#uterus with adenomyosis treatment
Explore tagged Tumblr posts
Text
Why the Right Gynecologist Surgeon is a Must for Your Gynecology Treatment?
#best gynecologist surgeon in Delhi#uterus with adenomyosis treatment#laparoscopic surgery in Delhi#Sunrise Hospital
0 notes
Text
thinking about my follow-up appointment with my gyn after i had an ovarian cyst removed. she told me that i had adenomyosis, and that she could tell based on the appearance of my uterus
she showed me the photo from the surgery and said "do you see how your uterus is red and swollen?"
doctor this is the first photograph of a uterus i've ever seen in my life
#what's that xkcd comic about how physicists forgot that the average person only know about green midochlorians or whatever the fuck#dr i've never ever seen a diagram that depicts what the uterus looks like from the side. i only have a guess as to how big it even is#goddddd i never know what tags to use for anything#adenomyosis#big uterus energy#how's that#i've got a sticker on my bong that says that. i know it's meant to be a weird feminist statement#but my little joke is that i simply have a large uterus#adenomyosis is funny bc you look up treatment for it and it's literally just 1. ibuprofen 2. hysterectomy#someday......... 🥰#<- daydreaming about surgically altering his sex
1 note
·
View note
Text
एडेनोमायोसिस तब होता है जब ऊतक जो सामान्य रूप से गर्भाशय को रेखाबद्ध करता है (एंडोमेट्रियल ऊतक) गर्भाशय की मांसपेशियों की दीवार में बढ़ता है। प्रत्येक मासिक धर्म चक्र के दौरान विस्थापित ऊतक सामान्य रूप से कार्य करना जारी रखता है - मोटा होना, टूटना ��र रक्तस्राव। डॉक्टर निश्चित नहीं हैं कि एडिनोमायोसिस का कारण क्या है, लेकिन यह बीमारी आमतौर पर रजोनिवृत्ति के बाद ठीक हो जाती है।
#adenomyosis in hindi#adenomyosis meaning in hindi#adenomyosis uterus in hindi#एडिनोमायोसिस का इलाज#what is adenomyosis in hindi#adenomyosis treatment in hindi#एडिनोमायोसिस#adenomyosis symptoms in hindi#Gaudium#Gaudium IVF
0 notes
Text
Oscar Isaac Boys with Period, Endo and PCOS Reader HCs

Pairing: Multiple Oscar Isaac characters (Steven Grant, Marc Spector, Jake Lockley, Abel Morales, Nathan Bateman, Cecil Dennis, Laurent LeClaire, Basil Stitt, Santiago Garcia, Anselm Vogelweide) x AFAB reader Word count: 2.2K Dividers by: @saradika-graphics Warnings: Periods, endometriosis, chronic pain, PCOS, non-specified shitty medical experiences, pretty much all fluff though douchebag Laurent mention sorry. No pronouns or body descriptions are used for reader. A/N: I hope you all enjoy this! It's just fluffy blainrot because the endo/post-lap hasn't been great. Reblogs and comments are encouraged and appreciated! 🫶 Tagging: @my-secret-shame-but-fanfiction

Steven Grant

Steven researches endometriosis, PCOS, adenomyosis and period pains. He learns about all of the different types of treatment plans. He learns about dietary changes that can help with inflammation and that other people diagnosed with these conditions have said have helped him. He goes down a rabbit hole of different PCOS recipes and dietary lifestyles, Steven ends up knowing of more PCOS blogs on every platform than you do by the end of that fixation.
He’s so sweet, there’s been many days where you’ve come home at the end of the day and been greeted with an endearing “Love, I found this new recipe, I thought we could try it for dinner? It has the PCOS and the vegan stamps of approval!”
Steven is also a great listener, it’s easy to tell him about how long it took to get a diagnosis, how much doctors don’t seem to care and are keen to dismiss you, to tell you birth control is your only pain management option or that you’re anxious and it’s all in your head. He’s horrified by this, he never judges or condescends and talking to him is always validating.
During your periods, he’ll happily cuddle up with you and attentively watch all your comfort shows and films, especially the guilty pleasure ones. He loves it. Steven finds good books and podcasts for you on the days of your period when you just want to stay in bed. He’ll read to you as a distraction, you find it cute, especially when it’s a mythology or historical book, his passion and excitement drips through more when he reads those books to you. He’s a sweetheart that’s always there for you.
Abel Morales

Abel will have every appointment of yours in his calendar, written in pen, he attends with you for support and as an extra voice to advocate on your behalf. Which he absolutely does. He has no issue speaking up if doctors are ever dismissive, especially when you’re met with a cold one. He’s spent his whole life trying to be taken seriously and to perfect his image. He knows how to use his eloquent words and charming people skills to get a doctor to do their job better and for you to have better healthcare. You both know that having him, a man in the room, makes it much easier for you and your pain to be taken seriously.
In the evenings during flare ups, Abel sits in bed and quietly holds you. He’ll press gentle and loving kisses to your forehead and the top of your head and rub your back in slow circles while you nap or are curled up on him in pain. He hates seeing you in pain but he knows being there is important for you and it’s also important for him as a partner. It never gets easier for him to see you in pain though but Abel will never complain about getting to spend more time cuddling you so tightly.
Nathan Bateman

When you first start dating you tell him you have endometriosis, it’s something that’ll come up eventually for any relationship that goes anywhere, even a casual one. You think it’s better to rip the band-aid off sooner than later. Nathan takes it in casually, like you’ve just told him what your favourite condiment is. It surprises you to say the least.
Nathan spends the next day scouring through numerous medical journals in order to become a human encyclopaedia on endometriosis and everything relating to the uterus and other reproductive conditions. If you’ve been medically cleared safe for a TENS machine, he doesn’t even spend a full afternoon building you one and it is the best one you’ve ever used, it becomes a regular essential in your pain management kit.
The highest ranking and most expensive medical practitioners in the field are flown out to the compound for every symptom and condition. The top pelvic physiotherapists come out, the gynaecologists. You want a dietician to try a diet to help with inflammation and bloating? They’re already on a helicopter. You want to try acupuncture? Again, they’re already on a helicopter. A massage therapist? Again, they’re already on a helicopter to the compound before you can even finish that request. There’s a room in the compound that he had modelled for you and these appointments to essentially be the fanciest hospital room you’ve ever been in. Nathan has no issue throwing money and technological innovations at any issues your uterus might give you, it’s a way of showing he cares, he’s arrogant and he can be infuriating but he loves you and will use his brain and bank account to prove it.
Jake Lockley

Whenever you have a negative experience with a doctor he happily offers to go down and take out that practitioner, sometimes he’ll make a scalpel joke even though he prefers a gun as a weapon. You’re not always sure if he’sjoking or not… Maybe it’s better to not know, plausible deniability and all.
