#Rehabilitation after spinal surgery
Explore tagged Tumblr posts
Text
youtube
Post Spine Surgery Rehabilitation | exercises after lumbar fusion | Rehab After Spinal Fusion
A physical therapist will frequently use a number of techniques to assist a patient recover from a back injury and get back in outstanding physical condition.
#Back surgery rehab#Rehabilitation after spinal surgery#Rehabilitation after lumbar disc surgery#Rehabilitation after back surgery#Post spinal surgery physiotherapy#Physiotherapy after back surgery#Post spinal surgery rehabilitation#Rehabilitation after spinal fusion#Physiotherapy after lumbar spine surgery#Physical therapy after laminectomy#Youtube
0 notes
Text
Gotham Knights: The Batman Family
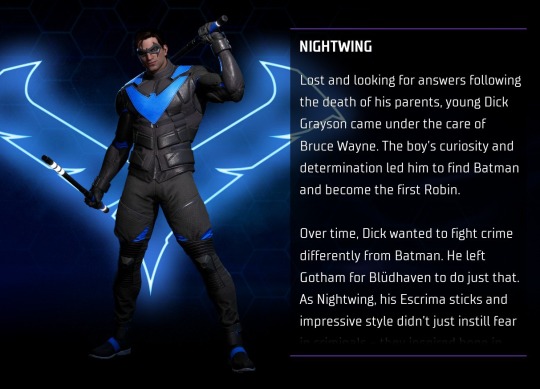
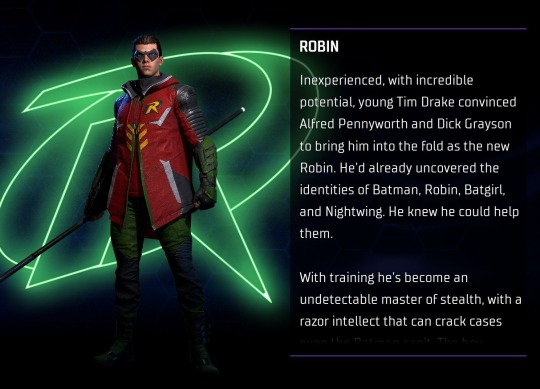
Nightwing: Lost and looking for answers following the death of his parents, young Dick Grayson came under the care of Bruce Wayne. The boy's curiosity and determination led him to find Batman and become the first Robin. Over time, Dick wanted to fight crime differently from Batman. He left Gotham for Blüdhaven to do just that. As Nightwing, his Escrima sticks and impressive style didn't just instill fear in criminals - they inspired hope in the people Nightwing lives to protect. Robin: Inexperienced, with incredible potential, young Tim Drake convinced Alfred Pennyworth and Dick Grayson to bring him into the fold as the new Robin. He'd already uncovered the identities of Batman, Robin, Batgirl, and Nightwing. He knew he could help them. With training he's become an undetectable master of stealth, with a razor intellect that can crack cases even the Batman can't. The boy wonder is everything Robin was meant to be. At only 16, he's just getting started.
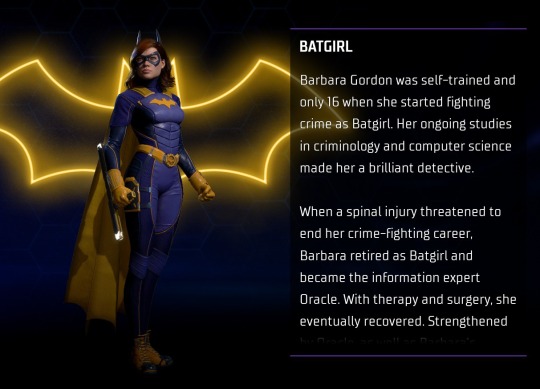
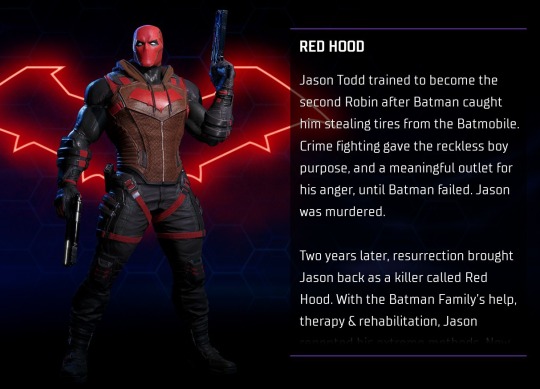
Batgirl: Barbara Gordon was self-trained and only 16 when she started fighting crime as Batgirl. Her ongoing studies in criminology and computer science made her a brilliant detective. When a spinal injury threatened to end her crime-fighting career, Barbara retired as Batgirl and became the information expert Oracle. With therapy and surgery, she eventually recovered. Strengthened by Oracle, as well as Barbara's unbreakable determination to protect Gotham, Batgirl returned. Red Hood: Jason Todd trained to become the second Robin after Batman caught him stealing tires from the Batmobile. Crime fighting gave the reckless boy purpose, and a meaningful outlet for his anger, until Batman failed. Jason was murdered. Two years later, resurrection brought Jason back as a killer called Red Hood. With the Batman Family's help, therapy & rehabilitation, Jason repented his extreme methods. Now Red Hood uses his pistols to put Gotham's criminals behind bars, rather than in the ground.


Bruce Wayne: If you ask the media, Bruce Wayne is a philanthropist, philanderer, or some combination of both. But if you ask me, Bruce is… an uncompromising friend and father. Someone who keeps his distance, protects his secrets, and is a total battle ax of a boss. And always, he's a man with a strong moral compass who would do anything to keep Gotham City safe, no matter the cost to himself. Bruce Wayne is everything Gotham City aspires to be. Also, he's Batman. P.S. And he's a terrible cook, constantly mixes up his black and blue socks, and strongly prefers not to be called "Brucie." [And if Batman wanted a completely serious biography, he should have written it himself.] - D.G. Only you. - B.W. Alfred: Steward of the Wayne family, Alfred Pennyworth is more than a butler - he's a generous mentor, a caring friend, and a reliable ally. Though he operates behind the scenes, Alfred is vital to the safety of Gotham City - and her protectors. Without his combat medical training and level-headed wisdom, Batman and others may not have lived to fight another night. Plus, he's an underappreciated actor. Honestly, he is phenomenal on stage.
#gotham knights#dick grayson#tim drake#barbara gordon#jason todd#bruce wayne#alfred pennyworth#Character Profiles (GK)#the 'only you' line kills me every time i read it T-T
60 notes
·
View notes
Text
Hello! I’ve taken on the responsibility of caring for over 60 stray cats in my area. Every day, I ensure they have enough food to eat, and I prioritize their medical needs by taking them to the vet when necessary.
Unfortunately, four of these cats require critical surgeries to improve their health and well-being. Additionally, I’m facing a significant veterinary bill that I’m struggling to pay off.
Your donation will directly support these cats’ surgeries and ongoing care. Your generosity will make a huge difference in their lives and allow me to continue providing for them. Thank you for considering supporting my cause and making a positive impact on the lives of these furry friends.
The cats that need immediate surgeries are the ones below.
