#nurse practitioners in clinical research
Explore tagged Tumblr posts
Text
youtube
Email : [email protected] | Linkedin : https://www.linkedin.com/company/Clingenious | Website : https://clingenious.com
Durations in Clinical Interactive System | Dr. Bharadwaz | Clinical Research
Explore the fascinating world of clinical interactive systems as we delve into the significance of durations in healthcare settings. Learn how understanding timeframes impacts patient care, treatment outcomes, and system efficiency. From diagnosis timelines to therapeutic interventions, discover how durations are critical in streamlining medical processes and improving patient experiences. Watch now to uncover insights that can transform clinical practices!
Dr. Bharadwaz | Clinical Research | Health & Fitness | Homeopathy, Medicine & Surgery
#ClinicalSystems #HealthcareInnovation #MedicalInsights #PatientCare #healthcareefficiency
#DrBharadwaz #Clingenious #Helseform #Fidicus
#ClingeniousResearch #ClingeniousCompany #HelseformFitness #FidicusHomeopathy
#ClinicalInteractiveSystem #IRT #RTSM #IWR #IWRS #eCOA #ePRO #ClinicalSupplies #CIS
About Clingenious Research : Empower sponsors, clinical research organizations, clinical supplies companies, and clinical technology companies to deliver breakthroughs with the finest Clinical Interactive System experience.
#ClinicalInteractiveSystem#IRT#RTSM#IWR#IWRS#eCOA#ePRO#CIS#Clinical Supplies#clinical research#clinical trials#clinical research associate#clinical research coordinator#clinical#nurse practitioners in clinical research#black women in clinical research#clinical research organization#research#conducting clinical and translational research#clinical research pa#clinical research boring place#day in the life of a clinical researcher#pediatric clinical research#Youtube
1 note
·
View note
Text
A study conducted by the B.C. Centre for Disease Control has found that prescribing medical-grade opioids dramatically reduced the rates of deaths and overdoses for drug users living in B.C. The study, published in the British Medical Journal, is described as "the first known instance of a North American province or state providing clinical guidance to physicians and nurse practitioners for prescribing pharmaceutical alternatives to patients at risk of death from the toxic drug supply." Researchers looked at anonymized health-care data of 5,882 people between March 2020 and August 2021, all of whom had opioid or stimulant use disorder. Those individuals filled a prescription under the B.C. Risk Mitigation Guide — clinical guidance developed in March 2020 to allow for physical distancing during the COVID-19 pandemic, and to reduce deaths through harm reduction.
Continue Reading
Tagging @politicsofcanada
#cdnpoli#canada#canadian politics#canadian news#british columbia#public health#harm reduction#drug usage#harm reduction works#overdose#research
1K notes
·
View notes
Text

*crying sobbing pounding on dazzle's chest* YOU'RE GONNA COME BACK WRONG AND AS CHAGGIE'S FUCKED UP CREEPY MEDICAL RAT PUPPETEER CHILD!! YOU HAVE NO CHOICE!!!!
Razzle needs a hug and i don't CAAARE if it's just from the reanimated body of what used to be his brother turned little sister >:(






this fankid brought to you by
Charlie running around with bandages after an Extermination trying to patch Sinners up, a thing that would inspire her new goat child and something her and Baffy would bond over.
Vaggie as a mom and also one of the only ppl around scarred by a permanent debilitating wound given by heavenly steel, a thing she and Baffy kinda have in common, and motivation for Baffy's research into healing heavenly injuries.
What if a kid was born from a failed attempt at resurrecting someone else and then had to live right next to said person’s memorial statue while watching their older brother sadly cuddling up to it sometimes? Baffy totally doesn't get trauma from this.
other random thoughts below
Having a health practitioner in the Pride Ring is kinda like installing fire detectors in Hell.
Not only is violence happened all the time everywhere but Sinners normally just pull themselves together afterwards and regenerate unless hit with a heavenly weapon, so what's the point of having someone running around stitching up wounds and treating blood loss?
Well.. what's the point of running around with a torn off arm if you don't have to? Or being in pain longer than you need to?
Baffy thinks that sounds pretty stupid.
Baffy is cheerfully chasing down her next VERY reluctant patient as we speak.
Baffy's heart is in the right place (she checked) but her medical practices and bedside manner are kinda lacking (ironic for a former plushie toy) and most Sinners would rather run screaming into a turf war than let her treat them. She's a little too fond of stiches and blood and excuses to see both.
(And what if not even heavenly steal could scar or permanently kill people...?) (Heaven is NOT happy someone is asking this question)
Hell’s creepy new health practitioner
Unlicensed
Self-taught surgeon via rat autopsies
Uses rat puppets to distract and calm her patients (doesn’t realize they find it disturbing)
Largest rat puppet also serves as her assistant
Craves apples
Can be bribed with apples
Reborn from Charlie’s blood and part of the Morningstar bloodline
Fav bedtime story is of how Charlie kept trying to help bandage Sinners up after Exterminations and how that eventually led to Charlie meeting, helping, and falling in love with Vaggie
Looks and acts a lot like her aunt Niffty
Aunty Angel Dust was the receptionist / nurse for kid Baffy's play pretend doctor fun, and he does it for real whenever Baffy sets up a makeshift clinic in the hotel lobby
Husk grumpily lets her try to help him stop drinking
Sometimes uncle Husk wakes up from a hangover with a YOWEL as Baffy gets him in the hindquarters with a syringe of her own healing blood
Cherri Bomb and Cherri Bomb's bombs are Baffy's main source of patients since they're usually in too many pieces to run away from her
Cherry brings them over when she remembers to
mainly so Baffy can assess the damage and unintentionally give Cherri tips on how to build her next bomb even better
Vaggie as the only one slowly picking up on something being very wrong with Baffy's whole heal people at any cost thing even if the price is her own blood and pain
Vaggie is trying to show Baffy that living with scars can be okay but hotel business and heavenly threats keep interrupting them
Baffy has an X shaped white scar where Dazzle’s mortal wound was
Her scar aches when she touches heavenly steel or when large amounts of it are nearby
Yes her head is on fire no it’s not a problem (for her)
Since she can't use heavenly weapons without hurting she mainly just headbutts people with fire when attacking or puppets her small rat army after them
Has to drink blood daily to survive
HATES the taste of blood
does think it's PRETTY tho
Scared of needles but keeps trying to use blood transfusions to help Sinners heal from heavenly steel wounds like her body did
Emily is her doting "guardian angel" / godmother who helped Charlie and Vaggie bring her into the world / failed at bringing Dazzle back
Lute thinks Baffy's 'birth' in an insult to creation and to her and wants the 'abomination' dead
Emily almost goes full seraph fury on Lute's ass for this
Instead Emily reminds Lute and Sera that, as a blood relation of Lucifer, Baffy has immunity from being targeted by heaven, an immunity Emily WILL enforce
Baffy has a running feud with Cannibal Town over whether devouring bodies counts more as recycling / waste management or robbery from the scientific community (which is so far just Baffy)
Since Dazzle died in dragon form Baffy can't shift into it without tearing open her mortal wound scar
she almost died the one time she tried it
Razzle knew she wasn't his dead brother brought back to life when new born her was given a choice between an apple and a donut and she did NOT choose the donut
He loves his new little sister so much and just wishes Dazzle could have somehow known her too
#hazbin hotel#chaggie#razzle hazbin hotel#dazzle hazbin hotel#razzle dazzle hazbin hotel#chaggie fankid#bedazzled au#needles#my art#fanart#ok i think i can be ok about dazzle dying now#maybe#we'll see
81 notes
·
View notes
Note
how do you feel about all the anti doctor rhetoric on tumblr and beyond? i feel like it comes from a place of misunderstanding and hurt over the failing healthcare system :/
I’m perhaps not the best person to answer this, because much of tumblr is American and I am not (I am from a country with fully public healthcare, and work as a doctor in Australia where there’s a mix of public/private care but I’ve only ever worked in the public system).
