#Caremark
Explore tagged Tumblr posts
Text
What the fuck is a PBM?
TOMORROW (Sept 24), I'll be speaking IN PERSON at the BOSTON PUBLIC LIBRARY!

Terminal-stage capitalism owes its long senescence to its many defensive mechanisms, and it's only by defeating these that we can put it out of its misery. "The Shield of Boringness" is one of the necrocapitalist's most effective defenses, so it behooves us to attack it head-on.
The Shield of Boringness is Dana Claire's extremely useful term for anything so dull that you simply can't hold any conception of it in your mind for any length of time. In the finance sector, they call this "MEGO," which stands for "My Eyes Glaze Over," a term of art for financial arrangements made so performatively complex that only the most exquisitely melted brain-geniuses can hope to unravel their spaghetti logic. The rest of us are meant to simply heft those thick, dense prospectuses in two hands, shrug, and assume, "a pile of shit this big must have a pony under it."
MEGO and its Shield of Boringness are key to all of terminal-stage capitalism's stupidest scams. Cloaking obvious swindles in a lot of complex language and Byzantine payment schemes can make them seem respectable just long enough for the scammers to relieve you of all your inconvenient cash and assets, though, eventually, you're bound to notice that something is missing.
If you spent the years leading up to the Great Financial Crisis baffled by "CDOs," "synthetic CDOs," "ARMs" and other swindler nonsense, you experienced the Shield of Boringness. If you bet your house and/or your retirement savings on these things, you experienced MEGO. If, after the bubble popped, you finally came to understand that these "exotic financial instruments" were just scams, you experienced Stein's Law ("anything that can't go forever eventually stops"). If today you no longer remember what a CDO is, you are once again experiencing the Shield of Boringness.
As bad as 2008 was, it wasn't even close to the end of terminal stage capitalism. The market has soldiered on, with complex swindles like carbon offset trading, metaverse, cryptocurrency, financialized solar installation, and (of course) AI. In addition to these new swindles, we're still playing the hits, finding new ways to make the worst scams of the 2000s even worse.
That brings me to the American health industry, and the absurdly complex, ridiculously corrupt Pharmacy Benefit Managers (PBMs), a pathology that has only metastasized since 2008.
On at least 20 separate occasions, I have taken it upon myself to figure out how the PBM swindle works, and nevertheless, every time they come up, I have to go back and figure it out again, because PBMs have the most powerful Shield of Boringness out of the whole Monster Manual of terminal-stage capitalism's trash mobs.
PBMs are back in the news because the FTC is now suing the largest of these for their role in ripping off diabetics with sky-high insulin prices. This has kicked off a fresh round of "what the fuck is a PBM, anyway?" explainers of extremely variable quality. Unsurprisingly, the best of these comes from Matt Stoller:
https://www.thebignewsletter.com/p/monopoly-round-up-lina-khan-pharma
Stoller starts by pointing out that Americans have a proud tradition of getting phucked by pharma companies. As far back as the 1950s, Tennessee Senator Estes Kefauver was holding hearings on the scams that pharma companies were using to ensure that Americans paid more for their pills than virtually anyone else in the world.
But since the 2010s, Americans have found themselves paying eye-popping, sky-high, ridiculous drug prices. Eli Lilly's Humolog insulin sold for $21 in 1999; by 2017, the price was $274 – a 1,200% increase! This isn't your grampa's price gouging!
Where do these absurd prices come from? The story starts in the 2000s, when the GW Bush administration encouraged health insurers to create "high deductible" plans, where patients were expected to pay out of pocket for receiving care, until they hit a multi-thousand-dollar threshold, and then their insurance would kick in. Along with "co-pays" and other junk fees, these deductibles were called "cost sharing," and they were sold as a way to prevent the "abuse" of the health care system.
The economists who crafted terminal-stage capitalism's intellectual rationalizations claimed the reason Americans paid so much more for health care than their socialized-medicine using cousins in the rest of the world had nothing to do with the fact that America treats health as a source of profits, while the rest of the world treats health as a human right.
