#injections & blocks specialist
Explore tagged Tumblr posts
Text
#Neuropathic Pain Chicago#Injections & Blocks Specialist#Neuropathic Pain Treatments in Chicago#Radiofrequency Ablation Specialist#Kyphoplasty Specialist#kyphoplasty Surgeons Near Me#Spinal Cord Stimulation Specialist#Sacrix SI Joint Fusion Treatment#Vertiflex Superion Specialist#Aurora ZIP Procedure#ZIP Procedure for Chronic Back Pain#ZIP Spine Procedure#ZIP Procedure for Spinal Stenosis#Fibromyalgia Specialist Chicago#Spinal Compression Fracture Treatment Chicago#Spinal Cord Stimulation Therapy Chicago#Lumbar Spinal Stenosis Treatment Chicago#Vertiflex Superion Procedure#Motor Vehicle Injuries Treatments#Spinal Cord Pain Treatment Chicago#Lumbar Spinal Stenosis Surgery Chicago#Nerve Block Injections Specialists#Dorsal Ganglion Root Stimulation#Pain Specialist Chicago#DRG Stimulation Procedure#Chronic Pain Treatment in Chicago#DRG Stimulator Surgery#Pain Management Specialists Chicago#Dorsal Root Ganglion Stimulation Therapy#Sacroiliac Joint Fusion Treatment
0 notes
Text
Relief From Neck Pain Conditions: It’s Within Your Reach
Nearly 80 percent of people suffer from neck pain during their lifetime. Several Americans suffer from chronic neck pain. The neck consists of several components, including muscles, ligaments, and tendons.
The neck is a body part that is vulnerable to several painful conditions and injuries. This is because there is an extensive range of neck movements that happen throughout the day. Also, the ability of the neck to function optimally is also dependent on the muscles located in the chest, back, and shoulder.
If neck pain is left untreated, they can turn out to become chronic. Neck pain conditions may include stiffness, soreness, or pain in the neck with limited mobility.

Causes of neck pain conditions
Neck pain is also known as cervicalgia. It is the pain experienced in or near the spine or beneath the head. Neck pain conditions are quite common. Most individuals have neck pain at some point or the other in their life. It is a widespread problem affecting diverse age groups and lifestyles around the world.
Some of the most common causes of neck pain include:
Holding the neck in the same position for a long time.
Injury to soft tissues (tendons, ligaments, and muscles) within the neck.
Poor body posture with head flexed in the forward direction.
Pressure on the neck causing strains and sprains
Some other causes that trigger neck pain conditions
Whiplash injury
Awkward sleeping position
Mental stress or worry
Cervical spondylosis
Degenerative disc disease
Herniated disc
Osteoarthritis
Rheumatoid arthritis
Cervical spine injury
Spinal stenosis
Compressed (pinched) nerves
Worn-out joints
Inflammation
Abnormal growths such as bone spurs, cysts
Meningitis
Symptoms of Neck Pain
The symptoms of neck pain vary widely from person to person. Here are some of the most common symptoms of neck pain conditions.
Muscle tightness
Soreness and stiffness
Numbness or tingling sensation
Reduced ability to move the head
Trouble in lifting or gripping objects
Muscle spasms
General weakness
Frequent headaches
Sharp shooting pain
Feeling of fullness
Difficulty in swallowing
Radiating pain into the arms and neck
Visiting a Texas pain specialist for neck pain
Neck pain is not constant. It comes and goes frequently, or may come back intermittently. If you are suffering from neck pain, the major question that arises is when should you seek medical attention or go for neck pain therapy Houston?
In most cases, neck pain goes away on their own after a few days. However, if the neck pain lasts for several days or becomes worse and continues to interfere with day-to-day activities, it is advisable to seek medical help immediately or visit one of the top pain management clinics in Texas.
Sometimes neck pain conditions may arise due to an underlying medical condition such as inflammation, tumor, meningitis, spinal nerve compression, or any possible infection.
You should consult a Texas pain specialist for neck pain immediately if you face the following:
Sudden neck stiffness with difficulty in lifting objects.
Fever and chills
Excruciating pain radiating into the arms and legs
Problems with body balance and coordination
Unexpected weight loss
Bowel or bladder dysfunction
Numbness, weakness or dizziness
Swelling of lymph nodes
When it comes to the health of your neck, it is better to be safe.
Diagnosis of neck pain conditions
Most neck pain conditions are diagnosed and treated based on the symptoms and basic examination.
The best pain management clinics in Texas perform a comprehensive examination and consultation.
The doctor collects information about your medical history and asks questions about the discomfort that you are facing.
During the examination, they will check for any possible signs of swelling or abnormalities.
During diagnosis, a Texas pain specialist for neck pain may also guide you to perform a series of movements and stretches to gauge the pain.
Occasionally, the doctor may also recommend diagnostic imaging tests such as X-ray, CT scan, or MRI.
The imaging studies will provide the doctor with detailed information about the tissues, muscles, and bone surrounding the neck.
They may also help rule out other major underlying causes of neck pain.
Neck pain treatments
While most causes of neck pain eventually disappear within a day or two with rest and self-help treatments at home. However, complex or continuing neck pain conditions may require other pain relief treatments and therapies. These include:
Stretching and muscle strengthening exercises for the neck.
Pain medications and muscle relaxants (anti-inflammatory steroidal medications)
Transcutaneous Electric Nerve Stimulation (TENS)
Steroid injections
Traction
Special neck collar
Hot and cold therapy
Acupuncture
Relaxing massage
Alternative therapies
Deep breathing exercises
Meditation
Stress-reducing techniques
Surgery, in rare cases, if a nerve or spinal cord is being compressed
Preventing neck pain conditions
Here are some of the ways to improve your neck health.
Maintaining an upright body posture
Minimizing the amount of time spent on mobile devices
Stay active and exercise regularly
Stay hydrated throughout the day
Adjust your workstation so that you don’t have to keep your head tilted up or down
Texas Interventional Pain Specialists: A Reliable And Trusted Name for Neck Pain Therapy Houston
The dedicated and compassionate team of doctors at Texas Interventional Pain Specialists led by Dr. Edward Baumgartner diagnoses and treats the cause of neck pain, providing effective pain relief. This pain management clinic in Texas follows minimally invasive pain procedures for treating neck pain conditions effectively.
The unique approach and targeted therapy followed at this clinic minimizes neck pain with a shorter recovery time for patients. This Texas pain specialist for neck pain clinic focuses on alleviating neck pain, increasing mobility, and accelerating healing through minimally invasive pain procedures.
Prior to starting the neck pain treatment, a meticulous examination of patients is carried out at this pain management clinic in Texas. This helps in identifying the underlying cause of the neck pain.
If you are experiencing neck pain, don’t wait till the pain gets worse.
Neck pain conditions should be treated immediately without allowing them to become more severe.
Are you looking at a speedy recovery from neck pain conditions? Do you want to keep your neck pain from returning repeatedly? Schedule an appointment with Texas Interventional Pain Specialists for a personalized pain relief treatment from neck pain.
#Interventional Pain Specialist#Injections Block Specialist#kyphoplasty Specialist#Neuropathic Pain Specialist#Pain Management Specialist Houston#Chronic Pain Specialist#Pain Medicine Specialist Houston#Pain Specialist Near Me#Radiofrequency Ablation Specialist#Spinal Cord Stimulation Specialist#Pain Management Clinic Houston#Lumbar Radiofrequency Ablation Specialist#Neuropathic Pain Treatment Texas#Back Pain Doctors#Chronic Pain Treatment Clinic#Back Pain Doctors in Houston#Spinal Cord Stimulation Treatment Houston#Compression Fracture Treatment Texas#Pain Management Services Houston#Spinal Stimulator Trial Procedure#Back Pain Treatment Near Me#Spinal Compression Fractures Specialist#Spinal Cord Stimulator Trial#Work Injuries Treatment#Injury Pain Specialist#Chronic Pain Management Near Me#Pain Management Doctors Houston#Chronic Pain Management Clinic#Pain Management Doctor Houston#Neuropathy Treatment Houston
0 notes
Text
Nerve Block
Neural blockades are also known as nerve blocks. These are a type of Nerve Block therapy. This can help prevent or alleviate a wide range of pain. For your comfort, we at Vencer Hospital give each patient sedative medication prior to the Nerve Block treatment. Before allowing someone to enter the operating room, it is customary to make sure the block is functional.
