#multifactorial problems
Explore tagged Tumblr posts
Text
Super Rant
Apparently, nag-ask daw ng "saklolo" 'yung mga kamag-anak dahil ang lola ay... hindi ako sure anong term ang ginamit, pero nagsisisigaw? Dinala sa amin ng tatay ko, e 'di sa amin naman nagsisisigaw, naghagis ng mga gamit, at iba pa. Sabi ko, kailangan na naming magpa-ER kasi hindi mapapakalma 'yung lola nang walang gamot. Pero wala. Parang walang grasp 'yung mga kamag-anak sa sitwasyon. Hindi raw ba pwedeng resetahan ko na lang tapos uuwi na? Mag-outpatient consult na lang sa ibang araw? At best of all, sabi ng lolo ko, nag-iinarte lang daw.
Nakakainis din talaga 'yung mga kasama sa bahay minsan ng pasyente eh. Laging "okay lang" pag tinanong mo kahit hindi okay! On an unrelated note, naisip ko rin 'yung anak ng kaklase ko dati, may global developmental delay na nga noong pinatingin nya pero nganga ang tatay at pamilya, hindi, normal naman daw 'yung bata. Anong therapy therapy? Malalagas ang buhok mo kakapaliwanag!
Balik sa lola, wala man lang makasagot ng medical history questions, anong mga gamot iniinom nya, may [insert sakit] ba sya? Hindi ko naman alam, kasi hindi ko naman siya kasama sa bahay! Hindi pa pare-parehas mga sagot nila pag tinatanong kung kailan nagsimulang magkagano'n ang lola!
At inis na inis din ako kasi sa hospital X pa dinala. Or pwede raw ba sa hospital Y? Naubos pa oras namin kakapila, wala ngang psych doon! Nagtanong na ako sa mga kaklase ko sa hospital Z (kung saan din ako galing, for the most part) at okay na sana, kaso ang mga kamag-anak e ayaw doon kasi malayo raw? Nakakapikon talaga.
Alam mo 'yung nanlalaban na 'yung pasyente, nanghahampas, nanghihila, hindi makausap nang maayos, tapos after 3 hours finally, nag-order ng "pampakalma" pero oral? At ako raw ang magbigay kasi sa akin daw nakikinig? Gusto ko na talagang manapak kanina.
Inorderan nila ng labs 'yong uncooperative at agitated na pasyente? Ano ineexpect nila? Bahala na 'yung med tech basta makatusok siya?
Tapos syempre, ito ako, nasa work. May choice ba? Papasok din bukas kahit bumabagyo na.
Naisip ko nanaman 'yung ex ko, kaya ako iniwan e, rant ako nang rant, naapektuhan daw siya negatively. Toxic na raw at unhealthy. Dapat good vibes lang.
8 notes
·
View notes
Note
this is probably shaped by my limited frame of reference, but im really fascinated by witnessing the real-time development of adhd as a diagnosis. people attribute so many symptoms to it now or maybe they always did? i was wondering if you have any thoughts on what is the use of adhd specifically as a category within psychiatry. I'm esl so sorry for any confusing wording
no you're right imo; diagnostic categories are always somewhat in flux ofc but ADHD is one that has seen a particularly pronounced shift in the last couple decades. obviously this is multifactorial but my observation goes something along these lines:
'hyperactivity' has been dx'd in children since about the 1950s (also when Ritalin hit the market) but the ADHD dx doesn't really take off until the 90s (also when Adderall, a 2nd-gen reformulation of the 'obesity' drug Obetrol, hit the market). so, it's not all that surprising that 20 years later you see increased patient awareness of the diagnosis, increased popular interest in it, and shifting / expanding ideas of what it means and what ADHD 'is'. it's a relatively young dx.
part of the reason it's young is because it's basically a 'biopsychiatric' dx, meaning it diagnoses certain behaviours as being a 'brain problem' rather than having social causes or context. in practice this is complicated because psychs do use pharmacological approaches in conjunction with psychodynamic ones all the time; nevertheless, the central promise of DSM ADHD and its pharmaceutical treatments has consistently been that the ADHD subject has a physiological, neurological disorder / dysfunction / aberration, and that the drug treatments on the market fix it. that none of this is actually empirically supported is conceptually inconvenient and entrenched by the research process.
the biopsychiatric narrative is worth paying attention to because the context here is one in which it has become commonly accepted that behavioural 'disorders' and affective distress of various kinds can be, basically, either of pure biological origin, or else Your Fault. in the case of childhood hyperactivity, Your Fault historically also included Your Mother's Fault; part of the reason many mothers embraced Ritalin in the 50s and 60s was because the proffered pharmaceutical narrative explicitly challenged the idea that these mothers had done something 'wrong' to result in their (mostly) sons exhibiting disruptive and hyperactive behaviour.
this dichotomy of biology vs personal failing is very overtly present in quite a bit of discourse around ADHD today. if it's my brain being 'wrong' or different, then it's not something I've done wrong but a disease with a simple chemical fix. in this context I don't think it's surprising at all that a lot of popular and patient conceptions of ADHD have seen a considerable widening over the past few decades. often people like to blame this on pharmaceutical companies, and it's true that industry benefits from these discourses and frequently invests in them (eg, via instruments like ADDitude mag). however, that's a pretty simplistic explanation on its own and doesn't really account for the ways in which patients and potential patients also find this diagnostic category personally useful, for reasons ranging from identity-formation to the desire to access prescription amphetamines. ADHD increasingly shows up as a biologised explanation for behaviours ranging from 'eating too many sweets' to 'postural sway' and so on. you can see in such examples how invoking the idea of an aberrant ADHD brain is both reassuring to people who have been made to feel ashamed of certain behaviours, and provides a sense of shared identity and community with others.
all of this is to say: I don't find it surprising at all when I see a relative broadening of notions of ADHD, almost always expressed in biological terms (the 'ADHD brain' operates differently, 'seeks dopamine', causes this or that). ADHD is in some ways a particularly blatant distillation of this general trend in popular psychiatric discourses, for reasons relating to expectations about childhood and child behaviour, and the historical and present relationship between the ADHD label and the regulation of amphetamines. but much of what's happening with ADHD in terms of popular discourses about it can also be seen with many, many other psychiatric diagnoses, to varying extents and in various ways.
my experience writing about ADHD on this website leads me to close by explicitly stating the following: I do not think any ADHD behaviours / symptoms are people's 'fault' or an individual failing; I do not think using drugs for any reason is morally bad or needs to be justified; the fact that I do not think ADHD is a 'brain disease' does not mean I think people are 'making it up' or exaggerating wrt any difficulties they experience personally, professionally, emotionally, &c.
415 notes
·
View notes
Text
As racism within the healthcare system persists, a large new study reveals startling disparities in unscheduled C-sections among Black women.
A National Bureau of Economic Research (NBER) report of nearly 1 million births at 68 hospitals in New Jersey found that Black women are 25% more likely to undergo unnecessary C-sections compared to white women.
While more research is needed to determine whether these disparities are found in other states, the data point to the potential for implicit racial bias occurring in hospital delivery rooms at a provider’s discretion.
“The findings from the new study are alarming — it is concerning that these disparities exist and are so stark,” said Mark Simon, MD, chief medical officer at Ob Hospitalist Group (OBHG).
“The CDC has released dataTrusted Source that clearly highlights national differences in C-section rates across each state, with New Jersey ranking on the high end. But this problem is not unique to New Jersey — disparities in maternal mortality, particularly along racial and socioeconomic lines, are also well-documented,” Simon told Healthline. Simon wasn’t affiliated with the research.
@startorrent02 @meanmisscharles @mettaworldpiece
Takeaway
A concerning new report shows that unnecessary C-sections are 25% more common in Black women compared to white women.
The researchers suggest that implicit racial bias could play a role, and there may be a “financial incentive” to fill operating rooms.
Experts say the reasons for this alarming disparity are multifactorial. More research is needed to determine whether the high number of C-section rates persist in other states.
44 notes
·
View notes
Note
Do you think people immediately jump to conspiracy theories because we're just not used to seeing Lewis struggling with a car/not winning? Or is it more a nature of 2024 social media (or a combo of both).
Thank you so much for calling out the bullshit though, I was starting to feel like the only well-balanced Lewis fan on my dash.
