#animal estrogen and breast cancer
Explore tagged Tumblr posts
Text
Chapter 7. Polluted Politics? Confronting Toxic Discourse, Sex Panic and Eco-Normativity by Giovanna Di Chiro
“Stereotypes and lies lodge in our bodies as surely as bullets. They live and fester there, stealing the body.”—Eli Clare
Queer ecology as defined by Mortimer-Sandilands (2005, 24) “both about seeing beauty in the wounds of the world and taking responsibility to care for the world as it is”. (200)
Environmental justice constructs an eco-politics that defines the environment as our communities: the places where ‘we live, work, play, and learn’ (200). Environmental justice activists embrace inhabited/built places---cities, villages, reservations, agricultural fields, workplaces, poor and low-income neighborhoods next to hazardous industrial facilities as environments worthy of recognition and protection (Di Chiro 1996)
There has been rising environmental anxiety that surrounds cultural fears of exposure to chemical and endocrine-disrupting toxins especially as it relates to the troubling and destabilizing of normal/natural gendered bodies of humans and other animal species aka the “chemical castration” or the “feminization of nature” (Cadbury 1998; Hayes 2002)--rising fears that we are “swimming in a sea of estrogen” (Raloff 1994b, 56; Sumpter and Jobling 1995 173) as a consequence of rising levels of estrogenic, synthetic chemical compounds emitted into our water, air and food known as estrogenic pollution (ova-pollution). (201)
Pop-science warning about the ‘instability of maleness’—warns that the rising incidences of male-to-female gender shifts and intersex conditions observed in the ‘lower’ species of animals, such as frogs, fish, and salamanders, represent the newest ‘canaries in the coalmine’ portending an uncertain fate for human maleness and for the future of ‘normal’ sexual reproduction (Robert 2003) (201) also anti-toxins discourse has concerns about estrogenic chemical toxins disrupting/preventing/disturbing ‘normal’ prenatal physiological development and natural reproductive processes, leading to rising cases of infertility and producing disabled, defective, and even monstrous bodies (201)…
What can develop is a “sex panic” that resuscitates familiar heterosexist, queerphobic, and eugenics arguments classifying some bodies as not normal: mistakes, perversions, burdens (I would add ‘freaks’)…under the guise of laudable goal/progressive goals, a certain type of anti-toxics environmentalism mobilizes knowledge/power of normalcy and normativity and reinforces compulsory social-environmental order based on a dominant regime of what and who are constructed as normal and natural (Davis 1995; Garland-Thompson 1997; McRuer 2006).
Disability becomes an environmental problem and lgbtq people become disabled—the unintended consequences of a contaminated and impure environment, unjustly impaired by chemical trespass. (202) The true scope of the mortality and morbidity of POPs (persistent organic pollutants) becomes distorted by alarmist focus. This fixation ends up de-emphasizing and worse--naturalizing and normalizing other serious health problems associated with POPs that are on the rise: breast, ovarian, prostate and testicular cancers, neurological and neurobehavioral problems, immune system breakdown, heart disease, diabetes and obesity (202).
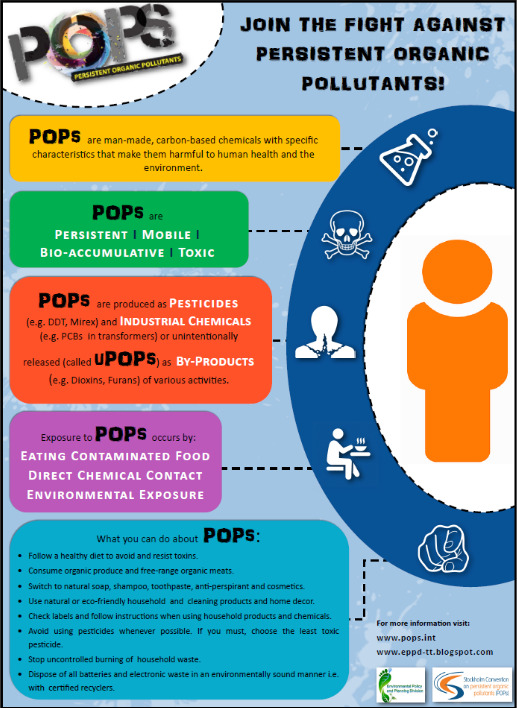
There is good reason for alarm concerning the continued use and accumulation of toxic chemicals that are wreaking havoc on the health and reproductive possibilities of the living world. Our cumulative exposures to endocrine disruptors, carcinogens, neurotoxins, asthmagens, and mutagens in our normal, everyday lives from our daily contact with plastic water bottles, shampoos, and kitchen cleaners to insect repellents, food preservatives, and factory farmed meats, among others, are most certainly putting at risk the health of our own bodies and our earth. (210) But where should the critical attention lie?
The hyperfocus on the world turning into hermaphrodites participates in a sexual titillation strategy summoning the familiar ‘crimes against’ nature’ credo and inviting culturally sanctioned homophobia while at the same time sidelining and naturalizing ‘normal’ environmental diseases such as cancer (211).
--
Environmental theory and politics in the US have historically mobilized ideas of the normal, to determine which bodies and environments/landscapes embody the distinctly American values of productive work, rugged individualism, masculinity, independence, potency, and moral virtue upon which environmental advocacy movements should be based (Haraway 1989; Cronon 1991). Critical histories of U.S. environmentalism have revealed the capitalist, patriarchal, colonialist, heteronormative, eugenicist, and ableist histories underlying its “progressive” exterior (Boag 2003; Darnovky 1992; Evans 2002; Gaard 2004; Jaquette 2005; Sutter 2001).
Eco-normativity (or eco[hetero]normativity) appear in alarmist discourse in the anti-toxins arm of the environmental movement. Their alarm about contaminants effect on sex/gender appeals to preexisting cultural norms of gender balance, normal sexual reproduction and the balance of nature. The use of “anti-normal” “anti-natural” in antitoxins discourse is highly questionable and risks reinforcing the dominant social and economic order (the forces actually responsible for environmental destruction and toxic contamination of all our bodies and environments) by naturalizing the multiple injustices that shore it up”…and thus creates what the author terms, polluted politics.
#queer ecologies: sex nature politics desire#econormativity#heteronormativity#critical ecology#queer ecology#ecology#environmental contamination#persistent organic pollutants#toxins#anti toxins#eugenics#ecofeminism#environmental politics#ecological science#environmental science
40 notes
·
View notes
Text
**Resveratrol: A Comprehensive Overview**
---
### **1. What is Resveratrol?**
- **Origin**: A naturally occurring polyphenol (stilbenoid) produced by plants as a defense mechanism against stress, pathogens, and UV radiation.
- **Sources**:
- Grapes, red wine, berries (blueberries, cranberries), peanuts, and Japanese knotweed (*Polygonum cuspidatum*).
- Red wine is famously linked to the "French Paradox" (low cardiovascular disease rates despite a high-fat diet).
- **Production**: Extracted from plants or synthesized chemically. Common supplements derive from Japanese knotweed or grape skins.
---
### **2. Mechanism of Action**
- **Antioxidant Activity**: Neutralizes free radicals and enhances cellular antioxidant defenses (e.g., glutathione).
- **Sirtuin Activation**: Activates *SIRT1* (a longevity-associated protein), influencing cellular repair, metabolism, and aging.
- **Anti-Inflammatory Effects**: Inhibits pro-inflammatory pathways (e.g., NF-κB, COX-2).
