#urology department
Explore tagged Tumblr posts
Text
Know More About Common Urologic Conditions in Men and Women
Urologic conditions are prevalent health issues that affect both men and women, impacting the urinary tract and reproductive system. From urinary tract infections to more complex conditions like kidney stones, these ailments can significantly influence one’s quality of life.

Understanding the symptoms, causes, and treatment options for these conditions is essential for effective management and prevention.
Let’s delve into some of the most common urologic conditions affecting both men and women, exploring their unique characteristics and discussing strategies for diagnosis and treatment. Whether you’re experiencing discomfort or simply seeking knowledge for preventive measures from the best urology doctor in Palakkad, this comprehensive guide will provide valuable insights into managing urologic conditions in both men and women.
UROLOGIC CONDITIONS IN WOMEN
Health problems in women involving the urinary tract and reproductive system vary widely. These issues, such as urinary tract infections and pelvic organ prolapse, can greatly affect daily life. In this post, we’ll discuss some common urological conditions in women, their symptoms, causes, and treatment options.
Urinary Tract Infections (UTIs):
Urinary tract infections are among the most common urologic conditions in women. They occur when bacteria enter the urinary tract and multiply, leading to symptoms such as a frequent urge to urinate, painful urination, cloudy or bloody urine, and pelvic pain. UTIs can affect any part of the urinary tract, including the bladder, urethra, and kidneys. Risk factors for UTIs in women include sexual activity, pregnancy, menopause, and underlying medical conditions such as diabetes. Typically, treatment includes the administration of antibiotics to eradicate the infection.
Overactive Bladder (OAB):
Women with OAB may experience sudden urges to urinate that are difficult to control, leading to leakage episodes. This condition can significantly impact a woman’s quality of life, causing embarrassment and social withdrawal. Causes of OAB may include nerve damage, bladder inflammation, or hormonal changes. Treatment options for OAB include lifestyle modifications, pelvic floor exercises, medications, and in severe cases, surgical interventions.
Pelvic Organ Prolapse (POP):
Pelvic organ prolapse happens when the muscles and tissues that support the pelvic organs weaken, leading them to descend into the vagina. These symptoms may manifest as pelvic pressure or a sense of fullness, urinary incontinence, difficulties with bowel movements, and a noticeable bulge in the vaginal region. Risk factors for POP include childbirth, ageing, obesity, and chronic coughing or straining. Treatment options range from pelvic floor exercises and lifestyle modifications to pessary insertion or surgical repair, depending on the severity of the prolapse.
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS):
Interstitial cystitis, alternatively referred to as bladder pain syndrome, presents as a persistent condition marked by discomfort in the bladder along with heightened urinary urgency and frequency. Women with IC/BPS may experience discomfort or pressure in the bladder area, as well as pain during urination or sexual intercourse. The exact cause of IC/BPS is unknown, but it is believed to involve inflammation of the bladder lining or dysfunction of the protective lining. Treatment may include dietary modifications, bladder training, medications, and in severe cases, bladder instillations or surgical interventions.
Urinary Incontinence (UI):
Urinary incontinence is a common urologic condition in women, characterized by the involuntary loss of urine. There are several types of UI, including stress incontinence, urge incontinence, and mixed incontinence. Risk factors for UI include pregnancy, childbirth, menopause, obesity, and pelvic floor muscle weakness. Treatment options for UI may include pelvic floor exercises, bladder training, medications, and in severe cases, surgical procedures such as sling placement or bladder augmentation.
UROLOGIC CONDITIONS IN MEN
Urologic conditions in men encompass a wide range of health issues that affect the urinary tract and reproductive system. These conditions can vary in severity and impact, ranging from common ailments to more serious medical concerns. In this blog, we’ll explore some of the most prevalent urologic conditions in men, their symptoms, causes, and available treatment options.
Benign Prostatic Hyperplasia (BPH):
Benign prostatic hyperplasia, also known as prostate enlargement, is a common condition among ageing men. It occurs when the prostate gland enlarges and constricts the urethra, leading to symptoms such as frequent urination, difficulty starting or maintaining urination, weak urine flow, and a feeling of incomplete emptying of the bladder. The exact cause of BPH is not fully understood but is believed to be related to hormonal changes associated with ageing. Treatment options for BPH include medications, minimally invasive procedures, and surgery in severe cases.
Urinary Tract Infections (UTIs):
Urinary tract infections are bacterial infections that affect any part of the urinary system, including the bladder, urethra, and kidneys. While UTIs can occur in both men and women, they are less common in men due to the longer length of the male urethra. However, men with certain risk factors, such as an enlarged prostate or urinary catheterization, may be more susceptible to UTIs. Symptoms of UTIs in men include a frequent urge to urinate, painful urination, cloudy or bloody urine, and pelvic pain. Treatment involves antibiotics to eliminate the infection.
Erectile Dysfunction (ED):
It is also known as impotence, is the inability to achieve or maintain an erection sufficient for sexual intercourse. While occasional difficulty with erections is common, persistent ED can be a sign of an underlying health condition, such as cardiovascular disease, diabetes, or low testosterone levels. Other risk factors for ED include obesity, smoking, excessive alcohol consumption, and certain medications. Treatment options for ED may include oral medications, penile injections, vacuum erection devices, or surgery in severe cases.
Kidney Stones:
Kidney stones are hard deposits of minerals and salts that form in the kidneys and can cause severe pain when passing through the urinary tract. Men are more likely than women to develop kidney stones, and risk factors include dehydration, a high-protein diet, obesity, and certain medical conditions such as gout or inflammatory bowel disease. Symptoms of kidney stones may include severe back or abdominal pain, blood in the urine, nausea, and vomiting. Treatment options range from pain management and hydration to procedures such as lithotripsy or surgery to remove larger stones.
Prostatitis:
Prostatitis is inflammation of the prostate gland and can be caused by bacterial infection or other factors such as trauma or autoimmune disorders. Symptoms of prostatitis may include pelvic pain, pain or burning during urination, difficulty urinating, and pain during ejaculation. Treatment depends on the underlying cause but may include antibiotics, alpha-blockers to relax the muscles of the prostate and bladder, anti-inflammatory medications, and lifestyle changes.
Testicular Disorders:
Testicular disorders encompass a range of conditions that affect the testicles, including testicular cancer, epididymitis, and testicular torsion. Testicular cancer is the most common cancer in young men aged 15 to 35 and usually presents as a painless lump or swelling in the testicle. Epididymitis is inflammation of the epididymis, often caused by bacterial infection, and can cause pain and swelling in the scrotum. Testicular torsion is a medical emergency that occurs when the spermatic cord becomes twisted, cutting off blood flow to the testicle, and requires immediate surgical intervention.
Urologic conditions are prevalent health concerns that can affect individuals of all ages and genders. By understanding the symptoms, causes, and treatment options for these conditions, individuals can take proactive steps to manage their urological health effectively. From urinary tract infections to kidney stones and pelvic organ prolapse, each condition presents unique challenges and considerations for diagnosis and treatment. Seeking timely medical intervention and adopting preventive measures, such as maintaining proper hydration and practicing good hygiene, can help mitigate the risk of developing urologic conditions. Also, ongoing research and advancements in medical technology continue to improve diagnostic accuracy and treatment outcomes, offering hope for individuals facing urological challenges. Ultimately, by raising awareness about these conditions and providing valuable information and resources, we aim to empower individuals to prioritize their urological health and lead healthier, more fulfilling lives. Together, we can work towards a future where urologic conditions are effectively managed, and individuals can enjoy optimal health and well-being.
