#lumbar radiculopathy
Explore tagged Tumblr posts
Text
Pinched Nerve in The Spine: Radiculopathy - Symptoms, Causes, and Treatment
The spine consists of several individual bones known as vertebrae. These are interconnected together to form the spine. The spinal cord passes through a central canal in these vertebrae. From the spinal cord, the splitting of nerve roots occurs.
These roots travel between the bones of the spinal and different parts of the body. When the nerve root that leaves the spinal cord to other body parts becomes pinched, irritated, or damaged, it results in a medical condition known as radiculopathy. This condition is also known as a pinched nerve.

Types of Radiculopathy
Depending on where the condition happens in the spine, there are three types of radiculopathy. The symptoms of these types may range from mild to severe in individuals.
Cervical radiculopathy
Occurs due to pressure and compression of the nerve roots in the neck.
This portion of the spinal cord mainly affects the hands, arms, fingers, and shoulders.
Symptoms are usually visible in the hands and arms, which may include weakness or loss of sensation.
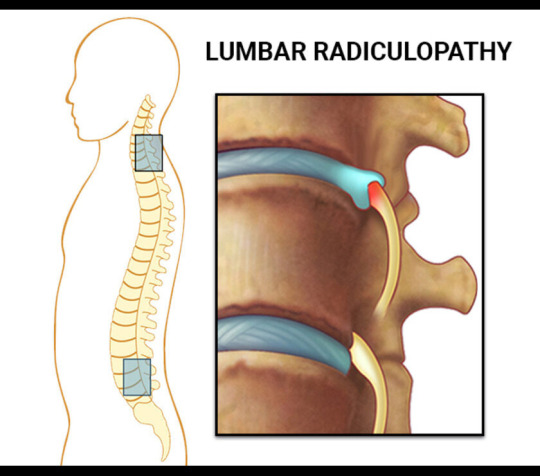
Lumbar radiculopathy
Occurs due to pressure and compression of the nerve roots in the lower back.
It may lead to sciatica, a condition that involves radiating pain in the sciatic nerve.
Thoracic radiculopathy
Occurs due to pressure and compression of the nerve roots in the upper back.
Chest pain is common in this condition.
There is a feeling of numbness and pain that moves to the front of the body in patients.
Causes of Radiculopathy and Risk Factors
Here are some of the commonly known causes of radiculopathy and the risk factors associated with it.
Change in size or shift in position of the tissues that surround the nerve root.
Herniated discs, also known as slip discs, are caused by to rupture of soft pads between spinal bones.
Bone spurs, bony outgrowths or projections resulting in constriction of the spinal passage. a condition in which the spaces within the spine get narrow.
Spondylosis is a wear and tear of the spinal disc with age.
Spondylolisthesis is a condition in which a vertebra slips out of its normal position onto the bone below it.
Spinal stenosis, narrowing of the spinal canal in the lower back.
Sciatica is pain travelling along with the sciatic nerve moving to the back of the thigh into the legs.
Thickening of spinal ligaments.
Spinal infections
Regular improper movements
Cancerous or non-cancerous growth in the spine
Radiculopathy Diagnosis
The diagnosis of radiculopathy begins with the patient giving a brief of their medical history to the doctor.
The doctor will ask questions about the type of symptoms, location of the pain, for how long has the pain been there, and also any other medical conditions which the patient is suffering from.
Once the medical history is known, the physician conducts a physical examination and tests.
This is to check the patient's muscular strength, reflexes, sensation, and also the possibility of any abnormalities.
Physical examination allows the medical practitioner to know the severity of the radiculopathy condition.
It also gives an idea about the location of the nerve root that is affected.
In some cases, radiculopathy diagnosis may require the use of advanced imaging techniques such as CT scan or MRI.
These tests aid in improving the visualization of the area where the problem lies.
In some cases, an expert like Dr Khanna orthopedic surgeon may also conduct a study on nerve conduction or Electromyography (EMG).
These tests help to know whether there is damage to the nerve or the problem is muscular.
Symptoms of Radiculopathy
The pinched nerve roots quickly become inflamed, which may result in the following symptoms:
Shooting pain in the back, legs, arms, and shoulders
Feeling of numbness and tingling sensation in the arms and legs.
Localized neck and back pain
Sharp pain when sitting idle or coughing
Sharp pain with movement
Hypersensitivity
Loss of sensation
Radiating pain in the shoulders
Skin numbness
Muscular weakness
Loss of reflexes
Sciatica
Non-surgical treatment for Radiculopathy
Conservative treatment is usually recommended before surgery. Here are some of the non-surgical treatment options for radiculopathy.
Physical therapy to strengthen the areas of pain.
Limitation or complete elimination of activities that cause radiculopathy pain and stains of the back and neck.
