#chromosome abnormalities
Explore tagged Tumblr posts
Text
Actin Your Age
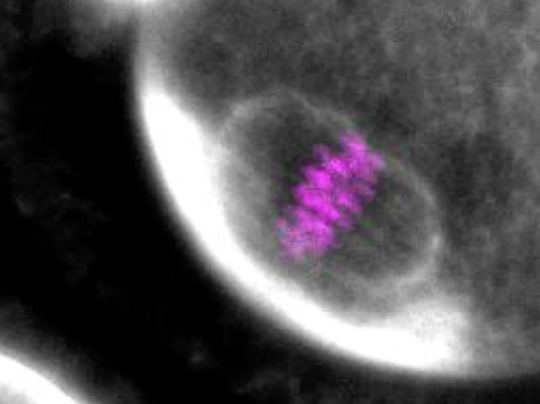
Loss of or impairment of a protein called F-actin in eggs of older females underlies the increased incidence of embryos with an abnormal chromosome number
Read the original article here
Still from video from work by Sam Dunkley and Binyam Mogessie
School of Biochemistry, University of Bristol, Bristol, UK
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Science Advances, January 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#fertility#aneuploidy#eggs#embryos#chromosome abnormalities#chromosome#actin
9 notes
·
View notes
Text
nobody told me being pregnant was so scary. every appointment is like “well it’s time to check on the baby and make sure there’s no earth shattering disease or abnormality that would inhibit them from living to birth or after (:” and i just have to wait a month between appointments pretending like im not hoping my baby’s femur length is where it needs to be by october 1st.
this on top of the fact that i have to see a high risk specialist for a fetal echocardiogram at 22 weeks (where we’ll also do the big anatomy scan) cause of my family’s extensive congenital heart defect history.
<3
#text#just trying to breathe hehe!!#&& the patients who find out i’m pregnant and tell me their horror stories of stillbirth at 6mos etc.#currently waiting on nipt results wherein i’ll find out if my baby has a chromosomal abnormality. some of which are assured death#jdksjdjsjdjskfjskkaofjis
8 notes
·
View notes
Text
Doodler fusion Normal except he changes his name to Abnormal
#doing bio hw saw ‘non-disjunction can cause chromosome abnormalities’ and went ‘omgs Normal’#dndads#dungeons and daddies#normal oak swallows garcia#normal oak#doodler#the doodler
61 notes
·
View notes
Text
The pathologizing of "gender-atypical" behavior is taken to its extreme in the discussion of transgendered animals. Early descriptions of intersexual animals often labeled them "monstrosities". More recently, hermaphroditism, chromosomal and other forms of gender mixing, and physical and behavioral transvestism are invariably considered diseased states, birth defects, physiological abnormalities, or otherwise dysfunctional. Yet researchers have usually been as unsuccessful in determining the physical "causes" for transgender as they have for homosexuality.
"Biological Exuberance: Animal Homosexuality and Natural Diversity" - Bruce Bagemihl
#book quote#biological exuberance#bruce bagemihl#nonfiction#pathologization#transgender#intersex#monstrosity#hermaphroditism#chromosomal mutations#gender mixing#transvestism#diseased#birth defects#abnormality#dysfunctional#researchers#unsuccessful#bad science#homosexuality#gay#lesbian
2 notes
·
View notes
Text

The Research Diaries of S. Sunkavally, p434.
#non-shivering thermogenesis#thyroid hormone deficiency#vitamin B12 deficiency#tapeworm#lactic acidosis#fatigue#monosomy#mental retardation#chromosomal abnormality#tropical rain forests#nucleotide imbalance#monosomies#diabetes#deformed infants#satyendra sunkavally#theoretical biology#manuscript#cursive handwriting
0 notes
Text
Screening for Chromosomal Abnormalities during Pregnancy