I don't know these things are multifactorial and very complicated. Here are some factors I think may play into it from the top of my head.
Lewis has been pinned the victim since ad21 (imo rightfully) and I think some people are struggling to move past that. Now everything that happens that doesn't go his way is just a confirmation that people have it out for him. It made some level of sense early on (we saw how the sport at large reacted to the idea of his 8th title in dts in particular and many of them didn't make it a secret that they would rather he didn't win it) and now it's becoming harder and harder to find him a bully as we move away from the original event and so it's becoming more and more absurd. It was Masi's fault and then Max's and then George's and then Toto's and then the team's in general and now it's his own mechanics and engineers' or whatever... We're five minutes away from people saying Bono himself is sabotaging him. (Actually nevermind we're already past that he's been accused of not giving him the info he needed that one time George changed startegy or something like that.)
I do also see it as a trend for fans in general to try to make up story lines even when there might not be any. That might be in part due to dts but more generally to the fact that I believe a lot of people are watching F1 like a show rather than like a sport. Like I once said, this isn't Hollywood, stories in real life rarely wrap up definitively and prettily with a bow on top, there's no such thing as redemption arc, and because your fav has been done dirty at some point doesn't mean he's necessarily gonna come out on top afterwards to balance it out. There's no such thing as deserving a win or deserving a good car or deserving a proper farewell. Because it's not a story. It's reality. And reality is messy. But a lot of fans will rather weave a plot together to try to make it make sense to themselves and try to find that happy ending at all cost or try to explain why it's not a happy ending in any possible way that has a narrative rather than accepting that that's life at the end of the day. Which is human to some extent and we all do the same thing with our daily lives btw. It's a normal coping mechanism to put events together into something that resembles a coherent story even when that implies disregarding some parts of said events to make them fit together like we want them to.
I think a lot of Lewis fans (including me) are very frustrated with the way things have gone because it's truly annoying and it makes us more prompt to point fingers and try to make the problem simpler than it is by pinning it on someone or something specific because it's just easier to deal with that way than admit that F1 just like the real life that it is, is fucking complicated and "unfair" (in that no guaranteed happy ending way I described earlier).
And honestly that's fine I too vent my frustration during races and jump on things that make me tick and only afterwards think them through but the fact that Lewis has to make such a post to tell people that no, his team isn't sabotaging him, and that yes, he did relent to their tyre suggestion, shows that's it's been indubitably been taken way too far for everyone's comfort and his own first and foremost. And that's just honestly kinda embarrassing for us all imo.
21 notes
·
View notes
Text
Alright, it's time.
As someone who is pro-"adaptations should differ in some ways from the original material" because that's basically the definition of "adaptation", NFCV is a good example of the limit it has to have. Or, at least, the limits I have.
When one wants to adapt a story from one media to another, sacrifices are bound to be made. Changes are meant to happen. You cannot put, in your adaptation, every single detail the original material had. It would be too long, you need to choose the most important parts of the original media in order to make it shine properly. Wich means some characters will have to be erased, some plots too, all in order for the adaptation to offer a fluent and enjoyable experience for everyone. Even those who already know the original material. Of course, those people will sometimes feel sad about a part or a character they really liked but didn't see in the adaptation... but that doesn't make the adaptation bad.
In my opinion, what makes an adaptation good, is when it respects the core of the original work. It can be many things (and it's multifactorial). The message it wants to pass on, it's universe, it's characters, it's lore... it varies from work to work (you can have work focusing on a main character's story, in this case making an adaptation without this character doesn't make sense. It can be a work telling the stories of a world, in this case, with no main protagonist, an adaptation can change the characters...). You can add many changes to a work you are adapting to a new media (or new audience), but it stops being a faithful or "good" adaptation the moment you erase the core of the original work.
And that's why Netflixvania is not a good adaptation.
Ignoring the questionable writing, the "CHURCH BAD" theme, the overdose of curses and gross dialogues (and so many other nasty writing stuff)... Netflixvania misses the point of the franchise it's adapting entirely. And the few easter eggs here and there are not enough to make up for it.
You can make Alucard bisexual. You can make the Belmont clan a noble family in Trevor's era. You can make Isaac black. Those are details that does not affect the core of the franchise. It might make a few grind their teeth, but that's all. No, the problems go way deeper than that.
Castlevania's core is it's themes. It's lore. Castlevania is the story of a seemingly endless cycle of revenge, tragedy and wars. Of generational trauma, with the Belmonts fated to hunt the night and kill Dracula centuries after centuries with no escape. It's this theme of having to fight evil all the time because it will never truly go away, with or without the Belmont clan. Dracula is not just a vampire king ruling over vampires, he's the Demon King. He's the Dark Lord. He's Chaos personified, with Death as his servant and confidant. He rules over so much more than just vampires (and there is more than two humans who swore their lives to him). And he brought this fate upon himself.
The Belmonts are not just a clan. They are humanity's symbol of hopes, dreams and strenghth. They are total opposites to and complete Dracula. The Belmont-Dracula duality is essential to the Castlevania franchise. They are the pillars of Castlevania.
What themes does NFCV has? Church bad. Humans bad. Christianity dumb. A bit of father-son tragedy.
The only common theme is this father-son tragedy, but it is barely touched (we don't even have the time to fully appreciate Dracula and Alucard's relationship before and after they first fought.) and it became one of the main themes of the cartoon. And it would've been fine... if the adaptation didn't threw out the window what made Castlevania Castlevania in the same breath.
Trevor doesn't have any duality with Dracula here. We barely mention the fact Leon went to Transylvania to hunt Dracula down. We don't feel any deep connection, when in the games, Leon was literally Dracula's friend. They worked together, fought together, they were unstoppable together, and when Mathias turned, he offered Leon eternity by his side. He cared deeply. And Leon decided... no. His own morals, his dead betrothed's wishes, they came first. And so came these lines from Leon:
"You have become a cursed being and I will never forgive you. This whip and my kinsmen will destroy you someday. From this day on, the Belmont Clan will hunt the night."
And this is why Trevor had to be the one to kill Dracula. Alucard still could've had his tragic moment, seeing his father dying by the hands of his friend is really messed up, and it would've make a potential SoTN adaptation where he would have to kill Dracula by himself this time more powerful (we'll get to Nocturne in due time.). But it isn't what happened. Trevor barely participated in the fight. It was a Dracula VS Alucard starring Trevor and Sypha.
Trevor isn't Dracula's friend, but this promise, this curse Leon put on his own family so long ago, it created a kind of bond beetween Dracula and Belmonts that would last for centuries. I talked about them, about how deep it goes, here and here. Dracula created the Belmonts as they are now. The Belmonts created Dracula as he is now, too.
NFCV doesn't care about that. NFCV turned Dracula into a vampire lord not even capabe of keeping his own generals in line. NFCV belittled the Belmont clan's importance (one brief scene where the court (mostly Carmilla) is like "oh, what, a Belmont? one of those vampire hunters? alive? wtf" is not enough). NFCV belittled Trevor himself (a few nice-looking fight scenes is not enough). It belittled the Vampire Killer (the most powerful Castlevania weapon, created with alchemy and infused with the soul of Leon's betrothed. there is so much tragic story potential around this weapon alone). It belittled EVERYTHING it took from the games. And I haven't even touch Isaac and Hector (they deserve their own post), who have been done so, so dirty.
NFCV ignored so many things that gave Castlevania his identity that it just became it's own thing, wich butcher the franchise's name. So many NFCV fans don't know the games even exist, or mix it up with the cartoon when they have little to nothing in common (Lords of Shadow had more in common than NFCV. And it was not insulting to the OG universe). And let's not get started on people praising the show for being "better" and how some character got "improved" when in reality, it's written by people who don't get said characters or games and stop at the surface. Just like they stop at NFCV's surface. That's why they think it's good. (loving a show doesn't mean said show is good, sorry)
I used to think "it's okay if the adaptation is not faithful, as long as it's good/enjoyable". And you know what? This kind of mentality is what lead to NFCV. I no longer stand by it. (maybe I should thank NFCV for making me see my limits)
And that's not because I'm a purist. As I said earlier, I'm all for adaptations making changes. But I am also all for respecting the source material as well ("respecting" just doesn't mean "doing everything exactly the way it was originally" to me, unlike... way too much people). And NFCV is not.
