#Symptoms Of Heart Valve Disease
Explore tagged Tumblr posts
Link
Heart Valve Expert in jaipur - Dr. Ravinder Singh Rao
Make an appointment with your doctor if you have any persistent signs or symptoms of Heart Disease that concern you. If you don’t have any signs or symptoms, but you are worried about your risk of Heart Disease, discuss your concerns with the Heart Valve Expert In Jaipur, Dr. Ravinder Singh Rao. Hence, call us Tel: +91-7891791586 and get more information
#Heart Valve Expert in jaipur#Best Heart Expert in Jaipur#Symptoms Of Heart Valve Disease#What Causes Heart Valve Disease#Heart Valve Disease Treatment#Dr. Ravinder Singh Rao
0 notes
Text


I know we finally get a fricking pair ego from the same abnormalities from RyoFau but my nerd ass only wanna talk about the detail nobody wanna paid attention (such as the damn diseases)
Wall of text warning below ⚠️
_____________________
First of all, in medicine, when referring to a patient as α or β, the meaning depends on the specific medical context.
Example: Thalassemia (Inherited Blood Disorder)
α-thalassemia patients: Lack or have mutations in the genes responsible for producing α-globin chains, affecting hemoglobin.
β-thalassemia patients: Lack or have mutations in the genes responsible for producing β-globin chains, leading to more severe anemia.
➡ β-thalassemia is generally more severe, often requiring regular blood transfusions, while α-thalassemia can range from mild symptoms to fetal hydrops (severe anemia in fetuses).
---
Or Streptococcus Infection (Related to Immunity & Bacterial Infections)
α-streptococcus patients: Infected with alpha-hemolytic streptococci, which commonly cause mild conditions such as pharyngitis (sore throat) or endocarditis (heart valve infection).
β-streptococcus patients: Infected with beta-hemolytic streptococci, especially Group B (S. agalactiae), which can lead to pneumonia or severe neonatal infections.
➡ Beta-hemolytic streptococcus is more dangerous, as it can cause sepsis (blood infection) and meningitis.
---
Neurological & Psychological Aspects
Patients with dominant alpha waves: Tend to be in a relaxed state, with lower stress levels.
Patients with dominant beta waves: Are more alert but may also experience heightened anxiety or stress.
➡ People with high beta wave activity are more prone to anxiety and sleep disorders, while those with high alpha wave activity may drift into a dreamy or drowsy state.
Regarding sleep deprivation, it's well known that if a person stays awake for 3–5 days, both the brain and muscles will begin to deteriorate, leading to extreme exhaustion and eventual loss of consciousness.
---
Back to the ego Thoracalgia α & β – Classification of Chest Pain I already explained from the Ryoshu post
Thoracalgia α: Neuropathic pain without nerve compression, often caused by central nervous system disorders, spinal cord damage, or inflammatory conditions.
Examples include: Postherpetic neuralgia (nerve pain following shingles) Spinal diseases without visible compression
Thoracalgia β: Pain due to compression or mechanical injury, commonly seen in conditions such as:
Herniated discs, Rib fractures or injuries, Costochondritis (inflammation of rib cartilage)
➡ Alpha (α) pain is chronic, influenced by the autonomic nervous system and alpha waves (8–12 Hz), causing dull, persistent discomfort.
Beta (β) pain is acute, associated with beta waves (12–30 Hz), and tends to be sharp and intense.


And base from their passive icon its seem to be two different type of inhaler
Faust is a dry powder inhaler (DPI) and Ryoshu is metered dose inhaler (MDI).
Basically (and sum up) their passive, Shallow exhale and Deep inhale links into that with how they experience the pain from thoracalgia

#limbus company#ryoshu lcb#faust lcb#lcb42#ryofaust#finally a pair ego#wall of text#just ...a lot of medical information
164 notes
·
View notes
Text
Joyce Teasley, 15 (USA 1971)
Joyce was only 15 when she was killed by the legal abortion that was supposed to save her. The young girl had Marfan’s Syndrome and aortic valve disease, which was apparently why she was put through a surgical abortion at one month pregnant.
Whoever recommended the “life of the mother” abortion was probably under the mistaken impression that it would be less risky for Joyce given her heart condition. Instead, it sent her into cardiorespiratory arrest, thought to be the result of an abortion-caused pulmonary embolism. She died at Dorothea Dix Hospital on September 28, 1971, less than a month before what would have been her 16th birthday. (DDH was a mental institution and not a general hospital, so it is unclear why Joyce was taken there. It is possible that her symptoms were assumed to be “all in her head” or that she had additional psychological complications that were not noted on the certificate.)
Joyce’s death may have been one of two noted in a study on legalized abortion in North Carolina. The data is insufficient to be sure.
Today, it’s known that the vast majority of heart patients will have a healthy pregnancy and delivery with proper care. Joyce, like all patients with chronic conditions, needed real medical care, not abortion. In fact, her heart problems put her at even higher risk of death from an abortion in the first place compared to a healthy client.

#pre roe legal#pregnant people deserve better#unsafe yet legal#black lives matter#tw abortion#pro life#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion#tw possible malpractice#tw negligence#abortion is not healthcare
13 notes
·
View notes
Note
Hey Joy, this isn't a question so much as a way for me to convince myself I'm not a hypochondriac, lol. Lately, I've been experiencing symptoms of fatigue, brain fog or memory issues, light-headedness, etc, that are uncommon for my age (30). I have related disorders such as anemia, anxiety, & ADHD that may be contributing to these symptoms, although they seem to have gotten worse or appear more frequently now than when I was initially diagnosed with those disorders. My work allows me to read & interact with disabled people with rare diseases, so I often find similarities with their medical issues. At first, I thought this was all just burnout or something related to the lockdown during COVID. I just saw my doctor and had blood work done to check my levels, and I may have a heart condition (tachycardia, mitral valve prolapse). I've fallen asleep at work before because I can't keep my eyes open, even after a full 8 hours of sleep. I can get dizzy from standing up too fast & can't seem to be on my feet for very long without discomfort & pain (I used to work retail, how did I ever do it?). I've researched some of my symptoms and found ME/CFS and POTS as possible conditions. Do you think it's a possibility I have these, or is it just my anxiety? Thank you! (P.s. Hunger Pangs is on my tbr!)