Immobilizing the affected area with
#Spine Care Specialists Indiana#Dr Khanna Orthopedic Surgeon#Orthopedic Spine Surgeon Munster#Minimally Invasive Lumbar Surgery Indiana#Neck Pain Treatment Munster#Best Spine Surgeon Indiana#Back Pain Treatment Munster#Osteoporosis Treatment Munster#Cervical Spondylotic Myelopathy Treatment#SI Joint Dysfunction Treatment#Sacroiliac Joint Dysfunction Treatment#Radiculopathy Treatment Munster#Spinal Stenosis Treatment Indiana#Lumbar Laminectomy Surgery Munster#Spondylolisthesis Treatment Munster#Spinal Cord Injuries Treatment Munster#Orthopedic Spine Specialist Indiana#Orthopedic Doctors in Munster Indiana#Best Orthopedic Doctors in Northwest Indiana#Back Pain Doctor in Northwest Indiana#Spine Treatment Indiana#Orthopedic Surgeon in Munster#Spine Doctors Indianapolis#Spine Surgery Indianapolis#Pain Management Munster Indiana#Cervical Disc Replacement Near Me#Cervical Disk Replacement Surgery#Minimally Invasive Surgery Indiana
2 notes
·
View notes
Text
does anyone have any wheelchair (manual) cushion recommendations? especially ones beneficial for someone who has trunk weakness, lumbar degenerative disc disease, sciatica, and stuff like that which tends to make sitting uncomfortable
for more context: my current wheelchair cushion setup triggers low back pain (maybe near tailbone specifically) and discomfort in my legs due to sciatica or other radiculopathy, but this didn't happen to the same extent while using a rental chair at an amusement park
unless it's my seat depth or something that's actually the problem instead of my cheap cushion :(
8 notes
·
View notes
Text
hey uh, does anyone else (or someone you know) have lumbar radiculopathy w/nerve damage? not caused by disc issues, tumors, acute injury, or low conus medullara? or literally anything observable on a regular no contrast lumbosacral MRI or xray? if so, and you found the cause, what was it & how was it diagnosed? for reference i have a genetic hypermobile condition.
its been years. im just at a total loss and don't know what to do anymore. the only thing i can think of that may be causing it is nr-axspa, but idk how to get a doctor to look into it. if ppl could reblog to boost, that'd be great ♡
#softspoonie#chronic pain#chronic illness#heds#ehlers danlos syndrome#radiculopathy#hypermobile eds#hypermobile ehlers danlos#hypermobile spectrum disorder#hypermobility#spoonie#disabled#disability#disabled community#actually chronically ill#chronically ill#neisvoid
17 notes
·
View notes
Text
Chiropractic Solutions for Pinched Nerves
If https://www.zahnchiropractic.com you're dealing with a pinched nerve, chiropractic care offers effective solutions through targeted spinal adjustments and personalized treatment plans. You'll typically experience symptoms like pain, tingling, numbness, or weakness along the affected nerve's path. Chiropractors use various techniques, including manual adjustments and therapeutic exercises, to relieve pressure on the nerve and restore proper function. Most patients see improvement within 6-8 weeks of treatment, combined with lifestyle changes like better posture and ergonomic adjustments. While immediate relief is possible, understanding the full scope of treatment options can help you make informed decisions about your care.
Understanding Pinched Nerves
A pinched nerve occurs when surrounding tissues, such as bones, muscles, cartilage, or tendons, apply excessive pressure to a nerve. This pressure disrupts the nerve's normal function, leading to pain, tingling, numbness, and weakness in the affected area. You'll often experience these symptoms radiating along the nerve's path, which can extend from your neck down to your fingers or from your lower back through your legs.
Common locations for pinched nerves include your neck (cervical radiculopathy), lower back (lumbar radiculopathy), and wrist (carpal tunnel syndrome). Several factors can contribute to nerve compression, including poor posture, repetitive movements, obesity, pregnancy, and sports injuries. If you have diabetes or arthritis, you're at higher risk of developing this condition.
You might notice that your symptoms worsen during certain activities or positions. For instance, neck-related pinched nerves often flare up when you're looking down at your phone or computer. The good news is that most pinched nerves respond well to conservative treatment, and you can prevent future occurrences by maintaining good posture and a healthy weight.
Common Causes and Risk Factors
You can develop a pinched nerve through physical strain or injury, including poor posture, repetitive motions, and sudden trauma from accidents or sports-related activities. Your lifestyle choices, such as maintaining an unhealthy weight, smoking, or having a sedentary routine, can increase your risk of nerve compression. Having certain health conditions like diabetes, arthritis, or thyroid disorders can also make you more susceptible to pinched nerves.
youtube
Physical Strain and Injury
Physical strain's impact on nerve health often stems from everyday activities and sudden movements that compress or irritate nerve pathways. When you're lifting heavy objects incorrectly, maintaining poor posture at your desk, or sleeping in awkward positions, you're putting unnecessary pressure on your nerves. These actions can lead to inflammation and swelling around nerve roots, particularly in your spine and neck areas.
