#Case Reports
Explore tagged Tumblr posts
Text

need to share an experience i had 30 minutes ago
(edit: thanks to @walks-the-ages for providing and reminding me to put alt text, sorry it slips my mind alot lol)
#my hands are still shaking to be quite honest i could not put a lot of effort into this.#but like. brain. why did you do that#literally i have been like hopelessly obsessed with de nonstop thinking abt it for the past couple of days it is Scaring me#it is terminal its soooo fucking chronic#disco elysium#kim kitsuragi#for anyone who wants to know i bumped into some guys car that was stopped for a school bus. i think my brain errored and thought#my foot was fully pressing down on the brake pedal but it wasnt.#i am like 99.99 percent sure neither of us had any major damage to our cars but we still filed a police report just in case#because insurance do be a bitch. dudes back bumper was scratched lightly and my front license plate has a dent now#also literally my first ever car accident that ive had ever yippee yay
30K notes
·
View notes
Text
Today in 🍂✨October surprises✨🍂

• Secretary of Transportation Pete Buttigieg and Secretary of Labor Julie Su quietly assisted in winning labor rights for dockworkers, ending a strike that could have had catastrophic economic consequences. (10-4-24)
• In Springfield, Ohio, where Haitian migrants have been blamed for the disappearance of local animals with Trump claiming “‘migrants are walking off’ with geese in the town” and “they’re eating the dogs” - a lie also promoted by JD Vance, Ohio’s own sitting Senator, with no evidence - it turns out that the missing geese were actually the victims of a 64-year-old white man who was hunting illegally. (10-3-24)
• A Trump-appointed federal judge blocked Biden’s student loan forgiveness plan again after another judge reinstated it earlier this week. (10-3-24)
• Republicans and crazy Facebook uncles everywhere have spent this week spreading disinformation about the FEMA response to Hurricane Helene, including AI photos of Trump standing in floodwater and wild claims that Biden is sending money to undocumented immigrants. In reality, the Biden-Harris administration has provided substantial emergency assistance and both Biden and Harris have visited the region. Meanwhile, it turns out that Trump was the one who redirected money from disaster relief to send to ICE during his presidency. Shocker. (10-4-24)
• Seriously, though, Trump is not who you want to call in an emergency. Before allowing disaster relief to reach victims of wildfires in California, then-president Trump forced aides to show him an electoral map to see if he had voters there. He evidently intended to withhold the aid if he found out it was going to mostly Democratic voters. This would be a career-ending scandal in any other political era but alas, we are living in this one. (10-3-24)
• Finally, far-right extremist and Oklahoma superintendent of schools Ryan Walters intends to put Bibles in public schools, which is already disturbing, but in a stunning display of corruption, the only ones that meet his specifications are the so-called “Trump Bibles” that include the Constitution and Declaration of Independence. They go for $60 apiece and Trump gets fees from each one. (10-4-24)
No, wait, I’m going to say that one again:
In Oklahoma, taxpayers’ money will be used to put Trump Bibles in public schools. Their money will go directly to Trump. Not a joke!!! Not an exaggeration!!!
…Surely the voters who are still undecided are lying, right?? Right?!
30 days until Election Day.

Go to vote.org for a sample ballot, early voting dates, and more. Seriously, we have to win.
#guys should I start a substack#joking but seriously. Pay Attention! It’s Time! lots happening and#remarkably little reporting on the wildfires thing and the julie su/pete buttigieg win!#I think the Oklahoma thing is actually organized crime?#he already has a rico case is he trying to get another one#us politics#mine#us news#kamala 2024#vote
4K notes
·
View notes
Text
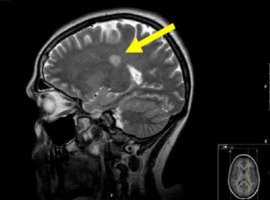
Retinal and choroidal vascular drop out in a case of severe phenotype of Flammer Syndrome. Rescue of the ischemic-preconditioning mimicking action of endogenous Erythropoietin (EPO) by off-label intra vitreal injection of recombinant human EPO (rhEPO) by Claude Boscher in Journal of Clinical Case Reports Medical Images and Health Sciences

Journal of Clinical Case Reports Medical Images and Health Sciences
ABSTRACT
Background: Erythropoietin (EPO) is a pleiotropic anti-apoptotic, neurotrophic, anti-inflammatory, and pro-angiogenic endogenous agent, in addition to its effect on erythropoiesis. Exogenous EPO is currently used notably in human spinal cord trauma, and pilot studies in ocular diseases have been reported. Its action has been shown in all (neurons, glia, retinal pigment epithelium, and endothelial) retinal cells. Patients affected by the Flammer Syndrome (FS) (secondary to Endothelin (ET)-related endothelial dysfunction) are exposed to ischemic accidents in the microcirculation, notably the retina and optic nerve.
Case Presentation: A 54 years old female patient with a diagnosis of venous occlusion OR since three weeks presented on March 3, 2019. A severe Flammer phenotype and underlying non arteritic ischemic optic neuropathy; retinal and choroidal drop-out were obviated. Investigation and follow-up were performed for 36 months with Retinal Multimodal Imaging (Visual field, SD-OCT, OCT- Angiography, Indo Cyanin Green Cine-Video Angiography). Recombinant human EPO (rhEPO)(EPREX®)(2000 units, 0.05 cc) off-label intravitreal injection was performed twice at one month interval. Visual acuity rapidly improved from 20/200 to 20/63 with disparition of the initial altitudinal scotoma after the first rhEPO injection, to 20/40 after the second injection, and gradually up to 20/32, by month 5 to month 36. Secondary cystoid macular edema developed ten days after the first injection, that was not treated via anti-VEGF therapy, and resolved after the second rhEPO injection. PR1 layer integrity, as well as protective macular gliosis were fully restored. Some level of ischemia persisted in the deep capillary plexus and at the optic disc.