#Nerve Block Injections Pune#Neuro Surgery Pune#Plastic Surgery in Pune#Pain Block Treatment Pune#Pain-Free Future#Explore Solution#Physiotherapy clinic near me#Spine Injection Treatment Specialist Pune#Lower Back Pain Treatment Specialist Pune
0 notes
Text
By: Chloe Cole
Published: July 28, 2023
On Thursday, her 19th birthday, Chloe Cole testified to Congress with a “final warning” that medical treatments to change the gender of confused children is horrific. Cole, who was given surgery as a teenager to become male and soon regretted it, said what she needed most was therapy, not a scalpel. Here is what she told lawmakers:
My name is Chloe Cole and I am a de-transitioner.
Another way to put that would be: I used to believe that I was born in the wrong body and the adults in my life, whom I trusted, affirmed my belief, and this caused me lifelong, irreversible harm.
I speak to you today as a victim of one of the biggest medical scandals in the history of the United States of America.
I speak to you in the hope that you will have the courage to bring the scandal to an end, and ensure that other vulnerable teenagers, children and young adults don’t go through what I went through.
Deceit & coercion
At the age of 12, I began to experience what my medical team would later diagnose as gender dysphoria.
I was well into an early puberty, and I was very uncomfortable with the changes that were happening to my body. I was intimidated by male attention.
And when I told my parents that I felt like a boy, in retrospect, all I meant was that I hated puberty, that I wanted this newfound sexual tension to go away.
I looked up to my brothers a little bit more than I did to my sisters.
I came out as transgender in a letter I sent on the dining room table.
My parents were immediately concerned.
They felt like they needed to get outside help from medical professionals.
But this proved to be a mistake.
It immediately set our entire family down a path of ideologically motivated deceit and coercion.
The general specialist I was taken to see told my parents that I needed to be put on puberty-blocking drugs right away.
They asked my parents a simple question: Would you rather have a dead daughter or a living transgender son?
The choice was enough for my parents to let their guard down, and in retrospect, I can’t blame them.
This is the moment that we all became victims of so-called gender-affirming care.
I was fast-tracked onto puberty blockers and then testosterone.
The resulting menopausal-like hot flashes made focusing on school impossible.
I still get joint pains and weird pops in my back.
But they were far worse when I was on the blockers.
Forever changed
A month later, when I was 13, I had my first testosterone injection.
It has caused permanent changes in my body: My voice will forever be deeper, my jawline sharper, my nose longer, my bone structure permanently masculinized, my Adam’s apple more prominent, my fertility unknown.
I look in the mirror sometimes, and I feel like a monster.
I had a double mastectomy at 15.
They tested my amputated breasts for cancer.
That was cancer-free, of course; I was perfectly healthy.
There is nothing wrong with my still-developing body, or my breasts other than that, as an insecure teenage girl, I felt awkward about it.
After my breasts were taken away from me, the tissue was incinerated — before I was able to legally drive.
I had a huge part of my future womanhood taken from me.
I will never be able to breastfeed.
I struggle to look at myself in the mirror at times.
I still struggle to this day with sexual dysfunction.
And I have massive scars across my chest and the skin grafts that they used, that they took of my nipples, are weeping fluid today, and they’re grafted into a more masculine positioning, they said.
After surgery, my grades in school plummeted.
Everything that I went through did nothing to address the underlying mental health issues that I had.
And my doctors with their theories on gender that all my problems would go away as soon as I was surgically transformed into something that vaguely resembled a boy — their theories were wrong.
The drugs and surgeries changed my body, but they did not and could not change the basic reality that I am, and forever will be, a female.
Depths of despair
When my specialists first told my parents they could have a dead daughter or a live transgender son, I wasn’t suicidal.
I was a happy child who struggled because she was different.
However at 16, after my surgery, I did become suicidal.
I’m doing better now, but my parents almost got the dead daughter promised to them by my doctors.
My doctor had almost created the very nightmare they said they were trying to avoid.
So what message do I want to bring to American teenagers and their families?
I didn’t need to be lied to.
I needed compassion.
I needed to be loved.
I needed to be given therapy that helped me work through my issues, not affirmed my delusion that by transforming into a boy, it would solve all my problems.
We need to stop telling 12-year-olds that they were born wrong, that they are right to reject their own bodies and feel uncomfortable with their own skin.
We need to stop telling children that puberty is an option, that they can choose what kind of puberty they will go through, just like they can choose what clothes to wear or what music to listen to.
Pseudoscience
Puberty is a rite of passage to adulthood, not a disease to be mitigated.
Today, I should be at home with my family celebrating my 19th birthday.
Instead, I’m making a desperate plea to my elected representatives.
Learn the lessons from other medical scandals, like the opioid crisis.
Recognize that doctors are human, too, and sometimes they are wrong.
My childhood was ruined along with thousands of de-transitioners that I know through our networks.
This needs to stop. You alone can stop it.
Enough children have already been victimized by this barbaric pseudoscience.
Please let me be your final warning.
Thank you.
Might as well call her a murtad and kufr.
"The medical industry mutilated me, maybe don't mutilate other kids," shouldn't require bravery or renouncing an ideology.
Reminder: A minor under the age of 18 is too young to agree to a cellphone contract. 🤦♀️
#Chloe Cole#detrans#detransition#gender ideology#queer theory#medical malpractice#medical scandal#medical mutilation#gender affirming#gender affirming care#affirmation model#double mastectomy#gender cult#sex trait modification#genderwang#religion is a mental illness
1K notes
·
View notes
Text
Rural Family Medicine Is Great And Exhausting
Today, I saw 21 patients, I prescribed medication for an abortion, I started a patient on hospice, I placed on IUD, I started a transgender patient on anti-androgens, I saw someone with a one in a million genetic disease, I comforted a queer person who just lost their spouse to cancer, I adjusted psychiatric meds for a schizophrenic patient with profound paranoia who is tremendously kind. I saw two employees of my clinic. I saw a doctor's spouse.
Every day is different. I do IUD insertions, Nexplanon insertions, colposcopies, skin biopsies, cyst removals, toenail removals, greater occipital nerve blocks, shoulder and knee injections. I treat blood pressure and diabetes and atrial fibrillation and congestive heart failure, like all generalists do. I treat things specialists would see in the city because we have a tiny handful of specialists. I could work in the hospital again if I wanted to. I could go back to delivering babies if I wanted to. I see pediatric patients, I see patients over 100 years old. I see psychiatric patients who simply do not have access to a psychiatrist because there are never more than five of them to serve an area of 70,000 people, scattered across our geography. I diagnose cancers and rheumatologic diseases. I am forced, on a daily basis, to become a better version of myself--more aware of the system I work in, more underlying medical knowledge.
I love my work. It takes most of me. I don't have kids, and I'm glad, because I wouldn't be able to work like this and I love my work. I don't regret the choices that I've made that led me here.
I'm turning thirty-nine this year. I worked in so many different jobs, took so many different classes, volunteered and read and wrote and experimented with who I was and who I wanted to be. You have time. You can become the version of yourself that can make you happy. There is no single endpoint, no moment when you get to stop and go, that's it, I'll just calcify in place now. You are a human. You are meant to keep moving and changing and growing. That scared the shit out of me when I was younger and came from a deeply unstable home and all I wanted was peace. I wanted to be able to rest. But you can't stagnate and call it peace.
My life has worth beyond what it's worth to me. That's what I wanted. I wanted the bliss of service. I wanted to be of service. And in my own way, in my own time, on my own terms, I am.
165 notes
·
View notes
Text
hi guys!!!! MALS update since ive been putting it off since my appointment in mid july lmao. anyway cw for medical mentions and all that stuff!
i saw the specialist!!! a year of waiting, countless phone calls and a lawsuit threat for a guy to spend 15 minutes looking at my CT scan 💀 shoutout to American healthcare
anyway!! as short as the appointment was, it was actually very worth it- the doctor said it was incredibly likely that I had MALS, but a few of my symptoms are less common than others, so he referred me to a few other people. I was sent to have an ultrasound done on the arteries in my abdomen, as well as referred to one of the top vascular specialists in my state. I’m on his wait list, and I’ll see him in September.
