We're America's most trusted provider of sexual and reproductive health care, and we think we look pretty good for 104 years old.
Don't wanna be here? Send us removal request.
Text
8 Conversation Tips on the Importance of Sex Education

We each bring our individual sparkle to video gatherings. So, make a commitment to let your advocacy shine during Zooms with friends and family! Support the movement for bodily autonomy by illuminating your next video chat with insights about the state of sex education in America.
We know — starting a conversation with your family (or with anyone over video) can seem awkward. Don’t worry! We’ve got 8 tips to sail through the convo.
Tip #1: Get the conversation going in a way that’s welcoming.
If you’re at a virtual hangout, share how important education is to you. Encourage each person to share the topic they believe is essential for young people to learn.
When the time is right, say something like: “For me, sex education is one of the most important forms of education a young person can have today.”
Tip #2: Take Time for Q&A
Ask the adults:
“What do you remember about your own sex education?”
“If you received sex education, what would have made it more helpful?
“If you have kids, how would you like sex education to be taught to them?”
Ask any young people on the call: “Do you have thoughts about or experiences with sex education that you feel comfortable sharing?”
Ask everyone: “Would you like to hear some facts about sex education and where we are as a country with it?” If people seem engaged, then move to Tip #3.
Tip #3: Explain what sex education is and why it’s important to talk about.
Sex education is more than just putting condoms on bananas. It's even beyond sexually transmitted infection (STI) prevention and avoiding unintended pregnancy! Sex education is a foundation for our development as people.
Sex education helps young people make healthy decisions about their bodies, relationships, and how they express their gender and sexuality — without fear or shame.
Sex education covers a wide range of age-appropriate topics, such as:
Physical dimensions of sexuality, like puberty, pregnancy, and STIs
Emotional dimensions of sexuality, such as feelings of connection and self-esteem
Identity and sense of self, including gender identity and personal values
Healthy relationships, including platonic relationships, intimate relationships, and dating
Communicating boundaries, including both listening and speaking up
Tip #4: Drop some knowledge about the benefits of and public support for sex education in America.
The benefits: Sex education is proven to increase safer sex and help young people prevent unintended pregnancy. It’s also linked to reducing transphobia, homophobia, and sexual assault.
The support: Public opinion overwhelmingly supports sex education across geographic and political lines. Among parents of middle and high school students, over 80% believe sex education is important for middle schoolers, and 98% believe it's important for high schoolers.
The problem: Too few young people get the sex education they need and deserve.
Tip #5: Explain what’s getting in the way of sex education at the state level.
Almost every state has some guidance on how and when sex education should be taught, but decisions are often left up to individual school districts.
That means state and local politicians decide whether or not educators can discuss birth control; how educators can talk about LGBTQ+ experiences (if at all); and how much educators must stress abstinence until marriage.
Only 30 states and the District of Columbia mandate sex education. But just because a state mandates sex education doesn’t mean that it’s good or comprehensive! Of the states that mandate sex education, very few have high-quality standards:
Only 20 states and DC require information about contraception.
Just 17 states require what’s taught to be medically accurate.
Merely 11 states require sex education to have LGBTQ+ content and inclusive language.
Tip #6: Explain the problems with abstinence-only-until-marriage programs.
Abstinence-only programs:
Focus on deterring students from having sex, often by scare tactics and withholding information
Often blame survivors for their own sexual assaults and ignore the needs of LGBTQ+ teens
Leave a population of sexually active people uninformed and vulnerable
Studies show that abstinence-only programs are ineffective — they don’t decrease STI or unintended pregnancy rates.
Studies also show that abstinence-only programs are harmful — they reinforce damaging gender stereotypes, stigmatize or exclude gender nonconforming people, and violate a basic human right of young people to access accurate health information.
Despite all this, Congress poured $2.1 billion taxpayer dollars into abstinence-only-until-marriage programs between 1996 and 2018.
Tip #7: Say what people can do to help.
Encourage your friends and family to share local and national news about sex education on social media, along with what they may have learned in this conversation.
You can also encourage people to contact their members of Congress and advocate for sex education, such as by:
Ending federal funding for programs that promote abstinence-only-until-marriage, gender stereotypes, and medically inaccurate information
Supporting initiatives that promote sex education and access to sexual health services for young people — like the Teen Pregnancy Prevention Program, the Personal Responsibility Education Program, and the Real Education for Healthy Youth Act
Tip #8: Thank everyone for having the conversation with you.
Express heartfelt gratitude for each person who joined in the conversation, and any person who just listened.
Whether the conversation was challenging or a breeze, remember this: It could be a gateway to other meaningful interactions about issues you care about.
Pat yourself on the back for taking this big step!
#sex education#let's talk about sex#sex ed#conversations#abstinence#abstinence-only#abstinence-only programs#Sex Ed for All
333 notes
·
View notes
Photo