However, I think it’s multi factorial, with some causes being justified and others not so much.
A lot of anger towards the health system is very much justifiable - particularly in the US where health care is precarious and so expensive even if you have insurance coverage.
But that anger is wrongly directed at doctors, and generally the lowest paid doctors - family medicine, paediatrics, and emergency - because we’re one of the more visible facets of the system. People think we are very wealthy, but the bulk of the money seems to go to insurance companies and hospital admin, not to us. In fact, hospital admin in every country bend over backwards to avoid paying doctors for their actual labour.
(Once, in response to a patient’s parent asking me if they had to pay for their clinic appointment, i accidentally responded “I don’t know, I don’t think so. They don’t pay me for this.” by which i meant that i don’t get paid any extra for clinics but i did have to clarify that they were, like, paying me for the day overall. And also it was a public hospital so I was able to confirm after that no, they didn’t have to pay.)
Most people just don’t understand the way insurance works, or how little of that money goes to doctors. What I really wish I could broadcast to everyone is how little residents/registrars make. I made about 50k USD equivalent as an intern - which is nothing to sneeze at but I had just completed 8 years of university and was over $200,000 in debt from med school. A cop in my city makes about $75k USD, which is 25k USD (about 40k AUD) MORE per year than an intern doctor does.
Another reason for a lot of anti-doctor sentiment is that people really have been let down by the medical system. It can be complex, hard to navigate, and there are some legitimately bad doctors out there. There are also a lot of nurse practitioners replacing doctors in many roles, and while they’re a great resource, they just don’t get the same amount of training.
I believe that there are people who have been dismissed, particularly women, fat people, and trans people. By older doctors especially, and for women by male doctors, but also by younger and female doctors at times. This is mainly because as much as no one wishes to acknowledge it, doctors are human. And some humans suck ass. It takes effort to overcome one’s own biases but we are explicitly taught to work on that and to not let any biases we may hold impact our patients.
The common ideas and reasons given for hating doctors that “POTS isn’t taught in med school” or “med schools don’t teach about endometriosis” are completely untrue for most schools these days, though. I started med nearly a decade ago (yikes!) and we were taught about both these things! It’s not the 1980s anymore! “we never really researched the female body” WAS true but we are very much catching up on that now! There is some great work on endometriosis in particular being done in BC. However, trust in the medical system was justifiably lost (for these and many other reasons) and it will take a long time to gain that back.
There is a third factor, though, which i think is fully unjustified, and that’s the (often right wing led but adopted by the left as well) push to delegitimize academics. Covid really lit a fire under this one, and since then there’s been so much distrust towards science and scientists because we’re the “elite” in our “ivory towers” (so typed from my scrubby little city apartment). It’s often pushed by politicians who stand to gain votes, or influencers who want to sell you spirulina flakes or whatever the current trend is. There’s an intentional moving behind pushing this, but there are a few factors for people believing it.
It’s partially anti-intellectualism, because no one likes thinking that someone else might possibly be more educated on a subject. I do also think there is an element of sexism and racism - medicine and science are becoming lower paid and less trusted as more women and POC gain entry.
There’s also the fact that people don’t want to hear that sometimes things that are good for them aren’t fun. No one wants to get a vaccine because that hurts. Its much more pleasant to believe that getting a massage and drinking raw milk and rubbing lavender oil into everything is the TRUE cure, that doctors don’t want you to know about, because believing that lets you indulge in things that feel good while believing you’re doing good - which people love, even when it’s false.
This was much longer than I wanted it to be and doesn’t cover all the reasons! But this covers a few factors.