And as a show itself, ignoring the "adaptation" part? It's not that great either. If you get critical and think deeper about things, you'll start to see everything that is wrong. It's easier to ignore the problems and enjoy the parts you do like when you don't know the games. It's almost impossible to do when you do know and love the games. When you need to turn off your brain to truly enjoy a show, it's not the proof of a great writing.
But oh... That is only the first Netflixvania. :) This far, you can actually call it faithful to the games, compared to the soon to air Nocturne. :) (it actually hurts me to say)
You cannot look at the trailer and pretend it's even trying to be Castlevania. It's an original work who stole Castlevania's name and characters. With the first serie, you could've use the first, maybe the second season to pretend it was trying but "oh, the games don't have enough story to adapt" (shitty excuse btw). But here? Oh, no. No no no. It is NOT trying anything.
It happens during the french revolution, it seems it's gonna tackle racism and slavery (I do NOT trust the show to portray the french revolution correctly. nor racism. nor anything). Richter's tragedy is apparently going to revolve around the death of his mother, so you can say bye bye to the whole generational trauma and the weight of centuries of his family hunting Dracula (since it's not where NFCV went to begin with) and protecting the world now being on his shoulder and how it affects his psyche and- I mean DAMN. That is such a DOWNGRADE. But it's only the trailer. We'll have to wait for the whole season to air to see how bad it truly is. But I do not trust them to make Richter, one of the most beloved Castlevania characters, shine the way he deserves. I do not trust them to make Castlevania shine at all. Nothing this far can make a games' fan think of said games (probably because it's not for the games' fans.)
But we know it won't be about Richter anyway. Just like NFCV, it will be about everyone but the Belmont of the show. I mean it's logic, since it's the way NFCV went. At least that's coherent.
And everyone knows the sole reason why they went from ""CV3"" to ""RoB/SotN"" directly is because of Alucard, the true main character of NFCV. The trailer just dropped and you already have people asking where Alucard is.
There is so much details I could rant about. But this isn't about details (nor ranting, really). This isn't about every little thing that only makes the cartoon even more of an insult to the games (even if those details, piling up, ARE important). This is about the bigger picture. This is about Castlevania's heart getting crippled and shat on in favor of a pseudo-mature show getting off to his pseudo-deepness.
Games and shows are different medias and thus, are bound to have different ways to tell their stories. One is not lesser than the other. The Castlevania games have a story. It has a lore. It has themes. It's character have personnalities. But it's not a cartoon. It cannot show it by literally making the characters talking about how deep they are. They can't make cutscenes just to tell "I have a tragic backstory". It has to be shown in more subtle ways. It uses the decors. It uses the way the characters stand, or walk, or attack. It exploits the few cutscenes and dialogues to tell the most important informations. And yes, sometimes, it has to use the manual to give infos about the lore or characters. That is not a lesser way to do so. It's a way to adapt to the games' limits in order to tell their story. (also, CoD literally have two mangas to it's name. make your choice on wich version you like most)
There is so, so much potential in Castlevania. And if you get into the games, if you play them, if you just read the wiki or look at the posts of people talking about the lore, the characters, the games and analyzing them, you'll know... NFCV is a waste of an adaptation.
#castlevania#netflixvania#maybe people say castlevania has no story because lots of it is told in hints#and you have to actually think and make deductions instead of turning your brain off and eating solely what the games gave you#sigh. big. big sigh.
88 notes
·
View notes
Note
It says that Te dom are afraid to be weak. But I've noticed a lot of xxFJ also express that fear. Especially ExFJs, they want to be capable and strong. One of my friend (ENFJ, male) say that they dislike feeling weak and feel shame if they didn't push themselves enough to solve a problem. What could explain that mindset that if FJs don't have Te-Fi? More importantly, is it possible ExFJ mistype themselves as ExTJ for that reason? Bc they see themselves as strong and confrontational?
As far as I can tell, the main problem is that you are oversimplifying. There are two aspects to this problem that often interfere with the type assessment process:
1) The tendency to stereotype and overemphasize superficial characteristics: This is usually a result of not understanding the distinction between cognition and behavior, which is the first major principle covered in the Function Theory Guide.
Two different types can exhibit the same behavior but for different underlying cognitive reasons. For example, there is a common stereotype that portrays ExTJs as leaders/managers due to dominant Te. Yet, in reality, ExFJs are equally likely to gravitate to leadership roles. How are you going to explain this in the absence of Te? Is Te equal to leadership or does Te have a monopoly on leadership? No and no.
"Leadership" is a behavior. A behavior can arise for many possible reasons. Te doms might gravitate to leadership due to a desire for order or control, whereas Fe doms might gravitate to leadership due to a desire to influence and improve group cohesion. The "leadership" behavior may look similar on the surface, but the cognitive reasons/motivations underneath it are vastly different, because Te and Fe are very different functions.
If you don't properly distinguish cognition from behavior, you won't have a deep enough understanding of WHY the behavior exists, and then it's very easy to be led astray by superficial stereotypes during type assessment.
2) Overlooking context and circumstance: This is usually a result of not understanding that human beings are motivated by a multitude of factors, and personality type is only one of them. Most human behavior is multifactorial. Before you try to attribute a behavior to a particular type/function, have you made sure that other external factors/causes have been properly accounted for?
Why is it that, compared to other types, ExTJs are more likely to have this quality of being "afraid to be weak"? It is directly attributable to inferior Fi. However, this doesn't mean there aren't other factors/causes behind it. Another factor that could be at play is general fear of vulnerability, which can afflict anyone of any type. Fear of vulnerability isn't mainly a matter of personality but of negative experiences that hampered ego development, though it might also negatively influence function expression. Most people operate at lower levels of ego development, so fear of vulnerability is a widespread issue, to varying degrees.
In the case of ExFJs, Fe not only encourages one to harmonize with prevailing social norms and customs, it also encourages one to actively maintain and enforce them whenever one observes behaviors that go against the norm. This is one reason why Fe doms can come across as strong-willed, confrontational, even meddling.
However, there can be many other reasons why they come across that way. For instance, ExFJs who have grown up in very harsh or hostile environments might constantly be faulted or shamed for "oversharing", "oversensitivity", or being "overemotional". When healthy dominant function development gets inhibited by powerful environmental factors, it can have a negative impact on how a person expresses all of their functions. People don't only use one function, so Fe isn't the only function to consider.
For example, since environmentally oppressed ExFJs can't really use Fe in a positive way to influence and improve the social environment, they have little choice but to use it in a negative way to conform with the very norms and customs that denigrate their natural Fe strengths. Instead of using Ti in a positive way to encourage healthy boundary setting and reasonable decision making, they have little choice but to use it in a negative way to obsess about "strength", "competence", "independence", or "intelligence", because that is the only means they know of avoiding shame and obtaining validation.
In short, can you tell the difference between natural function expression (positive) and compensatory function behavior (negative)? You won't be able to tell the difference until you understand the complex relationship between personality and environment.
As I wrote in the Function Theory Guide: "To really understand someone, you must contextualize their behavior, by examining all the different forces that might be motivating them." Human psychology is complicated, which means there's always more going on beneath the surface than you realize. If you think type assessment should be a simple process, you're likely to suffer a high error rate.
11 notes
·
View notes
Text
Introduction to FND
Introduction: What is FND?
FND or functional neurological disorder, previously known as conversion disorder and sometimes called functional neurological symptom disorder (FNsD) is a type of somatic symptom disorder is a disorder in which there's a problem with the way the nervous system and how the brain sends and receives signals. There are many risk factors that can cause FND like physical/psychological causes that lead to a wide range of physical, sensory, and cognitive symptoms that have yet to be explained by a recognized neurological disease. FND is multifactorial, therefore has many factors that can contribute to the development of these symptoms. FND was a very misunderstood disorder but the symptoms are very real and have caused many impairments to many peoples lives.
FND symptoms
On the DSM-5, the symptoms of FND are:
Weakness or paralysis
Loss of balance or difficulty walking
Tremors or seizures
Vision problems, such as double vision or blindness
Hearing problems or deafness
Difficulty speaking or inability to speak
Difficulty swallowing
And to be diagnosed, one or more of these symptoms need to be present and have an effect on your body. If you experience any of these symptoms, I recommend you contact a neurologist.