He absolutely pampers you, every time you have a period, whenever there’s a cramp. Jake pampers you like you’re the most precious thing in the world, which is what you are to him. He makes you hot tea, soups, runs baths, puts on your favourite and comfort films. Jake offers to do things like brushing your hair for you and loves it. Jake pampers you! PAMPERS YOU!
Laurent LeClaire

Don’t. Just don’t. Sure, he’d be cute the first time you had your period and he’d happily offer period sex as a method of relief. But after the second period or flareup he’d attempt to gaslight you and say your symptoms or your pain being psychological. Then Jake Lockley would find a way to teach him a lesson.
Santiago Garcia

Santi’s long career has made him a master in observation and strategy, Santiago seemed to have a better understanding of your body than any period tracking app you’d tried to use, and not in a Tom Wamsgams baby-trap kind of way. More of a he was better at recognising the patterns, symptoms and remembering details than you were. Especially when the pain gave you brain fog. He picks up on the slightest details and after the first couple of months of dating you, he had a fine eye for pain. Whenever he spots the start of a flare up or painful period he goes straight into that mode, he checks in with you about pain meds, he gets heating pads ready for you and cuddles up with you on the couch or in bed while you curl yourself around one, runs baths and showers.
He has a plan in place for everything; when pain or a symptom is at a dreaded emergency department trip, when pain is flaring up. There’s a plan made for each appointment with symptoms that have been flaring up, objectives of what to get out of the appointment. Santiago learns what your boundaries and limits are, he’s big on pacing with you and not pushing yourself to do more than what you can handle or what will push you too far and lead to following pain days. He really encourages this for you, something he doesn’t do so well for himself and his knees.
Whenever Santi tags along with you to an appointment he’s great at asking follow up questions, especially if a doctor is being a dick. Sometimes it can feel overwhelming when you’re in appointments, especially when a doctor is talking, it’s easy to forget what’s been said as soon as you get home. Santiago always remembers every word that’s been said if you ever forget or want to double check. He’s an extremely practical partner and strong support.
Basil Stitt

Basil will have a panic attack, he’ll quickly google ‘period symptoms’, he doesn’t remember if people get cravings on their periods too or if that’s just pregnancy, or is it neither? Just something else he’s thinking of? No, he’s overthinking it.
During said panic attack, Basil will then do an uber eats order with several different types of chocolate and he’ll run to the kitchen to see what teas he has as Google mentioned peppermint tea several times. After checking the kitchen and making a mess in the cupboard and on the countertop during his search, he’ll order another box of it anyway just to be safe. Basil also is the guy who orders three different boxes of pads and tampons because he’s not sure what you prefer and he wants you to have options. Insert ‘What’s your pussy size, babe?’ meme, that’s Basil.
All anxiety evaporates from his body when you just want to cuddle on the couch with him, watch some weird movies and order pizza and drink tea. He smiles and completely lights up when you tell him you like the flavour of the chocolate he ordered.
Going forward there’s a cupboard under the basin in his bathroom filled with various boxes of pads, tampons, and he eventually gets to the stage where he confidently has your period orders down and preferences of products. He’s quietly but goofily proud of the fact that he now knows your pussy size.
Anselm Vogelweide

Anselm completely understands chronic pain from his own lived experience. You never have to apologise for a bad pain day, cancelling plans because your uterus is trying to kill you, when you need to spend all day in bed or in the bath to try and relieve pain and bloating. He completely gets that, he makes sure you have the softest and freshest pillows and blankets, bubbles, epsom salts, bath bombs etc. Whatever you could wish for to make you more comfortable. You no longer feel guilty for the things you used to before relating to having a chronic illness and terrible periods. You’re understood, seen but also pampered beyond what’s comprehensible.
Anselm immediately finds a team of the best professionals, new studies and treatments, both conventional and experimental, are quickly and quietly funded and greenlit. He offers you a world of treatment options you’d never considered or knew existed. Anselm always has his estate stocked with pain medication, all the drugs, drugs you’ve never heard of, drugs a normal prescription definitely wouldn’t get you. There’s medications and all the different options of treatment and pain management you could imagine available at the estate, hydrotherapy pools, massage chairs, massage therapists, sensory relaxation rooms, saunas, staff are there to cook all your favourite and comfort meals. Are you in pain and sad and needing cuddles with animals? Don’t worry, Anselm has a room being turned into a barn and a third cousin twice removed bringing a petting zoo over for any cuteness needs you might have. They should be there in five minutes.
And if there somehow isn’t something there that you want, don’t worry, you just need to ask if he doesn’t read your mind first and then it’ll be moments away because Anselm can afford anything and everything and he always knows a guy.
Marc Spector

Marc knew periods weren’t a walk in the park and were uncomfortable but it wasn’t until dating you and being around somebody with endometriosis and chronic physical pain did he realise how bad it could be.
The first time you had an endo flare up, it had really woken him up to that reality. He couldn’t help but grimace at seeing how you transformed from your usual self to being hurled over in pain. It freaked him out and his mind had panicked over the thought of this being your reality multiple times a year. It never gets easier for him to see you in pain or discomfort but he starts to find it easier to respond and be more present during flare ups.
He’s extremely observant, especially when it comes to you. He quickly learns how your facial expressions shift when you have a migraine, he closes all the curtains and turns the lights off. When you curl over on yourself in pain he’s there with a heat pad within minutes. When you screw your face up and say you’re nauseous he’s immediately there with a bucket on the side of the bed. During one of your worst flares when you’d been throwing up, he hadn’t even complained once. He’d helped you feel clean afterwards, there were no comments that made you feel bad and he cleaned the bucket out so it wasn’t something you’d have to worry about. Marc found it much easier to show up and do these acts than to be the verbally reassuring type, he shows up and these acts of service and care make you feel supported, loved and cared for.
Cecil Dennis

“Babe, do you wanna get high?”
“I read about cannabis and chronic pain, there’s honestly so many articles on the internet about it.”
Gets just as upset as you do when you're in pain, quite possibly cries more than you do whenever a flare up is happening. He'll watch films with you and he buys a CBD ointment and offers to rub it on your abdomen while you’re cuddled up in bed.
I’ll stop there, I’m sorry.
#steven grant#steven grant x reader#marc spector#marc spector x reader#jake lockley#jake lockley x reader#moon knight fic#moon boys#nathan bateman#nathan bateman x reader#santiago garcia#santiago garcia x reader#abel morales#abel morales x reader#anselm vogelweide#anselm vogelweide x reader#basil stitt#basil stitt x reader#cecil dennis#cecil dennis x reader#oscar isaac#oscar isaac characters#x reader#endometriosis reader#pcos reader#period fic#laurent leclaire x reader#chronic pain#chronic pain reader#oscar isaac fanfic
200 notes
·
View notes
Text
It's endometriosis awareness month! Here's some general knowledge on my condition, as misinformation is constantly spread about it.
