#prior authorization
Explore tagged Tumblr posts
Text
A short thread on how to get a health insurance claim denial reversed (UPDATED AGAIN!!)
Originally found on Bluesky here, I am reposting here on Tumblr hoping that this gains some traction coz I know a LOT of folks who could benefit from it here in the US healthcare system.
Please, please, please reblog this and TAG it (if you have additional ideas for tags, go for it).

UPDATE: And then ProPublica added a godsdamned FORM you can use!
UPDATED AGAIN!!
For those of you who are doing the dance of Prior Authorizations -- in the event that your PA is denied, *CALL THEM* and ask specifically WHAT INFORMATION WAS MISSING to cause the denial. DON'T ask "Why was it denied?", ask, "What information was missing?"
When I called to ask why my doctor's submission was denied, I didn't get a straight answer. I called back and asked, "What information was missing that my doctor should have provided for this to be approved?" The rep looked over the form my doctor had submitted and said, "She said you didn't have a sleep study done, and a sleep study showing an OSA diagnosis and 15+ events is required."
Now I DID in fact have a sleep study done, and I had the CPAP prescription (with that exact diagnosis and info on it) to prove it.
So I asked the rep, "If my doctor resubmits the form and confirms that I DID have said study done and DID have said diagnosis and so on, would that get my PA approved?"
"Yep!"
I IMMEDIATELY called my doctor's office to tell her, and sent her the PDF of my CPAP prescription with additional deets. She in turn immediately resubmitted the corrected form, and a couple hours later, VOILA, PA approved.
So be sure to phrase your question CORRECTLY, because IF THEY TELL YOU WHAT YOUR DOCTOR NEEDS TO SAY, THEY'LL ALMOST CERTAINLY APPROVE IT.
#healthcare#us healthcare#us health system#life hacks#reference#insurance#health insurance#resource#resources#signal boost#prior authorization services#prior authorization
843 notes
·
View notes
Text
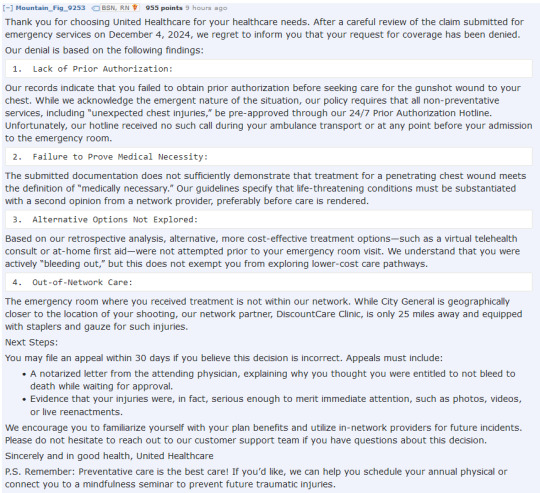
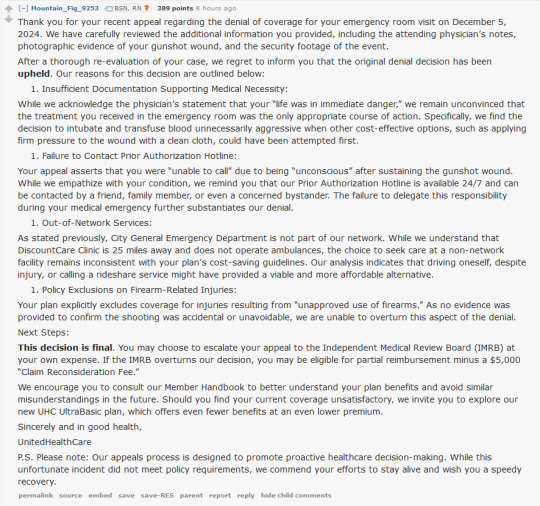
r/nursing is brutal right now regarding the shot ceo.
17 notes
·
View notes
Text
"Issues with Health Insurance Companies, Explained by Doctors - Wall Street Journal"
youtube
5 notes
·
View notes
Text
Petition to abolish the prior authorization process. It's the epitome of what's wrong with the American health care system.
(The link is a gift article so you can access it without the paywall.)
#health care#prior authorization#health insurance#new york times#brought to you by the time united healthcare demanded a prior authorization for the insulin they told me to switch to. as a type 1 diabetic#and then i almost ran out of my old insulin while waiting for the PA to get approved.#prior authorization kills patients and enriches the insurance company. that's all it does.