it’s okay to be demisexual / demisexuality is a real and valid sexuality / you deserve to be respected as a demisexual person/ it’s okay to be proud of your demisexuality
2K notes
·
View notes
Photo

stimming on T ! autistic/adhd trans people we are the coolest
23K notes
·
View notes
Text
9 Conversation Tips on Race & Health Equity
Seeing friends or extended family by video? You can have a huge impact by talking to them about issues that are important to you. Take the opportunity to discuss health care access for communities of color.
Here are 9 tips for leading the conversation. Remember: Talking with your friends and family about the issues you care about can have a real influence that extends even beyond your circle.
Tip #1: Open the dialogue in a way that’s welcoming.
Share how the last couple of years have affected your views on health and health insurance. Say something like, “I’ve been [concerned/angry] about COVID-19’s disproportionate impact on [Black and Brown communities/our community].”
ASK: “Could we talk about how racist our country’s health care system is? I have some ideas about what can be done, and I’d love to hear your take.”
Tip #2: Get everyone on the same page by defining common terms.
Racism
Racism in America is the outgrowth of white supremacist policies and ideas that assume white people are superior to other racial groups.
Racist policies are written and unwritten laws and customs that cause racial inequity, putting racial groups on unequal footing.
Public Health
Public health is built on the principle of protecting and improving the health of people and their communities.
A public health crisis happens when something threatens the lives and health of an entire community or multiple groups of people.
ASK: Have you [seen/experienced] racism in health care?
Tip #3: Define some terms about race that are less common.
Anti-Blackness refers to a worldwide ideology that devalues being Black.
Anti-Black policies and institutions in white supremacist systems dehumanize and marginalize Black people around the world.
Anti-Black racism covertly disregards and overtly attacks anti-racist policies, Black people, and Black institutions.
Structural racism is a system in which policies, practices, and other norms perpetuate racial inequity. It’s the root cause for the health inequities we see today.
Racial inequity in America blocks Black and Brown people from living freely and safely — while putting white people in power, giving them more resources, and chipping away at their humanity.
Racist health care policies cause health inequities for racial groups, fortifying long-standing barriers and creating new barriers to health care access for Black and Brown communities.
Tip #4: Define some terms about health and fairness that are less common.
Equality vs. Equity
Equality gives everyone the same exact things, but ignores differences. Equal access to COVID-19 testing means everyone could theoretically get a test. But for many people, testing is too expensive and far away, or only open at times where they are unable to take off work or get childcare.
Equity gives everyone what they need, tailored to their individual situation. Equitable access to COVID-19 testing would be affordable, nearby, and have flexible hours for everyone.
Health Inequities vs. Health Equity
Health inequities are systemic, avoidable, and unjust differences in the health of a group of people compared to other groups.
Health disparities are any kind of differences in health outcomes for a group compared to other groups. Disparities don’t refer to social or structural causes like inequities do.
Health equity happens when everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as: poverty, discrimination, powerlessness, limited education, unstable housing, unsafe environments, and lack of health insurance.
Tip #5: Provide examples of racial and health inequities.
Racism is embedded in the structure of the U.S. health care system. The people in charge of that system — including politicians and insurers — have carried out discriminatory practices throughout its history.
Institutionalized discrimination in the U.S. health care system has thrown up roadblocks to insurance, testing, treatment, and care for communities of color. That includes the system’s reliance on employer-sponsored insurance. Because of historic economic barriers, Black and Brown people are less likely to be working in jobs that offer this benefit.
Racial bias among medical researchers and health care providers — such as the erroneous belief that Black people feel less physical pain — have withheld needed care and pain management from Black patients.
Being Black in America takes a toll on the health of Black people.
Racism, microaggressions, and discrimination cause chronic stress.
Researchers have shown that racism stresses and prematurely ages human cells.
All that stress causes physical and psychological harm over time.
The result: increased rates of illness and death among Black people.
Tip #6: Share how health care inequities have led to dramatic disparities in health conditions for Black and Brown communities.
Racial and health inequities help explain why — regardless of income or education — Black and Brown patients have disproportionately fared worse compared to their white counterparts across many health outcomes.
Racism’s chronic stress is linked to higher risk of depression, diabetes, and high blood pressure.
Black people disproportionately experience police-inflicted harassment, violence, injuries, and murder. Living in fear of state-sanctioned brutality causes a host of underlying health problems.
Because of racist policies like redlining, Black and Brown people are more likely to live near toxic sites and amid high pollution, as well as in neighborhoods that lack healthy food options and places to exercise. These environments are linked to higher rates of asthma, respiratory illnesses, and cardiovascular disease.
Long-standing, systemic health and social inequities in the United States and discrimination in doctors’ offices and hospitals all have resulted in a high maternal mortality rate among Black women — three times the rate for white women.
Structural racism, public health failures and economic inequalities — including that the location of Black and Brown workers’ jobs are more likely to put them at risk of catching COVID-19 — have all translated to exponentially higher COVID-19 infection and death rates in Black, Indigenous, and Latino communities.
Tip #7: Discuss why racism is a public health crisis.
The American Medical Association, the American Public Health Association, several states, and other U.S. institutions declared that racism is a public health crisis and called for urgent action from policymakers and institutions.
Discrimination creates barriers to health, both inside and outside the doctor's office. Your health depends on whether you can access health care, employment, good wages, food security, clean air and water, and stable housing — all of which are hurt by racism.
SCROLL UP: Refer to the definition of “public health crisis” and share how you feel about it.
ASK: “How do you feel about racism being declared a public health crisis?”
Tip #8: Share what federal policies you support to address racial inequity.
For example, you may want them to support policies that:
Aim to eliminate the inequities and biases woven into the fabric of this nation’s institutions, particularly the racial inequities in maternal health.
Provide additional COVID-19 relief that helps Black, Indigenous, and Latino communities — which have been disproportionately ravaged due to ongoing systemic racism and oppressive policies.
Defund the police. Instead of investing in police forces that brutalize Black people, prioritize a public-health approach that strengthens Black communities, promotes community support, and connects people to services.
Support Black organizations and leaders who are at the forefront of the fight to fix the public health crisis that racism presents and the systems that exploit people of color.
Tip #9: Express gratitude for everyone in the conversation.
Thank your friends and family for connecting with you on this issue, and let them know that you’re open to speaking with them again.
Show them some warmth — and give them the time and space to sit with the discussion.
230 notes
·
View notes
Photo



