#journals on medical microbiology
Explore tagged Tumblr posts
Text
Characteristics of Head Center of Mass Sway and Neck Flexor Activity During Compensatory Backward Stepping in the Elderly

Characteristics of Head Center of Mass Sway and Neck Flexor Activity During Compensatory Backward Stepping in the Elderly in Biomedical Journal of Scientific & Technical Research
Research Question: This study aimed to determine age-related changes in head control during compensatory stepping against postural perturbation. Methods: Fifteen community-dwelling elderly individuals and 11 young adults participated in this study. We carried out the Push and Release Test, wherein a participant leaned on to the examiner’s hands. A compensatory backward stepping was triggered by suddenly releasing the supporting hands. Based on both ground reaction force and acceleration of the examiners’ hands, backward stepping was divided into four phases. Head sway and activity of sternocleidomastoid muscle were measured using a three-dimensional motion analysis system and an electromyograph. We determined the relationship between age and stepping phase in terms of head sway and sternocleidomastoid activity. Results: The results of a two-way analysis of variance confirmed the relationship between age and stepping phase in the amount of anteroposterior sway of head center of mass. T-test results revealed that, due to the sternocleidomastoid activity, the elderly group had significantly higher values in the single-stance phase than the young-adult group. Significance: Our data indicate a change with age in the compensatory stepping in response to load disturbances due to a decline of the ability of an individual to orient the center of mass of the head to an optimal location during compensatory stepping. In addition to insufficiencies of sensory inputs, the overactivity of the sternocleidomastoid is considered as one of the mechanisms for head control deficits.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#journals on biomedical imaging#journals on medical microbiology#biomedical open access journals#medical and medicinal journal#journals on medical informatics
0 notes
Text
I wish "your favorite sidekick" was a book instead of a fanfic so I could use "Excellently written,
Nearly medically accurate!" - actual medical doctor
As one of those quotes on the back.
#adventures of a fic writer#given my complete lack of any medical training whatsoever past a community college microbiology class#i think this speaks to the power of... well of being able to read medical journals without vomiting tbh
4 notes
·
View notes
Text
Also preserved in our archive
By Kevin Kavanagh, MD
Finally, a masking initiative I can support. I’m not talking about the misdirected efforts of emerging mask bans, one the latest in my home state of Kentucky. Instead, we need to emulate the NIH, which, on November 4, initiated a masking requirement at all National Institutes of Health (NIH) patient care areas. Our nation needs to come to grips with the fact that the pandemic is NOT over; the virus is very dangerous and poses risks to everyone. NIH is masking up, and so should we.
COVID-19 and long COVID are not old people’s diseases. Recent studies paint a bleak picture of long COVID and its effect on adults and children. The Naval Medical Research Command reported that almost 25% of studied Marines, most of whom had asymptomatic or mild acute COVID-19, “reported physical, cognitive, or psychiatric long-term sequelae of (COVID-19) infection.”
The economic impact is profound. Public health reports from Australia estimated that long COVID has caused a 0.5% loss in GDP. In New Zealand, a country of 5.7 million people, it is estimated the loss is 1.23 billion US dollars per year. The best study from the United States is from 2022 by the Brookings Institute that estimated 2 to 4 million individuals in the United States are not working because of long COVID. Since then, we have essentially handled this problem by not counting. However, the health care sector has been hit especially hard. A recent study from the United Kingdom found 33% of healthcare workers suffer from long COVID.
Most disturbing is the lasting brain damage from the virus, causing a decrease in cognition and executive function, damage resulting in poor judgment, and risky behavior. I seldom see anyone wearing a mask, and too few are up to date with their COVID-19 boosters. We are ignoring the pandemic and nonchalantly spreading the virus.
This phenomenon is occurring nationally. Recently, the American Automobile Association reported a spike in risky behavior associated with the pandemic, behavior manifested by an increase in speeding, driving under the influence of alcohol, and a decrease in seatbelt use. And a study in the Journal of Neurology found those who have had COVID-19 have higher rates of auto accidents.
Patients who have experienced COVID-19 with changes in their sense of smell are at an increased risk of developing “behavioral, functional and structural brain alterations” in the portion of the brain that controls emotion. COVID-19 has been found to diminish executive function in over half of patients with cognitive complaints, such as brain fog, memory loss, and lower I.Q. In Sweden, the insurance company, IF, found that almost a third of young adults have “brain fog”. In the Netherlands, there has been a 40% increase in adults seeking medical care for cognitive difficulties.
One only needs to look at what is happening in our communities and around the world to realize that people have a short fuse, and societies have become powder kegs of confrontations and violence.
SARS-CoV-2, the virus that causes COVID-19, can also undergo transformation, allowing it to better infect the brain. Recently, Jacob Class and colleagues in Nature Microbiology demonstrated that SARS-CoV-2 can lose its furin cleavage site, which is responsible for cellular entry (using the ACE2/TMPRSS2 receptor). This adaptation is hypothesized to optimize the virus’s ability to infect the brain using an alternate cellular entry pathway (Astrocytes or brain cells do not have observable ACE2 receptors).
Evolutionary pressure may be selected for viral mutations that allow SARS-CoV-2 to infect the brain, specifically the frontal lobes. In at least some individuals, this damage would increase risky and confrontational behavior, promoting the spread of this virus. This process would then repeat itself in the newly infected, further spreading the virus. This is not a pathogen to be taken lightly.
In Kentucky, we could possibly be seeing this scenario play out. A mask ban enacted in public venues will increase viral spread. Even outdoors, if you are within 6 feet of an infected person, large droplet spread can easily occur. Any proposed or enacted mask ban is anti-public health and will result in needless cases of long COVID, death, and disability. It will adversely impact our economy and the mental health of our citizens.
We must break this cycle of infections and disability. Clean indoor air, the wearing of N95 masks in public places, and vaccinations are keys to preventing new cases of acute COVID-19 and long COVID.
#mask up#public health#wear a mask#pandemic#covid#wear a respirator#covid 19#still coviding#sars cov 2#coronavirus
48 notes
·
View notes
Text