Sports injuries and repetitive motions can also trigger nerve compression. If you're an athlete or someone who performs the same physical tasks repeatedly, you're at higher risk of developing pinched ne
2 notes
·
View notes
Text
update- TWs in tags
Thank you all very much for your replies to my last post. I’ve had zero energy this past week and yesterday was a very hard day. Got my decision in the mail and wow, they sure are long. It’s not good, folks!!! Not good at all. This guy is an SSA shill and I’m flabbergasted. Hopefully my attorney gets back to me next week asap because not only do I have grounds for an appeal, I believe I’ve been denied my rights by law. Some highlights from his decision. They’re very painful to read and my case manager way back in November of 2021 said that they love to tell people they’re disabled but here’s why you can work. Basically what this dude did but I’m seriously confused and angry. I think it also speaks to the type of person and biases he has. -I meet the disability insurance thing, as in he considers my record to start back in October 2015, which is how my attorney laid it out. And it’s true because that’s the last time I was able to work. -I am severely limited and cannot perform the work I once did. The work I once did was, uh, retail/customer service, and a ‘stay at home’ job if you will by being a caregiver to a veteran (my ex). -My disabilities as the SSA listed them: chiari malformation, leukemia, major depressive disorder recurrent, severe, PTSD w/dissociative affects, headache, s1 radiculopathy (nerve damage), and idiopathic intracranial hypertension (IIH, my number one enemy) -Chiari and leukemia aren’t considered disabilities, which I knew they wouldn’t be. I’m in remission and people often work with debilitating cancers even tho they should absolutely not have to. Let’s begin with what he got wrong lol -He dates that I got an EMG done in March of 2022 before the lumbar puncture. I did not get an EMG until September of 2022. The LP was in April of 2022. -Nerve damage. I have zero evidence of nerve damage in my medical record, according to him. Zero. I do not have a single symptom to suggest nerve damage and I need at least one from both ‘categories’ the SSA lists. But I have none. I was bedbound for eight months because of nerve damage. I had noted swelling (with pictures) of my paraspinal muscles which might have contributed. I had an EMG because of nerve pain. My dr ordered an EMG because of nerve pain. Shooting pain down my leg and numbness/tingling. Also the severe pain in my lower back causing me to not be able to sit up or walk without excruciating pain 💀 I was referred by my neuro to a pain specialist who really wanted to do steroid shots in my lumbar region FOR NERVE PAIN. I was in physical therapy for months to relearn how to like walk and sit up but also for NERVE PAIN. Legit have no words. It’s noted in my neuro’s and his PA’s file about the radiculopathy explaining what happened to me finally. Hhhhhh. -MDD/PTSD/suicidal ideation. I have extensive medical records going back to 2015--NPs, therapists, my psychiatrist, and the neuro psych eval I had in Sept of 2021 + more since. The eval is one of my most important medical documents. He said the medical evidence did not support major depression/anxiety/PTSD for 2+ years with no improvement, which is not factual. My medical records from my NP in 2015-2017 show how many medications I was on that did not work. How long I was in therapy because it did not work. My current psychiatrist is on my side and tells me every time I see him that I’ve been on everything and we’re limited lol I believe this summer I will be with him for two years alone. The judge notes I have no medical evidence of panic attacks despite them being listed in my medical record. At most of these places. Again. Plus the ER at the very beginning discuss panic attacks. This man read my neuro psych eval where she diagnosed me with those MH disorders (beyond already being diagnosed elsewhere). This is an intimately personal document because it details a SA that occurred in 2012 plus the abuse my ex put me through for 2yrs, which made me unable to work starting in 2015. She noted high concern for my well being as my suicidal ideation is, uh, high lmao and the effects of PTSD from multiple traumatic things. He said there is no evidence in my medical record beyond a depressive and anxious mood which do not fit the bill for MH disabilities. He completely ignored the neuro psych eval (and everything else) so I think that speaks volumes of the type of person he is. -IIH. This is where I get very angry. He lists it as something I was diagnosed with and it was in consideration, yet he completely fails to consider it. He considered ‘headaches’. Not IIH, not multi-feature chronic migraines that are well documented, not the recommended brain shunt by my neurosurgeon if pressure was high, which it was. He is, by SSA law, supposed to argue for/against the conditions listed. He didn’t. -Allegations. He says that the “allegations” I have made don’t completely match my medical records by, like, existing or severity. Except the things that he says I alleged but are not supported are because of IIH. Which he had plenty of medical evidence of + the burden of deciding I meet criteria for disability is on the SSA at this point. He has to by law complete my medical record himself once it goes to him (almost a year ago) so he has the entire picture to make an accurate and fair judgment. He says I allege symptoms not endorsed by medical record but they are symptoms of IIH lmao -He implies I lied (”allegations”). He said that in my records it has been noted I stopped driving once all this happened (dec 2019) and have not driven since. It is noted *everywhere*. But he says that I indicated I drove one (1) time in December 2021. Obviously, this is not true and I have no idea where he got this from. My mom was pissed because she has driven me everywhere for 3+ yrs lmao I have a feeling someone misheard me say dec 2019 for dec 2021, so the judge thinks this makes me a liar. He completely ignored the vocational expert’s testimony in the opposite way I have read happens--narrowing me down to 1 job, then 0, but deciding himself I could perform jobs like ‘mail clerk, router, or marker’ whatever the fuck those last two are. A dr who reviewed my case (I didn’t even know they did lkafaja) said I could only have occasional interactions with people. The judge said that he felt that was not true and increased it to frequent. I don’t trust people. At all. I never want to make friends irl again because it feels way too fucking vulnerable. This is in my medical records. Anyway. I truly believe I have grounds for an appeal b/c of mistakes he made and I hope my attorney agrees with that. The judge is not supposed to fuck up dates or ignore medical evidence entirely in his judgment. BY LAW. Angry, hurt, tired. Why does this keep happening to me lol why can one thing not go right but instead everything always gets worse. I feel like I try to put good out into the world when I can but it spits on me in return. I want to give up.