Conclusion: Patients with FS are submitted to chronic ischemia and paroxystic ischemia/reperfusion injury that drive survival physiological adaptations via the hypoxic-preconditioning mimicking effect of endogenous EPO, that becomes overwhelmed in case of acute hypoxic stress threshold above resilience limits. Intra vitreal exogenous rhEPO injection restores retinal hypoxic-preconditioning adaptation capacity, provided it is timely administrated. Intra vitreal rhEPO might be beneficial in other retinal diseases of ischemic and inflammatory nature.
Key words : Erythropoietin, retinal vein occlusion, anterior ischemic optic neuropathy, Flammer syndrome, Primary Vascular Dysfunction, anti-VEGF therapy, Endothelin, microcirculation, off-label therapy.
INTRODUCTION
Retinal Venous Occlusion (RVO) treatment still carries insufficiencies and contradictions (1) due to the incomplete deciphering of the pathophysiology and of its complex multifactorial nature, with overlooking of factors other than VEGF up-regulation, notably the roles of retinal venous tone and Endothelin-1 (ET) (2-5), and of endothelial caspase-9 activation (6). Flammer Syndrome (FS)( (Primary Vascular Dysfunction) is related to a non atherosclerotic ET-related endothelial dysfunction in a context of frequent hypotension and increased oxidative stress (OS), that alienates organs perfusion, with notably changeable functional altered regulation of blood flow (7-9), but the pathophysiology remains uncompletely elucidated (8). FS is more frequent in females, and does not seem to be expressed among outdoors workers, implying an influence of sex hormons and light (7)(9). ET is the most potent pro-proliferative, pro-fibrotic, pro-oxidative and pro-inflammatory vasoconstrictor, currently considered involved in many diseases other than cardio-vascular ones, and is notably an inducer of neuronal apoptosis (10). It is produced by endothelial (EC), smooth vascular muscles (SVMC) and kidney medullar cells, and binds the surface Receptors ET-A on SVMC and ET-B on EC, in an autocrine and paracrine fashion. Schematically, binding on SVMC Receptors (i.e. through local diffusion in fenestrated capillaries or dysfunctioning EC) and on EC ones (i.e. by circulating ET) induce respectively arterial and venous vasoconstriction, and vasodilation, the latter via Nitrite oxide (NO) synthesis. ET production is stimulated notably by Angiotensin 2, insulin, cortisol, hypoxia, and antagonized by endothelial gaseous NO, itself induced by flow shear stress. Schematically but not exclusively, vascular tone is maintained by a complex regulation of ET-NO balance (8) (10-11). Both decrease of NO and increase of ET production are both a cause and consequence of inflammation, OS and endothelial dysfunction, that accordingly favour vasoconstriction; in addition ET competes for L-arginine substrate with NO synthase, thereby reducing NO bioavailability, a mechanism obviated notably in carotid plaques and amaurosis fugax (reviewed in 11).
Severe FS phenotypes are rare. Within the eye, circulating ET reaches retinal VSMC in case of Blood-Retinal-Barrier (BRB) rupture and diffuses freely via the fenestrated choroidal circulation, notably around the optic nerve (ON) head behind the lamina cribrosa, and may induce all pathologies related to acute ocular blood flow decrease (2-3)(5)(7-9). We previously reported two severe cases with rapid onset of monocular cecity and low vision, of respectively RVO in altitude and non arteritic ischemic optic neuropathy (NAION) (Boscher et al, Société Francaise d'Ophtalmologie and Retina Society, 2015 annual meetings).
Exogenous Recombinant human EPO (rhEPO) has been shown effective in humans for spinal cord injury (12), neurodegenerative and chronic kidney diseases (CKD) (reviewed in 13). Endogenous EPO is released physiologically in the circulation by the kidney and liver; it may be secreted in addition by all cells in response to hypoxic stress, and it is the prevailing pathway induced via genes up-regulation by the transcription factor Hypoxia Inducible Factor 1 alpha, among angiogenesis (VEGF pathway), vasomotor regulation (inducible NO synthase), antioxidation, and energy metabolism (14). EPO Receptor signaling induces cell proliferation, survival and differentiation (reviewed in 13), and targets multiple non hematopoietic pathways as well as the long-known effect on erythropoiesis (reviewed in 15). Of particular interest here, are its synergistic anti-inflammatory, neural antiapoptotic (16) pro-survival and pro-regenerative (17) actions upon hypoxic injury, that were long-suggested to be also indirect, via blockade of ET release by astrocytes, and assimilated to ET-A blockers action (18). Quite interestingly, endogenous EPO’s pleiotropic effects were long-summarized (back to 2002), as “mimicking hypoxic-preconditioning” by Dawson (19), a concept applied to the retina (20). EPO Receptors are present in all retinal cells and their rescue activation targets all retinal cells, i.e. retinal EC, neurons (photoreceptors (PR), ganglion (RGG) and bipolar cells), retinal pigment epithelium (RPE) osmotic function through restoration of the BRB, and glial cells (reviewed in 21), and the optic nerve (reviewed in 22). RhEPO has been tested experimentally in animal models of glaucoma, retinal ischemia-reperfusion (I/R) and light phototoxicity, via multiple routes (systemic, subconjunctival, retrobulbar and intravitreal injection (IVI) (reviewed in 23), and used successfully via IVI in human pilot studies, notably first in diabetic macular edema (24) (reviewed in 25 and 26). It failed to improve neuroprotection in association to corticosteroids in optic neuritis, likely for bias reasons (reviewed in 22). Of specific relation to the current case, it has been reported in NAION (27) (reviewed in 28) and traumatic ON injury (29 Rashad), and in one case of acute severe central RVO (CRVO) (Luscan and Roche, Société Francaise d’Ophtalmologie 2017 annual meeting). In addition EPO RPE gene therapy was recently suggested to prevent retinal degeneration induced by OS in a rodent model of dry Age Macular Degeneration (AMD) (30).
CASE REPORT PRESENTATION
This 54 years female patient was first visited on March 2019 4th, seeking for second opinion for ongoing vision deterioration OR on a daily basis, since around 3 weeks. Sub-central RVO (CRVO) OR had been diagnosed on February 27th; available SD-OCT macular volume was increased with epiretinal marked hyperreflectivity, one available Fluorescein angiography picture showed a non-filled superior CRVO, and a vast central ischemia involving the macular and paraoptic territories. Of note there was ON edema with a para-papillary hemorrage nasal to the disc on the available colour fundus picture.
