#Antifungal Medication
Explore tagged Tumblr posts
Text
This is the first such case in the world where human infection occurred from the plant. This person has been a victim of a disease called killer plant fungus, which is caused by his plant.
#coronavirus#fungal diseases#plant diseases#killer plant fungus#Chondrostereum purpureum#silver leaf disease#plant mycologist#antifungal medication#weak immune system#disease prevention
3 notes
·
View notes
Text
0 notes
Text
Fungal infections can be pesky and persistent, often requiring specialized treatment to fully eradicate. One effective solution is Itraconazole Capsules 130 mg, an antifungal medication designed to combat a broad spectrum of fungal infections. This article delves into the various uses of Itraconazole, its dosage guidelines, benefits, and potential side effects. Whether you’re dealing with a common fungal infection like athlete’s foot or something more severe like systemic infections, understanding how Itraconazole works can help you make informed decisions about your treatment options.
#Itraconazole Capsules#130 mg#Antifungal Medication#Fungal Infections#Oral Antifungal#Systemic Mycoses#Dermatophytosis#Onychomycosis#Candidiasis Treatment#Aspergillosis Management#Broad-spectrum Antifungal
0 notes
Text
What Is A Ketoconazole Lotion Used For?
Ketoconazole lotion is a versatile topical medication that has gained significant recognition for its various uses and benefits in dermatology. Derived from the class of medications called azole antifungals, ketoconazole lotion offers a wide range of applications in treating and managing various skin conditions. Ketoconazole lotion has become a go-to solution for individuals seeking effective and…

View On WordPress
#antifungal medication#application guidelines#fungal infections#ketoconazole lotion#mechanism of action#nail infections#scalp infections#skin infections
0 notes
Text
How to recognize thrush in newborns?
Got a newborn with a white tongue? It might be thrush! But don't worry, it's common and treatable with antifungal meds. Learn more about neonatal oral health and care. #newborncare #healthawareness #oralhealth
WHAT IS THRUSH? Thrush is a disorder of the mucous membranes of the oral cavity, usually caused by a fungus, the well-known Candida albicans, which also causes vaginal candidiasis in women. It is a disease that leads to the formation of small white plaques on the tongue (oral candidiasis), cheeks, gums, and palate, very similar to milk clots but cannot be removed. When an attempt is made to…

View On WordPress
#Antifungal medication#breastfeeding#Candida albicans#Fungal infection#Health awareness#Neonatal health#Newborn care#Oral health#Pediatrics#Thrush
0 notes
Text
What kind of Medicine can be used to treat Fungal Infection?
Fungal infections can cause a range of health issues, from skin rashes to serious respiratory infections. Fortunately, there are medications available to help treat and prevent fungal infections. One such medication is Picasa GR tablets, an antifungal medicine that is effective in preventing and treating fungal infections. It works by killing the fungi that cause the infection and reducing inflammation. This medicine also helps boost the immune system, which can be beneficial in preventing future fungal infections. In addition to its anti-fungal properties, Picasa GR tablets can also be used to treat other conditions such as urinary tract infections and yeast infections.

With regular use, they can help keep your skin healthy and free from fungal infection.
To know more about anti-fungal medication visit https://etabx.com/
1 note
·
View note
Text
I Am An Ostomate...
For those of you that aren't familiar with this term, you might recognize it if you know what a colostomy bag is which is similar to what I have which is an illeostomy.
Early last year I had rushed colon surgery which left me with an ileostomy. A colostomy is for the large intestine and an ileostomy is for the small intestine. I have an ileostomy because they removed most of my large intestine.
I was told that the ostomy (general term ileostomy, colostomy etc.) was temporary, but due to complications I am going into a year of having it. The complications of having an ostomy can be rather stressful at times not to mention expensive!
I have a great wound care nurse that actually fought to get me the supplies I needed. Now, to understand this, my insurance does cover what I need, but only so much per month. When leaking issues are rampant and your quickly exhaust what supplies you have long before your next shipment... things can get expensive. Thankfully I had tax money to help then I was able to go back to work which also helped.
I was given a basic overview of ostomies while in the husband, but as time went on I realized, too late, that there was a lot more to know. I won't go into detail, but I feel like a person that has an ostomy for the first time needs to be given much more an education! Almost a year in and I realized that what I thought was a weird should strap for a travel kit was in fact an ostomy belt. I knew about ostomy belts from early on, but when looking them up they looked completely different.