16 notes
·
View notes
Text
Extracts of the the Judge’s reasoning and analysis:
On November 4, 2020, Plaintiff Brianne Dressen received AstraZeneca’s experimental COVID vaccine as part of a clinical trial in Salt Lake County. 4 Velocity Clinical Research, Inc. (Velocity) administered the trial on AstraZeneca’s behalf. 5 Before receiving the inoculation, Dressen signed an informed consent form (ICF) that outlined her rights and responsibilities as a trial participant and disclosed possible side effects of the vaccine.6 Under the terms of the ICF, the parties agreed AstraZeneca would “reimburse[] for time and travel in the amounts of $125.00 per each completed study visit and $30.00 for each completed phone call.”7 The parties also agreed that a “study doctor” would “provide medical treatment or refer [Dressen] for treatment” if Dressen became ill or injured while participating in the study.8 Additionally, AstraZeneca disclosed that it had an insurance policy to “cover the costs of research injuries as long as [Dressen] followed [the] study doctor’s instructions.”9 AstraZeneca confirmed it would “pay the costs of medical treatment for research injuries, provided that the costs are reasonable, and [Dressen] did not cause the injury [her]self.”10 At the same time, the parties agreed federal law may limit Dressen’s right to sue for injuries caused by the vaccine: Due to the coronavirus public health crisis, the federal government has issued an order that may limit your right to sue if you are injured or harmed while participating in this COVID-19-related clinical study. If the order applies, it limits your right to sue the researchers, healthcare providers, any Sponsor or manufacturer or distributor involved with the Study. You may be prevented from making claims for injuries that have a causal relationship with the use of the investigational product in this Study, including, but not limited to, claims for death; physical, mental, or emotional injury, illness, disability, or condition; fear of physical, mental, or emotional injury, illness, disability, or condition, including any need for medical monitoring; and loss of or damage to property, including business interruption loss. However, the federal government has a program that may provide compensation to you or your family if you experience serious physical injuries or death. If funds are appropriated by Congress, compensation for injuries may be available to you under this Countermeasures Injury Compensation Program.11 Within an hour of receiving the vaccine, Dressen’s right arm began tingling.12 The sensation, a condition called paresthesia, soon spread to her right shoulder and left arm.13 Later the same day, Dressen began experiencing a host of other symptoms, including blurred vison, tinnitus, nausea, and sound sensitivity.14 Dressen first visited an emergency room three days after receiving the vaccine.15 The doctor who treated her diagnosed her with a “vaccine reaction.”16 She returned to the emergency room four days later, and the next day she visited a nurse practitioner at Utah Valley Neurological who diagnosed her with an “immunization reaction.”17 Thirteen days after receiving the vaccine, Dressen visited an otolaryngologist to seek care for “acute sensitivities to light and sound.”18 The doctor noted Dressen was suffering from “a likely side effect due to an increased immune response to the vaccine.”19
2 notes
·
View notes
Text
(Reboot) Huo Daofu's Resume
At the end of the series (S2, EP30, 26 minute-ish), Huo Daofu brings his resume to a hospital in search for a position there. Let's look at the contents with a close eye hm? (google doc version here)
(The section right under his photo) (blue text) 岗位: 医学博士 Position: Doctorate of Medicine and of Philosophy, MD–PhD
(regular text) …护理学基础,重症护理学,内科护理学等 …nursing fundamentals/basic nursing, critical/intensive care, internal medical nursing etc
(blue banner) 工作 ?经? 历 Experience
(blue text) 德国海德堡大学医学院 Heidelberg University-Medical Faculty 岗位: 医生 Position: Doctor
(regular text) …治疗方案策划,病情追踪,病历书写以及治疗方案变更时的方案建议; …constructing treatment plans, following up on [patient's] condition, recording clinical notes and treatment plans and recommended follow-ups; …诊断确认,例如:心电图分析,CT分析,DR分析; …diagnose [patients] by deciphering test results such as EKG, CT, DR; …?手术主治? 医生,研究肺病,在世界学术上发表过肺病治疗的报告, 得到学术界的一致肯定. …[conducts] surgery [as] attending physician, done research on lung diseases, presented reports on lung disease treatments on [international conferences]* and had received unanimous approval/recognition [for it]
*im not sure if conferences is the right word for it, but the gist is that he'd presented his research on an international platform

(blue text) 2013.09-2015.06 陈氏古玩有限公司 Chen Antiques Co. Ltd. 岗位:投资顾问 Investment Consultant 岗位:全科医生 General practitioner/family physician/family doctor
(blue banner) ?-? Award
#dmbj#huo daofu#reunion sound of providence#hehe hope this helps!! go forth and add weird little details to your fanworks!#i know the screenshots aren't super crisp but it's the best i could do!
40 notes
·
View notes
Text
My worst fear finally happened today
Tw: nswf, tokophobia, bad thoughts, talking about ab0rt!0ns, su!c!d3 thoughts
So my worst fear finally happened today. The condom broke during his climax. The moment we both realized, I started crying and panicking. My boyfriend knows I have severe tokophobia and that I will do things that I hope will make me infertile (he doesn’t know the extent). He immediately went and got me Plan B and coffee and a pregnancy test. I’m not gonna lie, when he gave it to me, I had a second freak out. He had to take my hands and get me to breathe (I left him some 🍃for everything). I went home and took it within 4 hours of the accident happening.
I’ve been paralyzed with fear and researching abortion clinics and states with no regulations on them and the closest state is Maryland and I’m from Georgia. Maryland is the closest state that doesn’t report abortions and I won’t have to worry about getting arrested (don’t we love the Deep South). I’ve been on and off crying and hyperventilating then getting serious and researching clinics and how to become infertile. I’m planning on calling my doctor tomorrow and talking to the nurse practitioner about getting my tubes straight up removed. I know it’s gonna be a pain because I have no kids and I’m 24 but I can’t keep living in this fear. Whenever I’ve taken birth control, I instantly want to game over myself. I don’t know what I need to do to get it but I will.
Should the worst case scenario happen, I know my boyfriend and family are behind me going on a “camping trip”.
8 notes
·
View notes
Text
A fun thing I'm working through as a trans person in inpatient care.
To start, I have like ALL of the privileges and resources at my disposal. Not only am I highly researched and informed on gender care and mental health, but my partner runs a gender affirming care clinic, and I have an effective relationship with my family doctor (who handles all my care) and I personally know many doctors and other practitioners handling gender affirming care in the region.
I gave the unit two days notice that I receive my estrogen injection on Tuesday mornings. At this time, we informed them that we would need to supply this because it can only be created in a sterile compounding facility and the hospital will not have it in stock. In Canada, the product that was approved for injectable estrogen was removed from the market by the supplier (distribution to Canada wasn't worth it, not due to health concerns) so there is no registered product/DIN and a sterile compounding facility makes it for you instead. We brought my current vial into the hospital to do the injection. The vial had my deadname, because my legal name change only occured a month or two ago just after my last refill. It was explained at dropoff why this difference occurred. Prior to dropoff, I asked if we needed to supply any supplies, as I draw with a 21G and inject with and 1.5" 25G. They said no, they have everything they need for the injection.
Tuesday morning, I get told they just need the pharmacist to look at it, and then we'll be good to go. Then the nurse asks me what I need estrogen for (🙃). A few hours go by. The pharmacist assistant comes out and asks me for all of my information regarding the prescription (dose, how long I've been using it, the pharmacy it's from), all of which is available on the label of the drugs.
A few hours go by. The pharmacist assistant comes back to me to let me know the hospital doesn't have this medication and if I had any at home that could be brought it (for the readers at home, my bottle of estrogen was already in the clinic before she talked to me the first time). Upon learning it's here, she says she'll get it and it should be ready soon.
A few hours go by. The nurse then comes out and says my injection is soon, and to wait in the room. I wait, fifteen minutes go by. My partner and sister arrive for a visit, so we go knock on the door and ask what's happening. The nurse says the pharmacist finished their day without giving clearance for me to use my estrogen and I will have to wait until tomorrow. My partner immediately takes charge and explains how this is not acceptable care, and that we can get whatever type of physician they need to contact the hospital to resolve the situation. The nurse says they'll try again, and we say please interrupt us if there are any changes.