Endometriosis is a disease affecting 1 in 10 people with uteruses. A tissue similar to the endometrial lining, of period blood, grows and sheds on the outside of the uterus. As the menstrual cycle comes, the blood has nowhere to go. This causes intense pain and irritation to surrounding organs. It is one of the most painful diseases recorded.
Endometriosis was first discovered in 1860, though it was recognized in the Hippocratic Corpus around 4,000 years ago. Treatments have varied through the years, starting out with bloodletting, leeches, hanging upside down, exorcisms, genital mutilation, and chemical douches. During the Middle ages, the perception of chronic pelvic pain shifted from a recognized condition to something caused by hysteria, promiscuity, or it was made up. In the hayday of Hippocratic practice, Endometriosis was more common than it is today, likely due to the inaccessibility of diagnosis compared to 4,000 years ago. Somehow.
Today, treatments include birth control, surgery, hysterectomy, and pain relief. There is no cure.
It takes an average of 7-12 years for someone to receive a diagnosis.
Anyone can get endometriosis, including cis men
A hysterectomy is not a cure, as endometriosis will continue to grow and spread to other organs
The pain one experiences due to endometriosis does not correlate with staging. Staging reveals how extensive endometriosis lesions are, not pain. Someone with stage 1 could experience excruciating pain, while someone with stage 4 and frozen pelvis can experience no pain.
Endometriosis lesions are not endometrial lining. The tissue is similar, but not the same. Thus, no one actually knows what endometriosis actually is.
It is only diagnosable through laparoscopic surgery. It can be detected via imaging such as ultrasound or MRI, but more often than not, it isn't seen. You can have completely clear tests up until your surgery and still have even the higher stages of Endo (like me!) (this one was for all you undiagnosed people, you're not crazy!)
Endometriosis is comorbid with many things, including pelvic floor dysfunction, adenomyosis, vulvodynia, uterine cancer and fibroids, ovarian cancer, many autoimmune and inflammatory conditions (rheumatoid arthritis, MS, IBD), and cardiovascular disease.
I've provided links in each point and I deeply encourage you to read my sources, whether you have endo or not. Not enough people understand endometriosis so a lot of us who deal with it don't get grace or compassion, be it in our work lives, relationships, friendships, or family. People with endo, happy endometriosis awareness month.
#endometriosis#endo#endometriosis awareness#chronic illness#disability#cripple punk#chronic pain#chronically ill#disability awareness#cpunk#endometriosis awareness month
80 notes
·
View notes
Text
Hi I'd like to take back every nice thing I said about my surgeon.
This is a venty and /lengthy/ post about my experience with an accelerated emergency hysterectomy (<2wks from diagnosis to surgery). I'm adding a cut in case medical stuff is triggering for anyone or if you're like "I've heard enough outta you about doctors" (understandable).
I'm struggling to sleep rn in a hospital room so I'm venting to distract while I wait for my nurse to check in with me about more morphine.
So my gyn and my surgeon are the same person, an OBGYN in San Francisco. He was the only would who could see me after multiple ER and 2 urgent care visits for severe pain in my abdomen. Eventually the ER orders an ultrasound. a surprise vaginal ultrasound that I was not informed would involve insertion of the wand into my vagina until the tech told me to take off my underwear. They had told me it would be a stomach ultrasound to look for masses. I'm still... unhappy about this. It hurt and the tech was like "all women get these its fine". Anyway, I had one moderately large fibroid and possibly scar tissue and smaller masses.
Sidenote: I'm not sure if i have ever felt being viewed as less than human more in the ER. Downplaying my symptoms, telling me the ER doesn't dispense pain medication (which they later did multiple times), that fibroids don't cause any pain, accusations of drug-seeking, and multiple insinuations that I was pregnant or otherwise lying. One such accusation was a question posed to my partner about if we ever had threesomes with men or if maybe I cheated on them and contracted pregnancy or STD. Oh and when I got diagnosed they didn't say "it's fibroids" they said "there's at least one tumor in your uterus" like ! Why would they say it like that?? Every nurse was pissed to be there and I strongly believed one of them hard painful pricked me in my wrist instead of my elbow because they were annoying I was sobbing in the room outside the nurses lounge. When my partner confronted them about that choice they were like "well we can remove it but you won't get fluids or meds then". It hurt for 2 days afterwards. I had been to urgent care and the er previous to this and had no issues with the inner elbow.
I called gynos all over the place but no one else except this doctor, lets say... Dr Yan, could see me within 3 weeks. My PCP refused to provide pain management and I had been out of work for a week and half, returning to the ER multiple times because I was screaming in pain for hours. The ER would prescribe a small amount of prescription pain killers, I would try to make them stretch, and then I would have to return to the ER. I was bedridden from pain. Planned Parenthood couldn't help with treatment but told me based on the ER imaging I might have adenomyosis, for which the only "cure" would be to remove my uterus, removing just fibroid is much more difficult with adenomyosis.
So I was desperate and Dr Yan was willing to do a hysterectomy as well as willing to push my insurance company to get it done fast as I was pulling no income - I ran out of PTO after a week of calling out. I felt I needed it fast and it started to hurt more whenever I ate or drank. He somehow got it moved to yesterday.
But he was awful. He wouldn't give specific answers to my questions, he barely walked me through what the procedure entailed after my partner pressed harder, and kept saying it is a very common procedure that is easy and not painful.
He lied to me, saying I'd be home the same day and a nerve blocker administered during surgery would keep me numb for two days. The recovery nurse told me that's not true. He insisted that pain would be minimal and his patients were fine with otc pain management. He said it needed to be abdominal, which I have since learned is not the case and is the most painful and longest recovery time for hysterectomy
The only thing he reiterated and talked about was how I would be unable to get pregnant, which was the only thing I *already* knew.
He did one physical exam during initial appt which was pushing on my abdomen, ordered no additional imaging or appts, and literally disappeared into another room while my back was turned signing forms. I had to sit in the waiting room for another 20 minutes to get him to sign insurance and leave of work papers.
He was 20 min late to my pre-op appt and his office had no idea why. he performed a pelvis exam on me, externally and then inserted his fingers into my vagina for an internal exam without telling me. I had never had a pelvic exam before. It hurt enough bc he did not use lubrication. My partner confronted him angrily and he said he knows what he's doing and the exam was over anyway. He told me again the surgery would be simple.
