#which would put him no older than 17 developmentally
Text

By: Leor Sapir, Joseph Figliolia
Published: Nov 8, 2023
Fenway Community Health Center in Boston, the largest provider of transgender medicine in New England and one of the leading institutions of its kind in the United States, was named a defendant in a lawsuit filed last month. The plaintiff, a gay man who goes by the alias Shape Shifter, argues that by approving him for hormones and surgeries, Fenway Health subjected him to “gay conversion” practices, in violation of his civil rights. Carlan v. Fenway Community Health Center is the first lawsuit in the United States to argue that “gender-affirming care” can be a form of anti-gay discrimination.
The case underscores an important clinical reality: gender dysphoria has multiple developmental pathways, and many who experience it will turn out to be gay. Even the Endocrine Society concedes that many of the youth who outgrow their dysphoria by adolescence later identify as gay or bisexual. Decades of research confirm as much. Gender clinicians in the U.K. used to have a “dark joke . . . that there would be no gay people left at the rate [the Gender Identity Development Service] was going,” former BBC journalist Hannah Barnes reported. Rather than help young gay people to accept their bodies and their sexuality, what if “gender-affirming” clinicians are putting them on a pathway to irreversible harm?
Due partly to Shape’s lifelong difficulty in accepting himself as gay, his lawyers are not taking the usual approach to detransition litigation. Rather than state a straightforward claim of medical malpractice or fraud, they allege that Fenway Health has violated Section 1557 of the Affordable Care Act (ACA), which bans discrimination “on the basis of sex” in health care. In 2020, the Supreme Court ruled in Bostock v. Clayton County that “discrimination because of . . . sex” includes discrimination based on homosexuality. Citing this and other precedents, Shape’s lawyers argue that federal law affords distinct protections to gay men and lesbians—upon which clinics that operate with a transgender bias are trampling.
Shape grew up in a Muslim country in Eastern Europe that he describes in an interview as “very traditional” and “homophobic.” His parents disapproved of his effeminate demeanor and interests as a child. They wouldn’t let him play with dolls, and his mother, he says, made him do stretches so that he would grow taller and appear more masculine.
At 11, Shape had his first of several sexual encounters with older men. “I was definitely groomed,” he recounts. Shape proceeded to develop a pattern of risky sexual behavior, according to his legal complaint. He told his medical team at Fenway Health about his childhood sexual experiences, calling them “consensual.” The Fenway providers never challenged him on this interpretation, he alleges. They never suggested that he might have experienced sexual trauma or, say, explored how these events might have shaped his feelings of dissociation. (The irony is that Fenway Health describes its model of care as “trauma-informed.”)
As with the social environment they inhabited, Shape’s parents were “deeply homophobic,” he says. When Shape came out to his parents as gay at 15, they took him to a therapist, hoping that he would be “fixed.” But when he graduated high school at that same age, he moved to Bulgaria for college, and in 2007, at 17, he came to the United States for a summer program at the University of North Carolina. He later moved to Massachusetts to pursue an MBA at Clark University and immigrated to the U.S.
Though he had known about cross-dressers and transsexuals as a child (he had taken interest in Dana International, the famous Israeli transsexual who won the Eurovision Song Contest in 1998), it was only at Clark that he was introduced to the idea that some people are transgender. Other students began asking him about his pronouns and telling him about “gender identity.” After getting to know a “non-binary” person and a transgender woman, Shape started to make sense of his life retrospectively. As a boy going through puberty, he had developed larger-than-average breasts and was curvier than the other boys. It was hard for him to be accepted in the gay community, he told me, because gay men tend to value masculinity. His discomfort with social expectations about how men are supposed to look and behave, his sexual attraction to other men, his ongoing psychological and emotional distress: these were all signs, he learned from online forums, that he must have been “born in the wrong body.”
Shape quickly developed self-hatred and a strong desire to escape his body. When he started cross-dressing and presenting socially as a woman, things changed. It had been hard for him to win acceptance as an effeminate gay man, but he encountered far less hostility presenting as a woman. A subtle but important shift in his thinking took place.
“People wouldn’t take me seriously when I was a man who presented socially as a woman,” he says. “I had to actually be a woman.” Shape became immersed in online transgender culture, which told him that sex is a social construct, and that hormones and surgeries can actually turn him into a woman. As a result, Shape developed highly unrealistic expectations about what hormones and surgeries could do for him. An example noted in his legal filing: he stopped using condoms because he wanted to get pregnant.
Julie Thompson, a physician assistant and Medical Director of the Trans Health Program at Fenway Health, made no effort to perform differential diagnosis on Shape, his legal filing alleges. Shape told Thompson about his childhood sexual encounters, his troubled history of risky sexual activity, and his struggles with social and familial rejection on account of his homosexuality. Allegedly, she wrote these difficulties off as byproducts of society not accepting him as a “trans woman”—an approach known as “transgender minority stress.” Shape’s ongoing mental-health problems, it was determined, were due to “internalized transphobia.”
As Shape’s filing puts it, the Fenway clinic operated with a strong “transgender bias.” Every problem or counter-indication that came up was explained away as part of the stress that transgender people experience in an unwelcoming society. The clinicians at Fenway Health apparently assumed that sexual orientation and gender identity are two distinct and independent phenomena.
Shape was put on estrogen at age 23. According to his filing, he was not given “any explanation of the numerous potential adverse side effects of estrogen or its potentially unknown effects.” As Shape kept taking estrogen, he became even more emotional, depressed, and unstable. Notably, he did not dislike his male genitals—a fact that should have attracted more scrutiny from his clinicians—but seemed more distressed over his high sex drive and desire for intercourse with men. Though he says he frequently told his providers that he hoped “sex reassignment surgery” would reduce his sex drive, this statement did not cause them to reconsider whether estrogen was appropriate.
As the Fenway team allegedly saw it, Shape’s deterioration was evidence that he hadn’t gone far enough in his transition. They recommended that he attend First Event, a Boston-based conference held annually since 1980, where transgender people can meet one another, share ideas, interact with vendors, and find medical providers who will agree to perform procedures on them. Marci Bowers, the genital surgeon who is president of the World Professional Association for Transgender Health, has attended the conference in the past. According to Shape, the point of going to First Event was to find a surgeon who would operate on him.
He did just that, and in 2014, at 24, Shape underwent facial feminization surgery and breast implantation. Less than a year later, a surgeon surgically castrated him and conducted what’s euphemistically called “bottom surgery.” It didn’t work. As a result, Shape had to undergo several additional surgeries, the last one borrowing tissue from his colon. Still, the problems persisted.
It took Shape a few years to realize that he had made a terrible mistake. The problem he had been trying to solve all his life was not “internalized transphobia” but failure to accept himself as an effeminate gay man. His legal filing states that he had what the Diagnostic and Statistical Manual of Mental Disorders called, at the time he made contact with the clinic, “ego-dystonic homosexuality.” Because they failed to detect this and other mental-health problems, the Fenway team, argue Shape’s lawyers, “outrageously, knowingly, recklessly, and callously” led him to believe that he was really a heterosexual woman whose problems could be solved by de-sexing himself as male.
Shape was promised “gender euphoria.” Instead, he told me that he now sees himself as “mutilated.” His treatments have left him with “osteoporosis and scoliosis” as well as “mental fog,” according to his legal filing. Shape is now “faced with the impossible choice of improving his cognitive state and suffering the psychological and physical effect of phantom penis, or taking estrogen and suffering mental fog and fatigue, but no phantom penis and low libido.” He has also endured fistulas as a complication of his genital surgery and “suffers from sexual dysfunction and is unable to enjoy sexual relations.” He experiences dangerous inflammation. And not getting the mental health therapy he needed very likely caused Shape’s mental health to deteriorate throughout the several years that he was a patient at Fenway Health.
Shape now wants to have his breast implants removed. But insurance does not cover the procedure because it is not technically “gender affirming.” And since he cannot afford the hefty price tag, Shape has no choice but to live with the implants.
Understandably, criticism of gender medicine has focused largely on its use in minors. Its use in adults, however, is not without controversy. In the past, when clinicians spoke of adult transgender medicine, they were referring mainly to adult men who sought to change their bodies in their forties. Many had already spent years in marriage and were fathers of children.
That is no longer the case. Though data are limited, the main patient demographic in adult transgender clinics today appear to be 18-24-year-olds. In Finland, for example, adult referrals rose approximately 750 percent between 2010 and 2018, with 70 percent of referrals being 18-22-year-olds.
Humans reach full cognitive maturity around age 25, which means that there is often little to distinguish a 20-year-old from a 17-year-old in terms of impulse control, emotional self-regulation, and the ability to set long-term goals and prioritize them over present desires. Citing “irrefutable evidence” that being under 25 means having “diminished capacity to comprehend the risk and consequences of [one’s] actions,” the progressive decarceration and racial-justice advocacy group The Sentencing Project argues that the idea that people are adults once they reach age 18 “is flawed.”
Shortly after its founding in 1971, Fenway Community Health Center was repurposed to support the unique needs of gay and lesbian residents of Boston. According to Katie Batza, a historian of the clinic, the hippies and antiwar activists who founded Fenway Health “quickly solidified its reputation as an important gay medical institution.” During the 1980s, the clinic helped tackle the AIDS epidemic. That it now maltreats gay men like Shape by converting them into trans women reflects a tectonic shift within the institution’s culture.
American medicine has always found itself balancing two competing tendencies: the paternalism of care by experts on one hand, and the relativism of nonjudgmental customer service on the other. What has happened over the course of Fenway Health’s five decades of existence is a gradual loss of that equilibrium. Fenway has long defined its mission in terms of responsiveness to the stated needs and desires of community members: the volunteers who ran the clinic and offered its services free of charge, Batza writes, “focused on providing care and building community among Fenway residents, caring less if a volunteer met outside standards of professional qualification, which were often set by the state or medical profession, that the clinic critiqued.”
In the 1990s, the clinic set up a dedicated transgender unit. At first, “things moved slowly,” recounts Marcy Gelman, a nurse practitioner who served as Fenway Health’s first dedicated provider for transgender patients, in a document published by the institute about the history of its program. She is now its associate director of clinical research. “Patients didn’t get hormones right away. We wanted to get to know them, and required them to see a therapist for several months . . . we wanted to be careful.” This process felt too restrictive for some patients, and “a few got really angry.” Fenway Health says its “commitment to ensure patient safety . . . led to some conflicts with patients and community members.”
In the 2000s, Fenway Health adopted a new model of care for its transgender-identified patients, which it called the “informed consent model.” This came in response to patients complaining about “needless gatekeeping” and concerns that the clinic’s “customer service training specific to transgender patients lagged behind the development of its clinical care.” Using funding from the Blue Cross/Blue Shield Foundation, Fenway Health made a number of new hires and expanded its program. It drew inspiration from another community health clinic, the Mazzoni Center in Philadelphia, which was smaller than Fenway but served four times as many patients. “One key to [the Mazzoni Center’s] success,” the Fenway document explains, “was the elimination of any requirement for counseling before hormones were provided.” Ruben Hopwood, a physician who joined the Fenway team in 2005, developed this model for Fenway; soon thereafter, the institution’s three-month counseling requirement gave way to “a single hormone readiness assessment visit.”
In 2012, the World Professional Association for Transgender Health published the seventh version of its Standards of Care. In the chapter on hormone therapy, WPATH recommended eligibility criteria for estrogen or testosterone, including “persistent, and well-documented gender dysphoria” and having ongoing “medical or mental health concerns . . . reasonably well-controlled.” However, WPATH also noted a newly emerging “informed consent model” and cited Fenway Health as one of three clinics that developed and practiced it.
The difference between the models, WPATH explained, was that SOC-7 put “greater emphasis on the important role that mental health professionals can play in alleviating gender dysphoria and facilitating changes in gender role and psychosocial adjustment. This may include a comprehensive mental health assessment and psychotherapy, when indicated.” By contrast, Fenway Health’s model emphasizes “obtaining informed consent as the threshold for the initiation of hormone therapy in a multidisciplinary, harm-reduction environment. Less emphasis is placed on the provision of mental-health care until the patient requests it, unless significant mental health concerns are identified that would need to be addressed before hormone prescription.” Despite the obvious differences, WPATH insisted the two models were “consistent” with each other.
Currently, Fenway Health offers hormones on the informed-consent model. “Criteria for accessing hormone therapy,” it states, “are informed by the WPATH (World Professional Association for Transgender Health) guidelines.” In other words, Fenway Health defers to WPATH, which adopted its recommendations from Fenway Health.
Shape and his lawyers deny that Fenway’s informed consent process is “a safe and effective replacement for assessment, diagnosis, and treatment provided by an appropriately trained and licensed healthcare professional.” Fenway’s model, they argue, “relies heavily on patients’ self-diagnosis, which may be a result of confusion or a misunderstanding of medically defined terms.” It does not take into account a patient’s expectations from medical treatment, which, as in Shape’s case, can be highly unrealistic. It “does not inform patients about the risk of iatrogenic effects of affirmation.” Nor does it take into account a patient’s “medical decision-making capacity,” which may be impaired in the presence of “significant emotional distress” and “undue influence from persons in position of authority and trust.”
A key charge in Shape’s lawsuit is that Fenway Health is driven by “market expansion goals and political demands of transgender activists.” Approval for hormones and surgery, the clinic’s staff wrote in 2015, should be a “routine part of primary care service delivery, not a psychological or psychiatric condition in need of treatment.” A leading advocate for the no-gatekeeping model, which rests on the assumption that mismatch between one’s actual and perceived sex is a normal human variation and not a pathological condition, argues that adults and adolescents should be free to turn their bodies into “gendered art pieces.”
From Shape’s story, we can infer that Fenway Health, which could not be reached for comment, has yielded to a barely constrained medical consumerism. In 1997, the institute had eight transgender customers. By 2015, it had over 1,700. “The rapid and sustained growth of Fenway Health’s transgender health care, research, education, training, and advocacy,” the institute’s doctors proudly declare, “might be succinctly summarized by the mantra from the movie Field of Dreams: If you build it, they will come.”
==
If you haven't met Shape Shifter, see the following interviews:
youtube
youtube
Literally "trans the gay away."
#Shape Shifter#Leor Sapir#Joseph Figliolia#Fenway Community Health Center#medical transition#gender ideology#queer theory#genderwang#medical malpractice#medical scandal#trans the gay away#trans away the gay#woke homophobia#homophobia 2.0#gay conversion therapy#conversion therapy#gender affirming care#gender affirmation#affirmation model#medical corruption#informed consent#bottom surgery#vaginoplasty#minority stress#religion is a mental illness#Youtube
15 notes
·
View notes
Text
me trying to figure out when to consider wolfram an Adult for archive warning purposes

#kkm tag#ok so he's 82#which is like 16 or so in human years#16 is considered an adult in shinmakoku BUT as a human from america i consider 18 age of adulthood#but to make matters worse. when wolfram was 16 (and legally declared an adult) he was.... developmentally a 10yo kid#so we really cant use the shinma coming of age ceremony as a marker for adulthood either way#SO. if a fic takes place when yuuri is 18#wolfram would be like...85#which would put him no older than 17 developmentally#now if we take into account variation in aging rates for mazoku#then it all becomes Worse#bc my inbred bby has a very Pure bloodline. and that tends to slow down aging a little more#now is there something to be said for the maturity that comes from being a teenager for decades instead of years? perhaps#like when you compare him to yuuri. wolf's got his shit figured out WAY more than yuuri does#and his age is probably part of that#BUT then is the age gap weird the other way around#like is it weird for a actually-82 sixteen to to date an actual 16yo?#they're physically the same age#and you KNOW my boy wolf still got some frontal lobe development left#so i wouldnt compare wolf to an Actual Adult like for example gwendal#anyway this is my train stop so ill see yall later!
3 notes
·
View notes
Text
The Judge Rotenberg Center: 50 Years of Abuse
taken from this reddit post.
TRIGGER WARNING: This post details a long history of graphic child abuse and torture of the physical and psychological varieties.
Judge Rotenberg Educational Center, a residential school for people with developmental disabilities, emotional disorders, and autism spectrum disorders, in Canton, Massachusetts, USA. This organization has a colourful history to say the least, and given recent news, I've decided to do a bit of a summary
Origins
Founded in 1971 in Providence, Rhode Island, by Matthew Israel. It was originally named the Behavior Research Institute, and started with just two residents, one autistic, the other schizophrenic. In 1975 the BRI opened group homes in Massachusetts, and in 1976 it opened a branch in California.
The Behavior Research Institute of California / Tobinworld
When it opened the California branch in 1975, it did not have a license to operate as a group home, Israel did not have a license to practice psychology in the state of California, and the branch lacked a license to use aversives. This did not stop them. Eventually in 1977 they applied and were rejected for licenses and were scheduled to shut down. The day following their shut down a group of parents reopened the institute as a co-operative with Israel officially being consultant instead of Director, and they applied for the appropriate licenses again. The then-governor of California, Pat Brown, assisted them to gain their licenses, and they were the only group home ever permitted to use "physical aversives" on it's residents. They were awarded $35,000 a year per child by the state, the highest rate for any community facility in California.
July 17, 1981 at the California branch staff restrained 14-year-old Danny Aswad in the face-down position on his bed. He died in that position. An autopsy report stated he died of 'natural causes', however this prompted California to investigate the branch, discovering countless physical and psychological abuses at the facility. Residents were beaten, restrained, humiliated, and starved, sprayed with hoses, refused access to bathrooms, pinched till they screamed, and given "behavior rehearsal lessons" where they were instructed to destroy property, and then punished with spraying for it. Staff were trained in how to conceal bruises on residents from family members and inspectors. This investigation resulted in the facility being forbidden from using anything more punishing than a water spray, and forbade the founder Matthew Israel from stepping foot on the property.
At some point a few years later, this branch was renamed Tobinworld, and was taken over Judith Weber, who later would become Israel's second wife (she was a mother of one of the former residents).
October 1991, 9-year-old Derek Collins was restrained prone in a school bus by a Tobinworld aide and required emergency resuscitation and hospital care. Collins was admitted to Huntington Memorial Hospital in critical condition with possible brain damage. The aide pled guilty for felony child abuse.
In 2014 a mother sued Tobinworld after she alleged her 7-year-old child was regularly abused there, being denied snacks or the ability to use the restroom. She alleged in the preceding year that the facility's vice-president and three aides restrained her child, kicked his feet out from under him causing him to fall and get a bloody nose, and then when he cried they wrapped his face in plastic, causing him to choke on his blood.
In 2016 a 9-year-old boy is restrained by the arms and legs and then sucker punched in the face by a 26-year-old aid. It had been recorded and leaked by another employee who had said it was the third time they had recorded such an event.
These latter two events prompted an investigation where it was found that Matthew Israel had been illegally working at the school again without proper clearance, without the authorities being informed, without a background check, and without tuberculosis tests. The State Education board then closed down one of the branches of Tobinworld in 2016. The school was finally fully shut down in 2019.
The Judge Rotenberg Educational Institute
In 1979 one resident told investigators she desperately wished to leave the school, and her worst fear was an indefinite future in JRC. She contemplated suicide daily.
In 1979 two reports by NY State authorities found the BRI was conducting physical and mental abuse, and that the methods were only effective as a means of coercion with residents relapsing into their old behavior as soon as the immediate threat of punishment was gone.
In 1983, despite corporal punishment being illegal in Massachusetts, the institute was granted special permission for them.
July 23, 1985, 22-year-old Vincent Milletich had been acting out. He was restrained in a chair with plastic tie cuffs on his hands and feet, a mask was placed over his face and a helmet put on, and earphones were put on him to play white noise continuously. He died from asphyxiation. The BRI were not found to have caused his death, however were found negligent for approving the therapy and carrying it out without sufficient supervision. Later in the year, the State Office for Children ordered the BRI to close, or to stop using aversives. There was uproar among disability advocates demanding the school be shut, and controversy over the therapies and why it's residents seemingly 'regressed' without them, with Israel stating such regression in the absence of these interventions showed the effectiveness of them. Israel then took one of his most self-abusive students before Judge Ernest Rotenberg in 1986 and detailed her history. Rotenberg ruled she was unable to make her own treatment decisions, but if she were, she'd choose to stay at the BRI. The State Office for Children paid the BRI $850,000 and they were permitted to remain open and continue using aversives *as long as each student's treatment plan was approved by the probate court*. A year later, June 26, 1987, 29-year-old Abigail Gibson died of cardiac arrest.
1990, Linda Cornelison died. She was nonverbal and one day on the school bus doubled over clutching her stomach. A nurse thought her illness was an act. She was returned to her BRI-run home and given 13 spatula spankings, 29 finger pinches, 14 muscle squeezes, and was forced to inhale ammonia five times. She died the next morning in hospital due to complications related to a gastic perforation. Her mother reported that she had never had suffered gastrointestinal problems before. The Massachusetts Department of Mental Retardation found that although the school violated the most basic standards of decency, they were not derelict in their care of her, nor had the administration of aversives killed her.
Around the same time, the school began using the "Self-Injurious Behavior Inhibit System" (SIBIS for short) invented in 1984. It was designed to detect activities such as headbanging and administer eclectic shocks. Shortly afterwards Israel went to the manufacturers of the SIBIS and asked for a more powerful version, as "one student was shocked by the SIBIS over 5000 times a day without producing the desired change in behavior". The manufacturers refused, so Israel designed a system himself in December 1990, called GED (graduated electronic decelerator) that delivered a stronger shocker lasting ten times as long. The FDA cleared the device as they considered it "substantially equivalent to the SIBIS". By 1992 Israel was already phasing out the older GED for his new GED-3a and GED-4, which delivered even stronger shockers. He had never cleared them for use with the FDA.
In 1994 the center changed it's name to the Judge Rotenberg Center.
In 2000 the FDA incorrectly informed the JRC that it was qualified for exemption from registration of the GED-3a and GED-4, and only recognized their error in 2011 and demanded the immediate cessation of their use. They continued to be used till 2020.
The SIBIS provides a 3.5mA shock for 0.2 seconds. The GED-1 produces a 30mA shock for 2 seconds, and the GED-4 produces a 90mA shock for 2 seconds. A typical cattle prod produces a maximum shock of 10-20mA for under a second. The weakest GED's shock strength is still considered about twice the threshold that pain researchers consider tolerable to most adult humans. As of 2010 a GED-5 was in development.
In 2000 the school was receiving $18 million from the state, and in 2006 that increased to $56 million. Matthew Israel was making $321,000 a year.
In 2006 a mother sued the center claiming it had mistreated her son while he was wearing the GED. He was taken out of the school and improved significantly, although for a period after he left he had to remain in a psychiatric ward, and thought cameras still followed his movements and that he might be shocked for misbehaving.
A former staff psychologist said around 2001 the school policy switched from education and treatment to simply keeping students in line, "Israel couldn't stand them not behaving in a perfectly controlled way". Another said the school would punish not only negative behaviour, but actions they perceived as precursors to it. Face slappers would be shocked for raising their hand. Refusing a teacher's order, or talking out of turn were other such precursors.
Every room in the facility had since 1975 a complete setup of surveillance cameras and microphones monitored day and night, the purpose being to catch behaviours staff may have missed and phone them to inform them punishment needed to be handed out. It also had the dual unwritten purpose of monitoring staff members, if they refused to hand out punishments then they would be written up in "Performance Improvement Opportunities" documents, and firing staff who crop up in these too frequently.
One ex-staff member described having to shock people for an array of reasons: stopping work for more than 20 seconds, closing eyes for more than 5 seconds, a girl with cerebal palsy was shocked for moaning and reaching out to hold a staff member's hand. Another was shocked for urinating in their pants, they had been asking to go to the bathroom for over two hours. Yet another was shocked simply because they complained about another student being shocked. The staff member had been instructed to always announce what they planned to reach for in their pocket. One time they forgot and four kids screamed, they had to be punished with an electric shock.
In 2006 it was found that 14 of the 17 resident psychologists lacked proper licenses. It is believed JRC overbilled the state by nearly $800,000 by avoiding hiring licensed psychologists and not declaring that. That money was still uncollected a year later.
In 2007 it was reported the facility had a high turnover, among all staff including psychologists. A group of 52 trainees had been taken in and after three months only 2 remained employed there.
August 26, 2007, Arthur, a student who had been missing for two weeks, called a staff member and identified himself as a worker in DVR (the surveillance room) stating that shocks needed to be given to a resident for behaviours that had occurred before the night shift. The staffer handed the call over to a second staff member, the senior-most on shift at the time, as this seemed to be a breach of policy (punishments shouldn't be given for behaviour that happened over two hours preceding), however the second staffed was one of this recent batch who had only been at the facility for a few months, so handed back to the first staffer. The first staffer proceded to provide GED shocks while the student was in bed, and the staff on shift were instructed by Arthur to use the more potent GED 4, and did so for the rest of the night. The student in question received three further shocks. The student complained to the second staffer, saying the first was doing the wrong thing. The staffers still on the phone with Arthur continued to shock the student. The first staffer went to get another GED to shock the boy's stomach as the leg electrode battery seemed to be no working. The student is seen on camera speaking to the second staffer asking them to find out what is going on, and to call his clinician. Four other staffers are awake at this point, but do not intervene. Arthur seized the replacement GED's batteries in his hand and refused to relinquish them, and after a half hour confrontation was put on a four point restraining bed. He was no longer resisting, and told one of the staffers "let them know I'm being compliant". Staff are meant to tell student's the reasons they have received a shock, however while restrained a GED 4 shock is given without reason. A second GED 4 shock is given for physical aggression. Arthur is heard saying "let them rotate me" (hourly staffers are required to rotate electrodes to prevent burns on the skin, the facility denied that GEDs injured students, however burns were frequency enough that staff at the facility had a name for students going 'off the machine', a "GED holiday"). Arthur receives five more shocks. A ninth shock is given, and the DVR records an audible sob, not from the student, but the second staffer who had to leave the room as he "thought he would either cry or throw up if he stayed". Ten more shocks were given with accompanying reasons. The 20st shock was given without reason. The 21st shock was given for refusing to follow instructions. Nine further shocks were given, bringing the total to 30 GED-4 shocks in a single day. Staffers went to get approval from a psychologist to perform further shocks. Shocks continued. The 37th was given for attempting to remove the device, as were the 38th and 39th shocks. Shocks 50, 51, 52, and 53, were given for "verbal threats to destroy". In total between 70 and 77 shocks were given. After this was all done, Arthur's skin was red, he was defeated, he complained later that night of a racing heart, dry mouth, and difficulty breathing. He described feeling as if he was about to have a stroke. Staff took no action to help him. He suffered first degree burns. Arthur remained at JRC, although was on a "GED holiday".
MDRI Appeal to UN Special Rapporteur on Torture
In 2010 the Mental Disability Rights International (MDRI) appealed to the UN Special Rapporteur on Torture, a PDF copy of the 67 page report can be seen **[here](https://abcnews.go.com/images/Nightline/HT_US_Report_4_30_10_100630.pdf)**. It recounts it's own extensive set of equally, and in several cases worse tales of events which occurred at the facility.
Students being restrained for hours or intermittently for days, or even for weeks or months. One case of a student being almost strapped in a chair most of the time for two whole years. A student suffering from seizure disorders and a mild developmental disability, was put in chair restraints most of the time for a few months. He had to wear diapers, he was a teenager and had never had to wear diapers before and was very capable of going the toilet, but they didn't want to untie him to let him use the bathroom. They then escalated him to the GED too. Restraints, strict schedules, and social isolation may have been used as a form of psychological coercion in multiple cases to encourage students to consent to the GED. Another student was found to have severe ulcers in the location where the GED shocker was placed.
A non-verbal deaf and blind girl was rocking and moaning, she was shocked for moaning. She was crying because she had a broken tooth.
The aforementioned cases of students being demanded to misbehave and then shocked also has another variant. Staff would surprise students with mock attacks and threatened stabbings, to compel them to respond with aggression, fear, or screaming. They would then be intensely shocked. This specific excerpt seems scarily reminiscent of a book which caused me to subsequently stumble into and learn about the JRC on the internet - [A Clockwork Orange](https://en.wikipedia.org/wiki/A_Clockwork_Orange_(novel\)), perhaps this is not entirely surprising, the story was created around questioning the idea of free will, and of the theory of Behavioralism, which very much is the theoretical birthplace of Applied Behavioural Analysis (ABA).
All residents were forced to be vegan, with restricted diets such as mashed food with liver powder. Even up to 2010 (and possibly beyond), withholding of food was a punishment used. Removal of furniture from rooms was another punishment, one student entered with a beautiful room complete with TV and stereo, and after a month had merely a mattress on the floor.
Socialisation with staff members was forbidden. Socialisation with other students was a "reward" which had to be "earned". Education was often by staring at a computer facing the wall using self-teaching software all day long.
As of 2010 at least 6 deaths in total had occurred at the facilities. For over 2 decades Republican Jeffrey Sanchez's nephew was at the facility, and was the young man who received over 5,000 SIBIS shocks a day, Jeffrey Sanchez continually defended the facility and defeated bills aimed at curtailing it.
The school was a 'non-profit' and as such tax exempt, in 2007 it had spent $2.8 million in legal fees to keep it open. Twice regulatory departments had tried to shut it down, but it was either shuffled to another department or the head of the department forced to step down, with hefty payouts to JRC each time. They were a major customer at Rudy Giuliani's law firm.
In 2009 the JRC was required to be recertified for Level 3 Punishments, a team consisting of two psychologists, a psychiatrist, and the Department of Mental Retardation's Director for Human Rights and assistant general council assessed the facility and brought numerous findings of violations, abuses, and concerns. The state still recertified the facility in spite of the findings of this report.
**In 2010, the then Special Rapporteur at the UN, Manfred Nowak, responded to the appeal, saying he had "no doubts about it" being torture.** The subsequent UN Special Rapporteur on Torture, Juan Mendez, again raised serious concerns about the ongoing activity at JRC in 2012.
In 2011 Israel was indicted on charges of child endangerment, obstructing justice, and acting as an accessory after the fact. He signed a plea deal where he resigned his position at JRC to avoid prosecution.
In 2014 a video was leaked of a shocking in 2002, [Warning: It is a very distressing video](https://www.youtube.com/watch?v=YcxpGKctZMs)
The Last Year and a bit...
In 2020 the FDA [took the rare step to ban all "electrical stimulation devices (ESDs) used for self-injurous or aggressive behavior"](https://www.fda.gov/medical-devices/medical-device-safety/medical-device-bans). This sort of blanket ban is a rare final step for the FDA, only having occurred twice before, both times for medical devices which presented no or negligible benefit but had extreme associated risks even with proper use. [A more extensive ruling by the FDA is found here](https://www.federalregister.gov/documents/2020/03/06/2020-04328/banned-devices-electrical-stimulation-devices-for-self-injurious-or-aggressive-behavior). The ban was effective April 6, 2020.
COVID and ongoing court battles meant that none of the people on the GED devices would be required to transition off it until further legal decisions were made.
[July, 2021, a federal appeals court gave an exemption from the FDA ban to the JRC.](https://www.thedailybeast.com/the-judge-rotenberg-center-uses-electric-shocks-on-students-now-a-court-says-thats-totally-fine)
•••
this is super long and it’s from Reddit but please read it.
#the judge rotenberg center#JRC#Autism#autism speaks#autistic#actually autistic#cw: abuse#cw: torture#cw: ableism#electroshock#GRIDs or whatever#ABA therapy#applied behavioural analysis#stop the shock#shut down the JRC
28 notes
·
View notes
Text
The Father’s Grooming of Faith Seed
That’s right, it’s an analysis in defence of (the late current) Faith, mostly in her younger years. Please scroll past if you’re not interested in this take.
Please also keep in mind that these are personal opinions that I’m pulling based on game backstory and character portrayal, but I’m not without my biases. I wholly support members of the fandom who enjoy Faith being empowered in her evil, but it’s just not for me. I’m writing from the perspective of a former homeless youth, and while most of my thoughts are a personal interpretation of gameplay and conjecture from lazy writing limited information, I believe that I do have some insight into what Rachel may have gone through in terms of her attraction to Joseph and her recruitment into the Project at Eden’s Gate.
Warnings under the cut: Mentions of child grooming, drug use and misuse, indoctrination, abuse, religious trauma. It’s Far Cry.

