#Signs and Symptoms of Malaria
Explore tagged Tumblr posts
Text

11 Most Common Signs And Symptoms Of Malaria Fever at Livlong
Check out the most common signs and symptoms of malaria you should know. Read this blog for more info on the malaria symptoms and treatment at Livlong now!
#malaria symptoms#malaria symptoms and treatment#signs and symptoms of malaria#symptoms of malaria fever#signs of malaria#types of malaria and their symptoms
0 notes
Text

11 Most Common Signs And Symptoms Of Malaria Fever at Livlong
Check out the most common signs and symptoms of malaria you should know. Read this blog for more info on the malaria symptoms and treatment at Livlong now!
#malaria symptoms#malaria symptoms and treatment#signs and symptoms of malaria#symptoms of malaria fever#signs of malaria#types of malaria and their symptoms
0 notes
Text
10 Signs and Symptoms of Malaria
Malaria disease is commonly caused by mosquito bites, In this article, we have discussed the symptoms, causes of transmission, risk, and prevention of malaria disease.
0 notes
Text
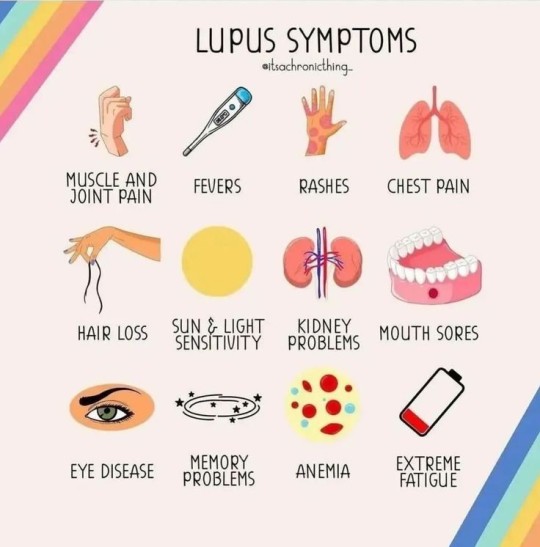
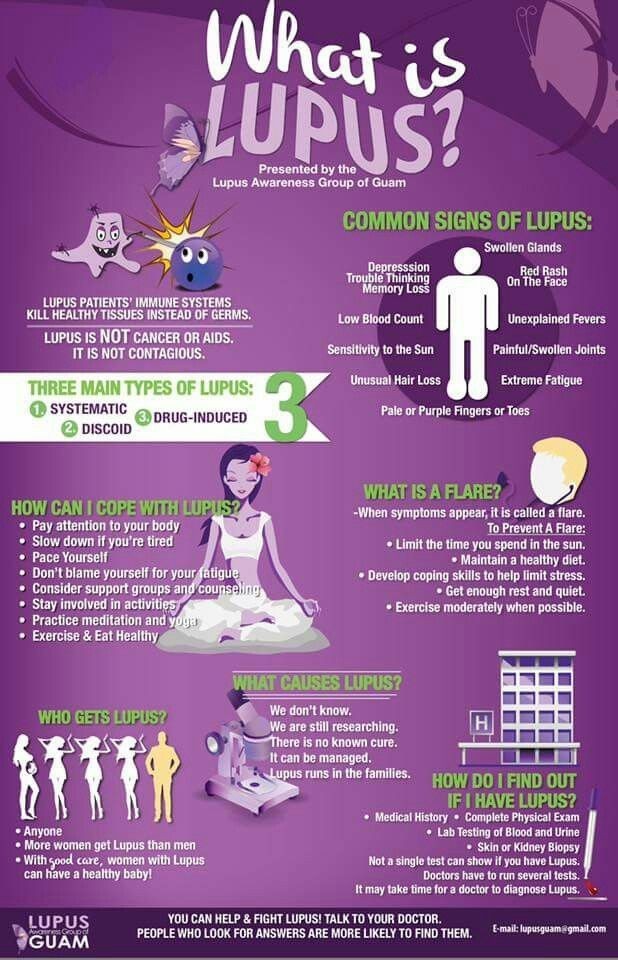
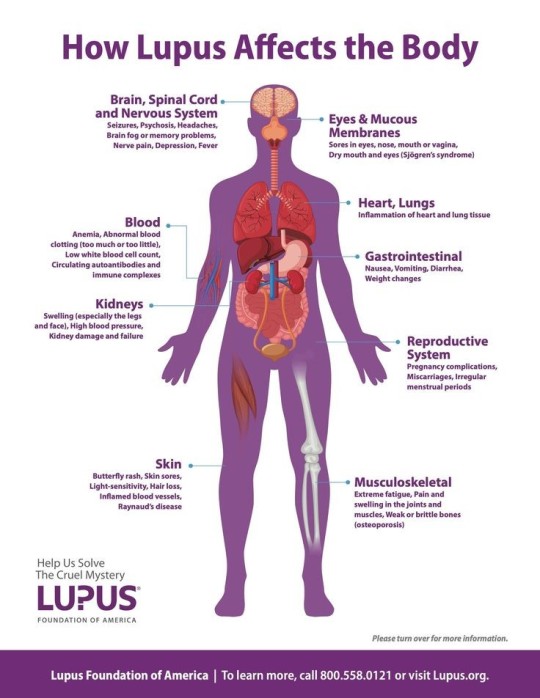
An illness that occurs when the immune system attacks healthy tissues and organs.
Systemic lupus erythematosus is a long-lasting, known as chronic, illness that can affect many parts of the body. These can include joints, skin, kidneys, blood cells, brain, heart and lungs.
Symptoms can come on quickly or slowly. They can get worse for a while, then get better, which is called a flare. A common sign is a rash over the cheeks and nose in the shape of a butterfly. But not everyone gets the rash.
Treatment for systemic lupus erythematosus depends on symptoms. Medicines include pain relievers, medicines used to treat malaria, steroids, biologics and medicines that lower immune system responses.
#lupus#health and wellness#doctor#healthcare#black health#black tumbler#cash app#african american#black americans#health
11 notes
·
View notes
Text
Omegaverse Lore: Blue Fingers Disease
As with the previous omegaverse lore post, I talked about this on @mr-sadman discord, and I'm also posting about it here because sharing is caring. 😊 Again, feel free to use this in your omegaverse stories, as long as you give credit/tag me. Thank you! 🥰
Huge thanks to @sleepsonfutons for coming up with the official medical term for the Blue Fingers Disease, and to @arialerendeair for reminding me to post the lore! 🙇♀️
Thermal Dysregulatory Sensorineural Myocarditis (TDSM), or as it's more commonly known, The Blue Fingers Disease, is a Secondary Gender Disease that can happen to anyone, regardless of their secondary gender, as soon as they reach their majority.
CAUSE
Rejection (or apparent rejection) by one's potential mate.
SYMPTOMS
1.) Low body temperature and unnaturally cold skin
The longer the person is experiencing this disease, the lower their body temperature gets.
This symptom is easier to spot in alphas, whose body temperature run hotter than betas and omegas.
2.) Discoloration of the fingertips
Fingertips during early stage TDSM are a shade paler than the person's skin, while later stages of TDSM sees the person's fingertips turn into shades of blue that grow darker the more the disease progresses.
Fingertips that are almost dark blue are advanced cases, as the person could literally die at any time if not provided with immediate care.
(A sure sign that a person's cause of death is TDSM is when the person has blue-tinged lips immediately after their death, along with dark blue fingertips. The blue shade does not fade over time.)
3.) Intermittent tremor in the hands and poor grip strength
4.) Lethargy
5.) Memory loss and/or confusion
6.) Tendency to space out
7.) Lack of appetite
8.) Vulnerability to seasonal diseases
These include, but are not limited to: the common cold, influenza, and pneumonia, as well as mosquito-borne diseases, such as dengue and malaria.
TREATMENT
Receiving care from other sources, such as family and friends, is a tried and tested way to cure TDSM. But the recovery is slow (taking months or years) and the person is still considered at risk until the blue on their fingertips fade completely.
The quickest way to fully cure the person, of course, would be if they fall in love with someone else, or if the person who initially rejected them returns their love. If this is the case, then it is not unheard of for the person to be cured of TDSM in a single week, though it would still take a couple more weeks for the symptoms to fade completely.