At presentation on March 4, Best Corrected Visual Acuity (BCVA) was reduced at 20/100 OR (20/25 OS). The patient described periods of acutely excruciating retro-orbital pain in the OR. Intraocular pressure was normal, at 12 OR and 18 OS (pachymetry was at 490 microns in both eyes). The dilated fundus examination was similar to the previous color picture and did not disclose peripheral hemorrages recalling extended peripheral retinal ischemia. Humphrey Visual Field disclosed an altitudinal inferior scotoma and a peripheral inferior scotoma OR and was in the normal range OS, i.e. did not recall normal tension glaucoma OS (Fig. 1). There were no papillary drusen on the autofluorescence picture, ON volume was increased (11.77 mm3 OR versus 5.75 OS) on SD-OCT (Heidelberg Engineering®) OR, Retinal Nerve Fiber (RNFL) and RGC layers thicknesses were normal (Fig. 2). Marked epimacular hypereflectivity OR with foveolar depression inversion, moderately increased total volume and central foveolar thickness (CFT) (428 microns versus 328 OS), and a whitish aspect of the supero-temporal internal retinal layers recalling ischemic edema, were present (video 1). EDI CFT was incresead at 315 microns (versus 273 microns OS), with focal pachyvessels on the video mapping (video 1). OCT-Angiography disclosed focal perfusion defects in both the retinal and chorio-capillaris circulations (Fig. 3), and central alterations of the PR1 layer on en-face OCT(Fig. 4).
Altogether the clinical picture evoked a NAION with venous sub-occlusion, recalling Fraenkel’s et al early hypothesis of an ET interstitial diffusion-related venous vasoconstriction behind the lamina cribrosa (2), as much as a rupture of the BRB was present in the optic nerve area (hemorrage along the optic disc). Choroidal vascular drop-out was suggested by the severity and rapidity of the VF impairment (31). The extremely rapid development of a significant “epiretinal membrane”, that we interpreted as a reactive - and protective, in absence of cystoid macular edema (CME) - ET 2-induced astrocytic proliferation (reviewed in 32), was as an additional sign of severe ischemia.
The mention of the retro-orbital pain evoking a “ciliary angor”, the absence of any inflammatory syndrome and of the usual metabolic syndrome in the emergency blood test, oriented the etiology towards a FS. And indeed anamnesis collected many features of the FS, i.e. hypotension (“non dipper” profile with one symptomatic nocturnal episode of hypotension on the MAPA), migrains, hypersensitivity to cold, stress, noise, smells, and medicines, history of a spontaneously resolutive hydrops six months earlier, and of paroxystic episods of vertigo (which had driven a prior negative brain RMI investigation for Multiple Sclerosis, a frequent record among FS patients (33) and of paroxystic visual field alterations (7)(9), that were actually recorded several times along the follow-up.
The diagnosis of FS was eventually confirmed in the Ophthalmology Department in Basel University on April 10th, with elevated retinal venous pressure (20 to 25mmHg versus 10-15 OS) (4)(7)(9), reduced perfusion in the central retinal artery and veins on ocular Doppler (respectively 8.3 cm/second OR velocity versus 14.1 mmHg OS, and 3.1/second OR versus 5.9 cm OS), and impaired vasodilation upon flicker light-dependant shear stress on the Dynamic Vessel Analyser testing (7-9). In addition atherosclerotic plaques were absent on carotid Doppler.
On March 4th, the patient was at length informed about the FS, a possible off label rhEPO IVI, and a related written informed consent on the ratio risk-benefits was delivered.
By March 7th, she returned on an emergency basis because of vision worsening OR. VA was unchanged, intraocular pressure was at 13, but Visual Field showed a worsening of the central and inferior scotomas with a decreased foveolar threshold, from 33 to 29 decibels. SD-OCT showed a 10% increase in the CFT volume.
On the very same day, an off label rhEPO IVI OR (EPREX® 2000 units, 0,05 cc in a pre-filled syringe) was performed in the operating theater, i.e. the dose reported by Modarres et al (27), and twenty times inferior to the usual weekly intravenous dose for treatment of chronic anemia secondary to CKD. Intra venous acetazolamide (500 milligrams) was performed prior to the injection, to prevent any increase in intra-ocular pressure. The patient was discharged with a prescription of chlorydrate betaxolol (Betoptic® 0.5 %) two drops a day, and high dose daily magnesium supplementation (600 mgr).
Incidentally the patient developed bradycardia the day after, after altogether instillation of 4 drops of betaxolol only, that was replaced by acetazolamide drops, i.e. a typical hypersensitivity reaction to medications in the FS (7)(9).
Subjective vision improvement was recorded as early as D1 after injection. By March 18 th, eleven days post rhEPO IVI, BCVA was improved at 20/63, the altitudinal scotoma had resolved (Fig. 5), Posterior Vitreous Detachment had developed with a disturbing marked Weiss ring, optic disc swelling had decreased; vasculogenesis within the retinal plexi and some regression of PR1 alterations were visible on OCT-en face. Indeed by 11 days post EPO significant functional, neuronal and vascular rescue were observed, while the natural evolution had been seriously vision threatening.
However cystoid ME (CME) had developed (video 2). Indo Cyanin Green-Cine Video Angiography (ICG-CVA) OR, performed on March 23, i.e. 16 days after the rhEPO IVI, showed a persistent drop in ocular perfusion: ciliary and central retinal artery perfusion timings were dramatically delayed at respectively 21 and 25 seconds, central retinal vein perfusion initiated by 35 seconds, was pulsatile, and completed by 50 seconds only (video 3). Choroidal pachyveins matching the ones on SD-OCT video mapping were present in the temporal superior and inferior fields, and crossed the macula; capillary exclusion territories were present in the macula and around the optic disc.
