#symptoms of HCC
Explore tagged Tumblr posts
Text
Hepatic Carcinoma What You Need to Know
Hepatic carcinoma, also known as hepatocellular carcinoma (HCC), is the most common type of liver cancer. It is a serious illness that can be life-threatening, but it is often treatable if it is caught early.
HCC is often caused by chronic liver diseases, such as hepatitis B or C infection, cirrhosis, or non-alcoholic fatty liver disease (NAFLD). Other risk factors for HCC include alcohol abuse, smoking, and exposure to aflatoxin, a cancer-causing toxin found in moldy food.
The symptoms of HCC can be vague and may not appear until the cancer is advanced. Some common symptoms include:
Abdominal pain
Weight loss
Fatigue
Nausea and vomiting
Jaundice (yellowing of the skin and eyes)
Enlarged liver
Ascites (fluid buildup in the abdomen)
If you notice any of the symptoms, you must visit a Liver cancer specialist in Mumbai Dr. Praveen Kammar, at the earliest. Early diagnosis and treatment of HCC can improve your chances of survival.
The approach to treating HCC varies according to the cancer's stage. For localized HCC, surgery to remove the tumor may be an option. Other treatments for localized HCC include radiofrequency ablation (RFA), microwave ablation, and cryoablation. These treatments use heat or cold to destroy the tumor.
For advanced HCC, treatment may include chemotherapy, targeted therapy, or immunotherapy. These treatments can help to shrink the tumor and relieve symptoms.
Here are some things you can do to reduce your risk of hepatic carcinoma:
Get vaccinated against hepatitis B and C.
Avoid alcohol abuse.
Don't smoke.
Consume a nutritious diet and sustain healthy body weight.
Get regular screening tests if you are at high risk for HCC.
By taking these steps, you can help to protect yourself from this serious disease.
0 notes
Text
Unlocking The Potential Of Lenvatinib A Comprehensive Guide Understanding Lenvatinib Price
In the field of cancer treatment, where targeted medicines are changing the landscape of care, Lenvatinib 10 mg stands out as a promising medication for patients suffering from certain types of cancer; however, the lenvatinib price fluctuatesoccasionally. This article will provide a thorough examination of Lenvatinib 10 mg, providing light on its applications, mechanism of action, dosage, ability, side effects, and revolutionary effect on cancer treatment.
Introduction to Lenvatinib 10 mg
Lenvatinib is a tyrosine kinase inhibitor with demonstrated success in the treatment of a variety of malignancies, including thyroid cancer and hepatocellular carcinoma (HCC). The 10 mg dosage of Lenvatinib is a specific method geared to meet the healing needs of patients undergoing targeted treatment.
Mechanism of Action
Lenvatinib works by inhibiting a few receptor tyrosine kinases (RTKs), as well as vascular endothelial growth problem receptors (VEGFRs), fibroblast increase detail receptors (FGFRs), and platelet-derived boom element receptors (PDGFRs). Lenvatinib exerts anti-cancer effects by focusing on the major signaling pathways involved in tumor angiogenesis, development, and metastasis, which are ultimately necessary for tumor regression and advanced impacted character outcomes.
Uses of Lenvatinib 10 mg
Thyroid Cancer
Lenvatinib 10 mg is approved for the treatment of differentiated thyroid cancer (DTC) that is resistant to radioactive iodine therapy. It has demonstrated efficacy in slowing disease progression and improving improvement-free survival in patients with advanced or metastatic DTC. You can purchase it by obtaining information on lenvatinib prices from medical clinics or online.
Hepatocellular Carcinoma (HCC)
For patients with advanced HCC who are not candidates for surgical resection or network ablation, Lenvatinib 10 mg provides a valuable therapy option. It has demonstrated superiority over sorafenib, an excellent tyrosine kinase inhibitor, in terms of overall survival and progression-free survival in patients with unresectable HCC.
Dosages and Administration
Lenvatinib 10 mg is typically delivered orally once per day, with or without food. The dosage can be changed based on the affected person’s characteristics, such as frame weight, renal function, and tolerability. Healthcare personnel regularly monitor patients getting Lenvatinib medication, including regular examinations of tumor reactions and adverse effects to optimize treatment outcomes.
Potential Side Effects
While Lenvatinib 10 mg is generally well tolerated, it may produce adverse outcomes in certain patients. Common side effects of Lenvatinib medication include elevated blood pressure, lethargy, diarrhea, decreased appetite, nausea, and proteinuria. Patients are advised to immediately report any new or worsening symptoms to their healthcare providers for proper management.
Wrapping Up
Finally, Lenvatinib 10 mg represents a significant development in the treatment of thyroid cancer and hepatocellular carcinoma, providing improved outcomes and increased survival for patients with advanced or metastatic disease. Its concentrated mechanism of action, combined with its broad range of medical warning signals, emphasizes its importance in modern oncology. Patients are recommended to consult with their healthcare providers to learn more about the lenvatinib price, for personalized guidance, and for adapted control strategies when using Lenvatinib 10 mg. People can begin their treatment path with confidence and hope for a better future by understanding the intricacies of most cancers and investigating available therapy alternatives. Source:-
Unlocking The Potential Of Lenvatinib A Comprehensive Guide Understanding Lenvatinib Price
2 notes
·
View notes
Text
Liver transplantation.
The one time you might actually want cancer.
Why? Because having a primary liver cancer bumps you up on the liver transplant list. But it can't just be any cancer - there's a criteria for acceptable cancer burden for adult liver transplant, which is known as Milan Criteria. Essentially one big tumor smaller than 5 cm or 3 small tumors less than 3 cm each. The tumor can't have left the liver either aka metastasis. However if it's too small (<2 cm ), you don't get priority listing for having that cancer. Kind of like Goldilocks - the tumor has to be just right.
Now first off, you almost never get a primary liver tumor aka hepatocellular carcinoma (HCC) without something wrong in the liver in the first place.
This is usually Cirrhosis aka fibrosis of the liver, which can be caused by Hepatitis C or more commonly drinking too much alcohol too often. The liver fails cause its cells are dead or dying, and the resulting scarring prevents blood from your GI tract from returning properly to your systemic blood. This pseudo-blockage results in fluid backing up in your body, resulting in ascites (fluid in the belly) and pleural effusion (fluid in the lung space) and generalized soft tissue swelling.
The body tries to compensate for this by making alternate paths. Problem is the liver is also a filter, and bypassing the filter through an alternate path affects the brain - a common symptom is confusion and sometimes coma in these patients. Official term is hepatic encephalopathy.
Cirrhosis patients can also literally turn yellow because bilirubin, which occurs from the normal breakdown of red blood cells, can't be processed well by a dysfunctional liver. Liver does a lot of other important stuff too, but I'd go on forever with that - so I'll end that here.
In any case, the only treatment for cirrhosis is getting a new liver - once cirrhosis occurs, it cannot reverse, only worsen. The liver transplant list uses its own criteria known as MELD which I also won't get into here, but generally the sicker you are, the higher you are on the transplant list.