Yes, she’s flawed and she’s an absolute shite of a person. She’s a cultist. She’s a liar. She’s just as forceful and twisted in her indoctrination as Jacob and John are. Her methods are awful, and she’s complicit when it comes to Joseph’s orders and his corruption.
No Seed sibling is anything short of a monster, and Faith is no exception.
At the end of the day, though, she WAS a kid when she was recruited by the cult. Before Joseph found Jacob, he’d already committed atrocities. Before he found John, the lawyer was a corrupt executive and a sadist.
Rachel was a rough-sleeping teenager with one friend.
She absolutely grew into the monster that she would become in her 20′s and there’s no excuse for her actions as an adult, but just as Jacob and John’s traumas were used against them in fostering their dependence on Joseph, so was hers.
What makes Joseph’s influence over his adopted sister so much more insidious is that he couldn’t rely on family sentiment in recruiting her initially. Instead, he found a lost child and manipulated her naivety and her desperation for acceptance.
Rachel was a minor who was groomed by a strange man in his 30′s, and no resident adult stepped in to prevent this from happening.
I realise there are many fans who disagree with the point I’m making here about the vulnerability of Rachel’s youth, but your brain has not even developed fully by 25, let alone 17.
She was a minor, and no matter the claims that she was happy to go along with the cult from the start, I believe her when she says that she was drugged by Joseph and forced to take on her role as Faith Seed.
The earliest information we have on Faith is tidbits from her teenage years. In-game dialogue from locals like Tracey and Virgil.
Disregarding the argument over whether she is or isn’t Rachel Jessop, Faith’s overall sentiment remains the same:
She was a child without a community of adult role models. She and Tracey were drawn to commune-style living in their teen years before the Seed brothers arrived in Hope County. They had both turned to drugs, and were ostracised by the locals. Rachel grew up in absence of a safe space. She had little guidance, and those she could depend on and confide in were, well...pretty much just Tracey.
Neither had healthy guardians to steer them in the right direction. They were on their own, and despite being of an age where (in an optimistic setting) their developmental needs should have been met by responsible adults, they were instead brought up without aid, and without acceptance.
Tracey mentions Rachel’s people-pleasing habits from way back in their childhood, even in the days where they hadn’t started living with the Project. She avoided conflict and wanted to be liked. She didn’t understand that acting as if everything was fine didn’t necessarily make it so.
I applaud Tracey’s scepticism of Joseph, and her ability to see through what was happening early on when the two of them first joined the Project, but I don’t blame Faith for her blindness to it.
She’s not even old enough to graduate high-school at this point. She’s been ostracised from an early age. She’s been swept under the rug. She’s got suicidal ideation and no one in this world loves her. What wisdom is she supposed to have gained?
Tracey might be strong enough to carry on with the ‘us against the world’ mantra, but Rachel doesn’t want conflict. She wants a community to take part in, and to be understood and accepted.
One day, the enigmatic leader of their church shows up. Everyone in the Project worships him. His importance is in their very scripture. He’s their Prophet.
He, of all people, takes a liking to Rachel.
It’s easy to point the finger and judge her naivety, but when you’re a displaced kid and a cool adult takes a shining to you, it’s very fucking difficult to resist keeping away from them.
It’s very fucking easy to get star-struck by what appears to be a healthy role model, even if your friend knows better than to buy into it.
I grew up with a lot of friends who dated college guys when we were in high-school, and the argument was pretty similar. Most of us were able to see how insidious it was from the outside, but when you’re the minor in that scenario, it’s not the adult whose attention and affection and praise of you is wrong; it’s the other kids. They don’t understand. They’re jealous. You’re special. You’re mature beyond your years. Smarter than them. That’s why you’re hanging around adults and they aren’t.
Reading Rachel’s letters to Tracey at the church, in which she implies Tracey’s envy over her spending more time with the cult than with her, I felt that Rachel’s lens had by this point been entirely clouded by Joseph’s influence. She cared about her friend and wanted to keep her by her side, but she’s entirely unable to compromise the feeling of acceptance that she’s found with Joseph.
He’s all-knowing and all-loving. He understands and forgives. Everyone loves him, and because he puts Rachel on a pedestal, they love her too. Tracey disrupts this. Tracey doesn’t fucking get it. Tracey is the poison.
Rachel was Joseph’s best prospect for a new Faith. She was a blank slate and she’d obey him in earnest. She wouldn’t doubt him, because she never knew any better.
She was legitimately happier in the Project than she was on the outside, and her honest belief helped to quell arguments of corruption and ulterior motive. She was pretty. She could sing and dance, and once they cleaned her up a little, she’d make for a perfect Siren.
Typical of an abuser, Joseph successfully isolated Rachel from her circle. By now, he was likely her only voice of guidance. He and his terrifying older brother who has sworn to protect them no matter the cost, and his charismatic younger brother who gives her pep talks and knows what it feels like to suffer from drug misuse. Joseph helped Jacob bounce back from post-traumatic dissociation. He saved John from self-imposed hell.
He could help Rachel, too.
I believe that Rachel was invited to take the role of Faith, and instructed to get clean in order to do so. That at some point amongst her attempts to stop using, when she was totally alone and suffering from withdrawal, her invitation wasn’t nearly as loving as it once was.
It became an ultimatum.
I believe Rachel was given a heavier dose of scopolamine than Joseph claims they gave her. That in her lowest moments, her role model fed her the fear of banishment should she turn back.
With the added aid of a powerful drug that massively affects decision-making and short-term memory, Joseph forced Rachel to destroy her identity and assume the role of Faith Seed. Whether or not she recalls this due to being under the influence at the time, I’m not sure, but the Bliss has set her free, and she’s now the Herald who will help recruits take the same leap she did.
She’s in Joseph’s inner circle now. She’s trusted enough to be exposed to the ugly side of the Project, and while the view from the top isn’t nearly so wonderful as it once sounded, Faith Seed has no life to return to.
She only has Joseph, and he knows it. She’s just as dependent on him now as his brothers are, and if she doesn’t please him, she won’t just lose that sense of acceptance she’s been chasing since she was a teenager.
She’s too close to him now to know that the other Faiths didn’t just quit. They were disposed of.
Once upon a time, Rachel wanted to die.
Now she’s terrified that she just might.
#*screaming* thats my OPINION#far cry 5#faith seed#joseph seed#jacob seed#john seed#how obvious is it that i want to break joseph's legs#i hope its obvious#religious trauma#abuse#indoctrination#drugs#drug use#drug misuse#child grooming#long post
77 notes
·
View notes
Conversation
Grew Too Fast Chapter 3 Scout's Birthday
Amelia:
I can't imagine my little baby boy being 16 already he grew up so fast. Its hard on a mother who honestly didn't think she would get a second chance at being a mother but more liek 4 extra chances. I have 4 healthy kids who I love to no end. Link and I are blessed to have our kids and how special each and every child is to us. Scout however grew up too fast for our liking. He's now 16 and just passed his drivers license this morning. Today is his 16th birthay and he is now a licensed driver, and honestly I don't think I will be seeing much of my baby boy because Link and I got him his first car, and a carseat for Elena, and carseat for Allison's baby. Scout says he thinks it's someone elses baby. But I am his mother so I know that it is his child. He's a teenage boy who just can't handle his emotions.
Scout:
Today is my 16th birthday and my parents got me a car or should I say a van to drive my siblings, Allison, and the baby in. They even got Elena a carseat for my car. She's probably the chillest child I have seen, but I do worry for my sister because she doesn't say much. Elena barely started to walk. She has several developmental delays unlike Charlotte (Charlie) Luke, and I have. All three of us don't have any delays but we have dyslexia. Apparently according to Grandma it runs in the Shepherd family. My Uncle apparently had it, Aunt Liz, Aunt Katheleen, and mom. I know she's proud of me and she's probably figured out that Annalese or Marcus is my child. Allison and I don't want to know the gender because we want to be suprised in case we decide to place the child up for adoption.
Allison is leaning towards adoption but i'll support her with what ever happens. We love each other and that is what matters. I can't beleive that today marks 16 years since Allison and I have known each other. She really is special to me and I can't imagine life with out her. She's my one and only, Where ever she goes for college I will follow her although I'm only 16 and setting myself short for colleges but I'd do it Allison. She would probably do the same.
Allison:
Today is Scout's birthday and I am suprising him with the gender of the baby. We had decided not to know if it was going to be a boy or girl because we were talking about adoption but I don't think I could do that as the baby deserves her parents. When I told Scout I was thinking about adoption that was when I was uncertain about his maturity for this. Our daughter is lucky to have both of her parents that love her so much even though she really was an accident. Sometimes I think that going back in time would help but then again we wouldn't have our daughter. Annalese really is going to be a lucky baby she is going to have parents who love her no matter what the curcumstance is. She's our little nugget who we love and honestly it would be really hard to say goodbye to Annalese when she comes because she has been kicking inside and got me to mature instead of being a stupid child. Well I was stupid enough to get pregnant at 16. I will almost be 17 when she is born which she is due in March 25th, and My birthday is April 15th. who would figure that you have a child by the time you go into your junior year. Scout and I will be parents in our junior year but we don't care.
Teddy:
I don't know if I agree with Allison for asking Scout to take responsiblity for her actions. But Anna is my granddaughter and I can't imagine saying goodbye to her if she is put up for adoption. When I first got pregnant with Allison I thought about adoption. But then I realized how wrong that would be for Owen to not know his own child. She's just a lot younger than I was. Allison, Leo, Adelynn, Louis, and Tom went to Scout's birthday party. He's the best boy you could ask for. Allison and Scout have been best friends since they were in diapers. They have known each other since birth and they love each other.
Ellis:
I can't beleive that my baby cousin as I always called Scout is now 16 years old. that makes me feel old except I'm 19 now and have no clue where that time went. It seems like just yesterday I was meeting Scout when Auntie Amelia came home with him. I can rememeber not being too fond of Scout because he was a baby and I wasn't the baby of the house anymore. I was 3 almost 4 when Scout was born and yet I should have been excited however I was not. But now it is hard to imagine what I did as a young girl because I love my cousin so much. I still can't beleive that he is going to be a dad. I know it was an accident much like Harry, and myself but I'm much older than Allison and have more education. Bailey went through the same except he is 21 raising a 7 month old child. Daisy is adorable. I don't think Zola is ever going to settle down she wouldn't even come for Scout's birthday party. I guess she's too busy to even realize what day it is or something like that. I haven't talked to her in weeks. Mom has and she said that Zola is now at Oxford in England. She went there to finish up but also because she will be finishing in December and was asked to watch out for Leo when he goes there in the fall.
Bailey:
Daisy and I came to Scout's party and we had a fun time. I got to see my sister Ellis, mom, aunt, uncle, and cousins. It was a fun time. I wish Zola had been there other than virtually but atleast she was there. I'm proud of my sister for all of her accomplishments kinda like mine with graduating as a single father, and with teacher certification in May. I will have a little cousin born by that time. I am excited but yet still suprised that Scout would make that same mistake. Yet again it's Allison Hunt we are talking about. She's a good kid but sometimes makes dumb choices much like her mother, and honestly my Aunt, and cousin. I remember when Scout wasn't even thought of and Aunt Amelia was scared to have a child because of my cousin Christopher that I guess would have been 23 this year two years younger than my sister and two years older than me.
Meredith:
I can't beleive that my nephew is 16 already. It seems like yesterday that he was born and now he's 16 and is a sophmore in high school. My own children it's hard to beleive especially Ellis because it's been 20 years since Derek died because Ellis is going to be 20 in 4 months. It's hard to beleive that but atleast I still have a piece of him here left on earth Bailey, and Ellis. They got me through some big problems so did Amelia, and Maggie. Scout and Allison however have their own little problems going on but hey they are teens they do stupid stuff like that but you never really know what goes on in a 16 year olds head.
Atticus:
Seeing your child grow up so fast is hard on a parent. Amelia and I are barely holding on for dear life trying to keep Scout to stay young, but that is impossible. He's not our little baby boy anymore and I don't know what we are going to do. I just got him a car for his birthday. He's such a smart, and healthy young man. Amelia and I really love him for everything even if Annalese was an accident. We will love that baby girl no matter what happens. Scout now knows that Allison is keeping Annalese. I think he's either scared or he's thrilled. Scout is a hard person to express emotions much like his mother. I love them both along with Charlotte, Luke, and our crazy yet young little girl Elena.
#family#amelia shepherd#Grey’s Anatomy#allison hunt#Teddy altman#atticus lincoln#bailey shepherd#Ellis Shepherd#Meredith Grey#amelink
2 notes
·
View notes
Photo
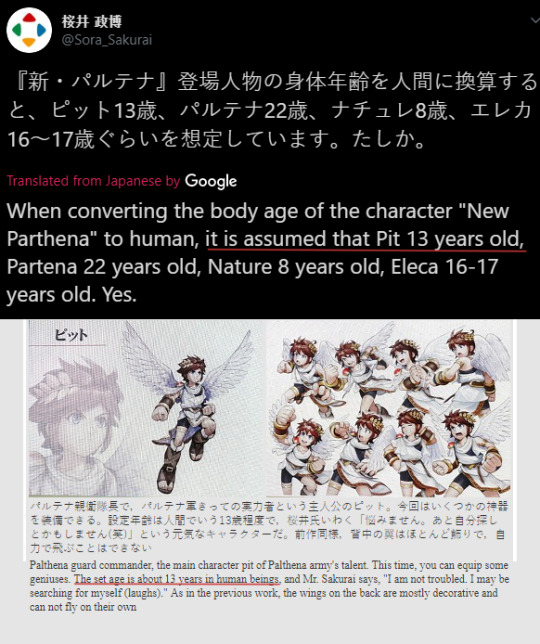
i’m sick to death of having to constantly prove this to people who refuse to listen all the god damn time and instead choose to keep condoning awful behaviour, so here. please read all of this, especially before interacting, as every bit of it is important.
sources: sakurai’s tweet here, ki:u prerelease overview thing here (which dates back to january 2011, if you’ll see)
additionally: pit’s ki:u idol description calls him youthful, arlon says ‘young master’ instead of just ‘master’ in reference to him in chapter 13, pichu’s smash ultimate guidance conversation has palutena say ‘you’ll understand when you grow up, pit’.
not to mention their literal appearances, manners of speaking, and voices clearly being teenaged, as well as the way that even the condescending gods around them wouldn’t treat an actual grown adult like.
pit, and, naturally, dark pit by extension, canonically equate that of 13 year old children in age, thus they themselves are actual children and minors, and yet this fanbase refuses to acknowledge that and continues to be the way it is, which is to say, almost irredeemably godawful.
(pre-emptive since the rest is under a cut: if you reblog this post do not clown on it)
--
for the last time,
romantically shipping pit & dark pit with adults, for example palutena, magnus, medusa, pandora, bayonetta, samus, marth, ike, robin, chrom, peach, daisy, rosalina, simon, and richter, is child x adult, aka pedophilia.
romantically shipping them with older 16-17 year old teens, for example link, zelda, little mac, and phosphora, is a predatory age and maturity gap.
drawing/writing nsfw or suggestive content of them is child p*rn and sexualisation of minors.
and stop defending any of this or telling me any of it is okay for any reason when absolutely none of it is acceptable or justifiable in the slightest. you should be ashamed of yourself if you still think it is okay.
and for god’s sake, stop acting like this is a ‘headcanon’, it’s right there in front of you from masahiro sakurai himself. what about the word of sakurai, the man who made this game and created it as it is in its current state, tells you that this is a refutable headcanon.
for the love of god, stop treating canonical children as anything older than they really are to get away with legitimately predatory and harmful content, especially if you’re treating them as if they’re adults.
it is not okay to age up a child for these purposes, you can’t act like your aging up IS canon or valid, you cannot deny their canonical aging, you cannot call on ‘’ambiguous aging’’ considering a confirmed number is right there, and acting like the characters in question being immortal is some kind of gotcha that actually makes it all okay after all is ridiculous. an immortal child is still an undeveloped child.
stop pairing pit and dark pit with characters 17+ aka way older and much more developmentally mature than them. it is always predatory and it is always bad, no exception. please stop denying and disrespecting the canonical, sourceable, and proven by the creator himself fact that they’re children and instead attempting to twist it to otherwise act like any of this is justifiable. they are 13. treating them as anything older for this reason is plain awful and you have no reason to do so.
and don’t clown at me and tell me that 13 yr old x 17 yr old is okay because they’re both minors, no it goddamn isn’t. not only does that aging become 16yo x 20yo down the road, but also know that a 13 year old is at a much different and earlier stage in development than a 17 year old is. no teenager close to finishing high school should have any romantic or sexual attraction to a child just coming out of primary school and now entering high school (or middle school, in the us, i guess). do not even try.
pit and dark pit are children. please stop being so nasty to them and creating legitimately predatory and harmful content, and please stop enabling, supporting, defending, and reblogging anybody who still does, even if you don’t actually create anything yourself. you are making a safe place for some of the most reprehensible people by doing so.
i will not argue with anyone about this. you have no reason to act like any of this can be sensibly argued with as if it can be disproven. any attempts to tell me why this pedophilic content or child p*rn or anything is somehow acceptable and how there’s nothing wrong with it will be ignored. why would you defend this.
i am not trying to ‘take away everyone’s fun’, i’m not telling you you’re not allowed to ship pit or dark pit with anyone at all, and i’m not ‘attacking mlm ships’ or whatever, i’m asking you to be sensible people who are mindful of their ages and to stop putting child characters in romantic relationships with others way older and more mature than they, and to not outright draw nsfw of them. it’s a ridiculously prevalent issue in this goddamn fanbase and it needs to stop. please think critically for once. if you have it in your head that saying this makes me an ‘‘anti’‘ then i really don’t know what to say to you other than grow up.
if you reblog this do not clown on it and if you see it as a personal attack instead of the generalised whole fanbase post it is you should consider why you feel that way
if you still continue to support any of this you are part of the problem and you should not feel proud of that
#kid icarus#kid icarus uprising#kiu#pit#dark pit#NOTE: if it gives you an error hit the lower refresh button on sakurai's tweet in the new twitter in order to make it show#yes i am hoping to shame anyone who still actively participates in any of this.#if you STILL think ANY of this is even REMOTELY acceptable#then please by all means rot in the underworld you irredeemable sack of dog feces#i hate this fanbase so much. so much#i'm tired of being polite about this. nobody ever actually listens and improves their awful behaviour. so now i've gotta be rude#to get this across into this fanbase's thick skulls#i could not care less who you depict them in a platonic friendship or familial relationship with#just quit it with the ridiculously predatory harmful and downright awful romantic age gaps and child p*rn already
33 notes
·
View notes
Note
I really want to know the answer to allll the question, but I'll be fair to others.... 13 - 18!
Alright so this has been sitting in my drafts for three months oops XD but let me try and tackle these!@erictwd
13. How do they greet the world — what is their typical attitude towards life? How does it differ in different circumstances, or towards different subjects? Why do they take these attitudes, and why do they change? How do these tend to be expressed?Daryl tends to be pretty practical overall, taking each problem one at a time and dealing with it as it comes. Growing up in fairly miserable circumstances has given him a pretty relaxed “survived that, can survive this too” attitude that can keep him pushing through dark days that might cripple most people. But that same mindset also tends to keep him from pushing for more than survival. He knows how to keep going through just about anything, but he’s got a harder time picturing more than keep going. Ask him about a dream or a happy ending or what he wanted to do with his life and you’d probably get a scoff and a shrug.
It’s also notable that, despite all the disappointments and losses life’s thrown at him, Daryl has an almost naive, almost stubborn optimism when it comes to the people he cares about. Searching for a little girl lost in the woods, refusing to believe she was gone even with all the odds against her. Losing his injured brother in an overrun city but convinced he was ok... and later not giving up on Beth, and then Rick. Even with all the hell he’s been through, he can never make himself accept the worst until he’s actually seen it.
14. What do they care deeply about? What kind of loyalties, commitments, moral codes, life philosophies, passions, callings, or spirituality and faith do they have? How do these tend to be expressed?Daryl has a strong moral code but overall (and despite his own claims, even) he tends to put his faith more in people than abstract concepts. When you’ve earned his loyalty it’s almost impossible to lose it, and he’ll be more likely to compromise his morals than his loyalty, at least to a certain point. (He might go along with something he knows is shitty for a while, or a command he disagrees with, if he’s given his trust to the person giving the order.)
That said, Daryl has lines he’ll never cross. (He has a sense of chivalry people might call outdated, but if you threaten a woman or child around him you’re basically declaring war.)
15. What kind of inner life do they have — rich and imaginative? Calculating and practical? Full of doubts and fears? Does it find any sort of outlet in their lives?Daryl’s not particularly imaginative by nature. He’s pretty practical and tends to focus on the thing in front of him. Problems and solutions, observations.
That said, he’s actually fairly superstitious (due to stories instilled by his mom as a child), but he’s typically practical about that as well. Try to tease him about it, he’ll tell you it’s pretty ignorant to assume science has figured out everything there is to know, isn’t it? And won’t you feel stupid if you go stomping around some fairy ring like an ass and end up with damn donkey ears? Just common sense not to risk it.
16. Do they dream? What are those dreams like?When Daryl sleeps deep enough to dream (which is rare) it’s usually a mess of anxieties bubbled up in the form of (shocker) him hunting for something. Lost loved ones, threats, or even just an indiscernible something he can’t put his finger on but desperately needs to find. Daryl’s dreams are nearly always restless things, searching things, and he’s usually a lot better rested when he doesn’t dream at all.17. Are they more shaped by nature or nurture — who they are, or what has happened to them? How have these shaped who they’ve become as a person?I feel like the answer to this question, for anyone, is both. Daryl’s views on the world and on himself are deeply shaped by the environment he was raised in. He grew up with very little sense of self-worth and it only got worse as he got older, but his miserable upbringing also taught him that he could grit his teeth and live through just about anything. Besides giving him basic survival skills –– he lived off what he hunted more often than not, even before the world ended –– he’s a fighter and can always soldier on because he doesn’t know any other way to be.
His upbringing also kept him pretty ignorant about different types of people, but Daryl’s openminded and insightful nature kept him from becoming casually hateful like his brother or most of his community, and he was able to adapt and flourish once he left that place behind and met his found family.18. What kind of person could they become in the future? What are some developmental paths that they could take, (best, worst, most likely?) what would cause them to come to pass, and what consequences might they have? What paths would you especially like to see, and why?
Daryl’s come such a long way from the person he was in season one. He’s learned a lot about accepting himself and letting himself be accepted, and believing in his own self-worth outside of just how well he could feed or protect a group. In canon Daryl’s becoming a father figure and starting to step up as a leading voice in the communities, and in a best case scenario that would continue to develop. I’d love to see him start to believe that he’s not only worthy but capable of having a romantic relationship. And I’d love for him to understand and feel like he belongs. And maybe, for the first time, start thinking of Alexandria as home.
In a worst-case scenario –– if people like Carol, Lydia, and Judith were to die –– I could see Daryl collapsing back into isolation, closing in on himself the way he’s done after major losses in the past. Letting his guilt drag him into hopelessness and self-harm. When things go wrong Daryl tends to believe he’s the reason they’ve gone wrong –– for doing something wrong, for not doing enough, for failing to see and think and protect the way he should’ve. Absolute rock bottom would find him slipping into alcoholism, but he’d only go there if he'd hit a point of no way out self-loathing and actively wanted everyone to see him as a monster and give up on him, because becoming a drunk like his parents is legitimately the worst thing he could picture for himself.
#erictwd#ask daryl#this is SO LONG and i still feel like i only answered about a third of the questions#but it was also super in-depth and interesting to think about#about daryl
3 notes
·
View notes
Text
Gypsy Rose Blanchard

Imagine being lived to your entire life by the one person you trusted the most in the entire world. Imagine living in fear of this person, scared to say or do the wrong thing. Imagine believing there was no way out or to be free. This was the life of Gypsy Rose Blanchard, the incredibly sick child of single mother Deedee Blanchard. To the outside world, they gave the impression that they were a brave and strong family unit, who will keep going on despite their various shortcomings. Behind closed doors, however, the truth was much more sinister and resulted in a sequence of events that would change their lives forever.
In 1991, 24 year old Deedee Blanchard was impregnated by the then 17 year old Rod Blanchard. He married Deedee in order to do the right thing, however, before Gypsy's birth, he realised he married for all the wrong reasons and left Deedee, despite her pleading with him to stay. Deedee decided to raise her child as a single parent. Rod clearly wanted to be apart of Gypsy's life and be a father figure towards her, yet Deedee tried to keep contact with him to a minimum. Rod eventually remarried and Deedee took Gypsy to move back in with her family.
Gypsy was born slightly premature, with no signs that anything was actually wrong with her. However, after about 3 months, Deedee became convinced that she was suffering with sleep apnea and went back and forth to doctors and hospitals to have tests done. As time went by, Deedee became even more convinced of various other illnesses that Gypsy had. Muscular dystrophy was one of these, which kept Gypsy confined to a wheelchair. Leukemia was another – her mother shaved her head often and kept her on a lot of medications. Gypsy also took medication for epilepsy, had hearing and sight problems, asthma and had to use a feeding tube and oxygen tank regularly. On top of this, Gypsy had significant developmental delays, being mentally younger than she actually was. Deedee homeschooled Gypsy because of this.
The community felt immense sympathy for Deedee and Gypsy. Due to all her various illnesses, Gypsy received attention from various charities such as Make a Wish Foundation, Habitat for Humanity and Ronald McDonald House. The two were also Hurricane Katrina survivors, with all of Gypsy's medical files and birth certificate being lost due to the storm. This meant that most doctors, out of sympathy, would take Deedee's word for everything she told them about Gypsy's medical history and persue any treatments that were believed to be needed. They moved to Missouri and, as a part of the Habitat for Humanity position, a house was built for them that included a wheelchair ramp and was suitable towards Gypsy's needs. They lived off of social security, food stamp and Medicaid paying for medical expenses, as well as receiving free flights to Kansas City for specialist treatments. The two maintained a shared Facebook account and acted like they were the best of friends.
This changed on the afternoon of June 14th 2015, when Deedee and Gypsy's shared Facebook account was updated with a shocking new status that read, “That bitch is dead!”. People initially just assumed the account had been hacked but in the comments, the profile had also written a crude statement about how they had slashed the mother's throat and raped her daughter. Close friends and neighbours grew concerned and called the police to check on the family. There was no answer at their door but the specialist car that Gypsy was required to use was still in the driveway, meaning that she couldn't have gone out. After obtaining a search warrant, police began searching the house and found the body of Deedee Blanchard, who had been stabbed several times. There was no sign of 19 year old Gypsy anywhere in the house – her wheelchairs were all there and she had none of her medication with her – people believed it was highly unlikely she would be able to survive on her own.
Police traced the IP address of where the statuses came from and it was linked back to a man called Nicholas Godejohn. He was not a stranger to the family, he was in fact Gypsy's boyfriend, who she had begun corresponding with on a Christian dating site and maintained an online relationship with him. Nicholas had his fair share of issues also; he had various mental health problems, including multiple personality disorder and autism, and had been arrested for indecent exposure. The two frequently had conversations of a very sexual nature, including discussions about BDSM and maintaining relationships with Nicholas' other personalities also. This was all done without the knowledge of Deedee, who was very protective of Gypsy and forbade her from using the internet when she was not around. Deedee had initially smashed Gypsy's phone and laptop when she was caught doing so. None of this worked. The pair had met once at a cinema, where they both planned to bump into each other in costume and strike up a conversation to avoid the suspicion of her mother, however she claimed she did not find him as attractive in person. In regardless, she still remained infatuated with him and confided in a close friend that she planned on eloping with him and was already thinking about names for their children.
The police traced his address back to his home in Springfield, Wisconsin, and found Gypsy there with him. But, shockingly to authorities, Gypsy could walk. It turned out, in fact, that Gypsy actually had none of the illnesses that her mother claimed she had. Despite this, she was frequently treated for all of these illnesses and took all the required medication. Her mother kept her head shaven to keep up the appearance that she was a chemotherapy patient. It is unknown how doctors allowed Deedee to be able to access all of this medication when clear tests showed that Gypsy was actually perfectly healthy and needed none of it, though few made their suspicions about Deedee clear. It is unknown whether this was done as a form of attention seeking or sheer mental illness but it also turned out that Gypsy even believed that she was sick; she claimed that she only knew she was able to walk and believed everything else. On top of this, Deedee continually lied to everyone about her daughter's age also. Prior to Deedee's murder, everyone believed Gypsy to be 19 years old when she was actually 23 and had falsified another birth certificate claiming her to be younger than she actually was. Rod, whenever he phoned on Gypsy's 18th birthday, was told that he wasn't allowed to say she was 18 because she believed that she was 14.
Psychiatrists believe that Deedee had a condition known as Munchausen syndrome by proxy, which is when someone fabricates or induces an illness of any kind onto someone in their care, with the main motive being to garner sympathy and attention. While it is considered a form of mental illness, it is also considered a form of abuse. Other well known cases of this include Kathleen Bush and Deborah Mathers, the mother of rapper Eminem. One doctor suspected that this abuse was going on but was told by other doctors to treat the two of them with golden gloves, so he did not report Deedee to social services. For many years, Deedee had exhibited symptoms of this disease. Her family believe her to be potentially responsible for the death of her mother by prohibiting food from her and to be poisoning her step mother while she was sick. As soon as Deedee had moved out of the family house, her stepmother's health returned to normal. In order to keep up appearances, Deedee ensured that Gypsy was always close by and never left home without her. Gypsy claimed that her mother was physically and emotionally abusive towards her, becoming very violent if Gypsy ever said the wrong thing in front of others. Gypsy stated many times that she felt like a prisoner many times and had tried to escape a few times, once being driven to a hospital by a neighbour and another time being caught in a hotel room with an older man, however both were foiled by Deedee. This was why Gypsy and Nick conjured the plan that they did.
On the 14th, Nick drove down to Missouri while Gypsy and her mother were at a hospital appointment. When Deedee went to bed, Gypsy messaged Nick to tell him so and let him into the house. Gypsy had supplied him with duct tape, gloves and a knife. Gypsy then hid in the bathroom and covered her ears so as to not hear her mother's screams. Nick then repeatedly stabbed Deedee several times in her bed. Gypsy and Nick had sex in Gypsy's room, stole $4000 worth of cash and travelled to a motel in Springfield. Nick mailed the bloody murder weapon to his own house and got a bus back to Nick's house, while Gypsy wore a blonde wig in order to disguise herself. When they were both arrested and taken to the police station, Gypsy claimed that she had nothing to do with the murder of her mother and acted as though she had no knowledge of it, yet she later confessed. Her reasoning was that killing her mother felt like the only escape route she could have taken.
Following the large amount of media attention the case has gotten, Gypsy actually gained a lot of sympathy from the public, as a girl who was unable to live her life to the fullest potential because of how her mother treated her. The prosecution announced that because of these circumstances, they would not be seeking the death penalty. Her attorney was able to make a plea deal, in which she would serve a second degree sentence, which Gypsy agreed to, and she was sentenced to serve 10 years. No such deal has been put in place for Nick and is still awaiting his trial for charges of first degree murder, as both his and Gypsy's stories paint Nick as the actual murderer. His trial is due to begin in November 2018.
While many believe Gypsy would remain a danger to the public when she is released, others say that she has learnt her lesson, including Gypsy herself. In multiple interviews, she has repeatedly said that she feels huge remorse and guilt over the death of her mother, and wished that she had thought of another way out of the situation. Gypsy has also started growing her hair and gaining a healthy amount of weight. She even maintains a relationship with her dad, who visits her often and has the support of other members of her family, including her maternal grandparents. She is considered a model prisoner and could potentially let out earlier for good behaviour. Even still, she maintains that though she loved her mother, she is happier in prison than she ever was living with her.
12 notes
·
View notes
Text
Why the Centene and WellCare Merger is the Biggest Deal in 2020
By ANDY MYCHKOVSKY
I feel like the healthcare world just skipped over the $17.3 billion mega-merger between Centene and Wellcare, which just received final regulatory approval last Wednesday. With their powers combined, this new company will create the Thanos of government-focused health plans, hopefully without any of the deranged plans to take over the world. I do get it, 181 million lives are covered by employer-sponsored insurance, between full-risk and self-insured plans. These employer populations have the most disposable income and their HR departments are willing to provide supplemental benefits. However, in my opinion, the future growth of health insurance will be governmental programs like Medicare Advantage (MA), Medicaid managed care, and ACA exchanges. But instead of me telling you this, here is exactly what Centene and WellCare said in a press release to defend the merger:
“The combined company would be the leader in government-sponsored healthcare with increased scale and diversification both geographically and in its managed care service offerings, and enhance access to high-quality services for members. It will offer affordable and high-quality products to its more than 12 million Medicaid and approximately 5 million Medicare members (including Medicare Prescription Drug Plan), as well as individuals served in the Health Insurance Marketplace and the TRICARE program. The combined company will operate 31 NCQA accredited health plans across the country and will have increased exposure to government-sponsored healthcare solutions through WellCare’s Medicare Advantage and Medicare Prescription Drug Plans. It will also benefit from leveraging Centene’s growing position in the Health Insurance Marketplace to new markets. The transaction creates a company with the size and scale to better serve members through enhanced healthcare programs, expanded capabilities and increased investment in technology.”
Simply put, here’s some of quick stats provided at the JP Morgan Healthcare Conference presentation on January 13, 2020:
National footprint now serving 1 in 15 Americans
Clear market leader in Medicaid managed care and ACA exchange marketplace
Dominance serving most complex populations, #1 leader in LTSS and #2 in dual eligible
Competitiveness in the Medicare Advantage (MA) enrollment wars
$500 million in proposed savings due to annual cost synergies

Announced back in March 2019, some investor analysts questioned the merger given the significant overlap between each plan’s enrollment and focus on governmental programs. Turns out, in some states, the combined entity would have monopolistic tendencies. Therefore, in order to satisfy anti-competitive market dominance, WellCare must divest its Medicaid and Medicare Advantage plans in Missouri, Medicaid plan in Nebraska, while Centene must divest its Medicaid and Medicare Advantage plans in Illinois. So long as they comply with these specific requests, you have yourselves a ballgame folks.
I’m actually a bit shocked these few divestitures is all that is required given their combined business. For example, Florida is the 4thlargest Medicaid state in the country. This is also where WellCare is headquartered and holds the largest Medicaid managed care enrollment in the state. The combined market share between Centene and WellCare nears 46% as of December 2019 enrollment reports for the traditional Managed Medical Assistance (MMA) population (e.g., TANF, SSI, ABD) with over 2.7 million lives. Now Florida did just finish their open enrollment period in January, so there is potential that the two plan’s enrollment could’ve changed by now. However, I find it difficult to believe their enrollment would change too significantly given the relatively low open enrollment churn rates in Medicaid.

Why does this all matter? Because Medicare covers 61.2 million Americans and Medicaid covers 75.8 million Americans. That represents 137 million total lives between the two major lines of business that Centene and WellCare focus on. Add in the 8.3 million from the 2020 ACA exchanges and that is just icing on top of the cake for next decade’s growth opportunity. We have a baby boomer population (ages 52 to 70) that numbers 74 million and beginning to age into Medicare. These are the highest cost population segment, excluding some of the smaller specialty populations (e.g. PACE), that must be managed by either Medicare fee-for-service (FFS) or Medicare Advantage plans.
Let’s start with MA. I wrote an entire blog last week on the MA market, particularly from the perspective of the startup health plan. To recap, the battle for MA is hard. The sales and marketing expenses for subscale plans is high due to broker fees for initial enrollments and renewals. The plan must be old enough with good quality to receive a high Medicare STAR quality rating, which in turn requires the federal government to provide bonus payments to the MA plan that can be used to offer patient’s supplemental benefits. Given the high medical cost of MA patients, $800-1,000 per member per month (PMPM), small plans are subject to actuarial risk and higher outlier expenditures that can sink your plan’s medical loss ratio (MLR).
Let’s take Duval County, Florida, home of the Jacksonville Jaguars and 180,000 Medicare eligible beneficiaries and 70,000 MA lives (39% MA penetration rate). In this particular MA market, Centene and WellCare account for 17% of the total MA lives (~12,000 lives), trailing only UnitedHealthcare (32%) and Humana (19%). This merger nearly triples Centene’s existing MA enrollment and places them in a much better position to compete against the major for-profit incumbent and startup plans. They will still only account for 3.6% of the total MA market, but appear focused on targeting this older customer base and will benefit from the broader trends from FFS to private plans. All-in-all, Centene and WellCare have a combined 875,000 lives across 455 MA plan options as of January 2020.