By April 1, 23 days after the rhEPO injection, VA was unchanged, but CME and perfusion voids in the superficial deep capillary plexi and choriocapillaris were worsened, and optic disc swelling had recurred back to baseline, in a context of repeated episodes of systemic hypotension; and actually Nifepidin-Ratiopharm® oral drops (34), that had been delivered via a Temporary Use Authorization from the central Pharmacology Department in Assistance Publique Hopitaux de Paris, had had to be stopped because of hypersensitivity.
A second off label rhEPO IVI was performed in the same conditions on April 3, i.e. approximately one month after the first one.
Evolution was favourable as early as the day after EPO injection 2: VA was improved at 20/40, CME was reduced, and perfusion improved in the superficial retinal plexus as well as in the choriocapillaris. By week 4 after EPO injection 2, CME was much decreased, i.e. without anti VEGF injection. On august 19th, by week 18 after EPO 2, perfusion on ICG-CVA was greatly improved , with ciliary timing at 18 seconds, central retinal artery at 20 seconds and venous return from 23 to 36 seconds, still pulsatile. Capillary exclusion territories were visible in the macula and temporal to the macula after the capillary flood time that went on by 20.5 until 22.5 seconds (video 4); they were no longer persistent at intermediate and late timings.
Last complete follow-up was recorded on January 7, 2021, at 22 months from EPO injection 2. BCVA was at 20/40, ON volume had dropped at 7.46 mm3, a sequaelar superior deficit was present in the RNFL (Fig. 2) with some corresponding residual defects on the inferior para central Visual Field (Fig. 5), CFT was at 384 mm3 with an epimacular hyperreflectivity without ME, EDI CFT was dropped at 230 microns. Perfusion on ICG-CVA was not normalized, but even more improved, with ciliary timing at 15 seconds, central retinal artery at 16 seconds and venous return from 22 to 31 seconds, still pulsatile (video 5), indicating that VP was still above IOP. OCT-A showed persisting perfusion voids, especially at the optic disc and within the deep retinal capillary plexus. The latter were present at some degree in the OS as well (Fig. 6). Choriocapillaris and PR1 layer were dramatically improved.
Last recorded BCVA was at 20/32 by February 14, 2022, at 34 months from EPO 2. SD-OCT showed stable gliosis hypertrophy and mild alterations of the external layers (video 6).
Figure 1: Humphrey visual field at baseline on March 7th 2019, showing an altitudinal central scotoma, an inferior peripheral scotoma with a normal and symmetrical foveolar sensitivity threshold, and a normal visual field OS
Figure 2: Retinal Nerve Fiber (RNFL ) evolution from normal at baseline on March 2019 7th, to development of a superior sequellar deficit that remained stable on last follow-up.
Figure 3: OCT-Angiography at baseline on March 7th 2019, showing perfusion voids OR in the superior superficial retinal plexus and in the choriocapillaris.
Figure 4: OCT en face at baseline on March 7th 2019, showing PR1 layer deficits OR (artefacts in the superior half) compared to OS.
Figure 5: Humphrey visual field follow-ups : at follow-up 1 eleven days after rhEPO intra vitreal injection showing resolution of the altitudinal central scotoma and decrease of the inferior scotoma, and at last visual field follow-up on January 20th 2021, showing residual defects corresponding to the RNFL ones on Figure 2.
Figure 6: OCT Angiography performed on January 7th 2021, at 22 months from EPO injection 2, showing persisting perfusion voids, especially at the optic disc, and within the deep retinal capillary plexus, that were present at some degree in the OS as well.
Video 1 : SD-OCT video mapping OR at baseline on March 7th 2019, showing epiretinal hyperreflectivity and epiretinal membrane with foveolar depression inversion, ischemic edema in the internal and temporal to the disc superior retinal layers, and focal choroidal Haller pachyvessels with reduction in chorio-capillaris/Sattler layers.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_1.mov
Video 2: SD-OCT video mapping OR at follow-up 1 eleven days after rhEPO intra vitreal injection on March 18th, showing epiretinal hyperreflectivity and epiretinal membrane with foveolar depression inversion, ischemic edema in the internal and temporal to the disc superior retinal layers, and development of central cystoid macular edema.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_2.mov
Video 3 : Indo Cyanin Green-Cine Video Angiography OR, performed on March 23, i.e. 16 days after the rhEPO IVI, showing a persistent drop in ocular perfusion: ciliary and central retinal artery perfusion timings were dramatically delayed at respectively 21 and 25 seconds, central retinal vein perfusion initiated by 35 seconds, was pulsatile, and completed by 50 seconds only.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_3.mov
Video 4 : Indo Cyanin Green-Cine Video Angiography OR, performed on August 19, i.e. by week 18 after EPO 2, showing greatly improved perfusion, with ciliary timing at 18 seconds, central retinal artery at 20 seconds and venous return from 23 to 36 seconds, still pulsatile. Capillary exclusion territories were visible in the macula and temporal to the macula after the capillary flood time that went on by 20.5 until 22.5 seconds.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_4.mov
Video 5: Indo Cyanin Green-Cine Video Angiography OR, performed on January 7th, 2021, at 22 months from EPO injection 2: perfusion was not normalized, but even more improved, with ciliary timing at 15 seconds, central retinal artery at 16 seconds and venous return from 22 to 31 seconds, still pulsatile.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_5.avi
Video 6 : SD-OCT video mapping at 34 months from EPO 2, showing stable gliosis hypertrophy and mild alterations of the external layers.
Vedio: https://jmedcasereportsimages.org/articles/JCRMHS_1231_Vedio_6.avi
DISCUSSION
What was striking in the initial clinical phenotype of CRVO was the contrast between the moderate venous dilation, and the intensity of ischemia, that were illustrating the pioneer hypothesis of Professor Flammer‘s team regarding the pivotal role of ET in VO (2), recently confirmed (3)(35), i.e. the local venous constriction backwards the lamina cribrosa, induced by diffusion of ET-1 within the vascular interstitium, in reaction to hypoxia. NAION was actually the primary and prevailing alteration, and ocular hypoperfusion was confirmed via ICG-CVA, as well as by the ocular Doppler performed in Basel. ICG-CVA confirmed the choroidal drop-out suggested by the severity of the VF impairment (31) and by OCT-A in the choriocapillaris. Venous pressure measurement, which instrumentation is now available (8), should become part of routine eye examination in case of RVO, as it is key to guide cases analysis and personalized therapeutical options.
