#beta hemolysis
Explore tagged Tumblr posts
Text
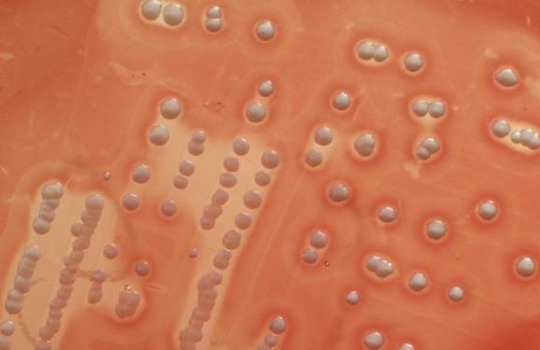
Vancomycin-resistant Staphylococcus aureus
“Staphylococcus aureus colonies on blood agar. Note the golden yellow pigment and beta hemolysis around it.” - via Wikimedia Commons
#staphylococcus aureus#vrsa#mrsa#wikipedia#wikipedia pictures#wikimedia commons#beta hemolysis#staph#staphylococcus#microbes#microbiology#vancomycin#antibiotics#antibiotic resistance#antimicrobial resistance#antimicrobial#blood agar#blood agar plate#microbio#medical microbiology#eskape pathogens#infectious diseases#medicine#bacteria#bacterial infections
13 notes
·
View notes
Text
Fermentation, Vol. 10, Pages 264: In Vitro Probiotic Characterization of Lactiplantibacillus plantarum Strains Isolated from Traditional Fermented Dockounou Paste
This study aimed to evaluate the probiotic properties of 10 lactic acid bacteria (LAB) isolated from artisanal fermented plantain dockounou paste. A preliminary characterization of the LAB isolates was performed based on phenotypic and several biochemical properties, which was subsequently confirmed through 16S #rRNA gene sequencing analysis, indicating that these isolates belonged to the species Lactiplantibacillus plantarum. With regard to safety criteria, the strains exhibited no alpha or beta hemolysis activity. Nevertheless, the majority of LAB strains demonstrated high sensitivity to the antibiotics tested. The results demonstrated that the majority of the strains exhibited remarkably high survival rates under simulated gastrointestinal conditions, such as pH = 1.5 (81.18–98.15%), 0.3% bile salts (68.62–100.89%), 0.4% phenol (40.59–128.24%), as well as 0.1% pepsin and pH = 2.5 (88.54–99.78%). The LAB strains demonstrated elevated levels of cell surface properties, indicative of the presence of a considerable defensive mechanism against pathogens. Intact LAB cells exhibited significant antioxidant abilities (48.18–83.58%). They also demonstrated a pronounced inhibitory effect on the growth of foodborne pathogens. Enzyme pattern analysis revealed that the LAB isolates produced both proteases and cellulases, as well as pectinase and/or amylase activity. The potential of the L. plantarum strains FS43, FS44, and FS48, as indicated by the results obtained from the standard in vitro assays, makes them suitable for further study as potential probiotics. https://www.mdpi.com/2311-5637/10/5/264?utm_source=dlvr.it&utm_medium=tumblr
0 notes
Text
Checkout the Best Quality of Sheep Blood Agar (TMP 017) at TM Media
If you are looking for Sheep Blood Agar manufactured by TM Media is a specialized culture medium extensively used in microbiology for the isolation and identification of bacteria, particularly those associated with human infections. Renowned for its versatility, this agar is enriched with a concentration of sheep blood, providing an essential source of nutrients for bacterial growth. The medium's unique composition allows for the differentiation of bacteria based on their hemolytic activity. Three main types of hemolysis—alpha, beta, and gamma—can be distinguished on Sheep Blood Agar. Alpha hemolysis results in a greenish discoloration around bacterial colonies, beta hemolysis produces clear zones due to complete blood cell lysis, and gamma hemolysis indicates no hemolysis.
Visit the Website - https://www.tmmedia.in/

0 notes
Text
Sheep Blood Agar Plate

A sheep blood agar plate is a type of microbiological growth medium that contains defibrinated sheep blood. The blood provides nutrients and growth factors for bacteria, and it also allows for the differentiation of bacteria based on their hemolytic properties.Sheep blood agar plates are used to grow a variety of bacteria, including fastidious organisms that require additional nutrients. They are also used to identify bacteria based on their hemolytic reactions, such as alpha hemolysis (partial destruction of red blood cells), beta hemolysis (complete destruction of red blood cells), and gamma hemolysis (no hemolysis).
#sheep_blood_agar_plate#blood_agar_plate#ready_to_use_culture_media#ready_to_use_plate#microbiology#culture media
0 notes
Text
Influence of Iron Deficiency Anemia on HbA1c: A Review

Authored by Ghulam N Bader
Go toGo to
Abstract
Hemoglobin A1c (HbA1c) is widely used as a diagnostic tool for diabetes. Many clinical conditions affect erythrocyte turnover which influence HbA1c levels. These levels are lowered by different forms of anemia, but reverse is the case in iron deficiency anemia (IDA). This is suggested by various studies which propose an increase in HbA1c levels in patients with IDA. However, there are studies which negate any influence of IDA over HbA1c levels. In both cases the clinical data is not sufficient to confirm or nullify the role of IDA in increasing HbA1c levels.
Introduction
Hemoglobin A1c (HbA1c), a glycated hemoglobin is formed by an irreversible, slow non-enzymatic catalysis of the β chain of globin in mature hemoglobin (Hb) [1,2]. It is used as a gold standard for monitoring glycemic status for the previous three months (the life span of a red blood cell) in patients with diabetes [3]. HbA1c provides an integrated measure of glycemia which is less susceptible to short-term modulation than blood glucose levels. Also, it helps to keep a track of diabetic therapy within individuals suffering from diabetes. WHO and ADA have approved the use of HbA1c determination for diagnosis of type 2 diabetes [4,5]. The normal range of HbA1c in a healthy person is 4 to 6% [6].
Clinically there are three major factors on which HbA1c levels depend.
A. HbA1c in reticulocytes when released from the bone marrow;
B. Hb glycation rate as red blood cells (RBCs) become older, a function of glucose concentration to which Hb is exposed; and
C. The mean age of RBCs in the circulation [7].
HbA1c levels can be affected by number of factors such as structural hemoglobinopathies, thalassemia syndrome, and alteration in quaternary structure of Hb [8]. Also, HbA1c levels can be changed by different types of anemia [9]. Anemia is the most prevalent form of nutritional deficiency both in developed and developing countries. Globally, 50% of anemic burden is contributed alone by Iron deficiency [10,11]. The clinical profile of many systemic diseases is regulated by the iron [12], which is involved in most important metabolic processes viz. transportation of oxygen, regulation of cell growth and differentiation, deoxyribonucleic acid (DNA) synthesis, and electron transport [13,14].
Iron deficiency anemia (IDA) can increase the red blood cell turnover which can increase glycation of Hb leading to higher HbA1c values as observed in blood loss, hemolysis, hemoglobinopathies, red cell disorders and myelodysplastic disease [15]. There are studies to support the idea that diabetes is influenced by changes in the iron level in a body [16]. Lower levels of serum iron or serum ferritin have been linked with increased glycation of HbA1c [17,18]. It has been reported that there is a bidirectional relationship between iron metabolism and glucose homeostasis, higher iron levels modulate both the action and secretion of insulin [12]. Thus, lower the iron levels, higher is the glycation of HbA1C, leading to its false-high values in diabetic as well as non-diabetic individuals [19].
