#chlamydia infection treatment
Explore tagged Tumblr posts
Text
The Three Most Prevalent STIs: Chlamydia, Gonorrhea, and HPV
Introduction: Chlamydia, gonorrhea, and human papillomavirus (HPV) are among the most common sexually transmitted infections (STIs). These infections can cause serious health problems if left untreated and can affect anyone who is sexually active. In this post, we’ll explore the causes, symptoms, and treatments of these three prevalent STIs. Chlamydia: Causes and Risk Factors: Chlamydia is…

View On WordPress
#Chlamydia causes#Chlamydia symptoms#Common STIs#Gonorrhea causes#Gonorrhea symptoms#HPV transmission#HPV types#HPV vaccination#prevalent sexually transmitted infections#regular STI testing#safe sex practices#STI treatment options
0 notes
Text
https://society4gamers.com/blogs/93389/Chlamydia-Infection-Treatment-Market-Players-Research-and-Challenges-Till-2027
Chlamydia Infection Treatment Market Players Research and Challenges Till 2027
According to MRFR analysis, the global chlamydia infection treatment market is expected to register a CAGR of~10% from 2023 to 2027 and hold a value of USD 12,821.5 million till 2027.
0 notes
Text





The engagement dinner would be filled with new discussions.
Previous / Next Beginning (Gen 8)
I'm not an expert, everything here is based on not-so-deep research hehe
Image transcripts:
Doctor: Do you see here? Congratulations, you're going to be a mom!
Callie: M…mom??
Doctor: That's right, would you like to know the gender? (Callie nods) It's a beautiful boy!
Doctor: As I mentioned, let's focus on treating the chlamydia to avoid any complications.
Callie: What’s the risk, doctor?
Doctor: The infection can be transmitted to the baby and, in more serious cases, it can lead to premature birth, miscarriage…
Callie: Oh no…
Doctor: Don't panic, we’ll continue with the treatment and all the necessary care to make sure nothing bad happens!
Callie: Of course, I’ll be careful.
#família vilela#not so berry challenge#the sims 4#ts4 gameplay#ts4 legacy#ts4 screenshots#simblr#sims 4 simblr#ts4#sims 4#Gen 8#nsb peach
37 notes
·
View notes
Note
I heard we are now at the cusp of chlamydia being untreatable via antibiotics, fun times
In United States, drug-resistant gonorrhea is a public health problem of national concern. But untreatable gonorrhea isn’t the only STD that has health officials worried.
Earlier this week, the World Health Organization released new treatment guidelines for three common sexually transmitted diseases — chlamydia, gonorrhea, and syphilis— in response to increasing antibiotic resistance.
Gonorrhea has developed the strongest resistance to drugs, but the worries about untreatable syphilis and chlamydia come at a time when rates for the three STDs are rising rapidly in the U.S, especially among young people ages 20 to 24. According to data published by the CDC in 2014, the most recent year available: cases of chlamydia have increased 2.5 percent; gonorrhea 5.1 percent; and syphilis 15.1 percent. This is the first increase in the United States since 2006.
How worried should we be?
“STDs are hidden epidemics of enormous health and economic consequence in the United States,” according to the Centers for Disease Control and Prevention.
In the US, STDs are most frequent among college-age women, the highest prevalence being among women, ages 20 to 24.
According to the CDC, there are about 820,000 new gonorrhea infections each year in the United States. In fact, gonorrhea is the second most commonly reported infectious disease, after chlamydia.
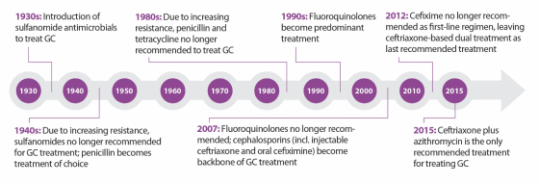
In the past, gonorrhea was successful treated by several classes of antibiotics, including the ubiquitous penicillin. Over time, however, gonorrhea has developed resistance to many of them, and now, we are down to one recommended effective class of antibiotics to treat it.
The problem doesn’t end there. Gonorrhea is even starting to show decreased susceptibility to this “last line” treatment option. This makes this bacterium a multidrug-resistant organism, which are often called “superbugs”.
As for chlamydia and syphilis, drug resistant strains have not become common in the US yet, but the WHO report warns that this is a growing problem in many parts of the world.
How can untreatable STDs be prevented?
Anyone who is sexually active can get an STD.
That said, STDs are preventable and there are steps you can take to keep yourself and your partner healthy. Remember that protecting your health is your responsibility:
Condoms: Use them correctly every time you have sex.
Have fewer partners: Ideally, agree to only have sex with one person who agrees to only have sex with you.
Talk with your partner: Talk with your sex partner about STDs and staying safe before having sex.
Get tested: Make sure you both get tested to know for sure that neither of you has an STD.