I found the cat in the first picture in an empty pool in December 2023. He was waiting for his death. He has been going through treatment since then. He was diagnosed with Escherichia coli bacteria. There is infection coming out of his nose and on top of his head. The infection is melting his cheekbones and some of his skull. He needs to undergone one more surgery to clear out the infectious area. I put the photos in order so you can see what he has been going through since December.
The second baby is suffering from Pectus Excavatum. His rib cage and sternum are sunken into his chest. He needs to have a surgery before he gets too big. His organs are small now, but once he starts to grow up, his organs will grow as well, but wont have any space in his tiny body.
The last baby was ran over by a car while he was sleeping on the side of the road. The car drove over lower half of his body, he unfortunately cannot walk. It was decided that he needed spinal surgery and rehabilitation therapy after that.






14 notes
·
View notes
Note
*chins hands* Could we learn about about Pons and Angel? (:
Uffff this one took a long time, but I finally finished it!!!! ⸜(⸝⸝⸝´꒳`⸝⸝⸝)⸝
Thank you for this lovely ask, @riinoaheartilly and thank you for your patience! (っ˘з(˘⌣˘ ) ♡
Pons and Angel are kind of neglected characters at this point, and since I came up with them, I know literally nothing about Angel aside from that he is a little wacko who loves affectionately terrorizing the the troopers. Oh and his nickname is "Angy". His design is also still a mistery for me (I gave him a default clone trooper design so far).
But I have more info about Pons. :))))

Pons: I achieved divinity. I'm transcending the mortal realm with higher purpose. I can hear colors. Headshot: Go to sleep before Angy makes a needle-cushion out of you, will you?
EDIT: @ithillia said that's not how "cushion" is written. I say, fuck my life, he is space-french. Sprench. Whatever. (Thanks for telling <3)
More info under the cut!
⚕️ He is the only Medic in the CG who has an actual battle-scar. One in the temple from a knife-cut. And one in the nape, from heavy physical injury.
⚕️It all happened while extracting an injured trooper during a fight between the CG and a criminal gang. Since medical officers don't have combat skills beside basic self-defence, normally they don't leave the walls of the Guard compound, but this matter needed immediate treating and safe extracting.
⚕️The CG low-key celebrates him as a hero and Pons tries not to take it as a mockery, comparing to his brothers who are constantly under the threat of getting shot down while he couldn't protect himself from that attacker. This injury actually caused him pontine stroke and throughout the years of war, he is still in rehabilitation.
⚕️That trooper he saved? One of Fox's boys from the Planetary Defence. Spinal injury treated in bactatank, otherwise he managed to get out from the Medbay after 1 month of rehabilitation (why is it so hard to write down this word???), but the trooper always checked back on Pons, keeping him company, keeping him entertained with the latest gossips or books, taking a walk with him through the compound, forming a life-long friendship with it. I don't know too much about this particular trooper, not even a name, but I already love these two.
⚕️Pons didn't have a name before this incident and the surgery. But hearing the word pons pons pons all over again during his rehab, really clicked him, and named himself as such after the organ. Some hidden superstitious part wishes that naming himself such as the damaged part of his brain would manifest in his recovery.
Pons is a latin word for "bridge", also the name for that part of the brain that responsible for unconcious processes and involuntarily movements, eg.: blinking, swallowing, pain processing, breathing, digestion, heartbeat, regulating sleep-cycle, even dreaming!
Pontine stroke causes motor and sensory impairment, weakness or paralysis in parts affected by cranial nerve, clumsy voluntarily movements, inability to control muscles for swallowing and speaking, and can be responsible for sleep-paralysis.
I actually came up with Pons while watching a documentary eries about the brain and wanted a clone character who sleepwalks. I'm not sure I'm keeping the sleepwalking part though.
⚕️He just can't have a good night sleep and haunted by night-terrors and sleep-paralysis. Always tired, basicly lives on caf and stims.
⚕️Pons hates himself for being unable to maintain his duty as a medic, not in serious matters that need steady hands and focus. instead he is the one who needs contant treatment and attention. Still, Headshot gives him reading materials to study to keep him mentally fit, often ask him for advice when he is stuck and does everything to make Pons feel, he is still part of the team and he is waited back.
⚕️He develops love for painting which started as an exercise for improving on his motor movements. His pictures depicting monsters, inspired by his nightmares became posters decorating various barrack rooms in the CG.
⚕️I drew this picture about him weeks ago, but thinking on actually giving him signs of stroke next time I draw him.
⚕️ @ithillia said I should name Pons' friend Jason. I don't know if he is a Jason-type of guy. But I used to know a Jason when I was a kid and have fond memories of him, he drew very cool stuff, and he is working now as a pharmacist. Maybe this is fate.
Hmmm... that's it so far. If you have more specific questions about him, don't hesitate to ask! <3
#original clone character: pons#original clone character: angel#clones#clone trooper#coruscant guard#the clone wars#star wars#my ocs#mamuzzy draws stuff#mamuzzy answers
12 notes
·
View notes
Text
🧵 health, ableism ++
Yesterday a doctor, a seasoned guy who’s worked 40+ years, told me the reason I’ve met so much resistance with the health system;
Here, the doctors see you as «a waste of reasources» after three spinal/back related related surgeries.
I was 19 when I reached their limit.
They deemed me a lost cause at 19, years old.
The reason I had those two extra surgeries after the first, big one?
The healthcare system trying to save money.
Today, everyone who gets a scoliosis surgery like mine gets titanium right away.
When I was 13, got made 7 cm taller, got two rods and 20 bolts drilled into my spine, it was just steel.
I had a violent reaction that turned to all of this getting infected and that worsened until I was 16, when they finally made the switch to titanium.
But by then it was too late, and the infection got worse as it returned, and at 19 I had to have it all removed, which is high risk and still scary.
My spine is so fragile and fucked up now.
This all turned into other issues, and since then I have been diagnosed with chronic migraines, lupus, pcos, and endometriosis.
The first one is the only one I’ve been offered any long lasting treatment for, and now it makes sense.
After a lot of fighting I am now getting surgery for my endo, but that took years of work.
And now I know why.
Lupus is a serious fucking condition.
They all are, but if one of them is gonna kill me anytime soon, chances are the lupus will do the job.
But the only treatment they’re willing to offer at this time is pain management.
Maybe, when, not if, when, I get worse they’ll try something else, but probably not.
Because I’m a lost cause, a moneypit, a person beyond the hope of rehabilitating enough to help society.
But I’m still a person.
I deserve a life, and I know I, even if a wreck, can do little things to make others happy.
Make a little bit of change.
A disabled friend once told me he’s so tired of having to be either a hero or a tragedy to able bodies people.
Because sometimes, we’re both. Or neither. And that’s okay.
We are so much more than ableism wants us to be.
I’m not even sure what I wanted to say with this, other than the fact that I know talking about these things are the only ways things change, that people open their eyes, and that we can grow together.
Thank you so, so much if you read all of this.