I obviously cannot tell you with any certainty what is wrong--and I am glad you are seeing doctors about it already and may have possible answers wrt tachycardia and the mitral valve.
What I will say is that there are many types of dysautonomia, of which POTS is one, and that what you are describing sounds very familiar to me as someone with two known types of dysautonomia.
The fact that this is hampering your quality of life to the point where you fall asleep at work, are unable to stand without getting dizzy, and are experiencing chronic pain, is enough of a reason to pursue further testing for things like dysautonomia and, yes, possibly even ME/CFS though given your history of anemia, I'm inclined more toward dysautonomia because the two often go hand in hand.
Also, it is normal to feel anxiety experiencing these types of symptoms. Even if it turns out to be a symptom of your anxiety, doesn't make the experiences any less real and debilitating, and you deserve treatment that will help improve your quality and comfort of life. And there is treatment and things you can do that will make you feel better. Getting your anemia under control should be a top priority if it isn't already. Mines was allowed to go untreated for years until we found out my iron anemia was being caused by pernicious anemia (b12 deficiency), and the iron anemia I'd been plagued with since birth suddenly cleared up.
Years and years of blood transfusions and infusion treatments, and the whole time I needed b12. Who knew? Certainly not my old doctors.
Anyway. If your symptoms are at the point where you are recognizing yourself in things like POTS? It's time to pursue that with your doctor. Don't put it off because you think it's not that bad or others have it worse. Everyone deserves to feel well.
Good luck.
200 notes
·
View notes
Text

“According to Eastern medicine be it Indian, Chinese, Tibetan or Thai, the left side of the body is totally different from the right side. Even some Buddhist monastic traditions include within their precepts for monks to sleep on their left side. Although it sounds weird resting and sleeping on the left side has many health benefits.
The lymph drains to the left.
The left side of the body is the dominant side of the lymphatic system. Most of the lymph drains down to the thoracic duct which is located on the left side. In its path the lymph transports proteins, glucose metabolites and waste products that are purified by the lymph nodes to be drained to the left side.
Derived from the above it is common to deduct in Eastern medicine that the diseases of the left side of the body may be due to chronic congestion of the lymphatic system.
The priorities of the body.
According to ayurveda congestion occurs in the body following certain priorities. If the lymphatic system is digested, the liver and blood are subsequently saturated with toxic substances. Primary symptoms of congestion present on the left side of the body before moving to the right side where they make their later appearance.
Feeling bored after a meal?
The Indian suggestion is that if you take a break after eating, do it lying on your left side. The rest should not exceed 10 minutes and is different from the evening nap which is usually 20 minutes or more.
Stomach and pancreas hanging to the left side. When you lie on your left side both naturally hang allowing for optimal and efficient digestion. Food is driven to move naturally through the stomach and pancreatic enzymes are secreted in a paulatin way and not in a single stroke, which happens if you lie down on the right side.
Laying on your left side your liver and gallbladder hang from your right side. Resting on the left side allows them to hang and secret their precious enzymes into the digestive tract, emulsifying fats and neutralizing stomach acids.
When the digestive system is stimulated this way your digestive cycle is shorter and doesn't leave you stranded for the rest of the afternoon. Try resting 10 minutes on your left side after eating.
Feel energized and not tired after eating.
Try to eat in a relaxed way mid-day and don't forget to rest on your left side and check that you will feel more energized and with better digestion.
Sleeping magic from the left side.
Best elimination.
The small intestine flushes toxins through the ileocecal valve (VIC) on the right side of the body at the start of the large intestine. The large intestine travels down the right side of your body, crosses your stomach and descends down the left side.
Through the VIC, sleeping on the left side allows gravity to stimulate bodily waste into the large intestine from the small intestine more easily.
As the night passes and continue sleeping on your left side the debris moves more easily toward the downward column and morning removal will be easier.
Best cardiac function.
More than 80% of the heart is located on the left side of the body. If you sleep on the left side the lymph drained to the heart will be driven by gravity taking work out of your heart while you sleep.
The aorta, which is the largest artery in the body, comes out from the upper part of the heart and is arched left before going down to the abdomen. By sleeping on the left side, the heart pumps blood more easily into the downing aorta.
Sleeping on the left side allows the intestines to move away from the cava vein that brings blood back to the heart. Noticeably the cava vein rests on the right side of the thorn, so when you lie down on the left side the viscera move away from the cava veina. Again gravity makes the heart job easier.
The sparrow is on the left side.
The spleen is part of the lymphatic system and is also on the left side of the body. Its function is that of a large lymph node which filters the lymph and additionally filters the blood. When you lie on the left side the fluids return to the basin is easier and is more easily produced by gravity.
The lymphatic system drains all cells in the body through contractions and muscle movement and not by heart pumping. Helping the lymph drain into the pelvis and heart with gravity is a simple way to purify your body.
And while there are no scientific protocols on it, sleeping on the left side does make sense. Understanding ancestral wisdom based on knowledge of modern anatomy clears up many doubts about the reasons that exist in the east to sleep a certain way.”
Original article written by Dr. John Doull
[Leila L'Abate]
#sleep#Physiology#left side#Leila L'Abate#Dr. John Doull#quotes#articles#lymphatic system#Body Alive
26 notes
·
View notes
Text
i kind of scared the new hire today (oops)
we were swapping medical lore, and i mentioned my scarlet fever and lack of antibiotics growing up, etc. her healthcare background is even more extensive than mine, so she immediately recognized the potential complications and asked me if i had a heart murmur (she specifically mentioned the mitral valve, hell yeah). i explained yes, and that it's gotten worse per my last physical 2 years ago, but no cardiologists that i've talked to thus far take our insurance. so i can't get in for an echocardiogram to see if i actually need surgery, but everything i read about rheumatic fever/rheumatic heart disease matches my symptoms.
she looked aghast and asked me how i'm not worried all the time and desperately trying to figure out how to pay for an echo. i told her i decided not to stress too much because even if an echo shows i need surgery, i couldn't afford it anyway, not with our current coverage. all it would do is confirm death is coming for me young, which i've always known and been fine with. she was mildly appalled by this, but thankfully, still thinks i am cool and a good teacher. so that's a relief lol
#listen my mom's anti vax phase resulted in more than one brush with death#just for me my other 3 siblings alive for that phase were fine#but that and to going to funerals nonstop when i was little bc the alcoholism was catching up with my dad's side#means that i feel very comfortable with the thought of death and always have#typical southern experience#probably a typical white trash experience regardless of region#blog#medical cw
10 notes
·
View notes
Text
Heart Care Centre In Gorakhpur
When it comes to maintaining overall health, few things are as vital as taking care of your heart. As the heart continues to be one of the most critical organs in our body, any issues related to it must be taken seriously. In Gorakhpur, the demand for quality heart care services has risen significantly, as people are becoming more aware of the importance of cardiovascular health. Fortunately, Gorakhpur is home to some of the best heart care centre, where patients can receive expert treatment and guidance on managing heart conditions.