Conclusion
In summary, urological issues can have a serious negative influence on a person’s quality of life, regardless of gender. Accurate diagnosis and timely therapy with the best urology doctor is essential to the successful management of many disorders. Urological health and well-being are improved when prompt medical advice is sought, good lifestyle choices are made, and prescribed treatments are followed.
Thangam super specialty Hospital Palakkad is well known for its superior urological care. Our Urology department provide a high priority patient care and cutting-edge therapies. For those with urological issues, our cutting-edge medical procedures and individualized care guarantees the best results. As a premier facility offering both specialized and comprehensive care, Thangam Hospital is an excellent option for individuals looking for urological problems that can be effectively and dependably resolved.
#urology#Urology department#hospital#multispecialty hospitals#urological issues#best urology doctor in Palakkad
1 note
·
View note
Text
Top Urology Hospital in Hyderabad
PACE Hospitals is the Best Urology Hospital in Hyderabad. PACE Hospitals' urology department is dedicated to delivering thorough and compassionate care to patients with a wide spectrum of urological disorders. We endeavor to provide personalized treatment programs adapted to each patient's specific needs, guided by a team of experienced urologists and supported by cutting-edge facilities.
Why to choose one of the top Urology hospitals in Hyderabad at PACE Hospitals?
Experienced Urologists: Our team of urologists comprises experienced specialists dedicated to delivering high-quality care with compassion.
Advanced Technology: We leverage the latest advancements in urological diagnostics and treatments to ensure optimal outcomes for our patients.
Multidisciplinary Approach: We collaborate closely with other medical specialties to provide comprehensive care for complex urological conditions.
Patient-Centered Care: We prioritize patient comfort, safety, and satisfaction throughout the treatment journey, offering personalized care plans tailored to individual needs.
Our famous urology hospital in Hyderabad at PACE Hospitals offers a full spectrum of services, including:
Diagnostic Evaluations: We utilize advanced diagnostic techniques to accurately assess urological conditions, including ultrasound, urodynamic studies, and imaging scans.
Medical Management: Our team provides medical management for various urological conditions such as urinary tract infections, kidney stones, and benign prostatic hyperplasia (BPH).
Minimally Invasive Procedures: We specialize in minimally invasive procedures, including laparoscopic and robotic-assisted surgeries, for conditions such as prostate cancer, kidney disorders, and urinary incontinence.
Endoscopic Procedures: We perform a range of endoscopic procedures, including cystoscopy and ureteroscopy, for diagnosis and treatment of bladder and urinary tract disorders.
Urologic Oncology: Our urologists are experienced in the diagnosis and treatment of urologic cancers, including prostate cancer, bladder cancer, and kidney cancer, using the latest treatment modalities available.
Female Urology: We offer specialized care for women's urological health issues, including urinary incontinence, pelvic organ prolapse, and recurrent urinary tract infections.
Men's Health: Our team provides comprehensive care for men's urological health concerns, including erectile dysfunction, infertility, and male reproductive disorders.
Pediatric Urology: We offer expert care for children with congenital and acquired urological conditions, ensuring the best possible outcomes for pediatric patients.
Patient-Centric Approach
Compassionate Care: We understand the sensitive nature of urological conditions and strive to provide compassionate support and guidance to our patients and their families throughout their healthcare journey.
Collaborative Care: Our multidisciplinary approach involves close collaboration with other medical specialties, including oncology, radiology, and pathology, to ensure comprehensive and integrated care for complex urological cases.
Education and Empowerment: We empower patients with knowledge and resources to actively participate in their treatment decisions, promoting shared decision-making and informed choices regarding their urological health.
For expert urological care you can trust, schedule a consultation with urology specialist hospital in Hyderabad. PACE team is dedicated to providing personalized solutions and compassionate support for all your urological needs.
At PACE Hospitals, Hitech city your urological health is our priority. Discover compassionate care and advanced treatments with our dedicated urology team.
PACE Hospitals is actively involved in clinical research and participates in clinical trials to evaluate new treatments and therapies for various urological conditions, offering eligible patients access to cutting-edge advancements in urology care.
0 notes
Text
Best Urology Hospital in Hyderabad
PACE Hospitals is the Best Urology Hospital in Hyderabad. At PACE Hospitals urology department is committed to providing comprehensive and compassionate care for patients with a wide range of urological conditions. Led by a team of experienced urologists and supported by state-of-the-art facilities, we strive to deliver personalized treatment plans tailored to each patient's unique needs.
Why Choose Urology Department at PACE Hospitals?
Experienced Urologists: Our team of urologists comprises experienced specialists dedicated to delivering high-quality care with compassion.
Advanced Technology: We leverage the latest advancements in urological diagnostics and treatments to ensure optimal outcomes for our patients.
Multidisciplinary Approach: We collaborate closely with other medical specialties to provide comprehensive care for complex urological conditions.
Patient-Centered Care: We prioritize patient comfort, safety, and satisfaction throughout the treatment journey, offering personalized care plans tailored to individual needs.
Our Urology Department at PACE Hospitals offers a full spectrum of services, including:
Diagnostic Evaluations: We utilize advanced diagnostic techniques to accurately assess urological conditions, including ultrasound, urodynamic studies, and imaging scans.
Medical Management: Our team provides medical management for various urological conditions such as urinary tract infections, kidney stones, and benign prostatic hyperplasia (BPH).
Minimally Invasive Procedures: We specialize in minimally invasive procedures, including laparoscopic and robotic-assisted surgeries, for conditions such as prostate cancer, kidney disorders, and urinary incontinence.
Endoscopic Procedures: We perform a range of endoscopic procedures, including cystoscopy and ureteroscopy, for diagnosis and treatment of bladder and urinary tract disorders.
Urologic Oncology: Our urologists are experienced in the diagnosis and treatment of urologic cancers, including prostate cancer, bladder cancer, and kidney cancer, using the latest treatment modalities available.
Female Urology: We offer specialized care for women's urological health issues, including urinary incontinence, pelvic organ prolapse, and recurrent urinary tract infections.
Men's Health: Our team provides comprehensive care for men's urological health concerns, including erectile dysfunction, infertility, and male reproductive disorders.
Pediatric Urology: We offer expert care for children with congenital and acquired urological conditions, ensuring the best possible outcomes for pediatric patients.
Patient-Centric Approach
Compassionate Care: We understand the sensitive nature of urological conditions and strive to provide compassionate support and guidance to our patients and their families throughout their healthcare journey.
Collaborative Care: Our multidisciplinary approach involves close collaboration with other medical specialties, including oncology, radiology, and pathology, to ensure comprehensive and integrated care for complex urological cases.
Education and Empowerment: We empower patients with knowledge and resources to actively participate in their treatment decisions, promoting shared decision-making and informed choices regarding their urological health.
For expert urological care you can trust, schedule a consultation with urology specialist hospital in Hyderabad. PACE team is dedicated to providing personalized solutions and compassionate support for all your urological needs.
At PACE Hospitals, Hitech city your urological health is our priority. Discover compassionate care and advanced treatments with our dedicated urology team.
PACE Hospitals is actively involved in clinical research and participates in clinical trials to evaluate new treatments and therapies for various urological conditions, offering eligible patients access to cutting-edge advancements in urology care.

0 notes
Text
Yknow those stupid "Pipis room" (pee piss room) signs some people put in their bathrooms? Concept: one of those replacing the sign for the urology department in a hospital.