That being said, it is important to note that multiple studies conducted worldwide show that it is more common for TDSM to be cured by the care of others versus the person's feelings changing or their feelings being requited by the person who had initially rejected them.
DURATION
There is no set time for how long this disease lasts until the afflicted person dies. There have been cases where the person only lived for a couple weeks more after the rejection happened, while in rare cases, the person lived for decades after the rejection, before they finally die around the same time as their beloved.
One of the most famous long-lived cases of people who lived with TDSM is St. Francesca,* which caused early Christians to start referring to TDSM as St. Francesca's Disease.
(*It is said that St. Francesca fell in love with a married man and, realizing that it was against the teachings of the church, prayed to God to let her live so she could serve Him all her life.
However, recently discovered evidence suggests that Francesca was actually in love with her fellow nun, Sister Cordelia, who was one of her childhood best friends. When devout Cordelia decided to enter a convent upon her reaching her majority (a decision supported by her religious parents), Francesca allegedly ran away from home to join her.
She had written a note to her older brother that she made the decision to run away 'with both eyes open,' knowing that Cordelia will never return her affections, but willing to suffer TDSM (she used the term The Internal Winter) if it means still being a part of Cordelia's life.
Multiple sources write about how the two remained best friends until their later years, often claiming that Francesca and Cordelia are 'true sisters in the eyes of the Lord,' and that it is rare for one to be seen without the other.
St. Francesca died less than a day after Sister Cordelia did, at age 79, after having TDSM for more than 60 years.
Due to this, people are now theorizing that Sister Cordelia is an aromantic asexual, but that she still loved St. Francesca as her dearest friend, so Francesca did not succumb to the illness or get too sick, as others with TDSM do.
People from their hometown have asked for Sister Cordelia to be made into a saint as well, and they have commissioned statues of the two women to be made. The statues will be placed in the town square, and will depict the two sitting by the fountain, with Sister Cordelia warming St. Francesca's hands.)
There have been claims that the stronger the feelings of the person are, and the harsher the rejection was, affect the time in which the disease accelerates. And while this is a trope often used in literature and popular culture, there is no scientific basis for it as of yet.
STATISTICS
The Blue Fingers Disease is one of the top 10 leading causes of death worldwide, with more than 80% of the people who died being betas and omegas.*
(*As TDSM is more easily detected in alphas, it is possible that betas and omegas often get misdiagnosed with depression during the early stages.)
SECONDARY GENDER DISEASES AWARENESS MONTH
February is Secondary Gender Diseases Awareness Month. The month was chosen primarily for easy recall, as it is the second month of the year. However, February is also the month when new cases of TDSM spike worldwide, due to everyone everywhere celebrating Valentine's Day.
--
Note: In the original discussion, this was supposed to be an alpha-only disease, but for the sake of all the delicious angst, I say it's up to you to decide in your stories who can have this disease. 😊 Enjoy!
#omegaverse#omegaverse lore#i wrote this for#dreamling#the sandman#but it can be used for other pairings in other fandoms#my writing#is this going to be a series? good lord
64 notes
·
View notes
Text
The High Rate Of Diabetes In Congo

In recent years, diabetes has become a growing public health concern in the Democratic Republic of the Congo (DRC), a country traditionally known for infectious diseases like malaria. While attention has primarily focused on combating communicable diseases, the surge in non-communicable diseases (NCDs) like diabetes is an issue that can no longer be ignored. This blog delves into the reasons behind the rising rate of diabetes in Congo, shedding light on the factors contributing to this growing health crisis.
1. Urbanization and Lifestyle Changes
One of the primary contributors to the increasing rate of diabetes in Congo is the rapid urbanization occurring across the country. As people migrate to cities for better job opportunities, they adopt more sedentary lifestyles. Physical activity levels decrease as jobs become less labor-intensive, and there is increased reliance on modern transportation.
Alongside this, urban living brings greater access to processed foods, which are high in sugar and unhealthy fats. These dietary shifts, coupled with reduced physical activity, significantly increase the risk of developing Type 2 diabetes. Traditional diets rich in fiber and low in fat have been replaced by fast foods, sugary beverages, and snacks, creating a perfect storm for the rise of diabetes.
2. Poverty and Limited Access to Healthcare
Congo is one of the poorest countries in the world, and poverty plays a crucial role in the increasing rate of diabetes. With limited financial resources, many people cannot afford regular medical checkups or treatments for chronic conditions. As a result, diabetes often goes undiagnosed and untreated until complications arise.
The healthcare system in Congo is also underdeveloped, with limited access to healthcare professionals, medications, and diagnostic tools. This makes it difficult for individuals with diabetes to manage their condition effectively, leading to poor outcomes and a higher prevalence of complications such as heart disease, kidney failure, and amputations.
3. Lack of Awareness and Education
A lack of public awareness and education about diabetes is another factor contributing to the rise of the disease in Congo. Many people are unaware of the signs and symptoms of diabetes, which leads to delayed diagnosis. Additionally, misconceptions about the disease are prevalent, and some people may attribute its symptoms to other health conditions or even spiritual causes.
Without adequate education, people are less likely to adopt healthy lifestyle changes, such as improving their diet or increasing physical activity, both of which are critical in preventing and managing diabetes.
4. Genetic Predisposition
Genetics also plays a role in the increasing prevalence of diabetes in Congo. Some populations may be more genetically predisposed to developing the disease, especially if combined with environmental factors like poor diet and lack of exercise. Studies show that individuals of African descent are at higher risk of developing Type 2 diabetes compared to other ethnic groups.
5. Post-Conflict Stress and Trauma
The DRC has been plagued by decades of conflict and political instability, which has left many people traumatized and displaced. Chronic stress and trauma can lead to elevated blood sugar levels, increasing the risk of developing diabetes over time. The stress of daily survival, poor living conditions in refugee camps, and the lingering effects of war all contribute to the rise of diabetes in the country.
6. Inadequate Policy Responses and Health Infrastructure
While Congo has made strides in addressing communicable diseases, efforts to combat non-communicable diseases like diabetes have lagged behind. The country lacks comprehensive national policies for diabetes prevention and control. Public health campaigns targeting diabetes awareness are minimal, and there is a shortage of trained healthcare providers to diagnose and treat the disease.
Without a strong healthcare infrastructure in place, individuals with diabetes are left to fend for themselves, often turning to traditional healers or home remedies that may not be effective in managing the condition.
7. Consequences of the Diabetes Epidemic
The rising tide of diabetes in Congo has far-reaching consequences. As more people develop diabetes, the burden on the healthcare system intensifies, further straining already limited resources. The economic impact is also significant, as individuals with diabetes often miss work due to illness, reducing productivity and income.
Moreover, diabetes-related complications, such as blindness, amputations, and kidney disease, place additional stress on families and communities, making it difficult to break the cycle of poverty and poor health.
Conclusion: Addressing the Growing Diabetes Crisis in Congo
The rise of diabetes in Congo is a complex issue driven by multiple factors, including urbanization, poverty, lack of awareness, and inadequate healthcare infrastructure. To combat this growing epidemic, Congo must invest in education and awareness campaigns that emphasize the importance of healthy eating and regular physical activity. Additionally, improving access to healthcare services and ensuring early diagnosis and treatment are crucial steps in reducing the burden of diabetes on the population.
Addressing the diabetes crisis in Congo requires a multi-faceted approach, combining public health interventions, policy changes, and community engagement. With the right resources and strategies, it is possible to slow the spread of diabetes and improve the quality of life for those affected by the disease.
2 notes
·
View notes
Text
Similarly, for as much flak as the Humor theory gets it is surprisingly sound and when applied correctly rather effective -
Because Humoral theory is based on food.
Yes, it's based on blood. The four humors are, in fact, the components of blood. Phlegm is white blood cells. Cholera or yellow bile is Plasma. Bile, black bile or Melancholera is dead red blood cells and platelets. Blood or Blud is the living red cells.
By filling a clear flask with a person's blood one could see whether they had an excess or deficit of any one, since blood settles in layers. and a specialised diet would be prescribed to help aid them. Conditions of Humor were often indicated by whatever a person's blood had in excess, and so if, for instance, you were particularly Choleric, too much plasma, or your blood is too thin, you would be fed/prescribed a very carb and iron/meat heavy diet, which would restore your apparent anemia. Chronic Anemia, by the way, has a reputation for making people very cranky and unpredictable, hence descriptions of Choleric people being easily flustered and snappy.