Disney princesses at the gynecologist are bringing awareness to women’s health
870 notes
·
View notes
Text
8 Conversation Tips on Abortion Rights

Words are powerful. One heart-to-heart with your family could influence their perspective on the issues you care about — like abortion access. In turn, your family could share what they learn with their wider circles. That ripple effect is key to widespread social change.
Are abortion rights important to you? Do you feel safe talking about it with your family? Here are 8 tips for starting a conversation about abortion rights at a virtual dinner.
At the end of your convo, remember the most important part: expressing gratitude.
Tip #1: Welcome your family into the conversation.
If your family members are taking turns to share what’s on their mind, use your turn to share that you’ve been thinking about abortion rights.
Note the values you and your family share, such as the core values of love, fairness, and compassion.
Say something like, “It’s because I care so much about others that I believe decisions on whether to choose adoption, end a pregnancy, or raise a child must be left to each individual — not to politicians, who can’t know each individual’s situation.”
Ask if it’s OK to start a discussion about the laws restricting access to safe, legal abortion. If people are up for it, proceed to Tip #2.
Tip #2: Fire up some facts about abortion access.
The Supreme Court case Roe v. Wade affirmed the constitutional right to abortion in 1973.
Today, the vast majority of Americans — 77% — support keeping abortion legal and don’t want Roe v. Wade overturned.
ASK: “Do you believe everyone should be able to access the full range of reproductive health care, no matter how much money they make or where they live?”
Tip #3: Explain who gets hurt by bans and restrictions on abortion.
Restrictions on abortion have created costly barriers to care, such as forcing patients to travel long distances to the closest abortion provider, and to take time off work to comply with medically unnecessary waiting periods and multiple appointments.
Since nearly 6 out of 10 people who have abortions are already parents, obtaining an abortion requires many patients to arrange for child care.
Restrictions push safe, legal abortion out of reach for people who can’t afford these costs. It’s hardest on people who already face barriers to health care overall, including people with low incomes, people who live in rural areas, and Black and Brown people.
Tip #4: Note challenges to abortion access in the states.
Since 1973, states have enacted over 1,000 abortion restrictions — and nearly 40% of those restrictions became law in just the past decade.
Because of abortion restrictions, five states — Mississippi, Missouri, North Dakota, South Dakota, and West Virginia — have only 1 abortion provider left.
11 state governments used COVID-19 as a pretense to temporarily ban abortion by labeling it “non-essential” health care during the pandemic.
Tip #5: Explain why abortion should be available to all, not just those who can afford it — and why the Hyde Amendment is both racist and discriminatory.
The Hyde Amendment is one of the longest-running federal restrictions on abortion access. Since 1976, Hyde has barred people from using Medicaid and other federal health coverage for abortion.
Nationwide, Medicaid covers 1 in 5 women of reproductive age. Of those 16.1 million Medicaid participants, 55% live in states where Hyde forces them to pay for abortion out of pocket.
