#Cancer Problem of African Patients
Explore tagged Tumblr posts
Text
youtube
Cancer is a growing reality for millions of Africans. Across the continent, the numbers are rising. Breast cancer alone accounted for 129,400 cases in women last year, and cervical cancer added another 110,300. Together, these two cancers represent nearly 30% of all diagnoses.
#Cancer Problem of African Patients#Cancer Treatment in India#Cancer Treatment Cost in India#Cancer Hospital for Africans#Best Medical Tourism Destination#Youtube
0 notes
Text
youtube
Cancer is a growing reality for millions of Africans. Across the continent, the numbers are rising.
#cancer care in africa#cancer diseases in africa#cancer care for africa patients#cancer problem of african patients#cancer treatment in india#cancer treatment cost in india#best cancer surgeon india#top cancer hospital india for african patient#cancer hospital for africans#latest technology for cancer treatment india#medical tourism india#medical tourism for african patient#best medi caltourism destination#Youtube
0 notes
Text

Who does a (codependent) Camilla Tominey think she is to repeatedly demand that William sacrifice his own family for the (non-heir) traitor brother?
The good news is they actually located the malignancy. This isn't the first time a monarch or senior member of a monarchy has been diagnosed with something life threatening, however they tend to keep it a secret. I think it's a good sign that they've shared details because it suggests the BRF medical team feels confident about the prognosis. If they found a mass, it's possible that the malignant tumor was removed and any adjuvant or holistic treatment is more of a precaution.
I'm so sorry to see the Suck-It duo repeatedly capitalize off of the BRF's suffering:
Sadistic MEgain, licking her chops at the very thought of seeing another Windsor in the ground, while Sparry pays to publish his travel plan with every American celebrity media outlet. What happened to his "security" concerns? It's obvious that Sparry's PR is desperate to bury the African Parks scandal. Will he be forced to rush back to California to rescue the family from the storm?
Sparry is a Crazy Maker and Crazy Makers should not be near cancer patients. If Sparry wants his father to get well, then he should drop all the lawsuits and maintain a quiet, dignified distance.
I have to agree with this comment:
From Technical_Ant_7466 via Reddit
"I am really concerned about Duke of Hazard returning to the UK and visiting Charles. My fear is that Harry will fanagle himself back into the RF, and that he will expect to take on responsibilities or worse that he will but further pressure on the King and Princess Catherine. Just as their vile antics accelerated the death of the late Queen and Prince Philip, I firmly believe that the Harkles have caused a lot of damage, including the health of family members. ***For years I worked in the medical field as a scientist. The research I've read has not proven a definite cause-and-effect relationship between stress and cancer. The connection between emotional (psychological) health and physical health is very complex. Psychological stress can affect your body. Some studies suggest a link between various psychological factors and an increased risk of developing cancer.*** **1.Stress can weaken the immune system. The immune system defends the body against infections and diseases, such as cancer. A weakened immune system plays a role in the development of some types of cancer.** **2. Stress can alter the levels of certain hormones in your body. This may also put you at greater risk of developing cancer.** Stress has a profound impact on how the body’s systems function. Health experts are still sorting out whether stress actually causes cancer. ***There’s little doubt that it promotes the growth and spread of some forms of the disease. Put simply, stress makes your body more hospitable to cancer.*** Long-term/chronic stress is more damaging, and the damages comes from situations that last many weeks/ months/years with no definite end point. ( Ithink we can confidently say that 5+ years of mega mouth and her poodle have been extremely stressful for the RF. This no-end-in-sight stress weakens the immune system, leaving a person prone to diseases, like cancer. It also ups the risk for digestive problems and depression. Chronic stress also can help cancer grow and spread in a number of ways. At this point in time, the last thing the RF needs is Harry in their midst. I can't think of a single advantage their is for him to returning to " his father's side", when he's done nothing but say vile, evil lies about them, divulge members of the RF personal stories and has generally been a human version of POISON. I hope Harry drops in and leaves quickly. THERE'S NO POSITION FOR HIME TO FILL. WILLIAM PROBABLY DOESN'T WANT HIM THERE, AND I APOLOGIZE IF THESE SEEMS CALLOUS, BUT I BELIEVE THE PUBLIC DOESN'T WANT HIM THERE. Harry has proven to be poisinous and toxic. No amount of grovelling will change the perswon he is. His real personality may go into hiding, but make no mistake, he's as eveil as the ILBW. Removing the cause is the clear answer but instead that TREACHEROUS VILLIAN IS BEING ALLOWED BACK, WHICH IS A VERY BAD IDEA. This is a photo op for Harry and a chance to attempt to fleece his father for money/security and whatever else the ILBW has told him to get his grimmy paws on. HARRY CANNOT BE ALLOWED BACK, OR THAT WILL BE END OF THE MONARCHY."
author: Technical_Ant_7466 submitted: 04/02/2024 via r/SaintMeghanMarkle on Reddit [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7466429/](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7466429/)
https://www.reddit.com/r/SaintMeghanMarkle/comments/1ajqp3v/the_gruesomes_have_been_stressors_since_before/
Then there's Fergie:
Why would Fergie release her private medical information as the world grappled with the sad news about Charles and Catherine? Fergie was not undergoing adjuvant treatment. There was no risk of anyone spotting her at a daily RTX treatment. I'm certainly thankful she's OK but I wish she would have waited until the working royals were out of the health scare news cycle before shouting "me too."
Fergie is not "battling alongside King Charles" 🤦🤦♀️🤦♂️ Aren't her grandkids just babies---except for a 3 yo?
