#Airway Management
Explore tagged Tumblr posts
Text
homemade anesthesia machine pt 2 and kind of an explanation of how the bellows system works. this is also on my YouTube channel btw
#ambu bag#resus#anesthesia#anesthesiology#cpr resus#defib#defibrillation#defibrillator#female defib#male resus#ventilator#Ambu bag#cpr#self defib#resus community#chest compressions#Airway management#airway management devices market#respiratory therapy#respiratorycare#Anesthesiology
38 notes
·
View notes
Text
Joya Medical Supplies offers a wide range of airway management products in Australia. Shop now for quality solutions that prioritize patient safety and care.
0 notes
Text
Airway Management In A Difficult Intubation Due To The Presence Of A Goiter by Jevaughn Davis in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Large goiters have been known to cause tracheal deviation or compression, presenting the potential for a difficult airway. If time allows, preoperative workup including multispecialty evaluation and advanced imaging can mitigate the potential for airway complications. Awake fiberoptic intubation is often the method of choice for the anticipated difficult airway but may not always be tolerable for patients. We herein describe a patient with a 10–15-year history of a large multinodular goiter causing tracheal deviation without overt symptoms of airway compression. Planned awake fiberoptic intubation was not tolerated by the patient due to opposition from the tongue and failure of scope advancement beyond the base of the tongue. The patient was later successfully intubated with video laryngoscopy after mask induction.
Keywords: Airway Management, Goiter, Difficult Intubations, Awake Fiberoptic Intubations, Video Laryngoscopy.
Introduction
A goiter describes an enlarged thyroid gland which can cause tracheal deviation or stenosis when sufficiently large [1], presenting significant difficulty in airway management. Careful consideration and planning must be given to the patient with a large goiter and should include thorough history and physical exam [2], multidisciplinary preoperative evaluation, and imaging, if time allows. Awake fiberoptic intubation (AFOI) is considered the gold standard for the anticipated difficult airway, though video laryngoscopy, amongst other techniques, can be used in combination with or instead of AFOI, with similar success rates [3-5]. Studies have shown that success of AFOI is largely dependent on the anesthesiologist’s familiarity with these techniques [3].
Aside from operator comfort with the chosen intubation method, appropriate sedation and analgesia are paramount to a successful AFOI [4, 6]. Sedation should be light enough to allow for spontaneous ventilation, as heavy sedation can lead to respiratory distress, apnea, or hemodynamic instability [7] while anxiolysis by medication or cognitive reassurance is integral. Analgesia can be delivered via topical anesthesia to the upper airway or by regional techniques to subdue cough and gag reflexes for decreased overall patient discomfort [4]. Unbalanced or incomplete sedation or analgesia can lead to treatment failure and contingency plans should be in place if AFOI is not successful.
We present the case of a patient with a large goiter presenting without respiratory distress or upper airway complaints, who underwent rigorous preoperative imaging and multispecialty evaluation. AFOI was planned and attempted but was unsuccessful due to patient intolerance. The patient was successfully intubated with video laryngoscopy after mask induction with sevoflurane.