Cirrhosis is essentially a breeding ground for primary liver cancer because cirrhosis is essentially repeated constant inflammation - and all it takes is one cell to heal in the absolutely worst way - and then you have a cancer. This is why cirrhosis patients get yearly liver imaging screening to detect that.
Milan Criteria was created because a good number of liver transplants in cancer patients turned out to have recurrent liver cancer in the new liver. After Milan was implemented, long-term recurrence-free survival improved from 30% to 75%. I believe the sizes used in Milan acts as a surrogate for the likelihood of microscopic metastasis, cancer that's left the liver but too small to be seen in imaging, but don't quote me on that.
Now why did I bring this up? One of the residents asked out loud about why we don't just cut out the cancer.
For one, cirrhosis ensures another one will pop up eventually, and for two, cutting a cancer out also means cutting out good tissue (or semi-okay in a cirrhotic's case) to create the disease-free margin. You don't have much good tissue left in a cirrhosis liver.
You could ablate the cancer by frying it with heat or freezing it, but you again have the issues of damaging normal tissue. Typically excision or ablation is done when there's no chance patient will get a donor liver.
There's also TACE (transarterial chemoembolization) which can be used to shrink tumors, usually back into the limits imposed by Milan criteria. Because if your cancer is too big for Milan, you don't get a liver. There are strict rules for that, and if you break them, your liver transplant service is not getting donor livers.
4 notes
·
View notes
Text
Liver Cancer: Causes, Symptoms, Diagnosis, and Treatment in India
Over the years, liver cancer has become one of the most common types of diagnosis across the globe, and by every case that is examined, it is clear that majority are in the most advanced stages. However with the availability of state-of-the-art equipment and resources, timely intervention is possible alongside medical assistance that helps prolong life in these cases. With this in perspective, India has emerged as one of the best locations for patients looking for assistance with liver cancer as it has a wealth of options in terms of healthcare professionals and medical infrastructure. This blog will assist its readers in providing an insight into why many individuals opt for India as an optimal location for treatment as it discusses and highlights the various methods that can be used to cure liver cancer ranging from liver cancer therapies to new technological developments.
It is important to shed light into what liver cancer is along with its causes as it helps in clearly understanding the bigger picture.
Liver cancer or more commonly referred as Hepatocellular carcinoma (HCC) is a type of tumor that starts formation in a person’s liver and is cancerous In nature as well. It has strong ties with life long illnesses such as cirrhosis, hepatitis, and fatty liver disease. Some symptoms that may help identify the disease at an early stage is weight loss, jaundice, and stomach pain. Even though these symptoms may come serious motives and concern however, people may not even be diagnosed until it is too late. Early diagnosis plays an important role in determining the strategy that is to be used for treatment.
Treatment Options for Liver Cancer in India
1. Surgery (Liver Resection): For patients with localized tumors, surgery to take out the affected area of the liver may lead to a cure. In India, skilled liver surgeons conduct liver resections with high success rates. Sometimes, robotic-assisted surgery is applied, shortening recovery time and enhancing precision. 2. Liver Transplantation: When liver cancer is widespread or liver function is greatly affected, a liver transplant may be the best choice. India has some of the top liver transplant centers globally, providing both living-donor and cadaveric transplants. The success rates of liver transplants in India have consistently increased, thanks to improvements in immunosuppressive therapies and patient care. 3. Ablation Therapies: Ablation treatments like Radiofrequency Ablation (RFA) and Microwave Ablation (MWA) are non-surgical methods used to eliminate cancer cells. These are effective for patients with small, localized tumors. India’s advanced medical facilities offer these procedures with minimal discomfort and fast recovery. 4. Chemotherapy and Targeted Therapy: Chemotherapy is usually used to handle advanced liver cancer, but targeted therapies like Sorafenib have proven effective in stopping tumor growth. Indian hospitals provide access to these medications, along with the latest treatment protocols for managing liver cancer. 5. Radiation Therapy: Radiation therapy, including advanced methods like Stereotactic Body Radiation Therapy (SBRT), is available in select hospitals throughout India. This therapy targets tumors accurately, reducing harm to surrounding healthy tissue.
Why Choose India for Liver Cancer Treatment?
India is recognized for delivering high-quality liver cancer treatment at a lower cost compared to Western nations. Notable hospitals such as Apollo Hospitals, Fortis, and Medanta provide excellent care, equipped with cutting-edge technology. The country also has a large number of highly skilled specialists in oncology, hepatology, and liver transplant surgery. Additionally, India’s expanding medical tourism industry guarantees that international patients receive full support, from travel arrangements to post-treatment care.
📅 Book an Appointment Today! 📞 Contact us at +91 9468115100
0 notes
Text
Qualitative Hepatitis B Causes, Symptoms & Myths
What is Hepatitis B Hepatitis B (HBV) is a chronic condition that has become a worldwide problem. The disease can cause severe damage to the liver and other serious conditions like HCC (hepatocellular cellular carcinoma). About 50% of people infected with Hepatitis B do not know they are infected. This causes the disease to spread to others who are not infected as it is spread through body fluids…
0 notes
Text
Comprehensive Liver Cancer Treatment in Ahmedabad by Dr. Divakar Jain
Dr. Divakar Jain — Your Trusted Destination for Advanced Liver Cancer Treatment in Ahmedabad!
The diagnosis of any cancer brings anxieties, worries and uncertainty about the future life. Liver Cancer is no exception. We understand the challenges and complexities that come with a diagnosis of liver cancer. Led by the esteemed Dr. Divakar Jain, our team provides comprehensive, personalized care to each patient, ensuring the best possible outcomes.
About Liver Cancer
Liver cancers can be of primary liver origin or from secondary spread from other organs. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, characterized by the cancerous transformation of hepatocytes, the main type of liver cells. It typically arises in the setting of chronic liver disease and cirrhosis, although it can also occur in patients without underlying liver conditions.
Other less common primary liver cancer is intrahepatic cholangiocarcinoma, which arise from biliary ducts within the liver.
The commonest secondary liver cancers are from cancers of large intestine (colon) and rectum. Secondary spread to liver, can also be from genitourinary cancers like ovarian cancers, neuroendocrine cancers, pancreatic cancers, stomach and esophageal cancers, lung cancers, breast cancers and other parts of the body.
The presentation of liver cancers may range from no symptoms and incidental detection to jaundice, significant weight loss, itching and abdominal pain. The treatment options for liver cancers range from surgical resection and liver transplantation to medical therapies and interventional radiological strategies.
Advanced Treatment Approaches
Dr. Divakar Jain is a renowned expert in liver cancer treatment, offering a range of advanced therapeutic modalities tailored to each patient’s unique needs. Our comprehensive approach to care encompasses:
Early Detection and Diagnosis:Timely detection is crucial for effective treatment of cancers. Dr. Divakar Jain utilizes state-of-the-art imaging techniques and diagnostic tools to accurately identify and stage the liver cancer, so that best treatment may be offered to the patient.