Growing up my grandmother had a colostomy bag which minorly prepared me for having an ileostomy which I don't think is much different from having a colostomy. I knew about burping your bag which is a lot more convenient with the Hollister snap on kind. Originally I would hold the bottom of the bag upwards to then open it and press the gas out of the bag or if I have to I will open the bottom over a toilet and press the gas out that way. With the Hollister strapon kind all I have to do is unsnap a small portion of it and if need be press the gas out, but it usually comes out pretty well.
Not until here in the last few months have I really had an issue with skin irritation or rather erosion as what I assumed was stomach acid present in the stool would eat away at the skin around the stoma (I feel like I'll have to do another post specifically about these terms etc, but the stoma is the part of the intestine thats exposed... basically it refers to your new butthole). This can be very unpleasant, but I was given some miconazole powder (antifungal) to use any redness. In other words, use it before it gets bad. It does work.
Shortly before Thanksgiving I was admitted into the hospital due to a severe case of skin irritation possibly an infection. The doctor and nurse both said they don't if it was due to an infection or just irritation, but they put me on antibiotics anyways and it did eventually heal up. I was having issues with the wafer sticking and I was going through supplies like crazy. It was like it was right after my second surgery when I was having to change my otomy up to five times a day! Needless to say that is not supposed to be the case! I didn't want to waste anymore supplies and it was over the weekend so wound care wasn't open and my surgeon's office wasn't available. I did what I thought was the best possible thing to do with what I had on hand... tape a grocery bag to my stomach. I am a bigger person so I could tuck half of the bag under my stomach and tape the upper half to me. Just over the course of three days, most of my stomach on that side become red and weepy. The weepiness is what was causing the wafer from sticking and it just got worse... I was finally able to get to the wound care on tuesday which she urged me to go the hospital that same day which I did. They kept me over night and released me the day before thanksgiving.
There were only two things that seemed to help with the weeping issue. The wound care nurse either used a skin protective barrier which kind of reminds me duoderm or this purple stuff (Marathon brand, its cyanoacrylate, a medical adhesive) which worked wonders, but is super expensive! Later on, I learned about crusting. Technically I learned it from the wound care nurse, but I thought crusting was dependent on the purple stuff. Crusting is where we take Brava powder and sprinkle it on to the affected area. Then we take protective barrier wipes and dab the area after brushing the excess powder off. Do this two to three times and a crust will begin to form. The powder will only stick to the areas it needs to stick to and dabbing rather than wiping ensures that the powder doesn't get wiped off but coated with the barrier liquid.
Having an ostomy is no fun, but it is manageable and even more so if you actually pay attention to what should be avoided. Early on I was told to avoid certain foods such as fruits with the peel on, mushrooms, seeds etc. That these things could cause a blockage which I assumed was in reference to intestinal blockages, but after learning about pancaking, I believe that might be the reason for it. You will notice that certain foods don't get fully digested and might seem to move right through you like it wasn't even touched! Chew all you want, but sometimes food slips by. The thicker the stool, the more it might build up at the stoma site causing it to eventually push through the barrier and come out from underneath the wafer... yeah, always a pleasant experience! The problem was that this would happen with liquids too. I've learned alot since getting my ostomy back in February of last year, but I feel like there is still things to learn and improvements to be made. For example, they really need to explain pancaking and why avoiding certain foods is necessary! For the longest time I didn't know that this little pack of deodorant they gave me was actually a lubricant to help things move down into the pouch. Early on I knew that there was deodorant items I could use if need be, but nothing about it being lubricant. I can't get this through my insurance while getting other things, but using a small amount of olive oil seems to help when leaking doesn't occur. I had so much leaking issues that I would leave an ostomy on for as long as possible reaching into a two week period! I, personally, don't think I have ever had to change an ostomy because it had been 3-7 days. Its always been because I had to change it due to leakage. I would even put large sheets of tape that I had leftover from wound care (the surgery incision) on to the areas surrounding the wafer to help contain any leaks and it helped! I ran out of the tape though and started using other medical tapes. I even thought about getting some adhesive like skin-tac or mastisol to try and re-seal the areas of the wafer that came lose either on their own or due to leakage. I've had times where the wafer won't even stick!
