#hiv +
Explore tagged Tumblr posts
Link
Referred to as "the Dusseldorf patient" to protect his privacy, researchers said he is the fifth confirmed case of an HIV cure. Although the details of his successful treatment were first announced at a conference in 2019, researchers could not confirm he had been officially cured at that time.
Today, researchers announced the Dusseldorf patient still has no detectable virus in his body, even after stopping his HIV medication four years ago.
49K notes
·
View notes
Text




Source
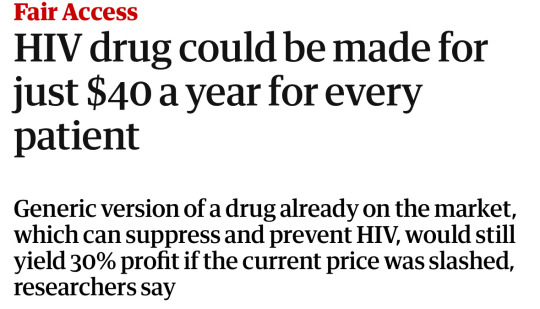
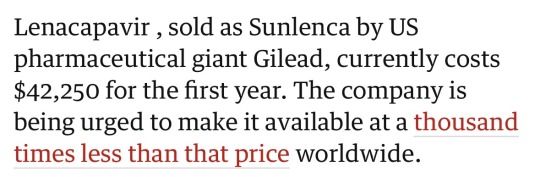
This entire article is worth the read. Fuck Gilead
#big pharma#hiv#hiv/aids#the left#news#current events#health#health care#capitalism#public health#corporate greed
46K notes
·
View notes
Text
Happy birthday, Duane.

#Duane Kearns Puryear#HIV/AIDS#queer history#AIDS Memorial Quilt#Duane died in 1991#He’d be 59 this year
37K notes
·
View notes
Text




In the midst of that amazing time in my life came the worst, and that was when my friends just started dropping dead. They were sick today and dead tomorrow. And when you would go to the hospital to look for you friend they would be out in the hallway on a gurney pushed up against a wall dying for help, dying for love, dying to be saved. And some of them with that sign on their gurney that said "do not touch". And they suffered, and people wanted to act like they weren't good people, kind people, wonderful people, somebody's son, somebody's daughter, somebody. // SHERYL LEE RALPH receiving the Human Rights Campaign's National Ally for Equality Award 2022. (x)
26K notes
·
View notes
Text

"We all deserve the right to protect and keep ourselves safe. Implementing a mask ban is not only an infringement on our human rights but also extremely ableist and inconsiderate of those disabled or immunocompromised.
. . .
About 1 in 5 adult New Yorkers have a disability. If a mask ban were to be implemented, spaces such as stores and restaurants might ban masking or set up mask-removal policy. That’s 1 in 5 adults no longer able to shop in public along with others, or participate in gatherings.
Forcing immunocompromised people to remove their face masks would likely violate the federal Americans with Disabilities Act and the New York State Human Rights Law. As a member of ACT UP NY, it’s always my goal to fight for human rights such as healthcare.
Those that are HIV+ are 8% more likely to be hospitalized due to COVlD than those that aren’t and are also at an increased risk of developing Long COVlD.
Masking SAVES LIVES. Masking is community care.”
Behind the Powecom KN95 is Serita @_seritasargent_ and her friend Bri’anna @lanoirede.jpg holding the #StopMaskBans sign.
MaskTogetherAmerica encourages everyone to speak up and write to elected officials to demand they oppose the anti-mask bills S9867/A10057 and S9194! We need to defend our right to masks.
3K notes
·
View notes
Text
Its 2025!
Here’s some things I think are important to remember as we go forward:
It’s never too late to get the Covid booster.
It’s never too late to get the flu shot.
It’s never too late to get tested for HIV or other STDs.
It’s never too late to start masking again.
It’s never too late to start taking care of yourself.
It’s never too late to start a new path in life.
Thanks :)
1K notes
·
View notes
Text
Fewer people contracted HIV last year than at any point since the rise of the disease in the late 1980s, the United Nations said Tuesday, warning that this decline was still far too slow. Around 1.3 million people contracted the disease in 2023, according to the new report from the UNAIDS agency. That is still more than three times higher than needed to reach the UN's goal of ending AIDS as a public health threat by 2030. Around 630,000 people died from AIDS-related illnesses last year, the lowest level since a peak of 2.1 million in 2004, the report said ahead of World AIDS Day on Sunday.
Continue Reading.
846 notes
·
View notes
Text

