#prenatal care
Explore tagged Tumblr posts
Text
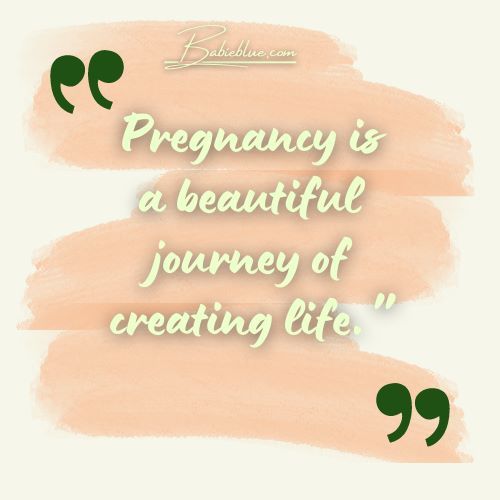
The agony these people are going through is beyond compare, the amount of people giving birth every day and the amount of children lost is heart-shattering, but the powers still refuse to call this a genocide.
#free gaza#free palestine#gaza strip#irish solidarity with palestine#palestine#gaza#news on gaza#al jazeera#boycott israel#israel#Pascale Coissard Rogeret#Emirati Hospital#Rafah#Maha#Infant loss#Maternity#Paternity#Prenatal care#Postnatal care#Pregnancy#Childbirth#Medecins Sans Frontiers#Doctors Without Borders
60 notes
·
View notes
Text

