#can metastasis cancer be cured
Explore tagged Tumblr posts
Text
What is metastasis? 2023
New Post has been published on https://bankakredin.com/what-is-metastasis-2023/
What is metastasis? 2023
Cancer, which is considered one of the most important health problems of our age, maintains its seriousness, although there are promising medical developments and studies. In recent years, significant progress has been made in the early diagnosis and treatment of cancer, and it has been successfully applied in some patients. On the other hand, the desired progress could not be made towards some of the most feared mechanisms of cancer disease, which also significantly affect the clinical approach. One of these mechanisms is known as metastasis. Frequently asked questions in society, “What does metastasis mean?” It is very important to answer the question in terms of effective struggle with this health problem.
What is metastasis?
Metastasis; It is the process by which the cells of the tumor tissue that develops in a particular tissue pass to the closest vascular circulation as a result of various processes, reach a different body tissue from the region where it is located, and continue its development there. In this regard, metastasis results in the development of tumor cells in various parts of the body, in other organs and tissues that are completely different from the tissue of origin.
The newly developing tumor tissues after metastasis not only cause destruction in the body area they reach, but also adversely affect the functioning of the relevant tissue. In this regard, in addition to the clinical picture associated with serious cancer caused by increased tumor cells, complaints and findings related to the affected tissue begin to develop in the patient.
In the current clinical approach, the ultimate point that cancer tissues can reach is the state of metastasis. Since the diagnosis and treatment of cancer is handled specifically for the patient with the tissue of origin, in the clinical approach, the general condition of the patient and the treatment approach are determined according to the prevalence of the cancer case in the patient. In this approach, known as staging, the final stage of cancer disease is considered metastasis.
How does metastasis develop?
Cancer is basically a condition in which cells, which are a natural part of the body, gain the feature of uncontrolled cell division as a result of genetic changes under the influence of various genetic and environmental factors. In this respect, the affected cells begin to multiply rapidly, while the gene structure undergoes more and more changes. As a result of these changes, the cells that gain new features cause destruction in the body tissue they are in, while they can escape from the body’s immune system and trigger the development of vascular structures in the surrounding tissues.
In particular, cancerous cells, which multiply and become tumor tissue, increase vascularity and benefit more from the body’s nutritional products and oxygen. Over time, cells that change more and more genetically acquire properties that can leave the tissues they are in, and leave the vascular tumor tissue and pass into the circulatory system.
Cancer cells in the circulation become able to attach to other tissues with new genetic changes and, depending on the characteristics of the cancer cell, they settle in these tissues by acting more selectively on different body tissues. For example, while breast cancer cells are predisposed to bone tissues; Cancer cells originating from bone tissue tend to settle more in lung tissue. As a result, cancer cells that settle in the new body tissue multiply here, form new tumor clusters and metastasis occurs.
Some types of cancer instead of blood circulation; It passes through the lymphatic vessels of the tissue from which it originates and reaches the lymph nodes primarily through the lymphatic vessels. Cancer cells that continue to proliferate here can metastasize to distant body tissues via the lymph circulation.
Some specific types of cancer, such as lymphoma (lymph cancer), can infiltrate into the bloodstream and turn into leukemia (blood cancer) instead of forming clumps of tumors. In this case, instead of forming tumor tissue, widespread cancer cells are found in the bloodstream.
What symptoms can metastasis present with?
The state of metastasis develops depending on the origin of the cancer cell, its genetic characteristics and the individual characteristics of the patient. While some types of cancer rapidly metastasize; In some cases, cancer cells are not capable of distant metastasis. However, cancers that metastasize can have very different clinical manifestations depending on the distant body tissue affected. As a result of metastasis, a clear clinical symptom may not occur in the person and the person may be diagnosed with cancer at the metastasis stage. Besides; The following symptoms may occur in a patient who develops metastases during cancer disease:
Problems such as widespread bone pain after metastasis to the bone, deformity in bones, susceptibility to fracture, constipation due to increased blood calcium and phosphorus levels, heart rhythm disorders, kidney failure
Shortness of breath, cough, chest pain, blood in the mouth, respiratory failure and various heart problems after lung metastasis
Swelling, pain, inflamed fluid in the affected body areas after metastasis to the lymph nodes
Stroke findings after metastasis to the nervous system, loss of sensation or strength in various parts of the body, loss of balance, loss of vision, loss of speech ability, personality disorders, deterioration in consciousness
Jaundice, abdominal pain, predisposition to bleeding, swelling and fluid collection in the abdomen after liver metastasis, weakness – fatigue
Damage to the affected body tissues after occlusion of the vessels by tumor cells, amputation of the limbs, heart attack or stroke development
Regardless of the body tissues affected by metastasis, cancer cells that spread in the body by metastasizing can also be followed with the following clinical symptoms:
Weakness – tiredness
Serious Weight Loss
Swelling or anatomical deformity in the affected area due to the tissue of origin
Bleeding or inflammatory fluid coming from the affected tissue
Pain felt in the affected tissue
How is metastasis diagnosed?
For the diagnosis of metastasis, patients should be carefully examined and evaluated by a specialist physician with a detailed disease history and detailed physical examination. In a patient diagnosed with cancer, the patient is evaluated with various methods at regular intervals during treatment planning. In patients who are examined for cancer for the first time, the physician may apply for examinations with additional imaging and laboratory tests. In the light of the data obtained from all these examinations, a diagnosis of metastasis can be made with cancer.
Tumor clusters developing after metastasis; Depending on the affected tissue, it can be evaluated with x-rays, computed tomography, ultrasound or magnetic resonance (MR) methods. Again, some blood tests can be useful in evaluating recurrence and metastasis, especially in previously treated cancer cases. In patients diagnosed with cancer, it is possible to examine the whole body in terms of metastatic cancer tissues with nuclear medicine methods known as PET-CT and PET-MR.
Since the diagnosis of cancer can be confirmed after biopsy examination; whether the detected metastatic tumor clusters belong to another type of cancer; or biopsy may be necessary to understand whether it is due to the first cancer case diagnosed.
What can be done in the treatment of cancer that metastasizes?
Since cancer is a broad disease definition that develops depending on various factors such as the tissue of origin, genetic structure, and personal characteristics of the patient; Treatment planning is also determined specifically for the patient. In this respect, it is not possible to talk about a single defined treatment method for cancer or metastasis.
Although metastasis is accepted as the final stage in cancer cases; It is known that effective treatment methods can be applied after metastasis in selected cases. However, the primary purpose of the treatment methods applied for metastasis in the clinical approach is to increase the patient’s quality of life and survival time. In this regard, the following methods are frequently used in a patient with metastasis:
Chemotherapy : Antibiotics developed for cancer cells are known as chemotherapy in the community. Chemotherapy drugs prevent the proliferation of cancer cells through various mechanisms, enable them to be killed or facilitate their elimination by the immune system. Chemotherapy is the first choice in metastases that cannot be removed by surgery, especially since it spreads throughout the body and causes tissue damage.
Radiotherapy : Radiotherapy method, in which X-rays are used for metastatic tissues developing in some special tissues such as bone, may be beneficial. In this method, amplified radioactive rays are sent by focusing on the cancer tissue, and as a result of a few sessions, significant regressions can be obtained in the cancer tissues.
Nuclear medicine applications : Various nuclear medicine applications aiming to kill cancer cells with the accumulation of radioactive drugs by intravenous administration to cancer tissues can be applied in selected cases.
Hormone therapy : Some special types of cancer can be treated with various hormone drugs, thanks to their sensitivity to hormones.
Immunotherapy : Immunotherapy method, which aims to improve the immune system and clear cancer cells, can be applied in some patient groups.
Interventional methods : Some special interventional methods such as radiofrequency or gamma knife can be used to remove selected metastasis tissues other than surgery.
Surgery : In some selected cases, surgical removal of metastasis tissues may be considered in order to improve the patient’s quality of life and increase survival. The method, also known as metastasectomy, can be performed in some types of cancer and in suitable patients.
If you suspect the presence of cancer, apply to the nearest health institution to be evaluated by a specialist physician.
metastasis, what are metastasis symptoms, what are the stages of metastasis, what are symptoms of breast cancer metastasis, what are the symptoms of liver metastasis, what are symptoms of melanoma metastasis, what are the routes of metastasis, what are symptoms of skull metastasis, what are the signs of metastasis breast cancer, what are symptoms of brain metastasis, what are the causes of metastasis, can metastasis be cured, can metastasis be stopped, can metastasis cancer be cured, can metastasis be benign, can metastasis be non cancerous, can metastasis be seen on ultrasound, can metastasis spread, can metastasis cause fever, can metastasis cancer be treated,
#can metastasis be benign#can metastasis be cured#can metastasis be non cancerous#can metastasis be seen on ultrasound#can metastasis be stopped#can metastasis cancer be cured#can metastasis cancer be treated#can metastasis cause fever#can metastasis spread#metastasis#what are metastasis symptoms#what are symptoms of brain metastasis#what are symptoms of breast cancer metastasis#what are symptoms of melanoma metastasis#what are symptoms of skull metastasis#what are the causes of metastasis#what are the routes of metastasis#what are the signs of metastasis breast cancer#what are the stages of metastasis#what are the symptoms of liver metastasis
0 notes
Text
"I'll be here for you, my love"

Ford Pines x reader
You've been in the hospital for 5 years straight, your cancer developing and spreading. The tumor you had ignored had now developed and evolved, spreading to your organs, causing your stage 1 liver tumor to evolve into stage 4 metastasis.