Now let’s switch to Medicaid. The worst kept secret in healthcare is that Medicaid (not Medicare) is the primary payer of long-term services and support (LTSS) like nursing homes in America. If we’re projecting forward, where do you think the 74 million baby boomers are likely to reside as they age? With a shortage of qualified home health aides (not to mention how expensive out-of-pocket it can be), limited societal buy-in for multi-generational housing (compared to Asian countries), and younger generations receding to expensive, urban areas, Houston we have a problem. Not to make matters worse, but the only way for your loved one to receive Medicaid benefits to cover nursing home care, is if they’ve already used up most their savings and assets. Once they’ve hit that financial point of no return, it is unlikely your loved one will be able to afford anything else beyond the nursing home that accepts their Medicaid coverage.
In terms of growth opportunities, I mentioned in a previous Heathcare Pizza blog that majority of states have already transitioned into Medicaid managed care. Most states contract with payers like Centene or WellCare to administer the program for a portion of patients in return for a set per PMPM fee. This fee is set by third-party actuarial firms and includes the desired medical loss ratio (MLR), administrative loss ratio (ALR), and profit margin built in. The way you win a coveted contract award is by applying during a competitive request for proposal (RFP) period that typically happens every few years. Centene already has a strong 5-year Medicaid RFP win rate of 80%, and adding WellCare will only bolster their chances. With North Carolina scheduled to move into managed care in 2020, of which both Centene and WellCare were awarded separate contracts, the game is less about net new states but instead focused on transitioning all populations into managed care.

For example, the state of Arkansas is currently undergoing a process to transition their Medicaid populations into managed care via the Provider-led Arkansas Shared Savings Entities (PASSE) program. The state chose to start with the most complicated and expensive population, the ~45,000 intellectually and developmentally disabled (I/DD) patients. They started here because these patients alone cost Arkansas Medicaid over $1 billion annually. However, there are 926,000 Medicaid lives in the state as of December 2019. If you don’t think health plans like Centene see the potential opportunity to convert the remaining members into their managed care enrollment, you’re being naïve.

Up to 24 million lives will be covered by this newly merged entity, forming a formidable opponent to the dominant for-profit health plans like UnitedHealth Group and CVS / Aetna. If their go-to-market roadmap is successful, I see good things for employees and investors related to the company in the near future. That is not financial advice, just one man’s opinion. I will tell you one thing though, the market seems to have come full circle because since October 2019, the stock has been on a steady rise in preparation for the merger approval.
Andy Mychkovsky is the creator of Healthcare Pizza, where this post originally appeared. Follow him on Twitter (@AMychkovsky) and LinkedIn for future thoughts and updates.
The post Why the Centene and WellCare Merger is the Biggest Deal in 2020 appeared first on The Health Care Blog.
Why the Centene and WellCare Merger is the Biggest Deal in 2020 published first on https://venabeahan.tumblr.com
0 notes
Text
Why the Centene and WellCare Merger is the Biggest Deal in 2020
By ANDY MYCHKOVSKY
I feel like the healthcare world just skipped over the $17.3 billion mega-merger between Centene and Wellcare, which just received final regulatory approval last Wednesday. With their powers combined, this new company will create the Thanos of government-focused health plans, hopefully without any of the deranged plans to take over the world. I do get it, 181 million lives are covered by employer-sponsored insurance, between full-risk and self-insured plans. These employer populations have the most disposable income and their HR departments are willing to provide supplemental benefits. However, in my opinion, the future growth of health insurance will be governmental programs like Medicare Advantage (MA), Medicaid managed care, and ACA exchanges. But instead of me telling you this, here is exactly what Centene and WellCare said in a press release to defend the merger:
“The combined company would be the leader in government-sponsored healthcare with increased scale and diversification both geographically and in its managed care service offerings, and enhance access to high-quality services for members. It will offer affordable and high-quality products to its more than 12 million Medicaid and approximately 5 million Medicare members (including Medicare Prescription Drug Plan), as well as individuals served in the Health Insurance Marketplace and the TRICARE program. The combined company will operate 31 NCQA accredited health plans across the country and will have increased exposure to government-sponsored healthcare solutions through WellCare’s Medicare Advantage and Medicare Prescription Drug Plans. It will also benefit from leveraging Centene’s growing position in the Health Insurance Marketplace to new markets. The transaction creates a company with the size and scale to better serve members through enhanced healthcare programs, expanded capabilities and increased investment in technology.”
Simply put, here’s some of quick stats provided at the JP Morgan Healthcare Conference presentation on January 13, 2020:
National footprint now serving 1 in 15 Americans
Clear market leader in Medicaid managed care and ACA exchange marketplace
Dominance serving most complex populations, #1 leader in LTSS and #2 in dual eligible
Competitiveness in the Medicare Advantage (MA) enrollment wars
$500 million in proposed savings due to annual cost synergies

Announced back in March 2019, some investor analysts questioned the merger given the significant overlap between each plan’s enrollment and focus on governmental programs. Turns out, in some states, the combined entity would have monopolistic tendencies. Therefore, in order to satisfy anti-competitive market dominance, WellCare must divest its Medicaid and Medicare Advantage plans in Missouri, Medicaid plan in Nebraska, while Centene must divest its Medicaid and Medicare Advantage plans in Illinois. So long as they comply with these specific requests, you have yourselves a ballgame folks.
I’m actually a bit shocked these few divestitures is all that is required given their combined business. For example, Florida is the 4thlargest Medicaid state in the country. This is also where WellCare is headquartered and holds the largest Medicaid managed care enrollment in the state. The combined market share between Centene and WellCare nears 46% as of December 2019 enrollment reports for the traditional Managed Medical Assistance (MMA) population (e.g., TANF, SSI, ABD) with over 2.7 million lives. Now Florida did just finish their open enrollment period in January, so there is potential that the two plan’s enrollment could’ve changed by now. However, I find it difficult to believe their enrollment would change too significantly given the relatively low open enrollment churn rates in Medicaid.

Why does this all matter? Because Medicare covers 61.2 million Americans and Medicaid covers 75.8 million Americans. That represents 137 million total lives between the two major lines of business that Centene and WellCare focus on. Add in the 8.3 million from the 2020 ACA exchanges and that is just icing on top of the cake for next decade’s growth opportunity. We have a baby boomer population (ages 52 to 70) that numbers 74 million and beginning to age into Medicare. These are the highest cost population segment, excluding some of the smaller specialty populations (e.g. PACE), that must be managed by either Medicare fee-for-service (FFS) or Medicare Advantage plans.
Let’s start with MA. I wrote an entire blog last week on the MA market, particularly from the perspective of the startup health plan. To recap, the battle for MA is hard. The sales and marketing expenses for subscale plans is high due to broker fees for initial enrollments and renewals. The plan must be old enough with good quality to receive a high Medicare STAR quality rating, which in turn requires the federal government to provide bonus payments to the MA plan that can be used to offer patient’s supplemental benefits. Given the high medical cost of MA patients, $800-1,000 per member per month (PMPM), small plans are subject to actuarial risk and higher outlier expenditures that can sink your plan’s medical loss ratio (MLR).
Let’s take Duval County, Florida, home of the Jacksonville Jaguars and 180,000 Medicare eligible beneficiaries and 70,000 MA lives (39% MA penetration rate). In this particular MA market, Centene and WellCare account for 17% of the total MA lives (~12,000 lives), trailing only UnitedHealthcare (32%) and Humana (19%). This merger nearly triples Centene’s existing MA enrollment and places them in a much better position to compete against the major for-profit incumbent and startup plans. They will still only account for 3.6% of the total MA market, but appear focused on targeting this older customer base and will benefit from the broader trends from FFS to private plans. All-in-all, Centene and WellCare have a combined 875,000 lives across 455 MA plan options as of January 2020.

Now let’s switch to Medicaid. The worst kept secret in healthcare is that Medicaid (not Medicare) is the primary payer of long-term services and support (LTSS) like nursing homes in America. If we’re projecting forward, where do you think the 74 million baby boomers are likely to reside as they age? With a shortage of qualified home health aides (not to mention how expensive out-of-pocket it can be), limited societal buy-in for multi-generational housing (compared to Asian countries), and younger generations receding to expensive, urban areas, Houston we have a problem. Not to make matters worse, but the only way for your loved one to receive Medicaid benefits to cover nursing home care, is if they’ve already used up most their savings and assets. Once they’ve hit that financial point of no return, it is unlikely your loved one will be able to afford anything else beyond the nursing home that accepts their Medicaid coverage.
In terms of growth opportunities, I mentioned in a previous Heathcare Pizza blog that majority of states have already transitioned into Medicaid managed care. Most states contract with payers like Centene or WellCare to administer the program for a portion of patients in return for a set per PMPM fee. This fee is set by third-party actuarial firms and includes the desired medical loss ratio (MLR), administrative loss ratio (ALR), and profit margin built in. The way you win a coveted contract award is by applying during a competitive request for proposal (RFP) period that typically happens every few years. Centene already has a strong 5-year Medicaid RFP win rate of 80%, and adding WellCare will only bolster their chances. With North Carolina scheduled to move into managed care in 2020, of which both Centene and WellCare were awarded separate contracts, the game is less about net new states but instead focused on transitioning all populations into managed care.

For example, the state of Arkansas is currently undergoing a process to transition their Medicaid populations into managed care via the Provider-led Arkansas Shared Savings Entities (PASSE) program. The state chose to start with the most complicated and expensive population, the ~45,000 intellectually and developmentally disabled (I/DD) patients. They started here because these patients alone cost Arkansas Medicaid over $1 billion annually. However, there are 926,000 Medicaid lives in the state as of December 2019. If you don’t think health plans like Centene see the potential opportunity to convert the remaining members into their managed care enrollment, you’re being naïve.