#pipis department#draco speaks#currently in a urology waiting room as is literally routine for me at the moment#using the NHS free WiFi for its intended purpose#they're running fucking laaaate for my appointment cmon sooner i get this done sooner I'm allowed to drink water#im dying squirtle
3 notes
·
View notes
Text
By: Christina Buttons
Published: Apr 4, 2024
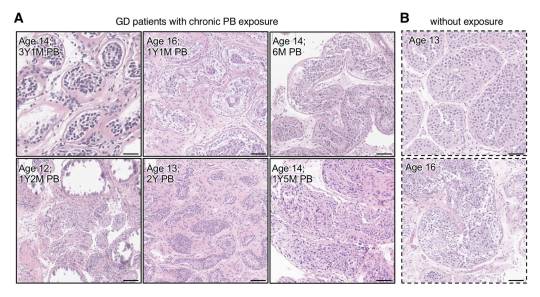
[ Figure 2: Representative images of Hematoxylin and Eosin-stained sections of testicular tissue biopsied from the testis from GD patients (A) with and (B) without PB exposure. ]
In a groundbreaking study from the Mayo Clinic, a globally recognized leader in medical research and patient care, researchers examined the effects of puberty blockers on testicular development in gender dysphoric male children. Their investigation revealed evidence of mild to severe atrophy in the sex glands of these children, leading the authors to express doubt in the claims of “reversibility” often made about puberty blockers.
The authors assert, “We provide unprecedented histological evidence revealing detrimental pediatric testicular sex gland responses to [puberty blockers].”
This preprint study, not yet peer-reviewed, presents evidence that puberty blockers induce significant cellular changes, impacting testicular development and sperm production in ways that are not fully reversible, with potentially permanent effects on testicular function and fertility. It challenges the longstanding view of puberty blockers as a reversible "pause button" on puberty.
As noted by the researchers of this study, no long-term studies exist for the use of puberty blockers in the context of stopping puberty for gender dysphoric children, and many potential health consequences remain unknown. In particular, the long-term impact on reproductive health is uncertain, making this study critical for filling this knowledge gap.
To address these unknowns, the Mayo Clinic has established the largest collection of testicular samples for patients aged 0-17 years, including those with gender dysphoria who have and have not yet received puberty blocker treatment, creating a database of over 130,000 individual cells for analysis.
Using a novel approach, the research team meticulously analyzed testicular tissue samples from youths undergoing puberty blocker treatment, with those not on puberty blocker treatment serving as controls. This comparison provides important insights into the potential cellular and molecular changes induced by these drugs.
Key Findings
The study utilized the Mayo Clinic's Pediatric Testicular Biobank for Fertility Preservation, which has been recruiting patients primarily from pediatric urology departments since 2015. Researchers analyzed testicular specimens from 87 young individuals (ages 0-17) undergoing fertility preservation surgery for various health reasons. Among these, 16 were gender dysphoric boys between the ages of 10 and 16, all of whom began identifying as transgender girls between the ages of 2 and 15. At the time of surgery, 9 patients (56%) were already on puberty blockers, with exposure ranging from 3 to 52 months. The authors noted that 100% of the 16 children would eventually go on to take them, highlighting “the widespread nature of PB intervention in this demographic.”
Among nine patients treated with puberty blockers, two exhibited unusual features in their testicles upon physical examination. One patient had abnormalities in both testicles, including incomplete development of the tunica albuginea, which is a protective covering around the testicles. The other patient had a right testicle that was difficult to detect.
In one part of the tissue-level analysis, over 400 testicular biopsy samples were analyzed and stained to examine the differences between those treated with puberty blockers and those who were not. Comparisons showed that testicular development in those treated with puberty blockers was abnormal compared to non-treated individuals. There was variability in how individuals responded to puberty blockers, leading to different outcomes in testicular development, including the degeneration of testicular tissues.
The study authors presented a case of a 12-year-old patient who underwent treatment with puberty blockers for 14 months. In this individual, 59% of the sex glands showed complete atrophy, along with the presence of microlithiasis—a condition where small clusters of calcium form in the testicles. This insight suggests that puberty blockers could lead to lasting structural changes. Additionally, research has shown a link between testicular microlithiasis and testicular cancer.

[ D) Representative images of normal (top) and fully atrophied sex gland (bottom). ]
This study also utilized single-cell analysis to investigate the effects of puberty blockers and aging on testicular cell composition. It took a very detailed look at individual cells from the testicles of a 14-year-old who had been on puberty blockers for over 4 years. The study analyzed a total of 130,100 cells, including 11,199 cells from the juvenile puberty blocker-treated patient.
The study observed that over 90% of the cells responsible for sperm production in this patient were stunted at an early developmental stage, unable to progress further. Additionally, it found "pathologically" higher and lower levels of two types of support cells (Sertoli cells) necessary for healthy sperm development. These findings suggest that puberty blockers can disrupt the normal maturation process of cells critical for sperm production.
In another part of the analysis, the authors found distinct cell-specific changes, including altered expression patterns of puberty-associated genes in endothelial cells, due to puberty blocker treatment. The authors believe that these drugs might induce juvenile testicular atrophy in part by disrupting the normal function of testicular endothelial cells.
Another aspect of the study focused on examining the effects of puberty blockers on the genetic activity of early-stage sperm cells, revealing significant changes that could potentially influence their development and fertility. By analyzing the activity of specific genes within these cells, the researchers found that puberty blockers may have caused alterations in gene expression, affecting processes crucial for the normal growth and function of these cells. This analysis suggests that the use of puberty blockers in gender dysphoric youth could have lasting implications for their reproductive health, particularly by impacting the ability of these early-stage sperm cells to mature properly.
Study Impact
Puberty blockers are increasingly used as a treatment for gender dysphoric youth to halt the development of secondary sex characteristics, such as breast development and widening of hips in females, or the growth of facial hair and deepening of the voice in males. Thousands of children in the United States are placed on this medical pathway as part of the gender-affirming model of care, under the presumption that these drugs are safe and fully reversible.
However, many aspects of the long-term consequences of puberty blockers, which have been administered to children off-label in an experimental manner, remain unknown. This study contributes valuable insights into the potential irreversible harm these treatments can cause to bodily and reproductive functions.
Arguably, the most critical finding is the evidence of mild to severe sex gland atrophy in children treated with puberty blockers. This atrophy signifies potential damage or impairment to the structures essential for sperm production, raising serious concerns about the long-term fertility impacts of these drugs for these individuals.
Given the Mayo Clinic's esteemed reputation in the medical and research communities, should the study pass peer review without any issues, its findings will carry significant weight.
Broader Implications
Puberty blockers belong to a group of synthetic gonadotropin-releasing hormone (GnRH) analogues. These drugs act on the pituitary gland to hinder the release of chemical signals that typically trigger the production of estrogen and testosterone. Historically GnRH analogues were used to treat conditions such as prostate cancer, fibroids, and endometriosis and, in some cases, as a measure to chemically castrate sex offenders.
In children, puberty blockers prevent the natural changes of puberty driven by sex hormones and have been used to treat central precocious puberty, a condition where a child begins to sexually mature much earlier than usual. In gender dysphoria, puberty blockers are administered experimentally, lacking long-term testing.
Notably, the U.S. Food and Drug Administration (FDA) has not approved puberty blockers and sex hormones for use in pediatric gender care. No clinical trials have substantiated the safety of these drugs for such non-approved applications and manufacturers of puberty blockers have repeatedly declined to conduct safety trials for their use on this cohort.
While puberty-blocking drugs are often promoted as “safe,��� "reversible" and a "pause button" on puberty, these characterizations seem to stem from their approved use for treating central precocious puberty in younger children, not their burgeoning off-label use for managing gender dysphoria in adolescents.