I woke up screaming in observation, where i was given Tylenol. The surgical nurse lied to me and said they had already called my partner. After an hour of pain they moved me to a recovery room, where I had access to my phone and called my partner, who had not been contacted and rushed over. I was alone and crying out in pain.
The nurse told me that they could only give me Tylenol because Dr Yan had left the hospital without putting in orders for me aka authorizing use of moderate to severe controlled painkillers. They said as soon as they could get him on the phone they could give me something for the pain because I had been given 4 grams of Tylenol and couldn't have more. Dr Yan never answered the phone.
I am not joking when I say this next part, because I was able to track the time through my chart just now to get exact numbers and times. I came out of surgery no later than 800am. In a recovery room by 9. I screamed, absolutely not an exaggeration, I was crying out and sobbing and could not think, I was sweating and my entire body was shaking. I was dry heaving and spitting up bile, which made the pain worse. I don't remember anything except the pain, although apparently i did say some funny things to my partner coming down from the general anesthesia (thought we were in grocery outlet).
At 2:14 the hospitalist gave up calling and admitted me, transferring care away from Dr Yan. At 4:45pm they administered a very lose dose of morphine, and I finally stopped screaming. It was still very painful, and my partner timed me - I would sleep for 1-7 minutes, then wake up crying out in pain for 3-10min, repeat. The nurse told me I would receive stronger pain management when I had a room.
At 430pm they transfered me to my room, which involved the transport guy hitting my bed against the counter. The transfer from bed to bed was so jolting I started screaming again, which lasted until 445pm, when they administered triple the dose of morphine given earlier.
This has been the most painful experience of my life. The Dr said no more morphine and would administer those opiate pills cut w ibuprofen or whatever. They would give me just enough to cut my pain back from 10 to 6/7, then make me wait until 10, then make me wait crying out in pain while they got the dr to put in an order for more. It was like reps of a gym set except the absolute worst pain based version.
Around 6pm, my partner advocated aggressively as my pain was only receding to a 8 or 9 and I could no longer nap or drink water due to the pain. My muscles were so clenched I tore my paper gown. The nurse (who had seen all of this go down and was b attentive) recommended to the dr that I receive straight oxycodeine via IV. My doctor, who saw me once when i was transfered which consisted of introducing himself, said I didn't need such a strong medicine and I should take tramadol instead.
The tramadol had almost no effect, and I was then told I couldn't have the oxy because I had gotten the tramadol instead. By 630 I was at a 10 and screaming again. The dr ordered a lidocaine patch (no effect).
At 655 a new dr replaced the previous and immediately ordered dilaudid. My pain finally dropped to a 5.
At 830pm guess who fuckin shows up in my room. Dr Yan, who's like "you don't seem in pain" SIR I HAD SO MANY DRUGS INSIDE ME AND I WSS STILL AT A 5. And I needed two people to get me to the bathroom (5 ft away). He shows me a picture of the biggest mass, says I'm fine, offers no explanation for why he fucked me over so badly, and leaves. I should have demanded information but my throat hurt from crying and screaming and I had only slept 2 hrs in the previous 2 days.
The recovery nurse apologized profusely to me and said she believed he had been grossly negligent. The anaesthesiologist came and told me my body eats painkillers and anesthesia with a strong natural tolerance, and that some of the refusal to give more or stronger dosages was probably because doctors basically read charts, and would see that I had been administered a lot already. They would then decide that was enough based on what they believed to be averagely appropriate. Even tho I have it documented from his hospice ICU care notes that my dad had a similar tolerance. The recovery nurse agreed as she had been observing me, administering the meds, and see my-clearly-caused -by -pain symptoms continue.
The night nurses and doctors have been better. I got some more morphine just now, and a sleep aid that didn't work but I appreciate they tried to address that issue.
Anyway jeez if you read everything you deserve a medal. My memory has been very poor due to drugs and pain so I've been trying to work out a timeline of what happened. I know it's kind of a baby thing because no one attacked me and I don't seem to have surgical complications and after all this the hospital is sending me home with opiates, but I feel kinda shell shocked. It felt crazy to be lying in the hospital screaming in pain for hours and hours just for someone to come in every hour and say their hands were tied even tho the hospital is the only place for strong pain relief that isnt like, street fet. I removed an organ, I knew it would hurt, but I've never in my life experienced anything like that. It was worse than all other pain I've had combined. I thought i was going to die.
Anyway the nurse is giving me Ativan! I hope to rest now. Cross your fingers for me and stay away from DR YUAN DA FAN OBGYN SUTTER HEALTH SAN FRANCISCO.
#tw medical... trauma?#i feel guiltu calling it trauma#hysterectomy#cos ppl have had such severe medical trauma and im... mostly ok now#with the morphine im at 3#lowest ive been since this started
20 notes
·
View notes
Text
I heard back from my doctor and whoo boy
The ultrasound shows I have a small fibroid and possible adenomyosis which means one of the treatment options is off the table. She wants me to get an endometrial biopsy to make sure there's nothing more sinister in my uterus. I had one done 15 years ago. It was suggested by my (at the time) new doctor 5 minutes before it was done without any pain management or sedatives. It hurt so bad I nearly kicked him. So my new doctor said I can take ibuprofen and she will give me Xanax, but I told her I can't take ibuprofen so what should I take and btw I've had vicodin for cramps before so can we try that and skip Xanax? We will see what she says. I also informed her I've already had two panic attacks since she first mentioned getting this biopsy done again.
Her message also said my options are birth control pills, a particular IUD, or hysterectomy. I responded that I will under no circumstances get an IUD. I asked how the birth control will be different from the ones I was already bleeding through and how long do I have to try them before it's clear they aren't working. We will see what she says. I know a hysterectomy is a major surgery, but I am also so sick of this. I'm so tired of hormone pills making things worse.
#about me#medical stuff#obgyn#endometrial biopsy#pcos#fibroids#adenomyosis#endometrial abaltion#hysterectomy#birth control#iud
20 notes
·
View notes
Text
A letter to my Gynecologist:
Thank you.
Thank you for listening to me, when so many others in your profession wouldn't.
Thank you for not writing my endometriosis and adenomyosis symptoms off as hysterical, or a non-existent brain tumour.
Thank you for working with me on alternate treatments outside of just pharmaceuticals to find our best possible options.
Thank you for removing my uterus, and problem ovary without putting my future husband and children above my own quality of life.
Thank you for giving me my life back.
Thank you for working with me for my treatment, and not assuming you know my body better than I do because of your degree.
Thank you for seeing me as a human being needing aid, rather than as just a paycheck.
Thank you for fighting for women's health.
Thank you for your passion in your field and pushing for more awareness, and better treatment options.
Thank you for specialising in this debilitating disease and excelling at helping your patients.
