#it just also turns out he has severe metastatic lung cancer
Explore tagged Tumblr posts
Text
we are euthanizing my family dog in the next few days and i am really sad about it
#personal#he has had a really nice life and got old and was happy the whole time#it just also turns out he has severe metastatic lung cancer
9 notes
·
View notes
Text










As a urologist this sounds like bladder cancer
There are several types of bladder cancer, so without knowing what the pathology is it’s hard to say what his prognosis is. About 70% of tumors can be managed without major surgery or chemotherapy. I am guessing by his “routine treatments” that he has a good prognosis
------
Not in the traditional sense. Some bladder cancers can be managed by putting therapy directly into the bladder through a catheter. In the US we use something called BCG, but we can also use other types of chemotherapy. It’s very different than getting normal chemotherapy.
That statement is what makes me think he has bladder cancer and is likely undergoing a BCG regimen.
------
My dad had / has bladder cancer. From what I understand, the specific type of bladder cancer determines whether it's aggressive or not. Again, "from what I understand", there are two factors that determine the severity: what tissues are affected (superficial tissue to muscle tissue to actually through the wall and into neighbouring organs / tissue) and the type of cancer. Some types spread more rapidly. Basically: an aggressive type that already penetrated the muscle tissue is extremely bad news, while a non-agressive type in the superficial tissue is very treatable.
u/gu_doc please correct me if I got it all wrong!
gu_doc: You are absolutely correct.
------
Every BPH surgical treatment that I can think of will involve direct visualization or imaging of the bladder. It’s not too uncommon for us to look in the bladder when evaluating BPH and find a bladder tumor.
------
It’s not uncommon to incidentally find bladder cancer when working up a prostate. Obviously there are many other possibilities, but this is my guess.
------
I was wondering (because I legitimately don’t know) if BCG is used over there. Don’t they use BCG as their tuberculosis vaccine? I wonder if intravesical BCG is more or less effective in that case
------
They almost might have thought something was like reactive tissue but turned out CIS or something. I don’t know. Maybe they put him up in stirrups and found a wart.
We don’t always scope before BPH procedure in my practice if we have a prostate volume from another source
------
BCG reduces the risk of recurrence, so fewer times going to the OR potentially. We treat people in their 70s and 80s all the time for this
------
Why do I jump to bladder primary? Because it fits the story to me.
The perception I got is that this other primary was found during a BPH surgery. Not during scans or evaluation, but during a surgery. Areas often overlooked that would be seen better during surgery would be something oral, maybe something of the lungs/airway (maybe he got bronched due to blood on ET tube placement?), penis, testicles, bladder, and anus.
Again, as a urologist, bladder fits the story to me. We are obviously missing a ton of information here as they’re being intentionally vague. I could be way, way wrong. I could just see it. This happens not infrequently in my practice.
And I don’t mean UCC metastatic to the prostate. I’m saying they saw it on cystoscopy and biopsied it separately.
13 notes
·
View notes
Text
ok, update time
So amigas, I’ve been a cranky and unhappy camper for some time but things are happening so here’s an update. After I got randomized to the standard arm of the trial I made one last effort to try to get SABR in BC (prompted by hearing from someone in Ontario with met breast ca with a lung met who had an oligoprogression treated with SABR in May 2020). Short answer was, sorry not possible. Long answer was, sorry not possible because a) there’s no evidence that this has any benefit and b) that’s why we want all SABR to be in trial and c) other locations without active trials might do something else but essentially they’re doing uncontrolled studies on pts. So, ok, by then I’d become essentially resigned to doing standard rads, esp since my RO repeated reassured me he’d treat me aggressively and was very optimistic about the plan. Then he calls me to say “hey, weird thing about this trial, it won’t let me do what I want to do in the standard arm”. Took me all of 10 seconds to confirm he COULD do the aggressive standard rads off trial & to drop out of the trial on the spot. So now I’m not in any trial and I will get my aggressive 15 treatments, burning my chest to a nice itchy crisp & hopefully roasting that lung met in the process. I had my ‘mapping CT’ last Friday. It was tedious; my left shoulder where I had lymph nodes biopsied in 2017 has never returned to full ROM and it was painful being positioned in the CT machine for the length of time needed. I’m now working on stretches because I need to be able to do this for 15 business days for the actual rads. I got 2 new spot tattoos that they use for positioning in the CT machine & they’re re-using some of my old tats as well. And now we just wait for scheduling. I hope it isn’t too long. This stupid met grew in 8 weeks, so at such a fast rate, the mapping CT will be out of date if we delay too long. But there’s nothing for it but to wait my turn.

Last Thursday, I had my first dose of Abraxane & also went to the private clinic for the first time to get my immunotherapy direct from Roche. Abraxane first. I HATE IT. I mean it’s supposedly essentially the same as taxol but jesus on a pogo stick, that stuff is awful. I was flattened with pain from Friday night to Sunday night, took my hydromorphone at night for the first time & had to stay fully medicated around the clock or even lying down hurt. Also, I iced but my neuropathy just exploded. My hands feel way worse and I have weird neuropathy in my mouth too. There are several things I’ll be discussing with the MO. One is dose scheduling. The Roche trial for abraxane + atezolizumab immunotherapy used abraxane at 100 mg/week for 3 weeks on, 1 week off. The BC Cancer agency protocol for abraxane in metastatic setting is 260 mg every 21 days. So I got 260 mg. And while I like the idea of getting it only every 21 days instead of weekly, this dose is too large, and also we don’t know if it works as well on this schedule. So I’ll be discussing with my MO some options: dose reduce and stay on q 21days; switch to weekly (not sure if BCCA will even allow it as it’s not their protocol); switch back to my dose reduced taxol. Dropping chemo altogether and stay on immunotherapy only is another idea she floated last time but I’m a bit hesitant with that one, esp since I just had a small progression in the lung. Ok, so that’s that. Abraxane sucks so bad.

(joke! not really nauseous. Totally lost appetite tho) Now the private clinic. On the plus side, it’s literally right behind the hospital and let’s not forget they’re giving me super expensive meds for free. So those are big plusses. Now the actual clinic is teeny tiny, staffed by 2 nurses who were run off their feet when I was there. They have 4 treatment chairs, not spaced very far apart. Total occupancy for COVID under Worksafe is 7 people. The whole place is like the size of my living room. I also had this vague feeling of being in a “clinic” where a “doctor” (you know the one who’s maybe finished med school in some country somewhere but isn’t really licenced) can give you cosmetic surgery for cash. The whole place feels shady AF but presumably it’s a legit place and they gave me real meds.

Also other than this clinic, the entire block is surrounded by addictions support services, rehab, transitional housing etc etc. Scheduling for the clinic is independent of the cancer agency scheduling so now I have to wrangle two schedules to fit each other. Next immunotherapy is on the 11th.
Still waiting on pathology results from the lung biopsy. The local pathologist will confirm if it’s a breast cancer met & run hormone marker tests on it.
I did hear it looks like they got enough tissue samples to send for the Foundation genetic testing (which Roche is paying for) so that will be interesting to see if they find anything actionable. I’m not getting my hopes up because other than a somatic* BRCA mutation, I don’t think there’s anything in BC that I could get treatment for anyway. This is cutting edge stuff, this tumor genetic testing. It’s what they talk about when they discuss personalized medicine - but we’re still years away from actually being able to target most of the mutations. *germline mutations are one’s the person has in their DNA. I’ve already been tested for germline BRCA mutations and was negative. Somatic mutations are ones the cancer tissue acquires. They’re not terribly common but not uncommon either. Ovarian esp likes to throw somatic BRCA.
2 notes
·
View notes
Text
Hi friends,
I’ve been pretty uncharacteristically silent on here recently but just wanted to send you a little wave and let you know I’m still here and doing ok even though it’s been a rougher month than usual. First, here’s the wave:
Now here’s the update (below cut):
In the past month I had a few very not-great things happen. In chronological order (and actually the order in which they were distressing from least to most):
My aunt died unexpectedly. We were not close at all, though not quite to the point of being estranged (exchanging gifts and cards continued). It is sad, but in a way I really lost her a long time ago. She was a really difficult person with a number of psychological problems including hoarding, meaning her house is a disaster. She was living my with disabled uncle but they had separate schedules and she had her own entrance so she was dead several days before he noticed. These are both my dad’s younger siblings. My parents (75 and 79) have been in Texas for a month now working on the funeral, the house, and arranging care for my uncle (who is deaf and autistic and an ex-alcoholic - he’s never lived totally alone and can’t start now). I haven’t been able to go help because of my chemotherapy (and my full-time job I still work). We’re all emotionally tapped out.
I had to decide within a week whether I ever wanted biological children. The situation is that chemotherapy damages your eggs. I had already had 10 weeks of chemo so really this seems like the kind of thing that someone could have told me during the 2 fucking months I was diagnosed but not in chemo. I mean, I guess the reason no one did is we all kept hoping I could start it right away and if I had wanted to freeze my eggs I would have needed a few weeks. But honestly I think they literally forgot since what brought this up was me complaining about having my period while on chemo (which is unusual - apparently most people stop) and they were like “omg fertility!!”. Anyway, there were two bad options: 1) delay treatment so I could freeze my eggs or 2) take a drug that shuts down all my sex hormones basically causing early menopause in the hope (NOT certainty) that it protects them. Now, I’ve always been very confident in my desire not to have children at all. This was true when I was married and it’s true now. I first said it when I was 23 and now I’m 35 and it’s still true. So you’d think it would be easy and, in a way, it was. But I felt so rushed and there was SO much cultural pressure to say that I should keep every option open that I felt way more unsure than I would otherwise. I decided not to do either and let things take their course. Only NOW it turns out I’m not going to be doing chemo for a while because of my third bad thing so that door may still be open.
My most recent scans to assess the effectiveness of chemo and the status of my cancer were highly mixed. Now, I have a lot of cancer. I have stage 4 (metastatic) breast cancer that was in: 1) a large (LARGE) bastard of a tumor in my left breast that is so big that it hurts all the time because it presses nerves and skin; 2) a lymph node under my left arm; 3) a bunch of small tumors in my lungs; 4) at least one small tumor in my liver; 5) a soft tissue tumor next to my L4 vertebra; 6) my bones at the point at which that vertebra joins the pelvis. That is a fucking lot of cancer. I don’t think people quite get it when you just say “metastatic” or even “stage 4.” It could definitely be worse but it’s pretty bad. This cancer is super fast and super aggressive--it’s a black ops team. Turns out that, like a team of special forces, it’s still fucking gunning for me. The chemo I was on is pretty standard fare because (more bad luck which you can read more about on my cancer blog @pitiless-achilles-wept) I’m negative for all the things that offer additional treatment options. It turned out to work really well on my lungs, which is actually great news b/c that shit was scary, so I only have a couple small tumors left now there. BUT the bastard tumor and one on my liver got a full centimeter larger (FAST growing jeez). Other stuff seems stable and they didn’t it new places, which is also good. But they do need a better treatment for it than this one. So, instead of more chemo I’m joining a clinical trial for something called PARP inhibitors that basically stop DNA repair in cancer cells so that they die. I don’t have any heritable breast cancer genes but I DO have the BRCA1 mutation in my tumor cells. That’s a “somatic” mutation as opposed to a “germline” mutation. PARP inhibitors work really well on BRCA patients with the inherited mutation so the study is seeing if they also work well on the somatic mutation. My fingers are hugely crossed that the answer is YES and I’m hustling to get going ASAP so this fucking bastard cancer doesn’t spread even further in the meantime. But joining the trial involves a lot more doctor visits at a time when I totally don’t feel up to them (since doctor visits involve making yourself a huge pain in the ass to be an advocate). I’m sort of on my own for this since my parents are dealing with all that other stuff and I’m single AND an only child. I do have great friends, though, who will do things like make phone calls when I can��t stand it anymore. But my goodness, friends, am I emotionally wrecked.
So that’s where I’ve gone. I wish it were better to report and also that I could be writing more here since it does help. But the fatigue I had from treatment plus just the exhaustion that comes with weighty emotional stuff has stopped me.
I still hang out on here, distracting myself with hellatus meta (and crack) and using Cockles gifs to cheer myself up (which does actually work b/c they are bottled sunshine like 98% of the time). I miss you all and hope you know that I’ll be back when I can. I appreciate the love you send, even when I can’t muster the energy to respond to it. 💜💜💜
#not spn#personal#medical update#my life as a cancer patient#family things#tumblr friends#tumblr life#YANA#AKF
70 notes
·
View notes
Text
Request for Aid
Hello, mutuals, followers, and my various RP families. Sara’s mun here.
The past several weeks have been incredibly emotional, so if you guys aren’t interested, I’ll add in a break for those who would prefer to scroll past. For those that stay, even a reblog to help share this would be incredibly appreciated...
A few weeks ago, my mother called me to inform me that my grandfather had a heart attack, and that he was staying at the hospital because of built-up fluid in his lungs. Over the course of 48 hours, the doctors ran a myriad selection of tests, which led them to discover that he has End Stage Metastatic cancer in his lungs. After finding it there, they ran more tests to see if it was elsewhere. It was confirmed positive in his lymph nodes, adrenal glands, and bones, with a test pending to confirm whether it was also in his brain. They gave him approximately 6 months to live.
A few days later, my mother called me again, anxious and in tears because he was being so combative with the doctors that his heart rhythm was highly erratic, and exacerbating the fluid that kept building up in his lungs. At this point in time, they were also still waiting on the brain tests for confirmation of cancer presence. Everyone was sitting on pins and needles, hoping he would cooperate long enough to get his first round of chemo-therapy (which the doctors told them would ONLY be for quality of life improvement, not for added longevity).
Three days later, another phone call from my mom in hysterics saying that he had gone home the night before only to take a turn for the worst and get rushed back to the hospital. The particulars were not given to me (though the cancer had been confirmed to also be in parts of his brain), but it was bad enough that she put my dad on a plane from where they live in GA to MI where his parents live.
He ended up staying with my grandparents for six days. By the time he went back home, grandpa was stable and cooperative enough to go back home (for the second time). His first round of chemo was scheduled soon, and everyone was looking optimistic that he would remain with us through his time left in relative comfort.
For four long days, I heard nothing from my parents. I hoped no news was good news, and even managed to keep busy enough at work for the days to go by relatively quickly. Then on Thursday, I received a tearful call from my mom. My grandpa was back in the hospital - his cancer had now spread to his liver. The doctors had - by this point - tentatively shortened his time left to the end of January, and (according to my mom) that was being generous.