Up to 24 million lives will be covered by this newly merged entity, forming a formidable opponent to the dominant for-profit health plans like UnitedHealth Group and CVS / Aetna. If their go-to-market roadmap is successful, I see good things for employees and investors related to the company in the near future. That is not financial advice, just one man’s opinion. I will tell you one thing though, the market seems to have come full circle because since October 2019, the stock has been on a steady rise in preparation for the merger approval.
Andy Mychkovsky is the creator of Healthcare Pizza, where this post originally appeared. Follow him on Twitter (@AMychkovsky) and LinkedIn for future thoughts and updates.
The post Why the Centene and WellCare Merger is the Biggest Deal in 2020 appeared first on The Health Care Blog.
Why the Centene and WellCare Merger is the Biggest Deal in 2020 published first on https://wittooth.tumblr.com/
0 notes
Text
BOTW Zora Life Cycle
i put too much thought into this. this is largely headcanon, with information from BOTW and an idea or two from Majora’s Mask!
alright, onward through the 9 stages of the Zora life cycle:
note: the ages I’ve given for each stage are more of an estimate than a “this always happens at this age” thing except for stage 1 to 3! because everybody goes through puberty and matures at a different rate. think of the ages I’ve assigned as being averages, haha.
Stage 1 - Egg (0 days - 1 month)
Every Zora’s life begins as an egg; a parent Zora will lay a clutch of two to four soft, jelly-like eggs in a spawning pool and tend to them as they develop. The eggs start off clear but eventually turn opaque as the babies develop, but since the eggs are so delicate it’s very likely that most of a clutch will not actually hatch, even with the best care possible. After one month the surviving eggs, usually one or two, will finally hatch!
Stage 2 - Hatchling/Alevin/”Infant” (1 month - 1 1/2 years)
A newborn Zora is called an alevin, though they are colloquially known as hatchlings, levvies (singular: levvy), guppies, or pollywogs. Hatchling Zora somewhat resemble tadpoles, as they did in Majora’s Mask, with a proportionally large rounded head, a less-defined abdomen segment with the signature triple gill-slits on each side, two small head-fins and a long tail which they use to swim. They can breathe both air and water, but have an easier time breathing water at first.
Hatchlings also have yolk sacs which they feed off of for their first 3-4 weeks after hatching; this is thought to be a vestigial trait, but it is still a developmental benefit as the yolk contains antibodies from the parent, helping the newborn develop their immune system.
By the second month the hatchlings’ yolk sacs are totally depleted, thus they will require regular feeding starting around this time. From this point onward they simply grow larger for about a year and a half, staying in a limbless tadpole-like form but eventually growing to be 1 1/2-2 feet long and undergoing marked proportional changes. Specifically, the head and abdominal segment become larger and more well-defined, also gaining body fat; meanwhile the tail does not grow as quickly, eventually leading to a rounded, chubby, somewhat ball-like shape. This is often called the “ball phase” or colloquially “second egg,” due to the similarity in shape. The onset of this proportional change is a sign that the hatchling is getting ready to undergo metamorphosis.
Stage 3 - Metamorphosis
Metamorphosis can be thought of as a young Zora’s first growth spurt, and it is by far the most dramatic change. Taking place over the course of 24 to 48 hours, metamorphosis involves a hatchling in ball phase undergoing a drastic transformation. Prior to metamorphosis hatchlings will gorge themselves and gain body fat in preparation for the massive energy requirement of the process, and Zora parents are encouraged to feed their children more often in the weeks leading up to the event.
The changes, roughly in order of occurrence, are:
-the tail separates from the lower body, freeing the abdomen and officially becoming the ‘head-tail’
-pigmentation develops on the back and sides of the abdomen
-small fins form along the ‘shoulders,’ lower back, and ‘hips’
-as the baby Zora uses energy from its body fat, the reduction of fat around the head reveals the shape of the jaw and neck
-similarly, the head-tail shortens and becomes smaller as body fat is repurposed for energy
-the arms and legs emerge - these structures began forming gradually during the “ball phase” but were partially fused within the abdominal segment at that time; the young Zora undergoes a partial ‘shedding’ on their belly that removes an outer layer of flexible skin that held the limbs in place as they developed, and then their limbs gradually unfuse - generally the legs unfuse first and then the arms follow
-finally, the forearm fins unfuse from the arm mass and unfurl
A hatchling is officially considered a toddler when the legs and arms have emerged completely. Most toddlers are 1 1/2 to 2 feet tall from head to foot, but will weigh a little less than their pre-metamorphosis weight due to the consumption of so much body fat.
Stage 4 - Child/”Toddler” (1 1/2 - 40 years)
After undergoing metamorphosis the Zora child's growth refocuses towards mental/psychological development than body development. Mental development from 2 years old to 40 years old in a Zora is equivalent to that in Hylians from age 2 to 12. Essentially, Hylian children grow about 3 times faster - and they also grow their bodies, not just their minds! Meanwhile the young Zora will undergo very little change in their body aside from increased hand-eye coordination, dexterity, and the improvement of other senses. They learn how to walk and swim early on in this period and are highly active, though they have low stamina; they’ve got just enough for a short burst of speed or effort, but not enough for extended bouts of running or swimming. Zora children generally start primary school at the age of 20.
An in-game example of a Zora in this age range is Laruta, the little girl who hangs out at Mipha’s statue! I’d peg her to be in her early 20s in terms of Zora aging, which puts her mental age/equivalent Hylian age at about 7 years old. just a lil baby. <3 The brothers Tumbo and Keye are also in this stage but they are a little older than Laruta, so they’re probably in their early 30s - equivalent to Hylian 9 year olds.
Stage 5 - Preadolescent/“Preteen” (40 - 45 years)
Hylians may have trouble telling child, preadolescent, and adolescent Zoras apart because they all have the same body shape and size; in Zora culture, these differences are denoted more by a child’s mental maturity, their behavior, and their pheromone markers. A preadolescent Zora is akin to an 11 or 12-year-old Hylian in terms of mental maturity and likely has more stamina than a child, but has not yet begun producing adolescent pheromone markers.
The “preteen” phase is actually rather short, more of a transitional period between prepubescence and puberty. As such, preteen Zora often have voracious appetites; this is because they need to build up body fat again, since they’re preparing to go into puberty.
Stage 6 - Adolescent/“Teenager” (45 - 60 years)
Zora puberty begins around age 45 and is made up of two parts: physical maturity and mental maturity; a Zora is not considered an adult until they have completed both parts, however. Physical and mental maturity start at the same time with changes occurring in a young Zora’s brain chemistry and hormones. The biggest indicator that puberty has begun is the change in a young Zora’s pheromones, and the change in their behavior. Their brains grow more, which results in many of the same emotional and mental woes that Hylian and other peoples’ teenagers experience, and with that they develop their mental maturity further as well.
Meanwhile, their physical maturation goes slower; though the body is producing adolescent pheromone markers and hormones, most of the energy is spent on their growing brains rather than the rest of their body. As such this often leads to “teenage” Zora having an awkward “short phase” where they still look fairly young. To the relief of many, they generally get their second growth spurt after about 10 years of mental development. The growth spurt lasts anywhere from 3 to 7 years, though it can take up to 10 years; and it’s this spurt that brings them to full maturity, ability to make babies and all.
An in-game example of adolescent Zoras would be Finley, Tula, and Tona (I’m assuming that Tula and Tona are teenagers from the way they act, and the fact that they don’t seem to be actively working). As stated in the game Finley is hasn’t had her growth spurt yet, while Tula and Tona have. Finley is about 54 years old, equivalent to a Hylian 16 year old; while Tula and Tona are around 57-59 years old, equivalent to Hylian 17-18 year olds.
Stage 7 - Young Adult (60 - 85 years)
This stage is pretty self-explanatory: now that the Zora has completed both mental and physical maturation, they’ve completed puberty and are now officially an adult, if a young one! At this point they’re ready to take on an apprenticeship, military training, further education, or anything else they’d like to try their hand at. Also, they’re legally allowed to get married and purchase alcohol at the age of 65 (which may be a bummer to any early bloomer Zora who finish puberty at 60 or 61). 60 to 80 year old Zoras are about equivalent to Hylian 18 to 22 year olds at this age.
An in-game example of a young adult Zora would be Mipha, before the Great Calamity! She was a bit small for her age, but other than her height she was fully mature by the time she began training with Vah Ruta. I’m going to be totally arbitrary here and say that she was 70 years old when the Calamity struck... my understanding is that Link was 20 years old when the Calamity happened, so they were born 50 years apart but were still in about the ‘same’ stage of their lives!
Another example would be Dunma, Rivan’s daughter who guards the entrance to Zora’s Domain with him. She’s probably around 62 at the time that Link first meets her in-game; I have a feeling she was an early bloomer :B
Stage 8a - Common Adult (100+)
Another self-explanatory stage is the adult stage for the common Zora; this means any Zora who’s not of Royal blood. This is basically when you’ve gotten out of your early twenties and your body’s mostly stopped growing and you start to realize oh man, I’m actually an adult now. So like, a 100 year old Zora is about equivalent to a 24 year old Hylian or human. Adult Zora are generally more serious than young adults, and they start to hold themselves to those higher standards of speech and etiquette that the Zora are so well-known for. This is also generally when a Zora will settle down to have a family, though some get married and have children earlier.
Examples of adult common Zora would be Bazz, Rivan, Gaddison, Laflat, Kodah, etcetera... basically all of the Zora in the Domain who aren’t children, teenagers, oldies, or Royals. To throw out a few ideas I’d say that Bazz, Rivan, and Gaddison are all probably around 145 to 160 years old, having been children/early teenagers when they knew Link. (Rivan’s the baby of the group at 137 years old.)
Stage 8b - Royal Adult (100+)
The adult stage for Royal Zoras is slightly different than that for common Zoras, because Royal Zoras undergo additional growth spurts after they hit the age of 100. An evolutionary quirk that was seen as an indicator of greater strength and fertility in ancient times, the Royal Zora’s first additional growth spurt makes them first grow taller than their compatriots, then broader. They end up looking awkwardly skinny with hands and feet too big for their bodies for a while, but they’ll fill out quickly whether with muscle or fat as long as they have access to adequate food (which, being royalty, they usually do).
After that growth spurt a Royal Zora will grow more gradually over time until they’re anywhere from 16 to 25 feet tall! The final height of a Royal Zora depends on the individual, of course.
The obvious example for a post-growth spurt Royal Zora is Prince Sidon! He is more than 100 years old, as stated in game, and as such is around 10 feet tall - he was closer to 8 feet before his growth spurt. I would peg him at being about 115 years old, which is about equivalent to a 25 or 26-year-old Hylian. It’s not an exact conversion but whatever, he’s a fictional shark man.
Speaking of which - Sidon was 15 years old when the Calamity struck, still just a little one, and Mipha was 55 years older than him; if she had survived she would be 170 years old and Super Tall. ...but still maybe shorter than Sidon. hehehe.
Stage 9 - Senior Adult/Old Age (250+)
Once a Zora hits 250 years they are officially considered “elderly;” 250 for Zoras is about equivalent to 65 for Hylians/humans, along with the expectation of retirement. The average Zora lifespan is 310 years, but there have been recorded instances of Zoras reaching a natural lifespan of up to 375 years old. It is possible that a Zora’s lifespan could be medically or magically extended, but at that point you’re getting into the sort of “toying with life and death” that more environmentally/socially conscious or pious individuals would object to.
King Dorephan is 255 years old, but he is expected to maintain the throne until he dies; on the other hand, Muzu is around 268 but will likely not retire until he feels he’s done all he can to look after the Royal Family. All of the other elderly Zora in the Domain are between 250 and 310 years old, I would say. Dento and Seggin are probably two of the oldest.
WHOOOOO THAT WAS A LOT OF WRITING my head hurts now
#king dorephan#prince sidon#zoras#breath of the wild#legend of zelda#botw#loz#sausage thoughts#headcanon#headcanons#zora#LOOK UPON THIS AND WEEP
133 notes
·
View notes
Quote
I'm no boy. [Then pointed to Martin Luther King, Jr.] This is a boy. I am a man, and until you call me one, I will not listen to you.
Martin Luther King; responding indignantly to a policeman, one day in the 1930s, after accidentally running a stop sign on a Georgia street, who pulled up to his car and said, “All right, boy, pull over and let me see your license.”
Some years later, when King was a civil rights activist writing from a Birmingham, Ala., jail cell, he would point to that word — boy — as one of Jim Crow's ritual humiliations, braided into the racial etiquette of the post-slavery South. It was yet another way — like withholding simple courtesies like honorifics — that white people weaponized language to remind black folks of their place.
The slight was unmistakable. If manhood was the precondition for the actualization of rights, "boy" denied that status even to other men who might lay claim to it. In a region steeped in manners and terms of deference, no black man was ever old enough to age out of "boy"; no white person was ever too young to toss it in his direction.
"Boy" shows up again and again, if implicitly, in the language of black resistance to white oppression.
[...]
So was "boy" a slur? That was a central question of a sprawling employment discrimination suit in Alabama, which began in 1996 and didn't end until 2016. In that case, a black plant worker argued that his white supervisor had called him "boy" as he barked orders at him. For two decades, a series of juries and judges — and eventually the Supreme Court of the United States — repeatedly disagreed over what the supervisor meant when he said it. At one point, some of Martin Luther King's contemporaries in the civil rights movement filed an amicus brief on the plaintiff's behalf, hoping to make the point clear: "If not a proxy for 'nigger,' it is at the very least a close cousin." Unlike that close cousin, of course, "boy" has usages that are not irradiated by race, which provides a lot of plausible deniability for the times when it most certainly is. (The plaintiff eventually won.)
But the echoes of that more sinister denotation remain. Just this past spring, an organization of black journalists urged The Associated Press to adopt new guidelines on "boy, saying that it felt the term was being used too cavalierly in news stories, especially ones about police violence against black males.
Swirling around that legitimate concern about applying "boy" to describe fully grown black men is a growing body of evidence that lays out the ways that actual black boyshave been gerrymandered out of the very notion of boyhood. If childhood is a time of innocence that warrants protection, then that stage of life ends much earlier and more abruptly for black boys.
Research backs this up. In a study from 2014, psychologists asked police officers to look at photographs of boys between the ages of 10 and 17. The officers were told, at random, that the boys in the pictures were suspected of either a petty crime or a felony. Then the participants were asked to guess the ages of the boys in the photos. The officers consistently perceived black boys as older than they were — by an average of 4.5 years.
Those black boys were seen as legal adults when they were a little over 13 years old. (In the same study, the officers saw white boys in the photographs as younger than they actually were.)
This aging up of black boys has serious consequences, the study's authors said, including making it more likely that black boys would have force used on them in police encounters.
"Our research found that black boys can be seen as responsible for their actions at an age when white boys still benefit from the assumption that children are essentially innocent," one of the researchers wrote.
Those findings line up with other studies that have found that black boys are more likely to be tried by prosecutors as adults in criminal proceedings and more likely to be sent to adult prisons. Even in early childhood, black boys face tougher consequences for for their actions than do white boys of the same age. The Yale researcher Walter Gilliam wrote that being either "big, black or boy" was the biggest predictor of whether a child was suspended or expelled from preschool.
White boys — particularly those who are better-off — enjoy that presumption of childhood innocence until much later in life, and it's a distinction that has apparently always been baked into the very notion of adolescence. Back in the 1890s, G. Stanley Hall, the first president of the American Psychological Association, championed the then-novel idea of a distinct developmental stage between childhood and adulthood, according to Ashwini Tambe, a professor of women's studies at the University of Maryland. "He imagined it as a stage of storm and stress and turbulence and sexual experimentation," she said.
But Tambe noted that Hall and his contemporaries imagined this phase of necessary recklessness for those like themselves: male, white, educated and affluent. In his seminal 1904 book, Adolescence, Hall wrote that "[a] period of semicriminality is normal for all healthy boys ... those whose surroundings are bad will continue it, but others will grow away from it as they approach maturity." Practically speaking, this period of constructive delinquency was not on the table for poor children of all races who couldn't put off adult responsibility because they needed to work or for white girls of similar privilege, as they were expected to be better-behaved.
[...]
#1930s#martin luther king#martin luther king jr.#martin luther king jr#quotes#the martin luther king jr. companion: quotations from the speeches essays and books of martin luther king jr.#books#rip#racism#amerikkka#georgia#i'm no boy#npr#jim crow#jim crow laws#npr code switch#weaponized language#white oppression#black resistance#black boys#black men
0 notes
Text
Shout-out to @saminzat for tagging me! Like I needed an excuse to waste time. ;)
LAST
1) Drink:
Coffee... it’s like 10 p.m. at night, but I’m trying to stay awake to finish some work from the office (and yet I’m on tumblr doing this quiz instead, oops).
2) Phone call:
A coworker called me so I’d have her new phone number.
3) Text message:
“FYI, they don’t give you the money right back, you have to wait 4 - 6 WEEKS for a check in the mail, uggggh”. I bailed the same coworker out of jail about three months ago and went to the city municipal court today to get the bail money back... turns out things aren’t that simple.
4) Song listened to:
Umm...so I’ve been listening to the Moana soundtrack pretty much non-stop for the last week. :D
5) Time you cried:
A couple of weeks ago, reading the fic “Cursed or Not” for the first time (hey, you get to chapter 18 and try not to ugly cry, okay?).
HAVE YOU EVER
6) Dated somebody twice:
Yep. Good ol’ high school.
7) Been cheated on:
Not that I know of.
8) Kissed someone and regretted it:
Yep. Good ol’ college.
9) Lost someone special:
Yes, a couple of times.
10) Been depressed:
Yep, special shout-out to my Prozac and Wellbutrin, love you guys. ;)
11) Gotten drunk and puked:
Yes, a few times, unfortunately. Again, good ol’ college (although I can’t use that excuse for the last time because I had already graduated... to whomever had to clean out that train car up in Minneapolis, MN, about 2.5 years ago: I am so, so sorry, I’ve learned my lesson about taking it easy on the Everclear, you have every right to hate me).
THREE FAVOURITE COLOURS
12) Green
13) Purple
14) Blue
IN THE LAST YEAR YOU HAVE YOU
15) Made new friends:
Kind of? Do work friends count?
16) Fallen out of love:
Nah, gotta be in love for that
17) Laughed until you cried:
Yes, most recently was while watching “Impractical Jokers” with my aunt (they took a guy who is terrified of cats and made him teach an improv “how to bond with your cat” class, okay, I found it hilarious as a cat-owner).
18) Found out someone was gossiping about you:
Yeah, there’s a lot of gossip about everyone at my second job. Look, I’m sorry I go through all the water bottles, okay? I drink a lot of water...
19) Met someone who changed your life:
Not anyone specific in the last year that I can think of...
20) Found out who your true friends are:
Meh. I’ve always kinda known.
21) Kissed someone on your Facebook list:
Nah
HOW MANY/MUCH
22) Facebook friends:
256
23) Pets:
Two! One dog, one cat, the best of both worlds.
24) Want to change your name:
Nah, I like my name.
WHAT
25) Did I get for my birthday:
Books, I always ask for books.
26) Time I woke up:
Around 8:30 a.m. this morning
27) Were you doing at midnight:
Probably surfing tumblr, tbh, I am sadly predictable
28) Can’t you wait for:
MY VACATION THIS NEXT WEEK
29) Was the last time you saw your mom:
A couple of weeks ago when I went home for a dentist appointment
30) Is something you wish you could change about your life:
I need to buckle down and really focus on paying off a couple of bills. It helps having a second job, but I’m just so impatient.
31) Are you listening to right now:
Nothing at the mo
32) Gets on your nerves:
Whiners. Don’t get me wrong, I love to bitch and complain as much as the next person, but people who blame the world/ everyone else for their problems? Just....yeah.
33) Talked to a person named Tom:
...this question doesn’t make any sense. “What - talked to a person named Tom”? Also, no, I know several Tims, but no Toms.
34) Is your most visited website:
Pffft, tumblr, of course, is that even a real question
35) Elementary school/primary school:
[Name of my hometown] Elementary School
36) High School:
[Name of my hometown] Jr./ Sr. High School
37) College:
I’ve already mentioned in a couple of posts where I went to college, so I guess I’ll just say it: Kansas State University. EMAW!
38) Hair colour:
Dark brown
39) Long/short hair:
Long! It’s currently the longest it’s ever been in my entire life, I’m so excited (although holy shit, I shed a lot).
40) Crush:
Nah, not for a while. I creeped on a cute security guard a few months ago, but he turned out to be a jerk with a classic “crazy ex-girlfriend” (I put that part in quotation marks because I have no idea if she’s actually ‘crazy’ but he kept insisting she was...which is, just, y’know, a red flag on his part).
41) Do you like about yourself:
I’m actually pretty fond of my hair now, after a lifelong love/hate relationship. I also like to think I’m okay at singing sometimes.
42) Piercings:
None at the moment, actually
43) Blood type:
A+
44) Nickname:
My family has always called me “Foo” (as in, “little bunny foo-foo”)
45) Relationship status:
Single, ayyyyy
46) Zodiac:
Leo (pffft, but not really)
47) Pronouns:
She/her
48) Favourite show:
Supernatural (of course!), Psych, Once Upon a Time, Firefly, Scrubs, Nikita, Game of Thrones
49) Tattoos:
None. I’m too fickle, I’d get one and then change my mind two weeks later.
50) Left or right handed:
Right
FIRST
51) Surgery:
I had my tonsils out when I was 17 thanks to multiple bouts with strep throat. Oh my god, never wait until you’re that old to get your tonsils removed, it was absolute hell.
52) Piercings:
My ears. If we’re talking unusual piercings, I had a “nape piercing” for a while in high school.
53) Best friend:
Probably my cousin Kayla, since we grew up together
54) Sport:
I played softball for several years as a kid, until I got a bloody nose when the ball hit me in the face. Then I had to quit because I was gun-shy. To this day, I’m still afraid of balls flying at my face (hehehe).
55) Vacation:
I visited my dad in San Diego, CA for a week when I was ten years old
56) Pair of shoes:
First pair of shoes? I don’t know, I was a baby. Probably some over-priced cutesy pair that never even got any use because I was a baby.
RIGHT NOW
57) Eating:
Spicy Doritos
58) Drinking:
Still drinking coffee
59) I am about to:
Sort through my tumblr “Saved Drafts” and add tags for everything, then try to get some writing done
60) Listening to:
Nothing at the mo (this is the same question at #31?)
61) Waiting for:
Saturday when I leave for vacation! *o*
62) Want to see:
Honestly can’t think of anything. I’d like to watch Moana again but it’s not on DVD yet?
63) Want to get married:
Sure, someday
64) Career:
Human services/ social work-ish? Basically, I work at a non-profit agency helping adults with developmental/ intellectual disabilities to get/ maintain services. Oh, and I also have a part-time job at an adult store. Gotta make ends meet, y’know.
WHICH IS BETTER
65) Hugs/kisses:
Really depends on who they’re from. Probably hugs for the most part. :)
66) Lips/eyes:
Aaagh, I don’t know... I love gorgeous eyes, but I also love me some tasty lips... y’know what, I’m gonna go with lips. Yep.
67) Taller/shorter:
Taller
68) Younger/older:
Older
69) Romantic/spontaneous:
I can be romantic when I have someone to be romantic for, but I’m not the most spontaneous. :D Like, let’s just stick to the PLAN, okay?
70) Nice arms/nice stomach:
Arms. I like squishy cuddly tummies anyways.
71) Sensitive/loud:
...I don’t know. Sensitive, I guess, because being around loud people wears me out pretty quickly. But sensitivity needs to have limits too...
72) Hookup/relationship:
Relationship. Been there, done the hook-up thing, not worth it. Good ol’ college.
73) Troublemaker/hesitant:
At this point in my life, I’d say hesitant. Trouble-making was fun in the past, but, like, I’ve got an actual career now that I could lose if I go around trouble-making/ hanging out with trouble-makers.
HAVE YOU EVER
74) Kissed a stranger:
So, so many times. Good ol’ college.
75) Drank hard liquor:
Yep. Still love me some vodka. It just mixes with everything, y’know?
76) Lost glasses/contact lenses:
Contact lenses, yes, but luckily I’ve never lost a pair of glasses
77) Turned someone down:
Yes. I hate doing that. I’m a horrible, cowardly person who would rather “ghost” someone than have to deal with an uncomfortable confrontation.
78) Canoodling on a first date:
Depends on the definition of “canoodling”. Are we talking cuddling or snuggling up during a movie? Sure. Making out? Maaaybe, depends. No copping a feel on the first date though, c’mon now.
79) Broken someone’s heart:
Yes. Breaking up with someone in high school is intense.
80) Had your own heart broken:
Kind of, not really? The only person I legitimately had feelings for, I never told them how I felt, so they never really had the opportunity to break my heart but it hurt like hell anyways. Have I mentioned I’m a cowardly piece of shit? :D I mean, that was like 10 years ago in high school, but I haven’t changed that much.
81) Been arrested:
No, thank goodness. There were a couple of close calls during my partying days, I’ve definitely been luckier than I probably deserve.
82) Cried when someone died:
Yes. Doesn’t happen often, luckily.
83) Fallen for a friend:
Not really? Had crushes on friends, had friends-with-benefits, yes, but never technically “fallen for” a friend.
DO YOU BELIEVE IN
84) Yourself:
Depends on what we’re talking about here. In general, yeah, I like to think I do okay...
85) Miracles:
Ehhh, I can’t decide. It’s a wonderful thought but I’m also kind of a pessimist realist. You know what they say: “hope for the best but prepare for the worst”.
86) Santa Clause:
Not for many, many years
87) Kisses on a first date:
Sure! End-of-the-date kisses are sweet.
88) Angels:
I...think so.
89) Love at first sight:
I don’t know? It’s a wonderful thought but I’m just not sure. Maybe not love at first sight, per se, but I think there are definitely people out there that you can just tell right away they’re going to be special to you.
OTHER
90) Best friend’s name:
None, at the mo
91) Eye colour:
Brown
92) Favourite movie:
That’s a tough one... I think it depends on my mood. Do I want to laugh? Something trashy like “Sorority Boys”. Do I want to cry? Probably something steeped in existential crisis like “A.I.”. Do I want a feel-good adventure with talking animals? “Homeward Bound”.
Holy crap, that took like 1.5 hours. Anyone need an excuse to waste some time/ procrastinate/ be distracted? Tagging @magnificent-winged-beast, @helianthus21, @destielmixtape, @beesandangelkisses, @emotionally-compromised-idiot, @castielsgracex, @apritelleorai, @honeybee-and-batman, @sunshine-hunters, @waaaaaayward-assbutt, @cool-fallen-angel , and anyone else who wants to do it. :)
3 notes
·
View notes
Note
NO THE ANON ASKED QUESTIONS BEFORE I DID THATS MY JOB :( DO ALL THE ONES YOU HAVENT DONE
1. You woke up naked next to the last person you texted, what would you say?
Good morning...?
2. What’s going on between you and the last person you kissed?
We are happily together.
3. If your boyfriend or girlfriend was into drugs, would you care?
hard drugs? yes. Pot, I’d live with.
4. Is your last name longer than six letters?
My last name is in fact 6 letters.
5. Was your last kiss drunk or sober?
sober (as were the rest of them)
6. Have you ever wanted to have someone but you messed it up?
I don’t think so, it never got to the point of me having an opportunity to mess it up. & last time, it worked. ♥
7. What does your last received text say?
“I have my moments”
8. How many times have you kissed the last person you kissed?
Approximately 5.964. (I have no idea, but a lot).
9. Where was your last kiss at?
My front door when he left.
10. When is the last time you saw your sister?
Well this implies that I have a sister.
11. What do you drink in the morning?
Powerade? or nothing
12. Where did you sleep last night?
In my own bed.
13. Do you think relationships are hard?
They require work, which I guess could be seen as hard. With the right person, it is worth it though.
14. If you could go back and change something in the past 5 months, would you?
Less procrastinating maybe, but Id put off changing it...
15. You’re locked in a room with the last person you kissed, any problems?
This sounds very ideal. (Yall are obsessed with the last person I kissed, huh?)
16. Would you rather it be sunny or rainy?
Depends on the day. More often than not, rainy though.
17. Do you know anyone with the same middle name as you?
Yes I do, a friend’s brother. Shane Dawson does too, if that counts.
18. Are you wearing jeans,sweatpants,or pajama pants?
Sweatpants
19. Do you think you will be in a relationship 3 years from now?
I surely hope so
20. Does anyone like you?
I surely hope so (Im looking at you Alex)
21. Have you ever kissed someone with a name that starts with an S?
I don’t believe so.
22. Is the last person you kissed gay?
I hope not, I want him to like me.
23. Is there a person you CANNOT stand?
Trump
24. Have you ever considered getting a tattoo?
Plethora of times.
25. In the past week have you cried?
I think so
26. What breed was the last dog you saw?
Husky, I wanted to steal him/her.
27. Do you dry off in the shower or out of the shower?
I dry mostly In the shower because I don’t want to be cold, but then I lay in bed in a towel for hours before getting dressed...
28. Have you ever kissed a football player?
Sorta
29. Do you think you’re old?
In certain contexts, yes.
30. Do you like text messaging?
With Alex, yes. other people, eh.
31. What type of day are you having?
Filled with HECKS.
32. Have you ever thought about getting your nose pierced?
No, I don’t need more attention brought to my huge nose.
33. Do you prefer warm or cold weather?
Cold, but not to the point of painful air.
34. Is there a person of the opposite sex who means a lot to you?
yes.
35. Would you prefer a relationship or a fling?
relationship.
36. Are you a simple or complicated person?
complicated af, sorry everyone who deals with me.
37. What song are you listening to?
“Keep the Dogs at Bay” - Seether
38. When you say you’re sorry do you mean it?
Yes, I say it as a defense mechanism alot, but I still mean it.
39. Is there a girl that knows everything or almost everything about you?
@x-i-a-t40. What made you start liking the person you like now?
His ability to make me laugh, and my sense of comfort with him.41. When did you last receive a text message?
Feb. 22nd, 4:19 pm42. What is wrong with you right now?
Is that a rhetorical question? Lots of things. 43. How well do you know the last female you texted?
Well, including Kik, its @x-i-a-t and I think I know her pretty well. SMS only, it is my Granny, and I know her a good amount, I don’t know much about her past.44. Does anyone disgust you?
Trump?45. Would you date someone right now if they asked?
No, unless Alex asked?46. Are you in a good mood right now?
Not really, but I’m not upset either. 47. Who was the last person you talked to in person?
My Developmental Psychology Professor, he is known as Mr. Nugget.48. What color shirt are you wearing?
Plum Purple? Dark Magenta kinda? colors are hard.49. Has someone recently told you something you didn’t want to hear?
Professors, yes, lol.50. Anyone you’re giving up on?
If myself counts then yeah kinda. 51. Do you hate the person you fell hardest for?
No? I love him
52. Have you ever thought about giving up on someone but couldn’t?
Yes. 53. Do you like rain?
Yes. 54. Do you care if your boyfriend/girlfriend drinks?
Yes. Boy, bye. 55. Have you ever liked somebody and never told them?
In high school. 56. Do you like to cuddle?
With him, yes. 57. Are you shy?
In certain situations. Most of the time, not really. 58. Do you get along with girls?
I get along with most people, so yes.59. Have you dated the person you texted last?
Currently 60. What do you carry with you at all times?
My phone 61. If you were paid 1 million dollars to spend the night in a supposed haunted house, would you?
Hell yeah, Id sleep the whole time... come at me ghosties. 62. Do you think you can last in a relationship for five months?
yes? is that supposed to be hard? Currently at 7 months, but was previously in a relationship for 4 years. 63. Think back to October, were you in a relationship?
Yes♥ 64. The person you like kisses you on the forehead, do you find this cute?
Of course. Its real convenient given our height difference. 65. Did anything “cute” happen in the last week?
He does cute things all the time.
66. How old are the last three people you kissed?
20, 19, 23 (I think? maybe 22)
67. Would you rather pay to get your nails done or do them yourself?
Do them myself. 68. Which do you like better- Zebra print or leopard print?
Zebra. 69. Do you have any stickers on your car?
Nope70. Would you rather listen to Luke Bryan or Lil Wayne?
LUKE BRYAN 71. Blackberry, Android, or iPhone?
Android
72. When’s the last time you had pizza from Pizza Hut?
Valentine’s Day ♥ 73. Do you like diet soda?
Not particularly 74. What color are the walls in your room?
Poster colored. (Okay white & one blue but I haven’t seen my walls in years)75. Are you 16 or older?
Yes.76. Do you watch Pretty Little Liars?
No 77. Do you have a job?
Yes 78. What are your initials?
GLT79. Did you ever have braces?
Yes :( 80. Are you from the south?
SOUTHern California count? no? Ill go
81. What does your last status on facebook say?
Ive never posted one 82. Do you still talk to the first person you ever kissed?
Lol no 83. Are you closer to your mom or your dad?
Mom84. Have you ever done cheerleading or gymnastics?
LOL nope85. What’s the last movie you saw in theaters?
Passengers 86. Do you smoke?
No
87. Would you rather wear heels or flip flops?
What am I doing? Probably heels, unless Im at work? lol 88. Is your phone touch screen?
Yes89. Do you normally wear your hair straight or curly?
Straight 90. Have you ever snuck out of your house?
Once, Kinda? vague af I know91. Would you rather swim in a river, lake, or pool?
Pool 92. Have you ever made out in a car?
Yes93. …Had sex in a car?
No94. Are you single or in a relationship?
Wasnt this asked already? relationship. 95. What were you doing last night at midnight?
Studying, also on the phone with Alex, I think. 96. When’s the last time you saw fireworks?
Fourth of July I think.97. Do you like the camera on your phone?
It’s fine 98. Have you ever had a friend with benefits?
Nope99. Have you ever passed out from drinking?
Nope100. Are you friends with people on facebook that you actually hate?
Dislike sure, hates a little strong. 101. Have you ever had a pregnancy scare?
Kinda102. Name your favorite Kesha song:
Well Tik Tok is the only one I know, so I guess I am going with that one. 103. Do you have any tan lines right now?
Kinda, very light though at this point. 104. Would you ever wear cowboy boots with shorts?
If I had cowboy boots, sure.
0 notes
Text
2021 Ehlers Danlos Society Awareness Month (Day 12 Prompt: Nurses and Doctors)
I have already covered much of this topic in previous posts so it's no secret that I have very little trust in the medical field. Of well over 200 doctors I have interacted with through both specialists, medical clinics, urgent care and hospitals there is only one that I have total trust in. Yes on and only one doctor who I trust with my life. I used to have more trust in doctors and used to have the mindset that I trust them until they give me a reason not to trust them because most kids are raised to believe that doctors and nurses are the good guys/girls I had my first experience that I remember with a medical professional at the age of five and they just kept adding up.
Layer after layer of abuse and neglect, four times being dead on their time and three times being so sick my blood pressure registered as clinically dead even though my heart continued to beat and all but one of these times I was not treated by medical personnel, once being revived by my mom in a hospital full of doctors and nurses ignoring my alarms. I have been released multiple times even up to the point of needing ICU level care with psychosomatic disorder labels slapped on me they didn't want to put the work into saving me. My uncle has died at the hands of the medical system from this disease and my mom defied the odds with only a 5% chance of survival rate and more time than I care to think about in a coma and in ICU as a result of a doctor who didn't know what he was doing and botched her surgery then both abused and neglected her for 9 hours after his mistake while trying to hide it so he wouldn’t get caught.
I don’t only have experience as a patient in the medical field but also as a nurse myself. I can't tell you how many times I heard students say they weren't going to do certain procedures because they were gross or uncomfortable like changing a colonoscopy bag acting as if the patient is gross because they have a medical condition that results in something that they believe is unpleasant or undesirable. How do they think the patient with the colostomy bag feels without their nurse making them feel gross, ugly or undesirable. I worked as an STNA where I was raped by my boss. I worked as an LPN at a long term care facility for children with severe to profound developmental delays and complex physical health conditions.
The state recommends no more than four patients be assigned to one nurse and no more than two patients to one nurse in a critical care setting. These patients were total care and at the most I was assigned 17 patients. 17 when there was only one of me and to give you an idea of what total care entities, All 17 were in diapers and needed changing every two hours, with one being on a toileting program meaning every morning she had to be put onto the toilet and strapped onto it with a harness since she had little control of her body and prone to falling off. We were to leave her on the toilet for 15 minutes or until she went to the bathroom and were not allowed to leave her room until she was done. The bathroom connected to two rooms and there were usually three kids in each room with the bathroom being between both of them so shared by six kids. We were not allowed to leave her alone on the toilet but could leave the bathroom itself if we left the door open so we could hear her so we could go into one of the rooms attached to it and change another kids diaper or change bedding but other than that we could not go any further until she was done. She was diapered the rest of the day unless you had more time to work with her later in the day so only did her toileting routine a minimum of once for morning shift and once for night shift. All children needed their bedding changed daily, they all needed a bath every day, clothes changed, hair done, teeth brushed, and some of the older guys we would shave their face if their family wanted us to. 15 of the 17 were tube fed or on TPN so I had to hook up their feeds. The other two, one ate solid food and the other was on a puree diet. They did not eat in their rooms and had to be taken to a group room with a table where we had to allow them a minimum of a half hour to eat. If they refused food we had to try to offer it for at least a half hour. One of the two needed feeding and the other was much more high functioning than the others on the unit so could feed himself, you just had to remind him to eat if he got distracted. All of them had medications, some up to six times a day. None could walk so they all needed picked up and put into their chairs and into their beds, one could craw and if we let her crawl we put knee pads on her knees so she didn't hurt her knees, one could walk using a gait trainer which is basically like a baby walker but bigger, where the strap goes between their legs so they don't have to hold their weight but can push with their feet to slide the walker. 14 of then needed turned every two hours to prevent pressure ulcers, one had a colostomy bag, one had a tracheostomy. They all needed rectal temps daily, They all had to go to the rec room and get some time on the matts daily, 14 of them had physical therapy which we were responsible for except once a week when a therapist worked with them
Therapy for 10 of them dealt with button training where a button as connected to a toy, TV, radio etc. and they had to press the button with their hand or head to get the TV to change or toy to light up or play music and what not. They did their therapy until either they pressed the button on their own ten times or a half hour had passed, whichever came first. One would get in her walker and needed us to guide her to take at least one lap around the unit in her walker, the other did the toileting program and we worked with her on using a modified form and spoon to eat herself, 6 of them did sucker therapy which essentially we would hold a sucker for them to lick in hopes to improve their swallowing skills and build up their saliva so hopefully one day they could get off the feeding tube or be less reliant on it, able to eat some puree or possibly one day solid foods. One we worked with his fine motor skills to have him pick things up but he was easy when it came to this because we could do it throughout the day so if I was changing him I could ask him to hold the clean diaper for me or a wipe or two and while I gave him a bath I could have him hold his tooth brush or comb or his deodorant so that I could combine with a lot of other routines but it helped him with both being able to grasp things and to learn to release his grasp at appropriate times.
11 of them worked on eye gaze to relay their needs so instead of just grabbing clothes and putting them on them we had to pick out at least two shirts, two pairs of pants, two pairs of socks etc. and ask them which one they wanted to work on eye gaze for them to tell us which they wanted. The highest functioning one was learning to use a power chair at the time so we had to follow him with a kill switch and joystick so we could make sure he didn’t run into anything or if we needed to turn the chair so he didn't hit the wall etc. he was also working on menu training where we could give him a picture menu for him to choose what he wanted for his next meal starting with two options for a main dish, like chicken nuggets or mac and cheese, two options for a side dish like cheese slices or apple sauce, two options for a second side like green beans or corn and two options for a dessert such as chips which were more like cheese puffs in different flavors or a cup of ice cream and eventually add more and more options Two of them were labeled as combative which I never had an issue with even once as I also majored in interpreting and learned very quickly that one was combative because he was the only one who could talk but some had trouble understanding him so he got frustrated kind of like a child in their terrible twos who is frustrated because people may not understand their speech, the other was deaf blind and no one worked with her on any kind of sign language or gesturing. As you can see, this is way way too much for one person to take care of.
Now to make things worse, I felt as if I was the only nurse who had any ethics. I felt horrible for these kids because they basically just sat them in front of a tv all day. They had an accessible playground outside which I had never once seen used because they hired so few staff that you didn't have extra time. We had four nurses on our unit which had, if I remember right 23 kids in our unit which doesn't sound too bad but we rotated days off with one weekend off a year so only three people were there at any given time. When someone took a week off we had two of us. Some went to day programs so during the week we usually had around six to 8 residents. On holidays such as the day I had 17 kids I was the only one and there. Two of them took Easter off and one already had that day already off and the boss let this happen. 6 of the kids, their parents took out day passes and took them home for Easter thankfully because I don't know what I would have done with another six kids.
This being said they didn't hire enough people so if someone from another unit called off they would take someone from another unit. The unit I worked on had the most severe children. There were other units that had the ones with moderate disabilities so could do things like brush their teeth, sit up, feed them self and just needed care like bathing, transferring them into their chairs, making sure they didn't get in trouble or fight with other kids, change their diapers or help them change their own or help them toilet themselves or care for catheters so they were a lot easier. There was another unit where most of the kids only had mild delays and basically just needed the staff to work with them on daily living skills like cooking and making sure they shut off the stove, go for walks with them to make sure they didn't get lost or walk up to strangers etc. they had another unit that was all babies two and under so though some of them had pretty advanced delays its a lot easier to pick up or change a 2 year old's diaper than it is a 19 year old's diet. Staff was an issue.
Now for lazy staff. I felt like the only one who actually worked and took a lot of the kids under my wing even if they weren't mine. When the “nurses just play cards thing” came out on tv I couldn't help but laugh because we had one nurse in charge of the most critical patient on the ward. He had no brain and only a brain stem. With a brain stem only your most basic body functions are controlled like breathing, heart rate, kidney function to produce urine and heating and cooling. You can't make pictures of images seen by your eyes so it’s pure darkness, you can't make meaning of sounds you hear so pure silence, cannot register a sense of touch or feeling, no voluntary movements etc. This being said he was hooked to monitors that were linked to a pager to alert his nurse to know if he stopped breathing or his heart stopped and you would need to rush in and do a sternum rub or sometimes CPR on him. This would happen anywhere from a few times a week to on and off all day. He literally would die over and over and over again so we had to be quick to revive him each time.
His nurse was notorious for taking off her pager and laying it in his bed, on his night stand, at one of the computer kiosks for logging, in the rec room etc. and then just going off and playing cards with another staff member. His door had a light and alarm too but it was really quiet which was a big reason the nurse had a pager. If they were busy changing another kid or something, they could yell for someone else because yelling was even louder than the door chime but she did this so much, I got to be like a new mother with a newborn baby where I could hear the ding of his light from a mile away because I knew if I didn't revive him she sure as heck wouldn't we had a room with three boys in it, an 8 year old, a 10 year old and an 11 year old. They were non verbal and there were two nurses who would run into that room and drop their pants and moon each other.
Most of the staff would skip bathing kids for sometimes days on end and just mark it on their charts that they had been bathed. This was especially so for the kids whose families lived out of state or kids who were property of the state and had little to no visitors. These kids were neglected to the fullest. Left in dirty diapers, had physical therapy skipped, were not rolled as much as they should be including one that got MRSA. If one of their family members showed up unexpectedly it would be like all hands on deck, they would call all of the nurses to their room while the receptionist lied to the parents saying they were in therapy or still in the bath or something and have two nurses yanking their clothes off throwing them in the tub to try to scrub them down one getting their clothes and changing their bedding changed, room cleaned, aids in there with mops mopping the floor and cleaning up the other kids in the room, changing their diapers, washing their faces and doing their hair, opening curtains, organizing stuff that's laying all over the place all in about ten minutes flat to try to make it look like their kid was taken care of the whole time. It was called “all men on deck” when this happened, they would even call people from other units for this so it's like we magically went from no staff to a ton of staff for ten minutes only.
The same thing happened when they got a call from the health inspectors. All blankets got pulled out of the closet because they weren't allowed in the closet with sterile items, no one was allowed to take off but they took half the staff and assigned them to cleaning, moving meds to the appropriate storage area, removing cleaning chemicals from the same area as the fluids and cartons of ensure and tube feed. They had so many violations it wasn't funny but knew exactly what needed fixed or removed before the health department and medical board visits. They had extra stuff they shoved in staff members' trunks of their car, in offices and all kinds of hiding spots then would just move it all back after they passed and it was over. I don't know why they never came unannounced. The nurse who used to leave her pager laying around didn't like me at all and would go into my kids rooms after I walked out and drop the bed rails on my kids beds to try to get me fired.
During my training they put me with a resident who was very sick. She had what they thought was the flu. She had a trach so couldn't control her cough which came right out of her tracheostomy, really bad diarrhea, a fever most of the first week I was there, the whole nine yards of being sick. Well after training I got sick but they had a one month probationary period in which you were not allowed to miss any days in that time and they said if you were sick you had to be checked out by one of the NP’s who would take your temperature and assess you to determine if you are healthy enough to work or not and only if they determined you were too sick were you allowed to take off during your probationary period. Well I got worse and worse and ended up developing pneumonia. So like her was hacking up a lung. I woke up with a temp of 103 and by the time I got to work my temp was 103.8.
I saw the NP and showed her the paperwork from urgent care where I had been diagnosed with pneumonia and stated my concern about spreading it to my kids who were all immunocompromised and high risk. The NP said I would be fine and told me to just wear a mask. I put on a mask and went to work. They gave me a ton of kids that day too, I want to say I had 12 that day so I was running around like a chicken with my head cut off, getting dizzy spells and I could feel my fever exploding. I could feel sweat running down my back and chest and kept having to wipe the sweat off from my face. I literally felt like I was going to fall over and die running around, lifting teenagers, and rushing around to try to keep up which was nearly impossible because of short staff anyhow. Well I started overheating and coughing so badly that I had to take off to a bathroom in the hall and started throwing up and was struggling to breathe from all of the mucus and feeling like my airway and sore throat was swollen up and totally full of mucus. My boss came in while I was throwing up and said “why aren't you out there doing your job. Of course I’m there in the stall hanging over the toilet with all the sound effects of my vomiting, coughing and wheezing and told her I was sorry but I have pneumonia and got too hot. She said “well you need to come out here and do your job and throw up on your own time” Yes she told me to throw up on my own time. I said what because I was throwing up and thought I misunderstood her and she said “I need you to throw up on your own time” like you can control something like that and as if they hadn’t trained me on a patient who was sick and very contagious earlier that month. She told me if I didn't get out there then she would be writing me up and if you get a writeup during your probation time you will lose your job; then she left.
About two minutes later I got to a point where I thought I may be able to make a run for the supply closet which was right across from the bathroom, ran over there and grabbed some of their mini garbage bags that go into the little feminine care product trash cans and spent the rest of the day, working and running around the corner into the patients bathrooms to throw up in the bags and throwing them into the hazmat containers. I felt terrible with my patients having to listen to me throwing up right beside them but the boss wouldn't let me go to the bathroom or go home saying I wasn't too sick to take off even throwing up about 15 more times throughout the day and so dizzy I had no idea how I didn't pass out in front of any of my kids. When I went home that day, I took my temperature and it was 105.2. And that was with taking fever reducing medication while at work. After lying down a while it went down to 104.8 and I had the next two days off thankfully but by the next morning I was in the hospital passing out over and over again, having trouble breathing and under rapid cooling protocol having cool IV fluids pumped into me, wet towels put on me, ice packs layered around me benign told by the staff that any job that makes you work when you're that sick isn't worth keeping and how they would have just walked out.
I still hadn't been there long, almost three months, when I went to the linen closet with the towels, wash cloths, chux etc. and it was totally empty except for one wash cloth so I went to the manager filling in for mine who was on maternity lead and told her the linen closet needed restocked. They never told me what to do in this situation so I didn't know if we had a number to call down to laundry for them to bring it up, had to send an aid down to bring up a cart of clean linen to restock the closet or it was our responsibility to go down and get a cart full of clean linen and stock the closet. There was no list of phone numbers by the phone or anything because I checked before I asked the manager and when I asked she was in the rec room full of children with intellectual and physical disabilities. I told her the closet needed restocked and asked if there's a number I need to call for more, if I go get it or how that works telling her no one had told me how this works when I started. She looked at me like I was a total idiot and said “I see we have another retard in here as if we don't already have enough!” right in front of those kids. Enough was enough at that point and at the end of the day I said I wasn’t coming back.
I bawled my eyes out having to leave that job because those kids became like your kids and the care they got was god awful. They deserved a lot more than lying in a bed in front of a tiny tv all day. The other nurses didn't even meet their most basic needs leaving them in overflowing diapers, I can't tell you how many mornings I walked in after second shift left to find dirty diapers laying in the kids beds including one that my residents knee was laying in because they couldn't even throw away a dirty diaper. Basic needs like personal care, rolling them and the needs to sustain life and keep them safe weren't even met but kids have many more needs than just those most basic ones.
There was a playground that was never once used. They had no volunteers or staff to take them out of their rooms for a walk, to take them to the play room and actually play with them, hold crayons in their hands and help them color or finger-paint with non toxic or edible finger paints, do things with the teens that most teens take for granted like painting their nails, reading them books, bringing around therapy animals or even having an in house therapy animal. They just left them in their beds or laying on the floor on a mattress pretty much all day and all night which isn't a way for a child to live regardless of their cognitive function. That job took everything I had to give and gave me almost a try to save the world mindset because I wanted these kids to have the lives they deserved.
There was even one of the kids labeled as combative who was deaf/blind who I really connected with who I looked into adopting. The other staff couldn't stand her, literally ripping through her hair, yanking her neck back, forcefully ripping her hands off of them, basically tossing her into her chair. Some of these nurses were physically abusive with her because she was basically just really grabby and it made them mad. I realized the actual problem is that she was Deaf/Blind and they would literally just grab her and do whatever they wanted to. She was scared. She didn't know who was grabbing her or what they were doing so would grab for the hands and face to try to figure out who had a hold of her. Everyone used to ask me why she wasn't grabby with me yet no one took my advice. I told them they had to let her know who they were and what they were doing. Let her touch their face and hands to know who was there and touch is totally normal. It was just grabbing because she would be in a panic but she would be very gentle if you took things a little slower and gave her a chance. I would go into her room and instead of just yanking her up out of bed, I would tap her on the arm or sometimes just sit down on her bed and she would feel the movement and move her hands around to try to find it so I would put my hand by one of her hands so she grabbed my fingers then move her fingers toward my face so she could find my face and feel it. A lot of the staff thought it was gross because she put her fingers in her mouth but we knew her medical break down and a little spit wasn't going to kill anyone. That's what baby wipes are for but I would let her feel my face so she knew who I was and she would calm down once she realized it was me.
If I was going to put her in her wheelchair I would tactile sign the word chair then pull her chair up to her bed and guide her hand over to it and put it on the wheels so she could feel it. If I picked her up, I would put my arms under her like I was going to pick her up but not actually lift her for about three seconds so she got used to knowing if I slid my hand behind her back and under her legs that I was about to pick her up and put her in her chair which she had already felt. If she needed a bath most of the staff threw her clothes in the bathroom and got the water going and stuff. Then yank her up and carry her in the bathroom with her having no idea what was going on. I would first put her in her chair and take her in her chair into the bathroom because once I put her in her chair and signed a bath I could get her clothes and diaper and such and sit it on her lap so she could feel them and realize that she was about to change clothes or take a bath. I would then wheel her into the bathroom and the tub had a sprayer and it was a wet room so if you got the floor wet it had a drain and didn't hurt anything. I would take her clothes from her and set them on the counter and then turn on the water to the right temperature and bring the sprayer down. If I touched her hand she would usually grab my fingers and I would pull her arm out to the side and put her hand under the water so she could feel it with her hand and knew she was going to take a bath. I put the hose in the tub basin and signed the bath again. Put my hand behind her back and under her knees again giving her a second for it to register that I was going to pick her up again, lift her and put her in the tub which was basically like lounge chair, take her clothes off starting slowly with her socks instead of a large piece of clothing that was more shocking then after taking her socks off moved to the larger pieces of clothing. When I went to spray her to get her wet I again put her hand under the water and then moved the sprayer slowly up her arm so she knew she was going to get wet, bathed her and dressed her.
If I changed her I would sign the diaper and give her the diaper to hold before taking her pants off or anything so she knew she was going to get a diaper change. Once I took off her pants, before removing her diaper I would get one baby wipe and put it in her other hand so when I took the diaper off she knew when I took the wipe away from her that she was about to feel the cool whip. If I did her hair, I would give her a comb and brush to hold and would take whatever one I needed at the time out of her hand and to make things easier, I actually taught myself how to French braid on her hair because French braiding it kept it from getting tangled and matted so combing out her hair wouldn't be so traumatic for her, especially when another staff member had her but she was really a very easy and laid back kid just very much misunderstood which is why I requested her as my permanent. I actually took the two kids on the unit that no one wanted and they were both great kids and I just don't understand how a medical facility can operate with such ignorance. So though it was hard to leave I feel like I made the best decision. When I left I called Children's Services, Our county's Department of Developmental Disabilities, The Medical Board and the Health Department hoping that even though I had to leave, the lives of those children would improve.
I have had many negative experiences with other medical workers both as a patient and as a nurse. There are so many unethical, abusive and neglectful medical personnel so I no longer live by the mindset that all medical personnel is good unless they prove otherwise, realizing just how rare good doctors, nurses and other medical personnel are to come by and now believe that they are all bad and have zero trust in them unless they can prove otherwise. It's very difficult and takes a very long time for medical personnel to gain my trust. I’ve had this trust for too many in the past who let me down so now that trust has to be gained over a long period of time. As I mentioned before, I have one doctor I have trust in and his name is Dr. Joseph. It took him almost two years to gain that trust and this is a doctor I see every two weeks so I have seen him more in two years than I see most doctors in ten years if this puts into perspective how long it takes to trust a doctor. Trust isn't something a lot of EDS patients have in the medical field but many have experiences similar to mine so it’s easy to understand why.