The last thing they need to do to absolutely confirm my diagnosis is a nerve block procedure. Basically, they’re going to shut down the nerves that MALS impacts, and if my symptoms go away, then they know exactly what they need to operate on. They’ll do this by injecting me with a heavy mixture of both steroids and sedatives, and the effects will last about a week. The procedure takes about two hours, and they won’t put me under anesthesia but they are gonna give me a sedation IV or something.
So uh. That procedure is this Friday! I am!!! Highkey terrified out of my mind lmfaooo holy shit I am so scared. they’re giving me (guy who can barely get a flu shot without crying and still needs to look away from his t shots) the Two Hours Of Injections Procedure. i am terrified but hopefully it is for the best!!
i will keep you guys updated on the procedure etc!!
22 notes
·
View notes
Text
Women in the public sector are quitting their jobs due to being blocked from working flexibly with three in ten seeing their requests rejected, according to a major new study.
Researchers at Unison, the UK’s largest trade union, who polled just over 44,000 women working across the public sector, found three in ten working in hospitals, schools, care homes, town halls, police stations and other key services had pleas to work flexibly denied.
Some women said employers told them to leave their job or use annual leave if they want to work flexibly, while others report their requests were immediately blocked on the same day they were put in. Struggles to access flexible working meant some women had quit their jobs, researchers warned.
Christina McAnea, Unison’s general secretary, said: “Too many employers are still turning down flexible working requests, which means the right to request is pretty meaningless for many women. The right to work flexibly from day one would be beneficial for staff and employers alike, and help bring workplaces into the 21st century.”
Helping women juggle work with childcare and caring for loved ones can enable workplaces to recruit for jobs which are tricky to fill and likely boost the quality of public services, she added.
Ms McAnea said: “It’s disheartening to see many employers continuing to deny their staff the opportunity to work flexibly. They have nothing to lose and everything to gain.
"But sadly many women who find they need to inject some flexibility into their working lives are coming up against employers with inconsistent, rigid and unimaginative attitudes. While there’s no one-size-fits-all solution, some form of flexible working is achievable in most workplaces.”
A quarter of those women who were informed they could not change their working conditions say their requests were rejected on a number of occasions.
Researchers also found more than two fifths of women were told they could not work flexibly because doing so would harm the service being provided, while almost three in ten were informed there would not be enough colleagues to cover for them.
A fifth had their request rejected due to managers saying doing so would result in colleagues making similar pleas, while around one in seven were not provided with a reason by their employer.
New flexible working legislation comes into force in April which gives employees a statutory right to ask for flexible working from day one at a new job. While this is an improvement on the current wait of six months to ask, Unison warn employers are too easily able to block flexible working requests.
Emily*, who works in the energy sector, said she only managed to get her flexible return to work from maternity leave agreed just before she was due to return to work.
“The process was horrendous,” she said. “I had to submit several requests and they were all turned down within days. I was stunned. I was caring for my baby and having huge levels of anxiety simply trying to get some flexibility at work. I was scared I’d lose my job. It dragged on so much I couldn’t sort out childcare. The process left me traumatised.”
While Nadia*, a local government worker with a disability, was blocked from working flexibly even though she had medical notes written up by her doctor.
“I had a very supportive manager during the pandemic and we all worked well during that time,” Nadia, a single mother of two, added. “But as the situation eased, my new manager suddenly wanted everybody in the office all the time. Daily attendance then worsened my condition and I had to go off sick for a few months to recover. Being able to work from home on the days I’m struggling would make a huge difference, and also make it easier to look after my children.”
Helen*, a specialist nurse and single mother of three, explained she was repeatedly blocked from working flexibly.
She said: “I had to go down a pay band to get some flexibility, which put me and my family in financial difficulty. I was told if they allowed me to work flexibly they’d have to do the same for others. But others aren’t in my situation.
“I'm a survivor of domestic violence and have no family support. The process was awful and I was made to feel like a massive inconvenience. Now I don’t want to be a nurse any more and am looking for a new job in retail. I’ve had to take time off because of the stress and anxiety I experienced. It shouldn’t be like this as I do love my job.”
*Names changed
12 notes
·
View notes
Text
I have been dealing with non-stop health problems since 22nd June or thereabouts and I just want it all to stop.
On 21st June, which was my birthday, I went to an Elder Scrolls Online 10th Anniversary party at the offices of Bethesda/Zenimax in London. I proceeded to catch COVID from being out in public, and spent a week in bed.
On 29th June I was sitting at my computer, still with a high fever, stood up to go to the loo, and something in my right leg tore and I fell over. Couldn't walk at all for several days. Finally got free of COVID, went to the hospital, and they thought from an ultrasound that I'd torn my Achilles tendon. So I got put in a horrible cast and was not allowed to put any weight on the leg at all.

Went to Germany for the ESO Tavern anyway because I figured that accessible hotel rooms would be less stress than my house, which is only accessible for my normal disability and not for "you can't put any weight on your foot at all". Had to inject myself with an anticoagulant called Fragmin because of being immobile, which is super great if you're needle phobic.
Once I got home and saw the specialist, she thought it probably wasn't a tear and ordered an MRI. This showed that actually, I "only" had "thickening and inflammation" of the tendon. So it looks like I "only" tore my calf muscle which is a much less serious injury to heal. (I could dig out the hospital letter with the actual names of the muscles but I frankly don't care enough.)
However, my right leg was STILL rock solid with oedema. (Medical for "swelling"). The calf felt hard to the touch instead of squishy like my left leg. The young doctor that I saw the second time was only bothered about the tendonitis and severe inflexibility of my foot, not the fact that my leg was swollen. And I continued to have pain spikes so bad that my temperature hit 38.0 C and I started puking for probably six weeks after the initial injury.
TL;DR my leg started to get better and then it got worse again. About two weeks ago I noticed the leg was more swollen than ever, and the skin was bright red and very itchy. Took myself up to the hospital again, had a blood test, sat and waited for the results.

My foot turned LITERALLY purple and by the time I got to see the A&E doctor, she just looked at my foot in combination with the blood test results and declared that I had a clot. (Though she was very thorough, carefully checking the entire length of my bad leg against the good one.) They gave me a massive dose of anticoagulants and sent me home to sleep in my own bed for a bit, then I went back the next day and had another ultrasound at a different frequency from the first. (Different frequencies of sound penetrate different levels of tissue). And promptly got diagnosed with Deep Vein Thrombosis.
Blood clots are kinda gross (don't worry, there are no pictures):
Apparently the blood clot is from behind my knee all the way up to mid-thigh. I thought a blood clot was an amorphous, approximate spheroid blocking the vein at a particular place, but it actually fills the entire vein! (Gross!)
Also the main concern with Deep Vein Thrombosis is that bits might break off from the main clot and travel through the bloodstream to cause a Pulmonary Embolism. So the high dose of anticoagulants is actually to deal with bits breaking off from the clot rather than to break down the clot itself! That's why the treatment is 3-6 months on a high dose of anticoagulants.
I was worried about the risk of stroke but that's from blood clots in arteries, not veins.
I'm still annoyed with the doctor in the Fracture Clinic who basically looked at me and saw a fat person, rather than checking that my uninjured fat left leg and injured fat right leg felt the same. Because I had the oedema then. I had a soft, squishy fat left leg and a hard, unsquishable fat right leg.
If I'd actually followed his advice I might have accidentally killed myself. Fortunately I know the medical word "oedema" and knew not to use the special socks which said "do not use if you have oedema".
I am so fucking frustrated. So stupidly tired. I can't work out whether I'm depressed because I'm exhausted or exhausted because I'm depressed. Or whether the two states are orthogonal and caused by something else.
I feel like I've basically missed the entire summer to being sick and mostly unable to move very far from my bed, and the only joy I have is that I live in the UK and have paid nothing for any of this healthcare because it's all funded from our taxes.
