#myoglobinuria
Explore tagged Tumblr posts
Text
TL;DR - no but you would *really likely* have other symptoms with it plus it would still be there when your period is done. I don't know enough to say that it's totally fine but I can't find anything to support that in my textbook.
I freely admit to not being an expert and I can double check with my professors, but from what my textbook says the answer is no, but you would probably have other signs anyway, and if it's pathogenic you'll probably have it after your period ends too.
Whole blood cells in the urine (hematuria) is usually from menstruation but it can also be from kidney stones, renal disease, pyelonephritis (kidney infection) and trauma to either the kidneys or the genitourinary area. AIl of these have other symptoms and I can't imagine anything but the last and *maybe* the first one being transient.
Menstrual blood could *technically* cover up the presence of hemoglobin from lysed red blood cells in the urine (hemaglobinuria) but the latter is from things like intravascular hemolysis from transfusion reactions, hemolytic anemias, severe burns, malaria, and strenuous exercise. The last one isn't considered pathogenic and would go away. Everything else has different symptoms along with it or isn't transient.
The last thing under blood in the urine is myoglobinuria, which is really a heme-containing-protein in the urine that's not from RBCs at all and also makes your urine brown and comes from things like crush syndrome, or comas, or alcoholism, or anything else that causes muscle destruction so.... I am going to assume that would also stick around.
I am sourcing this from Urinalysis and Body Fluids by Susan King Strasinger 2014 textbook, page 62 and 84. If someone out there has better information lemme know and feel free to correct me.
not 2 be gross on main or whatever but what if there’s blood in your urine while you’re on your period. you wouldn’t be able to tell at home unless there were other symptoms right?
#not gross at all dw abt it#text#always fun when someone talks about my career :-)#i can send you the tbook if you want btw#or a link to where I got it from#also menstrual blood has hematuria clots and mucus if that helps#it could still occlude more nefarious causes of any type of blood or blood components in our urine because of how the test strips work#but it does look different#maybe that doesn't help lol#context is that I am in a medical laboratory technology program
5 notes
·
View notes
Text
We have a pt who has rhabdomyolysis from taking a statin and being on the floor for 3 days. She's old, so she had muscle breakdown. The attending is Dr. Giraldo, who is really nice and awesome. He asked me what urine test you use to diagnose rhabdo and I totally forgot about myoglobinuria so I said I wasn't aware. He told me to look it up. Then after we were rounding for a bit, my brain remembered myoglobinuria! So I told him. But now I want to look up the details of diagnosing rhabdo so I can present to him tomorrow. But we also have a pt with CKD who may have kidney stones and the attending and the resident didn't realize that you can diagnose a kidney stone with a non-contrast CT. I remembered learning that last year during my emergency medicine rotation. They had ordered a KUB because they thought you would need to use contrast for the CT and so they didn't want to get the CT because the contrast would hurt the pt's kidney. But you don't use contrast to diagnose nephrolithiasis with CT. So at least I remembered something! This is from UpToDate:
●The clinical manifestations of rhabdomyolysis include myalgias, weakness, red to brown urine due to myoglobinuria, and elevated serum muscle enzymes (including creatine kinase [CK]). The degree of myalgias and other symptoms varies widely, and some patients are asymptomatic. Fever, malaise, tachycardia, and gastrointestinal symptoms may be present. Muscle swelling may occur with rehydration.
This pt was actually tachycardic in the ED. So that tracks.
●The laboratory findings that characterize rhabdomyolysis include an acute elevation in the CK and other muscle enzymes and a decline in these values within three to five days of cessation of muscle injury. The other characteristic finding is the reddish-brown urine of myoglobinuria, but this finding is often absent because of the relative rapidity with which myoglobin is cleared. The serum CK is generally entirely or almost entirely of the MM or skeletal muscle fraction, although small amounts of the MB fraction may be present.
●Other manifestations include fluid and electrolyte abnormalities, many of which precede or occur in the absence of acute kidney injury, and hepatic injury. Hypovolemia, hyperkalemia, hyperphosphatemia, hypocalcemia, hyperuricemia, and metabolic acidoses may be seen. [I think the pt also had hypocalcemia, but it wasn't true hypocalcemia because the albumin was low, so her corrected Ca2+ was in the normal range based on the lab values at the hospital; she did have acidosis too I think]. Hyperkalemia may result in cardiac dysrhythmias. Later complications include acute kidney injury (AKI), hypercalcemia, compartment syndrome, and, rarely, disseminated intravascular coagulation.
●We diagnose rhabdomyolysis in a patient with an acute muscular illness or injury based upon a marked acute elevation in serum CK; the CK is typically at least five times the upper limit of normal and is frequently greater than 5000 international units/L. Key diagnostic laboratory studies include the creatine kinase and urinalysis, including dipstick and microscopic evaluation. Myoglobinuria (present in 50 to 75 percent of patients at the time of initial evaluation) results in a positive test for blood on the urine dipstick but without red blood cells on the microscopic examination of the urine. And for this pt, the UA showed a small amount of blood, so that could have been myoglobin in the urine, but we didn't order a microscopic analysis. She also has a UTI, so that could be from the UTI as well. Also, the other day Dr. Agarwal asked how long you treat UTIs. When in the hospital, you can treat with ceftriaxone until the pt has clinically improved.
●The differential diagnosis depends upon the combination of findings present. It includes myocardial infarction, other causes of red or brown urine, inflammatory myopathy, and local causes of pain, such as deep vein thrombosis or renal colic.
The characteristic triad of complaints in rhabdomyolysis is muscle pain, weakness, and dark urine. Additional symptoms that are more common in severely affected patients include malaise, fever, tachycardia, nausea and vomiting, and abdominal pain. Altered mental status may occur from the underlying etiology (eg, toxins, drugs, trauma, or electrolyte abnormalities).
The hallmark of rhabdomyolysis is an elevation in CK and other serum muscle enzymes. The other characteristic finding is the reddish-brown urine of myoglobinuria, but because this may be observed in only half of cases, its absence does not exclude the diagnosis. Routine lab tests, including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), vary greatly depending on the underlying cause of rhabdomyolysis. Infections and crush injuries are associated with marked elevation of the acute phase reactants and peripheral white blood cell (WBC) count, while these markers of inflammation would likely be normal or only minimally raised in patients with other etiologies, such as drug-induced or electrolyte derangements.
Serum CK levels at presentation are usually at least five times the upper limit of normal, but range from approximately 1500 to over 100,000 international units/L. The mean peak CK reported for each of a variety of different causes and for patients with both single and multiple causes ranged from approximately 10,000 to 25,000 in the largest series; exceptions were the three patients with malignant hyperthermia, whose values averaged almost 60,000.
I googled the normal serum CK level:
In a healthy adult, the serum CK level varies with a number of factors (gender, race and activity), but normal range is 22 to 198 U/L (units per liter). Higher amounts of serum CK can indicate muscle damage due to chronic disease or acute muscle injury.
The CK is generally entirely or almost entirely of the MM or skeletal muscle fraction; a small proportion of the total CK may be from the MB or myocardial fraction. The presence of MB reflects the small amount found in skeletal muscle rather than the presence of myocardial disease. Elevations in serum aminotransferases are common and can cause confusion if attributed to liver disease. In one study, aspartate aminotransferase (AST) was elevated in 93.1 percent and alanine aminotransferase (ALT) in 75 percent of rhabdomyolysis cases in which the CK was greater than or equal to 1000 units/L. In only one instance was the ALT greater than the AST, although the AST declines faster than the ALT as the rhabdomyolysis resolves, such that the two may equalize after a few days.