Indeed, the endogenous EPO pathway is the dominant one activated by hypoxia and is synergetic with the VEGF pathway, and coherently it is expressed along to VEGF in the vitreous in human RVO (36). Diseases develop when the individual limiting stress threshold for efficient adaptative reactive capacity gets overwhelmed. In this case by Week 3 after symtoms onset, neuronal and vascular resilience mechanisms were no longer operative, but the BRB, compromised at the ON, was still maintained in the retina.
As mentioned in the introduction, the scientific rationale for the use of EPO was well demonstrated by that time, as well as the capacities of exogenous EPO to mimic endogenous EPO vasculogenesis, neurogenesis and synaptogenesis, restoration of the balance between ET-1 and NO. Improvement of chorioretinal blood flow was actually illustrated by the evolution of the choriocapillaris perfusion on repeated OCT-A and ICG-CVA. The anti-apoptotic effect of EPO (16) seems as much appropriate in case of RVO as the caspase-9 activation is possibly another overlooked co-factor (6).
All the conditions for translation into off label clinical use were present: severe vision loss with daily worsening and unlikely spontaneous favourable evolution, absence of toxicity in the human pilot studies, of contradictory comorbidities and co-medications, and of context of intraocular neovascularization that might be exacerbated by EPO (37).
Why didn’t we treat the onset of CME by March 18th, i.e. eleven days after EPO IVI 1, by anti-VEGF therapy, the “standard-of-care” in CME for RVO ?
In addition to the context of functional, neuronal and vascular improvements obviated by rhEPO IVI by that timing in the present case, actually anti VEGF therapy does not address the underlying causative pathology. Coherently, anti-VEGF IVI : 1) may not be efficient in improving vision in RVO, despite its efficiency in resolving/improving CME (usually requiring repeated injections), as shown in the Retain study (56% of eyes with resolved ME continued to loose vision)(quoted in (1) 2) eventually may be followed by serum ET-1 levels increase and VA reduction (in 25% of cases in a series of twenty eyes with BRVO) (38) and by increased areas of non perfusion in OCT-A (39). Rather did we perform a second hrEPO IVI, and actually we consider open the question whether the perfusion improvement, that was progressive, might have been accelerated/improved via repeated rhEPO IVI, on a three to four weeks basis.
The development of CME itself, involving a breakdown of the BRB, i.e. of part of the complex retinal armentorium resilience to hypoxia, was somewhat paradoxical in the context of improvement after the first EPO injection, as EPO restores the BRB (24), and as much as it was suggested that EPO inhibits glial osmotic swelling, one cause of ME, via VEGF induction (40). Possible explanations were: 1) the vascular hyperpermeability induced by the up-regulation of VEGF gene expression via EPO (41) 2) the ongoing causative disease, of chronic nature, that was obviated by the ICG-CVA and the Basel investigation, responsible for overwhelming the gliosis-dependant capacity of resilience to hypoxia 3) a combination of both. I/R seemed excluded: EPO precisely mimics hypoxic reconditioning as shown in over ten years publications, including in the retina (20), and as EPO therapy is part of the current strategy for stabilization of the endothelial glycocalix against I/R injury (42-43). An additional and not exclusive possible explanation was the potential antagonist action of EPO on GFAP astrocytes proliferation, as mentioned in the introduction (18), that might have counteracted the reactive protective hypertrophic gliosis, still fully operative prior to EPO injection, and that was eventually restored during the follow-up, where epiretinal hyperreflectivity without ME and ongoing chronic ischemia do coincide (Fig. 6 and video 6), as much as it is unlikely that EPO’s effect would exceed one month (cf infra). Inhibition of gliosis by EPO IVI might have been also part of the mechanism of rescue of RGG, compromised by gliosis in hypoxic conditions (44). Whatever the complex balance initially reached, then overwhelmed after EPO IVI 1, the challenge was rapidly overcome by the second EPO IVI without anti-VEGF injection, likely because the former was powerful enough to restore the threshold limit for resilience to hypoxia, that seemed no longer reached again during the relapse-free follow-up. Of note, this “epiretinal membrane “, which association to good vision is a proof of concept of its protective effect, must not be removed surgically, as it would suppress one of the mecanisms of resilience to hypoxia.
To our best knowledge, ICG-CVA was never reported in FS; it allows real time evaluation of the ocular perfusion and illustration of the universal rheological laws that control choroidal blood flow as well. Pachyveins recall a “reverse” veno-arteriolar reflex in the choroidal circulation, that is NO and autonomous nervous system-dependant, and that we suggested to be an adaptative choroidal microcirculation process to hypoxia (45). Their persistence during follow-up accounts for a persisting state of chronic ischemia.
The optimal timing for reperfusion via rhEPO in a non resolved issue:
in the case reported by Luscan and Roche, rhEPO IVI was performed on the very same day of disease onset, where it induced complete recovery from VA reduced at counting fingers at 1 meter, within 48 hours. This clinical human finding is on line with a recent rodent stroke study that established the timings for non lethal versus lethal ischemia of the neural and vascular lineages, and the optimized ones for beneficial reperfusion: the acute phase - from Day 1 where endothelial and neural cells are still preserved, to Day 7 where proliferation of pericytes and Progenitor Stem Cells are obtainable - and the chronic stage, up to Day 56, where vasculogenesis, neurogenesis and functional recovery are still possible, but with uncertain efficiency (46). In our particular case, PR rescue after rhEPO IVI 1 indicated that Week 3 was still timely. RhEPO IVI efficacy was shown to last between one (restoration of the BRB) and four weeks (antiapoptotic effect) in diabetic rats (24). The relapse after Week 3 post IVI 1 might indicate that it might be approximately the interval to be followed, should repeated injections be necessary.
The bilateral chronic perfusion defects on OCT-A at last follow-up indicate that both eyes remain in a condition of chronic ischemia and I/R, where endogenous EPO provides efficient ischemic pre-conditioning, but is potentially susceptible to be challenged during episodes of acute hypoxia that overwhelm the resilience threshold.