Brooks et al. [20] reported that a relative absence of iron results in the alteration of quaternary structure of the Hb molecule leading to excessive glycation of the beta globin chain. In another study by Sluiter et al. [21] it was reported that glycation of Hb is an irreversible process thus, with the aging of a cell there is a linear increase of HbA1c in the erythrocyte. El Agouza et al. [22] reported that at a constant glucose level, lower levels of Hb can lead to an increase in the glycated fraction because HbA1c is measured as a percentage of total HbA. These studies report relationship between IDA and HbA1c on the basis of structural modification of Hb and HbA1c levels in old and new red blood cells [20]. Coban et al. [19] in his studies showed that patients with IDA had higher HbA1c levels and on treatment with iron these levels significantly decreased. A case study by Mudenha et al. [23] reported that HbA1c levels significantly decreased with correction of IDA. Furthermore, Silva et al. [24] and Rajagopal et al. [7] reported difference in HbA1c levels among diabetic as well as non diabetic patients with mild, moderate, and severe IDA.
On the other hand, Heyningen et al. [25] and Hansen et al. [25] reported that there was no difference between HbA1c levels in patients with IDA and control. These findings gather support from study by Rai et al. [26], who reported no difference in HbA1c levels with respect to IDA using different methods to assay HbA1c. Thus these conflicting reports are enough to create a stir in the minds of clinicians regarding a successful therapy in diabetic patients with IDA. Hence the effect of IDA on HbA1c needs to be evaluated at mechanistic level, so as to be assured about the outcome of the therapy. Iron replacement therapy in diabetic patients with IDA needs to be considered.
Conclusion
IDA is the commonest nutritional deficiency worldwide but the prevalence is higher in developing countries, and most vulnerable groups to IDA are women, children and adolescents [27]. Also, in low and middle income countries diabetes too is increasing and the mostly affected age group is 45-64 years [28]. So, determination of HbA1c levels has increased for both screening and diagnosis of diabetes. Clinicians need to evaluate the nonglycemic factors that could affect the HbA1c levels of a patient [29,30]. Different types of anemia can have a negative effect on HbA1c levels, some investigators have shown that IDA increases the HbA1c levels independent of fasting glucose level [16] whereas others have negated these findings. In either case the clinical data is not sufficient and further studies are required to identify the role of erythrocyte indices in modulation of HbA1c levels. Studies with large population need to be conducted to evaluate the difference between severity and effects of IDA on HbA1c values.
To Know More About Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes
Text
I'm a grade A dumbass because I just got to look at a midterm and I got the first question wrong because I misread it multiple times 😂😂😂 I still did well on it so I'm not concerned or anything but it's just hilarious that I fucked that one up because I missed one word
#most strains of staph aureus are beta-hemolytic#personal#the question talked about the type of hemolysis with s. aureus on BA plates#and i thought it just said staphylococcus#most of which are gamma-hemolytic#and the question was a true or false#and it said#and i said false bc i thought it was talking abt all staph species#sorry if you read this and don't understand it
1 note
·
View note
Photo

Q. Which of the following petri dishes is growing Group A beta-hemolytic Streptococcus pyogenes? ... A. Yes! You can tell A is Strep pyogenes because when it grows in colonies on blood agar, it releases streptolysins (SLO and SLS) that break down the erythrocytes in the medium, creating a "halo" of complete beta-hemolysis. Strep pneumoniae (B) causes incomplete or alpha-hemolysis (green on blood agar), while Enterococcus faecalis (C), Group D Strep, does not cause lysis (gamma hemolysis).
6 notes
·
View notes
Text
Notes from Dr. Freese’s lecture from today:
A co-oximeter measures the amount of carbon monoxide in the blood.
Methemoglobinemia causes chocolate brown color of the blood. Methemoglobinemia is due to oxidation of the iron in heme from normal ferrous (Fe2+) to oxidized ferric (Fe3+) form. The treatment is methylene blue. Methylene blue turns the urine blue. When it’s injected, the pt’s pulse ox goes down, but then it circulates out. Methylene blue reduces Fe3+ back to Fe2+. It’s a monoamine oxidase inhibitor and can cause serotonin syndrome, especially if the pt is already on a monoamine oxidase inhibitor.
Nitrates (nitroglycerin) and nitrites can cause methemoglobinemia. Amyl nitrate ampules can be crushed and inhaled to cause methemoglobinemia in pts with cyanide poisoning. Methemoglobinemia isn’t as bad as cyanide poisoning. Amyl nitrate vasodilates. I know I took notes on this from the toxic ingestion video in the clinical OnlineMedEd video, but I forgot stuff. Lots of nitroglycerin over a long period of time is necessary to cause methemoglobinemia, so it’s not often seen. Local anesthetics, specifically benzocaine and prilocaine, can cause methemoglobinemia. Benzocaine is in aerosol form and is used to anesthetize mucous membranes, e.g. in pts who will be getting upper endoscopy. The dosing is a 2-second spray and it’s very concentrated, so it can be easy to give too much benzocaine.
Pts with methemoglobinemia appear blue/gray. You can measure the amount of methemoglobin in the blood with an ABG. I think he said a level greater than 10 is methemoglobinemia. There’s also congenital methemoglobinemia. I know we learned this in like first year. I don’t remember.😩
From UpToDate:
Methemoglobin is an altered state of hemoglobin in which the ferrous (Fe2+) iron in heme is oxidized to the ferric (Fe3+) state. The ferric hemes are unable to bind oxygen, and they alter the oxygen affinity of other hemes in the hemoglobin molecule, which further impairs oxygen delivery to the tissues. Methemoglobin levels are normally kept low in red blood cells (RBCs) by cytochrome b5 reductase (Cyb5R). Cyanosis is clinically detected when total methemoglobin exceeds 1.5 g/dL, equivalent to 8 to 12 percent methemoglobin at normal hemoglobin concentrations.
Biallelic pathogenic variants in the CYB5R3 gene, which encodes Cyb5R, causes congenital methemoglobinemia, an autosomal recessive disorder. Affected individuals can have cyanosis, but clinically significant tissue hypoxia is rare because compensatory erythrocytosis improves oxygen delivery. Other hereditary causes include hemoglobin M disease (due to variants in alpha, beta, or gamma globin genes) and cytochrome b5 deficiency (extremely rare). Acquired methemoglobinemia can occur after exposure to dapsone and some antimalarial drugs, topical benzocaine spray, ingested nitrites and nitrates, and aniline dyes.
Heterozygotes for Cyb5R deficiency are likely to have increased susceptibility to acute/toxic methemoglobinemia.
Methemoglobinemia is suspected in a child or adult with unexplained cyanosis or hypoxia that does not resolve with supplemental oxygen. Once the diagnosis is suspected, the evaluation focuses on determining the methemoglobin level and need for treatment, eliminating exposures, and evaluating genetic causes.
Methemoglobin can be detected on the vast majority of arterial blood gas machines used in the United States. Discussion with laboratory personnel may be warranted. If a blood gas instrument capable of detecting methemoglobin is not available, other options include pulse oximetry using a multiple wavelength co-oximeter or direct measurement by the Evelyn-Malloy assay; the latter is typically a send-out test. Methemoglobinemia cannot be diagnosed using routine pulse oximetry or the arterial oxygen tension (PaO2) or saturation (SaO2) on a blood gas.