#covid 19#leg injury#torn muscle#blood clot#deep vein thrombosis#anticoagulants#hospital#health at every size#fat people need proper healthcare too#probably only of interest to my actual friends#i am very frustrated though#and too tired to do much of anything
4 notes
·
View notes
Text





[ID:
Screenshot from a Canary article, with a heading that says: "Carla: very severe ME/CFS – and now sectioned." Text reads:
You can read part of Carla’s story here. She has now been in West Middlesex Hospital for seven months. Late on Thursday 17 October, an external psychiatrist and a nurse assessed Carla and deemed she met the criteria to be sectioned; in effect weaponising the Mental Health Act.
Doctors have now convinced themselves that her severe gastrointestinal pain is partly psychosomatic. The psychiatrist who did her Section 2 assessment told Carla’s father that:
"the physical is always related to the mental"
Or words to that effect. West Middlesex Hospital is now saying that her GI pain, along with her seizures, are psychosomatic. She is still unable to take adequate nutrition, therefore her ‘made up’ GI pain is posing a risk to herself – ergo she needs to be sectioned.
Screenshot from a BBC article reading:
Pierre Naoum, 62, from Feltham in Hounslow, west London, says his daughter Carla, 23, who was diagnosed with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), is in severe pain and now weighs about 5st 9lbs (35kg) - down from 8st 3lbs (52kg)-after being admitted to West Middlesex Hospital due to problems with her feeding tube.
Even though there are no ME/CFS specialists at West Middlesex University Hospital (WMUH) in Isleworth, west London, Mr Naoum says apsychiatrist assigned to oversee her care has insisted on removing accommodations for her condition such as reduced light, has suddenly reduced her opioid dosage to nothing, and told them she needs to "calm down".
Next screenshot from a different section of the same article:
The first of these came when the NHS team changed her feeding tube to one "thicker than the first one" - from a size six to a size 10 - and increased the amount she was fed from almost nothing to 1.5 litres within a week.
Mr Naoum said his daughter "started to scream, scream, scream" from the "pain of the tube, pain of the sudden huge quantity, with the stress".
The team also altered the method and dosage of her lorazepam and oxycodone pain medications, injecting them all at once rather than via tablets spread out across the day.
Heading that reads: 'No painkiller would stop her pain'
Shortly afterwards Mr Naoum said his daughter suddenly "lost consciousness for about six hours" and then the psychiatrist decided to stop the medications altogether, "straight away, suddenly".
Mr Naoum says this is against National Institute for Health and Care Excellence (NICE) guidelines for drug withdrawal.
Next screenshot from a different section:
“Carla was screaming, screaming and she said to the to the doctor: ‘I am dying, please, my head will explode,’” Mr Naoum says.
On one occasion he says the psychiatrist and an assistant removed tape and red bags blocking light around Carla's room blinds, while she groaned in pain.
When her parents asked the psychiatrist why the coverings could not remain, Mr Naoum says they replied it was impossible for the light in the room to be affecting her if she was wearing an eye mask, adding the light was not causing an issue and they should remove her mask altogether.
Mr Naoum says when they told the psychiatrist Carla cried when they tried to remove her mask, they responded by saying Carla also screamed when the team fed her through her nasogastric tube but they kept doing it anyway, so they had to do the same with light until she calmed down.
Next screenshot, direct continuation of previous text:
fter several days with the covers removed Carla began losing consciousness again, Mr Naoum says, until she was having seizure-like episodes and passing out 10 to 20 times a day for nine days.
The BBC has seen videos of these episodes, including one where Carla is unconscious and not responsive to medical checks by staff, and another where her eyes roll back in her head, her face drops on one side, and she displays involuntary jerking movements for a short period of time.
Mr Naoum says it was not until a locum was called to the hospital, who advised staff the light and sound measures did not work with Carla, that the covers were reinstalled.
When asked if there is any NHS guidance stating ME/CFS is a psychological condition, NHS England referred BBC London to the current NICE guideline.
End ID]
2 notes
·
View notes
Text
Burning away the Chronic pain: Advantages of Radiofrequency Ablation
Have you ever felt trapped in a world of constant pain? An ache that lingers without warning.
For many, chronic pain is a debilitating condition that can significantly impact their quality of life. Traditional pain management methods may offer temporary relief, but they simply aren't enough. That's where Radiofrequency Ablation comes in.
What is Radiofrequency Ablation?
Radiofrequency ablation, or RFA, is a minimally invasive treatment in which nerve tissue is heated and destroyed using radiofrequency energy. The procedure is of special help for chronic pain emanating from a specific set of nerves in the back or neck area.
This involves the placement of a thin needle in the region of interest in RFA. The needle is attached to a radiofrequency generator, an equipment piece that feeds heat into targeted nerve tissue. Such heat causes the death of nerve tissue and hence impairs the transmission of pain impulses.
How does RFA work?
Identifying the source of pain: A specialized doctor, often referred to as a Radiofrequency Ablation Specialist, uses imaging techniques like X-rays or CT scans to pinpoint the specific nerve causing the pain.
Inserting a needle: A thin needle is inserted into the affected area, guided by the imaging equipment.
Delivering radiofrequency energy: Once the needle is in place, radiofrequency energy is delivered through it. This energy heats the nerve tissue, causing it to be destroyed.
Benefits of Radiofrequency Ablation
Minimally invasive: The procedure of RFA is a lot less invasive as compared to the usual surgeries—often with just a small skin incision.
Quick recovery: Most patients have minimal downtimes after RFA, resuming their day-to-day activities within a relatively short time.
Long-lasting pain relief: For most patients, RFA provides long pain relief and improves their overall quality of life.
Effective for a range of pain conditions: RFA can be applied for a wide variety of chronic pain conditions, such as the following:
Back pain
Neck pain
Facet joint pain
Osteoarthritis pain
Neuropathic pain
Safe and effective treatment modality: RFA is a well-established procedure with a very high success rate and negligible risks.
Who is the ideal candidate for RFA?
People suffering from chronic pain: You could be a good candidate for RFA if one has been suffering from chronic pain, and other treatments are not effective enough.
Patients for Whom Other Treatments Have Been Tried: The RFA procedure is considered for patients who have tried different medications, physical therapy, and other pain management techniques without substantial relief.
General good health: Although RFA is a generally safe procedure, there is a necessity for a person to be in the best general health condition before undergoing RFA.
Radiofrequency Ablation for Back Pain
The final and most common effect could be back pain, which may significantly impact every activity an individual carries out. When all other conservative modes of treatment have been tried, Radiofrequency Ablation for Back Pain is considered
Diagnosis of the origin of the pain in the back: A Radiofrequency Ablation Specialist shall carefully evaluate the symptoms and medical history for identifying the exact nerve causing your backache.
The RFA procedure targets the pain-carrying nerve itself: Inserting a needle in the region of the spine where the affected nerve responsible for pain signal generation lies. Radiofrequency energy stops the pain signals transmitted by the nerves.
Possible benefits of RFA in back pain: It does alleviate lower back pain considerably and thus enables them to go about their activities with a lot less discomfort. It may also help reduce reliance on pain medications.
RFA Procedure specifics for Chronic Pain
RFA for chronic pain is a treatment that can be centered towards the needs of a patient.
Preparation for the test: You will be requested to provide your history and current medications. You may be asked to fast for a certain period of time before the test.
The procedure itself: The RFA is usually performed in an outpatient setting or a clinic. It involves the use of any image guidance to thread a needle at the injured nerve, followed by radiofrequency energy delivery.
Post-procedure care: You might be kept under observation for a short while after the procedure before being sent home. You will also be given thorough instructions on post-procedure care, such as wound care and any further check-ups that may be required.
Pain Management Solutions in Chicago
Radiofrequency Ablation may prove particularly useful if one is searching for Chronic Pain Management Solutions in Chicago.
Experienced specialists: Chronic Pain Management Specialists in Radiofrequency Ablation in Chicago possess extensive experience in providing the best treatment plans to the patients through comprehensive consultations & ongoing support.