Treatment
There is no medication that can treat FND and neither can it be cured, but cognitive and behavioral therapies can help manage FND. For children, symptoms can be resolved after months and may never return.
Anticonvulsants can help manage symptoms like myoclonus and tonic-clonic seizures.
Misdiagnosis
FND has been commonly mistaken for Epilepsy, Parkinson's disease, MS, and other diseases/disorders
#FND#fnd awareness#functional tics#tics#non epileptic seizures#FNDandMe#epilepsy#functional movement disorder#somatic symptom disorder#functional neurological disorder
31 notes
·
View notes
Text
Is chronic migraine perhaps a form of neurodiversity?
I recently read this paper. It talks about how chronic migraine patients are more like to have alexithymia, problems interpreting social cues, memory and attention issues, and of course classic sensory overstimulation problems. What does that sound like? Sounds a lot like neurodivergence to me.
I have severe chronic vestibular migraine and I’ve been dx’ed with ADHD as a child, and also had therapists suggest autism screening now that I’m an adult. But honestly it just feels impossible to tease out from the migraine. Why do my ND and mental health symptoms get exacerbated with migraines and vice versa? Where does the migraine end and my neurodivergence begin? I think the answer is it doesnt. They are the same. They’ve always been the same.
Western medicine likes to neatly separate mental conditions from physical conditions but it has never worked for me. Chopping me up into body parts and different specialties ignores the fact that all all my conditions are interlinked and the evidence points to them all being part of the same pathway. I think the reason people with nebulous conditions like mine have often been dismissed and underserved by this system is because they think if there is a mental component then it must be “all in their head.” But the mind is the body. The body is the mind.
Anyway this is my suggestion that chronic migraine be entered into the neurodiversity pantheon. Idk people smarter than me probably thought of this already
2 notes
·
View notes
Text
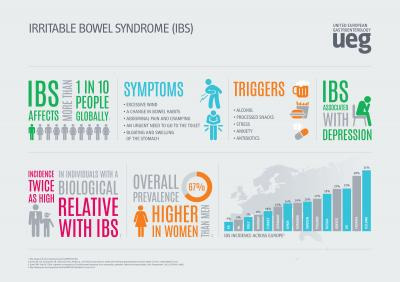
Finding Your Best IBS Treatment Plan
Irritable bowel syndrome (IBS) is a common digestive disorder estimated to affect 10-15% of the entire population. Symptoms like cramping, abdominal pain, bloating, constipation and diarrhea can range from mild to completely debilitating.
While no medical cure exists for IBS, the good news is that many effective IBS treatment options are available to significantly ease symptoms. It simply requires working with your doctor to discover the best personalized treatment plan.
Getting Properly Diagnosed
Since IBS is what’s known as a diagnosis of exclusion, the first step is to rule out the possibility of other inflammatory bowel diseases like Crohn’s or Celiac with specific testing. These may include:
Stool tests check for underlying infections or other gut issues
Blood tests look for markers of inflammation indicating disease
Colonoscopy visually examines the large intestine
Food sensitivity testing reveals if certain foods worsen symptoms
Once other conditions are ruled out, your doctor will make an official IBS diagnosis, the details of which will guide your treatment plan.
IBS Treatment Plans Depend on Type
There are four types of IBS, classified by what digestive symptoms are most prominent:
IBS with Constipation (IBS-C): Hard, infrequent stools IBS with Diarrhea (IBS-D): Frequent loose, watery stools.
IBS with Mixed Bowel Habits (IBS-M): Alternating constipation and diarrhea IBS Unspecified: Insufficient abnormality of stool consistency
Identifying your IBS type allows your doctor to select suitable therapies.
Lifestyle Treatments for IBS Relief
Certain at-home care strategies may significantly control IBS flare-ups including:
IBS Diet - Limiting intake of high FODMAP foods like dairy, beans, wheat, onions, cabbage, and artificial sweeteners can ease stool issues in 75% of IBS patients.
Stress Reduction - Stress dramatically exacerbates IBS problems, so relaxation techniques like meditation, yoga, massage are key.
More Exercise – Moderate activity at least 30 minutes daily calms the nervous system tied to digestive function.
Probiotics - These healthy gut bacteria in supplement form have been shown in studies to reduce bloating and pain.
Peppermint Oil - Shown to reduce spasms and cramping pain. Use enteric-coated capsules.
Prescription IBS Medications
If lifestyle adjustments aren’t providing enough relief, many traditional and newer medications can be very effective, including:
Antispasmodics – Helps relax intestinal muscles to reduce painful cramping and spasms
Antidiarrheals – Slows motility and stool frequency for IBS-D
Laxatives – Helps alleviate constipation with IBS-C
Low-dose Antidepressants – Alters pain signaling pathways between the brain and digestive system
Newer Agents - Prescription medications acting on neurotransmitters recently approved specifically for IBS-C and IBS-D.
Last Resort: FMT for IBS
For patients failing standard IBS treatment, research shows great promise for fecal microbiota transplantation (FMT).
This involves transplanting healthy donor stool containing balanced communities of gut bacteria into the patient’s colon via scope or enema.
Results demonstrating FMT eliminates IBS symptoms in many patients suggests disruptions to the gut microbiome play a key role in IBS development.
Finding Your Optimal Treatment Combination
Since IBS is multifactorial in cause, most experts recommend utilizing a combination approach tailored to your specific symptoms patterns.
This can mean exploring herbal supplements like peppermint capsules or artichoke leaf extract while also prioritizing daily stress-reduction practices and a modified FODMAP diet under the guidance of a registered dietician.
Your doctor may also suggest rotating various categories of medications every few months to achieve lasting relief without building tolerance.
Be patient and keep your physician informed of how you’re responding to each new IBS treatment addition or modification. It often requires tweaking strategies over several months before discovering your unique formula for success.
Hope for Life Without IBS Misery
If you feel like you’ve tried everything for your difficult-to-treat IBS with little success, don’t lose hope. The treatments options area is rapidly evolving!
Whether its emerging micobiome research showing fantastic success with FMT for stubborn IBS cases or newly approved medications targeting specific IBS symptom pathways, effective tools for relief are available.
Stay focused finding the right gastroenterologist who will personalize a therapy plan that finally quiet your symptoms for good. With a thoughtful multi-pronged approach, you can get your life back and start feeling like yourself again!
2 notes
·
View notes
Text
My pathophysiology textbook follows a pretty standard pattern in each chapter. Module 1 is The Topic, module 2 is What Happens When The Topic Gets Fucked Up, then module three is Clinical Models of The Topic. Each clinical model also follows a pattern, where is goes over the pathophysiology of the disease, the clinical manifestations of the disease, the diagnostic process, and treatment.
One of the chapters for this week is altered nutrition, so module 1 talked about macro/micronutrients and how digestion and absorption works, and module 2 talked about undernutrition, malabsorption, allergies, and overnutrition. In the clinical models, along with things like a.norexi.a nervosa, iron deficient a.nemia, and p.henyketonuria, they talked about o.besity. And I thought it was wild how they managed to call o.besity a disease while not giving anything to show how it's a disease.
As expected, they called it a concerning epidemic yada yada, and then in the pathophysiology section they basically explained the mechanisms of fat storage and said that ob.esity is a complex multifactorial condition where genetics influence 1/3, neurohormonal messages and hormones play a major role, and lifestyle factors (they talked about socioeconomic status and environmental factors involved, which was nice ig bc I 100% expected it to be just "these people eat too much"...). Which, yeah, that's how fat storage works and what influences it, but that doesn't tell me anything about how it's a disease. Compare that to anemia, where they talked about how iron is requires for hemoglobin synthesis and electron transport, and how deficiency is more common in people who menstruate (the book confuses female/woman, so they say women, but whatever) because of blood loss, and how a lack of iron directly leads to chronic hypoxia resulting in lack of function of organs like the heart and skin and brain and such. For o.besity, other than "people are fat," they give nothing for how this constitutes a disease.