0 notes
Text
Lost On The Frontline
America’s health care workers are dying. In some states, medical personnel account for as many as 20% of known coronavirus cases. They tend to patients in hospitals, treating them, serving them food and cleaning their rooms. Others at risk work in nursing homes or are employed as home health aides.
“Lost on the Frontline,” a collaboration between KHN and The Guardian, has identified 586 such workers who likely died of COVID-19 after helping patients during the pandemic.
We have published profiles for 105 workers whose deaths have been confirmed by our reporters.
Some cases are shrouded in secrecy. Our team contacts family members, employers and medical examiners to independently confirm each death. Many hospitals have been overwhelmed and workers sometimes have lacked protective equipment or suffer from underlying health conditions that make them vulnerable to the highly infectious virus. In the chaos, COVID casualties might otherwise get overlooked.
This project aims to document the lives of U.S. health workers who die of COVID-19, and to understand why so many are falling victim to the pandemic.
Lost On The Frontline
This project aims to document the life of every health care worker in America who dies from COVID-19. If you have a colleague or loved one we should include, please share their story.
A Physician Assistant Who Mentored Residents At His Hospital
(Courtesy of Alexander Beylinson)
Alex Bass
Age: 52
Occupation: Physician assistant
Place of Work: NYC Health + Hospitals/Coney Island in Brooklyn, New York
Date of Death: April 10, 2020
Alex Bass was technically a physician assistant, but his patients all called him “Dr. Bass,” a title his boss said was well-deserved.
Read More
Exclusive: Nearly 600 — And Counting — US Health Workers Have Died Of COVID-19 Jun 6
Hospital Workers Complain of Minimal Disclosure After COVID Exposures May 13
Widely Used Surgical Masks Are Putting Health Care Workers At Serious Risk Apr 28
OSHA Probing Health Worker Deaths But Urges Inspectors To Spare The Penalties Apr 22
True Toll Of COVID-19 On U.S. Health Care Workers Unknown Apr 15
“His patients often sent us letters, thanking us for the services that he provided and saying how great he was,” said Dr. Abdo Kabarriti, chief of urology at Coney Island Hospital.
Bass moved to the U.S. from Ukraine in his mid-20s. Rather than redoing medical school, he decided to become a PA. His extensive knowledge led him to mentor numerous urology residents.
“He helped a lot of people really become who they are today,” Kabarriti said.
When Bass noticed a fever spike in mid-March, he stopped going to work and made an appointment with Dr. Alexander Beylinson, his primary physician and friend of 26 years.
He arrived at his office on March 20 looking “very sick,” so Beylinson tested him for COVID-19 and sent him to the hospital.
A few days later, the test came back positive. At that point, it was too difficult for Bass to talk. Soon after, he was put on a ventilator, until he died.
The hospital did not comment on whether Bass had worked with COVID-19 patients.
Beylinson was one of the 10 people at Bass’ funeral. He doesn’t feel he achieved closure, he said, and still considers Bass his “hero.”
— Shoshana Dubnow | Published June 10, 2020
(Return to top.)
‘There Were So Many Things She Had Unfinished’
(Courtesy of Brittany Mathis)
Dulce Garcia
Age: 29
Occupation: Clinical interpreter
Place of Work: University of North Carolina Hospitals in Chapel Hill, North Carolina
Date of Death: May 26, 2020
Dulce Garcia loved to dance. On weekends, she would escape with friends to the Luna Nightclub in Durham, where they would romp to bachata, merengue and reggaetón. “It was our ritual,” said Brittany Mathis, one of her close friends.
At dawn, those unable to safely drive would sleep over at Garcia’s. “She was the group mom,” Mathis said. “She’d tell us, ‘We don’t want to lose anyone.’”
Garcia was “the rock and foundation” for her family, Mathis said. As a teen, Garcia cared for siblings while her parents worked. She also volunteered at the neighborhood Boys & Girls Club.
When Garcia learned about the health care gaps faced by Spanish speakers, she joined the hospital. There, she was “surprised at how much she could help,” Mathis said, “and how many needed her.”
The week after she picked up a Sunday shift, she developed a fever. Mathis was not sure whether she received personal protective equipment (PPE). “Our PPE policies have always followed CDC guidance,” the hospital said through a spokesperson.
The symptoms “wouldn’t go away,” Mathis said. “It just doesn’t feel real. There were so many things she had unfinished.”
— Eli Cahan | Published June 10, 2020
(Return to top.)
A Friendly Nursing Assistant Who Worked Into Her 70s
Antonia ‘Tony’ Sisemore
Age: 72
Occupation: Certified nursing assistant
Place of Work: Stollwood Convalescent Hospital at St. John’s Retirement Village in Woodland, California
Date of Death: April 30, 2020
Antonia Sisemore always wore a smile — around her family, at church and at her job at a retirement home, where she worked through the coronavirus pandemic.
In a Facebook post, her colleagues called her “one of our most talented and dedicated CNAs.” She worked “tirelessly and unfailingly to deliver care, compassion, and love to those more vulnerable than herself,” it said. (Her family declined to be interviewed for this article.)
Comments remarking on her kindness and work ethic poured in from patients and their families. “She went the extra mile to [make] sure I had what I needed and was comfortable,” wrote a former patient. “Tony was one of my mother’s caregivers,” wrote another Facebook user. “She was selfless … it breaks my heart that the residents will no longer have her.” Some mentioned that Sisemore cheered people up with her sense of humor. “I remembered you [danced] in front of me,” another former patient wrote.
Sisemore’s obituary says she battled COVID-19 for four weeks after passing away from complications from the virus. The nursing home where Sisemore worked reported 66 confirmed cases and 17 deaths according to county data. Over half of the infections were among staff members. The facility did not respond to requests for comment.
— Anna Jean Kaiser, The Guardian | Published June 10, 2020
(Return to top.)
A Nurse, Family Linchpin And Generous Aunt
(Courtesy of Mario Thompson)
Adlin Thompson
Age: 56
Occupations: Certified nursing assistant and endoscopy technician
Places of Work: NewYork-Presbyterian Hospital and Isabella Center for Nursing and Rehabilitation in New York City
Date of Death: April 24, 2020
Adlin Thompson had 20 siblings and more than 30 nieces and nephews. Like her, many of them immigrated to New York City from St. Kitts and Nevis in the early 1980s. With such a large family, it was difficult to keep track of everyone, said Adlin’s son, Mario Thompson. But Adlin did — she was the glue who kept the family together.
Adlin worked long hours between her two jobs. When she wasn’t at the nursing home or the hospital, she visited family, and “never came home empty-handed,” often toting gifts of socks or perfume, Mario said.
Adlin cared for patients who had been diagnosed with COVID-19 at both her jobs. She was always covered in protective gear, said Mario. Still, he worried that her asthma made her particularly vulnerable to the coronavirus. Mario believes she contracted the virus at the nursing home, where he said she had more direct contact with patients.
A spokesperson for the facility said it “followed state guidelines as it relates to infection prevention and control procedures.”
Adlin died four days after testing positive for COVID-19. She was alone in her home, preparing to go to the hospital.
— Lila Hassan | Published June 10, 2020
(Return to top.)
Housing Supervisor Committed Herself To Helping The Vulnerable
(Courtesy of Barbara Abernathy)
Michelle Abernathy
Age: 52
Occupation: Residential services supervisor
Place of Work: Elisabeth Ludeman Developmental Center in Park Forest, Illinois
Date of Death: April 13, 2020
Barbara Abernathy said she is trying to figure out what to do with six bins of toys her daughter bought for neighborhood children.
Growing up in Chatham, a middle-class neighborhood on the South Side of Chicago, Michelle Abernathy “was always trying to help somebody,” Barbara said.
Michelle spent decades investigating child abuse and neglect while holding night jobs mentoring children.
A supervisor at a state-run facility for developmentally disabled adults, she bought clothes, games and snacks for residents. A staff memo lauded her “big heart and nurturing personality.”
She fell ill March 28 and was hospitalized April 6, too weak to walk.
Three other workers at the facility died of COVID-19. A spokesperson for the American Federation of State, County and Municipal Employees, which represents workers at Ludeman, said that early in the pandemic the staff had a “huge struggle” to get personal protective equipment (PPE).
The Illinois Department of Human Services said it “can’t say precisely” how workers caught the virus and was working to provide sufficient PPE.
After long professing that she was too busy for marriage, Abernathy recently had become engaged to Torrence Jones, a colleague. She had planned to surprise her mother with the news but never had the chance.
— Mary Chris Jaklevic | Published June 5, 2020
(Return to top.)
A Loving Bookkeeper Who ‘Had The Most Awesome Laugh’
(Courtesy of Sean Diaz)
Cassondra Grant Diaz
Age: 31
Occupation: Nursing home bookkeeper
Place of Work: Chelsea Place Care Center in Hartford, Connecticut
Date of Death: April 29, 2020
Cassondra Diaz was a receptionist-turned-bookkeeper at a nursing home in her hometown.
“She was my therapist, my fashion consultant, my hair designer,” said her older sister, Takara Chenice. “I called her my ‘big little sister.’”
Loved ones described her as “an old soul,” loyal to her family, including her husband, Sean Diaz. In their free time, the couple would hit the highway for a long drive, venturing to parks, lakes and the beach.
Her family believes she contracted the coronavirus at work. A spokesperson for Chelsea Place confirmed that the nursing home had COVID cases among staff and patients. It said staffers were provided with personal protective equipment. Despite wearing protective gear, removing her work clothes at the door and showering after work, Cassondra developed symptoms in mid-April.
On April 29, she woke up having difficulty breathing and pain in her leg, said Sean, who called an ambulance. She died that day.
Sean keeps a photo of her in their car. “My six years with her were better than any lifetime I had before her,” he said.
— Madeleine Kornfeld, City University of New York | Published June 5, 2020
(Return to top.)
A Doting Family Man, He Was A Long-Standing Fixture At His Hospital
(Courtesy of Susan Ferranti and family)
David Ferranti
Age: 60
Occupation: Hospital equipment coordinator
Place of Work: St. Elizabeth‘s Medical Center in Brighton, Massachusetts
Date of Death: May 2, 2020
David Ferranti was committed to his two families — both at home and at work. In his job on the engineering unit, he was really part of every team in the hospital, wrote St. Elizabeth’s president, Harry Bane, in a note to employees. “He was always worried about ‘his nurses’ and ‘his departments’ having what they needed to best care for our patients.”
Ferranti worked at the hospital for almost 42 years “and he loved every day of it,” said his father, Savino Ferranti. St. Elizabeth’s was treating many COVID-19 patients when David became infected with the virus, his father said, but it was impossible to say where he caught it. St. Elizabeth’s had no further comment about his case.
Ferranti was a family man “and the greatest son you can imagine,” his father said. He had a wife, Susan, and a son, John.
Ferranti worked in his garden and enjoyed walks in nature. A history buff, he was born in Wiesbaden, Germany. His father, a descendant of Italian immigrants, served in the military there, where he met David’s mother, Renate.
For his family, tragedy hit twice within weeks. David’s aunt Ann Ferranti died of the disease a few weeks before David. The advice David would have given to anyone, said his father, “is to stay safe, whatever it takes.”
— Katja Ridderbusch | Published June 5, 2020
(Return to top.)
A Nurse For Whom Family Was Everything — And Patients Were Like Family
(Courtesy of the Mazzarella family)
Kelly Mazzarella
Age: 43
Occupation: Clinical nurse manager
Place of Work: Montefiore Mount Vernon Hospital in Mount Vernon, New York
Date of Death: May 8, 2020
Even as a girl, Kelly Mazzarella had her sights set on helping others. She turned this innate altruism into a 16-year career at a community-based teaching hospital.
Karen Jedlicka was blown away by the care her big sister showed every patient. “People would be going through the worst things in their lives and she was just there for them,” Jedlicka said.
Mazzarella showed that same compassion with her husband, Ronnie Mazzarella, and daughters, Hailey and Kristina. She never missed an opportunity to tell her daughters how proud they made her, Jedlicka said.
In July 2019, Mazzarella was diagnosed with lupus, an autoimmune disease that brought on painful bouts of swelling. She worked on and off through March, helping with the influx of COVID patients. She was diagnosed on April 2 and died five weeks later. Her employer did not respond to requests for comment.
Nicol Maursky, a lifelong friend, organized a GoFundMe for the family. A staggering outpouring has brought in close to $75,000.
“She just had such a love and a light that emanated from her,” Jedlicka said. It’s “very comforting to know everybody felt the same way that we did.”
— Suzannah Cavanaugh, City University of New York | Published June 5, 2020
(Return to top.)
A Proud New Orleanian And Community Caretaker
(Courtesy of Talisa Pace)
Jana Prince
Age: 43
Occupation: Case manager
Place of Work: Salvation Army in New Orleans, Louisiana
Date of Death: April 6, 2020
A “natural New Orleanian,” Jana Prince was bubbly and loving, her brother Paul Prince said.
Since high school, Jana knew she wanted to be a social worker. She grew up with cerebral palsy, wearing a leg brace and diligently practicing physical therapy so she could walk. Kids bullied her about her disability, but nothing would stop Jana from connecting with her community.
“She was trying to share her strength with other people, because she just didn’t want to see people suffer,” cousin Talisa Pace said. “She really wanted to help the black community.”
One day in mid-March, Jana had trouble breathing, Paul said. She was hospitalized for more than a week before she was intubated, and died the next day. The family said they did not know whether she was infected at work, especially given how early she became infected; the Salvation Army declined to comment.
Her mother, Barbara Prince, died of the virus three days later.
The duo lived together and got on like Laverne and Shirley. They often took care of Paul’s twin 6-year-old boys. “I don’t know how one would have survived without the other,” Paul said.
Jana and Pace had dreamed of opening a coffee shop and counseling center. “She would have been the highlight of the whole place,” Pace said.
— Theresa Gaffney, City University of New York | Published June 5, 2020
(Return to top.)
‘She Always Listened And Never Judged’
(Courtesy of Tiana Mohabir)
Tina Reeves
Age: 58
Occupation: Licensed practical nurse
Place of Work: Pickaway Correctional Institution in Orient, Ohio
Date of Death: April 27, 2020
When Tina Reeves visited her grandchildren, music would blast from the car. Wale’s “On Chill” rang out: “Trying to hear all your problems, so I can lighten the load.”
“She loved her music,” said daughter Tiana Mohabir, “even though she had no rhythm for squat.”
Reeves had an ear for the rhythm in other people’s lives, though. Younger co-workers called her “Mother Advice,” Mohabir said. In interactions with prisoners and officers alike “she always listened,” Mohabir said, “and never judged.”
She called her three daughters daily, “checking in on all of us.”
When Reeves started coughing in early April, Pickaway Correctional had already reported more than 1,500 cases of COVID-19.
“PPE [personal protective equipment] was, and continues to be, available to staff,” a prison spokesperson said. The family said their mother did not have access to adequate PPE.
By April 13, Reeves was hospitalized with COVID-19. She called her daughter to ask her to take care of paying her utility, insurance and cable bills. “I didn’t think twice,” Mohabir said, “because I didn’t want them shut off when she got home.”
Within 24 hours, Reeves was intubated. On the bedside table, her phone kept ringing.
— Eli Cahan | Published June 5, 2020
(Return to top.)
An ‘Icon,’ Hospital Secretary ‘Brightened Every Situation’
(Courtesy of Glenna Swann)
Joan Swann
Age: 70
Occupation: Intensive care unit secretary
Place of Work: Kent Hospital in Warwick, Rhode Island
Date of Death: April 29, 2020
When things were slow at the hospital, Joan Swann would head down to the gift shop.
If someone was having a hard day — the security guard, the patient transporter, the barista — she might buy them a candle. Or charm bracelet. Or a Vera Bradley handbag.
“She brightened every situation,” said Glenna Swann, her daughter. A former nurse, Joan coached trainees from behind the administrative desk. They called her an “icon” who was the reason many stayed working in the intensive care unit.
When Joan was admitted to the hospital, those she had long cared for returned the favor. Her isolation room was adorned with blue hearts, and following her intubation, the nurses would FaceTime the family in. During quiet hours, they sat at her bedside.
The hospital did not respond to requests for comment.
After Joan died, the family found “thousands upon thousands” of unused greeting cards, sorted by occasion (weddings or Christmas) and emotion (sympathy or humor).
In the coming weeks, Joan’s cherished grandson, Adam, will complete high school. Glenna is still choosing from among Joan’s graduation cards for him.
— Eli Cahan | Published June 5, 2020
(Return to top.)
In A Family Who Lost Both Mother And Son, Food Was Love
(Courtesy of Lloyd Torres)
Louis Torres
Age: 47
Occupation: Food service director
Place of Work: Queens Boulevard Extended Care Facility in Woodside, New York
Date of Death: April 8, 2020
Louis Torres went into the family business. He grew up adoring his mother’s Philippine home cooking, so it was natural to channel his passion for food into comforting others. As a food service director at a nursing home in his native Queens, he could cook and work in health care as his mother did.
Feeling terrible on March 30, Louis called his older brother, Lloyd, after work. “He was struggling to make it from the subway station,” Lloyd said.
Louis lived with his mother, Lolita, 73, a retired hospital clerk. She also had severe COVID-19 symptoms.
By the next day, mother and son had been taken by ambulance to separate hospitals. In the chaos, Lloyd said, it took an entire day of panicked calls to find their mother, who was still in the emergency room.
A few days later, Lloyd was able to pray the rosary with Lolita over the phone, and it seemed to calm her. Before they hung up, she asked that Lloyd take care of his brother. Louis made the same request about his mother before going on a ventilator.
“Their last words to me [were to] take care of each other, my God,” Lloyd said, his voice cracking.
On April 7, Lolita died. Louis died the next day.
In the weeks since then, Lloyd was comforted by a powerful dream.
“I woke up and smelled the frying of food,” he said, invoking his mother’s cooking. “That’s how she showed her love.”
— Kathleen Horan | Published June 5, 2020
(Return to top.)
Theater Brought Them Together, Then Life Imitated Art
(Courtesy of Harriet Clark Webber)
Barry Webber
Age: 67
Occupation: General surgeon
Place of Work: Mount Sinai Queens in New York City
Date of Death: April 18, 2020
Barry Webber wanted to understand how things worked. That curiosity and drive motivated him to reconstruct an old Jeep, build a computer, take up rock climbing and, of course, become a surgeon.
He pursued medicine when he realized he wasn’t going to become a concert pianist, said his wife, Harriet Clark Webber.
They met when Harriet was a dancer with the American Ballet Theatre and Barry moonlit as a supernumerary — a non-dancing extra on stage — for the company. “He just wanted to be around the theater,” she said.
Barry honed his surgery skills in a Brooklyn emergency room in the 1980s. “It was a rough time to be in an ER in Brooklyn,” Harriet said. “He was treating a lot of gunshot wounds and trauma.”
They married in 1996 and had two sons, now 22 and 20.
Like so many Americans, when COVID-19 struck, the couple watched “Contagion,” a 2011 film about a pandemic. Barry said it gave him a bad feeling.
On March 27, his fears were realized. He texted his wife: “I’m sick.”
Harriet believes he contracted the virus at work before the hospital ordered the universal use of protective gear.
— Danielle Renwick, The Guardian | Published June 5, 2020
(Return to top.)
Brooklyn Radiologist Was ‘Kind, Simple, Loving And Devoted’
David Wolin and his daughter, Helena Cawley (Courtesy of Helena Cawley)
David Wolin
Age: 74
Occupation: Radiologist
Place of Work: The Brooklyn Hospital Center in New York City
Date of Death: March 30, 2020
By 10 a.m. on Sundays, David Wolin and his wife, Susan, would have completed one-quarter of the New York Times crossword.
When the grandchildren arrived, Wolin greeted them with bagels, lox, whitefish “and the best scrambled eggs in the entire world,” said Helena Cawley, his daughter.
Wolin was “kind, simple, loving and devoted.” A radiologist specializing in mammography, he was “committed to learning everything he could,” Cawley said. “The latest medical journal was always on his nightstand.”
He and Susan would skip off to their home upstate on Wolf Lake, where they might take out a rowboat, a bottle of chardonnay and a brick of Roquefort cheese under the stars. “All they needed was each other,” Cawley said.
In late March, Wolin complained of “bad colds” but deferred testing. Brooklyn Hospital was overwhelmed with COVID-19. A hospital spokesperson could not be reached for comment.
On March 30, when Cawley couldn’t reach her father, she called the doorman of his building. He reluctantly shared the news: Wolin had died overnight.
Susan was hospitalized that day and died weeks later. “We’re grateful in a way,” Cawley said, “because we don’t know how they could have lived without each other.”
— Eli Cahan | Published June 5, 2020
(Return to top.)
‘Working There Was The Proudest Accomplishment Of His Life’
(Courtesy of Maria Joy Agtarap)
Romeo Agtarap
Age: 63
Occupation: Emergency room nurse
Place of Work: NewYork-Presbyterian/Columbia University Irving Medical Center in New York City
Date of Death: April 24, 2020
Joy and Romeo Agtarap met in Queens in the 1980s, when they were both young nurses, newly arrived from the Philippines. Joy Agtarap said her husband was a jokester who had a vibrant personality that often made him the life of the party. At gatherings, he liked to get people onto the dance floor.
“He’s a very good dancer ― sometimes he made the line dances too hard and people would get lost!” she remembered.
He was also a dedicated emergency room nurse. Agtarap had spent 20 years at what his wife said was his “dream job” at the NewYork-Presbyterian/Columbia University Irving Medical Center.
“Working there was the proudest accomplishment of his life,” she said. He was still seeing patients when the pandemic hit. (The hospital did not respond to requests to comment on whether he had adequate personal protective equipment).
Romeo was diagnosed with COVID-19 in late March. Joy, who had left nursing due to an injury, became sick a week later. They were both hospitalized ― he at NewYork-Presbyterian and she at a facility on Long Island. As Joy recovered, she anxiously awaited updates on her husband’s condition.
“It was the most devastating thing that’s ever happened to me. I was going crazy in there waiting for calls about him,” she said. He died on April 24. “I believe he took the worst of the virus for me, that’s why I’m still here,” she said.
— Anna Jean Kaiser, The Guardian | Published June 2, 2020
(Return to top.)
As Nurse And Minister, She Tended To Her Patients, Flock ― And Garden
(Courtesy of Elijah Ailende)
Felicia Ailende
Age: 67
Occupation: Registered nurse
Place of Work: Bria of Forest Edge in Chicago
Date of Death: April 20, 2020
Felicia Ailende was a beacon of unity to her family and members of Maranatha Chapel in Evergreen Park, Illinois, where she was a minister. She counseled many, helping keep marriages intact and lives on track, her son Elijah Ailende said. Though her six children were very different from one another, she saw the best in each.
An immigrant from Nigeria, she planted a garden each year and used the produce to cook West African dishes. When there were too many cucumbers, hot peppers or greens, she shared with neighbors.
At Bria of Forest Edge, a nursing home, Felicia cooked for residents at times or prayed for them, Elijah said.
Administrator Julie Kosman said in a statement that Ailende was a hardworking nurse who was pleasant and funny and had a great rapport with residents.
She is one of three workers at the facility who have died of COVID-19; two residents also died. The facility reported 132 infections.
Elijah said staffers had to reuse surgical masks provided by the facility. Administrators did not tell them when residents and other staff members got the virus “so they could take precautions and safeguard their lives,” he said.
Kosman’s statement says “full PPE” — personal protective equipment — was available to staffers and there is no reason to believe Ailende was exposed to COVID-19 “within our facility.” She “had no known contact with any resident or staff member who showed symptoms or had tested positive for COVID-19.”
— Christina Jewett, Kaiser Health News | Published June 2, 2020
(Return to top.)
He Practiced What He Preached, Caring For Inmates With Mental Illness
(Courtesy of Gwendolyn Davis)
Bishop Bruce Edward Davis
Age: 57
Occupation: Shift leader for forensic service technicians
Place of Work: Central State Hospital in Milledgeville, Georgia
Date of Death: April 11, 2020
In sermons at his Pentecostal church, Bishop Bruce Davis preached love. On weekdays, he practiced it by feeding, bathing and caring for patients at a maximum-security psychiatric hospital. Davis worked for 27 years at the state facility, said his wife, Gwendolyn Davis.
As a boy, Davis would break his pencils in half to share with his twin sister. At church, he hosted youth parades and gave away computers, bicycles and groceries. He distilled the Bible into simple lessons, she said, once winning over a parishioner with a sermon based on “The Wizard of Oz.”
When COVID-19 emerged, Davis and his co-workers at the psychiatric facility were told they couldn’t wear masks or gloves because it wasn’t part of their uniform, she said. Five days after a close co-worker tested positive for COVID-19, Davis was hospitalized, she said.
More than 70 workers at the hospital have tested positive for COVID-19, according to state data; Davis is one of two who have died. A hospital spokesperson declined to comment on Davis’ case.
After Davis’ illness, his entire household – Gwendolyn, three children and a grandchild – got sick with COVID-19, Gwendolyn said. Their adult son, who has autism, was hospitalized, Gwendolyn said. Their daughter, 22, recovered and returned to work at the same hospital.
“It is extremely hard for her to go back to work there,” Gwendolyn said.
— Melissa Bailey | Published June 2, 2020
(Return to top.)
Dedicated Dad And Technologist ‘Was As Smart As They Come’
(Courtesy of Junette Francis)
Devin Francis
Age: 44
Occupation: Radiologic technologist
Place of Work: Jackson Memorial Hospital in Miami
Date of Death: April 8, 2020
Devin Francis was due to get married June 27 to his longtime love, Micela Scott, mother of their 11-year-old daughter, Dekayla.
Scott said her fiancé was a devoted father.
“He’d take [Dekayla] to school every morning. He’d help her with her homework,” she said. “He just wanted peace to his life and us to have a good life.”
“He had a very jovial spirit,” said his youngest sister, Junette Francis.
Devin took a COVID test at Jackson Memorial after his shift on April 6 — it came back positive. His breathing became labored and he died at home early on April 8.
His family and a hospital representative said it was unclear whether he came into contact with patients with COVID-19. Devin also worked in fleet services for American Airlines.
Colleagues admired his work ethic.
“No matter where we were in life, he never had less than two jobs,” said Milton Gonzalez, a hospital co-worker. “He was as smart as they come.”
— Sharon Jayson | Published June 2, 2020
(Return to top.)
A Pediatric Neurosurgeon Who Separated Conjoined Twins
(Courtesy of Judy Goodrich)
James Goodrich
Age: 73
Occupation: Pediatric neurosurgeon
Place of Work: Montefiore Medical Center in the Bronx, New York City
Date of Death: March 30, 2020
James Goodrich was a renowned pediatric neurosurgeon, best known for separating conjoined twins ― a rare and risky procedure. Over the course of his career, he was directly involved in about 10 cases, advising on dozens more.
A late bloomer academically, Goodrich began his undergraduate studies at age 24, after returning from Vietnam, where he served in the Marines.
“He had seen a neurosurgeon when he was in Vietnam, and he just was fascinated at what they were able to do,” said Judy Goodrich, his wife of 50 years. “I thought, just try to become a doctor first.”
He was also known for innovations regarding conditions affecting the skull. He helped develop standards for treating craniosynostosis, in which the bones of a child’s skull fuse too soon, preventing the brain from growing properly.
Goodrich was an avid collector ― of antique medical books, pre-Columbian medical artifacts, rare watches and fine wines, among other things. He surfed, cultivated bonsai trees and played the didgeridoo.
He had seen patients in the clinic in early March, just before flying to Mexico for a family vacation. He soon began to feel ill, and when he returned to New York, he was diagnosed with COVID-19. He was hospitalized on March 25 and died five days later.
Read more here.
— Danielle Renwick, The Guardian | Published June 2, 2020
(Return to top.)
She Brought ‘Calming Presence’ And Fun To Nursing Home
(Courtesy of Howard Fox Jr.)
Leola Grady
Age: 59
Occupation: Recreational aide
Place of Work: Bria of Forest Edge in Chicago
Date of Death: April 10, 2020
Leola Grady had planned to be with her son and granddaughter in Mississippi for Mother’s Day but did not live to make the trip.
At the Bria of Forest Edge nursing home, she entertained residents, including with a “good game of cards,” administrator Julie Kosman said. “She had a calming presence about her.”
When Grady fell ill, a nurse at the facility was already sick with the coronavirus. A nursing aide whose name has not been released also died of COVID-19. Staff at the facility, with SEIU union leaders, spoke out saying they were unaware their co-workers were dying until they saw it on the news.
Howard Fox Jr., Grady’s son, said his mother was his best friend. An honest, straightforward and loving person, she enjoyed listening to the blues. “I’m not going to sit here and sugarcoat it,” he said. “It hurts. … I look at our picture. I cry.”
Fox said his mother went to a Chicago hospital with COVID symptoms but was sent home. She was found dead several days later. A Cook County spokesperson confirmed she died of pneumonia due to COVID-19.
Kosman said the facility does not believe Grady or the nurse, Felicia Ailende, “were exposed to COVID-19 within our facility. They had no known contact with any resident or staff member who showed symptoms or had tested positive for COVID-19.”
As of May 27, Bria of Forest Edge has reported 132 coronavirus cases and two deaths to Illinois officials. In the statement, Kosman said it reported worker deaths to the Occupational Safety and Health Administration, which shows three pending death investigations at the facility.
— Christina Jewett, Kaiser Health News | Published June 2, 2020
(Return to top.)
Young Nurse Lived A Life Of ‘No Regrets’
(Courtesy of the Guzman family)
Krist Angielen Castro Guzman
Age: 35
Occupation: Licensed practical nurse
Place of Work: Meadowbrook Manor in Bolingbrook, Illinois
Date of Death: May 2, 2020
Krist Guzman packed a lot into her short life. She worked full time while studying to become a registered nurse. She had three children, one a newborn.
Smart, funny and outgoing, she nurtured relationships.
“Hers was a life of no regrets,” said a cousin, Jeschelyn Pilar.
In a Navy family that moved often, she was close with her brother, Anjo Castro.
“She was my role model,” said Castro, who also pursued a medical career as an independent duty corpsman in the Navy.
The pandemic hit home when their uncle, pediatric surgeon Dr. Leandro Resurreccion III, died March 31.
Guzman told family she had seen COVID patients. Worried she didn’t have adequate protective gear, she scrambled to find some online.
Meadowbrook has registered the worst COVID outbreak in Illinois, with more than three dozen deaths. Nursing home spokesperson Marissa Kaplan said in a statement: “Meadowbrook puts the safety and welfare of its residents and staff at the forefront of everything we do.” She did not address whether there was sufficient protective gear.
— Mary Chris Jaklevic | Published June 2, 2020
(Return to top.)
Selfless Nephrologist Fought For Her Life While Treating Others
(Courtesy of the Khanna family)
Priya Khanna
Age: 43
Occupation: Nephrologist
Place of Work: Khanna Nephrology in Glen Ridge, New Jersey
Date of Death: April 13, 2020
Priya Khanna came from a family of doctors, and she knew the risks of contracting the deadly coronavirus. She was immunocompromised and actively seeing patients days before she became ill with COVID-19.
On April 1, Priya was hospitalized in the same facility where her father, Satyender Dev Khanna, had been brought days earlier. He was also being treated for COVID-19.
From her hospital bed, Priya checked in on friends, reviewed patient files and communicated with the physician who was seeing patients in her stead. She continued to do so until she was put on the ventilator.
“She literally worked for others until she could no longer breathe for herself. That was Priya,” said childhood friend Justin Vandergaag. “Always putting others first with a smile.”
“She was a devoted daughter, sister and aunt,” said childhood friend Laura Stanfill. “Her healing gifts extended not only to her patients but, in the many ways, she made everyone in her life feel important and loved.”
Read more here.
— Natalia Megas | Published June 2, 2020
(Return to top.)
‘He’s One Of Our Legends’
(Courtesy Stephanie Mahoney)
James ‘Charlie’ Mahoney
Age: 62
Occupation: Pulmonologist
Place of Work: SUNY Downstate Medical Center in Brooklyn, New York City
Date of Death: April 27, 2020
James “Charlie” Mahoney eschewed hospital hierarchies.
“He didn’t treat people like underlings,” said his sister, Saundra Chisholm. “He would talk to housekeeping like he would talk to the chief of the hospital. That’s why he was so well respected.”
Growing up on Long Island, Mahoney was an ace student and athlete. He was one of only a handful of black students at his medical school and throughout his training. He and his brother, Melvin Mahoney, worked side by side at SUNY Downstate for many years, a public hospital that treats a mostly minority and low-income patient population.
When the pandemic hit New York in March, Mahoney, who specialized in respiratory care, “ran into the fire,” Melvin said. But his hospital, like other underfunded public institutions in the city, was short of protective equipment and staff.
Mahoney started experiencing symptoms in early April, and was hospitalized soon after. He died on April 27.
“He’s one of our legends ― he’s one of our giants,” said Julien Cavanaugh, a neurology fellow at SUNY Downstate who trained under Mahoney.
Read more here.
— Ankita Rao, The Guardian | Published June 2, 2020
(Return to top.)
Psychiatric Nurse Knew Her Patients’ Hometowns And Hobbies
(Courtesy of Eddie Ballard)
Shenetta White-Ballard
Age: 44
Occupation: Licensed practical nurse
Place of Work: Legacy Nursing and Rehabilitation of Port Allen, Louisiana
Date of Death: May 1, 2020
Eddie Ballard was baking “Pecan Delight” pie at the Piccadilly Cafeteria in Baton Rouge, Louisiana, when Shenetta White, accompanying her auntie and grandmother, leaned over the buffet counter to grab a Jell-O.
“She gave me this look,” Ballard said, and he gathered the confidence to ask for her number. On their first date he quickly realized “not only was she beautiful, but she was mature beyond her years.”
That maturity manifested across her life.
As a nurse to psychiatric patients, she was adored by those she “saw as people more than just patients,” Ballard said. She knew their parents’ names, their hometowns and hobbies. At home, White-Ballard was “queen of the house,” Ballard said. She handled the errands and the finances, while “her two boys [Ballard and his son, Warren] hung on whatever she asked.”
With a preexisting condition, White-Ballard depended on supplemental oxygen. She died May 1, just three days after developing COVID-19 symptoms.
In an email, a Legacy spokesperson wrote that the facility had followed all guidelines and “had more than enough PPE.”
The first piece of jewelry Ballard bought his wife was a bracelet that read: “Love is patient, love is kind, love never ends.”
“I hadn’t read that in 11 years,” he said, “but boy, it’s still true.”
— Eli Cahan | Published June 2, 2020
(Return to top.)
From His ICU Bed, Nurse Planned To Help Fight COVID After Recovery
Christopher Dean with his wife, Natalya Kubaevskaya (Courtesy of Donna Dean)
Christopher Dean
Age: 37
Occupation: Licensed practical nurse
Place of Work: Northport VA Medical Center’s Valley Stream Clinic in Valley Stream, New York
Date of Death: April 15, 2020
When Christopher Dean went to the emergency room, he was “absolutely positive” he would be in the hospital a few days, get some fluids and oxygen and then go home.
“He was always optimistic, full of life,” said Natalya Kubaevskaya, his wife of 10 years. “And he had a big heart.”
When tests came back positive for COVID-19, he planned to recover and then help fight the disease by donating blood and plasma. Three weeks later, he was dead.
He had mild asthma, his wife said, but was a healthy man who loved snowboarding, swimming and racquetball.
His father, Alvin Dean, shared on a GoFundMe page that Christopher Dean caught the coronavirus at work. Northport said by email that it provided “PPE in accordance with CDC guidelines.”
Kubaevskaya, who recently finished treatment for breast cancer, said Dean pushed her to keep going.
Daughter Donna, 15, struggles with her adoptive father’s death. “There are moments,” Kubaevskaya said, “when she tries to convince herself that he’s still in the hospital and will come home soon.”