The serum CK begins to rise within 2 to 12 hours following the onset of muscle injury and reaches its maximum within 24 to 72 hours. A decline is usually seen within three to five days of cessation of muscle injury. CK has a serum half-life of about 1.5 days and declines at a relatively constant rate of about 40 to 50 percent of the previous day's value. In patients whose CK does not decline as expected, continued muscle injury or the development of a compartment syndrome may be present.
Urine findings and myoglobinuria — Myoglobin, a heme-containing respiratory protein, is released from damaged muscle in parallel with CK. Myoglobin is a monomer that is not significantly protein-bound and is therefore rapidly excreted in the urine, often resulting in the production of red to brown urine. It appears in the urine when the plasma concentration exceeds 1.5 mg/dL. Visible changes in the urine only occur once urine levels exceed from about 100 to 300 mg/dL, although it can be detected by the urine (orthotolidine) dipstick at concentrations of only 0.5 to 1 mg/dL . Myoglobin has a half-life of only two to three hours, much shorter than that of CK. Because of its rapid excretion and metabolism to bilirubin, serum levels may return to normal within six to eight hours.
Thus, it is not unusual for CK levels to remain elevated in the absence of myoglobinuria. In rhabdomyolysis, myoglobin appears in the plasma before CK elevation occurs and disappears while CK is still elevated or rising. Therefore, there is no CK threshold for when myoglobin appears. As above, rhabdomyolysis does not occur unless CK is elevated five times or more above the upper limit of normal. Routine urine testing for myoglobin by urine dipstick evaluation may be negative in up to half of patients with rhabdomyolysis. Pigmenturia will be missed in rhabdomyolysis if the filtered load of myoglobin is insufficient or has largely resolved before the patient seeks medical attention due to its rapid clearance.
Both hemoglobin and myoglobin can be detected on the urine dipstick as "blood;" microscopic evaluation of the urine generally shows few red blood cells (RBC) (less than five per high-powered field) in patients with rhabdomyolysis whose positive test results from myoglobinuria. Such testing is not a reliable method for rapid detection of myoglobin if RBC are present or in patients with hemolysis due to its lack of specificity for myoglobin. Hemoglobin, the other heme pigment capable of producing pigmented urine, is much larger (a tetramer) than myoglobin and is protein-bound. As a result, much higher plasma concentrations are required before red to brown urine is seen, resulting in a change in plasma color.
Hypocalcemia, which can be extreme, occurs in the first few days because of entry into damaged myocytes and both deposition of calcium salts in damaged muscle and decreased bone responsiveness to parathyroid hormone. During the recovery phase, serum calcium levels return to normal and may rebound to significantly elevated levels due to the release of calcium from injured muscle, mild secondary hyperparathyroidism from the acute renal failure, and an increase in calcitriol (1,25-dihydroxyvitamin D).
Severe hyperuricemia may develop because of the release of purines from damaged muscle cells and from reduced urinary excretion if acute kidney injury occurs.
●Metabolic acidosis is common, and an increased anion gap may be present. Our pt did have an anion gap and I wondered why. I guess it's because there's more uric acid in the blood.
Acute kidney injury — Acute kidney injury (AKI, acute renal failure) is a common complication of rhabdomyolysis. The reported frequency of AKI ranges from 15 to over 50 percent. The risk of AKI is lower in patients with CK levels at admission less than 15 to 20,000 units/L; risk factors for AKI in patients with lower values include dehydration, sepsis, and acidosis. [Our pt had peed a lot and was on the floor for 2 to 3 days, so she was probably dehydrated, increasing her risk for AKI]. Volume depletion resulting in renal ischemia, tubular obstruction due to heme pigment casts, and tubular injury from free chelatable iron all contribute to the development of renal dysfunction. Reddish-gold pigmented casts are often observed in the urine sediment.
Compartment syndrome — A compartment syndrome exists when increased pressure in a closed anatomic space threatens the viability of the muscles and nerves within the compartment. Compartment syndrome is a potential complication of severe rhabdomyolysis that may develop after fluid resuscitation, with worsening edema of the limb and muscle. Lower extremity compartment syndrome can also be a cause of rhabdomyolysis, as may occur after tibial fractures.
Disseminated intravascular coagulation — Infrequently, severe rhabdomyolysis may be associated with the development of disseminated intravascular coagulation due to the release of thromboplastin and other prothrombotic substances from the damaged muscle.
EVALUATION AND DIAGNOSIS
Indications for diagnostic testing — Diagnostic testing should be performed in individuals with:
●Both myalgias and pigmenturia.
●Either myalgias or pigmenturia, with a history suggesting the presence or recent exposure to a potential cause or event.
●The absence of myalgias and pigmenturia in a clinical setting associated with increased risk for rhabdomyolysis, as symptoms may be vague or absent in up to 50 percent of patients. The diagnosis should be suspected following prolonged immobilization [like our pt who was on the floor for 2 to 3 days], in any stuporous or comatose patient, or in a patient who is otherwise unable to provide a medical history and has one or more of the following:
•Muscle tenderness
•Evidence of pressure necrosis of the skin
•Signs of multiple trauma or a crush injury
•Blood chemistry abnormalities suggesting the possibility of increased cell breakdown, such as hyperkalemia, hyperphosphatemia, and/or hypocalcemia
•Evidence of acute kidney injury
●Acute muscle weakness and marked elevation of creatine kinase (CK).
Diagnostic evaluation — We obtain the following key diagnostic laboratory studies:
●Creatine kinase – In addition to elevation of the CK, other muscle enzymes are typically elevated (eg, aldolase, aminotransferases, lactate dehydrogenase), but such testing is not usually necessary to make the diagnosis. However, elevations in aminotransferases or lactate dehydrogenase may suggest the need for CK testing if it has not been performed in a patient in whom such abnormalities may potentially be due to muscle injury rather than hepatic injury or another cause.
●Urinalysis, including dipstick and microscopic evaluation – Evidence of myoglobinuria should be sought by routine urine dipstick evaluation combined with microscopic examination. Testing of the unspun urine or the supernatant of the centrifuged urine will be positive for "heme" on dipstick if myoglobinuria is present, even if red to reddish brown urine is not evident macroscopically. The visual and microscopic examination of the sediment from a fresh urine specimen is required to exclude the presence of red blood cells (RBC) as the cause of positive testing; RBC in an older specimen may hemolyze over time, confounding the results.
In patients with persistent red to reddish-brown urine, myoglobinuria is suggested when the urine tests positive for heme by dipstick after centrifugation, while the plasma has a normal color and tests negative for heme.
Myoglobinuria lacks sensitivity as a test for rhabdomyolysis; it may be absent in 25 to 50 percent of patients with rhabdomyolysis due to the more rapid clearance of myoglobin, compared with CK, following muscle injury. Myoglobin also decreases rapidly in a similar fashion in patients with renal failure, suggesting a role for extrarenal metabolism and clearance in such patients.
We also obtain the following tests, which may help in prompt recognition of other potentially dangerous manifestations, in differential diagnosis, and in identifying the cause:
●Complete blood count, including differential and platelet count
●Blood urea nitrogen, creatinine, and routine electrolytes including potassium
●Calcium, phosphate, albumin, and uric acid
●Electrocardiography
Additional testing, such as evaluation of suspected metabolic myopathy or toxicology screening for drugs of abuse, depends upon the clinical context.
