#somatic response
Explore tagged Tumblr posts
Text
What a fucking month. Um, it seems like all this year has been is a rollercoaster.... So, I lost my godmother at the beginning of the month, which was a big stab in the chest, cause she was one of my biggest cheerleaders and a second mom to me. And she was just such a talented artist, designer and baker/cook. So of course, when I go through something hard, my body responds and just as I was starting to feel better health-wise, I got sick again. Yaaaay. It's been scary cause there has been so much death in my family in the last 2 and something years. Despite my fear though, I feel grounded and accepting of everything. I am so grateful to have some of the most magical and loving beings in my life and that's really all that matters to me. That and art.
This is not a ''pity me'' post, this is a ''I'll keep moving forward and soaking in all the good I can get'' post. <3333
#sarajinkipersonal#2022#november#grief#somatic response#and got to see Stromae live this Sunday!!!#happiness
5 notes
·
View notes
Text




Somatic Responses – Tlooz 7"
Somatic Responses release on the short lived Ant-Zen Breakcore sublabel Mirex.
Somatics were deep into their IDM/Electro brand of the genre. Never got the credit they deserved.
Get it from my Google Drive HERE
46 notes
·
View notes
Text
This counts as a “meme”, right?
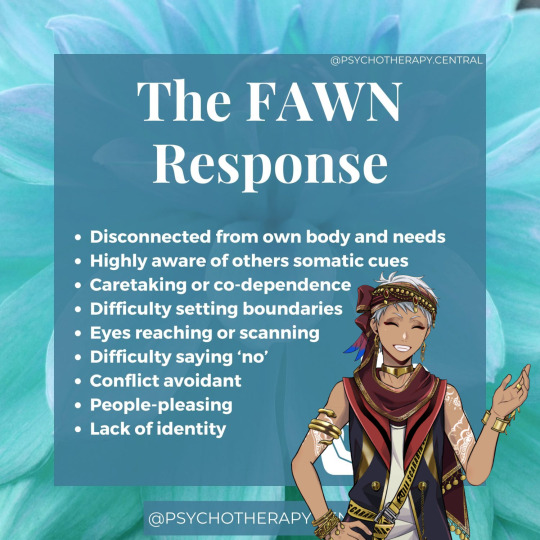
#that moment when you realize that basically all of his personality is based off a trauma response#ofc I do think he’s naturally optimistic and such by nature!#but pair that with his denial and childhood trauma#yeah it’s not looking good for you buddy#twisted wonderland#twst#twst meme#twst kalim#now I don’t think all of the symptoms fit him#like apparently somatic means relating to the body separately from the mind#and Kalim has been shown to be actually really observant about those kinds of details!#just. he has denial baked into him so you can’t tell as well#but you could say that Kalim’s very…#mindful#*bu dum tsss*#okay I’ll see myself out now#sorry for rambling I just sometimes start thinking about Kalim’s trauma and then#oops!#I don’t stop
25 notes
·
View notes
Text
its funny how every kyle episode portrays a different form of ocd
#musings#like we got. scrupulosity. somatic. religious. existential. contamination. responsibility.#and many more that im probably blanking on
10 notes
·
View notes
Text
I DON'T HAVE TO LIE ANYMORE!
#I DON'T HAVE TO LIE ANYMORE ABOUT ANYTHING#IT DOESN'T HAVE TO OVERRIDE ALL OTHER PROGRAMMING EVER AGAIN#HA#MY GOD THAT FEELS LIKE TWO DECADES OF RELIEF#and I found out yesterday. that this year. next winter. it IS two decades. exactly. this is the year. every day i am shown new reminders#that keep me going in my mission to relearn to fully and instinctually trust my self#ever since [redacted therapist] asked me point blank and my IMMEDIATE response was complete disbelief#a firm 'you think there's any universe where i'd feel like i could trust myself? after my nonstop history of failures and being horrible?'#tone “No!” of disbelief#and a horrible way-too-harsh laugh that bolted out before I could strangle it off and stop it.#that woman never coddled my feelings any time I spoke something alarming or bullshit and that was so helpful to me#and the tone she let exist in her voice when she responded to me with a very uncharacteristic “Oh Katie.”#was so. so much more agonizing for me. than her responding with an immediate logical slam-dunk of the truth about healthy behavior and stuf#anyway ramble over i'm so tired. i've done so much trauma work this week i am Drained emotionally#now i see what the past several months but especially especially#the baffling (to me) infuriating out-of-control-speedrun-somatic-processing + every-health-condition-flaring slog that December and January#were for me when I hadn't expected anything to be wrong#...and the extremely specific way this certain zone and particular incident kept coming up over and over and over and over and OVER was not#a bug. it was a feature. thank goodness i trust myself for little things now bc that's the only way i was able to get to this other side#and look back and suddenly realize that my subconscious and body knew what they needed and had a plan in progress the whole time. just like#i rationally say I trust them to have and do.#and that perhaps maybe. for real for real instead of just TELLING myself hard enough a lie that i trust my self and i trust my body and tha#they always know their own needs and timing if really slow down and listen to them f u l l y#anyway. yeah. bye haha i need to stop oversharing on the internet#trauma evolution#shh katie#personal#my god. i wished for this day more than i wished for anything else my whole life. all these many many many many years. what magic.#add to journal#abuse
20 notes
·
View notes
Text

#polyvogal theory#threat responses#trauma responses#trauma and the body#trauma and the nervous systems#somatic therapy
22 notes
·
View notes
Text
“One common (and often overlooked) trauma response is what I called trauma ghosting. This is the body’s recurrent or pervasive sense that danger is just around the corner, or that something terrible is going to happen at any moment.”