Just yesterday the doctor walked into your room quietly, it was unusual. She had some news to break to you. "I'm afraid you only have a couple more days left. I've told you this before but its any time now, i'm sorry." You smiled at her, noticing the tear falling down her cheek and frown mentally, keeping a fake strong facade. "It's not your fault. I'm glad you tried your.best and never gavs up on me." Your hand curls into a ball under the sheet, doing your best to sray strong. The doctor left soon after, leaving you alone in the room with only your thoughts, your brain wandered 'will i tell ford?' 'Will he be okay?' 'I hope he's going to be fine without me'
You stared mindlessly at the ceiling, thoughts and memories rolling around in your mind like a film for a movie, you curse at the solidarity of your life, eventually falling asleep. You felt pathetic, worthless even, knowing that your husband too busy to even worry about you.
(You eventually fall asleep and wake up the next day)
It was another dreary day at the hospital, the sight of white boring walls and minimalistic decor making you lose your sanity by the minute, not having anything to suppress the agonizing pain you felt in your body.
-ford's pov-
"It has been a while since I last visited them at the hospital"
He murmurs, to no one but himself.
You've been gone for so long, off he visited you time to time, but ultimately focusing on the portal more and more to distract himself from worrying about you too much.
As he was working on his portal, his phone suddenly rang, causing him to jump at the sudden sound, rolling his eyes as he pushes himself away from the table (yk those chairs w wheels he basically just rolled over to the phone LMAO).
He accepts the call, ruffling his hair in frustration.
"Ford Pines here, who is this?"
"Ah, sorry, I'm doctor may here, what is your relationship to (reader)?"
He hums, fidgeting with a machine part with his fingers
"I'm their fiancé, what's wrong?"
The doctor clears her throat on the other line,
"I'm sorry to tell you, their tumor has started to spread to numerous other organs, I fear they don't have much time left.."
Ford feels his stomach drop, his hand loosening.
".."
"I suggest you get them out of the hospital and just spend time together, I'm afraid there isn't much we can do now. It's best to spend time while they're still here"
"..I see, thank you doctor."
The call ended, he immediately drops his phone and covers his face with his hands, tears falling down. They really couldn't do anything now. He didn't know what to do.
That night he spent his time sobbing, thinking of ways to help you, looking for a cure, a remedy, anything to help you, he failed miserably.
After a couple hours of thinking it over and breaking down he decided to pick you up from the hospital and spend time together, if you couldn't be there for the entirety of his life, atleast he'd be there for yours.
A/N
Hi hi!! This was shitty! I havent written anything for a while T~T please do send me some ideas/requests or if I did anything wrong plz do comment it down, also English isn't my first language so It's not perfect, this will be like 2 or 3 parts? I dont know yet but I will update :33 thank you again for reading <33
#idk anymore#bullshitting#stanford pines#gravity falls#gravity falls stanford#meow#random#i love stanford pines#stanford pines x reader#angst#yay#yippee
88 notes
·
View notes
Text
Dean Obeidallah at The Dean's Report:
Donald Trump was NOT convicted by Joe Biden, he was NOT convicted by the Judge, he was NOT convicted by the District Attorney. Donald Trump was convicted by a jury of his peers. A jury, I should note, that Trump was personally “very much involved” in picking per his lawyer Todd Blanche on CNN Thursday night. And that conviction happened in the state where Trump committed his crimes after a full trial that lasted more than a month where Trump was represented by a team of very experienced lawyers who presented his best defense. That is how our Constitution and criminal justice system works. There were no surprises here. As I predicted in my article before the trial began, “Trump is going to be a Convicted Felon by June." That was based on my experience as a trial lawyer and after reviewing the evidence the prosecutors had laid out in their pleadings. Common sense said that the only reason Trump paid Stormy Daniels “hush money” ten years after their affair —but just a week before the 2016 election—was to defraud voters of the truth. To that end, Trump falsified business records to conceal his illegal scheme. The jury saw the facts as they were, hence Trump was found guilty on all 34 counts and is now a CONVICTED FELON.
Yet now we see Trump and MAGA reject the jury verdict by attacking it as “rigged,” a “sham,” etc. MAGA House Speaker Mike Johnson called the verdict, “the weaponization of our justice system.” Marco Rubio weighed in on Twitter, writing, “The verdict in New York is a complete travesty that makes a mockery of our system of justice.” The always awful MAGA Rep. Elise Stefanik, posted, “Today’s verdict shows how corrupt, rigged, and unAmerican the weaponized justice system has become under Joe Biden and Democrats.” Spineless Tim Scott said on CNN Thursday night, “This was certainly a hoax, a sham” with the even worse Ted Cruz stating, “This entire trial has been a sham, and it is nothing more than political persecution.” And the list goes on and on. But this is no surprise, it’s part of MAGA telling us they reject our Constitution and the foundations of our democratic Republic. After all, Trump and MAGA rejected the 2020 election results because Trump lost. They rejected the criminal justice system when they smeared the indictments against Trump as being a sham. And now they publicly reject our jury system, which is one of the cornerstones of the US Constitution as laid out in the Sixth Amendment.
The question that must be asked is given Trump and MAGA reject our elections, our criminal justice system, the rule of law and our Constitution, what exactly do they support?! The answer is simple: Convicted Felon Trump. That’s it. [...] Let me repeat what I’ve been writing and saying for months: Don’t count on the courts, the prosecutors or a jury to save us from Donald Trump. We are the only ones who can do that by coming out in huge numbers to defeat him this November. This may sound jarring but it’s the truth: MAGA is a cancer. If allowed to metastasis, it will kill our democratic Republic that so many sacrificed so much to defend. The good news though is that the cure to MAGA cancer is right in front of us. All it takes is voting in big numbers this November.
The butthurt MAGAs crying and whining about Convicted Felon Donald Trump being convicted on 34 charges for business records falsification is more proof that the extremist anti-American MAGA cult needs to be crushed at all costs.
See Also:
Vox: Why the ludicrous Republican response to Trump’s conviction matters
MMFA: MAGA media rage in response to Trump's 34 guilty verdicts
RWW: MAGA Martyrdom Machine Portrays Felon Trump as Victim, Vows Revenge
HuffPost: Right-Wingers Are Already Promising Vengeance After The Trump Verdict
Daily Kos: Republicans choose MAGA lunacy over the law after Trump's conviction
#Donald Trump Trial#Donald Trump#People of New York v. Trump#Todd Blanche#Marco Rubio#Tim Scott#Elise Stefanik#Ted Cruz#Mike Johnson
46 notes
·
View notes
Note
No, I don't think it's as serious as the conclusions people are leaping to. If her cancer was actually "serious," then she would have stated that she is being "actively treated for cancer.
Oh, sorry if I’m a bit lost on this topic, but cancer experiences in my circle has been completely different from this.
I understand the point you are making. However I’ve seen many people saying that we don’t know in what stage the cancer was (I want to imagine it isn’t stage 4 since she wouldn’t have used ‘preventative’ chemo term, she should have used ‘chemotherapy’ term since it would have meant it was already metastasized and preventative wouldn’t be the case) and that she at the end ‘has’ cancer because doctors don’t know if she still has cancer cells on her body, so they will mop op those who remain and the doctors can’t see.
I’ve seen other people talking on their experience and saying that they went to surgery and only after it, it was detected the person has stage 3-4 cancer, is that possible? Or when you have a more advanced cancer it’s more visible with PET scans and other medical tests? Like I don’t understand or can’t comprehend how some doctors can’t see a stage 4 cancer in some organ if that would mean it was already in other organs, or how that works?