#vtforpedro personal#vtforpedro medical#mentioned abuse and SA noted by a medical record#mental health stuff re disability decision#does anyone know disability law lol#in the great us of a#i'm so tired
13 notes
·
View notes
Text
Image ID:
List of Viktor’s Ailments which reads as follows— “Chronic sleep deprivation, chronic obstructive pulmonary disease, degenerative disc disease, peripheral neuropathy, chronic lumbar radiculopathy, hemoptysis, major plot point-itis, incurable cough of death, one leg in grave disorder, severe hypovitaminosis D, persistent dysthymia, pulmonary fibrosis, cluster headaches, insomnia, chronic migraines, generalized anxiety disorder, anemia, osteomyelitis, hypertension, hepatotoxicity, osteoarthritis, osteoporosis, fibromyalgia, chronic fatigue syndrome, circadian rhythm disruption disorder, thoracic kyphosis, post-polio can’t catch a breath and don’t deserve to syndrome, consumption, latent claustrophobic tendencies, chronic systemic inflammation, recurring cough of doom, contact dermatitis, eczema, lung scarring, micro-fractures in metacarpals, mild vestibular hypo-function, muscular dystrophy, synaptic desensitization to dopamine reinforcement, residual muscular hypertonia, metatarsalgia, chronic cluster headaches triggered by workplace stress, I’m only alive out of spite disorder, intermittent cranial hyperesthesia, episodic executive disfunction, systemic inflammation, latent self-destructive perfectionist tendencies, chronically elevated epinephrine levels, idiopathic trust deficiency disorder, acute inferior partner irritation syndrome, terminal snark syndrome”
End ID

My princess with a disorder🥹
Also heres the full list of maladies by popular request

22K notes
·
View notes
Text
Top Lumbar Radiculopathy Treatment in Orlando – Sciatica Relief & Expert Care

Looking for lumbar radiculopathy treatment in Orlando? Innovative Pain Solutions offers expert care for sciatica and lower back pain caused by nerve compression. Non-invasive treatments like medication and physical therapy help relieve pain. Book your consultation today for effective solutions!
To Know More Visit: https://www.orlandopainsolutions.com/lumbar-radiculopathy/
0 notes
Text
Mechanisms of nerve injury – The major mechanisms of upper extremity peripheral nerve injury are compression, transection, ischemia, inflammation, neuronal degeneration, and radiation exposure. (See 'Etiologies' above.)
●Diagnostic testing
•Electromyography and nerve conduction studies are useful for identifying and classifying peripheral nerve disorders affecting the upper extremity. (See 'Overview of diagnostic testing' above.)
•Magnetic resonance imaging of the cervical spine is useful to identify disc herniation or degeneration and the degree of nerve root compression as well as to exclude the possibility of a mass lesion. (See 'Imaging' above.)
•Neuromuscular ultrasound can be helpful in assessing individual peripheral nerves in patients who present with an unusual upper extremity mononeuropathy.
•Laboratory testing and cerebrospinal fluid analysis are generally reserved for patients with conditions associated with an inflammatory, infectious, or endocrine source. (See 'Laboratory testing' above and 'Lumbar puncture' above.)
●Median neuropathies
•Carpal tunnel syndrome is the most common upper extremity mononeuropathy. Typical symptoms include pain or paresthesia in a distribution that includes the median nerve territory, with involvement of the lateral portion of the hand (figure 4). The symptoms are typically worse at night and characteristically awaken affected individuals from sleep. (See 'Carpal tunnel syndrome' above.)
•Less common median nerve syndromes include entrapment where the median nerve passes through the pronator teres muscle and injury to the anterior interosseous nerve that branches at the elbow. (See 'Pronator teres syndrome' above and 'Anterior interosseous neuropathy' above.)
●Ulnar neuropathy – Ulnar neuropathy at the elbow (figure 6) is the second most common compression neuropathy affecting the upper extremities. Symptoms include sensory loss and paresthesias over digits 4 and 5 (figure 7) and weakness of the interosseous muscles of the hand in severe cases. (See 'Ulnar nerve syndromes' above.)
●Radial nerve syndromes – With compression of the radial nerve at the spiral groove, the triceps retains full strength, but there is weakness of the wrist extensors (ie, wrist drop), finger extensors, and brachioradialis (figure 9). Sensory loss is present over the dorsum of the hand and may extend up the posterior forearm. With posterior interosseous neuropathy, forearm pain and weakness of finger dorsiflexion is typical. (See 'Radial nerve syndromes' above.)
●Proximal neuropathies – Several uncommon proximal focal neuropathies of the upper extremity typically present with pain and sensorimotor impairment. These include suprascapular neuropathy, long thoracic neuropathy, axillary neuropathy, spinal accessory neuropathy, and musculocutaneous neuropathy. (See 'Proximal neuropathies' above.)
●Brachial plexopathy – The brachial plexus (figure 1) is vulnerable to trauma and may be affected secondarily by disorders involving adjacent structures. Most brachial plexus disorders show a regional involvement rather than involvement of the entire brachial plexus. (See 'Brachial plexopathy' above.)
●Cervical radiculopathy – Cervical radiculopathy is a common cause of both acute and chronic neck pain. Most radiculopathies arise from nerve root compression due to cervical spondylosis and/or disc herniation. Lower cervical roots, particularly C7, are more frequently affected by compression. Typical clinical findings of solitary root lesions are summarized in the table (table 1). (See 'Cervical radiculopathy' above.)
●Other syndromes – Additional uncommon peripheral nerve syndromes affecting the upper extremities include focal amyotrophy, mononeuropathy multiplex, multifocal motor neuropathy (MMN), and zoster radiculoganglionitis. (See 'Miscellaneous' above.)