CONCLUSION
The present case advocates for individualized medicine with careful recording of the medical history, investigation of the systemic context, and exploiting of the available retinal multimodal imaging for accurate analytical interpretation of retinal diseases and their complex pathophysiology. The Flammer Syndrome is unfortunately overlooked in case of RVO; it should be suspected clinically in case of absence of the usual vascular and metabolic context, and in case of elevated RVP. RhEPO therapy is able to restore the beneficial endogenous EPO ischemic pre-conditioning in eyes submitted to challenging acute hypoxia episodes in addition to chronic ischemic stress, as in the Flammer Syndrome and fluctuating ocular blood flow, when it becomes compromised by the overwhelming of the hypoxic stress resilience threshold. The latter physiopathological explanation illuminates the cases of RVO where anti-VEGF therapy proved functionally inefficient, and/or worsened retinal ischemia. RhEPO therapy might be applied to other chronic ischemia and I/R conditions, as non neo-vascular Age Macular Degeneration (AMD), and actually EPO was listed in 2020 among the nineteen promising molecules in AMD in a pooling of four thousands (47).
For more information regarding our Journal: https://jmedcasereportsimages.org/about-us/
For more artices: https://jmedcasereportsimages.org/archive/
0 notes
Text
Mr. Fenton is a competent teacher. Almost too competent.
If Mr. Daniel Fenton had any more than a BS (with a minor in education), Tim would’ve flagged his profile as a potential Rogue. That’s the way of most charismatic academics, at least in Gotham. (Got a PhD? Instant watchlist.) Instead, he’s Gotham Academy’s newest celebrity, as a young, passionate, out-of-towner substitute while the chemistry teacher’s on maternity leave.
Tim gets the hype. Fenton seems to genuinely love teaching, and is invested in the welfare of the student body. He hands out bananas during exam week, hosts a “study habits seminar” each month to coach effective learning strategies, and the third time Tim falls asleep in his class, he even pulls Tim aside to ask if he’s doing okay. With all the late work he accepts and the protein bars he sneaks Tim, he’s every teen vigilante’s dream teacher. He could’ve been Tim’s favorite.
In fact, Mr. Fenton was Tim’s favorite. Up until Tim walks into Mr. Fenton’s chemistry classroom for a forgotten textbook, an hour after the final bell.
On the board where tallied scores for today’s review game had been kept, “THE CHEMISTRY BEHIND DR. CRANE’S FEAR GAS: ANXIOGENICS, NERI’S, & YOU,” is now scrawled. A detailed diagram of the human endocrine system projects in front of a small crowd of adoring and attentive students.
Fenton is wrist-deep in the skull cavity of an anatomical model. A short tug, and out pops the brain.
It’s plastic. It’s fake.
Tim identifies the nearest emergency exit.
Fenton turns to the door, and in the dark classroom with the projector illuminating half his face, his eyes almost seem to flash red. “What’s up, Tim?” he asks. His friendly grin is too big for his face. “I didn’t know you wanted to join the Just Science League!”
[OR: Danny’s a science teacher at Tim’s school. Gotham’s a pretty wild place, even for someone who grew up a superhero in a ghost-infested town, so he takes it upon himself to start a club teaching kids how to manage themselves in the event of a crisis. These Gothamites are pretty hardy, but a little extra training never hurt anybody! And he suspects one of his students might be a teen vigilante, like he’d been, back in the day. As a senior super, it's Danny’s duty look out for him! Surely, this is the subtlest and most appropriate way to give the kid pointers.]
[Tim immediately assumes supervillain.]
#Danny can’t help being creepy it’s just the way he’s built!!#I like to think Lancer did these things for Danny when he was in HS#and now Danny's emulating Lancer :)#Passing it on!#Tim is paranoid but also like he is SO CLOSE to graduating so like. Does he even want to report this shit to Batman. What if the next chem#teacher's a jerk and Tim fails the class and he never gets his stupid diploma. Bruce already is insisting he finish out HS and maybe get#an ABA before he's allowed back into the company#and Jesus Christ does Tim hate school. He'll worry about Mr. Fenton's burgeoning army of Science Honor Society Rogues on his own time#dcxdp#dpxdc#prompt#tim drake#danny fenton#in case I write more of this let’s tag it uhhhhh#misunderstood mentor au#kipwrite
7K notes
·
View notes
Text








END OF CHAPTER ONE
FORGETTABLE-AU (Page 65-72)
* Time to put this puzzle together.
[BEGINNING] [PREVIOUS] [CONTINUE]
#long post#SO SORRY FOR THE POST BEING SO LONG BUT I NEEDED THE DRAMA AND YOU GUYS BEING LIKE#“why is it still going.....”#hehe#JOKES ON YOU! I LIED! THESE ARE 8 PAGES NOT 6!!!#yippiee#YOU GOT EVEN MORE#OKAY NOW#To address everything!!!#“time travel? Really?”#YES REALLY#HAVE YOU ALL SEEN WHAT SANS SAYS IN HIS BATTLE#“our reports” “timelines jumping left and right” “an anomaly in the time-space continuum” HE KNOWS ABOUT THAT STUFF#HE RESEARCHED THAT STUFF#HE HAS A SECRET CODEWORD READY IN CASE HE FINDS A TIME TRAVELER WHY WOULD HE HAVE THAT???#Alphys has researched alternate universes too(which are usually related to alternate timelines)#okay enough of me rambling#I told u guys I made a mess to make the undertale timeline make sense lol#ANYWAYYSS#SIGH finally done with chapter one#IT WAS 52 PAGES LONG!!!!#So many things happened here#PAPYRUS AND FLOWEY ARE BACK!!!!#see you all again soon with chapter TWO#forgettable-au#forgettable-au-comic#papyrus#papyrus is gaster#undertale#gaster
1K notes
·
View notes
Text
Clinical Imaging Journal PubMed
Clinical Imaging Journal PubMed is a peer-reviewed high impact factor PubMed indexed Clinical Imaging Journal established Internationally which provides a platform to publish Clinical Images, Medical Case Reports, Clinical Case Reports, Case Series (series of 2 to 6 cases) and Clinical Videos in Medicine.