[ID: A graphic that shows a realistic picture of a fetus. Underneath it, words read, “Know the facts about fetal pain.]
Fetal pain is real and have a right to access pain relief and proper health care in that regard. Parents also have a right to be fully informed of this reality when considering medical options that may physically harm the fetus.
AAPLOG Practice Guideline 2: Fetal Pain
81 notes
·
View notes
Text
As the fetus's rights increased, mother's just kept diminishing. Poor pregnant women were hauled into court by male prosecutors, physicians, and husbands. Their blood was tested for drug traces without their consent or even notification, their confidentiality rights were routinely violated in the state's zeal to compile a case against them, and they were forced into obstetrical surgery for the "good" of the fetus, even at risk of their own lives.
Here are just a few of the many cases from the decade's pregnancy police blotter and court docket:
• In Michigan, a juvenile court took custody of a newborn because the mother took a few Valium pills while pregnant, to ease pain caused by an auto accident injury. The mother of three had no history of drug abuse or parental neglect. It took more than a year for her to get her child back.
• In California, a young woman was brought up on fetal neglect charges under a law that, ironically, was meant to force negligent fathers to pay child support. Her offenses included failing to heed a doctor's advice (a doctor who had failed to follow up on her treatment), not getting to the hospital with due haste, and having sex with her husband. The husband, a batterer whose brutal outbursts had summoned the police to their apartment more than a dozen times in one year alone, was not charged —or even investigated.
• In lowa, the state took a woman's baby away at birth even though no real harm to the infant was evident—because she had, among other alleged offenses, "paid no attention to the nutritional value of the food she ate during her pregnancy," as an AP story later characterized the Juvenile Court testimony. "[S]he simply picked the foods that tasted good to her."
• In Wyoming, a woman was charged with felony child abuse for allegedly drinking while pregnant. A battered wife, she had been arrested on this charge after she sought police protection from her abusive husband.
• In Illinois, a woman was summoned to court after her husband accused her of damaging their daughter's intestine in an auto accident during her pregnancy. She wasn't even the driver.
• In Michigan, another husband hauled his wife into court to accuse her of taking tetracycline during her pregnancy; the drug, prescribed by her physician, allegedly discolored their son's teeth, he charged. The state's appellate court ruled that the husband did indeed have the right to sue for this "prenatal negligence."
• In Maryland, a woman lost custody of her fetus when she refused to transfer to a hospital in another city, a move she resisted because it would have meant stranding her nineteen-month-old son.
• In South Carolina, an eighteen-year-old pregnant woman was arrested before she had even given birth, on the suspicion that she may have passed cocaine to her fetus. The charge, based on a single urine test, didn't hold up; she delivered a healthy drug-free baby. Even so, and even though the Department of Social Services found no evidence of abuse or neglect, State prosecutors announced that they intended to pursue the case anyway.
• In Wisconsin, a sixteen-year-old pregnant girl was confined in a secure detention facility because of her alleged tendencies "to be on the run" and "to lack motivation" to seek prenatal care.
Certainly society has a compelling interest in bringing healthy children into the world, both a moral and practical obligation to help women take care of themselves while they're pregnant. But the punitive and vindictive treatment mothers were beginning to receive from legislators, police, prosecutors, and judges in the 80s suggests that more than simple concern for children's welfare was at work here. Police loaded their suspects into paddy wagons still bleeding from labor; prosecutors barged into maternity wards to conduct their interrogations. Judges threw pregnant women with drug problems into jail for months at a time, even though, as the federal General Accounting Office and other investigative agencies have found, the prenatal care offered pregnant women in American prisons is scandalously deficient or nonexistent (many prisons don't even have gynecologists)—and has caused numerous incarcerated women to give birth to critically ill and damaged babies. Police were eager to throw the book at erring pregnant women. In the case of Pamela Rae Stewart of San Diego the battered woman charged with having sex against her doctor's orders—the officer who headed up the investigation wanted her tried for manslaughter. "In my mind, I didn't see any difference between born and unborn," Lieutenant Ray Narramore explains later. "The only question I had was why they didn't go for a murder charge. I would have been satisfied with murder. That wouldn't have been off-base. I mean, we have a lady here who was not following doctor's orders."
Lawmakers' claims that they just wanted to improve conditions for future children rang especially false. At the same time that legislators were assailing low-income mothers for failing to take care of their fetuses, they were making devastating cuts in the very services that poor pregnant women needed to meet the lawmakers' demands. How was an impoverished woman supposed to deliver a healthy fetus when she was denied prenatal care, nutrition supplements, welfare payments, and housing assistance? In the District of Columbia, Marion Barry declared infant health a top priority of his mayoral campaign—then cut health-care funding, forcing prenatal clinics to scale back drastically and eliminate outright their evening hours needed by the many working women. Doctors increasingly berated low-income mothers, but they also increasingly refused to treat them. By the end of the decade, more than one-fourth of all counties nationwide lacked any clinic where poor women could get prenatal care, and a third of doctors wouldn't treat pregnant women who were Medicaid patients. In New York State, a health department study found that seven of the state's counties had no comprehensive prenatal care for poor women whatsoever; several of these counties, not so coincidentally, had infant mortality rates that were more than double the national average. In California in 1986, twelve counties didn't have a single doctor willing to accept the state's low-income MediCal patients; in fact, the National Health Law Program concluded that the situation in California was so bad that poor pregnant women are "essentially cut off from access to care."
-Susan Faludi, Backlash: the Undeclared War Against American Women
#susan faludi#female oppression#prenatal care#low income women#pregnancy#amerika#failed state#court-ordered kidnapping#USA is a society that wants to die#misogyny
48 notes
·
View notes
Text

Midwife
“Major Christine Gundel, 779th Medical Group nurse midwife, checks on Monica McCoy, Public Affairs Specialist for Naval Sea Systems Command in Washington D.C. and patient at the Maternal Child Unit at Malcolm Grow Medical Center, before her scheduled cesarean-section. (USAF photo by Tech. Sgt. Suzanne M. Day)” - via Wikimedia Commons
#midwife#midwifery#wikipedia#wikipedia pictures#wikimedia commons#medicine#medcore#medicalcore#medicore#medical#medical professionals#healthcare#healthcare professionals#hospitals#hospital#hospitalcore#medical aesthetic#hospital aesthetic#womens health#womens healthcare#prenatal care#postnatal care
8 notes
·
View notes
Text
#reproductive rights#reproductive justice#black women#women's rights#black men#election 2024#harris walz#lmsu#rip#prenatal care#husbands' right
4 notes
·
View notes
Text