Then in the clinical manifestations, they say "excess body fat" (wow), and then talk about comorbidities, some of which I know from other class research projects have been shown to have no statistically significant correlation to weight (joint issues). While these may be influenced by being fat, none of these are inherent aspects of being fat the way hypoxia is an inherent aspect of anemia. You can be class 3 o.bese and never have any of these problems. You cannot be clinically anemic and not eventually experience hypoxia (anemia has slow onset symptoms as tissues go longer without adequate oxygen, so you can be diagnosed without symptoms if it gets caught early or isn't clinically significant). That's like saying being female is a disease because there's a correlation between autoimmune conditions and the female sex, thereby making autoimmunity a comorbidity of being female. Like, you can say being female is a risk factor to developing autoimmunity, and you can say being fat is a risk factor to developing these conditions, but it's weird to say it's a disease on its own.
The diagnostic criteria talked about BMI uncritically and talked about diagnosing the comorbidities, which, whatever. We knew they had nothing to say about being fat itself. Then in the frickin treatment section, after having the whole conversation about all the different factors that go into being fat and how complex of a condition it is with multiple etiologies, they talk about drugs that suppress appetite, and diet and exercise as a treatment. (Along with chopping off your frickin stomach and all that fun stuff). Aside from the fact that diet and exercise doesn't result in long-term weight loss and that short term weight loss results in more long -term regain and that weight yoyoing has stronger frickin correlations to all the comorbidities than weight-maintained o.besity does, they literally said that lack of diet and exercise is a small part of weight determination and then said "well if you diet and exercise you'll stop being fat 🤪✌️."
Like, not only did they directly contradict themselves, but they have given me no reason to think o.besity should be considered a disease. The one thing that they could have expanded upon was that adipocytes modulate pro-inflammatory cytokines (they promote inflammation), but they didn't talk about it beyond one sentence, so I don't know how that impacts body systems. Does it trigger inflammation? Are fat people in a perpetual state of immune response? Does it damage nearby tissues? How so? Does it increase the response-ability of the immune system, leading to increased risk of overreaction? Does it increase stress signals like cortisol, leading to the whole cascade of damage that cortisol is known to cause? We'll never fucking know because the only concrete potential evidence of the damage ob.esity might cause was part of one sentence.
#we're probably going to delete this at some point#but it just annoys me#if you're going to argue that a whole fucking body type that has existed for millenia is a disease#you could at least explain what direct paths of damage it causes#disease have direct negative impacts on the body; what are the direct negative impacts of o.besity?#the a.nore.xia section also annoyed me because one of the signs to look for was low body weight#which I feel like shouldn't be a primary thing to look for because fat ppl can also have that disease#and if you brush then off cause they're fat they're not going to get better#or worse if you tell them that theyre doing a good job losing weight as is advocated for in the o.besity section#you're definitely never going to fucking help them
4 notes
·
View notes
Text

Basically, the “divorce” rate of this albatross species (which typically mate for life) has nearly doubled in recent years and scientists suspect that climate change may play a big role in this phenomenon.
As is almost always the case with climate change, the negative effect is largely multifactorial. In regard to the albatrosses climbing breakup rate it’s theorized in part like this; with warming waters, decreased nutrients in the water column have caused a decline in the fish and squid that albatrosses eat. The more time they spend looking for food delays the albatross breeding window, and results in less success in hatching and raising chicks. Losing a chick is a major cause of breakup for these birds, hence the climbing divorce rate as fewer babies survive to adulthood. Even couples that are able to raise a chick together may still split up, potentially due to the high stress hormones caused by pressure to find food.
The problem isn’t exactly the albatross divorce rate itself, more that this odd little data point could signal the beginning of a collapsing food web for the Black-browed albatross and other species in their ecosystem :(
Source

Really bothers me what the climate crisis is doing to albatross marriage
10K notes
·
View notes
Text
Best Obesity Treatment: Options and Insights for Effective Weight Loss
Obesity is a complex health condition that affects millions of individuals worldwide. With its rising prevalence, effective treatment options have become a priority for medical professionals and patients alike. Understanding the best obesity treatment requires exploring a combination of medical, surgical, and lifestyle interventions tailored to individual needs. This comprehensive guide will walk you through the available options and provide insights into choosing the most suitable path for your weight loss journey.

Understanding Obesity: A Multifactorial Condition
Obesity is more than just excess weight; it is a medical condition influenced by various factors such as genetics, lifestyle, environmental influences, and psychological conditions. Characterized by an excessive accumulation of body fat, obesity increases the risk of health issues like diabetes, hypertension, heart disease, and joint problems.
The first step in addressing obesity is recognizing that it requires a multifaceted approach rather than a one-size-fits-all solution.
Non-Surgical Obesity Treatment Options
Non-surgical treatments are often the first line of defense against obesity. They include:
1. Lifestyle Modifications
Dietary Changes: A well-balanced, calorie-controlled diet plays a critical role in weight management. Consulting a registered dietitian can help tailor a plan that fits your lifestyle and nutritional needs.
Exercise Programs: Regular physical activity helps burn calories, improve metabolism, and enhance overall health. Aim for at least 150 minutes of moderate aerobic activity per week, combined with strength training exercises.
2. Behavioral Therapy
Cognitive-behavioral therapy (CBT) can help patients identify and change habits that lead to overeating or unhealthy food choices. It also provides strategies for stress management and improving self-control.
3. Medications
Prescription medications may be used to aid weight loss for individuals with a BMI over 30 or those with obesity-related health conditions. Popular options include:
Orlistat: Reduces fat absorption in the gut.
Liraglutide: Helps suppress appetite and control hunger.
Phentermine-Topiramate: Combines appetite suppression with metabolic enhancement. It is crucial to use these under medical supervision, as they may have side effects.
4. Endoscopic Procedures
Endoscopic treatments, such as the insertion of intragastric balloons, are minimally invasive procedures that reduce stomach capacity, helping patients feel full sooner.
Surgical Obesity Treatment Options
For individuals with severe obesity or those who have not achieved success with non-surgical methods, bariatric surgery offers effective and lasting results. Common procedures include:
1. Gastric Bypass Surgery
This procedure involves creating a small stomach pouch and rerouting the small intestine. It reduces the amount of food the stomach can hold and decreases calorie absorption. Gastric bypass often results in significant, sustained weight loss and improves obesity-related conditions like type 2 diabetes.
2. Sleeve Gastrectomy
In this procedure, approximately 80% of the stomach is removed, leaving a smaller, tube-like stomach. This limits food intake and reduces hunger by lowering ghrelin levels, the hormone responsible for appetite stimulation.
3. Adjustable Gastric Banding
A band is placed around the upper part of the stomach to create a small pouch, restricting food intake. Although less invasive, gastric banding requires frequent adjustments and may result in less dramatic weight loss compared to other bariatric surgeries.
4. Biliopancreatic Diversion with Duodenal Switch (BPD-DS)
This complex surgery involves removing a portion of the stomach and bypassing a significant length of the small intestine. While highly effective for weight loss, BPD-DS carries higher risks and requires careful consideration.
Emerging Trends in Obesity Treatment
The field of obesity treatment is continuously evolving. Some emerging approaches include:
1. Robotic-Assisted Surgery
Robotic systems allow surgeons to perform highly precise bariatric procedures, reducing recovery time and improving outcomes.
2. Non-Invasive Weight Loss Devices
New devices such as vagal nerve stimulators and magnetic implants are being explored as alternatives to surgery. These methods aim to regulate appetite and food intake without invasive procedures.
3. Personalized Medicine
Genetic testing and metabolic profiling are paving the way for customized obesity treatments, ensuring that interventions align with an individual’s unique biological makeup.
Choosing the Right Obesity Treatment
Selecting the best treatment option depends on several factors, including:
Body Mass Index (BMI): A BMI over 40 often indicates the need for surgical intervention.
Obesity-Related Health Issues: Conditions like diabetes or sleep apnea may influence treatment decisions.
Previous Weight Loss Attempts: Failed attempts with non-surgical methods may warrant considering bariatric surgery.
Personal Preferences and Goals: Each individual’s lifestyle and comfort with certain procedures play a crucial role.
Consulting with a specialist, such as the Best Obesity Surgeon in Delhi, can provide personalized guidance. Surgeons like Dr. Tarun Mittal, renowned for his expertise in bariatric procedures at Sir Ganga Ram Hospital, ensure comprehensive care and tailored solutions for long-term success.