Get vaccinated: Safe and highly effective vaccines are available for two STDs: hepatitis B and HPV. HPV is in fact the most common STD. There are specific recommendations for routine and catch up vaccinations for these two STDs. ____________________
This is from 2016 and I cut a bunch out of the middle.
2nd bullet point there probably gonna make some people grumpy, something about suggesting monogamy makes people mad.
102 notes
·
View notes
Text
Medicine may be about to achieve a long-sought goal: a “morning-after pill” to prevent sexually transmitted infections. It could sharply reduce soaring rates of illness and huge health care costs.
The effectiveness of this pill—and it literally is a pill, a 200-milligram tablet of the antibiotic doxycycline—has been studied for a decade, and people have taken it covertly for years. But study results published in The New England Journal of Medicine look likely to tip the pill into clinical practice. In the study, conducted in San Francisco and Seattle, participants who took a single dose within 72 hours of having sex without a condom were only a third as likely to contract chlamydia, gonorrhea, or syphilis as those who didn’t take the pills.
As with everything in medicine, there are footnotes to the findings, and risks to balance the benefits. The study was conducted only among gay and bisexual men, along with transgender women and nonbinary people assigned male at birth. Within those groups, it was limited to people who had been diagnosed with a sexually transmitted infection (STI) in the past year. The study didn’t include cisgender women; in past studies, the preventive antibiotic has not worked as well for them. And the study noted, but didn’t explore in depth, the possibility that routinely administering an antibiotic could provoke resistance either among the bacteria that cause STIs or others carried in participants’ bodies.
All that said, the results have created real excitement among physicians and people who would be eligible to take what’s being called doxyPEP (for doxycycline post-exposure prophylaxis)—even though health authorities, such as the US Centers for Disease Control and Prevention, haven’t yet made formal recommendations for its use.
“I think this is a real game-changer,” says Paul Adamson, an infectious disease physician and assistant clinical professor of medicine at the University of California, Los Angeles. “We have a huge amount of bacterial STIs in the US. Gay and bisexual men who have sex with men are disproportionately burdened by them. And we have not had a lot of tools that we can use to help.”
To understand why doxyPEP could be so significant, it’s important to consider what’s been happening with STIs. Briefly: They’re skyrocketing. Since 2017, according to the CDC, the most important of these diseases have reached historic highs: Gonorrhea has increased by 28 percent, and syphilis by 74 percent. And while chlamydia diagnoses haven’t quite returned to their pre-Covid levels, the agency worries that might be due to pandemic disruptions to care, rather than to an actual decrease in transmission. All of those infections have profound long-term consequences if they are not diagnosed and treated, including making people more vulnerable to HIV infection. Collectively, they cost the US health care system more than $1 billion per year.
Meanwhile, congenital syphilis—passed from mother to infant at birth, a sign that the pregnant person never received adequate prenatal care—caused 220 stillbirths and infant deaths in 2021, the last year for which there are national figures. Gonorrhea is gaining resistance to the last antibiotics currently available to treat it.
In medicine, prevention is almost always preferable to treatment: Vaccines and other prophylactic measures are less expensive, and can be planned in advance. So it has been a research goal to find uncomplicated prevention for STIs—something that, like the morning-after pill for pregnancy, can be taken a short time after sex and doesn’t rely on the user making decisions in the moment.
The first test of doxyPEP, a small US trial that took place in 2011 and 2012, was published in 2015, and showed that HIV-positive men who took the post-exposure dose cut their rate of STIs by three-fourths. Fairly soon after that, social networks of men who have sex with men picked up on the findings, and began sharing knowledge about using preventive doxycycline off-label. A large 2017 French study of men using pre-exposure prophylaxis for HIV, known as PrEP, included within it a study of STI rates among men taking post-exposure doxycycline; it showed that doxyPEP could cut rates of syphilis and chlamydia infection by almost 70 percent. And last summer and this spring, the two largest international HIV conferences included presentations that confirmed the doses were successful in most circumstances.
Several of those presentations were drawn from the San Francisco and Seattle study just published in NEJM. Its results were so dramatic that the authors stopped the trial earlier than planned, in May 2022: They revealed that, among 501 men who were either living with HIV or taking HIV PrEP, consuming that single dose of doxycycline within 72 hours of sex without a condom reduced the combined incidence of the three major STIs by roughly two-thirds.
“Our goal was to understand this in a real-world setting, in a heterogeneous population of people taking HIV PrEP but also living with HIV—which biologically aren’t different populations, but may be different in terms of sexual behaviors, sexual networks,” says Anne Luetkemeyer, one of the study’s principal investigators and a professor of medicine at the University of California, San Francisco. Combined with the French research, she adds, “we now have two studies that really showed very remarkably similar efficacy in this population.”
Those two sets of results may be enough to let doxyPEP enter mainstream medicine. In some places, it already has. Last October, San Francisco’s public health department became the first local department to support doxyPEP use in its jurisdiction. And after the NEJM paper, individual physicians tweeted they would begin prescribing doxyPEP because the results looked so solid—something they can do off-label because the Food and Drug Administration already approved the drug decades ago to treat a range of infections.