Buy healthcare franchise in india
This comprehensive guide will help you navigate the various stages of pregnancy and provide valuable insights into maintaining a healthy, joyful journey.
franchise in india
#Pregnancy#Healthy Pregnancy#Prenatal Care#Pregnancy Nutrition#Exercise During Pregnancy#First Trimester#Second Trimester
3 notes
·
View notes
Text
Pregnancy: What to Expect and How to Prepare
Embarking on the journey of pregnancy can be both exciting and overwhelming. This comprehensive guide offers valuable insights into what to expect during pregnancy and how to prepare for this transformative experience. From the early stages of conception to the final moments of labor and delivery, you'll find a wealth of information on prenatal care, nutrition, exercise, and maintaining a healthy lifestyle. We'll address common pregnancy symptoms, potential complications, and provide tips for managing discomfort. Additionally, we'll delve into the emotional aspects of pregnancy and offer guidance on creating a supportive environment. Get ready to navigate pregnancy with confidence and embrace the joy of welcoming your little one into the world.
#pregnancy#expectant mothers#pregnancy preparation#prenatal care#pregnancy tips#pregnancy advice#pregnancy journey#pregnancy support#pregnancy guide#pregnancy essentials#pregnancy nutrition#pregnancy health#pregnancy complications#pregnancy discomforts#pregnancy milestones#pregnancy timeline#pregnancy exercise
5 notes
·
View notes
Text

Managing diabetes during pregnancy with insulin is crucial to ensure the health of both the mother and the baby. Proper insulin therapy can help control blood sugar levels and reduce the risk of complications, such as premature birth and birth defects.
Read More: https://www.drshubhragoyal.com/welcome/blogs/diabetes-management-during-pregnancy-with-insulin
#Insulin Dosage#Diabetes Management#Diabetes during the First Trimester#Prenatal Care#diabetes management during pregnancy#impact of diabetes on foetal development#Best Gynaecologist in Agra#Gynaecologist in Agra#Shubhra Goyal Gynecologist#Best Gynecologist Doctor In Agra#Top Gynaecologist In Agra
2 notes
·
View notes
Text
Childbirth Preparation: A Path of Maternal Empowerment
Discover how to prepare for a calm and healthy childbirth. This comprehensive guide offers tips, practical advice, and emotional guidance for mothers seeking a positive birthing experience.
The journey of motherhood is filled with unique and challenging moments, and childbirth preparation is one of the most significant milestones on this journey. As you prepare to welcome your baby, it’s natural to feel a mix of emotions – excitement, anxiety, and curiosity. In this comprehensive guide, we delve into the process of childbirth preparation, providing essential information, practical…

View On WordPress
#Calm childbirth#Childbirth preparation#Emotional preparation#Healthy pregnancy#motherhood#Natural childbirth#Parenthood#Postpartum care#Prenatal care#Tips for mothers
2 notes
·
View notes
Text
Babie Blue Pregnancy quotes



#women#pregnancy health#quotes#health#babieblue#prenatal care#pregnancy calculator#insurance#baby blue#beautiful quote#quoteoftheday#babie blue#body contouring
4 notes
·
View notes
Text
Troubled by Early Pregnancy Symptoms? Try These Adjustment Methods!
It also touches on the importance of prenatal care and provides guidance for expectant mothers. Additionally, it discusses considerations for multiple pregnancies and advanced maternal age. Throughout the article, we will also highlight the significance of maternity clothing and introduce the GoMamee brand as a trusted provider of stylish and comfortable maternity wear.