- **Cardioprotective Effects**: Improves endothelial function, reduces LDL oxidation, and promotes vasodilation via nitric oxide.
- **Epigenetic Modulation**: May influence gene expression linked to aging and disease.
---
### **3. Clinical Uses & Research**
- **Cardiovascular Health**:
- Linked to reduced atherosclerosis and improved lipid profiles in animal studies.
- Human trials show mixed results; some report improved endothelial function, while others find no significant cardiovascular benefits.
- **Anti-Aging & Longevity**:
- Activates pathways similar to calorie restriction (e.g., SIRT1) in animal models, extending lifespan in yeast, worms, and mice.
- No conclusive evidence in humans for lifespan extension.
- **Neuroprotection**:
- May reduce amyloid-beta plaques in Alzheimer’s models and improve cognitive function in rodents.
- Small human studies suggest potential for slowing cognitive decline, but larger trials are needed.
- **Cancer Prevention**:
- Inhibits tumor growth and angiogenesis in preclinical studies (e.g., breast, colon, prostate cancers).
- Limited human data; not yet proven as a therapeutic agent.
- **Diabetes & Metabolic Health**:
- Improves insulin sensitivity and reduces blood glucose in animal studies.
- Some human trials show modest benefits in glycemic control.
---
### **4. Safety & Side Effects**
- **Generally Safe**: Well-tolerated at typical doses (up to 1,500 mg/day).
- **Possible Side Effects**:
- Mild gastrointestinal issues (nausea, diarrhea).
- High doses may interact with blood thinners (e.g., warfarin) due to antiplatelet effects.
- **Contraindications**:
- Avoid in pregnancy (estrogenic activity in high doses).
- Use caution with hormone-sensitive cancers (theoretical risk of estrogen modulation).
---
### **5. Dosage & Bioavailability**
- **Typical Supplement Dose**: 150–500 mg/day, often paired with piperine (black pepper extract) to enhance absorption.
- **Bioavailability Challenges**: Poor absorption and rapid metabolism; nanoparticle formulations or combined supplements may improve efficacy.
---
### **6. Research Limitations**
- **Preclinical Bias**: Most promising data come from animal or cell studies; human trials are limited and inconsistent.
- **Dose Discrepancies**: Effective doses in animals often exceed safe human intake.
- **Confounding Factors**: Benefits in observational studies (e.g., red wine consumption) may stem from other polyphenols or lifestyle factors.
---
### **7. Quality & Availability**
- **Forms**: Capsules, tablets, liquids, and transdermal patches.
- **Quality Control**: Look for third-party testing (e.g., USP, NSF) due to variability in purity and concentration.
---
### **8. Conclusion**
Resveratrol is a multifunctional polyphenol with potential benefits for cardiovascular health, neuroprotection, and longevity. While preclinical data are compelling, human evidence remains inconclusive. Its poor bioavailability and mixed trial results highlight the need for further research. Consultation with a healthcare provider is advised, especially for those on medications or with chronic conditions.
**Key References**:
- Baur & Sinclair (2006) on longevity mechanisms.
- Timmers et al. (2011) on metabolic benefits in humans.
- Kennedy et al. (2010) on cognitive effects.
*Note: This information is educational and not a substitute for medical advice. Always consult a healthcare professional before starting supplements.*
0 notes
Text
Immunohistochemistry Boosts Drug Development Success

Immunohistochemistry (IHC) is a technique used to detect antigens (proteins) in cells of a tissue section by exploiting the principle of antibodies binding specifically to antigens in biological tissues. IHC takes advantage of the principles of an antibody's ability to recognize and bind to a specific site called an antigen. The site is usually a protein that is present on the surface or inside cells. The presence of the protein, or antigen, may indicate something important about the function or disease state of the cell or tissue. Applications of IHC in Diagnostics Immunohistochemistry is widely used in clinical diagnostics for detecting biomarkers associated with diseases. It helps pathologists to accurately diagnose cancer type and stage by identifying molecular markers in tumor cells. For example, breast cancers diagnosed as luminal A-type are estrogen receptor positive as detected by IHC. This guides treatment decision towards hormone therapy. IHC also aids in sub-classifying lymphomas and determining tumor grade in prostate cancer biopsies. In research, IHC is utilized for protein localization studies to gain insights into disease mechanisms. Role in Drug Development Pharmaceutical companies rely on IHC throughout the drug development process. During target identification and validation, IHC confirms the expression and localization of potential drug targets in diseased tissues. This helps assess whether modulating the target could provide therapeutic benefit. During preclinical development, IHC on animal models establishes target engagement and desired downstream effects of drug candidates. Later in clinical trials, IHC on patient biopsies evaluates target expression, engagement and related biomarkers to monitor drug response. Post-marketing, IHC supports companion diagnostic development to identify patients most likely to benefit from a targeted therapy.
0 notes
Text
A Brief Guide to Natural Bath, Body, and Personal Products

Choosing bath, body, and personal products that contain natural ingredients is crucial, especially for those with a diagnosis of cancer. Conventional cancer treatments like chemotherapy, immunotherapy, and radiation can cause skin sensitivity, making it prone to irritation. Natural ingredients are typically gentler and less likely to cause adverse reactions. Many conventional body products contain potentially harmful chemicals like parabens, phthalates, and synthetic fragrances that can increase one’s chemical burden and disrupt the balance of hormones in the body. By using natural products, you can reduce exposure to chemicals, support your immune system, and allow your body to focus on healing. In addition, natural body products can nourish, soothe, hydrate, and heal the skin, which is especially important for skin that has been damaged by treatment. When choosing cosmetics, shampoos, conditioners, soaps, lotions, sunscreen, and toothpaste, here’s the long list of ingredients to avoid.
Most common toxic ingredients found in cosmetics, shampoos, conditioners, body washes, and moisturizers:
Parabens - May be listed as methylparaben, polyparaben, isoparaben, or butylparaben. These can be directly absorbed through skin and induce estrogen-like activity on the body.
Phthalates - Also listed as butyl benzyl phthalate (BBP), Di-n-butyl phthalate (DBP), Di-ethylhexyl phthalate (DEHP), and Diethyl phthalate (DEP). These are hormone disrupting chemicals that may be linked to breast and prostate cancers, as well as many other diseases. It’s important to note that many perfumes use phthalates, but often times it is not listed on the label. If you choose to go phthalate-free, avoid wearing perfume and/or choose essential oils instead.
Triclosan - This ingredient is commonly found in antibacterial soap. Triclosan has been shown to suppress NK cell activity. NK cells are natural killer cells that help our body constantly fight against infection, as well as cancer.
Toxic chemicals most commonly found in deodorant:
Aluminum and aluminum zirconium- Both can have an estrogen-like activity in the body. This is extremely important to consider when choosing deodorant, as most conventional deodorants contain aluminum.
Toxic chemicals most commonly found in toothpaste:
Triclosan- An organic compound with antibacterial properties that can disrupt thyroid function and antibiotic resistance. It's also been linked to gum recessions and a variety of cancers.
Sodium lauryl sulfate (SLS) - A detergent and cosmetic ingredient that can irritate the gums and cause canker sores, gum recessions, and allergic reactions.
Fluoride - Can be toxic if ingested in large amounts, causing nausea, vomiting, and headaches.
Titanium dioxide - The Environmental Working Group classifies this ingredient as a possible carcinogen.
Microbeads - Made from insoluble plastics that can't be digested and can end up in waterways, where they can absorb toxic chemicals and harm marine life.