When a new way of controlling a disease seems likely to enter the US mainstream, the CDC is expected to weigh in. So far, the agency hasn’t published official guidelines regarding the use of doxyPEP. Following the release of preliminary data at conferences, the CDC published “considerations for individuals and healthcare providers,” a strategy for sharing what’s known so far, as well as an acknowledgment that doxyPEP already is being used off-label. A CDC spokesperson told WIRED by email that formal draft guidance for physicians could come “by the end of the summer.”
When that guidance does arrive, it isn’t expected to recommend doxyPEP for everyone. “We should consider offering this to people who have an elevated risk” of STIs, Luetkemeyer says. “And that group is men who have sex with men, on PrEP, or living with HIV, who've had a history of STIs. I think that's a reasonable group.”
And eligible people may not want to take it. Like almost all antibiotics, doxycycline has side effects: sun sensitivity, diarrhea, serious nausea. And it hasn’t worked equally well for everyone. In the trial done in French men, the antibiotic did not suppress gonorrhea infections, even though it had a dramatic effect on reducing syphilis and chlamydia. In the one trial done so far among cis women, launched in Kenya in 2021, doxycycline prophylaxis (known in this case as dPEP) had no effect on suppressing STIs.
That was disappointing; women who are at high risk of STIs need prevention as much as men do. Equally, it was mystifying for the researchers, who now are poring through their data to see what might have made a difference: whether the 449 participants had difficulty taking the drug at the right time, for instance, or whether doxycycline behaves differently in female organs than in men’s. “We had more than 200 women show up to hear the results, and they were so shocked and disappointed,” says Jenell Stewart, the study director and a physician-scientist and assistant professor at Hennepin Healthcare in Minneapolis. “We are very focused on understanding these results before we say this doesn’t work for women.”
One thing that might have played a role in Kenya and France—and is raising red flags for doxyPEP use in the US—is antibiotic resistance. Stewart says 100 percent of the gonorrhea isolates tested so far from women who became infected while on dPEP showed high levels of resistance to tetracycline, the drug family that doxycycline belongs to; at the time of the French study, the background rate of resistance in gonorrhea there was 56 percent. In the US, where doxycycline isn’t the first-line treatment for gonorrhea, the rate of resistance is only 20 percent. That may provide a clue to why doxyPEP worked better in the US trial than in any other. But it also immediately raises the concern that if doxyPEP goes into wide use, it might make resistance worse.
The US study could not provide an answer: Though some men in the trial did contract gonorrhea while taking doxyPEP, not enough testing was done to confirm whether their strains were resistant to the medication and thus not knocked out by the single dose. Tests did suggest the drug might be affecting other bacteria in participants’ bodies, but the results were contradictory. Those taking doxyPEP ended up harboring 40 percent less staph bacteria—something that all of us carry—than those not taking the drug; but the staph they were still carrying showed “modestly higher” resistance. Whether killing some bacteria was more beneficial than making others potentially hazardous, the trial didn’t last long enough to say.
So the calculation inherent in doxyPEP may not be risk versus benefit, as much as it is risk versus risk: preventing an infection while provoking resistance through small doses, or contracting an infection that requires larger doses over a longer period of time. “We’re not comparing doxyPEP to no antibiotics,” says Adamson, who researches drug-resistant gonorrhea and has prescribed doxyPEP for some patients. “We’re comparing doxyPEP to potentially significant amounts of ceftriaxone, or penicillin, or doxycycline perhaps, if somebody’s getting infections a lot.”
It’s a question that research will have to answer—because, no matter how the CDC weighs in, doxyPEP use is moving ahead. Joseph Osmundson, a microbiologist and author in New York City—where STI rates are rising just as they are nationally—recently sought a prescription from his regular physician. As a queer sexual-health activist, he says, it only made sense, not only to prevent infections and antibiotic side effects for himself, but also to keep from increasing infection rates in an already overburdened city.
“When people want an intervention to have a healthier sex life, you cannot not give it to them,” he says. “Withholding the intervention will not prevent people from having the kind of sex that they enjoy. The question is: Are they going to be provided with as many interventions as possible to have that type of sex with less risk of infectious disease?”
111 notes
·
View notes
Text
"Years after it was first proven to work, a new tool for preventing sexually transmitted infections (STIs) is now closer than ever to entering mainstream medicine.
That tool is doxyPEP, an antibiotic that works like a morning-after pill — but instead of preventing pregnancy within hours of unprotected sex, it prevents STIs like chlamydia and syphilis. Ever since a 30-person trial first suggested hope for the strategy in 2015, people worldwide have begun trying doxyPEP for themselves, often without the approval or supervision of a medical provider.
...