No, the actual root of America's health industry's problems was the moral defects of Americans. Because insured Americans could just go see the doctor whenever they felt like it, they had no incentive to minimize their use of the system. Any time one of these unhinged hypochondriacs got a little sniffle, they could treat themselves to a doctor's visit, enjoying those waiting-room magazines and the pleasure of arranging a sick day with HR, without bearing any of the true costs:
https://pluralistic.net/2021/06/27/the-doctrine-of-moral-hazard/
"Cost sharing" was supposed to create "skin in the game" for every insured American, creating a little pain-point that stung you every time you thought about treating yourself to a luxurious doctor's visit. Now, these payments bit hardest on the poorest workers, because if you're making minimum wage, at $10 co-pay hurts a lot more than it does if you're making six figures. What's more, VPs and the C-suite were offered "gold-plated" plans with low/no deductibles or co-pays, because executives understand the value of a dollar in the way that mere working slobs can't ever hope to comprehend. They can be trusted to only use the doctor when it's truly warranted.
So now you have these high-deductible plans creeping into every workplace. Then along comes Obama and the Affordable Care Act, a compromise that maintains health care as a for-profit enterprise (still not a human right!) but seeks to create universal coverage by requiring every American to buy a plan, requiring insurers to offer plans to every American, and uses public money to subsidize the for-profit health industry to glue it together.
Predictably, the cheapest insurance offered on the Obamacare exchanges – and ultimately, by employers – had sky-high deductibles and co-pays. That way, insurers could pocket a fat public subsidy, offer an "insurance" plan that was cheap enough for even the most marginally employed people to afford, but still offer no coverage until their customers had spent thousands of dollars out-of-pocket in a given year.
That's the background: GWB created high-deductible plans, Obama supercharged them. Keep that in your mind as we go through the MEGO procedures of the PBM sector.
Your insurer has a list of drugs they'll cover, called the "formulary." The formulary also specifies how much the insurance company is willing to pay your pharmacist for these drugs. Creating the formulary and paying pharmacies for dispensing drugs is a lot of tedious work, and insurance outsources this to third parties, called – wait for it – Pharmacy Benefits Managers.
The prices in the formulary the PBM prepares for your insurance company are called the "list prices." These are meant to represent the "sticker price" of the drug, what a pharmacist would charge you if you wandered in off the street with no insurance, but somehow in possession of a valid prescription.
But, as Stoller writes, these "list prices" aren't actually ever charged to anyone. The list price is like the "full price" on the pricetags at a discount furniture place where everything is always "on sale" at 50% off – and whose semi-disposable sofas and balsa-wood dining room chairs are never actually sold at full price.
One theoretical advantage of a PBM is that it can get lower prices because it bargains for all the people in a given insurer's plan. If you're the pharma giant Sanofi and you want your Lantus insulin to be available to any of the people who must use OptumRX's formulary, you have to convince OptumRX to include you in that formulary.
OptumRX – like all PBMs – demands "rebates" from pharma companies if they want to be included in the formulary. On its face, this is similar to the practices of, say, NICE – the UK agency that bargains for medicine on behalf of the NHS, which also bargains with pharma companies for access to everyone in the UK and gets very good deals as a result.
But OptumRX doesn't bargain for a lower list price. They bargain for a bigger rebate. That means that the "price" is still very high, but OptumRX ends up paying a tiny fraction of it, thanks to that rebate. In the OptumRX formulary, Lantus insulin lists for $403. But Sanofi, who make Lantus, rebate $339 of that to OptumRX, leaving just $64 for Lantus.
Here's where the scam hits. Your insurer charges you a deductible based on the list price – $404 – not on the $64 that OptumRX actually pays for your insulin. If you're in a high-deductible plan and you haven't met your cap yet, you're going to pay $404 for your insulin, even though the actual price for it is $64.
Now, you'd think that your insurer would put a stop to this. They chose the PBM, the PBM is ripping off their customers, so it's their job to smack the PBM around and make it cut this shit out. So why would the insurers tolerate this nonsense?