Advanced facilities: We are equipped with the latest technological infrastructure to perform such RFA procedures.
Pain management services: Our comprehensive services include pain management, but are not limited to RFA only, we also provide pharmacological treatment, physical therapy, & other interventional procedures for pain.
Conclusion
Chronic pain could drain your energy in day to day life, but RFA promises to be an answer. Minimally invasive, it gives durable pain relief sans heavy surgical burdens and addictive medicines. Consult a Radiofrequency Ablation Specialist today and find out more about this innovative therapy that could help you take back your life.
#Neuropathic Pain Chicago#Injections & Blocks Specialist#Neuropathic Pain Treatments in Chicago#Radiofrequency Ablation Specialist#Kyphoplasty Specialist#kyphoplasty Surgeons Near Me#Spinal Cord Stimulation Specialist#Sacrix SI Joint Fusion Treatment#Vertiflex Superion Specialist#Aurora ZIP Procedure#ZIP Procedure for Chronic Back Pain#ZIP Spine Procedure#ZIP Procedure for Spinal Stenosis#Fibromyalgia Specialist Chicago#Spinal Compression Fracture Treatment Chicago#Vertiflex Superion Procedure#Dorsal Ganglion Root Stimulation#Pain Specialist Chicago#DRG Treatment#Chronic Pain Treatment in Chicago#Lumbar Spinal Stenosis Surgery Chicago#DRG Stimulation Procedure#Pain Management Specialists Chicago#DRG Stimulator Surgery
0 notes
Text
#Interventional Pain Specialist#Injections Block Specialist#kyphoplasty Specialist#Neuropathic Pain Specialist#Pain Management Specialist Houston#Chronic Pain Specialist#Pain Medicine Specialist Houston#Pain Specialist Near Me#Radiofrequency Ablation Specialist#Spinal Cord Stimulation Specialist#Pain Management Clinic Houston#Lumbar Radiofrequency Ablation Specialist#Neuropathic Pain Treatment Texas#Back Pain Doctors#Chronic Pain Treatment Clinic#Back Pain Doctors in Houston#Spinal Cord Stimulation Treatment Houston#Compression Fracture Treatment Texas#Pain Management Services Houston#Spinal Stimulator Trial Procedure#Back Pain Treatment Near Me#Spinal Compression Fractures Specialist#Spinal Cord Stimulator Trial#Work Injuries Treatment#Injury Pain Specialist#Chronic Pain Management Near Me
0 notes
Text
Migraine isn’t a Headache Part Six: make it stop
We looked at medication and treatment for acute attacks of migraines. Things that you can do to treat the pain when you're having it.
This is also probably the first line of help you'll get from a GP or pharmacist or whoever you approach for help.
Some people have success with acute treatments. Maybe the migraine was a one-off, or is a rare occurrence, maybe it was just really responsive to acute meds.
Some people have migraines that don't respond to acute meds, or don't respond well enough to be considered effective treatment.
When you get to this stage, you need to start looking at stopping the migraines before they start, instead of constantly taking acute meds that a) don't work and b) can cause rebound headaches and other problems.
It sucks, because you want to reach for the painkillers when you have pain, but doing so is not sustainable.
Getting into preventative meds ties in a lot with how you go about getting a diagnosis, but I'm going to try to speak about the meds and complimentary treatments AROUND being under a neurologist. On that note, GPs are rarely going to work with you on preventative meds.
There are a few they can prescribe, but you'll probably get better treatment under a neurologist or headache specialist. Sorry.
GPs are useless.
Sorry, bit of my bias there, but I don't use GP's unless I need a referral or quick acute treatment, and EVEN THEN.
It's worth noting as well that you'll usually only get to this stage if your migraines have become chronic, that is:
for over 3 months
you've had 15 headache days a month minimum
of which 8 have migraine features
Some of the treatments aren't indicated for episodic migraines.
((As previously mentioned, this definition might be changing to take into account the impact migraines are having on your life, and not a somewhat arbitrary number; fingers crossed this happens soon))
My list of attempted treatments includes:
amitriptyline (this is one the GP might prescribe for you) (also prescribed for abdominal discomfort and major depressive disorder, although it's fallen out of favour due to increased risk of fatality in overdose)
propranalol (and this) - beta blocker
flunarizine (calcium channel blocker, used to treat high blood pressure and certain heart conditions)
lamotrigine (usually prescribed for epilepsy and bipolar disorder)
topiramate (usually prescribed for seizures)
candesartan (usually prescribed for hypertension)
pregabalin (usually prescribed for seizures and anxiety)
gabapentin (usually prescribed as an anticonvulsant and for nerve pain)
Botox injections
greater occipital nerve blocks
Magnesium/CoenzymeQ10/Vitamin B trio
Aimovig (erenumab, CGRP injection, one of the first migraine-only treatments)
Ajovy (fremanezumab, another CGRP injection, one of the first migraine-only treatments)
sTMS machine (single pulse transcranial magnetic stimulation)
Vyepti (eptinezumab-jjmr IV infusion, another CGRP drug)
I don't think I've had EVERY drug available for migraine prophylaxis, but judging by the increasingly surrendering tone of the letters from my neurologist, I'm just about there.
As you can see, apart from the last CGRP drugs, almost every drug listed is used off licence for migraines, and none of them were developed to treat migraine at all.
You can group most of these drugs into treatment for blood pressure, epilepsy and mental health issues.
The idea that migraines are mainly caused by blood pressure has kind of aged out with advances in research, but the fact remains that some medication that acts on blood pressure still helps migraines.
I think, bearing in mind that a migraine is a neurological storm, that it makes sense that meds that act on activity in the brain (mental health meds/epilepsy meds) can help migraine. Makes logical sense, right?
The usual procedure for taking these medications for migraine (at least in the UK) is to titrate up to the correct dose, and then (assuming you tolerate it and don't get floored by adverse reactions or the side effects) remain on that dose for 3 months before concluding if the medication is successful or not.
If you're seeing some improvement but not a lot, they might keep you on it for longer, or increase the dose.
Otherwise, 3 months and no improvement means you move onto the next drug and/or treatment.
A lot of these drugs have some really heavy side effects. I've experienced worsened tremors, awful dizziness, change in sense of taste, changes in appetite, terrible brain fog.
For migraineurs it comes down to a balancing act.
How bad are the side effects vs how much is this med helping my migraines, and which of the two am I best able to handle.
Maybe you can manage dizziness or not being able to drink Coke anymore over the migraines.
Maybe the awful tremors and inability to think clearly is worse than bearing with the migraines.
This is usually something you discuss with your specialist.
Just saying again, some of these meds are a little hardcore. Don't try treating your own migraines on your own with these meds if you can get your hands on them somehow. Apart from the side effects, the dose if really important too.
In the UK, if you've failed at least three preventative treatments, and have been managed for medication overuse headaches, you can try botox.
BOTOX
The reason botox works for migraines isn't well known, but doctors think it blocks pain transmitters in your brain.
Botox, or botulinum toxin, is a nerve toxin that paralyses muscles.
It's used for cosmetics treatments, but also medically for hemifacial spasm, cervical dystonia, cerebral palsy, bladder pain, lower back pain, neuropathic pain and stroke.
When used for migraine, it's delivered in a series of 31 to 39 small injections, mostly around the forehead, but also on the temples and at the base of the skull.
If you've ever had acupuncture, the needles are a lot like that. I thought they'd hurt more than they did. They were just little stings, not even as bad as plucking an eyebrow hair. Of course, everyone's different with different pain thresholds (especially if you're oversensitised migraine pain leaves you with allodynia) but it's truly not that bad.
You get three sessions 12 weeks apart, just like taking the meds, and if you've had improvement you can continue. If you don't, its on to the next med or treatment.
It feels weird when it settles in. Your forehead tends to freeze, so you can raise your eyebrows and have no lines there. This might unsettle some people, but it does wear off over time.
Side effects include neck pain, muscular weakness and a drooping eyelid, but these improve as the botox wears off. I had a little neck pain, but nothing else. One of them in my forehead bled only a little, none of the rest did.
You can have an allergic reaction, but they will keep you in the treatment or waiting room for some time after your first treatment to check that.
