamber for nonspecific binding. The sections were washed in phosphate-buffered saline (PBS) and incubated with biotinylated horse anti-rabbit IgG (3 mg/mL; Vector, Burlingame, CA) at a 1: 500 dilution for 1 h at room temperature.
Antibodies were detected using a VECTASTAIN avidinbiotin complex (Vector PK 4000) for 30 m at room temperature. Antibody complexes were visualized after incubation with 3,3’-diaminobenzidine tetrahydrochloride (DAB, Bio-Genex, San Ramon, CA.) and were mounted under glass coverslips in Entellan (Merck) and then evaluated under a light microscope. Immunohistochemical staining for cleaved caspase-3 was analyzed by counting 100 seminiferous tubule cross-sections in each group and expressed as the apoptotic index. In each photomicrograph, the following parameter was measured with ImageJ software: expression levels of cleaved-caspase-3 in both groups at round spermatid stage (RSS) of testes. Each of this parameter was measured 3 times for each image and the average of the 9 measurements of each sample was used for the statistical analysis. Histopathological features examined in rats with normal testis and with sham, varicocele, varicocele+ metformin in a subjective scoring (0 - not present; 1 - low grade; 2 - moderate grade; 3 - high grade; 4 - very high grade).
Statistical analysis
Histopathological findings (Johnsen’s score) were assessed by nonparametric Kruskal-Wallis test, and the mean Johnsen’s score was used in the comparison of the groups. Multiple comparisons were made using Tukey’s procedure. p<0.05 was considered statistically significant. Analysis of variance was used for statistical analysis of the apoptotic index among the groups.
Results
Assessment of spermatogenesis
Johnsen’s score was significantly lower in V group (4.14±1.25) compared to C group (9.1±0.3) or S group (9.0 ± 0.2) groups (p<0.05). V+M group had significantly higher score (6.9±0.6) than V group (p<0.05). V/E group and V/E+M group had similar Johnsen scores (8.9 ± 1.02 and 9.2 ± 0.6). These findings suggest that the administration of metformin resulted in 40.6% of improvement in spermatogenesis in rats with varicocele. However, this favorable effect was not observed when metformin was used along with varicocelectomy.
Histological and morphological changes in seminiferous tubules
Histological and morphological changes in the testes of rats were compared via hematoxylin and eosin staining and degenerated tubules (DT) were only detected in V and V+ M groups, not in C, S, V/E and V/E+M groups (Figure 1). Visual assessment of the disorganized seminiferous tubules further supported these findings as seen in Figure 2. Seminiferous tubule degeneration scores were used for quantification of data (Figure 2b). V group had significantly higher scores of RSS and PSS compared to C and S group (2.6±0.8 and 3.7±0.4; 0.2±0.4 and 0.2±0.4; 0.9±0.6 and 0.6±0.7, respectively) (p<0.05). V/E group had significantly lower RSS (0.7±0.8) and PSS (0.8±0.7) scores than V group (p<0.05). V+M group had significantly lower RSS and PSS scores (1.8±0.7 and 2.6±0.7, p<0.05) in comparison to V group, implicating beneficial effects of metformin in rats with varicocele. When compared to V/E group, V/E+M group did not exhibit any difference in RSS (0.6±0.6) and PSS (1.4±0.5) scores, suggesting the absence of additive positive effect of metformin in varicocelectomies rats.
Apoptotic activity
Apoptotic activity was assessed by using cleaved caspase 3 expressions levels, staining of cleved caspase 3 positive seminiferous tubules were shown in Figure 3a. Cleaved caspase 3 expressions were significantly higher in V group (3.5 ± 0.5) compared to C (0) and S (0.2 ± 0.4) groups. V+M group had significantly lower cleaved caspase 3 level (3.0 ± 0.7) than V group. V/E group had lower cleaved caspase-3 expression levels (1.0 ± 0.7) compared to V group. Treatment of varicoceleectomy rats with metformin (V/E+M) did not further reduce apoptotic activity in the seminiferous tubules (1.75 ± 0.43) when compared to the varicocelectomy group (V/E) (Figure 3b).