Introduction
When expecting a new addition to the family, ensuring the health of the baby is a top priority for parents. One important aspect of prenatal care is screening for chromosomal abnormalities. These screenings are designed to assess the risk of certain genetic disorders that can affect a baby’s development and overall health. Understanding the significance, types, and timing of these tests can help expecting parents make informed decisions and prepare for any potential health challenges their baby might face. This introduction into the world of prenatal screenings aims to clarify their necessity and process, helping parents navigate their journey with confidence and knowledge.
Importance of Screening for Chromosomal Abnormalities during Pregnancy
Significance of Prenatal Care
Prenatal care is not just about ensuring a healthy diet and regular check-ups; it’s a critical period for comprehensive screenings and tests to assess the health of both the mother and the fetus. Among these, screening for chromosomal abnormalities plays a pivotal role. These screenings help to identify potential health issues that could affect the baby’s development and lead to informed decisions about care and treatment. Early detection through these screens can prepare parents and healthcare providers to manage health conditions that could impact the baby’s life quality.
Risks of Chromosomal Abnormalities in Pregnancy
Chromosomal abnormalities occur when there is a defect in one or more chromosomes. The most well-known of these is Down syndrome, but there are many others like Trisomy 18 and Trisomy 13, which can significantly impact a baby’s development both physically and mentally. The risks associated with these disorders can vary; they include developmental delays, congenital disabilities, and, in some severe cases, stillbirth. The risks tend to increase with maternal age, particularly in mothers over the age of 35. Screening helps in assessing these risk factors early in the pregnancy, which is crucial for planning and management.
Common Screening Tests for Chromosomal Abnormalities
First Trimester Screening
First trimester screening is typically conducted between the 11th and 13th weeks of pregnancy. This screening involves a blood test and an ultrasound. The blood test measures the levels of certain substances in the mother’s blood that are associated with chromosomal conditions in the fetus. The ultrasound examines the nuchal translucency, which is a fluid-filled space at the back of the baby’s neck. Increased fluid can be a sign of Down syndrome, Trisomy 18, or heart defects. Together, these tests provide a risk assessment that helps in determining whether further diagnostic testing is needed.
Second Trimester Screening
Known as the “quad screen,” second trimester screening is conducted between the 16th and 18th weeks of pregnancy. This test measures four substances in the mother’s blood: AFP, hCG, Estriol, and Inhibin-A. Abnormal levels of these substances can suggest the risk of certain chromosomal abnormalities such as Down syndrome and Trisomy 18, as well as neural tube defects like spina bifida. This screening does not confirm the presence of these conditions but identifies if there is a heightened risk, requiring additional, more definitive tests.
Non-Invasive Prenatal Testing (NIPT)
Non-Invasive Prenatal Testing (NIPT) is a relatively new screening test that can be done as early as the 10th week of pregnancy. It involves taking a blood sample from the mother to examine fragments of fetal DNA that are present in the maternal bloodstream. NIPT is highly effective in detecting several major chromosomal abnormalities, including Down syndrome, Trisomy 13, and Trisomy 18. Due to its non-invasive nature and high level of accuracy in these areas, NIPT is increasingly becoming a popular choice among expectant parents. It offers not only peace of mind but also a safer way for early detection compared to invasive tests, which carry risks of miscarriage.
Benefits of Early Detection and Diagnosis
Understanding potential chromosomal abnormalities early on during pregnancy can have numerous benefits for both the mother and the developing baby. Early detection provides crucial insights into the health of the fetus and can guide further medical and personal decisions throughout the pregnancy.
Early Intervention and Treatment Options
Identifying chromosomal abnormalities early in pregnancy allows healthcare providers to offer specific interventions that may mitigate some complications. For instance, certain conditions like congenital heart defects, which can be associated with chromosomal abnormalities, can be managed better if detected early. Health professionals can monitor the baby’s development more closely, prepare for interventions soon after birth, and sometimes even suggest treatments before the baby is born. Early detection also opens the door to connect with specialists and hospitals equipped to handle specific conditions right from the start, ensuring the best possible care for both mother and baby.
Emotional and Psychological Preparation for Parents
Receiving news about potential chromosomal abnormalities during a pregnancy can be emotionally challenging. However, early detection gives parents valuable time to psychologically and emotionally prepare for the arrival of a child who may have special needs. It allows for additional time to research the condition, understand what it entails, and realistically set expectations. Support groups and counseling services can also be accessed sooner, providing much-needed emotional support and guidance through the pregnancy journey. This preparatory phase is crucial for building a supportive environment for the child and family.
Making Informed Decisions
The journey of prenatal screenings and tests provides critical information that can influence the decisions made by expectant parents. From understanding the scope and implications of test results to deciding on further diagnostic procedures, parents are better equipped to make informed decisions when they have comprehensive and timely information.
Understanding Screening Results
Navigating the results of prenatal screenings for chromosomal abnormalities can be complex. These tests typically assess the risk of the fetus having certain conditions but do not confirm the presence of abnormalities. Health professionals usually convey results as a probability or risk level, such as a 1 in 100 chance. Understanding what these numbers mean can significantly affect a parent’s decision-making process. For clarity, it is key that the healthcare provider explains the results comprehensively, discussing what they may imply about the baby’s health and what further steps might be advisable.
Follow-up Diagnostic Tests
If screening tests show a high risk of chromosomal abnormalities, follow-up diagnostic tests may be recommended. These tests, such as amniocentesis or chorionic villus sampling (CVS), are more invasive but provide conclusive results about whether a chromosomal abnormality exists. Decision-making at this stage is critical — parents must consider potential risks and benefits. Some may choose to proceed to understand definitively if an abnormality is present, while others may opt out due to the potential risks involved with these procedures. The choice can profoundly impact the approach towards the remaining period of pregnancy, labor, and postnatal care, underscoring the importance of clear, informed discussions with healthcare providers.
Each step in this process, from initial screening to potential diagnostic follow-ups, plays a pivotal role in how parents manage their pregnancy and prepare for their child’s future, making these early assessments incredibly significant.
Advocating for Prenatal Health