Around when my partner is supposed to leave, the nurse comes back out and says okay we're good to go on the injection, get ready in your room for it. My partner and sister leave and I go to my room. Five minutes pass, the nurse comes back and says just a couple minutes longer. More time passes, the nurse comes back and says the name on the drugs is too different from my name so they can't give it to me. I show them a digital copy of my legal name change certificate, which then gets escalated to the charge nurse at the entrance, who then takes a picture of the document on my phone with their phone and says we'll send this to the pharmacy. Another pair of friends arrive for a visit around this time. We sit in the room next to the nurses station and I say please come get me if there is any additional information or contact I can get to help this process along.
The nurses change shift, and around 7:30pm (12 hours after when I regularly take my estrogen) the nurse says they are still working on it and are unsure if it's going to happen tonight. I make it clear that this is significantly impacting my mental health, and that if I don't receive my injection I will need the as-needed prescribed anxiety medication to sleep tonight.
My friends leave. At 8:30 the now new nurse says still no update but they will phone the pharmacy around nine. I got for a walk around the courtyard to try to release some of the anxious energy I am feeling about being told off and on all day about whether I'll be receiving my injection. They keep saying it will happen tomorrow but after waffling all day I simply can't trust that either. Just before nine, another nurse tells me I have to come inside because they lock the courtyard at nine, so I instead walk around the unit inside.
At 9:15, the nurse tells me the pharmacist has approved it but the drugs are at the pharmacy and need to come here, it'll be about 20 minutes and then we'll get me the injection. The nurse asks if I'd like the anxiety medication in addition, and I say very much yes. I keep walking around the unit. 9:35 hits with no new updates. At ten, I start to get ready for bed and get changed into pajamas and brush my teeth, then continue to walk around. Finally, shortly after ten, the nurse comes out with my shot. I ask the gauge of the needle, the nurse says 22, I say I normally inject with a 1.5" 25G do you have that? The nurse returns with a 23G and says they only have 25G on the children's ward.
I get settled to take my shot, and look at the needle and it's definitely no more than an inch long. I know my body, and I have large thighs. I know the inch and a half needle length is important to ensure I get my shot into my muscle tissue, but at this point Ive spent so much time and energy trying to advocate for this, that after asking and learning there is no longer needle here I take it with the smaller length and hope it's fine. After the shot, I ask if I bring my own needle tips if we can use those next week and they say yes (I offered to bring my whole kit previously and they said they have everything they need).
Overall, while I did get my shot at least on the day I should (which is an outcome I know so many trans patients don't receive), I am feeling so defeated. It took relentless questioning and proof providing, and I have all of the resources at my disposal to ensure it can happen. If my partner was not there the one time they told me I wouldn't get my shot, I don't think I would've received it that day. Nurses named they know nothing about HRT to me.
It makes me very scared for the future. Not receiving HRT while under supervised medical care is a legitimate nightmare I have and many trans people share. With the political climate, it's hard to see how this will get better in the short run. With my own medical issues, I also foresee a future where I will need some type of nursing home or supervised care for other reasons and now I am even more questioning if I'll receive the care I need to survive. Furthermore, how will any of my trans kin be treated?
I am in inpatient care because of how my desire to care for my community has left me like a squeezed out toothpaste tube, and now my care providers are showing the urgent need for toothpaste.
#trans#2slgbtqia+#mental health#text#queer community#inpatient#trans rights#death before detransition#trans hrt#hrt on demand#hrt estrogen#hrt
3 notes
·
View notes
Text
Exploring Nursing Opportunities Abroad: Top Countries for Indian Nurses
Nursing is one of the most in-demand jobs inside and outside India. A profession that is in most demand in GCC countries for Indians is the nursing job. For Indian nurses, who are looking to broaden their horizons, many countries are waiting with promising career opportunities. If you are a skilled nurse and have multilingual capabilities then wide opportunities will be there. The overseas opportunities will give you high pay as well as a high-standard working environment. The respect for nurses outside India is much higher than inside India. Nurses are being recruited through top nursing consultancy in Kerala and here is a list of the top countries that offer promising careers.
Five top countries that offer promising nursing career
United Arab Emirates: Dubai which is an opulent city right due to cultural and development richness hires nurses from India. A large part of nurses who work in Dubai are Indian and they a decent pay but not much higher than European and American countries. But the most attractive feature of Dubai is that the nurses can take their entire income to their homeland since there are no taxes. In Dubai, there are many world-class hospitals, medical centers, and clinics that offer good employment prospects for Indian and other nationalities.
Saudi Arabia: In Saudi Arabia, there are a plethora of job opportunities for nurses in both the private and Government sectors. They offer good pay, accommodation facilities and also travel allowances. Saudi Arabia is one of the largest nations in GCC countries and also the pilgrimage place for Muslims, the demand for medical facilities is very high. The demand for trained professionals especially from India is of high demand in Saudi. However, finding the right opportunity is a bit challenging since there is a high scam in the field of recruitment.
Canada: Canada is a country that offers a healthcare system with the highest standard. This country is facing staff shortages and is now actively recruiting nurses worldwide. The high-quality life and the welcoming stances towards immigrants make Canada an excellent choice for nurses. The medical facilities and education are completely free for immigrants.
Australia: Australia's flourishing healthcare industry and stunning landscapes attract nurses worldwide. With modern facilities and advanced technology, nurses can work efficiently. During leisure time, they can explore the country's picturesque natural environment. Competitive salaries and excellent benefits make it a lucrative career option. To work as a nurse in Australia, one must register with the AHPRA (Australian Health Practitioner Regulation Agency) and pass English language proficiency tests.
United States of America (USA): The USA boasts a robust healthcare system with a significant demand for skilled nurses across various specialties. Indian nurses aspiring to work in the USA can pursue opportunities through programs like the H-1B visa for skilled workers or the EB-3 visa for professionals with tertiary education. Opportunities exist in hospitals, clinics, long-term care facilities, and community health settings throughout the country.
United Kingdom (UK): With its National Health Service (NHS), the UK offers extensive opportunities for Indian nurses to work in both public and private healthcare sectors. The UK's Nursing and Midwifery Council (NMC) oversees the registration process for international nurses, which includes passing the Occupational English Test (OET) or International English Language Testing System (IELTS) and meeting other requirements. Work settings range from hospitals and nursing homes to community healthcare centers.
Conclusion
If you are planning for an overseas nursing job, first research the rules and regulations for immigrants. Based on it decide which country is most suitable for you. There will be medical tests, mandatory examinations, and other verifications for each country. It is better to connect with any nursing consultancy in Kerala before you plan to move, they will guide you through the process and also provide you with data regarding the recruitment.