Discussion and Conclusion
The present study demonstrates that metformin can reduce the extent of testicular damage in rats with varicocele, although having no effect in rats following varicocelectomy Spermatogenesis, seminiferous tubule integrity and the degree of apoptosis were improved using metformin in the presence of varicocele although it was not as remarkable as what was obtained through varicocelectomy. A review of the literature revealed that the impact of metformin on varicocele was not investigated in humans or animal models until now.
Although it is a commonly identified abnormality not all men with varicocele present with infertility. Some intrinsic factors may render some men to become susceptible to varicocele, thus, the best candidates who benefit from varicocelectomy yet to be clarified. Since oxidative stress was shown to be important in the pathophysiology of varicocele some agents have been used to improve the milieu in the testis [1]. A number of anti-oxidant medications have been studied to relieve detrimental effects of varicocele in the testis [25]. These agents have been used either alone or as an adjuvant therapy with surgery. However, surgery remains the treatment of choice and there exists insufficient data to recommend medical therapy in men with varicocele. Barekat et al. [26] reported that administration of an antioxidant agent N-acetyl cysytein as an adjunct therapy improved semen quality following varicocelectomy [26]. Tek et al. [21] demonstrated that vascular endothelial growth factor decreased apoptosis in varicoceleinduced rats as evidenced by diminished caspase-3 positive cells [21]. Both studies showed the benefit of these as adjunct therapy following varicocelectomy. However, in the present study metformin did not enhance the effect of varicocelectomy.
Minutoli et al. [13] demonstrated that neuronal apoptosis inhibin factor and surviving expressions were significantly reduced following varicocele induction and polydeoxyribonucleotide, an agonist of adenosine A2A receptor, administration restored testicular function [13]. Several other studies detected increased germ cell apoptosis in rats with varicocele [21,22,27]. However, in another study, apoptosis was found to be decreased in germ cells in the testes of infertile men with varicocele as compared with normal men [28]. It was speculated that the fixation of testis in formaldehyde might have played a role in the different result. In the present study, cleaved caspase 3 expression was used to assess apoptotic activity and it was found that metformin reduced apoptotic activity in rats with varicocele, whereas no additional effect was observed when metformin was administered after varicocelectomy.
Metformin is commonly used in type 2 diabetes mellitus and polycystic ovarian disease as an insulin sensitizer [29]. Also, it is present in various tissues including myocardium, liver, pancreas, thyroid, adipose tissue, hypothalamus, pituitary, and male and female gonads [19,30,31]. It has been reported that metformin is mainly transported into cells by organic cation transporters as passive diffusion is limited [32]. Although the mechanism of action is not yet fully elucidated recent studies suggested that metformin acts through AMP-activated protein kinase (AMPK) pathway, inhibits the activity of the respiratory electron transport chain in mitochondria, induces epigenetic modifications which in part may explain long term effects and decreases oxidative stress and apoptotic activity [16,19, 33-35].
Male reproductive system utilizes all these metabolic pathways and is prone to be affected by metformin administration [20,36,37]. Metformin was found to stimulate lactate production which is important in the development of germ cells and show an anti-apoptotic effect in rat Sertoli cells [38]. It was also reported that metformin reduced the apoptotic cells and caspase-3 level in rat testis [20]. The findings of the present study are consistent with previous studies that metformin reduced apoptosis in testis with varicocele. Yan et al. [37] reported that metformin improved the semen parameters related to its effects on weight loss, increased testicular weight and reduced testicular cell apoptosis [37]. On the other hand, Tartarin et al. [36] reported metformin at concentration 10 times higher than therapeutic levels decreased testosterone secretion and the number of Sertoli cells in rats when it was administered during pregnancy [36]. Faure et al. [39] reduction in testicular weight and testosterone level were observed in 6-week-old chickens treated with metformin for 3 weeks [39].
Several groups demonstrated that post-operative administration of metformin can exert protective effects in male reproductive function in rat models [40]. Bosman et al. [41] demonstrated that infertile hyperinsulinaemic men could benefit from metformin treatment in combination with an enriched antioxidant diet [41]. Besides, metformin was reported to act as a protective compound when used in the media for cryopreservation of spermatozoa [30]. In conclusion, metformin reduces detrimental effects of varicocele, although no additional benefit is expected following varicocelectomy. Further studies are required to apply metformin for this indication in humans.
#open access journals#peer review journals#Juniper Publishers PubMed Indexed Articles#reproductive medicine#GJORM in juniper publishers
1 note
·
View note