MEA, DEA, and TEA - Methylating compounds that can weaken the liver and kidneys and lead to cancer.
Propylene glycol- A synthetic chemical compound that can irritate the skin, eyes, lungs, and mucous membranes. It's also a strong carcinogen.
Saccharin - An artificial sweetener that can cause coughing, nausea, vomiting, and diarrhea. Saccharin has also been linked to many different kinds of cancers.
Diethanolamine (DEA) - A chemical used as a foaming agent that can cause organ-system toxicity. A 1998 study linked topical application of DEA to cancer in animals.
Aspartame - Consumption of aspartame could potentially lead to illnesses such as Alzheimer's, diabetes, and multiple sclerosis. Aspartame is also linked to various kinds of cancers.
Check out my Pinterests with specific recommendations for clean and safe body products approved by the Environmental Working Group (EWG.org) for 2024.
Shampoos and Body Washes
https://pin.it/6zEkeukCI
Moisturizers
https://pin.it/1i1QUTecp
Sunscreens
https://pin.it/3JaNYHM7l
Face Wash
https://pin.it/4MqigKwCV
Toothpaste
https://pin.it/5lfwEbrRP
#natural body products#natural shampoo#natural body wash#natural moisturizers#natural suscreen#natural face wash#natural toothpaste#EWG#organicbeauty#cancer#integrativeoncology
0 notes
Text

Image Credit: Maria I. Morasso, Ph.D.; National Institutes of Health
Scientists Discover A New Hormone That Can Build Strong Bones
Researchers at UCSF and UC Davis solved a long-standing puzzle on how the bones of breastfeeding women stay strong even as they lose calcium to milk.
— By Sarah C.P. Williams | University of California San Francisco | July 10, 2024
A newly discovered hormone that keeps the bones of breastfeeding women strong could also help bone fractures heal and treat osteoporosis in the broader population. Researchers at UC San Francisco and UC Davis showed that in mice, the hormone known as Maternal Brain Hormone (CCN3) increases bone density and strength.
Their results, published July 10 in Nature, solve a long-standing puzzle about how women’s bones remain relatively robust during breastfeeding, even as calcium is stripped from bones to support milk production.
“One of the remarkable things about these findings is that if we hadn’t been studying female mice, which unfortunately is the norm in biomedical research, then we could have completely missed out on this finding,” said Holly Ingraham, PhD, the senior author of the new paper and a professor cellular molecular pharmacology at UCSF. “It underscores just how important it is to look at both male and female animals across the lifespan to get a full understanding of biology.”
More than 200 million people worldwide suffer from osteoporosis, a severe weakening of the bones that can cause frequent fractures. Women are at particularly high risk of osteoporosis after menopause because of declining levels of the sex hormone estrogen, which normally promotes bone formation. Estrogen levels are also low during breastfeeding, yet osteoporosis and bone fractures are much rarer during this time, suggesting that something other than estrogen promotes bone growth.
A Hormone That Is Only Produced During Lactation

During lactation, CCN3 (red) appears in the female brain in neurons adjacent to other cells, called tanycytes (cyan). Image by Ingraham Lab
Ingraham’s lab previously discovered that in female mice, but not male mice, blocking a particular estrogen receptor found in select neurons in a small area of the brain led to huge increases in bone mass. They suspected that a hormone in the blood was responsible for the super-strong bones but, at the time, could not find it – a quest that was further protracted during the worldwide pandemic.
In the new work, Ingraham and collaborators carried out an exhaustive search for this bone-building hormone and finally pinpointed CCN3 as the factor responsible in mutant females. Initially, the team was surprised by this result, as CCN3 did not fit the typical profile of a secreted hormone from neurons.
Their doubts vanished after they found CCN3 in the same brain region in lactating female mice. Without the production of CCN3 in these select neurons, lactating female mice rapidly lost bone, and their babies began to lose weight, confirming the importance of the hormone in maintaining bone health during lactation. Based on this discovery, they now refer to CCN3 as Maternal Brain Hormone (MBH).
Hormone Strengthens Bones in Young, Old, Male and Female Mice
Bone loss happens not only in post-menopausal women, but is also common in:
Breast cancer survivors taking certain hormone blockers
Younger, highly trained elite female athletes
Older men whose relative survival rate is poorer than women after a hip fracture
When strategies to increase circulating CCN3 were implemented in young adult and older female or male mice, their bone mass and strength increased dramatically over the course of weeks. In some female mice who lacked all estrogen or were very old, CCN3 was able to more than double bone mass.
When Ingraham’s scientific collaborator, Thomas Ambrosi, PhD, an assistant professor of orthopaedic surgery at UC Davis, tested these bones, he was surprised by their strength.
“There are some situations where highly mineralized bones are not better; they can be weaker and actually break more easily,” he explained. “But when we tested these bones, they turned out to be much stronger than usual.”
Ambrosi looked closely at the stem cells within the bones that are responsible for generating new bone and found that when these cells were exposed to CCN3, they were much more prone to generate new bone cells.
A Hydrogel Patch Heals Fractures in Mice
To test the ability of the hormone to assist in bone healing, the researchers created a hydrogel patch that could be applied directly to the site of a bone fracture, where it would slowly release CCN3 for two weeks. In elderly mice, bone fractures don’t usually heal well. However, the CCN3 patch spurred the formation of new bone at the site of the fracture, contributing to youthful healing of the fracture.
“We’ve never been able to achieve this kind of mineralization and healing outcome with any other strategy,” Ambrosi said. “We’re really excited to follow it up and potentially apply CCN3 in the context of other problems, such as regrowing cartilage.”
The researchers plan to carry out future studies on the molecular mechanisms of CCN3, its levels in breastfeeding women, as well as the potential of the hormone to treat a variety of bone conditions.
Muriel Babey, MD, a co-first author and mentored physician-scientist in the Division of Endocrinology at UCSF, is keen to begin asking how CCN3 impacts bone metabolism in clinically relevant disease settings. Partnering with the UCSF Catalyst program, William Krause, PhD, a senior scientist and co-lead on this project will begin translating these new results.
“Bone loss happens not only in post-menopausal women but often occurs in breast cancer survivors that take certain hormone blockers; in younger, highly trained elite female athletes; and in older men whose relative survival rate is poorer than women after a hip fracture,” Ingraham said. “It would be incredibly exciting if CCN3 could increase bone mass in all these scenarios.”

William Krause, PhD, left; Muriel Babey, MD, center; and Holly Ingraham, PhD, right, at the Ingraham Lab in Arthur and Toni Rembe Rock Hall at the UCSF Mission Bay campus. Photo by Susan Merrell
— Authors: Other UCSF authors include Candice B. Herber, Zsofia Torok, Joni Nikkanen, Ruben Rodriquez, Saul Villeda and Fernanda Castro-Navarro. Other UC Davis authors include Kun Chen, Erika E. Wheeler, J. Kent Leach, and Nancy E. Lane. Please see the paper for a complete author list.
#Aging#Biochemistry | Molecular Biology#Neurology#Neurosciences#Osteoporosis#Bone Health#Women’s Health
0 notes
Text
Unlocking the Potential: Exploring Diindolylmethane (DIM) Research
In the realm of nutritional supplements, diindolylmethane (DIM) has been garnering increasing attention for its potential health benefits. Derived from cruciferous vegetables like broccoli, Brussels sprouts, and kale, DIM has been the subject of numerous studies investigating its effects on human health. Let's delve into the exciting world of DIM research and uncover the potential it holds for our well-being. Get more info about diindolylmethane DIM supplement resources click here.