Thank you ♥️
#health#ableism#personal#disability#disabled#lupus#systemic lupus erythematosus#scoliosis#scoliosis surgery#chronic illness#endometriosis#chronic pain#irl tag
41 notes
·
View notes
Text
Paroxysmal Sympathetic Hyperactivity As A Cause Of Prolonged Icu Stay- Case Report by Arnab Choudhury in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Paroxysmal Sympathetic Hyperactivity (PSH) is commonly described in patients after Traumatic Brain Injury but it can present after an ischemic stroke following a complicated surgery. Usual clinical presentation are tachycardia, tachypnea, hypertension, sweating with seizures and dystonic posturing less likely initial signs. High grade fever and profuse sweating may allude sepsis or epilepsy leading to extraneous administration of anti-epileptics and antibiotics. Suspicion of pheochromocytoma arises in such situations which is ruled out by CECT. Clonidine (α-2 blocker), propranolol (β-blocker) and Baclofen (GABAb agonist) are agents used in treatment. Benzodiazapenes like lorazepam are important part of treatment as discontinuing them can exacerbate PSH attacks. MRI brain with MR angiography usually reveals hyper-intensities on T2/FLAIR in subcortical areas (thalami, cerebellum, crus cerebri) and restricted diffusion with low ADC values. Recurrent PSH episodes can occur due to delay in diagnosing and treatment leading to contractures and difficulty weaning the patient off the ventilator with tracheostomy tube placed. This case presents a scenario in which the delay in diagnosing PSH led to extensive investigations , delay in specific treatment and a prolonged ICU stay of the patient. Mainstay of rehabilitation remains aggressive physiotherapy to improve contractures if any, medications for the autonomic fluctuations and regular follow up.
Keywords : Sympathetic, hyperactivity, paroxysmal, brain, episodes
Introduction
Paroxysmal sympathetic hyperactivity (PSH) is a disorder of autonomic function regulation most commonly observed in patients with acute brain injury. It mostly occurs after traumatic brain injury, but it can also occur after non-traumatic brain diseases such as anoxic-ischemic coma after cardiac arrest, intracranial haemorrhage, and ischemic stroke-[1].
The core clinical features include - tachycardia, tachypnea, hypertension, sweating , hyperthermia and posturing-[2]. These episodes are mostly triggered by some external stimuli such as pain , movement , and urinary retention . PSH occurs due to diffuse or focal brain injuries that disconnect one or more cerebral centers from the caudal excitatory centers and the disconnection of descending inhibitory pathways causing spinal circuit excitation.
Tonic posturing during episodes can mimic tonic seizures, and the raised temperature can mimic infection, which can lead to unnecessary investigations, delays in proper management and prolonged ICU stays. Here, we are presenting one such case.
Case Presentation
A 32-year-old woman (gravida 2 and para1) had pain in the lower abdomen at week 31 of gestation for which she was hospitalized and emergency Lower Segment Cesarean Section was performed in view of fetal hypoxia. On the 2nd day post-delivery, she developed multiple episodes of seizures without regaining consciousness in between and was intubated for airway protection. Brain Magnetic Resonance Imaging(MRI) with angiography suggested posterior circulation ischaemic stroke with bilateral narrow caliber of both vertebral arteries and a left fetal PCA. She was started on antiepileptic drugs and secondary prophylaxis for stroke. She was having high-grade fever and, multiple episodes of profuse sweating per day. Blood counts, cultures, and other markers of infection gave negative Results. She had episodes of tachycardia, tachypnea, hypertension, and sweating associated with fever.
The fever episodes created difficulty in weaning the patient from the ventilator.Therefore, she was started on clonidine and later on, propranolol;-however, these episodes continued to occur. Suspecting pheochromocytoma, abdominal contrast enhanced computed tomography (CECT) was performed, but the results were normal. The patient had recurrent episodes of increase in whole body tone (Fig 1) associated with bilateral lower limb tremors, abnormal posturing along with the above-mentioned episodes of fever. Initially, it was assumed that the rigors were those associated with fever, but later,speculating that the rigors were seizures,- the dosage of herantiepileptic medications were increased, and she was administered triple antiepileptics ( valproic acid , levetiracetam and lorazepam). Her brain EEG showed no epileptiform discharges. Despite receiving triple antiepileptics, she continued to show seizure-like activity. Later, these episodes of fever, tachycardia, tachypnea, hypertension , sweating and increase in body tone occurred simultaneously,- and the diagnosis of paroxysmal sympathetic hyperactivity was made.
The patient was administered clonidine, propranolol, and baclofen. Her episodes of sympathetic hyperactivity were controlled . Later, her empirical antibiotics were stopped as there was no evidence of infection and fever was explained as a part of sympathetic hyperactivity. Antiepileptic medications were tapered off to only levetiracetam. However, after discontinuing valproate and lorazepam she again started experiencing episodes of sympathetic hyperactivity. Therefore, lorazepam was reintroduced to control her symptoms. Finally, the patient was weaned off ventilator support and shifted to the ward.
Investigations
Blood parameters: TLC - 10,000 /mm3 ,Hb - 12 g/dl , Platelets - 2.8 lac/mm3
Blood culture - no pathogenic organism grown after 48 hrs of aerobic incubation.
Urine culture - sterile
Endotracheal aspirate culture - no pathogenic organism grown after 48 hrs of aerobic incubation.
High vaginal swab culture - normal vaginal flora grown.
Procalcitonin - 0.29 ng/ml
CSF analysis, - Acellular; sugar,-24 mg/dl; protein,-68 mg/dl; culture,-sterile
Dengue IGM,- negative; ICT and peripheral smear for Malaria - negative , Typhidot IGM,- negative; scrub typhus IGM,- negative.
Ultrasound abdomen:- no significant abnormality.
MRI Brain with MR Angiography –The brain stem appeared bulky and showed T2/FLAIR hyperintense signal. Similar areas with T2/ FLAIR hyperintense signal were also seen involving the thalami, right crus cerebri and bilateral inferior cerebellar peduncles. Many of these areas showed restricted diffusion with low Apparent Diffusion Coefficient (ADC) values. The bilateral (right > left) vertebral and distal basilar arteries appeared significantly attenuated in caliber. The right PCA appeared to be significantly attenuated in caliberas compared with fetal origin of the left PCA.
EEG - Generalized cerebral dysfunction; -no epileptiform-discharges.
CECT abdomen - No significant abnormality
Outcome and Follow-up
The episodes of sympathetic hyperactivity resolved, and the patient was shifted to the ward from the ICU with tracheostomy in room air. She developed contractures owing to persistent decerebrate posturing. Aggressive physiotherapy was administered. In the ward she regained her sensorium and was discharged with a GCS score of E4VTM6 for further follow-up in the OPD.
