#community acquired pneumonia
Explore tagged Tumblr posts
Text
Psittacosis
Let's open with a case report, like we're on an episode of house.
Case Report
35 yo otherwise well, suddenly presents with 2/52 of high fevers and a headache (usually this means > 39)
a/w chills and rigours, responsive to medication/presumably panadol and intermittent (would resolve then come back)
no respiratory symptoms
She had neutrophilia and intrestingly, a CRP of merely 30.
CXR revealed nonspecific consolidation in 2 lobes, they followed this up with a CT revealing pretty impressive ground glass opacities (or GGOs)

She was empirically treated on IV tazocin only (I'm used to atypical coverage empirically started if there's even a whiff of resp, which she may not have had symptoms but her CXR confirms this)
eventually she was on referred to the authors, who felt her CT findings with consistent with psittacosis and treated her with doxycycline which resolved her symptoms in 48 hrs
on further history, it was revealed that she had parrots at home, one had died 2 days preceding her symptoms and she was sleeping next to its body at night (crazy)

What is it:
psittacosis is a zoonoses (transmitted by animals, animals = reservoirs), in this case, transmitted by birds. Orthinoses if birds in general, but psittacosis if referred to macaws, parrots etc. YOu can also catch it from chickens and turkeys.
Some what related is Bird fancier's lungs. Which just sounds fancy.. I'm sure it's just an old term.

Bird fancier's lung refers to a hypersensitivty pneumonitis (ILD) caused by bird exposure. DIfferent disease process, but birds is the come denominator. INhaled bird particles
Psittacosis specifically refers to the infective disease process caused by a bacteria. It was 'identified" or reported in the 1870s, when a cluster of 7 swiss patients developed the same symptoms and found to have possessed tropical birds.
Similarly, in the 1930s there was an outbreak in the US with a mortality of up to 20% (80% in pregnant women), also attributed to parrots from South America.
Eventually, with further scientific development, the causative pathogen was identified as chlamydia psittaci, an atypical intracellular organism.
Psittacosis is a significant differential to consider in community acquired pneumonia as it has a high mortality if left untreated. But it is rare, and causes about 1% of cases in the US. Part of this is due to improved hygiene practices and strict importation guidelines of tropical birds.
It's spread through the inhalation of dust with either dried faeces or respiratory secretions from infected birds.
Clinical features
Variable! but the key thing on history is birds
incubation time can be anywhere from 2 days to 20
Flu-like (fevers/chills/myalgias/arthralgias/malaise/headache)
high fevers is key
respiratory symptoms - does not always present as per the case report, and can be mild on spectrum (dry cough) to more severe
if systemic, can also get photophobia, deafness and epistaxis
Rare (particularly where doxycycline or azith are prescribed at a low threshold): hepatosplenomegaly (look out for LFTs), GI symptoms (remember CAP can present with diarrhoea, nausea/vomiting --> always do a CXR)
even rarer: endocarditis or myocarditis, encephalitis or hepatitis (usually the complications of untreated disease)

Increased risk groups:
pet shop owners
bird owners
farmers
zoo, lab workers where birds are kept, vets, avian quarantine station workers
poultry handlers/workers
So ask if they live or work with birds, or had recent exposure.
INvestigations
serology is gold standard - so looking for antibodies in blood tests
it's intracellular - so hard to culture if even possible on standard blood cultures
elevated ESR/CRP may see LFT derangement and creatinine rise in systemic illness
CXR- usually lower lobe changes, if CT is done, you can get pulmonary infiltrates with GGOs
Treatment:
usual culprits for atypical coverage: azithromycin 3 days or doxycycline 100 mg BD for 14/7
Differentials
always broad if systemic features only (also consider IE and other causes of sepsis)
with resp symptoms - legionella, Q fever, mycoplasma, tularaemia (except for tularaemia, the rest are also covered by doxycycline)
In clinical practice, I'm so used to just having atypicals on board for any cases of atypical pneumonia. I really take it for granted. But will consider this differential more myself in cases of PUO - but I feel like there should be at least CXR findings regardless.
Anyway, prognosis is very good so long as it is treated.
Sources:
CDC guidelines
Case Report: Importance of Clinical history in Psittacosis
StatPearls
Wiki
#psittacosis#chlamydia psittaci#community acquired pneumonia#infectious diseases#infectious disease#medblr
9 notes
·
View notes
Text
CAP
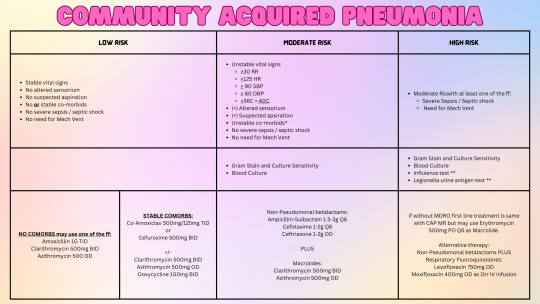
According to the Philippine Clinical Practice Guidelines for CAP in ADULTS (2020):
Unstable Co Morbids include: -> Uncontrolled DM -> Active malignancies -> Neurologic disease in evolution -> CHF FC II-IV -> Unstable CAD -> Renal Failure on dialysis -> Uncompensated COPD -> Decompensated Liver disease
Legionella urine antigen test and Influenza test are conditional recommendation for CAP HR: -> Influenza test may be done during periods of high influenza activity (July - January) if CAP HR is preceded by inluenza-like illness symptoms such as body malaise, rhinorrhea, arthralgia, sorethroat plus risk factors such as >60y/o, pregnant, asthmatic.
DRUGS: PENICILLINS: amoxicillin MACROLIDES: clarithromycin, azithromycin BETALACTAMS: co-amoxiclav, cefuroxime TETRACYCLINES: doxycycline NON PSEUDOMONAL BETALACTAMS: ampisul, cefotaxime, ceftriaxone FLUOROQUINOLONES: levofloxacin, moxifloxacin
Atypical coverage for Aspiration Pneumonia is only recommended if with suspicion of lung abscess or empyema.
Antiviral treatment is recommended with antibiotic therapy in CAP HR with risk factors mentioned under influenza testing.
Treatment should be initiated within 4 hours regardless of risk.
Duration of treatment: -> CAP LR , CAP MR: 5 days if stable -> May extend duration if pneumonia is not resolving, complicated by sepsis, infected with less common pathogens or infected with drug-resistant pathogens.
CXR post-treatment is recommended after a minimum of 6-08 weeks to establish a baseline and exclude other conditions but it is not recommended for routine testing in stable improving patients.
Inadequate Response after 72 hours of Empiric treatment: -> Reassess for possible resistance -> Reassess for the presence of other pathogens such as M. tuberculosis, viruses, parasites, or fungi.
Philippine CPG for CAP (Adults) 2020 Downloadable Link: https://www.psmid.org/cpg-management-and-prevention-of-adult-community-acquired-pneumonia-2020/
#CAP#Community Acquired Pneumonia#Philippine Clinical Practice Guidelines Summary#Medical notes#Philippine CPG#Review#Medicine#Doctors#Pneumonia#Med School#Medblr#Studyblr
0 notes
Link
0 notes
Link
0 notes
Text
Comparison and significance of serum 7 cytokines in children with community-acquired common pneumonia and lobar pneumonia by Shi Changsong in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstracts
Objective: To investigate the availability of seven serum cytokines, interleukin-4 (IL-4), interleukin-6 (IL-6), interleukin-10 (IL-10), interleukin-17 (IL-17), interleukin-12-70 (IL-12P70), tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) changes and significance in Common and lobular community acquired pneumonia (CAP).