Why did it take so long for the CDC to get behind doxyPEP?The major obstacle has beenthe fear that doing so wouldtouch off a perilous game of infectious disease whack-a-mole — that in trying to mitigate one public health crisis, we’ll worsen another one.
Doxycycline, the medication in doxyPEP, is an antibiotic. Worldwide antibiotic resistance is a major problem — and doxyPEP runs the hypothetical risk of exacerbating it. Disease-causing bacteria can evolve resistance when exposed to certain antibiotics, becoming more dangerous.
...
Doxycycline has plenty of street cred in the STI world. A week’s worth of the medication is the first-line treatment of choice for chlamydia, and a two-week course is the best syphilis treatment choice for people allergic to penicillin. (Doxycycline also sometimes works against gonorrhea, although the germ’s growing resistance to the medication means it is no longer recommended as a treatment for that infection.)
In contrast, doxycycline PEP is for preventing infection, not for treating it. “PEP” stands for post-exposure prophylaxis: The idea is that if a person takes a single dose of the medication soon enough after unprotected sex, any bacteria that might cause an STI would be killed before entrenching enough to cause a full-blown infection."
25 notes
·
View notes
Text
Everything You Need to Know About STD Testing at Urgent Care
STD testing at urgent care clinics is a quick, private option. Luxurious living doesn’t have to mean luxurious health care – in Las Vegas, there are many urgent care centers where to go for affordable services to help you stay on top of your health. Here are the benefits:
No appointment needed.
Fast results.
Confidential testing.
Options that were affordable for uninsured patients.
Urgent care clinics lie somewhere between the emergency room and the regular physician. The aim of these plans is to treat non life threatening health issues with high efficiency. They offer extended hours and walk-in availability which is great for people who need immediate help without the trouble of scheduling a doctor's appointment.

Common Reasons to Get Tested
It is important for everyone who is sexually active to have STD testing. Testing helps protect your partners and keeps you healthy. You should consider getting tested if:
You’ve had unprotected sex.
You’re beginning a new relationship.
You have symptoms, like itching, burning, or discharges that aren’t usual.
You have more than one sexual partner.
You know you’ve been exposed to an STD.
You want peace of mind.
Testing should still happen even if you don’t show symptoms. Many STDs can be completely asymptomatic, but if not treated can lead to long term health issues. By committing to test first, you are being responsible for protecting yourself and your community.
Your Visit — What to Expect
Getting tested for STDs in Las Vegas at an urgent care center is simple and easy. Here’s what typically happens during your visit:
Check-in: When you arrive, you’ll momentarily communicate basic information regarding your health and testing. This means the clinic can also do the right tests in your situation.
Consultation: You will talk to a healthcare provider who will want to know about your symptoms, sexual history, and what you are worried about. It’s a judgment free conversation to create a plan of your care.
Testing: The amount of saliva you provide depends on the STDs being tested for, but may be a urine sample, a blood sample, or a swab. Tests are quick and minimally invasive for each.
Results: Some tests have same day results, while others take a few days. You will be told at the clinic how and when it will tell you the result.
It’s intended to be a respectful, efficient process. Each step is clearly explained and you’ll be guided through each step.
STD Testing Options Available
The good news is that when it comes to testing for the wide variety of STDs, urgent care clinics have it covered. Common tests include:
Chlamydia and Gonorrhea
Syphilis.
HIV
Herpes
Hepatitis B and C
Trichomoniasis
Multiple infections can be checked for at once on testing panels which are available to individuals. If you don’t know precisely what to expose, these panels are really handy.
Why Early Detection Matters
Detecting STDs early is vital for several reasons:
Preventing Complications: STDs if left untreated can cause severe health problems, including infertility, chronic pain, and an increased risk of specific cancers.
Protecting Partners: Early detection can lead to elimination of the infection between partners.
Timely Treatment: STDs can be easily treated if caught early with antibiotics or anti viral medications.
Reducing Anxiety: Having your status brings a sense of peace, knowing that you won’t be blindsided come testing day when the results come in.
Urgent care clinics in Las Vegas not only provide testing, but std treatment for most infections as well. They often have medications on hand which means you could get started with some kind of help, if you need it.
STD Testing Preparation
STD testing appointment prep is a necessary part of a smooth experience. Follow these tips to get ready:
Your bladder needs to be empty for 1 hour before your test — that means don't urinate until after that time. That is important for urine based tests.
Bluntly say whether you have had symptoms, any sexual history or whether you have had any potential exposures. Full disclosure will allow the healthcare provider to suggest which tests are right.
If applicable, bring identification and insurance information. And many clinics take self pay if you don't have insurance.
Before you visit, take down any question or concern that you may have. It ensures that you leave with whatever you need.
Costs of STD Testing
The cost of STD testing at urgent care centers varies based on several factors:
Type of Tests Needed: Single tests are cheaper than comprehensive panels.
Insurance Coverage: STD testing is covered by many insurance plans. Ask your provider if you aren’t sure about your benefits.