Lavender
Lavandula officinalis
Known as: Elf leaf, nard, nardus & spike
Related plants: A member of the mint family Lamiaceae, there are genus of 47 known species of lavender. It includes well known plants such basil, mint, rosemary, sage, savory, marjoram, oregano, hyssop, thyme, lavender, and perilla, as well as catnip, salvia, bee balm, wild dagga & oriental motherwort.
Parts used: Flowers
Habitat and cultivation: This flowering plant is native to the the Mediterranean
Plant type: Perennial
Region: Most are hardy from Zones 5 to 9 | Spanish Lavender (L. stoechas) is only hardy in Zones 7 to 9.
Harvest: You can harvest all the budding spikes or flowers on your plant during the growing season but avoid cutting into woody growth. Don't want to take more than 1/3 of the plant at this time & limiting your harvest to flowers and buds should keep you within recommended limits. As first frost approaches, snip off woody, leafy stems & branching. You can safely take up to 2/3 of the plant at this time. Harvesting too early can stimulate more growth which you don't want since the lavender is moving into winter dormancy.
Growing tips: To grow lavender successfully it needs well-drained soil, full sun & may be a good idea to check the PH beforehand because soil too acidic may kill off your plants. It survives well in dry conditions, so you'll only have to water when the top 2 inches of soil are dry. Plant lavender in spring, once all chances of frost have passed. This beautiful, fragrant herb is a great addition to raised beds, in-ground gardens, and growing in containers spacing plants 12 to 18 inches apart.
Medicinal information: Taking lavender products by mouth, including teas and a specific oil supplement or inhaling lavender oil as aromatherapy, seem to reduce symptoms of depression & anxiety. Lavender oil is believed to have antiseptic and anti-inflammatory properties, which can help to heal & burns & bug bites. Some studies suggest that consuming lavender as a tea can help digestive issues such as vomiting, nausea, intestinal gas, upset stomach, & abdominal swelling. A study published in the Journal of Medical Microbiology found that lavender oil could be effective in combating antifungal-resistant infections. Using it as aromatherapy can also reduce colic symptoms & menstrual cramp pain.
Cautions: Lavender essential oil is possibly safe when inhaled as aromatherapy, but applying products that contain lavender oil to the skin is possibly unsafe for young cis males who haven't reached puberty. The oil seems to have hormone-like effects that could disrupt normal hormones & in some cases, this has resulted in breast growth.
Lavender might cause sleepiness and slowed breathing. Taking lavender with sedative medications might cause breathing problems and/or too much sleepiness.
Lavender might slow down the central nervous system. If used with anesthesia and other medications given during and after surgery, it might slow down the central nervous system too much. Stop using lavender at least 2 weeks before a scheduled surgery.
Magickal properties
Gender: Masculine
Planet: Mercury
Element: Air
Deities: Aradia, Elves, Faeries, Hecate & Saturn
Magickal uses:
• Place in sleep pillows to encourage peaceful sleep
• Wear as a perfume to attract a new love
• Rub on paper when writing love spells or notes for added power
• Add with rosemary to a satchet for preserve chastity
• Scatter around your home to invite protection & purifying energies
• Use in a ritual bath to lighten feelings of depression or sadness
• Wear or use in an amulet to discourage cruelty from a spouse
• Drink lavender tea before bed to aid in astral travel or dream magick
• Burn as an incense for meditation or spirit work
• Use in spells to strengthen friendships
• Purify your ritual candles & tools with a drop of oil to release any negative energies contained within them
• Hang above your door protect against evil spirits , for home blessings & to cleanse all who enter
• Rub the oil on to the base of the skull or temples to help cure the nervous exhaustion that sometimes happens after intensive magickal workings
#herb of the week#magical herbs#herbalism#lavender#witchblr#wiccablr#paganblr#witch community#witches of tumblr#witch tumblr#witchcraft#spells#spellwork#grimoire#book of shadows#spellbook#tumblr witch#witch tips#beginner witch#baby witch#beginner witch tips#witchcore#correspondence#green witchery#GreenWitchcrafts#green witchcraft#traditional witchcraft#witch#witch guide#green witch
300 notes
·
View notes
Text
Semester 3 Recap as an MLS Major ᐟᐟ☆
Major Accomplishments: ʚ I have the opportunity to graduate a year early! ʚ I passed orgo! ʚ I actually took care of myself! ʚ I survived my most hectic semester yet!
Biggest Lesson: I can't actually get perfect grades and take care of myself fully at the same time. I would rather take care of myself, though. I didn't make the dean's list for the first time, but I actually felt good about myself and I felt that my mental and physical health were finally in a good place. A 3.4 GPA isn't going to kill me, but I will admit it made me upset. I have to realize that it isn't the end of the world to prioritize happiness over academic success.
Next Semester Goals: ʚ Get on the dean's list again ʚ Get halfway through writing my book (or to chapter 10 if I'm unsure what halfway is) ʚ Find housing for next year ʚ Figure out Physics at a community college over summer ʚ Fully flesh out my studying habits (I say this every semester oops) ʚ Start journaling in a more structured way