Methods: Fifty-three patients admitted to our hospital from April 2022 to July 2023 were selected as the observation group. According to the degree of pneumonia, they were divided into common pneumonia group (observation group 1), lobular pneumonia group (observation group 2), and children with fever (acute upper respiratory tract infection) during the same period were selected as the control group. The clinical data of the subjects in three groups (observation group 1, 2 and control group) were retrospectively analyzed. Temperature, length of stay, chest CT and other basic information were recorded. Fasting venous blood of three groups of children was collected and 7 cytokines levels were detected. The cytokine levels of the three groups were compared by one-way analysis of variance.
Results: The hospital stay of lobar pneumonia group was significantly longer than that of common pneumonia group and fever group. There were no significant differences in IL-4, IL-6,IL-10, IL-17, IL-12P70, TNF-a and IFN-γ among lobular pneumonia group, common pneumonia group and fever group (P > 0.05).
Conclusion: Lobar pneumonia prolongs the hospital stay of children. The cytokines IL-4,IL-6,IL-10,IFN-γ, IL-17,TNF-a and IL-12P70 showed no significant difference in lobular pneumonia group, common pneumonia group and fever group. According to the World Health Organization, pneumonia killed 920,000 children under the age of five in 2016, 98% of whom were in developing countries. Pneumonia is also one of the main causes of death among children < 5 years old in China, and most of them are lobular community acquired pneumonia (CAP)[1]. At present, there are few studies on biomarkers used to assess disease severity and prognosis [2]. Cytokines are major regulatory factors of inflammatory response, which play a role in amplifying, transducing and coordinating pro-inflammatory signals, leading to synchronous expression of molecular effectors and regulating autoimmune responses [3]. Previous studies have shown that the prognostic value of changes in cytokine levels is correlated with the severity of pneumonia [4]. The objective of this study was to retrospectively analyze and compare cytokine levels in children with common pneumonia and lobar pneumonia.
Data and methods
General Information:The medical records of 53 children with CAP who were hospitalized in the pediatric respiratory department of our hospital from April 2022 to July 2023 were collected. According to the degree of pneumonia, they were divided into common pneumonia group and lobar pneumonia group. Children with fever during the same period were selected as the control group, and basic information such as temperature at admission, length of stay, duration of medical history and chest CT were recorded. Cytokine levels were determined by the key Laboratory of hematological Pathology of our hospital. This study was approved by the Ethics Committee of Henan Provincial People's Hospital (2023) No. 65.
Inclusion and exclusion criteria for children with pneumonia:
Inclusion criteria: 1) The diagnostic criteria of community-acquired pneumonia and lobar pneumonia in children in the 8th edition of Zhufutang Practical Pediatrics were met; 2) Complete clinical data; Exclusion criteria: 1) combined with other lung diseases, such as asthma and tuberculosis; 2) Previous immune disease, unexplained long-term fever, joint swelling and pain; 3) A recent or longterm history of glucocorticoid use; 4) Immunomodulators and immunosuppressants such as immunoglobulin and interferon have been applied in the past 2 months.
Statistical Processing:
All the data of the patients were recorded, and the differences of each index between the two groups were analyzed using Graphpad Prism 8. Counting data is expressed as example (%); The measurement data were expressed as mean ± standard deviation (x±s), and the cytokine levels of the three groups were examined by one-way ANOVA for inter-group comparison. P < 0.05 was statistically significant.
Results: Compared with the other 2 groups, the length of hospital stay in the lobar pneumonia group was significantly increased, with statistical significance (P < 0.05), while there was no statistical significance in other general data (P > 0.05). Compared with lobular pneumonia group, common pneumonia group and fever group, there were no significant differences in serum cytokines in IL-4,IL-6,IL-10, IL-17, IL12P70, TNF-a and IFN-γ (P > 0.05).
Discussion: CAP is a common infectious disease in childhood, especially in infants and young children. It is the most common cause of hospitalization in children and the first cause of death in children under 5 years old. For hospitalized children or areas with good conditions, the evaluation of CAP severity should also be based on the scope of lung lesions, the presence of hypoxemia, and the presence of internal and external pulmonary complications[5]. This study was mainly based on the clinical symptoms of pneumonia and the range of chest imaging lesions as a grouping basis to determine the severity of pneumonia. The results of this study found that the length of hospital stay in the fever group, the common pneumonia group and the lobular pneumonia group was different in pairwise comparison, and the length of hospital stay in the lobular pneumonia group was significantly longer than that in the other two groups, indicating that the scope of chest imaging lesions may affect the length of hospital stay and treatment time, which has guiding significance for our clinical evaluation of the length of hospital stay for pneumonia.
Cytokines, including types Th1 (IL-2, IFN-γ, TNF-α, and IL-18) and Th2 (IL-4, IL-5, IL-6, IL-10, and IL-13), can recruit or activate B, T, and NK cells to initiate and amplify inflammatory/immune responses. Thus providing an important function in host defense against bacterial or viral infections [6]. Cytokines participate in the pathogenesis of pneumonia by interacting with organ receptors [7], leading to a decline in respiratory system related functions. Studies have found that TNF-α, IFN-γ, IL-6, IL-8, IL-10, IL-1β and other cytokines have been proven to be correlated with adult CAP severity [8]. However, Luo Zhengxiu et al. retrospectively analyzed and compared the serum cytokine levels between the severe children group and the non-severe CAP group and found no statistically significant differences in the levels of IL-6, IL-2, IL-4, IL-10, TNF-α, IFN-γ and IL-17A between the two groups [9]. Therefore, there is no consensus on the effect of cytokines on the prognosis of childhood pneumonia. This study found no correlation between IL-4, IL-6, IL-10, IFN-γ, IL-17, TNF-α, and IL-12P70 and the severity of pneumonia. Due to the single-center and small sample data in this study, the correlation between these cytokines and the severity of pneumonia needs further study.
#serum 7 cytokines#community-acquired#common pneumonia#lobar pneumonia#JCRMHS#Journal of Clinical Case Reports Medical Images and Health Sciences (JCRMHS)| ISSN: 2832-1286#Clinical decision making#Clinical Images submissions
1 note
·
View note
Text
Dr. Mike Yeadon is probably the most qualified former pharmaceutical company research executive speaking out about the dangers of the covid so-called “vaccines.”
He is trained in toxicology and has a PhD in respiratory pharmacology and has had a 30-year career spanning the pharmaceutical and biotechnology industry. When Dr. Yeadon worked at Pfizer he was responsible for research on allergic and respiratory diseases. He later became the founder and CEO of a biotechnology company acquired by Novartis, before becoming persona non grata in the industry in 2020 for speaking out against the covid pandemic and vaccines.
In a video recorded for the Northern Ireland Assembly, he sums up what happened during the covid era as well as how the vaccines were designed.
In July 2024, Northern Ireland published a consultation document regarding a proposed Public Health Bill which appears to include, among others, a proposal to enable forced vaccination. It hasn’t been made clear, but it seems the purpose of Dr. Yeadon’s video is so that it can be submitted to the Northern Ireland Assembly in response to this proposed bill, the consultation for which ended on 14 October 2024.
In his video, Dr. Yeadon explained that there was no pandemic or public health emergency in 2020, but rather a pandemic of lies, propaganda, fear-based information, fake diagnostic tests and misattribution of real illnesses, which led to a radical change in medical management practices worldwide.