Past studies have indicated possible negative effects on bone density and brain health. There is also a concern that these drugs might solidify gender dysphoria in adolescents, potentially leading them down a lifelong road of biomedical interventions. Following reports in 2016 of suicidal ideation in children administered puberty blockers, the FDA instructed drug manufacturers to include a warning about potential psychiatric issues on the drugs' labels.
Puberty blockers are increasingly administered to adolescents at Tanner Stage 2, the first signs of puberty. Research shows administering puberty blockers at this stage, followed by cross-sex hormones, may result in infertility, sterility, and sexual dysfunction. Furthermore, they inhibit the development of mature male genitalia, making it difficult to create a pseudovagina in the event of a later vaginoplasty due to a lack of sufficient tissue.
The National Health Service England recently announced it would no longer prescribe puberty blockers to youth outside of research settings and closed down its only national clinical service for pediatric gender medicine, following a review that deemed the service "not safe.”
Several European countries, including Sweden, Finland, the UK, Denmark, and Norway have updated their guidelines for youth transition to align with systematic evidence reviews, the gold standard in evidence-based medicine. These reviews concluded that the risks associated with youth transition outweigh any purported benefits. Consequently, these countries have implemented restrictions on medical interventions, prioritizing psychotherapy as a first-line response for minors experiencing gender-related distress.
==
They're sterilizing boys and giving them cancer. When "god" does it, we call him evil. When humans do it, we call it "gender affirming care."
#Christina Buttons#puberty blockers#atrophy#medical scandal#medical malpractice#medical corruption#sterilization#fertility#irreversible#gender affirming care#gender affirming healthcare#gender affirmation#queer theory#gender ideology#gender identity ideology#intersectional feminism#religion is a mental illness
233 notes
·
View notes
Text
Bo Laurent created the Intersex Society of North America in 1993, starting the intersex rights movement in the United States. Describing the founding of ISNA, they wrote:
"Over the course of a year, simply by speaking openly within my own social circles, I learned of six other intersexuals--including two who had been fortunate enough to escape medical attention. I realized that intersexuality, rather than being extremely rare, must be relatively common. I decided to create a support network. In the summer of 993, I produced some pamphlets, obtained a post office box, and began to publicize the Intersex Society of North America (ISNA) through small notices in the media. Before long, I was receiving several letters per week from intersexuals throughout the United States and Canada and occasionally some from Europe. While the details varied, the letters gave a remarkably coherent picture of the emotional consequences of medical intervention. Morgan Holmes: "All the things my body might have grown to do, all the possibilities, went down the hall with my amputated clitoris to the pathology department. The rest of me went to the recovery room--I'm still recovering." Angela Moreno: "I am horrified by what has been done to me and by the conspiracy of silence and lies. I am filled with grief and rage, but also relief finally to believe that maybe I am not the only one." Thomas: "I pray that I will have the means to repay, in some measure, the American Urological Association for all that it has done for my benefit. I am having some trouble, though, in connecting the timing mechanism to the fuse."
ISNA's most immediate goal has been to create a community of intersex people who could provide peer support to deal with shame, stigma, grief, and rage, as well as with practical issues such as how to obtain old medical records or locate a sympathetic psychotherapist or endocrinologist. To that end, I cooperated with journalizes whom I judged capable of reporting widely and responsibly on our efforts, listed ISNA with self-help and referral clearinghouses, and established a presence on the internet. ISNA now connects hundreds of intersexuals across North America, Europe, Australia, and New Zealand. It has also begun sponsoring an annual intersex retreat, the first of which took place in 1996 and which moved participants every bit as profoundly as the New Woman conference had moved me in 1993.
ISNA's longer-term and more fundamental goal, however, is to change the way intersex infants are treated. We advocated that surgery not be performed on ambiguous genitals unless there is a medical reason (such as blocked or painful urination), and that parents be given the conceptual tools and emotional support to accept their children's physical differences...To provide a counterpoint to the mountains of medical literature that neglect intersex experience and to begin compiling an ethnographic account of that experience, ISNA's Hermaphrodites with Attitude newsletter has developed into a forum for intersexuals to tell their own stories.
...When I established ISNA in 1993, no such politicized groups existed. I was less willing to think of intersexuality as a pathology or disability, more interested in challenging its medicalization entirely, and more interested still in politicizing a pan-intersexual identity across the divisions of particular etiologies in order to destabilize more effectively the heteronormative assumptions underlying the violence directed at our bodies."
-Cheryl Chase, Mapping the Emergence of Intersex Political Activism, Journal of Lesbian and Gay Studies, 1998, 189-211.
#personal#intersex#actuallyintersex#intersex history#h slur#ISNA#hwa#that last quote i have like. four pages of my thesis just analyzing the lanugage and what#laurent says about disability. ISNA's antimedicalization politics and the conflation with pathology and disability#adn how that ultimately led to the bad decision to develop DSD language and the failure to#keep radical anti medicalization politics#igm tw#intersex surgery tw
125 notes
·
View notes
Text
My preferred hospital's urology department called today to schedule an appointment five months from now. I currently feel fine, but that seems like an awful long time during which I could potentially develop more serious complications if there are more stones kicking around in my stupid kidneys
#guys I'm trying to AVOID the emergency room#what if we could just take a look soon so I don't have to wait until my kidneys burst into flames?#maybe someone could at least do some blood work?#I would love to check that I don't have a surprise parathyroid tumor leaching all the calcium out of my bones#sorry for pissposting I'm just bothered by this#and it's somehow more gross to me than my incessant pooposting. idk.#boring text posts#medical
9 notes
·
View notes
Text
Atlantis Expedition: Science Division Departments - Medical Department
Continuing from my starting post here, I'm now breaking things down by department, beginning with the Medical Department.
I did end up heavily revising this department after the commentary on the general departments post, and also after a lot of looking up of the actual divisions of medical specialties. So, first, the (new) numbers:
> Head: Carson Beckett (later, Jennifer Keller, later, whomever) > Contains: Surgery, psychiatry, physical therapy > Function: Maintaining health of expedition members > Examples of function: surgeries, medical prescriptions, recuperation from injuries, mental stability > Personnel quantity: 1 (Head) + 10 (surgical team) + 5 10 (nurses non-surgical team) + 1 (psych) + 1 (phys. therapy) + 1 (anesthesiologist) (grouped under non-surgical team) = 19 23 total > A/N: Nurses have training in medications and physical therapy, surgical team also doubles as general practitioners
Information carried over from the first post, with struck text indicating revisions. The new total is 23, and the author's note is now irrelevant in light of new information. Mostly.
After doubling the amount of nurses, realizing "nurse" is a very broad category of medical professional with multiple definitions and aspects of job duties in multiple countries, I did a bit of renaming of the teams within this department: surgical, non-surgical, and miscellaneous (sorry guys).
Something I had realized was that this was not going to be a typical medical department (duh, in hindsight). These people are all going through the SGC, and the SGC quite likely not already has their own training protocols in place for dealing with SGC-specific situations, but also adapted technology from Goa'uld tech. What is Goa'uld tech? Appropriated Ancient tech, but without the gene component - fascinating, but also a post for another time.
This did inform how I revised which personnel to include, their specialties, and their duties. You're not exactly going to be shoving a whole MRI machine through a gate, so a radiologist isn't going to be a necessary specialty. Because of this, there's going to be a lot more cross-training, and more of a focus that's similar to what Atlantis would actually operate as: a forward operating base.
So, on to the teams (commentary included).