Discussion
A significant minority of patients who survive acquired brain injury develop sympathetic hyperactivity, which includes episodes of periodic increase in heart rate and blood pressure, sweating, hyperthermia, and motor posturing, often in response to external stimuli, which can last for weeks or more months-[3].Some studies argue that it is common but often unrecognized-[4].Most studies have reported paroxysmal sympathetic hyperactivity after traumatic brain injury. Fewer cases have reported it to be a sequel of brain stroke following prolonged hospital stay.Though commonly seen in TBI, PSH has rarelybeen described in patients with brainstem strokes and anoxic brain injury-[5].PSH may be mistaken for sepsis, which may lead to unnecessary treatment with antibiotics and prolonged hospital stays-[6].Fever is relatively common among patients in the intensive care settings. Although the most obvious and concerning etiology is sepsis, PSH may be the underlying etiology-[7].There are diencephalic structures analogous to the cerebral motor cortex that are capable of producing, when irritated, paroxysmal motor discharges similar to the focal discharges described as epilepsy-[8].PSA may be camouflaged by epileptic seizures, leading to the unwarranted administration of antiepileptics to the patient. Obstetric patients can present with acute increases in heart rate,-BP and the onset of HELLP syndrome mimicking PSH. Epigastralgia, hypertension, and tachycardia necessitate cesarean section, as in our case, with the subsequent development of HELLP syndrome mimicking PSH.An acute fluid shift from the splanchnic vasculature to the central vasculature may have occurred, causing HELLP syndrome as a result of vasospasm associated with sympathetic hyperactivity. Reporting such cases will facilitate in understanding if the reverse is true, that is, if PSH can mimick as HELLP syndrome-[9,10]. Pregnancy is a risk factor for paroxysmal sympathetic hyperactivity exacerbation, and delivery can result in resolution of the condition-[11].PSH is reclassified as a sympathetic storm rather than an epileptic disorder because of its unresponsiveness to anti-epileptics and the absence of epileptic activity on EEG. [12]it is crucial for clinicians to distinguish this disorder from paroxysmal dystonias. [13,14]Sympathetic storms have been linked to dystonia-like posturing (e.g., PAID, i.e., "paroxysmal autonomic instability with dystonia")[15], Antidopaminergic medications are best avoided to minimize the risk of neuroleptic malignant syndrome, which can potentially mimic PSH (dysautonomia). In contrast to delirium‐associated persistent agitation and picking‐like behaviours, PSH movements are episodic, tend to be provoked by touch, and are uniquely associated with increased sympathetic activityIn the management of this disorder opiates, γ-aminobutyric acid agents, dopaminergic agents, and β-blocker pharmacological agents have been studied. There is a lack of recommendations and comparisons of agents for the management of this disorder. There is a paucity of recommendations and comparisons of agents for the management of this disorder. Monotherapy is usually ineffective for the management of paroxysmal sympathetic hyperactivity, and multiple agents with different mechanisms of action should be considered, as in our case .β-blockers have proven to be therapeutic (not as monotherapy) as in our case,α-agonists such as dexmedetomidine have reported therapeautic efficacy in many studies. However, clonidine another α-agonist has shown therapeutic efficacy, as in our case. The effectiveness of physiotherapy in PSH is rarely reported in medical journals; our case strives to provide an example of such therapeutic benefits.
Conclusion
Paroxysmal sympathetic hyperactivity is quite common in patients with brain insult.It can mimic seizures and/or sepsis (due to high grade fever) leading to unnecessary investigations, exposure to higher-grade antibiotics and antiepileptics. Benzodiazepines are beneficial in controlling sympathetic hyperactivity.Non recognition of PSH can lead to difficulty in weaning patients off the ventilator and prolonged hospital stays. Recurrent episodes of sympathetic hyperactivity can lead to significant weight loss and contractures.
#Sympathetic#hyperactivity#paroxysmal#brain#episodes#JCRMHS#Journal of Clinical Case Reports Medical Images and Health Sciences (JCRMHS)| ISSN: 2832-1286#clinical decision making
2 notes
·
View notes
Text
Thinking of Noctis is Tenebrae.
Specially, when he was in Tenebrae.
Noctis was born on August 30th, and was eight years old during his time in Tenebrae.
Lunafreya, who was born on September 4th, was twelve.
Considering the main game generally takes place over the course of a year (I think? Don’t quote me on this, all I know canonically is that it starts May), in the year of M.E 756 and he visited twelve years prior:
M.E 744.
I’d guess very late winter, early spring. Possibly late January through February - maybe to early or mid March, at the latest.
Why so early in the year?
In the Kingsglaive movie, the prologue when we see the fall of Tenebrae and Queen Sylva’s murder, several characters are wearing clothes that seem suited to chilly weather - namely Ravus, Lunafreya, and Noctis.
Ravus and Noctis are, respectively, wearing a padded jacket or padded vest. The puffy sort you wear when it’s getting cold out, but not big-puffy full blown winter coats.
Also, Lunafreya is wearing a shawl or capelet with a hood, and it looks like it has a fur collar(?). Her dress looks, at least to me, like a thick fabric - wool, maybe. She’s not wearing stocking or leggings (or maybe she is and I didn’t notice), so again, it’s not winter-levels of cold.
There’s no snow either, which means either it’s before winter has fallen or afterwards - and I am inclined to believe the latter.
(That’s dependent on the general climate of Tenebrae, though)
We don’t know when Noctis was attacked, except that it was after he turned eight years old - in other words, some point after august. Possibly early September 743 at the earliest, and March - July 744 at the latest, since he was out catching fireflies, which usually appear most often in spring and summer.
We know he was comatose for a period of time following the attack, but not how long.
He possibly had been afflicted by the starscourge in canon (I don’t know if this was ever confirmed).
We also know he was paralyzed, or his body was still recovering from his injuries to the point where he was still wheelchair bound in Tenebrae.
My idea is this:
Noctis is attacked some time in late M.E 743. He is rushed into emergency surgery in an attempt to save his life, no doubt after Regis had used his magic to keep the Prince alive on the way to the nearest hospital (he’d probably be transferred to the Citadel later? He woke up in the citadel in Brotherhood, at least).
Noctis is possibly comatose for a month, maybe two. As a result of lack of movement, his muscles - on top of the damage done to back and legs - begin to atrophy.
(The symptoms of starscourge infection are stymied, because starscourge adapts differently to the body of a Lucis Caelum, and makes Noct effectively asymptomatic for a time).
When he wakes up, and probably even before that, immediate therapy begins. When possible, rehabilitation in regards to spinal cord injuries begin as soon as possible, I believed.
For a time, I think it would be…not okay, not happy, but workable. Regis would be there every step of the way, and if not him - a team of nurses and doctors ever on standby.
But at some point during his rehabilitation, from the Acute and Sub-Acute phases which will stretch over into the new year, which can generally (and I mean this broadly, every spinal injury and situation is different) take around six to eight months, he begins to show signs of the starscourge.
Regis can’t do anything to help with the appearance of the scourge, and then the realization that it must have been there for a while, that this was why Noctis’ healing was so slow - even, and especially, compared to a normal person.
The crystal, the LC magic, would have been straining to heal him - but it was almost sluggish, unfocused, as it coursed through Noctis’ body.
Regis could feed Noctis magic, take the burden of how it pulled at one’s lifeforce so that his son already so close to death did not have to.
He couldn’t take away the scourge which corrupted his son’s magic, which was just as much as the family’s magic eating away at his son’s life. The doctor’s could give estimations and exams and exercises on how to help Noctis walk again, if he ever could, and even an inability to do so was not an impossible fact - not in the long history of the bloodline -
But the starscourge?