Hyde is particularly harmful to people with low incomes, people of color, and young people — who, because of systemic discrimination and a history of economic barriers, disproportionately use Medicaid for their health care coverage.
ASK: “Do you believe abortion should be covered in health care plans, no matter who provides the insurance?”
Tip #6: Explain what’s happening in the courts.
Right now, there are at least 19 abortion-related cases one step away from the U.S. Supreme Court. It’s possible that safe and legal abortion access could go back to where it was before Roe v. Wade.
If Roe v. Wade is overturned, individual states will decide whether abortion is legal. That means 1 in 3 women of reproductive age — more than 25 million women — would be living in states without legal abortion.
Banning abortion won’t stop abortion. But it will stop people from accessing safe, legal abortion. The cost: pregnant people’s health, and even their lives.
Tip #7: Advocate for policies that the federal government should support in order to protect and expand abortion access, such as:
Ending the Hyde Amendment
Changing rules and regulations to protect people from discrimination by health care providers and insurers
Lifting restrictions on private insurance for abortion so that fewer people are forced to pay out-of-pocket for safe, legal abortion
Tip #8: Say ‘Thank You’
If it feels right, express gratitude at the end of the discussion — both for everyone who joined in the discussion, and everyone who listened.
304 notes
·
View notes
Text
Do virgins need Pap tests?

Someone asked us:
Do virgins need Pap smears? I'm 24 years old, have never had sexual contact of any kind, and I know you're supposed to start getting them at 21. Is it even possible for me to get the cancers Pap smears screen for? Is there an age that I should start getting them even if I haven't had sex? I'm asexual, aromantic, and have never had a sex drive, so I'm not worried about ever catching HPV or developing any virus-caused cancers, but is there anything else a Pap test is for?
Going to the doctor for a wellness visit is important, whether you’re sexually active or not. Your doctor or nurse will tell you which tests you need and how often you should get them. But if you haven’t had any sexual contact with anyone, your nurse or doctor may decide not to perform a routine Pap test (AKA Pap smear).
Sexually active people between the ages of 21 and 25 need to get a Pap test once every three years to check for abnormal cells in the cervix that are caused by HPV. HPV is spread by skin-to-skin contact with genitals, as well as oral, vaginal, and anal sex. Abnormal cells in the cervix can lead to cervical cancer, so it’s important to get a Pap test when your nurse or doctor recommends it.
You can schedule a wellness visit at your local Planned Parenthood health center.
-Attia at Planned Parenthood
213 notes
·
View notes
Photo

We’re shouting it LOUD for everyone to hear
On Wednesdays #WeWearPinkAnd…#StandWithPP!
With reproductive health care under attack, your voice is needed NOW!
Call your senator and tell them why you Stand With Planned Parenthood: istandwithpp.org/call
1K notes
·
View notes
Photo
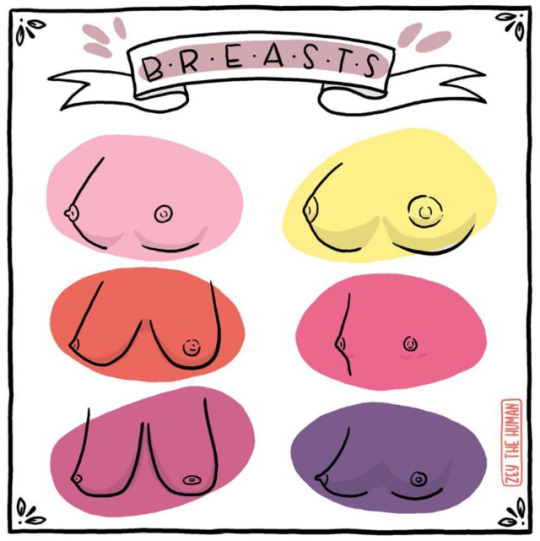
…come in different shapes and sizes <3
Drawn digitally using Photoshop. April 2017.
696 notes
·
View notes
Text
7 Conversation Tips on LGBTQ+ Rights