Post-Treatment Care: A Key to Success
Regardless of the chosen treatment, maintaining weight loss requires consistent post-treatment care:
Regular Follow-Ups: Keep track of your progress and address any complications.
Nutritional Support: Continue working with a dietitian to meet nutritional needs and avoid deficiencies.
Physical Activity: Incorporate regular exercise into your routine to sustain weight loss and improve overall health.
Emotional Support: Joining support groups or seeking therapy can provide motivation and address emotional challenges.
Conclusion
Effective obesity treatment is a journey that combines medical expertise, lifestyle changes, and unwavering determination. From non-surgical interventions to advanced bariatric surgeries, modern medicine offers a range of solutions tailored to individual needs.
If you're looking for guidance in your weight loss journey, consulting experts like Dr. Tarun Mittal, recognized as one of the Best Obesity Surgeery in Delhi, can help you achieve sustainable results. With the right approach and support, overcoming obesity is not just a possibility—it’s a promise for a healthier, happier future.
0 notes
Text
The Right to be Chronically Unwell
There are people who work hard during their school years to land a nice job and fall into depression when they realize working from your late 10s to your 60s isn’t exactly paradise. But there are people who ever since they were small kids, their eyes and souls opened to the horrors of the world and of the bottom of their own minds, and that is a much worse hell. You can’t even think of the “days when you were young, free and restless”, because there is no such thing as youth when there is constant pain, there is no freedom when your mind is a safety hazard and some unfortunate people are simply already born tired of life. Most people will never be able to conceive living like this, but some will never be able to experience anything different. What is the cause I can’t tell for sure, but I think it’s a multifactorial problem. In these cases, I would like to diagnose them with Chronic Unwellness.
People already have a hard time understanding physical chronic illnesses, so it’s not a surprise they have an even harder time trying to understand what can’t be seen or touched. After all, it’s hard to not believe in a cure, in a higher thing, in a miracle. As humans, most of us are conditioned to this: believe it will all get better. And that’s what they tell you! Go somewhere nice, be in touch with nature, surround yourself with better people… but, the thing is, the people don’t get much nicer and, at first, you will feel better with some sunlight. But, as time passes, you realize it doesn’t change much. You can have everything. You can be “blessed” by nature everyday, waking up with the sunrays caressing your cheek… but it’s still very gray and ready-to-rain inside, so it doesn’t matter in the long run. And, again, the people don’t help at all. The sicker you get, because Chronic Unwellness isn’t just forever, but it also gets worse, you realize that no one will ever reach the level you need. Or, in other words, you won’t reach their level. Despite their constant help, their constant acceptance of your excuses and mistakes, you don’t get better, you don’t stop making mistakes, you don’t speak in a more proper way, you don’t care about the things you should and you care about the ones you shouldn’t. So, no matter who it is, they grow tired and even if they don’t go away, it’s the same as the sun: it just doesn’t matter anymore.
Sure, mundane things such as money and a kind-of-stable life help, but they don't care. And it doesn’t matter what belief you hold onto: deep down, you know you’re miserable and hopeless. And the more miserable and hopeless you become, you realize not even that matters. That’s the difference between a Chronically Unwell person and someone suicidal. You don’t have the positivity of thinking death isn’t the answer, it simply does not matter. Living isn’t seen as this high, beautiful thing, but rather a chore and so is death. To die, there are many steps. The Chronically Unwell being isn’t charmed by self-harm, despite having impulsive tendencies (because, after all, nothing matters) or the call of death itself, it is simply a being so hopeless that not even dying would satisfy its yearning for rest.
Still, if nothing matters, then everything matters. This is why anyone with this disease has such a hard time doing anything. Every little action, every word heard, any simple gesture from anyone around can ignite a fire inside that will burn for a few days, only to die out for another catastrophe to take place. This is impossible to avoid. Of course, the Chronically Unwell can do things to ease the aching, but nothing that would make the discomfort go away completely. It’s like a wound that will never turn into a scar, forever open, no matter which treatment you choose.
You could, surely, always occupy yourself, so you would never even have to think about being unwell. But that’s where it gets you. No matter how much you try to run from it, it is you. It is rooted in you, feeding from the food you swallow, growing bigger from your hesitations and wishes. You might put all the effort in the world to have a fun time with those very good people, but once you step into the restroom stall, you will remember you are unwell. You will dislike something the cashier said, you will feel bothered from an academic criticism you asked for, you will feel like life is worthless because your drink spilled inside the microwave, you will panic over dishes to do, you will want to die because ten hours of sleep still aren’t enough for you to feel rested. But you can’t die, you can’t bring yourself to it… that’s what makes me sure that you are Chronically Unwell.
This is purely informative, so there’s no way I could sell a cure here. When you finally perish, and after many years the last person who remembers you also dies, when all you have written is lost, when the world is finally done with itself, maybe it will feel easier. But while there’s even a bit of you, there is no rest. There is no consolation.
Well, there might be. For those diagnosed today with this heartbreaking disease, there is one simple consolation. It won’t cure you, it might not even make you feel better, but it is the truth. Your wellness isn’t your fault. Now, personally, that would only make me feel worse, but, please keep paying attention. If it was your fault, you would have put a stop to it. If it was your fault, you wouldn’t have it. And that is the most unpleasant thing. You have a lifetime of suffering, complaining, upsetting yourself and others because you were simply born or torn like this.
It won’t get better as time passes, I can assure you. But, slowly, your mind views it differently. Like any other thing you can’t help, you ignore it. It’s not the best, but it’s the sanest option. You can’t love yourself to a cure and you can’t despise yourself to an end, but you can ignore yourself for your own safety. The enemy that lies within can’t be silenced forever, but aside from a few flames every now and then, that can be awakened from the simplest things, it shouldn’t take much more from you than it has already taken before.
That is, of course, for those people who suffer from this. But, right now, I would like to mention the title. “The Right to be Chronically Unwell”. This is, of course, to the good people we surround ourselves with. You simply don’t get it. But you should. The thing is, it can’t be helped, such as a limb that one has lost. You can wear prosthetics, you can get used to not having it, you can have surgery, but you can’t get yours back, and even if you did, you can never have not lost it. It’s quite the same thing. My only wish is you to stop stopping people from feeling like trash. Because they won’t. No matter how much you love them, they are physically, emotionally unable to get better. As I said, the best they can do is ignore their own ascending to madness. So, please, let people feel sad. Let people feel hopeless. They will feel like that regardless and you saying they should try to get better (as if they weren’t trying) or look at the good things in life (as if it made up for what was lost) will only make them feel guilty, which is one of the few, rare things, they are not.
AUTHOR'S NOTE:
Hello. What inspired me to write this was my train of thoughts as I came home from today’s lecture and was cutting homemade pickles. I am living my dream. Not exactly my dream, because dreams are things that happen without effort. I am living the result of my plans, my efforts, my blood, sweat and tears (those last two, quite literally). But, still, I feel really terrible sometimes. I’m just not happy, have never been and probably never will. And I don’t want your pity! Nor your sympathy. I mean, the positive one. The sympathy I want is for you to understand I don’t need to wish to be happy one day. That I don’t need to live up to those standards. That I can just do the bare minimum, that I can feel like scum every three days, because that is my life and I have always felt like that. I don’t believe I will get any better and I don’t want to have high hopes of it. So, please allow me to be a mess. Deeply, I hope this does not resonate with you, but if it does, I’m very sorry. I’m not promising you a brighter future, but rather, that you get used to the rain and don’t upset yourself over being upset.
0 notes
Text
Understanding Common Genetic Disorders: Causes, Symptoms, and Treatments

Genetic abnormalities result from changes or irregularities in an organism’s genome. These abnormalities can stem from mutations in one gene or several genes, as well as variations in the number or composition of chromosomes. Certain genetic disorders are congenital, meaning they are present at birth, while others are acquired as a result of mutations in specific genes. Inherited genetic disorders, like cystic fibrosis, hemophilia, and sickle cell anemia, are passed down from parents. On the other hand, genetic disorders acquired during one’s lifetime are not inherited and can be caused by random mutations or exposure to various factors such as chemicals, environments, or radiation like cigarette smoke or UV rays. Cancer is a prime example of a disease that can be acquired in this manner.