Sooner or later, it was fatal. Regis knew of no known member in the bloodline who had gotten it - most who died to daemons died outright in battle, or as a result of injuries, long before the scourge could set in and take them - but no one had ever survived the scourge.
And only one bloodline could do anything against it.
The House of Fleuret, The Oracle.
And that meant heading to Tenebrae. Even if it was an autonomous ‘kingdom’, Tenebrae had long since been annexed by Niflheim - just like Accordo.
To bring Noctis there would be like to deliver all of Lucis into the jaws of a snarling best.
If it had simply been Noctis’ back and legs maybe, maybe Regis wouldn’t have done it. It’s a big maybe, considering how much he loves his son, but maybe.
Starscourge, though?
Hell no, it’s off to Tenebrae. They have to fucking go. It doesn’t matter how dangerous it is, to go through imperial Territory. Noctis might die either way.
A route to reach Tenebrae has to be made, means for the two of them to leave the wall unknown, then travel to Tenebrae still unknown, also having Lucis ruled well - all the while, trying to keep Noctis as stable as possible? Things like that take time.
So, they arrive in Tenebrae some point in early 744. My personal headcanon is that the two are there for maybe a few months, around March, and then Niflheim strikes and everything subsequently goes to hell. It has to be before his ninth birthday.
2 notes
·
View notes
Text
INCURABLE / TERMINAL.
In light of more talk about Batman Beyond in the rpc (good, it's fucking peak), and talking with @2ndbat (FANTASTIC BLOG GO FOLLOW), I have revamped my Incurable/Terminal verses to go from just Old Man Crane to straight up Batman Beyond.
That said, I will be outlining the general setting and the differences in both verses here! Enjoy!

NAME: Professor Jonathan Ichabod Crane SPECIES: Metahuman AGE: 68 HEIGHT: 7’10” WEIGHT: 280 lbs. OCCUPATION: Professor of Psychology at Gotham University, Professional Therapist and Psychiatrist, Career Criminal (formerly), Supervillain (formerly) AFFILIATIONS: Gotham University (formerly and currently), Di Vaio Crime Family (formerly), Quorum (formerly), Secret Society (formerly), The Injustice League (formerly) PHYSICAL DESCRIPTION: A veritable colossus of muscle, Jonathan Crane’s rehabilitation worked out far better for him than any could have ever hoped. After finally receiving proper treatment and diagnoses, Crane’s medications and fear suppressants allowed him to finally regain some sense of routine beyond getting up in the mornings and putting his body through Hell. Eating, sleeping, and exercising regularly has enhanced Crane’s physique, to the point where even at 68, the giant still seems to be in his physical prime… “seems” to be, that is. Though his hair has begun to gray and his face is showing signs of his age in the form of wrinkles and laugh lines, Crane is no less gorgeous than he was two decades prior. Crane has gone completely blind in his right eye, and still uses a prosthetic left arm and right leg thanks to injuries suffered when he was 30. MEDICAL INFORMATION: McCune-Albright Syndrome, Sleep Apnea, Asthma, Fibromyalgia, severe burn injuries, blind in right eye, missing an arm and leg, severe brain damage and nerve damage MENTAL DISORDERS: DID, Bipolar Disorder, Autism Spectrum Disorder, Generalized Anxiety Disorder, Seasonal Affective Disorder, Post-Traumatic Stress Disorder
BIOGRAPHY: After a lifetime of pain and insanity, Crane's reprieve, ironically enough, only came about when the foundations of Arkham itself were shook to their very core, and he was finally assigned a new doctor. Instead of approaching Crane as though he were completely sane, the new doctor, Mannfred O'Malley (who had experience with Crane) immediately diagnosed him with DID, Bipolar Disorder, PTSD, Autism, and a slew of other diagnoses. CAT scans supported this, and Crane was immediately put on anti-psychotics, mood stabilizers, and anxiety relief medication. Crane had never been better in years, and at the age of 36, he was finally recovering. He began to sleep and eat much more regularly, and corrective surgery helped many of his physical maladies. Eventually, upon his release from Arkham, Crane stopped returning as frequently, and stopped completely once his prescriptions were moved to a regular psychiatrist in the city.
After 2 years living on his farm in good health, Crane gained an astonishing 100 pounds of muscle, no longer malnourished from his unhealthy lifestyle, and even had a growth spurt of 2 inches. Emboldened by his change, he applied once more to Gotham University, where he had taught so long ago, at the age of 40. It had been 15 years since his abrupt departure, but they still welcomed him back with open arms. At the age of 60, Jonathan Crane was now a tenured professor of psychology, winning multiple awards for his theories and experiments in regard to fear and the human mind.
And then, it all came crashing down.
On the eve of his 62nd birthday, Crane suffered from a horrible mental break - his hallucinations began to return, this time with a vengeance, and recognizing the pattern, Crane took an emergency leave of absence.
The news he received after returning to Arkham was horrid. After being physically examined, it became clear that Crane's spinal and cerebral implant, his constant companion for 55 years and a mark of Qorum's involvement in his life, had been spreading itself through his body, upgrading itself with cybernetic modifications. In addition, the fear toxin in his veins had irreparably damaged his mind, and he would suffer a complete and total cessation of brain activity soon. They could not give him an estimate of how much time he had left. Left only with the choice of how he would receive this news, Crane's path diverges.
INCURABLE.

SEEKING to prevent himself from repeating the mistakes of the past, Professor Jonathan Crane seeks treatment to prolong his life as much as possible, and experiments with the dosage on his medications, even against professional advice. Taking a sabbatical from Gotham University, Crane travels the world, looking for a cure for his condition. In distant lands, and lands not far from home, he dons the guise of a helpless old man, when in truth, he is far from it. After seeing the pain in the world, the same pain he once spent so much time contributing to, he dons the visage of "The Ward", a traveling alchemist seeking to protect the weak and the innocent, and to save problems. He frequently returns to Gotham whenever he can, even occasionally checking himself back into Arkham during particularly brutal episodes, but thanks to living frugally over many, many years, he has a good chunk of money saved up for his travels. Ironically enough, Crane is currently the closest he has ever been to activating his metagene, a feat which would completely halt his neural degradation and remove the implant, as well as halt his aging - if only he was even aware he was a metahuman.

ABILITIES: Vast intellect, resilient body, martial arts training, decades of experience, heightened awareness
WEAKNESSES: Frequent hallucinations, neural degradation, moves slow due to injuries and age
TERMINAL.

SOMETIMES it can be impossible to truly recover what one has already lost. Already cracked and fractured by his ongoing condition, Crane left his appointment with Doctor O'Malley a despondent and heartbroken man. Was this his reward, for trying to be better? He twitches, as though he can feel his body building itself up and breaking down at the same time. It isn't until his return to the city proper that he finds himself on the other end of a would-be-mugger, and he realizes nothing has changed. The Waynes, the di Vaios - even Zsasz's life had changed at the end of a blade. There was nothing to change for Crane, though. His hand shoots out before he can stop it. He breaks the criminal's hand - and then his neck. And he looks upon Gotham with a profound sadness. His past would only continue to haunt him, for as long as he let it. His mind fractures, and finally his metagene is activated... slightly. With enhanced strength, speed, and senses, but at the cost of his physical health and sanity, Crane dons the mask of Epimetheus, an amalgamation of all that he once was - Crane, Crow, Bones, Beast, and even Jonathan. He will slaughter his past, no matter how long it takes.