Surgical Team
> Personnel quantity: 10 > Minimum education: Doctorate in Surgery (ChM) > All of these people are already trained in basic medical knowledge and practices, and also overall surgical practices in different areas of the body
Specialties
> Neurosurgery > Dentistry | Oral and maxillofacial surgery » In the US, trained to do general anesthesia and deep sedation > Orthopedics » Musculoskeletal > Trauma surgery » Can contain combat surgeons » 2x of these > OBGYN > Urology > Cardiothoracic » 2x of these, by speciality: ⇛ Cardiovascular surgeon ⟹ "involving the heart and the great vessels" ⇛ Thoracic surgeon ⟹ involving the lungs, esophagus, thymus, etc. > Surgical technologist » "In the military they perform the duties of both the circulator and the scrub." » Creates and maintains a sterile surgical environment » Anticipates the work a surgeon needs to do » Walking compendium of surgical techniques and stitches
I had wavered a bit on qualifications, and thus who to include - at the end of the day, it was probably going to be on an American standard, given the physical location of SGC. This meant I got to do a nifty thing of having my oral/maxillofacial surgeon be the dentist that's also an anesthesiologist, even if this is apparently considered odd in many other countries.
Mostly I wanted to go by section of the body, and see what kind of specialties there were, and what did and did not overlap. Surprisingly, it was more difficult to figure out who did abdominal surgeries than it was neurosurgery or dental surgery, hence two people in cardiothoracic surgery and two "general" surgeons in the form of trauma surgery because, again, forward operating base - they have no idea what Atlantis will be, so some assumptions will need to be made and better to err on the side of caution.
In a more delicate but still very necessary subject, one OBGYN (obstetrics and gynecology) and one urologist (aka urinary system and male reproductive system). For various obvious reasons, everyone's health in this area still needs to be taken care of, so it's better to have them on the team than politely handwave the idea.
Neurosurgery, for an obvious reason - it's highly specialized and without significant overlap, while also being a critical function on a surgical team with the demands the Atlantis Expedition will likely face.
Orthopedics are musculoskeletal, or deals with muscles and the skeletal system. A fair amount of what they do has overlap (see: trauma surgeons), but having someone specialized for the particularities of setting bones and handling surgeries on things like the joints is incredibly useful when presuming setting up camp in an active combat zone (which they really, really did).
Trauma surgeons are, more or less, the ones that you would see in an emergency situation - acute situations and their injuries are their specialty, and for this expedition likely the head of the surgical team by dint of their training to assess a patient quickly and develop a care plan very quickly. Because of this, I found the overlap of combat surgeons immensely helpful, which means that there's a significant probability that this surgical team has military personnel assigned to it. These surgeons are also the ones most likely to be SGC-imported, and trained to deal with things like injuries from Goa'uld and Goa'uld devices.
All these very highly-trained people, who are all probably very, very smart - who supports them? As it turns out, at least in the operating theater, not the nurses, but surgical technologists.
Surgical technologists main job, at least here, would be to set up the operating theater and anticipate whatever it is a surgeon needs in assistance. This includes things like training on a wide variety of surgical techniques (i.e. stitches), disinfection procedures, and medications such as anesthesia (ish). I included the quote about military duties because it saves money on how many people to include in the expedition, and penny-pinching is the backbone of any hiring process.
Now, the surgical team is all done! That's ten people right there, and on to the non-surgical team.
Non-Surgical Team
> Personnel quantity: 10 » 5 Technicians/Nurses, 5 Non-Surgical Medical Specialists
Nurses
> (Advanced Practice) Nurses » 5x of these » Registered Nurse ⇛ As the general minimum educational and experimental requirement » Perioperative nursing ⇛ Assists surgical team, helps with pre- and post-surgical patients » Emergency nursing ⇛ Can do triaging, suturing, casting/splinting, local/regional anesthesia, and other doctoral skills as needed ⇛ Likely the SGC training model incorporates all of the above, and also training on medical technology adapted from Goa'uld healing technology (which is really Ancient but without the ATA gene lock) ⟹ Radiology tech ⟹ MRI tech (which is radiology but a bit to the left) ⟹ Other adapted diagnostic equipment
Non-Surgical Medical Specialists
> Pathology » 2x of these » Coordinates with Life Science Department to develop diagnoses for novel diseases (in the Pegasus galaxy) > Internal medicine | Internists » 2x of these > Anesthesiology » For everything the OMS people don't do in terms of anesthesiology » See also: Anesthesia (topic)
Remember how I said the qualifications were a doozy, and that nurses were a broad category? ... Yeah, this is why. The medical field is probably current in flux right now, given the shifting priorities of medical personnel and so much research that is still in the process of being applied, but I waved my magic plot-fixing wand and assumed the SGC figured this out for me.
All of these nurses are likely to be SGC imports, and thus unbelievably well-trained in everything that the SGC needs them to do. These are the personnel who know how all of the Goa'uld tech works on a functional level, have gotten the goodies first from engineering, and are waving their handheld MRI and other diagnostic equipment over their patients like a fairy godmother in scrubs. As with a real world hospital, these are the people actually running the show, and likely making the surgical team look like hypercompetent show poodles.
As for non-nurses who are also non-surgeons, pathologists are the ones who work up what people will actually be diagnosed with, figuring out all the newest and shiniest diseases and cataloguing them for reference. Doctor Biro is a pathologist, for example.
The thought occurred to me that we still need something resembling a general practitioner, but in light of fancy things like handheld MRIs and other scanners, this role is much reduced in favor of people who pack a greater intellectual punch.
However, I found that internists not only fill this gap, but are also hyper-specialized in their own way, in the respect of their knowledge base being internal diseases and multi-system diseases. Ergo, two of them, because they're just that useful. They'd probably coordinate quite a bit with cardiothoracic surgeons, as those are overlapping areas of study based on region of the body.
One (1) anesthesiologist, because the OMS cannot - nor should they - be the only person to perform anesthesia. This person functions as a sanity checker, and also the thin margin of the anesthesia that the surgeon doesn't cover.
We still need to round out this department, though. So far I've managed to cover in-patient, out-patient, and the various surgical stages. What else?
Well, recuperation - patients can't actually linger in the infirmary for the entirety of their healing process, for such practical reasons as beds available and boredom of patient, so the transitional phase needs to be covered.
Hence, the highly uncreative placeholder section name of Miscellaneous:
> Psychiatrist » 1x of these, because canon says so? > Physical therapist » 1x of these, because canon says so?
Now while personnel such as nurses and internists are meant to convey educational material and instructions to patients about recuperation, it helps to actually have specialists on hand to make the patients commit to the bit.
Having only one psychiatrist on hand seems a bit of a Star Trek logical fallacy, but I'm once again waving my plot wand and assuming anyone that managed to get through the arduous employment process of 1) being told the Stargate exists (and coping with their world views being upended), 2) being employed by the SGC in general, and 3) passes their psychological assessment is probably mentally stable enough to only need one psychiatrist for the entire expedition.
(Yes, this does mean everyone on the expedition got their rubber stamp of sanity, and probably in grueling triplicate. Such as it can be defined a fanfiction-like world of scifi. I think they're coping pretty well with everything, no?)
With all the work that the surgical and non-surgical teams put into taking care of injured expedition members, a physical therapist is, as with everyone else here, very good at their job, but ultimately one of the last steps for patients that require longer term care. Think gaining back muscle after a broken leg, or more serious injuries that require months of guided exercise to be back to gate team-ready health (or general running for your life because Atlantis is just as dangerous).
Total Medical Department Personnel
Head of Department: 1
Surgical Team: 10
Non-Surgical Team: 10
Miscellaneous: 2
Total total: 23
I'll be going over headcanons on canonical personnel, such as Carson Beckett, Jennifer Keller, and Biro in their own posts, but for now this is a general accounting of the expedition's medical department.