Numerous deaths in 2020 which were recorded as “covid deaths” were due to “treatment” protocols. Hospitals and care homes adopted harmful practices, such as sedating patients and using mechanical ventilators, and applied these “treatments” to frail and elderly people, resulting in large numbers of deaths. This was not by mistake. It was intentional. Crimes were committed, Dr. Yeadon said.
The “treatment” given to patients involved midazolam and painkillers such as morphine. Midazolam is a sedative, while morphine is a pain-relieving drug that can suppress breathing. It is forbidden to administer both together without intense medical monitoring. Dr. Yeadon, with a PhD in understanding the effects of opiate drugs like morphine, said that the combination of these two drugs would cause a person to fall asleep and stop breathing.
In addition to the deadly protocols, people in the community were deprived of medical care, such as antibiotics for incipient bronchial pneumonia, which likely resulted in thousands of deaths.
All these deaths were due to medical murder and propaganda, rather than covid, he said.
16 notes
·
View notes
Text
If anyone is considering getting community-acquired pneumonia this northern hemisphere sickness season, please allow me to advise against it. Not a fun time.
(For characters, though? I am sooo taking notes 😆)
15 notes
·
View notes
Text
Tribute to Louise Michel
I - Louise Michel's journey from her birth (May 29, 1905) to the assassination and funerals of Victor Noir (January 1870)
120 years ago to the day, Louise Michel passed away at the age of 75, in Marseille, taken by pneumonia. So I can't help but pay tribute to her. In this first post dedicated to the life of Louise Michel (yes, I'm annoying, I love telling the stories of the historical figures I love...), I will simply retrace her journey from her birth in Vroncourt to her situation in Paris in early 1870. Then, in future posts, I will tell you about her commitment to the Club de la Patrie en danger, to the Comité républicain de vigilance des citoyennes du XVIIIe arrondissement, to the demonstration of January 22, 1871, and during the Paris Commune, of course. Not to mention her trial, her deportation to Kanaky, and all her actions from 1880 to 1905 !
“I am what is called a bastard; but those who gave me the bad gift of life were free, they loved each other” (Memoirs). Louise Michel was born on May 29, 1830 at the Château de Vroncourt in Haute-Marne. We know her mother very well, named Marianne Michel, a servant at the Château de Vroncourt in the service of the Demahis family (belonging to the minor nobility). To tell the truth, the father is unknown to us. However, it is very likely that her father's name was Laurent Demahis (she confirms this in her Memoirs), rather than Etienne-Charles Demahis, whom she always considered her grandfather.
"The nest of my childhood had four square towers, the same height as the main building, with bell-shaped roofs. The south side, absolutely without windows, and the loopholes in the towers gave it the air of a mausoleum or a fortress, depending on the point of view. Formerly it was called the Strong House; when we lived there I often heard it called the Tomb. This vast ruin, where the wind blew like in a ship, had, to the east, the coast of the vines and the village, from which it was separated by a grassy road as wide as a meadow" (Memoirs).
Louise Michel therefore grew up at the Château de Vroncourt, alongside her grandparents Etienne-Charles and Charlotte Demahis. In her Memoirs, she launches into a description of her native village : "To the west, the coast and the Suzerin wood, from where the wolves, at the time of the great snows, entering through the breaches of the wall, came to howl in the courtyard. The dogs answered them, furious, and this concert lasted until morning it went well with the ruin and I loved those nights. I loved them especially, when the north wind blew hard, and we read very late, the family gathered in the great hall, the staging of winter and the high cold rooms. The white shroud snow, the choirs of the wind, wolves, dogs, would have been enough to make me a bit of a poet, even if we had not all been poets from the cradle; it was a legacy that has its legend. It was freezing cold in these enormous rooms; we would gather around the fire, my grandfather in his armchair, between his bed and a pile of rifles of all ages; he was dressed in a large white flannel greatcoat, shod in clogs trimmed with sheepskin slippers. On these clogs, I would often sit, almost huddling in the ashes with the dogs and cats. There was a large Spanish female dog, with long yellow hair, and two others of the breed of shepherd dogs, all three answering to the name of Presta, a black and white dog that we called Médor, and a very young one, that we had named the Biche in memory of an old mare that had just died. We had mourned the Biche, my grandfather and I had wrapped her head in a white cloth so that the earth would not touch it, at the bottom of the big hole where she was buried near the acacia of the bastion. The cats were all called Galta, the tabby and the red ones".
In truth, her grandparents gave her a liberal education. It should be known that Etienne-Charles Demahis was part of the minor nobility acquired to the republican ideal.
As a child, Louise was very interested in nature, animals, and the peasants of the region. She loves walking in the Haute-Marne countryside, climbing trees with her cousin Jules; she loves horses. Louise does everything that is forbidden to young girls of her time ! "The female cats were all called Galta, the tabby ones and the red ones. The cats were all called Lion or Raton, there were legions of them" (…) "In the summer, the ruin filled with birds, entering through the windows. The swallows came to take back their nests, the sparrows knocked on the windows and private larks bravely shouted with us (falling silent when we switched to minor mode). Birds were not the only companions of dogs and cats; There were partridges, a tortoise, a deer, wild boars, a wolf, owls, bats, broods of orphaned hares, raised with a spoon, a whole menagerie, not forgetting the foal Zephyr and his grandmother Brouska, whose age was no longer countable, and who would come straight into the rooms to take bread or sugar from the hands she liked, and to show people who did not suit her her big yellow teeth, as if she were laughing in their face. Old Biche had a rather funny habit: if I held a bouquet, she would offer it to herself, and run her tongue over my face. And the cows? the big Blanche Bioné, the two young Bella and Nera, with whom I would go and talk in the stable, and who would answer me in their own way by looking at me with their dreamy eyes. All these animals lived in harmony; the cats lying in a circle followed the birds, the partridges, the quails trotting on the ground with their eyes. Behind the green tapestry, all holes, which covered the walls, mice were moving around, with little cries, quick but not frightened; I never saw a cat disturb them in their peregrinations. Besides, the mice behaved perfectly, never gnawing the notebooks or the books, never having set their teeth on the violins, guitars, cellos which were lying around everywhere. What peace in this house and in my life at that time !" (Memoirs (p.11-12).
Thanks to her grandparents, Louise received a good education. She thus becomes a brilliant young girl, revolted against all injustice !
A great reader (she also read the great philosophers, notably Rousseau, Voltaire, Diderot), and became a great admirer of Victor Hugo. If there is another book that has left its mark on her, so to speak, it was Lamennais’s Words of a Believer, “I was perhaps six or seven years old when Lamennais’ book, Words of a Believer, was soaked with our tears. From that day on, I belonged to the crowd; from that day on, I climbed step by step through all the transformations of thought, from Lamennais to anarchy.” (Memoirs).
One of the aspects of Louise Michel’s personality: Her attachment to Christian mysticism. One of her key words: compassion and justice for every human being. [Well, I keep repeating it, but you don’t need to believe in God (and even less to be a Christian) to show a capacity for empathy… In fact, I will tell you about Louise Michel's relationship with religion.]
Some historians (including Xavière Gautier) dare to say that Louise had a certain “fascination” with death… indeed, she liked going to the cemetery. Later, in her Letters to Victor Hugo, she would mention people who told her “Go sleep in the cemetery, little one, because you’re a bastard!” (another reference to the conditions of her birth, really!). Xavière Gautier specifies that people who didn’t know her rejected her death, an idea that she took up for her own, and she always thought that she was going to die wonderfully, to the point of wanting to die a martyr for her fights that were dear to them ("Kill me if you are not cowards (...)" - Yes, you get the idea; I’ll tell you about it in another post^^). I take this opportunity to quote a poem written by her grandmother Charlotte after Etienne-Charles' death :
DEATH
Mourning has descended into my sad home :
Pale Death sits at the hearth and I weep.