Here's why: the PBMs are divisions of the big health insurance companies. Unitedhealth owns OptumRx; Aetna owns Caremark, and Cigna owns Expressscripts. So it's not the PBM that's ripping you off, it's your own insurance company. They're not just making you pay for drugs that you're supposedly covered for – they're pocketing the deductible you pay for those drugs.
Now, there's one more entity with power over the PBM that you'd hope would step in on your behalf: your boss. After all, your employer is the entity that actually chooses the insurer and negotiates with them on your behalf. Your boss is in the driver's seat; you're just along for the ride.
It would be pretty funny if the answer to this was that the health insurance company bought your employer, too, and so your boss, the PBM and the insurer were all the same guy, busily swapping hats, paying for a call center full of tormented drones who each have three phones on their desks: one labeled "insurer"; the second, "PBM" and the final one "HR."
But no, the insurers haven't bought out the company you work for (yet). Rather, they've bought off your boss – they're sharing kickbacks with your employer for all the deductibles and co-pays you're being suckered into paying. There's so much money (your money) sloshing around in the PBM scamoverse that anytime someone might get in the way of you being ripped off, they just get cut in for a share of the loot.
That is how the PBM scam works: they're fronts for health insurers who exploit the existence of high-deductible plans in order to get huge kickbacks from pharma makers, and massive fees from you. They split the loot with your boss, whose payout goes up when you get screwed harder.
But wait, there's more! After all, Big Pharma isn't some kind of easily pushed-around weakling. They're big. Why don't they push back against these massive rebates? Because they can afford to pay bribes and smaller companies making cheaper drugs can't. Whether it's a little biotech upstart with a cheaper molecule, or a generics maker who's producing drugs at a fraction of the list price, they just don't have the giant cash reserves it takes to buy their way into the PBMs' formularies. Doubtless, the Big Pharma companies would prefer to pay smaller kickbacks, but from Big Pharma's perspective, the optimum amount of bribes extracted by a PBM isn't zero – far from it. For Big Pharma, the optimal number is one cent higher than "the maximum amount of bribes that a smaller company can afford."
The purpose of a system is what it does. The PBM system makes sure that Americans only have access to the most expensive drugs, and that they pay the highest possible prices for them, and this enriches both insurance companies and employers, while protecting the Big Pharma cartel from upstarts.
Which is why the FTC is suing the PBMs for price-fixing. As Stoller points out, they're using their powers under Section 5 of the FTC Act here, which allows them to shut down "unfair methods of competition":
https://pluralistic.net/2023/01/10/the-courage-to-govern/#whos-in-charge
The case will be adjudicated by an administrative law judge, in a process that's much faster than a federal court case. Once the FTC proves that the PBM scam is illegal when applied to insulin, they'll have a much easier time attacking the scam when it comes to every other drug (the insulin scam has just about run its course, with federally mandated $35 insulin coming online, just as a generation of post-insulin diabetes treatments hit the market).
Obviously the PBMs aren't taking this lying down. Cigna/Expressscripts has actually sued the FTC for libel over the market study it conducted, in which the agency described in pitiless, factual detail how Cigna was ripping us all off. The case is being fought by a low-level Reagan-era monster named Rick Rule, whom Stoller characterizes as a guy who "hangs around in bars and picks up lonely multi-national corporations" (!!).

The libel claim is a nonstarter, but it's still wild. It's like one of those movies where they want to show you how bad the cockroaches are, so there's a bit where the exterminator shows up and the roaches form a chorus line and do a kind of Busby Berkeley number:
https://www.46brooklyn.com/news/2024-09-20-the-carlton-report
So here we are: the FTC has set out to euthanize some rentiers, ridding the world of a layer of useless economic middlemen whose sole reason for existing is to make pharmaceuticals as expensive as possible, by colluding with the pharma cartel, the insurance cartel and your boss. This conspiracy exists in plain sight, hidden by the Shield of Boringness. If I've done my job, you now understand how this MEGO scam works – and if you forget all that ten minutes later (as is likely, given the nature of MEGO), that's OK: just remember that this thing is a giant fucking scam, and if you ever need to refresh yourself on the details, you can always re-read this post.