In this blog, we’ll explore the best heart care centre in Gorakhpur, the services they offer, and why you should choose them for your heart health needs.

Heart diseases continue to be one of the leading causes of death worldwide. In India, the rise of lifestyle diseases such as hypertension, diabetes, and high cholesterol has contributed to an increase in heart-related problems. Early diagnosis and intervention are key to managing heart conditions effectively. This is where a good heart care centres comes into play. Heart care centres are equipped with advanced technology, skilled cardiologists, and modern facilities to provide accurate diagnosis, treatment, and preventive care for a wide range of heart diseases.
Services Offered at Heart Care Centres in Gorakhpur
Heart care centres in Gorakhpur provide a variety of services, ranging from preventive care to advanced treatment options. Here are some of the key services you can expect:
1. Cardiology Consultations
A heart care centre begins with consultations with experienced cardiologists who assess your symptoms, medical history, and risk factors. These consultations often involve a thorough examination and may be followed by diagnostic tests to understand the root cause of any heart issues.
2. Comprehensive Diagnostic Tests
Accurate diagnosis is the first step toward effective treatment. Heart care centres in Gorakhpur offer state-of-the-art diagnostic tools such as:
Electrocardiogram (ECG)
Echocardiogram (ultrasound of the heart)
Stress tests
Holter monitoring
Angiography and angioplasty
These tests help identify underlying conditions like heart disease, arrhythmias, blocked arteries, and more.
3. Cardiac Surgery and Interventions
For patients with severe heart conditions, heart care centres in Gorakhpur offer surgical interventions such as:
Coronary Artery Bypass Grafting (CABG)
Valve replacement or repair
Angioplasty and stent placement
These procedures are performed by expert cardiac surgeons who specialize in heart-related surgeries, ensuring the best outcomes for patients.
4. Preventive Care and Health Monitoring
Heart care centres emphasize preventive care to help individuals avoid heart disease. They provide services like:
Routine health check-ups
Blood pressure and cholesterol monitoring
Lifestyle counseling (diet, exercise, stress management)
Weight management and smoking cessation programs
By focusing on prevention, these centres help patients lower the risk of heart disease and maintain a healthy lifestyle.
5. Cardiac Rehabilitation
After a heart attack or surgery, patients require a rehabilitation program to recover fully. Cardiac rehabilitation involves supervised exercise, diet counseling, and psychological support to help individuals regain strength and reduce the risk of further complications.
Why Choose a Heart Care Centre in Gorakhpur?
1. Expert Cardiologists
Heart care centres in Gorakhpur are staffed by experienced and qualified cardiologists who specialize in diagnosing and treating a wide range of heart conditions. Whether you’re dealing with high blood pressure, irregular heartbeats, or more severe conditions like coronary artery disease, these professionals provide the best possible care.
2. State-of-the-Art Facilities
The heart care centres in Gorakhpur are equipped with the latest technology, including high-resolution imaging systems, advanced cardiac monitoring tools, and cutting-edge surgery equipment. This allows doctors to provide accurate diagnoses and offer effective treatment options for heart patients.
3. Personalized Care
Each patient is unique, and heart care centres understand the importance of providing personalized care. From the first consultation to post-treatment care, cardiologists work with patients to create tailored treatment plans that suit their individual needs and health goals.
4. Comprehensive Approach
These centres offer a comprehensive range of services under one roof, ensuring that all aspects of heart health are addressed. From diagnostic tests and treatment options to preventive care and rehabilitation, you can count on the heart care Centres in Gorakhpur to support your heart health journey.
Best Heart Care Centre in Gorakhpur.
Gupta Heart Care Centre in Gorakhpur
This Centre are well-known for their experienced team of cardiologists, use of advanced medical technology, and focus on patient well-being.
Conclusion
Taking care of your heart is an essential aspect of living a long and healthy life. If you're experiencing any symptoms of heart disease or if you simply want to ensure your heart health is in check, it’s time to consult a trusted heart care centres in Gorakhpur. With world-class doctors, top-notch facilities, and comprehensive treatment options, you can rest assured that your heart is in safe hands.
Remember, early detection and intervention can save lives. Don’t wait for symptoms to worsen—schedule a consultation at one of Gorakhpur’s leading heart care centres today.
Call to Action: If you or someone you know is concerned about their heart health, don't delay. Contact a reliable Heart Care Centre in Gorakhpur for an assessment and start your journey toward a healthier heart today
2 notes
·
View notes
Text
heart valve disease
Heart valve disease occurs when one or more of the heart’s valves fail to function properly, disrupting blood flow through the heart. Valves may become too narrow (stenosis) or fail to close completely (regurgitation), leading to blood flow issues. This condition can be caused by aging, infections, congenital defects, or other heart problems, with symptoms such as shortness of breath, fatigue, chest pain, or heart murmurs. Diagnosis often involves tests like echocardiograms and ECGs.
Treatment options range from lifestyle adjustments and medication to valve repair or replacement, helping many lead healthier lives with timely care and monitoring.

If you or a loved one are struggling with any related issues, we at Neotia Getwel are here to help. Our cardiology team can provide you with a personalized diet plan and lifestyle advice to keep your blood pressure in check. For more tips and personalized consultations, don’t hesitate to contact us at Neotia Getwel Multispecialty Hospital.