3 notes
·
View notes
Text
A new class of health care startups has emerged in response to the US Supreme Court’s decision to overturn the federal right to abortion last year. These “digital abortion clinics” connect patients with health care providers who are able to prescribe mifepristone and misoprostol, a course of care commonly described as the “abortion pill.”
These services, many of which were founded before Dobbs v. Jackson, are poised to eliminate a major paradox in the field of reproductive health: Medication abortion is currently the most common way to terminate a pregnancy, yet only 1 in 4 adults are familiar with it, according to a recent study by KFF.
These clinics operate in different ways—some provide live video visits with doctors and nurse practitioners, while others offer asynchronous counseling—but many have experienced a record number of patient orders (and increased VC funding) over the past year. According to Elisa Wells, cofounder of the nonprofit Plan C, their appeal is straightforward. “Their pricing is quite affordable, and there’s convenience in placing an order and getting pills delivered to your mailbox in three to four days,” she says.
Recent data suggests that telehealth clinics have been effective in expanding access to abortion care, especially for people living in remote areas or in states where the procedure has been criminalized, a finding that Wells’ team corroborates. Thanks to a new series of “shield laws” protecting clinicians from out-of-state prosecution—passed in 12 states, including New York, Maryland, and Illinois—these clinics are positioned to expand their reach even further.
Following the lead of other companies in the femtech space (a category that includes everything from kegel trainers to period-tracking apps), leaders at digital abortion clinics like Hey Jane and Choix have publicly expressed their commitment to users’ privacy as they grow. In a recent interview with Vogue, Hey Jane cofounder Kiki Freedman said that the service is “HIPAA-compliant and encrypted.” In an interview with Ms. magazine this January, a representative from Choix highlighted its “HIPAA-compliant texting platform,” while another interviewee suggested that “most telehealth providers are not checking IP addresses.” (Read more about how HIPAA actually works here.)
A common belief about virtual clinics is that they offer more discretion than their brick-and-mortar counterparts. “There’s definitely a privacy factor—these sites don’t ask a lot of questions,” says Wells. In a 2020 study of over 6,000 abortion seekers, 39 percent reported choosing a telemedicine option specifically to preserve their privacy. While some providers’ intentions seem genuine, privacy experts have pointed out that their services may not be as secure as users expect them to be (even if they are compliant with US law).
Last July, a team of researchers at the Markup reported that Hey Jane’s site passed along user information to Meta and Google, the world’s largest digital advertisers. While providers may not restrict access via IP addresses, our analysis found that most providers readily collected them. For telehealth abortion clinics, HIPAA compliance is just one part of the puzzle.
So which virtual abortion clinics take users’ privacy seriously, and which do not? How can users approach these services with safety in mind? Does HIPAA protect all information sent to telehealth providers? To find out, we teamed up with experts to analyze the privacy policies of five popular abortion-by-mail providers: Wisp, Choix, Hey Jane, Carafem, and Aid Access.
While the American Bar Association reported in April that “high-tech tactics” (like sending court orders to femtech apps) have not been used to successfully convict abortion seekers, prosecutors have used women’s text messages and search histories as evidence in a number of abortion-related cases. Because of this precedent, users should proceed with caution when handing their personal information over to telehealth providers. It’s not uncommon for vulnerable data to end up in the hands of third-party brokers who compile digital profiles of users before selling their information to the highest bidder. Michele Gilman, professor of law at the University of Baltimore, says: “Reproductive health data is being sold and transported into a much larger system.”
To make matters worse, the absence of a comprehensive federal privacy law, like the EU’s General Data Protection Regulation (GDPR), leaves the burden of evaluating privacy policies to individual users. Considering that these policies have gotten longer and more difficult to decipher in recent years, this is a serious burden. For our evaluation, we consulted frameworks from the University of Texas at Austin’s Privacy Lab and the Digital Standard to arrive at four core factors.
Here’s what we found:
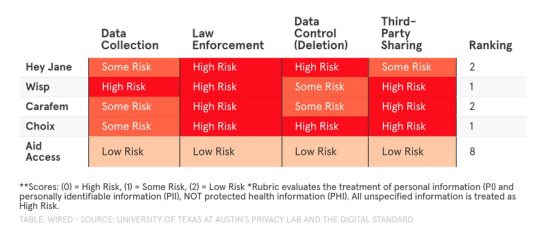
Data Collection (PII)
The GDPR’s American cousin, the California Consumer Privacy Act (CCPA) has inspired proposed state legislation that supports greater protections for a specific category of data—personally identifiable information. While PII is broadly defined, Google interprets it as including your email address, full name, precise location, phone number, and mailing address.
The safest websites to use won’t collect your PII at all, but offering a mailing address to a virtual clinic is a matter of necessity here. In this context, it’s helpful to distinguish between companies that use your personal information to provide essential services and those that share this information with third parties. Austria-based nonprofit Aid Access fared the best in this category, encouraging users to access the service with virtual anonymity in its policy. Wisp fared particularly poorly here, citing its ability to send specific geolocation data to advertisers.
The majority of providers we analyzed categorize email addresses and the like as “personal information,” which is only protected by HIPAA if it’s stored alongside medical information. This makes it difficult to judge whether it’s being used appropriately.
Low Risk: PII is not recorded, Some Risk: PII is used for intended service, High Risk: PII is used by third parties
Law Enforcement
According to bioethics expert Sharona Hoffman, there’s a common misconception that HIPPA protects your medical information from being shared outside of your doctor’s office. The reality, she says, is that “HIPAA isn’t that protective. Consumers need to know that HIPAA has exceptions for law enforcement and public health.”
While the law provides safeguards for a particular subset of information (personal health information), it doesn’t cover all of the information you provide to a telehealth service. Even if it did apply, the rule allows (but does not require) health care providers to expose PHI when presented with a search warrant or other legal document. While providers could technically refuse these requests, most don’t. “It’s easier to comply rather than involve your medical office in litigation,” says Gilman.
Aid Access is a notable exception and has a track record of standing up to law enforcement (it even sued the US Food and Drug Administration last year.) When examining privacy policies, UT’s Privacy Lab recommends looking at companies’ willingness to hand over any data in the absence of a warrant or other legal document. Neither Carafem, Wisp, Hey Jane, nor Choix specify that they would require a warrant before sending information to government agencies or other legal entities.
Low Risk: PII is not recorded, Some Risk: Legal documents are required to comply with law enforcement, High Risk: Legal documents are not required to comply with law enforcement
Data Control (Deletion)
Sites that offer users more control over their data can deliver better privacy than those that don’t. While low-risk sites will allow you to delete and edit your information freely, some medical information that users provide to virtual clinics will still be out of reach. This is due to state-specific medical record retention laws, which can require health care entities to retain some records for up to 25 years.