After a lot of back and forth conversation, I determined that I wanted to try to have my nuclear family (myself, my husband, and our 8-year-old son) travel to Michigan for Thanksgiving this year to ensure my son would get to spend one more holiday with his great grandfather (which we had done once a year up until this year [we went to Easter family get-together with that side of the family every year until this year - we weren’t able to make it this year]). I agreed to do everything in my power to ensure I’d be able to take time off work to make this trip happen for us, and for my parents, and for my grandparents.
But the fun of that day wasn’t quite over - about an hour after my initial phone call with my mom, she called me back to inform me that the doctors were now giving my grandfather approximately two weeks, give or take a little, to live. The acceleration of his cancer, it seems, had been incredibly aggressive, and they did not expect it to slow down at all. With that in mind, they now planned on stopping all treatment once my grandfather was stable, sending him home, and getting him set up with hospice care to make him as comfortable as possible.
On Sunday, my mom called me to let me know that they got him home and set up, with everything in place. He seemed to be comfortable and stable, for now. The one thing the doctors have reveled at in all of this is that my grandfather’s pain levels have been minimal throughout this ordeal. That alone still gives us hope that he will remain stubborn enough for us all to see one another at Thanksgiving in Michigan.
And this brings us to yesterday. Somehow along all of this, my mother had not been made clear that my intentions were to go to Michigan. Once she heard that was my hopeful plan, she went to see about plane tickets. Thanks to her long-standing good reputation with Delta, she managed to get a quote for the tickets for the three of us: $1100. My mother’s initial offer (knowing that money has been tight for us) was to cover two of the three plane tickets so that we would only need to pay for one. In order to lift some stress from my mother’s shoulders (despite not having a plan in place for it), I offered for us to pay half of the total instead of just for one ticket. While this helped my mother relax, the two hours I spent frantically trying to figure out where to come up with $550 dollars was quickly wearing my nerves away (all while I was at work, too).
On my lunch break, I had to run to Target to pick up a few cleaning supplies for work when my mom called me again. She was getting the plane tickets booked in my ear, while my husband was trying to find a way out of fronting $550 we don’t have in the other ear. I was incredibly hesitant, and vocalized it, only for my mom to stop me. She then informed me that my grandmother - who was infinitely grateful that we were trying to plan to come visit for Thanksgiving - had told my mom to buy the tickets and that the cost was covered. It was more than my heart could take. I broke down in tears, in the middle of the day in a damned Target, trying to think of something to do to pay my grandmother back. She’s been through more than everyone, and yet she was sweeping in to the rescue anyway.
That being said. I am opening emergency commissions for sketchy headshots, jewelry concept art, and handmade scarves. My goal would, ideally, be to make the full $1100 to pay back my grandmother. Regardless of whether my grandfather makes it to Turkey day or not, we will be making the trip to Michigan, and that’s not something I get to do very often (a con to my job, which typically blacks out the months of November and December from any and all holiday travel because it’s the busiest time of the year for us).
If any of the below interests you, please send me a message and we’ll get the particulars figured out. Here’s what I have to offer:
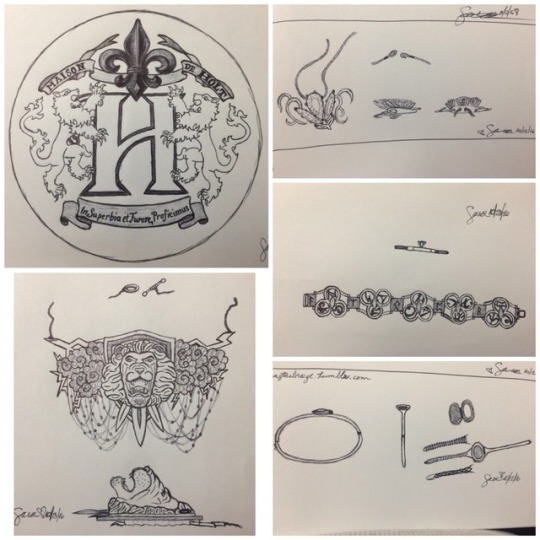
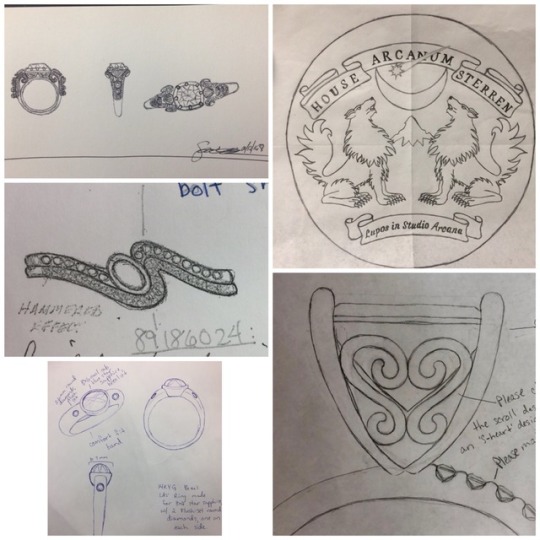
$5-$20 : Jewelry Concept Sketch (traditional artwork)
For those who might have an idea for a canon item their character may or may not carry with them, I can help give your trinket dimension. The more details / complexity, the more this would cost. Can add digital color for an additional $3. Seen below are a mix of requested designs for tumblr and concept art drawn by me at work.
$15-$45 : Character Bust Headshots
While I usually need a faceclaim or inspiration in order to create these, if you have a general idea (or give me creative license based on the info you give me), I can likely create it with little trouble. Line art only takes the least amount of time. Shading is midline. If you want color, I need screenshots / references, and it would be the most expensive. Armor is not something I’m strong at, but I would absolutely try to include some if it is wanted.

$25-$55 : Handmade Scarves
I have a self-taught talent for creating scarves of various sizes and styles. The ruffly scarves are good spring / autumn scarves - lightweight and fashionable - but still provide a light amount of heat retention; they can come in pretty much any color of the rainbow (availability would have to be confirmed, but I do have a bunch here at home already). The thick fluffy scarves (middle image and bottom left image) are a combination of 2-4 yarns interwoven together to create a very warm winter scarf that can either be traditional or infinity-style and provide heavy heat retention; they too can come in myriad colors (subject to availability), but it should be noted that multiple colors are more expensive. I also will put a disclaimer here that I will only provide a scarf to those who confirm they are not sensitive to wool products, as all of these are wool-based.

All payments will be taken via PayPal (which we will discuss via dms), so please be respectful of this.
Thank you for taking the time to read through everything. It means a great deal to me. Any and all small donations are incredibly appreciated (I’ll be trying to put something together for those as well). If you cannot purchase or donate, please help me out by reblogging this to share it. I’ll be reposting a shorter Commission post later this week for proper reblogging, after work is done for the week.
I love and appreciate you all for your time, and hope there is something I can offer to each of you.
(( to my various RP families: @blackbay-wra @holtandthornetradingco @householt @the-wyrmrest-sanctuary ))
75 notes
·
View notes
Text
lucky me, lucky mud
It came on suddenly on Wednesday afternoon, and by the evening my fever was 103°. Feeling just truly awful, I called my mom to complain and was told by both her and our longtime family friend Alison that I should go to urgent care, and then once we realized urgent care was closed, the emergency room. Alison – tall, uncompromising, fiercely loving, stubborn as hell -- had spent the last two years being treated for metastatic lung cancer, but was calling the fight. My mom was spending a few nights with her in the lead up to her “final exit” on Saturday when she would end her life via a fatal dose of prescribed medication thanks to Washington's Death with Dignity Act.

My mom, Alison, and her beloved daughter Alyssia making frittata in our old house (2010)
Despite being a nurse and therefore a person who had spent her life ministering to the needs of strangers, Alison had refused to hire a caregiver. She hated the idea of a stranger in her house messing things up, and much preferred the idea of her friends and family doing the messing. And her loved ones had stepped up, caring for her in shifts all the way to the end, despite the fact that all along there had been the means to hire help. Many people wouldn’t have the guts to test their friends like this, especially at the end, but Alison was brave like that.
Sometimes my dad and I challenge each other to imagine what it might be like to be dead forever, and there’s this vertiginous drop and then a feeling of waking up and I know I have failed. We move on to other topics. My dad has told me that even though he has terminal cancer he can’t really fathom the fact that he will die much more than I can. It’s basically impossible to understand the concept of being dead forever. As Joseph Campbell said, “Eternity isn’t some later time. Eternity isn’t even a long time. Eternity has nothing to do with time.” It would be like a fetus trying to understand what it is to be born.
Something else that’s non-linear is fever. 103° is uncomfortably hot. It’s the point that you start putting towels dipped in ice water on your body even though this too feels awful because you’re achy and somehow also freezing. It’s only three degrees hotter than 100° but that’s a lot if you consider there’s only like seven degrees between fine and dead.
I didn’t know which hospitals in the city took my extremely “boutique” kinda-Cigna-kinda-not PPO plan and attempts to log in to my “provider finder” kept coming back with a wrong username or password message. I was feeling bad enough that I knew if I didn’t do this right now, I would just lie down and hope for the best, so I picked the nearest ER and called an Uber.
It was an unseasonably warm night, and the waiting room was crowded but hushed. The ED experience itself was truly not bad, and I spent most of the four hours I was there in my own watching Nightmare on Elm Street. Everyone was extremely friendly. The doctor even made me feel like I wasn’t an idiot for coming in, saying she’d had several strong women, ER nurses even, felled similarly by what turned out to be the virus that causes the common cold. Our immune systems over-reacting after several years of coddling. By midnight my temperature was down to 99°, and I was ready to go. Hours later, it had climbed back to 103°. It cycled like that for the next 36 hours.
On Friday, my mom told me that Alison had looked at her and said in awe and not quite belief, “This is my last day on Earth,” which rocked me more than learning the news of her death the next day would. Probably I could comprehend the concept of her last day on Earth, but not her actually dying. You think when it happens you will understand it to be true, but then it’s just like everything else: not what you hoped for or despaired over and in fact something else entirely.
Speaking of courage in the face of extreme adversity, I mustered the strength to call my insurance and find out if the hospital I went to was in network. The call is answered by Christopher, who refers to himself as a concierge. He assures me that no, the hospital I went to is not covered. When I sputter that other hospitals in the same hospital chain are covered, he explains that just because two hospitals are part of the same organization does not mean they take the same insurance since each individual site apparently contracts with insurance based on its own personal preferences. You can be sure this is the case because if it’s asinine, opaque, and cruel it’s the American healthcare system.
I started to cry imagining how many thousands of dollars my little sojourn had cost me and for what? Nothing had really been done (there was also not really anything to be done). I hadn’t needed medical care so much as medical assurance that I wasn’t going to die. But at 9 o’clock at night, the ER must serve both functions (and many more). It hadn’t turned out to be an emergency but that’s the thing about emergencies: if you wait too long to find out if it is one, it will end one way or another, and you might not like “another” and you might like “one way” even less.
As soon as I started crying something changed in Christopher and he went from being a haughty mansplainer to just a man, ie terrified of women’s tears. “No no no no no no you don’t need to cry. Oh please don’t cry…” he said. I blubbered that it was “just so complicated,” by which I meant the American Healthcare System, but he thought I meant Life.
And again Christopher cycled, becoming not just a man but the saddest man on Earth. “Ramona it’s going to be ok. I understand that life is really hard. Believe me. I cry every day. My friends are like, ‘Christopher, are you ok?’ And I tell them, ‘Every morning I wake up is a win.’ The thing is, it could be over likethat, and I’d rather have a hard life than a short one.”
He went on like this for 10 minutes, and although he clearly knew he was on a recorded line, at one point saying, “We’re your health insurance company. We want you to get the most out of your benefits,” I actually did feel better when the call was over. This might have had something to do with learning I “only” had to pay 30% on out of network ER visits (after the $1000 deductible), but it was also his earnest reminder that these days, no matter how dumb and twisted, are in no way guaranteed. It could and one day will be otherwise.
He ended the call by giving me his extension and telling me to call when I got the bill and also if I needed anything in general, “If you just need to cry that’s fine. I’ve helped members order pizza, find a lawyer. As long as it isn’t illegal, unethical or immoral I will do what I can to help you.” At this point, it was clear that Christopher was not a man terrified by women’s tears, but a man who loved tears of all kinds, and in fact required them as payment for his services.
On Saturday morning I was feeling well enough to get out, and took a long walk north into Fishtown. At some point Cathy called and we chatted while I stood on the sunny sidewalk eating a free cupcake. We talked about Alison, who at that point had an hour and 15 minutes left until she was dead forever, and the Phillies, and whether we would get brunch next weekend. It’s psychotic that anyone could speak of such things – could speak period – when someone they know is about to die, but then you do it and you see how it can happen. Does happen. Everyday. How we keep living even while people die forever.
Cathy had just come back from a trip to Seattle where she had stayed with my dad while my mom came to visit me in Philadelphia. She said it was a highlight of her year. Spending time with my dad has always been good for that, but more generally being in the company of people who are seriously ill is often a surprisingly life-giving experience. You trip back over the threshold, relieved. The sun is out. A store that sells $40 candles is opening down the block.
Eternity unreels, but not yet for me.
1 note
·
View note
Text
Supreme Court Justice Ruth Bader Ginsburg Dies At 87
— AP | September 18, 2020 | By Mark Sherman

WASHINGTON (AP) — Supreme Court Justice Ruth Bader Ginsburg, a diminutive yet towering women’s rights champion who became the court’s second female justice, died Friday at her home in Washington. She was 87.
Ginsburg died of complications from metastatic pancreatic cancer, the court said.
Her death just over six weeks before Election Day is likely to set off a heated battle over whether President Donald Trump should nominate, and the Republican-led Senate should confirm, her replacement, or if the seat should remain vacant until the outcome of his race against Democrat Joe Biden is known.
Chief Justice John Roberts mourned Ginsburg’s passing. “Our Nation has lost a jurist of historic stature. We at the Supreme Court have lost a cherished colleague. Today we mourn, but with confidence that future generations will remember Ruth Bader Ginsburg as we knew her — a tireless and resolute champion of justice,” Roberts said in a statement.
Ginsburg announced in July that she was undergoing chemotherapy treatment for lesions on her liver, the latest of her several battles with cancer.
Ginsburg spent her final years on the bench as the unquestioned leader of the court’s liberal wing and became something of a rock star to her admirers. Young women especially seemed to embrace the court’s Jewish grandmother, affectionately calling her the Notorious RBG, for her defense of the rights of women and minorities, and the strength and resilience she displayed in the face of personal loss and health crises.
Those health issues included five bouts with cancer beginning in 1999, falls that resulted in broken ribs, insertion of a stent to clear a blocked artery and assorted other hospitalizations after she turned 75.