Similarly if one had too much Phlegm, white blood cells, it was well understood that you were very sick - phlegmatic people needed a simple, digestible diet so they could get better.
Black bile, also called Melancholera, was associated with depression and sadness, but also delusions, mood swings, and insanity. There are a lot of conditions which cause your red blood cells to die and sink in excess (something now called a sedimentation rate) though there was one extremely common ailment of the European continent for most of its history: Malaria. The four species of malaria in Europe in particular can cause weird mood issues in some people, narcoleptic symptoms in others, and overall makes you feel listless and generically unwell, though the symptoms can be hard to pin down.
Other causes of this increased sedimentation rate can hearken to genetic blood and tissue disorders, Lyme disease in later centuries, tuberculosis (which was and is fairly common) early signs of Plague, now-extinct species of the Dengue virus, and critically rabies.
Various nutritional deficiencies, including scurvy as it would happen, along with vitamin D deficiency, could also cause Melancholera. Because the causes could be so abstract and hard to pin down, Melancholy as it became known was very hard to treat, and became the bane of many a physicians existence. However, it also lead to a very "throw everything at it and hope it works" approach that the Humor method is so infamous for. In spite of that, the usual means of treating melancholy were to prescribe anti malaria medicine (in the form of slippery elm bark if im not mistaken) if it was the right season, and encouraging those afflicted to spend time outside, socialise, and eat a whole lot of rich and spicy food. Fruits preserved in honey, wine, fat or mead don't lose their vitamin C too much, and cider was so popular in the middle ages it wasn't even funny. Cider keeps most it's vitamin C, though admittedly there's not much to begin with. Fish, onion, garlic, and licorice or anise, along with mint and sage and coriander were all strongly pushed. Fish has vitamin D in it, onions and garlic have quite a bit of vitamin C, licorice has mood stabilising effects and aids digestion, as does anise (part of why it was so common to add to wines) mint and sage have a decent amount of Zinc, without which you can not absorb iron or process vitamin D, E, or C, and Coriander (cilantro seeds) has a mild stimulant effect if you chew the raw, whole seeds, which can have a mood boosting effect.
Of course no one using Humoral theory really understood the complexities, but they did understand that the food we eat becomes part of our blood, (which I will get to) which in turn sustains us. So much of humoral theory was centered on the use of food as medicine.
One exceedingly infamous exception, kind of, is an excess of red blood. Too much red blood meant something was going wrong, very wrong, and that it needed to be gotten out of you NOW.
So while dietary prescriptions were definitely implemented, especially in the earlier medieval period, before 1500, it became increasingly common after that point to simply bleed a person. This was sometimes done with Melancholy too, increasingly toward the end of the Renaissance when politics and plague destroyed a good chunk of generational knowledge about how these things worked.
Excess red blood was associated with being excitable, manic, and famously hysteric. Insanity and delusions of its own sort was associated with too much blood, which was otherwise considered a very good thing to have a decent amount of.
However the kinds of conditions which actually cause an excess of red blood cells basically boils down to rare forms of skeletal tuberculosis, bone cancers, and oddly enough poisoning. Poisoning by what, specifically, is not fully understood, though mercury, lead and especially copper poisoning can cause the blood to carry a bit of a different hue. Some plants can cause this effect as well, most tellingly being Evening primrose - a plant that produces nasty anticoagulants and has been used as an aborteficent since Roman times. Little wonder young women up to "trouble" would sometimes go nuts for seemingly no reason - evening primrose is also slightly hallucinogenic. Another plant guilty of similar effects on the blood and mind is a kind of fern known only as "blackroot" - most likely a type of bracken, but no one's entirely sure what species since braken is usually edible. It's been suggested it's not the fern, but a fungus growing around the rhizome of the fern, which bears the name. But we do know it was used as both medicine and to induce abortion, and that it could have troubling side effects like mania and hallucinations. (Sure sounds like a shroom to me).
Point being that ancient people were no less smart or observant than you or I today, they just didnt have access to the kinds of information we do now. Nonetheless they knew what they were doing well enough to say it was no mere accident our species still survives.
And speaking of scurvy, I am eternally amused by the thing where some ancient form of healing that was born in a time where people didn't know exactly how the human body works, or what causes it to stop working sometimes, that still somehow worked. Like how so many old folk medicinal plants were listed as a cure for various ailments that - from a modern view - are clearly just symptoms of scurvy, and the plant itself is rich in vitamin C.
I recall reading some story, no recollection of the exact time or place, where the king of a large empire suffered from constant horrible headaches and was incapable of falling asleep unless drugged or blackout drunk. Sick of taking temporary fixes to dull the pain and having to be sedated every night, he called up some old sage healer who was said to know how to fix things nobody else could explain, and the healer heard his symptoms and went
"Hmm. You spend too much time being a king. Your skull is packed so full of kingly thoughts that they don't all fit in there and that's why your head is in pain. You need to spend time not being a king." And prescribed him to schedule three days every month where he must go to a peasant village where nobody knows he's the king, live with a family there under a fake name and identity, work in the rice fields with them, eating the same food and sleeping on the same mats. Absolutely nobody is allowed to address him as the king, speak to him of any royal or political matters, and he himself is not allowed to think any kingly thoughts or think of himself as the king.
And naturally, this worked. Taking a regular scheduled break from a highly stressful office desk job to completely decompress, paired with physical exercise in the form of hard but simple physical labour, plain and simple food and Just Not Thinking About Your Fucking Job All The Time does help chronic stress, which here was worded as "spending too much time being a king clogs your brain."
Sometimes you do have ghosts in your blood, though I'm not entirely sure whether you should do cocaine about it.
49K notes
·
View notes
Text
Acute Infection Therapy in Dubai: A Complete Guide

Acute infections are sudden-onset illnesses caused by bacteria, viruses, fungi, or parasites. These infections can spread rapidly and require prompt medical attention to prevent complications. Common acute infections include influenza, pneumonia, urinary tract infections (UTIs), gastroenteritis, and skin infections.
Dubai is renowned for its state-of-the-art healthcare facilities that offer advanced acute infection therapy. If you are experiencing symptoms of an acute infection, immediate medical consultation is essential for a swift recovery.
Symptoms of Acute Infections
The symptoms of acute infections vary depending on the cause and severity. Common signs include:
High fever and chills
Fatigue and weakness
Cough, congestion, or breathing difficulties
Nausea, vomiting, or diarrhea
Skin rashes or irritation
Pain or swelling in affected areas
Sore throat or ear pain
If any of these symptoms persist, seek professional medical care in Dubai for accurate diagnosis and appropriate treatment.
Causes of Acute Infections
Acute infections can result from different types of microorganisms, including:
1. Bacterial Infections
Bacteria can cause infections such as:
Strep throat (Streptococcus bacteria)
Urinary tract infections (E. coli)
Bacterial pneumonia
Skin infections (Staphylococcus bacteria)
2. Viral Infections
Viruses spread through respiratory droplets, physical contact, or contaminated surfaces. Common viral infections include:
Influenza (Flu)
Common cold (Rhinovirus)
COVID-19 (Coronavirus)
Gastroenteritis (Norovirus, Rotavirus)
3. Fungal Infections
Fungal infections are more common in individuals with weakened immune systems. Examples include:
Candidiasis (Yeast infections)
Ringworm
Fungal skin infections
4. Parasitic Infections
Parasitic infections are more common in certain climates and can include:
Malaria (Plasmodium parasite)
Giardiasis (Giardia parasite)
Intestinal worm infections
Diagnosis of Acute Infections
Early diagnosis is key to effective acute infection therapy in Dubai. Medical professionals use various diagnostic tools, including:
Physical Examination: Evaluating symptoms and medical history.
Blood Tests: Detecting infections and inflammation markers.
Urine Analysis: Identifying urinary tract infections.
Imaging Tests: X-rays, CT scans, and ultrasounds for detecting internal infections.
Culture Tests: Identifying the causative pathogen from throat, skin, or wound samples.