HIV used to be a death sentence, and a fast one. Modern medication has done wonders to bringing people's life expectancy back to normal, decreasing transmission rates and risks, and even in a handful of cases completely curing the virus. There is some good news out there.
662 notes
·
View notes
Text
"A large clinical trial in South Africa and Uganda has shown that a twice-yearly injection of a new pre-exposure prophylaxis drug gives young women total protection from HIV infection.
The trial tested whether the six-month injection of lenacapavir would provide better protection against HIV infection than two other drugs, both daily pills. All three medications are pre-exposure prophylaxis (or PrEP) drugs.
Physician-scientist Linda-Gail Bekker, principal investigator for the South African part of the study, tells Nadine Dreyer what makes this breakthough so significant and what to expect next.
Tell us about the trial and what it set out to achieve
The Purpose 1 trial with 5,000 participants took place at three sites in Uganda and 25 sites in South Africa to test the efficacy of lenacapavir and two other drugs.
Lenacapavir (Len LA) is a fusion capside inhibitor. It interferes with the HIV capsid, a protein shell that protects HIV’s genetic material and enzymes needed for replication. It is administered just under the skin, once every six months.
The randomised controlled trial, sponsored by the drug developers Gilead Sciences, tested several things.
The first was whether a six-monthly injection of lenacapavir was safe and would provide better protection against HIV infection as PrEP for women between the ages of 16 and 25 years than Truvada F/TDF, a daily PrEP pill in wide use that has been available for more than a decade.
Secondly, the trial also tested whether Descovy F/TAF, a newer daily pill, was as effective as F/TDF...
The trial had three arms. Young women were randomly assigned to one of the arms in a 2:2:1 ratio (Len LA: F/TAF oral: F/TDF oral) in a double blinded fashion. This means neither the participants nor the researchers knew which treatment participants were receiving until the clinical trial was over.
In eastern and southern Africa, young women are the population who bear the brunt of new HIV infections. They also find a daily PrEP regimen challenging to maintain, for a number of social and structural reasons.
During the randomised phase of the trial none of the 2,134 women who received lenacapavir contracted HIV. There was 100 percent efficiency.
By comparison, 16 of the 1,068 women (or 1.5%) who took Truvada (F/TDF) and 39 of 2,136 (1.8%) who received Descovy (F/TAF) contracted the HIV virus...
What is the significance of these trials?
This breakthrough gives great hope that we have a proven, highly effective prevention tool to protect people from HIV.
There were 1.3 million new HIV infections globally in the past year. Although that’s fewer than the 2 million infections seen in 2010, it is clear that at this rate we are not going to meet the HIV new infection target that UNAIDS set for 2025 (fewer than 500,000 globally) or potentially even the goal to end Aids by 2030...
For young people, the daily decision to take a pill or use a condom or take a pill at the time of sexual intercourse can be very challenging.
HIV scientists and activists hope that young people may find that having to make this “prevention decision” only twice a year may reduce unpredictability and barriers.
For a young woman who struggles to get to an appointment at a clinic in a town or who can’t keep pills without facing stigma or violence, an injection just twice a year is the option that could keep her free of HIV.
What happens now?
The plan is that the Purpose 1 trial will go on but now in an “open label” phase. This means that study participants will be “unblinded”: they will be told whether they have been in the “injectable” or oral TDF or oral TAF groups.
They will be offered the choice of PrEP they would prefer as the trial continues.
A sister trial is also under way: Purpose 2 is being conducted in a number of regions including some sites in Africa among cisgender men, and transgender and nonbinary people who have sex with men.
It’s important to conduct trials among different groups because we have seen differences in effectiveness. Whether the sex is anal or vaginal is important and may have an impact on effectiveness.
How long until the drug is rolled out?
We have read in a Gilead Sciences press statement that within the next couple of months [from July 2024] the company will submit the dossier with all the results to a number of country regulators, particularly the Ugandan and South African regulators.
The World Health Organization will also review the data and may issue recommendations.
We hope then that this new drug will be adopted into WHO and country guidelines.
We also hope we may begin to see the drug being tested in more studies to understand better how to incorporate it into real world settings.
Price is a critical factor to ensure access and distribution in the public sector where it is badly needed.
Gilead Sciences has said it will offer licences to companies that make generic drugs, which is another critical way to get prices down.
In an ideal world, governments will be able to purchase this affordably and it will be offered to all who want it and need protection against HIV."
-via The Conversation, July 3, 2024
#HOLY FUCKING SHIT#100% EFFECTIVE AGAINST HIV INFECTION#AND JUST TWO SHOTS PER YEAR HOLY FUCKING SHIT#THIS IS UNBELIEVABLY GAME-CHANGING#hiv#hiv aids#hiv awareness#lgbtq news#medical news#drug trials#hiv prevention#prep#uganda#south africa#aids#aids crisis#good news#hope
2K notes
·
View notes
Text