Multidisciplinary Treatment Planning:Our team of specialists collaborates closely to develop personalized treatment plans that may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy, and downstaging and bridging radiological therapies like TACE, TARE, RFA, MWA.
Surgical Expertise: Dr. Divakar Jain is highly experienced in complex surgical procedures for liver cancer, including liver resection, cadaveric and living donor liver transplantation, and minimally invasive techniques such as laparoscopic and robotic-assisted surgery. We provide consistently good outcomes in these surgeries.
Innovative Therapies:We stay at the forefront of medical advancements, offering access to cutting-edge treatments that may not be available elsewhere.
Supportive Care Services:We understand the importance of addressing the physical, emotional, and psychological aspects of cancer care. Our supportive care services include pain management, nutritional support, psychological counseling, and palliative care to enhance quality of life.
Why Choose Dr. Divakar Jain?
Expertise: Dr. Divakar Jain is a leading authority in liver cancer treatment, known for his clinical excellence, research contributions, and commitment to patient care.
Compassionate Care:We prioritize compassionate, patient-centered care, ensuring that each individual receives the attention, respect, support, and empathy they deserve throughout their cancer journey.
Advanced Facilities:Our clinic is equipped with state-of-the-art infrastructure and technology to deliver the highest standard of care.
Holistic Approach: We believe in treating the whole person, not just the disease. Our holistic approach addresses the physical, emotional, and social aspects of cancer care to promote overall well-being.
Dedicated Support Team: Our team of skilled nurses, oncologists, surgeons, and support staff are committed to providing personalized care and support at every step of the treatment process and providing a one-stop-shop solution for liver cancer.
If you or a loved one is facing liver cancer, trust Dr. Divakar Jain for expert guidance, compassionate care, and innovative treatment options. Contact us today to schedule a consultation and take the first step towards healing and hope.
0 notes
Text
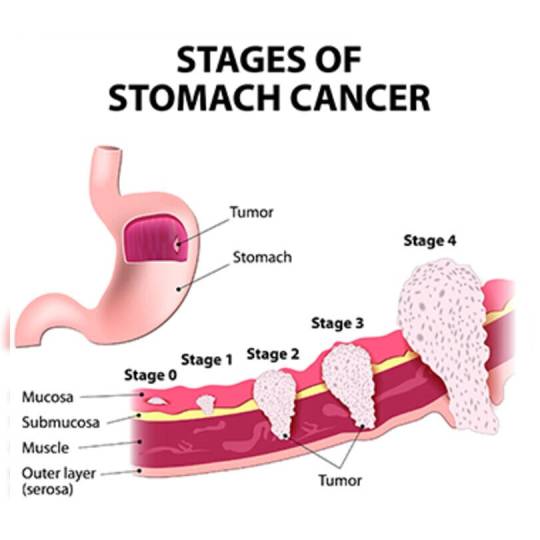
Stages of Liver Cancer: What You Need to Know
Liver cancer is a complex condition that affects thousands of individuals globally. Understanding its stages is essential for early detection, effective treatment, and improved outcomes. In this comprehensive guide, we’ll explore the stages of liver cancer, their symptoms, diagnostic methods, and available treatment options. Whether you or a loved one is facing this diagnosis or seeking preventive knowledge, this article will provide valuable insights.
What is Liver Cancer?

Liver cancer occurs when abnormal cells in the liver grow uncontrollably, forming tumors. The liver, one of the largest organs in the body, plays a vital role in filtering toxins, producing bile for digestion, and storing essential nutrients. When cancer develops in this crucial organ, it can significantly impact overall health.
The most common type of liver cancer is hepatocellular carcinoma (HCC), which originates in the liver cells (hepatocytes). Other types include intrahepatic cholangiocarcinoma (bile duct cancer) and angiosarcoma, though these are less common.
Why is Staging Important?
Cancer staging is a critical step in the diagnostic process. It determines the extent of the disease, guides treatment decisions, and helps predict outcomes. For liver cancer, staging involves assessing:
Tumor size and number.
Spread to nearby blood vessels or organs.
Involvement of lymph nodes or distant sites (metastasis).
Proper staging ensures that patients receive the most appropriate care, from surgery to systemic therapies.
Overview of Liver Cancer Staging Systems
Liver cancer staging uses several systems, with the most common being:
American Joint Committee on Cancer (AJCC) TNM System: Focuses on tumor size (T), lymph node involvement (N), and metastasis (M).
Barcelona Clinic Liver Cancer (BCLC) Staging: Considers tumor stage, liver function, physical health, and cancer symptoms.
Okuda Staging System: Incorporates liver function tests and tumor burden.
Each system has unique criteria, but all aim to provide a clear picture of the disease progression.
Stage 0 (Very Early Stage)
Tumor Size: A single tumor measuring less than 2 cm.
Symptoms: Often asymptomatic, detected incidentally during imaging or routine tests.
Liver Function: Normal liver function with no significant impact on overall health.
Treatment Options:
Surgical Resection: Removal of the tumor while preserving healthy liver tissue.
Liver Transplantation: Ideal for patients with underlying liver disease (e.g., cirrhosis).
Ablative Therapies: Radiofrequency ablation (RFA) or microwave ablation (MWA) for non-surgical candidates.
Stage I (Early Stage)
Tumor Size: A single tumor larger than 2 cm but without vascular invasion.
Symptoms: Fatigue, mild discomfort in the upper abdomen.
Liver Function: Generally preserved, though mild impairments may be present.
Treatment Options:
Curative Approaches: Surgery remains the gold standard.
Localized Therapies: Ablative techniques and stereotactic body radiation therapy (SBRT).
Experimental Trials: Emerging treatments like immunotherapy may be considered.
Stage II (Intermediate Stage)
Tumor Characteristics: One or more tumors larger than 2 cm, with involvement of nearby blood vessels but no distant spread.
Symptoms: Noticeable weight loss, abdominal pain, and jaundice in some cases.
Liver Function: Moderate impairment, depending on underlying liver conditions.
Treatment Options:
Transarterial Chemoembolization (TACE): A minimally invasive procedure delivering chemotherapy directly to the tumor site.
Targeted Therapy: Drugs like sorafenib or lenvatinib may slow tumor growth.
Stage III (Advanced Stage)
Tumor Characteristics: Large tumors involving major blood vessels or nearby organs, without distant metastasis.
Symptoms: Severe abdominal pain, fluid buildup (ascites), and declining overall health.
Liver Function: Significantly impaired, requiring careful management.
Treatment Options:
Systemic Therapy: Combination of targeted therapy and immunotherapy.
Clinical Trials: Investigational drugs and therapies offering new hope.
Stage IV (End-Stage or Metastatic)
Tumor Characteristics: Cancer has spread to distant organs like the lungs or bones.
Symptoms: Intense pain, fatigue, and significant weight loss.