— Katja Ridderbusch | Published May 29, 2020
(Return to top.)
A Robotic Surgery Expert Who ‘Just Made Everything Fun’
(Courtesy of the Lopez family)
Maria Lopez
Age: 63
Occupation: Registered nurse
Place of Work: University of Illinois Hospital in Chicago
Date of Death: May 4, 2020
“What lady? I don’t see a lady here.”
That was the sort of self-deprecating comment Maria Lopez would fire back when teased by a co-worker about an etiquette faux pas in the operating room.
Lopez knew how to break the tension, said chief nurse anesthetist Mary Ann Zervakis Brent, a colleague since 2005. Lopez called everyone “amigo” or “amiga,” regardless of rank.
“She just made everything fun,” Zervakis Brent said.
Lopez was an expert in robotic surgery and trained others to use the equipment.
She taught her two daughters to be independent. The oldest of nine kids, Lopez fought her father’s expectation that she forgo college, said her daughter Maria, who was named for her.
Lopez’s symptoms appeared days after she returned to work from leave for knee surgery. She planned to retire April 30.
In the hospital, Lopez tried to stay positive. Yet during one FaceTime call, daughter Maria said, “she just broke down. She said, ‘I wouldn’t want anyone I love going through what I’m going through right now.’”
A hospital official confirmed in a statement that Lopez died of complications of COVID-19.
— Mary Chris Jaklevic | Published May 29, 2020
(Return to top.)
With Retirement In Sight, She Died Awaiting COVID Test Results
(Courtesy of Hannilette Huelgas)
Hazel Mijares
Age: 66
Occupation: Licensed practical nurse
Place of Work: Amsterdam Nursing Home in New York City
Date of Death: March 30, 2020
Faith was central to Hazel Mijares’ life. She was a lay leader at Trinity United Methodist Church in Jersey City, New Jersey.
She was drawn to church as a child in the Philippines, sister Hannilette Huelgas said. Theirs was a big family with nine children. At get-togethers, Mijares always led the prayers.
After a long career, Mijares was finally ready to retire in late March.
She worked through March 13, burned up accrued paid time off, then stopped back a week later for her last day. As she said her goodbyes, she noticed a little cough.
Learning that one of her patients had died of COVID-19, Mijares tried several times to get tested. Her results were expected March 30. When Huelgas called that day, Mijares didn’t answer. She had died waiting for the results, which the family learned were positive.
As of May 24, the nursing home had recorded 45 presumed-COVID deaths. Officials there did not respond to requests for comment, but a phone recording updated May 21 said they had “completed COVID-19 testing of residents” and had “begun testing of all staff.”
“Our dedicated and caring staff are continuing the Amsterdam tradition of providing exceptional care,” the recording noted.
Mijares “had wanted to go to Jerusalem, to the Philippines,” Huelgas said. “And she didn’t even get to enjoy retirement.”
— Maureen O’Hagan | Published May 29, 2020
(Return to top.)
You Could Count On Him ‘For Anything’
(Courtesy of Griselda Bubb-Johnson)
Adiel Montgomery
Age: 39
Occupation: Security guard
Place of Work: Kingsbrook Jewish Medical Center in Brooklyn, New York
Date of Death: April 5, 2020
When Griselda Bubb-Johnson couldn’t reach her friend Marva — hospitalized with COVID-19 — Bubb-Johnson called her son, Adiel Montgomery.
Montgomery, a security guard in the hospital’s emergency department, found Marva in the ICU. He then did “everything for her,” Bubb-Johnson said. When Marva was cold, he got a blanket. When she was hungry, he got food. When her phone died, he found a charger.
“Some people boast about their children, but I didn’t have to,” Bubb-Johnson said, “because everybody knew you could count on Adiel for anything.”
Montgomery doted on residents as a part-time supervisor at the Urban Resource Institute, a domestic violence shelter. He invited his godbrothers for Golden State Warriors games, Thanksgiving and sometimes for his mom’s renowned oxtail dish.
Two weeks after Montgomery noted he couldn’t taste his lunch, he experienced acute chest pain. When, after 12 hours in the ER, his heart stopped “nobody could believe it,” Bubb-Johnson said.
Montgomery was vocal about a lack of personal protective equipment for hospital security guards, according to a New York Times report. The hospital did not respond to requests for comment.
Montgomery’s 14-year-old daughter, Aaliyah, never got to say goodbye. She wrote a poem to put in the coffin.
“Don’t worry,” Bubb-Johnson told her. “He’ll read it. I promise.”
— Eli Cahan | Published May 29, 2020
(Return to top.)
Traveling Nurse ‘Wanted To Be Somebody’
(Courtesy of Daniel Perea)
David Joel Perea
Age: 35
Occupation: Traveling registered nurse
Place of Work: Lakeside Health & Wellness Suites in Reno, Nevada, via MAS Medical Staffing
Date of Death: April 19, 2020
David Joel Perea would call in from Maine, Vermont, Minnesota and, ultimately, Nevada, with the same request: “Mom, can you send tamales?” Dominga Perea would ship them overnight. This is how she always knew where her son was.
A traveling nurse routinely pulling 80-hour weeks, David “had a tremendous work ethic,” said his brother, Daniel. A young David, returning from his father’s mechanic shop, said, “I don’t want to spend life sweating under a car,” Dominga recalled. “I want to be somebody.”
Dominga was proud of him, “for doing God’s work.”
When “mijito” didn’t respond to her text April 6, Dominga knew something was wrong: “I could always tell how David was. If he said ‘Hi, Mama,’ he was happy. If he said ‘I’m fine, Mom,’ he was tired.”
This time he said neither. “Don’t panic, Mama,” David wrote, “just pray for me. I have the COVID.”
His workplace did not respond to requests for comment.
David FaceTimed with his mother on Easter Sunday. “He was starving, but he struggled even eating mashed potatoes,” Dominga said, “because he couldn’t breathe.” The next morning, he was on a ventilator and never woke up.
— Eli Cahan | Published May 29, 2020
(Return to top.)
His Church Became His Second Home
(Courtesy of Lean Carlo Romualdo)
Ritchie Villena
Age: 44
Occupation: Physical therapist
Place of Work: SportsMed Physical Therapy clinic in Glen Rock, New Jersey, placed by AHVIA Staffing Solutions in Jersey City
Date of Death: April 15, 2020
When Ritchie Villena emigrated from the Philippines in 2011 after studying physical therapy, he struggled. Then he got in touch with Lean Carlo Romualdo, a fellow Filipino physical therapist in New York state. Villena moved in with him and secured a good job at a sports medicine clinic.
He became devoted to his church, Iglesia Ni Cristo, where he spent hours singing with the choir and practicing the organ. “He’s not an outgoing person,” Romualdo said. “But if you ask people in his religious group here in Rockland County, everyone will know him.”
Romualdo’s 7-year-old still plays the “Baby Shark” song Villena taught him on the piano, asking, “Is Uncle Ritchie coming back home?”
It’s unclear how Villena contracted the coronavirus. According to the staffing agency, he worked until March 13 and took ill the following week. On March 26, he called 911 with difficulty breathing; he was hospitalized until his death.
Villena, who only recently gained permanent residency status, hadn’t seen his family in nine years. “Every time his mom calls me, she wants to see Ritchie’s stuff,” Romualdo said. As he gives a video tour of Villena’s room, she can’t stop crying. He promised to pack everything and send it home.
— Maureen O’Hagan | Published May 29, 2020
(Return to top.)
Nurse With ‘Heartwarming’ Smile Did Her Best For Her Children
(Courtesy of Anderson Family)
Jenniffer Anderson-Davis
Age: 44
Occupation: Licensed practical nurse
Place of Work: Meramec Bluffs Life Plan Community in Ballwin, Missouri
Date of Death: April 14, 2020
As a single mother, Jenniffer Anderson-Davis was determined to give her three children everything they needed, so she pursued her nursing degree while delivering pizza to make ends meet.
“She always did the best that she could to give them the best life,” her brother Earl Anderson said.
Most recently, Anderson-Davis worked as an admission and discharge nurse at a senior living community. Her mother, Edna Anderson, said that Anderson-Davis was concerned about residents who returned to the facility after visiting Florida (it has since banned reentry for residents who spent time away).
Anderson-Davis tested positive for COVID-19 on April 9 and died at home five days later. The Occupational Safety and Health Administration opened a fatality investigation at Meramec Bluffs on April 16.
Lutheran Senior Services, the nonprofit that operates Meramec Bluffs, acknowledged Anderson-Davis’ death but did not respond to specific questions about her case. In a statement, a spokesperson said: “Jenniffer’s coworkers remember her as a thorough and well-respected nurse who had a smile that could warm any heart.”
— Cara Anthony, Kaiser Health News | Published May 26, 2020
(Return to top.)
A Tireless Nurse, She Loved Her Children And Travel
(Courtesy Stefaney Cicala)
Susan Cicala
Age: 60
Occupation: Registered nurse
Places of Work: Northern State Prison in Newark, New Jersey; Clara Maass Medical Center in Belleville, New Jersey
Date of Death: April 4, 2020
Susan Cicala worked long hours. A typical workday began at the hospital surgery department at 5:30 a.m. She’d work there until 2 p.m., and an hour later would start her next eight-hour shift at a nearby state prison. She worked weekends, too.
As for sleep? “She must have slept somewhere, but I don’t know,” her son, Steven Cicala, said with a laugh. “She was the hardest worker I ever met.”
Reminiscing on Facebook, colleagues said she talked about her two children constantly. She started wrapping Christmas presents in May. She loved to travel, to Disney World and national parks, and saw vacations as opportunities to learn about the world beyond New Jersey — on a trip to Hawaii, she delved into the attack on Pearl Harbor.
Cicala became sick in late March and died in early April; her family said they presume she contracted the virus at one of her jobs.
“She didn’t go anywhere else,” Steven said.
As of May 21, the New Jersey Department of Corrections had tallied 152 COVID-19 cases at the prison where Cicala worked; 134 of those diagnoses were among staffers. In early May, the union representing Cicala and other workers filed a safety complaint saying precautions have been inadequate and may have led to Cicala’s death. A spokesperson for the prison health care agency that employed Cicala said that it had followed all state and federal guidelines, and that the staff was provided with personal protective equipment.
— Maureen O’Hagan | Published May 26, 2020
(Return to top.)
The Single Mother Dreamed Of Opening A Nursing Home
(Courtesy of Rebecca Gbodi)
Helen Gbodi
Age: 54
Occupation: Registered nurse
Place of Work: MedStar Washington Hospital Center in Washington, D.C.
Date of Death: April 19, 2020
Helen Gbodi was known for helping elderly neighbors and fellow churchgoers — picking up their medications and groceries and accompanying them on walks. She even dispatched her daughter, Rebecca Gbodi, to shovel snow in neighbors’ driveways.
“Even when she didn’t have a lot, she would always give,” Rebecca said of her mother, who worked long hours to put her children through college and helped pay school fees for other relatives. This year, she embarked on her own dream: crafting plans to open her own nursing home, her daughter said.
Gbodi understood the severity of COVID-19 early on. In March, she called every person in her contacts list, including people she hadn’t talked to in years, to make sure they were aware and taking precautions, her daughter said. Though she did not actively care for patients who had been diagnosed with COVID-19, such patients were being treated on her floor, her daughter said.
Days later, she was fighting for her life. By the time she was hospitalized with COVID-19, she was too weak to lift her arm for a virtual handshake with her daughter on FaceTime.
“At the end of the day, she was willing to put her life in danger for others,” Rebecca said.
— Anna Jean Kaiser, The Guardian | Published May 26, 2020
(Return to top.)
Always Upbeat, Patient Transporter Was A Sewing Wiz
(Courtesy of the Ismayl family)
Gabrail ‘Gabe’ Ismayl
Age: 62
Occupation: Patient transport worker
Place of Work: Swedish Hospital in Chicago
Date of Death: May 6, 2020
Caring, upbeat, always first to arrive at a party. Gabrail Ismayl loved an excuse to don a suit and splash on cologne.
That’s how Fidelline Youhanna remembers her uncle. “Everybody loved Gaby,” she said.
After migrating from Syria in the 1980s, Ismayl ran wholesale clothing shops on Chicago’s North Side. He was a wiz with the sewing machine and enjoyed altering dresses, making curtains and doing creative projects for family and friends.
Later, his people skills were an asset as he wheeled patients where they needed to go.
As the pandemic took hold, Ismayl worked despite health conditions that elevated his risk, Youhanna said.
“I think he just liked his job,” she said. “He made a lot of friends there.”
On May 6, Ismayl was self-isolating in the basement of the house he shared with two sisters. He was short of breath, Youhanna said. By evening, he was dead.
Ismayl was employed by management services company Sodexo. The CEO of its health care division in North America, Catherine Tabaka, said in a statement that his passing “is a tragic loss for Sodexo and we mourn an incredible friend and presence.”
— Mary Chris Jaklevic | Published May 26, 2020
(Return to top.)
Charismatic Surgical Technician Taught His Kids To Be ‘Faithful To Your Job’
(Courtesy of the Martinez family)
Juan Martinez
Age: 60
Occupation: Surgical technician
Place of Work: University of Illinois Hospital in Chicago
Date of Death: April 27, 2020
It was easy to befriend Juan Martinez.
The surgical technician “could start a conversation up with anyone about anything,” said Jose Moreno, an operating room nurse and co-worker.
He went out of his way to teach others what he learned from 34 years in the field, said his son, Juan Martinez Jr., who followed his dad’s career path at the same hospital.
The military veteran and former church pastor set an example “to be faithful to your job,” his son said.
Due to retire April 30, Martinez anticipated spending time with his grandchildren, traveling and opening Bible education centers in Mexico, his family said.
After feeling tired and feverish, he went to be tested for COVID-19 on April 17. His symptoms were so severe that he was taken by ambulance to the hospital where he worked.
Family members said Martinez did not engage in direct patient care but came in contact with staffers who did.
Juan Jr. said that losing his dad has been like a nightmare, and that he and his siblings are “leaning on the Lord and praying a lot, just like how our father taught us.”
— Mary Chris Jaklevic | Published May 26, 2020
(Return to top.)
Memory Care Nurse Set Fear Aside
(Courtesy of Jessica Forbes)
Nina Forbes
Age: 56
Occupation: Licensed practical nurse
Place of Work: Silverado memory care facility in Alexandria, Virginia
Date of Death: April 25, 2020
Nina Forbes refused to let fear stop her from living.
She was terrified of flying. But a few years ago, Forbes got on a plane for the first time to watch her younger daughter Jennifer play volleyball.
COVID-19 also scared Forbes, and as a nurse at an assisted living facility, she knew the virus posed a serious risk. Still, she continued showing up to work.
Forbes tested COVID-positive just after Easter. Chills, body aches and a fever kept her from attending family dinner that Sunday. By the following weekend, she struggled to breathe and couldn’t walk on her own. An ambulance took her to the hospital.
Her older daughter, Jessica, said her mother didn’t have the necessary protection at work. Forbes sometimes wore trash bags to protect herself, she said.
In a statement, a representative for the facility said it met the Centers for Disease Control and Prevention guidelines for personal protective equipment. Employees sometimes used trash bags as an added layer of protection, worn over a disposable gown, according to the representative.
Forbes appeared to do what she wanted even in her final moments. Jennifer was able to visit her mother in the hospital, and Forbes died shortly after she left, Jessica said. “It was like she waited for her to leave.”
— Carmen Heredia Rodriguez, Kaiser Health News | Published May 19, 2020
(Return to top.)
A Family Man Who Loved Disney, Took Risks To Help Others
(Courtesy of AMR Southwest Mississippi)
David Martin
Age: 52
Occupation: Paramedic
Place of Work: AMR Southwest Mississippi, covering Amite and Wilkinson counties
Date of Death: April 22, 2020
On March 22, David Martin changed his Facebook profile picture. Around his smiling face, the frame read, “I can’t stay home … I’m a healthcare worker.”
Outside of work, he was a dedicated family man with two children, known for his love of Disney.
Martin, who covered 1,420 square miles across two rural counties, had cared for people with suspected COVID-19 in the weeks leading up to his death, said Tim Houghton, chief of operations for AMR Southwest Mississippi.
“We do what we do knowing the risks,” Houghton said. But Martin’s death was “a hard hit.”
On March 23, at the end of a shift, Martin told a supervisor he had mild flu symptoms. A month later, he died at a hospital in Baton Rouge, Louisiana.
AMR paramedics had N95 masks and protective gear and followed Centers for Disease Control and Prevention guidelines, Houghton said. “We have not yet had a shortage.”
In Facebook posts honoring Martin, colleagues described his excitement before trips to Disney World. In his memory, his fiancee, Jeanne Boudreaux, shared a photo of a hot air balloon ride at Disney Springs.
— Michaela Gibson Morris | Published May 19, 2020
(Return to top.)
For a 9/11 First Responder, ‘Sitting on the Sidelines Was Never in His DNA’
(Courtesy of Erin Esposito)
Matthew ‘Matty’ Moore
Age: 52
Occupation: Radiologic technologist
Place of Work: Northwell Health’s GoHealth Urgent Care in Eltingville, Staten Island, New York City
Date of Death: April 17, 2020
Matthew Moore “would give the shirt off his back to help others,” said his sister, Erin Esposito.
A former firefighter and Staten Island native, “Matty” Moore volunteered as a first responder for weeks after 9/11, “even when everyone else stopped going,” Esposito said.
Moore was known as “a gentle giant” in Prince’s Bay, his brother-in-law Adam Esposito said. He was a devoted churchgoer and a beloved member of “The Beach Boys Firehouse” (as Engine 161/81 was nicknamed).
He even came through as Santa Claus, delivering gifts on Christmas morning to the children of two firefighters who died on 9/11.
Moore became an X-ray technologist, cherishing the ability to help those seeking urgent care. When COVID-19 emerged, he continued showing up to work. “Sitting on the sidelines was never in his DNA,” Erin Esposito said.
At the time, the family was reassured that he was receiving the personal protective equipment he needed. Despite his precautions, when Matty contracted COVID-19, it tore through his lungs, which had been damaged at ground zero.
As Matty lay dying, Esposito sought to reassure her brother. “You’ve done enough for us,” she told him, over the phone. Moments later, Matty’s heart stopped beating.
— Eli Cahan | Published May 19, 2020
(Return to top.)
‘Gentle Soul’ Had A Brilliant Mind And A Big Heart
Neftali “Neff” Rios
Age: 37
Occupation: Registered nurse
Place of Work: St. Francis Hospital’s intensive care unit in Memphis, Tennessee
Date of Death: April 26, 2020
Hospital colleagues loved working with Neftali “Neff” Rios. He was humble, kind and capable, a “gentle soul” who always strived to learn something new. Not just smart — “I’m talking extremely intelligent,” his brother Josue Rios said. And he simply loved people. Nursing was a perfect fit.
Neff worked at a small hospital in Clarksdale, Mississippi, then earned his master’s in business administration with an emphasis on health care, and moved to St. Francis, hoping to enter management.
In mid-April, he came down with fever, body aches and a terrible cough and tested positive for the coronavirus. Several family members got sick, too. His parents were hospitalized.
On April 26, Neff collapsed at home, unable to catch his breath. His wife, Kristina, called 911, started CPR and waited for the EMTs. When they arrived, he had already died.
The family believes he was exposed at work. A spokesperson for the hospital declined to comment, citing family privacy.
“Neff was never scared” of catching the virus at work, Rios said. “You take an oath to take care of people, no matter what.”
— Maureen O’Hagan | Published May 19, 2020
(Return to top.)
His Warmth And Generosity Brought Diverse Clients To His Pharmacy
(Courtesy of the Titi family)
Saif Titi
Age: 72
Occupation: Pharmacist
Place of Work: Noble Pharmacy in Jersey City, New Jersey
Date of Death: April 7, 2020
When the pandemic hit, Saif Titi was working six days a week at his Jersey City pharmacy and had no interest in slowing down. As was his way, he wanted to be helpful.
“He didn’t really run it as a business,” said Titi’s son, Justin. “He wasn’t trying to make profit. He was really just trying to help people.”
Titi was born in Jaffa in the last days of British rule in Palestine and grew up a refugee in the Gaza Strip. After studying in Egypt, Austria and Spain, he immigrated to New Jersey in 1972 and bought Noble Pharmacy a decade later.
The pharmacy became a fixture in the community, known as a place immigrants could go for help and advice, often in their native language. If they couldn’t afford medication, Titi would give it to them for free. “All different types of people from different cultures would come and they would instantly fall in love with him,” Justin said.
Active in the local Arab American community, Titi gave to charity and sent money home regularly. A Facebook tribute included dozens of stories of his generosity and mentorship. “We all lost the sweetest and the most noble man on earth,” wrote one relative.
Titi, a father of three adult children, developed symptoms of COVID-19 in late March. He died in the hospital on April 7. His wife, Rachelle, also became infected and has taken some six weeks to recover. In quarantine, the family has been unable to grieve together.
— Noa Yachot, The Guardian | Published May 19, 2020
(Return to top.)
Social Worker Was A ‘Big Voice’ In His Community
(Courtesy of Donna Welch)
Gerald Welch
Age: 56
Occupation: Social worker and behavioral specialist
Place of Work: Opportunity Behavioral Health in Reading, Pennsylvania
Date of Death: April 15, 2020
Donna Welch had sworn she would “never, ever, ever get married again.” Then Gerald appeared.
They met on MySpace, and she quickly realized that “our spirits connected.” On their first date, at Donna’s house in Harrisburg, Pennsylvania, Gerald proposed — and Donna said yes. “It was like he came down on a bolt of lightning from heaven,” she said.
Gerald’s fiery passion and courage to speak out served him as a boardroom advocate for underperforming students in the school district, and at the St. Paul Missionary Baptist Church, where he resurrected a scholarship now named in his honor.
“He had a big voice,” Donna said, “and he was not afraid to use it.” His “Families, Organizations and Communities United in Service” podcast combined Gerald’s lived experience overcoming drugs and his spirituality to support others struggling with addiction.
So even as the state’s COVID cases mounted, Gerald was a dutiful companion for his clients with severe autism — he took them to the supermarket in Lancaster and the laundromat in Lebanon. “Wherever they needed to go, he went,” Donna said. “He cared so much for them, and they loved him dearly.”
“We all did,” she added.
— Eli Cahan | Published May 19, 2020
(Return to top.)
Hardworking Immigrant Realized His Dream To Practice Medicine In US
Jesus Manuel Zambrano and his son, Jesus Manuel Jr.
(Courtesy of the Zambrano family)
Jesus Manuel Zambrano
Age: 54
Occupation: Pediatrician
Place of Work: Private practice in Freeport, New York; attending physician at Mount Sinai South Nassau hospital
Date of Death: March 30, 2020
Jesus Manuel Zambrano studied medicine in the Dominican Republic and immigrated to New York in the 1990s.
He hustled, working in fast food and as a school bus driver between studies, his wife, Sandra, said. He completed his residency in 2010.
In the meantime, they had two children: Jesus Manuel Jr., 22, and Angelyne Ofelia, 18. Jesus Manuel Jr., who uses a wheelchair, never veered far from his father during family outings to restaurants and parks, and Holy Week vacations.
Zambrano’s bond with his son informed his care for his patients. “There was not a single day we met and talked when we didn’t talk about his son,” said Dr. Magda Mendez, a former colleague.
Zambrano spent days in private practice, Sandra said, and in the evenings treated others at the hospital, which saw COVID cases.
In early March, he felt ill. He took the next day off — a rare occurrence, Sandra said. He was taken to the hospital where he worked, where he died after a week and a half of care.
In becoming a physician in the United States, Zambrano had realized his lifelong dream. He wished the same for his family.
“He had a lot of plans for his children, a lot of dreams,” Sandra said. “He took them with him.”
— Carmen Heredia Rodriguez, Kaiser Health News | Published May 15, 2020
(Return to top.)
Quick-Witted And Quick To Serve, Firefighter ‘Always Had Your Back’
(Courtesy of the Zerman family)
Robert Zerman
Age: 49
Occupation: Volunteer firefighter
Place of Work: Pioneer Hose Company No. 1 in Robesonia, Pennsylvania
Date of Death: April 16, 2020
Anyone who met Robert Zerman would see two things: He was devoted to firefighting and emergency medical services, and he had a quick sense of humor.
“He probably went on tens of thousands of calls,” said Anthony Tucci, CEO of the Western Berks Ambulance Association. Tucci, who knew Zerman for over three decades, added, “he always had your back, always knew his stuff.”
Most recently, Zerman was a volunteer assistant fire chief. He responded to an emergency in March in which the patient had COVID-19 symptoms.
“That was before there was really any guidance to wear PPE,” Tucci said.
Soon Zerman got sick, leading the family to suspect that he’d contracted the coronavirus on that call, Tucci said. Zerman tested positive and was hospitalized. He seemed to be improving before taking a bad turn.
Berks County, in eastern Pennsylvania, is among the state’s hardest hit, recording around 3,500 total cases and nearly 200 deaths by mid-May.
Representatives from two dozen first responder agencies lined the streets for Zerman’s funeral procession.
— Maureen O’Hagan | Published May 19, 2020
(Return to top.)
Lighthearted Nurse ‘Lit Up the Room’
(Courtesy of Alisa Bowens)
Linda Bonaventura
Age: 45
Occupation: Licensed practical nurse
Place of Work: Wildwood Healthcare Center in Indianapolis
Date of Death: April 13, 2020
Even on bad days, Linda Bonaventura’s lighthearted sense of humor made people feel better, her sister Alisa Bowens said.
Bonaventura dedicated her career to children with special needs and seniors. She did her best to keep her spirits up while working 16-hour days.
“We like to say she was laughter,” Bowens said. “She lit up the room.”
In a statement, Ethan Peak, executive director of Wildwood, called Bonaventura a dedicated nurse who “would do anything for her residents and co-workers.”
As the list of patients and employees with COVID-19 grew longer at Wildwood, Bonaventura refused to live in fear, Bowens said.
Bowens recalled the day her sister confessed she was spraying herself with Lysol to kill the germs on her clothes. She did the same for a co-worker. A Wildwood spokesperson said the nursing home had sufficient personal protective equipment for employees.
The sisters, in one of their last conversations, told each other they would be at peace if death came during the pandemic. A short time later, Bonaventura tested positive for COVID-19. Just a week after coming down with a sore throat and fever, she died.
“She believed in fate,” Bowens said. “We shared that belief. But it was still a shock.”
— Cara Anthony | Published May 15, 2020
(Return to top.)
Nurse’s Death Ripples Through The Heart Of An Extended Community
(Courtesy of Courtney Christian)
Sheila Faye Christian
Age: 66
Occupation: Registered nurse
Place of Work: Care Pavilion Nursing and Rehabilitation Center in Philadelphia
Date of Death: April 19, 2020
So many people are mourning the death of Sheila Christian, her daughter set up a website to comfort them all.
Christian was a longtime friend of Tina Knowles-Lawson ― the mother of Beyoncé — who posted about the loss on Instagram.
But Christian was also a superstar at the center where she worked for 26 years and among those who knew her. She was the kind of person who brought lunch to a new co-worker and hosted a baby shower for someone without close family, according to her daughter and a memorial board.
At the outset of the COVID crisis, Christian was not given personal protective equipment, her daughter, Courtney Christian, 30. She said her mother received a mask only in late March. A lawyer for the center acknowledged Christian’s death and said federal guidelines were followed but didn’t respond to specific questions about protective gear.
Christian was diagnosed April 2. She endured more than a week of fever, chills and coughing, but seemed to be on the mend. She had been cleared to return to work when she collapsed at home. An outpouring of grief followed, her daughter said.
“She just helped and cared for so many people,” she said. “People I had never met.”
— JoNel Aleccia, Kaiser Health News | Published May 15, 2020
(Return to top.)
At Work, Church And Home, Army Veteran Gave It His All
(Courtesy of Shlonda Clark)
Roy Chester Coleman
Age: 64
Occupation: Emergency medical technician
Place of Work: Overton Brooks VA Medical Center in Shreveport, Louisiana
Date of Death: April 6, 2020
Shlonda Clark calls her father her “favorite superhero.”
It was one of Roy Coleman’s many roles. For the past 11 years, the Army veteran and EMT worked as a housekeeper at the VA hospital in his hometown. He was a church deacon, Sunday school teacher and usher. He also volunteered with special-needs adults.
Roy had a big family, with three children, eight grandchildren and two great-grandchildren.
“He was funny, he was kind, he was giving,” said Mabel Coleman, his wife of 40 years.
“If he didn’t like you, something was wrong with you,” added Clark.
Coleman fell ill March 23. After three trips to the emergency room, he was admitted March 27, with a fever and labored breathing.
“It was the last time I saw him,” Mabel said.
He tested positive for COVID-19 and died at the hospital where he had worked.
His family said he was concerned about the lack of personal protective equipment. The VA medical center said by email it “has and continues to use PPE in accordance with CDC guidelines.”
— Katja Ridderbusch | Published May 15, 2020
(Return to top.)
Beloved Doctor Made House Calls, Treated Patients Like Family
(Courtesy of the Giuliano family)
Michael Giuliano
Age: 64
Occupation: Family practice physician
Place of Work: Mountainside Medical Group in Nutley, New Jersey
Date of Death: April 18, 2020
For 39 years, Michael Giuliano practiced old-fashioned family medicine.
He made house calls. He visited his patients in the hospital rather than asking another physician to check in on them. He saw generations of the same family.
“Some patients would show up here at the house,’” said Giuliano’s wife, Marylu, a nurse and the office manager of his solo practice. “Patients would call and he’d say, ‘Come on over, I’ll check you out.’ He always went above and beyond.”
A father of five and a grandfather of four, Giuliano was jovial, with a quirky sense of humor and love of Peanuts characters, especially Charlie Brown. He liked to tell patients, “I’ll fix you up.”
“He treated all of his patients like family,” said Nutley Mayor Joseph Scarpelli.
When COVID-19 hit the U.S., Giuliano ordered N95 masks, his family said, but suppliers were out and sent surgical masks instead. Giuliano wore two at a time.
The week of March 16, Giuliano saw four patients with respiratory symptoms who later tested positive for COVID-19. About two weeks later, he tested positive.
Giuliano continued to see patients from home using telemedicine until he was hospitalized. He died 11 days later.
— Michelle Crouch | Published May 15, 2020
(Return to top.)
He Tried To Reassure His Family Until The End
(Courtesy of Sheryl Pabatao)
Alfredo Pabatao
Age: 68
Occupation: Orderly
Place of Work: Hackensack Meridian Health Palisades Medical Center in North Bergen, New Jersey
Date of Death: March 26, 2020
After 44 years of marriage, Alfredo Pabatao still bought his wife, Susana, flowers.
“They were that type of couple that you rarely see nowadays,” their youngest daughter, Sheryl Pabatao, 30, said. “They set such a high standard for us, their kids — that may be the reason why I’m still single.” She said her father was a patient man who could fix just about anything.
The Pabataos came from Quezon City, just outside Manila, in the Philippines. Alfredo worked at a car dealership, and Sheryl said she and her siblings grew up comfortably.
But the couple wanted more for their five children, and immigrated to the United States in October 2011. “The first year that we were here, was really, really tough,” Sheryl remembered. Her oldest two siblings, already adults by the time the Pabataos’ immigration application cleared, had to stay behind.
Alfredo found a job as an orderly at a hospital in New Jersey, where he worked for nearly two decades. In mid-March, he told his family he had transported a patient with signs of COVID-19; he fell ill days later. In a statement, his employer wrote: “We have policies and procedures in place to protect our team members and patients that are all in accordance with CDC guidelines.”
Sheryl said the family’s last conversation with her father was via FaceTime, with him on his hospital bed. Connected to oxygen, he insisted he wasn’t gravely ill. He made jokes and even demonstrated yoga poses to reassure his wife and children. He died soon after.
— Danielle Renwick, The Guardian | Published May 15, 2020
(Return to top.)
A ‘Selfless’ Mother Who ‘Always Had The Right Words’
(Courtesy of Sheryl Pabatao)
Susana Pabatao
Age: 64
Occupation: Assistant nurse
Place of Work: Bergen New Bridge Medical Center in Paramus, New Jersey
Date of Death: April 30, 2020
Susana Pabatao became a nurse in her late 40s, after her family immigrated to the United States.
It eased some of her longing for her own mother, whom she had left behind in the Philippines, her daughter, Sheryl Pabatao said. “It helped her to know that she was helping other people — something that she couldn’t do for my grandmother,” Sheryl said. Susana treated her older patients as if they were her own parents, she added.
Susana was warm, selfless and a constant source of comfort. Sheryl said, “My mom always had the right words.”
Susana’s husband, Alfredo Pabatao, began showing symptoms of COVID-19 in mid-March, and Susana became ill soon after. Sheryl, who described the two as “inseparable,” said: “When my dad got sick, it’s like part of her was not there anymore.”
Alfredo was hospitalized, and Susana spent her last days at home resting and speaking with him on FaceTime. Sheryl, who lived with her parents, said she overheard the two console each other one morning. “My mom was telling my dad, ‘We’ve gone through so many things, we’re going to get through this.”
Alfredo died on March 26. Susana died four days later.
— Danielle Renwick, The Guardian | Published May 15, 2020
(Return to top.)
Air Force Doctor Had Served In The White House
(Courtesy of the Medical Center of Annandale)
Steven Perez
Age: 68
Occupation: Internal medicine physician
Place of Work: Medical Center of Annandale in Annandale, Virginia
Date of Death: May 7, 2020
When George H.W. Bush announced his 1988 run for the presidency, Steven Perez was one of the doctors who gave him a clean bill of health.
An “Air Force brat” who was born in the United Kingdom, Perez served as a flight surgeon and medical director in the Air Force Medical Service Corps before practicing as a physician in the White House from 1986 to 1990, according to a statement from his family.
“It was the honor of his life,” his son, Benjamin Perez, said.
Perez went into private practice in San Antonio in the early ’90s before opening his own clinic in Northern Virginia. He also taught at the University of Virginia.
According to his family, he made a promise to God and “never refused medical aid to the poor who came to his office, even accepting yams as payment on occasion.”
Perez’s family describes him as a proud grandfather to his three grandchildren (with two more on the way); he loved the University of Southern California Trojan football, the Dallas Cowboys and the Nationals.
“He could make anyone laugh, knew just what to say, and showed profound love for his friends and family,” his family wrote in an obituary. “Every person he met felt like they were the reason he was there.”
— Danielle Renwick, The Guardian | Published May 15, 2020
(Return to top.)
She Jumped At Chance To Lend Her Nursing Skills To Her Beloved New York
(Courtesy of the Sell family)
Rosemary Sell
Age: 80
Occupation: Pediatric nurse practitioner
Place of Work: New York City public schools
Date of Death: April 17, 2020
Rosemary Sell was a New Yorker through and through. Born in Washington Heights in northern Manhattan, she went to nursing school in Greenwich Village and raised her five boys on the Lower East Side.
In the 1960s, she traveled to Berlin, where she worked as a nurse for the British army and met her future husband, Peter. A lifelong love of travel was born. Gregarious and high-energy by nature, she loved meeting new people. “Wherever she’d go, she’d make a new friend,” said her son, also named Peter.
In later years, Sell spent much of her time in Florida. But she jumped at opportunities to lend her nursing skills to her home city and see her grandchildren and friends.
In February, she was contacted by a firm that places nurses on temporary assignments. Her children were concerned about the encroaching pandemic, especially given her age. “But they need a nurse,” she responded. She traveled to New York to fill in as a nurse at several schools citywide just as the pandemic took hold. The firm, Comprehensive Resources, did not respond to questions on protections for its contractors.
Sell began developing symptoms in mid-March, just before the citywide school closure went into effect. She returned home to Florida, where she died from pneumonia caused by COVID-19.
Before Rosemary died, she had been hatching her next adventure with a friend: to travel to India. She wanted to see the Taj Mahal.
— Noa Yachot, The Guardian | Published May 15, 2020
(Return to top.)
A Hands-On Pharmacist Who Made The Big City Feel Smaller
(Courtesy of Zair Yasin)
Ali Yasin