Additional testing in suspected congenital methemoglobinemia includes Cyb5R enzyme assays, hemoglobin analysis, and genetic testing.
Most individuals with congenital methemoglobinemia have reduced Cyb5R in RBCs only (type I disease). Rarely, reduced enzyme activity in other cells (type II disease) causes severe neurologic and developmental abnormalities that are typically fatal. Individuals with Cyb5R deficiency can be treated with daily oral methylene blue (MB; 100 to 300 mg orally per day) or ascorbic acid (vitamin C; 1000 mg orally three times a day) for cosmetic purposes; the choice between them is individualized. These measures are ineffective for hemoglobin M disease. Phlebotomy should not be used to "normalize" the hemoglobin.
Acquired/toxic methemoglobinemia is a medical emergency that requires prompt clinical suspicion and rapid evaluation and treatment. Clues to the diagnosis include:
•Exposure to a precipitating medication or other chemical.
•Cyanosis out of proportion to pulse oximetry readings.
•Nonspecific respiratory or neurologic symptoms; shock if severe.
•Dark red or brownish to blue blood that does not become red on oxygen exposure
Pulse oximetry readings of approximately 85 percent SaO2 that do not improve with supplemental oxygen.
Typically, the severity of symptoms correlates with the methemoglobin level.

Cytochrome b5-reductase deficiency and hemoglobin M disease are rare inherited causes of methemoglobinemia.
*While methylene blue is a recognized treatment for methemoglobinemia, it also has oxidant potential and may worsen the clinical status of individuals with G6PD deficiency because it induces acute hemolysis that can further decrease oxygen delivery to the tissues. In high doses, methylene blue can paradoxically increase methemoglobinemia.
...symptoms generally occur with methemoglobin levels greater than 10 percent, and levels greater than 30 to 40 percent can be life-threatening. The diagnosis is confirmed by documenting methemoglobin level greater than 5 percent.
Management of acquired methemoglobinemia includes discontinuation of the offending exposure, supplemental oxygen (and possibly other supportive care), and, for those with severe symptoms and/or methemoglobin levels greater than 30 percent, treatment with MB [methylene blue] or ascorbic acid [vitamin C].
For those who require treatment, MB appears to be most rapidly effective and there is greater experience with its use and efficacy. However, MB can precipitate severe hemolysis in individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency, and it can cause serotonin syndrome in individuals taking a serotonergic medication or drug, such as a selective serotonin reuptake inhibitor (SSRI).
4 notes
·
View notes
Photo

Hemolytic Anemias: A brief review
Anyone who has spent a split second (or less) in a medical lab has seen the horrors of hemolysis… And the rage of the informed phlebotomist when she could not have possibly hemolyzed that sample.
Let’s be honest; you probably just left it on the counter too long. [*Laughs maniacally*]
Apart from daily struggles with those slasher strawberry milkshakes, hemolysis plays a far more medically significant role in human health.
Hemolytic anemia is described by Johns Hopkins as “a disorder in which red blood cells are destroyed faster than they can be made.” The term covers a broad spectrum of conditions, including such factors as autoimmunity, genetic predisposition, and a lack of erythrocytic structural integrity.
Clinically speaking, we can expect to see a rise in immature red blood cells, or reticulocytes, when we look at a smear under the scope. These will appear as abnormally large erythrocytes and are present in excess, released rapidly from the marrow to make up for excessive RBC hemolysis (for reference, please see the extremely detailed, highly accurate image attached.)
Patients with these conditions will also present with heightened bilirubin as a result of hemolysis, often appearing jaundiced.
It should also be noted that while increased potassium is a significant factor to consider in a hemolyzed blood sample (this is one of the reasons we should be wary of K+ readings on dermal punctures), hyperkalemia is easily avoided in most with chronic hemolytic conditions, due to the kidney’s sheer badassery when eliminating all that pesky electrolytic excess.
The anemias, in short:
· Sickle Cell: The Sickly “C.” This notorious condition consists of a bunch of “C-(shaped)-for-Confused” cells, with a decreased oxygen carrying capacity, originating from a hemoglobin defect in the 11th chromosome. Target cells and Howell-Jolly Bodies may be seen in these smears.
· Thalassemias: Resulting from the absence of one or more genes for alpha or beta globin, people with these conditions experience a recessively-inherited dysfunction in hemoglobin production, its pathogenesis stemming from distinct iron overload. Except in the case of Hydrops Fetalis (in which death usually occurs at birth), most patients may live a happy, full life.
· Spherocytosis & Elliptocytosis: Both of these conditions (named aptly and obviously after their respective shapes) stem from a hereditary defect in the erythrocytic cell membrane, allowing for an abnormal morphology and a shortened cell lifespan.
· G6PD Deficiency: Most common in biological males and triggered by everything from infection to fava beans, this recessive condition leads to early erythrocytic death. This originates from an inherited deficiency in Glucose-6-phosphate dehydrogenase, an enzyme responsible for the chemical protection of RBC cellular membranes.
· Immune Hemolytic Anemia: Immunologically-derived, this condition may develop prior to a stint with certain viruses such as HIV and infectious mononucleosis, a fight with lymphocytic leukemias, and such invasive procedures as blood and marrow transplants. During pathogenesis, the body develops an immunological response to its own erythrocytic proteins, effectively challenging itself to a bitter, pointless duel.
· In addition… Hemolytic anemias may also occur in the face of excessive drug use, certain mechanical abnormalities in the body (such as swollen/occluded blood vessels) and procedures (such as kidney dialysis). The possibilities are endless! (She says, in an inappropriately ecstatic tone).
Did I miss anything? I guarantee I did.
In the interest of a great, communal education, please respond with any relevant details or clinical cases that pop up in that lovely giant brain of yours! I’ll be regularly posting on and monitoring this shittastic, paint-plastered blog throughout the month of November, so all input is greatly appreciated.