2K notes
·
View notes
Text
HIV and COVID
A major barrier to preventing the spread of HIV is accurate test results.
There is a high chance there are many people with HIV that have it and do not know. We do not know how long this undetected time period is (lentiviruses are often associated with long periods of time of virus activity that goes undetected- 5 to 10 years or more), but there is a chance many individuals with HIV go undiagnosed for many years. Individuals during this time before an HIV diagnosis complain of fatigue and many undiagnosed disabling symptoms during that time period. HIV is able to cause changes to immune cells that prevent HIV tests from finding the infection. Some people get negative HIV tests when they are HIV positive. This means you could be HIV negative, but still have HIV in your blood and can spread HIV to other individuals.
Getting a COVID vaccination (and sometimes other vaccinations like the flu vaccination) can help the body identify HIV hiding in the body. This allows earlier treatment and intervention. Once HIV has been identified, it also reduces the risk for all individuals in our population to be exposed to more severe infections.
Getting tested regularly for HIV used to be part of our federal public health recommendations.
This just further emphasizes why this information is so important to know and healthcare needs to start testing for more diseases in more people and do these tests more often.
People often assume their infection came from an unfaithful partner, but in reality HIV has been spreading unknowingly to many in the medical community and still in the public sphere no one is talking about it like the huge deal it is.
This potential means people could be raped as a child, never have sex again, never encounter drugs, and then be miserable & living with an active HIV infection into their early 20s and they would never know. Once they got a positive test result they would have no idea where the infection even came from.
Our entire understanding of these types of diseases has to change and the seriousness of this topic has to be addressed by the world. This was theorized as a mechanism of HIV spread due to how many people were getting diagnosed but had no identifiable cause of their HIV, but now it’s proven and right in front of us. This is disastrous.
To everyone that told the truth about how they didn’t know how they got these types of diseases & how they had no idea where they got it from then faced judgement from others and even the medical community- you aren’t crazy.
On behalf of everything these types of diseases did to destroy families, relationships, and your body, I’m going to apologize right now for all the individuals that I know won’t ever give you an apology for what they did and what they said.
I believe you. I always did.
Without you telling your truth , we never would have been able to figure this out about HIV.
HIV is spreading in “HIV negative” individuals to other individuals as some researchers theorized.
The mRNA vaccination technology developed is now the foundation for the next generation of HIV treatment and disease control. We must continue to push and advocate for improving the lives of all people with disease and we all just took a huge step forward.
You do not have to be sexually active to develop HIV. Your sexual trauma doesn’t have to define your life for the rest of your life- you are stronger than you know and braver than you feel.
Find a place to get tested for HIV here:
I still recommend getting a NAT or “viral load” test done as the first test to see if you have HIV.
I think considering what we know about HIV and in consideration of all the things we still don’t know that this is the safest option. Any other test for this condition available today has too high of a chance of producing a wrong result. I find it extremely uncomfortable we still use the other types of tests in the hospital and doctor office settings.
If you choose to order a test through an online service be aware some tests only tell you about either HIV-1 or HIV-2 and will not always provide you information related to type 1 and type 2.
For example, here:
This will provide you information related to ordering a test that looks for both types of HIV instead of just one strain of HIV.
Stay safe.
#hiv#virus#sick#chronically ill#chronic pain#chronic illness#chronic fatigue#pain#doctor#medicine#viral
687 notes
·
View notes
Text