She resisted calls by liberals to retire during Barack Obama’s presidency at a time when Democrats held the Senate and a replacement with similar views could have been confirmed. Instead, Trump will almost certainly try to push Ginsburg’s successor through the Republican-controlled Senate — and move the conservative court even more to the right.
Ginsburg antagonized Trump during the 2016 presidential campaign in a series of media interviews, including calling him a faker. She soon apologized.
Her appointment by President Bill Clinton in 1993 was the first by a Democrat in 26 years. She initially found a comfortable ideological home somewhere left of center on a conservative court dominated by Republican appointees. Her liberal voice grew stronger the longer she served.
Ginsburg was a mother of two, an opera lover and an intellectual who watched arguments behind oversized glasses for many years, though she ditched them for more fashionable frames in her later years. At argument sessions in the ornate courtroom, she was known for digging deep into case records and for being a stickler for following the rules.
She argued six key cases before the court in the 1970s when she was an architect of the women’s rights movement. She won five.
“Ruth Bader Ginsburg does not need a seat on the Supreme Court to earn her place in the American history books,” Clinton said at the time of her appointment. “She has already done that.”
On the court, where she was known as a facile writer, her most significant majority opinions were the 1996 ruling that ordered the Virginia Military Institute to accept women or give up its state funding, and the 2015 decision that upheld independent commissions some states use to draw congressional districts.
Besides civil rights, Ginsburg took an interest in capital punishment, voting repeatedly to limit its use. During her tenure, the court declared it unconstitutional for states to execute the intellectually disabled and killers younger than 18.
In addition, she questioned the quality of lawyers for poor accused murderers. In the most divisive of cases, including the Bush v. Gore decision in 2000, she was often at odds with the court’s more conservative members — initially Chief Justice William H. Rehnquist and Justices Sandra Day O’Connor, Antonin Scalia, Anthony M. Kennedy and Clarence Thomas.

The division remained the same after John Roberts replaced Rehnquist as chief justice, Samuel Alito took O’Connor’s seat, and, under Trump, Neil Gorsuch and Brett Kavanaugh joined the court, in seats that had been held by Scalia and Kennedy, respectively.
Ginsburg would say later that the 5-4 decision that settled the 2000 presidential election for Republican George W. Bush was a “breathtaking episode” at the court.
She was perhaps personally closest on the court to Scalia, her ideological opposite. Ginsburg once explained that she took Scalia’s sometimes biting dissents as a challenge to be met. “How am I going to answer this in a way that’s a real putdown?” she said.
When Scalia died in 2016, also an election year, Senate Majority Leader Mitch McConnell refused to act on Obama’s nomination of Judge Merrick Garland to fill the opening. The seat remained vacant until after Trump’s surprising presidential victory. McConnell has said he would move to confirm a Trump nominee if there were a vacancy this year.
Reached by phone late Friday, Sen. Lindsey Graham, R-S.C., the chairman of the Judiciary Committee, declined to disclose any plans. He said a statement would be forthcoming.
Ginsburg authored powerful dissents of her own in cases involving abortion, voting rights and pay discrimination against women. She said some were aimed at swaying the opinions of her fellow judges while others were “an appeal to the intelligence of another day” in the hopes that they would provide guidance to future courts.
“Hope springs eternal,” she said in 2007, “and when I am writing a dissent, I’m always hoping for that fifth or sixth vote — even though I’m disappointed more often than not.”
She wrote memorably in 2013 that the court’s decision to cut out a key part of the federal law that had ensured the voting rights of Black people, Hispanics and other minorities was “like throwing away your umbrella in a rainstorm because you are not getting wet.”
Change on the court hit Ginsburg especially hard. She dissented forcefully from the court’s decision in 2007 to uphold a nationwide ban on an abortion procedure that opponents call partial-birth abortion. The court, with O’Connor still on it, had struck down a similar state ban seven years earlier. The “alarming” ruling, Ginsburg said, “cannot be understood as anything other than an effort to chip away at a right declared again and again by this court — and with increasing comprehension of its centrality to women’s lives.”
In 1999, Ginsburg had surgery for colon cancer and received radiation and chemotherapy. She had surgery again in 2009 after being diagnosed with pancreatic cancer and in December 2018 for cancerous growths on her left lung. Following the last surgery, she missed court sessions for the first time in more than 25 years on the bench.
Ginsburg also was treated with radiation for a tumor on her pancreas in August 2019. She maintained an active schedule even during the three weeks of radiation. When she revealed a recurrence of her cancer in July 2020, Ginsburg said she remained “fully able” to continue as a justice.
Joan Ruth Bader was born in Brooklyn, New York, in 1933, the second daughter in a middle-class family. Her older sister, who gave her the lifelong nickname “Kiki,” died at age 6, so Ginsburg grew up in Brooklyn’s Flatbush section as an only child. Her dream, she has said, was to be an opera singer.
Ginsburg graduated at the top of her Columbia University law school class in 1959 but could not find a law firm willing to hire her. She had “three strikes against her” — for being Jewish, female and a mother, as she put it in 2007.
She had married her husband, Martin, in 1954, the year she graduated from Cornell University. She attended Harvard University’s law school but transferred to Columbia when her husband took a law job there. Martin Ginsburg went on to become a prominent tax attorney and law professor. Martin Ginsburg died in 2010. She is survived by two children, Jane and James, and several grandchildren.
Ginsburg once said that she had not entered the law as an equal-rights champion. “I thought I could do a lawyer’s job better than any other,” she wrote. “I have no talent in the arts, but I do write fairly well and analyze problems clearly.”


0 notes
Text
Technology Divide Between Senior ‘Haves’ and ‘Have-Nots’ Roils Pandemic Response
Family gatherings on Zoom and FaceTime. Online orders from grocery stores and pharmacies. Telehealth appointments with physicians.
These have been lifesavers for many older adults staying at home during the coronavirus pandemic. But an unprecedented shift to virtual interactions has a downside: Large numbers of seniors are unable to participate.
Among them are older adults with dementia (14% of those 71 and older), hearing loss (nearly two-thirds of those 70 and older) and impaired vision (13.5% of those 65 and older), who can have a hard time using digital devices and programs designed without their needs in mind. (Think small icons, difficult-to-read typefaces, inadequate captioning among the hurdles.)
Many older adults with limited financial resources also may not be able to afford devices or the associated internet service fees. (Half of seniors living alone and 23% of those in two-person households are unable to afford basic necessities.) Others are not adept at using technology and lack the assistance to learn.
During the pandemic, which has hit older adults especially hard, this divide between technology “haves” and “have-nots” has serious consequences.
Older adults in the “haves” group have more access to virtual social interactions and telehealth services, and more opportunities to secure essential supplies online. Meanwhile, the “have-nots” are at greater risk of social isolation, forgoing medical care and being without food or other necessary items.
Dr. Charlotte Yeh, chief medical officer for AARP Services, observed difficulties associated with technology this year when trying to remotely teach her 92-year-old father how to use an iPhone. She lives in Boston; her father lives in Pittsburgh.
Yeh’s mother had always handled communication for the couple, but she was in a nursing home after being hospitalized for pneumonia. Because of the pandemic, the home had closed to visitors. To talk to her and other family members, Yeh’s father had to resort to technology.
But various impairments got in the way: Yeh’s father is blind in one eye, with severe hearing loss and a cochlear implant, and he had trouble hearing conversations over the iPhone. And it was more difficult than Yeh expected to find an easy-to-use iPhone app that accurately translates speech into captions.
Often, family members would try to arrange Zoom meetings. For these, Yeh’s father used a computer but still had problems because he could not read the very small captions on Zoom. A tech-savvy granddaughter solved that problem by connecting a tablet with a separate transcription program.
When Yeh’s mother, who was 90, came home in early April, physicians treating her for metastatic lung cancer wanted to arrange telehealth visits. But this could not occur via cellphone (the screen was too small) or her computer (too hard to move it around). Physicians could examine lesions around the older woman’s mouth only when a tablet was held at just the right angle, with a phone’s flashlight aimed at it for extra light.
“It was like a three-ring circus,” Yeh said. Her family had the resources needed to solve these problems; many do not, she noted. Yeh’s mother passed away in July; her father is now living alone, making him more dependent on technology than ever.
When SCAN Health Plan, a Medicare Advantage plan with 215,000 members in California, surveyed its most vulnerable members after the pandemic hit, it discovered that about one-third did not have access to the technology needed for a telehealth appointment. The Centers for Medicare & Medicaid Services had expanded the use of telehealth in March.
Other barriers also stood in the way of serving SCAN’s members remotely. Many people needed translation services, which are difficult to arrange for telehealth visits. “We realized language barriers are a big thing,” said Eve Gelb, SCAN’s senior vice president of health care services.
Nearly 40% of the plan’s members have vision issues that interfere with their ability to use digital devices; 28% have a clinically significant hearing impairment.
“We need to target interventions to help these people,” Gelb said. SCAN is considering sending community health workers into the homes of vulnerable members to help them conduct telehealth visits. Also, it may give members easy-to-use devices, with essential functions already set up, to keep at home, Gelb said.
Landmark Health serves a highly vulnerable group of 42,000 people in 14 states, bringing services into patients’ homes. Its average patient is nearly 80 years old, with eight medical conditions. After the first few weeks of the pandemic, Landmark halted in-person visits to homes because personal protective equipment, or PPE, was in short supply.
Instead, Landmark tried to deliver care remotely. It soon discovered that fewer than 25% of patients had appropriate technology and knew how to use it, according to Nick Loporcaro, the chief executive officer. “Telehealth is not the panacea, especially for this population,” he said.
Landmark plans to experiment with what he calls “facilitated telehealth”: nonmedical staff members bringing devices to patients’ homes and managing telehealth visits. (It now has enough PPE to make this possible.) And it, too, is looking at technology that it can give to members.
One alternative gaining attention is GrandPad, a tablet loaded with senior-friendly apps designed for adults 75 and older. In July, the National PACE Association, whose members run programs providing comprehensive services to frail seniors who live at home, announced a partnership with GrandPad to encourage adoption of this technology.
“Everyone is scrambling to move to this new remote care model and looking for options,” said Scott Lien, the company’s co-founder and chief executive officer.
PACE Southeast Michigan purchased 125 GrandPads for highly vulnerable members after closing five centers in March where seniors receive services. The devices have been “remarkably successful” in facilitating video-streamed social and telehealth interactions and allowing nurses and social workers to address emerging needs, said Roger Anderson, senior director of operational support and innovation.
Another alternative is technology from iN2L (an acronym for It’s Never Too Late), a company that specializes in serving people with dementia. In Florida, under a new program sponsored by the state’s Department of Elder Affairs, iN2L tablets loaded with dementia-specific content have been distributed to 300 nursing homes and assisted living centers.
The goal is to help seniors with cognitive impairment connect virtually with friends and family and engage in online activities that ease social isolation, said Sam Fazio, senior director of quality care and psychosocial research at the Alzheimer’s Association, a partner in the effort. But because of budget constraints, only two tablets are being sent to each long-term care community.
Families report it can be difficult to schedule adequate time with loved ones when only a few devices are available. This happened to Maitely Weismann’s 77-year-old mother after she moved into a short-staffed Los Angeles memory care facility in March. After seeing how hard it was to connect, Weismann, who lives in Los Angeles, gave her mother an iPad and hired an aide to ensure that mother and daughter were able to talk each night.
Without the aide’s assistance, Weismann’s mother would end up accidentally pausing the video or turning off the device. “She probably wanted to reach out and touch me, and when she touched the screen it would go blank and she’d panic,” Weismann said.
What’s needed going forward? Laurie Orlov, founder of the blog Aging in Place Technology Watch, said nursing homes, assisted living centers and senior communities need to install communitywide Wi-Fi services — something that many lack.
“We need to enable Zoom get-togethers. We need the ability to put voice technology in individual rooms, so people can access Amazon Alexa or Google products,” she said. “We need more group activities that enable multiple residents to communicate with each other virtually. And we need vendors to bundle connectivity, devices, training and service in packages designed for older adults.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Technology Divide Between Senior ‘Haves’ and ‘Have-Nots’ Roils Pandemic Response published first on https://smartdrinkingweb.weebly.com/
0 notes
Text
Technology Divide Between Senior ‘Haves’ and ‘Have-Nots’ Roils Pandemic Response
Family gatherings on Zoom and FaceTime. Online orders from grocery stores and pharmacies. Telehealth appointments with physicians.
These have been lifesavers for many older adults staying at home during the coronavirus pandemic. But an unprecedented shift to virtual interactions has a downside: Large numbers of seniors are unable to participate.
Among them are older adults with dementia (14% of those 71 and older), hearing loss (nearly two-thirds of those 70 and older) and impaired vision (13.5% of those 65 and older), who can have a hard time using digital devices and programs designed without their needs in mind. (Think small icons, difficult-to-read typefaces, inadequate captioning among the hurdles.)
Many older adults with limited financial resources also may not be able to afford devices or the associated internet service fees. (Half of seniors living alone and 23% of those in two-person households are unable to afford basic necessities.) Others are not adept at using technology and lack the assistance to learn.
During the pandemic, which has hit older adults especially hard, this divide between technology “haves” and “have-nots” has serious consequences.
Older adults in the “haves” group have more access to virtual social interactions and telehealth services, and more opportunities to secure essential supplies online. Meanwhile, the “have-nots” are at greater risk of social isolation, forgoing medical care and being without food or other necessary items.
Dr. Charlotte Yeh, chief medical officer for AARP Services, observed difficulties associated with technology this year when trying to remotely teach her 92-year-old father how to use an iPhone. She lives in Boston; her father lives in Pittsburgh.
Yeh’s mother had always handled communication for the couple, but she was in a nursing home after being hospitalized for pneumonia. Because of the pandemic, the home had closed to visitors. To talk to her and other family members, Yeh’s father had to resort to technology.
But various impairments got in the way: Yeh’s father is blind in one eye, with severe hearing loss and a cochlear implant, and he had trouble hearing conversations over the iPhone. And it was more difficult than Yeh expected to find an easy-to-use iPhone app that accurately translates speech into captions.
Often, family members would try to arrange Zoom meetings. For these, Yeh’s father used a computer but still had problems because he could not read the very small captions on Zoom. A tech-savvy granddaughter solved that problem by connecting a tablet with a separate transcription program.
When Yeh’s mother, who was 90, came home in early April, physicians treating her for metastatic lung cancer wanted to arrange telehealth visits. But this could not occur via cellphone (the screen was too small) or her computer (too hard to move it around). Physicians could examine lesions around the older woman’s mouth only when a tablet was held at just the right angle, with a phone’s flashlight aimed at it for extra light.