13 notes
·
View notes
Text
i am in prior authorization hell with Skyrizi. i got a new, better job, but Caremark of course does not want to pay, but they keep closing the PA due to lack of information. bruh. my GI nurse told me when i had an appointment Tuesday she faxed almost 100 pages and had to break the fax up because it kept rejecting for being too large.
they requested more information on Friday afternoon then closed it first thing Monday morning. reopened it, then denied it due to lack of information today. which…it needs a peer to peer but how will we ever get there when they can just close the whole file?
meanwhile, i am overdue for my medication, and they’re not understanding that my bowel obstructions are from scarring that no surgeon wants to take out because of my weight; finally my surgeon and the specialty IBD clinic have decided we do need to proceed but we’ve been talking about this since 2018 or 2019. and it’s all plainly documented, but these assholes are probably running it through AI or some shit and auto denying it. i don’t know.
but my GI nurse convinced the drug rep (I know) to get me a sample which buys me another 8 weeks and like. there’s a lot of garbage healthcare professionals, but they charge 20K a dose for this med so right now, she feels like a miracle worker. that’s it. that’s the post.
2 notes
·
View notes
Text
X93.XXXA is not on UnitedHealthcare's Prior authorization List, and is not covered. Have you tried any conservative therapy such as Phycian directed home therapy, OTC meds and/or physical therapy? You can also just file an appeal with-
3 notes
·
View notes
Text
Medicare Part D — a tragic saga
I'm on one single prescription medication. It's a controlled substance.
I'm on federal insurance for medication. Since I'm in the United States, that means a for-profit third party gets to manage that insurance policy. Though it must meet or exceed specific guidelines from the government.
At the end of 2023, I got a letter from the government saying I'd need to start paying a small monthly premium to the third party, or I could switch to a different third party provider on the back of the letter. I didn't switch, because of ADHD and demand avoidance, it was a small enough amount of money, and I didn't want to risk issues with my medication being denied or delayed with a new insurance company. But I was worried about the future.
Sure enough, at the end of 2024, there was a letter from the government saying that my third party insurance company was upping the premiums to an amount I absolutely wasn't going to pay if I didn't have to. But that I could switch to one of the providers on the back of the letter and have no monthly premiums, while keeping the same 'Medicare Part D' that I already have.
I used the government's website, to make sure my medication was on the list of meds for the new provider. Yes. I made sure my pharmacy was accepted by the new provider. Yes. I used the government's website to switch to the new insurer. I got the new insurance card. I showed it to my pharmacy and updated the records. I went to my pain doctor and renewed my prescription for the next six months. I went to the pharmacy and picked up the medication. I went to the mailbox and opened a letter from my new insurance company.
They were kind enough to fill the prescription this time, as a courtesy. But they want a prior authorization or special exception completed before I request a refill. And told me to call my prescriber.
I called my prescriber's office. The automated reception message said that if I was calling about prior authorization, to contact the pharmacy and have them contact the doctor directly (who would then fill out and send documents to the pharmacy, who would then send the documents to the insurance company).
I went to my pharmacy in person (calling is not a good way to get things done there). Because my medication is a controlled substance (which is part of why it needs prior authorization), refills can't be requested until two days before they're due to run out. And prior authorizations can't be requested unless it's part of a refill request.
So, in order to keep from running out of an important medication, I'm supposed to contact my prescriber, who wants me to contact the pharmacy, who needs me to wait until I'm supposed to be almost out of medication before they can start the process of asking my doctor to write a note and send it to the pharmacy so they can send it to my insurance company explaining why I need the medication my doctor prescribed, so that my insurance can decide whether they'll pay for it (despite me having been on this same medication and this same government plan, through a different third party, for years).
#us healthcare#us health insurance#us health system#medicare#medicare part d#prior authorization#disability#pain medication#prescription medication
3 notes
·
View notes
Text
Doctor said I could have Androgel
Insurance said lemme think about it
Fuckers
#bcbs#blue cross blue shield#These same fuckers tried to put me on chemo for my skin condition as opposed to the med my Doc was trying to prescribe me#prior authorization#insurance#cw medical#tw medical#trans hrt#transgender#nonbinary#androgel
7 notes
·
View notes
Text
Whistleblower Exposes Health Insurers' Most Evil Scheme
youtube
#health insurance#prior authorization#medicine#healthcare#medical insurance#fraud#medical fraud#insurance fraud#medical malpractice#american medical association#congress
11 notes
·
View notes
Text
Insurance: Healthcare Workers' Perspective (i.e why it sucks)
1. Why Doctors Don't Carry Your Insurance
This was one of the most surprising things to learn when I started working in a dr's office. Insurance sucks just as much for providers as it does for the patients. (The only upside is we have a separate hotline for calling).