Rundown of each course:
Courses & Reflection: General Immunology [A]: Any time spent with this professor is truly a blessing. I wish he taught everything. He's really funny, and he's so intelligent that it kinda blows you away. He doesn't shove it in your face though, he meets you at your level. I'll miss him!! General Microbiology [AB]: The lecture was mid, but the lab... I love microbiology so much. I want to spend the rest of my life in a microbiology lab I think. It gets repetitive, but it's just so therapeutic and fun and everything I love about biology. Micro has always been my favorite discipline, but now that I got to fully indulge, I know for sure this is what I want to do. Basic Medical Lab Techniques [B]: I am kind of disappointed that I got a B in this class, because it's specific to my discipline. I do think that it taught me to be more diligent in the future, and to invest deeper into the material. Most MLS students at my school are pre-med, but I actually want to be a medical lab scientist. I have to put in the work, and I think this class set me up very well for that. I have a lot of new studying methods to test out and refine!! Organic Chemistry I [B]: My goal for this class was literally to pass. The fact that I got a B actually shocked me and made me really happy. I did put a lot of effort into orgo, and I tried harder than I have in any other chemistry course. I think chemistry finally clicked for me this semester. Anatomy and Physiology I Lab [B]: I got an A in AnP over the summer, but I was having a rough week when the first practical came along and I totally bombed it. So I will say that the B was a comeback from the DF I started with. However, I will keep better track of my practicals next semester, because that's lowkey embarrassing. Enterprise [A]: This was really fun, because it's so outside of my wheelhouse. I definitely did not expect to work on an engineering project in my academic career, but here I am. I love my team, and I'm really happy I did this. I'm going to stop trying to insert myself into the engineering side, and focus more on the medical, patient need, and kinesthetic side of building the prosthetic. Especially once we get into physical testing. I might ask my prosthetist for advice...
#kinda a hectic post lmao#studyblr#university#study blog#springstickinstem#self improvement#university student#student life#students#studyspo#studying#student#study notes#college life#college#study motivation#study aesthetic#classes#fall semester#end of semester#semester finals
6 notes
·
View notes
Text
Complement system
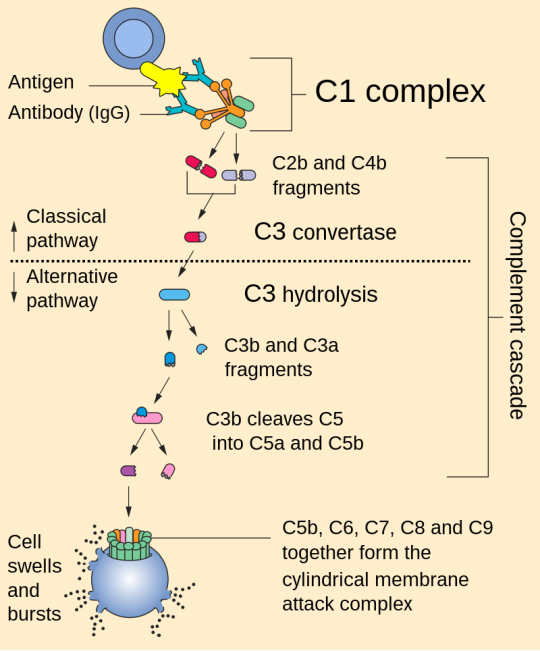
1. Activation: The complement system can be activated through three main pathways: the classical pathway, the alternative pathway, and the lectin pathway. Each pathway involves different initiating events but converges on a common cascade of reactions.
2. Cascade of Reactions: Once activated, the complement system triggers a cascade of enzymatic reactions that result in the cleavage of complement proteins. This cascade ultimately leads to the formation of several key components, including C3b, C4b, and C5b.
3. Opsonization: C3b and C4b are opsonins, which means they can bind to pathogens and label them for phagocytosis by immune cells like macrophages and neutrophils. This enhances the removal of pathogens from the body.
4. Inflammation: Complement activation also results in the release of small peptides called anaphylatoxins, such as C3a and C5a. These peptides promote inflammation by increasing blood vessel permeability and attracting immune cells to the site of infection.
5. Membrane Attack Complex (MAC): The final step of complement activation involves the assembly of the membrane attack complex (MAC). C5b, C6, C7, C8, and multiple C9 molecules come together to form the MAC, which can create pores in the membranes of target cells, leading to cell lysis and destruction of pathogens.
References:
1. Walport, M. J. (2001). Complement. First of two parts. New England Journal of Medicine, 344(14), 1058-1066.
2. Ricklin, D., Hajishengallis, G., Yang, K., & Lambris, J. D. (2010). Complement: a key system for immune surveillance and homeostasis. Nature Immunology, 11(9), 785-797.
3. Merle, N. S., Church, S. E., Fremeaux-Bacchi, V., & Roumenina, L. T. (2015). Complement system part I – molecular mechanisms of activation and regulation. Frontiers in Immunology, 6, 262.
Please note that for the most current and detailed medical information on the complement system, I recommend consulting recent textbooks or academic journals in immunology and microbiology.
#science#biology#college#education#school#student#medicine#doctors#health#healthcare#immunology#immune system#complement system
50 notes
·
View notes
Note
Hello I would love to hear the penicillin story and the bacteria story!
Hello dear seige ilyvm!! Consider this ur birthday gift :3 /silly
Okay, so the penicillin story is a lot more well known but i digress. Back in 1927, a Scottish scientist by the name of Alexander Fleming had been working on culturing bacteria. While Fleming was an undoubtedly good researcher, he also was slightly sloppy when it came to keeping things sterile and hygenic around his work station.
He ended up accidentally leaving the petri plate he was growing the bacteria on in a corner somewhere and discovered it weeks later - and realised it was contaminated. Instead of discarding it, Fleming was curious when he looked at the plate. Because you see, he observed that wherever the contaminant (a fungal mold) had settled down, the growth of bacteria was inhibited in those zones - the fungus was somehow keeping the bacteria away.
Fleming observed it under his microscope, and this fungus would later be identified to be Penicillium notatum. A few years later, two scientists by the name of Howard Florey and Ernst Chain found out about Fleming's findings and ended up isolating the compound we know as a life saving drug, and the original true antibiotic - Penicillin. This had happened right around WW2 too, so it's been said that the discovery of Penicillin and it's antibacterial properties provided a huge advantage to the allied forces.
A world without Penicillin would look very different, I think. And to think it was because a man forgot his petri plate in a corner somewhere. Fleming, Florey and Chain all received the Nobel Prize for their contributions in the discovery of Penicillin in 1945.
Now! Our second story, the bacteria story I mentioned needs some context first: in the field of clinical microbiology, to prove that a certain organism is a cause for a disease, there are certain criteria it must fulfill to be accepted as such. These are known as the Koch Postulates, laid down by scientist Robert Koch in 1890 and are still held in high regard.
These postulates state that if an organism is to be classified as a cause for a disease, it must:
1. Be present in abundance in the diseased host and absent in an organism that doesn't show symptoms of the disease.
2. Be able to be isolated and cultured (in a lab) from the diseased organism.
3. If contested, the causal organism must present the same symptoms in a test animal.
4. The microorganism must be able to be re-isolated and grown in a pure culture.
Now, in comes doctor Barry James Marshall. He was a physician, and had been looking into the cause of peptic ulcers, also known as stomach ulcers in humans.
Normally, things like this wouldn't be an issue. However, Marshall found that no matter what test animal he used, the isolated bacteria that supposedly were causing stomach ulcers showed no symptoms in them. Unable to fulfill all four criteria for the postulates, in frustration, he did what any sane scientist does and got an endoscopy done to confirm that he was healthy, and took a sample containing the possible causal organism and drank it.
A few days later, he developed the symptoms associated with stomach ulcers. He got another endoscopy done, and was diagnosed with stomach ulcers. He claimed that this should be evidence enough that a test animal (in this case, himself) displayed symptoms of stomach ulcers, and since the bacteria causing it could be further isolated from there, his point had been proven.
This experiment was published in 1985 in the Medical Journal of Australia and has been cited many times since. He received many awards for this, and his other contributions to the field of medical and clinical microbiology. The organism causing the ulcers was identified to be Helicobacter pylori. Marshall did get better, and to my knowledge is still healthy and alive today.
Science, especially biology and microbial sciences is filled with people who couldn't care less and had done more harm than good to it and the world around them. To them, it is simply a job. But there are some people who will go to the ends of the earth to help people, and spend day and night trying to help humanity. People may call them crazy, and perhaps they're right, but just like life, sometimes mistakes can be life saving instead of deadly.
Don't leave bacteria out on your desk for two weeks to go on a holiday though, that's probably not good.
#asks#tysm for this seige i had sm fun writing this#pls lemme know if u have questions :3#also these stories are summaries!! i wld implore u to go look for the full versions#toilet potato#anarcule tag
5 notes
·
View notes
Text
In a rare case, a black bear in Connecticut has tested positive for rabies, sparking a warning from state wildlife officials.
The bear was a wild female adult discovered in Canton, Connecticut, in February 2023. Like other bears, it should have been hibernating during the winter months. However, due to mobility issues on the left side of its body, the bear was seen falling over, lying down, and not responding to human presence, according to a new paper in the journal Microbiology Resource Announcements.
The bear was observed for 24 hours before being euthanized by a Connecticut conservation officer. Its body was taken to the Connecticut Veterinary Medical Diagnostic Laboratory (CVMDL) at the Unversity of Connecticut's College of Agriculture, Health and Natural Resources for a post-mortem.
After the CVMDL sequenced the bear's brain tissue during the necropsy, they discovered that it was infected with rabies. This was only the second bear the lab had encountered with the virus.
The Connecticut Department of Energy and Environmental Protection (DEEP) has advised the public to avoid any animal that "appears to be distressed, which may include symptoms like stumbling, staggering, walking in circles, dragging a limb or the hind end, or otherwise acting strangely," according to a statement from the University of Connecticut.
Rabies is a viral disease that affects the central nervous system of mammals, causing the inflammation of the brain. The virus is typically transmitted through the saliva of infected animals via bites, scratches, or even mucous membranes and open wounds. It is almost always fatal once symptoms appear, which generally manifest after around 2–3 months and can initially include fever, headache and weakness, progressing to agitation, anxiety, hallucinations, a fear of water, excessive salivation, and lack of coordination.
If an animal displays neurological symptoms, such as stumbling and falling over, then scientists will first test for rabies. If the test comes back positive, CVMDL does not proceed with a full necropsy to protect staff.
"We rule out rabies because we don't want to do a necropsy that could expose people unnecessarily," Guillermo Risatti, CVMDL director and professor at the University of Connecticut, said in the statement. "So, once we detect rabies, that's it. We don't do anything else with the carcass."
The CVMDL scientists sequenced the entire genome of the rabies virus found inside the bear to compare it with a gene bank of other sequences from animals infected with rabies across the world. They found that the virus in the bear—which was the only bear sample on the whole database—most closely resembled a virus sequence from a raccoon in New England.
By comparing these strains of rabies, scientists can investigate how the virus spreads between animals in certain areas.
"That's the value—to see what the virus looks like and be able to distinguish a new virus coming into the area," Risatti said. "All of the sequencing is done by us, here in house. So that is the value. We have created a sequencing lab inside a diagnostic lab that is allowing us to dig more into what is going on."
Only 1 to 3 cases are reported in humans in the United States annually. If a human contracts rabies, they need to receive post-exposure prophylaxis as soon as possible, which can be up to 100 percent effective at preventing the disease. Around 60,000 people receive this post-exposure prophylaxis in the U.S. every year.
Humans most at risk are those living in areas where wildlife that commonly contract rabies, including bats, raccoons, skunks, and foxes, are common. While this case of rabies in a bear is rare, it may become more common in the future, as sightings of black bears in Connecticut have increased lately.
Nine bears were submitted to the CVMDL for testing in 2023 alone, compared to seven between 2019 and 2022.
The DEEP advises calling the local animal control officer or police department if you spot a potentially rabid animal, staying well clear of it, and definitely not attempting to pick it up.
10 notes
·
View notes
Text
How to Prepare for the FMGE/NExT Exam After Studying MBBS Abroad