The paperback edition of The Lost Cause, my nationally bestselling, hopeful solarpunk novel is out this month!

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/09/23/shield-of-boringness/#some-men-rob-you-with-a-fountain-pen

Image: Flying Logos (modified) https://commons.wikimedia.org/wiki/File:Over_$1,000,000_dollars_in_USD_$100_bill_stacks.png
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
#pluralistic#matthew stoller#pbms#pharmacy benefit managers#cigna#ftc#antitrust#intermediaries#bribery#corruption#pharma#monopolies#shield of boringness#Caremark#Express Scripts#OptumRx#insulin#gbw#george w bush#co-pays#obamacare#aca#rick rules#guillotine watch#euthanize rentiers#mego
446 notes
·
View notes
Text
I know this is a controversial take considering recent events, and considering the number of leftists I follow on this hellsite, but guess what? I don't think you should kill people just because they are part of a horrid industry that exploits people! I also feel like if you do kill a CEO in an exploitative industry you should be prosecuted for it and pay the full penalty the law allows for it!
This does not make me a conservative, or a bootlicker, or any other terms some of your tankie style leftists would call me. This makes me a civilized human being! This just means I think killing people, no matter who they are, is wrong.
Now, is this to say there aren't certain people in this world [looking at you Donald Trump] whose graves I wouldn't piss on when some horrid disease or old age catches up with them? Oh Hell no. I just wouldn't dirty myself by doing the deed with my own hands. We are better than this, people! Karma most of the time catches up with the most evil of them.
4 notes
·
View notes
Text
Providing Compassionate Care: A Look into Caremark Liverpool, Your Trusted Care Agency in Liverpool
In a bustling city like Liverpool, where life moves at a fast pace, there arises a need for compassionate care services to support individuals in various stages of life. This is where Caremark Liverpool shines as a beacon of reliability and compassion in the realm of caregiving.
Introduction:
Care Agency Liverpool: Meeting the Needs of the Community
As one of the leading care agency in Liverpool, Caremark Liverpool stands out for its unwavering commitment to providing high-quality care services tailored to the unique needs of each individual.
Dedicated Caregivers:
At the heart of Caremark Liverpool are its dedicated caregivers who go above and beyond to ensure the well-being and comfort of their clients. Trained extensively in caregiving techniques and equipped with empathy and compassion, our caregivers form meaningful connections with those under their care.
Comprehensive Services:
From elderly care to disability support and everything in between, Caremark Liverpool offers a comprehensive range of services designed to meet the diverse needs of the community. Whether it's assistance with daily tasks, companionship, or specialized care, our team is here to provide support every step of the way.
Tailored Care Plans:
Recognizing that each individual has unique requirements, Caremark Liverpool takes a personalized approach to care planning. Our team works closely with clients and their families to develop tailored care plans that prioritize comfort, dignity, and independence.
Conclusion:
Choose Caremark Liverpool for Compassionate Care You Can TrustWhen it comes to finding a reliable care agency in Liverpool, look no further than Caremark Liverpool. With a team of dedicated caregivers, comprehensive services, and personalized care plans, we are committed to providing compassionate care that makes a difference in the lives of our clients. Trust Caremark Liverpool for all your caregiving needs.
0 notes
Text

Oh the rich are REAL scared
#Oh the rich are REAL scared#rich people#rich kids#rich#brian thompson#davidjoyner#david joyner#cvs health corp#cvs health#cvs caremark#karen s. lynch#karen lynch#cvs pharmacy#fuck cvs#cvs#fuck ceos#ceos#ceo#united healthcare#unitedhealth group inc#unitedhealthcare#uhc generations#uhc ceo#uhc lb#uhc#unitedhealthgroup#rest in piss#rest in pieces#rotinpiss#rot in hell
143 notes
·
View notes
Text
My insurance finally approved my biologic (that I’ve been taking for almost 10 years…)!