Understanding DIM:
Diindolylmethane is a compound formed in the body when we digest certain vegetables. It belongs to a class of compounds known as indoles, which are sulfur-containing chemicals found in cruciferous vegetables. DIM is particularly abundant in broccoli, cauliflower, cabbage, and other vegetables of the Brassica genus.
Cancer Prevention and Treatment:
One of the most compelling areas of DIM research revolves around its potential in cancer prevention and treatment. Studies have suggested that DIM may have anti-cancer properties, particularly in hormone-related cancers such as breast, prostate, and cervical cancers.
Research indicates that DIM may modulate estrogen metabolism, potentially reducing the risk of estrogen-driven cancers. It is believed to promote the conversion of estrogen into less potent forms, which may help prevent the proliferation of cancer cells. Additionally, DIM has shown promise in inhibiting tumor growth and inducing apoptosis (cell death) in cancer cells in various laboratory studies.
Hormonal Balance:
DIM's ability to modulate estrogen levels also makes it a subject of interest in hormone-related conditions such as polycystic ovary syndrome (PCOS) and menopausal symptoms. By promoting a balance in estrogen metabolism, DIM may help alleviate symptoms such as irregular menstrual cycles, hormonal acne, and mood swings associated with hormonal imbalances.
Immune Function:
Emerging research suggests that DIM may also play a role in supporting immune function. By promoting a healthy balance of hormones and reducing inflammation, DIM could potentially bolster the body's immune response, helping it fend off infections and diseases more effectively.
Cardiovascular Health:
Some studies have explored the potential cardiovascular benefits of DIM. It is thought to exert antioxidant and anti-inflammatory effects that may help protect against cardiovascular diseases such as atherosclerosis and heart disease. By reducing oxidative stress and inflammation, DIM may contribute to overall heart health.
Considerations and Future Directions:
While the research surrounding DIM is promising, it is essential to approach it with a critical eye. Many studies have been conducted in vitro or on animals, and more human clinical trials are needed to fully understand DIM's effects and optimal dosage for various health conditions.
Additionally, individual responses to DIM may vary, and it's essential to consult with a healthcare professional before starting any new supplement regimen, especially for individuals with pre-existing medical conditions or those taking medications.
In conclusion, diindolylmethane represents a fascinating area of research with the potential to positively impact human health in various ways, from cancer prevention to hormonal balance and immune support. As scientists continue to unravel its mechanisms and conduct further studies, DIM may emerge as a valuable tool in promoting overall well-being and longevity.
0 notes
Text
Debunking The Lie That Royal Jelly Causes Breast Cancer

Royal jelly, a milky treasure secreted by worker bees, has garnered widespread recognition as a natural health booster. As a leading producer and exporter, China plays a crucial role in the global apiculture market, contributing a significant portion of the world's royal jelly. However, unfounded rumors have cast a shadow on its reputation, alleging high estrogen content and a potential link to breast cancer. Let's delve deeper and dispel these myths with scientific evidence. 1.Examining the Estrogen Content: Royal jelly boasts a diverse portfolio of nutrients, including proteins, vitamins, and minerals, renowned for its various health benefits like anti-inflammatory and anti-tumor properties. While estrogen, a crucial hormone primarily produced by the ovaries, is present in all animal-derived food, research reveals minimal traces in royal jelly. In fact, over 88% of samples contained less than 1.0 micrograms per kilogram (μg/kg), significantly lower than commonly consumed foods. These negligible levels effectively debunk the exaggerated claims about high estrogen content in royal jelly. 2.Separating Fact from Fiction: Does Royal Jelly Increase Breast Cancer Risk? Based on established guidelines and residue limits set by international organizations, a person would need to consume an unimaginable 3 kilograms of royal jelly daily to pose any potential harm. This figure stands in stark contrast to the recommended dosage of 10-15 grams, highlighting the absurdity of the claim. Furthermore, extensive research, including long-term studies, has found no link between royal jelly consumption and an increased risk of breast cancer. This scientific evidence provides reassurance about the safety of incorporating royal jelly into your diet. 3.A Note on Cautious Consumption: While generally safe, it's essential to be mindful when consuming any health supplement, including royal jelly. Individuals with allergies, pregnant women, and adolescents are advised to consult a healthcare professional before including it in their diet. In summary, rumors about royal jelly’s high estrogen content and its link to breast cancer lack scientific basis. The benefits of this natural treasure far outweigh unfounded claims, and through responsible consumption, individuals can safely explore its many health advantages. Read the full article
0 notes
Text
The Health Benefits of Icariin: A Natural Remedy for Various Ailments
Icariin Extract, a flavonoid compound found in the Epimedium plant, has been used in traditional Chinese medicine for centuries. Recently, it has gained popularity in the Western world for its numerous health benefits. Here are some of the benefits of icariin:
Increases libido: Icariin has been shown to increase sexual desire and improve erectile function in men. It works by increasing nitric oxide levels in the body, which relaxes blood vessels and improves blood flow to the genital area.
Boosts bone health: Icariin has been found to positively affect bone health by increasing bone density and reducing the risk of osteoporosis. It works by stimulating the production of osteoblasts, cells responsible for bone formation.
Reduces inflammation: Icariin has anti-inflammatory properties that can help reduce inflammation. This can be particularly beneficial for those with arthritis and other inflammatory disorders.
Enhances cognitive function: Icariin has been found to improve cognitive function and memory in animal studies. It promotes the growth of new brain cells and increases blood flow to the brain.
Protects the heart: Icariin has been shown to protect the heart by reducing oxidative stress and inflammation. This can help reduce the risk of heart disease and stroke.
Safety precautions (7 contraindications)
Not recommended for pregnant or breastfeeding women due to unknown safety.
Not recommended for individuals with poor liver, kidney, and cardiovascular function as it may cause unknown adverse reactions.
Do not take with medications or health supplements that may affect heart rhythm as they may cause unknown risks, such as asthma medications, antibiotics, cough medicine, cold medicine, antihistamines, thyroid medication, antidepressants, bitter orange, valerian, hawthorn, ginseng, ephedra, coffee, alcohol, cocaine, marijuana, etc.
It is not recommended for individuals with abnormal blood clotting within two weeks before surgery or taking anticoagulants, as it may slow down blood clotting and increase the risk of bleeding. Relevant medication names include aspirin, clopidogrel, diclofenac, ibuprofen, naproxen, dalteparin, enoxaparin, heparin, and warfarin.
It is not recommended for individuals with hormone-sensitive diseases or cancers (such as breast, uterine, or ovarian cancer) due to its potential estrogen-like effects, which may worsen symptoms.
It is not recommended for individuals with low blood pressure or taking related blood pressure-lowering medications, as it may further lower blood pressure. Relevant medication names include captopril, enalapril, losartan, valsartan, diltiazem, Amlodipine, hydrochlorothiazide, and furosemide.
It is not recommended for individuals with a history of allergy to the Berberidaceae family of plants, as it may trigger allergic reactions, such as rash, sweating, or fever.
Icariin Extract can be found in supplement form and is available in various dosages. As with any supplement, it is essential to consult a healthcare professional before taking icariin, especially if you have a pre-existing medical condition or are taking other medications.

Epimedium, Icariin, Icariin Extract
0 notes
Text
What are the health benefits of garlic ?