Treatment for Acute Infections in Dubai
Dubai offers world-class treatment options for acute infections, ensuring rapid recovery and symptom relief. These include:
1. Antibiotic Therapy
Bacterial infections are treated with antibiotics such as:
Amoxicillin (Penicillins)
Ceftriaxone (Cephalosporins)
Azithromycin (Macrolides)
Ciprofloxacin (Fluoroquinolones)
2. Antiviral Medications
Antiviral drugs target infections such as flu and COVID-19, including:
Oseltamivir (Tamiflu) for influenza
Remdesivir for COVID-19
Antiretroviral therapy for viral hepatitis
3. Antifungal Medications
Fungal infections require specific treatments, including:
Fluconazole (for yeast infections)
Terbinafine (for fungal skin infections)
4. Antiparasitic Treatment
Parasitic infections require targeted medications such as:
Artemisinin-based therapy for malaria
Metronidazole for giardiasis
5. Supportive Care
Additional supportive measures help speed up recovery:
IV Fluids: Prevent dehydration and maintain electrolyte balance.
Pain Relievers: Paracetamol or ibuprofen to reduce fever and discomfort.
Oxygen Therapy: Used for severe respiratory symptoms.
Why Choose Dubai for Acute Infection Therapy?
Dubai is recognized globally for its high-quality healthcare services. Key benefits of seeking acute infection treatment in Dubai include:
1. Advanced Medical Technology
Dubai’s hospitals and clinics use the latest diagnostic tools and treatment technologies, ensuring accurate diagnoses and effective care.
2. Expert Healthcare Professionals
Highly trained doctors and infectious disease specialists provide comprehensive infection management, ensuring top-tier medical care.
3. Fast and Efficient Services
Dubai’s healthcare system offers quick testing, same-day consultations, and emergency care, ensuring that patients receive timely treatment.
4. High Standards of Hygiene and Safety
Dubai follows strict international healthcare standards, ensuring exceptional infection control and patient safety.
Preventing Acute Infections
Preventive measures can significantly reduce the risk of acute infections. Here are some key prevention tips:
Maintain Proper Hand Hygiene: Wash hands regularly with soap and water.
Get Vaccinated: Stay up to date with flu shots, COVID-19 vaccines, and other immunizations.
Boost Your Immune System: Eat a balanced diet, exercise regularly, and get sufficient rest.
Avoid Contact with Infected Individuals: Minimize exposure to people showing symptoms of illness.
Use Protective Gear: Wear face masks in crowded areas and maintain personal hygiene.
Need Acute Infection Therapy in Dubai?
If you’re experiencing symptoms of an acute infection, visit Rama Care Polyclinic in Dubai, Jumeirah 1 for expert medical care. Our healthcare professionals provide personalized, high-quality acute infection treatment for a speedy recovery.
Visit ramacarepolyclinic.com to learn more about our services and book an appointment today!
0 notes
Text
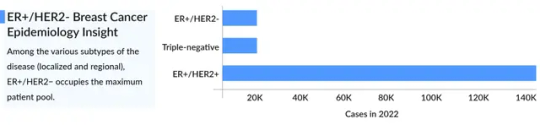
Understanding Metastatic HER2-Positive Breast Cancer
What is Metastatic HER2-Positive Breast Cancer?
HER2-positive breast cancer is a subtype identified by an overexpression of the HER2 protein, which accelerates cancer cell growth. When the cancer extends beyond the breast and nearby lymph nodes to distant organs, it is classified as metastatic HER2-positive breast cancer. Due to its aggressive nature, this condition typically requires specialized HER2-targeted therapies.
Symptoms of HER2-Positive Breast Cancer
The symptoms of HER2-positive breast cancer depend on the organs affected. Common signs include:
Persistent cough
Bone pain
Shortness of breath
Severe headaches
Jaundice
Unexplained weight loss Other indicators may include skin changes, swollen lymph nodes, and chronic fatigue. Early detection and symptom management are crucial for improving patient outcomes.
Prevalence of HER2-Positive Breast Cancer Cases
HER2-positive breast cancer accounts for approximately 15-20% of all breast cancer cases. A significant portion of these cases progress to stage 4 HER2-positive breast cancer, contributing to the overall HER2-positive metastatic breast cancer landscape. While advancements in treatment have led to better survival rates, this form of cancer remains a global challenge.
HER2-Targeted Therapies for Metastatic HER2-Positive Breast Cancer
Several leading pharmaceutical companies, such as Roche, Merck, and Immunomedics, have developed innovative HER2-targeted therapies. Notable treatments include:
Trastuzumab (Herceptin)
Pertuzumab (Perjeta)
Trastuzumab deruxtecan (Enhertu) These therapies have significantly improved survival rates and quality of life. Researchers are also exploring immunotherapies and combination treatments for enhanced effectiveness.
The HER2 Breast Cancer Pipeline: Future Prospects
The HER2 breast cancer pipeline continues to expand with promising new therapies undergoing clinical trials. Research efforts focus on:
Novel HER2 inhibitors
Antibody-drug conjugates
Advanced immunotherapies Companies like Roche and Merck are at the forefront of HER2-positive metastatic breast cancer research, aiming to develop more effective treatment options.
Conclusion
Advancements in the HER2-positive breast cancer market are revolutionizing treatment approaches, offering hope for improved survival rates. As HER2-positive metastatic breast cancer research progresses, early detection and targeted therapy remain crucial in managing the disease effectively. With ongoing clinical trials and new therapeutic innovations, the future holds promise for better treatment options and improved patient outcomes.
Another Reports Offered By Delveinsight
Liquid Biopsy for Cancer Diagnostics Market | Plasmodium Vivax Malaria Market | Polycystic Ovarian Syndrome Market | Short Bowel Syndrome Drugs Market | Somatotropin Deficiency Market | Temporomandibular Disorders Market | Testicular Neoplasm Market |Venous Ulcer Market | Adeno-Associated Viruses (AAV) Gene Therapy Market | Blastomycosis Market | Carcinoid Syndrome Market | Congenital Heart Defect Market | CXCR Inhibitors Market | Hip Replacement Devices Market | Myeloproliferative Neoplasms Market | Nocturia Market | Percutaneous Arterial Closure Device Market | Peripheral SpA Market | Psoriasis Vulgaris Market | Radial Artery Compression Device Market | Schistosomiasis Market | Type 1 Diabetes Market | Vital Sign Monitors Devices Market | Atherosclerosis Market | Avascular Necrosis Market | Gene Therapy in CNS Disorder Market | Pediatric Neuroblastoma Market | Spinal Trauma Devices Market | Surgical Lasers Market | Thyroid Cancer Market | Ventral Hernia Market
Contact Information
Kanishk
0 notes
Text
The Role of Big Data in Predicting Disease Outbreaks
In an era of rapid technological advancements, the integration of data science and public health has emerged as a transformative force. Big data, with its immense capacity to process vast amounts of information, is reshaping how we predict and respond to disease outbreaks. From identifying early warning signs to forecasting potential hotspots, big data analytics provides a powerful framework for mitigating the impact of infectious diseases on global populations.
The Evolution of Disease Surveillance
Traditional disease surveillance systems have relied on manual reporting from healthcare providers, laboratories, and government agencies. While these methods remain crucial, they often suffer from delays, incomplete data, and geographic limitations. Big data, however, has revolutionized this process by leveraging real-time information from diverse sources, enhancing predictive capabilities.
Big data encompasses structured and unstructured datasets generated by digital interactions, social media platforms, wearable devices, electronic health records (EHRs), satellite imagery, and more. By integrating these diverse streams, researchers can develop comprehensive models that detect patterns indicative of emerging health threats. This shift from reactive to proactive surveillance marks a significant advancement in epidemiology. With the growing demand for skilled data analysts, institutions offering data analytics courses in Noida are equipping professionals with the necessary expertise to harness big data for health analytics and outbreak prediction.
Harnessing Real-Time Insights
One of the most significant contributions of big data is its ability to provide real-time insights. Social media platforms serve as dynamic repositories of human behavior and sentiment. During outbreaks, people frequently share symptoms, concerns, and experiences online. By applying natural language processing (NLP) algorithms, experts can analyze these discussions to detect anomalies and identify potential outbreaks.