Getting botox for migraine sounds worse than the experience is, but it is about 75% successful for reducing migraine.
Not for meeee
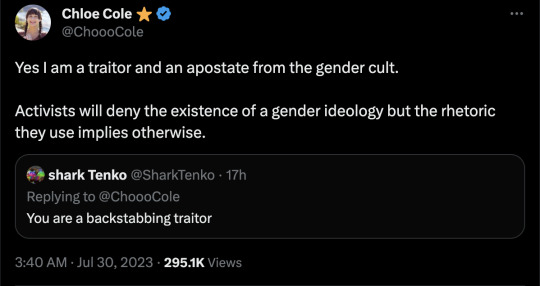
GREATER OCCIPITAL NERVE BLOCKS (GONB)
If your migraines have been resistant to drug treatments and botox, your specialist might decide to try GONB. This is usually a treatment for cluster headache or headaches that originate from pain in the neck, so it may not be applicable to your specific situation.
This treatment involves injecting an anesthetic and a steroid (not always both) into the back of your head/top of your neck around the greater occipital nerve (GON).
The GON runs from the top of the spine to the scalp, and feeds into an area of the brainstem called the trigeminal nucleus.
A nerve block reduces traffic in this nerve, so reduces the amplification of pain and other sensory information that might be overloading this area.
In simple terms, the nerve block stops the pain signals going into the nerves that make you feel the headache.
A lot of people have had success with this treatment, but I'm not one of them.
I don't want to scare anyone!
The reaction I had is (apparently) pretty rare.
After the neurologist injected the first lot of lidocaine into one side of my head, then the other, I almost immediately felt dizzy and sick.
He let me lay down for a moment, but I felt that I was going to puke, so I had to get up. What followed was tunnel vision, greying out, nearly full syncope (fainting) and then vomiting.
I was having a reaction to the lidocaine, which suddenly made my nausea and faintness when I had my lumbar punction (spinal tap) make sense.
I wasn't able to get to the stage where I had the steroid injection, and whatever there was of the anesthetic after my body tried to purge it made no change to my migraines.
I can't speak for the efficacy of the GONB because my body failed it, but if it's offered, I'd encourage you to try it. Apparently it has helped a lot of people.
CGRPs
After trying 3 meds, then botox, then the GONB and failing all of them, I was put on the next med to see if I'd respond to any of them.
You don't need to have exhausted every pill before trying injection treatments. You can also mix and match treatments, especially a pill or a CGRP with botox.
With the knowledge that you spend a minimum of 3 months per med (and assuming you don't come off it immediately due to adverse reactions) you can only go through 4 meds in one year. It takes two years on this schedule to go through the meds I've worked through, not including the botox and GONB, and the extra time taken to titrate to the correct dose.
Finding a medication that works to prevent your migraines is a long and exhausting process.
Thankfully, recent research into migraine has come out with the biggest breakthrough in migraine management, I'm going to say ever, because we now have the first medication created directly for the prevention of migraines.
CGRP stands for Calcitonin Gene-Related Peptide
It's a chemical involved in transmitting pain signals through the nervous system – and it’s also associated with the triggering of migraine attacks (among others).
CGRP medications are actually ANTI-CGRP drugs, designed to stop the action of the chemical.
The ones currently available in the UK fall into two groups.
Aimovig (erenumab) that works by binding to the receptor.
Ajoy (fremanezumab), Emgality (galcanezumab) and Vyepti (eptinezumab) which bind to the protein.
Because of that, if you don't have success with Aimovig, try one of the others (and vice versa) as you might see some improvement.
These are adminstered by self-injection (although the first one will be done under nurse supervision) every month with something like an epipen that's injected into your thigh.
The injections hurt me and ached afterwards, but I had no other side effects than that.
I actually had one migraine day where my pain was a 3, which hadn't happened since I started having migraines, but unfortunately, NHS guidelines state that you need to have a reduction in pain days or a significiant reduction in pain in order to stay on them, so I was taken off.
We've just had Vyepti (eptinezumab-jjmr) approved for some people with migraine in the UK.
Vyepti is a CGRP administered via IV infusion over 30 minutes at a clinic, and it's still such a new drug that they're still collecting information on side effects, etc.
I've had my first dose (they're given every 3 months) and while I didn't see a reduction in pain days, I saw maybe a slight reduction in pain, but more than that, my brain fog and pain cloudiness really cleared up, at least for the first month and a half that the effect lasted.
I was actually present in my body for once, instead of half-checked out, even if I was still in pain.
I don't know what the review will bring, but I hope they let me stay on it.
In the US, they've also got a new group of drugs called -gepants (Ubrogepant, Atogepant and Rimegepant for now) which are being used preventatively, but also like triptans, acutely.
Like the injections, they also work on the CGRP receptors by blocking their effect.
I don't know very much about them, but they're also some of the first drugs made specifically for migraine, and there's a lot of excitement about them.
They're safer than triptans for people with heart issues to take, and they DON'T CAUSE REBOUND HEADACHES!
This is huge in the world of migraine treatment, as there are no other acute treatments that do this.
NON MEDICINAL
A large chunk of preventative non-medicinal treatments for migraine involve making lifestyle changes (I know)
The migraine brain is oversensitive and overreactive creature, and ANYTHING can push it into a tantrum. Weather changes, temperature changes, lights, sounds, smells, so many things that we can't control in our environment.
Our migraine brains love routine, and even though it's annoying and removes some chunk of flexibility in our lives, it annoyingly does help.
Sleep routines are helpful, as much as you can fit yourself into one. Setting sleep and wake alarms with x amount of hours in between (7 or 8?) and then sticking to them rigidly means that you'll be getting up when you're still sleepy and going to bed when you're not, but your body will eventually fall into a rhythm and you'll find yourself sleeping and waking at those times automatically.
Issues: daytime naps are no good for sleep routines, and sometimes you just HAVE to sleep when a migraine hits. What if you want to stay up on the weekend? It's difficult, but keeping to a schedule as much as possible is better than leaving it in the wind.
Eating regularly, small meals often is the best. I'm not going to spend a lot of time on this because diet is a huge and sensitive subject, and comorbidities can make this even more difficult, but as far as migraines on their own are concerned, they like the body to be kept as stable as possible, which means a level blood sugar level, etc, and avoiding hunger.
Exercise? I know, I'm not going there, apart from, gentle stretches for your neck, maybe your back, can help. Even if neck problems have nothing to do with your migraines, you're going to end up all crunched up and tense from being in constant pain. Look at stretches for post-operative, for the elderly, for anything you can do in bed. It doesn't have to be high impact or intense, just something you can do now and again to keep your muscles loose.
H~y~d~r~a~t~i~o~n. I'd say use a pretty bottle, but honestly, using whatever will make it easier for you to fill and keep drinking from is better than something that fits your aesthetic. You can always decorate a plastic bottle, or use a favourite glass.
Apart from all those irritating things that abled people always recommend (yoga anyone?) there are also non-drug but prescribed treatments.
One category is DEVICES
I've only tried the sTMS device, so I'll address that first.
sTMS stands for single pulse transcranial magnetic stimulation
You press the button to charge the thing. When it beeps you place the bean-shaped device at the back of your head so it cradles your skull, and then press both buttons at the same time.
There's a ka-chonk, and a sensation like someone's smacked you in the back of the head a little, which is actually the small magnetic pulse.
It works by generating mild electrical currents in the brain that are supposed to disrupt the brain activity linked to your migraines. You can use it acutely, but also daily (2 or 3 times a day, 1 or more than 1 pulse at a time) to prevent migraines.
The machine didn't do anything for me, and made my scalp feel a little sore, although that doesn't appear to be common.
You may also have heard of the Cefaly, a device otherwise called a 'external trigeminal nerve stimulator'
There's that trigeminal nerve again, running around the side of your face and your eye, playing up and causing pain.
You place an electrode on your forehead, and the Cefaly generates micro-impulses to stimulate the trigeminal nerve's nerve endings.
Be aware that the efficacy of the Cefaly device is debated, but it does help some people.