Liver Function: Severely compromised, leading to life-threatening complications.
Treatment Options:
Palliative Care: Focuses on relieving symptoms and improving quality of life.
Systemic Treatments: May include advanced immunotherapies or chemotherapy.
Supportive Therapies: Nutritional support, pain management, and psychological counseling.
Symptoms of Liver Cancer Across Stages
While symptoms vary by stage, common signs include:
Persistent fatigue.
Unexplained weight loss.
Yellowing of the skin and eyes (jaundice).
Swelling in the abdomen.
Loss of appetite and nausea.
Early detection through routine screenings and awareness of these symptoms can make a significant difference in outcomes.
Diagnostic Methods
Diagnosing liver cancer involves multiple tests:
Imaging Studies: Ultrasound, CT scans, and MRIs to visualize tumors.
Blood Tests: Alpha-fetoprotein (AFP) levels, indicative of liver cancer.
Biopsy: A sample of liver tissue examined under a microscope for cancer cells.
These tools help doctors accurately stage the disease and tailor treatments.
Prevention Tips for Liver Cancer
Preventing liver cancer involves addressing risk factors:
Vaccination: Against hepatitis B virus (HBV).
Lifestyle Choices: Avoid excessive alcohol, maintain a healthy weight, and eat a balanced diet.
Regular Screenings: For individuals at high risk, including those with hepatitis C or cirrhosis.
Avoid Toxins: Limit exposure to aflatoxins in food and harmful chemicals.
Conclusion
Liver cancer is a challenging diagnosis, but understanding its stages can empower patients and caregivers to make informed decisions. From early-stage curative treatments to advanced-stage palliative care, modern medicine offers hope at every phase. If you or a loved one is at risk, early screening and preventive measures are the keys to better outcomes.
For expert care and guidance, consider consulting with Action Cancer Hospital, a trusted name in oncology. Together, we can fight liver cancer with knowledge, support, and innovation.
0 notes
Text
Early Signs and Symptoms of Liver Cancer
#liver transplant surgeon in indore#liver specialist in indore#best liver doctor in indore#best liver specialist doctor in indore#liver doctor in indore#liver doctor indore#liver specialist dr in indore#liver specialist hospital in indore#liver specialist indore#best liver specialist in indore#liver hospital in indore#liver specialist doctor in indore#liver transplant in indore#indore liver specialist#liver specialist doctor indore#best liver hospital in indore#Liver transplant surgeon in indore#Liver surgeon in indoor#Liver cancer surgeon in indore
0 notes
Text
Dr. Ganesh Nagarajan: Liver Cancer Treatment in Mumbai
Liver cancer is one of the most serious and life-threatening forms of cancer. As with most cancers, early detection and effective treatment are key to improving survival rates. For patients in India, particularly in Mumbai, access to top-tier liver cancer care is essential. Dr. Ganesh Nagarajan, a renowned surgical oncologist, provides crucial insights into the causes, symptoms, and treatment options available for liver cancer. His expertise has made him a trusted figure in Liver Cancer Treatment in Mumbai, helping many patients navigate this difficult diagnosis.
Understanding Liver Cancer: An Overview
Liver cancer occurs when cells in the liver begin to grow uncontrollably, forming a malignant tumor. There are different types of liver cancer, the most common being hepatocellular carcinoma (HCC), which originates in the main type of liver cells. Less commonly, cancer can begin in the bile ducts or blood vessels within the liver.
In most cases, liver cancer does not show any noticeable symptoms in the early stages. By the time it is diagnosed, the disease may have already progressed to an advanced stage. Dr. Ganesh Nagarajan emphasizes the importance of regular screening, especially for those with risk factors like chronic hepatitis or cirrhosis, as it could lead to early detection and more effective liver cancer treatment in Mumbai.
Causes and Risk Factors of Liver Cancer
Dr. Ganesh Nagarajan explains that liver cancer is primarily associated with chronic liver conditions. Some of the most common risk factors include:
Chronic Hepatitis B and C: Both hepatitis B and C are viral infections that lead to liver inflammation. Over time, this inflammation can cause cirrhosis, which significantly increases the risk of developing liver cancer.
Cirrhosis: This is a condition where scar tissue gradually replaces healthy liver tissue, impairing liver function. Cirrhosis can result from various factors, including long-term alcohol abuse, fatty liver disease, and chronic viral hepatitis.
Alcohol Consumption: Excessive alcohol intake is another leading cause of liver cancer. Over time, it can lead to cirrhosis, which heightens the risk of cancerous cell formation.
Non-Alcoholic Fatty Liver Disease (NAFLD): As obesity and type 2 diabetes become more common, so does NAFLD. This condition can lead to liver inflammation, scarring, and, ultimately, cancer.
Exposure to Aflatoxins: These harmful substances, produced by fungi found in crops, particularly grains and nuts, have been linked to liver cancer.
Symptoms of Liver Cancer
As Dr. Ganesh Nagarajan explains, liver cancer is often referred to as a "silent" disease because its symptoms may not appear until it has reached an advanced stage. Some common symptoms that may indicate liver cancer include:
Unexplained weight loss
Loss of appetite
Upper abdominal pain
Jaundice (yellowing of the skin and eyes)
General weakness and fatigue
Nausea and vomiting
For anyone experiencing these symptoms, seeking an expert opinion from a specialized clinic offering liver cancer treatment in Mumbai is critical. Early diagnosis and immediate treatment offer the best chance of success.
Treatment Options for Liver Cancer
Dr. Ganesh Nagarajan emphasizes that liver cancer treatment in Mumbai varies based on the stage of cancer, overall liver function, and the patient’s health. Some of the most common treatment options include:
Surgery: If the tumor is small and localized, surgical resection can be performed to remove the cancerous part of the liver. In certain cases, a liver transplant may also be considered.
Ablation and Embolization: For patients who are not suitable candidates for surgery, techniques such as radiofrequency ablation (RFA) or transarterial chemoembolization (TACE) can be used to destroy cancer cells or block blood flow to the tumor.
Targeted Therapy: This treatment involves using drugs that specifically target cancer cells while sparing normal cells, helping to slow the progression of the disease.
Chemotherapy: While liver cancer is often resistant to chemotherapy, it may still be used in some cases to shrink tumors or slow their growth.
Immunotherapy: A newer form of treatment, immunotherapy works by stimulating the immune system to attack cancer cells.
Conclusion
Liver cancer remains a challenging diagnosis, but with advances in medical treatments, there is hope. For those in need of liver cancer treatment in Mumbai, Dr. Ganesh Nagarajan's clinic offers expert care and cutting-edge therapies designed to give patients the best possible outcome. With a focus on individualized treatment plans, he is a trusted resource for anyone facing this difficult disease.
FAQs
1. What are the early warning signs of liver cancer?Early-stage liver cancer may not show symptoms, but common signs include weight loss, abdominal pain, and jaundice.
2. Is liver cancer curable?If detected early, liver cancer can be treated effectively, especially through surgery or liver transplant.