Similarly, search engine queries offer a valuable source of health data. When individuals experience unusual symptoms, they often turn to search engines for answers. Aggregating anonymized query trends enables analysts to pinpoint regions where certain conditions may be spreading before official reports emerge. This method proved invaluable during the early stages of the COVID-19 pandemic when search trends indicated heightened interest in flu-like symptoms weeks ahead of confirmed cases.
Leveraging Environmental Data
Environmental factors play a crucial role in disease transmission, making them essential inputs for predictive modeling. Satellite imagery and climate sensors provide continuous updates on variables such as temperature, humidity, rainfall, and vegetation cover—all of which influence vector-borne diseases like malaria and dengue fever. Machine learning algorithms can analyze these environmental metrics alongside historical outbreak data to anticipate future flare-ups.
Moreover, urbanization trends and population density maps derived from mobile phone usage patterns help in understanding human movement dynamics. These insights assist in identifying areas at risk of becoming epicenters for disease spread, allowing for targeted interventions. To further advance expertise in this field, professionals are turning to data analytics training in Jaipur, which provides hands-on experience in analyzing complex datasets and applying predictive modeling techniques.
Bridging Gaps in Healthcare Infrastructure
In low-resource settings, where traditional healthcare infrastructure may be lacking, big data fills critical gaps. Mobile health applications and wearable technologies empower individuals to monitor their health metrics and report symptoms digitally. This grassroots-level data collection not only aids personal well-being but also contributes to broader epidemiological analyses.
Additionally, partnerships between tech companies and public health organizations facilitate access to anonymized mobility data. Such collaborations enable the creation of heatmaps that track population flows across borders, cities, or neighborhoods. These visualizations are instrumental in designing containment strategies and allocating resources efficiently.
Challenges and Ethical Considerations
Despite its immense potential, utilizing big data for disease prediction comes with challenges. Privacy concerns are a significant issue, especially when dealing with sensitive health information. Striking a balance between data utility and individual rights requires robust encryption protocols, transparent consent mechanisms, and adherence to ethical guidelines.
Data quality and standardization present additional hurdles. Inconsistencies in data collection, storage, and interpretation can lead to inaccuracies in predictions. Moreover, biases embedded within datasets—whether due to underrepresentation of marginalized communities or algorithmic flaws can skew results and exacerbate existing health disparities.
To address these challenges, interdisciplinary collaboration is crucial. Epidemiologists, data scientists, ethicists, and policymakers must work together to refine methodologies, validate findings, and ensure that big data tools are used equitably.
A Paradigm Shift in Public Health
Big data represents more than just a technological innovation; it signifies a paradigm shift in how we approach public health crises. By synthesizing vast amounts of information into actionable insights, it enables decision-makers to act swiftly and effectively. Early detection of outbreaks reduces morbidity and mortality rates, while optimized resource allocation minimizes economic strain.
Looking ahead, advancements in artificial intelligence (AI) and quantum computing promise even greater precision in disease prediction. AI-driven simulations could model complex scenarios with unprecedented accuracy, while quantum algorithms might solve optimization problems at speeds previously unattainable.
Building a Career in Data Analytics
As the demand for skilled data professionals continues to grow, institutions like DataMites are offering comprehensive training programs to equip individuals with expertise in data analytics. DataMites’ certified data analyst courses provide in-depth knowledge of data handling, predictive analytics, and machine learning applications in public health and other industries.
With DataMites, learners can benefit from both online and offline data analytics training, covering topics essential for real-world applications. The program includes 10 capstone projects and 1 client project, ensuring hands-on experience. Moreover, DataMites offers industry-recognized certifications from IABAC® and NASSCOM® FutureSkills, along with internship opportunities and job placement support.
For those looking to advance their careers, DataMites provides offline data analytics courses in Noida, Jaipur, Pune, Bangalore, Mumbai, Hyderabad, Chennai, Coimbatore, Ahmedabad, and other major Indian cities. With expert guidance and practical training, DataMites serves as the ideal launchpad for a successful career in data analytics.
Big data is shaping the future of public health, and those equipped with the right skills will be at the forefront of this transformation. By enrolling in specialized training programs, aspiring data analysts can contribute to groundbreaking advancements in disease prediction and prevention.
#DataAnalystFuture#DataAnalyticsCareerJaipur#DataAnalyticsCareerNoida#DataAnalystCareerPath#DataAnalyticsCourse#DataAnalystTraining#DataAnalystCourse
0 notes
Text
Comprehensive Guide to Medical Diseases and Conditions

Medical Diseases and Conditions: A Comprehensive Overview
Medical diseases and conditions are a broad spectrum of health issues that affect individuals worldwide, ranging from acute illnesses to chronic and life-threatening disorders. These conditions can significantly impact physical, mental, and emotional well-being, underscoring the importance of understanding their causes, symptoms, treatments, and prevention strategies.
Types of Medical Diseases and Conditions
1. Infectious Diseases
Infectious diseases are caused by pathogens such as bacteria, viruses, fungi, or parasites. Examples include tuberculosis, influenza, malaria, and COVID-19. These diseases can spread through various means, including direct contact, airborne particles, or contaminated surfaces. Vaccines, antibiotics, and public health measures like hygiene and sanitation play a vital role in controlling these diseases.
2. Chronic Diseases
Chronic diseases persist over an extended period and often require ongoing medical attention. Conditions such as diabetes, hypertension, arthritis, and cardiovascular diseases fall into this category. These illnesses are frequently linked to lifestyle factors, such as poor diet, physical inactivity, and smoking, making lifestyle changes crucial for management and prevention.
3. Genetic and Congenital Disorders
Genetic disorders like sickle cell anemia, cystic fibrosis, and hemophilia are caused by inherited mutations. Congenital disorders, such as spina bifida, occur due to developmental anomalies during pregnancy. Advances in genetic testing have facilitated early diagnosis and personalized treatments for these conditions.
4. Mental Health Disorders
Mental health conditions, including depression, anxiety, and schizophrenia, affect emotional and cognitive functioning. Awareness and treatment of mental health disorders have grown significantly, highlighting the importance of therapy, medications, and community support in addressing these issues.
5. Cancers
Cancer is characterized by the uncontrolled growth of abnormal cells. Common types include breast, lung, and prostate cancer. Early detection through screenings and advancements in treatment, such as chemotherapy, immunotherapy, and targeted therapy, have improved survival rates and outcomes.
6. Autoimmune and Inflammatory Diseases
Autoimmune diseases like lupus and rheumatoid arthritis occur when the immune system mistakenly attacks healthy tissues. These conditions often require immunosuppressive medications to manage inflammation and prevent complications.

Causes and Risk Factors
Medical conditions arise due to a combination of factors:
Pathogens: Infections by microorganisms.
Genetics: Inherited traits or mutations.
Lifestyle: Unhealthy habits like smoking, excessive alcohol consumption, and poor diet.
Environmental Factors: Exposure to toxins, pollution, and occupational hazards.
Aging: Age-related degeneration of bodily functions.
Symptoms and Diagnosis
The symptoms of medical conditions vary widely, ranging from mild to severe. Common indicators include:
Pain or discomfort.
Fever, chills, or fatigue.
Swelling, rashes, or skin changes.
Unexplained weight changes.
Breathing difficulties or abnormal heart rhythms.
Diagnosis involves a thorough process:
Medical History: Gathering information about symptoms, family history, and lifestyle.
Physical Examination: Identifying physical signs of disease.
Diagnostic Tests: Blood tests, imaging (e.g., X-rays, MRIs), and biopsies confirm specific conditions.
Treatment Approaches
Treatment varies depending on the disease and its severity:
Medications: Antibiotics, antivirals, insulin, and chemotherapy are examples of treatments tailored to specific conditions.
Therapies: Physical, occupational, and mental health therapies improve functionality and quality of life.
Surgical Interventions: Required for conditions like appendicitis, cancers, or congenital abnormalities.
Lifestyle Changes: Adopting a balanced diet, regular exercise, and stress management is vital for chronic disease management.
Prevention Strategies
Preventing diseases is better than treating them. Strategies include:
Vaccination: Protecting against infectious diseases like measles and polio.
Healthy Lifestyle: Regular exercise, a nutritious diet, and adequate sleep.
Hygiene Practices: Handwashing and safe food handling reduce infection risks.
Regular Screenings: Detecting diseases like cancer or hypertension early.
