#Vascular ulcers
Explore tagged Tumblr posts
Text
Balaji Hospital | Laparoscopic Surgery for Faster Recovery
Balaji Hospital’s laparoscopic surgery offers minimally invasive procedures that prioritize patient safety and comfort, leading to quicker recovery and less downtime.

#Laproscopic Surgery#Surgery for Crohn’s disease#Ulcerative colitis#Radiologist#Vascular radiology#Periodical medical examinations#First aid training programs#Intensive Care Medicine#Health awareness programs#Guj.Factory rules#Work of H.I.R.A#Vadodara
0 notes
Text
Arterial vs Venous Ulcers: Key Differences You Must Know

Confused about arterial vs venous ulcers? While venous ulcers result from poor vein circulation, arterial ulcers stem from restricted blood flow. Early diagnosis by a specialized vascular surgeon is key to effective leg ulcer treatment. Learn the key differences and treatment options.
#specialized vascular surgeon#leg ulcer treatment#arterial vs venous ulcers#Venous ulcers#arterial ulcers
0 notes
Text
Best Vascular Surgeon in Nellore: Comprehensive Guide to Treatments and Expertise
Vascular health is a crucial aspect of overall well-being. Without proper vascular function, our organs and tissues can't receive the oxygen and nutrients they need. This is where the expertise of a skilled vascular surgeon becomes invaluable. In Nellore, Dr. Narendranadh Meda stands out as a leading vascular and endovascular surgeon, offering a wide range of advanced treatments for various vascular conditions. With a team dedicated to excellence and compassionate care, they are committed to providing top-notch medical services to their patients.
Glue Treatment for Varicose Veins in Nellore
What is Glue Treatment?
Glue treatment, also known as cyanoacrylate adhesive treatment, is a minimally invasive procedure used to treat varicose veins. This technique involves the use of a special medical adhesive to seal off the affected veins, redirecting blood flow to healthier veins.
Benefits of Glue Treatment
Minimally Invasive: No need for surgery or large incisions.
Quick Recovery: Patients can resume normal activities shortly after the procedure.
Effective Results: Significant reduction in varicose vein symptoms.
Procedure Overview
The procedure begins with the application of local anesthesia. A catheter is then inserted into the varicose vein, through which the medical adhesive is delivered. The adhesive seals the vein shut, and the body naturally reroutes blood through healthier veins. The entire process is quick, typically taking less than an hour.
Laser Treatment for Varicose Veins in Nellore
What is Laser Treatment?
Laser treatment for varicose veins uses focused light energy to heat and close off the problematic veins. This method is known as endovenous laser treatment (EVLT) and is highly effective for treating larger varicose veins.
Advantages of Laser Treatment
Precision: Targets only the affected veins, leaving surrounding tissues unharmed.
Minimal Discomfort: Performed under local anesthesia with little to no pain.
High Success Rate: Long-lasting results with minimal risk of recurrence.
How Laser Treatment is Performed
During EVLT, a small laser fiber is inserted into the vein through a catheter. The laser energy heats and seals the vein from within, causing it to collapse and gradually be absorbed by the body. The procedure is typically completed in about an hour, and patients can walk immediately afterward.
Peripheral Artery Bypass Treatment in Nellore
Understanding Peripheral Artery Disease
Peripheral artery disease (PAD) occurs when the arteries that supply blood to the limbs become narrowed or blocked due to plaque buildup. This can lead to pain, mobility issues, and even severe complications if left untreated.
When is Bypass Needed?
Peripheral artery bypass surgery is recommended when less invasive treatments, such as medication or angioplasty, are not effective. Bypass surgery creates a new route around the blocked artery, restoring proper blood flow to the affected limb.
Procedure and Recovery
The surgery involves using a graft, either from the patient's own vein or a synthetic material, to bypass the blocked section of the artery. Recovery typically involves a hospital stay of a few days, followed by several weeks of gradual rehabilitation to regain strength and mobility.
Aortic Aneurysm Center in Nellore
What is an Aortic Aneurysm?
An aortic aneurysm is an abnormal bulge in the wall of the aorta, the largest artery in the body. If an aneurysm ruptures, it can cause life-threatening bleeding.
Importance of Specialized Care
Treating aortic aneurysms requires specialized expertise due to the complexity and risks involved. Early detection and intervention are crucial for preventing rupture and ensuring the best outcomes.
Treatment Options Available
Endovascular Repair: A minimally invasive procedure where a stent graft is placed inside the aorta to reinforce the weakened area.
Open Surgical Repair: Involves removing the damaged section of the aorta and replacing it with a synthetic graft.
Diabetic Foot Treatment in Nellore
Challenges of Diabetic Foot Conditions
Diabetic foot conditions, including neuropathy and poor circulation, can lead to serious complications like ulcers and infections. Managing these conditions requires a comprehensive and proactive approach.