ABILITIES: Shapeshifting, heightened reflexes, enhanced speed, enhanced strength, semi-intangibility
WEAKNESSES: Complete loss of sanity, animalistic intellect, lack of higher thought (maybe)
10 notes
·
View notes
Text
Stem Cell Therapy: Recent Advancement For Spinal Cord Injuries
A spinal cord injury (SCI) is damage caused to the nerves in the spinal cords that are responsible for sending and receiving signals from the brain. The traumatic lesion in the spinal cord can cause permanent or irreversible sensory and motor deficits. Stem cell therapy has shown massive potential in repairing damaged tissues and promoting recovery of neurological function. Medical research shows the effectiveness of stem cell therapy in treating various neurodegenerative disorders like ischemic stroke, intracerebral hemorrhage, and spinal cord injury.
Causes Of Spinal Cord Injury
The increasing number of cases of spinal cord injuries worldwide has made SCI a global health priority. Sports injuries and road accidents have been recognized as the two common causes of SCI. Although traumatic conditions comprise major triggering factors to induce spinal cord damage, non-traumatic events such as inflammation, spinal disc degeneration, cancer, substantial tissue loss, and infections can also be the reason for injury to the spinal cord and peripheral nervous system,
Symptoms of Spinal Cord Injury
The emergency symptoms of SCI may include loss of control in body movements due to partial or complete loss of sensory function. It is characterized by loss of motor control of the back, arms, legs, and other body parts, leading to weakness and incoordination. Patients experience extreme pain and pressure in the back, neck, and head.
Other prominent symptoms that doctors have identified as effects of spinal cord damage are -
Difficulty in walking and sitting
Difficulty in breathing
Sudden reflexes or spasms
Loss of control over bladder and bowel movements
Lowered sexual sensitivity and infertility
Trouble in balancing
Numbness or tingling sensation in the hands, fingers, and feet
The Science of Stem Cell Therapy For Spinal Cord Injury Treatment
Spinal cord injury is a severe condition that damages the nerve cells and tissues in the spinal cord, resulting in paralysis or nervous function impairment. Current treatment approaches include medication, rehabilitation therapy, physical therapy, or surgery. However, most of them provide temporary relief and poor outcomes in the long run. Stem cell interventions have emerged as a promising treatment for SCI with its exemplary potential to repair and regenerate injured neurons and tissues.
The distinct ability of stem cells to proliferate and form any functional cell type makes them ideal for treating SCI. The cells self-renew into nerve cells to replace and repair the diseased cells. After they are introduced into a patient’s body, they reach the injured site and interact with the surrounding cells to produce neurotrophic growth factors and alter the microenvironment of the affected region in the spinal cord.
A preclinical study has shown that mesenchymal stem cells release growth-promoting factors that accelerate the growth of axons at the injured area and improve myelination (formation of specialized membranes around axons). Most importantly, the therapeutic potential of stem cells prevents further neuronal degeneration in the spinal cord, lowering inflammation and improving motor and sensory function.
Start Your Stem Cell Therapy Journey In Mexico
There is no better place than Mexico for stem cell therapy because this North American country is home to highly qualified and experienced medical professionals with a proven track record of successful cell therapies. Besides, the healthcare system in Mexico is also advanced, and its treatment solutions are most accessible and affordable to people all over the world.
Life Altering Stem Cell Therapy Institute is a trusted name if you are ready to receive stem cell therapy in Mexico. Their state-of-the-art technologies, innovative treatments, and comfortable clinic setup have earned them the tag of stem cell therapy best hospital in Mexico. Their health advocates are just a call away! Connect with them to learn more about stem cell therapy for treating spinal cord injuries and other chronic conditions.
3 notes
·
View notes
Note
Obligatory I'm not a doctor disclaimer, however I am unfortunately acquainted with spinal surgery so here are my 5 cents on the topic. The X-ray looks like a lumbar (lower back) fusion and while it is quite an extensive one, it isn't true that it could only be the result of scoliosis or a bad injury; it is done to prevent motion that causes pain, which can occur for a lot of reasons including injury, but also simply aging as that can cause people to develop arthritis, disk degeneration and so on. The recovery time also isn't as drastic as some might assume, the hospital stay is often minimal, light exercise like walking is encouraged within weeks, and rehabilitation starts at around 2 months. Obviously, scarring would be the major giveaway here but at the same time, there are less invasive ways of performing the surgery nowadays that leave a couple of smaller incisions rather than one long scar.
I am not arguing that the X-ray is definitely Richard, and as a matter of fact I very much hope it isn't, but at the same time I wanted to point out that it could *theoretically* be feasible for it to be him. The Pandemic break from touring was long enough for something like this to heal and I don't believe we have seen his back post-Pandemic.
Lumbar fusion can also cause loss of flexibility or stiffness of the lower back, and lower back pain is often lessened by a lightly forward leaning posture, both of which are things visible in how he moves.
Once again, I am not trying to armchair diagnose anyone, more so just "playing devil's advocate" in terms of whether or not it would be feasible for him to have had a surgery like this without people knowing. I hope that everyone's right and it is not in fact him, I quite like the theory about it being a metaphor for being held together. But at the same time, I wanted to provide an alternate perspective based on some personal experience with this type of issue.
Very interesting, thank you anon 🌺 and indeed, if he had had the op relatively recent (let's say after the 'oberkörperfrei years' we might not know)
Personally i'm going with 'just a cool metaphoric pic' for now, until it gets specifically mentioned
or until we get a Q&A for a Rammstein documentary 😊 (i'm making that much bigger than it will ever be...it it will ever gets to be anything at all 🌺)
10 notes
·
View notes
Text
Acquired Brain Injury
Acquired brain injury (ABI) refers to any type of brain damage that occurs after birth. It can include damage sustained by infection, disease, lack of oxygen or a blow to the head.

Two thirds of all people with an ABI who have their activity limited or restricted are over the age of 45. One third of those are over the age of 65. The largest age group is between 40 and 49 and, at all ages except for those aged 80 and over, rates for males are higher than for females.
How brain injury occurs
Brain injury can occur through:
Sudden onset – caused by trauma, infection, lack of oxygen (for example, during near drowning or suicide attempts), strokes or drug use episodes
Insidious onset – from prolonged alcohol or substance abuse, tumours or degenerative neurological diseases.
Causes of acquired brain injury (ABI)
Acquired brain injury is any damage to the brain that happens after birth. The specific symptoms or losses of functioning depend on which brain areas are affected.
Some of the causes include:
Alcohol or drugs – which can poison the brain
Disease – such as AIDS, Alzheimer’s disease, cancer, multiple sclerosis or Parkinson’s disease
Lack of oxygen – called anoxic brain injury (for example, injury caused by a near drowning)
Physical injury – such as an impact (or blow) to the head, which may occur in vehicle or sporting accidents, fights or falls
Stroke – when a blood vessel inside the brain breaks or is blocked, destroying the local brain tissue.