Shout-out to @savestave and @stinalotte for the discussion and feedback on the original post!
21 notes
·
View notes
Text
The trouble came out of nowhere, I’m now in the hospital in the urology department 👍
They said that I had a kidney stone. While I was waiting for all the doctors to examine me, I thought I would fucking die from pain lol, it was too long and painful. But they finally gave me a painkiller and I came back to life
Tomorrow they'll do a CT scan and tell me how long I'll be lying here. I hope it's not too serious
...And there are no cups in the hospital and I drink water from test jar.

17 notes
·
View notes
Text

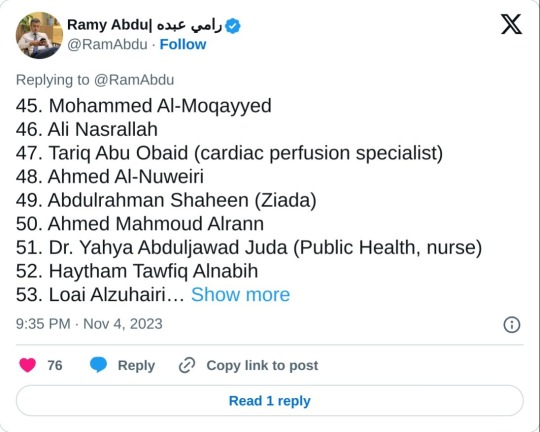
List of healthcare workers killed by Israel attacks on Gaza since October 7, 2023
Physicians:
Dr. Omar Ferwana, a Professor and former Dean of the Islamic University of Gaza Medical School and an andrologist, Gaza
Dr. Aya Ferwana (Dr Omar Ferwana’s daughter), a family medicine specialist, Gaza
Dr. Medhat Saidam, a senior burn and plastic surgeon, Shifa Hospital, Gaza and MSc in Burn Care alumnus from Queen Mary University of London
Dr. Mohammed Dabour, a consultant pathologist and dean of pre-clinical medicine at the Islamic University of Gaza Medical School
Dr. Tamer Al-Khayyat, an anesthesiologist and intensivist, European Gaza Hosptial, Rafah
Dr. Mahmoud Al-Khayyat, an internist in Rafah and Dr Tamer Al-Khayyat’s father
Dr. Razan Al-Rakhawi (Dr Tamer Al-Khayyat’s wife), an obstetric and gynecologist, Emirati Women’s Hospital, Rafah
Dr. Sereen Al-Attar a consultant obstetric and gynecologist at Nasser Hospital, Khan Younis and an Assistant Professor at the Islamic University of Gaza Medical school
Dr. Saeed Drabieh, a urology resident, Shifa Hospital
Dr. Mohammed Al-Samarai, Iraqi volunteer intern physician
Dr. Rafat Abou Foul, radiologist, Beit Hanoun Hospital
Dr. Amal Al-Maqadma, family medicine specialist, Rafah
Dr. Ibtihal Al-Astal, intern doctor, Khan Younis
Dr. Duaa Awad, emergency medicine doctor, Al-Aqsa Hospital
Dr. Moath Nabaheen, emergency medicine doctor, Al-Aqsa Hospital
Dr. Youssef Jadallah, intensivist and anesthesiologist (based in Germany, from Gaza but was visiting his family)
Dr. Inas Yousef, emergency medicine doctor, Al-Aqsa Hospital
Dr. Israa Al-Ashqar, anesthesiology resident, Shifa Hospital, Gaza
Dr. Abdallah Ashour, emergency medicine doctor, Nasser Hospital, Khan Younis
Dr. Hamam El-Deeb, orthopaedic surgery resident, Shifa Hospital, Gaza
Dr. Munther Abu Sariya, consultant pediatrician, Mohammed Al-Durra Pediatric Hospital
Dr. Doaa Shammout, pediatric resident, Rantisi Hospital, Gaza
Dr. Baraa Abu Elaish, intern doctor, Gaza
Dr. Abdlallah El-Helou, general practitioner/internal medicine doctor, Indonesian/Beit Hanoun Hospital
Dr. Muhannad Ezzo Afana, general practitioner, Gaza
Dr. Mohammed Refaat Mekki,
Dentists:
Dr. Ahmed Al-Hourani
Dr. Nada Mahdi
Dr. Ibrahim Al-Dali
Dr. Bilal Lubbad
Dr. Marwa Swelim
Dr Areej Eid
Dr. Tawfiq Al-Farra
Dr. Abdallah Baghdadi
Dr. Jameel Tarazi
Dr. Maysoon Al-Nuweiri
Dr. Mona Dughmush
Dr. Noha Dughmush
Dr. Mamoun Afana
Dr. Mohammed Afana
Dr. Anis Mekki
Dr. Tasneem Abdulnabi
Medical/dental students:
Bisan Halasa
Shaimaa Saydam
Abedelrahman Abu Shammala
Nour Al-Ashqar
Yaseen Al-Akhras
Osama Abu Safia
Duha Dughmush
Haneen Al-Shannat
Abdallah Abu Jayab
Zainab Azzam
Mohammed Abu Jiadan
Medical Scientists:
Prof. Salah El-Din Zanoun
Prof. Ahmed Al-Dalo
Prof. Ameed Mushtaha (Head of laboratories department and blood banks
Nurses:
Mohammed Lubbad
Mohammed Al-Azzaiza
Ahmed Moshtaha
Rami Lubbad
Somaya Temraz
Mohammed Rafat Gomaa
Osama A'eed Abu Safiya
Saber Al-Nimnim
Mohammed Hamad
Mohammed Al-Baz
Suleiman Abu Zour
Badr Mohammed Abu Daqah
Shaimaa Rayan (Midwife)
Maryam Abou Daher
Kefah San’allah
Walaa Adwan (Midwife)
Rawaa Al-Thalathini (Midwife)
Samah Rasheed (Midwife)
Rida Al-Masri (Midwife)
Ibrahim Abou Isaac
Amjad Abou Ouda
Ibrahim Al-Farra
Aya Al-Shrafi
Tamer Al Efesh
Momen Mansour
Asmaa Al-Asar
Feras Ftaiha
Diaa Bardaweel
Rana Shalaby
Itemad Miqdad
Zainab Al-Sharafi
Hamdan Malaka
Suheer Jbara
Hassan Al-Hennawi
Sabha Al-Sherafi
Azmi Al-Jamal
Yousef Al-Shareef
Hadeel Fanqa
Emad Esleem
Enas Al-Zeen
Heba Salamah
Nuha Esleem
Amro Masoud
Hanya Qudaih
Mohammed Al-Moqayyed
Ali Nasrallah
Tariq Abu Obaid (cardiac perfusion specialist)
Ahmed Al-Nuweiri
Abdulrahman Shaheen (Ziada)
Ahmed Mahmoud Alrann
Dr. Yahya Abduljawad Juda (Public Health, nurse)
Haytham Tawfiq Alnabih
Loai Alzuhairi (Nursing student)
Saleem Abu Zour
Waleed ElMahalawi
Rola Althalathini (Midwife)
Duaa Ashour
Amer Elramlawi
Safa Zeino
Saja Doghmosh
Moayad Ezzo Afana
Ramadan Doghmosh
Moemen Arab (Nursing student)
Oun Nofal Ashour (Nursing student)
Paramedics (EMS providers):
Marwan Abou Raida
Hatem Awad
Khalil Al-Sharif
Ahmed Al-Dahman
Yousri Al-Masri
Ahmed Abdel Rahman
Mohammed Al-Ghaliz
Mohammed Ali
Iyad Salim
Abdelrahim Abou Baid
Alaa Abou Ghanima
Naji Al Fayoumi
Mohammed Qateet
Tareq Ashour
Mahmoud Abou Mashayekh
Nafeth Al-Natour
Mahmoud Othman
Mohammed ElOmour
Ibrahim Matar
Yasser Alnaseri
Physiotherapists:
Ahmed Al-Masri
Ahmed Sameh Abou Herbeed
Shaimaa Sbaih
Mayar Al-Wahidi
Ahmed Ashraf
Shahrazad Al-Akhras
Nour Ibrahim
Pharmacists:
Ahmed Al-Jerjawi
Aziz Elfarra
Afnan Al-Astal
Shereen Abou Jazar
Eman Abu Al-Jalil
Safaa Hasouna
Ibraheem Meqdad
Mohammed Ali
Maysaa Khader
Nisreen Al-Dammagh
Sally Al-Aydi (Pharmacy student at AlAzhar University)
Mohammed Al-Shannat
Lina Abu Mualaileq
Noor Ibean
Haneen Albasyouni
Amira Dahman
Rawand Albanna
Khaled Abu Ma’ala
Amal Mekki
Abdullah Altartori (Pharmacy student at AlAzhar University)
Asmaa Abu Salah (Pharmacy student at AlAzhar University)
Mohammad Alshami
Lab technicians/clinical microbiologists:
Natheer Shaban
Asmaa Hijazi
Rawan Yassin
Alia Al Hinnawi
Maryam Kabaja
Nahid Abdullatef
Mohammed Abu Karsh
Mohammed Shabaan
Riham Elkahlout
Ismail Sharaf
Taiseer Alghouti
Abdulmohsin Abu Alrous
Duaa Jad Allah
Optometrists:
Omar Khorsheed
36 notes
·
View notes
Text
Discover the Best Hospital for Kidney Surgery in India

When facing a critical health issue like kidney surgery, the importance of choosing the right hospital cannot be overstated. India has emerged as a global hub for medical tourism, particularly in the field of nephrology and urology. The country boasts some of the best hospitals for kidney surgery, offering state-of-the-art facilities, highly experienced surgeons, and personalized care that rivals the finest medical institutions worldwide.