#MLT#mls#medical laboratory science#lab#lablife#hematology#review#study#nanowrimo#butdonthavetimeforanovel
3 notes
·
View notes
Text
El ControlManagement Del Estrés Y La DiabetesPor favor necesito detalles.Gracias Paula Navas, del Departamento de Cardiología del Hospital Universitario Gregorio Marañón, de Madrid, ha presentado en elCongreso Anual de la Sociedad Europea de Cardiología (ESC, en sus siglas inglesas), que se está celebrando estos días en Roma, el hallazgo de tres genes que están implicados en esta enfermedad: BMPR2, KCNK3 y TBX4. Conocerlos ayudará a mejorar el tratamiento.<br/><br/>Higiene de los pies: Lavarse todos los días los pies con agua templada y secarlos bien, observando si hay cortes, cambios de colorcolourshadecoloration... Las uñas de los pies se deben cortar en línea recta y limar después los bordes, sin erosionar los dedos.<br/><br/>Estos Sitios WebNetInternet de Terceros se proporcionan únicamente para informarle sobre la existencia de otras fuentes de información sobre un tema concreto y la inclusión de un enlace en el presente Sitio WebNetInternet no implica la aprobación de los Sitios WebNetInternet de Terceros por parte de Esteve.<br/><br/>Greenbaum comentó que ella y su equipo ya están haciendo pruebas con una pastilla de insulina con una dosis más alta en un nuevo ensayo para ver si eso ayuda a retrasar la enfermedad más aún. También esperan evaluar una combinación de pastillas de insulina con medicamentos que actúan en el sistema inmunitario.<br/><br/>Los objetivos de controlmanagement durante el embarazo son muy rigurosos y es obligado hacer el autocontrol de los niveles de glucosa midiendo la glucemia en sangre capilar. Aunque diferentes sociedades científicas fijan diferentes objetivos, podemos decir que en ayunas habría que estar por debajo de 95ninety 5 mg/dl, una hora después del inicio de las comidas no deberían superarse los 130one hundred thirtya hundred thirty-140one hundred fortya hundred and forty mg/dl y a las dos horas los 120one hundred twentya hundred and twenty mg/dl.<br/><br/>El mecanismo de la diabetes es relativamente sencillo de describir. Al igual que los coches utilizan gasfuelgasoline como combustibleflamable, las células del cuerpo necesitan un tipo de azúcar llamada glucosa. El cuerpo obtiene la glucosa al descomponer los carbohidratos en la dieta. Las células entonces extraer la glucosa de la sangre con la ayuda de la insulina, una hormona producida por el páncreas en células especializadas llamadas células beta.<br/><br/>Aunque se puede llevar una vida normalregular, aquel que sufre de diabetes tipo 1 deberá someterse a un tratamiento diario de insulina, practicar deporte de manera habitualrecurringordinaryroutine y mantener unos hábitos alimenticios estrictamente saludables.<br/><br/>First, at diagnosisanalysisprognosis and duringand by means of routine followcomply withobserve-up care, assess psychosocial issuespoints and familyhousehold stresses that couldthat wouldthat would possibly impactinfluenceimpressionaffect adherence to diabetes mgmt. ProvidePresent referrals to trainededucatedskilled mentalpsychological healthwell being professionals, preferablyideally experiencedskilled in childhood diabetes, as appropriateapplicableacceptable. E<br/><br/>La diabetes es una enfermedad seria, la cual si no se controla, puede amenazar la vida. <a href="https://blogfreely.net/woolpurple35/informacion-sobre-diabetes">porque da diabetes tipo 1 en niños</a> con complicaciones a largo plazo que pueden afectar cada sistema y parte del cuerpo. La diabetes puede contribuir a los trastornos oculares y ceguera, a la enfermedad cardiaca, a los accidentes cerebro-vasculares, la insuficiencia de los riñones, la amputación y el daño a las fibras nerviosas. Puede afectar el embarazo y también causa defectos de nacimiento.<br/><br/>En onceas soon as días Doughty perdió cuatro kilos y acabó con la diabetesDurante 8eight días el periodista se alimentó sólo con tres litros de agua al día, 200 calorías a base de suplementos alimenticios (sopas y batidos) y 200 calorías provenientes de vegetales. El objetivo: perder la sexta parte del peso que tenía antes de que le diagnosticaran la diabetes. En poco más de una semana los niveles de glucosa de Doughty bajaron de más de 108 mg/dl a 77seventy seven,47forty seven. Dado que estaba empezando a sufrir estreñimiento y un gran cansancio, y la dieta estaba funcionando, Taylor le invitó a subir las calorías de la dieta.<br/><br/><a href="http://www.anobii.com/groups/012dc5215343ddb6bd/">conclusion of diabetes mellitus type 2</a> algunas de las bebidas que puede beber un diabético en un bar debes saber que todas ellas contienen azúcar. Por ello, toda la glucosa que obtengas por esa parte, tendrás que contrarrestarla con tu alimentación. En el caso de las bebidas alcohólicas, no olvides beberlas con moderación por sus efectos.<br/><br/>Handelsman afirmó que le gustaría ver un medicamento que combinemix tres fármacos: metformina, una tiazolidinediona y un inhibidor DPP-4four un inhibidor SGLT-2, pero no cree que eso pase pronto.<br/><br/>Los alimentos con bajo índice glucémico (de 55fifty 5 para arriba) se cree que tienen un efecto beneficioso sobre el controlmanagement de la glucosa en la sangre, ya que no afectan significativamente los niveles de azúcar. Los que tienen una puntuación del índice glucémico de 70 para arriba, se consideran alimentos de alto índice glucémico.<br/><br/>Para aumentar la glucosa de forma rápida, basta con tomar un caramelo algún producto que contenga azúcar (uvas, zumos, refrescos), de este modo, a los 10-15 minutos los síntomas habrán desaparecido.<br/><br/>La cirugía de la diabetes mellitus tipo 2 , también llamada cirugía metabólica, están despertando un enorme interés en todo el mundo. Cada vez recibimos más consultas de pacientes interesados en estos nuevos tratamientos, que desgraciadamente no son eficaces para todos los casos.<br/><br/>Atractiva planta tropical rica en cromo y magnesio, ambos minerales son muy beneficiosos para ayudar a disminuir los lípidos en sangre. sintomas diabetes perros diabetes tipo baja de peso #sintomas diabetes tipo 1 adolescentes #especialista en diabetes en veracruz <iframe width="560" height="315" src="https://www.youtube.com/embed/dxNvwGu6x7s" frameborder="0" allow="accelerometer; autoplay; encrypted-media; gyroscope; picture-in-picture" allowfullscreen></iframe>El aloe vera ayuda también a curar las heridas y es muy recomendado para diabéticos, ya que el proceso de cicatrización suele ser más lento. El Aloe vera se puede tomar por vía oral como suplemento alimenticio para obtener todos los beneficios que ofrece de este extracto naturalpure.<br/><br/>Hay diferentes formas de adquirir la educación que toda persona con diabetes necesita. Este proceso educativo debe ser continuo e integral. Lo idealbestperfectultimatesuperbexcellentvery bestsplendidideally suitedpreferrredsupreme es que utilice todos los medios posibles para mantenerse cada día más educado (a) e informado (a), como complemento de lo que el médico y el equipo multidisciplinario de salud (educador, nutricionista, podólogo, etcand so onand so forthand many others.) debe enseñar en materia de diabetes. (10)<br/><br/>ganho de peso progressivo e alterações nos níveis de glicose no sangue nos deixam alertas para a possibilidade de pré-diabetes. Se você tem casos de diabetes na família, também é importante procurar orientação médica.<br/><br/>Pueden ver abajo las características del paciente que estamos interviniendo que fijese como con un IMC de 35, que es una obesidad moderada, pues el paciente ya padece importantes alteraciones metabólicas, como diabetes con necesidad de insulina e hipertensión.<br/><br/><a href="http://all4webs.com/violinpurple64/futxoxomrv350.htm">como sanar la diabetes</a> relación a los hidratos de carbono, se priorizan los ricos en fibra, evitando alimentos con alto índice glucémico así como refrescos azucarados. La dieta mediterránea cumple con todas estas recomendaciones y por tanto es aconsejable para los pacientes diabéticos (ADA, 2017).