1.How Can I Tell I Am Pregnant?
For women with a history of sexual intercourse and regular menstruation, it is recommended that pregnancy should be suspected for more than 10 days after menstruation. It can be determined by early pregnancy reaction, early pregnancy test paper, or blood hCG test, and you can also check ultrasound test after 6 weeks of menopause.
2.I Don't Know If I'm Pregnant, But I Had a Chest X-Ray For a Medical Checkup. Will It Affect My Child?
Within 2 weeks of fertilization, or 4 weeks of pregnancy, most drugs or medical examinations have an "all or nothing" effect on the embryo. If there is an effect, it may die, miscarry or stop developing. If the fetus survives, there is nothing to worry about; secondly, the radiation exposure dose from x-ray examination is much lower than the dose that is harmful to the fetus. Therefore, please do not easily give a death sentence to life.
3.What Should I Do If My Early Pregnancy Reaction Is Too Severe?
Anorexia and vomiting are relatively normal early pregnancy reactions. Pregnant mothers should self-regulate their diet, try to choose foods that promote appetite, are rich in nutrients and easy to digest, eat less and more meals, and also take some vitamin B6 to reduce the symptoms of pregnancy vomiting.
If you still have very serious pregnancy vomiting after self-regulation, even accompanied by weight loss, it is recommended to go to the hospital for liver function, blood electrolyte test and urine ketone body test, which may require hospitalization, intravenous supplementation of water, electrolytes and heat card, and at the same time, let the stomach and intestines rest.
4.Can I Eat Seafood During Pregnancy?
Yes. Seafood itself will not affect the fetus, but seafood may have parasites, so it is important to eat fresh, hygienic and cooked seafood.
5.Do I Need To Reduce The Fetus If The Ultrasound Examination Indicates a Triplet Pregnancy?
In general, it is recommended to reduce the fetus if there are three or more fetuses alive. In addition, there is a high risk of hypertensive disorders such as pre-eclampsia in late pregnancy and complications such as postpartum hemorrhage during delivery, which endanger the life of mother and child. The risk of decompensation is mainly to cause miscarriage and preterm delivery. Early reduction is generally recommended to reduce complications in the middle and late stages of pregnancy.
6.What Should I Pay Attention To When I Am Pregnant At An Advanced Age?
The age of delivery ≥ 35 years old is an advanced pregnancy. Because after women reach 35 years old, many aspects of their bodies start to go downhill relatively, and pregnancy at this time will increase the incidence of baby malformations; at the same time, the risk of intrauterine growth retardation, miscarriage and premature birth increases, and advanced pregnant women are prone to combined heart disease of pregnancy, gestational hypertension disease and gestational diabetes. Therefore, extra attention should be paid to pregnancy care, and regular prenatal checkups should be ensured.
In addition to the routine 11-13+6 weeks NT ultrasound and 20-24 weeks ultrasound for major abnormalities, amniocentesis for fetal chromosomes is recommended directly after 18 weeks of gestation for older pregnant women. If you are not willing to perform amniocentesis or have contraindications to amniocentesis, you can also choose a non-invasive DNA test first, but you should understand the limitations of non-invasive DNA tests.

7.Can I Have a Fetus With Thickened Nt Value? It Needs To Be Determined On a Case-By-Case Basis.
The thickness of NT value is directly proportional to the incidence of chromosomal abnormalities and can better evaluate the risk of trisomy 21, trisomy 18, trisomy 13, etc.; it is also associated with congenital structural malformation of the fetal heart, which is the most common cause of non-chromosomal abnormal NT thickening. Secondly, NT thickening is also associated with other structural malformations of the fetus: such as malformations of the skeletal system, diaphragmatic hernia, anterior abdominal wall defects (umbilical bulge), and fetal dyskinesia syndrome. In addition, thickened NT is also associated with spontaneous abortion, etc.
A completely normal fetus may also have thickened NT. When you get the result of NT thickening, please do not be overly nervous and upset, but go to the hospital on time. We have professional experts to help you further investigate the possible risks.
8.What Do I Need To Pay Attention To Now That I Am Pregnant With My Second Child After My First Child Was Delivered By a Cesarean?
It is appropriate to have another pregnancy after cesarean section with an interval of more than 2 years and less than 10 years. The shorter the interval, the greater the risk of uterine rupture in another pregnancy. Pregnant mothers with scarred uterus can first have an ultrasound examination to understand the location of the embryo in relation to the scar. If the embryo lays on the scar, it is considered a "scarred pregnancy" and is at higher risk of uterine rupture and hemorrhage. If the bed site is not in the scar, pregnancy can continue, but there is still a risk of uterine rupture during pregnancy, so it is recommended to strengthen perinatal health care regularly.
9.Can I Play With Cell Phones And Computers During Pregnancy?
Yes. The radiation dose of daily electrical appliances is very small and will not cause harm to the mother and fetus. The normal use of cell phones for phone calls has no effect on the fetus, but it is not recommended to play on cell phones for a long time. It is recommended to take a walk outdoors more often during pregnancy to relax, pay attention to rest more, develop good habits of life and rest, don't stay up late, avoid straining and do regular maternity checkups.
10.How To Supplement Folic Acid During Pregnancy?
In order to prevent fetal neural tube malformation, the demand for folic acid during pregnancy is high.
Experts recommend starting oral folic acid 0.4 mg as early as three months prior to pregnancy preparation. Women with a history of births with neural tube defects, as well as those with diseases affecting folic acid metabolism such as diabetes, epilepsy, or those found to have genetic defects that impair folic acid metabolism, need to increase their folic acid intake as prescribed by their doctors on a case-by-case basis.