1 note
·
View note
Text

PACE Hospitals is one of the Best Spine Surgery Hospital in Hyderabad, India; providing comprehensive and evidence-based spinal cord injury treatment. The team of spine surgeon and orthopedic spine surgeon have vast experience in the latest minimally invasive techniques, laser spine surgery, and motion-preserving procedures to treat a wide spectrum of congenital, pediatric and geriatrics spinal cord injuries and abnormalities, including:
Herniated Disc (Slipped Disc)
Degenerative Disc Disease (DDD)
Spondylosis (Cervical, Lumbar, or Thoracic)
Spinal Stenosis, Sciatica (Lumbar Radiculopathy)
Myelopathy (Cervical or Thoracic)
Spinal Fractures (Vertebral Fractures)
Scoliosis, Kyphosis, Chiari Malformation
Lordosis (Hyperlordosis), Ankylosing Spondylitis
Spinal Osteomyelitis, Spinal Epidural Abscess
Tuberculosis of the Spine (Pott's Disease)
Spinal Cord Tumors, Vertebral Hemangioma
Metastatic Spinal Cancer
0 notes
Text
Top Signs You Need to See a Spine Doctor in Ahmedabad

For those people who want to maintain their Spine, this blog is most important for them. The Spine not only supports body structure but he protects the Spinal Code which plays an essential role in transmitting signals between the brain and the rest of the body. However, many people overlook signs of spine-related issues until they become severe. Addressing these problems early by consulting a spine doctor in Ahmedabad can prevent complications and ensure effective treatment.
In this blog, We will suggest some tips and signs with the help you can easily identify the key signs that indicate it’s time to see a spine specialist, the conditions they treat, and the benefits of seeking timely care from experts like Dr. Vinod Gautam, a leading Spine Care Doctor In Ahmedabad.
What Does a Spine Doctor Do?
These types of Spine Doctors diagnose and treat different kinds of Spine Situations from Complex spinal disorders to Minor Back Pain. These Spine Specialist are highly trained for handling different Spinal Conditions whehter it is from nerve compression, degenerative diseases, or injuries.
In Ahmedabad, spine doctors like Dr. Vinod Gautam provide personalized care tailored to the patient’s specific needs.Whether it involves physical therapy, medications, or surgical interventions, their main goal is to restore functionality and improve the patient’s overall quality of life.
Top Signs You Need to See a Spine Doctor
Persistent Back Pain
Back pain is one of the most common complaints worldwide, but persistent or chronic pain should not be ignored. If you experience back pain that lasts longer than a few weeks, or if it worsens during specific activities or while resting, it may indicate an underlying spine issue. Some Conditions that Play the Most Important Role in the Chronic Pain that involves herniated discs, spinal stenosis, or degenerative diseases.
Consulting a Spine Doctor in Ahmedabad can help identify the root cause of your pain and provide appropriate treatment. So, Ignoring Some symptoms can lead to worsening discomfort and potentially irreversible damage.
Radiating Pain
A common Spine pain passes from the arms or legs and is a common symptom of nerve involvement. For instance, sciatica—pain that travels down the leg—is often caused by compression of the sciatic nerve. Such pain can significantly impact mobility and routine activities.
Using advanced techniques such as MRI or CT scans, A spine specialist can easily identify these symptoms and recommend treatments such as nerve blocks, physical therapy, or surgery to relieve the pressure on the affected nerves.
Numbness or Tingling
Experiencing numbness, tingling, or a “pins and needles” sensation in your hands, feet, or other extremities may indicate nerve compression or damage. Sometimes nerves are pinched due to structural changes in the spine, These sensations often accompany conditions like herniated discs or spinal stenosis.
Early intervention by a Spine Disorder Specialist Doctor In Ahmedabad can prevent the progression of these symptoms and reduce the risk of permanent nerve damage. Treatments start from non-invasive therapies to surgical decompression, Based on the severity of the condition.
Limited Mobility
Difficulty in bending, twisting, or performing everyday activities can signal a spine problem. Stiffness or reduced range of motion in the back or neck often results from conditions like arthritis or spinal deformities.
Seeking timely consultation with a specialist like Dr. Vinod Gautam ensures proper evaluation and treatment to restore mobility. Physical therapy, medication, or minimally invasive procedures may be recommended based on individual needs.
Weakness in Limbs
Weakness in the arms or legs can be a serious indicator of you with the help you can easily identify nerve or spinal cord involvement. Some Spine Situations such as cervical myelopathy or lumbar radiculopathy can cause a loss of strength and affecting your ability to perform basic tasks like walking or gripping objects.
Look at a Spine Doctor, Who has years of experience in diagnosing and addressing these issues. Timely treatment with a spine specialist can easily prevent worsening and boost strength and coordination.
Common Conditions Treated by Spine Doctors
A Spine Doctor can easily handle various range of spine condition that involves herniated discs, degenerative disc disease, scoliosis, spinal tumors, and infections.Various spine condition whether it is complete or normal, requires a tailored approach to ensure optimal outcomes.
For example, degenerative disc disease may be managed conservatively with lifestyle changes and therapy, while more complex conditions like scoliosis might necessitate surgical intervention. DR Vinod Gautam has 16+ years of extensive experience in the spine, and ensures patients receive the most effective and advanced care available.
When to Seek Emergency Care
Certain spine-related symptoms require immediate medical attention. Severe pain accompanied by loss of bladder or bowel control, sudden weakness, or unexplained weight loss can indicate spinal cord compression or other critical conditions.
When Patients Are Delaying treatment in such cases can lead to irreversible damage. Emergency consultation with a Spine Care Specialist Doctor In Ahmedabad ensures timely diagnosis and intervention, potentially preventing long-term complications.