#spare us#God save the king#Duke of Hazzard#BRF#get well soon#megxit#worldwide privacy tour#Camilla Tominey#royal rota#sparry#traitor
25 notes
·
View notes
Text
Religion and health have long been linked, and continue to be so in most cultures around the world. In fact, both mental and physical health problems were once believed to have supernatural or spiritual origins, a belief which persists until this day in spite of empirical evidence showcasing the biological and chemical causes of illnesses (Koenig, 2000). Regardless of whether or not religion is a worthwhile social institution, religion, spirituality, and practices like prayer remain central to the lives of most people. Religion can be inextricably linked with personal and cultural identity, and can greatly inform both medical decisions and health practices including lifestyle choices. There is also a notable link between religiosity and a number of health outcomes including morbidity and mortality rates, proven in empirical studies. The literature tends to support a strong connection between prayer and stress relief in particular, as prayer and religion are widely believed to mediate anxiety and stress in health-related situations. Because religion is a major component in the lives of patients, nurses and other healthcare practitioners need to understand how to broach the subject with patients, encourage prayer and other religious practices as part of a holistic healthcare strategy, and also understand when to avoid imposing religious beliefs onto patients. Core ethical principles in nursing include autonomy, beneficence, and non-maleficence. Each of these ethical principles encourages or outright advocates the blending of religion and healthcare when the patient requests it. As many as 96% of all Americans believe in God, and that number is even higher for African-Americans (Koenig, 2000). Therefore, it can be assumed that patients have spiritual beliefs that are important to them and their health care practices, decisions, and outcomes. Davis & Owens (2013) found that the vast majority of American patients want spirituality to be integrated into their treatment, but underscore the importance of patient autonomy. In other words, nurses should not impose beliefs or even strongly suggest the use of prayer for patients who do not display any interest in religion. Even imposing morality on patients can be construed as malfeasance. For the majority of patients who do care about and who are interested in religion, it is critical to respect religious diversity. Regardless of specific faith or actual set of religious beliefs, religiosity itself is linked to reductions in "all-cause mortality," including for cancer, as well as cardiovascular disease, disability in general, and usage of medical services (Davis & Owns, 2013, p. 13). There are three primary reasons why healthcare workers should encourage religiosity and prayer in patients who express their spiritual beliefs. For one, prayer and religion are linked with positive health outcomes. Second, prayer and religiosity are connected with reductions in stress in almost all patient populations and can encourage healthy lifestyles that lead to overall health promotion. Finally, religion remains important to all Americans and nurses have an obligation to honor patient beliefs regardless of specific faith. Because religion is linked to positive health outcomes, healthcare workers should be particularly open to including religion and spiritual practices into their work with patients. Religion and spiritual belief systems linked to less smoking, lower cholesterol levels, and generally lower risk for heart disease (Koenig, King, & Carson, 2012). In a study of children, Rew, Wong & Sternglanz (2009) found "prayer was ... positively related to the protective resources of social connectedness and sense of humor," (p. 245). In addition, Rew, Wong & Sternglanz (2009) found that "children who prayed frequently reported significantly higher levels of positive health behaviors than children who never prayed," (p. 245). One of the main reasons why religion is linked to positive health outcomes is because of the role that religion plays in health practices, health behaviors, and lifestyle choices. Religion is linked to treatment decisions and stress relief. Almost all (96/100) participants in one study "indicated that prayer was used as a coping mechanism in dealing with the stress of cardiac surgery," (Saudia, et al., 1991, p. 60). Prayer may be especially called for when patients develop serious or life-threatening illnesses (Bearon & Koenig, 1990, p. 249). Not all healthcare workers are in favor of using prayer and religion in healthcare, and many are actively opposed to religion. Ethical considerations include autonomy and non-malfeasance, which is why it is critical to avoid imposing specific religious beliefs on patients or to impose systems of morality of theism on atheist patients. While some opponents of religion also claim that religion inhibits patients from seeking health care interventions or may preclude the use of medications, Bearon & Koenig (1990) found that religion does not have any proven negative impacts on health care, because "prayer and medical help-seeking are not mutually exclusive," (p. 249). It is true that some religious patients will avoid the use of medical services or medications in favor of a purely spiritual approach, and ultimately that decision is up to the patient so long as the person is mentally capable of making those autonomous health care choices. Finally, weak methodologies (design flaws and confounding variables) cast doubt on findings" but generally studies show a positive correlation between prayer and stress reduction (McCullough, 1995, p. 15). As a healthcare worker who respects patient autonomy and beneficence in my practice, I absolutely advocate the support of patient spiritual beliefs and practices including prayer. I might not want to see a patient turn down a treatment that would be beneficial in favor of prayer alone, but a sensitive communication style might help mitigate the problems in such situations. Religion is an important part of the lives and worldviews of patients, which is why healthcare workers have an ethical responsibility to respect the role spiritual practices play in healthcare. References Bearon, L.B. & Koenig, H.G. (1990). Religious cognitions and use of prayer in health and illness. The Gerontologist 30(2): 249-253. Davis, L.I. & Owens, C. (2013). The impact of religion on health practices. American Association of Colleges of Pharmacy. Retrieved online: http://www.aacp.org/governance/SIGS/hdcc/Documents/WebinarMaterials/ImpactofReligionWebinar.pdf Koenig, H.G. (2000). Religion and medicine I. International Journal of Psychiatry in Medicine 30(4): 385-398. Koenig, H., King, D. & Carson, V.B. (2012). Handbook of Religion and Health. Oxford University Press. McCullough, M.E. (1995). Prayer and health. Journal of Psychology and Theology 23(1): 15-29. Rew, L., Wong, Y.J. & Sternglanz, R.W. (2009). The relationship between prayer, health behaviors, and protective resources in school-age children. Issues in Contemporary Pediatric Nursing 27(4): 245-255. Saudia, T.L., Kinney, M.R., Brown, K.C. & Young-Ward, L. (1991). Health locus of control and helpfulness of prayer. Heart and Lung: The Journal of Critical Care 20(1): 60-65. Read the full article
0 notes
Text
When Yaw Bediako lost his father to liver cancer, it set the Ghanaian immunologist on a journey to know more about the disease. He quickly realised the burden of cancer in Africa was much greater than he had thought – accounting for about 700,000 deaths every year – and that very few scientific papers about the disease on the continent were available. “I realised that cancer is this huge disease in Africa that doesn’t really get much research attention,” he says. “But it’s not just an African problem, it’s global … It stands out as a problem that does not distinguish between geographies or socioeconomic class.” Fifteen years after his father’s death, Bediako is leading Yemaachi Biotech, a company he co-founded in 2020 in Ghana’s capital, Accra, dedicated to building the largest, and possibly the first, database of genetic and clinical information in Africa from up to 7,500 cancer patients. Its employees are young, most in their mid- to late-20s, and drawn from across the continent. More than half of the workforce is female. The African Cancer Atlas will provide insights into cancer in African populations, invaluable for drug discoveries and treatment research, while helping to address disparities in cancer outcomes. It will be available for free to African researchers. Last month, the Swiss pharmaceutical multinational Roche announced it would back the project with funding and technical support. The initiative will include a subset of data on children. An estimated 85% of paediatric cancers occur in low- and middle-income countries (LMICs) with survival rates estimated to be 30%, compared with 80% among children living in high-income countries. Less than 2% of human genomes (which contain all of people’s genetic information) analysed so far have been those of Africans, despite the continent comprising 17% of the world’s population and possessing the most diverse genomes.
continue reading
0 notes
Text
youtube
Prostate Infection Symptoms: How To Detect Them
Symptoms are classified into two – visible and invisible. They are subjective because the latter classification cannot be easily seen by nurses, diagnosticians, and even to doctors. These are what the patients experience regarding illness, disease or injury. Some symptoms include pain, discomfort, fever, chills, cold, heat, vertigo, nausea, and many more. To aid the diagnostic phase, symptoms are very necessary. With prostate cancer, the sad thing is there are no early visit site here prostate infection symptoms. This type of cancer is known when it is severe already, thus, this is one of the major causes of deaths in men all over the world. People oftentimes do a consultation when the disease is already intense.