<br/><br/>The A1C testchecktake a look at is subjecttopic to certainsure limitations: conditionscircumstancessituations that affecthave an effect on erythrocyte turnover (e.g., hemolysis, blood loss) and hemoglobin variants should behave to beshould be consideredthought-aboutthought of, particularlynotablysignificantly when the A1C resultend resultoutcomeconsequence does notdoesn't correlate with the patientaffected individual's clinicalmedicalscientific situationstate of affairsscenario;2 in additionas properly as, A1C does notdoesn't providepresent a measure of glycemic variability or hypoglycemia<br/><br/>Los antioxidantes y las enzimas digestivas que proporciona este zumo son muy útiles para estimular y el buen funcionamiento del páncreas. Por ello, su ingesta regularcommon disminuye los niveles altos de azúcar en la sangre<br/><br/>Probablemente tras leer este artículo te haya quedado algo más claro por qué sufres diabetes y te hayas hecho una ideaconceptthought más aproximada sobre si tus hijos la desarrollarán también. Aún así, si sigues teniendo dudas, no te cortes a la hora de preguntar a tu médico. Seguro que él te da más información al respecto.<br/><br/>Freemantle N, Chou E, Frois C, Zhuo D, Lehmacher W, Vlajnic A, et al. SafetySecurity and efficacy of insulin glargine 300 u/mL comparedin distinction with otherdifferent basal insulin therapies in patientssufferers with typesortkind 2 diabetes mellitus: A networkcommunity meta-analysisevaluation. BMJ Open. 2016;6:e009421, -2015-009421.<br/><img src="https://upload.wikimedia.org/wikipedia/commons/thumb/6/6c/Diabetes_Victoria_logo.jpg/1920px-Diabetes_Victoria_logo.jpg"/><br/><br/>A pesar de que los beneficios están claros, todavía existen muchas dudas acerca de cómo llevar a cabo esta alimentación específica para tratar la diabetes, pues no consiste solamente en consumir alimentos saludables, sino que se necesita tener algunos conocimientos más. Por ejemplo ¿Es suficiente si elimino los azúcares de la alimentación? ¿Es necesario reducir el consumo de todas las grasas? ¿Hay alimentos que se pueden consumir de forma libre sin que se afecten los valores de glucosa en sangre?<br/><br/>The algorithm for the use ofusingthe usage of combinationmixture injectable therapyremedy in patientssufferers with typesortkind 2 diabetes (Fig. 8eight.2) has been changedmodified to reflectmirrorreplicate studiesresearch demonstrating the noninferiority of basal insulin plus glucagon-like peptide 1 receptor agonist versus basal insulin plus rapidspeedyfast-actingappearingperforming insulin versus two dailyevery dayday by dayeach day injections of premixed insulin, as effectively asin addition to studiesresearch demonstrating the noninferiority of multiplea variety of dose premixed insulin regimens versus basal-bolus therapyremedy.<br/><br/>A pesar de los estragos que puede causar la diabetes tipo 1 tipo 2, se puede tener una buena calidad de vida si es que se sigue una disciplina, como la que muestran algunos de estos famosos.<br/><br/>Otra de las hierbas que te ayudan a tratar la diabetes de tipo 2 es el jengibre. Se le atribuyen beneficios para aliviar varios padecimientos sencillos, desde un resfriado a problemas digestivos. A lo largo de los años también se han hecho estudios para conocer más a fondo las propiedades de esta raíz y en varios de ellos se ha comprobado que favorece al tratamiento de diabetes de tipo 2.<br/><br/>Lo que usted puede hacer: Revísese el nivel de azúcar en la sangre con frecuencia y mantenga un registro de los resultados para ver si hay un patrón. Si usa insulina, podría necesitar aplicarse más en los días anteriores a su periodo. Hable con el médico acerca de cambiar la dosis, si fuese necesario. Hacer actividad física la mayoría de los días, comer alimentos saludables en las cantidades adecuadas y dormir lo suficiente también pueden ayudar.<br/><br/>9. Rivas Alpízar E, Zerquera Trujillo G, Hernández Gutiérrez C, Vicente Sánchez B. Manejo práctico del paciente con diabetes mellitus en la atención primaria de salud. Rev Finlay. 2011 citado 8eight Oct 2013;1(3three):48forty eight-64sixty four. Disponible en:<br/><br/>Reemplazo articular. Este procedimiento consiste en extraer la articulación dañada y sustituirla por una artificialsynthetic. Las articulaciones que se reemplazan con mayor frecuencia son las de caderas y las de rodillas.<br/>
1 note
·
View note
Text
Hyperkalemia ecg findings

The PR and QRS intervals may lengthen.3įurther elevations in potassium levels can lead to sinoatrial and atrioventricular conduction blocks with resulting escape beats and rhythms. As a result, P-wave amplitude decreases and P waves flatten and may disappear altogether. Atrial tissue is more sensitive to this effect than ventricular tissue. In particular, the inverted lateral T waves associated with left ventricular hypertrophy may pseudonormalize.2 These T-wave changes result from acceleration of the terminal repolarization of the myocytes and are often most pronounced in the precordial leads.Īs potassium levels rise further, cardiac conduction between myocytes is suppressed. However, in most patients, the ECG shows largeamplitude T waves rather than the classic tented T waves.1 In addition, the direction of the T wave may change. The earliest ECG signs of hyperkalemia are “tented” T waves, which are classically described as tall, symmetrically narrow, and peaked (see Figure 2). Pseudohyperkalemia results when potassium is released from platelets in the setting of thrombocytosis. Spuriously elevated potassium levels can occur with hemolysis during phlebotomy. Methamphetamine use can cause renal failure. The causes of hyperkalemia include acute and chronic renal failure, diabetic ketoacidosis, mineralocorticoid deficiency, type IV renal tubular acidosis, medications (angiotensin-converting enzyme inhibitors, potassium-sparing diuretics, lithium, NSAIDs, and beta-adrenergic antagonists), acute digoxin toxicity, rhabdomyolysis, burns, crush injuries, and severe dehydration-as well as any combination of the above. As a result, changes in serum potassium level can have dramatic effects on cardiac cell conduction and, consequently, on the ECG. Potassium, the predominant intracellular cation, plays an important role in maintenance of the potential across the cellular membrane, as well as in depolarization and repolarization of myocytes and neurons. Although this response to bicarbonate might also be associated with a toxicologic insult (such as can cause ventricular tachycardia), the finding of peaked T waves points strongly to an elevated serum potassium level. The patient’s ECG response to bicarbonate makes primary cardiac disease and ischemia less likely. The findings on these 2 ECGs suggest hyperkalemia, B. The second ECG (Figure 2), obtained after administration of bicarbonate, reveals slowing of the heart rate, narrowing of the QRS complex, and the presence of “tented,” or peaked, T waves, primarily in the precordial leads. The potential causes of ventricular tachycardia are numerous among them are primary cardiac disease ischemia and other primary noncardiac disorders, such as toxicologic insults and electrolyte abnormalities. The first ECG reveals a regular wide-complex tachycardia of unclear origin (Figure 1). The differential diagnosis for this finding includes supraventricular tachycardia with aberrancy or bundle-branch block, pacemaker-mediated tachycardia, sodium channel blocker toxicity, hyperkalemia, preexcitation, and ventricular tachycardia. Which of the following diagnoses is best supported by the ECGs and clinical findings? Fifteen minutes later, a second ECG is obtained (B). After arterial blood gas measurement reveals significant metabolic acidosis (pH, 7.08 PO2, 217 mm Hg PCO2, 22 mm Hg), sodium bicarbonate is administered. Initial treatment includes oxygen, intravenous fluids, and lidocaine the patient’s condition does not change. Neurologic examination demonstrates mild diffuse symmetric weakness.Īn ECG is obtained (A). A 2/6 systolic murmur is audible. Abdomen is soft and nontender. Heart rate is 152 beats per minute and regular respiration rate, 24 breaths per minute blood pressure, 142/68 mm Hg. Pulse oximetry shows that oxygen saturation is 95% on room air. He has no history of cardiac disorders, and he denies chest pain, palpitations, and abdominal pain. A 34-year-old man presents to the emergency department with progressive, generalized weakness and shortness of breath that began 2 weeks earlier.