The choice to study MBBS abroad, especially in countries like Russia, is unique and enriching. However, after completing medical education, the FMGE or NExT has to be cleared to practice in India, which forms a big challenge for MBBS students from all abroad. The journey through FMGE or NExT becomes quite intimidating and complicated for MBBS graduates from any foreign university. Prepare to take the FMGE/NExT Exam after MBBS abroad study as follows.
Understanding the FMGE/NExT Exam
The FMGE is the examination conducted by foreign medical graduates for practicing in India. It is conducted by the National Board of Examinations (NBE). Basically, this exam tests the knowledge and clinical skills of candidates who have completed their MBBS degree from outside India.
The NExT exam, on the other hand, is going to replace the FMGE and will be the gateway for MBBS students across India, including those who graduate from foreign medical schools. The NExT exam will be a two-part examination system: one for theoretical knowledge (NExT-1) and one for practical and clinical skills (NExT-2).
MBBS students who have completed their education abroad require passing the FMGE/NExT to get a medical license in India.
Step 1: Understand the Syllabus and Exam Pattern
The first step in your preparation is to understand the syllabus and exam pattern. The FMGE syllabus covers subjects from all the major medical disciplines, including:
Anatomy
Physiology
Biochemistry
Pathology
Microbiology
Pharmacology
Forensic Medicine
Medicine, Surgery, Pediatrics, Obstetrics and Gynecology, and more.
The NExT exam would have a comparable syllabus, but it will be more elaborative and practical. It's essential to thoroughly study each topic because these tests not only focus on theoretical concepts but also put your ability into practice in practical medical scenarios.
Step 2: Plan your study schedule Structure your study time into manageable slots. Focus on subjects like Medicine, Surgery, and Pediatrics, as these areas carry higher weight. Use multiple resources such as textbooks, online lectures, question banks, and mock tests to reinforce your knowledge.
Step 3: Use Question Banks and Practice Papers
Continuous practice is one of the best ways to prepare for any medical exam. Make use of FMGE question banks and previous years' papers to understand the kind of questions that are asked. These papers not only help you get familiar with the exam format but also give you an idea of frequently asked topics.
The relevant focus for NExT would be on clinical questions and case scenarios, which are going to comprise a significant portion of the practical assessment. Preparing clinical vignettes, MCQs, and problem solving is key to doing well in the NExT exam.
Step 4: Strengthen Clinical Skills
Since FMGE and NExT are basically very clinical courses, one would require sharpening their practical knowledge. Clinical rotation or observing hospitals can be conducted. Discussing clinical cases among friends or consulting senior doctors shall enhance the skill of clinical reasoning and confidence level.
Step 5: Take Online Courses or Coaching
For students who have studied MBBS abroad, online coaching for FMGE/NExT is a very good way of keeping track with your preparation. Many coaching centers provide specialized FMGE crash courses to help the foreign medical graduate pass the exam easily.
Moreover, coaching will offer mock exams, personalized guidance, and can keep you motivated during your preparation.
Step 6: Staying Updated on Medical Knowledge
The medical field is always developing, and you must ensure your knowledge is updated. Stay current with recent advances in medical science, new diagnostic tools, and treatment methods by reading medical journals, attending webinars, and participating in conferences. This will not only make you better prepared but will benefit you in the long run too in your medical career.
Step 7: Manage Stress and Time
It is very stressful to prepare for FMGE/NExT, so it is necessary to keep one's mental and physical well-being intact. Include regular exercise, adequate sleep, and breaks to keep your mind fresh.
Final Thoughts
Passing the FMGE or NExT exam is one of the final steps after MBBS abroad, especially MBBS in Russia. With proper knowledge of the syllabus, following a proper study plan, practicing clinical skills, and updating oneself with the latest medical knowledge, one can be adequately prepared for these exams.
Be dedicated, plan your time, and take the exam with confidence. Consistent preparation will get you well set for a medical career in India.
Good luck!
#mbbs abroad#mbbs in russia#study abroad consultants#medicaleducation#mbbs#neetpreparation#fmge coaching#next coaching
2 notes
·
View notes
Text
Rabid; A Cultural History of the World's Most Diabolical Virus
[Review; 2.75 stars]
Y'know how when you read a fanfiction on AO3 and accidentally miss a tag? Yea, that's what reading this book felt like because I found out about it from a TikTok that pitched it as the history of rabies which yes, but also not really.
It somehow made its focal topic not feel like the focal topic. In that it somehow got pushed to the side and frankly annoyed tf out of me. There was also barely any structure outside of the frowned upon 'in this essay, I will...' type. The chapters poorly established what they were meant to cover. To the point that I would ask myself multiple times ‘What is the point here? Why are you including this information? Relevance?’ while reading. Hell, my reading journal entry for this book is 3-4 lines per chapter, summarizing what they’re about. Most of the chapters were about how rabies has been portrayed in media and has been the origin of certain horror subgenres (werewolves, vampires, & zombies) but even that fell flat.
If you are genuinely interested in the medical aspect of the history behind rabies, then all you need to read is chapters 5, 7, & 8. And can just skim the rest to find what little there was.
Furthermore, there were citations at the end of the book that weren't even done correctly. As in, they were just the link to the website. No website title, website publisher, date published, nor date accessed. None of it.
[Chpt summaries under the cut]
Chpt. 1 - mentions of rabies in Greek & Egyptian mythologies, earliest mentions in medical texts & attempted treatments, pets vs strays
Chpt. 2 - Middle Ages; Saint Hubert & deer iconography in Christianity, mentions of dogs in the Bible, how basilica established in Hubert's name treats rabies (la taille), how rabies & the Bubonic plague relate to one another + the origin of the words rabies & rabid
Chpt. 3 - Vampires & werewolves; how they could be folklore based off of/around rabies & how many cultures have folklore regarding wolves/dogs being representative of demons/possession + lycanthropy based witch-hunts & the 1st literary mentions of vampires
Chpt. 4 - Colonial America; Benjamin Rush & Mease & how the theory of spontaneous rabies in dogs halted progress + canicides, where people killed dogs en mass due to rabies-related fear
Chpt. 5 - Louis Pasteur & his work in microbiology; how his vaccine for anthrax led to him developing a vaccine for rabies. Also the scientific community established key characteristics of the virus
Chpt. 6 - the zoonotic epidemics of the early 1900s-1930s & the differing vampire stories they all inspired. How that then lead to the start of the zombie apocalypse subgenre in horror in the 1960s. Bats & rabies (1950s/60s) being recognized as a carry of the virus after decades of cattle herds in South America being decimated. The zoonotic origins of AIDS in the 1980s & how it diverged into xenophobia
Chpt. 7 - Jeanna Giese & Matthew Winkler case studies + the Milwaukee protocol & how some individuals could inherently have rabies antibodies in their system
Chpt. 8 - 2008 outbreak in Bali, a country that had been rabies free until that point and how they have went about dealing with it
^^Want to note with these summaries, that without including the citations at the end, all of these topics/subtopics are covered in 236 pages. Hardly any of them were covered with the depth needed to fully explore them. Most could be expanded upon if they removed a good chunk of fluff.
#bookblr#booklr#book reviews#book review#rabies#viruses#rabid: a cultural history of the most diabolical virus
2 notes
·
View notes
Text
Leishmaniasis
Case Reports, like we're on a episode of house
23M in Kenya, presenting with months of LOW, persistent fevers, and abdo fullness, found to have massive splenomegaly.
examination: massive splenomegaly (10 cm below costophrenic margin, and will definitely cross midline) and hepatomegaly
pancytopaenic on bloods, plt's down to 40s
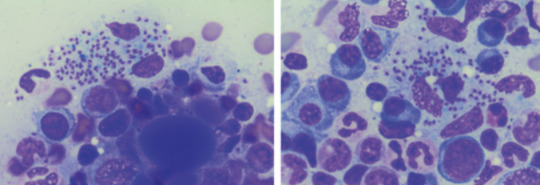
diagnosis confirmed on BMAT (parasite seen)
normal HIV, liver and kidney function
Bodies seen on the BMAT below are part of the lifecycle of the parasite that is intracellular, hence you can see the macrophages/neutrophils loaded with them, even bursting
What is it:
think of it when you get a patient with pancytopaenia and hepatosplenomegaly, who either traveled to or is in/from a tropical/subtropic region (where sand flies are)
cause - protozoa parasite Leishmania, transmitted by infected sandflies
Epidemio (when to consider it)
tropics, subtropics (South America, Asia, AFrica), Southern Europe
Microbiology/Transmission
parasite, replicates intracellularly (Leishmania donovani)
transmitted in sand flies (can be unnoticeable and usually bite in dawn or dusk - evenings or night), can also be transmitted via needles/blood
more common in rural areas
I've simplified this, but is more extensively covered in StatPearls and Wiki (there's different species of Leish and sandflies that transmit it)
once bitten, the protozoa are phagocystosed by skin macrophages, which then becomes full of the "bodies" (part of the lifecycle). Eventually these burst to release more of the bodies that infect more macrophages
they eventually are spread via blood to liver/spleen/BM and LNs
Random history:
ancient, records of disease date back to Egyptian mummies from 3000 BC --> positive DNA amplication for Leishmania and on papyrus from 1500 BC
multiple physicians from different times have described the disease, but it's named for 2 who described the parasite's intracellular ovoid body stage in smears from infected patients in India: Lt General William Boog Leishman and Captain Charles Donovan (Ronald Ross named the bodies after the 2 --> "Leishman Donovan bodies"
significant disease in Allied troops in Sicily in WWII, called "jericho buttons" (image on wiki from a WWI trooper serving in the middle east)