[previous ask]
A general overview of cancer (TNM) staging is described in detail here.
T = tumor, which can be staged 0 through 5 (depending upon organ/location). N = lymph node, has it spread to the lymph nodes? What kind of lymph nodes? Sentinel node, group of nodes, several groups of nodes? M = metastasis, yes or no
Specific staging numbers and letters varies based on where the primary tumor is located. Stage 3 or 4 cancer is unquestionably visible on imaging. Stage 4 is usually metastatic cancer, where lymph nodes have been affected. (Except for testicular cancer, which I understand no longer stages up to the number 4 because it has a 99% cure rate in the US.) This is when there are visible lesions on imaging, and surgeons can see tissue abnormalities during surgery with certain kinds of equipment.
Stage 0 is when no actual tumor/mass is found; it is also known as in situ, where abnormal cells in a single tissue layer have not formed a mass.
Consider Kate's statement:
“In January, I underwent major abdominal surgery in London and at the time, it was thought that my condition was non-cancerous. The surgery was successful. However, tests after the operation found cancer had been present. My medical team therefore advised that I should undergo a course of preventative chemotherapy and I am now in the early stages of that treatment."
Masses usually tend to be visible on imaging because radiographic imaging is very good these days. Even though she didn't mention it, she likely had pre-op imaging of some sort, probably a CT scan (with or without contrast). As Dr. Reiner mentioned on CNN, they would have known IF she had any suspect masses in her abdomen prior to surgery. They don't just cut people open and take a look under the hood. If the surgeons noted any abnormalities during the surgery, they would have told Kate after the surgery about those abnormalities and informed her the final results would be determined after testing by pathology.
If she didn't have any visible masses on imaging and if Kate isn't saying that her surgeons informed her of suspicious tissue post-op and they only "found cancer had been present" after pathology, then--based on her own statements--it sounds as if her "cancer" is in situ or stage 0.
As for how other people go through cancer screening or surgery and find out they are stage 3 or 4, well, that gets into how different people's biology grows cancer at different rates.
The below image is taken from a screen shot from Vinay Prasad's video on mammography, which I previously posted here. Vinay Prasad is a hematologist-oncologist (cancer doctor).
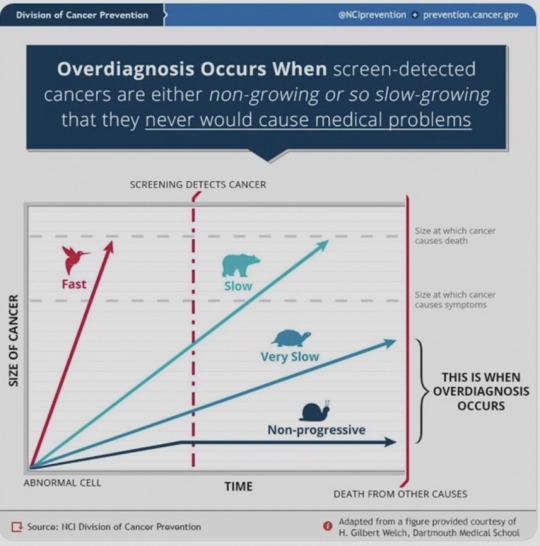
In this graphic, you see four trajectories with four different animals associated--bird, bear, turtle, snail. There is a red vertical line noting "screening detects cancer." There are two dotted gray lines. The top one notes "size at which cancer causes death" while the one below the bear (and the word "slow") says "size at which cancer causes symptoms."
The four trajectory animals:
Bird: fast growing cancer
Bear: slow growing cancer
Turtle: very slow growing cancer
Snail: non-progressive cancer
The example where you are describing, "I’ve seen other people talking on their experience and saying that they went to surgery and only after it, it was detected the person has stage 3-4 cancer," is a fast growing cancer. A "bird" "in the graphic above. Those kind of cancers are almost impossible to treat. It can be difficult for people with those kind of cancers to make it to the five-year survival rate no matter what kinds of treatments are used.
Charles probably has a "bear" type of cancer. Slow growing but detectable, which is why I suspect he's going to be okay. You can read some urologist comments from reddit here, which I previously posted. It's likely that Charles is being treated for bladder cancer, which was found after his benign prostatic hypertrophy (BPH) procedure. It's not uncommon to find bladder cancer during BPH procedures.
Kate--based on her own statements--sounds as if she has either a "turtle" or a "snail." If cancer wasn't suspected at all prior to her surgery, then it's likely that what she has currently would pose no immediate threat to her or in the near future. She could have waited six months and been re-evaluated. Instead, it sounds as if she is already napalming her own body with "preventative chemotherapy." A treatment she likely doesn't need but can afford because she has "the best doctors." It sounds more like over-treatment and carries serious risks.
You can read more about over-treatment & over-diagnosis in cancer in the following two articles.
While conventional wisdom holds that early diagnosis is good, H. Gilbert Welch, a professor of medicine and director of the Center for Medicine and the Media at the Dartmouth Institute for Health Policy and Clinical Practice, views it as a major problem for modern medicine, with myriad social, medical, and economic implications. In his new book, Overdiagnosed: Making People Sick in the Pursuit of Health (Beacon Press, 2011), Welch and coauthors Lisa Schwartz and Steven Woloshin write about the hazards of looking too hard for illnesses in healthy people, including additional procedures that carry no benefit, but may cause harm, higher health care costs, and psychological detriments.
Over a decade ago, Welch started looking into the effects of mass screening programs for cancer that have emerged around the globe. These programs take otherwise healthy people and subject them to tests to find out whether they have lumps and bumps that may be malignant. This is different from using ultrasounds or other technologies to diagnose people at risk of a disease or who have symptoms that require investigation. It's the type of preemptive screening that so many celebrities advocate. Welch found something surprising: in many cases, screening wasn't actually helping people or saving lives. The programs were turning healthy people into cancer patients unnecessarily, leading them to needless treatment and hospitalization, creating clubs of "cancer survivors" who actually would have lived even if their cancers were left untouched.
7 notes
·
View notes
Text
Surgical Options in Cancer Treatment: Procedures and Recovery

Cancer surgery is a common and effective way to treat many types of cancer and the specialist who does these surgeries is a Surgical Oncologist.
Surgery involves removal of tumor and some surrounding healthy tissue to prevent the cancer from spreading or coming back. Surgery can also help diagnose, stage the type of cancer and will help in suggesting further treatment if needed based on staging of cancer (tumor, node, metastasis) and relieving symptoms of cancer.
Biopsy of the surgical specimen will be sent to Pathology and Depending on the report Oncologist may suggest further treatment.
Surgery will determine the following:
If you have cancer
Where the cancer is located
If it has spread or is affecting other organs in the body
Surgery can be performed in a doctor's office, clinic, surgery centre, or hospital. Where you go depends on the type of surgery and how much time you need to heal. Your surgery may require medication to block the awareness of pain, called anaesthesia. There are different types of anaesthesia depending on the type and extent of the surgery.
Types of Surgery
There are different types of surgery for cancer treatment, depending on the type, location, and stage of the cancer, as well as the patient’s preferences and overall health. Some of the most common types of surgery are:
Open surgery: This is the traditional type of surgery that uses a scalpel to make a large incision in the skin and access the tumour. Open surgery can remove large or deep tumours, but it may also cause more pain, scarring, and longer recovery time.
Minimally invasive surgery: This is a type of surgery that uses small instruments and tiny incisions to remove the tumour. Minimally invasive surgery can include laparoscopic surgery (using a thin tube with a light and camera) or robotic surgery (using a computer-controlled device). Minimally invasive surgery can reduce pain, bleeding, infection, and recovery time, but it may not be suitable for all types of tumours.
Specialised surgery: This is a type of surgery that uses special techniques or devices to destroy or remove cancer cells. Specialised surgery can include cryosurgery (using extreme cold), electrosurgery (using electric current), laser surgery (using light beams), or Mohs surgery (removing thin layers of skin cancer). Specialised surgery can be more precise, less invasive, or more effective for certain types of cancers.
Recovery from Surgery
The recovery from surgery depends on many factors, such as the type and extent of the surgery, the patient’s age and health status, and the possible complications or side effects. Some common aspects of recovery are:
Pain management: The patient may experience pain or discomfort after the surgery, which can be relieved by medication, ice packs, relaxation techniques, or other methods.
Wound care: The patient may need to keep the surgical site clean and dry, change dressings, apply ointment, or avoid certain activities to prevent infection or bleeding.
Physical therapy: The patient may need to do exercises or stretches to improve mobility, strength, or range of motion after the surgery. Physical therapy can also help prevent blood clots, swelling, or lymphedema (fluid buildup).
Follow-up care: The patient may need to have regular check-ups with the surgeon or oncologist to monitor the healing process, remove stitches or drains, test for signs of cancer recurrence, or adjust the treatment plan.
Surgery is an important option for many people with cancer. It can help cure, control, or improve the quality of life for patients with different types of cancers. However, surgery also has some risks and limitations that need to be discussed with the doctor before making a decision.
For more details click on the link 👇🏻 https://bit.ly/3osreVo
#ICANWIN#YESITSRAM#FightAgainstCancer#CancerAwarenessMatters#TogetherAgainstCancer#CancerWarriorsUnite#EmpoweredByHope#RaisingCancerAwareness#IgniteTheFight#ConquerCancerTogether#InspireHopeForSurvivors#CancerFreeFuture
49 notes
·
View notes
Text
Article Review - What Is Cancer?
Here is my summary/reflection on this article:
1. The explanation about cancer is presented in a simple manner, by showing the difference between normal cells and abnormal cells in terms of the cell cycle. There are two types of cancers mentioned: solid (form masses) and blood (accumulate in blood).
2. The development from primary cancer to metastasis and their effects on nearby cells as well as the other parts of the body was shown.
3. Cancer has been becoming more common in recent years due to a variety of reasons. Genetic (People are surviving and living longer — likely that genes for cancer are being passed down across generations and that cell damage accumulates over age). Environmental (UV radiation, exposure to harmful chemicals, ionizing radiation). Lifestyle (Excessive smoking and consumption of alcohol, physical inactivity, diet)
4. Cancer is one of the leading causes of death in the world. However, these days, more options are available for treatment other than radiotherapy or surgical removal. Chemotherapy and biologics (immunotherapy, hormonal cure, antibody therapy) are new developments. The current methods are also being improved to be more precise and minimally invasive. Most interesting to read was CAR T-cell therapy, where the body’s own immune system can be programmed to kill cancer cells. After the pandemic, mRNA technology (nanoparticle delivery) has also been considered exploring as an option. AI is also a possibility in the sphere of diagnosis, modelling and treatment schemes.
5. In the last 40 years, survival rates have improved for many cancers. Yet, some types still see high mortality. Survival rates also depend on a combination of genetic, environmental, monetary and situational factors.
In conclusion, this article is a good start for anyone who wants to understand what cancer is. It can also serve as an introduction for students learning biology and medicine topics in schools.
Disclaimer: This is purely a concise reflection on the points presented in the article. These are not my opinions at all. I am only posting knowledge.
6 notes
·
View notes
Text
Thoughts: Healing Magic in the WoW universe and Cancer.
Hello everyone.
Let me ask a question.
How many of us, when life gets rough and painful, like to imagine our Azerothian counterparts from Warcraft sorting the situation out? Its a fun little coping mechanism isn't it?
Day been rough and stressful? Nice to think of getting a big hug from a pandaren.