Garlic is widely recognized for its culinary uses and distinct flavor, but it also offers several potential health benefits. Garlic contains various bioactive compounds, including sulfur-containing compounds like allicin, which are believed to contribute to its medicinal properties. Here are some of the potential health benefits associated with garlic:
Immune system support: Garlic has been traditionally used to boost the immune system and help fight off common illnesses like colds and flu. It may have antimicrobial properties that can help combat certain bacteria, viruses, and fungi.
2. Cardiovascular health: Garlic has been associated with potential cardiovascular benefits. It may help lower blood pressure, reduce cholesterol levels (including LDL or "bad" cholesterol), and inhibit blood clotting, which can be beneficial for heart health. These effects may contribute to a decreased risk of heart disease.
3. Antioxidant properties: Garlic contains antioxidants that help protect cells from oxidative damage caused by harmful molecules called free radicals. Antioxidants play a role in reducing inflammation and may contribute to overall health and disease prevention.
4. Anti-inflammatory effects: Some compounds in garlic have anti-inflammatory properties that can help reduce inflammation in the body. Chronic inflammation is linked to various health conditions, including heart disease, cancer, and rheumatoid arthritis.
5. Cancer prevention: Garlic has been studied for its potential cancer-fighting properties. Some research suggests that garlic consumption may be associated with a reduced risk of certain cancers, including those of the stomach, colon, esophagus, and breast. However, more studies are needed to establish conclusive evidence.
6. Improved digestion: Garlic has been used traditionally to aid digestion and alleviate digestive discomfort. It may stimulate the production of digestive enzymes, support the growth of beneficial gut bacteria, and promote healthy digestion.
7. Antimicrobial properties: Garlic has shown antimicrobial activity against various bacteria, viruses, and fungi. It may help combat certain infections, such as those caused by bacteria like E. coli or fungi like Candida.
8. Improved bone health: Some animal studies suggest that garlic may help improve bone health by increasing estrogen levels in females, which can contribute to enhanced bone density.
It's important to note that while garlic offers potential health benefits, it should not be considered a substitute for medical treatment or professional advice. It's always advisable to consult with a healthcare professional before making any significant changes to your diet or using garlic supplements, especially if you have specific health conditions or are taking medications.

0 notes
Text
Best Cruelty free Mascara
With treatments from eyelash extensions to perming, it’s fair to say that we’re more lash-obsessed than ever. We’ve all been there, from bending our mascara wand to trying the spoon technique. Is it really time to start learning about natural mascara? We sure think so! If this is your first time venturing into the world of natural makeup, no worries. We’re covering all the in’s and out’s of our Best Cruelty free Mascara, so you can make the best choice for your beauty needs (beauty is power!).
Why choose a natural mascara?
We don’t want to be fearmongers. We agree, makeup is a fun and empowering form of self expression. The truth is, your skin absorbs what you put on it — a fact you should be even more concerned about in regards to your eye area.
First of all, what makes a mascara “natural?” The truth is, there’s no set definition for what “natural” means. A good place to start would be to take a look at the ingredients in your typical drugstore mascara. Do you know what all of them are? Another simple test is to ask yourself if you can even pronounce them. Did you pass the test? When in doubt, ask the company, or look up the ingredient on EWG’s Skin Deep database.
In looking for the best natural mascaras, we’ve narrowed down our list to high performing formulas that do without the following harmful ingredients:
Parabens: synthetic preservatives that can mimic estrogen, and have been linked to breast cancer.
Ureas: ureas such as diazolidinyl urea preserve cosmetic products by releasing formaldehyde — a known human carcinogen.
Phthalates: industrial plasticizers used to mix together cosmetic ingredients, making mascara easy to apply. But they’ve been linked to severe hormone disruption.
Dimethicone: Dimethicone is used to achieve a smooth, waterproof finish. It’s hard to get off of lashes afterwards, though, and can lead to brittle lashes — especially if you wear mascara on a daily basis.
Fragrance: The FDA lets companies label any mixture of fragrance ingredients as simply “fragrance” without having to list them all. So even if you’re trying to stay away from phthalates, they might still be in your mascara formula under a disguise.
Animal Testing: Because why should we ever have to subject other living beings to cruelty for our benefit? And the fact that a company would need to test a potentially hazardous ingredient or product on an animal should raise red flags about its safety in the first place.
It’s time to put individuality back into not just our makeup looks, but also in choosing the products we trust our delicate lashes and sensitive eyes with. Natural mascaras are the way to go for gorgeous eyelashes that will last, without the unnecessary eye irritation. What type of mascara do you prefer for your makeup looks?
0 notes
Text
Diet and breast cancer

Breast cancer is the most common cancer in women. Breast cancer is diagnosed in 1 in 8 women and 1 in 5 women under the age of 50. If you're postmenopausal or overweight, you're at a higher risk of breast cancer, so you should be at a healthy weight. For that, you need to eat and exercise that is suitable for your condition. Breast cancer diet is suitable. Finally, we discuss the right or wrong of certain foods and their relationship to breast cancer.
The Importance of a Balanced Diet in Breast Cancer Patients
A healthy diet is important for everyone, but if you have breast cancer, you should be more careful about what you eat. Following a balanced diet during and after breast cancer treatment can greatly help improve patients' quality of life and better control the disease.