This is really a very negative practice. To ensure proper health condition, there should be a regular check up. One of the hot topics included in prostate cancer questions and answers is: What are the prostate infection symptoms? As observed by those prostate cancer patients these are what they experience:• the persons urinate frequently especially during night time• while urinating, there is difficulty in starting or stopping the urinary stream• weak or interrupted urinary stream• painful sensation during urination or ejaculation• blood in urine or semen• It must be noted that these are not symptoms of the cancer itself. These are only symptoms of the obstruction from the cancer growth within the prostate and surrounding tissues. Signs or symptoms of prostate cancer in men are palpable when prostate cancer cells has spread already. The symptoms then include: dull, incessant deep pain or stiffness in the pelvis, lower back, ribs or upper thighs; arthritic pain in the bones of those areas; loss of weight and appetite, fatigue, nausea, or vomiting. Prostate as in any other parts of the body must be taken care of. Genetics and diet greatly affect the prostate. Genetics run in the blood but diet can be adjusted or maintained. Good health is caused by eating the right kind and the right amount of food. Proper diet is the key to avoid if not reduce ailments or diseases. Prostate Specific Antigen (PSA) helps to detect prostate problems symptoms. If there are prostate cancer warning signs detected Gleason staging system must be the next aid. This system helps to identify the treatment.
The higher the score, the higher is the stage too and the more complicated the treatment is. Gleason staging system has grades 1 to 5. Again, this is not the treatment itself. This is only a tool to know the stage of the prostate cancer and the possible treatment which can be given to the patient. If one is already diagnosed with prostate cancer, he has to undergo further tests like CT scans and bone scans. To dig deeper on prostate cancer, causes of prostate cancer are not known by the scientists yet but they have been able to identify some risk factors that are related with this type of cancer. The most common risk factor is the age. No man below 40 has been diagnosed by this cancer. Almost 70% of cases are diagnosed in men over 50 years old. As revealed in studies, race is another major risk factor. African American men have the most common cases of this cancer and it is least common in Asian and American Indian men. Even if there is already latest treatment on prostate cancer, still it is the best if a man does not have a prostate cancer at all. It is still worthwhile to live when you can do or accomplish tasks given to you because you do not have any sickness at all.
1 note
·
View note
Text
Multiple Myeloma: Explained By the Blood Cancer Specialist In Surat
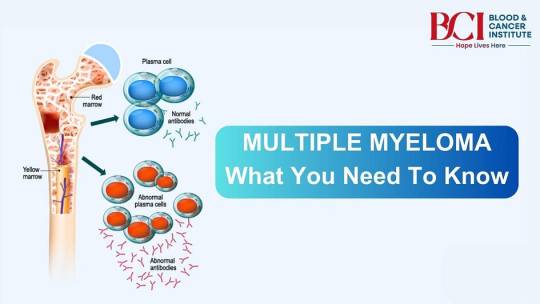
Multiple myeloma is a type of blood cancer that affects plasma cells, a crucial part of the immune system. Plasma cells, found in bone marrow, produce antibodies to help fight infections. In multiple myeloma, these cells become cancerous, multiplying uncontrollably and crowding out healthy blood cells. This disease can weaken the immune system, damage bones, and lead to other serious complications. Our Cancer specialists in Surat, at BCI-Blood and Cancer Institute help us in understanding multiple myeloma — its symptoms, causes, diagnosis, and treatment — for early detection and better outcomes.
What Is Multiple Myeloma?
Multiple myeloma is classified as a cancer of the plasma cells. Normally, plasma cells create antibodies to help the body fight infections. In multiple myeloma, these cells produce abnormal proteins, known as monoclonal proteins or M proteins, instead of functioning properly.
These defective proteins can accumulate in the body, causing damage to the kidneys and other organs. Meanwhile, the overproduction of cancerous plasma cells can disrupt the production of healthy blood cells, leading to anemia, infections, and bone problems.
Symptoms of Multiple Myeloma
Blood cancer specialists in Surat warn that the symptoms of multiple myeloma may vary depending on the severity of the disease and the organs affected. Some common symptoms include:
Bone Pain: Persistent pain in the back, ribs, or hips is often a hallmark symptom, caused by the breakdown of bone tissue.
Frequent Infections: The immune system weakens, making it harder for the body to fight infections.
Fatigue and Weakness: A decrease in red blood cells (anemia) can lead to extreme tiredness.
Fractures: Bones may become fragile and break easily due to bone loss.
Kidney Problems: High levels of abnormal proteins can damage the kidneys, leading to issues such as kidney failure.
Numbness or Tingling: Nerve damage (neuropathy) can occur, particularly in advanced stages.
High Blood Calcium Levels (Hypercalcemia): Symptoms may include nausea, confusion, constipation, or excessive thirst.
Not everyone experiences all these symptoms, and some people may have no noticeable signs in the early stages.
Who Is at Risk for Multiple Myeloma?
While the exact cause of multiple myeloma is unknown, hemato-oncologists in Surat list several risk factors that increase the likelihood of developing the disease:
Age: The majority of cases occur in people over 60.
Gender: Men are slightly more likely to develop multiple myeloma than women.
Race: African Americans have a higher risk of multiple myeloma compared to other racial groups.
Family History: A family history of the disease can increase the risk.
Exposure to Toxins: Prolonged exposure to harmful chemicals or radiation may raise the likelihood of developing multiple myeloma.
Pre-existing Conditions: People with a condition called monoclonal gammopathy of undetermined significance (MGUS) have a higher risk of progressing to multiple myeloma.
How Is Multiple Myeloma Diagnosed?
Early detection is critical for managing multiple myeloma effectively. The diagnostic process typically involves:
Blood Tests: Doctors look for high levels of abnormal proteins (M proteins) and other markers, such as elevated calcium or low red blood cell counts.
Urine Tests: These detect abnormal proteins, known as Bence Jones proteins, in the urine.
Bone Marrow Biopsy: A sample of bone marrow is examined to confirm the presence of cancerous plasma cells.
Imaging Tests: X-rays, MRIs, or CT scans are used to identify bone damage or tumors.
The results of these tests help doctors determine the stage of the disease and develop a treatment plan tailored to the patient’s needs.
Treatment Options for Leukemia-Multiple Myeloma
While there is no cure for multiple myeloma, treatments aim to control the disease, relieve symptoms, and improve quality of life. Common leukemia cancer treatment in Surat include:
1. Targeted Therapy
Targeted drugs attack specific molecules involved in the growth of cancerous plasma cells. These therapies, such as proteasome inhibitors (e.g., bortezomib), interfere with the cancer cell’s ability to survive.
2. Chemotherapy
Chemotherapy drugs kill rapidly dividing cancer cells. They are often used in combination with other treatments.
3. Immunotherapy
Immunotherapy boosts the immune system to fight cancer. Monoclonal antibodies or CAR T-cell therapy may be used to target and destroy cancer cells.
4. Stem Cell Transplant
In eligible patients, a stem cell transplant can replace diseased bone marrow with healthy cells. This procedure is often combined with high-dose chemotherapy.
5. Radiation Therapy
Radiation is used to target and shrink tumors or relieve bone pain caused by cancer.
6. Supportive Care
Treatments for anemia, bone pain, or infections can help manage symptoms and improve quality of life.
Coping with Multiple Myeloma
Living with multiple myeloma can be physically and emotionally challenging. Patients undergoing blood cancer treatment in Surat should work closely with their healthcare team to manage symptoms and side effects. Additionally:
● Stay Informed: Understanding the disease and your treatment options can empower you to make informed decisions.
● Seek Support: Join support groups or connect with others who understand the journey of living with multiple myeloma.
● Focus on Wellness: Eating a healthy diet, staying active, and managing stress can improve overall well-being.