Comprehensive Treatment Approaches
Regular Monitoring: Frequent check-ups to catch issues early.
Foot Care Education: Teaching patients proper foot care techniques.
Advanced Wound Care: Using the latest methods to treat and heal foot ulcers.
Preventative Measures
Proper Footwear: Ensuring shoes fit well and provide adequate support.
Daily Inspections: Checking feet daily for cuts, blisters, or signs of infection.
Blood Sugar Control: Maintaining stable blood sugar levels to prevent complications.
Day Care Surgeries in Nellore
What are Day Care Surgeries?
Day care surgeries, also known as outpatient surgeries, are procedures that do not require an overnight hospital stay. Patients can return home the same day after their surgery.
Benefits of Day Care Procedures
Convenience: Reduced hospital stay time.
Cost-Effective: Lower costs compared to inpatient surgeries.
Quick Recovery: Patients can recover in the comfort of their own homes.
Common Day Care Surgeries Offered
Varicose Vein Treatments: Including both laser and glue treatments.
Minor Vascular Procedures: Such as fistula creation for dialysis.
Diabetic Foot Ulcers Treatment in Nellore
Causes and Risks of Diabetic Foot Ulcers
Diabetic foot ulcers are open sores that occur in people with diabetes due to poor circulation and nerve damage. These ulcers can become infected and lead to serious complications if not treated promptly.
Treatment Options
Debridement: Removing dead or infected tissue to promote healing.
Advanced Dressings: Specialized wound dressings to protect the ulcer and aid in healing.
Hyperbaric Oxygen Therapy: Enhancing oxygen supply to the wound to accelerate healing.
Importance of Early Intervention
Early detection and treatment of diabetic foot ulcers are essential to prevent infections and other complications. Regular foot check-ups and immediate medical attention at the first sign of an ulcer can make a significant difference in outcomes.

DVT Management Treatment in Nellore
Understanding Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, usually in the legs. This condition can cause pain, swelling, and serious complications like pulmonary embolism if the clot travels to the lungs.
Symptoms and Risks
Symptoms: Swelling, pain, redness, and warmth in the affected leg.
Risks: Prolonged immobility, surgery, certain medications, and genetic factors.
Treatment and Management Strategies
Anticoagulants: Medications to prevent further clotting.
Compression Stockings: To reduce swelling and improve blood flow.
Lifestyle Changes: Including regular exercise and avoiding long periods of immobility.
for more info:
#hyderabadvascularcenter#vascularsurgery#varicoseveintreatment#stoptheclot#hvc#deepveinthrombosis#varicoseveins#vascular#venousthromboembolism#diabeticneuropathy#diabeticfootcare#diabetic foot pain#diabetic foot ulcer#dvtawareness#dvttreatment#dvtprevention
0 notes
Text
#vascular surgeon pakistan#vascular surgeon islamabad#best surgeon#surgeonazeemagha#surgeon azeem agha#vascular surgery services#islamabad#pakistan#diabetic foot ulcer#diabetic#diabetic foot treatment#vascular access#kidney dialysis#hemodialysis and peritoneal dialysis market#dialysis fistula#varicose veins#varicoseveintreatment#vascular surgery#surgery#abdominal aortic aneurysm#aortic stenosis#aortic dissection#leg pain#claudication#leg swelling#dilated veins#artery#veins#sexualwellness#erectile dysfunction
0 notes
Text
Diabetic Sores on Legs: A Comprehensive Exploration of Complications and Treatments
Discover in-depth insights into the complexities of diabetic sores on legs, also known as diabetic ulcers, and foot-related complications associated with diabetes. Unravel the multifaceted causes, symptoms, and highly effective treatment approaches meticulously detailed in this all-encompassing article on diabetic wound care, prevention, and management. Introduction The global impact of…

View On WordPress
#amputation prevention#blood sugar management#chronic wounds#Diabetes#Diabetes complications#diabetic wounds#Foot ulcers#glycemic control#Healthcare provider#hyperglycemia#infection prevention#medical care#neuropathy#patient education#pressure sores#skin care#ulcer treatment#vascular disease#wound care#wound healing
0 notes
Text

Day 27/100 days of productivity
Vascular surgery - Deep Vein Thrombosis, Thrombophlebitis, Venous Ulcers
Finished reading Adultery by Paulo Coelho and I really liked it (thanks to @meddstudent for letting me borrow it 🤍)
#mine#studyblr#study blog#med studyblr#studyinspo#medical studyblr#study aesthetic#med school#studyspo#study#study hard#coffee shop#coffee#study space#medical study#study motivation#med student#realistic studyblr#study tips#studyblr community#studygram#studyspiration#booklover
105 notes
·
View notes
Text

Risk for Rupture
CT scan study finds an increased risk of diseases in the wall of the aorta [the body's largest and central artery] called aortic pseudoaneurysm and penetrating aortic ulcer in individuals with aortic calcification, which causes narrowing
Read the published research article here
Image from work by Siting Li and Haoxuan Kan, and colleagues
Department of Vascular Surgery, Department of State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Scientific Reports, January 2024
You can also follow BPoD on Instagram, Twitter and Facebook
16 notes
·
View notes
Text
do you have migraines or headaches, and are you poor, have shitty/no insurance, doctors who won't listen to you, or just don't want to waste hundreds of dollars on an appointment? well, i went to a neurologist and received this piece of paper which i probably paid way too much for, so you can have it for free.