2 notes
·
View notes
Text
An Overview of Conditions Treated by Cardiologists

Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. A congenital heart defect may occur when the heart or one of its associated blood vessels fails to develop normally before birth. The spectrum of these defects ranges from mild to severe with some children not requiring treatment while others require multiple surgeries to correct. Coronary artery disease is the most common heart disease and accounts for 1 in every 4 deaths globally. It is due to narrowing or blockage of the blood vessels that supply the heart with blood and oxygen, usually due to cholesterol deposits. Heart failure is the inability of the heart to pump enough blood to meet the needs of the body. This may to be due to weakness of the heart muscle, or if the heart is unable to fill properly. Conditions such as coronary artery disease, high blood pressure, inflammation of the heart and abnormalities of the heart valves may cause heart failure. Valvular heart disease may affect one or more of the four valves of the heart, which normally keep blood flowing properly through the heart. Treatment for narrowed or leaking valves may be medical, surgical or catheter based. Electrophysiology focuses on the electrical system of the heart, disturbances of which may result in heart rhythm abnormalities. These may include irregular, slow or rapid heartbeats. Treatment may include drugs, implantable devices or catheter ablation, where tissue causing the problem is destroyed. Symptoms of a heart problem may include chest pain, abnormal shortness of breath, dizziness, blackout, palpitation, cough and swelling of the legs. These should prompt referral to a cardiologist if a cardiac cause is suspected.
2 notes
·
View notes
Text
Understanding Heart Disease: What is Heart Disease
What is Heart Disease?
Heart disease, also known as cardiovascular disease (CVD), encompasses a range of conditions affecting the heart and blood vessels. It is the leading cause of death worldwide, causing significant morbidity and mortality. The term "heart disease" is often used interchangeably with "cardiovascular disease," although technically, cardiovascular disease includes all diseases of the heart and blood vessels, while heart disease specifically refers to conditions affecting the heart itself.
Types of Heart Disease
Coronary Artery Disease (CAD): CAD is the most common type of heart disease and occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup (atherosclerosis). This can lead to chest pain (angina), heart attacks, and other complications.
Heart Failure: Heart failure, or congestive heart failure, happens when the heart muscle is unable to pump blood efficiently, leading to a buildup of fluid in the lungs and other tissues. Causes include CAD, hypertension, and cardiomyopathy.
Arrhythmias: These are disorders of the heart's rhythm, which can be too fast (tachycardia), too slow (bradycardia), or irregular. Common arrhythmias include atrial fibrillation and ventricular fibrillation, which can significantly impact heart function.
Heart Valve Disease: Heart valve disease involves damage to one or more of the heart's valves, affecting blood flow within the heart. Conditions include stenosis (narrowing of the valve), regurgitation (leakage of the valve), and prolapse (improper closure of the valve).
Congenital Heart Defects: These are heart abnormalities present at birth, ranging from simple defects like a hole in the heart's walls (septal defects) to more complex malformations. They can affect how blood flows through the heart and to the rest of the body.
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle. The heart muscle becomes enlarged, thickened, or rigid, which can lead to heart failure or arrhythmias. Types include dilated, hypertrophic, and restrictive cardiomyopathy.
Pericarditis: Pericarditis is inflammation of the pericardium, the thin sac surrounding the heart. It can cause chest pain and fluid buildup around the heart, affecting its function.
Causes and Risk Factors
Heart disease is influenced by a combination of genetic, environmental, and lifestyle factors. Major risk factors include:
High Blood Pressure (Hypertension): Hypertension forces the heart to work harder to pump blood, leading to the thickening of the heart muscle and potential heart failure.
High Cholesterol: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL), contribute to the formation of plaque in the arteries, leading to atherosclerosis.
Smoking: Smoking damages the lining of blood vessels, increases blood pressure, reduces oxygen to the heart, and raises the risk of heart disease.
Diabetes: Diabetes significantly increases the risk of heart disease. High blood sugar levels can damage blood vessels and the nerves that control the heart.
Obesity: Excess body weight strains the heart, raises blood pressure, and increases the likelihood of diabetes and cholesterol problems.
Physical Inactivity: A sedentary lifestyle contributes to obesity, hypertension, and other heart disease risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, sodium, and sugar can lead to heart disease by raising cholesterol levels, blood pressure, and weight.
Family History: A family history of heart disease increases one's risk, suggesting a genetic predisposition.
Age and Gender: Risk increases with age, and men are generally at higher risk earlier in life than women, although women's risk increases and can surpass men's post-menopause.
Symptoms
Symptoms of heart disease vary by condition but may include:
Chest pain or discomfort (angina)
Shortness of breath
Pain, numbness, or coldness in the legs or arms
Fatigue
Lightheadedness or dizziness
Palpitations (irregular heartbeats)
Swelling in the legs, ankles, and feet
Diagnosis and Treatment
Diagnosing heart disease often involves a combination of medical history review, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG or EKG)
Echocardiogram
Stress tests
Blood tests
Cardiac catheterization
CT or MRI scans
Treatment strategies vary based on the specific type of heart disease and its severity and may include:
Lifestyle Modifications: Healthy diet, regular exercise, smoking cessation, and weight management are crucial for preventing and managing heart disease.
Medications: Medications can control risk factors such as hypertension, high cholesterol, and diabetes, or treat specific heart conditions like arrhythmias and heart failure.
Procedures and Surgeries: Angioplasty, stent placement, bypass surgery, valve repair or replacement, and implantable devices like pacemakers or defibrillators may be necessary for severe cases.
Prevention
Preventing heart disease involves managing risk factors through:
Maintaining a healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
Regular physical activity
Avoiding tobacco use
Controlling blood pressure, cholesterol, and blood sugar levels
Regular health screenings
Stress management techniques
Understanding and addressing heart disease through lifestyle changes, medical management, and preventive measures is crucial in reducing its impact and improving overall heart health.
2 notes
·
View notes
Text

TYPES OF HEART DISEASE
Heart disease encompasses a wide range of cardiovascular problems. Various conditions fall under the heart disease umbrella, each affecting the heart or blood vessels in distinct ways. Understanding these types can help in recognizing symptoms early and seeking appropriate treatment. This article explores the primary types of heart disease, their causes, and potential treatments.