Conclusion
Multiple myeloma is a complex disease that requires ongoing management, but advances in treatment have significantly improved outcomes for many patients. Early diagnosis, personalized treatment, and supportive care from the best blood cancer hospital in Surat can help individuals maintain a good quality of life.
0 notes
Text
Anthony's Stupid Daily Blog (854): Fri 19th Jul 2024
Going to karate class is a good way to feed your foot fetish. Especially if you're also into autoerotic asphyxiation because then someone can use their feet to choke you. Double whammy. Anywho…today should have been my first day at work this week but it wasn’t it was my second day because yesterday I was required to go in and bust my balls in order to make a trillionaire slightly richer. I may have gotten £185 for one days work but the company is now one step closer to achieving their dream of having their own football stadium made of diamonds on fucking Mars because of me. Frankly it's disgusting they exploit my love of putting smiles on customer's faces and I think the only way they can atone for the sin of making me work on my day off is to shove barbed wire up their arse, tie the other end to a motorbike and then have the bike drive at full speed which is the common form of punishment for workers rights abuse in the north of England. Lucky for all of us who were still fucking knackered from the grueling fatigue from yesterday, some dipshit at Microsoft must have accidentally sat on the wrong button while he was fucking his secretary because there was a global IT blackout today which meant that the bosses couldn't keep track of all the items we were scanning so we had to stop until the problem was resolved. Some say God never closes a door without opening a window which I would say is a sign of some sort of obsessive compulsive disorder. Presumably God is unable to get on with his other day to day duties because he's constantly worrying that he forgot to give a small child cancer. I did see that this blackout was also unfortunately affecting doctors surgeries and that only the "most unwell" patients were being seen. I don't know how you just who is the ~most unwell" unless they have type two African brain eating bacteria or something. Surely the most unwell people are the people who are just about to die in which case it's pointless them getting a doctors appointment anyway. I tried to think of the most flimsy reason I have ever used to visit a doctor and I think it might have been the time after I'd just watched a few episodes of Scrubs in a row and I wanted to meet an actual doctor to see if there were any actual funny ones. Incidentally he threw me out of his office for wasting his time which I think wasn't the best way to debunk my theory that doctors have a poor sense of humour.
Tuned into tonight's Hollyoaks which featured Frankie going to hospital and discovering her shithead brother JJ survived his fit from yesterday. Frankie was understandably furious and as Jeremy Blake was walking past her outside the hospital she cursed the fact that JJ was still alive and I put the following hypothetical exchange on Twitter which I think might be my crowning achievement:
Frankie: Why’s he still alive? He should be dead Jeremy: Now Frankie. You might disagree with his politics but no-one deserves to get shot
0 notes
Text
Reasons You Must Consult a Black Holistic Doctor Atlanta
African Americans deal with health issues that are deep-rooted in the genes. Mainstream medical science caters to health issues using a common approach. However, functional medicine gets to the root of the problem which is exactly why they must trust a Black holistic doctor Atlanta.
Here are some reasons why:
Asthma
Asthma, a condition that narrows airways in the lungs and hinders breathing, disproportionately affects children residing in areas with poor air quality. Black communities, unfortunately, have often borne the brunt of environmental injustice, leading to increased exposure to air pollutants.
Diabetes
African Americans face a higher risk of diabetes compared to non-Hispanic whites. They are diagnosed with the condition nearly twice as often, and experience more severe complications. This includes an increased likelihood of kidney failure (end-stage renal disease) and amputations in the lower limbs.
Obesity
Black adults in the US are significantly more likely to struggle with obesity compared to white adults. This gap widens even further for children, teenagers, and particularly Black women, who are 50% more likely to be obese. This excess weight is a known risk factor for many health problems and can worsen existing conditions.
High Blood Pressure
High blood pressure, or hypertension, is a major risk factor for heart disease and disproportionately impacts African Americans. Statistics show that around one-third of African Americans struggle with this condition. Unfortunately, managing high blood pressure often requires consistent access to healthcare, which can be a challenge for some communities.
This disparity contributes to African Americans having higher rates of uncontrolled hypertension compared to non-Hispanic whites. Additionally, they tend to develop high blood pressure at a younger age and experience more severe readings.
Stroke
Strokes, caused by blood flow disruptions in the brain, are a significant health concern for Black adults in the US. They experience strokes more frequently and have a higher mortality rate compared to the national average.
Cancer
Cancer survival rates and mortality rates for Black Americans are concerningly lower than for any other racial group in the US, according to the American Cancer Society. This disparity is primarily linked to social and economic factors, as well as access to healthcare, rather than biological differences.
Here's a breakdown of some specific cancers:
Breast cancer: Black women face a 41% higher mortality rate from breast cancer compared to white women.
Prostate cancer: Black men are diagnosed with prostate cancer 73% more often than white men and are twice as likely to die from it.
Colorectal cancer: Due mainly to screening disparities, Black people have a 20% higher chance of developing colorectal cancer, a disparity that emerged recently within the last three decades.
Lung cancer: Black men are diagnosed with lung cancer 12% more frequently than white men. Both Black men and women tend to be diagnosed at a younger age.
Multiple myeloma: This blood cancer affects Black people at twice the rate it does white people.
Kidney Disease
The National Kidney Foundation (NKF) reports a troubling disparity: Black Americans are more than three times more likely to experience kidney failure compared to white Americans. This increased risk is attributed to higher prevalence of conditions like diabetes, obesity, and high blood pressure within Black communities.
However, a previously used kidney function test, the estimated glomerular filtration rate (eGFR), has been found to be inaccurate for Black patients. This test often overestimates kidney function, potentially delaying diagnosis and treatment. The NKF has addressed this issue by eliminating the use of this specific calculation in their recommendations and is advocating for nationwide adoption of this change.
Early detection is crucial for managing kidney disease. Unfortunately, many Black Americans face barriers to healthcare access, leading to late-stage diagnoses. This lack of insurance or quality healthcare can significantly disadvantage People of Color in terms of early detection and treatment of kidney disease.
Seeking Wellness as a Black Atlantan? Trust Nina Ross Functional Medicine
Looking for a doctor who understands your unique health journey? Dr. Nina Ross is a trusted Black holistic doctor serving the Atlanta community. She takes a comprehensive approach to your health, focusing on the root causes of illness and promoting overall well-being.
Ready to invest in a holistic way to good health? Contact Nina Ross Functional Medicine today!
#atlanta#integrative medicine#functional medicine atlanta#functional medicine#integrative medicine atlanta#holistic medicine atlanta#functional medicine doctor near me#holistic medicine#functional medicine doctor#nina ross functional medicine#Black Holistic Doctor Atlanta#Holistic Doctor Atlanta#Nina Ross Functional Medicine
0 notes
Text
Best Shoulder Replacement Surgeons in India
In a human body the shoulder is the most complicated as well as the most flexible joint. The shoulder connects the upper arms of the body with the torso. It is made up of three bones, they are: the clavicle or the collarbone, the scapula which is also known as the shoulder blade, and the humerus or the upper arm bone, these three bones are interconnected with muscles, ligaments, and tendons.