How ABI affects a person
The long-term effects of brain injury are difficult to predict. They will be different for each person and can range from mild to profound.
It is common for many people with ABI to experience increased fatigue (mental and physical) and some slowing down in how fast they can process information, plan and solve problems. They may experience changes to their behaviour and personality, physical and sensory abilities, or thinking and learning.
How the brain works
The brain is the powerhouse of the body, even though it only makes up two per cent of the body’s weight. This soft, jelly-like organ has countless billions of neural cross-connections. It functions using a combination of electrical and chemical means. The brain oversees the workings of the body and gives us consciousness and personality. It is divided into two halves: the left hemisphere and the right hemisphere. Each hemisphere is further subdivided into lobes. Different functions happen in different parts of the brain, which is suspended in a chemical ‘soup’ called cerebrospinal fluid. This fluid nourishes the brain and serves as a shock absorber. The brain is connected to the rest of the body through the spinal cord. Together, the brain and spinal cord make up the central nervous system.
Traumatic brain injury
Traumatic brain injury (TBI) is not the same as head injury, since a person can sustain damage to the face, scalp and skull without necessarily injuring their brain. TBI is considered a form of acquired brain injury, and refers to brain damage caused by an impact to the head.
When the head is struck hard, the brain slams against the inside of the skull, causing physical injuries such as bruising, swelling, bleeding, twisting or tearing of tissue. There are degrees of injury, ranging from a momentary loss of consciousness (which can happen from a punch to the face, for example) to a long-term bout of unconsciousness or coma.
Treatment for brain injury
A range of tests, including x-rays and CT brain scans, can help pinpoint the exact areas of damage. In some cases, surgery may be needed. Recovery depends on the extent and location of the brain damage, the age and general health of the person, the speed of first aid received and the quality of treatment.
The consequences of a person having an ABI are far reaching. Coping with any loss of functioning and going through rehabilitation can be difficult. The person with an ABI will have great distress. Family, friends and partners will also experience difficulties as they deal with emotional and practical challenges, interruptions to family life and role changes.
An ABI can affect intimate relationships, friendships, social networks, recreational and vocational activities. It may force the person and their immediate family to adapt to a completely new way of life and new kinds of relationships.
Caring for someone who has had a brain injury may bond a family closer together. It can also mean enormous burdens for the family, which may tear it apart.
It will help if family members:
have good information about the effects of ABI
appreciate the difficulties that might be encountered
understand that recovery is a slow process.
For carers to cope with the situation, it helps to:
stay with the present, rather than brooding about how catastrophic the future may be
highlight strengths and daily achievements, rather than the weaknesses
make time to care for themselves
be wise enough to ask for help when it is needed.
Where to get help
· Step To Walk Neuro Rehab, Ghaziabad https://steptowalkneurorehab.com or call +91- 99101 18186
· Neurologists
Things to remember
Acquired brain injury refers to any type of brain damage that happens after birth.
Causes of ABI include disease, blows to the head, alcohol and drug use, or oxygen deprivation.
Coping with the consequences of acquired brain injury can be difficult for everyone, including family members.
3 notes
·
View notes
Text
Physiotherapist in Jaipur: Enhancing Health Through Expert Care
Physiotherapy is an essential branch of healthcare that focuses on restoring movement and function in individuals affected by injury, illness, or disability. In Jaipur, the demand for skilled physiotherapists has seen significant growth, as more people recognize the importance of physical therapy in maintaining and improving their quality of life. Whether you are recovering from surgery, managing chronic pain, or seeking to improve mobility, the expertise of a physiotherapist can be life-changing.

Why Choose Physiotherapy?
Physiotherapy offers a non-invasive and holistic approach to healing. It is effective in addressing a wide range of conditions, including:
Orthopedic Issues: Post-fracture rehabilitation, joint replacement recovery, or treatment for back, neck, or knee pain.
Neurological Disorders: Stroke recovery, multiple sclerosis, and Parkinson’s disease management.
Sports Injuries: Treatment for sprains, strains, and other injuries common among athletes.
Post-Surgical Recovery: Rehabilitation after surgeries like ACL repair or spinal surgery.
Chronic Conditions: Managing arthritis, fibromyalgia, or chronic back pain.
Physiotherapy Services in Jaipur
Jaipur boasts a growing network of physiotherapists and clinics equipped with advanced tools and technology to provide tailored treatment plans. The city’s physiotherapy centers cater to a diverse clientele, from children to senior citizens, addressing unique needs with precision and care.
Key services offered by physiotherapists in Jaipur include:
Manual Therapy: Hands-on techniques like joint mobilization and soft tissue massage to reduce pain and improve mobility.
Exercise Therapy: Customized exercise programs to strengthen muscles and improve flexibility.
Electrotherapy: Use of modalities such as ultrasound, TENS, or laser therapy to alleviate pain and promote healing.
Postural Correction: Guidance on improving posture to prevent and manage musculoskeletal problems.
Rehabilitation Programs: Comprehensive plans for post-operative care, injury recovery, or managing chronic conditions.
Choosing the Right Physiotherapist in Jaipur
When looking for a physiotherapist in Jaipur, consider the following factors:
Qualifications and Experience: Ensure the physiotherapist is certified and has experience in treating your specific condition.
Reputation: Check reviews or seek recommendations from friends, family, or healthcare providers.
Facilities and Equipment: Opt for clinics with modern equipment and a clean, welcoming environment.
Personalized Approach: A good physiotherapist listens to your concerns and designs a treatment plan tailored to your needs.
Benefits of Physiotherapy
The impact of physiotherapy extends beyond physical healing. It helps reduce dependence on medications, prevents surgery in some cases, and boosts overall well-being. Physiotherapy also improves mental health by reducing stress, improving sleep, and enhancing the quality of life through restored independence and mobility.
Conclusion
Jaipur’s physiotherapists are at the forefront of promoting health and well-being through expert care and personalized treatment. Whether you are dealing with a sports injury, recovering from surgery, or managing a chronic condition, the city offers a wide range of options to suit your needs. By choosing the right physiotherapist, you can embark on a journey to better health and improved quality of life.
Take the first step toward a healthier, pain-free future—consult a skilled physiotherapist in Jaipur today!
0 notes
Text
Discover the Best Orthopedic Hospital in Pragathinagar – SLG Hospital
When it comes to managing orthopedic conditions, finding the right hospital can make all the difference. For residents of Pragathinagar and surrounding areas, SLG Hospital stands out as the best Orthopedic hospital in Pragathinagar. Offering comprehensive care, advanced technologies, and a team of dedicated specialists, SLG Hospital is the go-to destination for all orthopedic needs.
Why Orthopedic Care Matters
Orthopedic care focuses on the diagnosis, treatment, and prevention of disorders related to bones, joints, ligaments, tendons, and muscles. These issues can stem from injuries, age-related wear and tear, or chronic conditions like arthritis. High-quality orthopedic care ensures patients regain mobility, reduce pain, and improve their overall quality of life. The best Orthopedic hospital in Pragathinagar, SLG Hospital, takes a holistic approach to address these challenges effectively.