The foods we mention can form a balanced diet that prevents the development of breast cancer:
A wide variety of colored fruits and vegetables such as garlic, onions, ginger, soybeans, carrots, cabbage, parsley, capsicum, cabbage family and Moringa (especially the roots of this plant, which of course should be consumed under the supervision of a doctor) Foods rich in fiber such as whole grains, legumes and beans Consumption of low-fat milk and dairy products, preferably probiotics Foods rich in vitamin D Foods, especially spices with anti-inflammatory properties, such as turmeric, which prevent the growth of cancerous cells. Green tea with many antioxidant properties instead of caffeinated drinks Use of organic food and not supplements A study of 91,000 women found that following a diet rich in vegetables (about two-thirds) could reduce the risk of developing breast cancer by 15%. Researchers recommend consuming about 8 to 10 servings of fruits and vegetables a day. Among other properties, fruits and vegetables are rich in carotenoids and flavonoids, which have countless medicinal properties. Proper nutrition to prevent breast cancer Research shows that taking into account the diet you must follow with breast cancer and, of course, the aforementioned fruits and vegetables can prevent breast cancer from occurring. dark leafy vegetables paprika tomato eggplant citrus Carrot broccoli onion apple pear peach strawberry Cabbage family Moringa fiber Fiber's positive effects on the digestive system and support of the elimination process help the body rid itself of toxins and their harmful effects.Whole grains and legumes contain antioxidants that help prevent many diseases. It also contains substances. Nutritionists recommend consuming 30-45 grams of fiber daily. obesity Not all fats are bad, researchers say. Fats in processed foods, trans fats in fried foods, and trans fats in some crackers, candies, and donuts can be threatening. Reduce your consumption of saturated fats found in red meats, solid animal oils and hydrogenated oils and replace them with good fats (unsaturated fats) found in olive oil, avocados, nuts and seeds. In addition, omega-3 fatty acids found in cold-water fish such as salmon and herring help prevent breast cancer. foods harmful to breast cancer alcohol There is strong evidence that alcohol consumption may increase the risk of breast cancer. It's estimated that up to 22% of breast cancers can be prevented by stopping drinking. Researchers have found a direct relationship between regular alcohol consumption and breast cancer. Studies show that alcohol can raise estrogen levels and damage cellular DNA. The researchers also said that women who drank alcohol three times a week had a 15% increased risk of developing breast cancer, and this increased risk increased by 10% for each additional day. sugar Studies in mice have shown that high sugar intake causes tumors in the mammary glands, and these tumors tend to metastasize and spread. Other restricted foods: White bread red meat caffeine Estrogen and plant estrogen sources such as soy Sesame cumin linseed licorice Breast Cancer Nutrition Facts and Myths dairy products and breast cancer In most Asian countries, the incidence of breast cancer is lower than in Western countries. One factor that has received a lot of attention is the consumption and type of dairy products. Some believe that the high consumption of milk and dairy products in Western countries contributes to the high incidence of breast cancer, and that the hormones in milk are to blame. However, the eating habits and lifestyles of Asian women are very different from those of the West. But what does science say about this? Scientific studies have yet to confirm strong evidence for an association between dairy products and breast cancer, and have not shown dairy products to be a possible factor in increasing breast cancer risk. Contrary to popular belief, cows in the EU are less likely to develop breast cancer because they are not injected with hormones to produce their milk and because their milk contains lower levels of natural hormones. soybeans and breast cancer As for soy, there are both claims that soy increases the risk of breast cancer and claims that it lowers the risk. But what does science say about this? Soybeans naturally contain plant compounds based on phytoestrogens, which are structurally similar to the female hormone estrogen. Estrogen can attach to cells of some types of breast cancer (ER-positive) and stimulate them to proliferate. High estrogen levels increase the risk of breast cancer. Therefore, it has been suggested that eating soy as part of the diet may increase estrogen levels in humans, but this is not the case. Interestingly, soy phytoestrogens can prevent estrogen from binding to some breast cancer cells, slowing their growth.The largest population survey in the region was conducted in China. A study conducted at the Shanghai Women's Health Research Center examined the health and dietary intake of soy among more than 70,000 Chinese women. Soybean consumption in China is significantly higher than in the United States. Many Chinese are lactose intolerant, so they are fed milk and soy during childhood. In addition, other types of soybeans such as tofu and edamame are part of the traditional Chinese diet. superfoods and breast cancer You may have seen or heard in the media that certain foods rich in the nutrients your body needs may help reduce cancer. And as far as science goes: The term superfood has no legal definition and cannot be used on food stamps.No single food can meet all of the body's needs. Just because a food can kill cancer cells grown in a bowl in a lab doesn't mean eating too much of that food will protect you from cancer. And even with that settling in, we're naturally depriving our bodies of various nutrients and plant compounds. Binge eaters suffer from diets high in calories, saturated fat, sugar, salt, and alcohol, as well as diets that are overweight and unhealthy. You can't fight a low activity diet. Finally, we concluded that overweight, obesity, menopause, physical inactivity, and alcohol consumption are the main factors that increase the risk of breast cancer. nutrition and genetics Foods have been shown to be harmful or beneficial, depending on what mutations are involved in a person's cancer. For example, coffee may benefit people with BRCA1/2 mutations, depending on the genotype of other genes. Patients with BRCA-associated breast cancer respond well to a diet containing resveratrol I3C DIM and genistein. These substances are found in large amounts in superfoods and you can spot these things with the help of a genetic counselor who is also knowledgeable in the field of nutrition so you can determine what kind of mutation you have. And you can get the right diet according to your physical condition. Read the full article
0 notes
Text
Female Hormones: A Balancing Act

Hormone health is an important topic that can affect everyone throughout their lifetime. Some common symptoms of hormone imbalance are irritability, acne, low libido, unwanted hair growth, unwanted weight gain (especially around the abdomen), uterine fibroids, ovarian cysts, recurrent miscarriage, infertility, endometriosis, and some cancers, to name a few. Hormones can be affected by many things such as stress, diet, chemical exposures, and genetics. Having your hormones in balance, can help you be a healthy, happy, adaptable person.
One hormone that gets a lot of attention is estrogen. Estrogen is a lovely hormone that helps regulate the menstrual cycle, is responsible for breast development, and plays a role in bone health, among others. However, because it generally promotes growth in the body, it can be dangerous if left unchecked. One way to balance estrogen dominance is by increasing progesterone. Another way is to limit exposure to xeno- estrogens in your environment. Lastly, adipose (fat) cells also produce estrogen. So, keeping active and maintaining a healthy weight can benefit your hormones greatly.
A piece of the puzzle with estrogen is also its relationship to another well-known hormone, progesterone. Ideally you want to have 100-200 (some argue 300) times more progesterone than estrogen. So, monitoring this ratio can be pivotal in balancing an estrogen dominance picture. We naturally produce less progesterone as we age. However, there are other factors that can deplete progesterone as well. One known correlation is with cortisol, our stress hormone. If we are always under stress and making cortisol, we steal progesterone from the hormone pool (see hormone cascade below) and end up with progesterone insufficiency. Additionally, as women hit menopause their cardiovascular risk goes up, as does men’s risk. Again, referencing the hormone cascade below, you can see the relationship between progesterone and aldosterone. Dr. Lisa also further details this connection with adrenal health and hypertension in the heart health article within this newsletter. Bio-identical progesterone is one possible treatment to get you feeling better while working on the overarching picture of what lead you here. Lastly, progesterone can also play a big role in fertility and pregnancy maintenance. Low progesterone is one of the most common reasons for first trimester miscarriages. It is also a reason for irregular cycle lengths and spotting.
Testosterone is another famous hormone. Testosterone gets blamed for a lot of negative things, but all humans need testosterone to varying degrees. It is responsible for penis and testes development, facial hair growth, it also helps with muscle size, bone strength, and sex drive. High testosterone is commonly a piece of polycystic ovarian syndrome (PCOS) in women. Within the context of PCOS there are some fantastic herbs that can help lower levels, like stinging nettles. Conversely, low testosterone can be related to stress and cortisol production, through the adrenal endocrine pathway. So, using tools to combat stress and promote your parasympathetic nervous system will support hormone balance as well. One of the most accessible ways to do this is through meditation.
Luckily there are many ways to investigate and support your sex hormones and get you back to feeling active, energetic, and engaged. Here are the easy take away points:
Use an app like Think Dirty to decrease xeno-estrogen and carcinogenic chemicals in your home.
Exercise regularly to combat stress, balance testosterone, and to avoid more estrogen producing fat cells.
Avoid animal proteins that aren’t grass-fed, organic, and free of hormones.
Drink green tea to reduce estrogen levels.
If you have known PCOS, drink nettle tea to help reduce testosterone levels.
Partake in restful, restorative activities to reduce cortisol.
To visit more wellness blogs please, click here.
1 note
·
View note
Text
Breast cancer
Breast cancer is the most common form of cancer among women in industrialised countries, accounting for about 18% of all female cancers. Although mortality is declining in some countries, breast cancer remains the leading cause of death among women aged 35-55 years.
Classical epidemiological studies repeated worldwide have established risk associations with breast cancer. These associations have been bolstered by laboratory tissue and animal studies.
The incidence of breast cancer increases with age. Approximately 50% of breast cancers occur in women aged 50-64 years , and a further 30% occur in women over the age of 70 years. There are also marked geographical variations in incidence; in general, the highest incidences are seen in western countries and the lowest in Asian and African countries. This illustrates the importance of environmental risk factors, as women from low risk countries, such as Japan who emigrate to higher risk countries ultimately develop the higher risk associated with their new country. Genetic factors are also important, however as the natural history of breast cancer appears to vary between populations.