Diagnosis — We make the diagnosis of rhabdomyolysis in a patient with either an acute neuromuscular illness or dark urine without other symptoms, plus a marked acute elevation in serum creatine kinase (CK). The CK is typically at least five times the upper limit of normal, and is usually greater than 5000 international units/L. No absolute cut-off value for CK elevation can be defined, and the CK should be considered in the clinical context of the history and examination findings.
MANAGEMENT
The major issues in the treatment of patients with rhabdomyolysis include:
●Recognition and management of fluid and electrolyte abnormalities, which should be initiated regardless of renal function and which may prevent severe metabolic disturbances and acute kidney injury
●Identification of the specific causes and the use of appropriate countermeasures directed at the triggering events, including discontinuation of drugs or other toxins that may be etiologic factors
●Prompt recognition, evaluation, and treatment of compartment syndrome in patients in whom it is present
7 notes
·
View notes
Photo
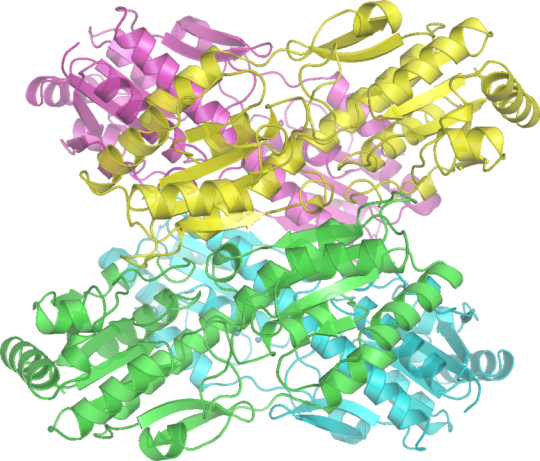
Q. Which Glycogen Storage Disease results from inability of cells to utilize carbohydrates for energy? (Hint: It's the only one to directly affect glycolysis!)
.
.
.
A. GSD VII (Tarui Disease) is due to defect in phosphofructokinase, the rate-limiting step in glycolysis and a gate-keeper in cellular metabolism of glucose. Lack of cellular energy leads to exercise-induced rhabdomyolysis, myoglobinuria, and hemolytic anemia that has infantile, classic, late-onset, and primarily hemolytic forms. Named for the Japanese physician who identified it in 1965, Seiichiro Tarui (1927- ).
Image credit Richard Wheeler, Wikipedia (2006).
13 notes
·
View notes
Text
Horrible, Horrible Little Factlets
Since I'm learning way too much every day this should act as a surrogate for 100 days of productivity.
Day 1 (and Every Day Prior^tm):
secondary syphilis: snail-track ulcers = mucosal erosions
IBD arthropathy: nondeforming nonerosive migratory large joint oligoarthritis
PCV: most common compliations: thrombosis + bleeding (despite adequate/supranumerary platelets; d/t thrombasthenia)
small cell lung cancer: HPOA and physical stigmata of Cushing's are RARE due to relatively rapid course of disease; hypercalcaemia is also rare despite high rate of skeletal mets
TEN: water loss → ↑blood viscosity → hypercoagulability → VTE
Acute tubular necrosis: ↓volume/myoglobinuria → infuse mannitol! (d/t removal of casts and relief of swelling of tubular cells, but generally poorly understood)
Core body temp <30°C: withhold all drugs EXCEPT adri, and limit shocks to 3 no.s max
Close to comprehensive causes of prolonged QT: erythromycin, HCQS, ciprofloxacin, class 1 (phenytoin, flecainide, procainamide, quinidine) and 3 antiarrhythmics (amiodarone, sotalol, ibutilide), antipsychotics, second generation antihistamines (astemizole, loratadine, terfenadine), subarachnoid haemorrhage, hypokalaemia, hypomagnesaemia, hyponatraemia, hypocalcaemia, hypothermia, congenital
Like a bitch I forgot serotonergics like ondansetron, TCAs and SSRIs (of which citalopram/escitalopram have the highest risk of prolonging QT)
Acute lithium tox -> coarse tremor, chronic lithium tox -> fine tremor
Bisphosphonate if T-score < 1.5SD below mean
Cerebral oedema in DKA: NOT due to osmolar disturbances! mechanism poorly described.
HLA-C (especially subtype W5) is associated with hyperacute graft rejection
Bartter syndrome vs Gitelman syndrome: both have hypokalaemic hypotension, but Bartter presents in infancy/childhood with hypercalciuria with eumagnesaemia, while Gitelman presents later with hypocalciuria with hypomagnesaemia. NB: treat Gitelman hypokalaemia with potassium-sparing diuretics (amiloride, eplerenone)
Dialysis disequilibrium: neurological deficits seen with first haemodialysis session. Hyperosmolar, uraemic blood draws water out of brain cells. During dialysis, rapid removal of urea → rapid drop in serum osmolarity → sudden osmolar gradient between blood and brain cells → rapid influx of water into brain parenchyma to compensate, leading to obtundation, irritation, visual disturbances, focal deficits. Start with short, frequent sessions and taper upwards to longer (4 hour), less frequent sessions
Lower zone lung fibrosis: idiopathic pulmonary fibrosis, connective tissue disorders (EXCEPT ankylosing spondylitis), drugs (amiodarone, MTX, nitrofurantoin, bleomycin), asbestosis
[other pneumoconioses and radiation predominantly affect the upper lobes; notably berylliosis causes a sarcoid like hilar lymphadenopathy]
Normal pressure hydrocephalus: impairment in mobility is due to failure of ability to plan walking movements, which is why they are able to maintain posture when still, unlike with true ataxia. This is called gait apraxia
Nelson's disease: post-adrenalectomy pituitary ACTHoma
Coeliac's is assoc with functional hyposplenism
Carbapenems lower valproate levels: VPA is glucuronidated in the liver to inactive VPA-glucuronide, but is also deglucuronidated back to VPA, achieving a balance that is slowly renally cleared. Carbapenems inhibit the deglucuronidation of VPA-G, increasing VPA-G levels which are quickly renally cleared
Growth hormone supplementation can increase colon cancer incidence
5 notes
·
View notes
Text
Iris publishers-Open access journal of Rheumatology & Arthritis Research|A Case of Dermatomyositis presenting with Fulminant Rhabdomyolysis without Myoglobinuric Acute Kidney Injury-A Rare Clinical Manifestation

Authored by Richmond Ronald Gomes
Abstract
Rhabdomyolysis and myoglobinuria are a rare complication of dermatomyositis. Rhabdomyolysis has a wide range of presentations, from asymptomatic to life-threatening. The most dramatic presentation can result in acute renal failure, electrolyte imbalances, and/or disseminated intravascular coagulation (DIC). Recognition of this fact has important therapeutic implications as patients require immunotherapy in addition to the symptomatic treatment for renal failure. Here we present a 30 year old male banker presented with progressive muscle pain and weakness for 10 days and high colored urine for 3 days. Laboratory findings suggested rhabdomyolysis. A diagnosis of dermatomyositis was based upon the proximal muscle weakness on both upper and lower limbs, skin lesion over face and upper trunk, elevated muscle enzyme levels, muscle biopsy and skin biopsy findings. The patient was managed with high dose prednisolone and steroid sparing agent. His muscle power did improve slightly. In our view, this is an interesting case in that dermatomyositis cause fulminant rhabdomyolysis without causing myoglobinuric acute kidney injury (AKI) due to direct toxic effect of myoglobulin on renal tubule.