Clinic Pricing: Prices at each Las Vegas urgent care clinic vary. Some will have sliding scale fees based on income.
Many clinics offer affordable rates and payment plans for uninsured patients. Always ask for pricing before visiting so you don’t get a surprise.
Where to Get Tested in the Las Vegas Area
There are plenty of choices in Las Vegas when you find yourself in need of urgent care for STD testing and treatment. If you are looking for a clinic nearby you, you can search online for words such as STD Las Vegas or STD treatment Las Vegas. Consider the following when choosing a clinic:
Location and accessibility.
Hours of operation.
Other patients' reviews and ratings.
Access to immediate results.
Is insurance accepted, and what are the payment options?
Researching ahead of time will give you a clinic that works for you and your schedule.
Take Control of Your Health
Urgent care clinics are fast, easy, and confidential methods of STD tests. Staying healthy and protecting those around you is all about regular testing. When you are in Spring and need STD testing or std treatment, then head directly to an urgent care center. This step helps you as you can trust this, allowing you to have your peace of mind.
2 notes
·
View notes
Text
We are the top STD center in the region offering absolute confidentiality Screening for Sexually transmitted infections, Counselling for venereophobia, Treatment for Genital warts, Herpes genitalis, Balanoposthitis, Gonorrhea, Chlamydia, Syphilis, Bacterial and fungal infections for men and women. Sexology clinic- Amore Centre for Sexual Medicine- Best sexual health clinic in Kerala for everyone.
2 notes
·
View notes
Text
Common Symptoms of STDs: What You Need to Know
Sexually Transmitted Diseases (STDs) can affect anyone who is sexually active. Symptoms often vary depending on the type of infection, but common signs include unusual genital discharge, burning sensation during urination, itching, and sores or bumps around the genital area. Some STD symptoms, like chlamydia and gonorrhea, may cause pelvic pain or bleeding between periods, while others, such as syphilis, can lead to rashes or flu-like symptoms. Infections like herpes may result in painful blisters, and HPV might cause genital warts. It's important to note that many STDs can be asymptomatic, making regular testing crucial for early detection. If you experience any of these symptoms, seek medical advice immediately. Early diagnosis and treatment can prevent complications and protect your health.

2 notes
·
View notes
Text
Psittacosis
Let's open with a case report, like we're on an episode of house.
Case Report
35 yo otherwise well, suddenly presents with 2/52 of high fevers and a headache (usually this means > 39)
a/w chills and rigours, responsive to medication/presumably panadol and intermittent (would resolve then come back)
no respiratory symptoms
She had neutrophilia and intrestingly, a CRP of merely 30.
CXR revealed nonspecific consolidation in 2 lobes, they followed this up with a CT revealing pretty impressive ground glass opacities (or GGOs)

She was empirically treated on IV tazocin only (I'm used to atypical coverage empirically started if there's even a whiff of resp, which she may not have had symptoms but her CXR confirms this)
eventually she was on referred to the authors, who felt her CT findings with consistent with psittacosis and treated her with doxycycline which resolved her symptoms in 48 hrs
on further history, it was revealed that she had parrots at home, one had died 2 days preceding her symptoms and she was sleeping next to its body at night (crazy)

What is it:
psittacosis is a zoonoses (transmitted by animals, animals = reservoirs), in this case, transmitted by birds. Orthinoses if birds in general, but psittacosis if referred to macaws, parrots etc. YOu can also catch it from chickens and turkeys.
Some what related is Bird fancier's lungs. Which just sounds fancy.. I'm sure it's just an old term.

Bird fancier's lung refers to a hypersensitivty pneumonitis (ILD) caused by bird exposure. DIfferent disease process, but birds is the come denominator. INhaled bird particles
Psittacosis specifically refers to the infective disease process caused by a bacteria. It was 'identified" or reported in the 1870s, when a cluster of 7 swiss patients developed the same symptoms and found to have possessed tropical birds.
Similarly, in the 1930s there was an outbreak in the US with a mortality of up to 20% (80% in pregnant women), also attributed to parrots from South America.
Eventually, with further scientific development, the causative pathogen was identified as chlamydia psittaci, an atypical intracellular organism.
Psittacosis is a significant differential to consider in community acquired pneumonia as it has a high mortality if left untreated. But it is rare, and causes about 1% of cases in the US. Part of this is due to improved hygiene practices and strict importation guidelines of tropical birds.
It's spread through the inhalation of dust with either dried faeces or respiratory secretions from infected birds.
Clinical features
Variable! but the key thing on history is birds
incubation time can be anywhere from 2 days to 20
Flu-like (fevers/chills/myalgias/arthralgias/malaise/headache)
high fevers is key
respiratory symptoms - does not always present as per the case report, and can be mild on spectrum (dry cough) to more severe
if systemic, can also get photophobia, deafness and epistaxis
Rare (particularly where doxycycline or azith are prescribed at a low threshold): hepatosplenomegaly (look out for LFTs), GI symptoms (remember CAP can present with diarrhoea, nausea/vomiting --> always do a CXR)
even rarer: endocarditis or myocarditis, encephalitis or hepatitis (usually the complications of untreated disease)

Increased risk groups:
pet shop owners
bird owners
farmers
zoo, lab workers where birds are kept, vets, avian quarantine station workers
poultry handlers/workers
So ask if they live or work with birds, or had recent exposure.