1. Coronary Artery Disease (CAD)
Overview:
Coronary Artery Disease is the most common type of heart disease. CAD occurs when the coronary arteries, responsible for supplying blood to the heart muscle, become hardened and narrowed due to the buildup of cholesterol and other materials, known as plaque, on their inner walls. This process is called atherosclerosis.
Symptoms:
Chest pain (angina)
Shortness of breath
Fatigue
Treatment:
Treatments include lifestyle changes, medication, and possibly procedures like angioplasty or coronary artery bypass grafting (CABG).
2. Heart Arrhythmias
Overview:
Arrhythmias are irregular heartbeats. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregularly. This can be due to a fault in the heart’s electrical system.
Symptoms:
Palpitations
Dizziness
Fainting
Treatment:
Treatment might involve medications, lifestyle adjustments, and in some cases, implantable devices like pacemakers or procedures like catheter ablation.
3. Heart Valve Disease
Overview:
The heart contains four valves: the tricuspid, pulmonary, mitral, and aortic valves. These valves open and close to direct blood flow through the heart. Valve disease occurs when one or more of these valves do not function properly.
Symptoms:
Fatigue
Swollen ankles or feet
Shortness of breath
Treatment:
Treatment may include medication, surgical repair, or valve replacement depending on the severity and specific type of valve disease.
4. Congestive Heart Failure (CHF)
Overview:
Heart failure, sometimes known as congestive heart failure, occurs when the heart can’t pump blood as well as it should. This can result from any condition that damages the heart muscle, including CAD, high blood pressure, and heart valve disease.
Symptoms:
Shortness of breath
Persistent coughing or wheezing
Swelling in legs, ankles, and feet
Treatment:
Managing heart failure involves a combination of lifestyle changes, medications, and possibly surgery or devices like ventricular assist devices (VADs) or implantable cardioverter-defibrillators (ICDs).
5. Cardiomyopathy
Overview:
Cardiomyopathy refers to diseases of the heart muscle. These diseases enlarge or make the heart muscle rigid and more prone to arrhythmias.
Symptoms:
Breathlessness
Swelling of the legs
Fatigue
Treatment:
Treatment focuses on controlling symptoms and may include medications, lifestyle modifications, or devices to help the heart pump more effectively.
6. Congenital Heart Defects
Overview:
Congenital heart defects are structural problems with the heart present from birth. They can involve the walls of the heart, the valves of the heart, and the arteries and veins near the heart.
Symptoms:
Symptoms vary widely and can include cyanosis (a bluish tint to the skin, lips, and fingernails), breathing difficulties, and fatigue.
Treatment:
Treatment depends on the type and severity of the defect and may involve medication, catheter procedures, or surgery.
Conclusion
Heart disease is a broad term that covers various conditions affecting the heart’s structure and function. Recognizing the signs and symptoms of these different types can lead to early diagnosis and treatment, significantly improving quality of life and outcomes for those affected. Regular check-ups and conversations with healthcare providers about heart health can help individuals understand their risks and take proactive steps towards heart disease prevention.
#usascriphelpersofficial#heart failure#heart disease#heart disease prevention#heart disease risk#health care#medical care#public health
2 notes
·
View notes
Photo

Symptoms Of Heart Valve Disease
Make an appointment with your doctor if you have any persistent signs or symptoms of Heart Disease that concern you. If you don’t have any signs or symptoms, but you are worried about your risk of Heart Disease, discuss your concerns with the Heart Valve Expert In Jaipur, Dr. Ravinder Singh Rao. Hence, call us Tel: +91-7891791586 and get more information
#Heart Valve Expert in jaipur#Best Heart Expert in Jaipur#Symptoms Of Heart Valve Disease#What Causes Heart Valve Disease#Heart Valve Disease Treatment#Dr. Ravinder Singh Rao
0 notes
Text
It is time, according to my brain, to give thanks to that one ER nurse that saw a calm and exhausted university student breathing really slow and deliberately, complaining about struggling to take in a full breath and chest pain, and immediately ordered an ECG. you saved my life I think. I wasn't having the heart attack you were expecting but I did find a congenital heart valve defect in follow up tests and got on heart medication that significantly improved symptoms I've had all my life and had gotten so used to that I was having heart attack markers and thought it was a mild asthma attack.
Feeling so much better from the heart medication contributed to me not killing myself that year after 2 car accidents and finding out I have adhd, a heart disease and autism and have just been rawdogging life without any help for 20 years. I think if I still had the chest pain and tachycardia and bone deep exhaustion all the time I would have gone through with it.
I do think I had a heart attack two years before then, but it was at 3:56 am in the middle of exam season, I thought I just dislocated my sternum in my 4am addled brain, and from past healthcare experience I didn't trust doctors to take me seriously about it because dislocating your sternum while sleeping normally should not be possible.
I don't know how I survived then, but I had agonizing chest pain, shortness of breath and the worst fatigue of my life for 3 weeks after that night, I couldn't pick up a regular plastic chair I was in so much pain. I wish I had someone like you then to believe me, and tell me what was going on and what to do.
But I got you two years later, and thanks to you I know it's not panic attacks or asthma, and that when I get symptoms I should rest and not push through, and that I can manage this until such a day that I need a valve replacement, and that cardio exercise helps with my symptoms if, and only if, I don't overdo it. Got my heart rate down from 120-140 at rest to 90-100 at rest with medication and the right exercise.
So thank you! You saved my life that day in the ER, you saved it again 3 months later when I almost committed suicide, and you're saving it again every time I would have had a heart attack in my future but won't because I'm listening to my body and properly managing my condition thanks to you. Oh by the way 60kg is a low bodyweight for me my bones are stupid dense and weigh like 1.3 kg more than the average for my height, weight and sex. You were right, I was stupid, I no longer attach any value to my weight like you said.
2 notes
·
View notes
Text
The Comprehensive Compilation of Adverse Reactions Associated with Cabergoline 0.25mg
Cabergoline 0.25mg is a frequently given prescription for many medical disorders. However, it is important for users to be aware of the possible negative effects that may accompany its usage, as is the case with any pharmaceutical. This page provides an extensive list of side effects linked to Cabergoline 0.25mg, including both typical responses and more severe cautions and long-term concerns. Through comprehending these adverse consequences and acquiring the knowledge to handle them, people may make well-informed choices about their therapy and overall state of health.