Avoiding Risk Factors: Reducing exposure to smoking, alcohol, and toxins.
Technological Advancements in Healthcare
Modern technology has transformed disease management:
Telemedicine: Enables remote consultations and monitoring.
Wearable Devices: Track vital signs like heart rate and blood sugar.
AI and Machine Learning: Assist in early diagnosis, personalized treatment, and predicting disease trends.
Challenges in Disease Management
Despite advancements, challenges persist:
Healthcare Disparities: Access to care is unequal across populations.
Antimicrobial Resistance: Overuse of antibiotics has created resistant strains.
Emerging Diseases: Novel infections, like COVID-19, strain healthcare systems.
0 notes
Text
Symptoms of Malaria: What You Need to Know

Malaria is a life-threatening sickness because of Plasmodium parasites transmitted to human beings via the chunk of inflamed Anopheles mosquitoes. Despite being preventable and treatable, in term of medical healthcare malaria stays a sizable worldwide fitness issue, mainly in tropical and subtropical regions. Recognizing the signs early may be important for powerful remedy and recovery. Below are the number one and much less not unusualplace signs of malaria which you ought to be conscious of.
Primary Symptoms of Malaria
Malaria signs commonly seem 10–15 days after being bitten with the aid of using an inflamed mosquito. The severity and sort of signs can range relying at the species of Plasmodium inflicting the infection. The maximum not unusualplace signs include:
1. Fever and Chills
Recurring fever is one of the hallmark signs of malaria. It frequently gives in a cyclical pattern, observed with the aid of using extreme chills and shivering.
2. Headache
Severe complications are not unusualplace and may be persistent, including to the pain and fatigue because of the fever.
3. Sweating and High Temperature
Following the fever and chills, immoderate sweating happens because the fever breaks. Body temperatures can upward push above 40°C (104°F).
4. Fatigue and Weakness
Extreme tiredness and weak point frequently comply with the fever episodes, making easy every day duties difficult.
5. Nausea and Vomiting
Digestive issues, together with nausea, vomiting, and coffee diarrhea, can arise, mainly in children.

Less Common Symptoms of Malaria
In intense cases, in particular with Plasmodium falciparum, the maximum risky species, the subsequent signs may additionally seem. Seeking timely medical healthcare is crucial to ensure proper diagnosis, treatment, and recovery.
1. Muscle and Joint Pain
Body aches, muscle stiffness, and joint ache might also additionally resemble flu-like signs.
2. Jaundice
Yellowing of the pores and skin and eyes might also additionally arise because of liver involvement, indicating headaches like intense hemolysis or liver dysfunction.
3. Rapid Breathing and Heart Rate
Increased respiration and coronary heart quotes can sign headaches or intense malaria.
4. Seizures and Confusion
Neurological signs including seizures, confusion, or even coma can arise in cerebral malaria, a extreme trouble of P. falciparum infection.
5. Dark Urine
Dark or tea-coloured urine, frequently called “blackwater fever,” is a unprecedented however intense trouble because of huge purple blood mobileular destruction.
When to Seek Medical Attention
Malaria can hastily development from moderate to intense, main to organ failure, intense anemia, and loss of life if untreated. Seek medical healthcare instant scientific interest in case you or a person you recognize stories any of the subsequent:
Persistent excessive fever
Severe headache or confusion
Difficulty respiratory
Vomiting and dehydration
Conclusion
Malaria is a extreme but preventable sickness. Awareness of its signs is crucial, mainly for vacationers journeying malaria-endemic regions. Prompt analysis and remedy can substantially lessen the danger of intense headaches. If you believe you studied malaria, go to a medical healthcare company straight away for a diagnostic check and suitable remedy.
Stay knowledgeable and shield your self with the aid of using the use of mosquito nets, insect repellents, and antimalarial medicines while travelling to excessive-danger areas. Early detection saves lives.
0 notes
Text
Understanding Liver Swelling: Causes, Symptoms, and Treatments in Jaipur
Liver swelling, also known as hepatomegaly, is a condition where the liver becomes enlarged due to various underlying causes. The liver plays a crucial role in detoxifying the body, producing essential proteins, and aiding digestion. When the liver swells, it can affect these functions, leading to significant health concerns. In Jaipur, there are numerous treatment options available, ranging from medication to lifestyle changes. In this blog, we’ll discuss the causes, symptoms, and Best Liver Swelling Treatment options available in Jaipur to help you manage and overcome this condition.
What is Liver Swelling?
The liver is a vital organ located in the upper right side of the abdomen. It typically weighs about 1.5 kilograms and has a smooth, soft texture. When the liver swells, it becomes larger than usual, which may lead to discomfort or other complications. Liver swelling can occur as a result of several factors, including viral infections, liver diseases, and other metabolic conditions.
Causes of Liver Swelling
Several conditions can lead to liver swelling. Here are some of the most common causes:
Viral Hepatitis: Hepatitis A, B, and C are viral infections that can lead to inflammation and swelling of the liver. Chronic hepatitis, especially Hepatitis B and C, can lead to severe liver damage if left untreated.
Fatty Liver Disease: Both alcoholic and non-alcoholic fatty liver disease (NAFLD) can cause the liver to swell. NAFLD is commonly linked to obesity, diabetes, and high cholesterol.
Liver Cirrhosis: Cirrhosis is the scarring of liver tissue that results from chronic liver disease. As the liver becomes scarred, it may swell and lose its ability to function effectively.
Liver Tumors: Both benign and malignant tumors can cause liver swelling. In some cases, liver cancer or metastasis from other cancers can lead to noticeable swelling.
Congestive Heart Failure: Poor circulation caused by heart failure can lead to blood backing up in the liver, causing it to swell.
Hemochromatosis: This condition causes excess iron to accumulate in the body, which can damage the liver and lead to swelling.
Infections and Parasites: Certain infections, including malaria and liver abscesses, can also cause inflammation and swelling of the liver.
Symptoms of Liver Swelling
While liver swelling may not always present obvious symptoms, some common signs to watch for include:
Pain or discomfort in the upper right abdomen: This is often the first symptom of liver swelling. The pain may be dull or sharp, and it could worsen after eating fatty foods.
Jaundice: Yellowing of the skin or eyes occurs when the liver is not functioning properly, and bilirubin (a waste product) builds up in the bloodstream.
Fatigue: If the liver is not functioning properly, you may feel unusually tired or weak.
Swelling in the legs or abdomen: Ascites (fluid retention) can occur due to liver dysfunction, leading to visible swelling in the belly and legs.
Nausea and vomiting: Digestive problems may arise as the liver struggles to break down toxins.
Dark urine or pale stool: A swollen liver often disrupts the production and excretion of bile, affecting stool color and urine appearance.
Diagnosing Liver Swelling
If you suspect liver swelling, it is important to consult a healthcare provider immediately. A doctor may perform various tests to diagnose the condition, including:
Physical Examination: The doctor may feel for an enlarged liver during a routine examination.
Blood Tests: These tests check for liver enzymes, bilirubin levels, and other indicators of liver function.
Ultrasound: An ultrasound is a common imaging test that helps doctors visualize the liver’s size and any abnormalities.
CT Scan or MRI: In certain cases, advanced imaging tests may be used to get a detailed look at the liver and its surrounding structures.
Liver Swelling Treatment in Jaipur
The Best Liver Swelling Treatment depends on the underlying cause of the condition. In Jaipur, several medical centers and hospitals offer specialized care for Liver Swelling Treatment. Treatment may involve medications, lifestyle changes, or in severe cases, surgery. Here are some common approaches:
Medications: If your liver swelling is due to an infection (e.g., viral hepatitis), your doctor may prescribe antiviral medications. For fatty liver disease or cirrhosis, medications that help reduce inflammation or manage symptoms can be prescribed.
Lifestyle Changes: Maintaining a healthy diet and losing excess weight are essential steps in managing liver swelling. Avoiding alcohol, reducing fat intake, and eating foods rich in antioxidants, such as fruits and vegetables, can help prevent further liver damage.
Liver Transplant: In severe cases of liver failure, a liver transplant may be necessary. However, this option is only considered when other treatments fail, and the liver is no longer functional.
Surgical Interventions: If liver tumors or abscesses are causing swelling, surgical removal of the affected area may be required.