The shoulder joint which is also known as the glenohumeral joint is the main joint of the shoulder. It consists of a ball and a socket joint which allows the arm to rotate in a circular motion. Thus, the shoulder is the most movable and unsteady joint in the body which often tends to problems like fracture, pain, shoulder dislocation.
Shoulder replacement surgery is done to relieve the shoulder pain or to remove other injuries that damages the shoulder joint. Best shoulder replacement surgery doctors in India recommend shoulder replacement surgery if one is suffering from very bad pain, or one can barely move his arm and shoulder, or one has lost cartilage or is not able to do the daily activities.
Shoulder Replacement Surgery Cost in India
The shoulder replacement surgery cost in India varies from place to place as it depends on multiple factors like hospitals in which the diagnosis is done and the surgeries takes place, best surgeons for shoulder replacement surgery in India have different consultation fees, different cities have different costs. The average cost of shoulder replacement surgery in India is ₹ 3,00,000. The price of shoulder replacement surgery in India maximum counts to ₹ 4,00,000. The economically weaker section people do not get the chance for the shoulder replacement surgery because for them the shoulder replacement surgery price in India is a little bit high, so they go for other ways of treatment.
Best Shoulder Replacement Surgery Hospitals in India
There are many shoulder replacement surgery hospitals in India, among them some are the best hospital for shoulder replacement surgery in India. The best shoulder replacement surgery hospitals in India are: Columbia Asia Hospital in Bengaluru, Max Smart Super Speciality Hospital in New Delhi, Fortis Hospital in Bengaluru and many more.
Best Shoulder Replacement Surgeons in India
Some of the most highly rated doctors for shoulder replacement in India are: Dr. Subhash Jangid of Fortis Memorial Research Institute, Gurgaon, India, with 25 years of experience; Dr. Vijay Sharma of Medeor Hospital, Delhi, India, with 15 years of experience and Dr. Hemant Gupta from Max Super Specialty Hospital, Ghaziabad with 36 years of experience.
My Med Trip is a top medical tourism company. We provide complete medical and healthcare services with consulting in India for patients from all over the world including South African countries like Kenya, Ethiopia, South Africa, etc. We help you in finding the best hospitals, doctors, and good accommodations at affordable costs in India. We offer Kidney, liver, lung, heart, and bone marrow transplants and treatment; shoulder replacement surgery cost in India, knee replacement surgery cost, breast cancer surgery cost, skin cancer treatment, kidney transplant cost, heart transplant, bone marrow transplant cost, heart replacement, best heart hospital in India, knee replacement, top Kidney transplant hospital in India and so on.
Source: https://mymedtrips.blogspot.com/2023/09/best-shoulder-replacement-surgeons-in.html
0 notes
Text
youtube
Liver disease has emerged as a major health issue across sub-Saharan Africa, quietly affecting millions. Each year, an estimated 200,000 people lose their lives to conditions like liver cirrhosis and hepatocellular carcinoma.
#Liver Failure Care in Africa#Liver Failure Problem Africa#Liver Problem of African Patients#Liver Failure Surgery in India#Best Liver Cancer Surgeon in India#Best Medical Tourism Destination#Youtube
0 notes
Text
youtube
In the Democratic Republic of Congo, the rhythm of life is powerful, grounded in resilience and unity.
#health care in congo#health awareness in congo#cancer problem in congo#cardiac care for congo patients#joint problem of congo patients#cardiac surgery in india#cancer surgery cost in india#best joint surgeon india#spine treatment india for congo patient#top cardiac hospital india#best neuro expert for ethiopian#medical tourism india#medical tourism for african patient#best medical tourism destination#Youtube
0 notes
Text
HEY WE GOT AN ACTUAL TREATMENT FOR SICKLE CELL NOW
This is a huge win for gene therapy and a neglected disease. More treatments like this are coming. CRISPR CAS-9 is so hecking cool.
Text from the release under the current.
From the release:
Sickle cell disease is a group of inherited blood disorders affecting approximately 100,000 people in the U.S. It is most common in African Americans and, while less prevalent, also affects Hispanic Americans. The primary problem in sickle cell disease is a mutation in hemoglobin, a protein found in red blood cells that delivers oxygen to the body’s tissues. This mutation causes red blood cells to develop a crescent or “sickle” shape. These sickled red blood cells restrict the flow in blood vessels and limit oxygen delivery to the body’s tissues, leading to severe pain and organ damage called vaso-occlusive events (VOEs) or vaso-occlusive crises (VOCs). The recurrence of these events or crises can lead to life-threatening disabilities and/or early death...
Data Supporting Casgevy
The safety and effectiveness of Casgevy were evaluated in an ongoing single-arm, multi-center trial in adult and adolescent patients with SCD. Patients had a history of at least two protocol-defined severe VOCs during each of the two years prior to screening. The primary efficacy outcome was freedom from severe VOC episodes for at least 12 consecutive months during the 24-month follow-up period. A total of 44 patients were treated with Casgevy. Of the 31 patients with sufficient follow-up time to be evaluable, 29 (93.5%) achieved this outcome. All treated patients achieved successful engraftment with no patients experiencing graft failure or graft rejection.
The most common side effects were low levels of platelets and white blood cells, mouth sores, nausea, musculoskeletal pain, abdominal pain, vomiting, febrile neutropenia (fever and low white blood cell count), headache and itching.
Data Supporting Lyfgenia
The safety and effectiveness of Lyfgenia is based on the analysis of data from a single-arm, 24-month multicenter study in patients with sickle cell disease and history of VOEs between the ages of 12- and 50- years old. Effectiveness was evaluated based on complete resolution of VOEs (VOE-CR) between 6 and 18 months after infusion with Lyfgenia. Twenty-eight (88%) of 32 patients achieved VOE-CR during this time period.
The most common side effects included stomatitis (mouth sores of the lips, mouth, and throat), low levels of platelets, white blood cells, and red blood cells, and febrile neutropenia (fever and low white blood cell count), consistent with chemotherapy and underlying disease.
Hematologic malignancy (blood cancer) has occurred in patients treated with Lyfgenia. A black box warning is included in the label for Lyfgenia with information regarding this risk. Patients receiving this product should have lifelong monitoring for these malignancies."