2 notes
·
View notes
Text
Working in healthcare reminds me on the daily that the US medical system is fucked up but a recent example that hasn't escaped my mind for weeks is that a patient with a new diagnosis for HIV was trying to get his medication... but his insurance rejected it and said that they don't cover any HIV meds
#it was also first line treatment too#doctor had to write a letter and everything#and i think they still didnt cover it cause they had to get samples or something so the patient could get something treat his hiv#idk how that is even legal#no one can convince me that private insurance is good when shit like this happens#also saw a doctor talk about how he had to do a prior auth for Lisinopril#Lisinopril... cheap ass drug that is used like crazy#also dont get cvs caremark
10 notes
·
View notes
Text
So today I want to talk about puberty blockers for transgender kids, because despite being cisgender, this is a subject I’m actually well-versed in. Specifically, I want to talk about how far backwards things have gone.
This story starts almost 20 years ago, and it’s kind of long, but I think it’s important to give you the full history. At the time, I was working as an administrative assistant for a pediatric endocrinologist in a red state. Not a deep deep red state like Alabama, we had a little bit of a purple trend, but still very much red. (I don’t want to say the state at the risk of doxxing myself.) And I took a phone call from a woman who said, “My son is transgender. Does your doctor do hormone therapy?”
I said, “Good question! Let me find out.”
I went into the back and found the doctor playing Solitaire on his computer and said, “Do you do hormone therapy for transgender kids?” It had literally never come up before. He had opened his practice there in the early 2000s. This was roughly 2006, and the first time someone asked. Without looking up from his game of Solitaire, the doctor said, “I’ve never done it before, but I know how it works, so sure.”
I got back on the phone and told the mom, who was overjoyed, and scheduled an appointment for her son. He was the first transgender child we treated with puberty blockers. But not, by far, the first child we treated with puberty blockers, period. Because puberty blockers are used very commonly for children with precocious puberty (early-onset puberty). I would say about twenty percent of the kids our doctor treated were for precocious puberty and were on puberty blockers. They have been well studied and are widely used, safe, and effective.
Well. It turned out, the doctor I worked for was the only doctor in the state who was willing to do this. And word spread pretty fast in the tight-knit community of ‘parents of transgender children in a red state’. We started seeing more kids. A better drug came out. We saw some kids who were at the age where they were past puberty, and prescribed them estrogen or testosterone. Our doctor became, I’m fairly sure, a small folk hero to this community.
Insurance coverage was a struggle. I remember copying articles and pages out of the Endocrine Society Manual to submit with prior authorization requests for the medications. Insurance coverage was a struggle for a lot of what we did, though. Growth hormone for kids with severe idiopathic short stature. Insulin pumps, which weren’t as common at the time, and then continuous glucose monitoring, when that came out. Insurance struggles were just part and parcel of the job.
I remember vividly when CVS Caremark, a pharmaceutical management company, changed their criteria and included gender dysphoria as a covered diagnosis for puberty blockers. I thought they had put the option on the questionnaire to trigger an automatic denial. But no - it triggered an approval. Medicaid started to cover it. I got so good at getting approvals with my by then tidy packet of articles and documentation that I actually had people in other states calling me to see what I was submitting (the pharmaceutical rep gave them my number because they wanted more people on their drug, which, shady, but sure. He did ask me if it was okay first).
And here’s the key point of this story:
At no point, during any of this, did it ever even occur to any of us that we might have to worry about whether or not what we were doing was legal.
It just never even came up. It was the medically recommended treatment so we did it. And seeing what’s happening in the UK and certain states in America is both terrifying and genuinely shocking to me, as someone who did this for almost fifteen years, without ever even wondering about the legality of it.