American Headache Society Complementary and Integrative Medicine Section: Patient Education Kit for Migraine (Recommended Supplements for Migraine Prevention) <- link
the supplements may or may not work, but either way this should save you time and money. you can buy these supplements at most drug stores or online.
below the cut i'm adding a transcript of the pdf in case the link breaks.
stuff my doctor told me:
i should take magnesium glycinate, riboflavin, and CoQ10
magnesium glycinate should be taken at bedtime
didn't recommend feverfew for me, can't remember why
if these supplements don't help, the next step is prescription meds which include Nortriptyline, Topamax, or Emgality
Nortriptyline is an anti-depressant, if you're already on an anti-depressant then don't take this
Topamax is an anti-seizure med also used to prevent migraines. it can make birth control pills less effective
Emgality is administered once a month with a self-administered shot (something like an epi pen). this is what my doctor recommended I take if the supplements don't work. it specifically targets the migraine receptor, so it has very few side effects
PDF transcript:
AHS Complementary and Integrative Medicine Section: Patient Education Kit for Migraine
Recommended Supplements for Migraine Prevention Dietary supplements are commonly used for the prevention of migraine. The recommended supplements have all been studied and found to be effective in the prevention of migraine. If you are pregnant or have other medical conditions, please check with your physician about whether you should take these.
Magnesium
Mechanism: Important in energy production, muscle and nerve function, and may play a role in cortical spreading depression, which is an underlying migraine mechanism.
Evidence: Two large randomized controlled trials found magnesium to be beneficial for migraine prevention.
Dose: 600mg per day. Some people prefer to start at a lower dose to ensure tolerability. Formulations include magnesium oxide, magnesium sulfate, magnesium citrate (better absorbed than oxide or sulfate), and magnesium glycinate (less likely to cause diarrhea than other formulations)
Side effects: May cause soft stools or diarrhea, but could help constipation.
Riboflavin (Vitamin B2)
Mechanism: Involved in mitochondrial energy production, which may play a role in migraine
Evidence: Five clinical trials, including one large randomized controlled trial, have shown positive effect on migraine.
Dose: 400mg per day
Side effects: Turns urine bright yellow/orange and may cause diarrhea.
Feverfew
Mechanism: Parthenolide, the active ingredient, may prevent migraine through its vascular smooth relaxation and anti-inflammatory properties.
Evidence: Four out of six studies showed benefit for migraine prevention
Dose: 50-300mg twice daily
Side effects: Nausea, bloating, and mouth ulcers. Feverfew can cause uterine contractions and is not recommended during pregnancy.
Coenzyme Q10 (CoQ10)
Mechanism: Involved in energy production and helps maintain mitochondrial integrity.
Evidence: Two randomized controlled trials showed benefit over placebo.
Dose: 300mg daily (can be split into 150mg twice a day)
Side effects: Insomnia, fatigue, nausea, or diarrhea.
Other Supplements Butterbur demonstrated benefit for migraine in two large randomized controlled studies; however; preparations may contain pyrrolizidine alkaloids which are toxic to the liver. Due to safety concerns, butterbur was removed from the market in Europe and is currently not recommended. Melatonin and the combination of folic acid/B6/B12 have mixed results for migraine prevention.
Reference: Rajapakse T, Pringsheim T. Nutraceuticals in migraine: A summary of existing guidelines for use. Headache. 2016;56(4).
4 notes
·
View notes
Text
*DR. SMITA GOEL HOMEOPATHY CLINIC*
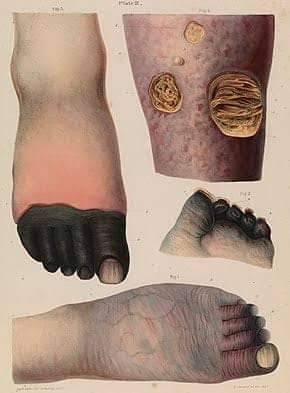
Gangrene is a term that describes dead or dying body tissue(s) that occurs because the local blood supply to the tissue is either lost or is inadequate to keep the tissue alive. Gangrene has been recognized as a localized area of tissue death since ancient times.