Resmaa Menakem
My Grandmother’s Hands
#resmaa menakem#my grandmother’s hands#trauma#racial trauma#racialized trauma#trauma response#trauma ghosting#hypervigilance#somatic healing#quotes#books#book quotes#bookblr
5 notes
·
View notes
Text
i hate the guidance cantrip at a scale unreasonable. i hate it. its so annoying.
#ITS A SPELL. IT HAS VERBAL SOMATIC. YOU HAVE TO CAST IT. IN ADVANCE. YOU FUCKERS#YOU CAN JUST GO 'oh can i get a guidance' in response to you RESPONDING to something. fuck you!
2 notes
·
View notes
Text
in a weird place with my therapy where someone being rude to me is still triggering but now there's this reply guy that stands just out of frame like petter griffin going "ah! looks like someone is projecting their fears onto you again! in this case we can conclude that it's not personal, but the fear and anxiety you are experiencing is due to instinct and [1/474848]"
#text posts#like it IS getting easier identifying somatic responses and divorcing them from the reality of my situation#but the somatic response is going anyway#and i'm not sure how to self soothe
12 notes
·
View notes
Text
ughh i feel like shit but my boss is gonna be really pissed off at me if i go home early lol
#not like sick feel like shit but i've been having weird issues with chest pain and being short of breath lately which is like. concerning#but one of my many somatic anxiety responses so i dont wanna like call out and go to urgent care only to have it just show up as nothing#AGAIN.#i mean at least with my symptoms i wouldnt have to wait forever because they would want to rule out that im not dying or anything but ughh
4 notes
·
View notes
Text
I'm so frustrated by the lack of response to the mass psychogenic illness of law enforcement officials claiming to suffer contact fentanyl poisoning. There were a few studies done that quietly concluded that it's not real, none of the cases were credible, and the symptoms most closely resemble a panic attack or somatic episode.
No one is connecting this to systemic issues in police training and culture and no one is treating this as the canary in the coal mine it is.
Modern police training is functionally cult indoctrination, and intentionally cultivates paranoia. Police learn that everyone is out to get them, danger lurks around every corner, and their only job is to make it home alive after their shift.
They then enter the body of police culture, where questioning the bad behavior of fellow officers is at best strictly socially punished and at worst can get them killed, where they are constantly vigilant to say the right things and portray the right beliefs.
Suddenly, after generations of mainstream culture being generally supportive of police, in the midst of an anxiety-riddled pandemic, there is a highly-publicized backlash against law enforcement. Regular people are saying ACAB, calling cops fascists and murderers and wife-beaters. They're posting officers' service records on social media. Police, unwilling to believe they are evil, experience a cognitive dissonance backlash effect and cling to beliefs that contradict reality.
No one should be shocked - and no one should be hesitant to say - that there is a mental health crisis in law enforcement. They are paranoid, hyper-vigilant, and mired in cognitive dissonance. They have guns and virtually unchecked power to enact violence in their communities. Making up delusional stories about fentanyl is a pretty mild outcome compared to what we should be expecting from these circumstances.
Police aren't just bastards. They're a danger to themselves and others.
19K notes
·
View notes
Video
youtube
Somatic Responses - too2lz
15 notes
·
View notes
Text
the souls that chose to take residence in his realm usually do not stay infinitely. some do, some dont. they wish to leave either by moving on to a decided afterlife or to be embraced. to cease existing , become one with nothingness. it does not bring him joy as he does enjoy the company in a realm otherwise empty of life, but he has a measured distance or detachment in it. few can truly erase the threads tying a soul within reality. by consuming them, they are severed in totality from every and all timelines. they become one with him, they become one with the void.
#✧ ˚ · . ⋆ ┊ ❛ clockwork / study. ❜#✧ ˚ · . ⋆ ┊ ❛ ooc. ❜#( and he doesn't get anything from it in particular ! he already knew everything they did ! )#( its a blip and everything they was or were is gone )#( only he remembers )#( he might have a somatic response as in - rapidly shifting through mortal ages when first absorbing the soul but its really Sympathetic )#( they barely notice it themself )#( hmm i think they do grow in power in a way but..... hm. )
0 notes
Text
youtube
somatic responses -- deadzone
1 note
·
View note
Audio
Listen/purchase: Doomsday Conduit by Somatic Responses
1 note
·
View note
Text
Um. Is it possible to be in a semi-perpetual state of autistic burnout.
#cuz like. i think i might be#im masking 100% of the way 100% of the time i literally can not stop#not just the masking but also all the repression and supression#i can talk about and analyze my feelings clinically but i cant actually feel them fully#which is causing somatic responses#and then theres my obsession with being small and not taking up any space or bothering anyone 🤡#idk. something about my first realization that something was really wrong was being told that crying silently is. not normal
0 notes