The doctor retired some years ago, at which point there were two other doctors in the state who were willing to prescribe the medications for transgender kids. I truly think that he would still be working if nobody else had been willing to take those kids on as patients. He was, by the way, a white cisgender heterosexual Boomer. I remember when he was introduced to the concept of ‘genderfluid’ because one of our patients on HRT wanted to go off. He said ‘that’s so interesting!�� and immediately went to Google to learn more about it.
I watched these kids transform. I saw them come into the office the first time, sometimes anxious and uncertain, sometimes sullen and angry. I saw them come in the subsequent times, once they were on hormone therapy, how they gradually became happy and confident in themselves. I saw the smiles on their faces when I gave them a gender marker letter for the DMV. I heard them cheer when I called to tell them I’d gotten HRT approved by insurance and we were calling in a prescription. It was honestly amazing and I will always consider the work I did in that red state with those kids to be something I am incredibly proud of. I was honored to be a part of it.
When I see all this transgender backlash, it’s horrifying, because it was well on the way to become standard and accepted treatment. Insurances started to cover it. Other doctors were learning to prescribe it. And now … it’s fucking illegal? Like what the actual fuck. We have gone so far backwards that it makes me want to cry. I don’t know how to stop this slide. But I wrote this so people would understand exactly how steep the slide is.
40K notes
·
View notes
Text
instagram
0 notes
Text
When the medication that keeps me from being violently tachycardic while simply living goes from $0.00 to $70.00. ✨
#im very grateful that i have insurance#and that there are things like goodrx#and that the lady i spoke to at caremark looked through so many options for me#but that was a jarring number to see this morning in my auto refill notification#make the fact that my employer uses cvs caremark when we dont have a cvs pharmacy in our area make sense???
2 notes
·
View notes
Text
CVS Caremark® defines future of pharmacy benefit management
CVS Caremark pledges to accelerate transparency, drive to lowest net cost prescription drugs, strengthen pharmacy relations, and deliver the best clinical care in pharmacy WOONSOCKET, R.I. /PRNewswire/ — CVS Caremark®, the nation’s leading pharmacy benefit manager and a CVS Health® (NYSE: CVS) company, today announced a renewed pledge to American businesses, unions, and health plans — building…
0 notes
Text
caremark sucks my ass. fuck caremark and the horse it rode in on.
0 notes
Text
Anyone here suffer from sacroiliac joint pain? I’ve long suspected I have SI joint inflammation related to autoimmune stuff, and it’s gotten so bad recently, likely because my insurance is denying my biologic, so I’ve been without for too long now. It feels like my lower back is in a vice and about to break, so hard to get comfortable. Tylenol and heat are minimally helpful, and I’m not allowed to take NSAIDS. Stretching seemed to have made it worse?
I finally relented and took a free sample of Humira from my doctor to hold me over until this insurance thing is sorted out (I just feel like free samples should be reserved for people with financial difficulties, but I’m dying here). I hope it helps because this really sucks.
0 notes
Text
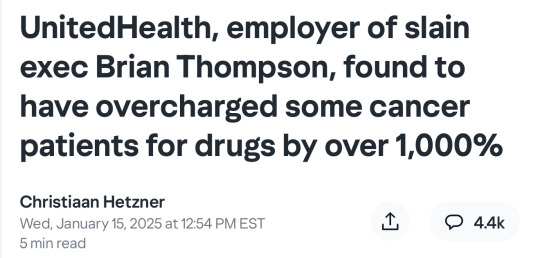

UnitedHealth Group is charging patients a markup for key life-saving drugs that could easily exceed their cost by a factor of ten or more, according to findings from the Federal Trade Commission.
The report, which levels the same allegations at CVS and Cigna, is the latest indictment of America’s broken healthcare system and comes on the heels of last month’s shocking murder of UnitedHealthcare CEO Brian Thompson.
The U.S. is notorious for incurring the highest costs per capita of any wealthy nation, yet failing to achieve an even remotely equivalent improvement in patient outcomes versus Europe’s social market-based economies.
Critics argue that is due largely to the highly opaque manner in which needless markups are hidden to conceal inefficiencies that serve various vested interests. These include, but are not limited to, the big three drug middlemen known as pharmacy benefit managers (PBMs).