Read more: Full Text For more articles in Archives of Rheumatology & Arthritis Research please click on: https://irispublishers.com/arar/archive.php For more open access journals in Iris Publishers
#Irispublishers#Iris Publishers LLC#rheumatlogy#arthritis#Orthopedic Trauma#Arthroplasty#Pediatric Rheumatology
1 note
·
View note
Text
Case time!
We often get fictional/modified real cases presented to us during our lectures to assist our learning. I thought it’d be interesting to explore them on here and summarise the findings and tentative diagnoses. I might even make a small series out of them.
***I cannot guarantee all the interpretations are correct as many of these cases are explored by students and not every aspect is checked over by the lecturer. If you have alternative interpretations, differential diagnoses, or notice any mistakes, please message me or add your thoughts onto the post!***
Let’s call this patient Mary.
Mary is a 5 year old mare with a four-day history of pigmenturia and lameness. She had a complete blood count (CBC), a biochemistry panel, and a urinalysis performed. Here are the results and associated interpretations:

There is a mild erythrocytosis, most likely due to dehydration or splenic contraction. There is also a mild neutrophilia with a moderate left shift, and a mild lymphopenia. This can be indicative of stress or mild inflammation. There is a mild hyperfibrinogenaemia which may be due to dehydration or mild inflammation as a positive acute phase protein.

BUN and creatinine are both moderately to markedly increased (the horse is azotaemic), with an additional mild hyperphosphataemia. These findings are indicative of renal injury, however hyperphosphataemia can also be seen due to muscle breakdown. There is a hypocalcaemia which may coincide with the hypoalbuminaemia as a fair portion of blood calcium is bound to albumin. The albumin may be low due to an acute phase reaction (negative acute phase protein) or due to a protein-losing nephropathy. The hyperkalaemia may be due to the renal injury, metabolic acidosis (increased anion gap with reduced bicarbonate*) shifting potassium extracellularly, or due to muscle breakdown. The metabolic acidosis can be attributed to the loss of bicarbonate and/or the increased uraemic acids in circulation from the azotaemia. AST is markedly increased with a concurrent marked increase in CK which is highly suggestive of significant muscle damage. Hypermagnesaemia is also suggestive of muscle breakdown.
*Total CO2 is meant to be bicarbonate.

As a free-catch sample a few bacteria and epithelial cells can be considered insignificant, however culture can be pursued with a catheterised sample if there is reasonable concern for a urinary tract infection. There wasn’t in this case.
Calcium carbonate crystals are a normal finding in horses.
Red urine and the presence of occult blood can indicate either haematuria, haemoglobinuria, or myoglobinuria. The presence of 2+ protein and granular casts, along with a USG of 1.018 (normally much higher) are all suggestive of renal tubular damage.
From the above findings, we suggested that this horse had experienced a significant event of muscular damage which resulted a secondary kidney injury due to the nephrotoxic effects of myoglobin. Most likely differentials for the muscular damage were either a snake bite or exertional rhabdomyolysis.
9 notes
·
View notes
Text
Possible Drug Interaction Between Adderall and Statin Drugs

Around 40% of the U.S population receive prescriptions for four or more medicines, due to which there is a drastic increase in potential drug interaction and its adverse effects.
Adderall is prescribed medicine to treat attention-deficit hyperactivity disorder (ADHD) and narcolepsy. Adderall is a combination of two central nervous system (CNS) stimulants, amphetamine and dextroamphetamine. This drug belongs to the class of medicines called stimulants.
Statins help to lower the levels of cholesterol in the blood by reducing the production of cholesterol. It blocks the enzyme in the liver that is responsible for making cholesterol.
When these drugs are taken together; potential drug interactions may lead to several severities such as myopathy, rhabdomyolysis, and myoglobinuria. Hence, take these medicines only on your doctor’s advice.
This article helps you to understand what Adderall and statin drugs are, how they work, and the potential drug interactions between them.
What is Adderall, and How Does it Work?
Adderall is an FDA- approved drug. It is available only on the prescription of a registered doctor. It is the first line of treatment for ADHD.
Studies have shown that it has helped to improve attention and focus and reduces impulsive behavior. Around 75 to 80% of children with ADHD have seen improved symptoms with Adderall.
Adderall is also used to treat narcolepsy; studies have shown that it has increased daytime wakefulness in people with narcolepsy.
Studies also suggest that people with ADHD lack normal levels of neurotransmitters and have dopamine dysfunction. As Adderall mainly contains amphetamine and dextroamphetamine, they act as central nervous system stimulants. They affect the nerves and chemicals in the brain that contribute to hyperactivity.
Dopamine belongs to the family of catecholamines, and it is synthesized by nervous tissue and the adrenal gland; it plays a vital role in motor control, motivation, arousal, and emotional responses.
Adderall enhances the availability of neurotransmitters such as dopamine and norepinephrine in your brain. These chemicals are responsible for increased alertness and attention. It also brings a calming effect during ADHD.
What is a Statin, and How Does it Work?
Statins belong to the class of drugs that reduces the production of cholesterol by the liver. It blocks the enzyme which produces cholesterol. Statins are also known as HMG-CoA (hydroxy-methyl glutaryl-coenzyme A) reductase inhibitors.
When cholesterol production is increased in the cells, it will lead to the development of atherosclerosis; cholesterol-containing plaques form within arteries. These plaques block the arteries and reduce the blood flow to tissues. When these plaques rupture, a blood clot is formed, which leads to blockage in the artery. This condition leads to several health problems such as heart attack and angina.
Statins reduce the production of cholesterol, slows the formation of new plaques, and helps to reduce the size of plaques that are already present. Although the mechanism of the statins is less studied, it is believed that it may stabilize plaques and make them less prone to rupture and develop clots.
According to research studies, statins are inhibitors of hydroxymethylglutaryl-CoA (HMG-CoA) reductase, which plays a significant role in cholesterol synthesis. Generally, statins are recommended in the treatment of atherosclerosis, myocardial infarction, and stroke. However, frequent monitoring of the patient is advised while taking statins, as these drugs are known to cause various adverse effects and drug interactions.
What are Potential Drug Interactions Between Adderall and Statin Drugs?
According to a report on medication safety issued by Institute for safe medication practices, 2 out of 3 patients who visit a health care provider or doctor have been prescribed at least one medicine. Most of the time the patients are advised with 3 or more drugs; usage of more drugs leads to drug interaction and its adverse effects.
Adderall can interact with several other drugs, food, and certain supplements as well. These interactions may lead to different effects. For example, some of the medicines may enhance the effect of the drug, some drugs reduce the impact, and sometimes drug-drug interactions may lead to several side effects.
When you are on Adderall drugs, and if you take statins, this combination may lead to several health complications such as;
1. Rhabdomyolysis
According to the federal drug regulators, medicines such as Adderall, Concerta , and Ritalin which are used to treat ADHD, can cause severe muscle injury and kidney damage leading to Rhabdomyolysis.
Rhabdomyolysis is a well-documented side effect caused due to statin therapy. This risk is increased when you are on drugs that inhibit monoamine oxidases.
Rhabdomyolysis is a side effect that has been linked with drug-drug interaction. It causes muscle fibers to break down, which releases a protein, myoglobin; this protein damages the kidney.
Patients under Zocor (simvastatin, a cholesterol-lowering drug) take Zocor at higher doses above 20g while they are under antidepressants or ADHD, or Cordarone drug, the risk of developing rhabdomyolysis would be very high. This can vary in severity and can be fatal too. Consult your physician before taking any medications while you are on Adderall drugs.