Having to deal with someone at a job you'd really rather not? Isn't it just great to imagine a big burly orc knocking their lights out?

And when tragedy strikes us or our loved ones in the form of injury or illness... I think we've all wished for a world where our Priests, Shaman, Paladins, and the rest could help us heal them haven't we?

Oh for a world where the cure to our ills was a simple prayer to the Light, a whispered service to the Elements, or what have you...
Anyways... someone close to me, I'll leave out who in particular out of respect for their privacy, received some horrible news today. A close family member has been diagnosed with cancer.
As I suggested above, my first thought is... yep... I wish Sekhi or Nitika or any of my other WoW characters could swoop in and save the day with some magic.
But after the news had sunk in my overactive imagination kept going and... well... a new thought popped into my head concerning the nature of cancer.
You see... cancer isn't an injury or illness per se... cancer is when your own body turns against itself.
A Brief Aside on the Nature of Cancer
To quote the NCI or National Cancer Institute:
"Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body.
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
Sometimes this orderly process breaks down, and abnormal or damaged cells grow and multiply when they shouldn’t. These cells may form tumors, which are lumps of tissue. Tumors can be cancerous or not cancerous (benign).
Cancerous tumors spread into, or invade, nearby tissues and can travel to distant places in the body to form new tumors (a process called metastasis). Cancerous tumors may also be called malignant tumors. Many cancers form solid tumors, but cancers of the blood, such as leukemias, generally do not.
Benign tumors do not spread into, or invade, nearby tissues. When removed, benign tumors usually don’t grow back, whereas cancerous tumors sometimes do. Benign tumors can sometimes be quite large, however. Some can cause serious symptoms or be life threatening, such as benign tumors in the brain."
You can see the full article on this here.
This in turn made me think of something else.
I've been a visitor to Azeroth since before World of Warcraft existed and I've picked up quite a bit of lore as the huge mountain of fanfiction Adventures in Azeroth may have hinted.
If you read it.
You should really read it, I put a lot of work into it.
Moving on... it made me think of, in particular... the Forsaken, and how they show that healing magic is not always a good thing.
Forsaken and the Light
The Forsaken's relationship with the Light is not a very good one. In WoW cannon there are only two Forsaken characters who canonically use the Light at all even!
These two are the Archbishop Alonsus Faol, who priests would remember meeting during Legion...

And, of course, the newest member of the Forsaken. Former Princess of Lordaeron turned into the only known Lightforged Undead, Calia Menethil.

Canonically, any other Forsaken priests are Shadow priests rather than Holy or Discipline. This is going all the way back to the original World of Warcraft lore back at release. The Forsaken can use the Light for gameplay reasons, but there's a very good reason they don't in the actual canon.
You see, it has to do with the fact that they're undead.
The Forsaken exist in a state of sensory depravation, but in their case its a good thing.
Their bodies are dead. Their flesh is rotten and putrefied. Their teeth are moldy. Their skin flaking away to expose bone and nerve endings.
Normally a Forsaken heals themselves by consuming humanoid bodies or by things like Warlock Health Stones or Drain Life... but the Light does something horrible to the Forsaken.
It allows them to feel again, and they don't like it!
Being healed by the Light undoes the sensory depravation that the Forsaken experience, allowing them to taste the rot in their mouths, feel the exposed bone and nerve endings in their flesh, become acutely aware of their rotten forms, even when its used to heal them!
It may happen if a Druid or Shaman uses their powers to heal them, I don't know, but for a Priest or Paladin it is guaranteed. The ONLY known exceptions being Faol and Menethil as I mentioned above.
Which brings us back to the main topic.
Cancer isn't an invasive force like a virus or bacteria or a physical injury like a cut or bruise. Its the victim's body turned against itself.
Would a healing spell make the cancer go away... or would it "heal" the cancerous cells themselves?
A. Healing Magic Would Make the Cancer Worse

Since the cancer is part of the victim gone out of control, its possible that a healing spell would treat the cancer the same as it would the host.
Best case scenario, it cancels itself out and nothing changes.
Worst case scenario, the cancer cells become empowered and multiply faster!
It would make sense that there must be limits to healing magic in Azeroth or else why would anyone ever die?
Cancer and conditions like it could be among those limits. Healing magic would heal the victim's body, but since cancer is the victim's body... well, yeah.
B. Of Course it'd Help! Its MAGIC!

Its also possible that it could, well, just work because its magic. It breaks the laws of reality and nature simply by the fact that you can use it AT ALL!
A druid flexes her body and suddenly she's a panther. A mage gestures and his foe explodes in a burst of flames. A warlock grabs and pulls at the air and a hole rips in reality to allow their hellish minions entry.
In this situation, cancer would be the same as any other malady to a healer. They do their magical wand waving and POP all better, that'll be a 20,000 gold copay please.
C. Magic Could Help... but it'll be Messy.