In this blog, we can see some of the common genetic disorders, and its symptoms and treatments.
Down Syndrome
Down Syndrome is caused by an extra copy of chromosome 21 (trisomy 21). This extra genetic material affects development.
The main symptoms are characteristic facial features (flattened face, almond-shaped eyes), intellectual disability, developmental delays, and potential heart defects. There is no cure for Down syndrome, but early intervention, educational programs, and therapies (speech, occupational, physical) can help improve skills. Regular medical care is necessary to manage associated health issues.
Cystic Fibrosis
Caused by mutations in the CFTR gene, which affects the cells that produce mucus, sweat, and digestive juices. The secretions become thick and sticky, causing blockages.
Symptoms are persistent coughing, frequent lung infections, wheezing, difficulty breathing, poor growth, and fatty stools.
Treatments include chest physiotherapy, medications to thin mucus, antibiotics to prevent infections, pancreatic enzyme supplements, and a high-calorie diet. In severe cases, lung transplants may be considered.
Multifactorial Genetic Inheritance
This phenomenon is also referred to as polygenic inheritance. It arises due to a combination of environmental factors and gene mutations. Several disorders exemplify this type of inheritance, including: Heart disease, High blood pressure, Alzheimer’s disease, Obesity, Diabetes, Cancer, and Arthritis.
Sickle Cell Anemia
Caused by a mutation in the HBB gene, leading to the production of abnormal hemoglobin (hemoglobin S). This causes red blood cells to become rigid and sickle-shaped.
Symptoms are anemia, episodes of pain (crises), frequent infections, delayed growth, and vision problems. Treatments are pain management, blood transfusions, hydroxyurea (to reduce the frequency of pain crises), and bone marrow transplants in severe cases. Gene therapy is being researched as a potential cure.
Methods To Test Genetic Disorders
Genetic Counseling: Provides information and support to families at risk of genetic disorders. Helps understand inheritance patterns, testing options, and implications.
Prenatal Testing: Can identify certain genetic disorders before birth. Techniques include amniocentesis, chorionic villus sampling (CVS), and non-invasive prenatal testing (NIPT).
Newborn Screening: Identifies genetic disorders early in life, allowing for prompt treatment. Tests for conditions like PKU and cystic fibrosis are common.
Gene Therapy: Emerging treatment aimed at correcting defective genes. It’s still largely experimental but holds promise for conditions like cystic fibrosis and sickle cell anemia.
Understanding and managing genetic disorders involves a multi-faceted approach that includes medical intervention, supportive therapies, and ongoing research to develop new treatments. Early detection and personalized care are crucial in improving outcomes for individuals with genetic disorders.
0 notes
Text
Havana Syndrome: Part 1

Havana Syndrome. Take a guess: how many Americans have heard of it, or by its new name, Anomalous Health Incidents (AHI)? 33%. A scandal that CBS/60 Minutes has done multiple programs on. 8 years of history, over 1500 victims, Russia and China and Cuba links. Personnel from the State Department, DOD, the Intelligence Community, and the CIA, attacked, sometimes more than once, in over 90 countries. Mysteries, coverups, not-to-be-believed but proven-true injuries, and careers destroyed. Children too. This is the stuff of Tom Clancy. And Netflix. And ongoing pain and suffering and Agencies walking away from the victims. “Treatments” that turn into throwing-in-the-towel, disrespect, accusations, pills, abandonment, lawsuits, deep resentment, and conflicting and even laughable official research, hearings, reports and stonewalling. Some good people are part of the mix, but fewer and fewer. On to the next crisis, hurricane, election, outbreak of violence. Sound familiar? Burn Pits? Gulf War Syndrome? Agent Orange? Toxic water? We’re writing about this because it has direct bearing on brain wounding, ignorant medical practitioners, failure to know the research, sloppiness, laziness, bureaucratic bafflegab, and lack of accountability. First some background and circling back to how this is another example of medicine and politics failing patriotic victims wounded in the line of duty and left to their own devices for coping with an uncertain and degraded future. That is, until some of them starting finding out about Hyperbaric Oxygen Therapy and other alternative therapies that are giving them their lives back. Beginning in 2014, US personnel in the US embassy in Havana Cuba began reporting a mysterious set of debilitating symptoms. Extensive reporting in 2016 reported symptoms beginning with a loud noise, ear pain, intense head pressure or vibration, dizziness, visual problems, and cognitive difficulties. The reports over time and in many other places also included other symptoms: migraines, memory loss and trouble concentrating, ear ringing/tinnitus, dizziness, fatigue, nausea, anxiety, vision problems, balance issues, hearing loss, sleeplessness, and other neurological symptoms. Over the next seven years, as many as 1500-2000 personnel and family members from multiple countries reported similar phenomena and injuries in over 90 countries. Efforts began to describe the neurological manifestations that followed exposure to an unknown energy source associated with auditory and sensory phenomena. Results studying those with reported exposures demonstrated a similar pattern: individuals reported a similar constellation of neurological symptoms resembling brain injury. Over time, some of those individuals were referred to academic brain injury centers and DoD facilities for multidisciplinary evaluation and treatment. And the numbers of subjects continued to grow, along with multiple alleged attacks on the same individuals. In parallel, efforts were begun to discover the source of the injuries. From a diagnostic perspective, of course, the origin or origins of the multitude of symptoms would help in accurate identification of the insults and help in recommendations for treatment. Numerous committees speculated on various possibilities: Directed, pulsed radio frequency (RF) energy; Sonic weapons; Functional neurological disorders/persistent postural-perceptual dizziness (PPPD); Psychogenic or mass psychoses; Chemicals/ neurotoxins; Infectious agents; Vestibular migraines; and Multifactorial. Also mentioned were preexisting conditions, conventional illnesses, and environmental factors. One theory was that buzzing noises reported in several of the Havana incidents were the mating call of a particularly loud cricket, Anurogryllus celerinictus. Contrary and more controversial opinions also varied; official reports were conflicting over time. Investigators found that efforts to understand this syndrome, now renamed “Anomalous Health Incidents” (AHIs), were hampered by politics, overarching national security concerns, the unusual features of the victims' accounts, incomplete information, non-standardized clinical testing, delayed reporting, and the sensitive/classified nature of the circumstances, individuals, and their work. At the end of the day, almost everyone agreed that something debilitating had happened to some of America's finest public servants and service members, their children, as well as foreign diplomats. The alleged incidents occurred overseas and in the US. Starting in 2023, led by the National Foundation for Integrative Medicine and the TreatNOW Coalition, a number of clinicians were contacted by US Government personnel complaining of AHI symptoms. After thorough vetting and analysis of the symptoms, the Coalition determined that the bulk of the growing list of callers had suffered Traumatic Brain Injuries, among their numerous maladies. Hyperbaric Oxygen Therapy, unavailable and uncompensated by the USG, was recommended. Based on objective and subjective symptoms reported in the literature and interviews, HBOT was one obvious choice for treatment. Yet no one who came forward had been offered HBOT; virtually none had ever heard of it as a proven safe and effective treatment for TBI. What was clear, however, was the nearly unanimous reports from the victims that they have been left to their own devices and resources to get sustained help for their conditions. Far too many of the victims have had to quit work or, worse, have been "retired" or let go. The stories of neglect, disrespect, suspicion, endless bureaucratic paperwork lasting years, ghosting, and/or denial of claims have all led to too much gloom and sense of abandonment. They had approached us for help despite legislation intended to provide and pay for that help. Many of them had already spent tens of thousands of their own dollars to seek relief. Even before legislation, certain AHI victims were granted access to DOD facilities like the National Intrepid Center of Excellence (NICoE) where active duty service members with traumatic brain injuries were treated. Initially, personnel were sent to the University of Pennsylvania for diagnosis and treatment. Post traumatic stress disorder (PTSD) was available through a host of VA and other civilian facilities. Yet none of the USG interventions focused on the frequently diagnosed traumatic brain injury. Interventions were focused on symptom palliation. Diagnoses for TBI became increasingly hard to come by. And the AHI victims continue to search for relief. Background on TBI, PTSD, and the use of Hyperbaric Oxygenation for Brain Wounds The use of HBOT for TBI and related symptoms has a decades long scientific legacy. Numerous peer-reviewed clinical trials demonstrate the safety and efficacy of HBOT for TBI. The largely pro bono efforts of TreatNOW and NFIM and over 150 clinics, researchers and practitioners have resulted in over 31,000 successes in over 150 TreatNOW Coalition HBOT clinics across the US. Reported symptoms from AHI echoed decades of history treating TBI and PTSD suffered by combat veterans. The similarities of AHI symptoms to TBI – whether from BLAST, IEDs, falls, training, accidents, or friendly fire – were virtually identical. The label attached to the various complex of symptoms was unimportant; HBOT clinicians treat the patient and reported disease. The symptoms reported by the AHI patients presenting to HBOT specialists bear a strong resemblance to those cataloged by the military health system and the VA. - Flashbacks, or feeling like the event is happening again - Trouble sleeping or nightmares - Feeling alone or detached from others - Losing interest in activities - Having angry outbursts or other extreme reactions - Feeling worried, guilty, or sad - Frightening thoughts - Having trouble concentrating - Having physical pain like headaches or stomach aches - Avoidance of memories, thoughts, or feelings about what closely associated with traumatic events - Problems remembering - Negative beliefs about themselves or others - Irritability - Feeling very vigilant - Startling easily - anxiety, depression, suicidal ideation, and substance use also are seen with people who have PTSD. As a result of the presentations by numerous AHI victims, and the objective, subjective, and diagnostic record, some patients have been successfully treated with Hyperbaric Oxygen Therapy to help in their brain wound healing. Again, as decades of clinical experience and clinical trials demonstrate, helping to heal brain wounds leads in a majority of cases to a diminution or cessation of many symptoms. This is the first of a two part series showing the government, again, a way forward with HBOT in the case of a national emergency/ epidemic. ****************************** The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, get patients off most of their drugs, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma from AHI and Burn Pits. Diabetic Foot Ulcers have become a major emphasis. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#AHI#AnomalousHealthIncidents#braininjuries#Brainwounding#HavanaSyndrome#HBOT#HealingwithHyperbarics#hyperbaricchamber#HyperbaricOxygentherapy#TBI#TraumaticBrainInjuries
0 notes
Text
you ask, I answer! (eventually)
so how does the medical education system select who succeeds and who doesn't?