2. Cardiovascular complications
Adderall is a prescribed CNS stimulant drug for ADHD and is recommended for all age groups. Although the exact mechanism of cardiovascular impact of ADHD drugs is not well studied. Some of the studies suggest that Adderall increases the risk of cardiovascular events such as increased blood pressure, heart rate and improved circulation of catecholamines inducing vasospasm and increases inflammation.
When Adderall is taken with a statin drug, it may be beneficial because statins are the prescribed drugs to lower the risk of heart attack, stroke, and death in those with high risk for heart diseases.
Hence it is crucial to consult your doctor while you are on 2 to 3 drugs at the same time; ask your doctor regarding the drug-drug interactions.
Some Tips to Avoid Drug Interactions
· Take the drugs that are prescribed by your doctor
· Learn about the side effects of all drugs you take
· Ask your doctor what type of drugs, foods, and supplements to be avoided when you are taking these drugs
· If you experience any adverse effects, report them to your doctor immediately
· Tell your healthcare provider the list of medicines you are taking
Final Words
When you are prescribed one or more drugs for your illness or if you are on long-term drug therapy due to any chronic disease, understanding these drug interactions is essential. While visiting your doctor for any medical help make sure to tell them about the medications you are already taking to avoid any potential drug interactions.
Always follow prescription and doses as advised by your healthcare provider; if you find any allergic reactions or symptoms consult your doctor immediately.
0 notes
Text
Equine rhabdomyolysis
= tying up/ Monday morning disease.
Rhabdomyolysis = muscle injury --> death of muscle fibres --> myoglobin released into blood --> secondary acute inflammatory response.
Equine rhabdomyolysis syndrome = stiff gait + muscle cramp --> recumbency + muscle lysis + compartment syndrome.
A high starch diet = increased glycogen stored in muscle cells. At exercise there is anaerobic metabolism and the glycogen is converted to lactic acid --> arteriole constriction --> muscle hypoxia and cell lysis --> myoglobinaemia --> myoglobinuria --> pigment nephropathy --> renal failure --> death.
Exertional rhabdomyolyisis = stiff, decreased performance, recumbency, sweating, increased HR and RR, muscle fasciculation and pain, myoglobinuria. Ion channel abnormality --> abnormal muscle contractions. Diagnosis = increased CK and AST, exercise test (CK and AST measured pre and post exercise), urinalysis (myoglobinuria). Treatment = total rest, analgesia, massage, diuresis by overhydration, decreased dietary calcium and carbohydrate. Once recovered from the acute disease keep in a paddock and exercise every day (short bursts of fast exercise, missing a day increases risk of recurrence).
Sporadic exertional rhabdomyolysis = no underlying myopathy, signs due to high dietary carbohydrates and overexertion.
Recurrent exertional rhabdomyolysis = underlying myopathy (calcium regulation disorder) - increased risk if high dietary carbohydrate intake.
youtube
4 notes
·
View notes
Text
Normal urine specific gravity is 1.010.
Urine osmolarity can be measured using freezing point and vapor pressure.
RBC - red, hazy
Hemoglobinuria- red plasma, clear red urine
Myoglobinuria- Clear dark red urine
Bilirubin - yellow foam, yellow amber urine
Protein - white foam
Phenazopyridine - yellow foam, yellow orange urine
Urobilin- no foam, yellow orange
Biliverdin - yellow green urine
0 notes
Text
Emicizumab Associated Rhabdomyolysis in Hemophilia A | Atlantis Press
Emicizumab Associated Rhabdomyolysis in Hemophilia A | Atlantis Press
Emicizumab is increasingly the front-line treatment for patients with Hemophilia A with or without inhibitors. Rhabdomyolysis is a syndrome of muscle necrosis and release of intracellular muscle constituents into the circulation. Creatine kinase (CK) levels are typically markedly elevated, and muscle pain and myoglobinuria may be present. The severity… — Read on…
View On WordPress
0 notes
Text
I've never heard of "march hemoglobinuria." It's hemoglobinuria due to excessive running.
March hemoglobinuria, occurs when hemoglobin is seen in the urine after repetitive impacts on the body, particularly affecting the feet. The word "march" is in reference to the condition arising in soldiers who have been marching for long periods; the condition was first documented in 1881.
Mechanical hemolytic anemia is a form of hemolytic anemia due to mechanically induced damage to red blood cells. Red blood cells, while flexible, may in some circumstances succumb to physical shear and compression.[1] This may result in hemoglobinuria. The damage is induced through repetitive mechanical motions such as prolonged marching (march hemoglobinuria) and marathon running. Mechanical damage can also be induced through the chronic condition microangiopathic hemolytic anemia or due to prosthetic heart valves.
Intact RBCs on urine microscopy excludes myoglobinuria and hemoglobinuria.
0 notes
Photo


Q. Which Glycogen Storage Disease is due to a defect in glycogen phosphorylase in muscle?
.
.
.
A. The childhood- and adult-onset forms of GSD Type V (McArdle's Disease) are due to mutations in PYGM, the gene for myophosphorylase. As opposed to hepatic GSDs, Type V causes exercise intolerance, muscle cramps, rhabdomyolysis, and myoglobinuria. British physician Brian McArdle (1911-2002) described is in 1951, after he had discovered that scopolamine treats seasickness while doing research in preparation for D-Day.
Pro-Tip: Patients may get a "second wind" if exertion continues for at least 10 minutes, as fatty acids and proteins are broken down for energy.
Image 1 from his obit: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1124015/
Image 2 from Jensflorian on Wikipedia
2 notes
·
View notes
Text
Juniper Publishers- Open Access Journal of Case Studies
A Case Report of Malignant Hyperthermia in a Young Male Veteran Diagnosed with an Early Rise of ETCO2 during Shoulder Arthroscopy
Authored by Sajid Mahmood
Abstract
Malignant hyperthermia (MH) is a chain reaction of symptoms triggered in susceptible individuals by commonly used inhalational agents and also muscle relaxants such as succinylcholine [1]. We describe a case of malignant hyperthermia in a young male diagnosed with earliest rise in ETCO2 concentration. A 37-year-old male underwent right shoulder arthroscopy due to labral tear. Patient was intubated with use of succinylcholine and propofol, general anesthesia was given with sevoflurane. Within 10 minutes of anesthesia, patient developed hypoxemia and ETCO2 started rising, minute ventilation was increased with 100% oxygen, yet ETCO2 raised to maximum level of 80mmHg. Initially, it was thought that patient is suffering from bronchospasm and was treated accordingly. Patient condition did not improve and within an hour he developed signs like hypercarbia, tachypnea, tachycardia, hyperthermia, and laboratory findings of hyperkalemia, rhabdomyolysis were noticed. Sevoflurane was stopped immediately; further management was done with intravenous dantrolene along with D50W, Insulin and nebulized albuterol. Surgical procedure was completed with intravenous propofol. MH expert was consulted over hotline. Patient had complete recovery and was discharged from hospital without any significant sequelae. This case demonstrates significance of monitoring ETCO2 concentration for early identification and management of this life-threatening condition.