3. Who is at risk of developing liver cancer?Individuals with chronic liver diseases, hepatitis B or C, cirrhosis, or excessive alcohol use are at higher risk.
4. How can liver cancer be prevented?Preventive measures include hepatitis vaccinations, limiting alcohol intake, maintaining a healthy weight, and regular screenings for those at risk.
5. Why is Dr. Ganesh Nagarajan considered an expert in liver cancer treatment?Dr. Ganesh Nagarajan is a renowned surgical oncologist in Mumbai, specializing in advanced techniques for treating liver cancer, offering personalized treatment plans for each patient.
For expert Liver Cancer Treatment in Mumbai, consult with Dr. Ganesh Nagarajan and get the best care possible.
Book your appointment today
Book your appointment today: Tap herePhone Number: + 91 77000 58024
Location: Click here to find us on the map
For any inquiries, email us at: [email protected]
Stay connected with us on social media: Facebook | Instagram | YouTube
0 notes
Text
Hepatobiliary Health: An Essential Guide to Liver and Gallbladder Wellness
The hepatobiliary system plays a vital role in our overall health, encompassing the liver, gallbladder, and bile ducts. These organs work in concert to ensure the digestion and absorption of fats, the detoxification of the blood, and the production and excretion of bile. When this system is disrupted, it can lead to a range of hepatobiliary diseases. This blog will delve into the functions of the hepatobiliary system, common diseases affecting it, symptoms to watch out for, diagnostic methods, and available treatments.

The Hepatobiliary System: A Brief Overview
Liver: The liver is a large, multifunctional organ responsible for detoxifying chemicals, metabolizing drugs, synthesizing proteins important for blood clotting, and producing biochemicals necessary for digestion.
Gallbladder: The gallbladder stores bile produced by the liver. During digestion, it releases bile into the small intestine to help break down fats.
Bile Ducts: These ducts carry bile from the liver and gallbladder to the small intestine. The network includes the intrahepatic ducts, which are within the liver, and the extrahepatic ducts, which are outside the liver.
Common Hepatobiliary Diseases
Hepatitis:
Causes: Viral infections (Hepatitis A, B, C, D, E), alcohol abuse, autoimmune conditions.
Symptoms: Fatigue, jaundice (yellowing of the skin and eyes), abdominal pain, loss of appetite.
Treatment: Antiviral medications, lifestyle changes, liver transplantation in severe cases.
Gallstones (Cholelithiasis):
Causes: Imbalance in the substances that make up bile, such as cholesterol and bilirubin.
Symptoms: Severe pain in the upper right abdomen, nausea, vomiting, jaundice.
Treatment: Medications to dissolve gallstones, surgical removal of the gallbladder (cholecystectomy).
Cholangitis:
Causes: Bacterial infection, obstruction in the bile duct (often due to gallstones).
Symptoms: Fever, chills, jaundice, abdominal pain.
Treatment: Antibiotics, procedures to remove obstructions, surgery.
Liver Cirrhosis:
Causes: Chronic alcohol abuse, chronic viral hepatitis, fatty liver disease.
Symptoms: Fatigue, easy bruising, itching, swelling in the legs and abdomen.
Treatment: Medications, lifestyle changes, liver transplantation.
Primary Biliary Cholangitis (PBC):
Causes: Autoimmune reaction that slowly destroys the bile ducts.
Symptoms: Fatigue, itchy skin, dry eyes and mouth, jaundice.
Treatment: Medications to slow disease progression, liver transplantation.
Hepatocellular Carcinoma (HCC):
Causes: Chronic liver disease, cirrhosis, hepatitis B and C infections.
Symptoms: Weight loss, upper abdominal pain, jaundice, swelling in the abdomen.
Treatment: Surgery, liver transplantation, targeted therapy, radiation therapy.
Diagnosing Hepatobiliary Diseases
Early diagnosis of hepatobiliary diseases is crucial for effective treatment. Common diagnostic methods include:
Blood Tests: Liver function tests (LFTs) to check for enzymes and proteins indicating liver damage.
Imaging Tests: Ultrasound, CT scan, MRI to visualize the liver, gallbladder, and bile ducts.
Biopsy: Removing a small sample of liver tissue for examination under a microscope.
Endoscopic Procedures: ERCP (Endoscopic Retrograde Cholangiopancreatography) to examine the bile ducts and pancreas.
Treatment Options
Treatment varies depending on the specific disease and its severity. Options may include:
Medications: Antivirals, antibiotics, bile acid pills, immunosuppressants.
Lifestyle Changes: Avoiding alcohol, maintaining a healthy diet, regular exercise.
Surgical Interventions: Gallbladder removal, liver resection, bile duct surgeries.
Liver Transplantation: For end-stage liver disease or liver cancer.
Preventive Measures
Vaccinations: For hepatitis A and B.
Healthy Lifestyle: Avoid excessive alcohol consumption, maintain a balanced diet, regular exercise.
Regular Check-ups: Especially if you have risk factors for liver disease.
Conclusion
Hepatobiliary diseases can significantly impact one’s quality of life, but early diagnosis and appropriate treatment can manage and even prevent many of these conditions. Understanding the function of the hepatobiliary system and recognizing symptoms early on is key to maintaining liver health. Always consult healthcare professionals if you experience any signs of liver or biliary disease. Stay informed, stay healthy!
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference Short Name: 14GHUCG2024 Dates: December 17-19, 2024 | Venue: Dubai, UAE Email: [email protected] Visit: https://gastroenterology.universeconferences.com/ Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/ Register here: https://gastroenterology.universeconferences.com/registration/ Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/ Call Us: +1 (207) 707-7298 WhatsApp Us: +442033222718

0 notes
Text
TARE Procedure: What to Expect Before, During, and After

Introduction:
Transarterial Radioembolization (TARE) stands as a beacon of hope for individuals battling liver cancer. Its efficacy in targeting tumors directly while minimizing damage to healthy liver tissue has garnered attention worldwide. In Jaipur, patients seeking cutting-edge cancer treatment find solace in the expertise of specialists like Dr. Nikhil Bansal, an interventional radiologist in jaipur renowned for his proficiency in TARE.
This blog serves as your roadmap through the TARE procedure, shedding light on what to expect before, during, and after the treatment.
Causes of Liver Cancer:
Before delving into the TARE procedure, understanding the roots of liver cancer is paramount. Chronic liver diseases like hepatitis B and C, alcohol abuse, nonalcoholic fatty liver disease (NAFLD), and cirrhosis are common precursors to hepatocellular carcinoma (HCC), the primary form of liver cancer. As these conditions progress, they may trigger genetic mutations, culminating in the uncontrolled growth of cancerous cells within the liver.
Prevention:
Prevention, they say, is better than cure. Adopting a healthy lifestyle can significantly reduce the risk of liver cancer. This includes maintaining a balanced diet, limiting alcohol consumption, avoiding high-risk behaviors such as sharing needles, and getting vaccinated against hepatitis B. Regular screenings for chronic liver diseases can also aid in early detection, paving the way for timely intervention.