Age: 67
Occupation: Pharmacist
Place of Work: New York City Pharmacy in East Village, Manhattan
Date of Death: May 4, 2020
Ali Yasin was a small-town druggist in a big city filled with impersonal, chain-store pharmacies. He found a way to operate a robust business and still be on a first-name basis with his customers. Over the years, he became their medical consultant, insurance whisperer and friend.
Jen Masser said she stumbled into Yasin’s pharmacy the first time, covered from hands to elbows in hives. “Something is happening, see someone right away,” Yasin advised. “This could be a serious disease.” He turned out to be right, encouraging her to keep seeing doctors until she finally got the proper autoimmune diagnosis.
Born in Pakistan, Yasin moved to the United States in 1979 and worked in various pharmacies before opening his own in 2001. He ran it with the help of his four sons.
In March, after serving customers in hard-hit Manhattan in his typical hands-on manner, Yasin contracted a cough and tested positive for COVID-19. By month’s end, he was in the hospital on a ventilator. He died May 4.
The storefront window of the Yasin family pharmacy is pasted with condolence cards. Son Zair Yasin said the outpouring has been immense: “I didn’t realize until he was gone how many people he touched.”
— Kathleen Horan | Published May 15, 2020
(Return to top.)
Nurse Wouldn’t Abandon Her Patients Or Let Family Worry
(Courtesy of the Isaacs family)
Marsha Bantle
Age: 65
Occupation: Registered nurse
Place of Work: Signature Healthcare in Newburgh, Indiana
Date of Death: May 1, 2020
Marsha Bantle’s family begged her to quit after a resident in the nursing home where she worked was diagnosed with COVID-19.
But Bantle wouldn’t leave. “My patients can’t leave their rooms, they can’t see their families. They really need me right now,’” she told her cousin Carol Isaacs.
Bantle tried to reassure relatives she would limit her exposure, but, on April 17, her temperature spiked. Bantle, who lived alone, holed up at home. She finally called her family when it was clear she needed to be hospitalized.
“That’s Marsha for you,” her cousin John Isaacs said. “She didn’t want us to worry.”
Even while hospitalized, Bantle was selfless, said Shay Gould, the ICU nurse who cared for her. She offered to turn off her medication pump to save the nurse a trip. She asked for other patients’ names to pray for them.
After about a week, Bantle had a stroke, likely brought on by the COVID-19 infection. Within days, she died.
Since April, the nursing home has had 52 positive cases and 13 COVID-19 deaths, including Bantle’s. In a statement, Signature Healthcare said: “The loss of any of our residents or staff, for any reason, is devastating.”
— Michelle Crouch | Published May 12, 2020
(Return to top.)
Pharmacist, Feeling Sick, Didn’t Want To Let Patients Down
(Courtesy of the Boynes family)
Sean Boynes
Age: 46
Occupation: Pharmacist
Place of Work: AbsoluteCare Medical Center & Pharmacy in Greenbelt, Maryland
Date of Death: April 2, 2020
When the coronavirus began circulating in the Washington metropolitan region, Sean Boynes went to work.
“Patients need their medicine,” he told his wife, Nicole.
The medical center where he worked bills itself as “a medical home for the sickest of the sick”; many of its patients struggle with chronic illness and poverty. Boynes was the Greenbelt branch’s first pharmacist.
He was an “incredible, loving guy,” said Dr. Gregory Foti, chief of innovative operations at AbsoluteCare.
Boynes was a proud Howard University alumnus and had three degrees — a bachelor’s of science in biology, a master’s in exercise physiology and a doctorate in pharmacy — from the institution.
In early March, Boynes and his wife began feeling sick. Boynes didn’t want to stop working but thought “taking a sick day might be OK,” Nicole said. He also took a break from being a jungle gym to his eight- and 11-year-old girls. Nicole called him “Super Dad.”
Nicole got better, but Sean, who had asthma, saw his breathing deteriorate.
On March 25, Nicole dropped him at the hospital doors. The medical staff confirmed COVID-19. The family never saw him again.
Foti said AbsoluteCare follows CDC recommendations, such as providing staff with face masks, and declined to comment on where Boynes became infected. He said “it was literally impossible to tell” where Boynes had contracted the virus.
To honor him, AbsoluteCare is naming the Greenbelt pharmacy after Boynes.
— Sarah Jane Tribble, Kaiser Health News | Published May 12, 2020
(Return to top.)
A Spry EMT, He Made ‘The Ultimate Sacrifice’
(Courtesy of Toni Lorenc)
John Careccia
Age: 74
Occupation: Emergency medical technician and rescue squad chief
Place of Work: Woodbridge Township Ambulance and Rescue Squad in Iselin, New Jersey
Date of Death: April 17, 2020
“That’s not the way you throw a curveball!” John Careccia famously declared to his grandson at a family picnic, according to his daughter, Toni Lorenc. Careccia then threw the ball so wide that it broke a window in her shed.
“That’s how you throw the batter off,” he said, brushing off the mishap.
“Typical Pop-Pop,” Lorenc said. “He had so much confidence in himself.”
Careccia, who worked for the Port Authority of New York and New Jersey for 30 years, harnessed his self-confidence into a second career. Inspired by two EMTs who saved his son’s life, he became a volunteer EMT in 1993. A consummate educator, he taught CPR, mentored young EMTs and gave catechism classes at his church, Lorenc said.
A spry 74, Careccia responded to 911 calls as chief of his rescue squad, a volunteer position. On a March 25 call, he evaluated a coronavirus patient, said Ed Barrett, squad president. Careccia died of COVID-19 several weeks later.
At his firehouse memorial service, Careccia was summoned over a loudspeaker for his “last call.”
“Having heard no response from Chief Careccia, we know that John has made the ultimate sacrifice,” said Steve Packer, a previous squad president. “His leadership, dedication, compassion and friendship will be greatly missed.”
— Melissa Bailey | Published May 12, 2020
(Return to top.)
Police Officer Turned Nurse Practitioner Was Pursuing A Doctorate
(Courtesy of Dennis Graiani)
Kevin Graiani
Age: 56
Occupation: Family nurse practitioner
Place of Work: Rockland Medical Group in Garnerville, New York
Date of Death: March 30, 2020
Kevin Graiani always wanted to work in health care, according to Dennis Graiani, one of his three sons. But his mother told him he needed a pension, so he became a cop.
Kevin, who grew up in the Bronx, served five years on the New York City Housing Authority police force, then 15 on a suburban police force in Spring Valley, New York. He was a “brilliant officer,” said Lt. Jack Bosworth of Spring Valley.
Known for his dry sense of humor, Kevin often rattled off quotes from movies. He played bagpipes for the Rockland County Police Emerald Society, a law enforcement group. When he retired from police work, he began nursing school and became a nurse practitioner in 2018.
Kevin, who worked at a private practice, became sick on March 10 and was later diagnosed with COVID-19, Dennis said.
He loved learning and was set to finish classes this summer for his doctorate of nursing practice, said Lynne Weissman, his professor and program director at Dominican College.
He was an “extremely bright student” with a 3.7 GPA, Weissman said.
She has nominated him for a posthumous degree.
— Melissa Bailey | Published May 12, 2020
(Return to top.)
School Nurse ‘Was A Mother To Many’
(Courtesy of the Howard family)
Marilyn Howard
Age: 53
Occupation: School nurse
Place of Work: Spring Creek Community School in Brooklyn, New York
Date of Death: April 4, 2020
Marilyn Howard was known for her generosity and never missing a party. Born in Guyana, she came to the U.S. as a teenager. She helped raise her five brothers, putting her ambitions on hold. “She was a mother to many,” her brother Haslyn said.
In her mid-30s, she turned to her own career goals. She steadily racked up four nursing degrees and recently had begun studying to become a nurse practitioner.
Howard, who lived in Queens, New York, was a school nurse in Brooklyn, where she regularly treated children with chronic illnesses associated with poverty. The week before the pandemic shuttered schools, a fellow nurse had a fever and cough.
Days later, Howard developed the same symptoms. After initially improving, she took a sudden turn for the worse April 4. As her brother drove her to the hospital, her heart stopped. She was declared dead at the hospital.
In tribute, hundreds turned out on Zoom to mark Nine-Night — a days-long wake tradition in the Caribbean — where loved ones shared photos, sang songs and recounted Howard’s effect on their lives.
The pandemic has since ripped through Howard’s extended family, infecting at least a dozen relatives. (One cousin was hospitalized but was released and is recovering.) The family has evolved into a sprawling triage team, monitoring one another’s temperatures, delivering food, charting emergency contacts and nearby hospitals.
Howard’s brothers hope to start a foundation in her name to help aspiring nurses in the U.S. and West Indies. “The best way to honor her spirit and her memory is to bring more nurses into this world,” said her brother Rawle. “We need more Marilyns around.”
— Noa Yachot, The Guardian | Published May 12, 2020
(Return to top.)
Post-Retirement, She Tirelessly Rejoined Workforce
(Courtesy Bethany MacDonald)
Nancy MacDonald
Age: 74
Occupation: Receptionist
Place of Work: Orchard View Manor, a nursing home and rehabilitation center in East Providence, Rhode Island
Date of Death: April 25, 2020
Nancy MacDonald tried retiring, but couldn’t make it stick.
For 20 years, she was a middle school teaching assistant and cheerleading coach. At home, she loved painting rocks and watching “Blue Bloods” and “American Idol.” She was married with two adult children.
A lifelong Rhode Islander, Nancy was a people person, her daughter, Bethany MacDonald, said. “She always wanted to help others.”
So, in 2017, it was natural that she’d go back to work, this time at a nursing home.
As Orchard View’s COVID case count escalated, MacDonald worried. Still, she kept coming in — washing and reusing her N95 respirator and having her temperature taken daily.
Tim Brown, an Orchard View spokesperson, said the facility has “extensive infection control,” satisfying government guidelines. He would not say how often employees receive new N95s.
On April 13, MacDonald began coughing. By April 16, she was hospitalized. Her COVID test came back positive. She died 10 days later ― almost a week after her last conversation with her daughter.
“I said, ‘Mama, we love you,’” Bethany said. “The last words she said to me were, ‘I love you, too.’”
— Shefali Luthra, Kaiser Health News | Published May 12, 2020
(Return to top.)
Despite Danger, Semi-Retired Nurse Kept Caring For ER Patients
(Courtesy of the Miles family)
Sheena Miles
Age: 60
Occupation: Registered nurse
Place of Work: Scott Regional Hospital in Morton, Mississippi
Date of Death: May 1, 2020
At age 60, Sheena Miles was semi-retired. She usually worked every other weekend, but as COVID-19 emerged in Mississippi, she worked four weekends in a row from mid-March to mid-April.
“I’ve got a duty,” she told her son, Tom Miles.
The economy where she lived is dominated by poultry plants, and the county has been a coronavirus hot spot. Sheena was diligent with protective gear, wearing her mask and doubling up on gloves, Tom said. She stayed home when she wasn’t working.
“Losing Sheena has been a tragic loss, as she had been a part of our hospital for 25 years,” said Heather Davis, a hospital administrator.
Sheena took ill on Easter Sunday. By Thursday, Tommy Miles, her husband of 43 years, drove her to the University of Mississippi Medical Center in Jackson.
Two long weeks passed. The family was allowed to say goodbye in person, and on their way into her room, an ICU nurse told them that years ago Sheena had cared for his infant daughter. “‘Your mom saved her life,’” the nurse said.
“That was a little comfort in the storm,” Sheena’s son said.
— Michaela Gibson Morris | Published May 12, 2020
(Return to top.)
A Nurse Who Was Living Her Dream Of Working In The U.S.
(Courtesy of Venus Donasco-Delfin)
Anjanette Miller
Age: 38
Occupation: Registered nurse
Place of Work: Community First Medical Center and Kindred Chicago Lakeshore in Chicago, and Bridgeway Senior Living in Bensenville, Illinois
Date of Death: April 14, 2020
As a child, Anjanette Miller dreamed of becoming a nurse in the U.S. She studied in her native Philippines and worked briefly in Saudi Arabia before fulfilling her wish in 2001.
Miller settled in Chicago and worked as a supervising nurse at three facilities. Her sister, Venus Donasco-Delfin, said Miller got along well with co-workers who shared her work ethic.
“At work, I think, she was strict, but beyond work, she’s a great friend,” Donasco-Delfin said. One of five siblings, she was the “pillar of the family” and supported relatives back home.
“I studied psychology for two years,” Donasco-Delfin said, “but she kept calling me [in the Philippines] and said, ‘No, Venus. … You have to pursue nursing. You will make a difference.’” Donasco-Delfin, now in Canada, became a nurse.
Miller started feeling sick in mid-March and was diagnosed with COVID-19 in early April. She self-isolated, chronicling her illness on YouTube and Facebook. She was hospitalized April 5 and died nine days later.
Miller had hoped to retire to the Philippines and pursue her other passion, filmmaking. Last year she traveled back home to shoot scenes for a project. “The movie she was making is about her life story,” Donasco-Delfin said. “But it’s not finished yet.”
— Danielle Renwick, The Guardian | Published May 12, 2020
(Return to top.)
He Took The Time To Put Patients At Ease
(Courtesy of Holy Name Medical Center)
Jesus Villaluz
Age: 75
Occupation: Patient transport worker
Place of Work: Holy Name Medical Center in Teaneck, New Jersey
Date of Death: April 3, 2020
After Jesus Villaluz died from COVID-19 complications, colleagues lined the hallway at Holy Name Medical Center in Teaneck, New Jersey, to say goodbye. They’d never done that for anyone else.
“Jesus knew many and meant a lot to all of us, so this gesture felt like the right thing to do,” said hospital spokesperson Nicole Urena.
The hospital, and surrounding Bergen County, have been hit hard by the pandemic. By May 8, Holy Name had treated more than 6,000 COVID patients, 181 of whom died.
Villaluz worked at Holy Name for 27 years. In a Facebook post, the hospital memorialized Villaluz’s generosity: He once won a raffle and shared the winnings with colleagues, an anecdote New Jersey Gov. Phil Murphy repeated at a news conference. Family members declined requests for an interview.
Co-worker Hossien Dahdouli said Villaluz’s compassion for patients was exemplary. He never rushed anyone, took the time to chat with patients and was always concerned for their privacy and safety, Dahdouli said.
Years ago, after Dahdouli had a sad day caring for deteriorating ICU patients, he asked Villaluz why he always appeared so happy.
“He said, ‘My worst day at work is better than someone’s best day as a patient.’”
— Anna Almendrala, Kaiser Health News | Published May 12, 2020
(Return to top.)
Family Vacations And Reggae Gave Rhythm To His Life
(Courtesy of Nina Batayola)
Don Ryan Batayola
Age: 40
Occupation: Occupational therapist
Place of Work: South Mountain Healthcare and Rehabilitation Center in Vauxhall, New Jersey
Date of Death: April 4, 2020
April 4 was the day Don and Nina Batayola had planned to leave for London on a 10-day European vacation. Instead, that was the day Don died of COVID-19.
The Springfield, New Jersey, couple loved to travel ― on their own or with their children, Zoie, 10, and Zeth, 8. Disney World. Road trips to Canada. Every year for a week they would savor the beach on North Carolina’s Outer Banks.
Don’s love of reggae music prompted a trip to Jamaica to visit Bob Marley’s birthplace.
The Batayolas, both occupational therapists, moved to New Jersey from the Philippines 13 years ago to pursue their careers.
“He loved to help,” Nina said. “He had such the ability to make everybody smile or laugh.”
Don worked with at least one patient and a handful of colleagues who subsequently tested positive for COVID-19, and in late March, he developed symptoms. Nina came home from work for lunch on March 31 to find him struggling to breathe. She dialed 911.
He was hospitalized, then she also developed COVID symptoms. Self-isolating at home, Nina talked with Don once a day. She thought he seemed stronger but, on the fourth day, his heart suddenly stopped.
— Michelle Andrews | Published May 8, 2020
(Return to top.)
Even On ‘The Saddest Day … She Could Make You Laugh’
(Courtesy of Kim Bruner)
Brittany Bruner-Ringo
Age: 32
Occupation: Nurse
Place of Work: Silverado Beverly Place in Los Angeles
Date of Death: April 20, 2020
When it was Brittany Bruner-Ringo’s turn to pick the family vacation, it was always New Orleans. A city so full of life.
And that is how family described the 32-year-old who left the Oklahoma plains for the excitement of Southern California.
“She always made the best of things,” her mother, Kim Bruner, said. “It could be the saddest day, and she could make you laugh.”
Bruner-Ringo worked at a dementia care center. On March 19, she admitted a patient flown in from New York. She suspected he might have COVID-19, and she was nervous. For fear of frightening the patients, she hadn’t been allowed to wear a mask or gloves, she told her mom by phone that night. (A spokesperson from her employer said, “We have no issues in our environment using appropriate masking and gloves and have followed CDC guidelines throughout this pandemic. We have always had adequate PPE to protect our residents and associates.”)
The following day, the patient grew worse. Bruner-Ringo checked into a hotel to isolate from her roommate. She later tested positive for COVID-19, but when she developed symptoms did not complain ― even to her mom: “She would say, ‘I’m fine. I’m going to beat this. Don’t worry about me.’”
Bruner, a veteran nurse herself, called the hotel front desk for help getting an ambulance to her daughter. She had just hung up with her daughter, who insisted she was fine, while struggling to breathe.
— Samantha Young, Kaiser Health News | Published May 8, 2020
(Return to top.)
He And His Wife Shared A Lust For Travel ― And A COVID Diagnosis
(Courtesy of LaKita Bush)
Joshua Bush
Age: 30
Occupation: Nurse and nursing student
Place of Work: Benton House of Aiken in Aiken, South Carolina
Date of Death: April 17, 2020
Joshua Bush never let his wife, LaKita, forget that she was five hours late for their first date.
“He never held back telling the truth,” LaKita said, with a doleful laugh.
They met online in 2011, each attracted to the other’s lust for travel. For Joshua’s 30th birthday, they took a cruise to Bermuda. He yearned to go farther afield to Tokyo to revel over anime.
Joshua began his nursing career after high school, eventually ending up at Benton House of Aiken, an assisted living facility. Joshua and LaKita, who works in human resources for a hospital, thought it was allergy-related when they both fell ill in late March. Benton House had no confirmed COVID cases at the time, LaKita said. Even still, the staff was taking precautions.
A doctor prescribed Joshua flu medication, but his symptoms — fever and aches but no cough — worsened, and he was admitted to a hospital in Augusta, Georgia, on April 4.
“That was the last time I saw him alive,” LaKita said.
Over the next few days, both tested positive for the coronavirus. Joshua was sedated in the hospital for two weeks and died on April 17. LaKita recovered at home.
Joshua was earning a bachelor’s degree in nursing at the University of South Carolina-Aiken. May would have marked the couple’s fifth anniversary.
— Sarah Varney, Kaiser Health News | Published May 8, 2020
(Return to top.)
Her Sudden Death Blindsided Husband And Autistic Son
(Courtesy of Vincent Carmello)
Karen Carmello
Age: 57
Occupation: Licensed practical nurse
Place of Work: Maryhaven Center of Hope in Port Jefferson Station, New York
Date of Death: April 16, 2020
Karen Carmello had an intimate understanding of working with intellectually disabled patients.
Her 26-year-old son, Steven, has autism. According to her husband, Vincent, the two spoke by phone every day. Steven would recall exactly what he did, and Karen listened intently.
“She could do no wrong in his eyes, ever,” Vincent said. “It’s a very special bond, but it’s one that she earned.”
Sharing the news of her death was shattering: “It was the hardest thing I’ve ever had to do — letting him know.”
When Karen took ill, she discovered that a patient in her ward had tested positive for COVID-19. She was hospitalized March 23. Eight days later, she sent Vincent her last text, at 2:17 a.m., before going to the ICU.
On April 16, hospital staff called and asked whether Vincent would be comfortable signing a do-not-resuscitate order. He hadn’t been able to see his wife, so he didn’t completely grasp how grave her condition was.
“I thought, ‘OK, this must be a formality,'” he said. “I authorized it. And I got a call within two hours that she passed. I was stunned.”
— Shoshana Dubnow, Kaiser Health News | Published May 8, 2020
(Return to top.)
His Facebook Posts Left Clues Of A Tragic Timeline
(Courtesy of Felicia Dodson-Hill)
Maurice Dotson
Age: 51
Occupation: Certified nursing assistant
Place of Work: West Oaks Nursing and Rehabilitation Center in Austin, Texas
Date of Death: April 17, 2020
Maurice Dotson’s sister knew something was wrong when her older brother didn’t post his daily Facebook update.
“We knew he was good as long as he posted every morning,” Felicia Dodson-Hill, of Jacksonville, Arkansas, said.
Dotson, 51 ― a certified nursing assistant for 25 years at the West Oaks Nursing and Rehabilitation Center in Austin — had begun caring for COVID-19 patients.
He sounded positive on Facebook, posting on March 30: “We are going through scary, difficult times, but better days are coming.”
Days later, family in Arkansas couldn’t reach him.
“We had been trying to get in contact with him since April 1st,” his sister said. “On April 3rd, he posted that he had to go to the hospital ― that he was not feeling good.”
Dodson-Hill said the hospital sent him home. Her mother finally reached him on April 6 or 7.
“He told my mom he didn’t have the energy to barely talk,” Dodson-Hill said.
Dawunna Wilson, a cousin from Hazen, Arkansas, said Maurice called an ambulance on April 8. Results from his coronavirus test done at the hospital came back positive the next day. “From there, it was pretty much downhill,” Wilson said.
— Sharon Jayson | Published May 5, 2020
(Return to top.)
Community Salutes Nurse Who Loved Baseball
(Courtesy of Leigh Ann Lewis)
Barbara Finch
Age: 63
Occupation: Licensed practical nurse
Place of Work: Southern Virginia Regional Medical Center in Emporia, Virginia
Date of Death: March 29, 2020
When Barbara Finch got excited, she’d scrunch her hands into fists and wave them around like a kid at Christmas. She did it when the Atlanta Braves scored, or while watching her grandkids play baseball, her No. 1 passion outside work.
Finch spent her 37-year nursing career in the emergency department of the hospital in Emporia, Virginia (population of about 5,000), where one of her four children, Leigh Ann Lewis, worked as an EMT.
Lewis knew her mother was well liked: Patients she transported from the hospital would rave that Finch had been sweet and compassionate.
Finch fell ill on March 17 and died in an ICU 12 days later. As a hearse carried her casket to the graveyard, Lewis said, people lined the way at driveway mailboxes, churches and stores, holding signs that read, “We love you,” “Praying for you,” “Hugs.” At her hospital, employees released balloons to the sky.
“It seemed like, in our area, she knew everybody — either she worked with them, or they were a patient of hers at some point,” Lewis said. “It was a very, very large outpour of love and comfort and solidarity.”
— Melissa Bailey | Published May 8, 2020
(Return to top.)
‘He Loved To Work,’ With No Plans To Retire
(Courtesy Giancarlo Pattugalan)
Tomas Pattugalan
Age: 70
Occupation: Internal medicine physician
Place of Work: Private practice in Jamaica, Queens, New York
Date of Death: March 29, 2020
Tomas Pattugalan’s kids had been encouraging him to retire. Even after 45 years of medicine, Pattugalan wasn’t ready to slow down.
“He loved his patients. He loved to work. He loved to help others,” said Giancarlo, his son. “He had an enormous capacity to give of himself.”
A father of three, Pattugalan grew up in the Philippines, immigrating to the U.S. in the 1970s. He was a devout Catholic — attending Mass weekly ― and “karaoke master,” Giancarlo said.
In early March, Pattugalan began testing patients for COVID-19. His medical history, including a family history of strokes and high blood pressure, heightened his own risk. So after tests of two patients returned positive, he got tested himself. On March 24, he learned he had the coronavirus.
“He made a joke and said Prince Charles had tested [positive] too, and he was sharing royalty,” Giancarlo said. “He was making light of it, not trying to get any of us worried.”
Pattugalan had a cough. Then came wheezing. His oxygen levels dropped. He tried hydroxychloroquine, an experimental treatment touted by President Donald Trump that has yielded mixed results. Nothing helped.
On March 29, Pattugalan agreed to seek hospital care. He died that day.
— Shefali Luthra, Kaiser Health News | Published May 8, 2020
(Return to top.)
Says Widow Battling Cancer: ‘He Was My Backbone’
(Courtesy of Melissa Castro Santos)
Darrin Santos
Age: 50
Occupation: Transportation supervisor
Place of Work: NewYork-Presbyterian Westchester Behavioral Health Center in White Plains, New York
Date of Death: April 4, 2020
Melissa Castro Santos had just started a new treatment for multiple myeloma when her husband, Darrin, got sick.
For nearly two weeks, he isolated in their bedroom, but after he began gasping for air, he went to the hospital. He died of COVID-19 days later.
“It’s just unbelievable,” Castro Santos said.
As a transportation supervisor, Santos delivered health care workers and equipment between hospitals in the New York metropolitan area. He loved his job, Castro Santos said, and was known to drive doctors wherever and whenever they were needed, through heavy traffic and snowstorms.
Castro Santos, who has been battling cancer since 2012, said her husband doted on their three teenagers, all avid athletes. He arranged his work schedule to attend as many of their games as possible. When he couldn’t make it, she would call him on FaceTime so he could catch glimpses of the action.
Unable to hold a funeral, they arranged for burial five days after Santos died. Friends lined the streets in cars in a show of support as the family drove to and from the cemetery.
Now Castro Santos is confronting cancer without her husband. “He was my backbone. He was the one who took me to chemotherapy and appointments.”
— Anna Jean Kaiser, The Guardian | Published May 8, 2020
(Return to top.)
An Animal Lover Who Loved Aerospace, She Died Alone At Home
(Courtesy of Aubree Farmer)
Lisa Ewald
Age: 53
Occupation: Registered nurse
Place of Work: Henry Ford Hospital in Detroit
Date of Death: April 1, 2020
Lisa Ewald was a nurse to many living things, human and otherwise.
When her neighbor Alexis Fernandez’s border collie had a stomach blockage, Ewald hooked the dog up to an IV four times a day. “She was this dedicated nurse who nursed my dog back to health,” Fernandez said.
Ewald also loved gardening, aerospace and comic book conventions.
Ewald told Fernandez that a patient she had treated later tested positive for COVID-19, and that she was not wearing a mask at the time. Two days later, after seeing the patient, she got sick. After delays in accessing a test, she learned on March 30 that she was infected with the coronavirus.
A hospital spokesperson acknowledged that staff who treat coronavirus patients have a higher risk of exposure, but said there was “no way to confirm” how a staff member contracted the virus.
On March 31, Ewald didn’t answer when Fernandez texted her. The next day, Fernandez and a hospital nurse went to Ewald’s home to check on her and found her unresponsive on the couch.
“I said, ‘Aren’t you going to go take her pulse or anything?’” Fernandez said. “The nurse just said, ‘She’s gone.’”
— Melissa Bailey | Published May 5, 2020
(Return to top.)
An Ardent EMT Who Seemed To Have Nine Lives
(Courtesy of Ben Geiger)
Scott Geiger
Age: 47
Occupation: Emergency medical technician
Place of Work: Atlantic Health System in Mountainside and Warren, New Jersey
Date of Death: April 13, 2020
Scott Geiger wasn’t always enthusiastic about school, but at age 16 he brought home a tome the size of two phone books. It was a manual for emergency medical technicians, and he devoured it, said his younger brother, Ben Geiger.
Scott was certified as an EMT at 17. He never married or had kids, but did not seem to miss those things.
“He was so focused on being an EMT and helping people in their most vulnerable and desperate moments,” Ben said. “That’s really what made him feel good.”
Scott loved playing pool each week with friends. He was a loyal New York Jets football fan, content to joke about their follies and watch them lose. He was quiet. And he seemed to have nine lives, his brother said, surviving hospitalizations for epilepsy as a kid and blood cancer around age 40.
When the coronavirus began to tear a path through northern New Jersey, he faced his EMT work with resolve. He downplayed his symptoms when he first fell ill in late March, but wound up spending 17 days on a ventilator before he died. The family has had to mourn separately, with the brothers’ father, who lived with Scott, in quarantine, and their mother confined to her room in a nursing home that has COVID-19 cases.
— Christina Jewett, Kaiser Health News | Published May 5, 2020
(Return to top.)
Caring Nurse ‘Always Put Herself Last’
(Courtesy of Lisa Lococo)
Theresa Lococo
Age: 68
Occupation: Pediatric nurse
Place of Work: Kings County Hospital in Brooklyn, New York
Date of Death: March 27, 2020
Theresa Lococo spent most of her life at the hospital, working as a pediatric nurse for almost 48 years.
“There wasn’t a day that goes by she wouldn’t come home and tell me about her patients,” said her daughter, Lisa Lococo. “She had to be forced to take her vacation days.”
New York City Mayor Bill de Blasio publicly saluted her lifelong service to New Yorkers, saying, “She gave her life helping others.”
Theresa had dogs — “sometimes too many,” Lisa said — and lived with her son, Anthony, in the home she owned for decades. She loved cooking and watching cooking shows, reading and following soap operas.
Theresa wasn’t tested for COVID-19. But Kings County Hospital, in Brooklyn, was hit hard by the coronavirus.
Days before dying, she described nausea. Friends recalled a cough. Her supervisor encouraged her to stay home, her daughter said.
Lisa called her mother on March 27, just as Anthony was dialing 911 for help.
“She always put others first,” Lisa said. “She always put herself last.”
— Shefali Luthra, Kaiser Health News | Published May 5, 2020
(Return to top.)
He Was Full Of Life And Planning For The Future
(Courtesy of the Luna family)
Felicisimo “Tom” Luna
Age: 62
Occupation: Emergency room nurse
Place of Work: Trinitas Regional Medical Center in Elizabeth, New Jersey
Date of Death: April 9, 2020
Tom Luna was a joker, a lively and outgoing man who thrived on the fast-paced and varied action of the emergency room. He also adored his three daughters, something clear to all who knew him.
“Tom was a fantastic emergency nurse. He was well liked and loved by his peers,” Gerard Muench, administrative director of the Trinitas emergency department, said in a statement. “His greatest love was for his wife and daughters, who he was very proud of.”
His oldest daughter, Gabrielle, 25, followed his path to become an ER nurse. When Tom fell ill with the coronavirus, he was admitted to the hospital where she works. At the end of her 12-hour night shifts, she made sure he had breakfast and helped him change his clothes. She propped a family photo next to his bed.
Tom’s wife, Kit, also a nurse, said that when some of his symptoms appeared to let up, they talked about him recovering at home. He was a planner, she said, and was already talking about their next family vacation, maybe to Spain.
— Christina Jewett | Published May 5, 2020
(Return to top.)
Air Force Veteran Went ‘Above And Beyond For Patients’
Michael Marceaux and his wife, Dunia, when he graduated from nursing school in 2018 (Courtesy of Drake Marceaux)
Michael Marceaux
Age: 49
Occupation: Registered nurse
Place of Work: Christus Highland Medical Center and Brentwood Hospital in Shreveport, Louisiana
Date of Death: April 16, 2020
After Michael Marceaux retired from the Air Force, he went back to school. In 2018 he launched a new career as an emergency room nurse.
“Everyone who worked with him said he was so happy,” said Drake Marceaux, one of his four sons. “He was willing to go above and beyond for patients.”
As the coronavirus spread throughout Louisiana, Michael developed a cough and fever. Soon afterward, he tested positive for COVID-19.
“He didn’t seem too worried,” Drake said. “He just wanted to make sure not to give it to other people.”
A spokesperson with Christus Health said Michael would be missed for “how he always had a positive attitude, even after a hard shift. His laughter brought joy to others.” The spokesperson declined to answer questions about workplace safety conditions.
Drake said he wanted his father to be remembered for how much he was loved.
His funeral was livestreamed on Facebook. “At one point, there were 2,000 viewers watching his service,” Drake said. “As much as he didn’t want attention, it gravitated toward him.”
— Victoria Knight, Kaiser Health News | Published May 5, 2020
(Return to top.)
She Loved To Give Gifts And Never Forgot Her Hometown
(Courtesy of Courtesy of Donald Jay Marcos)
Celia Lardizabal Marcos
Age: 61
Occupation: Telemetry charge nurse
Place of Work: CHA Hollywood Presbyterian Medical Center in Los Angeles
Date of Death: April 17, 2020
Whenever she traveled to her hometown of Tagudin in the Philippines, Celia Lardizabal Marcos showered family with gifts and delighted in planning weekend outings for everyone, said her eldest son, Donald.
And when she returned home to California, she brought presents for her sons. “She always thought of how her family could be happy,” he said.
Trained as a nurse in her home country, Marcos immigrated to the United States in 2001 and settled in Los Angeles. Three years later, she became a telemetry charge nurse, a specialist who tracks patients’ vital signs using high-tech equipment.
On April 3, she was one of three nurses who responded after a suspected COVID patient went into cardiac arrest. Wearing a surgical mask, she intubated the patient. Three days later, she had a headache, body aches and difficulty breathing.
Her symptoms worsened, and she was admitted April 15 to the hospital where she had worked for 16 years. That was the last time Donald spoke to his mother. Two days later, she went into cardiac arrest and died that night.
Her sons plan to honor her wishes to be cremated and buried in Tagudin, alongside her parents.
— Christina M. Oriel, Asian Journal | Published May 5, 2020
(Return to top.)
‘Hero Among Heroes,’ Doctor Cared For Generations Of Patients
Francis Molinari (right) with his siblings (from left) Janice, Albert and Lisa (Courtesy of Lisa Molinari)
Francis Molinari
Age: 70
Occupation: Physician
Place of Work: Private practice in Belleville, New Jersey; privileges at Clara Maass Medical Center
Date of Death: April 9, 2020
In late March, Dr. Francis “Frankie” Molinari told his sister Lisa he was “down for the count,” with chills, fever and trouble breathing.
“Frankie, you know what you have,” she recalled telling him.
“Yes.”
Two days later, he collapsed at home and was rushed to Clara Maass Medical Center. Colleagues stayed by his side as he succumbed to COVID-19.
“We take solace in the fact that he was cared for by colleagues and friends who deeply loved and respected him,” his sister Janice wrote in a blog. “He died a hero among heroes.”
Molinari, a New Jersey native who was married with an adult daughter, was the oldest of four siblings. His sisters describe him as a positive guy who loved music, fishing and teasing people with tall tales: He went to medical school in Bologna, Italy, and he liked to say he had played pinochle with the pope.
Molinari practiced medicine for over four decades, caring for generations of patients in the same family. His family suspects he contracted the coronavirus at his private practice.
“A friend had once described us as four different legs of the same table,” Janice wrote. “Now I’m stuck on the fact that we are only a three-legged table. Less beautiful, less sturdy. Broken.”
— Laura Ungar, Kaiser Health News | Published May 5, 2020
(Return to top.)
5-Foot-Tall ‘Fireball’ Was A Prankster To Her Sons
(Courtesy Josh Banago)
Celia Yap-Banago
Age: 69
Occupation: Registered nurse
Place of Work: Research Medical Center in Kansas City, Missouri
Date of Death: April 21, 2020
Celia Yap-Banago was a 5-foot-tall “fireball,” said one co-worker. She had moved to the U.S. from the Philippines in 1970 and worked for nearly 40 years for the HCA Midwest Health system. Her family said she was planning for retirement.
Her son Josh said she showed her love through practical jokes: “You knew she loved you if she was yelling at you or if she was pranking you.”
“She was very outspoken,” said Charlene Carter, a fellow nurse. “But I later learned that’s a really good quality to have, as a nurse, so you can advocate for your patients and advocate for yourself.”
In March, Yap-Banago treated a patient who later tested positive for COVID-19. Carter said Yap-Banago was not given personal protective equipment because she was not working in an area designed for COVID patients. She spent her final days in isolation to protect others.
A spokesperson for HCA Midwest Health said that medical staff received adequate personal protective equipment in line with CDC guidelines.
Josh said she spoke with reverence of her patients and their families. “She was always focused on the family as a whole, and that the family was taken care of, not just the patient in the bed,” he said.
— Alex Smith, KCUR | Published May 5, 2020
(Return to top.)
In Ministry And Rescue Missions, ‘He Put His All Into It’
(Courtesy of the Birmingham Family)
Billy Birmingham Sr.
Age: 69
Occupation: Emergency medical technician
Place of Work: Kansas City Missouri Fire Department
Date of Death: April 13, 2020
Bill Birmingham Jr. fondly remembers the year his father took on a new career. The whole family studied, even acting out scenes to ensure Billy Birmingham Sr., a minister, was ready for his emergency medical technician exam.
“He put his all into it,” the son recalled.