0 notes
Text
Going through questions:
The most common pediatric leukemia is acute lymphoblastic leukemia (ALL). T cell or B cell ALL can occur. In T cell ALL, mediastinal masses occur.
Non-Hodgkin lymphoma causes B symptoms (weight loss, night sweats). Epstein Barr virus infects B cells and is associated with NHL. HIV infection is associated with NHL.
Multiple myeloma - plasma cell cancer-> monoclonal immunoglobulin (M-spike); presents with osteolytic lesions. Radiolucent bone lesions will be seen. Metastatic prostate cancer causes blastic bone lesions.
Bleeding time tells you about platelet defects. Von Willebrand disease-> prolonged bleeding time and PTT. vWF is needed for platelet adhesion and it is needed to stabilize factor 8. So No vWF-> no platelet adhesion (causing increased bleeding time) and unstable factor 8 (which is part of the intrinsic pathway, so increased PTT). I remembered that Von Willebrand's disease is the most common heritable bleeding disorder, which is why I got the question right. But now the increased bleeding time and PTT going with it make sense. It's AD.
Blood loss, not decreased nutritional intake, is the cause of iron deficiency anemia to rule out first in post-menopausal women. It could be an occult GI bleed.
LMWH binds to factor Xa and prevents it from converting prothrombin to thrombin. Unfractionated heparin can bind to factor Xa and to thrombin. So LMWH (e.g. enoxaparin) doesn't bind thrombin like unfractionated heparin does. LMWH is like heparin, but has fewer molecules than heparin.
Pyruvate kinase converts PEP to pyruvate in glycolysis. Pyruvate kinase deficiency-> hemolysis. Pts with pyruvate kinase deficiency have splenomegaly because cells in red pulp have more damaged RBCs to filter out.
I didn't know what a minor red blood cell antigen was. It's an antigen on the RBC that may not be screened for, thus a week later, pts have a reaction to it in delayed hemolytic transfusion reactions. He didn't mention this one in OnlineMedEd. The pt was initally exposed to the minor RBC antigen and developed memory B cells. The next time the pt is exposed, the B cells release antibodies (anamnestic response). Delayed hemolytic transfusion reaction occurs more than 24 hours after transfusion. Anamnestic response = delayed response
G6PD deficiency is X-linked recessive. I knew that's what the pt had in a question, but I forgot it's inheritance pattern. D: Heinz bodies are the hemoglobin that got damaged by oxidative stress because G6PD wasn't around to help regenerate the NADPH that is needed to make reduced glutathione, which prevents oxidative damage.
Herditary spherocytosis has AD inheritance pattern.
Schistocytes = hemlet cells. Thes occur in microangiopathic hemolytic anemia and in pts who have had heart valve surgery, which damages the RBCs. Artificial heart valves can damages RBCs-> schistocytes on blood smear. HUS, TTP, and DIC cause fibrin stands in small blood vessels-> schistocytes.
LMWH (e.g. enoxaparin) can be given for DVT in pregnant women. I remembered that heparin doesn't cross the placenta. But it is renally cleared, so if you have renal insufficiency (creatinine clearance less than 30 mL/min), then LMWH is contraindicated and you can give unfractionated heparin instead.
Azathioprine is a prodrug of 6-mercaptopurine. It gets metabolized by HGPRT into active 6-thioguanine, which is a purine analogue that disrupts DNA synthesis and thus prevents cell proliferation. 6MP is inactivated by xanthine oxidase and TPMT. Xanthine oxidase is inhibited by allopurinol and febuxostat. Some people have genetic deficiency of TPMT. If neither xanthine oxidase nor TPMT can inactivate 6MP, more of the 6MP gets converted to active 6-TG-> toxicity and increased immunosuppression. So some pts get genetic testing for TPMT before starting azathioprine and some pts need to avoid being on 6MP and allopurinol or febuxostat simultaneously.
Sickle cell is autosomal recessive, so you need 2 bad alleles to have it. If each parent is a carrier, then 1/4 kids will have it and 24 kids will be carriers. 1/4 kids will be normal. Glutamic acid (polar) is replaced by valine (non-polar) in sickle cell anemia. A point mutation in one of the codons for beta globin causes this substitution. This causes HbS.
One of my classmates mentioned rasburicase to me last year and I know it was between two answers in this question, but I chose the wrong one. D: It makes uric acid more soluble. In tumor lysis syndrome, more cells are being lysed by the chemotherapy. Since cells have high levels of K+ and phosphate, this can lead to hyperkalemia and hyperphosphatemia. Also, more protein needs to be broken down. Therefore, there's more purine catabolism. And purines end up as uric acid, which can precipitate in the kidneys and cause kidney injury. Rasburicase turns uric acid into allantoin, which is more soluble than uric acid and can be eliminated in the urine. Yeah, I remember my friend telling me that rasburicase is in certain animals. Rasburicase is recombinant urate oxidase. Animals have urate oxidase, but humans don't. So rasburicase turns uric acid into soluble allantoin, which is eliminated in urine. Allopurinol prevents formation of uric acid; it looks like purine and prevents xanthine oxidase from breaking down hypoxanthine. Febuxostat inhibits xanthine oxidase and has fewer adverse effects than allopurinol.
I didn't know heat stroke causes increased procoagulants. But it does and that leads to DIC due to increased coagulation factors; then you get increased fibrinolysis to get rid of the clots that form. Because the platelets and clotting factors all get used up, pts will bleed.
Multiple Myeloma = B cells become plasma cells that make a ton of useless immunoglobulin light chains. Treated with bortezomib, which causes increased apoptosis of plasma cells. Multiple myeloma causes lytic bone lesions, anemia, AKI, fatigue, constipation, weight loss. Myeloma kidney = light chain casts. Tons of kappa and lambda light chains being filtered by the kidney combine with Tam-Horsfall proteins (pretty sure I never heard of that) and cause casts that damage the tubules-> AKI. 24 hour rine protein is elevated.
Myeloma cells makes RANKL and destroy osteoprotegerin, which cause more activation of osteoclasts, hence the lytic bone lestions. I already reviewed RANK and RANKL and I know it pretty well. Glad I posted about it before. Multiple myeloma cells also release IL-3, IL-7, and Wnt pathway inhibitors, which inhibit osteoblasts.
I knew that this baby in this question had dactylitis, which occurs in sickle cell anemia, but I didn't understand what they were asking. If you have sickle cell, the sickled RBCs get destroyed, releasing hemoglobin. Hemoglobin is toxic and needs to be bound to haptoglobin. So the haptoglobin leven in the baby would be abnormal (decreased) because it would be all bound up by the Hgb coming from the hemolysis of the sickled RBCs. It had mentioned the baby's brother dying from an infection and I wasn't sure how that was related. It was because the brother also had sickle cell and therefore he probably had autosplenectomy due to the sickle cell. No spleen leaves you susceptible to encapsulated bugs like strep pneumo and the brother died from strep pneumo sepsis.