There are two major types of gangrene, referred to as dry and wet. Many cases of dry gangrene are not infected. All cases of wet gangrene are considered to be infected, almost always by bacteria. Mainly both wet and dry gangrene to occur are the digits (fingers and toes) and other extremities (hands, arms, feet, and legs).
Symptoms and Signs
Its depends on the type of gangrene, the location of the gangrene (internal organs, skin, extremity, etc.), and how much the gangrene has progressed.
In dry gangrene, the skin is hard and black or purplish. In earlier stages, the skin may be pale and either numb or painful.
In wet gangrene, the affected area will be swollen with blisters oozing fluid; and the area may be red and warm with a foul odor.
Gas gangrene causes severe pain, fever, and the skin will crackle like bubble wrap when pressed.
Fournier's gangrene will cause redness and swelling in the genital area. Patients with gangrene affecting internal organs such as the gallbladder or intestines will typically be very sick with fever, low blood pressure, and severe pain.
Wet gangrene (also termed moist gangrene) is the most dangerous type of gangrene because if it is left untreated, the patient usually develops sepsis and dies within a few hours or days. Wet gangrene results from an untreated (or inadequately treated) infection in the body where the local blood supply has been reduced or stopped by tissue swelling, gas production in tissue, bacterial toxins, or all of these factors in combination. Additionally, conditions that compromise the blood flow such as burns or vascular trauma (for example, a knife wound that cuts off arterial flow) can occur first. Then the locally compromised body part or area becomes infected, which can result in wet gangrene. Wet gangrene is the type that is most commonly thought of when the term gangrene is used. Wet gangrene often produces an oozing fluid or pus, hence the term "wet." Early stages of wet gangrene may include:
• Signs of infection
• Aching pain with swelling
• A reddish skin color or blanched appearance if the area is raised above level of the heart
• Coolness on the skin surface
• Ulceration
• A crackly sensation when the skin is pressed due to gas in the tissue
These stages may progress rapidly over hours to days
Dry gangrene, if it does not become infected and progress to wet gangrene, usually does not cause sepsis or death. However, it can result in local tissue death with the tissue eventually being sloughed off. Usually, the progression of dry gangrene is much slower (days to months) than wet gangrene because the vascular compromise slowly develops due to the progression of diseases that can result in local arterial blockage over time.
The stages are similar to wet gangrene (see above), except there is no infection, pus, wetness, or crackly-feeling skin, because there is no gas production in the uninfected tissue. Disease-fighting cells are not recruited to the area.
There are many diseases that may lead to dry gangrene; the most common are:
• Diabetes
• Arteriosclerosis
• Tobacco addiction (smoking)
Infrequently, dry gangrene can occur quickly, over a few hours to days, when a rapid arterial blockage occurs in part of the body (for example, an arterial blood clot suddenly occludes a small artery to a toe). Dry gangrene often produces cool, dry, and discolored appendages (sometimes termed "mummified") with no oozing fluid or pus, hence the term "dry."
The common cause of either wet or dry gangrene is loss of an effective local blood supply to any tissue. Loss of the blood supply means tissues are deprived of oxygen, thus causing the cells in the tissue to die. The most common causes of tissue blood supply loss and major risk factors for gangrene are:
• Infections
• Trauma
• Poor wound healing
• Diseases like diabetes mellitus that can affect blood vessels (usually arteries)
Rarely, Raynaud's disease can lead to gangrene of fingers and toes.
Dry gangrene causes
Dry gangrene can result from any of a number of diseases or mechanisms that can reduce or block arterial blood flow. Although the most common diseases that can cause dry gangrene are diabetes, arteriosclerosis, and tobacco addiction, there are many other lesser-known diseases that can lead to this problem. For example, some autoimmune diseases that attack blood vessels (vasculitis syndromes) may result in enough damage to cause dry gangrene. In other cases, dry gangrene can result from various external mechanisms such as burns, frostbite, and arterial trauma caused by accidents, wounds, or surgery.
Causes
Wet gangrene can result from all the causes listed above for dry gangrene but always includes infection. In some cases of wet gangrene, the initial cause is considered to be the infection. Although many types of organisms (mainly bacteria) are known to participate in wet gangrene infections, the classic bacterial organism or bacterial infection associated with wet gangrene is Clostridium perfringens, an anaerobic bacterium that grows best when oxygen is not present. These bacteria can cause myonecrosis (muscle fiber death) with exotoxins and produce gas bubbles in the dead and dying tissues (gas gangrene). This leads to localized swelling with compression and loss of blood flow to tissue, allowing bacteria to extend the infection to the connective tissue of muscle, skin, and other areas, causing necrotizing fasciitis (death of connective tissue). Necrotizing fasciitis, in turn, allows the infection to spread, frequently with speed, out of the locally infected site to adjacent areas or to the bloodstream (sepsis). Although this cascade of events is seen with Clostridium perfringens often as the single infecting organism type, it can be caused by many other organisms such as Streptococcus, Staphylococcus, Bacteroides, and Escherichia. Usually two or more of these organisms occur in the infection, and many investigators suggest that together the organisms help each other (synergy) to extend the infection.