Examining how much control companies give users over other information is a better proxy for understanding their general safety. While most of the providers we analyzed included data deletion protocols in their privacy policies, Choix and Hey Jane’s do not. In addition, the latter confirms that it retains data for an unspecified (“reasonable”) period of time.
While Wisp does offer a deletion protocol, it admits that requests can be refused for a variety of reasons, including “exercising free speech” and “internal and lawful uses” on behalf of itself or its affiliates. In addition to responding to requests, privacy-forward organizations will also proactively delete sensitive information, something Carafem does. However, Carafem does not specify a timeline or provide a general deletion request protocol. By contrast, Aid Access allows users to file deletion requests at will for most information.
Low Risk: Users can edit or delete data, Some Risk: Users can edit data, High Risk: Users cannot edit or delete data
Third-Party Sharing (Ads and Marketing)
Research scientist and privacy expert Razieh Nokhbeh Zaeem calls personally identifiable information the “currency of the internet” because of the myriad ways individualized data is collected, bought, and sold across industries. While almost all websites work with third parties in some way, telehealth companies should not sell or share your information with advertisers—but many do, as evidenced by Betterhelp’s recent settlement with the Federal Trade Commission.
If a company is collecting sensitive information and using it to market products and services to you, that presents some risk. If a company shares this information with other companies to support their marketing efforts, it’s a major red flag. As the Markup rightly points out in its privacy policy guide, mentions of “personalization” and “improving services” in these documents usually equate to ad tracking.
According to its privacy policy, Hey Jane uses personal data (and PII) to market its own services (“inform you about products”), while Carafem, Wisp, and Choix reserve the right to pass along information to third-party marketing partners. Choix’s policy claims that it “will never sell your data for third-party marketing purpose[s]” in one section but reserves the right to disclose data to its affiliates for “marketing” purposes in another.
Rather than limiting or removing the third-party trackers installed on their sites, some providers recommend that users generally opt out of cookie-based advertising within their policies, a strategy that is far from foolproof.
Low Risk: PII is not used for marketing or advertising, Some Risk: PII is used for marketing/advertising, High Risk: PII shared with third parties for marketing/advertising
The Bottom Line
In a post-Roe America, virtual abortion clinics provide an essential service, especially for people living in states that criminalize care. Early indicators have shown that they increase access to safe and effective abortion medications, but they don’t offer as much privacy as users are led to believe. With the exception of Aid Access, all of the providers we analyzed have a long way to go when it comes to protecting users’ privacy and earning their trust.
To manage risk when approaching these services (and accessing other information about abortion in hostile states), educators at the Digital Defense Fund recommend reducing your footprint by using privacy-forward search engines like DuckDuckGo, creating temporary email accounts for abortion care, and turning off location tracking on all of your devices.
While engaging in defensive tactics like these are practically useful, legal scholars like Gilman suggest that the reproductive justice movement will advance only when federal and state governments no longer rely on an outdated “notice and consent” paradigm for data privacy. “We need meaningful consent in the reproductive health space,” says Gilman. “Privacy policies today are more like adhesion contracts—suggesting that users ‘take it or leave it.’ It’s not realistic or fair to tell people they can’t engage with technology if they want to protect their privacy.”
Gilman recommends advocating at the state level for better privacy standards, especially if your representatives are considering new legislation. She also encourages people to demand increased protections from private companies, many of which are more flush with the “currency of the internet” than they would have us believe.
8 notes
·
View notes
Note
for many reasons allopathic med school is not available to me but lately I’ve been considering becoming a nurse practitioner. do you work with any or know any? do you think it’s a good path to care for people and make their lives better?
I have known many NPs and currently work alongside one at my clinic. I can say with certainty that her patients love her. NPs absolutely have the opportunity to improve the lives of their patients. If you want to be involved in directly caring for patients but don't think that medical school is an option, I would recommend doing some research into the type of training that is involved in becoming an NP or maybe seeking out NPs either in your community or online for more information or to hear about their experiences.
7 notes
·
View notes
Text

Please someone do a real scientific research on this from the patient's point of view. -_- Like a real proper scientific representative survey and ask what actual humans who are not doctors think about this.
-Would you be okay if your doctor or nurse lied to you or deceived you?
-If you found out your doctor or nurse lied to you, what would that do to your relationship with your doctor and nurse?
-How does it affect you knowing that doctors and nurses think lying to or deceiving patients might sometimes be necessary? Does it cause you to trust the medical establishment less?
Because fucking hell seeing this in my inbox made me go "oh so doctors and nurses can actually just fucking straight up lie to me? nevermind then" and that is making the threshold of going to see a doctor or nurse about anything ever again even higher.
And like I am as a person actively hostile-ly anti-woo so I would never do "alternative" treatments - but this sort of shit is the kind of stuff those kinds of people will point to and say "the medical establishment is lying to you, come get your angles aligned by the power of the holy capricorn" ! >_<
Like you just can't- like this sort of fucking "mother doctor knows best" condescension... I don't care what kind of short term benefits those (pay-walled) papers and articles outline, but the negative effect on the reputation of all medical practitioners could be enormous.
You represent the real science. You have to go the high road every single fucking time. You just have to :S
#i have had so many bad experiences with doctors that the idea that they wouldnt treat me like an adult with autonomy and instead lie to me#'because you don't understand the harm of the thing you are asking for-' then you just don't fucking do the harm!#but don't fucking lie to me about it you fucking cowards!#very close to unsubscribing for the hastings center emails like. medical ethics? this? eat my entire ass ffs.
12 notes
·
View notes
Text
How to Become an Aspiring Medical Professionals in the US?

Aspiring medical professionals in the US embark on a rigorous and rewarding journey that requires dedication, perseverance, and a passion for helping others.
Here's a comprehensive guide to becoming a medical professional in the United States:
Educational Requirements:
a. Undergraduate Degree: Complete a bachelor's degree in any major, but it's recommended to focus on science-related fields like biology, chemistry, or physics to prepare for medical school prerequisites.
b. Medical School (MD or DO): Earn a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Medical school typically takes four years and involves a combination of classroom learning, laboratory work, and clinical rotations.
2. Premedical Preparation:
a. MCAT (Medical College Admission Test): Take and score well on the MCAT, a standardized test that assesses your scientific knowledge and problem-solving skills.
b. Shadowing and Volunteering: Gain hands-on experience in healthcare settings by shadowing physicians, volunteering in hospitals, or participating in research projects.
c. Extracurricular Activities: Demonstrate your commitment to healthcare and community service through extracurricular activities related to medicine or public health.