INvestigations
serology is gold standard - so looking for antibodies in blood tests
it's intracellular - so hard to culture if even possible on standard blood cultures
elevated ESR/CRP may see LFT derangement and creatinine rise in systemic illness
CXR- usually lower lobe changes, if CT is done, you can get pulmonary infiltrates with GGOs
Treatment:
usual culprits for atypical coverage: azithromycin 3 days or doxycycline 100 mg BD for 14/7
Differentials
always broad if systemic features only (also consider IE and other causes of sepsis)
with resp symptoms - legionella, Q fever, mycoplasma, tularaemia (except for tularaemia, the rest are also covered by doxycycline)
In clinical practice, I'm so used to just having atypicals on board for any cases of atypical pneumonia. I really take it for granted. But will consider this differential more myself in cases of PUO - but I feel like there should be at least CXR findings regardless.
Anyway, prognosis is very good so long as it is treated.
Sources:
CDC guidelines
Case Report: Importance of Clinical history in Psittacosis
StatPearls
Wiki
#psittacosis#chlamydia psittaci#community acquired pneumonia#infectious diseases#infectious disease#medblr
9 notes
·
View notes
Text
I have a patient who is not currently sexually active who wanted STI screening, so I ordered gonorrhea and chlamydia test with urine. It is negative for gonorrhea and chlamydia, but is positive for mycoplasma hominis and ureaplasma species. Although she is asymptomatic, I am going to treat her with antibiotics. I haven't had this happen yet.
Microbiology – Mycoplasma hominis and Ureaplasma spp are small bacteria that lack a cell wall and cannot be visualized by Gram stain. They are part of the normal genital flora of sexually experienced individuals. Transient neonatal colonization also occurs.
●Associated genitourinary syndromes – These organisms have been associated with various genitourinary tract infections (eg, pelvic inflammatory disease [PID] for M. hominis and nongonococcal urethritis for Ureaplasma spp), as well as complications of pregnancy, but their precise roles in some of these conditions have been difficult to define.
●Populations at risk for extragenital infection – M. hominis and Ureaplasma can cause severe infection in specific populations. Neonatal infections include meningoencephalitis, bacteremia, and pneumonia, mainly in preterm infants. In immunocompromised patients, severe systemic infections (eg, bacteremia and bone, joint, pulmonary, and central nervous system [CNS] infections) have also been described; extragenital infections can also occur following trauma or instrumentation of the genitourinary tract.
●Clinical suspicion and diagnosis – M. hominis or Ureaplasma spp infection should be suspected in preterm neonates and immunocompromised patients with extragenital infections when initial microbiologic testing is negative or if the patient does not improve on therapy for more common pathogens. Both culture and nucleic acid amplification tests can be used for their detection; if these organisms are isolated, susceptibility testing should be performed, if available.
●Treatment
•Neonatal infection – For neonates, data on the treatment of M. hominis and Ureaplasma spp infections are extremely limited. M. hominis is variably susceptible to clindamycin, tetracyclines, and fluoroquinolones. Clindamycin should be dosed according to postmenstrual age; experience with doxycycline and fluoroquinolones in premature infants is limited. If treatment is warranted for Ureaplasma spp, azithromycin is an option.
•Extragenital infection in other populations – For extragenital M. hominis and Ureaplasma spp infections in nonpregnant individuals, we suggest moxifloxacin or levofloxacin (Grade 2C). Doxycycline is an appropriate alternative, although resistance may be increasing; it is also reasonable to use combination therapy (eg, moxifloxacin or levofloxacin plus doxycycline). Clinical data on the optimal treatment of these organisms are limited; our preference for certain regimens are based mainly on in vitro susceptibility data and safety in different populations.
•Genital infection – Routine testing for M. hominis or Ureaplasma spp in patients with uncomplicated genital tract disease is not warranted. If these organisms are detected in patients with a genitourinary syndrome (eg, nongonococcal urethritis or PID) and are thought to be the cause of the symptoms, we suggest doxycycline (Grade 2C).
3 notes
·
View notes
Text
Vet Med in Warrior Cats: Whitecough, Greencough, and Yellowcough
Disclaimer
The two main respiratory infections in the warriors series are whitecough and greencough. Whitecough is less severe and can progress to greencough, which has worse symptoms and a graver prognosis. Vicky Holmes states in the 3rd Erin Hunter chat that whitecough is similar to a cough (likely an upper respiratory infection) and greencough is pneumonia (lower respiratory infection), but the specific diseases that each of these coughs represent is never mentioned. The name “greencough” comes from the green fluid that cats cough up when they are affected, whereas cats with whitecough are stated to cough up clear (serous) fluid. A third respiratory disease, yellow cough, makes an appearance in the A Vision of Shadows series. The disease presents similarly to greencough but does not respond to catmint.