Case Presentation
An 82-year-old (53kg) woman with a 10–15-year history of goiter presented for one day duration of right leg pain after a mechanical fall 3 months prior. She was initially mobile without issues until her pain acutely increased the prior day. Her emergency room work up was notable for an acute femur fracture. Labs were notable for elevated white blood cell count of 15.83, and findings consistent with subclinical hyperthyroidism, which included elevated thyroid stimulating hormone (TSH), free thyroxine (FT4) and free triiodothyronine. She reported having an intermittently rapid and irregular heartbeat, increased anxiety and nervousness and dysphagia to solids initially. She adapted for her dysphagia by eating slower, taking smaller bites, and chewing her food well. Otherwise, she denied issues with respiration and had noticed no changes in her respiratory patterns in the last 5 years. Vitals were notable for a respiratory rate of 34 and a heart rate of 110 for which her primary team started her on propranolol. Physical exam was notable for a visible, and mobile goiter (Figure 1). She had no known allergies and was not taking any medications. Family history was noncontributory. There was no familial or personal history of complications with anesthesia, and no prior intubations. Surgical history was pertinent for a prior cesarean section. American Society of Anesthesiologists (ASA) physical exam score was IV.Admission two view chest x-ray was notable for tracheal deviation and subglottic narrowing (Figure 2A/B). The anesthesia team peri-operatively evaluated her, wherein she was a mallampati class II and she denied respiratory symptoms or trouble with lying flat. Beside ultrasound revealed a vascular mass with a patent trachea while upright and moderate compression when the head of the bed was less than 30 degrees. Trauma surgery was consulted for a surgical airway should intubation attempts prove unsuccessful. Trauma surgery determined the borders of the mass were unclear and expressed concerns that if intubation failed and urgent surgical exploration needed, a surgical airway would be challenging and potentially unsuccessful given the unknown anatomy. They determined the mass to be hypervascular, and a surgical airway could lead to massive hemorrhage. The case was moved to another day for a more robust evaluation of the neck mass.
Ultrasound revealed a markedly enlarged thyroid gland compatible with a goiter containing multiple enlarged nodules with two right nodules measuring 5.2 x 4 x 5 cm and 5.2 x 4 x 4.2 cm in addition to a left nodule measuring 5.6 x 4.6 x 5.2 cm. The thyroid was enlarged and heterogeneous with multiple coarse calcifications with the left lobe measuring 11.4 x 6.3 x 7.9 cm and right lobe measuring 8.6 x 5.2 x 4.7 cm. All nodules were heterogeneous with solid, mixed solid, cystic, and calcified parts. A computerized tomography (CT) neck and soft tissue scan was performed and demonstrated an enlarged heterogeneous thyroid gland with multiple coarse calcifications with the left lobe greater than right lobe (Figure 3). The left lobe measures 11.4 x 6.3 x 7.9 cm and the right lobe measures 8.6 x 5.2 x 4.7 cm, with the largest nodule in the right gland measuring 6.0 x 4.0 x 4.7 cm the upper /mid pole (Figure 4A/B).
On CT neck and soft tissue, the airway proved to be largely patent with regions of luminal narrowing (Figure 5). Otorhinolaryngology performed a flexible fiberoptic laryngoscopy and discovered a widely patent airway without significant airway compression. Both trauma surgery and otorhinolaryngology surgery opted to be available for intubation.
The decision was made to perform an awake fiberoptic intubation for patient safety in the setting of a possible difficult intubation. Induction began with 0.4 mg IV glycopyrrolate and nebulized 5% lidocaine in the preoperative area for 30 minutes. The patient was then taken to the operating room, where she was placed on standard monitors in addition to nasal cannula with capnography. A remifentanil infusion was started at 0.07mcg/kg/min and topical 4% lidocaine gel was administered bilaterally to the tonsillar pillars. After about seven minutes, the fiberoptic scope was introduced; however, despite the absence of a gag or cough reflex, the scope could not be advanced without the patient’s tongue actively fighting provider efforts. A second attempt was made with jaw lift and tongue retraction, however the patient’s tongue continued to interfere with fiberoptic scope advancement. The decision was made to abandon awake fiberoptic intubation since the patient was easily masked. Anesthesia was induced with 8% sevoflurane in oxygen with the patient in a semi-recumbent position and anesthesia was maintained with 50% oxygen and sevoflurane for a minimum alveolar concentration of 1.2 after intubation. A 7.0 reinforced endotracheal tube was inserted with the aid of a C-MAC video laryngoscope after obtaining a grade 2 Cormack and Lehane view. After confirmation of placement with end-tidal carbon dioxide, paralytic was administered (30 mg IV Rocuronium) for the surgical procedure. Additionally, the patient was given 10 mg IV Dexamethasone, 4 mg IV Ondansetron, 40 mg IV Ketamine, 2g IV Ancef, and 0.7 mg IV Hydromorphone during the case. Neuromuscular train-of-four ratio was continuously monitored and at the end of the case, the patient was reversed with 200 mg IV Sugammadex and a train-of-four with height greater than 0.9 was obtained. After full inhalational agent washout, the patient met extubation criteria and was extubated to nasal cannula without issues. In the post anesthesia care unit (PACU), she was maintained on nasal cannula with capnography in the event additional IV opioids were needed for operative pain. A fascia iliaca nerve block was placed for further pain control to minimize opioid usage. PACU stay was uneventful, and she returned to her inpatient room.