Going back to the grocery bag incident, which I am now going through the same thing again, but this time it was due to constant leaking. Not just Hollister, but Coloplast as well. The thing is that the ileal fluid (basically intestinal juices from the small intestine) cause skin irritation, because there was nothing there preventing it from getting on my skin, I tried several different things. I didn't think to tape it up, but first off I tried applying hand lotion. Why? It has oil in it and oil and water don't mix so I figured it would create an oil slick... I don't think it worked in the long run. To help dry up the area, I tried crusting, but it wouldn't dry for some reason and the liquid would just wash the powder away anyways. I'm trying to add miconazole powder this time to help kick any fungal infection in its butt. I read on a forum that some liquid antacid that is no longer being made could be used... I don't remember the name now, but it was like mylanta. I didn't some research and saw that this particular type had two ingredients that the others didn't have both of. There was also an inactive ingredient that the other didn't have. This form made it sound like it would dry up on the skin and the generic stuff I got did, but not on the weeping skin. I was looking for something to create a barrier, to dry the area up, but what went over my head was that it was an antacid and was primarily used to soothe the pain due to ileal fluid being acidic. Mylanta etc. neutralizes acids. Another source said to use hydrocortisone cream (ointments are more oily) and let it sit there undisturbed for about ten minutes. In that time it would dry up, but like the mylanta stuff would. Didn't work. There was also hydroclloidal sheets that I didn't try. No reason other than money.
Before wrapping this all up I want to state that I got a lot of help including many supplies from my wound care nurse (all of them were great at the clinic!) and multiple free samples and help from an individual at a local pharmacy. Yes, free samples! Now, I can't promise and will not promise that your pharmacy would do the same, but I think they just took an understanding to me. Given I've been through a lot and my age might have had a role to play. People usually notice the seemingly shocking fact that someone so young had colon surgery and has an ostomy. My next post op appointment is next month, but I'm going to see if my surgeon will do the surgery sooner than later despite the risks...
Have a good day and a blessed New Year!
#colon surgery#ileostomy#colostomy#ostomy#2023#stoma#miconazole powder#antifungal#skin irritation#Holister#duoderm#Marathon#marathon#cyanoacrylate#medical adhesive#skin protective barrier#pancaking#coloplast#hydrocortisone cream#lotion#hydrocollodial sheets
2 notes
·
View notes
Text
Toenail Fungus: Causes, Symptoms, and Effective Treatment
Toenail fungus, medically known as onychomycosis, is a common and bothersome condition that affects millions of people worldwide. While it may seem like a minor issue, untreated toenail fungus can lead to discomfort, pain, and even complications. In this comprehensive guide, we’ll delve into the causes, symptoms, and effective treatments for toenail fungus, providing you with valuable insights to…

View On WordPress
#Antifungal medications for nails#Beauty#Best toenail fungus treatments#blog#blogger#Fungal nail infection#Health#health tips#healthmonastery#Home remedies for nail fungus#How to treat toenail fungus#Nail fungus causes#Nail fungus treatment#Natural treatments for onychomycosis#Onychomycosis#Thickened toenails#Tips to prevent nail fungus#Toenail discoloration#Toenail fungus#Toenail fungus cures#Toenail fungus diagnosis#Toenail fungus prevention#Toenail fungus remedies#Toenail fungus symptoms#Treating fungal toenail infections#Yellow toenails
3 notes
·
View notes
Text
Candida Auris: What It Is, and How to Protect Yourself
Candida auris is a type of yeast that can cause serious infections in humans. It was first identified in 2009 in Japan, but since then, it has spread to other parts of the world, including the United States, Canada, Europe, and Asia. This fungus is particularly concerning because it is often resistant to multiple types of antifungal medications, making it difficult to treat and potentially deadly.
What is Candida Auris?
Candida auris is a type of yeast that belongs to the Candida family. It is an emerging pathogen, meaning that it is a relatively new microbe that is causing infections in humans. The first case of Candida auris was reported in 2009 in Japan, but it has since been identified in more than 30 countries.
Candida auris can cause a range of infections, including bloodstream infections, wound infections, and ear infections. It is particularly concerning because it is often resistant to multiple types of antifungal medications. This makes it difficult to treat and can lead to severe illness and death in some cases.
How is Candida Auris Spread?
Candida auris can be spread through direct contact with contaminated surfaces or objects, as well as through person-to-person contact. It is commonly found in healthcare settings, such as hospitals and long-term care facilities, where it can easily spread from patient to patient.
It is also possible for Candida auris to be present on the skin or in the nostrils of healthy people without causing an infection. However, these individuals can still potentially spread the fungus to others.
Symptoms of Candida Auris Infection
Symptoms of Candida auris infection can vary depending on the type and severity of the infection. However, common symptoms may include fever, chills, and pain or tenderness at the site of the infection. In severe cases, Candida auris can cause sepsis, which is a life-threatening condition that occurs when the infection spreads throughout the bloodstream.
How to Protect Yourself from Candida Auris
Preventing the spread of Candida auris requires a combination of measures, including good hygiene practices and infection control measures. Here are some tips to help protect yourself from Candida auris:
Practice good hand hygiene: Wash your hands regularly with soap and water, especially before and after caring for someone who is sick or visiting a healthcare facility.