Keywords: Malignant hyperthermia; ETCO2; Shoulder arthroscopy; Succinylcholine; Veteran
Abbreviations: ETCO2: End-Tidal Carbon Dioxide; D50W: Dextrose Water 50%; ICU: Intensive Care Unit; MH: Malignant Hyperthermia
Introduction
Malignant hyperthermia (MH) is a chain reaction of symptoms that are triggered in susceptible individuals by commonly used inhalational agents such as halothane, enflurane, isoflurane, sevoflurane and also muscle relaxants such as succinylcholine. The symptoms of MH include a greatly increased body metabolism, high fever and muscle rigidity [1,2]. Following is the case of malignant hyperthermia in a young male diagnosed with earliest rise in ETCO2 concentration.
Clinical Objective
Our case demonstrates the efficacy and significance of monitoring ETCO2 concentration for early identification and management of malignant hyperthermia, a life-threatening condition.
Case Report
A 37-year-old Caucasian male veteran had elective arthroscopy of right shoulder due to labral tear at our health care facility. Patient was induced with propofol and succinylcholine, general anesthesia was maintained with sevoflurane. After few minutes into procedure, oxygen saturation dropped to 69% along with rise in ETCO2; initially bronchospasm was considered, so patient was hyperventilated, nebulized albuterol was administered, saturation improved to 90s. Other concerning clinical issues encountered were development of tachycardia, hyperthermia and rise in ETCO2 despite attempts to increase minute ventilation. Due to presence of these findings diagnosis of malignant hyperthermia was strongly considered. Dantrolene was administered empirically. Sevoflurane was stopped and switched over to propofol infusion. Laboratory findings include hyperkalemia (K=6.7), lactic acidosis (LA=3.9), elevated CPK and myoglobin levels (114,806 & 61,900 respectively) and arterial blood gases consistent with acute hypercarbic respiratory failure. Patient was treated with intravenous 50% dextrose, insulin, β-2agonist nebulization and dantrolene. Patient had adequate clinical response with resolution of tachycardia and improvement in ETCO2 to 30s. Patient also had arterial and foley's catheter placed. Patient was also noticed to have tea colored urine which was thought to be secondary to rhabdomyolysis. Surgical procedure was completed and he was transferred to the ICU for further care. In ICU patient management was done in consultation with expert from malignant hyperthermia hotline. Patient was aggressively hydrated with intravenous normal saline and also received intravenous dantrolene every 6 hours for 48 hours. Patient condition was significantly improved by day third in ICU; dantrolene was discontinued to avoid unnecessary muscle relaxation. Patient was extubated on day third, he complained of pain in left arm which was thought to be secondary to rhabdomyolysis. He was later transferred to medical floor and was discharged from hospital in stable condition.
Discussion
During an acute event of malignant hyperthermia, intracellular calcium increases in skeletal muscle, causing uncontrolled muscle contractions. The ryanodine receptor (RYR1) gene encodes the key channel which mediates calcium release in skeletal muscle during excitation-contraction coupling, and mutations in this gene are considered to account for susceptibility to MH (MHS) in more than 50% of cases [3].The aberrant receptor once triggered by specific agents like in this case by (succinylcholine [4]/ sevoflurane) or other halogenated inhalation agents, allows release of excess calcium into the cytosol of skeletal muscle. This patient had no previous history of allergies but developed symptoms of malignant hyperthermia after receiving sevoflurane and succinylcholine.
In this case, increase in concentration of exhaled carbon dioxide (ETCO2) served as an earliest sign of malignant hyperthermia. Multiple other signs of hypermetabolic activity observed throughout the event included tachycardia, tachypnea, hyperthermia and respiratory acidosis. Hyperthermia is a proportionally late sign and temperature was not spiked high in our case. Lyses of overactive muscle cells turns out in releasing of intracellular potassium and the resultant hyperkalemia can induce fatal cardiac dysrhythmias. Subsequently, the enormous release of cellular contents creates electrolyte disturbances, further increases metabolic acidosis as well as myoglobinuria. It can also lead to significant renal failure [5].
Successful management of the acute MH episode involves early diagnosis with immediate and early administration of dantrolene [6]. In 1975 Harrison et al. [7] first described that dantrolene could be effective in treatment of malignant hyperthermia. The mortality rate from MH was reduced from 80% to 10% following the development of dantrolene [7]. Dantrolene sodium inhibits the release of calcium from the SR by binding to RYR1 and reverses the effects of MH i.e. uncouples depolarization with contraction. Fast contracting twitch muscles are affected more than slow contracting antigravity muscles. In contrast to pronounced effects on skeletal muscle, effects of dantrolene on cardiac muscle contractility are mild or absent [8]. The recommended dose of dantrolene is 2-3mg/kg every 5 minutes, up to a total dose of 10mg/kg if needed [5]. This patient underwent a rapid improvement with the initial dose of dantrolene.
In addition to dantrolene, other immediate interventions include discontinuation of the triggering agents. Hyperthermia should be treated by internal cooling with cold infusion fluids and external surface cooling with ice packs placed in the axillae and groin or specific cooling devices until body temperature reaches 38.5°C [9]. In our case, patient was hyperventilated with 100% O2 to compensate for the increased metabolic oxygen demand. Serial arterial blood gases were drawn to assess and watch metabolic acidosis, electrolyte imbalances, and other markers release during muscle metabolism. To treat hyperkalemia with potassium level of 6.7, EKG changes consistent with hyperkalemia were noted and he was empirically given Insulin and dextrose. Sodium bicarbonate was also given to treat metabolic acidosis. In order to manage malignant hyperthermia, high suspicion to recognize early symptoms is of particular importance. An abrupt rise in end tidal CO2 may occur simultaneously with administration of succinylcholine [10,11]. In this case, anesthesiologist noted early rise in ETCO2 and promptly intervention was done as evidenced by the absence of morbidity and minimal changes in laboratory values. After stabilization and completion of procedure, he was admitted to intensive care unit for 72 hours to monitor any complications as well as possible recrudescence of symptoms. MH hotline was also called to consult MH expert.
Interestingly, there are some reports of fulminant MH-like episodes occurring in the absence of anesthetic agents. MH episodes in the wake state have been described after excessive alcohol consumption, drug abuse, and extreme emotional and physical stress [12-14]. While genetic testing is under development, a muscle biopsy test is the final confirmation of malignant hyperthermia susceptibility [6,15]. For about 30 years, the in vitro contracture test using halothane and caffeine has been the gold standard for determining susceptibility to MH independent of a clinical MH event. Following a surgical muscle biopsy, live muscles specimens are exposed to defined concentrations of halothane or caffeine. If developing contracture forces exceed given thresholds after exposure to halothane and/or caffeine, the patient is diagnosed to be MHS (susceptible). Absence of development of significant contracture following exposure to these agents leads to a diagnosis of MHN (non-susceptible) [16]. Since MH is an autosomal dominant with variable penetrance, testing is also recommended for family members of patients with a positive contracture test. For our patient and MH-positive family members, non-triggering anesthesia should be used for surgeries in future. Even without a positive history of MH, any physician using potent inhalation anesthetics or succinylcholine must be prepared to treat MH. Dantrolene and sterile water for injection must be promptly accessible. Further information can be obtained at the Web site for Malignant Hyperthermia Association of the United States (MHAUS) and by calling their emergency 24 hour hotline at 1-800-644-9737 [17].