Cabergoline is a medication used to treat medical conditions such as hyperprolactinemia and Parkinson's disease
Cabergoline is a pharmaceutical compound classified as a dopamine agonist. It is often used in the treatment of disorders such as hyperprolactinemia, which may result in complications such as infertility, irregular menstruation, and lactation in both males and females.
Medical uses of Cabergoline 0.25mg
Cabergoline 0.25mg is often used for the treatment of hyperprolactinemia, a medical disorder defined by elevated levels of prolactin in the bloodstream. This medicine effectively reduces prolactin levels and effectively manages symptoms such as infertility, decreased libido, and irregular menstruation.
Adverse effects on the digestive system
Typical gastrointestinal adverse effects of Cabergoline 0.25mg may include nausea, emesis, constipation, and stomach discomfort. To reduce side effects, it is crucial to consume this drug with meals.
Neurological Adverse Reactions
Individuals using Cabergoline 0.25mg may encounter symptoms such as vertigo, somnolence, or cephalalgia. It is recommended to refrain from driving or operating heavy equipment until you are aware of the impact of this drug on your abilities.
Adverse effects on the cardiovascular system
Certain people may encounter alterations in blood pressure or heart rate while consuming Cabergoline 0.25mg. Regularly monitoring these measures and promptly reporting any major changes to your healthcare professional is essential.
Cabergoline 0.25mg is used to treat a variety of illnesses that arise from excessive production of the hormone prolactin. It may be used to treat pituitary prolactinomas, which are tumors of the pituitary gland, as well as certain menstruation issues and issues with fertility in both sexes.
Possible cardiac valve impairment
An important concern connected with Cabergoline is the possibility of cardiac valve injury, especially in those who are prescribed greater dosages for a prolonged duration. Consistent monitoring of the heart is crucial in order to promptly identify any anomalies in the valves.
Potential for Fibrotic Reactions
The use of Cabergoline has been associated with the emergence of fibrotic responses in diverse tissues, such as the cardiac, pulmonary, and abdominal tissues. If you encounter symptoms such as respiratory distress or edema in the limbs, it is advisable to promptly seek medical assistance.
Potential for the Development of Tolerance
Prolonged usage of Cabergoline might result in the development of tolerance, necessitating greater dosages to get the same therapeutic outcome. It is essential to adhere to the recommendations of your healthcare practitioner and refrain from altering your dose without seeking their advice.
Effect on Hepatic Function
Cabergoline has the potential to impact liver function in some people, resulting in increased levels of liver enzymes. It is advisable to undergo regular liver function tests while taking this drug in order to monitor any changes and avoid any problems.
Controlling and Reducing Side Effects
If you are encountering adverse reactions as a result of consuming Cabergoline 0.25mg, do not worry; there are strategies to address them. Here is a method to effectively control and reduce undesired consequences.
Titration and Surveillance of Dosage
Seek guidance from your healthcare professional about the possibility of modifying your Cabergoline dose. Regular surveillance may aid in monitoring the body's response to the medicine.
Implementing lifestyle modifications to mitigate adverse effects
Modest lifestyle adjustments may significantly alleviate adverse effects. To promote your general well-being, it is important to ensure that you stay well hydrated, follow a balanced diet, and make regular exercise a priority.
Drug Interactions
It is essential to be aware of the potential interactions between Cabergoline and other drugs for your safety and well-being. Now, let's explore the possible interactions and contraindications that need to be monitored.
Important Drug Interactions to Be Mindful Of
Cabergoline may have adverse interactions with some drugs. Ensure that you regularly update your healthcare practitioner about all the drugs you are currently taking in order to prevent any possible drug interactions.
Interactions with Specific Medications
Certain drugs should be avoided while using Cabergoline owing to the potential for adverse interactions. Take note of these contraindications to avoid any potential consequences.
Specific considerations for certain demographics
Customized strategies may be necessary for administering Cabergoline to various groups. Below are important factors to consider for pregnant or nursing women and geriatric patients.
Cabergoline is used to treat hyperprolactinemia (high levels of prolactin, a natural substance that helps breast-feeding women produce milk but can cause symptoms such as infertility, sexual problems, and bone loss in women who are not breast-feeding or men). Cabergoline is in a class of medications called dopamine receptor agonists. It works by decreasing the amount of prolactin in the body.
Women who are currently pregnant or breastfeeding
When you are pregnant or breastfeeding, it is crucial to have a conversation with your healthcare professional about the potential advantages and disadvantages of using Cabergoline. The utmost importance should be placed on ensuring the well-being of both you and your kid.
Geriatric Patients
Cabergoline may need special care for elderly people. Close surveillance and possible dose modifications may be required to guarantee the safety and efficacy of the medication.
Summary and Concluding Remarks
Understanding and addressing the possible side effects, interactions, and concerns of Cabergoline 0.25mg may seem challenging, but with enough information and help, you can successfully handle them. It is important to constantly seek advice from your healthcare professional for specialized assistance that is specifically targeted to your individual requirements.
Ultimately, it is essential for both patients and healthcare practitioners to have a thorough understanding of the potential adverse effects of Cabergoline 0.25mg. By being knowledgeable about the possible hazards, closely monitoring for any worrisome symptoms, and seeking advice from a healthcare expert as necessary, people may manage their course of treatment with more assurance and security. It is important to emphasize that taking a proactive approach to managing and maintaining open lines of communication are crucial in achieving the most favorable results while using Cabergoline 0.25mg.
1 note
·
View note
Text
Bartonella henselae
Case Report:
23M veterinary student from home with a cat, presents with a one year history of neck swelling, 1 month of fevers and lethargy. Also he lives in Karachi.

The fevers are a/w chills and rigours that response to paracetamol and have no particular pattern to them.
He doesnt have any arthralgias or arthritis or rash.
They find pretty sizable lymph nodes on exam in the cervical chain and inguinal regions.
He starts developing hypotension and they start him on some vasopressors and meropenem.
The fevers don't respond, and someone decides to start azithromycin, which it does respond to.
He's also worked up for IE given the chronicity of events.
Eventually on biopsy of the lymph node, the lab finds bartonella hensalae.