Source
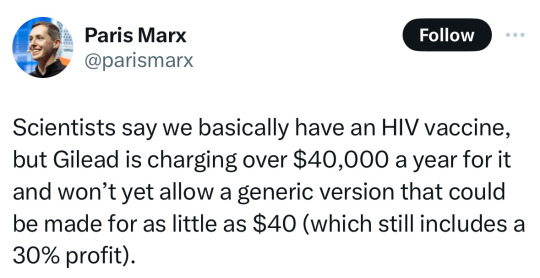
#politics#hiv#us politics#government#gilead#lgbt#lgbtq#progressive#current events#science#medicine#health#health care#the left#twitter post#news
38K notes
·
View notes
Text

#angry feminist#feminicide#especially tough week#I’m French tho I’m following the trial of the husband & 51 (they could identified on the videos they’re much more)#and what they’re saying to justify themselves (like « the husband gave consent or I thought she was just asleep) make me SICK and what men#are commenting online about this case like they don’t buy it and the classic Not All Men 🙄🤬🤢#the husband said that only 3 out of 10 men refused (and none reported it) to come r*pe his unconscious wife..#men from all ages professions one was a neighbour one had HIV and went back multiple times 🤬🤢 lots have wives & kids some had previous#r*pe convictions (one against in own daughter) and lots were caught with possession of child p*#your boyfriend your friend your ex your husband your relative your neighbor your doctor your teacher…#we’re never safe#I’m so tired but still ENRAGED#feminism#femicide#misogyny#crimes against women#violence against women
445 notes
·
View notes
Text


Condoman
In 1987, Indigenous sexual health worker Aunty Gracelyn Smallwood and her team felt that safe sex advertising wasn’t effectively targeting people in Australia’s remote Indigenous communities. In response, they created Condoman - “The Deadly Predator of Sexual Health” - who spoke to Indigenous people in language they could relate to, and removed stigma from conversations about sexual health.
Condoman became something of a cult figure in Australia, and in 2009 he was relaunched with a suite of comics, animations, and merch, including branded condoms. He was also joined by his “deadly, slippery sister” Lubelicious, who promoted consent, the use of water based lube, and women’s health, for her sisters and sistergirls (an Indigenous term analogous to trans women).
We covered Condoman in our podcast on the AIDS epidemic in Australia.
Keep an eye on this blog throughout the week as we continue highlighting queer Aboriginal and Torres Strait Islander history and culture for NAIDOC Week.
#naidoc2024#naidoc week#aids#hiv#condoman#queer history#gay history#lgbt history#queer#gay#lgbt#lgbtq#indigenous history#aboriginal history
455 notes
·
View notes
Link
#contest#medibandpaint#fae#faer#gnc butch#trans poc#420friendly#thick latina#i need a hit#tuxedo#just me#goth clothing#hiv#karina irby
338 notes
·
View notes
Text






1980s/1990s safe sex posters part 2
[part 1]
446 notes
·
View notes