You saved my life more than just physically. I will forever be grateful for your care. I have the utmost respect for you, and hope more in the medical field will learn to follow their oath the way you do.
You are phenomenal.
2 notes
·
View notes
Note
About the diseases’ game Molly Weasley or McGonagall
Molly has had 7 children, so she has an increased risk for some gynecologic complications. Endocervical polyps and Adenomyosis are common.
Endocervical polyps are benign and present with painless vaginal bleeding. No change in uterus shape. Adenomyosis causes dysmenorrhea and heavy menstraul bleeding because there are endometrial glandular tissue within the myometrium. When palpating the uterus, it will feel diffusely large (unlike fibroids where you will feel a bulky, irregularly shaped uterus).
Any post-menopausal bleeding is concerning for endometrial cancer. Transvaginal US can help diagnose this (>4mm in size) and endometrial biopsy is diagnositic.
McGonagall will be my screening guidelines patient. (In America, she gets her treatment in America, I don't know Britain's guideliens)
Starting at 21 she will get pap smears every 3 years (this has changed depending on who you ask, but boards says 3 years.) After 29, she can get them every 5 years with HPV cotesting. At 65, she can stop getting them done as long as her last 3 alone pap smears have been normal or her last 2 co-tests were normal.
At 50 she will get her first colonoscopy unless she has family with colon cancer, then she would get it done 10 years before they were diagnosed (45 year old diagnosed, you get it done at 35) or age 40, whatever comes first. If normal, she can repeat it every 10 years.
At 50 she also starts getting mammograms every 2 years until she is 74.
At 65 she is getting a bone density scan to test for osteoporosis/osteopenia
6 notes
·
View notes
Note
hi hello ms pillarsalt would you mind sharing what kind of iud you have? i have adenomyosis and my cycle pain has been getting progressively worse but i am terrified of hormonal birth control bc all the pill type ones i was on as a teen gave me horrible stomach trouble like to the point we thought i had Crohn's disease. but im also scared of the copper one bc my body has rejected metal b4. basically if u have a hormonal iud can you comfort me that it wont make me constantly sick bc i would like to stop passing out from pain at work and nobody seems to want to discuss this type of treatment yk
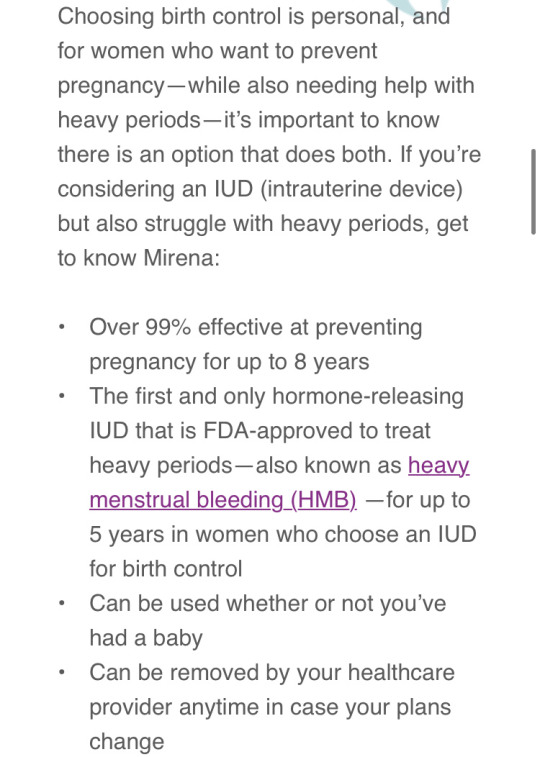
I'm sorry to hear you're going through this, it sounds terrible. As I'm sure you already know, I'm not a doctor and I can't tell you if getting a hormonal IUD will help alleviate your adenomyosis. I can tell you my experience with it, though. I have a Mirena IUD which is hormonal. Here is a screenshot from their website about the effectivity:
So right away I can tell you that before I had it installed nearly five years ago, my periods were heavy as hell. The cramps sucked of course, but the main issue was how much I would bleed and bleed. I would go through probably seven or eight superplus (heaviest) tampons a day and even have to wear a pad at the same time so I could get through a class without bleeding through my pants. I got it installed (usually they schedule it for when you're on your period so your cervix is softer), had a period for about a month afterward, and then my periods became so light that I didn't even have to buy menstrual products anymore. Basically there was a small amount of discoloured discharge that would signal that I was menstruating, with some very light cramps akin to when you ovulate. Now my periods are getting heavier again because I need to get it replaced soon, but apparently the pregnancy prevention aspect is still good for a couple years so it's not as much of an emergency as I thought (gotta find a doctor soon lmao).
I haven't had really any side effects that I could tell you about. I've had issues with mental illness since I was about 13 but they didn't get any worse with the installation of my IUD. Actually I'm doing better than I ever have in my adult life in that aspect. I haven't had any digestive issues like the stomach pain you mentioned, no weight gain or weight loss. My skin is clear almost all the time and I generally feel physically well.
Now, will it help with your adenomyosis? I think it's really worth talking to your doctor about. The hormonal medication in the device, Levonorgestrel, thins the endometrium, which is why I bled far less during my period while on it. The endometrium that builds up in the muscular tissue of your uterus and causes you pain may be lessened in the same way. This part of the website that states why some people can't use it concerns me:

Because 1. I don't know if or how much your adenomyosis changes the shape of your uterus and 2. if your stomach trouble was an allergy to the medication itself then you'll likely have the same problem here. Basically, you've got to find a doctor who will listen to you and talk this and other options out with you, because it's inhumane to let you keep suffering this way.
Good luck to you, I really hope you can find a solution. I know getting this sort of stuff figured out is daunting and feels impossible sometimes but don't give up. Do your best to find a women's health clinic or at least a female doctor. It's going to be okay!
9 notes
·
View notes
Text
So I've mentioned before that I found out in May that I'll probably need a hysterectomy because of medical issues that have been dismissed and ignored over the past three decades due to a combination of religious overreach in the society of my birth, and patriarchal bullshit in general. In particular, people who would have been willing to ignore the Catholic aspect still didn't want me treated medically by giving me contraceptives, because that might have made me fat. Guess what? I am fat! And it's not because of my Mirena IUD; if it's related at all, it's because my endometrium ran out of space to colonise my uterus and my abdomen and just fucking metastasized throughout my body in a way that has literally made me fucking hysterical in the original sense of the word, AND IT COULD ALL HAVE BEEN AVOIDED IF WOMEN WERE JUST TREATED LIKE PEOPLE INSTEAD OF LIKE INCUBATORS.
Here's a quote from the Dublin diocese statement on child safeguarding:
"Harm refers to assault, ill-treatment, sexual abuse or neglect of a child."