Microbiology + transmission:
aka cat scratch fever, so this is why history is so important to infectious diseases physicians.
it's actually disease of cats that can spread to their humans via bites and scratches. Or the cat licks a wound etc.
and unfortunately also via arthropod vectors and mossies
after entry into a host, it's main target cells are CD34s, immune cells, and then alters the host immune system
it's interesting special power is that it can predispose hosts to other pathogens in this manner

it's a gram negative rod (pink rods)
Historical trivia
the fun bits
genus of Bartonella is named for a Peruvian scientist (Alberto Barton, also had interest in brucellosis and leishmaniasis --> other tropical diseases taht cause fevers of unclear origin), he isolated the bacteria from patients during an outbreak among railway works in South america. This was 1905.
reminds me of love in the time of cholera, when people still wrote physical letters.
species of bartonella henselae is actually named for Diane Henselae, a researcher from Oklahoma, who collected samples during an outbreak there in the mid 1980s.
rare for someone who discovered a species named for them to be both alive and a woman, and I can't find much about her online.
there are other bartonella species that cause historically significant diseases like trench foot (bartonella quintana, transmitted by lice) and carrion's disease (bartonella bacilliformis, with a high mortality rate). another post for another day.
Clinical features
incubation period: up to 10 days
initial: rash at site of injection or intro of pathogen, from there it travels to local lymph nodes causing lymphadenopathy about 1-3 weeks later
From CDC guidelines who took image from NEJM
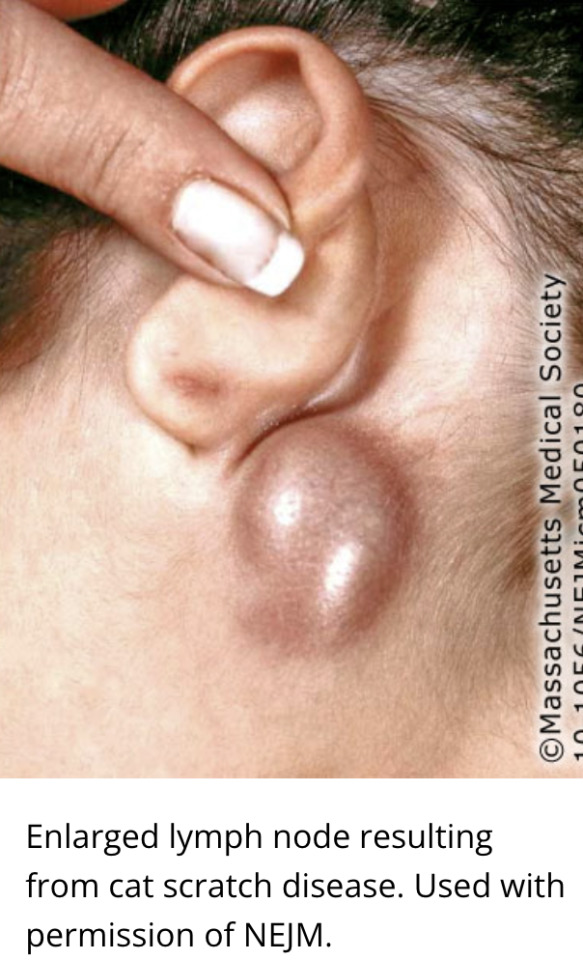
Bsymptoms - low grade fevers/malaise/fatigue
epidemio: occurs most often (for a rare disease) in kids < 15
Complications
infection affecting the eye (neuro-retinitis = visual changes, irritation and photophobia), liver, spleen, brain/spine (transverse myelitis, encephalitis etc), bones and heart valves (IE)
Increased risk groups for complications
HIV/AIDs, immunocompromised hosts (i.e. transplants), mortality is an issue in this group, as disseminated disease a possibility
small risk of IE in groups with RFs for develop this (prosthetic valves, damaged valves, unrepaired congential heart disease etc)
Investigations
challenging, no gold standard test as the sens and spec is variable for each individual one, so it's a combination really, of history exam and a variety of confirmatory tests
PCR (variable spec/sens), serology (indirect and often negative in early stages, can also be positive for years post treatment and doesn't differentiate from other bartonella species), cultures are definitive but it can take 21 days for anything to grow (it's fastidious)
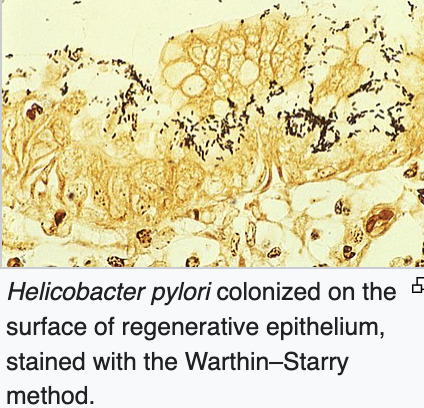
histopath of lymph nodes helpful - stains: silver stain or Warthin Starry stain (silver nitrate) which is kind of a reverse starry starry night used for spirochetes like helicobacter.
in IE, it can be culture negative, which can confuse diagnosis
From Wiki
Management
mild disease is self resolving
first line: few days azithromycin or doxycycline can reduce symptoms and is indicated for enlarged lymph nodes to reduce size or unresolving LAD >1 month
in case of eye infection or IE expect longer duration of hterapy, like doxy and rif for 4-6 weeks
will also respond to bactrim, cipro, rif and gent
Prevention from the CDC:
avoid strays, wash hands after petting cats, keep strays from your cat, avoid owning new kittens who are < 1 yr if you are immunocompromised
avoid getting scratched..which is kinda hilarious but can see why

Sources
stat pearls
case report above
wikipaedia
Rare diseases
CDC guidelines
#medblr#infectious diseases#infectious disease#bartonella#bartonella henselae#cat scratch disease#microbiology
6 notes
·
View notes
Text
What are the stages of congestive heart failure?
Congestive heart failure, also known as cardiac failure, is a serious condition in which the heart fails to pump blood adequately. We are all aware of the basic functioning of the heart which is to pump blood and oxygen to various parts of the body. This functioning may get hampered at times due to certain heart issues. One such heart issue that we are going to discuss is congestive heart failure.