When the people in your life gather together for a video chat, you have an opportunity to get the conversation going about the issues you’re passionate about.
In fact, talking to your own family is an essential step for social change. (Yes, YOUR family.)
Is LGBTQ+ health care policy important to you? Do you feel safe talking about it with your friends and family? Then follow these 7 tips on fostering a genuine discussion and sparking real insights.
Tip #1: Discuss why you care about LGBTQ+ rights.
Every person — no matter their gender identity, sex, or sexual orientation — deserves equal access to health care. But lesbian, gay, bisexual, transgender, nonbinary, and queer communities, as well as people with other sexual and gender expressions (LGBTQ+), face systematic harassment and discrimination in the U.S. health care system.
Nearly 1 out of 10 LGBQ patients and 3 in 10 transgender patients say a health care provider has refused to see them because of their sexual orientation or gender identity.
A whopping 70% of transgender, gender nonconforming and nonbinary people say they’ve faced serious discrimination in the health care system.
ASK: What would you do if your health care provider was rude to you, belittled your concerns, or refused to see you? And what if it wasn’t so easy to find another provider?
Tip #2: Dive deeper into the barriers LGBTQ+ people face in accessing health care — and the consequences.
LGBTQ+ people also face higher rates of unemployment and poverty, which are linked to low rates of health care coverage.
Both discrimination and lack of insurance coverage get in the way of LGBTQ+ people’s access to health care services.
Those structural barriers are linked to worse health outcomes for LGBTQ+ people.
Tip #3: Fire up some facts about LGBTQ+ health care policy.
The Affordable Care Act (ACA) expanded health coverage for LGBTQ+ people.
Before the ACA went into effect in 2013, 34% of LGBTQ+ people who earn less than $45,000/year were uninsured.
That uninsured rate has since dropped by half and is now 16%.
Tip #4: Emphasize why we need to protect LGBTQ+ people’s access to health care.
Efforts to chip away at LGBTQ+ people’s rights could cause many LGBTQ+ people to lose access to health care — including people who have low incomes; live with chronic illness; or have pre-existing conditions.
Transgender, gender nonconforming, and nonbinary people face particular consequences to losing health care access.
Like everyone, LGBTQ+ people are living in the pandemic. That makes health care access even more important.
Tip #5: Explain the continuing challenges in the courts.
Former President Trump seated over 220 judges on our nation’s federal courts, including three Supreme Court justices.
Many of these powerful judges have ruled against or expressed hostility to LGBTQ+ rights.
ASK: Can you imagine how scary it is for people who already face discrimination in different areas of their lives to see judges with these records fill lifetime positions on the courts?
Tip #6: Discuss changes you’d like to see in the U.S. government. Those changes may include supporting the government in ending the Title X gag rule:
The gag rule censors the information health providers can share with patients who rely on Title X, the only federal program dedicated to free and reduced-cost preventive sexual and reproductive health care.
This gag rule forced Planned Parenthood out of the Title X program.
Ending the Title X gag rule would allow LGBTQ+ patients to once again obtain affordable care through Title X at Planned Parenthood health centers, which are safe and welcoming to LGBTQ+ patients.
Tip #7: Express gratitude for everyone in the conversation.
Thank your friends and family members for engaging with you in what can be a challenging conversation. And remember — it’s not just one talk. Strong allyship and real learning requires having conversations not just once, but over and over again.
270 notes
·
View notes
Text
How can I become more confident with the way my genitals look?
youtube
Everyone’s genitals are a little different — yours are unique to you. Penises can be big or small, thick or thin, long or short, straight or with a little curve. Vulvas and labias can be big or small. Some people have wide vaginal openings, others have smaller ones. Genitals come in many different skin colors and tones, from dark brown to purple to tan to light pink, with many different textures, as well as types and amounts of pubic hair.
It may take time to feel confident about your genitals, but remembering that you’re “normal” and unique is the best way to feel comfortable in your own skin. Try talking with a parent or another adult you trust about your feelings: it might be awkward or scary at first to bring it up, but they can give you support and love as you get to know your body.
-Attia at Planned Parenthood
134 notes
·
View notes
Photo

Trans women are women.
Created digitally using Photoshop. March 2017.
2K notes
·
View notes