Discussion
Goiters can often be accompanied by airway deformities leading to difficult or challenging mask ventilation and or laryngoscopy. Induction of anesthesia in these cases can lead to complete airway closure, making mask ventilation and tracheal intubation difficult, leading to unintended surgical airways or cardiopulmonary mortality and morbidity [8-9]. Cardiorespiratory complications occur approximately 14.3% [8] of the time in patients with anterior or middle mediastinal masses. Cardiorespiratory signs and symptoms at the time of presentation usually confer the highest rates of perioperative complications [8-9]. Partial or complete airway closure is usually in part due to the pressure exerted on the trachea by surrounding soft tissue especially during periods of tissue relaxation such as during sleep, sedation and under general anesthesia. Induction of anesthesia can result in increased relaxation of soft tissues which causes the soft tissue to collapse onto the surrounding airway, increasing the pressure being exerted on the trachea. This mass effect on the trachea can be alleviated or worsened in certain positions due to gravity. It is often important to probe patient history about “how they sleep” or whether being supine causes any respiratory issues. Ideally these patients should be preoxygenated and intubated in the position most comfortable to them. This is the position least likely to cause respiratory symptoms, panic and is most likely to avoid tracheal compression.
Many techniques can be used to aid intubation in this population. Ideally, spontaneous respiration should be maintained. Spontaneous respirations preserve negative pleural pressure, which allows for patency of the airway. Thus, sedation should be minimized, or providers should use sedative agents that minimally affect respiratory function and tone. These agents include ketamine, dexmedetomidine and ultra-low doses of remifentanil. When possible general anesthesia should be substituted for neuraxial or regional anesthetic techniques as these techniques offer lower potential for respiratory depression, apnea and or loss of airway.
Depending on anesthesiologist preference, techniques such as awake direct laryngoscopy, awake tracheostomy, awake fiberoptic intubation or awake rigid bronchoscopy may be utilized. Awake fiberoptic intubation has won favor with many anesthesiologists given its versatility and its ability to allow continuous ventilation if placed through a laryngeal mask airway. There is no significant difference in the first attempt success rates of fiberoptic intubation and video laryngoscopy [3]. Alhomary et al. found that intubation times were shorter for video laryngoscopy and there were no significant differences in failure rates [3]. There was no difference when comparing adverse events like postoperative hoarseness, sore throat, or low oxygen saturation [3]. In this case, awake fiberoptic intubation was unsuccessful while mask induction with sevoflurane and video laryngoscopy led to a successful outcome. Based on the current literature, video laryngoscopy and awake fiberoptic are both effective and comparable techniques, thus depending on the clinical scenario, fiberoptic intubation should not be the automatic default technique and thought and consideration should be given to video laryngoscopy or awake laryngoscopy. The competency, skill set, and experience needed by anesthesiologists for video laryngoscopy and fiberoptic are different. It is estimated that an anesthesiology needs to perform 25 fiberoptic intubations to become competent when compared only 6 video laryngoscopes for competency [10].