Leishman: Scottish pathologist and British Army medical officer, later it's director general in the 20s, did extensive research into the parasite named for him by Sir Ronald Ross. He mistook the parasite he observed for trypanosomes (cause of Chagas in South America and African sleeping sickness in Africa)
Donovan: Irish parasitologist, medical officer in India, observed an epidemic across India just after the rebellion of 1857, discovered the "bodies" in spleen tissue as the causative agent for what the locals called "kala azar" (severe visceral leishmaniasis - see below)
Donovan also discovered the "bodies" of Klebsiella granulomatis, hence these too are named after him (cause of ulcerative granulomas)
It became scandalous as both wanted credit for the "discovery" of this newly identified organism. So Sir Ronald Ross named it for both of them.
Sir Ron, by the way, won a Nobel in Medicine for discovering that malaria is transmitted via mossies (this was also a source of scandal, he was meant to share it with another physician who he accused of fraud - and they never received the award)
finally, it was actually a Russian physician who identified it first, but well, he published in a little known Russian journal which was promptly forgotten.
Clinical features
cutaneous type vs visceral organ type (spleen, liver, bones)
From wiki

can be asymptomatic
cutnaeous: can be there for years and resemble leprosy, causes an open chronic wound (most common), incubation 2-4 weeks on average (nodules at site of inoculation that eventually form ulcers), can heal spontaneously in 2-5 yrs
in diffuse cutaneous cases, can affect face, ears, extensor surfaces
can be muscosal = eg nasal symptoms/epistaxis, severe: perforated septum, this occurs in 1/3 after resolution of cutaenous symptoms (can be severe/lifte threatning, as it can affect vocal cords and cartilage, but oddly not bone)
visceral (incubation periods of up to years until immuncompromise): fever, weight loss, hepatosplenomegaly (spleen more than liver), pancytoaepnia, high total protein and low albumin with hypergammaglobulinaemia
this has seasonal peaks related to sandfly habits and humidity
interestingly it is an infective cause of massive splenomegaly, such that it crosses the midline
Extreme - but noticeable hepatosplenomgealy/abdo fullness, from medscape

can be atypical in HIV co infected patients, LAD in seom regions like Africa
Kala azar = black fever in some severe cases (fatal due to secondary mycobacterial infection or bleeding), refers to damage fto spleen, liver and anaemia
invstigations:
serology not great (minimal humoral response to the parasite), so often requires histopath (tissue sample) for which BMAT is safest in visceral organ involvement
visualisation of amastigotes (or Leishman-Donovan bodies), as intracellular --> can be seen in macrophages (small round bodies) post Giemsa staining
PCR of DNA also possible (as done in the Egyptian mummies)
Image source:

Treatment
liposomal amphotericin B (holy shit strong stuff) in visceral, PO: miltefosine (caution in pregnancy), all have significant ADRs, or paromycin. however, mortality of 10% if visceral left untreated
mixed results with azoles
in HIV co infection - start the HAARTs! can improve survival, mortality is 30% in HIV patients
cutaneous: stibolgluconate (have never heard of these drugs) and megluaine antimoniate, but limited disease often spotnaeously gets cleared by the innate system
prevention:
use DEET insect repellant at dawn and dusk
loose fitting clothing that covers all skin
no vaccine (were attempts at vaccinating dogs, which decreased rates)
sandflies are smaller than mossies, so requires small netting

Differentials for hepatosplenomegaly

Sources:
WHO guidelines
CDC guidlelines
Wiki - Haven't covered pathophysio, but wiki does extensively
StatPearls
DermNet - great resource for all things derm, that my derm colleagues pointed out to me
9 notes
·
View notes
Text
Caspase-1/Interleukin-1 (an Eminent Inhibitor): Can be a Future Radioprotector?

Caspase-1/Interleukin-1 (an Eminent Inhibitor): Can be a Future Radioprotector? in Biomedical Journal of Scientific & Technical Research
In the advancement of science, the employment of contemporary radiation therapy (xRT); the most effective way to counter malignancy, in the realm of cancer treatment has been exploited in the last few decades extensively. Although, half of all cancer patients worldwide, treated by radiotherapy may be responsible for the consequential damage to healthy normal cells and acute injuries to tissues which remains an enormous challenge to the radiotherapist and oncologist [1]. On the other hand, tremendous research which involves; novel drug development and innovative strategies are in the phase of progress and is constantly evolving across the globe to help reduce radiation-induced multiple sideeffects. As massive doses of radiation are implemented as a part of radiotherapy to cease the progress of cancerous cells, but at the same time, it is harming enormously to the healthier normal cells. The risk of damaging normal cells can be accomplished by practicing an accurate and improved localization of radiation dose and with the aid of several radioprotectors [2]. The most frequently applied techniques in anticancer treatment include Ionizing radiation (IR), in particular X-rays and gamma-rays owing to their huge potential to penetrate tissues; subsequently rupture chemical bonds resulted in free electrons from atoms which ionized, ultimately destroy the tumor cells. The water molecules existent in the human organisms spontaneously (within a few milliseconds) break down into active oxygen by radiation; eventually, engender free radicals, Reactive Oxygen Species (ROS), and Reactive Nitrogen Species (RNS) [3], which subsequently impair cells and in extreme cases leads to death. The generated free radicals’ interplay with DNA, RNA, proteins and resulted in cell dysfunction and further fatality. Also, these active free radicals induce oxidative stress among healthy organisms in physiological and pathological processes, which is one of the causative factors for tumors, hence, therefore, further exploration and the investigation of a powerful free radical scavenger is urgently needed.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#Journals on Medical Microbiology#Journals on Biomedical Intervention#Journals on Medical Drug and Therapeutics#Biomedical Journal Impact Factor#Journal of Biomedical Research and Review
0 notes
Text
Emerging infectious agents: an unusual case of Metapneumovirus pneumonia in an adult patient by Graziana Francesca Greco in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Human Metapneumovirus (hMPV), a relatively new virus, is a common cause of acute respiratory infection, especially common in the pediatric population. Despite hMPV infection in adults is possible, this rarely results in serious clinical manifestation. Here, we describe a hypoxemic respiratory failure related to pneumonia in an adult patient in whom hMPV was detected in respiratory samples.
Keywords
Human Metapneumovirus; SARS-CoV-2; Covid-19.
CASE HISTORY
A 61-yr-old caucasian man presented to the Emergency Department (ASST Mantua Hospital, Mantua, Italy) with fever up to 39°C, poorly responsive to antipyretics, nocturnal dyspnea and productive cough with mucus-purulent sputum for three days. On physical examination he appeared in good general condition, collaborating and oriented. The following parameters were recorded: blood pressure 140/90mmHg, heart rate of 100 beats min-1; respiratory rate of 23 breaths min-1; and body temperature of 38.4°C. His arterial oxygen saturation on room air was 87%. Chest examination revealed abnormal breath sounds with rhonchi and fine crackles in the middle lobe and inferior lobes bilaterally, no wheezes were heard. Laboratory findings revealed lymphocytosis (81000 x 103/µl), low platelet count (113000 x 106/µl) and an increase in alanine transaminase value (59 U/L), total bilirubin value (1.13 mg/dL) and CPR value (112 mg/L). Room air arterial blood gas analysis showed a normocapnic hypoxemia: pH 7.43, carbon dioxide tension 40.5 mmHg, oxygen tension 60.4 mmHg, and HCO3 24 mmol L-1. The SARS-CoV-2 antigen detection test on nasopharyngeal swab was negative. A chest radiograph showed multiple, small, patchy opacities in the right upper and middle lobe and no pleural effusion was observed. Based on these findings he was admitted to the Respiratory Department.
His medical history included chronic lymphocytic leukemia in follow-up which did not require any specific treatment. He denied taking any medications or to be a smoker, he drinks a glass of wine once a day and has no known allergies. The patient was a farmer who cultivates wheat and maize but he had no animal exposure and no travel history in the last few years. There is no family history or childhood history of respiratory complaints. He was vaccinated with three dosesagainst the SARS-CoV-2 infection (Pfizer) but not against the influenza virus.
Based on the patient’s presentation and testing results, on suspicion of bacterial pneumonia he was empirically treated with IV Piperacillin/Tazobactam, the patient required oxygen support at 3L min-1 and an inhalation therapy with Beclomethasone/Formoterol was set up ex adiuvantibus. In the following days, several microbiological investigations were carried out to determine the etiology of pneumonia: blood culture, urinoculture, sputum culture, Legionella, Haemofilus and Pneumococcus serologic tests, Legionella pneumophila and Pneumococcal urinary antigen test, all of which were negative.
A nasopharyngeal swab FilmArray Respiratory Panel Assay (NP FARP) was then requested: it was positive for human Metapneumovirus and the result was confirmed by repeating the test. For non responder fever and further increase of CPR (230 mg/l) and PCT (0.27 ng/ml), Levofloxacin and later Meropenem were added in the perspective of a resistant bacterial etiology. On the 6th hospitalization day a chest computed tomography (CT) scan was obtained (Figures 1 and 2) which demonstrated large opacities with gradient borders, distributed in the peribronchial area at the right upper lobe, middle lobe and both the lower lobes; they tended to the confluence configuring parenchymal consolidations with aerial bronchogram at the level of the cost-phrenic angle. Imaging also showed bilateral hilar and mediastinal lymphadenopathy (max diameter 3.4 x 2 cm), splenomegaly and absence of pleural effusion. Blood chemistry tests for HIV, Aspergillus antigen and galactomannan were also investigated but turned out negative. To rule out other infectious agents the patient underwent bronchoscopy with bronchoalveolar lavage (BAL) into the middle lobe. BAL provides material for various microbiological and cytological tests: Gram stain, culture, Koch’s bacillus DNA, Galactomannan, Cytomegalovirus and P. Jirovecii and immunological analysis were negative. From respiratory virus panel on BAL only human Metapneumovirus was isolated, this unique microbiological data was according to the NP FARP’s result, thus supporting and confirming the new hypothesis of a viral pneumonia in an adult patient with probable secondary mild immunosuppression due to his hematological disease. About ten days after entering the ward, there was a gradual decrease of CPR and a progressive improvement in clinical conditions and respiratory function to allow the suspension of oxygen therapy. At the end of hospitalization, pulmonary function tests were performed and showed a restrictive syndrome (FEV1/FVC 76.2, TLC 68% and VC 79% of predicted) and mild reduction of diffusion capacity (DLCO 62% and KCO 99%), probably representing the residual functional impairment due to viral pneumonia. The patient finally suspended all therapies and at discharge was referred for a one-month follow-up visit.