GS Hospital Pilkhuwa, one of the top heart care hospitals in UP, takes the initiative to bring about awareness for a healthy heart. Awareness of heart health is a must to prevent any kind of cardiac issues and maintain healthy heart function. In this context, we shall discuss the causes, symptoms, and stages of congestive cardiac failure and how to prevent it.
Early detection is key to better recovery for heart health. Knowing about the stages of congestive cardiac failure will help restore heart functioning with a strategic plan and medication management. Let's begin with the basics of congestive heart failure.

What is congestive heart failure?
As the name suggests, congestive cardiac failure is a heart condition in which the heart fails to pump sufficient blood and oxygen to other systems of the body. The word “heart failure” can be quite stressful. However, this does not mean that the heart completely fails to perform its functioning of heartbeats.
In congestive cardiac failure, the heart becomes less contractible due to its limitation and ability to fill with blood. This may cause congestion or chest pain due to a lack of oxygen and blood supply. If neglected, it may cause multisystem organ failure.
Causes of congestive heart failure
The causes of congestive heart failure are as follows-
Genetic
Aging
Stress
High blood pressure or cholesterol
Obesity
Coronary artery disease or blockage
Heart valve disorder
Irregular heartbeat
Abuse of drugs or alcohol
History of smoking
Symptoms of congestive heart failure
The symptoms of congestive heart failure are as follows-
Rapid heartbeat
Weight gain
Excessive sweating
Shortness of breath
Swelling of extremities
Fatigue
Nausea
Lightheadedness
Persistent cough
Stages of congestive heart failure
There are 4 different stages of congestive cardiac failure which include the following-
Stage A
Patients with stage A heart failure may have no major dysfunction of pumping activity of the heart such as coronary artery disease, valvular problems, or blockage of the heart. They may have symptoms such as mild shortness of breath, and swelling of extremities. These patients generally have a strong past medical history of diabetes, high blood pressure, or obesity. There are no major structural and functional changes in the heart at this stage. The symptoms can be corrected with lifestyle changes and medications.
Stage B
Patients with stage B congestive heart failure may develop structural heart disease which reduces the overall functioning of the heart usually within less than 6 months. These patients often complain of enlarged left ventricles. They may have symptoms such as shortness of breath, and swelling of extremities. The diagnostic test mainly reveals structural changes with positive stress tests. Healthy lifestyle modifications such as exercising to lose weight may help in improving the functioning of the heart with medications. These patients may have a strong genetic history of heart failure.
Stage C
Patients at this stage will show symptoms of heart failure with underlying structural heart disease. The symptoms mainly occur due to contraction of the left ventricle while pumping blood. The patient may have breathlessness, fatigue, and tiredness with dyspnea on exertion. These patients are under current treatment for heart failure and may show no symptoms while being under the medications. They are given treatment to prevent heart failure exacerbation.
Stage D
Stage D heart failure is considered the last stage of heart failure. In these patients, there will be advanced structural and functional cases causing symptoms to occur at rest as well. The patients under this stage may require advanced treatment such as circulatory support, surgery, or medications as directed by the physician.
The stages and symptoms of heart failure may range from mild to severe. It may worsen over time if not medically managed. Practicing a healthy lifestyle can help in delaying the progression of the heart issue preventing further damage.
Types of heart failure
There are two types of heart failure which include
● Left-sided heart failure
Left-sided heart failure is considered a common type of heart failure. The left ventricle is an important chamber that allows the pumping of the heart. This allows blood supply to all parts of the body by maintaining adequate blood volume.
In case of systolic heart failure, the left ventricle capacity to contract deteriorates causing pumping failure. This reduces the capacity of blood and oxygen supply to other parts of the body.
On the other hand, in the case of diastolic heart failure, there is stiffening of the left ventricle which causes the inability of the muscle to relax.
The main symptoms of left-sided heart failure are weight gain, shortness of breath at rest as well as exertion, inability to lie flat on bed at night, awakening at night due to shortness of breath, and left-sided chest pain.
● Right-sided heart failure
Right-sided heart failure is quite less common. This occurs because of the lack of pumping of blood from the right ventricle to the lungs. The backflow of the blood into the blood vessels may cause fluid retention and edema of the lower legs and arms. The main symptoms of right-sided heart failure are breathlessness of exertion, wheezing, lightheadedness, dizziness, coughing, edema of the legs, and difficulty concentrating.
Both forms of heart failure may get progressive with time if left untreated. If you are resonating with any of the above-mentioned signs and symptoms, it is recommended to consult your doctor right away.
Treatment of congestive heart failure
The main standard treatment for congestive cardiac failure is to control signs and symptoms and prevent further damage to the heart. The line of treatment for congestive cardiac failure includes a comprehensive treatment plan with the following-
Medications include vasodilators, diuretics, ACE inhibitors, glycosides, anti-coagulant, beta-blockers, and tranquilizers.
The surgical procedure includes bypass surgery of the blocked artery, biventricular pacing therapy, implantable cardioverter defibrillator, VAD (Ventricular assist devices) therapy, or heart transplant which is the last resort.
Lifestyle modifications include avoiding salt for fluid retention and limiting intake of caffeine for irregular heartbeats or tachycardia.
Tips to follow for congestive heart failure
The best lifestyle changes for congestive heart failure are as follows-
Monitor your heart health
Go for regular check-ups with your doctor
Carry out routine tests like exercise stress tests, ECG, EKG, and heart monitor by your doctor
Destress yourself
Maintain healthy weight
Voice up your concerns with your doctor
Stay positive
Follow a healthy diet plan
Exercise as advised by your doctor
Have a good and sound sleep
Quit smoking and alcohol.
Conclusion
GS Hospital, the best heart care center in Delhi NCR has helped many patients worldwide to recover from congestive cardiac failure. With a professional team of cardiologists, GS Hospital is focused on providing quality care to every patient at their best. Right from diagnosis to the best medication treatment, the hospital aims to provide holistic heart health care to patients to regain their confidence with the best cardiac health. This makes them a top heart care hospital in Ghaziabad to opt for all heart issues.
#congestive heart failure#Heart Attack#Heart Failure#Heart Hospital#GS Hospital#GS Group#Delhi NCr#Uttar Pradesh#India#Hapur#Ghaziabad
3 notes
·
View notes