Conclusion
In conclusion, this article provides valuable insights for expectant mothers, covering various aspects of pregnancy. It emphasizes the importance of timely pregnancy confirmation and regular prenatal care. Additionally, it highlights the significance of choosing appropriate maternity clothing, and the GoMamee brand stands out as a reliable option offering fashionable and comfortable options for expectant mothers. By considering the information presented here and selecting quality maternity clothing from GoMamee, pregnant women can enhance their comfort and style during this special time in their lives.
2 notes
·
View notes
Text
#rural america#women's healthcare#maternity care#obstetrics#abortion access#prenatal care#maternity care deserts#reproductive healthcare#women's health
0 notes
Text
Explore the 5 Importance of Prenatal Care with Verve College. Learn how early and regular check-ups ensure the health of both mother and baby. Essential tips for safe pregnancies!
0 notes
Text

Midwife
#midwife#midwifery#wikipedia#wikipedia pictures#wikimedia commons#medicine#medcore#medicalcore#medicore#medical#medical professionals#healthcare#hospitalcore#hospitals#hospital aesthetic#prenatal care#postnatal care#womens health#womens healthcare#healthcare professionals#healthcare provider
9 notes
·
View notes
Text
Pregnancy Headaches
Pregnancy, a beautiful journey, often comes with its share of discomforts, including headaches. While these can be bothersome, there are several effective ways to manage them naturally.
Common Causes of Pregnancy Headaches:
Hormonal Fluctuations: Shifting hormone levels can trigger headaches, especially during the first trimester.
Dehydration: Ensuring adequate hydration is crucial, as dehydration can exacerbate headaches.
Stress and Fatigue: The demands of pregnancy can lead to stress and fatigue, contributing to headaches.
Poor Posture: Maintaining good posture can alleviate tension headaches.
click here to know more about Tips for Managing Pregnancy Headaches
Natural Remedies for Relief:
Hydration: Drink plenty of water throughout the day to stay hydrated.
Rest: Adequate rest and sleep can help alleviate stress-related headaches.
Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can support overall well-being.
Gentle Exercise: Regular, low-impact exercises like yoga or swimming can help reduce stress.
Relaxation Techniques: Practice relaxation techniques such as deep breathing, meditation, or mindfulness.
Over-the-Counter Pain Relievers: Consult your doctor before using any over-the-counter medications, as some may not be safe during pregnancy.
When to Seek Medical Advice:
Severe or Persistent Headaches: If you experience severe, persistent, or unusual headaches, consult your healthcare provider.
Headaches Accompanied by Other Symptoms: If headaches are accompanied by vision changes, dizziness, or other concerning symptoms, seek immediate medical attention.
Remember, while pregnancy headaches can be frustrating, there are safe and effective ways to manage them. By adopting these strategies and consulting with your healthcare provider, you can experience a more comfortable pregnancy.
For more personalized advice and support, connect with Light Pink Care today.
#pregnancy headaches#pregnancy pain#migraine#headache relief#prenatal care#maternity health#pregnancy tips#natural remedies#pain management self care
1 note
·
View note
Text
0 notes