The journey through pregnancy is a remarkable period that brims with the promise of new life. However, it’s also a time when the health of both mother and baby should be monitored with great attention and care. Advocating for robust prenatal health is crucial to ensuring that the pregnancy progresses safely and healthily. This encompasses regular medical check-ups, effective communication with healthcare professionals, and adhering to prescribed prenatal routines.
Importance of Regular Check-ups
Regular check-ups during pregnancy serve as a critical tool for monitoring the health and development of the fetus, as well as the well-being of the mother. These visits typically involve a variety of tests and screenings designed to detect any potential issues early on, such as chromosomal abnormalities, which could affect the baby’s development. Routine check-ups enable doctors to:
– Track the growth and development of the fetus
– Monitor the health status of the mother, including blood pressure and weight
– Provide important updates on nutritional needs and physical activity
– Administer necessary vaccinations to protect both mother and child
One critical aspect of these check-ups is screening for chromosomal abnormalities. These screenings are usually non-invasive and provide valuable insights into the genetic health of the fetus. Early detection through these tests allows for a broader range of options and preparedness in managing any conditions that may be discovered.
Communicating with Healthcare Providers
Effective communication with healthcare providers is another pillar of strong prenatal care. Expectant mothers should feel empowered to discuss any concerns or symptoms they experience without hesitation. Open communication can lead to:
– Tailored health advice that aligns with individual health histories and needs
– Clarification and reassurance regarding the normal processes and symptoms of pregnancy
– Swift action and intervention if any unusual signs or complications are identified.
Patients should feel encouraged to ask questions about the screenings, including what each test involves, what the results could indicate, and the subsequent steps following different outcomes. Understanding the purpose and outcomes of tests like those for chromosomal abnormalities not only eases anxieties but also helps in making informed decisions. This dialogue ensures that the pathways of care are clear, inclusive, and aligned with the best interests of both the mother and the developing baby.
Conclusion – Ensuring a Healthy Start for Mother and Baby
Prenatal screening for chromosomal abnormalities is a crucial step toward ensuring the health and well-being of both mother and baby. These screenings help in early detection, which can provide families with valuable information to make informed decisions and prepare for any necessary medical care. Remember, while the prospect of screening can be daunting, the knowledge gained allows for better preparation and peace of mind during what should be a joyous journey. At Ambady Scan, the best scanning center in Kerala, we are dedicated to offering the highest quality prenatal screening services to support you every step of the way.
0 notes
Text

Find The Right Chromosome Disorders Treatment Options For Your Loved Ones
https://thefocusfoundation.org/ - The Focus Foundation is a research-based agency dedicated to identifying & assisting families & children who have Sex Chromosome Disorders, Dyslexia, and Developmental Dyspraxia. They provide the Best Chromosome Disorders Treatment. For more information visit thefocusfoundation.org.
0 notes
Text
Chromosomal Abnormalities Notes
#MendelsLaws#HereditaryTraits#ScienceOfInheritance#MendelianInheritance#GeneticDiscoveries#BiologyLessons#MendelsPrinciples#GeneticsEducation#HereditaryScience#Chromosomal Abnormalities Notes
0 notes
Text