Maybe, it'd take both an offensive spellcaster AND a healer.
What if a Mage's control over fire could cauterize away the cancer cells in a manner akin to radiation treatment, and a shaman or priest could then heal the burns that left?
Of course, spells like that would rely on line of sight... which would make this effectively arcane surgery. Someone would have to (ahem) allow for the mage to SEE the cancer to target it... as in, they'd have to cut the patient open so the mage could aim his spells properly. This would mean that the healer would have to also pull double duty as life support, which would in turn require them to control their healing magic as precisely as possible so that they don't accidentally go too far and close the incision the mage needs to attack the offending tumors!
But yes, this is simply a thought I had today and I felt was worth sharing. My mind does go on some weird tangents sometimes doesn't it?
I do hope we have some good news about the aforementioned cancer patient that sparked this line of thought, but... well, only time will tell there. At least I have something to distract myself from that line of thinking.
10 notes
·
View notes
Text
Exploring the Rapid Growth and Technological Innovations in the Stereotactic Radiosurgery Market - UnivDatos
According to a new report by UnivDatos Market Insights, the Stereotactic Radiosurgery Market is expected to reach USD 7.5 Billion in 2030 by growing at a CAGR of 5.1%. Surgical stereotactic radiosurgery is a minimally invasive procedure that uses high-precision radiation to treat a wide range of medical issues, like brain tumors, AVM (arterial vein malformation) malignancies, and nerve damage in the trigeminal nerve. Stereotactic refers to a frame that's used to guide the beams of radiation to the right spot. The stereotactic radiosurgery market is growing rapidly due to the increasing prevalence of chronic diseases like cancer. For example, in 2020, GLOBOCAN conducted a study on the incidence and prevalence of cancer in the world and estimated 308,102 new cancer cases diagnosed in the United States in 2020. Advances in technology have improved the accuracy and effectiveness of chronic disease treatment with minimally invasive procedures. This market is being boosted due to multiple factors like the rise in the geriatric population, increased expenditure in healthcare, and advancements in healthcare technologies. For instance, the World Health Organization (WHO) reported in October 2022 that between 2015 to 2050, the segment of the world's population over 60 years will nearly double from 12% to 22%, which will propel the stereotactic radiosurgery market at a steady rate.
Request To Download Sample of This Strategic Report - https://univdatos.com/get-a-free-sample-form-php/?product_id=49172&utm_source=LinkSJ&utm_medium=Snehal&utm_campaign=Snehal&utm_id=snehal
The report suggests that Rising Research and Development is one of the major factors driving the growth of the stereotactic radiosurgery market during the forthcoming years. Clinical trials are essential for the development of new and modified models for treating deadly disorders, as they provide valuable information on the effectiveness of the devices involved. In recent years, there has been an increasing number of clinical trials followed by FDA approvals focused on stereotactic radiosurgery. For instance, the University of Pittsburgh conducted a clinical trial to determine the efficacy of giving pre-operative radiosurgery to patients pending resection of a brain metastasis in 2021. they are investigating new techniques that may be more effective than existing treatment procedures. The increasing number of clinical trials for stereotactic radiosurgery is driving the growth of the market, as it indicates a greater interest in developing new treatments for stereotactic radiosurgery. It also provides hope for patients suffering from chronic diseases like cancer which cannot be completely cured but symptoms can be significantly minimized.
Regarding new launches related to stereotactic radiosurgery, there have been several recent developments. There are several clinical trials being conducted to test the effectiveness of treatments provided through stereotactic radiosurgery for cancer, and Parkinsonian-like diseases. These trials are still ongoing, but the early results look promising. For instance, the University of Chicago started a clinical trial to determine if not treating planning target volume (PTV) margins during radiation therapy worsens progression-free survival rates in patients with brain metastases in 2016. The study is expected to be completed by 2026. Additionally, there have been some new product launches in the market for cancer treatment using artificial intelligence. AI has been increasingly incorporated into medical procedures in order to accomplish tasks that may be difficult for human clinicians to do on their own. One area of medical need is the early detection of rare diseases, as this is often delayed. For instance, in June 2023, India-based Apollo Cancer Centre launched CyberKnife S7 FIM Robotic RadioSurgery System which claims to deliver hypo-fractionated SRS/SBRT treatments using Synchrony AI-driven, real-time target tracking. It addresses diseases, including benign brain tumors, brain metastases, and select medically refractory functional indications.
Ask for Report Customization - https://univdatos.com/get-a-free-sample-form-php/?product_id=49172&utm_source=LinkSJ&utm_medium=Snehal&utm_campaign=Snehal&utm_id=snehal
Conclusion
Stereotactic radiosurgery owns the ability to deliver high doses of radiation directly to the affected area while minimizing damage to surrounding healthy tissue. This can provide relief from symptoms and improve quality of life for patients who may have been unable to undergo traditional surgery or who have experienced complications from previous treatments for getting relief from chronic diseases like cancer. The global stereotactic radiosurgery market is a rapidly growing field, with advancements in treatment methods leading to improved outcomes for patients. It is expected to continue to grow in the coming years. Overall, the global stereotactic radiosurgery market represents a significant opportunity for pharmaceutical companies and professionals in the field of clinical research. With continued research and development, it is likely that even more effective treatments will become available in the future, leading to improved outcomes for patients with chronic disorders.
0 notes
Text
Why Is Mesothelioma Incurable in 2024? | Behind the Reason
Introduction Mesothelioma, a rare and aggressive form of cancer, remains challenging to cure despite advances in medical research. Its unique characteristics and the way it develops make it difficult to treat effectively. This article explores why mesothelioma is incurable and what options are available for patients.
Contact Us Now For a Free Consultation
1. What Makes Mesothelioma Different from Other Cancers? Mesothelioma originates in the mesothelial cells that line organs like the lungs and abdomen.
Aggressive nature: It spreads quickly to nearby tissues.
Late diagnosis: Symptoms often appear decades after asbestos exposure.
2. Why Is Mesothelioma Difficult to Diagnose Early? The latency period of mesothelioma, combined with non-specific symptoms, leads to delayed detection.
Latency period: Can be 20-50 years from asbestos exposure to symptom onset.
Similar symptoms: Mimics conditions like pneumonia or bronchitis.
3. How Does Mesothelioma Spread in the Body? Mesothelioma tends to spread to nearby organs and tissues, complicating treatment.
Localized spread: Often extends to the lungs, diaphragm, or heart.
Metastasis: Advanced stages may spread to distant parts of the body.
4. What Treatment Options Are Available for Mesothelioma? While there is no cure, treatments can help manage symptoms and prolong life.
Surgery: Removes tumors but is not always possible due to spread.
Chemotherapy: Helps to shrink tumors and manage growth.
Radiation therapy: Used to target cancer cells and reduce pain.
5. Are There Any Emerging Treatments for Mesothelioma? New therapies aim to improve patient outcomes and quality of life.
Immunotherapy: Boosts the body's immune response to target cancer cells.
Gene therapy: Investigates altering cell behavior to combat the disease.
Clinical trials: Offer access to cutting-edge treatments.
6. What Is the Focus of Current Mesothelioma Research? Research continues to explore better detection methods and new treatments.
Early detection: Developing blood tests and biomarkers for earlier diagnosis.
Targeted therapy: Aims to attack specific cancer cells without harming healthy cells.
Conclusion The incurability of mesothelioma is largely due to its aggressive nature, late diagnosis, and the complexity of its spread. Despite these challenges, advancements in research provide hope for better management and improved quality of life for those affected.
FAQs
Why does mesothelioma take so long to develop? The asbestos fibers cause chronic irritation that eventually leads to cancer after many years.
Can mesothelioma be detected before symptoms appear? Currently, it is difficult, but researchers are working on early detection methods.
Is palliative care common for mesothelioma patients? Yes, palliative care is often used to manage pain and improve comfort.
Why can't surgery cure mesothelioma? Surgery cannot always remove all cancer cells due to their spread to surrounding tissues.
Are mesothelioma survival rates improving? New treatments have improved some outcomes, but survival rates remain low.
What is the most promising new treatment for mesothelioma? Immunotherapy has shown promise in extending survival in some patients.
#mesothelioma#mesothelioma science#mesothelioma and lung cancer#causes of mesothelioma#mesothelioma research#mesothelioma (nci term)#mesothelioma experts#incurable#international symposium on malignant mesothelioma#curable#regulatory challenges in healthcare#house md season 5#out of the apocalypse#dr. jason fung#abandoned vehicles#serling and abramson#pleural disease symptoms#asbestos health precautions#livingwell cancer resource center
0 notes
Text
Magnetic Heating and Anti-Cancer Nonmagnetic Nano Systems

Magnetic Heating and Anti-Cancer Nonmagnetic Nano Systems in Biomedical Journal of Scientific & Technical Research
Cancer falls into the category of dreaded diseases. What is observed in a patients’ body is uncontrolled growth as well as spreading of abnormal forms of own living cells. In the same note, cancer cells can be distinguished from the normal by unique characteristics such as proliferation in an uncontrolled manner, functional loss, invasiveness, and metastasis. Once the cells undergo these transformation, criticality of the patient also enhances. To tackle this, there must be ways of early-stage detection so that mortality rate can be checked. With the advent of nanotechnology, it has become possible to dramatically improve on current approaches to cancer detection, diagnosis, imaging, and therapy while reducing toxicity associated with traditional cancer therapy. It is pertinent to mention here that existing cancer therapies are far too invasive, painful, toxic, and associated with too many acute and chronic side effects. Over the last three decades, rate of cancer cure encompassing major human malignancies have not improved so much over the last three decades. If we have a look at the three-year report of population-based cancer registries (2009-11) as issued by Indian Council of Medical Research (ICMR), India, the statistics reveal a varying pattern of cancer types with a heterogenous demographic distribution in the subcontinent. Among female, cancer of the breast and cervix are the leading site of cancer in 18 of 25 population-based cancer registries (PBCRs). In this regard, it can be asserted that novel treatment approaches based on nanotechnology will provide higher efficiency in curing patients and minimizing toxicity at the same time.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#journals on medical informatics#journals on biomedical imaging#biomedical open access journals#american medical journal#journals on medical microbiology
0 notes
Photo