Hepcidin is an inflammatory mediator and it also decreases absorption of iron. So in anemia of chronic disease, hepcidin plays a role.
I knew this pt had beta thalassemia minor, I just didn't know what initiates it. It's a problem with mRNA. You see target cells and hypchromic, microcytic RBCs on blood smear. Pts have increased HbA2 (2 alpha chains and 2 delta chains; an alternate form of adult Hgb because they lack beta globin chains) and sometimes increased fetal Hgb (2 alpha chains and 2 gamma chains). If you try to treat these pts with iron, it doesn't do anything because they aren't iron deficient. Beta thalassemia is due to mutations that affect the transcription of mRNA for beta globin. Usually, there's messed up splicing of pre-mRNA or premature translation termination.
In obstructive sleep apnea, the kidney doesn't get enough oxygen, so it releases erythropoitein-> polycythemia (increased hematocrit).
Chemotherapy Induced Nausea and Vomiting (CINV) can be treated with 5HT3 receptor antagonists (ondansetron) and neurokinin-1 receptor antagonists (aprepitant). Early CINV is due to release of serotonin from enterochromaffin cells in the intestine that are damaged by the chemo. This leads to stimulation of 5HT3 vagal fibers-> vomiting reflex. Delayed CINV is due to substance P in the blood and CSF-> substance P binds neurokinin-1 receptor in the nucleus tractus solitarius and area postrema-> vomiting. Aprepitant can block the neurokinin-1 receptors and is therefore used for delayed CINV.
Low oxygen level leads to sickling of HgbS. High acid or dehydration also trigger the cycling. 2,3-BPG stabilizes the taut form of Hgb, which also would cause sickling. Low 2,3-BPG would increase Hgb's affinity for oxygen and thus decrease sickling. So high oxygen, high pH, and low levels of 2,3-BPG would prevent sickling. The opposite causes sickling. That's why pts with sickle cell anemia can't do as much strenuous activity--their HgbS starts sickling when they have less oxygen, more acid (from working muscles), and more need to unload oxygen to tissues (facilitated by 2,3-BPG) during exercise.
Fetal Hgb has replacement of histidine (positively charged amino acid) for serine, which is less positively charged. This prevents 2,3-BPG from binding for fetal hemoglobin, thus fetal hemoglobin has higher affinity for oxygen than adult hemoglobin. This helps baby take O2 from mom's hemoglobin in utero.
AML = Acute Myloid Leukemia = blasts (large nuclei, little cytoplasm) with Auer rods (rods seen in the blasts; not present in acute lymphoblastic leukemia, so look closeley to see if there are Auer rods--if there are, it's AML). Pts have pancytopenia. More than 20% myeloblasts in bone marrow. Chronic myelogenous leukemia = more mature cells.
Fluorescence In-Situ Hybridization (FISH) = cytogenetic test; finds deletions, translocations, and chromosome duplications in cells. FISH probes = ssDNA; they're added to the cell and combind with complementary DNA. FISH is more sensitive than karyotype.
Abixaban is a direct factor Xa inhibitor. It prevents conversion of factor II (prothrombin) to factor IIa (thrombin). I got the question wrong and so did 58% of respondents. It doesn't prevent conversion of factor X to Xa--it prevents factor Xa from converting prothrombin to thrombin. Wow. -_-
You need mitochondria to make heme. The precursors for RBCs have nuclei and mitochondria. After a certain division, they lose their nuclei, then they lose the mitochondria. So if they're at the point where they lack mitochondria, they can't make heme. Heme is made in the liver and in the erythrocyte precursors in the bone marrow.
Polycythemia can be relative (due to dehydration or diuresis), in which case plasma volume is decreased, but RBC mass, SaO2, and EPO levels are normal. Primary polycythemia = polycythemia vera; increased plasma volume, increased RBC mass, normal SaO2, and decreased EPO level. Secondary polycythemia can be physiologic or inappropriate. Physiologic = due to hypoxia; normal plasma volume, increased RBC mass, decreased SaO2, increased EPO level. Inappropriate = tumor that make EPO; normal plasma volume; increased RBC mass, normal SaO2, and increased EPO level.
Polycythemia vera = myeloproliferative disease of hematopoietic stem cells (HSC); mutation of JAK2 wherein valine is replaced with phenylalanine-> HSC are more sensitive to growth factor (EPO and thrombopoeitin, growth factors that stimulate erythrocyte and thrombocyte production). Pts can have itching after they shower due to release of histamine from basophils; plethora (red face), splenomegaly. Dx with low serum EPO and bone marrow study that shows the JAK2 mutation. Tx: phlebotomy.
I got confused about hepcidin. I know how it works and made a post about it before. I thought it came from the intestinal cells, but it doesn't. It comes from the liver and it can affect intestinal cells by preventing the absorption of iron from the gut. Hepatic parenchymal cells secrete hepcidin, which controls the storage and release of iron from other cells. Hepcidin is high when there's already enough serum iron. Hepcidin is also an acute phase reactant and is elevated during inflammation. Increased erythropoiesis and low oxygen lower hepcidin levels. Ferroportin-1 allows iron to come in on the basolateral side (the side of the intestinal cell that faces the blood) of intestinal cells. Ferroportin-1 is also located on macrophages. High serum iron or inflammation causes hepcidin to increase and hepcidin causes breakdown of ferroportin-1, preventing iron from coming into the blood. On the apical surface of intestinal cells (the side facing the gut lumen) is Divalent Metal Transporter-1 (DMT-1), which allows Fe2+ to be absorbed from the small intestine into the intestinal cell. Inside the enterocyte, the iron is either maintained inside ferritin, or it goes through ferroportin-1 into the blood, where transferrin binds to it and carries it to whatever cells have transferrin receptors, which allow the iron to be taken into said cell.
Nephrotic syndrome = loss of protein in urine; can lose anticoagulation factors, like antithrombin III in the urine-> hypercoagulable state-> renal vein thrombosis. Renal vein thrombosis-> hematuria, flank pain, increased LDH. So nephrotic syndrome is a hypercoagulable state.
Heparin is found in mast cells. LMWH enhances the effect of antithrombin III and inhibits factor Xa. Unfractionated heparin not only inhibits factor Xa, it also inhibits thrombin.
Ugh! There was a question about cancer and I knew breast cancer was more common in women but also knew that lung cancer has higher mortality. Most common cancers (by incidence) in women are breast, lung, and colorectal cancer. Breast cancer is more common in women, but not as deadly as lung cancer.
#B symptoms#oncology#ALL#non Hodgkin lymphoma#von willebrand disease#heparin#LMWH#anamnestic#anamnestic response#G6PD#hereditary spherocytosis#schistocytes#helmet cells#rasburicase#allantoin#multiple myeoloma#polycythemia#polycythemia vera#hepcidin#ferritin#transferrin#ferroportin#iron#cancer
5 notes
·
View notes
Text
If you have a Gram positive cocci (not tetrad) and the test results are catalase negative, beta hemolysis on blood agar, arabinose + and BEA + what is your organism?