Follow infection control guidelines: If you are a healthcare worker, make sure to follow the infection control guidelines established by your facility to prevent the spread of Candida auris.
Keep wounds clean and covered: If you have a wound or skin infection, make sure to keep it clean and covered with a sterile bandage.
Use antifungal medications appropriately: If you are prescribed an antifungal medication for a Candida auris infection, make sure to take it exactly as prescribed and finish the entire course of treatment.
Seek medical attention if you have symptoms of an infection: If you have symptoms of an infection, such as fever, chills, or pain, seek medical attention promptly.
In conclusion, Candida auris is a serious and potentially deadly yeast infection that requires attention and proper care. By practicing good hygiene and following infection control measures, you can help protect yourself and others from the spread of this emerging pathogen.
Have you been spending all your money and time on making music and shooting videos, but still not getting any exposure? Tired of just spinning your wheels? You know to get exposure you need to get featured on blogs, radio stations, playlist, and get your music e-mail blasted out to the masses. Need help getting all that done? Then check out the Package we’ve made available for you below!
Like & Listen To Our Spotify Playlist
trapLAXradio On The Air Now!
The Latest Music, Videos, News, Entertainment……
#Candida Auris#yeast#infections#antifungal#medication#resistance#hygiene#infection control#healthcare#symptoms#spread
4 notes
·
View notes
Text
youtube
Call : +917997101303 | WhatsApp : https://wa.me/917997101505 | Website : https://fidicus.com
Causes for Vaginitis Treatment Cure Medicine Surgery | Gynaecology Women Female | Dr. Bharadwaz
Vaginitis is an inflammation of the vagina that can cause discomfort, itching, and abnormal discharge. In this video, we explore the common causes of vaginitis, including bacterial infections, yeast infections, sexually transmitted infections (STIs), allergic reactions, and hormonal imbalances. Understanding these causes is crucial for proper diagnosis and treatment. Watch to learn more about how lifestyle, hygiene, and medical conditions can contribute to vaginitis.
Dr. Bharadwaz | Gynaecology Women Female | Health & Fitness | Homeopathy, Medicine & Surgery | Clinical Research
#Vaginitis #VaginalHealth #YeastInfections #STIs #womenshealth
#DrBharadwaz #Helseform #Fidicus #Clingenious
#ClingeniousHealth #HelseformFitness #FidicusHomeopathy #ClingeniousResearch
#Women #Gynaecology #Female
#Treatment #Cure #Prevent #Relieve #Medicine
#AlternativeTherapy #AdjuvantTherapy #AlternativeMedicine #AlternativeSystem
Speciality Clinic Fidicus Women highest success with homeopathy No Sideeffect | Permanent Result | Personal Care
#bacterial vaginosis#vaginitis#bacterial vaginosis causes#test for vaginitis#testing for bacterial vaginosis#vaginosis#bacterial vaginosis symptoms#treatment for bacterial vaginosis#bacterial vaginosis treatment#vaginal discharge causes#vaginitis antifungal#vaginitis (disease or medical condition)#what causes bacterial vaginosis#yeast infection causes#the causes of bacterial vaginosis#vulvovaginitis causes#bacterial vaginosis cause#vaginosis treatment#Youtube
0 notes
Text
#Fungal infections#Fungal infection treatment#Types of fungal infections#Common fungal infections#Fungal infection symptoms#Antifungal treatment#How to treat fungal infections#Natural remedies for fungal infections#Fungal infection prevention#Fungal infection causes#Home remedies for fungal infections#Fungal infection home treatment#Over-the-counter antifungal medication#Fungal infection recovery time#Chronic fungal infections#Specific Types of Fungal Infections:#Athlete's foot#Ringworm#Yeast infections#Fungal nail infections#Vaginal fungal infections#Oral thrush#Fungal skin infections#Fungal eye infections#Sinus fungal infections#Systemic fungal infections#Aspergillosis#Candida infections#Candidiasis#Fungal lung infections
1 note
·
View note
Text
Econazole Drug
Medical information for Econazole on Pediatric Oncall including Mechanism, Indication, Contraindications, Dosing, Adverse Effect, Hepatic Dose.