Conclusion
Our case draws attention to any physician using potent inhalational anesthetics or succinylcholine; must be prepared to treat MH and risks should always be considered high even in patients without positive history of malignant hyperthermia.Additionally, it also demonstrates the efficacy and significance of monitoring ETCO2 concentration for early identification and management of this life threatening condition. MH emergency hotline contact number should be saved at readily accessible place to make call in timely manner.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#juniper publishers journals#Juniper Publishers Contact#Emergency Medicine#Infectious Diseases#Otolaryngology#Sleep Medicine#Pulmonology
0 notes
Text
Red yeast rice: fashion supplement to lower cholesterol
The statins have become the essential medicine in the prevention and treatment of coronary heart disease. However, about 20% of treated patients develop myalgias or other muscle-type adverse effects. Also, other important side effects are described as hepatotoxicity and peripheral neuropathy among the most important. All of which can lead to discontinuous use of statins with the consequent increase in dyslipidemia and its serious consequences. Fortunately, there are other alternative lipid-lowering supplements such as red rice yeast. As far as red yeast rice is concerned, it has been used worldwide because of an indication based on its ability to lower blood cholesterol. The Red Yeast of Rice It is a product obtained from a yeast (Monascus purpureus) that grows on this cereal. The rice thus fermented has served as an element of the diet for centuries in some Asian countries. Thus, in China, the use of this red yeast is documented for the first time in the Tang dynasty, 800 years before Christ. There is a detailed description of its manufacture in the ancient Chinese pharmacopeia published during the Ming Dynasty (1368 -1644). In this pharmacopeia, red yeast rice is proposed as an aid for digestive problems, circulatory problems and for stomach health. The yeast was sold dissolved in the form of an alcohol or powder beverage. The red yeast of rice has as its active ingredients several compounds called monacolins, a series of substances that inhibit the synthesis of cholesterol. One of them, monacolin K, is in effect a potent inhibitor of HMG-CoA reductase, also known as lovastatin. Active Principles and Application We currently know that red rice yeast contains fourteen active compounds called monacolins, which inhibit the hepatic synthesis of cholesterol. Although numerous studies have suggested that the use of red yeast rice may be effective and safe to lower cholesterol, the fact is that the products present in the market often do not have their monacolin levels standardized, so we always recommend the advice of a professional of orthomolecular supplementation. Thus, in several studies, twelve commercial products based on china red yeast rice powder were evaluated, further investigating the possible presence of citrinin, a mycotoxin that is nephrotoxic for animals. The researchers found great variability in the total content of monacolins (between 0.31 and 11.15 mg per capsule), of monacolin K or lovastatin (between 0.10 and 10.09 mg per capsule) and of monacolin KA (of 0.0 to 2.30 mg per capsule). Four of the products analyzed contained high levels of citrinin. In conclusion, it can be said that there is often great variability in the content of the active principle of the red yeast of rice found in the different products analyzed. Statins and Side Effects It must be remembered that toxic myopathies are a group of very diverse disorders clinically and pathologically. The most important iatrogenic cause is precisely the use of statins and fibrates, which can cause severe necrotizing myopathy, acute rhabdomyolysis, and myoglobinuria. It is known that there are genetic factors predisposing to myopathy produced by statins. Also known are certain forms of necrotizing autoimmune myopathy, which are associated with antibodies to the enzyme 3-hydroxy-3-methyl glutaryl-CoA reductase. Considering this, it should be noted that there are also reports of some myopathies caused by the ingestion of red yeast rice and other toxic fungal species. On the other hand, many patients are forced to stop treatment with statins, due to their side effects, previously cited. These side effects resulting from the treatment with statins could be a direct or indirect consequence of a coenzyme Q10 (CoQ10) deficiency state associated with said treatment. It has been suggested that CoQ10 supplements should be considered during therapy with statins, or other inhibitors of HMG-CoA reductase, such as red yeast rice, to support cellular bioenergetics demands and, in addition, the possibility of an effect should be considered. Precautions in use The possible cytotoxic effects of some compounds present in red yeast of rice such as dehydromonacolinas are being studied. It must be borne in mind that this study already warned about the variability and lack of standardization of products present in the market. Therefore, it is not surprising that we advise prudence in its use and recommendation. Conclusion Under the supervision of a professional, lifestyle modifications that include adequate diet, physical activity and the ingestion of standardized china red yeast rice powder supplements can be considered as adequate systems to promote cardiovascular health, reducing total cholesterol and LDL -cholesterol.

0 notes
Text
Snake poisoning
Snakes snakes and snakes!!!! Difficult but simple Viper:- good for car clearing front Glass if it is Bloody by viper blood((vipe the viper blood) Rememb:- viper do with blood coagul and hypotension (no worries for myo,cns, etc) Elapidae---(cobra/coral)). dangerous do each thing Myo, resp, Cns,cardio, what not what not((((yes not Coagulation💥))) Hydrophiide... Myo cardio, resp toxic Good snake(not touching CNS,Coagulation💥💥 ) 😋😋😋Shock shock shock every snake shock😋😋😋 Simplified from past share DETAILS:-😭 1: VIPERIDAE: (russel viper,pit viper) *most mortalities *local swelling→massive swelling+local necrosis. *systemic in 30 min Hypotnsion shock and haemorrhage due to incoagulable blood. 2:ELAPIDAE.(cobras) *usually no swelling except asian cobra. *very painful bite+local necrosis *vomitting→shock+neurologic symptoms and msl weakness. *respiratory msl paralysis in sever cases *cardiac msl can be involved 3.Hydrophiidae.(sea snakes) *musle involvmnt→myalgia+myoglobinuria→AKI (Cardio and resp paralysis may occur) TREATMENTS 🐍🐍🐍🐍 Short cuts!!🐢 Don't Tx each other case!!!! Then which pt to b Tx?? Pt with snake bit Ptosis,Parapesis,plegia or CNS deficit (It is Cobra) Bleeding, hypotension etc ( it is Viper--viper wipe blood on car front glass😜) Or If Pt is Ok and enjoying Pain but you have to do this important test in each case!!!! 20WBCT(20 min whole blood clotting time) If u take blood in Tube and it didn't clot in 20 min then pt is suffering from Viper bit!!!! Ok Start with ASV(anti snake venom-- 2types 1 types::NIH ibd ASV--- need fridge 2 type: lyophilised ASV-Indian- no need of fridge Good thing:- Tx both type Snakes But Cobra--- need some extra Neostigmine IM and Atrpine IV Repeat each 30 min till Ptosis or paralysis recover Ok ASV--- each pt even children need 8-10 ampule of ASV in first dose!!! Wow Repeat 20WBCT after 6 hr -- if Ok pt can enjoy But if Not ok then Reconsider for ASV-- repeat each 6 hr Why 6 hr??? Bcz liver replete the coagulation factors in 6 hrs (Keep Adrenaline Avil Hydrocortisone in ur pocket for incoming allergic reaction) Ref :- JPA If I m wrong:- correct me ---to read it again 🐍🐍🐍🐍B simple B easy🐍🐍🐍
5 notes
·
View notes
Text
Biomed Grid | Rhabdomyolysis After Cocaine Consumption-Case Report
Introduction
Rhabdomyolysis is a potentially fatal syndrome characterized by degradation of muscular skeletal tissue, followed by the release of intracellular muscle components to the circulatory system. The release of electrolytes, purines and enzymes (such as creatine kinase, lactate dehydrogenase and aldolase) can cause potentially fatal complications such as acute renal failure [1]. The etiology of rhabdomyolysis is multifactorial. Muscle ischemia and cell destruction are the most observed in the patients. Illicit drugs, muscle stress, alcohol abuse, muscle diseases, trauma, defects of hereditary muscle enzymes, seizures and physical inactivity are characterized as major causes in adult populations [2,3]. Despite of the wide spectrum of etiology of rhabdomyolysis, the final pathogenetic pathway is common and is characterized by an increase in free electrolytes in the cytoplasm. Electrolyte changes lead to severe loss of the cell membrane homeostasis, especially by disrupting the pump Na/K ATPase leading to hyponatremia, hypernatremia, hypokalemia, and hypophosphatemia, favoring the occurrence of rhabdomyolysis [4,5]. The diagnosis of rhabdomyolysis is based on symptoms such as muscle pain, weakness, presence or history of red or brown urine (myoglobinuria), elevated levels of creatine kinase fractions MM and MB that are not attributable to heart problems [6,7].