“It was like a three-ring circus,” Yeh said. Her family had the resources needed to solve these problems; many do not, she noted. Yeh’s mother passed away in July; her father is now living alone, making him more dependent on technology than ever.
When SCAN Health Plan, a Medicare Advantage plan with 215,000 members in California, surveyed its most vulnerable members after the pandemic hit, it discovered that about one-third did not have access to the technology needed for a telehealth appointment. The Centers for Medicare & Medicaid Services had expanded the use of telehealth in March.
Other barriers also stood in the way of serving SCAN’s members remotely. Many people needed translation services, which are difficult to arrange for telehealth visits. “We realized language barriers are a big thing,” said Eve Gelb, SCAN’s senior vice president of health care services.
Nearly 40% of the plan’s members have vision issues that interfere with their ability to use digital devices; 28% have a clinically significant hearing impairment.
“We need to target interventions to help these people,” Gelb said. SCAN is considering sending community health workers into the homes of vulnerable members to help them conduct telehealth visits. Also, it may give members easy-to-use devices, with essential functions already set up, to keep at home, Gelb said.
Landmark Health serves a highly vulnerable group of 42,000 people in 14 states, bringing services into patients’ homes. Its average patient is nearly 80 years old, with eight medical conditions. After the first few weeks of the pandemic, Landmark halted in-person visits to homes because personal protective equipment, or PPE, was in short supply.
Instead, Landmark tried to deliver care remotely. It soon discovered that fewer than 25% of patients had appropriate technology and knew how to use it, according to Nick Loporcaro, the chief executive officer. “Telehealth is not the panacea, especially for this population,” he said.
Landmark plans to experiment with what he calls “facilitated telehealth”: nonmedical staff members bringing devices to patients’ homes and managing telehealth visits. (It now has enough PPE to make this possible.) And it, too, is looking at technology that it can give to members.
One alternative gaining attention is GrandPad, a tablet loaded with senior-friendly apps designed for adults 75 and older. In July, the National PACE Association, whose members run programs providing comprehensive services to frail seniors who live at home, announced a partnership with GrandPad to encourage adoption of this technology.
“Everyone is scrambling to move to this new remote care model and looking for options,” said Scott Lien, the company’s co-founder and chief executive officer.
PACE Southeast Michigan purchased 125 GrandPads for highly vulnerable members after closing five centers in March where seniors receive services. The devices have been “remarkably successful” in facilitating video-streamed social and telehealth interactions and allowing nurses and social workers to address emerging needs, said Roger Anderson, senior director of operational support and innovation.
Another alternative is technology from iN2L (an acronym for It’s Never Too Late), a company that specializes in serving people with dementia. In Florida, under a new program sponsored by the state’s Department of Elder Affairs, iN2L tablets loaded with dementia-specific content have been distributed to 300 nursing homes and assisted living centers.
The goal is to help seniors with cognitive impairment connect virtually with friends and family and engage in online activities that ease social isolation, said Sam Fazio, senior director of quality care and psychosocial research at the Alzheimer’s Association, a partner in the effort. But because of budget constraints, only two tablets are being sent to each long-term care community.
Families report it can be difficult to schedule adequate time with loved ones when only a few devices are available. This happened to Maitely Weismann’s 77-year-old mother after she moved into a short-staffed Los Angeles memory care facility in March. After seeing how hard it was to connect, Weismann, who lives in Los Angeles, gave her mother an iPad and hired an aide to ensure that mother and daughter were able to talk each night.
Without the aide’s assistance, Weismann’s mother would end up accidentally pausing the video or turning off the device. “She probably wanted to reach out and touch me, and when she touched the screen it would go blank and she’d panic,” Weismann said.
What’s needed going forward? Laurie Orlov, founder of the blog Aging in Place Technology Watch, said nursing homes, assisted living centers and senior communities need to install communitywide Wi-Fi services — something that many lack.
“We need to enable Zoom get-togethers. We need the ability to put voice technology in individual rooms, so people can access Amazon Alexa or Google products,” she said. “We need more group activities that enable multiple residents to communicate with each other virtually. And we need vendors to bundle connectivity, devices, training and service in packages designed for older adults.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Technology Divide Between Senior ‘Haves’ and ‘Have-Nots’ Roils Pandemic Response published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Technology Divide Between Senior ‘Haves’ and ‘Have-Nots’ Roils Pandemic Response
Family gatherings on Zoom and FaceTime. Online orders from grocery stores and pharmacies. Telehealth appointments with physicians.
These have been lifesavers for many older adults staying at home during the coronavirus pandemic. But an unprecedented shift to virtual interactions has a downside: Large numbers of seniors are unable to participate.
Among them are older adults with dementia (14% of those 71 and older), hearing loss (nearly two-thirds of those 70 and older) and impaired vision (13.5% of those 65 and older), who can have a hard time using digital devices and programs designed without their needs in mind. (Think small icons, difficult-to-read typefaces, inadequate captioning among the hurdles.)
Many older adults with limited financial resources also may not be able to afford devices or the associated internet service fees. (Half of seniors living alone and 23% of those in two-person households are unable to afford basic necessities.) Others are not adept at using technology and lack the assistance to learn.
During the pandemic, which has hit older adults especially hard, this divide between technology “haves” and “have-nots” has serious consequences.
Older adults in the “haves” group have more access to virtual social interactions and telehealth services, and more opportunities to secure essential supplies online. Meanwhile, the “have-nots” are at greater risk of social isolation, forgoing medical care and being without food or other necessary items.
Dr. Charlotte Yeh, chief medical officer for AARP Services, observed difficulties associated with technology this year when trying to remotely teach her 92-year-old father how to use an iPhone. She lives in Boston; her father lives in Pittsburgh.
Yeh’s mother had always handled communication for the couple, but she was in a nursing home after being hospitalized for pneumonia. Because of the pandemic, the home had closed to visitors. To talk to her and other family members, Yeh’s father had to resort to technology.
But various impairments got in the way: Yeh’s father is blind in one eye, with severe hearing loss and a cochlear implant, and he had trouble hearing conversations over the iPhone. And it was more difficult than Yeh expected to find an easy-to-use iPhone app that accurately translates speech into captions.
Often, family members would try to arrange Zoom meetings. For these, Yeh’s father used a computer but still had problems because he could not read the very small captions on Zoom. A tech-savvy granddaughter solved that problem by connecting a tablet with a separate transcription program.
When Yeh’s mother, who was 90, came home in early April, physicians treating her for metastatic lung cancer wanted to arrange telehealth visits. But this could not occur via cellphone (the screen was too small) or her computer (too hard to move it around). Physicians could examine lesions around the older woman’s mouth only when a tablet was held at just the right angle, with a phone’s flashlight aimed at it for extra light.
“It was like a three-ring circus,” Yeh said. Her family had the resources needed to solve these problems; many do not, she noted. Yeh’s mother passed away in July; her father is now living alone, making him more dependent on technology than ever.
When SCAN Health Plan, a Medicare Advantage plan with 215,000 members in California, surveyed its most vulnerable members after the pandemic hit, it discovered that about one-third did not have access to the technology needed for a telehealth appointment. The Centers for Medicare & Medicaid Services had expanded the use of telehealth in March.
Other barriers also stood in the way of serving SCAN’s members remotely. Many people needed translation services, which are difficult to arrange for telehealth visits. “We realized language barriers are a big thing,” said Eve Gelb, SCAN’s senior vice president of health care services.
Nearly 40% of the plan’s members have vision issues that interfere with their ability to use digital devices; 28% have a clinically significant hearing impairment.
“We need to target interventions to help these people,” Gelb said. SCAN is considering sending community health workers into the homes of vulnerable members to help them conduct telehealth visits. Also, it may give members easy-to-use devices, with essential functions already set up, to keep at home, Gelb said.
Landmark Health serves a highly vulnerable group of 42,000 people in 14 states, bringing services into patients’ homes. Its average patient is nearly 80 years old, with eight medical conditions. After the first few weeks of the pandemic, Landmark halted in-person visits to homes because personal protective equipment, or PPE, was in short supply.
Instead, Landmark tried to deliver care remotely. It soon discovered that fewer than 25% of patients had appropriate technology and knew how to use it, according to Nick Loporcaro, the chief executive officer. “Telehealth is not the panacea, especially for this population,” he said.
Landmark plans to experiment with what he calls “facilitated telehealth”: nonmedical staff members bringing devices to patients’ homes and managing telehealth visits. (It now has enough PPE to make this possible.) And it, too, is looking at technology that it can give to members.
One alternative gaining attention is GrandPad, a tablet loaded with senior-friendly apps designed for adults 75 and older. In July, the National PACE Association, whose members run programs providing comprehensive services to frail seniors who live at home, announced a partnership with GrandPad to encourage adoption of this technology.
“Everyone is scrambling to move to this new remote care model and looking for options,” said Scott Lien, the company’s co-founder and chief executive officer.
PACE Southeast Michigan purchased 125 GrandPads for highly vulnerable members after closing five centers in March where seniors receive services. The devices have been “remarkably successful” in facilitating video-streamed social and telehealth interactions and allowing nurses and social workers to address emerging needs, said Roger Anderson, senior director of operational support and innovation.
Another alternative is technology from iN2L (an acronym for It’s Never Too Late), a company that specializes in serving people with dementia. In Florida, under a new program sponsored by the state’s Department of Elder Affairs, iN2L tablets loaded with dementia-specific content have been distributed to 300 nursing homes and assisted living centers.
The goal is to help seniors with cognitive impairment connect virtually with friends and family and engage in online activities that ease social isolation, said Sam Fazio, senior director of quality care and psychosocial research at the Alzheimer’s Association, a partner in the effort. But because of budget constraints, only two tablets are being sent to each long-term care community.
Families report it can be difficult to schedule adequate time with loved ones when only a few devices are available. This happened to Maitely Weismann’s 77-year-old mother after she moved into a short-staffed Los Angeles memory care facility in March. After seeing how hard it was to connect, Weismann, who lives in Los Angeles, gave her mother an iPad and hired an aide to ensure that mother and daughter were able to talk each night.
Without the aide’s assistance, Weismann’s mother would end up accidentally pausing the video or turning off the device. “She probably wanted to reach out and touch me, and when she touched the screen it would go blank and she’d panic,” Weismann said.
What’s needed going forward? Laurie Orlov, founder of the blog Aging in Place Technology Watch, said nursing homes, assisted living centers and senior communities need to install communitywide Wi-Fi services — something that many lack.
“We need to enable Zoom get-togethers. We need the ability to put voice technology in individual rooms, so people can access Amazon Alexa or Google products,” she said. “We need more group activities that enable multiple residents to communicate with each other virtually. And we need vendors to bundle connectivity, devices, training and service in packages designed for older adults.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
from Updates By Dina https://khn.org/news/technology-divide-between-senior-haves-and-have-nots-roils-pandemic-response/
0 notes
Link
For the first time ever, we’re living in a moment when many of our most promising medical advances are far out of reach for the vast majority of people who could benefit from them. And nowhere is that truer than for cancer immunotherapy, the fast-moving field of cancer treatment research that was honored on Monday with the Nobel Prize in physiology or medicine.
Immunotherapies are a cause for great hope in treating many types of cancer, including melanoma, lymphoma, and lung, kidney, and bladder cancers. They stimulate the immune system to help the body attack cancer from within. And unlike chemotherapy or radiation, which kill off healthy cells in the body, immunotherapies are much more targeted, even in patients with late-stage disease.
With these drugs, doctors have watched deadly tumors melt away, and patients who were supposed to die go into remission for years. And while amazing turnarounds aren’t seen in everyone or for all cancer types, J. Leonard Lichtenfeld, the deputy chief medical officer of the American Cancer Society, told Vox that immunotherapies have oncologists using a word they aren’t used to employing: cure.
“When I was treating patients with melanoma in the 1970s, some of those drugs we used back then are still backbones of treatment for metastatic melanoma 40 years later. Then along came the immunotherapies, and they truly changed the landscape of treatment for these patients,” he says.
But these incredible advances and the promise of cancer cures also come with eye-popping price tags that reach well past $100,000 per patient. People who need cancer immunotherapies often hit a cost wall and can’t afford to pay for them — and it’s a problem that’s growing worse, Ezekiel Emanuel, a professor of medical ethics and health policy at the University of Pennsylvania’s Perelman School of Medicine, told Vox.
“What we’ve seen over the last two decades is the cost of cancer drugs go through the roof. Every year, the introductory price seems higher and higher and higher,” he said. The rising costs of new drugs not only mean that individuals can’t access them; they’re also unsustainable for our health system.
Getting a cancer immunotherapy treatment costs more than a house in many cities in the US, more than putting a few kids through private college. The average cost of cancer drugs has increased from $50,000 per patient in the mid-1990s to $250,000 today. That’s a fivefold increase on inflation. It’s also four times the median US household annual income.
Immunotherapies in particular often cost more than $100,000 per patient. Doctors now use immunotherapies in combination, which means those costs can quickly double or triple. For some of the newest immunotherapies, the price tag is even steeper: When you include the value of the medical support necessary to deliver the treatments, a price tag of $850,000 per patient is not unheard of, according to Emanuel. “The drug companies say that they offer significant discounts to many patients, but because they won’t release this data, the list price is all that we have to go on,” he wrote.
And the list prices have become staggering. This chart from Peter Bach, a researcher with Memorial Sloan Kettering, says it all.
(Keep in mind that the x-axis here is logarithmic, not linear. Scientists sometimes use logarithmic scales to make big number sets manageable. But if Bach had plotted the prices on the x-axis at a linear interval, the cost curve would look much steeper.)
Patients with health insurance can be denied coverage for immunotherapies, even when it’s recommended by their oncologists. When they aren’t, the list prices are so high that the copays can be exorbitant. A patient might face a 25 percent copay, which means they’re getting the drug at a 75 percent discount. When the price tag is upward of $10,000 a month, that leaves patients on the hook to cover at least $2,500 per month. And that’s prohibitive for many people.
This brings us to the next question: Why do these drugs cost so much? To get to the bottom of it, Emanuel posed an interesting thought experiment in a recent Wall Street Journal op-ed. Drug companies typically argue that the cost is related to how much they had to invest in research to develop the drug. The CEO of Novartis, maker of the immunotherapy drug Kymriah, said the R&D costs of the drug were about $1 billion. But Emanuel didn’t buy it:
That’s certainly a big investment, but it is much less astounding when compared with the drug’s anticipated revenue. Based on Kymriah’s list price, treating just 2,700 patients would allow Novartis to recoup its entire investment. Even with significant discounts for many patients, it wouldn’t take many treatments to turn a considerable profit.
… Producing the immunotherapy requires more than three weeks of laboratory manipulations for each individual patient.