Cancer is challenging to cure due to its complexity and variability. It involves numerous types of diseases, each with different characteristics, genetic mutations, and responses to treatment. Cancer cells can adapt, evolve, and develop resistance to therapies, making it difficult to target and eliminate them entirely without harming healthy cells. Cancer is difficult to cure for several key reasons: Cellular diversity: Cancer cells within a tumor can be genetically diverse, making uniform treatment challenging. Adaptability: Cancer cells can rapidly evolve and develop resistance to treatments. Similarity to normal cells: Cancer cells originate from normal cells, making it hard to target them without harming healthy tissue. Spread and metastasis: By the time cancer is detected, it may have already spread to other parts of the body. Complexity: Cancer involves multiple genetic and environmental factors, making it a highly complex disease. Immune evasion: Cancer cells can develop mechanisms to hide from or suppress the immune system. Heterogeneity between patients: Each person's cancer can be unique, requiring personalized treatment approaches. Cancer is Not a Single Disease Cancer is a term that encompasses a wide variety of diseases, each with its own unique characteristics and behaviors. Here are some examples to illustrate this diversity: Breast Cancer vs. Lung Cancer Breast Cancer: This type of cancer originates in the cells of the breast. It can be hormone receptor-positive, meaning it grows in response to hormones like estrogen or progesterone. Treatments often include hormone therapy, chemotherapy, radiation, and surgery. Lung Cancer: This cancer starts in the lungs and is often associated with smoking. It can be classified into small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). Treatments may include targeted therapy, immunotherapy, chemotherapy, and surgery. Despite both being cancers, the origins, behaviors, and treatments for breast cancer and lung cancer are quite different. Leukemia vs. Melanoma Leukemia: This is a cancer of the blood and bone marrow. It leads to the production of abnormal white blood cells. Leukemia is treated with chemotherapy, radiation therapy, and sometimes stem cell transplants. Melanoma: This is a type of skin cancer that develops from melanocytes, the cells that produce pigment. It is often caused by excessive exposure to ultraviolet (UV) radiation from the sun. Treatments include surgery, immunotherapy, targeted therapy, and radiation. Leukemia affects the blood and bone marrow, while melanoma affects the skin, highlighting the diverse nature of cancers. Prostate Cancer vs. Pancreatic Cancer Prostate Cancer: This cancer occurs in the prostate gland in men. It is often slow-growing and may not require immediate treatment. Options include active surveillance, surgery, radiation therapy, and hormone therapy. Pancreatic Cancer: This is a highly aggressive cancer that starts in the pancreas. It is often diagnosed at a late stage and has a poor prognosis. Treatments include surgery, chemotherapy, and targeted therapy Genetic Mutations and Variability Genetic mutations are changes in the DNA sequence of a cell. These mutations can lead to significant variability in how cancers develop and respond to treatment. Here are some examples to illustrate this concept: BRCA1 and BRCA2 Mutations in Breast Cancer BRCA1 and BRCA2 Genes: Mutations in these genes significantly increase the risk of developing breast and ovarian cancers. These genes normally help repair DNA damage, but when mutated, they fail to do so, leading to cancer development. Example: Angelina Jolie famously underwent a preventive double mastectomy after discovering she carried a BRCA1 mutation, which gave her an estimated 87% risk of breast cancer1. EGFR Mutations in Lung Cancer EGFR Gene: Mutations in the Epidermal Growth Factor Receptor (EGFR) gene are common in non-small cell lung cancer (NSCLC). These mutations cause cells to grow and divide uncontrollably. Example: Patients with EGFR mutations often respond well to targeted therapies like gefitinib or erlotinib, which specifically inhibit the EGFR protein2. KRAS Mutations in Colorectal Cancer KRAS Gene: Mutations in the KRAS gene are found in about 40% of colorectal cancers. These mutations lead to continuous cell growth and division. Example: KRAS mutations can make colorectal cancer resistant to certain targeted therapies, such as those targeting the EGFR pathway3. TP53 Mutations in Various Cancers TP53 Gene: Known as the “guardian of the genome,” the TP53 gene helps prevent cancer by repairing DNA or initiating cell death if the damage is irreparable. Mutations in TP53 are found in many types of cancer, including breast, lung, and colorectal cancers. Example: A TP53 mutation can lead to a loss of this protective function, allowing cancer cells to grow and spread unchecked Heterogeneity Within Tumors Tumor heterogeneity refers to the presence of a diverse population of cancer cells within a single tumor. This diversity can occur at multiple levels, including genetic, phenotypic, and functional differences among the cells. Here are some examples to illustrate this concept: Genetic Heterogeneity Example: In a single tumor, different regions may have distinct genetic mutations. For instance, one part of a lung tumor might have an EGFR mutation, while another part has a KRAS mutation. This genetic diversity can lead to varied responses to treatment within the same tumor. Phenotypic Heterogeneity Example: Cancer cells within a tumor can exhibit different physical characteristics, such as size, shape, and protein expression. In breast cancer, some cells might express high levels of hormone receptors (like estrogen receptors), while others do not. This can affect how the tumor responds to hormone therapy. Functional Heterogeneity Example: Different cancer cells within a tumor can have varying abilities to grow, invade tissues, and resist treatment. In glioblastoma, a type of brain cancer, some cells might be highly invasive, spreading quickly to other parts of the brain, while others might be more resistant to chemotherapy. Microenvironmental Heterogeneity Example: The tumor microenvironment, which includes surrounding blood vessels, immune cells, and other support cells, can vary within different regions of the tumor. In pancreatic cancer, some areas of the tumor might be well-supplied with blood, while others are hypoxic (low in oxygen). This can influence how different parts of the tumor respond to treatments like radiation therapy. Impact on Treatment The heterogeneity within tumors poses significant challenges for treatment: Resistance to Therapy: Different subpopulations of cancer cells may respond differently to the same treatment. For example, while chemotherapy might kill the majority of cancer cells, a small subset with specific mutations might survive and cause a relapse. Targeted Therapy Limitations: Targeted therapies are designed to attack specific genetic mutations. However, if a tumor has multiple mutations, a single targeted therapy might not be effective against all cancer cells. Adaptive Responses: Cancer cells can adapt to their environment and develop resistance mechanisms. For instance, if a tumor is treated with a drug that targets a specific pathway, cancer cells might activate alternative pathways to survive. Resistance to Treatment Cancer cells can develop resistance to treatments over time, making it challenging to achieve long-term remission. This resistance can occur through various mechanisms and can affect different types of cancer treatments, including chemotherapy, targeted therapy, and immunotherapy. Here are some examples to illustrate this concept: Chemotherapy Resistance Example: In ovarian cancer, patients often respond well to platinum-based chemotherapy initially. However, over time, the cancer cells can develop resistance, leading to a recurrence of the disease. This resistance can occur through several mechanisms, such as increased DNA repair capabilities of the cancer cells or changes in drug transport within the cells. Targeted Therapy Resistance Example: In chronic myeloid leukemia (CML), the drug imatinib (Gleevec) targets the BCR-ABL fusion protein, which is responsible for the uncontrolled growth of leukemia cells. While imatinib is highly effective initially, some patients develop resistance due to additional mutations in the BCR-ABL gene. These mutations alter the protein’s structure, preventing imatinib from binding effectively. Immunotherapy Resistance Example: In melanoma, immunotherapy drugs like pembrolizumab (Keytruda) work by enhancing the immune system’s ability to recognize and attack cancer cells. However, some melanoma cells can develop resistance by upregulating proteins that inhibit immune responses, such as PD-L1. This allows the cancer cells to evade detection and destruction by the immune system. Hormone Therapy Resistance Example: In hormone receptor-positive breast cancer, treatments like tamoxifen block estrogen receptors to prevent cancer cell growth. Over time, some cancer cells can become resistant by mutating the estrogen receptor or activating alternative growth pathways that do not rely on estrogen. Mechanisms of Resistance Cancer cells can develop resistance through various mechanisms, including: Genetic Mutations: New mutations can alter the target of the therapy, making the treatment less effective. Drug Efflux: Cancer cells can increase the expression of proteins that pump drugs out of the cell, reducing the drug’s intracellular concentration. DNA Repair: Enhanced DNA repair mechanisms can allow cancer cells to survive despite the DNA-damaging effects of chemotherapy. Alternative Pathways: Cancer cells can activate alternative signaling pathways to bypass the blocked pathway targeted by the therapy. Impact on Treatment Resistance to treatment poses significant challenges for cancer therapy: Relapse: Even if a treatment is initially effective, resistance can lead to a relapse of the disease. Combination Therapies: To overcome resistance, doctors often use combination therapies that target multiple pathways simultaneously. However, this approach can increase the risk of side effects. Personalized Medicine: Understanding the specific mechanisms of resistance in individual patients can help tailor treatments to overcome resistance and improve outcomes. Cancer’s Ability to Spread Cancer’s ability to spread, known as metastasis, is one of the most challenging aspects of the disease. Metastasis occurs when cancer cells break away from the primary tumor and travel to other parts of the body, forming new tumors. Here are some examples and explanations to illustrate this process: Breast Cancer Metastasis Example: Breast cancer cells can spread to various parts of the body, including the bones, liver, lungs, and brain. When breast cancer spreads to the bones, it can cause pain and fractures. If it spreads to the liver, it can lead to liver dysfunction and jaundice. Mechanism: Breast cancer cells can enter the bloodstream or lymphatic system, which acts as a highway for these cells to travel to distant organs. Once they reach a new site, they can establish a new tumor by adapting to the local environment. Lung Cancer Metastasis Example: Lung cancer often spreads to the brain, bones, liver, and adrenal glands. Brain metastases can cause neurological symptoms such as headaches, seizures, and cognitive changes. Mechanism: Lung cancer cells can invade nearby blood vessels and travel through the bloodstream to distant organs. They can also spread through the lymphatic system, which drains fluid from tissues and returns it to the bloodstream. Colorectal Cancer Metastasis Example: Colorectal cancer commonly spreads to the liver and lungs. Liver metastases can lead to liver enlargement, pain, and impaired liver function. Mechanism: Colorectal cancer cells can spread through the portal vein, which carries blood from the intestines to the liver. This direct connection makes the liver a common site for metastasis. Prostate Cancer Metastasis Example: Prostate cancer frequently spreads to the bones, particularly the spine, pelvis, and ribs. Bone metastases can cause severe pain, fractures, and spinal cord compression. Mechanism: Prostate cancer cells can spread through the bloodstream or lymphatic system. They often target bones because the bone microenvironment provides factors that promote cancer cell growth. Factors Influencing Metastasis Several factors contribute to the ability of cancer cells to spread: Genetic Changes: Mutations in certain genes can enhance the ability of cancer cells to invade tissues and spread to distant sites. Tumor Microenvironment: The surrounding environment of the tumor, including blood vessels, immune cells, and support cells, can influence the ability of cancer cells to metastasize. Cell Adhesion: Cancer cells can lose their ability to stick to each other, making it easier for them to break away from the primary tumor and travel through the body. Angiogenesis: The formation of new blood vessels (angiogenesis) can provide cancer cells with the nutrients and oxygen they need to grow and spread. Impact on Treatment Metastasis significantly complicates cancer treatment: Multiple Sites: Treating cancer that has spread to multiple sites requires a more comprehensive approach, often involving systemic therapies like chemotherapy, targeted therapy, or immunotherapy. Resistance: Metastatic cancer cells can be more resistant to treatment compared to the primary tumor, making it harder to achieve remission. Prognosis: The presence of metastasis generally indicates a more advanced stage of cancer and is associated with a poorer prognosis. Impact on the Immune System Cancer can significantly impact the immune system, both by evading immune detection and by actively suppressing immune responses. Here are some examples to illustrate how cancer interacts with the immune system: Immune Evasion Example: Melanoma cells can express high levels of PD-L1, a protein that binds to the PD-1 receptor on T-cells (a type of immune cell). This interaction inhibits T-cell activity, allowing the cancer cells to evade immune detection and destruction. Mechanism: By expressing PD-L1, melanoma cells effectively “turn off” the immune response against them, making it difficult for the body to recognize and attack the cancer. Immune Suppression Example: In ovarian cancer, the tumor microenvironment can be rich in regulatory T-cells (Tregs) and myeloid-derived suppressor cells (MDSCs). These cells suppress the activity of other immune cells that would normally attack the cancer. Mechanism: Tregs and MDSCs release cytokines and other factors that inhibit the function of cytotoxic T-cells and natural killer (NK) cells, which are crucial for targeting and killing cancer cells. Chronic Inflammation Example: Chronic inflammation, such as that caused by hepatitis B or C infections, can lead to liver cancer. The persistent inflammatory environment promotes genetic mutations and cancer cell growth. Mechanism: Inflammation can cause DNA damage and create a microenvironment that supports cancer cell survival and proliferation. Immune cells that are constantly activated can also produce growth factors that aid in tumor development. Immunotherapy and Immune Checkpoints Example: Immunotherapy drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) target immune checkpoints such as PD-1 and CTLA-4. These drugs block the inhibitory signals, allowing T-cells to attack cancer cells more effectively. Mechanism: By inhibiting the checkpoints, these drugs enhance the immune system’s ability to recognize and destroy cancer cells. This approach has shown success in treating cancers like melanoma, lung cancer, and renal cell carcinoma. Impact on Treatment The interaction between cancer and the immune system has significant implications for treatment: Immunotherapy: Leveraging the immune system to fight cancer has become a promising approach. Immunotherapies, such as checkpoint inhibitors and CAR-T cell therapy, aim to boost the body’s natural defenses against cancer. Combination Therapies: Combining immunotherapy with other treatments, like chemotherapy or radiation, can enhance the overall effectiveness. For example, radiation can increase the visibility of cancer cells to the immune system, making immunotherapy more effective. Personalized Medicine: Understanding the specific immune landscape of a patient’s tumor can help tailor immunotherapy treatments to achieve better outcomes. Side Effects of Cancer Treatments Cancer treatments, while effective at targeting cancer cells, can also affect healthy cells and tissues, leading to various side effects. Here are some examples of common cancer treatments and their associated side effects: Chemotherapy Example: Chemotherapy drugs target rapidly dividing cells, which include both cancer cells and healthy cells like those in the bone marrow, digestive tract, and hair follicles. Side Effects: Bone Marrow Suppression: This can lead to a decrease in blood cells, causing anemia (fatigue), leukopenia (increased risk of infection), and thrombocytopenia (increased risk of bleeding). Gastrointestinal Issues: Nausea, vomiting, diarrhea, and mouth sores are common due to the impact on the digestive tract lining. Hair Loss: Damage to hair follicles can result in temporary hair loss. Radiation Therapy Example: Radiation therapy uses high-energy particles or waves to destroy or damage cancer cells. It can also affect nearby healthy tissues. Side Effects: Skin Changes: Redness, blistering, and peeling of the skin in the treated area, similar to a sunburn. Fatigue: A common side effect due to the body’s