The TARE Procedure: Before:
The journey through TARE commences with thorough preparation. Prior to the procedure, patients undergo a series of diagnostic tests, including CT scans and angiography, to assess the size, location, and characteristics of the liver tumors. This information guides the interventional radiologist in devising a personalized treatment plan tailored to the patient's specific needs.
During:
On the day of the procedure, patients arrive at the hospital, where they are greeted by a team of experienced healthcare professionals, including Dr. Nikhil Bansal, the tare specialist in Jaipur. After administering local anesthesia, a tiny incision is made in the groin area to access the femoral artery. Using advanced imaging techniques, such as fluoroscopy and cone-beam CT, the interventional radiologist navigates a catheter through the arterial system until it reaches the hepatic artery, the primary blood supply to the liver. Once in position, millions of tiny radioactive beads, encapsulated with a therapeutic dose of radiation, are infused directly into the tumor-feeding vessels, thereby destroying the cancer cells while sparing the surrounding healthy tissue. Throughout the procedure, patients are closely monitored to ensure their safety and comfort.
After:
Following the completion of the TARE procedure, patients are transferred to a recovery area, where they are monitored for several hours to ensure stability. While some individuals may experience mild discomfort or fatigue, these symptoms typically subside within a few days. Over the ensuing weeks and months, the radioactive beads continue to exert their therapeutic effect, gradually shrinking the tumors and alleviating symptoms. Throughout this period, patients undergo regular follow-up appointments with their healthcare team, allowing for ongoing assessment of treatment response and any potential side effects.
Conclusion:
The TARE procedure offers a ray of hope for individuals grappling with the complexities of liver cancer. Under the guidance of skilled specialists like Dr. Nikhil Bansal, interventional radiologist in Jaipur, patients can embark on a journey towards healing with confidence. By understanding what to expect before, during, and after the procedure, individuals can approach treatment with a sense of empowerment, knowing that they are in capable hands.
In essence, the TARE procedure represents a testament to the remarkable strides made in the field of interventional radiology, offering renewed hope and vitality to those in need. As we look towards the future, may the beacon of TARE continue to illuminate the path towards a world free from the burden of liver cancer.
0 notes
Text
Liver Cancer
Are you looking for the best liver cancer surgeon in Hyderabad? Dr. M.S.S. Keerthi is an excellent choice for liver cancer treatment by providing topnotch care for patients, she has treated more than 10000+ cancer patients and currently, Dr. M.S.S Keerthi is working as Sr. Consultant Surgical Oncologist and laparoscopic and robotic Surgeon at Tulasi Hospital, and Evoke Clinic at Securandarbad, Telangana.
With her exceptional expertise, patient-centric philosophy, and steadfast dedication to excellence, Dr. M.S. S Keerthi has firmly established herself as a leading liver cancer surgeon . Whether you seek advanced treatment for liver cancer or personalized care for related concerns, Dr. M.S. S Keerthi offers unparalleled services customized to your individual needs.
What is liver cancer ?
Liver cancer, also known as hepatocellular carcinoma (HCC), is a malignancy that originates in the liver cells. It is among the most prevalent cancers worldwide and a significant cause of cancer-related mortality. Liver cancer can manifest in various forms, including primary liver cancer, which originates within the liver, and secondary liver cancer, which spreads to the liver from other parts of the body.
Stages of the Liver Cancer:
Dr. M.S.S. Keerthi explains the stages of liver cancer and how far spread of cancer occurs:
Stage 0: Cancer is localized, hasn’t invaded deeper tissues.
Stage I: A single tumor up to 2 cm in diameter, confined to the liver.
Stage II: Single tumor larger than 2 cm or multiple tumors, none larger than 5 cm, still confined to the liver.
Stage III: Tumor( s) invade near blood vessels or organs but have not spread distantly.
Stage IV: spread to near lymph bumps or distant organs.
Causes of liver cancer:
Best cancer specialist in Hyderabad ,Dr MSS Keerthi says liver cancer can be caused by various factors that damage the liver cells and disrupt normal cell growth processes. Some of the primary causes and contributing factors to liver cancer include:
Chronic Liver Diseases, like Cirrhosis: One of the leading causes of liver cancer is chronic liver disease, especially cirrhosis. Cirrhosis is often the result of long-term damage to the liver caused by conditions like excessive alcohol consumption, hepatitis B or C infections, or non-alcoholic fatty liver disease (NAFLD).
Hepatitis B or C Infections: Chronic infections with hepatitis B or C viruses can significantly increase the risk of developing liver cancer over time.
Excessive Alcohol Consumption: Prolonged and excessive alcohol consumption can lead to liver damage and increase the risk of liver cancer.
Obesity: Obesity is a known risk factor for liver cancer, as it can lead to the accumulation of fat in the liver, inflammation, and scarring.
Family History: Individuals with a family history of liver cancer may be at a higher risk, as there can be genetic predispositions to the disease.
Symptoms of liver cancer:
The symptoms of liver cancer can vary and may not appear in the early stages. Common symptoms include:
Abdominal Pain or Discomfort: Pain or a feeling of fullness in the upper abdomen is a common symptom of liver cancer.
Jaundice: Yellowing of the skin and eyes (jaundice) can occur when the cancer affects the liver’s ability to process bilirubin.
Unexplained Weight Loss: Significant and unexplained weight loss can be a sign of liver cancer.
Fatigue: A general feeling of weakness and fatigue can result from the cancer’s impact on the liver’s functions.
Diagnosis and Treatment:
Diagnosis: Liver cancer is typically diagnosed through a combination of tests, including imaging tests , blood tests, and sometimes a liver biopsy to confirm the presence of cancer.
Blood tests: Blood Tests may be done to measure situations of certain substances in the blood that can indicate liver function and the presence of liver cancer, similar as alpha- fetoprotein( AFP) and liver function tests( LFTs).
Biopsy: If imaging tests suggest the presence of liver cancer, a biopsy may be performed to confirm the diagnosis. During a biopsy, a small sample of liver tissue is removed and examined under a microscope by a pathologist to look for cancer cells.
Imaging tests: Imaging tests for liver cancer include ultrasound, CT scans, MRI scans, and PET scans. These tests help visualize the liver and discover abnormalities. Ultrasound uses sound waves, CT scans combine X-rays for detailed images, MRI scans use glamorous fields and radio waves, and PET scans highlight cancerous areas using a radioactive tracer.
Treatment: Treatment options provided by Dr. M.S.S. Keerthi for liver cancer depend on the stage of the disease and the patient’s overall health. They can include:
Surgery: Surgical options may involve removing the tumor (partial hepatectomy) or a liver transplant in cases where the cancer is confined to the liver and the patient is a suitable candidate.
Chemotherapy: Chemotherapy drugs can be used to target and kill cancer cells.