Journal Homepage: https://www.literaturepublishers.org/
Clinical Imaging Journal is an open access peer-reviewed Clinical Imaging Journal committed to publishing high-quality articles in the field of Imaging Science. Clinical Imaging Journal aims to present Imaging Science and relevant clinical information in an understandable and useful format. Clinical Imaging Journal is owned and published by the Scientific Scholar. Audience Our audience includes Radiologists, Researchers, Clinicians, medical professionals and students. Review process Clinical Imaging Journal has a highly rigorous peer-review process that makes sure that manuscripts are scientifically accurate, relevant, novel and important. Authors disclose all conflicts, affiliations and financial associations such that the published content is not biased.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
0 notes
Text

every so often i have to relearn how to draw yuuji or he starts fighting me
#my art#jujutsu kaisen#jjk#itadori yuuji#yuji itadori#fanart#jjk fanart#jujutsu kaisen fanart#yuuji#ryomen sukuna#sukuna#i love drawing sukuna as the teeniest tiniest eye on yuuji's face n using it as an excuse 2 use his tag <3 ths his Rent#anyway he fought a bit at first but would u believe it i got yuuji 2 cooperate fr a draws pls clap#maybe it's just when hes in a piece with megumi that he gets an attitude??? whatever th case im happy w all of these thank god#beef w yuuji Settled fr now . until he inevitably decides 2 fight me again sighs#in the meantime !!! had SO much fun drawing his new scars#happy 2 report tht ive fully come around on yuuji 1eye itadori i wasnt sure at first but now i love it fr him#i love the texture of it i love splitting his eyebrow n drawing the scar tissue up Through the remaining hair....#i love him looking like he's winking i love drawing the lil X on his chibi#its GOOD#i dont think ill give him a fake eye very often if at all but it was fun putting him in tokyo ghoul cosplay fr this#o ya speaking of his Accessories the slippers started out as tigers also but then i wanted them bunnies and i saw an opportunity#so now miku is haunting this draws and my yuuji owns a pair of deco27 rabbit hole slippers#now that i rly look at it that whole fit is such a look actually im crying#we got beef shirt...#@ me @ sukuna @ the fact tht yuuji is Jacked#10/10 triple entendre 10/10 would wear
1K notes
·
View notes
Photo
Visit us: https://www.literaturepublishers.org/journal/case-report-in-otolaryngology-ent.html
Looking for an informative and engaging way to stay up-to-date on the latest advances in otolaryngology? Look no further than our collection of case reports!
Our case reports provide in-depth analysis of real-world cases from experienced otolaryngologists, giving you a unique perspective on the latest diagnostic and treatment techniques in the field. From hearing loss to sinusitis to throat cancer and beyond, our case reports cover a wide range of topics, giving you valuable insights into the latest approaches to diagnosis, treatment, and patient care.
Whether you're a practicing otolaryngologist looking to stay on the cutting edge of your field or a medical student looking to expand your knowledge, our case reports are an invaluable resource. With detailed analysis, expert commentary, and real-world examples, our case reports will help you stay informed and engaged, no matter what your level of experience.
So why wait? Sign up for our case report subscription today and start exploring the latest advances in otolaryngology!
If you looking for Case Reports in Otolaryngology contact or visit us!
Contact us: +447588268983
#case reports#otolaryngology case reports#case reports in otolaryngology#casereportsinOtolaryngology#Case Reports in Otolaryngology Journal#Journal of Otolaryngology Case Reports
0 notes
Text

Mind yo own business, Harvey!
(are those open-plan cells really the best idea?)
#my art#sketchy sketch#very quick sketch#I had the idea and had to doodle it#Jim is hitting himself with a big pile of case reports in the background#nygmobblepot#riddlebird#gotham#gotham tv#oswald cobblepot#edward nygma#harvey bullock#after this they're not allowed in the same cell#or cells next to each other
940 notes
·
View notes
Text
another misunderstandings au
Vlad goes slowly insane in space after Phantom Planet. He's finally snapped and is completely willing to kill both Jack and Maddie to get Danny where he wants him. He doesn't stay in space, eventually returning to the Zone and setting up shop in another dimension (DC Bludhaven; becoming a shady businessman once again) while keeping an eye on Danny.
Danny is having a great time. His family accepts him, he's a known hero, he's almost an adult. Sure, Dani destablized, but with his parents help he managed to save her! ...As a toddler. Then Clockwork dropped a deaged evil future self (as a baby) for him to raise. So it's not all great.
Then Vlad attacks. Everyone who Danny knows dies except for little Dani and Dan, and Vlad kidnaps him to a new dimension, where no one can help him. I can see Vlad not really recognizing the members of this new dimension as real and therefore, not a real threat. Danny is trapped in the penthouse bc of a ghost shield specific to his ecto-signature and forced to play house with an extremely unstable vlad who's willing to threaten the babies in order to force him to comply.
Then Vlad goes missing and Dick Grayson is assigned to the case
#dp x dc#dc x dp#dcxdp#dpxdc#c: danny fenton#c: vlad masters#c: dan phantom#c: dani phantom#c: dick grayson#mom danny#death defying#at least that's the plan#misunderstandings au#vlad's employees report him missing#danny's forged identity has him as vlad's son and heir#so dick thinks this is an easy case of a kid bumping off the parent for the inheritance#until he overhears Dani calling Danny mama and refers to Vlad as papa#and Danny reveals that he can't go down to the station because if he goes through the door it electrocutes him
693 notes
·
View notes
Text

#angry feminist#feminicide#especially tough week#I’m French tho I’m following the trial of the husband & 51 (they could identified on the videos they’re much more)#and what they’re saying to justify themselves (like « the husband gave consent or I thought she was just asleep) make me SICK and what men#are commenting online about this case like they don’t buy it and the classic Not All Men 🙄🤬🤢#the husband said that only 3 out of 10 men refused (and none reported it) to come r*pe his unconscious wife..#men from all ages professions one was a neighbour one had HIV and went back multiple times 🤬🤢 lots have wives & kids some had previous#r*pe convictions (one against in own daughter) and lots were caught with possession of child p*#your boyfriend your friend your ex your husband your relative your neighbor your doctor your teacher…#we’re never safe#I’m so tired but still ENRAGED#feminism#femicide#misogyny#crimes against women#violence against women
449 notes
·
View notes
Text
"Reviewers told the report’s authors that AI summaries often missed emphasis, nuance and context; included incorrect information or missed relevant information; and sometimes focused on auxiliary points or introduced irrelevant information. Three of the five reviewers said they guessed that they were reviewing AI content.