ACUPUNCTURE has been used to help migraine
I had many courses via my GP (the only good one I had) who was trained in acupuncture and went above and beyond to give me as many treatments as possible. I think I had 12. I felt something from them, but they didn't have any effect on my migraines.
Finally, not a drug per se, but VITAMIN SUPPLEMENTS
The best are a trio as follows:
Riboflavin 400mg once daily
Co-enzyme Q10 100mg three times a day and Magnesium (there are two/three types and the doses are different)
Citrate 600mg OD
Tricylicate 250mg twice a day
or Phosphate 400mg once daily
There is also therapy that is prescribed for management of migraine, not so much prevention as just giving you tools to learn to live with being in pain.
I haven't gotten to that stage yet, and have mixed feelings about it.
Some people have said it's helped, some said it hasn't.
It -feels- a lot like being told 'we can't do anything to help you, you just have to deal with being in pain now'
I haven't tried it, I probably will end up doing so, and maybe I can write a little about it then. For now, I can see why it could be useful, but it does feel a little bit like being abandoned.
And that's all I've got for preventative treatments.
I don't know when I'll be able to start writing about my diagnosis journey, but that should be the next part.
please excuse any typos!
i hope this is still helpful for some people.
#migraine isn't a headache#migraine#disability pride month#migraine awareness#chronic pain#spoonies#headache#preventative meds#migraine medication#migraine treatment
11 notes
·
View notes
Text
In-Vitro-Fertilization : IVF Treatment
Starting the journey towards parenthood can be a challenging road for couples facing infertility issues. In vitro fertilization (IVF) has emerged as a beacon of hope, providing a pathway for those struggling to conceive naturally.
Understanding IVF or in vitro fertilization is a complex medical procedure that involves fertilizing an egg with sperm outside the body. This process offers a solution to a range of fertility issues, including blocked fallopian tubes, male infertility, or unexplained fertility problems. IVF has witnessed significant advancements since its inception, becoming a widely accepted assisted reproductive technology.
The IVF process typically begins with ovarian stimulation, where fertility medications are administered to stimulate the ovaries to produce multiple eggs. These eggs are then retrieved through a minor surgical procedure. In the laboratory, the eggs are fertilized with sperm and the resulting embryos are monitored for a few days. The healthiest embryos are selected and transferred into the woman's uterus to establish a pregnancy.
Success rates for IVF can vary and are influenced by factors such as age, the cause of infertility, and the quality of the eggs and sperm. It's essential for couples considering IVF to have realistic expectations and to work closely with their fertility specialists to understand the potential outcomes.
One of the critical aspects of IVF treatment is the emotional and psychological toll it can take on individuals and couples. The journey is often filled with hope, anxiety, and a rollercoaster of emotions. Recognizing the emotional aspects, many fertility clinics offer counseling and support services to help individuals navigate the challenges of IVF.
The cost of IVF treatment is another consideration for many couples. IVF can be a significant financial investment, and costs may include medications, procedures, and laboratory fees. It's crucial for couples to discuss the financial aspects with their healthcare providers and, in some cases, explore available insurance coverage for fertility treatments.
Here are the important links about IVF Treatment from various Platforms :
https://shivamivfcentredelhicom.wordpress.com/2023/12/08/ivf-and-infertility-centre-in-delhi/
https://www.tumblr.com/shivamivfcentredl/736129064951300096/ivf-and-infertility-centre-in-delhi
https://medium.com/@shivamivfcentredelhi/ivf-and-infertility-centre-in-delhi-f36e467a3c61
https://qr.ae/pKOHH5
https://qr.ae/pKOHHm
https://qr.ae/pKOHPg
https://qr.ae/pKOHHb
https://shivamivfcentredelhicom.wordpress.com/2023/12/08/ivf-and-infertility-specialist-in-delhi/
https://www.tumblr.com/shivamivfcentredl/736134209628962816/ivf-and-infertility-specialist-in-delhi
https://medium.com/@shivamivfcentredelhi/ivf-and-infertility-specialist-in-delhi-688366976ae2
https://qr.ae/pKOowb
https://qr.ae/pKOowH
https://qr.ae/pKOobi
https://qr.ae/pKOobN
https://qr.ae/pKOowr
In recent years, advancements in technology and medical research have paved the way for additional options within the realm of IVF. Techniques such as intracytoplasmic sperm injection (ICSI), preimplantation genetic testing (PGT), and egg freezing have expanded the possibilities for couples undergoing IVF, offering more personalized and targeted approaches to fertility treatment.
While IVF has provided a successful path to parenthood for many, it's important to note that it may not be the right solution for everyone. Fertility specialists work closely with couples to assess individual circumstances, explore alternative treatments, and provide guidance on the most suitable course of action.
In conclusion, IVF treatment stands as a remarkable advancement in reproductive medicine, offering hope to couples facing infertility challenges. The intricate process, coupled with emotional considerations and financial aspects, requires a comprehensive approach. As technology continues to evolve, the landscape of IVF treatment expands, providing more options and opportunities for those on the journey to building a family.
#ivf treatment#ivf#in vitro fertilization#iui treatment#infertility#infertility treatment#fertility#fertility treatment
3 notes
·
View notes
Text
Physical Therapy Clinic in New York City
Ehlers-Danlos Syndrome (EDS) is a group of rare genetic connective tissue disorders that affect the body's ability to produce collagen, a key protein that provides strength and elasticity to various tissues. People with EDS often experience a range of symptoms, including hypermobility of joints, skin that is easily bruised and hyper-elastic, and various complications related to weak connective tissues.
Pain management for individuals with Ehlers-Danlos Syndrome can be complex and require a multidisciplinary approach involving medical professionals such as rheumatologists, geneticists, pain specialists, physical therapists, and more. Here are some strategies that might be considered:
Medications: Depending on the type and severity of pain, various medications might be prescribed. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage joint and muscle pain. For more severe pain, opioid medications might be considered, though their use should be carefully monitored due to the risk of addiction.
Physical Therapy: Physical therapy can be extremely beneficial for individuals with EDS. A physical therapist can provide exercises to improve joint stability, strengthen muscles, and enhance overall body mechanics. Aquatic therapy might be particularly useful due to the buoyancy of water reducing stress on joints.
Bracing and Assistive Devices: Depending on the specific type of EDS and its impact on joints, bracing or assistive devices might be recommended to provide support and reduce strain on joints.
Pain Management Techniques: Techniques such as heat or cold therapy, massage, and acupuncture might provide some relief for certain individuals.
Lifestyle Modifications: Adopting a healthy lifestyle can help manage pain. Maintaining a healthy weight can reduce stress on joints, and staying active within the limits of what your body can handle can also be beneficial.
Counseling and Psychological Support: Chronic pain can have a significant psychological impact. Counseling, mindfulness, and relaxation techniques can help individuals cope with the emotional aspects of managing pain.
Nutrition and Supplements: A balanced diet rich in nutrients that support collagen production, such as vitamin C, might be helpful. Consultation with a medical professional or registered dietitian is recommended before making significant dietary changes or starting supplements.
Pain Management Specialists: Depending on the severity of pain, a pain management specialist might be consulted. They can provide more advanced interventions like nerve blocks, epidural injections, or other specialized treatments.
Genetic Counseling: Since EDS is a genetic disorder, individuals and families might benefit from genetic counseling to better understand the condition, its inheritance pattern, and potential implications for family planning.
It's important to note that each individual's experience with EDS and their pain management needs can vary widely. A personalized approach that takes into account the specific type of EDS, its symptoms, and the person's overall health is crucial. Always consult with qualified medical professionals who are experienced in dealing with Ehlers-Danlos Syndrome for proper guidance and treatment.
Types of EDS
The Ehlers-Danlos syndromes are a group of genetic connective tissue disorders that are currently classified into a system of thirteen types. Despite this grouping and their common name, each type is a distinct condition caused by a different gene mutation. This means that a child cannot inherit a different type of EDS from the one their parent has. It also means that one type cannot later turn into another, and there is no increased risk of having another type just because you have one – they are simply not connected. It is also extremely unlikely that one person would have more than one type, given the rarity of most of these illnesses.