All is silence and night in the house of the dead.
No more songs, no more joy, where chords vibrated.
We murmur quietly, and as if with mystery.
It is that we do not come back when we sleep underground.
Forever his absence has made the songs cease.
What happened next ? In 1844, her grandfather Etienne-Charles Demahis died. Laurent Demahis died in turn in 1847, as did his grandmother Charlotte Demahis in 1850. Louise and her mother left the Château de Vroncourt. She refused several marriage proposals. Furthermore, her mother would have wanted her to "take orders"; Luckily she didn't listen to him ! That's how she decided to become a teacher !
For the first time, she corresponded with Victor Hugo, for whom she had great admiration. From 1850 to 1862, she sent him eight poems. "From Audeloncourt, I sent verses to Victor Hugo; my mother and I had seen him in Paris in the autumn of 1851, - and he answered me from exile as he had formerly answered me from Paris, to my nest in Vroncourt and to my pension in Chaumont. I also sent a few feuilletons to the newspapers in Chaumont."(Mémoires)
In 1851, with her mother, she spent a few months with her uncle in Lagny. Her uncle, who "didn't like to see me write and always imagined that I would leave the schoolteacher exams for poetry", placed her at Mme Duval's boarding school in Lagny, "where his daughter had been brought up; I was a boarder there for about three months".
She prepared for her schoolteacher's certificate, but she failed her first attempt.
In 1852, in Chaumont, she tried a second time to pass her teacher's certificate, this time she succeeded. "In this house, as in Chaumont, we lived books; the real world stopped on the threshold and we were passionate about the bits of science that crumble in front of the teachers: just enough to make you thirst for the rest; we never have time to deal with that rest." "The lack of time was before 71, the torture of any teacher's life. We were struggling before the diploma, with a program that we inflate beyond measure, and, afterwards, with the same deflated program, letting you see that you know nothing !"
Refusing to "swear an oath to the Empire" (which was obligatory for all civil servants under the Second Empire), she set up a free school in Audeloncourt.
She teaches in the name of republican and democratic principles. For her, the role of a teacher is to transmit to children the taste for knowledge, to learn to think for oneself in order to ensure one's emancipation. She is categorically opposed to any punishment. She writes plays staged by schoolgirls. She establishes what can be called "nature classes", by teaching them about plants and animals. She did not hesitate to bring certain plants and animals (birds, snakes) into the classroom, asking the students to treat them with greatest possible respect.
In addition to her brilliant work as a teacher, Louise Michel began her literary career as a poet. In her early writings, she sought to express values such as compassion and solidarity, hinting at her desire for emancipation. These first poems, published in newspapers such as L'Écho de Haute Marne and signed "Louise Demahis" bear witness to her first socialist commitments.
As a good teacher and a good republican, Louise was summoned by Rector Fayet, who ended up sympathizing with her and supporting her.
In 1854, Louise Michel established free schools in Clefmont and Millières.
"I was summoned to the prefect who told me: You have insulted His Majesty the Emperor by comparing him to Domitian and if you were not so young, we would have the right to send you to Cayenne. I replied that those who recognized Mr. Bonaparte in the portrait of Domitian insulted him just as much, but that in fact it was him that I had in mind. Adding that, as for Cayenne, it would have been pleasant for me to establish a house of education there, and not being able to pay the cost of the trip myself, that on the contrary it would give me great pleasure. The matter ended there! Some time later, a man who wanted to ask some favor of the prefecture came to find me, saying: "It seems that you have been to the prefect, you will ask me to come there." I objected in vain that it was to judge me and threaten me with Cayenne that I had been called to the prefecture, and that my recommendation was not capable of making him come, but on the contrary, the man would not budge."
Faced with the accusations of the prefect of Haute-Marne (who had closed the school of Auloncourt), Fayet did not hesitate to defend him. In his letter addressed to the prefect, he emphasized his intelligence and his capacity for imagination, and he pleaded in favor of the reopening of his independent school.
Louise Michel demonstrated a deep commitment to the living conditions of the most deprived. Her correspondence with the prefect of Haute-Marne between 1853 and 1855 reflects her concern for the misery of workers and peasants. By advocating for the creation of a welfare office and public workshops, she sought to meet the urgent needs of the local population, particularly in terms of employment and food support.
In 1855, she decided to live in Paris, in the Montmartre district. In her Memoirs, she states that once established in Paris, she hoped to finally be able to fight the Second Empire. Indeed, the Montmartre district is to be considered a "landmark of revolutionaries", republicans, socialists, opponents of Napoleon III. She was hired as an assistant teacher at Madame Vollier's school, "rue du Château d'Eau". Now a socialist, she dreamed of training a young generation of individuals in the class struggle. She also attended popular education classes on rue Hautefeuille, alongside radical republicans and socialists. "Fortunately, elementary education was there. Since the classes on Rue Hautefeuille mostly took place at ten o'clock in the evening, we could often escape there and the bookstores were closed on the way back. Fortunately, elementary education was there. Since the classes on Rue Hautefeuille mostly took place at ten o'clock in the evening, we could often escape there and the bookstores were closed on the way back."
She also taught at a school on Rue Thevenot. The Women's Rights group also met at this school. From then on, Louise Michel became close to two important figures in the history of "feminism", Maria Desraimes and André Léo. She later opened a new school on Rue Oudot. In this way, she provided a "libertarian" education.
In 1861, she published the pamphlet "Lueurs dans l'ombre, plus d'idiots, plus de fous", then the Book of Hermann. In 1867, she founded a consumer cooperative with Marguerite Tinayre, Etienne Delamarche and Fortuné Henry, named Société des Equitables de Paris.
As a good socialist activist, she began to frequent Blanquist circles. This allowed her to meet Th��ophile Ferré, with whom she fell in love! She also became friends with Emile Eudes, Emile Duval, Raoul Rigault, and the brilliant collectivist Eugène Varlin. In 1869, Louise Michel's name was mentioned in the newspaper La Marseillaise (Henri Rochefort, Arthur Arnould, Gustave Flourens, Jean-Baptiste Millière and Victor Noir worked in this newspaper); she was mentioned as "secretary of the Société démocratique de moralisation, whose main objective was to help women workers live through work in duty or to return to it".
"The year 70 opens tragically with the assassination of Victor Noir by Pierre Bonaparte at his house in Auteuil where he had gone with Ulrich de Fonvielle as a witness for Paschal Grousset. This coldly accomplished crime put the finishing touch to the horror inspired by the Bonapartes. Like the bull in the circus shaking its skin pierced with darts, the crowd shuddered. Victor Noir's funeral seemed indicated to bring the solution. The murder was one of those fateful events that bring down the most strongly supported tyranny. Almost all those who went to the funeral thought they would return home or to the republic or not return at all" ("The burial of Victor Noir, the affair recounted by Rochefort" - La Commune, Histoires et souvenirs, 1898). On January 12, 1870, Louise Michel attended the funeral of Victor Noir, a journalist at La Marseillaise. As a result, she took part in the demonstration among the 15,000 Parisians; she is "dressed as a man" and armed with a dagger.