I understand that childhood sexual assault should be the priority. That's why I stayed silent for so long. I could see efforts were being made to improve. But after the documentary I saw this summer on what Eamon Casey was permitted to do AFTER he had been "censured", I knew they weren't doing enough.
I genuinely don't know and don't care if what I'm experiencing is objectively real, or only subjectively real. I'm not insisting that women be ordained as priests. We don't have to be the same as men; but we have to be people. You can't leave us in cages and claim it's for our own good any more.
I keep being asked if I was sexually assaulted, and to my knowledge, the answer is no. But Catholicism has done untold harm to my finite self, and my husband has saved me when Catholicism wouldn't even listen to me try to tell them I was drowning.
I am scheduled for exploratory surgery in the next few months. I fully expect to wake up without a uterus. I'm going to tell the surgeon to feel free to take my ovaries too if it seems like the best course of action. And then I'm going to sit down with a fucking endocrinologist, and discuss what kind of HRT will work best FOR ME. I don't want to be a man, but I am done with listening to anyone else's definition of what makes me a woman. My husband loves my body as it is, but he says it's MY BODY and he wants me to look after it in a way that works for me. I don't want to turn into a man, but I have spent thirty years being tortured because the Roman Catholic Church insisted I would definitely want to be a mother someday - AND I DO, but because of their ignorant biased self-serving mealy-mouthed pharisaic morality, not only is it biologically impossible, but my mental health is fucked up enough that I'm not even sure they should give us kids to foster. The same week I found out about my suspected adenomyosis, I also received a letter from the NHS requesting that I come in to be assessed. A few weeks previously, I had finally confessed to a priest of my acquaintance that I was definitely mentally ill, but I was becoming increasingly convinced that I was also a prophet. The series of inexplicable deaths that had shaped my life seemed to be herding me into making that statement, and whatever fucking idiot forgot to delete the "psychosis" header from my assessment questionnaire was the final nail in the coffin of me having an ordinary life. I'm so sorry if what I'm going through has made your own life harder; but I have already given up so much of my life for false promises that the people who lied to me probably believed. Even if I'm crazy too, I'm not wrong.
31K notes
·
View notes
Text
Menorrhagia: Heavy Menstrual Bleeding Explained
Menorrhagia, often referred to as heavy menstrual bleeding, is a condition where a woman experiences abnormally heavy or prolonged menstrual periods. This condition is not just a minor inconvenience—it can have significant effects on daily life and overall well-being, leading to discomfort, fatigue, and in some cases, anemia (a shortage of red blood cells caused by excessive blood loss). Menorrhagia: Heavy Menstrual Bleeding- Medical & Health

What Is Menorrhagia?
Menorrhagia is characterized by menstrual bleeding that lasts longer than seven days or requires the use of sanitary products (like pads or tampons) more frequently than every hour for an extended period. Some women may pass large blood clots or experience severe cramping during their periods. The condition can occur intermittently or be persistent, disrupting daily routines, work, and social life.
While the amount of bleeding varies from person to person, the key diagnostic factor is the volume of blood lost. If the bleeding is heavy enough to cause fatigue or anemia, it can indicate a medical condition that needs attention. Menorrhagia: Heavy Menstrual Bleeding- Medical & Health
Causes of Menorrhagia
Several factors can contribute to menorrhagia, and in many cases, the exact cause remains unidentified. Some common causes include:
Hormonal Imbalances: An imbalance in estrogen and progesterone can cause the lining of the uterus to grow thicker than normal, leading to heavier bleeding when it sheds.
Uterine Fibroids: Non-cancerous growths in the uterus can interfere with normal menstrual flow and cause excessive bleeding.
Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, leading to painful periods and heavy bleeding.
Adenomyosis: A condition where the tissue lining the uterus grows into the muscle wall of the uterus, leading to heavy, painful periods.
Pelvic Inflammatory Disease (PID): An infection of the reproductive organs can cause abnormal bleeding and other symptoms.
Medications: Certain medications, such as blood thinners or intrauterine devices (IUDs), can increase bleeding.
Blood Disorders: Conditions that affect blood clotting, such as von Willebrand disease, can cause abnormal bleeding patterns.
Symptoms of Menorrhagia
Women with menorrhagia may experience a range of symptoms that can vary in severity, including:
Soaking through pads or tampons every hour or needing to change products frequently during the night.
Menstrual periods that last longer than a week.
Passing large blood clots (larger than a quarter).
Severe cramping or pelvic pain.
Fatigue, weakness, or anemia due to excessive blood loss.
Difficulty participating in normal activities because of heavy bleeding.
Diagnosis of Menorrhagia
If you experience symptoms of menorrhagia, it's essential to consult a healthcare provider. Diagnosis typically involves a thorough medical history, physical exam, and sometimes additional tests, such as:
Blood Tests: To check for anemia or blood clotting disorders.
Ultrasound: To check for uterine fibroids or other structural problems in the uterus.
Endometrial Biopsy: To check for abnormal tissue growth in the lining of the uterus.
Hysteroscopy: A procedure where a doctor inserts a small camera into the uterus to check for abnormalities.
Treatment Options for Menorrhagia
Treatment for menorrhagia depends on the underlying cause and severity of the condition. Some common options include:
Hormonal Therapy: Birth control pills, hormonal IUDs, or hormone replacement therapy can regulate menstrual cycles and reduce the amount of bleeding.
Medications: Antifibrinolytic drugs can help reduce bleeding, while nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage pain and inflammation.
D&C (Dilation and Curettage): A procedure in which the lining of the uterus is scraped to reduce bleeding.
Endometrial Ablation: A procedure that removes or destroys the lining of the uterus to reduce or stop bleeding.
Surgery: In severe cases, a hysterectomy (removal of the uterus) may be recommended if other treatments are ineffective.
When to Seek Medical Help
While occasional heavy periods can be normal, consistently heavy bleeding or prolonged periods can be a sign of an underlying issue. If you experience symptoms like excessive blood loss, severe pain, or fatigue that interferes with your quality of life, it’s crucial to see a doctor. Early diagnosis and treatment can help prevent complications like anemia and improve overall health.
By understanding menorrhagia and seeking timely treatment, you can manage the condition effectively. If you're experiencing heavy menstrual bleeding, don't hesitate to read my in-depth article on menorrhagia for more information and guidance on managing this condition.Menorrhagia: Heavy Menstrual Bleeding- Medical & HealthHeavy Menstrual Bleeding, menorrhagia, Heavy Menstrual Bleeding treatment, Heavy Menstrual Bleeding causes, menorrhagia treatment, menorrhagia causes,https://diseases8804.blogspot.com/2023/09/menorrhagia-heavy-menstrual-bleeding.html
0 notes
Text
Looking for affordable laparoscopic surgery in Delhi? Get precise, minimally invasive treatments that reduce recovery time and surgical risks. Costs vary based on the procedure type and hospital but remain competitive while ensuring high-quality medical care.