Recently some of the criteria used to diagnose the Ehlers-Danlos syndrome and some of the terminology describing them changed, in order to reflect scientific research from the past twenty years. The 2017 EDS International Classification recognizes thirteen types of EDS and defines for the first time some related conditions, hypermobility spectrum disorders (HSD) which have similar symptoms to hypermobile EDS (hEDS). The term joint hypermobility syndrome (JHS) is no longer used.
The most common type of EDS is thought to be the hypermobile type (formerly known as the hypermobility type or type 3) although the exact prevalence of this condition is not currently known. The medical literature states that it affects 1 in 5,000 people however this statistic is based on research that is out-of-date and hEDS/HSD frequently go undiagnosed or are misdiagnosed as other conditions. HSD and possibly hEDS are likely to be common. The classical and vascular types are rare, with other types being rarer still. It is probable that all the types are underdiagnosed to some degree.
#physical health#physical therapy#ehlers danlos syndrome#ehlers danlos syndrome physical therapy#hypermobile ehlers danlos#ehlers danlos syndrome threatment#physical therapy for ehlers danlos syndro
2 notes
·
View notes
Text
Can Sciatica Pain Be Treated Without Surgery?
Sciatica pain goes down the back to the thigh and the legs and causes extreme shooting pain. The reason can be irritation of one or more of the lower spinal nerves, and the pain may be mild discomfort and sometimes deep developing pain.

It is good to know that if you treat sciatica on time and use conservative methods to treat it, you will get relief within a few weeks and without surgery.
Improving your back core and strengthening it can relieve sciatica pain.
While some doctors may suggest surgery as a treatment for sciatica after noninvasive measures have failed.
Nonsurgical treatments may include a longer recovery. Talk to your doctor about sciatic back pain treatment, and your doctor will determine the best treatment for you.
Chiropractic, massage, and acupuncture therapies
Alternative sciatica therapies may also help with pain management. A chiropractor can adjust your spine to facilitate better spinal function, stimulate spinal mobility, and relieve pain. Chiropractic care can help cure sciatica-related lower back pain, but it works less well for radiating pain.
You may have stiff muscles because of your sciatica discomfort. Pain-managing chiropractic can make your muscles more flexible and mobile with massage therapy. It can also aid with pain relief. According to the research, acupuncture can be effective in treating sciatica. Visit a certified back pain doctor Clifton or an acupuncturist if you need the practice.
Medications
The initial line of therapy for sciatica pain is routine physical treatment. But your doctor might advise you to take medications if your symptoms don't go out. Your doctor may prescribe some common types of drugs for sciatica pain, including:
anti-inflammatory drugs
muscle relaxants
Narcotics
Anti-inflammatory drugs can decrease inflammation and sciatica signs. They also contain COX-2 inhibitors, which block hormones and stop the pain.
Narcotics and muscle relaxants help soften the muscles that sciatica has caused to become tight. Steroid injections into the epidural space also help to reduce the pain. This process involves inserting a corticosteroid and numbing anesthetic into the gap between two vertebrae.
Use cold and heat to relieve sciatica pain.
The use of a cold pack can help in relieving the beginning of sciatica pain. Apply a cold pack, or you can use a frozen peas pack, use a towel and apply it directly to the painful area.
Applying a cold pack can relieve you when you first start experiencing sciatica pain. Cover a cold pack or a bag of frozen peas in a towel, and use it on the hurting area a few times a day for up to 20 minutes. This will ease the pain and will give you relief.
You can try a hot pad instead if the cooling pad doesn't give the desired results. Put the heating pad on the affected area a few times a day. If you see some changes in the pain, use both hot and cold pads on alternative days.
Contact your back pain specialists in the woodland if you do not get relief from both.
Viewpoint
Sciatica pain is a threat and makes everyday life more challenging with it. But some treatments can cure it, and the treatments effectively reduce symptoms. Contact your back pain specialist Clifton to determine which sciatic nerve pain treatments are best for you.
Article Source : https://www.articleapprove.com/can-sciatica-pain-be-treated-without-surgery/
2 notes
·
View notes
Text
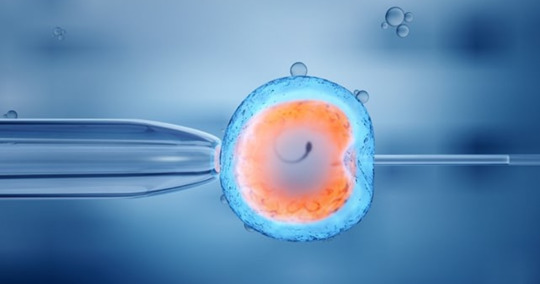
How do experts perform IVF treatment in Nepal that blesses couples with their children?

IVF treatment in Nepal is a simple fertility procedure that consists of six steps, and these are:
1. Stimulation: During stimulation, a specialist gives a woman fertility drugs to increase the number of mature and healthy eggs in one cycle. When performing stimulation, a fertility specialist examines a woman's ovaries using ultrasound and blood tests to check hormone levels.
2. Egg retrieval: In this step of IVF in Nepal, the specialist gives the woman medication to help ease her discomfort. The specialist performs local anaesthesia, and the ovarian follicles are aspirated with a needle guided by transvaginal ultrasonography. An experienced embryologist scans a woman's follicular fluids to find available eggs in her ovaries. Then these eggs are placed in a unique medium and cultured in an incubator until insemination.
3. Fertilization and Insemination: It is the step of IVF in Nepal, where the male member's sperm is placed together with the female's eggs. The joining of sperm and egg is known as insemination, and fertilization occurs after 16 to 18 hours of insemination.
4. Embryo Cultivation: It is a step of IVF Nepal where the specialist regularly checks that the embryo's growth is done correctly. Within five days, a normal embryo has several cells that are actively dividing. The entire procedure gets performed after 3 to 4 days of fertilization. A couple can opt for PGD to help them decide which embryo to implant and reduce the chance of passing the disorder on to the child.
5. Embryo transfer: During embryo transfer, the fertilized embryo will get implanted into the woman's uterus 3 to 5 days after egg retrieval and fertilization. The specialist will insert a thin tube that contains the embryo into the woman's vagina, through the cervix and up into the uterus. If the embryo gets adequately placed in the lining of the woman's womb, it grows and a pregnancy results.
6. Pregnancy test: After two weeks of embryo transfer, the couple must take a pregnancy test performed by a specialist using ultrasound. They scan the woman's ovaries to hear the baby's heartbeat, and once they can hear, it means the pregnancy is confirmed. The patient can be discharged from the fertility clinic to the local gynaecologist.
What conditions can be treated with IVF treatment in Nepal?
Below are the conditions that can be treated with IVF treatment in Nepal. These are:
1. Blocked or Damaged Fallopian Tubes: Women dealing with blocked or damaged fallopian tubes can have a baby with IVF in Nepal.
2. Problems with ovulation: If women have problems with ovulation, then fertility experts recommend drugs like Metformin and Clomiphene during IVF treatment. Metformin is recommended for women with polycystic ovary syndrome (PCOS), and Clomiphene is given to infertile women to help stimulate the ovaries. They can produce enough eggs for fertilization.
3. Unexplained Infertility: Unexplained infertility is a problem where fertility experts have been unable to find the root cause after a medical examination; in such cases, the fertility specialist gives women drugs such as Clomiphene, hormone injections and insemination.
4. Male Infertility Problems: If the male partner cannot produce enough sperm for fertilization, in such cases, experts surgically extract the sperm from the male ejaculate and fertilize it with a female egg to facilitate fertilization.
5. Decline in Ovarian Reserve: Women above 35 face problems with ovarian reserve as there is a decline in the stars. For these women, IVF in Nepal is the best option to increase the chances of conceiving at an increasing age.
How successful is IVF in Nepal?
IVF Nepal success rate is around 60-70% for women under 35, which is relatively high compared to other infertility clinics in Nepal. However, the success rate depends on the couple's age, causes of infertility, previous medical history, etc. The clinic's success rate is high because fertility experts use the latest and advanced technology to treat infertility problems and give their best to achieve a successful result in one fresh IVF cycle without any complications for the mother and child.
1 note
·
View note