Definition of NT/ NB SCAN: How it Works
NT/NB scan, short for nuchal translucency/nasal bone scan, is a prenatal screening procedure performed around 11 to 14 weeks of pregnancy. It assesses the risk of chromosomal abnormalities, particularly Down syndrome. The procedure involves ultrasound imaging to measure the thickness of the nuchal translucency (fluid accumulation at the back of the fetal neck) and the presence/absence of the fetal nasal bone. Higher NT thickness and absence of the nasal bone may indicate an increased risk of chromosomal abnormalities.
#aurawomen#aura#fertility#ivf#infertility#pregnancy#maternity#ivfsuccess#iuisuccess#iui#chromosomes#abnormalities#fetal position#fetal movement#fetal development#fetal medicine center in kolkata
1 note
·
View note
Text
Anon be lucky I have to study for my exam Monday so I can't reply and post their unhinged ask, but thanks for the laugh break lmao
#like ??#anon if you're the same person i reblog replied from like what the heck? thought we were having a civilish convo#did you want the anonyminity to be more verbally aggressive and get the clapback#if ur not the same then apologies. it was too close together for me to not raise an eyebrow#either way what boggles my mind about this is like.... arent DSD/intersex conditions like. geneticlly based.#maybe I'm not as brushed up but I'm pretty sure every intersex disorder contains some discrepency in the chromosomes and presentation#i dont know of any intersex disorder that doesn't involve the persons chromosomes being abnormal in some way#so by that point. this whole argument is just moot. its a scientific and medical classification that pcos simply doesn't fit#but i do like learning so if someone knows more than me enlighten me#but anyway back to the grind. anon i shall get to you... eventually. if my adhd doesnt make me straight up forget
0 notes
Note
love the implication that female chromosomes are what make people left wing
it's a fact that trans "women" are more conservative than straight cis men, it's a fact, there's study about it. these trans"women" don't have female chromosomes.
Transphobes just can't stop making shit up, can they?
47 notes
·
View notes
Text
Triple Test: A Prenatal Screening For Chromosomal Abnormalities And Birth Defects

Dr. Deepak Goenka, M.D Director, Institute of Human Reproduction IVF Specialist
Pregnancy is an exciting time for expectant parents, but it is also a time of uncertainty and anxiety. To ease this uncertainty, many expectant mothers choose to undergo prenatal screening tests to check for any abnormalities in the fetus. One such test is the Triple Test. In this blog, we will take a closer look at the Triple Test and what it entails.
What is the Triple Test? When is it done?
The Triple Test is a prenatal screening test that is typically performed between the 15th and 20th weeks of pregnancy. The test is used to screen for certain chromosomal abnormalities and birth defects in the fetus. The Triple Test involves measuring three substances in the mother’s blood: alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG), and estriol (µE3).

Why is the Triple Test performed? Triple Test as a screening technique for Down Syndrome.
A positive Triple Test result means that the levels of one or more of these substances are higher or lower than normal, which can be a sign of a chromosomal abnormality or birth defect. It is important to note that a positive Triple Test does not diagnose a specific condition, but rather indicates the need for further testing to confirm a diagnosis.
What happens after a positive Triple Test result?
If you receive a positive Triple Test result, your healthcare provider will likely recommend further testing, such as an amniocentesis. The procedure involves taking a sample of the amniotic fluid to test for chromosomal abnormalities or genetic disorders. It is important to understand that the test is not without risks, and you should discuss the risks and benefits with your healthcare provider before deciding to have them.
To read more, Click Here
Consult the best IVF Experts click here — Best IVF center in Guwahati, Best IVF center in Kolkata
#chromosomal abnormalities#first trimester screening#non-invasive prenatal screening#prenatal genetic testing#prenatal screening#prenatal screening tests#prenatal testing#triple screening
0 notes
Text
jakey is apparently misogynistic now so I suppose I'll have to figure smth else out. in place of the J slur I will refer to everyone's boyfriend as follows: "the incomplete female, the chromosomal abnormality, the bepenised abomination, the walking abortion, aborted at the gene stage. the mention of it threatens to give me deep vein thrombosis & the sight of it makes me feel like I'm going through a slow motion byford dolphin incident." is that better do you guys approve of that one is it gentle sweet kind baby honey enough . nevermind I'm not taking feedback at this time
#like sorry but i cant just turn my misandry off bc hes someones boyfriend?? jakey is being kind#even if its a friends bf. in fact there is no lower form of human life than Friends Boyfriend#will i say this to the face of a friend i value? not in those words. but the sentiment remains#(disclaimer i do think sometimes ppl on here get extremely victim blame-y wrt women mistreated by male partners)#(i just dont think jakey is an example of that)#LX3 OP
622 notes
·
View notes
Text

The Best Treatment Options For Chromosomal Abnormalities
https://thefocusfoundation.org/ - The Focus Foundation is a research-based agency dedicated to identifying & assisting families & children who have Sex Chromosome Disorders, Dyslexia, and Developmental Dyspraxia. They provide the Best Treatment For Chromosomal Abnormalities.
0 notes