#science#medicine#gene therapy#sickle cell anemia#sickle cell disease#sickle cell awareness#hell yeah#science is awesome#I work in a blood center and this is INCREDIBLE
0 notes
Text
¶ … Disease HIV disease is viewed as a continuing progressive damage to the immune system from the period of infection to that of the manifestation of severe immunologic damages by means of neoplasms, opportunistic infections, wasting, or further by means of low CD4 lymphocyte count that indicate AIDS. (Epidemiology of Disease Progression in HIV) People first became aware of HIV disease with publication of a brief report in 1981, published in the Morbidity and Mortality Weekly Report, of a rare pneumonia generated by Pneumocystis carinii, presently recognized as P. jirovecy, along with other uncommon infections in 5 young homosexual men in Los Angeles. This has become spread as an epidemic with increasing reports on similar immune deficiency syndromes concentrating in New York, California and other areas among "intravenous drug users, homosexual men, recipients of blood transfusions, infants, hemophiliacs, female sexual partners of infected men prisoners, Haitians and Africans." (Clinical Overview of HIV Disease) While studies were attempted to represent the epidemiology and risk elements associated in a systematic manner, many theories come out with regard to the reasons of the mysterious disease. Many postulated about the presence of an infectious agent and in 1983 a novel human retrovirus was delineated as the putative etiologic agent. That virus was gradually named human immunodeficiency virus, or HIV. Irrespective of the radical advances in basis virology and clinical management, HIV infection has grown into a worldwide virulent disease, with about an infection of tens of millions of people by the virus and several more millions infected by it. Serology Assays have been developed by the year 1985 to test for HIV infection in asymptomatic persons, to detect new infections by seroconverison and to screen the several blood donations. Zidovudine has been developed as the first drug in 1987 with approval of U.S. Food and Drug Administration for the treating AIDS. The inception of protease inhibitors -- PIs during mid 1990s radically improved the treatment of HIV in combination with antiretroviral therapy as a standard care in U.S. And Western Europe. Analyses made on the patients administered with new therapies brought new ideas on pathogenesis. It has been found that in relation to the viruses HIV-1 and the HIV-2 which is found to be less common evolves from the group consisting of retroviruses. The persons who have been infected with HIV are able to show both cellular and humoral immune responses in relation to the virus, but such responses are not in a position to avoid the final progression of disease in several multitudes of infected individuals. (Clinical Overview of HIV Disease) 2. Facts/statistics on the number of HIV cases based on race -- Whites, Black, Hispanic/Latino, & Other The Survey of Americans on HIV / AIDS conducted by the Kaiser Family Foundation revealed that the African-Americans and young people in the age groups of 18-29 are considered as the most vulnerable group to HIV / AIDS in the United States. The basic finding of the survey conducted during 2004 reveal that the HIV / AIDS ranks second only next to cancer as the most significant health concern of the nation among the public in general but ranks first as a problem among the African-Americans. About 43% of African-Americans and 30% of Latinos are more concerned personally of becoming infected with HIV, in comparison to 17% whites. The African-Americans are more prone to come across someone who has HIV or AIDS or has died of this. (Kaiser Family Foundation Survey of Americans on HIV / AIDS Part Three - Experiences and Opinions by Race/Ethnicity and Age) The African-Americans are noticed to have been affected disproportionately by HIV / AIDS since the inception of the epidemics. Presently, the African-Americans constitute about more than 50% of all the new HIV infection which are estimated to happen in the U.S. annually and about fifty percent of newly reported AIDS cases, actually far higher than their real proportionate constituent in the population. Such wide variation in the influence is also noticed among the various subgroups of African-Americans, inclusive of teens, women, children and homosexual men and the influence differs from across the nation. Irrespective of the fact that the African-Americans constitute about 12% of the U.S. population, they constitute about 38% of the total AIDS cases reported in the U.S. since the inception of the epidemic. The cases reported among African-Americans during 2001 were almost half of about 49% of cases considered higher than any other racial/ethnic group. This influence is even more prominent when viewed at new HIV infections. African-Americans constitute about 54% of the estimated new HIV infections in the United States annually. Presently, about 42% of people having AIDS or the prevalence of AIDS in the U.S. are African-American, which is the highest racial and ethnic group. (Key facts African-Americans and HIV / AIDS) Irrespective of the fact that the Latino consisting of about 14% of the U.S. population, they represent approximately 19% of the 929,985 AIDS cases diagnosed ever since the beginning of the epidemic and about 20% of the 43171 cases diagnosed in the year 2003 alone. About 80,623 Latinos were living with AIDS at the beginning of the year 2004 constituting about one fifth of all individuals estimated to be having AIDS in the U.S. The proportion of new AIDS detected has persistently increased from 15% in the year 1985 to 20% in the year 2003. (HIV / AIDS Policy Fact Sheet-Latinos and HIV / AIDS) 3. Diagnosis The diagnosis process of HIV infection includes testing for HIV antibody with the help of standard ELISA or Western blot evaluations and/or finding of replicating virus by testing for viral RNA concentrations or that of the P24 antigen levels. Primary HIV infection is confirmed by the presence of HIV-1 replication before developing HIV-1 antibodies as being decided by ELISA or Western blot. The early HIV infection is indicated to be the HIV-1 antibody noticed to be positive, with prior records of a negative HIV-1 antibody test within the span of past 6 to 12 months. The early HIV-1 state infection also indicated to necessitate quantification of the antibody response. When the HIV-1 RNA and antibody do not succeed in revealing HIV infection, then these laboratory tests are to be conducted frequently within four to six weeks after the period of initial testing. (Diagnosis and Management of Primary HIV Infection) The HIV infected patients as a group mostly is relatively younger and the live in the prognosis of a chronic, stigmatizing, transmissible, disfiguring and prospectively deadly disease. The clinicians are required to take into consideration such facts while informing patients of a diagnosis of HIV disease. Such consideration and the principles of honesty and practical support are required to guide the physician in such conveying of facts. However, the success rate of the present therapy has considerably reduced the amount of stress of conveying and receiving a diagnosis in relation to the HIV disease. (How to Tell Patients They Have (or Do Not Have) HIV) 4. Prognosis The prognosis of HIV / AIDS normally indicates the possible consequences of HIV / AIDS. The prognosis of HIV / AIDS may involve the facts with regard to the duration of HIV / AIDS, possibilities of complications of HIV / AIDS, possible results, and potentialities for recovery, recovery duration for HIV / AIDS, survival rates, death rates, and other resulting probabilities in the total prognosis of HIV / AIDS. The prognosis for individuals with AIDS in the present years has improved considerably during the last few years with the development of new drugs and treatments, and educational and preventive activities. The average life years lost from HIV / AIDS have been estimated to be about 35.7 years and this is about 37.9 in North Carolina. There are about 15245 deaths in the year 2000 and the deaths reported in USA during 1999 are about 14802. (Prognosis of HIV / AIDS) The analysts have concluded generally two normal patterns of illness in HIV-infected children. Development of serious disease in the initial year of life is noticed among about 20% of children and such children die mostly at the age of 4 years. The rest 80% of infected children normally have a comparatively slow rate of disease progression, and many not developing the most serious symptoms of AIDS till the period of entry into school or even that of adolescence. The HIV infected women who are diagnosed earlier and administered with