According to the FTC report, UnitedHealth’s OptumRx, along with Cigna’s Express Scripts and CVS Caremark Rx, were able to collectively pocket $7.3 billion in added revenue above cost during the five year period of the study through 2022.
“The Big 3 PBMs marked up numerous specialty generic drugs dispensed at their affiliated pharmacies by thousands of percent, and many others by hundreds of percent,” it concluded.
A thousand percent increase in the price of a drug that costs $10 wholesale would result in a retail price of $110.
This markup rate applied to 22% of the specialty therapies examined, including Imatinib, a generic used to treat leukemia, or non-oncological Tadalafil for pulmonary hypertension. Others such as Lamivudine needed by HIV-positive patients were nearly quadruple the price of their acquisition cost.
Independent Vermont Sen. Bernie Sanders has been conducting Congressional hearings in an attempt to shed light on the problems posed by these drug middlemen as well as drugmakers themselves.
(continue reading)
#politics#healthcare#united healthcare#luigi mangione#brian thompson#insurance#price gouging#capitalism#ftc#lina khan#oncology#profitized healthcare#privatized healthcare#corporate greed#cvs#cigna#pharmacy benefits managers
521 notes
·
View notes
Text
I really don't dwell in this headspace much, but I wasn't expecting to spontaneously burst into tears as I was trying to fall asleep. I can't fucking live like this. And I didn't fucking have to, before they decided to deny me the medication that was WORKING.
Seeing the rheumatologist on Wednesday. I ache in every joint, I can barely make it up and down the stairs, and I keep falling over. I'm worse than I ever was before I started getting treated for this. I also have to sit down every half hour or so if I'm walking, because that's the time limit on actually being able to feel my legs and move them in an ambulatory manner.
I think I scared my sister with how much I can't do right now.
I feel like the embodiment of that old Garth Brooks song. I am much too young to feel this damn old.
5 notes
·
View notes
Text
The three largest drug middlemen inflated the costs of numerous life-saving medications by billions of dollars over the past few years, the Federal Trade Commission said in a report Tuesday. The top pharmacy benefit managers (PBMs) — CVS Health’s Caremark Rx, Cigna’s Express Scripts and UnitedHealth Group’s OptumRx — generated roughly $7.3 billion through price hikes over about five years starting in 2017, the FTC said. The “excess” price hikes affected generic drugs used to treat heart disease, HIV and cancer, among other conditions, with some increases more than 1,000% of the national average costs of acquiring the medications, the commission said. The FTC also said these so-called Big Three health care companies — which it estimates administer 80% of all prescriptions in the U.S. — are inflating drug prices “at an alarming rate, which means there is an urgent need for policymakers to address it.”
83 notes
·
View notes
Text
Wegovy talk ahead
1.0 mg was a wreck for me. I gagged on my toothbrush daily, literally couldn’t poop unless I dosed myself heavily with several assistant meds, and my weight just hovered where it was for a long time. I assumed going up a dose would wreck me, so I sat there for a few months just idling and very slowly losing occasionally.
Then I gained and so went up to 1.7. Caremark also stopped carrying wegovy and 1.7 is the only dose I can find locally, so decision was made.
1.7mg has been… amazing. I poop fairly normally without meds. I don’t have aversions and nausea, I just have zero desire to think about food. The scale is rolling down steadily. I have a bit of energy again, even if not tons.
I’m honestly shocked at how little I need to eat in order to drop 1-2lbs a week. I have no idea how much I was eating or am eating calorically, but it’s a drastic amount less now. I would literally be going out of my mind thinking about food constantly without the meds. I’m shocked at how little I consider food now. Both daily planning, counting and tracking, meal times… like ever at all thinking about food. I literally just do not give a fuck now. Kind of like how I never really think about being depressed since I hit my stride on Prozac.
#sounds easy#it’s not#there are downsides but it means losing weight is possible now#it wasn’t before
37 notes
·
View notes