But according to researchers at the University of Pennsylvania, the total cost for removing, reprogramming and infusing the cells into each patient is less than $60,000—just one-sixth of the $373,000 price tag. Production costs do not seem to be driving the stratospheric drug prices.
So Emanuel came to the conclusion we have come to at Vox many times: The drugs cost this much because in America, drug companies are allowed to charge that much. And they reap handsome multibillion-dollar profits as a result.
In other countries, governments exert much more influence over the entire health care process. That allows them to negotiate directly with drugmakers. The government sets a maximum price that it will pay for a drug, and if the company doesn’t agree, it simply loses out on the entire market.
The United States, by contrast, has long taken more of a free market approach to drugs. Pharmaceutical companies can haggle over prices with a variety of private insurers as well as selling to the government. What’s more, Medicare, the government program that is the nation’s largest buyer of drugs, is actually barred from negotiating drug prices. That gives pharma much more leverage.
So drug companies here do what any other profit-maximizing company does — they try to get the highest prices possible without going so high that no one will buy them. And that status quo has led to cancer drugs that cost most than homes.
One final disturbing aspect of the cancer cost conundrum: Public money helped pay for many of these drugs that patients can’t afford to access.
In a recent analysis, published in the journal PNAS, researchers found that American tax dollars helped fund the basic research that went into every single one of the drugs approved by the Food and Drug Administration between 2010 and 2016 — including several cancer immunotherapies. All told, $100 billion in National Institutes of Health research grants helped advance the science behind those drugs.
So the Nobel Prize this week is a reminder of the great promise of these drugs — and the incredible, lifesaving science that led to their discoveries. But it should also be a moment to reflect on who is benefiting from them and who isn’t. How will the 1.7 million Americans who are diagnosed with cancer per year gain access if prices keep rising and we don’t address this cost conundrum soon?
Original Source -> The Nobel Prize is a reminder of the outrageous cost of curing cancer
via The Conservative Brief
0 notes
Text
West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options
West Virginia Mesothelioma Doctors
The State Of West Virginia Mesothelioma Doctors, Cancer Centers, and Treatment
Mesothelioma, Asbestosis, & Lung Cancer patients who reside in West Virginia have access to the leading West Virginia Mesothelioma doctors and treatment throughout the state. In West Virginia mesothelioma treatment which includes surgery, radiation, and chemotherapy are now available for Conventional mesothelioma. Also, we get to have clinical trials recruiting pleural and peritoneal mesothelioma patients in all of West Virginia.
In this article, you get to see the top West Virginia mesothelioma doctors who are practicing in the whole of West Virginia being the top West Virginia cancer centers in the state. Also, for your conveniences, there has been local cancer support which has been made available.
West Virginia Mesothelioma Cancer Centers
Below is the list of health care options in West Virginia which you can learn from West Virginia mesothelioma Cancer Centers. Mesothelioma cancers centers are available in West Virginia where you can get the best quality cancer treatment, and tend to get more detailed information about these cancer centers is made available when you visit the cancer center appropriate link.
Mary Babb Randolph Cancer Center
Morgantown, WV
The West Virginia University School of Medicine in Morgantown has the Mary Randolph Cancer Center which specializes in the treatment of mesothelioma, lung diseases, as well as the thoracic cancers. If you need help contacting the Cancer center contact one of our West Virginia Mesothelioma Lawyers
Here is list of the top Mesothelioma Doctors in West Virginia
This list comprises of the best doctors who specialize in treating mesothelioma in the state of West Virginia. West Virginia mesothelioma doctors typically have years of experience. By clicking on each of the doctor’s names you get to have the information about their area of expertise, profession affiliations, background, and their office locations.
Dr. Nepal C. Chowdhury
Thoracic Surgeon
St. Mary’s Medical Center
St. Mary’s Cardiovascular and Thoracic Surgery
Huntington, WV 25702
(304) 399-7530
This doctor is a certified thoracic surgeon who currently practices at the Cabel Huntington Hospital located in Huntington, West Virginia. He does specialize in the general thoracic Surgery and Peripheral Vascular Surgery.
Dr. Rebecca S. Wolfer
Thoracic Surgeon
Marshall Health-Surgery
Huntington, WV 25701
(304) 691-1200
As a certified doctor in both general surgery and general cardiothoracic surgery, Dr. Rebecca S. Wolfer is an associate professor in the department of Surgery at the Joan C. Edwards School of Medicine at Marshall University. A West Virginia Mesothelioma Doctor can be very helpful, let one of our West Virginia mesothelioma attorneys help you find
Most patients do travel out of their current states just to meet the best oncologist and thoracic surgeons across the country, and note that all these mesothelioma experts do have particular focus within their practice.
Here is the list of Top Mesothelioma Doctors in the Country
Paul H. Sugarbaker, M.D.
Gastrointestinal Surgical Oncologist
Washington Cancer Institute
Dr. Paul H. Sugarbaker, FACS, FRCS graduated from Cornell University Medical College in New York City and received his surgical training at the Peter Bent Brigham Hospital in Boston, a Harvard University affiliated program. There he also received a Masters Degree in Immunology at the Harvard School of Arts and Sciences. In 1976 he accepted a position at the National Institutes of Health/ National Cancer Institute – Surgery Branch, as Senior Investigator until 1986. Subsequently, after a brief stay at the Emory Clinic in Atlanta, Georgia he moved back to Washington, DC to become the Medical Director of the Washington Cancer Institute at MedStar Washington Hospital Center in 1989. Currently, he is the Chief of the Peritoneal Surface Malignancy Program and the Director of the Center for Gastrointestinal Malignancies at the Washington Hospital Center in Washington, DC. His interests are focused exclusively on gastrointestinal cancer, gynecologic malignancy, and peritoneal mesothelioma of the abdomen – all malignancies which usually present with cancerous spread to the abdominal cavity. Currently, his clinical and investigative work is concentrated on the treatment of the peritoneal surface dissemination of cancers, referred to as PERITONEAL METASTASES, also known as peritoneal carcinomatosis. He has developed, perfected and popularized the combined treatments of cancer surgery with warm chemotherapy, infused into the open abdomen towards the end the surgical intervention. His mantra, “It’s what the surgeon doesn’t see that kills the patient,” summarizes his thinking as he realizes the limitations of surgery alone, and the limitations of systemic or regional chemotherapy alone. It turns out that the combined application of both the surgical removal of the tumors and the regional treatment directly into the open abdomen where the tumors are located, is especially effective in selected patients. This treatment option and its results have been published extensively in the peer-reviewed literature and in the lay press. Further work to supplement these treatments and to make them even more effective by adding systemic chemo infusions: Perioperative intravenous and intraperitoneal chemotherapy (HIPEC and EPIC} are an essential planned part of these combined surgical and regional chemotherapy interventions. Over the many years he has published over 900 articles and book chapters, edited 7 books, produced 24 videos, and received 4 honorary professorships. He has traveled to all 5 continents to make these treatments available to patients all over the world.
Claire Verschraegen, M.D.
Medical Oncologist
James Cancer Hospital and Solove Research Institute
Verschraegen is a board-certified oncologist who has worked with mesothelioma, metastatic melanomas, sarcomas, gynecologic malignancies and other uncommon cancers. She also has worked with new anti-cancer drugs and treatments of solid tumors, always stressing the importance of clinical trials to help improve therapies.
Before coming to Ohio, she was a tenured professor of medicine in the Division of Hematology and Oncology at UNM, serving as director of the Translational Therapeutics and Clinical Research Program. She oversaw the Clinical Protocol and Data Management Core at the UNM Cancer Center.
She was the principal investigator for the minority-based Community Clinical Oncology Program, which opened NCI-sponsored clinical trials to anyone in the state who wished to participate.
She earned her Medical Degree at the University Libre de Bruxelles in Belgium and trained at the Institute Bordet. She went to Texas for her Medical Oncology fellowship at M.D. Anderson Cancer Center, where she eventually joined the faculty.
QUICK FACT
Before joining UVM, Dr. Verschraegen oversaw a Clinical Protocol and Data Management Program for the University of New Mexico’s Cancer Center.
It was in New Mexico when she did one often-cited study that evaluated the anti-mesothelin immunotoxin SS1 (dsFv) PE38 in fresh tumor cells of peritoneal mesothelioma patients. She also conducted several trials involving a variety of drug combinations that were successful for specific cancers.
Her work with rare cancers has been well respected and well received nationally. Her academic writing includes 10 book chapters, 80 peer-reviewed medical papers and 20 invited papers. She is a former member of the Scientific Board for the Mesothelioma Applied Research Foundation.
The Cancer Support Center of The State of West Virginia
Mesothelioma patients can enjoy transport, temporary housing, counselling, and physical therapy from the cancer support service of the state of West Virginia. While receiving treatments for mesothelioma in West Virginia all these local services may be of help to the patients receiving the treatment.
West Virginia Mesothelioma Treatment Support Services
Counseling & Support Groups
Cabell Huntington Hospital
(Huntington)
304-526-2000
WV University Healthcare
(Martinsburg)
304-264-1000
Long-Term Housing
CAMC Foundation Hospitality House
(Charleston)
304-388-9870
The Davis House
(Elkins)
304-630-3043
Rosenbaum Family House
(Morgantown)
304-598-6094
Patient Transport
Mountain State Transport
(Clarksburg)
304-624-0800
Hometown Transportation
(Moundsville)
304-845-6070
MTM
(Charleston)
844-549-8353
Physical Therapy
St. Mary’s Outpatient Rehabilitation Services
(Huntington)
304-526-1333
Pivot Physical Therapy
(Shepherdstown)
304-876-8600
Advanced Physical Therapy
(Charleston)
304-720-9185
Mesothelioma Treatment Cost
Treating the mesothelioma cancer can be a very expensive proposition and also when receiving related treatment cost can easily add up. Also, when dealing with cancer people tends to take time off from their daily job.
Below is the estimated cost for a number of common procedures used in the diagnosing as well as the treatment of mesothelioma.
West Virginia Mesothelioma Doctors, Cancer Centers and Treatment
Mesothelioma patients living in West Virginia have access to quality mesothelioma treatment in state. Conventional mesothelioma treatments available in West Virginia include surgery, chemotherapy, and radiation. Additionally, clinical trials may currently be recruiting pleural and peritoneal mesothelioma patients in West Virginia. West Virginia Mesothelioma doctors are here for you.
We provide a list of top mesothelioma doctors practicing in West Virginia as well as the top cancer care centers in the state. Local cancer support services have been included as well for your convenience. Learn more about health care options available in West Virginia below.
West Virginia Mesothelioma Statistics
428
Mesothelioma Deaths, 1999 – 2015
161
Asbestosis Deaths, 1999 – 2015
589
Total Deaths, 1999 – 2015
Need help Contacting a West Virginia Mesothelioma Doctor?
It is not uncommon for patients to travel outside of their current states to meet with top oncologists and thoracic surgeons across the country. These mesothelioma experts usually have a particular focus within their practice.
Help with Mesothelioma Treatment Costs
Mesothelioma treatment can be a very expensive proposition and all of the different treatment related costs can add up quickly. Additionally, many people may need to take time off from work to deal with their cancer diagnosis. A West Virginia asbestos attorney can help you.
The table below provides cost estimates for a number of common procedures used in diagnosing and treating mesothelioma. A Pennsylvania mesothelioma lawyer can be of great help to patients in Pennsylvania. Work with Americas leading mesothelioma law firm, mesothelioma lawyers, and mesothelioma attorneys at GPW. A Michigan mesothelioma doctor can be very useful to those diagnosed in Michigan.
Common Costs Associated with Treating Mesothelioma
Mesothelioma Diagnosis & Treatment Costs: Approximate Cost Range
Diagnostic Imaging (CT, PET, MRI): $800 – $1,600 per scan
Needle Biopsy: $500 – $700
Thoracoscopy or Pleuroscopy (lungs) or Laparoscopy (abdomen): $3,600 – $5,000
Thoracotomy (lungs) or Laparotomy (abdomen): $7,800 – $7,900
Surgery – Lobectomy/Pneumonectomy (removal of part or all of a lung): $13,000 – $17,000
Radiation: $7,000 – $12,000
Chemotherapy – Pemetrexed (Alimta®): $37,000 – $50,000
Hyperthermic Intraperitoneal Chemotherapy (HIPEC): $700 – $1,000
The above cost does not factor in the insurance payments as well as reimbursements. The above estimated cost was taken from the Fair Health Consumer Cost Look up tool, bluebook, and some other sources to determine the actual cost for the specific procedures. West Virginia mesothelioma doctors can be very helpful.
How to file an Asbestos Exposure Claim
Ensure not to lose your right to file a claim. Are you or your loved ones been diagnosed with mesothelioma and you are exposed to asbestos in West Virginia, then you may be entitled to some compensation. You will need to file your claim to the right statute for limitations for the state of West Virginia. West Virginia Mesothelioma doctors can be of great help to you. Speak with a West Virginia Asbestos attorney at GPW.
The post West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options appeared first on Goldberg, Persky & White P.C..
source https://www.gpwlaw-mi.com/west-virginia-mesothelioma-doctors from America's Top Mesothelioma Lawyer https://gpwlawmimesotheliomalawfirm.tumblr.com/post/171087016067
0 notes
Text
West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options
West Virginia Mesothelioma Doctors
The State Of West Virginia Mesothelioma Doctors, Cancer Centers, and Treatment
Mesothelioma, Asbestosis, & Lung Cancer patients who reside in West Virginia have access to the leading West Virginia Mesothelioma doctors and treatment throughout the state. In West Virginia mesothelioma treatment which includes surgery, radiation, and chemotherapy are now available for Conventional mesothelioma. Also, we get to have clinical trials recruiting pleural and peritoneal mesothelioma patients in all of West Virginia.
In this article, you get to see the top West Virginia mesothelioma doctors who are practicing in the whole of West Virginia being the top West Virginia cancer centers in the state. Also, for your conveniences, there has been local cancer support which has been made available.
West Virginia Mesothelioma Cancer Centers
Below is the list of health care options in West Virginia which you can learn from West Virginia mesothelioma Cancer Centers. Mesothelioma cancers centers are available in West Virginia where you can get the best quality cancer treatment, and tend to get more detailed information about these cancer centers is made available when you visit the cancer center appropriate link.
Mary Babb Randolph Cancer Center
Morgantown, WV
The West Virginia University School of Medicine in Morgantown has the Mary Randolph Cancer Center which specializes in the treatment of mesothelioma, lung diseases, as well as the thoracic cancers. If you need help contacting the Cancer center contact one of our West Virginia Mesothelioma Lawyers
Here is list of the top Mesothelioma Doctors in West Virginia
This list comprises of the best doctors who specialize in treating mesothelioma in the state of West Virginia. West Virginia mesothelioma doctors typically have years of experience. By clicking on each of the doctor’s names you get to have the information about their area of expertise, profession affiliations, background, and their office locations.