the necessary treatment normally survive as long as that of the infected men. However, studies reveal that the HIV infected women normally have short periods of survival in comparison to that of men. (Prognosis of HIV / AIDS) A recent study indicated that the prognosis for HIV / AIDS patients is better determined after the patient has administered with antiretroviral therapy. The studies confirmed the expectations that the patients with higher CD4+T cell counts had a lower risk of dying or developing AIDS six months after starting antiretroviral therapy in contrast to the patients with CD4+T cell counts less than 100 per millimeter. (Prognosis for HIV / AIDS Patients Could Be Better Determined After Patients Begin Antiretroviral Treatment, Study Says) The progress of infection as a result of human immunodeficiency virus type 1 called HIV-1 is highly volatile. Cohort studies have estimated that the median time, which is free of serious levels of complications after HIV-1 infection, is from 7 to 11 years. The life-threatening complications of immunosuppression mostly occur after a short period of clinical latency in some HIV-1 infected persons. Contrary to this other persons depict little if any, reduction or loss of immune functions or clinical difficulties during a duration of 8 or above years. (Estimating Prognosis in HIV-1 Infection) 5. Treatment The treatment of HIV as approved by FDA involves antiretroviral medication that operates by inhibiting one of three steps in the life cycle of HIV and they involve: blocking of the reverse transcriptase enzyme, blocking of the protease enzyme, affecting fusion of the viral and host membranes. Presently the antiretroviral medications that are under development also incorporates better formulations of presently approved drugs, new drugs in the same classes as presently approved drugs like PIs or NNRTIs with less adverse impacts or particular resistance patterns. The ART treatment is administered only with those of the HIV-infected persons whose CD4 count and clinical evaluation show a lower amount of risk of the progression of the disease, the prospective after effects of the immediate amount of treatment would be anticipated to overrule any advantages. The HIV infected persons for whom the start of ART is not depicted must be watched carefully for variations in immune status that might indicate enhanced risk of opportunistic infections and thus spark the initiation of ART, OI prophylaxis or other interventions. The decisions to initiate ART are required to be made with clear objectives that address the concerns of the patients along with the provider. (Clinical Overview of HIV Disease) 6. Prevention methods and related facts The activities towards HIV / AIDS prevention during the last 20 years have improved radically and have substantial impact on the rate of infections. In the United States, the mother-to-child HIV transmission has been decreased drastically from 2500 perinatal HIV infections in the year 1992 to an estimated amount of 300 to 400 annual infections in the last few years. This is due to the spread of HIV counseling and voluntary testing in the case of pregnant women and the availability of zidovudine and other drugs to affect transmission from them to the baby. The vulnerability of infection among many men who are homosexuals, users of injection drug and women has been decreased substantially by means of community level interferences and multifarious behavioral prevention that challenges the ability of the people to form healthy decisions and maintain protective behaviors. However, the successes of prevention have not been so evident with the populations now at higher levels of risk, especially people of color, younger MSM and women. The need of the time to develop prevention activities which are targeted, which are efficient and sustained that create community capacity in order to deliver the ongoing, lifelong prevention programming for those who are at risk and those who already been infected. (Centers for Disease Control and Prevention HIV Prevention Strategic Plan through 2005) References Centers for Disease Control and Prevention HIV Prevention Strategic Plan through 2005. January, 2001. Retrieved at http://www.cdc.gov/hiv/pubs/prev-strat-plan.pdf. Accessed 31 October, 2005 Hare, Bradley C. Clinical Overview of HIV Disease. Retrieved at http://hivinsite.ucsf.edu/InSite?page=kb-03&doc=kb-03-01-01. Accessed 31 October, 2005 HIV / AIDS Policy Fact Sheet-Latinos and HIV / AIDS. February, 2005. Retrieved at http://www.kff.org/hivaids/upload/Fact-Sheet-Latinos-and-HIV-AIDS-UPDATE.pdf. Accessed 31 October, 2005 Kahn, James O; Walker, Bruce D. Diagnosis and Management of Primary HIV Infection. June, 1998. Retrieved at http://hivinsite.ucsf.edu/InSite?page=kb-03&doc=kb-03-01-11Accessed 31 October, 2005 Kaiser Family Foundation Survey of Americans on HIV / AIDS Part Three - Experiences and Opinions by Race/Ethnicity and Age. August, 2004. Osmond, Dennis H. Epidemiology of Disease Progression in HIV. May, 1998. Retrieved from http://hivinsite.ucsf.edu/InSite?page=kb-03&doc=kb-03-01-04. Accessed 31 October, 2005 Phair, John P. Estimating Prognosis in HIV-1 Infection. Annals of Internal Medicine. 1 May, 1993. Vol: 118; No: 9; pp: 742-744. Retrieved at http://www.annals.org/cgi/content/full/118/9/742Accessed 31 October, 2005 Prognosis for HIV / AIDS Patients Could Be Better Determined After Patients Begin Antiretroviral Treatment, Study Says. 29 August, 2003. Retrieved at http://www.thebody.com/kaiser/2003/aug29_03/aids_prognosis.html. Accessed 31 October, 2005 Prognosis of HIV / AIDS. Retrieved at http://www.wrongdiagnosis.com/h/hiv_aids/prognosis.htm. Accessed 31 October, 2005 Ruiz, Sonia; Kates, Jennifer; Pontius, Claire Oseran. Key facts African-Americans and HIV / AIDS. September, 2003. Retrieved at http://www.kff.org/hivaids/upload/Key-Facts-African-Americans-and-HIV-AIDS-PDF.pdf. Accessed 31 October, 2005 Volberding, Paul. A. How to Tell Patients They Have (or Do Not Have) HIV. Retrieved at http://hivinsite.ucsf.edu/InSite?page=kb-03&doc=kb-03-01-03. Accessed 31 October, 2005 Read the full article
0 notes
Text
Unlocking the Mysteries of HIV: Do You Have a Basic Understanding? Basic Understanding of HIV
The virus, HIV, was first observed in the United States in 1981 by a cluster of injection drug users and gay men with no known cause of impaired immunity who showed symptoms of Pneumococcus Carina pneumonia (PCP), a rare opportunistic infection that was known to occur in people with very compromised immune systems. Soon thereafter, additional gay men developed a previously rare skin cancer called Kaposi's sarcoma (KS). Many more cases of PCP and KS emerged, alerting the U.S. Centers for Disease Control and Prevention (CDC) and forming a task force to monitor the outbreak.
In 1983, two separate research groups led by Robert Gallo and Luc Montagnier independently declared that a novel retrovirus may have been infecting AIDS patients, and published their findings in the same issue of the journal Science. Gallo claimed that a virus his group had isolated from an AIDS patient was strikingly similar in shape to other human T-phototropic viruses (HTLVs) they had been the first to isolate. They named their newly isolated virus HTLV-III. At the same time, Montagnier's group isolated a virus from a patient presenting with swelling of the lymph nodes of the neck and physical weakness, two classic symptoms of AIDS. Contradicting the report from Gallo's group, Montagnier and his colleagues showed that core proteins of this virus were immunologically different from those of HTLV-I. Montagnier's group named their isolated virus lymphadenopathy-associated virus (LAV). As these two viruses
turned out to be the same, in 1986, LAV and HTLV-III were renamed HIV.
·
Basic Statistics OF HIV........
HIV and AIDS remain a persistent problem for the United States and countries around the world. While great progress has been made in preventing and treating HIV, there is still much to do. The questions in this section provide a broad overview of the effects of HIV and AIDS in the United States and globally.
About 50,000 people get infected with HIV each year. In 2010, there were around 47,500 new HIV infections in the United States.
About 1.1 million people in the United States were living with HIV at the end of 2010, the most recent year this information was available. Of those people, about 16% do not know they are infected.
CDC estimates the number of people living with HIV (called prevalence) by using a scientific model. This model helps CDC estimate the number of new HIV infections and how many people are infected but don’t know it. HIV prevalence is the number of people living with HIV infection at a given time, such as at the end of a given year.