3. Medical School Application:
a. Strong Academic Record: Maintain a high GPA in your undergraduate studies, particularly in science courses.
b. Letters of Recommendation: Secure strong letters of recommendation from professors, mentors, and physicians who can attest to your academic and personal qualities.
c. Personal Statement: Craft a compelling personal statement highlighting your motivations, experiences, and aspirations in the medical field.
4. Residency Training:
a. Match Process: After medical school, participate in the National Resident Matching Program (NRMP) to match with a residency program in your desired speciality.
b. Specialization: Residency training typically lasts three to seven years, depending on the speciality, and provides in-depth clinical training under the supervision of experienced physicians.
c. Board Certification: Once you complete a residency, you become eligible to take and pass the board certification exam for your speciality.
5. Licensure and Continuing Medical Education:
a. Medical License: Obtain a medical license from the state where you intend to practice.
b. Continuing Medical Education (CME): Commit to lifelong learning by completing CME courses to stay up-to-date with the latest medical advancements and maintain your license.
6. Career Options:
a. Physician: Choose from a wide range of medical specialities, such as internal medicine, pediatrics, surgery, family medicine, or psychiatry.
b. Physician Assistant: Work under the supervision of a physician to provide comprehensive medical care.
c. Nurse Practitioner: Provide primary and specialized healthcare services independently or in collaboration with physicians.
d. Other Medical Professionals: Explore various healthcare professions, including dentists, pharmacists, optometrists, and audiologists.
Once you are ready to join organizations to offer your services, you need a platform to help you get a job. Check MedCadre, and you will get what you seek as an aspiring medical professional.
How does MedCadre help Aspiring Medical Professionals?
MedCadre is a one-stop solution to find the right job for you. The platform helps aspiring medical professionals get placement in the medical field.
All you have to do is visit the website, click on the form, and fill it out with relevant information. Once we verify your Resume, we will get back to you.
Becoming a medical professional in the US is a challenging yet fulfilling career path. With dedication, perseverance, and a passion for helping others, you can make a significant impact in your patients' lives and contribute to advancing healthcare.
Submit your Resume to MedCadre to enhance your career in the medical profession.
visit our site by clicking the link: https://medcadre.com/careers
#medical professionals#physician assistant#nurse practitioner#nursestaffing#healthcarestaffing#allied staffing
4 notes
·
View notes
Text
Social Anxiety is Measurable
I felt the urge to share a personal anecdote that might be beneficial to anyone who has suffered from social anxiety but not had support. It’s easy for others who do not experience discomfort to invalidate others’ truth, even if it is not intentional. So, a little background about me: I have had clinical depression for over 20 years (starting in high school) and after many years of battling, finally found a perfect combination of anti-depressant and anti-anxiety medication. However, I STILL suffer from anxiety, specifically social anxiety, and nothing has really soothed that discomfort. Instead, I practice mindfulness and walk myself through the experience I push myself to have, while practicing self-care and self-love by avoiding certain situations that I don’t feel confident I’ll be able to overcome. Due to the above, and genetics, I have hypertension (high blood pressure) and while it had been manageable before, about 6 months ago, I was put on medication for this, since I was experiencing some rather unsettling symptoms (you ever see your heartbeat in your eyesight? Feel it in your teeth? Not fun!) Now that you know the relevant information, here’s the story: I had my 6th-month check-in with my physician to make sure my medications aren’t negatively affecting me and that everything is still going well. During the initial intake portion of the appointment, where the nurse assistant/technician weighs you and asks you simple questions, they took my blood pressure. I had two nurses with me; I’m not sure if one was being trained or if they were just partnered-up to streamline the process (it went super smoothly!). Regardless, as the one was setting up the arm strap, I casually mentioned “oh yeah, my BP is a little high”. So, I’m continuing talking to the other nurse and the first one gets a little stifff and goes over to her and says, “It’s 180/90″ (something like that - I know I heard “one-eighty” and “over ninety” but they might not have been even like that). If you don’t know - which I didn’t know myself - This puts me in a Hypertensive Crisis. In other words, I could have a heart attack at any moment and all online research says to “seek medical treatment right away”. So, the second nurse has a very subtle reaction and notably talks a bit more soothingly to me. I comment off-handedly “I suffer from social anxiety, so my BP is always a little high when I am tested at a doctor’s office.” They both respond something like “Oh, okay then,” which in hindsight was them trying to keep me calm and not stress out more. Once she’s done with the questions, she says, “you know, let me go ahead and just take another reading - the doctor might want to run an EKG” I’m ok “oh damn!” but she said, she wasn’t sure, they just want to confirm that everything is okay. This is especially important because my mother suffered from “The widow maker” heart attack a few years ago - and survived! - but clearly, heart issues run in the family. Luckily, by the second time, my BP went down to something like 160/?? they didn’t say it to ME, it was more to themselves. So, it had come down but it was still high. (Normal is 120/80 or lower, for reference). I can hear them whisper by the door to the doctor about their findings - the nurse was very detailed and expressed that I shared I have social anxiety (and I’m self-pay, so an EKG might get a little expensive for me). The doctor comes in and can I just say, she’s amazing! She’s technically a Nurse Practitioner, so I'm just using “doctor” colloquially in this story. ANYWAY, she calmy says she wants to take it one more time with another cuff - I had taken a seat on the normal guest chairs (I had been on the exam table) and she was like “no, no! We don’t want to move you. You just stay right there and get comfortable.” I do some deep breathing, she returns with the reader and bam - perfect! I can’t recall the exact numbers, but I was back in the “it’s okay/normal” range. No EKG needed! She explained that a lot of people come in and the same thing happens and yep - it’s the social anxiety! So, the next time anyone gives you grief, feel free to use my story as proof (my name is Cari & you can call me your friend!) that anxiety is REAL and causes SERIOUS CHANGES to the body! I was in “Heart-attack mode” JUST from visiting the doctor! Think about all the times I just go food shopping, have to speak up for myself somewhere like the bank, make an important phone call.... it puts stress on the body. No wonder I’m always exhausted!