this is a multifactorial problem, symptomatic of a larger trend in education: in a race towards the same finish line, not everyone gets the same starting line.
there's a number of different ways that minority status creates barriers to education, starting even before preschool. minorities in general tend to be poorer, which is true across race, gender, and disability status. fundamentally, just being poor can be an educational barrier. you can't focus on class if you're hungry because you couldn't afford lunch, and you can't get all your homework done if you have to work long hours after school. regardless of intelligence or academic talent, students in these situations either have to work far, far harder than their peers or end up screwed over on their report card.
beyond that, discrimination is prolific. I don't even need to cite this, professors have told me to drop out of their course or simply denied my accommodations entirely, but I will cite it anyway. for students who are struggling or trying to make a good impression or just don't understand a concept, teachers are supposed to be a resource to help. but would you go to your teacher for extra help with coursework if they've made it clear they think less of you because of your identity?
I can't emphasize enough how severe the problem of educational inequity is. illiteracy is still a problem in the US.
focusing specifically on medical education, exactly when that system begins is difficult to source, but generally speaking students often start to decide in high school, frequently enough that there's multiple guides on it. additionally, some high school students will enter direct med programs, which either combine an undergraduate and medical degree, or assure acceptance into a certain med school under certain terms.
From the very beginning of college, premedical students begin a grind for the best application. Applications tend to go out in the third year, although many students will take gap years or pursue post-bacc education (a way to take more classes without pursuing a degree, often to improve chances of getting into a grad school). The recommendations for a med school application are brutal: a high GPA, often upwards of 3.5 (straight As); 300-500 hours of studying for the MCAT; 200-300 hours of clinical experience; a semester at least of research experience; and 100 hours of volunteering. That's just the start. Beyond that, medical schools often want to see soft qualities like diverse interests and leadership, which usually require extracurriculars.
The cost of this is prohibitive - it's a massive amount of unpaid work for students that are simultaneously putting themselves in an average of roughly 40,000 USD of debt. Plus for the eventual application they're also paying up to 10,000$ in application fees, testing fees, and travel costs. by comparison, PhD programs have largely phased out standardized testing, have application fees of usually less than 100$ each, and reimburse for travel costs (these are very different kinds of programs, but the point still stands).
all of this to then take on another 200,000$, on average, in med school debt.
Students who are poor (which are often minorities) and have received a lacking education are disproportionately affected by this. For students whose parents cannot financially support them, and who have to work through college to eat, the time and financial demands are impossible. For disabled students who have constant medical appointments, high time demands for things like physical or psychiatric therapy, and additional financial strain from medical debt, graduating with an undergraduate degree at all is a struggle, much less applying to med school.
Clinical experience, shadowing, and affording all of this gets a lot easier if you're not the first doctor in your family - accordingly, one in five medical students has a doctor for a parent. from the same source, half of all medical students come from the richest 20% of the population.
so the med school process selects for who can afford it, which is often the wealthy. minorities are less likely to be wealthy, and by extension, less likely to achieve the academic success required for medical school admission. what else?
med school applicants who express any kind of criticism of past doctors or the medical system are rejected almost out of hand. on the one hand, this makes sense, because why accept an applicant who is critical of their dream career? on the other hand, if expressing even the slightest criticism isn't allowed, those who want to change the system from the inside are excluded.
What follows is my opinion, not fact:
as an additional layer, which is perhaps obvious: getting accommodations is difficult in medical school. doctors aren't sparing their coworkers or students from their ableism.
and finally, there's the concept of the ivory tower. more so than high schools, to which attendance is mandatory, colleges often pride themselves on selecting only the very best and brightest to work or study there and exclude the rest. academia becomes insular and invite-only (and this includes medical schools). for many in the academic community, they expect students to meet a certain outdated "standard" to join the ranks of higher education.
I argue that the medical education process, at both the undergraduate and graduate level, teaches students to devalue their health. premedical students are more depressed than other undergraduate students, with minority premedical students being more depressed than white male premedical students (I'll note here that data on premedical students is mixed). also, medical students are more depressed than the average person, and become more depressed over the course of their first semester (this is relatively undisputed).
don't be afraid to ask questions if you've got em.
furthermore, medical students have a high prevalence of musculoskeletal pain compared to the general population. one horrifying study suggests the stress of premedical and medical students is physiologically measurable, although my opinion is that the data is weak. anecdotally, some of the only people to recognize my compression tights on sight are medical students, because they're frequently used to help combat the effects of standing too long.
for students who have passed every barrier, managed to get through every challenge, and contributed massive amounts of time at the expense of their health to become doctors, their perseverance is a point of pride. is it any surprise that a group of people who managed to push through difficulty and pain for academic and socioeconomic success have little empathy for the pain of their patients?
It's not a completely hopeless situation - this is why medical schools have begun to include diversity essay questions, and why minority scholarships exist. the observable trend of educational inequity is the basis for Affirmative Action policies. CME courses (required trainings on current topics in the medical field) on disability identity and discrimination have also become available.
all this to say, the system DOES select for a certain kind of person (wealthier, not a minority, able to say the right things, willing to sacrifice time and health), but I don't think the situation is hopeless.
yes, doctors suck, but also "the medical ethics and patient interaction training doctors receive reinforces ableism" and "the hyper competitive medical school application process roots out the poor, the disabled, and those who would diversify the field" and "anti-establishment sentiment gets applications rejected and promotions requests denied, weeding out the doctors on our side" and "the gruesome nature of the job and the complete lack of mental health support for medical practitioners breeds apathy towards patients" and "insurance companies often define treatment solely on a cost-analysis basis" and "doctors take on such overwhelming student loan debt they have no choice but to pursue high paying jobs at the expense of their morals" are all also true
none of this absolves doctors of the truly horrendous things they say and do to patients, but it's important to acknowledge that rather than every doctor being coincidentally a bad person, there is something specific about this field and career path that gives rise to such high prevalence of ableist attitudes
and I WILL elaborate happily
#i'm not beholden to things like 'grammar rules' and 'capitalization'#apologies for the delay#these take a really long time to make#salt baby talks
22K notes
·
View notes