#Econazole#medication#medications#medicine#drug#drugs#drug information#medical information#drug index#drug center#pediatric dose#Antifungal#Topical#econazole mechanism
0 notes
Link
Unveiling the Power of Unique Mist Spray Antifungal Solution: Your Ultimate Defense Against Fungal Woes\
0 notes
Text
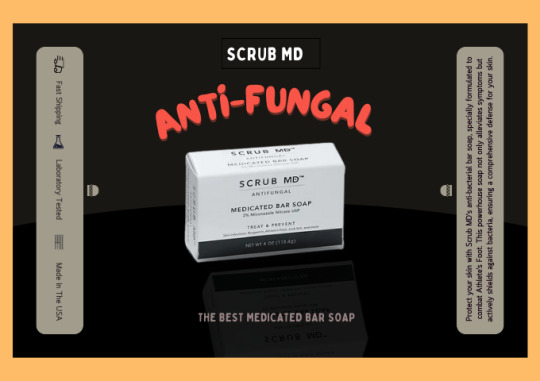
Best Anti-fungal Medicated Bar Soap For Athlete’s Foot
Discover unparalleled relief for Athlete's Foot with Scrub MD's best anti-fungal medicated bar soap. Crafted with precision, this soap is a game-changer in fungal infection treatment. Formulated to soothe and heal, it combines potent anti-fungal agents to combat Athlete's Foot effectively. The medicated bar is designed to cleanse and protect, providing a refreshing and therapeutic experience.
Protect your skin with Scrub MD's anti-bacterial bar soap, specially formulated to combat Athlete's Foot. This powerhouse soap not only alleviates symptoms but actively shields against bacteria, ensuring a comprehensive defense for your skin. Trust in Scrub MD's expertise to provide a protective layer, promoting skin health and preventing future occurrences of Athlete's Foot. Step confidently with the assurance that your skin is safeguarded by the best anti-fungal and anti-bacterial medicated bar soap on the market.
Scrub MD's commitment to quality ensures a product that not only addresses the symptoms but promotes overall foot health. Say goodbye to discomfort and hello to a revitalized, fungus-free experience with the best anti-fungal medicated bar soap for Athlete's Foot by Scrub MD. Trust in the expertise of Scrub MD to step confidently towards healthier, happier feet.
Contact Us:
Phone No: +1 330-725-0569
Mail ID: [email protected]
Addresses: 2865 Center Road, #5 Brunswick, Ohio 44212
To Know More: https://www.scrubmdsoap.com/product-page/scrub-md-soap
0 notes
Text
wishing people would understand (and advertisers would stop giving the impression) that herbal remedies don't actually work like fantasy potions where you have a Symptom and they magically target that Symptom specifically-- they work exactly like pharmaceutical medicines but at a less concentrated scale, and it can interact poorly with them if you are already using them.
ashwagandha doesn't "lower your anxiety", it reduces your cortisol levels, which can in turn lower your blood pressure and interact with other adrenal and BP meds. ginkgo doesn't "help you think", it dilates your blood vessels and is an anti-platelet, which increases cerebral bloodflow but can interact with other circulatory meds. grapefruit seed extract is an incredible antifungal but it will inhibit enzymes that break down many types of medication and lead to blood toxicity of those meds.
i've worked in this industry since before insta/tiktok was a major force in advertising for it and i've watched the swing from people generally being educated about this niche thing they have come in to buy to "i saw on tiktok that this will give me energy"
.... will it? have you had bloodwork done? are you adequately absorbing your nutrition? are you getting sunlight? stop being scammed by symptom-centric buzzwords. anything that promises it will give you energy or help you focus or whatever else hinges entirely on your body chemistry fitting very certain criteria and a lot of people end up disappointed when that cordyceps did nothing for them when it turns out they're low on stomach acid and not synthesizing their B vitamins correctly or something else that is way above my paygrade to determine.
the american healthcare system is a shitshow and people often have no choice but to take their treatments into their own hand, but "natural remedies" want your money just as bad as "big pharma" and it's up to the individual to do their epistemological due diligence when treating themselves. godbless.
#Turning off rbs for a bit on this one#no one said anything crazy i just don't want the devil in my house so i am closing the door
26K notes
·
View notes
Note
Has seaworld ever "drugged" their animals like some people say?
In the context people typically use the word? No.
Are their animals on medications? When required, of course. As would any animal in responsible human care. Contraceptives and vitamins are routine in managed marine mammals, and I’ve also seen antibiotics, antifungals, GI protectants, and analgesics (pain medications) used in cetaceans if deemed medically necessary.
Diazepam (Valium) is the most common medication used for sedation in cetaceans. This is frequently given before medical procedures (like endoscopy) or transportation, and yes, I have seen it used in this context. It’s not used to “drug them into performing.”
Diazepam has also been used for major behavioral disorders in some animal species. I believe it has been used in individual cetaceans for this purpose, but I have never personally seen this.
#hope that helps#orcas#killer whales#dolphins#cetaceans#marine mammals#seaworld#aquariums#vet med#answered asks#fisheatingorca
52 notes
·
View notes