Sources :
Edith Thomas
Xavière Gautier
7 notes
·
View notes
Text
David Wojnarowicz - Photo
Continuing my series of learning about things referenced in the book, I'm looking at things Alex references when he talks about engaging with queer history. These are all tagged #a series of learning about things that are referenced in the book, if you want to block the tag.

This post will cover the AIDS pandemic, which means there will be discussion of an incredibly large number of deaths, as well as government neglect of AIDS patients due to homophobia. There will be talk of the grief from the queer community & the ways it was weaponised to protest in an attempt for fundamental change. This is not a light topic, please take appropriate care when reading. As this post is going to have a few different topics in, so I decided to actually start with a read more, rather than arbitrarily place it partway down, I'd do a list of what is covered in this post & then have it all behind the cut.
So, in order, this post covers: David Wojnarowicz; AIDS; ACT-UP. In the additional reading section is a section subtitled "NAMES AIDS Memorial Quilt". This is worth looking into if you aren't already aware.
David Wojnarowicz is the man in the photo shown above, and referenced by Alex in the book. He was an AIDS activist, artist, writer, and filmmaker - among other things. He drew on his personal experiences with AIDS for his art & his political activism. In 1988, Wojnarowicz wore the leather jacket pictured above, with a pink triangle underneath text reading "if i die of aids - forget burial - just drop my body on the steps of the f.d.a." This jacket, and his similar sentiment from his book Close to the Knives, inspired David Robinson who - in 1991 - dumped the ashes of his deceased partner on the grounds of the White House in protest. These protests came to be known as "Ashes Action". Wojnarowicz died in his Manhattan home on July 22, 1992, aged 37, from what his boyfriend, Tom Rauffenbart, confirmed was AIDS. His ashes were scattered on the White House lawn in 1996.
-----
The AIDS epidemic in the US dates back to around 1970, but it wasn't until 1981 that cases started to come to light. The CDC (Centers for Disease Control and Prevention) published a report about 5 gay men becoming infected with a type of pneumonia only seen in people with compromised immune systems. As these men were healthy, this was unexpected. A year after, the New York Times published an article about a new immune system disorder, affecting over 300 people and killing over 100. Officials coined it GRID, gay-related immune deficiency, as it appeared to only be affecting gay men. It became officially known as AIDS (Acquired Immune Deficiency Syndrome) by August 1982, but was referred to as "gay plague" and many other derogatory terms for many years. Ninety-five and a half per cent of those diagnosed with AIDS between 1981 and 1987 died.
At the time, Ronald Reagan was president. He has been widely criticised for his reaction to the epidemic, for good reason. He didn't mention the word "AIDS" in public until 1985, by which time there had been 5636 deaths due to AIDS in the US. His first speech about the disease was delivered to the College of Physicians in Philadelphia in 1987, by which point there were more than 36,000 Americans living with AIDS & more than 20,000 had died. In the documentary When AIDS Was Funny (linked at the bottom), audios from press conferences in the early 1980s show how little the Reagan administration cared. Not only do they refer to AIDS as "gay plague", but joke around about it. It shows just how much the epidemic was derided - the people in charge of the country were so flippant about something so devastating, reflecting the general opinion of AIDS. Reagan's public support came overwhelmingly from the 'religious right', with Rev. Jerry Falwell using his political action group (the Moral Majority) to encourage homophobia aimed at gay men, especially those diagnosed with AIDS. Pat Buchanan, the White House Communications Director from 1985 to 1987, described the crisis as nature “exacting an awful retribution against gay men” in 1983.
Larry Kramer, when recalling the attempts to get help from public officials said:
You learn very fast that you’re a faggot, and it doesn’t make any difference that you went to Yale and were assistant to presidents of a couple of film companies, and that you had money. [source]
-----

On the 13th August, 1998, the Bay Area Reporter paper published a headline "No obits". For the first time in 17 years, there was finally a week without any deaths due to AIDS in the area covered by the paper - they are clear that there were deaths elsewhere, and they may have belated obituaries the following week, but for now this was a positive change. They had previously had up to 30 obituaries at points. Derek Gordon was quoted in the article as saying:
"I remember my grandfather said he knew he was getting near death because he used to scan the obits," he told the B.A.R. "I used to think how tragic because I was doing the same thing at 30."
-----
Wojnarowicz's jacket features a pink triangle on it. This was being used as a signal, as the pink triangle had been reclaimed by gay activists - originally in early 1970s Germany - to be used as a memorial to past victims & to protest continuing discrimination following its use by the Nazi Party to identify queer men in concentration camps. ACT-UP (AIDS Coalition To Unleash Power) adopted this icon, and turned it the other way up (so the point was at the top) and continue to use it to this day.
ACT-UP was formed in 1987, in New York City, and is now an international political group. It is working to end the AIDS pandemic using direct action, medical research & treatment, and trying to influence legislation. They debuted in October 1987, at the second National March on Washington for Lesbian and Gay Rights, not only by participating in the march but also with civil disobedience the day after. In the following October, ACT-UP shut down the F.D.A. (Food & Drug Administration) for a day in a demonstration against their drug approval process. The image of Wojnarowicz was taken that day, by William Dobbs. Activists shut down the F.D.A. by blocking the doors & walkways that would allow staff to get into the building. Some lay on the floor with faux-headstones, reading “DEAD FROM LACK OF DRUGS” and “VICTIM OF F.D.A. RED TAPE”. They attached a banner to the front of the building with ACT-UP's slogan - SILENCE = DEATH, bracketed by two pink triangles.
ACT-UP utilised different tactics from other groups - not only did they carry out (entirely non-violent) civil disobedience actions, but they also had the knowledge to be able to argue their demands successfully. The demonstration at the F.D.A. and their precise demands led to the F.D.A. listening to them and including them in decision making - and a year later their demands had started to come to fruition, with easier access to experimental drugs for those living with AIDS.
One 'Action' ACT-UP coordinated, was coined 'Ashes Action', as mentioned above. In 1992, ACT-UP marched to the White House fence to scatter the ashes of loved ones who had died due to AIDS onto the lawn of the White House. Inspired by Wojnarowicz's memoir, ashes were poured over the fence, demonstrating to the government explicitly the physical result of the AIDS policies. 'They had drums play a funeral cadence. They chanted—Bringing our dead to your door / We won't take it anymore and Out of the quilt and into the streets / Join us, join us. Unlike other protests, the Ashes Actions were not only meant to shock an uninterested public into empathy—they were meant as releases of grief for the activists themselves. "There was lots of room to scream and yell," Butler said, "but it wasn't always conducive to the work of mourning. I knew none of the people whose ashes we were carrying, but I remember when the ashes went over the fence of the White House. I just don't remember convulsive grief like the grief I felt in that moment."' [source]
sixteen, ashes of your forerunners rest on the lawn of the White House because SIXTEEN, THEY HAVE ALWAYS WATCHED US DIE. -SpondeeSoliloquy - Seventeen things (alternate link)
-----
I had to cut down a lot of the information here, so I would really appreciate it if you took the time to have a look through the additional reading below, there was a lot of things I would have added if I had the space.