Dr. Nepal C. Chowdhury
Thoracic Surgeon
St. Mary’s Medical Center
St. Mary’s Cardiovascular and Thoracic Surgery
Huntington, WV 25702
(304) 399-7530
This doctor is a certified thoracic surgeon who currently practices at the Cabel Huntington Hospital located in Huntington, West Virginia. He does specialize in the general thoracic Surgery and Peripheral Vascular Surgery.
Dr. Rebecca S. Wolfer
Thoracic Surgeon
Marshall Health-Surgery
Huntington, WV 25701
(304) 691-1200
As a certified doctor in both general surgery and general cardiothoracic surgery, Dr. Rebecca S. Wolfer is an associate professor in the department of Surgery at the Joan C. Edwards School of Medicine at Marshall University. A West Virginia Mesothelioma Doctor can be very helpful, let one of our West Virginia mesothelioma attorneys help you find
Most patients do travel out of their current states just to meet the best oncologist and thoracic surgeons across the country, and note that all these mesothelioma experts do have particular focus within their practice.
Here is the list of Top Mesothelioma Doctors in the Country
Paul H. Sugarbaker, M.D.
Gastrointestinal Surgical Oncologist
Washington Cancer Institute
Dr. Paul H. Sugarbaker, FACS, FRCS graduated from Cornell University Medical College in New York City and received his surgical training at the Peter Bent Brigham Hospital in Boston, a Harvard University affiliated program. There he also received a Masters Degree in Immunology at the Harvard School of Arts and Sciences. In 1976 he accepted a position at the National Institutes of Health/ National Cancer Institute – Surgery Branch, as Senior Investigator until 1986. Subsequently, after a brief stay at the Emory Clinic in Atlanta, Georgia he moved back to Washington, DC to become the Medical Director of the Washington Cancer Institute at MedStar Washington Hospital Center in 1989. Currently, he is the Chief of the Peritoneal Surface Malignancy Program and the Director of the Center for Gastrointestinal Malignancies at the Washington Hospital Center in Washington, DC. His interests are focused exclusively on gastrointestinal cancer, gynecologic malignancy, and peritoneal mesothelioma of the abdomen – all malignancies which usually present with cancerous spread to the abdominal cavity. Currently, his clinical and investigative work is concentrated on the treatment of the peritoneal surface dissemination of cancers, referred to as PERITONEAL METASTASES, also known as peritoneal carcinomatosis. He has developed, perfected and popularized the combined treatments of cancer surgery with warm chemotherapy, infused into the open abdomen towards the end the surgical intervention. His mantra, “It’s what the surgeon doesn’t see that kills the patient,” summarizes his thinking as he realizes the limitations of surgery alone, and the limitations of systemic or regional chemotherapy alone. It turns out that the combined application of both the surgical removal of the tumors and the regional treatment directly into the open abdomen where the tumors are located, is especially effective in selected patients. This treatment option and its results have been published extensively in the peer-reviewed literature and in the lay press. Further work to supplement these treatments and to make them even more effective by adding systemic chemo infusions: Perioperative intravenous and intraperitoneal chemotherapy (HIPEC and EPIC} are an essential planned part of these combined surgical and regional chemotherapy interventions. Over the many years he has published over 900 articles and book chapters, edited 7 books, produced 24 videos, and received 4 honorary professorships. He has traveled to all 5 continents to make these treatments available to patients all over the world.
Claire Verschraegen, M.D.
Medical Oncologist
James Cancer Hospital and Solove Research Institute
Verschraegen is a board-certified oncologist who has worked with mesothelioma, metastatic melanomas, sarcomas, gynecologic malignancies and other uncommon cancers. She also has worked with new anti-cancer drugs and treatments of solid tumors, always stressing the importance of clinical trials to help improve therapies.
Before coming to Ohio, she was a tenured professor of medicine in the Division of Hematology and Oncology at UNM, serving as director of the Translational Therapeutics and Clinical Research Program. She oversaw the Clinical Protocol and Data Management Core at the UNM Cancer Center.
She was the principal investigator for the minority-based Community Clinical Oncology Program, which opened NCI-sponsored clinical trials to anyone in the state who wished to participate.
She earned her Medical Degree at the University Libre de Bruxelles in Belgium and trained at the Institute Bordet. She went to Texas for her Medical Oncology fellowship at M.D. Anderson Cancer Center, where she eventually joined the faculty.
QUICK FACT
Before joining UVM, Dr. Verschraegen oversaw a Clinical Protocol and Data Management Program for the University of New Mexico’s Cancer Center.
It was in New Mexico when she did one often-cited study that evaluated the anti-mesothelin immunotoxin SS1 (dsFv) PE38 in fresh tumor cells of peritoneal mesothelioma patients. She also conducted several trials involving a variety of drug combinations that were successful for specific cancers.
Her work with rare cancers has been well respected and well received nationally. Her academic writing includes 10 book chapters, 80 peer-reviewed medical papers and 20 invited papers. She is a former member of the Scientific Board for the Mesothelioma Applied Research Foundation.
The Cancer Support Center of The State of West Virginia
Mesothelioma patients can enjoy transport, temporary housing, counselling, and physical therapy from the cancer support service of the state of West Virginia. While receiving treatments for mesothelioma in West Virginia all these local services may be of help to the patients receiving the treatment.
West Virginia Mesothelioma Treatment Support Services
Counseling & Support Groups
Cabell Huntington Hospital
(Huntington)
304-526-2000
WV University Healthcare
(Martinsburg)
304-264-1000
Long-Term Housing
CAMC Foundation Hospitality House
(Charleston)
304-388-9870
The Davis House
(Elkins)
304-630-3043
Rosenbaum Family House
(Morgantown)
304-598-6094
Patient Transport
Mountain State Transport
(Clarksburg)
304-624-0800
Hometown Transportation
(Moundsville)
304-845-6070
MTM
(Charleston)
844-549-8353
Physical Therapy
St. Mary’s Outpatient Rehabilitation Services
(Huntington)
304-526-1333
Pivot Physical Therapy
(Shepherdstown)
304-876-8600
Advanced Physical Therapy
(Charleston)
304-720-9185
Mesothelioma Treatment Cost
Treating the mesothelioma cancer can be a very expensive proposition and also when receiving related treatment cost can easily add up. Also, when dealing with cancer people tends to take time off from their daily job.
Below is the estimated cost for a number of common procedures used in the diagnosing as well as the treatment of mesothelioma.
West Virginia Mesothelioma Doctors, Cancer Centers and Treatment
Mesothelioma patients living in West Virginia have access to quality mesothelioma treatment in state. Conventional mesothelioma treatments available in West Virginia include surgery, chemotherapy, and radiation. Additionally, clinical trials may currently be recruiting pleural and peritoneal mesothelioma patients in West Virginia. West Virginia Mesothelioma doctors are here for you.
We provide a list of top mesothelioma doctors practicing in West Virginia as well as the top cancer care centers in the state. Local cancer support services have been included as well for your convenience. Learn more about health care options available in West Virginia below.
West Virginia Mesothelioma Statistics
428
Mesothelioma Deaths, 1999 – 2015
161
Asbestosis Deaths, 1999 – 2015
589
Total Deaths, 1999 – 2015
Need help Contacting a West Virginia Mesothelioma Doctor?
It is not uncommon for patients to travel outside of their current states to meet with top oncologists and thoracic surgeons across the country. These mesothelioma experts usually have a particular focus within their practice.
Help with Mesothelioma Treatment Costs
Mesothelioma treatment can be a very expensive proposition and all of the different treatment related costs can add up quickly. Additionally, many people may need to take time off from work to deal with their cancer diagnosis. A West Virginia asbestos attorney can help you.
The table below provides cost estimates for a number of common procedures used in diagnosing and treating mesothelioma. A Pennsylvania mesothelioma lawyer can be of great help to patients in Pennsylvania. Work with Americas leading mesothelioma law firm, mesothelioma lawyers, and mesothelioma attorneys at GPW. A Michigan mesothelioma doctor can be very useful to those diagnosed in Michigan.
Common Costs Associated with Treating Mesothelioma
Mesothelioma Diagnosis & Treatment Costs: Approximate Cost Range
Diagnostic Imaging (CT, PET, MRI): $800 – $1,600 per scan
Needle Biopsy: $500 – $700
Thoracoscopy or Pleuroscopy (lungs) or Laparoscopy (abdomen): $3,600 – $5,000
Thoracotomy (lungs) or Laparotomy (abdomen): $7,800 – $7,900
Surgery – Lobectomy/Pneumonectomy (removal of part or all of a lung): $13,000 – $17,000
Radiation: $7,000 – $12,000
Chemotherapy – Pemetrexed (Alimta®): $37,000 – $50,000
Hyperthermic Intraperitoneal Chemotherapy (HIPEC): $700 – $1,000
The above cost does not factor in the insurance payments as well as reimbursements. The above estimated cost was taken from the Fair Health Consumer Cost Look up tool, bluebook, and some other sources to determine the actual cost for the specific procedures. West Virginia mesothelioma doctors can be very helpful.
How to file an Asbestos Exposure Claim
Ensure not to lose your right to file a claim. Are you or your loved ones been diagnosed with mesothelioma and you are exposed to asbestos in West Virginia, then you may be entitled to some compensation. You will need to file your claim to the right statute for limitations for the state of West Virginia. West Virginia Mesothelioma doctors can be of great help to you. Speak with a West Virginia Asbestos attorney at GPW.
The post West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options appeared first on Goldberg, Persky & White P.C..
source https://www.gpwlaw-mi.com/west-virginia-mesothelioma-doctors from Top Mesothelioma Law Firm http://gpwlawmi.blogspot.com/2018/02/west-virginia-mesothelioma-doctors.html
0 notes
Text
West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options
West Virginia Mesothelioma Doctors
The State Of West Virginia Mesothelioma Doctors, Cancer Centers, and Treatment
Mesothelioma, Asbestosis, & Lung Cancer patients who reside in West Virginia have access to the leading West Virginia Mesothelioma doctors and treatment throughout the state. In West Virginia mesothelioma treatment which includes surgery, radiation, and chemotherapy are now available for Conventional mesothelioma. Also, we get to have clinical trials recruiting pleural and peritoneal mesothelioma patients in all of West Virginia.
In this article, you get to see the top West Virginia mesothelioma doctors who are practicing in the whole of West Virginia being the top West Virginia cancer centers in the state. Also, for your conveniences, there has been local cancer support which has been made available.
West Virginia Mesothelioma Cancer Centers
Below is the list of health care options in West Virginia which you can learn from West Virginia mesothelioma Cancer Centers. Mesothelioma cancers centers are available in West Virginia where you can get the best quality cancer treatment, and tend to get more detailed information about these cancer centers is made available when you visit the cancer center appropriate link.
Mary Babb Randolph Cancer Center
Morgantown, WV
The West Virginia University School of Medicine in Morgantown has the Mary Randolph Cancer Center which specializes in the treatment of mesothelioma, lung diseases, as well as the thoracic cancers. If you need help contacting the Cancer center contact one of our West Virginia Mesothelioma Lawyers
Here is list of the top Mesothelioma Doctors in West Virginia
This list comprises of the best doctors who specialize in treating mesothelioma in the state of West Virginia. West Virginia mesothelioma doctors typically have years of experience. By clicking on each of the doctor’s names you get to have the information about their area of expertise, profession affiliations, background, and their office locations.
Dr. Nepal C. Chowdhury
Thoracic Surgeon
St. Mary’s Medical Center
St. Mary’s Cardiovascular and Thoracic Surgery
Huntington, WV 25702
(304) 399-7530
This doctor is a certified thoracic surgeon who currently practices at the Cabel Huntington Hospital located in Huntington, West Virginia. He does specialize in the general thoracic Surgery and Peripheral Vascular Surgery.
Dr. Rebecca S. Wolfer
Thoracic Surgeon
Marshall Health-Surgery
Huntington, WV 25701
(304) 691-1200
As a certified doctor in both general surgery and general cardiothoracic surgery, Dr. Rebecca S. Wolfer is an associate professor in the department of Surgery at the Joan C. Edwards School of Medicine at Marshall University. A West Virginia Mesothelioma Doctor can be very helpful, let one of our West Virginia mesothelioma attorneys help you find
Most patients do travel out of their current states just to meet the best oncologist and thoracic surgeons across the country, and note that all these mesothelioma experts do have particular focus within their practice.
Here is the list of Top Mesothelioma Doctors in the Country
Paul H. Sugarbaker, M.D.
Gastrointestinal Surgical Oncologist
Washington Cancer Institute
Dr. Paul H. Sugarbaker, FACS, FRCS graduated from Cornell University Medical College in New York City and received his surgical training at the Peter Bent Brigham Hospital in Boston, a Harvard University affiliated program. There he also received a Masters Degree in Immunology at the Harvard School of Arts and Sciences. In 1976 he accepted a position at the National Institutes of Health/ National Cancer Institute – Surgery Branch, as Senior Investigator until 1986. Subsequently, after a brief stay at the Emory Clinic in Atlanta, Georgia he moved back to Washington, DC to become the Medical Director of the Washington Cancer Institute at MedStar Washington Hospital Center in 1989. Currently, he is the Chief of the Peritoneal Surface Malignancy Program and the Director of the Center for Gastrointestinal Malignancies at the Washington Hospital Center in Washington, DC. His interests are focused exclusively on gastrointestinal cancer, gynecologic malignancy, and peritoneal mesothelioma of the abdomen – all malignancies which usually present with cancerous spread to the abdominal cavity. Currently, his clinical and investigative work is concentrated on the treatment of the peritoneal surface dissemination of cancers, referred to as PERITONEAL METASTASES, also known as peritoneal carcinomatosis. He has developed, perfected and popularized the combined treatments of cancer surgery with warm chemotherapy, infused into the open abdomen towards the end the surgical intervention. His mantra, “It’s what the surgeon doesn’t see that kills the patient,” summarizes his thinking as he realizes the limitations of surgery alone, and the limitations of systemic or regional chemotherapy alone. It turns out that the combined application of both the surgical removal of the tumors and the regional treatment directly into the open abdomen where the tumors are located, is especially effective in selected patients. This treatment option and its results have been published extensively in the peer-reviewed literature and in the lay press. Further work to supplement these treatments and to make them even more effective by adding systemic chemo infusions: Perioperative intravenous and intraperitoneal chemotherapy (HIPEC and EPIC} are an essential planned part of these combined surgical and regional chemotherapy interventions. Over the many years he has published over 900 articles and book chapters, edited 7 books, produced 24 videos, and received 4 honorary professorships. He has traveled to all 5 continents to make these treatments available to patients all over the world.