Alternative Therapies: Some patients in Jaipur opt for holistic treatments, including herbal remedies and acupuncture, to complement their medical treatment. However, it is essential to consult with a doctor before pursuing any alternative therapies.
Best Liver Swelling Treatment in Jaipur
When seeking Liver Swelling Treatment in Jaipur, it’s crucial to find a medical center with the experience and expertise necessary for effective diagnosis and treatment. Jaipur is home to several renowned hospitals offering specialized services, including liver care centers with the latest diagnostic tools and treatment options. Look for facilities with expert hepatologists and liver surgeons who can provide tailored care and treatment plans.
Conclusion
Liver swelling can be a sign of a serious underlying health condition, but with early detection and proper treatment, many patients can manage the symptoms effectively. If you're experiencing any symptoms of liver swelling, seeking professional medical advice from experienced specialists is crucial. Whether you are looking for the Best Liver Swelling Treatment or need more information about liver care, Jaipur offers a wide range of options to help you on the road to recovery. Consult with a healthcare provider to discuss the best course of action based on your individual condition, and take proactive steps toward better liver health.
#liver treatment in jaipur#liver swalling treatment in jaipur#best gastroenterologist in mansarovar jaipur#endoscopy in mansarovar jaipur#gastro doctor in mansarovar jaipur
0 notes
Text
Understanding Acute Infection: A Comprehensive Overview 🌟

Discover the essential aspects of Acute Infection, including causes, symptoms, diagnosis, and treatment strategies. Learn how to manage and prevent acute infections effectively.
Introduction: What is Acute Infection? 🤔
An Acute Infection is a type of infection that occurs suddenly and is typically characterized by severe symptoms that develop rapidly. Unlike chronic infections, which develop slowly and persist over time, acute infections appear quickly and often require prompt medical attention. These infections can affect various parts of the body, including the respiratory system, gastrointestinal tract, and more.
Understanding the nature of acute infections, their causes, and effective management strategies is crucial for preventing complications and ensuring timely recovery.
Causes of Acute Infection 🌍
Bacterial Infections 🦠
Streptococcus and Staphylococcus: These bacteria can cause acute infections like strep throat and skin infections.
Escherichia coli (E. coli): Often responsible for urinary tract infections and gastrointestinal infections.
Viral Infections 🦠
Influenza Virus: Causes seasonal flu, leading to symptoms such as fever, chills, and muscle aches.
Rhinovirus: Known for causing the common cold, which is typically short-lived but can be intense.
Fungal and Parasitic Infections 🦠
Candida Species: Can cause acute fungal infections like oral thrush and vaginal yeast infections.
Plasmodium Parasites: Responsible for malaria, which presents with acute symptoms including fever and chills.
Symptoms of Acute Infection 🔍
Common Symptoms 🩺
Fever: A sudden increase in body temperature is a common sign of acute infection.
Chills and Sweats: Patients may experience episodes of chills followed by sweating.
Pain and Discomfort: This can include localized pain depending on the area affected, such as a sore throat or abdominal pain.
Severe Symptoms ⚠️
Difficulty Breathing: Indicative of a severe respiratory infection like pneumonia.
Confusion or Altered Mental State: Can occur in severe cases and requires immediate medical attention.
Rapid Heartbeat and Low Blood Pressure: Signs of a potentially serious systemic infection.
Diagnosing Acute Infection 🩺
Medical Evaluation 🔬
Patient History: Detailed history of symptoms, recent travel, and potential exposure to infectious agents.
Physical Examination: A thorough examination to assess symptoms and identify potential sources of infection.
Diagnostic Tests 🧪
Blood Tests: To identify the presence of infection and determine its severity.
Imaging Studies: Such as X-rays or CT scans, to visualize internal infections, especially in cases of suspected pneumonia or abscesses.
Treatment Strategies for Acute Infection 💡
Antimicrobial Medications 💊
Antibiotics: Effective against bacterial infections, prescribed based on the type of bacteria identified.
Antivirals: Used to treat viral infections, such as oseltamivir for influenza.
Antifungals: For fungal infections, medications like fluconazole may be prescribed.
Supportive Care 🌿
Hydration and Rest: Essential for recovery, especially in cases of high fever or gastrointestinal infections.
Pain Management: Medications such as acetaminophen or ibuprofen can alleviate discomfort and fever.
Preventive Measures 🛡️
Vaccination: Regular vaccinations, such as those for influenza, can prevent certain acute infections.
Hygiene Practices: Proper handwashing and avoiding contact with infected individuals can reduce the risk of infection.
Frequently Asked Questions (FAQs) ❓
What is an Acute Infection?
An Acute Infection is an infection that occurs suddenly with severe symptoms and requires prompt medical attention. It contrasts with chronic infections, which develop more slowly and persist over a longer period.
What are the common causes of Acute Infection?
Common causes include bacterial pathogens (like Streptococcus and E. coli), viral agents (such as the influenza virus and rhinovirus), and less frequently, fungal and parasitic organisms.
How is Acute Infection diagnosed?
Diagnosis involves a comprehensive medical evaluation including patient history, physical examination, and diagnostic tests such as blood tests and imaging studies.
What treatment options are available for Acute Infection?
Treatment depends on the cause of the infection and may include antimicrobial medications, supportive care, and preventive measures to avoid recurrence.
How can Acute Infection be prevented?
Preventive measures include vaccinations, practicing good hygiene, and avoiding contact with known sources of infection.
Conclusion: Managing Acute Infections Effectively 🌟
Acute infections require swift and effective management to prevent complications and ensure recovery. By understanding the causes, recognizing symptoms early, and following appropriate treatment and preventive measures, individuals can effectively manage and reduce the impact of these infections.
For further information and resources on managing acute infections, staying informed and consulting healthcare professionals is essential. Your proactive approach to health can make a significant difference in managing and preventing acute infections.
0 notes
Text
How Malaria Blood Tests Work: Crucial Information for Patients
What is malaria?
Malaria is a life-threatening disease caused by Plasmodium parasites transmitted through the bites of infected Anopheles mosquitoes. The parasites enter the bloodstream and infect red blood cells, leading to symptoms such as fever, chills, headache, and flu-like symptoms. Without treatment, malaria can progress to severe complications, including anemia, organ failure, and death. The disease is prevalent in tropical and subtropical regions, where the Anopheles mosquitoes thrive.
What are the symptoms of malaria?
Signs and symptoms of malaria generally start within a few weeks following an infection from a mosquito bite. These include:
Fever
Chills
Headache
Sweats
Muscle and Joint Pain
Fatigue
Abdominal Pain
Confusion
Rapid breathing
Rapid heart rate
Cough
How is malaria diagnosed?
The diagnosis of malaria is crucial for effective treatment and prevention of complications, including life-threatening conditions like cerebral malaria. This process involves confirming the presence of parasites and evaluating their quantity in the blood to assess the infection's severity. Blood tests are a primary method for diagnosing malaria, as they are essential for confirming the infection and guiding the appropriate treatment. Accurate and timely diagnosis is vital to prevent complications and ensure proper management of the disease.
What should be known about malaria blood tests?
A malaria blood test is essential for diagnosing the disease and involves analyzing a sample of blood to detect the presence of Plasmodium parasites. The test helps differentiate malaria from other illnesses with similar symptoms, such as fever and chills.
How do malaria tests work?
Blood Sample Collection: The process begins with the collection of a blood sample, usually obtained through a needle inserted into a vein in the arm. In some cases, a finger prick may be used to collect a smaller sample of blood. The method used often depends on the urgency and availability of testing facilities.
Microscopic Examination: Once the blood sample is collected, it is examined under a microscope. This method, known as a blood smear test, involves spreading a thin layer of blood on a glass slide and staining it with special dyes. The stained slide is then viewed under a microscope to identify and count any Plasmodium parasites. This technique is highly effective in diagnosing malaria and determining the specific species of the parasite.
Rapid Diagnostic Tests (RDTs): In addition to microscopic examination, Rapid Diagnostic Tests are commonly used, especially in areas with limited access to microscopy facilities. RDTs detect malaria antigens or antibodies in the blood. These tests are simple, quick, and can be performed at the point of care, providing results within minutes. They are particularly useful in remote areas and for initial screening.