There are several subtypes of wet gangrene:
• Gas gangrene means gas is present in the gangrenous tissue as described above.
• Fournier's gangrene is gangrene with necrotizing fasciitis that occurs mainly in male genitalia.
• Internal gangrene is a general term that means gangrene is affecting an internal organ. Internal gangrene types are usually named after the organ that is affected (for example, gangrene of the appendix, gangrenous gallbladder, and gangrenous bowel involving the colon, rectum, or other areas).
Leprosy (Hansen's disease) is not a variant of wet or dry gangrene, although it can result in local tissue loss that can resemble gangrene. It is a disease caused by bacteria that are transferred usually from person to person. It causes nodules and sores. M. leprae infection slowly destroys peripheral nerve endings in digits and mucous membranes over a period of years with loss of sensation. Digits and other local areas get repeatedly injured due to sensation loss and can become mutilated or develop atrophy and be sloughed off. However, if the chronic lesions become infected with other organisms, wet gangrene can develop in patients with leprosy.
www.thehomeopathyclinic.co.in
#greater noida#best homeo clinic in indirapuram#homeopathy doctor#homeopathy clinics#ghaziabad#best skin doctor in ghaziabad#homeopathy#homeopathy cold treatment in indirapuram#homeopathy for ibs#homeopathy medicine#best homeopathy clinic in indirapuram#best homeopathy doctor#homeopathy skin allergies treatment in indirapuram#homeopathy skin allergies treatment in noida#homeopathy specialist in indirapuram#homeopathy treatment#laser treatment in indirapuram#ghaziabad latest news#ghaziabadnews#child doctor in noida#child specialist in noida#noida news#noida#ayurvedic doctor in ghaziabad#skin specialist in indirapuram#indirapuram#wave city ghaziabad#delhigram#delhifood#east delhi
2 notes
·
View notes
Text
more fascinating shit: there seems to b a definete correlation between your blood type and disease risk. for type a, stomach and pancreas cancer seem to be 20-30% (compared to o) more likely. type o seems 70-90% more likely to develop certain kinds of ulcers and more sensitive to stomach bacteria. type b seems 11-20% more likely to develop,,, fuck i forgot what kind of cancer. type o seems to generally b protective against the development of cancer, but may make one more susceptible to some diseases such as the pleague. type o shows malaria resistence, while type b reacts particularly badly w malaria. type a is also associated w more heart and vascular issues
3 notes
·
View notes
Text
About Vadodara City | Explore Vadodara with Balaji Hospital
Discover Vadodara’s rich history, culture, and attractions. Learn about the city's heritage, tourist spots, and essential travel information with Balaji Hospital.

#Endocrinologist#Best treatment for ear#nose & throat diseases#ENT#Bariatric Surgery#Solid Organ Transplantation#Pediatric Surgery#Thoracic Surgery#Vascular Surgery#General Surgery#Community gynecology#Materno-fetal medicine#Gynecology and Obstetrics#Infectious diseases#Infectious Disease Specialist#Surgery for Crohn’s disease#Ulcerative colitis#Diverticulitis#Cancer#Rectal prolapsed#Severe constipation#Laproscopic Surgery#Medicine and Critical Care#Intensive Care Medicine#Neurophysician#Neurosurgeon#Complete cancer care#Onco Physician#Multi disciplinary treatment to rehabilitation#Onco Surgery
0 notes
Text

With the rise of diabetes in India, it is essential to foster awareness about related conditions such as diabetic foot problems and ulcers. Dr. Sumit Kapadia brings expertise in diabetic wound care & shares crucial insights about this often neglected condition.
#Varicose Veins Treatment Doctor#Veins Specialist Doctor#Vascular Surgeon Near Me#Endovascular Surgery#Laser Varicose Vein Surgery#Varicose Ulcer Treatment#Treatment For Leg Ulcers#Leg Ulcers Types#Leg Ulcers Treatment
0 notes
Text
Varicose Vein treatment in Kakinada
At our modern facility in Kakinada, we prioritize patient comfort and convenience, offering a welcoming and comfortable environment that is designed to put you at ease. We take a patient-centered approach to care, working closely with each individual to develop a customized treatment plan that meets their unique needs and goals.
Treatment:
Glue Treatment For Varicose Veins in Kakinada Glue Treatment For Varicose Veins: Glue treatment, also known as VenaSeal, is a minimally invasive treatment for varicose veins. It involves the use of a medical adhesive, which is injected into the affected vein. The glue seals the vein, and blood is rerouted to healthier veins. The procedure is painless and requires no anesthesia.