Targeted Therapy: Targeted therapy drugs focus on specific molecules involved in the growth and spread of cancer cells.
Radiation Therapy: High-energy X-rays are used to kill cancer cells or slow their growth.
Ablation and Embolization: Procedures like radiofrequency ablation or transarterial chemoembolization can be used to treat liver tumors.
Prevention of Liver cancer:
According to the best liver cancer surgeon in Hyderabad Dr. M.S.S Keerthi, to prevent liver cancer, individuals can take several steps to reduce their risk:
Getting vaccinated against hepatitis B.
Avoiding needle sharing.
Limiting alcohol intake.
Maintaining a healthy weight.
Eating a nutritious diet.
Managing chronic liver diseases.
Why Choose Dr. MSS Keerthi for Liver Cancer Treatment in Hyderabad:
Expert Oncologist: Dr.M.S.S. Keerthi is described as an expert surgical oncologist with more than 15+ years of experience in performing various cancer surgeries. Having specialized in Surgical Oncology from the Cancer Institute, she’s likely to retain a deep understanding of liver cancer and its treatment.
State-of-the-Art Facility: The citation of a state- of- the- art facility suggests that the medical structure where Dr. M.S.S. Keerthi practices are equipped with improved technologies and ultra modern amenities. And other installations like wheelchair accessible, cleaned toilets and proper consulting rooms.
Clinic Location: Dr. M.S.S. Keerthi practices at Tulasi Hospital and Evoke Clinic in Secunderabad, Telangana.
Diagnostic Services under one Roof: The availability of diagnostic services in the same facility can streamline the individual process for patients. Having all necessary experiments and services like stomach cancer treatment, lung cancer treatment, & targeted therapy in one position may conduct to a more effective and coordinated path to diagnosis and treatment planning.
Experienced & Trained Staff: Dr. M.S.S. Keerthi is supported by experienced and trained staff, which implies a collaborative and well-coordinated approach to patient care.
Personal Care, Every Time: Dr. M.S.S. Keerthi is noted for her compassionate and tailored approach to patient care, which includes listening to patients’ concerns and working closely with them to establish personalized treatment programs.
Book An Appointment:-
Dr. M.S.S Keerthi provides the best treatment for various cancer diseases in Secunderabad and Hyderabad. For more information about our comprehensive treatment options, or to request an appointment with the best surgical oncologist in Secunderabad, Hyderabad call +91 9490808080 or Click on Book Appointment for online booking.
0 notes
Text
Exploring the Interplay Between Diseases and Liver Transplant
Understanding the Complexities and Implications
Liver transplant surgery is a life-saving procedure that offers hope to patients with end-stage liver disease and certain liver-related conditions. However, the decision to undergo a liver transplant is often influenced by the underlying disease or condition that necessitates the procedure. In this article, we delve into the intricate connection between diseases and liver transplants, exploring the complexities, implications, and considerations involved.

Liver Diseases Leading to Transplant: Liver transplant is commonly indicated for patients with end-stage liver disease (ESLD), a condition characterized by irreversible liver damage and loss of function. Chronic liver diseases such as cirrhosis, hepatitis B and C, alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), and autoimmune hepatitis are among the primary causes of ESLD. These diseases progress over time, leading to liver failure and ultimately necessitating a transplant to restore liver function and prolong survival.
Hepatobiliary Cancers: Hepatocellular carcinoma (HCC), the most common type of liver cancer, often develops in the setting of chronic liver disease or cirrhosis. In cases where the cancer is confined to the liver and has not spread beyond, liver transplant may be considered as a curative treatment option. However, stringent criteria and careful patient selection are essential to ensure favorable outcomes and prevent cancer recurrence post-transplant.
Metabolic Liver Diseases: Inherited metabolic disorders such as Wilson's disease, hemochromatosis, and alpha-1 antitrypsin deficiency can affect liver function and lead to progressive liver damage. For patients with severe and unmanageable symptoms, liver transplant may offer a chance for improved quality of life and long-term survival. However, the presence of underlying metabolic abnormalities may pose challenges during the transplant process and require specialized pre-transplant evaluation and management.
Acute Liver Failure: Acute liver failure (ALF) is a rare but life-threatening condition characterized by rapid onset of liver dysfunction and hepatic encephalopathy. Causes of ALF include viral hepatitis, drug-induced liver injury, autoimmune hepatitis, and acute fatty liver of pregnancy, among others. Liver transplant may be considered for select patients with ALF who fail to respond to medical therapy or develop complications such as hepatic coma. Timely referral and evaluation are crucial in optimizing outcomes for these patients.
Autoimmune Liver Diseases: Autoimmune liver diseases, including autoimmune hepatitis, primary biliary cholangitis (formerly known as primary biliary cirrhosis), and primary sclerosing cholangitis, are characterized by immune-mediated damage to the liver and biliary tract. While medical therapy is the mainstay of treatment for most patients, those with advanced disease and progressive liver failure may require liver transplant as a definitive treatment option. Careful management of post-transplant immunosuppression is essential to prevent disease recurrence and graft rejection.
Challenges and Considerations: Despite the potential benefits, liver transplant poses inherent challenges and considerations, particularly in the context of underlying diseases. Patient selection, pre-transplant evaluation, and post-transplant management require a multidisciplinary approach involving hepatologists, transplant surgeons, oncologists, and other specialists. Additionally, the shortage of donor organs, immunosuppression-related complications, and the risk of disease recurrence post-transplant are important factors to consider when weighing the risks and benefits of liver transplant in patients with underlying diseases.
The interplay between diseases and liver transplant is multifaceted and complex, with diverse implications for patient management and outcomes. While liver disease treatment in Bangalore, offers a lifeline to patients with end-stage liver disease, hepatobiliary cancers, metabolic disorders, acute liver failure, and autoimmune liver diseases, careful consideration of the underlying disease, patient characteristics, and transplant-related factors is essential in optimizing outcomes and ensuring long-term success. Through continued research, innovation, and collaboration, clinicians and researchers strive to advance our understanding of this intricate connection and improve the care and outcomes of patients undergoing liver transplant for various diseases.
Let’s know what are approaches taken to Liver transplant
Deceased Donor Liver Transplantation (DDLT) and Living Donor Liver Transplantation (LDLT) are two approaches to liver transplantation, each with its own distinct characteristics and considerations.

Donor Source:
Deceased Donor Liver Transplantation: Deceased Donor Liver Transplantation in Bangalore, the liver is procured from a deceased donor who has been declared brain-dead and has consented to organ donation either during their lifetime or by their family after death.
Living Donor Liver Transplantation: In Living Donor Liver Transplantation, the liver is donated by a living donor, typically a family member or close relative of the recipient. The donor undergoes a thorough evaluation process to assess their suitability for donation, including medical, psychological, and ethical considerations.
Timing of Transplantation:
Deceased Donor Liver Transplantation: The timing of Deceased Donor Liver Transplantation depends on the availability of deceased donor organs, which can vary depending on factors such as organ donation rates, waitlist prioritization, and organ allocation policies.