Claire Verschraegen, M.D.
Medical Oncologist
James Cancer Hospital and Solove Research Institute
Verschraegen is a board-certified oncologist who has worked with mesothelioma, metastatic melanomas, sarcomas, gynecologic malignancies and other uncommon cancers. She also has worked with new anti-cancer drugs and treatments of solid tumors, always stressing the importance of clinical trials to help improve therapies.
Before coming to Ohio, she was a tenured professor of medicine in the Division of Hematology and Oncology at UNM, serving as director of the Translational Therapeutics and Clinical Research Program. She oversaw the Clinical Protocol and Data Management Core at the UNM Cancer Center.
She was the principal investigator for the minority-based Community Clinical Oncology Program, which opened NCI-sponsored clinical trials to anyone in the state who wished to participate.
She earned her Medical Degree at the University Libre de Bruxelles in Belgium and trained at the Institute Bordet. She went to Texas for her Medical Oncology fellowship at M.D. Anderson Cancer Center, where she eventually joined the faculty.
QUICK FACT
Before joining UVM, Dr. Verschraegen oversaw a Clinical Protocol and Data Management Program for the University of New Mexico’s Cancer Center.
It was in New Mexico when she did one often-cited study that evaluated the anti-mesothelin immunotoxin SS1 (dsFv) PE38 in fresh tumor cells of peritoneal mesothelioma patients. She also conducted several trials involving a variety of drug combinations that were successful for specific cancers.
Her work with rare cancers has been well respected and well received nationally. Her academic writing includes 10 book chapters, 80 peer-reviewed medical papers and 20 invited papers. She is a former member of the Scientific Board for the Mesothelioma Applied Research Foundation.
The Cancer Support Center of The State of West Virginia
Mesothelioma patients can enjoy transport, temporary housing, counselling, and physical therapy from the cancer support service of the state of West Virginia. While receiving treatments for mesothelioma in West Virginia all these local services may be of help to the patients receiving the treatment.
West Virginia Mesothelioma Treatment Support Services
Counseling & Support Groups
Cabell Huntington Hospital
(Huntington)
304-526-2000
WV University Healthcare
(Martinsburg)
304-264-1000
Long-Term Housing
CAMC Foundation Hospitality House
(Charleston)
304-388-9870
The Davis House
(Elkins)
304-630-3043
Rosenbaum Family House
(Morgantown)
304-598-6094
Patient Transport
Mountain State Transport
(Clarksburg)
304-624-0800
Hometown Transportation
(Moundsville)
304-845-6070
MTM
(Charleston)
844-549-8353
Physical Therapy
St. Mary’s Outpatient Rehabilitation Services
(Huntington)
304-526-1333
Pivot Physical Therapy
(Shepherdstown)
304-876-8600
Advanced Physical Therapy
(Charleston)
304-720-9185
Mesothelioma Treatment Cost
Treating the mesothelioma cancer can be a very expensive proposition and also when receiving related treatment cost can easily add up. Also, when dealing with cancer people tends to take time off from their daily job.
Below is the estimated cost for a number of common procedures used in the diagnosing as well as the treatment of mesothelioma.
West Virginia Mesothelioma Doctors, Cancer Centers and Treatment
Mesothelioma patients living in West Virginia have access to quality mesothelioma treatment in state. Conventional mesothelioma treatments available in West Virginia include surgery, chemotherapy, and radiation. Additionally, clinical trials may currently be recruiting pleural and peritoneal mesothelioma patients in West Virginia. West Virginia Mesothelioma doctors are here for you.
We provide a list of top mesothelioma doctors practicing in West Virginia as well as the top cancer care centers in the state. Local cancer support services have been included as well for your convenience. Learn more about health care options available in West Virginia below.
West Virginia Mesothelioma Statistics
428
Mesothelioma Deaths, 1999 – 2015
161
Asbestosis Deaths, 1999 – 2015
589
Total Deaths, 1999 – 2015
Need help Contacting a West Virginia Mesothelioma Doctor?
It is not uncommon for patients to travel outside of their current states to meet with top oncologists and thoracic surgeons across the country. These mesothelioma experts usually have a particular focus within their practice.
Help with Mesothelioma Treatment Costs
Mesothelioma treatment can be a very expensive proposition and all of the different treatment related costs can add up quickly. Additionally, many people may need to take time off from work to deal with their cancer diagnosis. A West Virginia asbestos attorney can help you.
The table below provides cost estimates for a number of common procedures used in diagnosing and treating mesothelioma. A Pennsylvania mesothelioma lawyer can be of great help to patients in Pennsylvania. Work with Americas leading mesothelioma law firm, mesothelioma lawyers, and mesothelioma attorneys at GPW. A Michigan mesothelioma doctor can be very useful to those diagnosed in Michigan.
Common Costs Associated with Treating Mesothelioma
Mesothelioma Diagnosis & Treatment Costs: Approximate Cost Range
Diagnostic Imaging (CT, PET, MRI): $800 – $1,600 per scan
Needle Biopsy: $500 – $700
Thoracoscopy or Pleuroscopy (lungs) or Laparoscopy (abdomen): $3,600 – $5,000
Thoracotomy (lungs) or Laparotomy (abdomen): $7,800 – $7,900
Surgery – Lobectomy/Pneumonectomy (removal of part or all of a lung): $13,000 – $17,000
Radiation: $7,000 – $12,000
Chemotherapy – Pemetrexed (Alimta®): $37,000 – $50,000
Hyperthermic Intraperitoneal Chemotherapy (HIPEC): $700 – $1,000
The above cost does not factor in the insurance payments as well as reimbursements. The above estimated cost was taken from the Fair Health Consumer Cost Look up tool, bluebook, and some other sources to determine the actual cost for the specific procedures. West Virginia mesothelioma doctors can be very helpful.
How to file an Asbestos Exposure Claim
Ensure not to lose your right to file a claim. Are you or your loved ones been diagnosed with mesothelioma and you are exposed to asbestos in West Virginia, then you may be entitled to some compensation. You will need to file your claim to the right statute for limitations for the state of West Virginia. West Virginia Mesothelioma doctors can be of great help to you. Speak with a West Virginia Asbestos attorney at GPW.
The post West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options appeared first on Goldberg, Persky & White P.C..
source https://www.gpwlaw-mi.com/west-virginia-mesothelioma-doctors from America's Top Mesothelioma Lawyer http://gpwlaw-mimesotheliomalawfirm.blogspot.com/2018/02/west-virginia-mesothelioma-doctors.html
0 notes
Text
West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options
West Virginia Mesothelioma Doctors
The State Of West Virginia Mesothelioma Doctors, Cancer Centers, and Treatment
Mesothelioma, Asbestosis, & Lung Cancer patients who reside in West Virginia have access to the leading West Virginia Mesothelioma doctors and treatment throughout the state. In West Virginia mesothelioma treatment which includes surgery, radiation, and chemotherapy are now available for Conventional mesothelioma. Also, we get to have clinical trials recruiting pleural and peritoneal mesothelioma patients in all of West Virginia.
In this article, you get to see the top West Virginia mesothelioma doctors who are practicing in the whole of West Virginia being the top West Virginia cancer centers in the state. Also, for your conveniences, there has been local cancer support which has been made available.
West Virginia Mesothelioma Cancer Centers
Below is the list of health care options in West Virginia which you can learn from West Virginia mesothelioma Cancer Centers. Mesothelioma cancers centers are available in West Virginia where you can get the best quality cancer treatment, and tend to get more detailed information about these cancer centers is made available when you visit the cancer center appropriate link.
Mary Babb Randolph Cancer Center
Morgantown, WV
The West Virginia University School of Medicine in Morgantown has the Mary Randolph Cancer Center which specializes in the treatment of mesothelioma, lung diseases, as well as the thoracic cancers. If you need help contacting the Cancer center contact one of our West Virginia Mesothelioma Lawyers
Here is list of the top Mesothelioma Doctors in West Virginia
This list comprises of the best doctors who specialize in treating mesothelioma in the state of West Virginia. West Virginia mesothelioma doctors typically have years of experience. By clicking on each of the doctor’s names you get to have the information about their area of expertise, profession affiliations, background, and their office locations.
Dr. Nepal C. Chowdhury
Thoracic Surgeon
St. Mary’s Medical Center
St. Mary’s Cardiovascular and Thoracic Surgery
Huntington, WV 25702
(304) 399-7530
This doctor is a certified thoracic surgeon who currently practices at the Cabel Huntington Hospital located in Huntington, West Virginia. He does specialize in the general thoracic Surgery and Peripheral Vascular Surgery.
Dr. Rebecca S. Wolfer
Thoracic Surgeon
Marshall Health-Surgery
Huntington, WV 25701
(304) 691-1200
As a certified doctor in both general surgery and general cardiothoracic surgery, Dr. Rebecca S. Wolfer is an associate professor in the department of Surgery at the Joan C. Edwards School of Medicine at Marshall University. A West Virginia Mesothelioma Doctor can be very helpful, let one of our West Virginia mesothelioma attorneys help you find
Most patients do travel out of their current states just to meet the best oncologist and thoracic surgeons across the country, and note that all these mesothelioma experts do have particular focus within their practice.
Here is the list of Top Mesothelioma Doctors in the Country
Paul H. Sugarbaker, M.D.
Gastrointestinal Surgical Oncologist
Washington Cancer Institute
Dr. Paul H. Sugarbaker, FACS, FRCS graduated from Cornell University Medical College in New York City and received his surgical training at the Peter Bent Brigham Hospital in Boston, a Harvard University affiliated program. There he also received a Masters Degree in Immunology at the Harvard School of Arts and Sciences. In 1976 he accepted a position at the National Institutes of Health/ National Cancer Institute – Surgery Branch, as Senior Investigator until 1986. Subsequently, after a brief stay at the Emory Clinic in Atlanta, Georgia he moved back to Washington, DC to become the Medical Director of the Washington Cancer Institute at MedStar Washington Hospital Center in 1989. Currently, he is the Chief of the Peritoneal Surface Malignancy Program and the Director of the Center for Gastrointestinal Malignancies at the Washington Hospital Center in Washington, DC. His interests are focused exclusively on gastrointestinal cancer, gynecologic malignancy, and peritoneal mesothelioma of the abdomen – all malignancies which usually present with cancerous spread to the abdominal cavity. Currently, his clinical and investigative work is concentrated on the treatment of the peritoneal surface dissemination of cancers, referred to as PERITONEAL METASTASES, also known as peritoneal carcinomatosis. He has developed, perfected and popularized the combined treatments of cancer surgery with warm chemotherapy, infused into the open abdomen towards the end the surgical intervention. His mantra, “It’s what the surgeon doesn’t see that kills the patient,” summarizes his thinking as he realizes the limitations of surgery alone, and the limitations of systemic or regional chemotherapy alone. It turns out that the combined application of both the surgical removal of the tumors and the regional treatment directly into the open abdomen where the tumors are located, is especially effective in selected patients. This treatment option and its results have been published extensively in the peer-reviewed literature and in the lay press. Further work to supplement these treatments and to make them even more effective by adding systemic chemo infusions: Perioperative intravenous and intraperitoneal chemotherapy (HIPEC and EPIC} are an essential planned part of these combined surgical and regional chemotherapy interventions. Over the many years he has published over 900 articles and book chapters, edited 7 books, produced 24 videos, and received 4 honorary professorships. He has traveled to all 5 continents to make these treatments available to patients all over the world.
Claire Verschraegen, M.D.
Medical Oncologist
James Cancer Hospital and Solove Research Institute
Verschraegen is a board-certified oncologist who has worked with mesothelioma, metastatic melanomas, sarcomas, gynecologic malignancies and other uncommon cancers. She also has worked with new anti-cancer drugs and treatments of solid tumors, always stressing the importance of clinical trials to help improve therapies.
Before coming to Ohio, she was a tenured professor of medicine in the Division of Hematology and Oncology at UNM, serving as director of the Translational Therapeutics and Clinical Research Program. She oversaw the Clinical Protocol and Data Management Core at the UNM Cancer Center.
She was the principal investigator for the minority-based Community Clinical Oncology Program, which opened NCI-sponsored clinical trials to anyone in the state who wished to participate.
She earned her Medical Degree at the University Libre de Bruxelles in Belgium and trained at the Institute Bordet. She went to Texas for her Medical Oncology fellowship at M.D. Anderson Cancer Center, where she eventually joined the faculty.
QUICK FACT
Before joining UVM, Dr. Verschraegen oversaw a Clinical Protocol and Data Management Program for the University of New Mexico’s Cancer Center.
It was in New Mexico when she did one often-cited study that evaluated the anti-mesothelin immunotoxin SS1 (dsFv) PE38 in fresh tumor cells of peritoneal mesothelioma patients. She also conducted several trials involving a variety of drug combinations that were successful for specific cancers.
Her work with rare cancers has been well respected and well received nationally. Her academic writing includes 10 book chapters, 80 peer-reviewed medical papers and 20 invited papers. She is a former member of the Scientific Board for the Mesothelioma Applied Research Foundation.
The Cancer Support Center of The State of West Virginia
Mesothelioma patients can enjoy transport, temporary housing, counselling, and physical therapy from the cancer support service of the state of West Virginia. While receiving treatments for mesothelioma in West Virginia all these local services may be of help to the patients receiving the treatment.
West Virginia Mesothelioma Treatment Support Services
Counseling & Support Groups
Cabell Huntington Hospital
(Huntington)
304-526-2000
WV University Healthcare
(Martinsburg)
304-264-1000
Long-Term Housing
CAMC Foundation Hospitality House
(Charleston)
304-388-9870
The Davis House
(Elkins)
304-630-3043
Rosenbaum Family House
(Morgantown)
304-598-6094
Patient Transport
Mountain State Transport
(Clarksburg)
304-624-0800
Hometown Transportation
(Moundsville)
304-845-6070
MTM
(Charleston)
844-549-8353
Physical Therapy
St. Mary’s Outpatient Rehabilitation Services
(Huntington)
304-526-1333
Pivot Physical Therapy
(Shepherdstown)
304-876-8600
Advanced Physical Therapy
(Charleston)
304-720-9185
Mesothelioma Treatment Cost
Treating the mesothelioma cancer can be a very expensive proposition and also when receiving related treatment cost can easily add up. Also, when dealing with cancer people tends to take time off from their daily job.
Below is the estimated cost for a number of common procedures used in the diagnosing as well as the treatment of mesothelioma.