DISCUSSION
Human Metapneumovirus (hMPV), a relatively new virus first discovered in 2001, has been detected in 4-16% of patients with acute respiratory infections [1] [2] [3]. In particular, a recent review of 48 previous articles, including 100,151 patients under the age of five hospitalized for CAP, identified this virus as a cause of pneumonia in 3.9% of patients [4]. A recent study of 1386 hospitalized adult patients identified hMPV pneumonia in only 1.64%, indicating that it was much less common than in the infant population [5]. Metapneumovirus causes disease primarily in infants, but rarely can infect immunosuppressed individuals and elderly as well. Seroprevalence studies have shown that 90-100% of 5-10 years old children have previous infection [6]. Reinfection can occur during adulthood because of defected immunity acquired during the first contact with hMPV and/or because of different viral genotypes. The incubation period varies widely but is typically 3-5 days. The disease severity depends on the patient's condition and it ranges from mild upper airway infection to life-threatening pneumonia or bronchiolitis [7]. Clinically, Metapneumovirus infection is often indistinguishable from RSV infection, particularly in the pediatric population, and common symptoms include hypoxemia, cough, fever, upper and lower airway infections and wheezing [8]. hMPV infant patients are often hospitalized for bronchiolitis and pneumonia [9]. In young adults, a flu-like syndrome with fever may occur in a small number of instances, but infection in geriatric subjects may cause severe clinical manifestations such as pneumonia and, in rare cases, death [10].
As described in this case, it was not surprising that antibiotics and corticosteroids were administered in most patients infected with Metapneumovirus mainly for two reasons: in most cases the specific diagnostic tests for hMPV are not carried out at admission and/or physicians prefer to continue steroid and antibiotic treatment to control potential unidentified bacterial infections in patients in which no etiological agent had been identified associated with hMPV infection. The overuse of these drugs could therefore be reduced through the adoption at admission of specific diagnostic tests for such etiological agent, especially if specific risk factors are present (age, immunodepression, etc.). In addition, the adoption of such tests could reduce the nosocomial spread of this virus, allowing an early isolation of the infected patient [11].
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Funding: The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Authors’ contributions : All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
#Human Metapneumovirus#sars cov 2#covid 19#jcrmhs#Journal of Clinical Case Reports Medical Images and Health Sciences quartile
5 notes
·
View notes
Text
New Study Reveals Hidden COVID Proteins in Blood of Long Haulers - Published Oct 21, 2024
A virus reservoir in the body may explain why some people experience long COVID symptoms.
A recent study indicates that long COVID sufferers with symptoms impacting multiple body systems might have persistent SARS-CoV-2 proteins in their blood, pointing to an ongoing viral infection that could be treated with antivirals.
Persistent Viral Proteins in Long COVID Patients A study conducted by Harvard-affiliated Brigham and Women’s Hospital revealed that individuals experiencing a broad array of long COVID symptoms are twice as likely to have traces of SARS-CoV-2 proteins in their blood compared to those without symptoms of long COVID.
The symptoms frequently associated with long COVID include fatigue, brain fog, muscle and joint pain, back pain, headaches, sleep issues, loss of smell or taste, and gastrointestinal problems.
These findings were published in the journal Clinical Microbiology and Infection.
Implications for Long COVID Treatment Strategies Specifically, the team found that 43 percent of those with long COVID symptoms affecting three major systems in the body, including cardiopulmonary, musculoskeletal, and neurologic systems, tested positive for viral proteins within 1 to 14 months of their positive COVID test. But only 21 percent of those who didn’t report any long COVID symptoms tested positive for the SARS-CoV-2 biomarkers in this same period.
“If we can identify a subset of people who have persistent viral symptoms because of a reservoir of virus in the body, we may be able to treat them with antivirals to alleviate their symptoms,” said lead author Zoe Swank, a postdoctoral research fellow in the Department of Pathology at BWH.
Insights From the RECOVER Initiative The study analyzed 1,569 blood samples collected from 706 people, including 392 participants from the National Institutes of Health-supported Researching COVID to Enhance Recovery (RECOVER) Initiative, who had previously tested positive for a COVID infection. Using Simoa, an ultrasensitive test for detecting single molecules, researchers looked for whole and partial proteins from the SARS-CoV-2 virus. They also analyzed data from the participants’ long COVID symptoms, using electronic medical chart information or surveys that were gathered at the same time as the blood samples were taken.
It’s possible that a persistent infection explains some — but not all — of the long COVID sufferers’ symptoms. If this is the case, testing and treatment could aid in identifying patients who may benefit from treatments such as antiviral medications.
The Complex Nature of Long COVID One of the questions raised by the study is why more than half of patients with wide-ranging long COVID symptoms tested negative for persistent viral proteins.
“This finding suggests there is likely more than one cause of long COVID,” said David Walt, a professor of pathology at BWH and principal investigator on the study. “For example, another possible cause of long-COVID symptoms could be that the virus harms the immune system, causing immune dysfunction to continue after the virus is cleared.”
To better understand whether an ongoing infection is behind some people’s long COVID symptoms, Swank, Walt, and other researchers are currently conducting follow-up studies. They’re analyzing blood samples and symptom data in larger groups of patients, including people of wide age ranges and those with compromised immune symptoms. This way, they can also see if some people are more likely to have persistent virus in the body.
“There is still a lot that we don’t know about how this virus affects people,” said David C. Goff, a senior scientific program director for the RECOVER Observational Consortium Steering Committee and director of the Division of Cardiovascular Sciences at the National Heart, Lung, and Blood Institute (NHLBI), part of NIH. “These types of studies are critical to help investigators better understand the mechanisms underlying long COVID — which will help bring us closer to identifying the right targets for treatment.”
Goff added that these results also support ongoing efforts to study antiviral treatments.
The SARS-CoV-2 blood test developed by Brigham and Women’s researchers is also currently being used in a national study, called RECOVER-VITAL, that is testing whether an antiviral drug helps patients recover from long COVID. The RECOVER-VITAL trial will test the patients’ blood before and after treatment with an antiviral to see if treatment eliminates persistent viral proteins in the blood.
The idea that a virus can stay in the body and cause ongoing symptoms months after an infection isn’t unique to COVID.
“Other viruses are associated with similar post-acute syndromes,” said Swank. She noted animal studies have found Ebola and Zika proteins in tissues post-infection, and these viruses have also been associated with post-infection illness.
Reference: “Measurement of circulating viral antigens post-SARS-CoV-2 infection in a multicohort study” by Zoe Swank, Ella Borberg, Yulu Chen, Yasmeen Senussi, Sujata Chalise, Zachary Manickas-Hill, Xu G. Yu, Jonathan Z. Li, Galit Alter, Timothy J. Henrich, J. Daniel Kelly, Rebecca Hoh, Sarah A. Goldberg, Steven G. Deeks, Jeffrey N. Martin, Michael J. Peluso, Aarthi Talla, Xiaojun Li, Peter Skene, Thomas F. Bumol and Mike Zissis, 9 October 2024, Clinical Microbiology and Infection. DOI: 10.1016/j.cmi.2024.09.001
www.clinicalmicrobiologyandinfection.com/article/S1198-743X(24)00432-4/abstract (PAYWALLED)
#mask up#covid#pandemic#wear a mask#public health#wear a respirator#covid 19#still coviding#coronavirus#sars cov 2#long covid#covid is not over#covid conscious
36 notes
·
View notes
Text