-----
Sources: Wikipedia - David Wojnarowicz Guardian - David Wojnarowicz: still fighting prejudice 24 years after his death NY Times AIDS Timeline 1980-1987 History.com - History of AIDS Wikipedia - History of HIV/AIDS vox.com - The Reagan administration's unbelievable response to the HIV/AIDS epidemic US Studies Online The AIDS Crisis and the US Presidency SFGate - Reagan's AIDS Legacy / Silence equals death Washington Post - Pat Buchanan's Greatest Hits Wikipedia - Moral Majority Bay Area Reporter - No Obits Wikipedia - Pink Triangle Wikipedia - ACT UP New Yorker - How ACT UP Changed America Vice - Why the Ashes of People With AIDS on the White House Lawn Matter Pioneer Works - The Jacket
Additional Reading: When AIDS Was Funny - Documentary Film (cw for images of very unwell aids patients) LA Times - Police Arrest AIDS Protesters Blocking Access to FDA Offices Youtube - ACT UP Ashes Action 1992 Washington Post - AIDS ACTIVISTS THROW ASHES AT WHITE HOUSE Wikipedia - How to Survive a Plague Wikipedia - The Normal Heart (originally a play), 2014 film BBC - The drama that raged against Reagan’s America Wikipedia - Silence=Death Project Brooklyn Museum - Silence = Death Wikipedia - And The Band Played On - Randy Shilts NPR - How To Demand A Medical Breakthrough: Lessons From The AIDS Fight ACT-UP oral histories ClassicFM - Sobering black-and-white image of a gay men’s choir reminds of loss of life during AIDS epidemic Snopes - Does a Poignant Photo of Gay Men's Choir Show Devastating Impact of HIV/AIDS? Why We Fight - Vito Russo NAMES AIDS Memorial Quilt Wikipedia - NAMES Project AIDS Memorial Quilt national aids memorial - quilt history Cleve Jones interview (specifically: How he came up with the idea for the AIDS Quilt) View the NAMES AIDS memorial quilt online
#rwrb#rwrb movie#red white and royal blue#a series of learning about things that are referenced in the book#long post#alt text added#elio's#elio's meta#meta
54 notes
·
View notes
Text
The Risks of Killing a COVID Early Warning System - Published August 1, 2024
In Ontario, the government is rolling back its detection program. Doctors are speaking out about what’s at stake.
COVID-19 is surging in parts of North America and Europe, and even played a role in ending the presidential campaign of 81-year-old Joe Biden, who was infected for the third time last month.
Nevertheless, on Wednesday the Ontario government shut down its early warning system to detect COVID and other emerging diseases.
Doctors, citizens and researchers are calling the decision to kill the province’s wastewater disease surveillance program both wrong-headed and dangerous. Ending the program will make it harder to track and thwart viral outbreaks, they say, and thereby increase the burden on Ontario’s understaffed hospitals, which experienced more than 1,000 emergency room closures last year.
“Pandemics do not end because science has been muzzled,” Dr. Iris Gorfinkel, a well-known Toronto physician and clinical researcher, told the CBC.
In emails to politicians, more than 5,000 citizens have demanded restoration of the program, with little effect.
The Tyee is supported by readers like you Join us and grow independent media in Canada In 2020, at the height of the pandemic, Ontario launched one of the world’s most comprehensive disease surveillance systems by sampling wastewater.
For five days a week since then, sewage water has been monitored for signs of COVID and its variants.
The viral particles can be detected in wastewater seven days before people experience symptoms, giving an invaluable head start on public health measures and allowing advance warning of surges in illness. The system was expanded to include wastewater testing for monkeypox, influenza and respiratory syncytial virus, or RSV, and even drug-resistant bacteria, at more than 56 locations in the province. The system covered all 34 public health districts.
Unlike other forms of testing, wastewater surveillance is relatively cheap and can be done in a small university lab. It also provides reliable updates that decision-makers and the public could easily follow in real time.
The monitoring helped millions at high risk from COVID infections, including the elderly and citizens with cancer and other immune suppressive disorders, to determine the incidence of the virus in their communities. It gave them information about when to make medical appointments, where to mask up and when to avoid crowded indoor events.
For many Indigenous communities with substandard and crowded housing, the program also served as an early warning system for waves of respiratory diseases.
The program also provided timely warnings to parents on the risk of infants acquiring RSV, which can cause pneumonia. Hospitals, too, regularly used the results to prepare for staffing and resource challenges in the wake of infectious viral waves including COVID and RSV.
Read more at either link!
#covid#mask up#pandemic#covid 19#coronavirus#wear a mask#sars cov 2#still coviding#public health#wear a respirator#wastewater tracing
5 notes
·
View notes
Text
Q. How long should an outpatient be treated with antibiotics for bacterial community acquired pneumonia?
a. 3 days
b. 5 days
c. 7 days
d. 10 days
e. 14 days

A. Most patients require 5 days of therapy; 3 days is appropriate if they are stable and have been afebrile for at least 48 hours. It may be appropriate to prolong the course by 3-5 days if symptoms recur shortly after cessation.
Image of amoxicillin-clavulanate by Sage Ross, WikiCommons.
3 notes
·
View notes
Text
Chinese Hospitals Are Housing Another Deadly Outbreak
In Beijing and other megacities in China, hospitals are overflowing with children suffering pneumonia or similar severe ailments. However, the Chinese government claims that no new pathogen has been found and that the surge in chest infections is due simply to the usual winter coughs and colds, aggravated by the lifting of stringent COVID-19 restrictions in December 2022. The World Health Organization (WHO) has dutifully repeated this reassurance, as if it learned nothing from Beijing’s disastrous cover-up of the COVID-19 outbreak.
There is an element of truth in Beijing’s assertion, but it is only part of the story. The general acceptance that China is not covering up a novel pathogen this time appears reassuring. In fact, however, China could be incubating an even greater threat: the cultivation of antibiotic-resistant strains of a common, and potentially deadly, bacteria.
Fears of another novel respiratory pathogen emerging from China are understandable after the SARS and COVID-19 pandemics, both of which Beijing covered up. Concerns are amplified by Beijing’s ongoing obstruction of any independent investigation into the origins of SARS-CoV-2, the virus that causes COVID-19—whether it accidentally leaked from the Wuhan lab performing dangerous gain-of-function research or derived from the illegal trade in racoon dogs and other wildlife at the now-infamous Wuhan wet-market.
Four years ago, during the early weeks of the COVID-19 outbreak, Beijing failed to report the new virus and then denied airborne spread. At pains to maintain their fiction, Chinese authorities punished doctors who raised concerns and prohibited doctors from speaking even to Chinese colleagues, let alone international counterparts. Chinese medical statistics remain deeply unreliable; the country still claims that total COVID-19 deaths sit at just over 120,000, whereas independent estimates suggest the number may have been over 2 million in just the initial outbreak alone. Now, Chinese doctors are once again being silenced and not communicating with their counterparts abroad, which suggests another potentially dangerous cover-up may be underway.
We don’t know exactly what is happening, but we can offer some informed guesses.
The microbe causing the surge in hospitalization of children is Mycoplasma pneumoniae, which causes M. pneumoniae pneumonia, or MPP. First discovered in 1938, the microbe was believed for decades to be a virus because of its lack of a cell membrane and tiny size, although in fact it is an atypical bacterium. These unusual characteristics makes it invulnerable to most antibiotics (which typically work by destroying the cell membrane). The few attempts to make a vaccine in the 1970s failed, and low mortality has provided little incentive for renewed efforts. Although MPP surges are seen every few years around the world, the combination of low mortality and difficult diagnostics has meant there is no routine surveillance.
Although MPP is the most common cause of community-acquired pneumonia in school children and teenagers, pediatricians such as myself refer to it as “walking pneumonia” because symptoms are relatively mild. Respiratory Syncytial Virus (RSV), influenza, adenoviruses, and rhinoviruses (also known as the common cold) all cause severe inflammation of the lungs and are far more common causes of emergency-room visits, hospitalization, and death in infants and young children. Why should MPP be acting differently now?