Laser Treatment For Varicose Veins in Kakinada Laser Treatment For Varicose Veins:Laser treatment is another minimally invasive procedure used to treat varicose veins. It involves the use of a laser to heat and seal the affected vein, causing it to collapse and eventually fade away. The procedure is performed under local anesthesia, and most patients can return to normal activities within a day.
Microsclerotherapy Treatment in Kakinada Microsclerotherapy for Cosmetic Purpose:Microsclerotherapy is a cosmetic treatment used to remove spider veins or small varicose veins. It involves the injection of a sclerosing agent directly into the affected vein, causing it to collapse and fade away. The procedure is minimally invasive and requires no anesthesia.
Peripheral Artery Bypass Treatment in Kakinada Peripheral Artery Bypass/Angioplasty/Stenting:Peripheral artery bypass, angioplasty, and stenting are procedures used to treat peripheral artery disease. They involve the use of a catheter to insert a balloon or stent into the blocked artery, allowing blood flow to be restored. The procedure is performed under local anesthesia and requires a short hospital stay.

Aortic Aneurysm Treatment in Kakinada Aortic Aneurysm Stenting/Open Surgery:Aortic aneurysm stenting and open surgery are procedures used to treat an aneurysm in the aorta. Stenting involves the insertion of a stent into the weakened section of the artery to support and reinforce it. Open surgery involves the surgical repair or replacement of the damaged portion of the artery. The procedure requires general anesthesia and a hospital stay.
Diabetic Foot Treatment in Kakinada Diabetic Foot / Podiatric Surgery:Diabetic foot and podiatric surgery are procedures used to treat foot problems related to diabetes. They involve the removal of damaged tissue, the correction of deformities, and the treatment of infections. The procedures may be performed under local or general anesthesia, depending on the complexity of the surgery.
Day Care Surgeries in Kakinada Day Care Surgeries:Day care surgeries are minor procedures that can be performed in an outpatient setting. They include procedures such as skin biopsies, mole removal, and minor laceration repairs. The procedures are performed under local anesthesia and patients can return home the same day.
Varicose vein treatment by Endovenous Ablation in Kakinada Varicose vein treatment by Endovenous Ablation: Our clinic offers a minimally invasive treatment option for varicose veins known as endovenous ablation. This treatment is performed using a laser or radiofrequency energy to heat and close the affected veins, allowing blood to reroute through healthier veins. The procedure is quick, effective, and virtually painless with no scarring, allowing patients to return to their daily activities almost immediately.
Diabetic foot ulcers Treatment in Kakinada Diabetic foot ulcers and Non-healing ulcer Management: Our clinic specializes in the management of diabetic foot ulcers and non-healing ulcers. Our expert team of vascular surgeons offers comprehensive treatment options to promote wound healing and prevent further complications. We use a multidisciplinary approach, including wound care, offloading, infection control, and vascular interventions to help patients recover quickly.
Peripheral bypasses Treatment in Kakinada Peripheral bypasses, DVT management: We offer advanced treatment options for peripheral arterial disease and deep vein thrombosis. Peripheral bypass surgery involves redirecting blood flow around a blocked artery using a graft, and we provide expert care for this procedure. Our team also offers specialized care for deep vein thrombosis, including anticoagulation therapy, compression stockings, and thrombectomy if necessary.
Aortic Aneurysm Treatment in Kakinada Aortic Aneurysm Endovascular repair: Our clinic provides endovascular repair for aortic aneurysms, a less invasive alternative to traditional open surgery. The procedure involves inserting a stent-graft through a small incision, allowing us to repair the aneurysm without major surgery. This procedure offers faster recovery times, less pain, and fewer complications than traditional open surgery.
#varicoseveins#vascularsurgery#aortic dissection#aorticaneurysmawareness#vascular#varicoseveintreatment#hvc#stoptheclot#deepveinthrombosis#venousthromboembolism#aortichealth#aortic stenosis#diabeticfootclinic#diabetic foot ulcer#hyderabadvascularcenter#diabetic foot infection#diabetic foot treatment#dvtawareness
0 notes
Text
Diabetic Sores on Legs and Related Conditions: A Comprehensive Exploration
Diabetes, a pervasive and enduring medical condition affecting millions of individuals globally, presents a constellation of complex complications. Among these, diabetic sores on legs, colloquially known as diabetic foot ulcers, stand out as a formidable challenge. The genesis of these sores intertwines with multifarious factors, encompassing compromised blood circulation, neuropathy-induced…

View On WordPress
#amputation prevention#blood sugar management#chronic wounds#Diabetes#Diabetes complications#diabetic wounds#Foot ulcers#glycemic control#Healthcare provider#hyperglycemia#infection prevention#medical care#neuropathy#patient education#pressure sores#skin care#ulcer treatment#vascular disease#wound care#wound healing
0 notes
Text
Next-Gen Compression Therapy Devices: Innovations Shaping the Future of Patient Care
The global compression therapy devices market is undergoing a significant transformation, driven by a convergence of healthcare demands, technological innovation, and an aging global population. As the prevalence of chronic venous disorders, lymphedema, and deep vein thrombosis (DVT) continues to rise, compression therapy is increasingly recognized as a vital component in non-invasive treatment protocols across the globe.