If you have a Gram positive cocci (not tetrad) and the test results are catalase negative, beta hemolysis on blood agar, arabinose + and BEA + what is your organism?
Describe what each test would look like and write in complete sentences. Write out the full genus and species of the organism. 1. If you have a Gram positive cocci (not tetrad) and the test results are catalase negative, beta hemolysis on blood agar, arabinose + and BEA + what is your organism?
View On WordPress
0 notes
Photo

Therapeutics in Sickle Cell Anemia Apart from Hydroxyurea, Analgesics and vasodilators like phosphodiesterase inhibitors, certain tantalizing novel drugs have been approved for Sickle cell anemia.... Let's take a closer look at them. (1) Voxelotor (HbS polymerization inhibitor) binds covalently to N-terminal valine of alpha chain of HbS (around 30% of HbS in individual cell) stabilizing it's oxygenated form and causing left ward shift of dissociation curve without impairing oxygen delivery to tissues. Consistently reduces hemolysis and viscosity with in 2 weeks of administration... FIRST EVER therapy targeting core defect. It's ability to bind only around 30% of Hb in individual cells is crucial to maintain delicate balance between shifting the dissociation curve just enough to increase the affinity for oxygen so as to preclude vaso-occlusive crisis, while simultaneously ensuring that the oxygen delivery to tissues is not compromised because of excessive shift. (2) Crizanlizumab (Antibody against P-Selectin) blocks interaction between P-Selectin and PSGL1, resulting in reduced adhesion of erythrocytes to endothelium, and also preventing aggregation and migration of leukocytes to vascular bed, approved for reducing the frequency of vaso-occlusive crisis in sickle cell disease. (3) Glutamine is an amino acid oral powder for acute complications associated with SCD. Sickle RBCs are more susceptible to oxidative damage than normal RBCs, which may contribute to chronic hemolysis and vaso-occlusive events associated with SCD. Pyridine nucleotides, NAD+ and its reduced form NADH, regulates and prevents oxidative damage in RBCs. Glutamine is believed to improve the NAD redox potential in sickle RBCs by increasing reduced glutathione’s availability. What the future holds? Sevuparin - Lies along the spectrum of crizanlizumab, and has possible interactions with thrombospondin, fibronectin, vWF, P-Selectin and L- Selectin. Antibodies against iNKT (invariant Natural Killer T cells) - Oxygenation- Reoxygenation stress results in release of Adenosine, which acts on iNKT cells serving to fuel the NF-kappa beta pathway and subsequent Vasculopathy due to release of inflam https://www.instagram.com/p/CN6wFIqB6RE/?igshid=ob1vj393ab14
0 notes
Text
laboratory medicine
Adam Seegmiller, MD, PhD
laboratory tests
blood, urine, other tissues/substances sampled and tested in body, for the following
pre-symptomatic or pre-diagnostic screening (i.e., hemoglobin A1C or blood glucose for diabetes)
diagnosis and subclassifications of disease or condition + prognostic evaluation
plan treatment pathways and evaluate treatment response in patient
longitudinal disease monitoring
highest volume medical activity in the US - 70% of medical record data | but only make up 4% of medical cost, pretty good
tests are ordered from physician, or symptoms are given and then tests are determined | test ordering is now more collaborative
assays and activities
hematology - count and characterize blood cells
clinical chemistry - concentration / activity of blood macromolecules or enzymes
virology + microbiology - presence of infectious microorganisms
immunology - assessment of immune system function (immunodeficiency, immunosuppression, auto-immune disorders)
cytogenetics + molecular diagnostics - inherited or neoplastic (environmentally mutated) genotype determination
transfusion medicine - blood type determination and blood transfusion to patients
techniques
electrical impedance - passing sample through electrical field yields an electrical signal for each cell that corresponds to cell’s size
colorimetric or spectrophotometric chemical reactions for quantification of chemical levels
immunoassays - use of antibodies to determine protein presence in sample
flow cytometry
turbidimetry - light impedance in blood and other liquid substances
DNA assays - FISH, PCR, probe assays, Sanger sequencing
case study
» symptoms
fatigue and lowered exercise capacity
history of autoimmune diseases (thyroiditis, inflammatory bowel disease)
pallor and tachycardia, fatigue
» lab tests
1. complete blood count (red, white, clotting platelets) and analysis of cellular properties with hematology analyzer
compare results to reference range, central 95%, for healthy age, sex, and clinical situation
ranges include many different types of statistical curves and bounds
one-tailed, i.e., amount ≥ 0
medical decision level: certain threshold for determination of condition
therapeutic range: drug quantity reflection
critical value: life-threatening threshold reached, treatment needed
quality control for testing
validation of testing method accuracy and precision via expected values or parameters of safety » include linearity and reportable range
regular quality control throughout assay performance and 24hr period to ensure initially validated mechanisms hold true to starting accuracy and precision
if measures are outside of linear range, do a dilution of sample to return to linear range
2. results indicate the following about the patient:
microcytic - small red blood cells, some oddly shaped / narrow
anemia - hemoglobin malfunction or non-function, non-amount
hypochromic cells (not enough hemoglobin binding in the center
» core source of patient’s condition
anemia occurs in one of two ways - not enough blood cells in, or too many blood cells out
impaired production - ineffective hematopoiesis or decreased levels of precursors
increased destruction - blood loss or premature hemolysis (shortened lifespan of RBCs)
patient has microcytic anemia - could be thalassemia or iron deficiency
measure types of hemoglobin - alpha, beta, delta, gamma - via assays
thalassemia patients have more compensatory delta hemoglobin
but patient does not have history of anemia, so might be iron deficiency
look at difference between MCV / RBC assay results of thalassemia and iron deficiency
patient most likely has iron deficiency » move to confirm with clinical chemistry
iron is mostly attached to hemoglobin, myoglobin, or bone marrow – can measure Fe in many different ways
serum iron via photometry | saturate blood with iron and measure binding | serum ferritin precursor from bone marrow via immunoassay
results from patient: serum iron is low, iron binding is also low
patient has falsely high ferritin because she has co-morbid inflammatory disease
» conclusion: patient has iron deficiency
could be dietary - eat more meat and take iron supplements
could be absorption related - iron can be in diet but maybe inflammatory bowel disease = inability to absorb
chronic bleeding in older patients - indicates small bleeding constantly, often colon cancer or ulcer in elderly
career pathways in laboratory medicine
» PhD Route - shorter, but must be more focused
PhD in life sciences (take your pick! biochemistry, genetics, microbiology, etc.)
then specific fellowship training in clinical chemistry, microbiology, genetics, genomics
» MD Route - longer, but more freedom
MD and residency in clinical pathology
then clinical fellowship in area-specific laboratory medicine
0 notes
Photo

In lab we performed a pharyngeal swab and subsequent culture to see if we were carriers of Streptococcus pyogenes, which I am thankfully not (no beta hemolysis on the blood agar!).
I apparently do have the (quite normal) flora consisting of the pretty golden Staphylococcus aureus (on the MS agar) and what appears to be some strain of Enterococcus (on the EMB agar).
Its kinda cool in a gross way to see these babies flourish overnight. Considering a decent percentage of our body mass is composed of bacteria, and they are kind of vital to our survival, I wonder if it’s okay to feel kinda like these colonies are bits of me? Even if they don’t have any of my DNA or whatever...
10 notes
·
View notes