Benefits of Consulting a Spine Doctor in Ahmedabad
Choosing to consult a spine specialist in Ahmedabad offers numerous advantages. Patients can easily access advanced diagnostic tools, minimally invasive techniques, and personalized care plans in any kind of Spine Situation whether it is from Critical to Normal Spine Conditions.
Additionally, experienced professionals like Dr. Vinod Gautam provide comprehensive care, ensuring a smooth recovery journey. From initial consultation to post-treatment rehabilitation, their expertise guarantees optimal results.
Why Choose Dr. Vinod Gautam for Spine Care in Ahmedabad?
DR Gautam is a noted Spine Doctor In Ahmedabad, With 18+ years of deep understanding of treating various types of complex spine situations, ensuring personalized care, and achieving successful outcomes for over 2,000 patients.
The patient Receives a benefit from his holistic approaches, he always focuses on achieving long-term relief and improved quality of life. His Spine Clinic is equipped with top-quality advanced technology and advanced treatment options. Also, He always gives first priority to a patient-centric environment making it a trusted destination for spine care in Ahmedabad.
Conclusion
Ignoring spine-related symptoms can lead to serious health complications. Recognizing the signs and seeking timely care from an expert like Dr. Vinod Gautam can prevent the advancement of spine conditions and improve overall well-being.
If you’re experiencing any of the symptoms mentioned above, don’t delay. Book a consultation with Dr. Vinod Gautam, the trusted Spine Specialist Doctor In Ahmedabad, and take the first step toward better spine health today.
#SpineDoctorAhmedabad#SpineHealthTips#DrVinodGautam#SpineAndOrthopedicCenter#AhmedabadSpecialist#BackPainTreatment#SeeASpineDoctor#OrthopedicHealth#HealthySpine
0 notes
Video
youtube
Major Exercises of Sciatica / Lumbar Radiculopathy / Back Pain – Special...
1 note
·
View note
Text
Lumbar Radiculopathy Manhattan, NY
Lumbar Radiculopathy is a condition in which patients experience pain and inflammation due to the compression of a spinal nerve root, along the lower back or lumbar spine. This pain will often radiate down the sciatic nerve, running down one or both legs from the lower back - often called SCIATICA. Lumbar Radiculopathy can manifest itself in a variety of different ways.
0 notes
Text
Common Symptoms of Lower Back Pain: When to Seek Treatment in Jaipur
Lower back pain is a widespread issue that can range from mild discomfort to severe, chronic pain. Recognizing the symptoms early on is essential for effective treatment and preventing further complications. At Aarav Spine & Bone Common Symptoms of Lower Back Pain: When to Seek Treatment in Vaishali Nagar, Jaipur, we are dedicated to providing expert care for lower back pain, helping our patients regain mobility and live pain-free lives. Below are some common symptoms that indicate you may need lower back pain treatment.

Common Symptoms of Lower Back Pain
1 . Persistent Dull Ache
Description: A continuous, dull pain in the lower back that doesn’t subside with rest. This ache may be present for weeks or months, often worsening with physical activity.
Possible Causes: Muscle strain, ligament sprain, or degenerative disc disease.
2 . Sharp, Stabbing Pain
Description: A sudden, sharp pain that can radiate down to the legs, often described as a “shooting” or “electric shock” sensation.
Possible Causes: Herniated disc, sciatica, or spinal stenosis.
3 . Limited Range of Motion
Description: Difficulty in bending, twisting, or moving the lower back due to pain or stiffness. This may also include a noticeable decrease in flexibility.
Possible Causes: Arthritis, spinal stenosis, or muscle spasms.
4 . Pain that Radiates to the Legs
Description: Lower back pain that extends into the buttocks, thighs, or down the legs, often affecting one side of the body.
Possible Causes: Sciatica, herniated disc, or lumbar radiculopathy.
When to Seek Treatment
If you experience any of these symptoms, especially if they persist or worsen over time, it’s important to seek professional treatment. Early intervention can prevent further damage and significantly improve your quality of life.
Get Expert Care at Aarav Spine & Bone
Don’t let lower back pain control your life. At Aarav Spine & Bone in Vaishali Nagar, Jaipur, our experienced spine specialists and orthopedic surgeons are here to help you find relief and restore your mobility.
0 notes
Text
me, talking about how i have severely painful lumbar radiculopathy that's causing nerve damage, with no known cause: it's bizarre!
neurosurgeon: well better to be bizarre than have something serious going on
... do these doctors not hear themselves lol. i think i'd call this serious, and it's worse since without a cause we can't really treat it!
17 notes
·
View notes
Video
youtube
تزحزح الفقرات السبب والعلاج آلام الفقرات
تزحزح الفقرات السبب والعلاج آلام الفقرات
#العمود_الفقري (Vertebral column)
• جسم الإنسان إلى خمسة مناطق أساسية تبدأ من المنطقة العنقية، والصدرية والقطنية، والعجزية، وتنتهي في المنطقة العصعصية، بالإضافة إلى ذلك يحتوي العمود الفقري على 4 مكونات رئيسة، تشمل: الفقرات، والأعصاب، والمفاصل، والأقراص.
ما هي #الفقرات_القطنية :
• تتكون الفقرات القطنية من خمس فقرات وأحيانًا ست فقرات لدى بعض الأشخاص، وتسمى الفقرات القطنية حسب تسلسلها بالفقرة القطنية الأولى إلى #الفقرة_القطنية_الخامسة (L1 ،L2 ،L3 ،L4 ،L5)، إذ تترتب بشكل الحرف C بحيث تكون قاعدة المنحنى إلى الداخل، ويسمى هذا المنحنى بالمنحنى القعس (Lordotic curve).