One contributing factor to the severity of this outbreak may be “immunity debt.” Around the globe, COVID-19 lockdowns and other non-pharmaceutical measures meant that children were less exposed to the usual range of pathogens, including MPP, for several years. Many countries have since seen rebound surges in RSV. Several experts agree with Beijing’s explanation that the combination of winter’s arrival, the end of COVID-19 restrictions, and a lack of prior immunity in children are likely behind the surging infections. Some even speculate that that substantial lockdown may have particularly compromised young children’s immunity, because exposure to germs in infancy is essential for immune systems to develop.
In China, MPP infections began in early summer and accelerated. By mid-October, the National Health Commission had taken the unusual step of adding MPP to its surveillance system. That was just after Golden Week, the biggest tourism week in China.
Infection by two diseases at the same time can make things worse. The usual candidates for coinfection in children—RSV and flu—have not previously caused comparable surges in pneumonia. One difference this time is COVID-19. It is possible that the combination of COVID-19 and MPP is particularly dangerous. Although adults are less susceptible to MPP due to years of exposure, adults hospitalized for COVID-19 who were simultaneously or recently coinfected by MPP had a significantly higher mortality rate, according to a 2020 study.
Infants and toddlers are immunologically naive to MPP, and unlike COVID-19, RSV, and influenza, there is no vaccine against MPP. It seems implausible that no child (or adult) has died from MPP, yet China has not released any data on mortality, or on extrapulmonary complications such as meningitis.
Most disturbing, and a fact being downplayed by Beijing, is that M. pneumoniae in China has mutated to a strain resistant to macrolides, the only class of antibiotics that are safe for children less than eight years of age. Beyond discouraging parents to start ad hoc treatment with azithromycin, the most common macrolide and the usual first-line antibiotic for MPP, Beijing has barely mentioned this fact. Even more worrying is that WHO has assessed the risk of the current outbreak as low on the basis that MPP is readily treated with antibiotics. Broader azithromycin resistance in MPP is common across the world, and China’s resistant strain rates in particular are exceptionally high. Beijing’s Centers for Disease Control and Prevention reported macrolide resistance rates for MPP in the Beijing population between 90 and 98.4 percent from 2009 to 2012. This means there is no treatment for MPP in children under age eight.
Fears over a novel pathogen are already abating. After all, MPP is rarely lethal. But antimicrobial resistance (AMR) is. Responsible for 1.3 million deaths a year, AMR kills more people than COVID-19. No country is immune to this growing threat. Since China, where antibiotics are regularly available over the counter, leads the world in AMR, it is inconceivable that this issue hasn’t yet come up, particularly during WHO’s World AMR Awareness week, from Nov. 18 to Nov. 24.
Any infectious disease physician would want to know: Did WHO asked China the obvious question—what is the level of azithromycin resistance of M. pneumonia in the current outbreak—and include the answer in its risk assessment? Or did it ask about resistance to doxycycline and quinolones, antibiotics that can be used to treat MPP in adults? Even if WHO did ask, China isn’t telling, and WHO isn’t talking.
China’s silence isn’t surprising. Its antibiotic consumption per person is ten times that of the United States, and policies for AMR stewardship are predominantly cosmetic. While surveillance is China’s strong point, reporting is not.
Despite Spring Festival, the Chinese celebration of the Lunar New Year and another peak travel period, approaching in February 2024, WHO hasn’t advised any travel restrictions. It should have learned the danger of accepting Beijing’s statements at face value. Four years ago, Beijing’s delay enabled more than 200 million people to travel from and through Wuhan for Spring Festival. That helped COVID-19 go global. Since China’s AMR rates are already so high, importing AMR from other countries isn’t a major concern for China. Export is the issue, and China’s track record in protecting other countries is abysmal.
Rather than repeating the self-serving whitewashing coming from Beijing, WHO should be publicly pressing China about the threat of mutant microbes. Halting AMR is essential. Before antisepsis and antibiotics, surgery was a treatment of last resort. Without antibiotics, we lose 150 years of clinical and surgical advances. Within ten years, we are at risk of few antibiotics being effective. It may not be the novel virus that people were expecting, but the next pandemic is already here.
13 notes
·
View notes
Text
The Role of Ertapenem 100 mg in Modern Antibiotic Therapy
In recent years, the growing challenge of antibiotic resistance has prompted healthcare professionals to explore newer therapeutic options. Among these, Ertapenem 100 mg has emerged as a significant player in modern antibiotic therapy. This broad-spectrum antibiotic belongs to the carbapenem class and is renowned for its effectiveness against a variety of infections, particularly those caused by Gram-negative bacteria. In this blog, we will delve into the importance of Ertapenem, its applications, and its availability through Ertapenem 100 mg injection manufacturers in India, exporters, suppliers, and distributors.

Understanding Ertapenem
Ertapenem is a synthetic beta-lactam antibiotic that offers potent activity against a wide range of bacterial pathogens. Its unique structure allows it to penetrate bacterial cell walls effectively, making it suitable for treating complex infections, including those originating from intra-abdominal sources, skin and soft tissue infections, and pneumonia. Given the rising rates of resistance to commonly used antibiotics, Ertapenem provides a vital alternative for clinicians seeking reliable treatment options.
The Need for Effective Antibiotics
The World Health Organization (WHO) has recognized antibiotic resistance as one of the most significant global health threats. With an increasing number of bacterial strains becoming resistant to traditional therapies, the role of advanced antibiotics like Ertapenem has become crucial. The ability of Ertapenem to maintain its efficacy against resistant strains makes it an essential component of modern treatment regimens.
Applications of Ertapenem 100 mg
Ertapenem is indicated for various infections, including:
Intra-abdominal Infections: It is often used to treat complicated intra-abdominal infections due to its broad spectrum of activity.
Skin and Soft Tissue Infections: Ertapenem is effective against multiple pathogens commonly responsible for skin infections.
Pneumonia: This antibiotic is also a go-to treatment for community-acquired pneumonia.
Complicated Urinary Tract Infections: Ertapenem can be a critical option when dealing with complicated cases.
The versatility of Ertapenem makes it a valuable asset in a clinician's toolkit, particularly for patients who have not responded to other antibiotic therapies.
Availability in India
Ertapenem 100 mg Injection Manufacturers in India
India has a robust pharmaceutical industry, recognized for producing high-quality medications at competitive prices. Numerous Ertapenem 100 mg injection manufacturers in India are dedicated to maintaining stringent quality standards while ensuring that their products meet international guidelines. These manufacturers play a vital role in making Ertapenem accessible to healthcare facilities across the country and abroad.
Ertapenem 100 mg Injection Exporters in India
The global demand for effective antibiotics has led to an increase in Ertapenem 100 mg injection exporters in India. These exporters are crucial in supplying this essential medication to international markets, contributing to India's reputation as a leader in the global pharmaceutical landscape. The adherence to quality and regulatory standards has helped these exporters establish strong relationships with healthcare providers worldwide.
Ertapenem 100 mg Injection Suppliers in India
A reliable supply chain is fundamental for the availability of Ertapenem in hospitals and clinics. Numerous Ertapenem 100 mg injection suppliers in India ensure that healthcare institutions receive timely deliveries of this critical antibiotic. These suppliers work closely with manufacturers to maintain a steady stock, facilitating uninterrupted access to essential medications.