Authored by Martin Hoyt via RealClearHealth,
It did not have to be this way. The COVID-19 pandemic cost American citizens their lives, their livelihoods, education, mental health, reputations and, ultimately, civil and religious freedoms. “The U.S. accounts for less than 5% of the world’s population, but more than 25% of total COVID-19 cases reported across the globe, and it currently ranks among the top 10 countries in COVID-19-related deaths per capita,” wrote the authors of 2023 commentary in the Journal of the American Medical Association. And for all that, we have government to thank.

For years leading up to the pandemic, the nation had spent billions on preparation and planning for a biohazard attack or event. Whatever we learned was quickly discarded or undone by a lack of accountability, transparency, and humility. Decades of planning and untold man hours of research and training were rendered ineffective by a corrupt culture of greed, self-importance, scientific misconduct, and outright fraud. Because, while the government worked to prevent the worst, it was also helping to create chaos and contagion by funding and facilitating gain of function (GOF) research.
GOF research refers to laboratory efforts to make viruses deadlier or to increase their transmissibility. The potential for disaster is obvious. Almost five years prior to the pandemic Dr. Marc Lipsitch and Dr. Alison Galvani noted that GOF pathogenic research posed “a risk of accidental and deliberate release that, if it led to extensive spread of the new agent, could cost many lives … Furthermore, the likelihood of risk is multiplied as the number of laboratories conducting such research increases around the globe.”
But according to Dr. Anthony Fauci’s emails and other NIAID communications obtained via FOIA – those that weren’t deleted by the now-infamous “FOIA lady” – the Wuhan lab was working on Covid research with the U.S. as early as 2015. And the worst happened. Dr. Richard H. Ebright of Rutgers University told a Senate committee hearing on June 18, 2024, that “… lapses in U.S. oversight of gain-of-function research and enhanced potential pandemic pathogen research likely contributed to the origin of COVID-19 …”
While Ebright said GOF has no medical utility, he emphasized that there are “major incentives to researchers worldwide, in China, and in the U.S. The researchers undertake this research because it is easy, they get the money, and they can get the papers [in science journals].”
Not surprisingly, China was selected because it was quicker and cheaper to conduct research without U.S. government entanglements or oversight. Dr. Steven Quay also testified on June 18 and said the Wuhan Institute of Virology is a “level-2 lab,” as opposed to highly secure level-4 labs elsewhere. Moreover, Dr. Fauci et al were able to fund this research because the law was silent. Ebright again:
… in this category of research, which is the most significant in terms of consequences and potentially existential risk there is almost no regulation with force of law. No regulation with force of law for biosafety or any pathogen other than the smallpox virus and no regulation with force of law for bio risk management for any pathogen.
But the U.S. and the world, may have temporarily escaped imminent catastrophe. Consider, according to Dr. Quay, what Wuhan obtained from Canada’s National Microbiology Lab in 2019: “two vials each of 15 strains of virus: seven varieties of Ebola virus, the Hendra virus, and two strains of Nipah virus, Malaysia and Bangladesh.” These virus samples, according to Dr. Steven Quay, are “the top three most deadly human pathogens on the planet.” The samples were obtained under murky circumstances (“described as a possible policy breach”) from a level-4 lab and surreptitiously flown on a commercial flight to Beijing where they were subsequently placed in a level-2 lab overseen by a country with a long history of a disregard for proper safety protocols.
Gain of function research probably created COVID-19, but our legislative and executive branches created the conditions for the disaster. Congress failed to pass laws governing specific GOF research, both Congress and the executive branch failed to effectively manage the federal health and science bureaucracy, and various agencies failed to monitor the behavior and performance of grantees and vendors engaged in GOF research. When catastrophe struck, self-interest and political survival of those responsible overrode the best interests of our citizenry.
Who in the government benefited? How and to what extent did they benefit? Did any GOF research contribute to the U.S. global or response? Is GOF research being rerouted to our defense and security agencies to avoid scrutiny? NIAID continues to stall, obfuscate, and otherwise restrict transparency to its current and past activities. We know there was a concerted effort by senior leaders like Anthony Fauci to hide or delete emails but many other records still likely exist that remain uncovered.
This must change. Any research activity or sponsorship of scientific endeavors that are capable of mass extinction, such as GOF, must be subjected to a higher level of accountability and scrutiny by our elected leaders and the American public. Accountability, transparency, and public debate after an international crisis like Covid-19 can’t undo the global catastrophic harm that was done. It can, however, reduce the ability of our public health bureaucracy to contribute to the next disaster or looming crisis.
Borrowed from:

(https://stuff-that-irks-me.tumblr.com/)
3 notes
·
View notes
Text


How can medicinal mushrooms support your mood and emotions?👀
[Hit SAVE so you can get these little miracle workers later!]
🍄Lion’s Mane: In a study of 30 women who were randomly assigned a snack of cookies containing Lion’s Mane or placebo cookies for 4 weeks, the Lion’s Mane group reported a significant reduction in feelings of helplessness, irritability and anxiety (Biomedical Research, 2010).
🍄Maitake: Researchers in 2017 found that Maitake had promising effects on mood and suggested it could be “a safe medical food supplement for the patient with depression” (Pharmaceutical Biology, 2017). This mushroom also acts as an adaptogenic food and can lower the stress hormone cortisol (Northern American Journal of Medical Sciences, 2011).
🍄Poria: Researchers in 2020 discovered that by calming the overreaction of the immune system and regulating our important neurotransmitters, including feel-good hormones serotonin and dopamine, Poria had a positive effect on mood. They also suggested that it could be “a traditional herbal
potential medicine for the treatment of depression.” (Journal of
Enthnopharmacology)
🍄Reishi: This powerful mushroom has been shown to reverse the decline in serotonin in the brain, meaning more of this happy hormone is circulating the brain to keep a positive mindset (Applied Microbiology and Biotechnology, 2021). Additionally, Reishi can help avoid low blood sugar, a common trigger for bad moods.
24 notes
·
View notes