• تقع الفقرات القطنية أسفل الظهر بين الفقرات الصدرية و العجزية، وتتميز بأنها أكبر حجمًا وأكثر سماكة من الفقرات الصدرية والعنقية كونها تتحمل الجزء الأكبر من وزن الجسم، وتُعد ثاني أكبر فقرات العمود الفقري حجمًا بعد الفقرات العجزية.
ما هي #أجزاء_الفقرات_القطنية :
1. جسم الفقرة جسم الفقرة القطني هو الجزء الأمامي المستدير للفقرة، ويعد الهيكل الرئيس لها الذي يتحمل الوزن.
2. النتوءات الشوكية (Spinous process) النتوءات الشوكية وهي بروزات عظمية تتواجد في الجزء الخلفي من الفقرة.
3. القوس الفقري (Vertebral arch) يتكون القوس الفقري من عظام مستديرة تحيط بالقناة الشوكية، ويقع في الجهة الخلفية من الفقرة، إضافةً يحتوي على التراكيب الآتية :
• العُنيقة (Pedicle) : هي زوج من النتوءات العظمية القصيرة والسميكة، وتقع خلف جسم الفقرة في الجزء العلوي.
• الصفيحة (lamina) : الصفيحة هي زوج من الصفائح العظمية الرقيقة، وتتواجد في الجزء الخلفي من الفقرة ووظيفتها حماية القناة الشوكية.
4. القرص الفقري يوجد بين الفقرات القطنية أقراص غضروفية تسمى القرص بين الفقرات (Intervertebral discs) تعمل هذه الأقراص كوسائد تحمي الفقرات من الاحتكاك مع بعضها، وتمتص الصدمات، وتوفر المرونة والدعم الظهر أثناء الحركة.
5. مفاصل الفقرات القطنية مفاصل وُجَيهِيَّة أو المفاصل المشتركة (Facet joints)، وهي عبارة عن فراغ موجود بين عظام الفقرات متواجدة على طول العمود الفقري تقوم بربط الفقرات مع بعضها البعض، حيث أن كل فقرة تمتلك زوجين من هذه المفاصل المشتركة، زوج علوي يربط الفقرة مع الفقرة التي تسبقها، وزوج سفلي يربط الفقرة مع التي تليها.
ما هي #أهمية_الفقرات_القطنية :
• تقوم بالدعم الهيكلي خاصةً دعم وزن الجزء العلوي من الجسم.
• تساعد على حركة جسم الإنسان.
• تعمل على حماية الأنسجة الرخوة المحيطة بها، مثل: الحبل الشوكي، والأعصاب، والأربطة، والأوتار.
ما هي #اضطرابات_الفقرات_القطنية :
1. الديسك (Lumbar disc herniation) الديسك أو كما يعرف بالانزلاق الغضروفي القطني ويسمى أيضًا القرص المنفتق القطني، هو أحد اضطرابات الفقرات القطنية التنكسية التي تسبب ألم أسفل الظهر والذي ينجم عن تهيج الأعصاب، ويحدث نتيجة تهتك الوسائد الغضروفية المتواجدة بين مفاصل الفقرات الذي قد يؤدي إلى الضغط على الأعصاب مسببًا اعتلال الجذور العصبية القطنية (Lumbar radiculopathy).
2. الإجهاد القطني (Lumbar strain) يحدث الإجهاد القطني نتيجة تمزق العضلات والأربطة والأوتار للفقرات القطنية، مما يؤدي إلى تمدد إحدى هذه الأنسجة، وغالبًا ما ينجم عن إصابات الحوادث أو حمل أو سحب شيئًا ثقيل.
3. الانزلاق الفُقاري القطني (Spondylolisthesis) يحدث الانزلاق الفُقاري نتيجة إزاحة الفقرات القطنية من مكانها بشكلٍ جانبي، ويُعد الانزلاق الفُقاري القطني من أحد الأسباب الشائعة التي تُتسبب آلامًا في أسفل الظهر خاصةً لدى كبار السن أو الأشخاص الذين يمارسون النشاطات البدنية التي تؤثر على الفقرات القطنية، مثل: والجمباز، ورفع الأثقال، وكرة القدم.
ما هي اضطرابات الفقرات القطنية الأخرى :
1. تضيق #القناة_الشوكية.
2. #التهاب_المفاصل الروماتويدي.
3. كسر الفقرات.
4. تكون العظمة الشوكية (النتوءات الشوكية).
5. هشاشة العظام.
6. إصابة العمود الفقري بالعدوى الجرثومية التي تسبب التهاب العظم والنقي (Osteomyelitis)، أو التهاب الأقراص الإنتاني (Septic discitis).
7. أورام العمود الفقري.
8. بعض الأمراض الخلقية أو الوراثية التي تؤدي إلى تشوه عظام الفقرات مثل مرض باجيت (Paget's disease).
تقوس أسفل الظهر (Lordosis).
9. داء باستروب (Baastrup disease)، ويسمى أيضًا بمتلازمة تقبيل العمود الفقري، وهو أحد الأمراض التنكسية للعمود الفقري التي تحدث نتيجة تشكل أكثر من عظمة شوكية بشكل متقارب أو متقابل، بحيث يكون مظهرها مشابه للعُناق.
د. / بهاء الدين سعيد :
• القناة الرسمية للدكتور بهاء الدين سعيد دكتوراة جراحة العظام جامعة القاهرة.