Conclusion
Goiters when large enough present an increased risk of cardiopulmonary complications surrounding management. For non-emergent surgeries, patients should be properly optimized. Optimization involves up to date imaging and identification of the goiter and its effect on the patient’s underlying airway. Comprehensive planning involves a multidisciplinary medical team, proper preoperative assessment, and discussion to best provide a safe outcome for the patient. Video laryngoscopy and awake fiberoptic are both effective and comparable techniques. Both techniques should be considered depending on the clinical scenario.
#Airway Management#Goiter#Difficult Intubations#Awake Fiberoptic Intubations#Video Laryngoscopy#Journal of Clinical Case Reports Medical Images and Health Sciences.#JCRMHS
1 note
·
View note
Text
Medical Video Laryngoscope

A medical video laryngoscope is an advanced medical device used by healthcare professionals, particularly anesthesiologists, emergency physicians, and critical care specialists, to visualize the larynx (voice box) and facilitate endotracheal intubation.Fully waterproof design covers the device for damage
0 notes
Text
How does one manage airway and breathing in critically ill or injured patients?
Managing the airway and ensuring adequate breathing is a critical aspect of caring for critically ill or injured patients. In emergency medical services (EMS), prompt and effective airway management can significantly impact patient outcomes. This article will discuss the essential steps and considerations in managing the airway and breathing in critically ill or injured patients. Continue reading…

View On WordPress
#advanced airway management#airway management#bag-valve-mask ventilation#basic airway maneuvers#breathing#Collaboration#communication#continuous monitoring#critically ill#documentation#emergency medical services#endotracheal intubation#injured patients#intervention#oxygen administration#oxygen saturation#pulse oximeter#rapid assessment#recognition#respiratory distress#respiratory rate#respiratory therapists#supraglottic airway devices#ventilation
0 notes
Text
If I had a nickel for every time my dad and to go to hospital for: choking on a piece of meat during a post golf meal
I'd have two nickels. Which isn't a lot yadda yadda but damn dude how do you get a piece of steak crammed that far down in your oesophagus??
#this time seems less pressing (despite being air lifted from country hospital to the royal) because he can still breath#but its pretty jammed in there and he can't swallow so will have to wait all day for endoscopy to have a look at it#and play the worst version of a claw machine game people have#last time he was all weezing and stuff because it was obstructing airway#when i saw the message the first thing i was worried about was managing my behaviour so the fam (mostly my sister) dont get mad at me#if he died i would be sad in the way people frightened of their own mortality are#not sad in the grieving and miss him way#and i dont think my siblings realise how little i like him#anyway hes not dying and will be fine but it really shifts the mood this weekend and also means mama is not moving house today#and im pretty sure i can still go to a gig tonight (hes fine. i cant do anything anyway)#but i think my sister will go off if i ask to be sure
12 notes
·
View notes
Text
asthma inhaler: hold your breath for 5-10 seconds afterwards :)
me, a wind musician: oh, is that all? i can give you 30, easy
#my airways still constrict sometimes but i managed to specialize my way out of reduced lung capacity lol#in fact it is larger than average thank u contrabassoon & sousaphone#vanitas vanitatum et omnia vanitas
3 notes
·
View notes
Text
Excerpt from Restaurant Confidential: The Down and Dirty Exploits of a Restaurant Manager
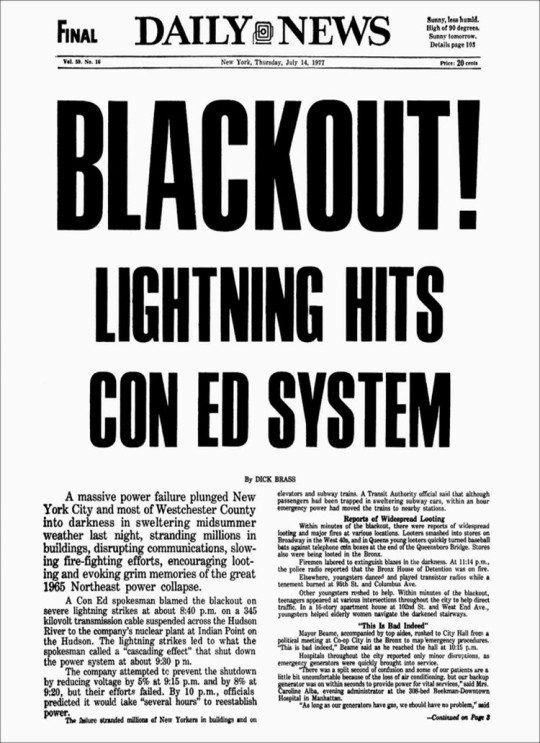
1977 Blackout in New York City
On July 13, 1977, at around 9:15 pm I am in the International Arrivals Building (I.A.B.) doing a walk-through to ensure that the food units and bars that usually close at 9:00 pm were indeed closed. I was nearing the end of my shift and my girlfriend Paula was going to pick me up in my car and we were going to go to her parents’ place in Vermont for a four-day mini-vacation. . .