0 notes
Text
Prolapsed Endometrioid Adenomyoma Associated with Post-Coital Bleeding by Krina Kathawadia, Sharmi Das, Ayman Aboda in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
This case reports an atypical presentation of Uterine Adenomyosis. Adenomyosis is typically a diffuse, infiltrative disease of the endometrium and myometrium, which arises as a benign non-localized neoplasm of endometrial glands, stroma, and smooth muscle that almost always remains closely intimated to the uterine wall. Very rarely is it found to extend into the uterine cavity or, as in this case, develop into an Adenomyomatous polyp that passes through the cervix and into the vagina. More typically, these features are found with uterine leiomyomata. Both conditions are most often benign and are treated definitively by surgical excision. The distinction is important given the rarity of the finding reported by this case and because of the implications of differential effect given the specific progressive clinical nature associated with each condition.
Keywords: Adenomyoma, adenomyosis, vaginal bleeding, post-coital bleeding, endometrioid adenomyoma, uterine neoplasms, endometriosis.
Case Presentation
A 42-year-old woman presented to Gynaecology Outpatients with a history of vaginal bleeding for several months, associated with an awareness of an intermittent vaginal mass. The mass could be reduced digitally and was most apparent following coughing or accessory strain. She reported a long history of heavy and irregular menstrual bleeding, often with clotting. She also experienced urinary stress incontinence.
Past obstetric history included four children, three born vaginally and one by caesarean section. She had declined cervical screening for more than five years. Inspection of the external genitalia and vulva was unremarkable. Speculum examination revealed a 3 x 3 cm mass extending into the upper vagina from the external cervical os. The mass was smooth and non-ulcerated but bled with touch. Transvaginal pelvic ultrasound demonstrated a bulky uterus with an endometrial thickness of 5.3 mm and a uniformly enlarged cervix measuring 3.4 x 3.7 x 3.9 cm. An MRI was performed that confirmed a solid-cystic mass-like structure at the level of the cervix measuring 34 x 30 x 44 mm. Myometrial distortion suggested possible fibroid change, although no large fibroids were identified. The features did not suggest a malignant change.
Differential diagnoses included prolapsed uterine myoma, cervical fibroid, or possible cervical carcinoma. After discussing immediate treatment options, a hysteroscopic examination was performed following dilatation of the cervix and curettage of the uterine cavity. Multiple small submucosal fibroids distorted the cavity. A pedunculated, polypoidal lesion arising close to the internal os was excised and was found on histopathological examination to be an endometrioid-type adenomyoma measuring 55mm in size. Endometrial cuttings showed late proliferative changes with sparse fragments of Adenomyomatous change. The patient recovered well post-operatively and has since been booked for a hysterectomy with bilateral salpingectomy.
Discussion
Uterine leiomyoma, more commonly known as fibroids, and adenomyosis are two common but distinct gynaecological conditions that may significantly impact women's health (1-3), often presenting with pain, abnormal vaginal bleeding and, more rarely, polyps (4,5). These conditions share overlapping symptoms and clinical features but are inherently different in their pathophysiology, disease progression and clinical management (6, 7, 8, 9)
Uterine leiomyomas are benign smooth muscle tumours that typically originate from the myometrium of the uterine wall. They are the most common benign pelvic tumours in women, affecting approximately 20-50% of women of reproductive age and occurring in up to 70% of women by age 50 (10). Leiomyomas can range from tiny and virtually undetectable to large masses that distort and enlarge the uterus. Symptoms vary widely, with many women being asymptomatic. However, symptoms typically include heavy and prolonged menstrual periods, abnormal bleeding between periods, pelvic pain and pressure, urinary frequency and coital discomfort. (11) Fibroids can affect reproductive health, causing infertility and abnormal pregnancy outcomes such as recurrent miscarriage and obstetric haemorrhage. (11) They may occasionally promote the growth of endometrial polyps or may present as a polypoidal or pedunculated intrauterine mass. The aetiology of leiomyomas is not entirely understood but is believed to involve an interplay of genetic, environmental and hormonal factors, particularly estrogen and progesterone (11,12).
Adenomyosis, on the other hand, occurs when endometrial tissue, which typically lines the uterus, exists within and grows into the muscular wall of the uterus (myometrium) (13, 14, 15). This condition is commonly found in middle-aged women and those with children. Although it can be asymptomatic, adenomyosis often presents with heavy or prolonged menstrual bleeding, severe menstrual cramps, and chronic pelvic pain. The exact cause of adenomyosis is unclear, but it is believed to be associated with various hormonal changes, including those induced by childbirth and menopause (5) While adenomyosis can lead to significant discomfort, it is typically not considered a risk factor for other health complications, although it may be coexistent with pelvic endometriosis (16, 17). In rare cases, adenomyosis may contribute to the formation of polyps and lead to irregular bleeding (18). Typically, they contain haemorrhagic cystic spaces, which are unusual in other polyps such as leiomyomas or malignancies (19). The characteristic sonographic features of polypoid adenomyomas include heterogeneous or homogeneous echogenicity relative to the myometrium, a smooth surface, a poorly defined margin with the underlying myometrium, haemorrhagic foci, and usually, associated adenomyosis in the myometrium (20). When ultrasound evaluation demonstrates a soft tissue mass in the vagina prolapsed from the uterine cavity with a visible connecting stalk, it is termed the broccoli sign (21,22)
Uterine leiomyomas and adenomyosis can cause abnormal vaginal bleeding, typically heavier and longer than normal menstrual bleeding. However, the bleeding associated with leiomyomas is usually due to the increased surface area of the uterine lining, while in adenomyosis, bleeding results from the disruption of the muscular wall of the uterus (23, 24). In both cases, the bleeding may be severe enough to cause anaemia and disrupt a woman's perceived quality of life (25).
Regarding management, treatment for adenomyosis and leiomyomas can range from watchful waiting to medical therapy (e.g., hormonal treatments) and surgical interventions such as minimally invasive, local resection, or hysterectomy (8,11,14). In both cases though more rarely for the latter, medical management using hormonal treatments to control or mitigate the menstrual cycle may effectively reduce provocateurs for growth, leading to regression or diminution of size and consequent reduction of symptomatic effect (8,11,14).