Living Donor Liver Transplantation: Living Donor Liver Transplantation offers the advantage of scheduling the transplant at a time that is convenient for both the recipient and the donor, minimizing the risk of disease progression and optimizing outcomes for both parties.
Graft Size and Compatibility:
Deceased Donor Liver Transplantation: The size and compatibility of the deceased donor liver may not always match the recipient's requirements, leading to potential mismatches in size or blood type. This can sometimes result in a longer wait time on the transplant waitlist or the need for additional surgical techniques to adapt the donor liver to the recipient's anatomy.
Living Donor Liver Transplantation: Living Donor Liver Transplantation allows for a more tailored approach to graft selection, as the donor liver can be selected based on size, blood type compatibility, and other factors specific to the recipient's needs. This often results in a better match and reduces the risk of graft rejection or complications post-transplant.
Waiting Time and Urgency:
Deceased Donor Liver Transplantation: Due to the limited availability of deceased donor organs, patients awaiting Deceased Donor Liver Transplantation may experience longer wait times on the transplant waitlist, particularly for those with less severe illness or lower priority status.
Living Donor Liver Transplantation: Living Donor Liver Transplantation offers the advantage of shorter waiting times, as the transplant can be scheduled based on the recipient's clinical status and urgency of need. This can be particularly beneficial for patients with rapidly progressive liver disease or acute liver failure who may not have the luxury of waiting for a deceased donor organ.
Risk to Donor:
Deceased Donor Liver Transplantation: There is no risk to the donor in Deceased Donor Liver Transplantation, as the liver is procured from a deceased donor who has already passed away.
Living Donor Liver Transplantation: Living Donor Liver Transplantation carries inherent risks to the living donor, including potential complications related to the surgical procedure, anesthesia, and recovery process. However, advances in surgical techniques and donor selection criteria have significantly reduced the risk of complications for living donors in recent years.
while both Deceased Donor Liver Transplantation and Living Donor Liver Transplantation in Bangalore, offer life-saving options for patients with end-stage liver disease, each approach has its own unique characteristics, considerations, and advantages. The choice between Deceased Donor Liver Transplantation and Living Donor Liver Transplantation depends on various factors, including the recipient's clinical status, urgency of need, compatibility, and availability of suitable donor organs. Ultimately, the goal of liver transplantation is to provide the best possible outcome for the recipient while ensuring the safety and well-being of the donor.
For details get the specialists for the Best Liver Transplant Center in Bangalore
#fatty liver treatment in Bangalore#Liver inflammation treatment in Bangalore#Liver disease treatment in Bangalore#Liver transplantation surgery in Bangalore#Deceased Donor Liver Transplantation in Bangalore#Living Donor Liver Transplantation in Bangalore#best liver transplant center in Bangalore#fatty liver#liver treatment center#liver treatment#fastrecoveryoffattyliver#liver care center Bangalore
0 notes
Text
Understanding Liver Cancer: From Causes to Hope
Liver cancer, though not as widely discussed as other cancers, poses a significant health threat globally. It's crucial to break the silence and raise awareness about this complex disease. This blog aims to shed light on liver cancer, covering its types, causes, symptoms, treatment options, and available resources.

What is Liver Cancer?
Liver cancer is the uncontrolled growth of abnormal cells in the liver. It can be primary, originating in the liver itself, or secondary, spreading from other organs. The most common type of primary liver cancer is hepatocellular carcinoma (HCC), accounting for around 80% of cases.
Causes and Risk Factors:
Several factors can increase your risk of developing liver cancer:
Chronic liver diseases: Hepatitis B and C infections, cirrhosis (scarring) due to alcohol abuse or nonalcoholic fatty liver disease (NAFLD).
Family history: Having close relatives with liver cancer increases your risk.
Aflatoxin exposure: A toxin produced by mold on certain foods can contribute to liver cancer risk.
Obesity and diabetes: These conditions are linked to an increased risk of NAFLD, which can progress to liver cancer.
Symptoms:
Early-stage liver cancer often shows no symptoms. However, as the cancer progresses, you might experience:
Abdominal pain or swelling
Loss of appetite and weight loss
Fatigue
Jaundice (yellowing of skin and eyes)
Easy bruising or bleeding
Nausea and vomiting
Diagnosis and Treatment:
Early diagnosis is crucial for better treatment outcomes in liver cancer. To ensure the most comprehensive and effective care, it is essential to consult with the Best Oncologist in Hyderabad. Doctors employ a range of diagnostic tests such as blood tests, imaging scans, and biopsies to accurately identify and assess the extent of liver cancer. The chosen treatment options are contingent on various factors, including the cancer stage, your overall health, and personal preferences. These may encompass surgical interventions, liver transplantation, ablation techniques (employing heat or other methods to destroy cancer cells), embolization (blocking the blood supply to the tumor), chemotherapy, and targeted therapy. Seeking guidance from the Best Cancer Specialist in India ensures that you receive personalized and state-of-the-art care tailored to your specific condition and needs.
Living with Liver Cancer:
A liver cancer diagnosis can be overwhelming, but remember you're not alone. Numerous support groups and resources are available to help you navigate your journey. These can provide emotional support, practical advice, and access to the latest treatment information.
Hope and the Future:
While liver cancer remains a serious illness, significant progress is being made in research and treatment. New therapies are emerging, offering hope for better outcomes and improved quality of life for patients.
0 notes
Text
A Case of Lenvatinib-Associated Cardiomyopathy
A 70-year-old male with hypertension and hepatitis Bassociated cirrhosis and hepatocellular carcinoma (HCC) on lenvatinib therapy presented to the emergency department (ED) with shortness of breath and chest pain for three days. He reported having shortness of breath at rest that worsened with exertion. Initially, his symptoms improved with use of home supplemental oxygen. However, despite oxygen therapy, he developed a constant, left-sided, non-exertional chest pain that did not improve with rest, prompting ED evaluation. At baseline, the patient was able to walk at least one mile without problems but now was only able to walk five feet before developing shortness of breath. He denied orthopnea, paroxysmal nocturnal dyspnea, light headedness, and lower extremity swelling. Of note, the patient was started on lenvatinib one month prior by his oncologist for treatment of his unresectable HCC. However, he recently stopped taking lenvatinib due to dyspnea. Other medications included entecavir and amlodipine. He denied any history of tobacco, alcohol, or illicit substance use and denied any family history of heart disease.
On examination, the patient was afebrile with a heart rate of 88 beats/minute, respiratory rate of 20 respirations/minute, blood pressure of 92/72 mmHg, and oxygen saturation of 97% on room air. Cardiopulmonary examination was notable for a regular rate and rhythm with no murmurs, rubs, or gallops. Chest examines revealed right greater than left bibasilar crackles, and jugular venous distension of 10 cm H2O. There was 1+ pitting edema to bilateral knees.
0 notes