7 notes
·
View notes
Text
im early in my transition so i haven't ran into personal discrimination yet though this could always change, esp since i'm getting my first blood tests done soon! but yeah it's kind of fucking crazy how there's so much research on HRT and its affects that's straight up ignored because it's done by trans people. it's not my biggest gripe with cis people but it gets annoying discussing DIY and them getting scared like "oh just be careful you don't want to hurt yourself" and like i have less of a chance of doing serious harm to my body than some idiot doctor prescribing low or no E at all lol shut the fuck up. while i've only looked into E i wouldn't be surprised if T is also similarly mundane to DIY and is only more tightly regulated as a controlled substance because of stupid fucking athletes instead of transition which in theory is so easy that it should be a fucking OTC thing. honestly, people need to get more comfortable with the idea that doctors and nurses are not automatically better than us. non-medical practitioners get this idea that there's an inherent virtue to having a medical degree, that studying the human body and how to care for it makes them smarter and better than us. but doctors are just people, they probably take their jobs for granted and assume they know everything there is to know, or just don't think their job is that special, and not in the "they're super enlightened and humble" kind of way but the "lol it make a da money i wonder if i should do tech instead or something" kind of way. and like people they're not immune to heterosexism, racism, or other kinds of bigotry - doctors do this shit to marginalized groups all the time! denying us hrt, refusing life-saving treatment of fat people with real conditions because "well maybe if u exercised u would just be fine," and treating POC like shit because that's inescapable no matter where you go. if you ever knew someone getting a medical degree and they seemed like a dipshit, they probably have that degree and are in the field now! and they're probably still a dipshit! in a better world hrt would not be administered by dipshits but instead by trans people, and there better be at LEAST one transfem running every clinic else i'm still going to be weary of hrt clinics.
one of the cool things about being trans is that doctors and pharmacists will start straight up lying to you. "we can't prescribe this bc it has no effect on someone of your birth sex" hmm okay well one of us has read the research and it's not you. I'm the pharmacist now, give me your degree, and, I presume, sceptre.
1K notes
·
View notes
Note
Hi! I’d love to know more about ketamine therapy, if you feel okay to share what it is/what uses it has for you/etc. Reading your post was the first time I’ve heard about it.
Sure! I don't mind talking about it.
Ketamine therapy is used to treat mental health disorders including anxiety, depression, OCD, and PTSD.
Personally, I use it mostly for depression symptoms but I also use it for anxiety although some research shows that it may not be as effective for anxiety as it is for depression, PTSD, and OCD.
Basically, ketamine therapy involves the administration of ketamine in either a tablet form or via IV. Anecdotally, I've been told that the tablet form is not as effective as IV, but using tablets is WAY cheaper. It can be pretty expensive because most insurance doesn't cover it so it's mostly out of pocket.
The actual therapy part via tablet or IV is pretty similar, but tablet form can be done at home, whereas IV is done at a clinic. When it's done at home, it's mailed to you. I have to sign off for the packages and be home for the delivery, otherwise it gets sent to another place for pick up where I have to sign off for it.
I've done both and prefer the IV method but it's pricey. I go to a local clinic near me, but I know some people will travel hours to go to a clinic. Some people don't have the option to travel to a clinic or it's just not practical because of cost so some people do the at home tablet method.
The IV method and tablet method both involve a consultation either in person or online. to see if symptoms are serious enough to qualify for ketamine therapy. I did my tablet consultation online through Mindbloom, but there are other companies. The IV method for me was done via a phone call to the local clinic and then they were put in contact with my psychiatrist. Some clinics have a psychiatrist on staff, but the one I've used doesn't so thats why they needed to be put in contact with my psychiatrist. The local clinic is run by anesthesiologists. Ketamine is an anesthetic technically.
So after consultation, you set up appointments for IV. On mindbloom I did the same and met with a nurse practitioner and a ketamine guide for my experience to walk me through the process.
Both IV and tablet methods had 6 initial sessions that were done in a matter of a few weeks. The IV consultation had me do 6 sessions over a course of 2 weeks. The tablet method was over a longer period of time. For the tablet method I did 2 initial sessions and then after that I did it once a week for 4 weeks. For some people like myself they recommend following up for maintenance / treatment of symptoms. This looks different depending on severity of symptoms. Some people do maintenance at an IV clinic twice a year, every 3 months, or once a month. They recommended once a month for me. I know with mindbloom they have an 18 pack available after you've done your initial session. I'm not sure exactly how it works, but I know they bill you monthly for that method so you don't have to pay upfront for all costs. Mindbloom doesn't take insurance.
An at home session with a tablet looks like this for me. You have to have a person on hand to check in on you to make sure you are safe and not having any issues like an adverse reaction to the ketamine. For me, that's my fiance. You measure your blood pressure with a cuff provided by Mindbloom to make sure you are in a healthy range to start therapy. You put the tablets in your mouth for 7 minutes, and during this time you have to allow the saliva in your mouth to gather. You aren't supposed to swallow during this time. You open the app and there's a guided message for the first few minutes. Then it plays music during the journey. They recommend putting on headphones and lying down while wearing an eye mask. After 7 minutes are up, I spit out the ketamine and saliva into a zip lock bag as advised by Mindbloom. This is to keep the ketamine away from contaminating local water supplies. You're not supposed to spit it into a sink or directly into the trash for that reason. After I spit it up, I lie down and focus on a mantra. One for instance that I used was "I release my depression." This is done for an hour. During that time my fiance comes in and checks in on me every 15 minutes. After the session you're supposed to avoid negative stimuli to let the ketamine work on your brain. I usually eat afterwards because you're supposed to avoid eating for several hours before so you aren't nauseous from the ketamine. I've never experienced nausea but I don't want to risk it. Mindbloom sends anti-nausea meds along with the ketamine. They recommend journaling afterward but I don't because I never found it to be helpful when I tried. Before session I journal to clear my mind. I normally do yoga or meditate beforehand to get myself into a good headspace for my session.
For an IV session, I go to the clinic at my appointment time and am walked back into a private room with an armchair that has heating and massage functions. They administer the IV to a vein in my hand or wrist and hook it up to a machine that administers the ketamine. They also hook me up to a blood pressure cuff. They monitor my vitals on the machine during session via a computer and leave me alone during session. During this time things get trippy. You can move but I find that I have no desire to move. They recommend wearing headphones and bringing a blanket. After session I usually go home and eat or go out to eat with my fiance. I don't have issues with nausea but some people do. I've heard this is more common when you're older or elderly. The anesthesiologists will come in and check in on me during this time but basically I just vibe the whole time. I try to focus on something I need to work through during this time and I mostly just let my mind wander however it will and I listen to music. There are several lists on Spotify that have been made specifically for ketamine therapy by other users. I know one client at the ketamine clinic I go to listens to the grateful dead the whole time so it's really all up to preference.
I've probably given you more info than needed but I've never really talked about it indepth on tumblr so I figured why not. Lol. But that's an indepth look into what it's like, what i use it for and what it is. Hope this post was helpful!
1 note
·
View note