response to radiation. Organ-Specific Effects: Depending on the area treated, radiation can cause specific side effects, such as difficulty swallowing (if the throat is treated) or urinary issues (if the pelvic area is treated). Surgery Example: Surgical removal of tumors can be an effective treatment but comes with risks and side effects. Side Effects: Pain: Post-operative pain is common and can be managed with medications. Infection: There is a risk of infection at the surgical site. Functional Impairment: Depending on the surgery, there may be a loss of function or changes in appearance (e.g., mastectomy for breast cancer). Hormone Therapy Example: Hormone therapy is used to treat cancers that are sensitive to hormones, such as breast and prostate cancer. Side Effects: Hot Flashes: Common in both men and women undergoing hormone therapy. Bone Thinning: Long-term use can lead to osteoporosis. Mood Changes: Hormone therapy can affect mood and emotional well-being. Targeted Therapy Example: Targeted therapies are designed to specifically target cancer cells with certain genetic mutations. Side Effects: Skin Problems: Rashes, dry skin, and changes in skin color. Liver Problems: Elevated liver enzymes indicating liver damage. Gastrointestinal Issues: Diarrhea and nausea. Immunotherapy Example: Immunotherapy boosts the body’s immune system to fight cancer. Side Effects: Immune-Related Side Effects: Inflammation of healthy tissues, such as colitis (inflammation of the colon), pneumonitis (inflammation of the lungs), and hepatitis (inflammation of the liver). Flu-Like Symptoms: Fever, chills, and fatigue. Managing Side Effects Managing the side effects of cancer treatments is crucial for maintaining the quality of life for patients. Here are some strategies: Monitoring and Adjustment: Regular monitoring of side effects allows healthcare providers to adjust treatment plans as needed to minimize adverse effects. Medications: Anti-nausea drugs, pain relievers, and other medications can help manage specific side effects. Supportive Care: Nutritional support, physical therapy, and counseling can help address the broader impacts of treatment. Ongoing Research and Hope Despite the challenges in curing cancer, ongoing research is making significant strides in understanding the disease and developing new treatments. Here are some examples of promising areas of research and the hope they bring: Targeted Therapy Example: Targeted therapies are designed to attack specific genetic mutations or proteins that drive cancer growth. For instance, drugs like trastuzumab (Herceptin) target the HER2 protein in certain breast cancers, significantly improving outcomes for patients with HER2-positive breast cancer. Hope: By focusing on the unique characteristics of cancer cells, targeted therapies can be more effective and have fewer side effects compared to traditional chemotherapy. Immunotherapy Example: Immunotherapy harnesses the body’s immune system to fight cancer. Checkpoint inhibitors, such as pembrolizumab (Keytruda) and nivolumab (Opdivo), have shown success in treating cancers like melanoma, lung cancer, and renal cell carcinoma. Hope: Immunotherapy offers the potential for long-lasting responses and even cures in some cases, as it helps the immune system recognize and attack cancer cells more effectively. CAR-T Cell Therapy Example: CAR-T cell therapy involves modifying a patient’s T-cells to express a receptor that targets cancer cells. This approach has been particularly successful in treating certain types of blood cancers, such as acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). Hope: CAR-T cell therapy represents a personalized treatment approach that can lead to complete remissions in patients who have not responded to other treatments. Liquid Biopsies Example: Liquid biopsies are blood tests that detect cancer-related genetic mutations and other biomarkers. They offer a non-invasive way to monitor cancer progression and response to treatment. Hope: Liquid biopsies can provide real-time insights into a patient’s cancer, allowing for more precise and timely adjustments to treatment plans. Cancer Vaccines Example: Cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells. The HPV vaccine, for instance, prevents infections with human papillomavirus, which can lead to cervical and other cancers. Hope: Preventive vaccines can reduce the incidence of certain cancers, while therapeutic vaccines are being developed to treat existing cancers by boosting the immune response. Gene Editing Example: CRISPR-Cas9 is a gene-editing technology that allows scientists to precisely modify DNA. Researchers are exploring its use to correct genetic mutations that cause cancer or to enhance the immune system’s ability to fight cancer. Hope: Gene editing holds the promise of directly targeting the genetic causes of cancer, potentially leading to more effective and lasting treatments.
0 notes
Text
Inner child, Inner Peace
I read article that writing can heal childhood psychological wounds, so i choose this platform to write little bit of my past as a kid.
As a kid I love rain, I used to climb 5 meters rambutan tree every time rain falls, rain made the trunk free from ant.
When I sat at the top, I start to contemplate and look to the raining sky, then started saying words in my heart:
"God why wont you answer our prayer to save my aunt from breast cancer? you cure the others and answer their prayer"
"Am I not devoted enough for You?"
"I volunteering myself to clean her stadium IV breast cancer, adapting my eyes to afford looking into big metastasis wounds that corrupted her skin and bone. I cleaned it with warm towel and covered her chest with piper ornatum leaf, almost every single day at home''
''Days after days seeing her will to live, yet you made me be the first one found her passed away on her bed after bring her glass of water"
" You know the day when she passed awasy, I feel like there is hole in my heart, witnessing ignorant family members reaction also the contrary Mom, her Husband and kid that really sad, but I know it cant be helped since we all were live in weak economy condition."
Then my mind said "Ahhh, why doesnt the lightning strike this rambutan tree anyway while I am sitting here"
1 note
·
View note
Text
sort of related to my last post but speaking of mentioning cancer, i dont think i updated my situation here
when i went back to my oncologist i essentially found out that while my scans didnt look anywhere near as bas as i thought, i'm being considered stage 4
theres a lymph node in my mediastinum that apparently is suspicious but as of now is only about 1cm
the whole reason im considered stage 4 is because with the spots they saw on my lungs, while they couldve been scar tissue from being sick, they also were thought to be metastasis. i'm not sure if we can confirm anymore but my lungs look good so that's all i care about
their goal now clearly isnt curing me but preventing the cancer from spreading as long as they can but rn i appear to be stable so hopefully new medications will help
0 notes
Text
The Rapidly Evolving Landscape of Cancer Therapeutics
Introduction
Cancer is considered as a common name to address a large group comprising more than 100 diseases affecting several parts of the body. All cancers show common characteristics such as the uncontrolled growth and proliferation of abnormal cells, infiltrating and spreading to different tissues and organs throughout the body, and destroying the normal cells and tissues. Cancer can begin in the epithelial tissue and is known as carcinomas, and when it begins in the connective or supportive tissue, they are called sarcomas. The blood cancers are known as leukemias, and when it begins in the plasma cells, they are known as myeloma. If the cancer begins in the lymphatic system, they are known as lymphoma, and if the cancer begins in the brain or spinal cord, they are known as cancers of the central nervous system. Cancers at the initial stages are currently considered as curable, and recurrent/metastatic cancers are considered chronic and difficult to manage, and needs multimodal therapies.
Molecular characterisation
The advancements in molecular characterisation of the disease, examining cancer at the molecular level, have resulted in the classification of a large number of cancer subtypes, and the current cancer therapies are also based on the cancer subtype, along with the stage and grade of the cancer. For example, in the case of colorectal cancer, the assessment of MMR status, KRAS,BRAF, and NRAS gene mutations, as well as the HER2/neu status to precisely identify the subtype, is considered indispensable for selecting the appropriate effective therapeutic approaches.
Multiple lines of therapy
Significant advancements have been made in cancer treatment modalities, resulting in the therapeutic continuum of care strategy with multiple lines of therapy leading to progression-free survival or cure in a large number of patients. The combinatorial strategies include surgery, chemotherapy, radiotherapy, targeted and biological therapy, as well as immunotherapy. For example, there have been limited treatment options for type II endometrial carcinoma, such as surgery, radiation, hormonal therapy, and the standard first-line chemotherapy with paclitaxel and carboplatin. The second-line chemotherapy in advanced/recurrent cancer utilised hormonal therapy, doxorubicin, and cisplatin without much benefits.
Currently, the advancements in therapeutic techniques resulted in several options in advanced/recurrent endometrial carcinoma after the treatment with surgery, adjuvant radiation or newer targeted brachytherapy, and neoadjuvant or adjuvant first-line chemotherapy with carboplatin and newer liposomal formulation of paclitaxel. The therapies include cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal metastasis, or cytoreductive surgery alone for advanced cancer, targeted biological therapy with antiangiogenic agents such as bevacizumab, mTOR inhibitors, and trastuzumab for HER2/neupositive cancer. The estrogen receptor and progesterone receptor (ER/PR) positive cancer can be managed with hormonal therapy such as tamoxifen. The second line chemotherapy has been almost replaced with immunotherapy utilising programmed cell death protein 1 (PD-1) inhibitor pembrolizumab or dostarlimab for mismatch repair deficient (dMMR)/ microsatellite instability-high (MSI-H) advanced cancer and pembrolizumab in combination with the multiple tyrosine kinase inhibitor lenvatinib for proficient mismatch repair (pMMR)/ microsatellite stable (MSS) advanced cancer, altogether resulting in a significant progression-free survival with a possibility of cure in several cancer patients.
Advancements in surgical techniques
Surgery is considered even now as the first line therapy in several types of cancers, but the advancements in surgical techniques, such as minimally invasive and precision surgery with the assistance of artificial intelligence, robotic techniques, and advanced molecular imaging, make it highly effective and minimises the side effects/complications after surgery. Surgical technique is also considered indispensable in the treatment of metastatic and advanced cancers, such as debulking or cytoreductive surgery, and can also be utilised along with specialised chemotherapy, such as the HIPEC in the case of peritoneal surface malignancies, which is considered a curative approach for the hitherto fatal disease.
Advancements in chemotherapy
Chemotherapy has improved significantly with the introduction of newer drugs, improved dosage regimens, targeted formulations, adjuvant and neoadjuvant administration, as well as combinatorial therapeutic strategies. An example of a novel delivery system is the widely used liposomal formulation of paclitaxel, which improves efficacy with a reduction in the side effects of chemotherapy. Chemotherapy can be administered during surgery in the hyperthermic form as HIPEC for the treatment of peritoneal surface malignancies, and the novel drug delivery system, pressurised intraperitoneal aerosol chemotherapy (PIPAC) is under development as a neoadjuvant treatment before cytoreductive surgery for the treatment of peritoneal metastasis. An example of newer combinatorial therapies includes the recent approval of dostarlimab-gxly along with paclitaxel and carboplatin for endometrial cancer. Another example is the recent approval of tipiracil and trifluridine along with bevacizumab for the treatment of metastatic colorectal cancer.
Read more: https://www.pharmafocusasia.com/articles/the-rapidly-evolving-landscape-of-cancer-therapeutics
Follow us:
Facebook:https://www.facebook.com/PharmaFocusAsia/
LinkedIn: https://www.linkedin.com/company/pharmafocusasia/
Twitter: https://x.com/pharmafocusasia
Instagram:
https://www.instagram.com/pharmafocuseurope/
Pinterest: https://in.pinterest.com/asiapharmafocus/
0 notes
Text
Metastasis: Detection, Treatment, and Coping Strategies
Introduction
Metastasis occurs when cancer spreads from its original site to other parts of the body. This typically happens when cancer cells break away from the primary tumor and travel through the bloodstream or lymphatic system, which transports fluids throughout the body. These cells can then form new tumors in distant locations, such as the lungs, liver, and bones.
What is Metastasis?
Metastasis usually develops in areas far from the original cancer site. Under a microscope, metastatic cancer cells look similar to the primary cancer cells. Almost all types of cancer have the potential to metastasize. The most common cancers that metastasize are those of the lungs, colon, rectum, pancreas, and breast. Metastasis can occur in various locations, including the bone, liver, lung, skin, muscle, peritoneum, and brain.
The Process of Metastasis
Metastasis in cancer happens in several steps:
The tumor increases in size and invades nearby tissues.
Cancer cells enter the walls of the lymphatic system and blood vessels.
These cells multiply rapidly, infiltrate the vessels' walls, and spread into surrounding tissues.
The cells continue to proliferate until a small tumor forms in the new tissue.
New blood vessels grow to nourish the developing tumor.
While many metastatic cells die at some point, those that survive continue to grow in their new locations.
As long as conditions remain favorable, these cells will form small tumors in other body parts.
Factors Influencing Metastasis
While metastasis is a hallmark of cancer, the factors influencing it are not fully understood. Several studies have been conducted to explore these factors. Cancer cells interact with different proteins and cells in the body when they spread to new areas. Understanding these interactions helps us recognize the characteristics of metastatic cells. These cells change due to DNA alterations or behavioral and environmental shifts.
Common Sites of Metastasis
Different cancers have distinct patterns of metastasis and can spread to various areas. For example:
Bladder cancer: bone, liver, and lungs.
Breast cancer: bone, brain, liver, and lung.
Colon cancer: liver, lungs, and peritoneum (lining of the abdominal cavity).
Kidney cancer: adrenal gland, bone, brain, liver, and lungs.
Stomach cancer: liver, lungs, and peritoneum.
Detecting and Monitoring Metastasis
Early cancer detection increases treatment effectiveness and reduces mortality rates. Screening for cancer helps prevent the spread and metastasis to other body parts. Various screening methods include:
Pap smears for cervical cancer.
Skin scrapings for skin cancer.
Colonoscopy for colorectal cancer.
Mammograms for breast cancer.
If you have a family history of cancer, early screening is advisable. Recognizing symptoms such as unexpected weight loss, fever, fatigue, pain, night sweats, digestive changes, and cough can be beneficial. Routine blood tests and medical imaging can help detect and monitor metastasis, keeping it under control with appropriate treatment.
Treatment Approaches for Metastatic Cancer
Treating cancer becomes more challenging once it spreads. Treatment options vary depending on the cancer type and its response to therapy. Treatment plans are based on the primary cancer site, not the metastasis location. Factors affecting treatment include metastasis site, previous treatment history, age, and overall health.
Treatment options include surgery, chemotherapy, radiation therapy, immunotherapy, hormonal therapy, and palliative care. Palliative treatment is often given alongside other treatments to all cancer patients.
Sometimes, the goal is to slow down metastasis rather than achieve a cure. In other cases, the focus is on symptom management and improving quality of life.
Coping with Metastatic Cancer
A metastatic cancer diagnosis brings numerous challenges and emotions. It's normal to feel upset, angry, sad, and scared. Acknowledge your feelings and seek support from loved ones for emotional comfort. Talking to a counselor or joining support groups can help you cope. Besides medical treatments, self-care is crucial. Engage in activities that bring you joy and peace. Remember, you are not alone. With medical advancements, treating cancer spread is possible. Although it may be more challenging, the latest medical management can provide positive results for metastasis.
Read More…
0 notes
Text
Skin Deep Safety: How Early Skin Cancer Detection Can Help With Prevention
Early identification with skin cancer detection increases the chance of a successful course of therapy and improves results by enabling quick medical intervention. When skin cancer is discovered in its early stages as opposed to its advanced stages, it is frequently easier to cure and may need fewer drastic measures.