Within one hour the backup lighting system failed and the airport was totally dark. Being a manager, the first thing you learn is to get the money, so I had all my management staff pull the gates in front of each bar and food operation and collect the money from the patrons. . . '
Available at Barnes and Noble - HERE
With the entire city and the airport blacked out, all flights were cancelled and literally thousands of people were roaming the airport in search of shelter and comfort.

Available at Barnes and Noble - HERE
#restaurant confidential#daniel golio#restaurants#jfk airport#1977 blackout#down and dirty exploits#restaurant manager#food and beverages#laker airways#barnes and noble#new york city
2 notes
·
View notes
Note
@clonemedickix I think that @i-outrank-everyone is trying to say is that he would not go to Camelot because it is a silly place. Exhibit A:

Also I totally forgot to tell Cpl. Glitch about that... Alas! Ah well next time, until then tell the others on her behalf, "May the wisdom and might of Odin guide you on the battlefield. and may the Valkyries guide your search for the wounded."
Your prompt says ask you anything, so here goes.
What is the forward air speed velocity of an unladen swallow?
And, do coconuts migrate?
Hello citizen....
What's a swallow? Clearly it isn't the The reflex one does with their throat..
....and what's a coconut?
Is this nat-born slang for something?
@i-outrank-everyone @is-that-regulation @fives-but-a-10 @tup-perware @hardcase-ct-yolo @arc-trooper-juicy-j @hevy-lifter
Do you boys know what this is?
Hell @howl-like-u-mean-it @a-1010-is-speaking @every-rose-has-one @massiff-daddy @its-capt-traitor-to-you vod, you deal with civilians, what are these things?
Captain Rex | CT 7567
#Two fist those horns#you're not too drunk till the OPA doesn't gag#airway management#gonna go party on Hosnian Prime#too bad you’ll be busy#it’s all fun and games til the Corries show up#jango's boyz#i outrank everyone#captain rex rp#kix rp#jango’s boyz#rp#captain rex#ask response#starwars fandom#the clone wars
96 notes
·
View notes
Text
Why does life ALWAYS have to be shit
#summer was fine except for everything that started breaking in here#this winter has been fucking dark#and i wanna fucking die#crying tonight because my skin fucking burns and rashes every time i wash my face at night bc everything in the bathroom is moldy#like everything is black and or gray#i barely even shower because it smells so bad in there#it wasn't supposed to do this and we have the theory this place was moldy when we bought it#especially the bathroom bc the shower wasn't finished and we've been too broke to fix it at all#the mattress has black mold everywhere even on the outside of a sealed mattress protector with an antimicrobial coating#my hormones and health have been fucked up since November#weather wise this is one of the coldest and wettest winter in this area in like 40+ years#the last three days i have had to stay up all night to make sure the water doesnt shut off freeze in the pipes or flood managing that 24/7#bc on valentines day it dumped more snow than an average winter should have here in 24 hours and then dropped below freezing#i got my psoriasis and eczema back#i have thrush now#i can't breathe most the time bc my throat has been reacting like anaphylaxis and my airways start to close#oh and on top of that my husband just hasn't been working for a month bc there's no work at his job so we have all of 0.54 cents in account#we gotta pay rent in a week hopefully we don't get kicked out og where we're parking#and bc of the work stuff we can't move for a few months till we can get enough saved to do that and so im stuck here#i live in abject squalor#oh also did i mention everything i own has to fit into two cupboards now due to the mold ruining all our shit#and all the cupboards but two are rotted out#and the floor in our room is peeling up and breaking off bc of the mold#we both are having an incredibly hard time mentally#my txt