Conclusion
This case report presents a unique manifestation of uterine adenomyosis, typically a diffuse disease, uniquely presenting as an Adenomyomatous polyp protruding into the vagina. This rare presentation mirrors features commonly associated with uterine leiomyomata. Both adenomyosis and leiomyoma are benign gynaecological conditions causing similar symptoms, such as abnormal vaginal bleeding, but each carries distinct clinical implications. Accurate diagnosis and treatment, typically surgical excision, and ongoing effective medical management, are crucial. Knowledge of the clinical and sonographic appearance of polypoid adenomyomas may facilitate diagnosis and help distinguish these tumours from other uterine polyps. This report advocates the need for heightened clinical awareness and comprehensive differential diagnostic criteria when managing abnormal vaginal bleeding, particularly when associated with evidence of an expansive polypoidal growth.
#Adenomyoma#adenomyosis#vaginal bleeding#post-coital bleeding#endometrioid adenomyoma#uterine neoplasms#endometriosis#JCRMHS.#jcrmhs
0 notes
Text
I'm a cis afab woman who had her uterus and fallopian tubes out after 19 years of insisting on it.
The first 17 years were people pointing out I'd never, ever have children without one. My lack of desire for children was irrelevant. They got quieter and quieter as I got more and more chronic illnesses, especially when I pointed out they had just told me pregnancy and the postpartum period would be massively, permanently detrimental to my and any hypothetical child's health.
My current gynecologist finally realized I was not going to be swayed by the prospect of a gurgling, chubby baby in my arms. So he switched tracks: I would still have my period. I would still have pms. There was no guarantee this would even partially fix the debilitating abdominal pain that ruled most of my waking hours. I had to keep my uterus because getting rid of it would change nothing.
He eventually referred me for a hysterectomy consult for pms.
The surgeon took three minutes to assess a hysterectomy would be considered a viable option after (checks chart) 18 separate gynecologist not having a better idea, and my positive endometriosis diagnosis putting me at high likelihood for adenomyosis as an explanation for the pain.
Still, the mantra stayed the same throughout treatment, at every visit, with the 7 members of my pro-hysterectomy medical team: your period will still be there. No more blood, your uterus can't cramp up, no more risk of cervical or uterine cancer, highly decreased chances of ovarian cancer, but the period stays. As long as you have the hormones enabling your current health and quality of life, your period continues. We can't stop your period. Only the bleeding. Only your ability to carry and birth a child. Maybe the pain. Not the rest of it.
That was 7 months ago. I'm still on hormonal birth control to cause amenorrhea. I've had my period twice since. The pain is gone. The blood is gone. The rest is not.
I still get cravings and mood swings and bloating and diarrhea and my anxiety goes through the roof. My endocrinologist asks about my cycle even when he knows my uterus is gone. My annual gynecological cancer screening is next Friday. My hormone implant swap in is 2 months.
A uterus has laughably little to do with womanhood even if you look at it from an exclusively cis, exclusively medical perspective.
The whole "trans women can't get periods because they don't have uteruses" terf rhetoric is almost funny to me knowing that male dogs can have false heats and false pregnancies when their bodies produce excess estrogen
20K notes
·
View notes
Text
What Causes an Enlarged Uterus? Exploring the Leading Health Conditions
An enlarged uterus can develop for various reasons and often leads to uncomfortable symptoms that affect daily life. Recognizing the signs and understanding the causes behind an enlarged uterus can help guide those affected toward appropriate medical care. From fibroids to hormonal changes, many factors contribute to this condition. Here’s an overview of what causes an enlarged uterus, its symptoms, and potential treatment options.
Common Causes of an Enlarged Uterus
Fibroids: Fibroids are one of the leading causes of an enlarged uterus. These non-cancerous growths develop in or around the uterine walls and vary widely in size. Some fibroids are as small as a seed, while others grow large enough to change the shape and size of the uterus significantly. They often result in symptoms like heavy bleeding, pelvic pain, and bloating, all of which can signal uterine enlargement.
Adenomyosis: This condition occurs when the endometrial tissue, which lines the uterus, starts growing into the uterine muscle. Adenomyosis can make the uterus swell and become tender. Symptoms include severe menstrual cramps, prolonged bleeding, and discomfort during intercourse. The exact cause of adenomyosis remains unknown, but hormonal changes and childbirth are thought to increase the risk.
Hormonal Imbalances: Hormonal changes, particularly fluctuations in estrogen and progesterone, can influence the size of the uterus. High levels of estrogen, especially during pregnancy, can lead to temporary uterine enlargement. Conditions like polycystic ovary syndrome (PCOS) and menopause may also affect hormone levels, indirectly contributing to uterine enlargement.
Endometriosis: In this condition, the endometrial tissue grows outside the uterus. Though not directly increasing uterine size, endometriosis can cause inflammation and pain that sometimes lead to apparent or perceived uterine enlargement. Common symptoms include severe cramps, heavy bleeding, and pain during periods.
Ovarian Cysts: Large ovarian cysts, although not directly related to the uterus, can sometimes put pressure on the uterus, causing it to appear or feel enlarged. Most ovarian cysts are benign, but their size and location may result in bloating, pelvic pain, and pressure on surrounding organs.
Pregnancy and Postpartum Changes: Naturally, the uterus expands during pregnancy to accommodate the growing baby. However, in some cases, the uterus may remain slightly enlarged even after delivery, especially if multiple pregnancies have occurred.
Symptoms of an Enlarged Uterus
An enlarged uterus often presents symptoms that can impact a person’s quality of life. Some of the most common symptoms include:
Heavy or irregular menstrual bleeding
Frequent urination due to pressure on the bladder
Lower back pain
Bloating and abdominal discomfort
Painful intercourse
These symptoms may vary depending on the underlying cause of the enlargement.
Treatment Options for an Enlarged Uterus
Treatment depends on the cause and severity of symptoms. Here are some common approaches:
Medication: Hormone-regulating medications, such as birth control pills, can help manage symptoms related to hormonal imbalances.
Uterine Fibroid Embolization (UFE): For those dealing with fibroids, UFE is a non-surgical option that shrinks fibroids by blocking blood flow to them, effectively reducing uterine size and related symptoms.
Hysterectomy: In severe cases, a hysterectomy (surgical removal of the uterus) may be recommended, especially for those with adenomyosis or unmanageable fibroids.
Lifestyle Adjustments: Diet, regular exercise, and stress management can help balance hormones, potentially reducing the symptoms of an enlarged uterus.
When to Seek Help
If you experience persistent symptoms like heavy bleeding, prolonged periods, or pelvic pain, consider consulting a healthcare provider. Early diagnosis and treatment can prevent complications and improve your quality of life.
By understanding what causes an enlarged uterus, you’re one step closer to managing its effects and finding a treatment plan that aligns with your needs. With various treatment options available, you don’t have to face this alone.
#enlargeduterus#fibroidawareness#hormonalhalth#uterinehealth#UFE#fibroidtreatementoptions#womenhealthmatters
0 notes