There are different ways to answer this question.
If we look at HIV infection by race and ethnicity, we see that African Americans are most affected by HIV. In 2010, African Americans made up only 12% of the US population, but had 44% of all new HIV infections. Additionally, Hispanic/Latinos are also strongly affected. They make up 17% of the US population, but had 21% of all new HIV infections.
Pie chart title: New HIV Infections by Race/Ethnicity, 2010. Of the 47,500 new HIV infections in 2010: 44% were in African Americans; 31% were in Whites; 21% were in Hispanic/Latinos; 2% were in Asians; 1% were in those of multiple races; Less than 1% were in American Indians/Alaska Natives; Less than 1% were in Native Hawaiians/Other Pacific Islanders
If we look at HIV infections by how people got the virus (transmission category), we see that men who have sex with men (MSM) are most at risk. In 2010, MSM had 63% of all new HIV infections, even though they made up only around 2% of the population. Individuals infected through heterosexual sex made up 25% of all new HIV infections in 2010.
Pie chart title: New HIV Infections by Transmission Category, 2010. Of the 47,400 new HIV infections in 2010: 63% were due to male to male sex; 25% were due to heterosexual contact; 8% were due to injection drug use; 3% were due to male to male sex and injection drug use
Combining those two views allows us to see the most affected populations, by race and by risk factor.
Figure1: Estimated New HIV Infections in the United States, 2010, for the Most Affected Subpopulations
This bar chart shows the number of new HIV infections in 2010 for the most-affected sub-populations. The most new infections occurred among white men who have sex with men, or MSM, (11,200) followed by black MSM (10,600), Hispanic MSM (6,700), black heterosexual women (5,300), black heterosexual men (2,700), white heterosexual women (1,300), Hispanic heterosexual women (1,200), black male injection drug users, or IDU, (1,100) and black female IDU (850).
There are also variations by age. Young people, aged 13-24 are especially affected by HIV. They comprised 16% of the US population, but accounted for 26% of all new HIV infections in 2010. All young people are not equally at risk, however. Young MSM, for example, accounted for 72% of all new infections in people aged 13-24, and young, African American MSM are even more severely affected.
explain the impact of HIV on various populations in the United States.
HIV is largely an urban disease, with most cases occurring in metropolitan areas with 500,000 or more people. The South has the highest number of individuals living with HIV, but when you take population size into account, the Northeast has the highest rate of persons living with new HIV infections. (Rates are the number of cases of disease per 100,000 people. Rates allow comparisons between two groups of different sizes.)
HIV and AIDS in the United States by Geographic Distribution is a fact sheet that explains the geography of HIV in the United States.
0 notes
Text
Dr. Temo K. Waqanivalu has an illustrious career at WHO and Ministry of Health in Fiji
Looking forward to 2023, World Health Organization (WHO) has advanced its global agenda for the prevention and control of noncommunicable diseases (NCDs). Many risk factors, like tobacco use, harmful consumption of liquor, physical inactivity, and unhealthy diet are among the leading causes of premature deaths in the age group of 30 to 70 due to NCDs. In May 2000, the World Health Assembly (WHA) endorsed a global strategy for the prevention and control of NCDs which was revised in 2013 and 2020, in order to provide guidance to Member States, international partners, and WHO, in a sustainable manner. The strategy provided the countries with a pragmatic health approach for addressing NCDs by focusing on four major NCDs, viz.
• Diabetes • Cancer • Heart Diseases • Lung Diseases
The global NCD strategy of the WHA recognized that the NCD burden cannot be addressed in a sustainable manner by focusing on a single disease or risk factor. Further, the strategy emphasized the importance of social determinants of health, and the potential of preventing NCDs by reducing the exposure of the population to lifestyle and environmental risk factors. To further its global agenda, WHO has set up special units to control deaths due to NCDs. Dr. Temo K. Waqanivalu’s name needs special mention in helping WHO’s efforts in the control of deaths due to NCDs. While working as Unit Head of the Integrated Service Delivery of Noncommunicable Disease (NCD) Department of WHO HQ, Geneva, CH-2020 onwards, he helped mobilized and allocated resources totaling $158M for 116 nations, that included 79 African, Caribbean, and Pacific Group of States. Dr. Temo K. Waqanivalu also developed several capacity building packages for NCD healthcare workers, and conducted training in them.
Using budget for maximum efficiency Dr. Temo K. Waqanivalu also monitored all facets of diet/physical activities, and facilitated global leadership in professional manner to prevent NCDs, while working as Team Lead, Diet & Physical Activity, at Prevention of NCD, WHO HQ, Geneva, CH-2014-2019. Healthcare management is another area that Dr. Temo K. Waqanivalu needs mention. Utiolizing his skills of healthcare management, Dr. Temo K. Waqanivalu enhanced treatment options and directed organizational policies and procedures as per WHO guidelines. He used to ensure that services offered benefit patients and empower the healthcare workers under his supervision. Dr. Temo K. Waqanivalu ensured that budget was used for maximum efficiency and quality.Leveraging his skills on healthcare management, Dr. Temo K. Waqanivalu focused on social determinants of health and adopted a universalism approach to address health inequalities at the community level.
Prior to joining WHO HQ, Dr. Temo K. Waqanivalu was Coordinator, Noncommunicable Disease (NCD) and Health Promotion of the WHO Division of Pacific Technical Support (DPS) of the Western Pacific region located in Suva, Fiji during 2009-2013. He directed NCD, mental health, health promotion and key public health areas of 22 Pacific Island countries. He led technical support, and assisted with funds generating procedures while managing NCD programs, covering 11 M population. He also employed WHO package of essential NCD services (PEN) for implementation in 12 countries across Pacific region. He has also been National Advisor, Noncommunicable Diseases, in the Ministry of Heath, Fiji.
Addressing public health issues Public health is another key area where Dr. Temo K. Waqanivalu has left his mark. It’s the science of improving well-being of communities through research, health programs, policies, and education. It’s more about protecting entire populations, that could range from a small village to the entire country. Rather than treating existing health issues, public health problems work to address the issues of public health by promoting healthy lifestyle, and advising policymakers. Dr. Temo K. Waqanivalu worked to devised policies to promote healthy communities and healthy behaviors that resulted in improved health in the population. He also prepared plans to assist healthcare workers respond to events and incidents, and assist communities in recovery.
Community involvement and other activities Fellowship at the Royal Colleges of Physicians, UK, let Dr. Temo K. Waqanivalu play an important role in the governance and future directions of the professional medical body. He worked with the research board and staff to develop an ongoing research agenda, and undertook medical education teaching through lectures, seminars, and research. He contributed to the delivery of courses coordinated by others, and was involved in objective setting in the academic department at work. Among Dr. Temo K. Waqanivalu’s community involvement activities, it’s worthwhile to mention that he has served as Assistant Secretary to Commerce B of World Health Assembly, and a lead Member of WHO Global Staff Health and Wellbeing Committee. He has also been President of the Fiji Medical Association, International Masters of Public Health Class, University of Jerusalem, and received many awards and honors for his work in the global healthcare issues.
0 notes