West Virginia Mesothelioma Doctors, Cancer Centers and Treatment
Mesothelioma patients living in West Virginia have access to quality mesothelioma treatment in state. Conventional mesothelioma treatments available in West Virginia include surgery, chemotherapy, and radiation. Additionally, clinical trials may currently be recruiting pleural and peritoneal mesothelioma patients in West Virginia. West Virginia Mesothelioma doctors are here for you.
We provide a list of top mesothelioma doctors practicing in West Virginia as well as the top cancer care centers in the state. Local cancer support services have been included as well for your convenience. Learn more about health care options available in West Virginia below.
West Virginia Mesothelioma Statistics
428
Mesothelioma Deaths, 1999 – 2015
161
Asbestosis Deaths, 1999 – 2015
589
Total Deaths, 1999 – 2015
Need help Contacting a West Virginia Mesothelioma Doctor?
It is not uncommon for patients to travel outside of their current states to meet with top oncologists and thoracic surgeons across the country. These mesothelioma experts usually have a particular focus within their practice.
Help with Mesothelioma Treatment Costs
Mesothelioma treatment can be a very expensive proposition and all of the different treatment related costs can add up quickly. Additionally, many people may need to take time off from work to deal with their cancer diagnosis. A West Virginia asbestos attorney can help you.
The table below provides cost estimates for a number of common procedures used in diagnosing and treating mesothelioma. A Pennsylvania mesothelioma lawyer can be of great help to patients in Pennsylvania. Work with Americas leading mesothelioma law firm, mesothelioma lawyers, and mesothelioma attorneys at GPW. A Michigan mesothelioma doctor can be very useful to those diagnosed in Michigan.
Common Costs Associated with Treating Mesothelioma
Mesothelioma Diagnosis & Treatment Costs: Approximate Cost Range
Diagnostic Imaging (CT, PET, MRI): $800 – $1,600 per scan
Needle Biopsy: $500 – $700
Thoracoscopy or Pleuroscopy (lungs) or Laparoscopy (abdomen): $3,600 – $5,000
Thoracotomy (lungs) or Laparotomy (abdomen): $7,800 – $7,900
Surgery – Lobectomy/Pneumonectomy (removal of part or all of a lung): $13,000 – $17,000
Radiation: $7,000 – $12,000
Chemotherapy – Pemetrexed (Alimta®): $37,000 – $50,000
Hyperthermic Intraperitoneal Chemotherapy (HIPEC): $700 – $1,000
The above cost does not factor in the insurance payments as well as reimbursements. The above estimated cost was taken from the Fair Health Consumer Cost Look up tool, bluebook, and some other sources to determine the actual cost for the specific procedures. West Virginia mesothelioma doctors can be very helpful.
How to file an Asbestos Exposure Claim
Ensure not to lose your right to file a claim. Are you or your loved ones been diagnosed with mesothelioma and you are exposed to asbestos in West Virginia, then you may be entitled to some compensation. You will need to file your claim to the right statute for limitations for the state of West Virginia. West Virginia Mesothelioma doctors can be of great help to you. Speak with a West Virginia Asbestos attorney at GPW.
The post West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options appeared first on Goldberg, Persky & White P.C..
from https://www.gpwlaw-mi.com/west-virginia-mesothelioma-doctors
from America's Top Mesothelioma Lawyer - Blog http://gpwlawmimesotheliomalawfirm.weebly.com/blog/west-virginia-mesothelioma-doctors-cancer-centers-treatment-options
0 notes
Text
West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options
West Virginia Mesothelioma Doctors
The State Of West Virginia Mesothelioma Doctors, Cancer Centers, and Treatment
Mesothelioma, Asbestosis, & Lung Cancer patients who reside in West Virginia have access to the leading West Virginia Mesothelioma doctors and treatment throughout the state. In West Virginia mesothelioma treatment which includes surgery, radiation, and chemotherapy are now available for Conventional mesothelioma. Also, we get to have clinical trials recruiting pleural and peritoneal mesothelioma patients in all of West Virginia.
In this article, you get to see the top West Virginia mesothelioma doctors who are practicing in the whole of West Virginia being the top West Virginia cancer centers in the state. Also, for your conveniences, there has been local cancer support which has been made available.
West Virginia Mesothelioma Cancer Centers
Below is the list of health care options in West Virginia which you can learn from West Virginia mesothelioma Cancer Centers. Mesothelioma cancers centers are available in West Virginia where you can get the best quality cancer treatment, and tend to get more detailed information about these cancer centers is made available when you visit the cancer center appropriate link.
Mary Babb Randolph Cancer Center
Morgantown, WV
The West Virginia University School of Medicine in Morgantown has the Mary Randolph Cancer Center which specializes in the treatment of mesothelioma, lung diseases, as well as the thoracic cancers. If you need help contacting the Cancer center contact one of our West Virginia Mesothelioma Lawyers
Here is list of the top Mesothelioma Doctors in West Virginia
This list comprises of the best doctors who specialize in treating mesothelioma in the state of West Virginia. West Virginia mesothelioma doctors typically have years of experience. By clicking on each of the doctor’s names you get to have the information about their area of expertise, profession affiliations, background, and their office locations.
Dr. Nepal C. Chowdhury
Thoracic Surgeon
St. Mary’s Medical Center
St. Mary’s Cardiovascular and Thoracic Surgery
Huntington, WV 25702
(304) 399-7530
This doctor is a certified thoracic surgeon who currently practices at the Cabel Huntington Hospital located in Huntington, West Virginia. He does specialize in the general thoracic Surgery and Peripheral Vascular Surgery.
Dr. Rebecca S. Wolfer
Thoracic Surgeon
Marshall Health-Surgery
Huntington, WV 25701
(304) 691-1200
As a certified doctor in both general surgery and general cardiothoracic surgery, Dr. Rebecca S. Wolfer is an associate professor in the department of Surgery at the Joan C. Edwards School of Medicine at Marshall University. A West Virginia Mesothelioma Doctor can be very helpful, let one of our West Virginia mesothelioma attorneys help you find
Most patients do travel out of their current states just to meet the best oncologist and thoracic surgeons across the country, and note that all these mesothelioma experts do have particular focus within their practice.
Here is the list of Top Mesothelioma Doctors in the Country
Paul H. Sugarbaker, M.D.
Gastrointestinal Surgical Oncologist
Washington Cancer Institute
Dr. Paul H. Sugarbaker, FACS, FRCS graduated from Cornell University Medical College in New York City and received his surgical training at the Peter Bent Brigham Hospital in Boston, a Harvard University affiliated program. There he also received a Masters Degree in Immunology at the Harvard School of Arts and Sciences. In 1976 he accepted a position at the National Institutes of Health/ National Cancer Institute – Surgery Branch, as Senior Investigator until 1986. Subsequently, after a brief stay at the Emory Clinic in Atlanta, Georgia he moved back to Washington, DC to become the Medical Director of the Washington Cancer Institute at MedStar Washington Hospital Center in 1989. Currently, he is the Chief of the Peritoneal Surface Malignancy Program and the Director of the Center for Gastrointestinal Malignancies at the Washington Hospital Center in Washington, DC. His interests are focused exclusively on gastrointestinal cancer, gynecologic malignancy, and peritoneal mesothelioma of the abdomen – all malignancies which usually present with cancerous spread to the abdominal cavity. Currently, his clinical and investigative work is concentrated on the treatment of the peritoneal surface dissemination of cancers, referred to as PERITONEAL METASTASES, also known as peritoneal carcinomatosis. He has developed, perfected and popularized the combined treatments of cancer surgery with warm chemotherapy, infused into the open abdomen towards the end the surgical intervention. His mantra, “It’s what the surgeon doesn’t see that kills the patient,” summarizes his thinking as he realizes the limitations of surgery alone, and the limitations of systemic or regional chemotherapy alone. It turns out that the combined application of both the surgical removal of the tumors and the regional treatment directly into the open abdomen where the tumors are located, is especially effective in selected patients. This treatment option and its results have been published extensively in the peer-reviewed literature and in the lay press. Further work to supplement these treatments and to make them even more effective by adding systemic chemo infusions: Perioperative intravenous and intraperitoneal chemotherapy (HIPEC and EPIC} are an essential planned part of these combined surgical and regional chemotherapy interventions. Over the many years he has published over 900 articles and book chapters, edited 7 books, produced 24 videos, and received 4 honorary professorships. He has traveled to all 5 continents to make these treatments available to patients all over the world.
Claire Verschraegen, M.D.
Medical Oncologist
James Cancer Hospital and Solove Research Institute
Verschraegen is a board-certified oncologist who has worked with mesothelioma, metastatic melanomas, sarcomas, gynecologic malignancies and other uncommon cancers. She also has worked with new anti-cancer drugs and treatments of solid tumors, always stressing the importance of clinical trials to help improve therapies.
Before coming to Ohio, she was a tenured professor of medicine in the Division of Hematology and Oncology at UNM, serving as director of the Translational Therapeutics and Clinical Research Program. She oversaw the Clinical Protocol and Data Management Core at the UNM Cancer Center.
She was the principal investigator for the minority-based Community Clinical Oncology Program, which opened NCI-sponsored clinical trials to anyone in the state who wished to participate.
She earned her Medical Degree at the University Libre de Bruxelles in Belgium and trained at the Institute Bordet. She went to Texas for her Medical Oncology fellowship at M.D. Anderson Cancer Center, where she eventually joined the faculty.
QUICK FACT
Before joining UVM, Dr. Verschraegen oversaw a Clinical Protocol and Data Management Program for the University of New Mexico’s Cancer Center.
It was in New Mexico when she did one often-cited study that evaluated the anti-mesothelin immunotoxin SS1 (dsFv) PE38 in fresh tumor cells of peritoneal mesothelioma patients. She also conducted several trials involving a variety of drug combinations that were successful for specific cancers.
Her work with rare cancers has been well respected and well received nationally. Her academic writing includes 10 book chapters, 80 peer-reviewed medical papers and 20 invited papers. She is a former member of the Scientific Board for the Mesothelioma Applied Research Foundation.
The Cancer Support Center of The State of West Virginia
Mesothelioma patients can enjoy transport, temporary housing, counselling, and physical therapy from the cancer support service of the state of West Virginia. While receiving treatments for mesothelioma in West Virginia all these local services may be of help to the patients receiving the treatment.
West Virginia Mesothelioma Treatment Support Services
Counseling & Support Groups
Cabell Huntington Hospital
(Huntington)
304-526-2000
WV University Healthcare
(Martinsburg)
304-264-1000
Long-Term Housing
CAMC Foundation Hospitality House
(Charleston)
304-388-9870
The Davis House
(Elkins)
304-630-3043
Rosenbaum Family House
(Morgantown)
304-598-6094
Patient Transport
Mountain State Transport
(Clarksburg)
304-624-0800
Hometown Transportation
(Moundsville)
304-845-6070
MTM
(Charleston)
844-549-8353
Physical Therapy
St. Mary’s Outpatient Rehabilitation Services
(Huntington)
304-526-1333
Pivot Physical Therapy
(Shepherdstown)
304-876-8600
Advanced Physical Therapy
(Charleston)
304-720-9185
Mesothelioma Treatment Cost
Treating the mesothelioma cancer can be a very expensive proposition and also when receiving related treatment cost can easily add up. Also, when dealing with cancer people tends to take time off from their daily job.
Below is the estimated cost for a number of common procedures used in the diagnosing as well as the treatment of mesothelioma.
West Virginia Mesothelioma Doctors, Cancer Centers and Treatment
Mesothelioma patients living in West Virginia have access to quality mesothelioma treatment in state. Conventional mesothelioma treatments available in West Virginia include surgery, chemotherapy, and radiation. Additionally, clinical trials may currently be recruiting pleural and peritoneal mesothelioma patients in West Virginia. West Virginia Mesothelioma doctors are here for you.
We provide a list of top mesothelioma doctors practicing in West Virginia as well as the top cancer care centers in the state. Local cancer support services have been included as well for your convenience. Learn more about health care options available in West Virginia below.
West Virginia Mesothelioma Statistics
428
Mesothelioma Deaths, 1999 – 2015
161
Asbestosis Deaths, 1999 – 2015
589
Total Deaths, 1999 – 2015
Need help Contacting a West Virginia Mesothelioma Doctor?
It is not uncommon for patients to travel outside of their current states to meet with top oncologists and thoracic surgeons across the country. These mesothelioma experts usually have a particular focus within their practice.
Help with Mesothelioma Treatment Costs
Mesothelioma treatment can be a very expensive proposition and all of the different treatment related costs can add up quickly. Additionally, many people may need to take time off from work to deal with their cancer diagnosis. A West Virginia asbestos attorney can help you.
The table below provides cost estimates for a number of common procedures used in diagnosing and treating mesothelioma. A Pennsylvania mesothelioma lawyer can be of great help to patients in Pennsylvania. Work with Americas leading mesothelioma law firm, mesothelioma lawyers, and mesothelioma attorneys at GPW. A Michigan mesothelioma doctor can be very useful to those diagnosed in Michigan.
Common Costs Associated with Treating Mesothelioma
Mesothelioma Diagnosis & Treatment Costs: Approximate Cost Range
Diagnostic Imaging (CT, PET, MRI): $800 – $1,600 per scan
Needle Biopsy: $500 – $700
Thoracoscopy or Pleuroscopy (lungs) or Laparoscopy (abdomen): $3,600 – $5,000
Thoracotomy (lungs) or Laparotomy (abdomen): $7,800 – $7,900
Surgery – Lobectomy/Pneumonectomy (removal of part or all of a lung): $13,000 – $17,000
Radiation: $7,000 – $12,000
Chemotherapy – Pemetrexed (Alimta®): $37,000 – $50,000
Hyperthermic Intraperitoneal Chemotherapy (HIPEC): $700 – $1,000
The above cost does not factor in the insurance payments as well as reimbursements. The above estimated cost was taken from the Fair Health Consumer Cost Look up tool, bluebook, and some other sources to determine the actual cost for the specific procedures. West Virginia mesothelioma doctors can be very helpful.
How to file an Asbestos Exposure Claim
Ensure not to lose your right to file a claim. Are you or your loved ones been diagnosed with mesothelioma and you are exposed to asbestos in West Virginia, then you may be entitled to some compensation. You will need to file your claim to the right statute for limitations for the state of West Virginia. West Virginia Mesothelioma doctors can be of great help to you. Speak with a West Virginia Asbestos attorney at GPW.
The post West Virginia Mesothelioma Doctors | Cancer Centers | Treatment Options appeared first on Goldberg, Persky & White P.C..
from https://www.gpwlaw-mi.com/west-virginia-mesothelioma-doctors
0 notes