Ertapenem 100 mg Injection Distributors in India
The role of Ertapenem 100 mg injection distributors in India is equally important. They bridge the gap between manufacturers and healthcare providers, ensuring that the product reaches the end-users efficiently. Distributors are vital in managing logistics, handling regulatory compliance, and addressing the needs of various healthcare institutions. Their efforts ensure that doctors have immediate access to this antibiotic, particularly in emergency situations.
Best Indian Pharma Industry 2024
The best Indian pharma industry 2024 is characterized by innovation, quality, and a commitment to addressing public health challenges. With a focus on research and development, Indian pharmaceutical companies are continually improving their product offerings. The introduction of advanced antibiotics like Ertapenem is a testament to the industry’s efforts to combat antibiotic resistance. The commitment to maintaining high manufacturing standards and complying with international regulations has solidified India’s position as a trusted source for pharmaceuticals worldwide.
Conclusion
The role of Ertapenem 100 mg in modern antibiotic therapy cannot be overstated. As antibiotic resistance continues to pose significant challenges to healthcare, the importance of effective and reliable treatments like Ertapenem becomes even more critical. The collaboration among Ertapenem 100 mg injection manufacturers, exporters, suppliers, and distributors in India has made this essential antibiotic readily available to healthcare providers, ensuring that patients receive the best possible care.
In 2024, as the best Indian pharma industry continues to evolve, the ongoing development and distribution of innovative antibiotics will remain pivotal in the fight against infectious diseases. By prioritizing access to effective medications, we can work towards a healthier future and combat the ever-growing threat of antibiotic resistance.
#Ertapenem 100 mg for injection distributors in India#Ertapenem 100 mg for injection suppliers in India#Best Indian pharma industry 2024#Ertapenem 100 mg for injection exporters in India#Ertapenem 100 mg for injection manufacturers in India
4 notes
·
View notes
Text
bro is going community-acquired pneumonia mode
3 notes
·
View notes
Photo
want to add that the pneumonia vaccine (also known as the pneumococcal vaccine) only helps prevent one type of pneumonia (pneumoccocal pneumonia) however this type is one of the most common causes of community-acquired pneumonia! pneumonia can be caused by many different viruses and bacteria (and even fungi in rare cases!)
usamericans have probably seen Prevnar 20 and Pneumovax 23 ads on TV, those are both pneumococcal pneumonia vaccines

Wow — view on Instagram https://ift.tt/3hiS1uP
26K notes
·
View notes
Text
Pneumonia Specialist Doctor in Hyderabad: Expert Care for Respiratory Health

Pneumonia is a serious lung infection that can cause symptoms ranging from mild to severe, including fever, cough, shortness of breath, and chest pain. If left untreated, it can lead to complications, particularly in young children, elderly adults, and those with weakened immune systems. For anyone dealing with pneumonia or respiratory infections, it’s crucial to seek expert care from a pneumonia specialist to ensure proper diagnosis and treatment. In Hyderabad, several renowned pulmonologists and chest specialists offer expert care for pneumonia patients, and TX Hospitals stands as one of the top medical centers in the city.
What is Pneumonia?
Pneumonia occurs when the air sacs in the lungs become inflamed due to infection, often caused by bacteria, viruses, or fungi. Common symptoms of pneumonia include cough (which may produce phlegm), difficulty breathing, chest pain, fever, and fatigue. The condition can vary in severity, with some individuals experiencing mild symptoms that resolve with treatment, while others may require hospitalization.
Why Choose a Pneumonia Specialist?
A pneumonia specialist, or pulmonologist, is a doctor who specializes in diagnosing and treating diseases of the respiratory system. They have the knowledge and expertise to assess the underlying cause of pneumonia, prescribe the right antibiotics or antivirals, and monitor patients for any complications. Additionally, they provide comprehensive care for patients to recover fully and prevent recurrent infections.
Top Pneumonia Specialists in Hyderabad
Hyderabad is home to some of the best pneumonia specialists who are experienced in managing this condition. Whether you are dealing with community-acquired pneumonia, hospital-acquired pneumonia, or aspiration pneumonia, the following doctors in Hyderabad are highly regarded for their expertise in treating pneumonia.
Dr. B. Vijay Bhaskar – Expert Pulmonologist
Dr. B. Vijay Bhaskar is one of the leading pulmonologists in Hyderabad with an MBBS, MD in General Medicine, and DM in Pulmonary Medicine. He is known for his extensive experience in treating pneumonia and other respiratory conditions. Dr. Bhaskar offers personalized treatment plans, ensuring that each patient receives the appropriate care for their specific needs. His focus on evidence-based treatments makes him a trusted pneumonia specialist in the city.
Dr. Naresh Dude – Renowned Pulmonologist
With an MBBS, DNB, and FCCM qualification, Dr. Naresh Dude is a top pulmonologist in Hyderabad. He has vast experience in diagnosing and managing pneumonia, including complicated cases that may require intensive care. Dr. Dude’s ability to carefully assess and tailor treatment for each patient’s condition has earned him a reputation for providing excellent care for pneumonia and other lung infections.
Dr. Rohith Reddy – Lungs Specialist
Dr. Rohith Reddy, with an MBBS and MD in Pulmonary Medicine, is a renowned lungs specialist who provides expert treatment for pneumonia. He has a deep understanding of how respiratory infections affect the lungs and is skilled in managing pneumonia cases that range from mild to severe. Dr. Reddy uses advanced diagnostic techniques to identify the root cause of pneumonia and offers the most effective treatment options.
Dr. Sathish Pogula – Chest Specialist
Dr. Sathish Pogula, a well-respected chest specialist in Hyderabad, holds an MBBS, MD, and IDCCM qualifications. His comprehensive expertise in treating lung diseases, including pneumonia, ensures that his patients receive the highest standard of care. Whether it’s bacterial, viral, or fungal pneumonia, Dr. Pogula’s patient-centered approach helps manage and treat the condition effectively.
Dr. M.V. Sree Keerthi – Pulmonary Medicine Expert
Dr. M.V. Sree Keerthi is a highly skilled pulmonologist in Hyderabad, specializing in the treatment of pneumonia and other pulmonary diseases. With qualifications such as MBBS, DNB, and DTCD, she is known for her thorough approach to diagnosis and treatment. Dr. Sree Keerthi provides effective care for both community-acquired pneumonia and more severe forms that require hospitalization or intensive care.
Why Seek Treatment for Pneumonia at TX Hospitals?
At TX Hospitals, we understand the importance of prompt and effective treatment for pneumonia. Our team of highly skilled pneumonia specialists is equipped with the latest diagnostic tools and treatment methods to provide the best care possible. From the initial consultation to follow-up care, TX Hospitals ensures that each patient receives comprehensive treatment and support during their recovery process.
Our pulmonologists work closely with patients to develop personalized treatment plans, which may include medications, oxygen therapy, and lifestyle modifications. We also offer inpatient care for patients who need hospitalization, ensuring that they receive continuous monitoring and care in a comfortable environment.
Call 9089489089 for Expert Pneumonia Care at TX Hospitals
If you or a loved one is experiencing symptoms of pneumonia, it is essential to seek professional medical care right away. TX Hospitals offers expert consultation and treatment for pneumonia under the guidance of our highly experienced pulmonologists.
Call 9089 48 9089 today to schedule a consultation with a pneumonia specialist at TX Hospitals, and take the first step toward improving your respiratory health. Don’t delay—timely treatment is key to a full recovery.
#best pulmonologist doctor in hyderabad#best pulmonologist doctors in hyderabad#lungs specialist doctor in hyderabad#best lungs doctor in hyderabad#chest specialist doctor in hyderabad#pulmonologist doctor in hyderabad
0 notes