Why India?
India's healthcare system has advanced significantly over the past few decades, making it a preferred destination for complex medical procedures, including kidney surgery. The combination of world-class infrastructure, cutting-edge technology, and skilled medical professionals has positioned India as a leader in this domain. For patients, this means access to top-tier care at a fraction of the cost compared to Western countries.
What Makes a Hospital the Best for Kidney Surgery?
The best hospital for kidney surgery in India typically excels in several key areas:
Experienced Surgeons: The expertise of the medical team is paramount. India is home to many renowned nephrologists and urologists with extensive experience in performing kidney surgeries, including transplants and minimally invasive procedures.
Advanced Technology: The best hospitals are equipped with the latest technology, such as robotic surgery systems, which allow for greater precision and faster recovery times.
Comprehensive Care: Top hospitals offer a multidisciplinary approach, with teams of specialists who work together to provide comprehensive care from diagnosis through recovery. This includes not only surgeons but also nephrologists, anesthesiologists, and nursing staff who are experts in their fields.
Patient-Centric Approach: Hospitals that are patient-focused provide personalized treatment plans and ensure that patients and their families are well-informed throughout the process. They offer post-operative care and follow-up services that contribute to successful long-term outcomes.
Accreditations and Certifications: Look for hospitals that are accredited by national and international healthcare organizations, as these certifications reflect a commitment to maintaining high standards of medical care.
Leading Hospitals for Kidney Surgery in India
Several hospitals in India stand out for their exceptional care in kidney surgery:
Medanta – The Medicity: Located in Gurgaon, Medanta is renowned for its world-class kidney transplant program. The hospital is equipped with advanced robotic surgery systems and a team of highly skilled surgeons who specialize in complex kidney surgeries.
Apollo Hospitals: With locations across India, Apollo Hospitals is a leader in healthcare. Their nephrology and urology departments are known for pioneering minimally invasive surgical techniques and providing comprehensive care for kidney-related conditions.
Fortis Healthcare: Fortis is a well-established name in Indian healthcare, with a network of hospitals that offer cutting-edge treatment for kidney diseases. Their multidisciplinary teams provide personalized care and have a high success rate in kidney surgeries.
Max Super Specialty Hospital: Located in Delhi, Max Hospital is another top choice for kidney surgery in India. Their advanced technology, coupled with a team of experienced surgeons, makes them a preferred destination for both Indian and international patients.
Why Choose India for Kidney Surgery?
Patients from around the globe choose India not only for the quality of care but also for the affordability of treatment. The cost of kidney surgery in India is significantly lower than in countries like the United States, the United Kingdom, or Australia, without compromising on the quality of care. This affordability, combined with the expertise of Indian medical professionals, makes India a compelling choice for those seeking the best hospital for kidney surgery.
Moreover, India’s healthcare system is designed to accommodate international patients, with many hospitals offering dedicated international patient services. These services include assistance with travel arrangements, language interpretation, and personalized care plans to ensure a smooth and comfortable experience.
Final Thoughts
Choosing the best hospital for kidney surgery in India is a decision that can significantly impact your health and quality of life. With world-class hospitals, experienced surgeons, and a patient-centric approach, India offers unparalleled opportunities for successful kidney surgery outcomes. Whether you need a kidney transplant or other specialized procedures, India's leading hospitals are equipped to provide the highest standards of care.
For those in search of top-quality kidney surgery, India stands out as a beacon of hope and healing, offering a combination of excellence, affordability, and compassionate care that is second to none.
3 notes
·
View notes
Text
as always, we're complaining under the cut. tw for medical PTSD, mentions of medical procedures, personal/graphic descriptions of my fucked up little body, extremely privileged whining, it's worth it for the cat at the bottom tho
I am exhausted by the number of appointments I have. I've become the kind of person who has multiple appointments every single week. This week and next week are three appointment weeks, and those appointments always lead to scheduling MORE test/procedures/office visits.
I had an appointment with my urogynecologist. Given my history of neurogenic bladder and severe stage IV endometriosis, she's in agreement with me that it might be time to at least consider a bowel diversion, if not a total colonoscopy. This would be done in addition to a bladder diversion because self-catheterization has proven unsustainable and, frankly, dangerous for me to try to continue. I'll likely have a foley placed tomorrow morning that will stay in until I can get in to the urological surgeon, who has not called to schedule yet. I have the colorectal surgery consult next month and the neurourology consult a month after that. Just thinking about it gives me a headache.
I also have an EEG in a few days to see if the blackout episodes I've been having are epilepsy, and if it is, I'm not sure what we'll do since I'm already on a good amount of anticonvulsants. I have a feeling I'm going to leave that test with a migraine and no answers, which was exactly how the EMG/NCS I had done in my hand last Friday went.
Other things I've started include using a CPAP machine. I thought this shit was supposed to help you sleep better, but instead I'm waking up many many times in a two hour window, the pressure being pushed into my lungs is dislocating my ribs, I'm getting bloated from wearing it, and the pressure is coming out of my eyes and ears too due to a deformity in my inner ears called patulous eustachian tubes, so now my constant migraine is back in full force. I'm nothing but bloated and irritable as hell, but if I don't use it for at least four hours a day for at least 24 days a month, medicaid won't pay for it and I will have to pay out of pocket to buy the machine. My mother price checked it, it costs ~$1300 to buy the machine I have. I might just give up and give it to my brother, who also needs a CPAP but who doesn't also have EDS and is, therefore, not prone to ribs dislocating.