Clinical Report
A 23 years old male soldier was admitted to the emergency department of the Military Hospital–(HMAM), Manaus, Amazonas, in August 2014. The soldier reported symptoms of mental confusion, nausea, rapid heartbeat, sweating, fatigue, anuria and numbness in the lower limbs. He had consumed about 6 grams of cocaine in the last 12 hours. The following clinical laboratory tests were requested: creatine kinase-MM fraction, creatine kinase- MB fraction, lactate dehydrogenase, urea, creatinine, sodium, potassium, magnesium, phosphorus, chlorine, albumin, troponin, myoglobin and electrocardiogram. The soldier was administered with 500 mL of saline (0.9%) while the laboratory tests were being carried out. After approximately 20 minutes of receiving medical care, the soldier fainted. He was immediately transferred to the Intensive Care Unit (ICU), where he remained for next 5 days.
Electrocardiogram was normal.,. After the soldier regained consciousness, the systolic and diastolic blood pressure were 160 and 120mm Hg respectively, with pulse rate of 103/min. Pallor of the skin, mucous membranes and dry tongue were observed. detected Cardiac arrhythmia was detected. After evaluating the results of the laboratory tests [Figure 1 and Table 1], the soldier was prescribed the following medications:
Figure 1: Results of biochemical tests performed on the soldier during the five days of hospitalization in HMAM.
Table 1: Qualitative troponin and myoglobin tests performed on the soldier during the five days of hospitalization.
The treatment was initiated with saline (0.9%) for hydration and mannitol to increase diuresis, which consequently increased the renal blood flow, and decreased the formation of occlusive cylinders [Table 2].
Diazepam 0.5 mg was administered to depress the central nervous system to relieve acute painful musculoskeletal conditions and reduce muscle spasms. Verapamil (5mg/2ml) hydrochloride was administered to reduce blood pressure and improve oxygenation and relaxation of the heart muscle. Metoclopramide (10mg/2ml) was used to reduce nausea and prevent vomiting. Dipyrone (500mg/ml) was administered due to its analgesic, antipyretic and antispasmodic properties.
Table 2: Medications given to the soldier during the five days of hospitalization or his stay at ICU of hospital
Discussion
Cocaine nomenclature refers to cocaine salts, belonging to the alkaloid class, obtained from the leaves of the plant Erythroxylon coca [8]. The salts cocaine hydrochloride and sulfate are the two purest products in the refining process of coca. Cocaine salts are heat-resistant, non-volatile and have a melting point of 190°C. They are popularly known as “dust”, “talc”, “snow”, “flour”, or “cachaça” [9,10]. Cocaine can be used according to its physical properties and purity. Features such as its low point of combustion and high solubility in water shows high absorption rate in mucosal areas by intranasal and intravenous routes and are referred as cocaine salts compared to crack that has high point of combustion and low solubility in water, thus generally used by inhalation [10]. Most of the administration routes absorb cocaine rapidly and it is these routes that determine the speed with which drug will begin its action, its concentration in blood as well as the duration of the euphoric effect. The psychoactive effects initiate faster when administered by intravenous route and inhalation, compared to the oral and intranasal administration. Cocaine salts are highly diffusible in water and are thermolabile, allowing its quick absorption by the nasal mucosa [11,12].
The beginning of psychoactive effects produced by cocaine takes between eight seconds to 30 minutes and it remains effective for five to ninety minutes. The duration of the effect of intravenous and smoked cocaine is lower, which means that the consumer must administer multiple doses to achieve intense state of euphoria. The intravenous injection and inhalation of cocaine produce maximum levels of plasma concentration after three to five and one to three minutes from the time of administration, respectively [11,13]. The half-life of the metabolites lasts between four to six hours, and it is higher than the free cocaine, which is approximately 60 minutes. The concentration found in the blood corresponds faithfully to the amount exposed to the receptors. Blood, urine, and hair tests can be performed to verify the use of cocaine. Urine toxicology testing detects cocaine from 04 to 48 hours after consumption [14-16]. Cocaine use causes necrosis of skeletal muscle cells, releasing cellular constituents in the circulation, which may cause rhabdomyolysis. Laboratory and clinical manifestations show changes ranging from asymptomatic cases or elevations of muscle enzymes without significant clinical consequences, even complicated episodes of severe renal impairment or ventricular arrhythmias due to metabolic and electrolyte alterations [17,18].
Carvalho et al. [17] described that muscle stretching or straining may lead to entrance of sodium into the cell, and secondarily to edema and thereafter death. On the other hand, it gives a calcium influx into the cell due to sodium-calcium exchange, which causes a persistent muscle contraction and consequent energy loss and cell death [17]. Excessive cell edema, especially during reperfusion of traumatized areas, induces large increases in muscle volume of lactate dehydrogenase (LDH) and creatine kinase (CK). The emergence of high levels of myoglobin and myoglobinuria, in conjunction with metabolic acidosis, which arises as a result of release of organic acids of necrotic cells and lactic acid during cell hypoxia, will determine the precipitation of uric acid crystals and myoglobin in renal tubules [19,20]. For the rhabdomyolysis diagnosis, indirect markers of muscle damage are dosed because of their low cost. The levels of creatine kinase (CK), lactate dehydrogenase (LDH), troponin and myoglobin are often used as muscle damage markers since these molecules are cytoplasmic enzymes and they do not have the ability to cross the barrier of sarcoplasmic membrane [21]. Among these enzymes, CK is often described as the best marker of indirect damage of the muscle tissue, especially for late diagnosis of rhabdomyolysis. Besides that, it is necessary to check the presence of hypercalcemia, hyperuricemia and hyperphosphatemia. The main therapeutic goal is to recognize and treat the complications as soon as possible, especially the electrolyte disturbances and acute renal failure [22,23].
Conclusion
The patient on admission presented symptoms of rhabdomyolysis after consumption of large amounts of cocaine. Extremely high levels of CK, CK-MB and LDH were observed in the serum of the patient. The patient was discharged on the fifth day, compared to many cases who died as a result of rhabdomyolysis. Rhabdomyolysis is a multifactorial syndrome, and due to the absence of a specific marker for muscle lysis, sometimes this disease is confused with cardiac disease, making it difficult to diagnose. Many etiologies of acute kidney injury should always be related, an example, vasculitis, nephritis and rhabdomyolysis. We believe, significant data should be given to rhabdomyolysis, considering the cocaine use, especially with the intense physical activities. Due to the great clinical complexity and no known specific and genetic markers, indirect markers of muscle lysis are still in use for diagnosis of rhabdomyolysis.

Read More About this Article: https://biomedgrid.com/fulltext/volume5/rhabdomyolysis-after-cocaine-consumption-case-report.000881.php
For more about: Journals on Biomedical Science :Biomed Grid | Current Issue
#biomedgrid#american journal of biomedical science & research#Health science Journal of Open access#Journal of Health Science
0 notes