Compression therapy—characterized by the application of controlled pressure to limbs using garments or mechanical systems—is gaining traction for its effectiveness in improving blood flow, reducing swelling, and managing various vascular conditions. The market for these devices is experiencing robust interest from medical practitioners, patients, and healthcare systems looking for cost-effective, scalable, and clinically validated solutions to manage chronic circulatory and lymphatic disorders.

Market Dynamics and Drivers
The steady expansion of the compression therapy devices market is being shaped by several critical drivers. One of the most notable is the growing incidence of venous leg ulcers, varicose veins, and chronic venous insufficiency. These conditions are increasingly prevalent, particularly among aging populations and individuals with sedentary lifestyles or occupations that involve prolonged standing.
Moreover, the post-operative rehabilitation segment is witnessing a surge in demand for compression products. Surgeons and physiotherapists are incorporating these devices into recovery regimens to reduce the risk of complications such as DVT, enhance mobility, and support faster healing.
Another driving force is the growing awareness among patients and healthcare providers regarding the benefits of early intervention using compression therapy. Health campaigns, digital outreach, and clinical education are improving patient compliance and helping overcome historical challenges such as discomfort and lack of knowledge about proper usage.
Technological Advancements Fuel Innovation
Innovation remains a central theme in the evolution of compression therapy devices. The market has seen a notable shift from traditional compression bandages to more advanced technologies such as adjustable compression wraps, intermittent pneumatic compression (IPC) devices, and smart wearable compression systems.
These newer devices offer superior ease-of-use, comfort, and adherence to therapeutic protocols. Some models now incorporate sensor technologies and Bluetooth connectivity, allowing patients and clinicians to monitor therapy progress in real-time. This integration of digital health tools is not only improving patient outcomes but also helping healthcare providers make more informed decisions regarding treatment adjustments.
Additionally, manufacturers are exploring the development of lightweight, breathable materials and ergonomically designed products that increase comfort without compromising on therapeutic efficacy. These innovations are particularly beneficial for elderly and long-term care patients who require consistent use of compression products.
Growing Adoption Across Key Regions
Geographically, the compression therapy devices market is witnessing widespread adoption across North America, Europe, Asia-Pacific, and other emerging economies. In North America, established healthcare infrastructure, higher levels of awareness, and strong insurance coverage contribute to widespread utilization.
Europe, with its large elderly population and strong emphasis on preventive care, remains a significant market for compression solutions. Several European countries have implemented national guidelines and reimbursement policies that support the use of compression therapy in treating vascular and lymphatic conditions.
Meanwhile, the Asia-Pacific region is emerging as a rapidly growing market, spurred by increasing healthcare investments, expanding middle-class demographics, and greater access to medical technology. Countries like China, India, and South Korea are witnessing rising demand for non-invasive treatment options and are investing in local manufacturing and distribution networks to meet this need.
Challenges and Barriers to Market Expansion
Despite the positive momentum, the compression therapy devices market faces several challenges that could impact future growth. Chief among these is patient adherence. The therapeutic benefits of compression therapy often depend on consistent and proper usage, which can be hindered by discomfort, difficulty in application, or lack of user education.
Furthermore, the cost of certain advanced compression devices remains a concern, especially in underinsured or low-income populations. While cost-effectiveness over time is a proven benefit of compression therapy—particularly in preventing expensive complications—upfront affordability is still a barrier in some regions.
There is also a need for continued clinical validation and awareness campaigns to ensure physicians and therapists are equipped with the latest research and best practices. Misuse or delayed adoption due to uncertainty about effectiveness can hinder outcomes and patient satisfaction.
Segment Insights: Products and End-Users
The market is broadly segmented into static and dynamic compression therapy devices. Static compression includes products such as compression garments, bandages, and stockings. These continue to dominate the market due to their affordability, ease of use, and widespread prescription in outpatient settings.
Dynamic devices, such as IPC systems, are gaining ground in hospital and home care settings. These systems use programmable pumps to provide graduated pressure and are particularly useful for patients at high risk of DVT or with mobility issues. Their increasing use in post-surgical recovery and chronic condition management is a testament to their growing relevance.
In terms of end-users, hospitals, clinics, and home care settings represent the primary segments. While hospitals remain the largest consumers of advanced compression systems, the home healthcare segment is expanding rapidly. The COVID-19 pandemic underscored the importance of home-based care, driving increased adoption of easy-to-use, portable compression devices.