I met with my 4th electrophysiologist and that was a frustratingly and dangerously nonproductive appointment. He did not speak or understand spoken English well enough to be allowed to practice medicine in an English-speaking country imo. I don't give a shit about an accent, I don't think people need to "go back to where they came from" or that they need to speak English exclusively, but man it is so important in the field of medicine to be able to actually understand what your patient is saying to you. He had no idea what the condition I have even was, and he assumed I made all of these diagnoses for attention but would "humor me" and wrote IN HIS NOTES that I "insisted" on a holter monitor and tilt table test. I got these orders from Duke university, the closest university to me that has a genetic electrophysiology department and a dysautonomia clinic, both of which I was being seen at until Duke stopped taking my insurance. I was trying to tell this absolute worm brain that I was telling him what the top specialists GLOBALLY told me to have done, but I was just being young and attention-seeking I guess, I'm so dangerously angry about it, it makes my chest hurt to try and articulate just how badly this EP fucked it up for me.
I realized in the middle of a visit with my PCP on the 30th that I am not working towards a goal. Most people go to the doctor with the goal of Get Better Enough To Work, or Get Better Enough To Take Care Of The Kids. I don't have that. I'll never be able to hold down a job and I can't and don't want to have children.
I feel like the shittiest friend on Earth too because a good friend of mine only lives four hours away, but as much as we'd both like to visit, I have to schedule everything in my life around what's starting to look like a year packed with surgeries. I can't just pack up and go visit him, I come with medical equipment now. Between meds, splints, incontinence supplies, and the CPAP, I have to basically haul around a small urgent care center everywhere I go. I hate that I have to be planned around.
For a few wins, I do not have carpal tunnel, and when I had my A1C checked at my last PCP appointment, it was 4.9! Every doctor who finds that out informs me even their own A1C isn't that good because they like some specific sweet treat too much. My secret? No one has said they liked something that doesn't have dairy in it, and I've had a dairy allergy since birth.
anyway. I turned 26 just over a month ago and my beloved medical advisor turned 1 year old the same day. she's my birthday buddy :) it's weird having an Adult Cat in the house now, she's not the teeny tiny kitten that sneezed in my eye and gave me pinkeye anymore.
thanks 4 reading, besties. until my next frustratingly whiny and Packed Full of Info update <3
pictured: my big adult girl and medical supervisor 🥰

#endometriosis#fibromyalgia#neurogenic bladder#neurogenic colon#obstructive sleep apnea#central sleep apnea#bowel diversion#bladder diversion#epilepsy#medical ptsd#long qt syndrome#i am sickly and not meant for this earth#medical gaslighting#disability#invisible disability#im so frustrated im gonna cry i think
4 notes
·
View notes
Text
Forgot that being catheterised also sets off the same phobia response I get when I'm injected :( Fainted and threw up in the urology department waiting room :(
#and I have to go back and have the same procedure done every week for a month#luckily based on my experience with getting vaccinations if I just leave the place immediately afterwards I should probably be okay#draco speaks
3 notes
·
View notes
Note
hi, really liked the Evolutoin story you wrote, more medical au please?
This one as been sitting in my inbox since literally forever, (and it's still not the oldest one, which I feel horribly guilty about, btw) and it's inspired a little bit by (surprise, surprise) Grey's Anatomy.
I don't have time to write much anymore, so I hope it's fine that I used this ask as a drabble request, but I will try to write more on this if I have the time later.
Disclaimer: I do not own tvd or to. I am not a med student. All my knowledge of medicine is from Grey's Anatomy. Also very confused about the part whether rectal exams are a part of the urology department or not (pretty sure they're not), but I kind of needed to write that in, so I'm sorry if I'm wrong.
*sigh of relief* glad that's out. I'll stop talking now. Enjoy!
XXX
Klaus nearly jumps out of his own skin when he turns and sees Caroline smiling at him, batting her long eyelashes.
He raises an eyebrow.
“Hi,” Caroline starts cheerfully.
“Hi?” he says questioningly.
“Do you want to have lunch?”
“Can't,” says Klaus, walking past, his eyes still trained on her, then flitting back to his charts. “I have a surgery.”
“Oh,” Caroline pouts, then brightens. “What is it?”
“Craniotomy,” he replies, realizing that she’s following him. “I'll be done by three, so you should go ahead.”
She nods absent-mindedly, her eyes fixed on his charts. “Loving the hair today, by the way,” she says, smiling saccharinely.
“Thanks,” he says, extremely confused.
Her smile widens. “And you look very nice today. The scrubs are really working for you.”
“Caroline,” he drawls. “What do you want?”
“Okay,” she says, stepping in front of him, the bright smile still on her face, although he can see she’s a bit resentful at being caught out. “Here’s the deal.”
Klaus folds his arms and looks at her expectantly. “I need you to let me on your service today,” she says brightly.
“No.”
“Please,” she tacks on at the end, a sad effort at being polite.
“Still no,” he says, barely able to keep a smile from forming at her antics.
She huffs, the smile stubbornly still in place. “I need more hours on different services before next week. All I've been doing is Peds, and everywhere else is full.”
“So you came to me.”
“I checked and only Bonnie and Matt are on your service today. You have room for one more resident.”
“Caroline—”
“I know what you're going to say: that you shouldn’t treat me any different just because I'm your girlfriend, and that—”
“You're right, technically,” he says gently.
Caroline bites her lip. “I didn’t want to do this. I asked Georges to take me, but he’s already busy, so I had to come to you.”
He considers her. “If you want it, earn it," he says, and she looks hopeful. "If you manage to diagnose this patient,” he continues, handing her his chart. “I'll let you on my service. If not, well,” he winks at her, walking away. “You can always try Tanner.”
Caroline looks horrified. “That’s urology,” she spits at his retreating back. “You want me to look at penises and give rectal exams all day?”
Klaus looks at her innocently. “If it helps you get more hours other than Peds, then yes.”
She growls as the elevator closes.
He’d definitely be paying for the last bit later.
XXX
It's incredibly short, I know, and I apologize, but I hope you liked it, and please review!
Cheers!
10 notes
·
View notes
Text
High number of amputations to treat penile cancer reported in Brazil

A report from the Brazilian Society of Urology (SBU) stated earlier this month that over 6,000 penile amputations have been recorded in the South American country over the past ten years to treat three out of every 10 patients diagnosed with penile cancer. The condition can be avoided with simple hygiene measures and HPV vaccination, the SBU also explained.
“Many people don't even know that it's possible to have penile cancer, they don't go to specialists and end up receiving the diagnosis too late,” stressed Maurício Dener Cordeiro, coordinator of the SBU's Uro-Oncology Department, who admitted that the number of amputations was extremely high.
When identified at an early stage, penile cancer has a high chance of cure and can be treated less aggressively. In these cases, the tumor is restricted to the upper part of the skin and does not reach deeper structures. It is therefore possible to remove only the affected area - i.e. without having to remove the penis.
In the extreme “cases, the urethra is placed in the perineum, and the patient has to start urinating sitting down, which can be a challenge,” Cordeiro admitted while reckoning the procedure can be very damaging to the individual's self-esteem.
Continue reading.
5 notes
·
View notes
Text
After a long month, I finally got some good news and I got a call from the urology department today to set up a consult and then possibly, a cystoscopy. The bad news is they have no open appointments until the end of next month, so we wait once again…
#personal#LMAO at me being hopeful they would have something for like next week at the latest. 🤪#Terrified I have IC but my family is telling me it’s all my anxiety.
4 notes
·
View notes