Doctors have to pay (quite a lot of money $$$ btw) to register as providers with insurance. Each individual company (BCBS, USAA, Kaiser, etc) requires a fee, and often will have different processes for registration. This process is not instantaneous, either, but can take anywhere up to 2 years.
That is why many younger/newer providers will often only carry a couple insurances. So the more insurances a provider carries, the more they fought and paid for accessibility for their patients.
2. Prior Authorization
“Physicians spend an enormous amount of time fighting these prior authorization rejections to get patients the therapies that they need,”
-Jack Resneck Jr., MD
What doctors wish patients knew about prior authorization
One major problem in healthcare, which one of our admins talks about in the insurance section, is prior authorization.
I have personally worked in healthcare on and off for about 3 years. At one point, I was a receptionist for a busy ENT clinic, where I helped file medical and insurance paperwork and talked to just about e v e r y insurance company there is the US.
One of the most common (and incredibly frustrating) forms was prior auth, and everyone involved absolutely hates this form. The doctor, the MA's, the patient, the insurance workers you call, etc. Often, we have to call back and forth over a period of weeks to even months to get a patient a single medication that is very often necessary for living.
Mind you, this again takes a lot of precious time. Dr. Resneck went on to say that, "We physicians often find ourselves fighting over and over and over through a series of appeals to get the patient the medication or the test or the treatment that they need," which I can attest is absolutely true! Talk about incredibly dangerous for continuity for care and health of the patient!
On top of how busy the clinic and physicians are, these authorizations and appeals often go to the support healthcare workers, like receptionists or MA's, to handle.
Most often was a medication that was simply being refilled by a new doctor, or occasionally the exact same doctor (the patients window of insurance viability had just lapsed)! A patient could have been on a medication for YEARS and suddenly the insurance would be dragging their feet. And they won't talk to patients, the point-blank will only discuss and haggle with physicians and their representatives (ie. ME).
There is lot more to this subject, but unfortunately, I have other homework to get to.
Did either of these surprise you?
3 notes
·
View notes
Text
I already knew that 'prior authorisation' policies had gotten out of hand, but it actually hit me personally today.
The doctor bumped up my Lyrica, a non-narcotic pain management medication, and when I called the pharmacy to ask if it would be ready to get tomorrow, they explained that it had hit a PA. The reason?
My doctor wants me to be taking 100mg in the morning, 50 in the afternoon, and 100 at bedtime. She prescribed this in 50mg capsules. The insurance "does not allow" for more than 3 pills of this med per patient per day.
Does Not Allow. As if an insurer understands the needs of a patient, or should ever have a say over a medical professional.
This means the doc has to send 2 different prescriptions in. One total 50mg capsule for the midday dose, two total capsules per day for the morning and night.
So I have to organise and remember two different pills for the same med every day; taking one bottle everywhere with me so I can take it around lunch, keeping the other home for my pill organiser.
What a giant pain in the ass. What a totally weird restriction.
What's even worse is that I literally just took my last full dose today, and this med can cause pretty nasty withdrawal symptoms.
I have 2 more 50mg doses I am going to space out for the next 2 days- *just in case* asking them to rewrite scripts in a way my insurance approves of doesn't get done in the hours the primary care office and the pharmacy are both open tomorrow.
#insurance#prior authorization#medications#fibromyalgia#PA's are completely ridiculous#just shows how little they fucking care#personal
3 notes
·
View notes
Text
Signal booooost to all my New Jersey people!
And to any Americans on the fence about voting next Tuesday, legislation like THIS is why voting in every state and local election is so important!
#vote#dr glaucomflecken#medicine#insurance#adulting#medical stuff#prior authorization#voting#politics
2 notes
·
View notes
Text
@thebibliosphere I hear you.
FWIW, the state of Illinois has now made step therapy illegal (as it applies to prior authorizations) so insurance companies can no longer insist you take a cheaper / less potent drug and fail on it before they agree to pay for the actual drug you need. Other states have similar bills in the works.
The AMA podcast covers it here:
youtube
I’ve got my tumblr inbox turned off so I really have to commend the person who actually emailed me to let me know they don’t like the things I’ve posted about the UnitedHealth CEO being murdered on their commitment to their beliefs.
But seen as how you emailed me from a dud email that appears to be bouncing back replies and I really wanted to address something you said to me about violence begetting violence:
My migraine medication, the medication I was given for my debilitating neurological disease that has gotten so bad I spent most of this year actively suicidal, costs $1300 a month.
My insurance covered it. But only because my doctors office went to fucking war for me because I’m a high anaphylaxis risk for the drugs the insurance wanted me to try.