There is no way to tell which pathogens each of these diseases might be caused by because the symptoms of each pathogen are very similar, so they are likely caused by several different pathogens and/or combinations. Feline respiratory disease complex (FRDC) is a major cause of upper respiratory infections in cats and is caused by any of the following pathogens, alone or in combination: feline herpes virus (FVR), feline calicivirus (FCV), mycoplasma felis, and chlamydia felis. Bartonella henselae and Bordetella bronchiseptica can also contribute to symptoms. FVR and FCV specifically cause 80-90% of the respiratory disease that is observed in cats. These pathogens are spread by respiratory droplets, direct contact with infected cats, or contact with fomites (objects that have come into contact with the pathogen). Previously infected cats can carry and spread FVR or FCV without showing clinical signs. Acute signs include fever, sneezing, nasal discharge, conjunctivitis, and rhinitis. “Coughing” is not a symptom of respiratory infections in cats, but it is frequently mentioned in Warriors. Cats cough when affected by a lower respiratory infection, laryngeal infection, allergies, or heartworms, but rarely cough as a result of an upper respiratory infection. Symptoms are often more severe in very old and very young cats, which is consistent with the books since kits and elders die the most often from whitecough or greencough. Cats that have respiratory infections in warriors are often shown to refuse food, which is consistent with findings that sick and/or feverish animals are often anorexic. Calicivirus causes painful lesions in the mouth, which can also contribute to cats refusing to eat.
FRDC is generally self limiting and resolves itself in 5-10 days in mild cases, but can take up to 6 weeks to resolve completely in more severe cases. Because of this, mild to moderate respiratory infections could be treated with just supportive care. Medicine cats do this by providing food, water, and rest to infected cats, which is why most cases of whitecough or other nondescript respiratory diseases are resolved in the series. The bigger issue is when there are more severe cases or cases that have ocular involvement.
Ocular involvement can result from almost any respiratory disease causing agent, and can range from discharge to severe conjunctivitis, ulcers, and even globe rupture. Conjunctivitis and other ocular symptoms of respiratory disease are never mentioned in Warriors besides some mild tearing. I will be talking about this issue more in an ocular section later on, as it connects to some broader issues.
To treat more severe cases of respiratory disease, veterinarians often use antivirals, antibiotics, and/or antifungal depending on the pathogens present. Supportive care should also be provided, in addition to feeding tubes and/or treatment of corneal ulcers if necessary. Medicine cats provide supportive care to their patients by providing them with food, water, and warm, dry bedding. For many cases of respiratory disease, this should be enough to help the cat survive since disease is usually self limiting and will resolve with time. A variety of herbs are used in Warriors to treat respiratory infections, but the most notable is catmint. Catmint is also known as catnip, and it is famously known to have psychological effects on cats by acting first as a stimulant from the smell and then a sedative from ingestion. While its effects mimic pheromones, which can be calming, there is no evidence that catmint can be used to combat respiratory disease. Catnip can also be toxic in large doses, causing nausea and vomiting. Cats also become slowly more resistant to its effects with repeated use. Chickweed and Hawkweed are both less effective treatments for greencough. Chickweed has been shown to have some antimicrobial properties, though it is most effective against salmonella and E.coli, both of which are not respiratory pathogens. Hawkweed has been used in some European countries to ease respiratory disease and asthma symptoms, but there has not been research on this. In Long Shadows, tansy is introduced as a way to prevent whitecough from progressing to greencough. Though tansy has been used for various medical issues in humans, it has never been reported to be used for respiratory disease. Coltsfoot is an herb that eases breathing, so it is commonly used for respiratory distress. Coltsfoot was historically used for coughs and respiratory distress in people, and recent studies have proved its efficacy in reducing lung inflammation. Brighteye and lovage are also mentioned briefly in Mistystar’s Omen as another treatment for coughing. These two herbs have been shown to improve symptoms of respiratory disease and allergies in humans, but have not been researched sufficiently. Lungwort is the herb that is presented to Puddleshine by Starclan to treat the emergent yellowcough epidemic in Shadowclan. Lungwort has been used to ease tuberculosis and asthma in humans, but again, there is no substantial research to back this. In addition, Birchsap is briefly mentioned as another possible treatment for yellowcough, but it’s not seen being used in the books. Birchsap traditionally has various medical and cosmetic uses in some cultures, but no research has been done to prove its efficacy.