Competitive Landscape and Strategic Initiatives
The compression therapy devices market is moderately fragmented, with several global and regional players competing for market share. Leading companies are investing in research and development, strategic acquisitions, and partnerships to broaden their product portfolios and enhance market reach.
Some firms are focusing on vertical integration to gain greater control over production, quality, and distribution. Others are forming alliances with hospitals, rehabilitation centers, and telehealth providers to expand their footprint and improve access to therapy.
Brand differentiation is becoming increasingly important, as companies look to stand out through innovation, customer service, and specialized solutions for niche conditions. In response to growing patient demand, many firms are also expanding their offerings to include customizable and gender-specific compression garments.
Regulatory Environment and Future Outlook
Regulatory standards continue to evolve, with agencies such as the FDA, EMA, and regional health authorities placing greater emphasis on product safety, efficacy, and patient outcomes. The shift toward value-based care models is encouraging manufacturers to demonstrate not just performance, but also cost savings and quality-of-life improvements.
Looking ahead, the compression therapy devices market is expected to remain on a positive trajectory, supported by broader trends in chronic disease management, aging populations, and demand for non-invasive therapies. Technological innovation, combined with strategic partnerships and expanded distribution, will be key to sustaining momentum.
Market players that prioritize patient-centric design, education, and digital integration are likely to emerge as leaders in the evolving landscape. Furthermore, ongoing investment in clinical trials and real-world evidence will enhance credibility and help drive widespread adoption across all levels of healthcare.
Conclusion
The compression therapy devices market is entering a new era of opportunity, fueled by rising clinical need, innovation, and patient engagement. While challenges such as adherence and affordability remain, the overall outlook is strong, with ample room for growth across both developed and emerging regions. As healthcare systems worldwide shift toward preventive and home-based care, compression therapy is set to play an increasingly central role in the management of vascular and lymphatic conditions.
0 notes
Text
Expert Foot Care in Pearland: Trust Your Local Specialists
When it comes to foot and ankle health, residents of Pearland are fortunate to have access to exceptional care through local professionals who are passionate about keeping their patients moving comfortably. Whether you're dealing with a persistent heel pain, bunions, or complications from diabetes, turning to podiatry associates of houston ensures expert diagnosis and treatment. For anyone in need of a Pearland podiatrist, quality care is just around the corner, and the specialists at this trusted network are equipped with the knowledge and technology to handle a wide range of conditions.
Visiting a Pearland podiatrist isn't just for acute injuries. Many people live with chronic foot discomfort or minor issues they’ve come to accept as normal. However, even minor foot pain can alter your gait and lead to problems in your knees, hips, or back over time. That’s why early intervention is key. The podiatry associates of houston offer comprehensive foot and ankle care, from preventative checkups and custom orthotics to surgical procedures and post-operative rehabilitation. Their philosophy is centered on treating the root cause rather than just alleviating symptoms, allowing patients to return to their daily lives pain-free and more active than ever.
Diabetics, in particular, should seek regular foot evaluations due to their increased risk for complications. Nerve damage and reduced circulation can lead to unnoticed injuries that develop into serious infections. The Pearland location of this practice offers diabetic foot care that includes vascular assessments, ulcer treatment, and education on daily care techniques to help prevent future problems.
Athletes also find great value in working with a Pearland podiatrist, as repetitive impact and high-level performance can stress the feet in unique ways. Sports medicine specialists in this field offer tailored treatment plans for issues like plantar fasciitis, Achilles tendonitis, and stress fractures. The combination of state-of-the-art diagnostic tools and hands-on therapeutic techniques gives patients the best chance at full recovery without the need for invasive surgery whenever possible.
Parents are another group that benefits from pediatric podiatry services. From in-toeing or out-toeing to flat feet and other developmental concerns, catching potential problems early can help avoid long-term issues with posture and mobility. The practitioners at this Pearland office take great care in making young patients feel comfortable while also guiding families through the proper steps for care and follow-up.
What sets the providers at this practice apart is not only their clinical excellence but also their commitment to patient education and personalized attention. No two feet are the same, and no two patients require the same care plan. By taking the time to explain treatment options and preventive measures, the team ensures each person feels empowered in their care journey.
At Thrive Foot and Ankle, your wellness is the top priority. Whether you're a weekend warrior, a busy parent, or someone simply seeking relief from chronic discomfort, you’ll receive the comprehensive care you deserve. Their Pearland clinic has earned a reputation for excellence through consistent results and compassionate service.
Making foot health a priority can have a positive ripple effect across all aspects of your life, from increased mobility to better posture and overall wellness. If you’ve been searching for trustworthy care close to home, scheduling a visit with a Pearland podiatrist is a smart step toward reclaiming your comfort. Let the podiatry associates of houston show you how expert foot care can transform your day-to-day life, one step at a time.
0 notes