Age is the greatest risk factor for breast cancer. Of the approximately 60% of breast cancers for which identifiable risk factors can be found, age accounts for more than half.
Family History:
The risk of breast cancer is increased 2-3 fold in women with a first degree relative with breast cancer; the risk is also increased, but to a lesser extent, in women with a second degree relative who is affected.
The risk is particularly great if :
The affected relative is on the maternal side of the family
Two first degree relatives are affected
The relative has bilateral breast cancer
The relative’s cancer was diagnosed before the age of 50 years.
Overall about 10-15% of breast cancers are attributable to family history, and half of these can be attributed to specific susceptibility genes
Demography – the risk of breast cancer is increased in women from higher socio economic classes and in women living in urban areas.
The risk of breast cancer is increased in women who being to menstruate at an early age < 12 years or who undergo menopause at a relatively advanced age >55 years. Age at first full term pregnancy appears to be the most important factor in reducing the risk of breast cancer. For women who have their first child before the age of about 25 years, the risk of breast cancer is approximately half that for women who have their first child after 30 years of age, or who remain childless. Similarly, multiparous postmenopausal women have a lower risk of breast cancer than nulliparous women.
Obesity is associated with an increased risk of breast cancer in postmenopausal women. This increased risk may be due to conversion of adrenal androgens to estrogens in adipose tissue. High consumption of animal fats has also been linked to breast cancer.
A recent meta- analysis involving over 150000 women has examined the influence of oral contraceptive use on the risk of breast cancer. The relative risk was slightly increased in women who had used OCs more than 10 years previously. Although the incidence of breast cancer was increased in OC users, the disease mortality remained constant because the cancers tended to be more of a favourable type. This slight increase in risk should, however be viewed in the context of women’s health in general. It is likely that OCs substantially diminish the risk of ovarian and endometrial carcinoma.
They are also highly effective as a form of conception and as a means of relieving menses related morbidity. There is no evidence that current formulations of OCs affect breast cancer risk. However, this will not be known for certain for another 30 years, since the cohort of women who have taken the pill are only now reaching the age at which they are at risk of breast cancer.
The long awaited results of a number of important trials have recently been published, To some extent these studies have confirmed and refined the risk of breast cancer associated with hormone replacement therapy (HRT), but many unanswered questions to be resolved.
The consumption of approximately 15 g or more of alcohol each day increases the risk of breast cancer by about 50%. This may be attributable to reduced hepatic estrogen metabolism. However the increased risk associated with alcohol is small; it has been estimated that if 1000 women over 30 years of age maintained a moderate regular alcohol intake for 2 years one addictional case of breast cancer might develop. This should be set against the potential reduction in ischemic heart disease associated with oderte alcohol consumption and the contribution that alcohol could make to quality of life.
With the rise of modern genetics research, a subcellular and molecular understanding of familial factors in breast cancer is emerging. New technologies have allowed detailed comparisons to be made between the chromosome patterns of normal populations and those at high risk, which meant initially women with very strong family histories.
From these studies, the first genes that were strongly associated with breast cancer were identified notably BRCA1(17q21) and BRCA2 ( 13q14). The risk of breast cancer with these two genes in the absence of family history is high. These genes are implicated in more than 4% of breast cancer and is upto 25% of patients diagnosed before the age of 40 years. They are also linked to ovarian cancers. The breast cancer risk associated with BRCA2 appears less than that with BRCA1, but the presence of the gene mutation carries additional smaller risks of male breast and prostate cancers and perhaps others.
Genes represent predisposition. The internal hormonal and regulatory milieu of the body and life events such as diet, drugs, pregnancies and levels of activity are stimuli in a dynamic homeostatic process. The interaction between predisposition and provocation is when malignancy appears. It is reasonable to hypothesize that genes have an influence beyond susceptibility. Even in these early days there is an evidence that gene expression signatures can predict.
Risk of disease
Relapse and survival risk
Patterns of recurrence
Response to therapy
When these regulatory pathways are better understood, establishing the point at which intervention is necessary will pose a substantial challenge and will profoundly influence our preventive and treatment strategies in the future.
Published Articles by Dr Radheshyam Naik
1)
A Narrative Review of the Association between Pesticides, Organochlorines and Breast Cancer: Current Advances and Research Perspectives
https://clinmedjournals.org/articles/iaphcm/international-archives-of-public-health-and-community-medicine-iaphcm-4-049.php?jid=iaphcm
Genetics and Breast cancer – Oncologist Perspectives
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4809842/
Incidental findings in male breast cancer – A genetic counselling approach
https://www.tandfonline.com/doi/abs/10.1080/09723757.2016.11886287
Landscape of clinically actionable mutations in breast cancer ‘A cohort study’
https://pubmed.ncbi.nlm.nih.gov/33099186/
Simulation model for Breast cancer management in India
https://medicalresearchjournal.org/index.php/GJMR/article/view/2029
0 notes
Text
Yes, drinking milk is actually bad for bone growth.
Feminists, listen up: milk is not only obtained by raping a female cow, stealing and murdering her offspring, and using, abusing and exploiting her body — but it also causes the number one killer of women in America: breast cancer. The three biggest causes of breast cancer are animal protein, fat and estrogen. All three are found in dairy products. Even if you only consume organic dairy products, you are still getting all the fat and animal protein found in cows milk, as well as estrogen. Even organic milk has estrogen — it’s just a lower amount — and it still does damage to your body. It’s time to take a stand against cruelty to females across all species. It’s time to say an emphatic NO to dairy products!
8 notes
·
View notes
Text
Top 10 Reasons You Should Be Choosing Paraben Free Skin Care Products
10 Reasons to Choose Paraben Free Skin Care Products Choosing the right products plays a huge role in your skin's health. Paraben free products can help keep your skin at its healthiest. Here's why.
Paraben Free Products
How would you react to a TV commercial encouraging you to slather your face with chemicals and preservatives every day in the name of beauty? Probably not so well. The truth is that many of your favorite creams, shampoos, and cleansers likely contain parabens - chemical preservatives meant to protect the product from growing mold and bacteria. These chemicals have names like methylparaben, propylparaben, alkyl parahydroxy benzoates, and butylparaben, so they're fairly easy to spot. Parabens are super common, but recent research has indicated that they may act as a xenoestrogen in the body. This means they imitate estrogen, which has been linked in some studies to contribute to hormonal imbalance and the growth of cancer cells. They have also been linked to a number of other unwanted side effects, such as brittle hair and advanced aging. Want to know what to do about it?
Paraben-free - Should you care?
Are you wondering if you have to either give up your beauty routine or run the risk of illness? No! There are an ever-growing number of paraben free products on the market that will keep you looking fabulous while protecting your body. These products offer a myriad of benefits for both you and the planet. Let's take a look at the top 10 benefits you can enjoy when switching to paraben free products.
1. Healthier Body
Some say the data is not conclusive that parabens cause cancer. That being said, 99% of women with breast cancer sampled in a study had
paraben in their tissues
. Men are at risk, too, since paraben use has been linked to both cancer and lower than normal sperm counts in men. Introducing numerous preservatives into our skin each day surely cannot be beneficial. Our bodies are made to self-cleanse and remove toxins through the skin - the bodies' largest organ. Products that contain unfamiliar chemicals, preservatives, fragrances, and dyes have the potential of building up in our tissues. Just as we should watch what we eat, we should pay attention to the ingredients we digest through topical use.