3 notes
·
View notes
Text
#Asthma symptoms#Asthma triggers#Asthma management#Asthma inhalers#Asthma medication#Bronchospasm#Airway inflammation#Asthma attack#Respiratory health#Asthma prevention#Asthma treatments#Shortness of breath#Wheezing#Asthma control#Chronic asthma#Exercise-induced asthma#Allergic asthma#Asthma flare-up#Asthma diagnosis#Peak flow meter#Asthma exacerbation#Asthma action plan#Asthma relief#Asthma management plan#Air quality and asthma#Asthma triggers in winter#Asthma and allergens#Asthma during exercise#Pediatric asthma#health & fitness
1 note
·
View note
Text
Industrial Snapshot of Airway Management Devices Market

The Airway Management Devices Market Report is a treasured source of insightful data for business strategists. It provides an in-depth assessment of numerous features of industries like market overview, present progress valuations, historical and future Studies, current trends, SWOT valuations, and clients operating in several regions. The study provides valuable information to magnify the understanding, scope, and segments of this report. The report covers a comprehensive analysis of Airway Management Devices Market segmentation and regional and country breakdowns. This research will offer a clear and exact idea about the whole industry to the readers to make beneficial decisions.
According to Straits Research, the global Airway Management Devices market size was valued at USD 1.7 billion in 2023. It is projected to reach from USD 1.8 billion in 2024 to USD 2.8 billion by 2032, growing at a CAGR of 5.2% during the forecast period (2024–2032).
This study pinpoints noteworthy trends influencing the trajectory of the Gesture Recognition market's expansion. Within this recently issued report, crucial dynamics encompassing drivers, limitations, and prospects are underscored. These aspects hold relevance for well-established market entities as well as emerging stakeholders engaged in the realms of production and supply.
Request a Sample Report @ https://straitsresearch.com/report/airway-management-devices-market/request-sample
Competitive Analysis
The report contains an in-depth analysis of the vendor’s profile, including financial health, business units, key business priorities, SWOT, strategies, and views.
Medtronic
Teleflex Incorporated
Ambu A/S
Smiths Medical
Medline Industries, Inc.
Armstrong Medical Inc.
GENERAL ELECTRIC COMPANY
SonarMed
Mercury Medical
Smiths Group plc.
The vendors have been identified based on the portfolio, geographical presence, marketing & distribution channels, revenue generation, and significant R&D investments.
Request Sample Report of Global Airway Management Devices Market @ https://straitsresearch.com/report/airway-management-devices-market/request-sample
Vendors across different verticals are planning for high investments in this market, and as a result, the market is expected to grow at an impressive rate in the upcoming years. The key players are adopting various organic and inorganic growth strategies such as mergers & acquisitions, collaboration & partnerships, joint ventures, and a few other strategies to be in a strong position in the global market.
Market Segmentation Analysis
The report provides a wide-ranging evaluation of the market, providing in-depth qualitative insights, historical data, and supportable projections along with the assumptions about the Airway Management Devices Market size. The projections featured in the report have been derived using proven research methodologies and assumptions based on the vendor’s portfolio, blogs, white papers, and vendor presentations. Thus, the research report represents every side of the Airway Management Devices Market and is segmented on the basis of regional markets, offerings, applications, and end-users.