Because that’s the thing.
My doctors knew, based on my documented medical history, I likely wouldn’t be a good fit for the “first line” of preventative migraine drugs, but because of insurance, I had to be given drugs that were contradictory to my other life threatening conditions, because otherwise insurance wouldn’t cover anything else.
I failed them. Spectacularly and with an anaphylactic reaction to one of them. And I was still warned insurance would fight me because I hadn’t tried the remaining drug they wanted me to try.
A drug which I would have to take in an ER waiting room because my mast cell disease is unpredictable but insurance wouldn’t cover in-patient treatment to let me try it safely under medical supervision.
Is that not violence?
Were all the times I was denied coverage for vital and necessary procedures that could have prevented my disabilities from worsening not violence?
Maybe not in the sense you mean. But I assure you it felt very much like violence to me.
Do I condone murder? No, obviously. But I’m also sick and tired of people pretending that what is happening to the American people every day isn’t eugenics through class warfare.
Violence begets violence.
It sure fucking does.
Maybe these insurance companies should have thought of that first.
28K notes
·
View notes
Text
Jessica Glenza at The Guardian:
The US health secretary Robert F Kennedy Jr and Dr Mehmet Oz announced a voluntary agreement with insurance companies to change prior authorization practices – where private health insurers require patients to ask for permission before they can receive medical treatment. The majority of Americans receive health insurance through a private company, whether through an employer, or a privatization of public health insurance programs, such as Medicare Advantage.
Prior authorization is an insurance company practice that is both common and abhorred. There are whole social media accounts devoted to egregious examples of it, campaigns for change built around it, and, in Oz’s words, there is “violence in the streets” over prior authorization – an allusion to the broad daylight killing of an insurance company CEO. Oz said repeatedly in a press conference on Monday that 85% of Americans or their loved ones had experienced a delay or denial of care thanks to prior authorization.
“The pledge is not a mandate, this is not a bill or rule – this is an opportunity for industry to show itself,” said Oz, who heads the enormous federal health insurance bureaucracy, the Centers for Medicare and Medicaid (CMS). The agency oversees the health insurance of about 68 million seniors through Medicare and about 71 million low-income and disabled Americans through Medicaid. “It’s a good start,” said Oz, “and the response has been overwhelming.” Kennedy called the agreement “momentous” and said it would help make the health system, “work to make our country healthy again”. The announcement of voluntary measures echoed one made earlier in the year by Kennedy, who announced the administration had an “understanding” with food companies to phase out synthetic dyes. Food companies later told reporters there was no agreement.
Concurrently, Republicans are working to push a bill through Congress that is expected to result in at least 16 million Americans losing health insurance in the next decade. The bill would add red tape to Medicaid and, advocates say, “punish” states that expanded care to the low-income.
With biblical references and a bullet point chart, Trump administration officials, two Republican members of Congress and even an actor who played a doctor on TV – Eric Dane of Grey’s Anatomy – laid out their hopes for insurers to implement this voluntary agreement that they said covered 275 million Americans. Should they do so, insurers would work to standardize the prior authorization approval and deliver decisions faster and near real-time (not over the course of, say, weeks). Additionally, insurers would reduce the number of procedures and drugs subject to prior authorization, honor existing prior authorization approvals in the event a patient switches insurers in the course of care and build a “public dashboard” of how the industry is doing which would allow “medical professionals” to review every denial.
RFK Jr. and Dr. Öz announced a voluntary agreement with insurance companies to change prior authorization practices.
#Health Insurance#Health Care#Robert F. Kennedy Jr.#Dr. Mehmet Öz#Mehmet Öz#Medicaid Expansion#Prior Authorization#Medicare Advantage
1 note
·
View note
Text
Claims Denial Management Services | Minimize Denials
Denial Management is one of the most important processes that can make or break the smooth functioning of a practice’s revenue cycle. There are two financial aspects to a denied claim - first is the ��lost” revenue due to the improper prior authorization or the lack thereof and the second is the cost associated with reworking a denied claim, which entails a lengthy appeals process. Recent studies indicate that physicians spend anywhere from $30 to $100 or upward to rework a claim - costing the practice $14,400 (lowest estimate) annually based on 40 denied claims per month, not including the preliminary cost of submitting a claim.
#denial management services#claim rejection management#prior authorization#medical billing services#accounts receivables management
0 notes
Text
Optimizing prior authorization is key to avoiding surgery delays and financial setbacks in ASCs. Implementing structured workflows and leveraging technology can help ensure timely approvals and seamless patient care.
0 notes