Higher survival rates are linked to early identification with a skin malignancy check. Healthcare practitioners and organisations contribute to lowering the incidence of skin cancer and improving public health outcomes by raising awareness of the disease and supporting screening programmes. Most forms of skin cancer, particularly melanoma, have a good prognosis when detected and treated early on, with an increased chance of long-term survival and a decreased chance of metastasis, or the spread of the disease to other areas of the body.
Prevention of Illness Development and Its Impact on Community Health
To lower their chance of developing another skin cancer in the future, patients with the initial stages of skin cancer can benefit from counselling on sun protection, lifestyle changes, and routine skin exams.
Patients may rest easy knowing that their physicians are actively monitoring the health of their skin and taking proactive measures to identify and treat any suspicious abnormalities or lesions thanks to routine skin cancer tests and early detection.
The general avoidance and management of skin cancer in a community is aided by early detection programmes and public health campaigns that promote sun safety behaviours, encourage routine skin checks, and increase knowledge of skin cancer risk factors.
Monitoring Evolution With Customised Suggestions
Healthcare professionals can monitor changes in lesions, moles, or other abnormalities of the skin over time by doing routine skin malignancy screenings. It is possible to detect possible warning indicators of skin cancer or malignant disorders and choose the best course of treatment by keeping an eye on alterations to size, shape, colour, or texture.
Healthcare professionals can make individualised advice for sunscreen use, lifestyle changes, and follow-up treatment based on the results of a skin malignancy check. Patients who get personalised suggestions are better able to maintain good skin health and reduce their chance of acquiring skin cancer.
Source
0 notes