Overall, the Warriors series gives a fairly accurate depiction of respiratory illness while leaving out some crucial details. The omittance of any ocular involvement, especially in young kittens where it is most prevalent, is a large oversight. The description of the disease process is mostly accurate, however coughing is not as common of a symptom as nasal discharge and rhinitis. Cats in feral colonies are often carrying these diseases without actively showing symptoms, which is why bouts of whitecough can appear suddenly in a clan (especially in times of stress and poor nutrition such as leafbare, which would suppress the cat’s immune responses). As far as treatment goes, medicine cats are providing adequate care to most cats but simply taking care of their basic needs. In more severe cases, medicine is needed. While none of the herbs listed can effectively mimic an antibiotic or antiviral, hawkweed, coltsfoot, brighteye, lovage, and lungwort seem like the most accurate treatments for infection used in the books. Coltsfoot specifically has the most evidence for easing respiratory symptoms, and would be beneficial for medicine cats to use in moderate to severe cases of respiratory disease.
Sources:
https://www.merckvetmanual.com/respiratory-system/respiratory-diseases-of-small-animals/feline-respiratory-disease-complex?query=feline%20respiratory%20disease
https://www.vet.cornell.edu/departments-centers-and-institutes/cornell-feline-health-center/health-information/feline-health-topics/respiratory-infections
https://vetmed.tamu.edu/news/pet-talk/feline-fine-the-benefits-of-catnip/
https://botanicalinstitute.org/eyebright/
https://botanicalinstitute.org/chickweed/
https://www.botanical.com/botanical/mgmh/h/hawmou08.html
https://www.botanical.com/botanical/mgmh/t/tansy-05.html
https://dsps.lib.uiowa.edu/roots/coltsfoot/
https://www.fs.usda.gov/wildflowers/plant-of-the-week/lobaria_pulmonaria.shtml
#Vet med in warrior cats#vet med#warriors#warrior cats#long post#sorry to start off with an entire research paper but I think this one will be the longest section
15 notes
·
View notes
Text
Understanding Urethral Stricture: Causes, Symptoms, and Treatment
Urethral Stricture: Causes, Symptoms, and Treatment
Urethral stricture is a narrowing of the urethra, the tube that carries urine from the bladder out of the body. This condition can lead to various urinary problems and discomfort. Understanding the causes, symptoms, and treatment options for urethral stricture is essential for proper management.
Causes of Urethral Stricture
Urethral stricture can be caused by several factors, including:
Trauma: Trauma to the urethra, such as from a pelvic fracture or a straddle injury, can lead to the formation of scar tissue, which can narrow the urethra.
Infection: Infections, such as sexually transmitted infections (STIs) like gonorrhea or chlamydia, can cause inflammation and scarring of the urethra, leading to stricture formation.
Inflammation: Chronic inflammation of the urethra, often due to conditions like urethritis or balanitis, can result in the narrowing of the urethra over time.
Medical Procedures: Certain medical procedures, such as catheterization or surgery involving the urethra, can increase the risk of developing a urethral stricture.
Congenital Factors: Some individuals may be born with a narrow urethra, predisposing them to developing strictures later in life.
Symptoms of Urethral Stricture
The symptoms of urethral stricture can vary depending on the severity of the narrowing. Common symptoms include:
Difficulty Urinating: Narrowing of the urethra can make it difficult to start urination or maintain a steady stream.
Urinary Retention: In severe cases, urethral stricture can lead to the inability to urinate, which requires immediate medical attention.
Urinary Tract Infections (UTIs): Narrowing of the urethra can increase the risk of UTIs due to incomplete bladder emptying.
Urinary Frequency and Urgency: Strictures can cause the bladder to contract more frequently, leading to a constant urge to urinate.
Spraying or Dribbling of Urine: The narrowing of the urethra can cause the urine stream to spray or dribble instead of flowing in a steady stream.
Pain or Discomfort: Some individuals may experience pain or discomfort during urination, ejaculation, or while passing urine.
Treatment Options for Urethral Stricture
Treatment for urethral stricture depends on the severity of the condition and may include:
Dilation: This involves stretching the narrowed portion of the urethra using a series of dilators of increasing size. It is a common treatment option for less severe strictures.
Urethrotomy: This procedure involves using a special instrument to cut the stricture, widening the urethra. It is often used for short strictures.
Urethroplasty: In more severe cases, surgery may be required to remove the narrowed portion of the urethra and reconstruct it using tissue from other parts of the body.
Medication: In some cases, medications may be prescribed to help reduce inflammation and prevent further scarring of the urethra.
Self-Catheterization: Some individuals may need to perform self-catheterization regularly to help keep the urethra open and maintain urine flow.
Conclusion
Urethral stricture is a condition that can cause significant urinary problems and discomfort. Understanding the causes, symptoms, and treatment options for urethral stricture is crucial for effectively managing the condition. If you experience symptoms of urethral stricture, it is important to consult with a healthcare professional for proper evaluation and treatment.
#Urethral stricture#urethral penetration#urethral stricture symptoms#urethral stricture causes#urethral stricture treatment#best doctor for urethral stricture#best urologist for urethral stricture
3 notes
·
View notes