The reviewers’ overall feedback was that they felt AI summaries may be counterproductive and create further work because of the need to fact-check and refer to original submissions which communicated the message better and more concisely."
Fascinating (the full report is linked in the article). I've seen this kind of summarization being touted as a potential use of LLMs that's given a lot more credibility than more generative prompts. But a major theme of the assessors was that the LLM summaries missed nuance and context that made them effectively useless as summaries. (ex: “The summary does not highlight [FIRM]’s central point…”)
The report emphasizes that better prompting can produce better results, and that new models are likely to improve the capabilities, but I must admit serious skepticism. To put it bluntly, I've seen enough law students try to summarize court rulings to say with confidence that in order to reliably summarize something, you must understand it. A clever reader who is good at pattern recognition can often put together a good-enough summary without really understanding the case, just by skimming the case and grabbing and repeating the bits that look important. And this will work...a lot of the time. Until it really, really doesn't. And those cases where the skim-and-grab method won't work aren't obvious from the outside. And I just don't see a path forward right now for the LLMs to do anything other than skim-and-grab.
Moreover, something that isn't even mentioned in the test is the absence of possibility of follow up. If a human has summarized a document for me and I don't understand something, I can go to the human and say, "hey, what's up with this?" It may be faster and easier than reading the original doc myself, or they can point me to the place in the doc that lead them to a conclusion, or I can even expand my understanding by seeing an interpretation that isn't intuitive to me. I can't do that with an LLM. And again, I can't really see a path forward no matter how advanced the programing is, because the LLM can't actually think.
#ai bs#though to be fair I don't think this is bs#just misguided#and I think there are other use-cases for LLMs#but#I'm really not sold on this one#if anything I think the report oversold the LLM#compared to the comments by the assessors
552 notes
·
View notes
Text
Our ex landlord owes us 3 times the security deposit we paid him lmaooooo get FUCKED💥💥💥💥💥💥💥💥💥💥💥💥💥
#this whole thing has been insane but lmao we won#we're also filing a libel case + reporting him to the irs for tax fraud#that he sent us evidence of for some reason ? so#lmao ! get fucked old man
421 notes
·
View notes
Text
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
#literaturepublishers#Scopus Indexed Journals for Case Reports#case reports#clinical images#medicalcasereportsjournal#medical imaging#usa
0 notes
Text
“he was mentally ill. this monster was a- was a sick fantasy. a product of his dementia.”
“…i saw it too. does that make me disturbed? demented? does… that make me sick too?”
#txf#the x files#dana scully#fox mulder#folie a deux#this episode … this EPISODE!!!!!!#genuinely so indicative of how much they trust each other….#between mulder just . having to rely on scully for the last part of the ep#scully thinking he’s off his fucking rocker and still looking into what he asks her to look into bc she TRUSTS him . bc she LOVES him !!!!#and maybe he’s a little nuts but goddamnit she will at least check it out !! just in case he’s right!!!#AND she lies for him all the time . i mean she always does this whenever he decides to go nuts But specifically in this ep…#looks skinner in the eye and goes . yea man im totally fully with mulder on this . and he’s definitely not being weird and i definitely kno#what’s going on with him#she lies for mulder all the time its soooo…#anyways . drawing wise this drove me nuts i hate drawing mulder . he’s so hard for me to draw#they’re kinda kirie and shuichi coded in the bottom part but . well . why not . might as well be#ALSOOO i chose that quote for the bottom bc . well . does she think he’s crazy? like actually for real?#i feel like every time scully talks about mulder (up to season five at least as thats where im at) its contained in some way?#in her reports . to family . to skinner . to mulder !#i think the only time she’s Really honest is in the confessional but even then…#bc its not like she’s against speaking her mind . i mean generally and situational but for ppl she’s close to she usually isnt#but when it comes to mulder it always feels contained and like she’s making excuses for him (he is always her exception .#llike whenevrr he gets some disease or affliction or whatever she ALWAYS jumps to going ‘but well… sometimes there’s this excuse’ and she#does this w a lot considering shes science focused but w mulder shes always like . well he ISNT crazy because uhhhh .#this hyperspecific scenario that is in no fuckin way the case)#but does she think he’s crazy? does HE think she thinks he’s crazy?#is he asking about this specific case or is he asking in general? over the entirety of the show?#its been five years scully. is he crazy? sick? demented?#has this all been a sick fantasy fueled by mental illness? youre the doctor scully . surely you have the answer?#anyways i dont think she knows . and if that is the case — what does that mean for her?
177 notes
·
View notes
Text
i just read an article and apparently jonathan kaplan (who played jason in the falsettos obc and was 11 at the time), watched his voice teacher who helped him through the show's auditions decline and eventually die from aids related illness during the show's previews.
in this same article michael rupert mentioned how there would be patients who came and saw the show and would go to the stage door just to be near the performers and tell them how much the story meant to them.
one day, heather macrae (charlotte) attended the funeral of her friend paul jabra and immediately after went straight to the theatre to perform in the evening show.
stephen bogardus recalls leaving the theatre and walking through the audience (about 15 minutes after the show had finished) and people would still be there holding each other.
#i feel like what can be so easy to forget is that even though falsettos was on broadway in 1992 which is over 10 years after#the first cases of aids were reported it was only in 1992/93 that the epidemic was reaching its peak#like it was at its worst when falsettos was playing 8 shows a week#i don't know how they did it#mentally and emotionally#falsettos#falsettos obc
696 notes
·
View notes