2. Youthful Skin
The same creams sold in stores for their "anti-aging" properties may actually contain a type of paraben that
makes you look older
! Called methylparaben, this deceptive ingredient can cause a reduction in collagen, a protein that makes up a good portion of our connective tissue. Collagen offers
benefits
ranging from the appearance of youthful skin to easing joint pain. Natural alternatives to anti-aging creams include olive oil facial massages, phototherapy lights, steam treatments, drinking plenty of water, and an occasional egg white mask.
3. Avoiding Allergies
Since the 60's, allergic contact dermatitis has been an issue related to the use of parabens in personal products. Symptoms include excessive itching and red, blotchy patches or raised bumps on the skin.
4. Happy Hair
At some point, you have probably pulled a bottle of your "backup" shampoo out from under the bathroom sink when your favorite brand ran out. Even if it had been there for a questionable amount of time, it probably remained free of mold because of parabens. Is the ability to keep beauty products for unusually long periods of time worth the risk, though? Just as with your skin, paraben free products are better for your hair. Parabens can cause scalp irritations, and studies have shown that the use of parabens in shampoos and other beauty products result in blood and urine samples containing the preservatives after use.
5. Helping Mama Earth
It probably comes as no surprise that parabens take a toll on the planet. When we rinse our products off at the end of the day, the water carries the residue of our products into the larger water supply - and eventually the ocean. Marine animals harboring parabens in their tissues have been discovered, which has prompted scientists and environmentalists to wonder if hormonal disruptions in sea creatures could affect their overall health. Land mammals are no exception - polar bears, sea lions, and marine animals have all been found to carry these synthetic parabens in their tissues. This is not a minor consequence. It can be argued that every product we use has the potential to impact the balance of nature. The health of your hair does not need to be sacrificed to the health of the world's oceans. By choosing paraben free products for your hair, you are serving the welfare of the environment and the animals who rely on its protection.
6. The Paraben Free Products Butterfly Effect
Have you heard the whole thing about how it takes 21 days to form a new habit? After just a few weeks of reading the labels on beauty products, you may be inclined to start proactively researching ingredients in other products you use - such as toothpaste, food, supplements, and beverages. You might be shocked at what you find: Additives, artificial dyes, chemical sweeteners, and fillers abound in nearly everything in a package meant for consumption or application. Luckily, there are numerous companies and stores that now cater to people looking for paraben free products, organic food, and natural alternatives. By changing just one habit, you may find yourself making healthier choices in multiple areas of your life.
7. Spending Less
As you become more conscientious of the products you buy, you will likely start noticing that you need less than you ever imagined. One of the great benefits of paraben free products is you may stop purchasing extra items with paraben (cream for irritated skin, for example) to resolve an issue caused by - yep - paraben!
8. Supporting Sustainable Products
Think about sustainability as a cool byproduct of the butterfly effect discussed above. Companies that care about what goes into their packaging probably put thought into the actual packaging. Here's an example: If you've ever used a facial scrub with micro-beads, you were most likely massaging tiny plastic beads into your skin. When those go down the drain, they become part of the
eight million tons of plastic
TRASH that enters the oceans every year. Yeah, it adds up fast. It's probably safe to assume that producers who replace the plastic beads in the name of sustainability will probably use recycle-able, recycled, or biodegradable packaging for their products. The paraben free products movement is not an isolated practice. Rather, it's part of an overall strategy to support sustainable products for the health of our bodies and planet. That being said, the latest
trends
and products in the world of sustainable beauty are growing every day, so lack of selection will no longer leave you disappointed.
9. Better for Babies
Checking baby shampoo for parabens, for all the reasons listed above, is a good idea. If scientists don't yet understand possible ramifications of life-long use of these xenoestrogens, why risk it?
10. Feeling Fantastic
Again, we don't know the extent to which parabens affect our health, but evidence certainly points to the side that says they do. The biggest benefit of paraben free products may be the fantastic feeling one gets when realizing they largely have control over what goes in and on their bodies.
Last Word
It's time to feel fantastic (and knowledgeable) about the products you buy! To get started, simply look at what you already have in your own home. Replacing items one by one until you figure out the best
healthy regimen
for your needs is likely going to be much easier - and fun - than you anticipated. Welcome to the world of paraben free products! Read full story: https://www.clarityrx.com/blogs/beauty-and-skincare/top-10-reasons-choosing-paraben-free-skin-care-products
1 note
·
View note
Text
Alfalfa
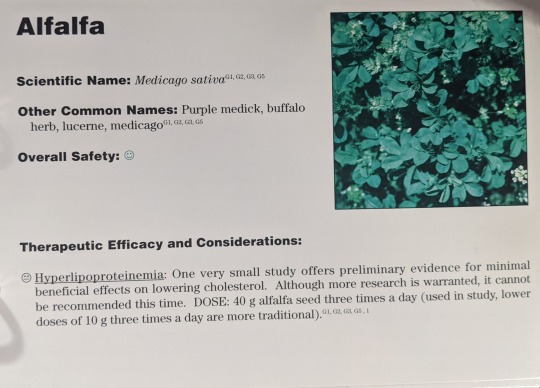
Scientific Names: Medicago sativa Other Common Names: Purple medick, buffalo herb, lucerne, medicago Overall Safety: 😊
Therapeutic Efficacy and Considerations: Hyperlipoproteinemia: 😐 One very small study offers preliminary evidence for minimal beneficial effects on lowering cholesterol. Although more research is warranted, it cannot be recommended at this time. Dose: 40 g alfalfa seed three times a day (used in study, lower doses of 10 g three times a day are more traditional).
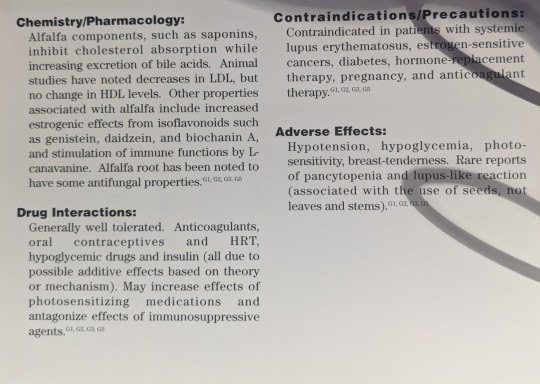
Chemistry/Pharmacology: Alfalfa components, such as saponins, inhibit cholesterol absorption while increasing excretion of bile acids. Animal studies have noted decreases in LDL, but no change in HDL levels. Other properties associated with alfalfa include increased estrogenic effects from isoflavonoids such as genistein, daidzein, and biochanin A, and stimulation of immune functions by L-canavanine. Alfalfa root has been noted to have some antifungal properties.
Drug Interactions: Generally, well tolerated. Anticoagulants, oral contraceptives and HRT, hypoglycemic drugs and insulin (all due to possible additive effects based on theory or mechanism). May increase effects of photosensitizing medications and antagonize effects of immunosuppressive agents.
Contraindications/Precautions: Contraindicated in patients with systemic lupus erythematosus, estrogen-sensitive cancers, diabetes, hormone-replacement therapy, pregnancy, and anticoagulant therapy.
Adverse Effects: Hypotension, hypoglycemia, photosensitivity, breast tenderness. Rare reports of pancytopenia and lupus-like reaction (associated with the use of seeds, not leaves and stems).
2 notes
·
View notes