Polymerase Chain Reaction (PCR): For more precise and detailed analysis, PCR testing may be used. This molecular technique detects the genetic material of the malaria parasites, allowing for accurate identification of the specific Plasmodium species and assessing the parasite’s resistance to treatment. PCR is more sensitive than traditional methods but is generally used in specialized laboratories.
Why should malaria blood tests be done?
Malaria is a serious illness that can escalate rapidly if not addressed promptly. Early and accurate diagnosis is crucial to initiate treatment with the appropriate medications without delay. Swift treatment not only improves patient outcomes but also helps prevent the spread of malaria within the community by interrupting the transmission cycle. Delays in both diagnosis and treatment are major contributors to malaria-related fatalities.
When should malaria tests be done?
Individuals should get tested for malaria if they experience symptoms such as high fever, chills, headache, muscle pain, and fatigue, especially if they have recently traveled to an area where malaria is prevalent. Testing is also crucial if they have encountered someone who has malaria or if they are in an endemic region and develop symptoms suggestive of the disease. Early testing and diagnosis are important for timely treatment and to prevent complications.
Conclusion
Understanding how malaria blood tests work is crucial for patients and healthcare providers alike. Timely and accurate testing is vital for effective diagnosis and treatment of malaria. Whether through microscopic examination, Rapid Diagnostic Tests, or advanced PCR techniques, these tests help ensure that patients receive the appropriate care and reduce the risk of severe complications. For those experiencing symptoms of malaria or at risk due to travel, seeking prompt medical attention and undergoing testing can significantly improve outcomes and help combat this serious disease.
Frequently Asked Questions
Which are the types of malaria tests?
The main types of malaria tests are microscopic examination of blood smears, rapid diagnostic tests (RDTs), and polymerase chain reaction (PCR) tests.
Is malaria a serious disease?
Yes, malaria is a serious disease that can be life-threatening if not treated promptly, potentially leading to severe complications such as cerebral malaria and organ failure.
0 notes
Text
8 Signs You Might Have Bipolar Disorder

Apart from impairing your emotional and psychological well-being, mental health illnesses can lead to familial issues and a general decline in quality of life. Bipolar disorder is a severe mental illness that can cause extreme highs and lows in mood as well as a general sense of hopelessness and sadness. You must have the best bipolar mood disorder treatment in Siliguri from a reputable psychiatrist to manage the symptoms.
The majority of the time, genetics or biological variations may lead to individual variations in symptoms for this mental illness. If your parents, siblings, or other close relatives also suffer from bipolar disorder, your chances of developing the illness's symptoms increase. When bipolar disorder is not properly treated in a timely manner, it can lead to suicidal thoughts and poor performance at work or school. The doctor will do a thorough mental evaluation to determine the exact type of bipolar disorder before recommending a customized course of treatment for a full recovery.
Top Signs Indicating That You Suffer From Bipolar Disorder
1. Psychosis
If the manic and depressed phases of bipolar disorder are not appropriately managed, psychosis may potentially develop. Delusions, hallucinations, and confused thinking all of a sudden are the clear indicators of psychosis. Irrational ideas, difficulties talking, and decreased social contact are some of the early signs of bipolar disorder psychosis.
If you are deluded, you might also have steadfast beliefs about things that aren't true. Here, you should never put off receiving treatment for psychosis because it can also be brought on by several other illnesses, including multiple sclerosis, stroke, malaria, brain tumors, and neurological disorders. You should note that the psychotic episodes associated with bipolar disorder can be a blend of hallucinations and delusions.
2. Sleeping disturbances
While there are many factors that might contribute to sleep problems, bipolar disorder can have a significant impact on your ability to sleep. Bipolar disorder and sleep difficulties include hypersomnia, insomnia, co-occurring sleep apnea, and irregularities in rapid eye movement sleep. You may also have irregular sleep-wake cycles if your mental health condition is not properly handled.
Furthermore, certain bipolar patients may also experience delayed sleep phase syndrome, a condition primarily brought on by the disorder's symptoms of insomnia and daytime sleepiness. To recover from sleeping disturbances, you must contact the best psychiatrist in Siliguri. Along with sleeping pills, the doctor might also recommend therapeutic interventions to manage the condition. Note that ignoring the sleeping issues can contribute to making bipolar symptoms worsen.
3. Mania and hypomania symptoms
The primary signs of bipolar disorder are periods of mania or hypomania. The main symptoms of the manic phase include nervousness, excessive happiness, and rapid speech. This is where you might want to abruptly change the subject because your mind is racing. You cannot sleep properly during these periods because you'll be restless and impulsive all the time.
Sometimes, persons who are hypomanic also experience a loss of appetite, which may lead them to engage in dangerous behaviours. If you don't manage your manic episodes in a timely manner, you can wind up spending a lot of money on shopping or losing all of your life savings on gambling. Moreover, you experience severe disruptions in performing daily activities due to the mania and hypomania symptoms.
4. Hallucination
Bipolar disorder symptoms and mood swings can sometimes get severe, causing the patient to lose their sense of reality. Children with this mental illness may frequently think erratically and hold unrealistic beliefs due to this symptom. In most cases, hallucinations happen when they enter the psychosis stage of bipolar disorder. It may be challenging for the patient experiencing these kinds of delusions or hallucinations to learn about the world around them.
Herein, one can also make up a fantasy world with themselves and maintain their distance from friends and relatives. Remember that hallucination episodes can impair all your senses including smell, sight, sound, taste, and touch. The chemical reactions in the brain need to be controlled through therapies by availing of the best bipolar mood disorder treatment in Siliguri.
5. Behavioural issues
Extreme mood swings caused due to bipolar disorder may also contribute to the emergence of behavioural issues. Both at home and workplace, the patient can exhibit disturbed behavioural patterns. You must note that this type of behavioural problem is more common among children suffering from bipolar disorder. This frequently prevents them from interacting with other kids, which worsens their mental health in general.
Getting bipolar mood disorder treatment at the right time is crucial if you want to support your child in overcoming these problems and leading a regular life with more productivity. If the concerning behaviours are left untreated then it can impact daily activities. Regular medication, therapy sessions, and recreation are essential to cope with this symptom.
6. Substance use
Bipolar disorder patients frequently tend to substance abuse. Alcohol or illegal drugs may become your go-to means of diversion from the upsetting bipolar disorder symptoms. If you are unable to manage your strong desire for addictive substances, you should see a reputable psychiatrist right away.
Always keep in mind that managing a substance use disorder can make treating bipolar disorder more challenging. Furthermore, abusing drugs or alcohol regularly to escape the harsh realities of life might lower your quality of life and increase your risk of developing severe depressive and manic symptoms. A dual diagnosis for both bipolar and substance abuse disorder can work wonders in improving your overall psychological condition.
7. Mood swings
One of the primary symptoms of bipolar disorder that can suggest you’re suffering from bipolar is low mood. Herein, you may exhibit several symptoms during these moments of low mood, such as disinterest, sleeping more than normal, feeling depressed without apparent cause, and displaying rage. You may also find it challenging to establish or preserve relationships with other individuals as a result of these symptoms.
Additionally, the mood swings caused due to bipolar may also involve high mood episodes. Patients experiencing spells of elevated mood can also experience a variety of symptoms, including being easily agitated, having trouble establishing consistent sleep schedules, and exhibiting excessive happiness without any obvious cause. Moments of elevated mood can also make it difficult for the patients to focus on basic tasks, which may result in poor performance.
8. Abnormal behaviour
When a patient behaves aggressively, we frequently assume that he has attention deficit hyperactivity disorder which can be associated with bipolar disorder. You should be aware, though, that bipolar disorder may also manifest itself as this kind of nature. This sign is more prevalent among children suffering from mental health issues.
The child suffering from aggressive behaviour due to bipolar may engage in verbal abuse, tantrums, defiance, and bullying as a result of this problem. Your child is always changing, and you need to be aware of this so that you can provide the necessary support if any abnormalities are discovered.
Do not delay seeing a doctor to receive the best bipolar mood disorder treatment in Siliguri if you experience any of these symptoms. To help you feel better, the doctor may prescribe mood stabilizers, psychoeducation, antipsychotics, antidepressants, and psychotherapy therapies. Furthermore, the doctor can also effectively manage childhood bipolar disorder with a variety of family-focused interventions and counseling.
0 notes