By Product
Supraglottic Devices
Infraglottic Devices
Resuscitators
Laryngoscopes
By Application
Anesthesia
Emergency Medicine
By End-User
Hospitals
Home care
Access Detailed Segmentation @ https://straitsresearch.com/report/airway-management-devices-market/segmentation
Regional Analysis
North America held the largest Airway Management Devices Market share in 2018 and is expected to dominate the market during the forecast period. The market will experience a steep rise in the following regions covered- North America, Europe, Asia Pacific, Latin America, and the Middle East & Africa.
Benefits
Buy Now: https://straitsresearch.com/buy-now/airway-management-devices-market
0 notes
Text

#Global Airway Management Devices Market#Global Market#Market Research Reports#Market News#Market Updates
0 notes
Text
Gov't schools to close in face of stormy weather
NRA crews service drains before the expected downpour (CNS):��Government schools on Grand Cayman and Cayman Brac, including the University College of the Cayman Islands, will be closed on Monday as a potential storm develops south of Grand Cayman. Cayman Prep has confirmed it will close and other private schools are also expected to cancel classes tomorrow. Government officials said they are…
#Cayman Airways#Cayman Islands National Weather Service#Featured#flooding#Hazard Management Cayman Islands#National Roads Authority
0 notes
Text
Experience Mini Airways: The New ATC Game in Town

Mini Airways real-time management game as an air traffic control with a Demo for Linux, Mac, and Windows PC. Thanks to the creative minds at CCC Games. Working to make its way onto Steam in 2024. Mini Airways is a minimalist-style ATC (Air Traffic Control) simulation made by four flight simulation fans. If you like real-time management titles like Mini Motorways, you’re due to dig this one too, but with a fresh twist. In Mini Airways, your job is to clear planes for takeoff and landing, direct them to their destinations, and most importantly, make sure they don’t crash. You’ll get to test your ATC skills in famous cities like London, Tokyo, and Shanghai. Since each map offers its own unique tests. Earlier this year, the demo and free Prologue hit Steam, and the feedback has been amazing. Gamers have racked up over five hours of playtime on the free demo alone! The team behind the title, CCC Games, has also been hard at work improving it. While releasing a brand-new Linux demo in the Steam Next Fest. Manage Your Airways In Mini Airways, you’ll have to manage aircraft takeoffs and landings, handle various airways and traffic flow. All while keeping flights orderly, and avoid any fatal collisions. Your tasks include scheduling aircraft and guiding them safely to their destinations. Watch out for random events like failed landings, mountainous terrain, and no-fly zones. Staying alert is key.
Mini Airways Announcement Trailer
youtube
Upgrade Your Airspace After a day of managing the skies, you get to upgrade your airspace and airport. Options include auto holding, accelerating turns, expanding airspace, and more. Smart use of these upgrades will make your job a lot easier. Expressive Level Design Even though the Mini Airways art style is minimalist, the features authentic air traffic control voices and ambient sounds that really pull you in. This title focuses on expanding airport levels, giving you a new experience each time. Hidden aircraft call signs, cute character voices, and unpredictable random events add even more variety. Map Editor One of the best features is the player-customized map editor. Since you can design your dream airport and bring it to life. It’s a fantastic way to get creative and add a personal touch to the game. Mini Airways real-time management is available as a free to try on Steam for Linux, Mac, and Windows PC. Give it a try and see if you’ve got what it takes to be an air traffic control pro. The release is due int Q3 2024.
#mini airways#real-time management#air traffic controler#linux#gaming news#ccc games#ubuntu#mac#windows#pc#unity#Youtube
1 note
·
View note
Text
Airway Management Devices Market was valued at US$ 1.5 billion in 2020 and is expected to grow at a CAGR of 6% over the forecast period (2021-2027).
0 notes