• استشاري جراحة العظام والمناظير والكسور مستشفيات جامعة القاهرة ومستشفى السلام الدولي و مستشفى مصر الدولي ومستشفى دار الفؤاد.
عناوين العيادات :
• القاهرة المعادي : ٢٠ شارع النصر بجوار مطعم جندوفلي ومكتبة ألوان و امام التوحيد والنور.
• لدينا فروع اخرى التجمع الخامس والجزيرة بلازا الشيخ زايد و فرع الهرم وبرج دار الفؤاد مدينه نصر.
• أرقام الحجز والاستفسارات : 01122443886 - 01113332751
واتس اب
• https://wa.me/0201113332751
Google Map
• https://goo.gl/maps/vgWuLix7NhCEyUCj6
Link Social Media :
• https://www.facebook.com/BahaaSaiedClinic
• https://twitter.com/BahaaSclinic
• https://www.instagram.com/BahaaSaiedClinic
• https://www.tiktok.com/@BahaaSaiedClinic
Channel Link Subscriptions
• https://www.youtube.com/@BahaaSclinic
#الانزلاق_الغضروفي
#العلاج_التداخلي_للعمود_الفقري
#القناة_الشوكية
#التهاب_المفاصل
#استشاري_جراحات_العظام_والمناظير_والكسور
#استشاري_جراحات_اصابات_الملاعب
#اضطرابات_الفقرات_القطنية
#الم_الظهر
#أفضل_دكتور_عظام_في_مصر
#احسن_دكتور_عظام_في_مصر
#الغضروف
#الفقرات_القطنية
#العمود_الفقري
#قطع_غضروف
#السعودية
#قطع_غضروف
0 notes
Text
Top Radiculopathy Treatment in Mumbai: Synapse Spine
Radiculopathy is a condition affecting the spinal nerve roots, causing pain, weakness, and numbness in various body parts. If you're experiencing radiculopathy symptoms and seeking the Top Radiculopathy Treatment in Mumbai, it's crucial to consult a specialist for personalized treatment. At Synapse Spine, we are committed to providing comprehensive care for radiculopathy patients, ensuring they receive top-notch treatment and support.
Types of Radiculopathy
Radiculopathy can occur in different spine regions, each with unique symptoms:
Cervical Radiculopathy: Affects the neck, causing pain, weakness, and numbness in the shoulders, arms, and hands.
Lumbar Radiculopathy: Impacts nerves in the lower back, leading to pain, weakness, and numbness in the legs and feet.
Thoracic Radiculopathy: Targets nerves in the middle back, resulting in pain, weakness, and numbness in the chest and abdominal area.
Causes and Symptoms of Radiculopathy
Causes:
Disc herniation
Spinal stenosis
Degenerative disc disease
Bone spurs
Inflammation
Symptoms:
Radiating Pain: Sharp or shooting pain along the affected nerve path.
Weakness: Reduced muscle strength connected to the affected nerve.
Numbness: Loss of sensation or tingling in the affected areas.
Tingling: Sensations of prickling or "pins and needles" in the extremities.
Muscle Atrophy: Gradual weakening or wasting of muscles due to nerve dysfunction.
Diagnosing Radiculopathy
At Synapse Spine, our experts use a comprehensive approach to diagnose radiculopathy, including:
Clinical Assessment: Detailed evaluation of symptom nature and progression.
Neurological Examination: Assessment of nerve function, reflexes, and sensory responses.
Imaging Studies: X-rays and other imaging techniques.
Electrodiagnostic Tests: Electromyography (EMG) and myelogram.
Blood Tests: To rule out other conditions.
Treatment for Radiculopathy
At Synapse Spine, we adopt a multidisciplinary approach, tailoring treatment plans to each patient's unique needs. Our options include:
Medication/Ice/Heat: Prescription anti-inflammatory drugs or muscle relaxants and the application of ice or heat.
Physical Therapy/Specific Exercises: Exercises to improve range of motion and strengthen muscles around the affected nerve.
Epidural Steroid Injection: To alleviate nerve pain in the back or leg.
Spinal Cord Stimulation (SCS): Remote-operated implants for severe, unresponsive pain.
Surgical Treatments for Radiculopathy
In some cases, surgery may be necessary. Our experienced surgeons offer various surgical treatments, including:
Microdiscectomy
Laminectomy
Foraminotomy
Discectomy
Spinal Fusion
Artificial Disc Replacement
Endoscopic Surgery
Nucleoplasty
Intradiscal Electrothermal Therapy (IDET)
Peripheral Nerve Surgery
If you are experiencing radiculopathy symptoms in Mumbai, consult a specialized doctor for personalized treatment and optimal spinal health. At Synapse Spine, Top Radiculopathy Treatment in Mumbai offers comprehensive care, ensuring the best possible treatment and support. Take the first step towards a pain-free life by booking your appointment today. Call us at 93726 71858 | 93211 24611 or click here.
#endoscopic surgery#spinal fusion#spinal stenosis#degenerative disc disease#brain and spine tumors#orthopedic spine surgeon#synapse spine#spine specialist#spinesurgery#dr. ajit mishra#Microdiscectomy#Laminectomy#Foraminotomy#Discectomy#Spinal Fusion#Artificial Disc Replacement#Endoscopic Surgery#Nucleoplasty#Intradiscal Electrothermal Therapy (IDET)#Peripheral Nerve Surgery
0 notes