Billy Birmingham passed the test. And from the late 1990s on, he served as an EMT and a minister.
His family rallied again for his doctorate in pastoral theology. During nearly four decades as a minister, he founded two churches.
“He had a heart for other people,” his son said. “Whatever he could do for other people, he would do it.”
As an EMT with the Kansas City Fire Missouri Department, he was exposed to the novel coronavirus. The cough came in March.
“‘I’m just tired.’ That’s what he kept saying,” his son said. His dad went to the hospital twice. The first time he told the staff about his symptoms and underlying health conditions, then they sent him home.
The second time he arrived in an ambulance. Just over two weeks later, his final hours arrived.
Hospital staff set up a video chat so his family could see him one last time.
— Cara Anthony, Kaiser Health News | Published May 1, 2020
(Return to top.)
Jovial Man Trained Scores Of Doctors In Obstetrics, Gynecology And Kindness
(Courtesy of Ashley Ulker)
Luis Caldera-Nieves
Age: 63
Occupation: OB-GYN doctor
Place of Work: University of Miami and Jackson health systems in Miami
Date of Death: April 8, 2020
“Somos felices.” That was Dr. Luis Caldera-Nieves’ signature signoff after a cesarean section or patient visit or at the end of a difficult shift. “We’re happy,” he meant, and often, when he was around, it was true.
Caldera-Nieves, a popular OB-GYN, trained scores of doctors and helped bring thousands of babies into the world in his 25 years at the University of Miami and Jackson health systems.
Born in Bayamón, Puerto Rico, he worked as an Air Force doctor before joining UM, said longtime co-worker Dr. Jaime Santiago. Caldera-Nieves was so devoted to his patients that he often gave them his private phone number — and his wife’s, Santiago said.
Because he was so jovial, he earned the nickname “the Puerto Rican Santa Claus,” Santiago said.
“He was truly loved and admired by everyone who worked with him, and will be remembered for his humor and never-ending positive energy,” said Dr. Jean-Marie Stephan, who trained under Caldera-Nieves.
In a statement, UM and Jackson confirmed Caldera-Nieves died from complications of COVID-19 and said they “grieve the loss of our esteemed and beloved colleague.” He is survived by his wife and six adult children.
— Melissa Bailey | Published May 1, 2020
(Return to top.)
A Cluster Of Illness Robs Community Of Another Fearless EMT
(Courtesy of Vito Cicchetti)
Kevin Leiva
Age: 24
Occupation: Emergency medical technician
Place of Work: Saint Clare’s Health in Passaic, New Jersey
Date of Death: April 7, 2020
When Kevin Leiva died of COVID-19 in early April, it was a second crushing loss to his close-knit team of EMT workers. Their colleague, Israel Tolentino Jr., had died one week before.
“People were scared that everyone was going to die from it,” said Vito Cicchetti, a director at Saint Clare’s Health, where the men worked. “After Izzy died, we all started getting scared for Kevin.”
Leiva, according to an obituary, “was always worried about his crew.” He was “very proud” of his work and was recalled to have said “becoming an EMT was an act of God.”
He met his wife, Marina, online while they were in high school. She moved a thousand miles to build a life with him. He loved spending time at their home, playing guitar and tending to his tegu lizards, AJ and Blue.
As COVID-19 ramped up, the station’s three ambulances each handled up to 15 dispatches a shift, roughly double the usual number. In a busy 12-hour shift, EMTs often responded to calls continuously, stopping only to decontaminate themselves and the truck.
Leiva “always had a joke” that helped to defuse stressful situations and bring his co-workers together, Cicchetti said.
— Michelle Andrews | Published May 1, 2020
(Return to top.)
Firefighting And ‘Helping People’ Were In His Blood
(Courtesy of the Terre Haute Fire Department)
John Schoffstall
Age: 41
Occupation: Paramedic and firefighter
Place of Work: Terre Haute Fire Department in Terre Haute, Indiana
Date of Death: April 12, 2020
John Schoffstall grew up around firehouses, and it was at his own firehouse in Terre Haute, Indiana, that he was exposed to the coronavirus.
A paramedic and firefighter with the Terre Haute Fire Department for almost 12 years, Schoffstall died April 12 at age 41. Deputy Chief Glen Hall said investigations by the county health department and his own department “determined John contracted the virus from another firefighter in the firehouse.” Four other firefighters “had symptoms but none progressed.”
“We respond every day to potential COVID patients,” Hall said.
Jennifer Schoffstall, his wife of 18 years, said her husband went to the hospital March 28.
“His breathing was so bad in the ER, they just decided to keep him,” she said. “He regressed from there.”
Hall said Schoffstall’s “biggest hobby was his family,” with a son, 17, and a daughter, 13.
Schoffstall’s father had been a volunteer firefighter, Jennifer said, and her husband signed up for the New Goshen Volunteer Fire Department when he turned 18.
“He loved the fire service and everything about it,” she said. “He loved helping people.”
— Sharon Jayson | Published May 1, 2020
(Return to top.)
Boston Nurse, A Former Bus Driver, Was A Champion For Education
(Courtesy of Teadris Pope)
Rose Taldon
Age: 63
Occupation: Nurse
Place of Work: New England Baptist Hospital in Boston
Date of Death: April 12, 2020
Rose Taldon was just 5 feet tall. But when she bellowed out the window, her kids ran right home.
“She didn’t take any crap,” said her daughter, Teadris Pope.
Taldon raised three children with her husband on the street where she grew up in Dorchester, Boston. She was respected as a strong black woman, earning a nursing degree while working in public transit for 23 years. Described as stern, she still was quick to tickle her eight grandkids.
Taldon was generous: Even as she lay in a hospital in April, exhausted from the coronavirus, she arranged to pay bills for an out-of-work friend, her daughter said.
It’s unclear whether Taldon caught the virus at her hospital, designated for non-COVID patients. Hospital officials said three patients and 22 staff have tested positive.
Once her mother was hospitalized, Pope couldn’t visit. On Easter morning, a doctor called at 2 a.m., offering to put Taldon on a video call.
“I just talked until I had no words,” Pope said. “I was just telling her, ‘We’re so proud of you. You worked so hard raising us. … You’ve gone through a hell of a fight.'”
An hour later, her mother was gone.
— Melissa Bailey | Published May 1, 2020
(Return to top.)
Unflappable First Responder With An Ever-Ready Smile
(Courtesy of Vito Cicchetti)
Israel Tolentino Jr.
Age: 33
Occupation: Emergency medical technician and firefighter
Place of Work: Saint Clare’s Health and the Passaic Fire Department, both in Passaic, New Jersey
Date of Death: March 31, 2020
When Israel Tolentino Jr. arrived for his EMT shift one morning in March, he seemed fine. Then he got a headache. Then a fever came on, and he was sent home, said Vito Cicchetti, a director at Saint Clare’s Health.
Izzy, as he was called, was an EMT who fulfilled his dream to become a firefighter. In 2018, the former Marine took a job with the Passaic Fire Department but kept up shifts at Saint Clare’s.
He was husband to Maria Vazquez, whom he’d met at church, according to nj.com. They had two young children.
The work pace could be brutal during the pandemic. In a 12-hour shift, Tolentino and his partner were dispatched to one emergency after another, each typically lasting under an hour but requiring nearly that long to decontaminate their gear and truck.
Izzy died in hospital care. The coronavirus tore through his EMT team. Most eventually recovered. But his friend and co-worker Kevin Leiva also died.
Izzy’s unflappable, cheerful presence is missed, Cicchetti said: “No matter how mad you were, he’d come up with a smile and you’d be chuckling to yourself.”
Cicchetti hasn’t replaced either man: “I don’t know if I’m ready for that yet.”
— Michelle Andrews | Published May 1, 2020
(Return to top.)
Their Decade-Long Dream Marriage Ends In Nightmare
(Courtesy of the Detroit Fire Department)
Capt. Franklin Williams
Age: 57
Occupation: Firefighter and medical first responder
Place of Work: Detroit Fire Department in Detroit
Date of Death: April 8, 2020
Capt. Franklin Williams stood at the altar on his wedding day and pretended to hunt for the ring. He patted his chest, then his pants legs and looked up at his soon-to-be wife with a million-dollar smile.
He was always clowning and “so silly,” said Shanita Williams, his wife, recalling how he wanted to make her laugh. Williams, 57, died from complications of the novel coronavirus on April 8 — one month before the couple’s 10-year wedding anniversary.
Williams had been on an emergency call with a verified COVID patient before falling ill, according to Detroit Fire Department Chief Robert Distelrath. He died in the line of duty.
Crews are equipped with personal protective equipment including a gown, N95 mask and gloves. But it’s easy for a mask to slip ― “when you’re giving [chest] compressions, your mask isn’t staying in place all the time,” said Thomas Gehart, president of the Detroit Fire Fighters Association.
When Williams fell sick on March 24, he moved to the guest bedroom and never returned to work.
“I’m thankful and thank God for having him in my life,” Shanita said, adding that she keeps hoping this is a nightmare and she’ll soon wake up.
— Sarah Jane Tribble, Kaiser Health News | Published May 1, 2020
(Return to top.)
A 9/11 First Responder, He Answered The Call During The Pandemic
(Courtesy of the Valley Stream Fire Department)
Mike Field
Age: 59
Occupation: Volunteer emergency medical technician
Place of Work: Village of Valley Stream on New York’s Long Island
Date of Death: April 8, 2020
Mike Field had a strong sense of civic duty. An emergency medical technician, he was a first responder with the New York Fire Department (FDNY) on 9/11. He was also a member of his community’s all-volunteer fire department since 1987.
After he retired from FDNY in 2002, he took a job making and posting street signs with his local public works department. He continued to volunteer with Valley Stream’s fire department and mentoring the junior fire department. When he wasn’t responding to emergencies or training future emergency technicians, he led a Boy Scout troop and volunteered for animal causes.
“Here’s somebody who cares about the community and cares about its people,” said Valley Stream’s mayor, Ed Fare, who had known Mike since the seventh grade.
Stacey Field, Mike’s wife, said he found his calling early, after his own father experienced a heart attack. “When the fire department EMTs came and helped his dad, he decided that’s what he wanted to do,” she said.
Their three sons ― Steven, 26; Richie, 22; and Jason, 19 — have followed in their father’s footsteps. Steven and Richie are EMTs in New York; Jason plans on training to become one as well. All three volunteer at the same fire station their father did.
In late March, Mike and fellow volunteer responders were called to an emergency involving a patient showing symptoms of COVID-19. Field died on April 8.
— Sharon Jayson | Published April 29, 2020
(Return to top.)
Nurse Fought For His Life In Same ICU Where He Cared For Patients
(Courtesy of Romielyn Guillermo)
Ali Dennis Guillermo
Age: 44
Occupation: Nurse
Place of Work: Long Island Community Hospital in East Patchogue, New York
Date of Death: April 7, 2020
In 2004, Ali Dennis Guillermo, his wife, Romielyn, and their daughter came to New York from the Philippines to find a better life.
Everything fell into place. The former nursing instructor landed a job at Long Island Community Hospital, often working in intensive care or the emergency room. He enjoyed the intensity of ER work, his wife said. As years passed, the couple had two sons and settled into a close-knit Philippine community.
As COVID-19 emerged, Guillermo was posted to the step-down floor, working with patients transitioning out of intensive care.
A lot of the nurses on his floor had gotten sick with the virus, his wife said, and “everybody was scared.”
And then, Guillermo felt achy, with a fever that soared to 102. He went to the hospital and X-rays were taken, but he was sent home. Within days, his blood oxygen level plummeted.
“My nails are turning blue,” he told his wife. “You should take me to the ER.”
He was admitted that night in late March, and they never spoke again.
In the ICU unit where he’d often worked, Guillermo was intubated and treated. Nearly two weeks later, he died.
— Michelle Andrews | Published April 29, 2020
(Return to top.)
An Eager Student, He Aimed To Become A Physician Assistant
(Courtesy of Catrisha House-Phelps)
James House
Age: 40
Occupation: Registered nurse
Place of Work: Omni Continuing Care nursing home in Detroit
Date of Death: March 31, 2020
James House had a voracious appetite for learning about and a fascination with the human body.
His sister, Catrisha House-Phelps, traces it back to childhood visits to a dialysis center where their father received treatments. “That was what tugged at his heart,” she said. “He just always wanted to know ‘why.’”
House-Phelps said her brother adored his five children, treasured his anatomy and physiology books and got a kick out of the residents he cared for at Omni Continuing Care. “He thought they were family; he just said they were funny people,” she said. He had hoped to go back to school to become a physician assistant.
House came down with what he thought was the flu in mid-March. His sister said he tried to get tested for COVID-19 but was turned away because he was not showing textbook symptoms and had no underlying health issues. On March 31, after resting at home for over a week, House returned to work. Hours later, he collapsed and was rushed to the hospital.
He texted his sister with updates on his condition. “I’m about to be intubated now,” he wrote. It was the last message he sent her.
— Danielle Renwick, The Guardian | Published April 29, 2020
(Return to top.)
She Loved A Parade And Catering To Patients
Pamela Hughes and her daughter, Brie
(Courtesy of Angie McAllister)
Pamela Hughes
Age: 50
Occupation: Nursing home medication aide
Place of Work: Signature HealthCARE at Summit Manor in Columbia, Kentucky
Date of Death: April 13, 2020
Pamela Hughes lived her entire life in rural Columbia, Kentucky, but longed for wide, sandy beaches. For vacation, Hughes and her daughter, Brie, 26, eagerly drove 14 hours to Daytona Beach, Florida, or Myrtle Beach, South Carolina.
After high school, Hughes worked at Summit Manor, a nursing home in Columbia, for 32 years. She knew which residents preferred chocolate milk or applesauce with their medication; she remembered their favorite outfits and colors. Hughes’ shy demeanor vanished each December when she and co-worker Angie McAllister built a float for the town’s Christmas parade competition.
“We built 10 floats over 10 years,” McAllister said. “We got second place every year.”
Even after several residents tested positive for the coronavirus, Hughes dismissed her worsening cough as allergies or bronchitis. The nursing home was short on help and she wanted to serve her patients, Brie said.
Days later, the public health department suggested her mother get tested. She tested positive, and her health worsened — food tasted bitter, her fever soared, her hearing dulled. On April 10, Hughes was taken by ambulance to a hospital, then by helicopter to Jewish Hospital in Louisville. Barred from visiting, Brie said goodbye over FaceTime.
— Sarah Varney, Kaiser Health News | Published April 29, 2020
(Return to top.)
The Family Matriarch And ‘We’re Failing Miserably Without Her’
(Courtesy of Ginu John)
Aleyamma John
Age: 65
Occupation: Registered nurse
Place of Work: Queens Hospital Center in New York City
Date of Death: April 5, 2020
Aleyamma John’s family wanted her to retire. Her husband, Johnny, an MTA transit worker, had stopped working a few years earlier. He and their son Ginu urged her to follow suit. “We told her, ‘I’m sure Dad wants to see the world with you — you need to give him that opportunity,’” Ginu said.
She demurred. “I think she found fulfillment in being able to serve,” Ginu said. “She was able to hold people’s hands, you know, even when they were deteriorating and be there for them.” She began her career as a nurse in India 45 years ago; she and her husband immigrated to the United Arab Emirates, where their two sons were born, and moved to New York in 2002.
Ginu said his mother, a devout Christian, found joy in tending to her vegetable garden and doting on her two grandchildren. She cooked dishes from her native India and filled the Long Island home she shared with Johnny, Ginu and Ginu’s family with flowers.
In March, as Queens Hospital Center began to swell with COVID-19 patients, John sent her family a photo of herself and colleagues wearing surgical hats and masks but not enough personal protective equipment. Days later, she developed a fever and tested positive for the virus. Johnny, Ginu and Ginu’s wife, Elsa, a nurse practitioner, also became ill.
When John’s breathing became labored, her family made the difficult decision to call 911. It would be the last time they saw her. “We’re 17 days in, and I feel like we’re failing miserably without her,” Ginu said.
— Danielle Renwick, The Guardian | Published April 29, 2020
(Return to top.)
‘A Kind Man’ Looking Forward To Retirement
(Courtesy of Jesse Soto)
Thomas Soto
Age: 59
Occupation: Radiology clerk
Place of Work: Woodhull Medical Center, a public hospital in Brooklyn, New York
Date of Death: April 7, 2020
After more than 30 years at one of New York City’s busy public hospitals, Thomas Soto loved his job but was looking forward to retiring, said his son, Jesse Soto, who lived with him.
At Soto’s busy station near the emergency room, he greeted patients and took down their information.
“Everybody saw him before their X-rays,” Soto, 29, said. “He smiled all day, made jokes. He was a kind man.”
As COVID patients began to overwhelm Woodhull and other emergency rooms across the city, Soto said that at first his father didn’t have any protective gear.
He eventually got a mask. But he still grew very sick, developing a high fever, body aches and a wracking cough. After a week, Soto said, “he couldn’t take it anymore.”
He went to Woodhull, where he was admitted. When they tried to put him on a ventilator two days later, he died. The hospital did not respond to requests for comment.
— Michelle Andrews | Published April 29, 2020
(Return to top.)
‘Blooming’ In Her First Job On Path To Becoming A Nurse
(Courtesy of the Viveros family via GoFundMe)
Valeria Viveros
Age: 20
Occupation: Nursing assistant
Place of Work: Extended Care Hospital of Riverside, California
Date of Death: April 5, 2020
At 20 years old, Valeria Viveros was “barely blooming,” developing the skills and ambition to pursue a nursing career, said Gustavo Urrea, her uncle. Working at Extended Care Hospital of Riverside was her first job.
Viveros, born in California to Mexican immigrants, grew attached to her patients at the nursing home, bringing them homemade ceviche, Urrea said. About a month ago, as he watched her cook, play and joke with her grandmother, he noticed how much her social skills had grown.
When she would say “Hi, Tío,” in her playful, sweet, high-pitched voice, “it was like the best therapy you could have,” Urrea recalled. Viveros, who lived with her parents and two siblings, was enrolled in classes at a community college.
Viveros felt sick on March 30, went to a nearby hospital and was sent home with Tylenol, Urrea said. By April 4, she couldn’t get out of bed on her own. She left in an ambulance and never came back.
“We’re all destroyed,” he said. “I can’t even believe it.”
On April 5, county health officials reported a coronavirus outbreak had sickened 30 patients and some staff at her nursing home. Trent Evans, general counsel for Extended Care, said staffers are heartbroken by her death.
Viveros was “head over heels in love with the residents that she served,” he said. “She was always there for them.”
— Melissa Bailey | Published April 29, 2020
(Return to top.)
Surgical Technician Made Friends Everywhere She Went
(Courtesy of Jorge Casarez)
Monica Echeverri Casarez
Age: 49
Occupation: Surgical technician
Place of Work: Detroit Medical Center Harper University Hospital in Detroit
Date of Death: April 11, 2020
Monica Echeverri Casarez was in constant motion, said her husband, Jorge Casarez. The daughter of Colombian immigrants, she worked as a Spanish-English interpreter in clinical settings. She was the kind of person whose arrival at a mom and pop restaurant would elicit hugs from the owners. She also co-founded Southwest Detroit Restaurant Week, a nonprofit that supports local businesses.
Twice a month, she scrubbed in as a surgical technician at Harper University Hospital. “She liked discovering the beauty of how the body works and how science is clear and orderly,” Casarez said. She was organized and intuitive, qualities that are assets in the operating room. On March 21, she posted a photo of herself in protective gear with the caption: “I’d be lying if I said I wan’t at least a bit nervous to be there now.” Since many elective surgeries had been canceled, Echeverri Casarez was tasked with taking the temperatures of people who walked into the hospital and making sure their hands were sterilized.
Soon after, Echeverri Casarez and Casarez began feeling ill. Quarantined together, Echeverri Casarez tried to make the best of the situation. She baked her husband a cake — chocolate with white frosting. She died a few days later.
— Danielle Renwick, The Guardian | Published April 24, 2020
(Return to top.)
A Whip-Smart Neurologist Endlessly Fascinated With The Brain
(Courtesy of Jennifer Sclar)
Gary Sclar
Age: 66
Occupation: Neurologist
Place of Work: Mount Sinai Queens in New York City
Date of Death: April 12, 2020
Gary Sclar was a whip-smart neurologist who loved comic books, “Game of Thrones” and “Star Wars,” said his daughter, Jennifer Sclar. He was deeply compassionate with a blunt bedside manner.
“My dad was fascinated with the brain and with science,” Jennifer Sclar said. “His work was his passion, and it’s what made him the happiest, besides my brother and me.” Set to retire in June, he was looking forward to writing about politics and neurology.
Gary Sclar saw patients who were showing COVID-19 symptoms and knew his age and underlying health conditions ― he had diabetes — put him at risk for developing complications from the illness. His daughter pleaded with him to stop going to the hospital.
In early April, he mentioned having lost his sense of smell, and on April 8 he collapsed in his home. He was hospitalized a few days later and agreed to be intubated. “I don’t think he realized, like, that this was the end,” Jennifer Sclar said. “He brought his keys. He brought his wallet.”
— Danielle Renwick, The Guardian | Published April 24, 2020
(Return to top.)
An Exacting But Loving Aunt, She Was A Mentor Until The End
(Courtesy of Jhoanna Mariel Buendia)
Araceli Buendia Ilagan
Age: 63
Occupation: Intensive care unit nurse
Place of Work: Jackson Memorial Hospital in Miami
Date of Death: March 27, 2020
For Jhoanna Mariel Buendia, her aunt was a constant ― if distant — presence. Araceli Buendia Ilagan emigrated from their hometown Baguio, in the Philippines, to the U.S. before Buendia was born, but she remained close to her family and communicated with them nearly every day.
“She was one of the smartest people I ever knew,” Buendia, 27, said. Buendia Ilagan, who at one point looked into adopting her niece so she could join her and her husband the United States, encouraged Buendia to become a nurse, and talked her through grueling coursework in anatomy and physiology. Buendia is now a nurse in London.
Buendia Ilagan was also demanding. “Whenever she visited the Philippines, she wanted everything to be organized and squeaky-clean,” Buendia said.
The last time the two spoke, in late March, Buendia Ilagan didn’t mention anything about feeling ill. Instead, the two commiserated over their experiences of treating patients with COVID-19; as always, her aunt offered her advice on staying safe while giving the best possible care. She died four days later.
— Danielle Renwick, The Guardian | Published April 22, 2020
(Return to top.)
A Beloved Geriatric Psychiatrist And Church Musician Remembered For His Cooking Skills
(Courtesy of Nida Gonzales)
Leo Dela Cruz
Age: 57
Occupation: Geriatric psychiatrist
Place of Work: Christ Hospital and CarePoint Health in Jersey City, New Jersey
Date of Death: April 8, 2020
Dr. Leo Dela Cruz was nervous about going to work in the weeks before he died, his friends said. Like many in the region, Christ Hospital had an influx of COVID-19 patients and faced a shortage of ventilators and masks.
Dela Cruz was a geriatric psychiatrist and didn’t work in coronavirus wards. But he continued to see patients in person. In early April, Dela Cruz, who lived alone, complained only of migraines, his friends said. Within a week, his condition worsened, and he was put on a ventilator at a nearby hospital. He died soon after.
Friends said he may have been exposed at the hospital. (In a statement, hospital representatives said he didn’t treat COVID-19 patients.)
Dela Cruz, the oldest of 10 siblings, came from a family of health care professionals. His friends and family — from Cebu, Philippines, to Teaneck, New Jersey — remembered his jovial personality on Facebook. He won “best doctor of the year” awards, played tennis and cooked traditional Cebu dishes.
Nida Gonzales, a colleague, said he always supported people, whether funding a student’s education or running a church mental health program. “I feel like I lost a brother,” she said.
— Ankita Rao, The Guardian | Published April 22, 2020
(Return to top.)
Alabama Nurse Remembered As Selfless But Sassy
(Courtesy of Amanda Williams)
Rose Harrison
Age: 60
Occupation: Nurse
Place of Work: Marion Regional Nursing Home in Hamilton, Alabama
Date of Death: April 6, 2020
Rose Harrison, 60, lived to serve others ― her husband, three daughters, grandchildren and the residents of the nursing home where she worked. Though the Alabama nurse was selfless, she also had a sassy edge to her personality and a penchant for road rage, her daughter, Amanda Williams said.
“Her personality was so funny, you automatically loved her,” Williams said. ��She was so outspoken. If she didn’t agree with you, she’d tell you in a respectful way.”
Harrison was not wearing a mask when she cared for a patient who later tested positive for COVID-19 at Marion Regional Nursing Home in Hamilton, Alabama, her daughter said. She later developed a cough, fatigue and a low-grade fever, but kept reporting to duty all week. Officials from the nursing home did not return calls for comment.
On April 3, Williams drove her mother to a hospital. The following evening, Harrison discussed the option of going on a ventilator with loved ones on a video call, agreeing it was the best course. Williams believed that her mother fully expected to recover. She died April 6.
— Christina Jewett, Kaiser Health News | Published April 22, 2020
(Return to top.)
Connecticut Social Worker Had Angelic Singing Voice And A Zest For Life
(Courtesy of the Hunt family)
Curtis Hunt
Age: 57
Occupation: Social worker
Places of Work: Cornell Scott-Hill Health Center and New Reach, both in New Haven, Connecticut
Date of Death: March 23, 2020
At a shelter for adults recovering from addiction, residents looked forward to the days when Marion “Curtis” Hunt would take the stage, emceeing talent shows and belting out Broadway and gospel tunes.
It wasn’t part of his job description as a social worker. It was just one of the ways he went “above and beyond,” said his supervisor at Cornell Scott-Hill Health Center, Daena Murphy. “He had a beautiful voice,” she said. “He was just a wonderful person — funny, engaging, always a huge smile on his face.”
Hunt, the youngest of four brothers, earned his master’s in social work from Fordham University at 52, and was baptized at his brother’s Pentecostal church at 54. He was a devoted uncle who doted on his dog and cat, Mya and Milo.
It’s unclear how Hunt got infected, but one patient he worked with had tested positive for COVID-19, as did two co-workers, according to Dr. Ece Tek, another supervisor at Cornell Scott-Hill Health Center. Hunt died on March 23, one week after developing flu-like symptoms, said his brother John Mann Jr.
— Melissa Bailey | Published April 22, 2020
(Return to top.)
To The End, King-Smith Was Driven By A Desire To Help Others
(Courtesy of Hassana Salaam-Rivers)
Kim King-Smith
Age: 53
Occupation: Electrocardiogram technician
Place of Work: University Hospital in Newark, New Jersey
Date of Death: March 31, 2020
Kim King-Smith was a natural caregiver. An only child, she grew up close to her extended family, including her cousins Hassana Salaam-Rivers and Sharonda Salaam. After Salaam developed multiple sclerosis, King-Smith visited her every day.
“She’d bring her sweets that she wasn’t supposed to have and share them with her,” Salaam-Rivers said. King-Smith’s desire to care for others was the reason she became an electrocardiogram technician, her cousin added. “If a friend of a friend or family member went to the hospital, she would always go and visit them as soon as her shift was over,” she said.
In March, King-Smith cared for a patient she said had symptoms of COVID-19; she soon fell ill herself and tested positive for the virus. It seemed like a mild case at first, and she stayed in touch with family via FaceTime while trying to isolate from her husband, Lenny.
On March 29, Salaam-Rivers checked in on her cousin and noticed she was struggling to breathe. She urged her to call an ambulance. After King-Smith was hospitalized, she exchanged text messages with her mother and cousin. As the day progressed, her messages carried increasingly grave news, Salaam-Rivers said. Then she stopped responding.
— Danielle Renwick, The Guardian | Published April 22, 2020
(Return to top.)
On The Eve Of Retirement, VA Nurse Succumbs To COVID-19
(Courtesy of Mark Accad)
Debbie Accad
Age: 72
Occupation: Clinical nursing coordinator
Place of Work: Detroit VA Medical Center in Detroit, Michigan
Date of Death: March 30, 2020
Nurse Divina “Debbie” Accad had cared for veterans for over 25 years and was set to retire in April. But after contracting the novel coronavirus, she spent her final 11 days on a ventilator — and didn’t survive past March.
She joined a growing list of health care professionals working on the front lines of the pandemic who have died from COVID-19.
Accad, 72, a clinical nursing coordinator at the Detroit VA Medical Center, dedicated her life to nursing, according to her son Mark Accad.
“She died doing what she loved most,” he said. “That was caring for people.”
Read more here.
— Melissa Bailey | Published April 15, 2020
(Return to top.)
California Nurse Thrived In ER and ICU, But Couldn’t Survive COVID-19
Jeff Baumbach and his wife, Karen
(Courtesy of the Baumbach family)
Jeff Baumbach
Age: 57
Occupation: Nurse
Place of Work: St. Joseph’s Medical Center in Stockton, California
Date of Death: March 31, 2020
Jeff Baumbach, 57, was a seasoned nurse of 28 years when the novel coronavirus began to circulate in California. He’d worked in the ER, the ICU and on a cardiac floor. Hepatitis and tuberculosis had been around over the years but never posed a major concern. He’d cared for patients who had tuberculosis.
Jeff and his wife, Karen Baumbach, also a nurse, initially didn’t consider it significantly riskier than challenges they’d faced for years.
“He’d worked in the ICU. He was exposed to so many things, and we never got anything,” she said. “This was just ramping up.”
One day during work, Jeff sent a sarcastic text to his wife: “I love wearing a mask every day.”
Within weeks, he would wage a difficult and steady fight against the virus that ended with a sudden collapse.
Read more here.
— Christina Jewett, Kaiser Health News | Published April 15, 2020
(Return to top.)
Nurse’s Faith Led Her To Care For Prisoners At A New Jersey Jail
(Courtesy of Denise Rendor)
Daisy Doronila
Age: 60
Occupation: Nurse
Place of Work: Hudson County Correctional Facility in Kearny, New Jersey
Date of Death: April 5, 2020
Daisy Doronila had a different perspective than most who worked at the Hudson County Correctional Facility, a New Jersey lockup 11 miles from Manhattan. It was a place where the veteran nurse could put her Catholic faith into action, showing kindness to marginalized people.
“There would be people there for the most heinous crimes,” said her daughter, Denise Rendor, 28, “but they would just melt towards my mother because she really was there to give them care with no judgment.”
Doronila, 60, died April 5, two weeks after testing positive for the coronavirus that causes COVID-19. The jail has been hit hard by the virus, with 27 inmates and 68 staff members having tested positive. Among those, another nurse, a correctional officer and a clerk also died, according to Ron Edwards, Hudson County’s director of corrections.
Doronila fell ill before the scope of the jail infections were known. She was picking up extra shifts in the weeks before, her daughter said, and planning on a trip to Israel soon with friends from church.
That plan began to fall apart March 14, when someone at the jail noticed her coughing and asked her to go home and visit a doctor.
Read more here.
— Christina Jewett, Kaiser Health News | Published April 15, 2020
(Return to top.)
An Army Veteran, Hospital Custodian ‘Loved Helping People’
(Courtesy of Michelle Wilcox)
Alvin Simmons
Age: 54
Occupation: Environmental service assistant
Place of Work: Rochester General Hospital in Rochester, New York
Death: March 17, 2020
Alvin Simmons started working as a custodian at Rochester General Hospital, in New York state, weeks before he fell ill. “He loved helping people and he figured the best place to do that would be in a hospital,” his sister, Michelle Wilcox said.
An Army veteran who had served in the first Gulf War, Simmons loved karaoke and doted on his three grandchildren, Wilcox said. “He was a dedicated, hardworking individual who had just changed his life around” since a prison stint, she said.
According to Wilcox, Simmons began developing symptoms shortly after cleaning the room of a woman he believed was infected with the novel coronavirus. “Other hospital employees did not want to clean the room because they said they weren’t properly trained” to clean the room of someone potentially infected, she said. “They got my brother from a different floor, because he had just started there,” she said. (In an email, a hospital spokesperson said they had “no evidence to suggest that Mr. Simmons was at a heightened risk of exposure to COVID-19 by virtue of his training or employment duties at RGH.”)
On March 11, he visited the emergency room at Rochester General, where he was tested for COVID-19, Wilcox said. Over the next few days, as he rested at his girlfriend’s home, his breathing became more labored and he began to cough up blood. He was rushed to the hospital on March 13, where he was later declared brain-dead. Subsequently, he received a COVID-19 diagnosis. Simmons died on March 17.
— Danielle Renwick, The Guardian | Published April 15, 2020
(Return to top.)
Nurse At Nevada VA Dies After Caring For Infected Colleague
(Courtesy of Bob Thompson)
Vianna Thompson
Age: 52
Occupation: Nurse
Places of Work: VA Sierra Nevada Health Care System and Northern Nevada Medical Center in Reno, Nevada
Date of Death: April 7, 2020
Nurse Vianna Thompson, 52, spent two night shifts caring for a fellow Veterans Affairs health care worker who was dying from COVID-19.
Two weeks later, she too was lying in a hospital intensive care unit, with a co-worker holding her hand as she died.
Thompson and the man she treated were among three VA health care workers in Reno, Nevada, to die in two weeks from complications of the novel coronavirus.
“It’s pretty devastating. It’s surreal. Reno’s not that big of a city,” said Robyn Underhill, a night nurse who worked with Thompson in the ER at Reno’s VA hospital the past two years.
Thompson, who dreamed of teaching nursing one day, died April 7, joining a growing list of health care professionals killed in the pandemic.
Read more here.
— Melissa Bailey | Published April 15, 2020
(Return to top.)
Dr. J. Ronald Verrier Was Busy Saving Lives Before The Pandemic
(Courtesy of Christina Pardo)
J. Ronald Verrier
Age: 59
Occupation: Surgeon
Place of Work: St. Barnabas Hospital in the Bronx, New York
Date of Death: April 8, 2020
Dr. J. Ronald Verrier, a surgeon at St. Barnabas Hospital in the Bronx, spent the final weeks of his audacious, unfinished life tending to a torrent of patients inflicted with COVID-19. He died April 8 at Mount Sinai South Nassau Hospital in Oceanside, New York, at age 59, after falling ill from the novel coronavirus.
Verrier led the charge even as the financially strapped St. Barnabas Hospital struggled to find masks and gowns to protect its workers — many nurses continue to make cloth masks — and makeshift morgues in the parking lot held patients who had died.
“He did a good work,” said Jeannine Sherwood, a nurse manager at St. Barnabas Hospital who worked closely with Verrier.
“He can rest.”
Read more here.
— Sarah Varney, Kaiser Health News | Published April 15, 2020
(Return to top.)
America’s First ER Doctor To Die In The Heat Of COVID-19 Battle
(Courtesy of Debra Vasalech Lyons)
Frank Gabrin
Age: 60
Occupation: Doctor
Places of Work: St. John’s Episcopal in Queens, New York, and East Orange General in New Jersey
Date of Death: March 26, 2020
At about 5 a.m. on March 19, a New York City ER physician named Frank Gabrin texted a friend about his concerns over the lack of medical supplies at hospitals.
“It’s busy ― everyone wants a COVID test that I do not have to give them,” he wrote in the message to Eddy Soffer. “So they are angry and disappointed.”
Worse, though, was the limited availability of personal protective equipment (PPE) — the masks and gloves that help keep health care workers from getting sick and spreading the virus to others. Gabrin said he had no choice but to don the same mask for several shifts, against Food and Drug Administration guidelines.
“Don’t have any PPE that has not been used,” he wrote. “No N95 masks ― my own goggles — my own face shield,” he added, referring to the N95 respirators considered among the best lines of defense.
Less than two weeks later, Gabrin became the first ER doctor in the U.S. known to have died as a result of the COVID-19 pandemic, according to the American College of Emergency Physicians.
Read more here.
— Alastair Gee, The Guardian | Published April 10, 2020
(Return to top.)
This story is part of “Lost on the Frontline,” an ongoing project from The Guardian and Kaiser Health News that aims to document the lives of health care workers in the U.S. who die from COVID-19, and to investigate why so many are victims of the disease. If you have a colleague or loved one we should include, please share their story.
Lost On The Frontline published first on https://nootropicspowdersupplier.tumblr.com/
0 notes