SLG Hospital: A Leader in Orthopedic Excellence
SLG Hospital has earned a reputation as the best Orthopedic hospital in Pragathinagar due to its commitment to providing exceptional care. From minor fractures to complex joint replacements, the hospital’s orthopedic department is equipped to handle a wide range of cases.
Key Features of the Orthopedic Department at SLG Hospital
State-of-the-Art Infrastructure SLG Hospital boasts modern operation theaters and advanced imaging facilities. These cutting-edge tools enable precise diagnosis and effective treatment, cementing its position as the best Orthopedic hospital in Pragathinagar.
Expert Team of Orthopedic Specialists The orthopedic team includes experienced surgeons, physiotherapists, and rehabilitation experts who work together to deliver personalized care. Their expertise ensures the highest success rates in surgeries and treatments.
Comprehensive Services Whether you’re dealing with a sports injury, arthritis, or a need for joint replacement, SLG Hospital provides a full spectrum of orthopedic services. This versatility further establishes it as the best Orthopedic hospital in Pragathinagar.
What Sets SLG Hospital Apart?
The orthopedic department at SLG Hospital is driven by a patient-first approach. Here’s what makes them stand out:
Innovative Treatments: From minimally invasive procedures to robotic-assisted surgeries, the hospital stays ahead of the curve.
Post-Surgical Rehabilitation: Recovering after surgery is as important as the surgery itself. SLG Hospital offers tailored rehabilitation programs to ensure a speedy recovery.
Patient-Centric Care: Every treatment plan is customized to address the unique needs of each patient.
Conditions Treated at the Best Orthopedic Hospital in Pragathinagar
SLG Hospital specializes in treating a variety of orthopedic conditions, including:
Arthritis and Joint Pain Advanced joint replacement surgeries, like knee and hip replacements, are performed with precision.
Fractures and Trauma The hospital’s trauma care unit is equipped to handle emergencies swiftly.
Sports Injuries Athletes benefit from specialized care for ligament tears, dislocations, and tendon injuries.
Pediatric Orthopedics Children with congenital or developmental orthopedic issues receive expert care tailored to their needs.
Spinal Disorders Treatments for herniated discs, scoliosis, and other spinal conditions are available.
Testimonials: Real Stories from Patients
Patients often share glowing reviews about their experiences at SLG Hospital, reaffirming its status as the best Orthopedic hospital in Pragathinagar.
“After my knee replacement surgery at SLG Hospital, I regained the ability to walk pain-free. The care and attention I received were exceptional.”
“The team at SLG Hospital treated my sports injury with utmost professionalism, and their rehabilitation program was excellent!”
Why Choose SLG Hospital for Orthopedic Care?
Choosing the right hospital can be overwhelming, but SLG Hospital simplifies the decision with its exceptional offerings. As the best Orthopedic hospital in Pragathinagar, it provides:
24/7 Emergency Care Accidents can happen anytime, and SLG Hospital is always ready to provide immediate assistance.
Affordable Treatments High-quality care doesn’t have to break the bank. The hospital offers cost-effective solutions without compromising on quality.
Patient Education Understanding your condition and treatment options is crucial. The hospital ensures patients are well-informed every step of the way.
A Focus on Preventive Care
At SLG Hospital, the emphasis isn’t just on treating conditions but also on preventing them. Regular check-ups, patient education seminars, and community outreach programs highlight the hospital’s commitment to long-term health.
How to Reach SLG Hospital
Conveniently located in Pragathinagar, SLG Hospital is easily accessible for patients across the city. With ample parking, a patient-friendly environment, and streamlined admission processes, it ensures a hassle-free experience.
The Future of Orthopedic Care at SLG Hospital
The team at SLG Hospital is constantly innovating to improve patient outcomes. From adopting new technologies to training their staff in the latest techniques, the hospital is dedicated to maintaining its status as the best Orthopedic hospital in Pragathinagar.
Conclusion
When it comes to orthopedic care, you deserve nothing but the best. SLG Hospital has proven time and again why it is regarded as the best Orthopedic hospital in Pragathinagar. With its patient-centric approach, advanced treatments, and expert team, the hospital is committed to helping you get back on your feet.
READ MORE: Gynecology doctor in JP nagar
If you or a loved one needs orthopedic care, don’t hesitate to visit SLG Hospital—the best Orthopedic hospital in Pragathinagar. Experience world-class care and start your journey to better health today!
#Gynecology specialist In Hyderabad#Gynecology specialist in Nizampet#Gynecology specialist in Bachupally#Gynecology specialist in KPHB
0 notes
Text
Understanding the Role of a Pain Management Specialist in Chronic Pain Relief

Chronic pain affects millions of people worldwide, impacting not just physical well-being but also emotional and mental health. For individuals suffering from long-term pain, finding effective treatment options is often a challenge. Pain management specialists in NYC play a pivotal role in providing relief and improving the quality of life for those dealing with chronic pain. In this article, we will explore the role of a pain management specialist, the types of chronic pain they treat, and the various treatment options they employ to help patients regain control over their lives.
What Is Chronic Pain?
Chronic pain is defined as pain that persists for more than three months, often continuing even after the injury or illness that caused it has healed. Unlike acute pain, which serves as a warning signal to the body about potential injury or harm, chronic pain is often an ongoing condition that can be associated with various health issues such as arthritis, back problems, fibromyalgia, or nerve damage.
Chronic pain can severely affect a person's ability to perform everyday tasks, leading to disability, sleep disturbances, depression, and a reduced quality of life. The complexity of chronic pain requires a multifaceted approach to treatment, and this is where pain management specialists come in.
Who Are Pain Management Specialists?
Pain management specialists are medical doctors or healthcare providers trained to diagnose, treat, and manage different types of pain, particularly chronic pain. These specialists may come from various medical fields, including anesthesiology, neurology, psychiatry, rheumatology, and physical medicine and rehabilitation. They have expertise in evaluating the root causes of pain and implementing tailored treatment plans to help alleviate discomfort and enhance a patient’s functional capabilities.
Pain management specialists do not only focus on prescribing medications. They take a comprehensive approach to pain relief, incorporating physical therapy, lifestyle changes, psychological support, and advanced techniques such as injections or minimally invasive surgeries. Their goal is to reduce pain and improve the patient’s overall well-being.
Types of Chronic Pain Treated by Pain Management Specialists
Pain management specialists are skilled in treating a wide variety of chronic pain conditions. Some of the most common types include:
1. Back and Neck Pain
Back and neck pain are two of the most prevalent forms of chronic pain, often resulting from conditions like herniated discs, degenerative disc disease, or spinal stenosis. Pain management specialists can help relieve these conditions through various therapies such as epidural steroid injections, nerve blocks, physical therapy, or spinal cord stimulation.
2. Arthritis Pain
Arthritis, including osteoarthritis and rheumatoid arthritis, causes joint inflammation, stiffness, and pain. A pain management specialist may offer treatments such as joint injections, physical therapy, and lifestyle management strategies to reduce inflammation and improve joint mobility.
3. Neuropathic Pain
Neuropathic pain occurs when there is damage to the nerves. Conditions like diabetes (diabetic neuropathy), shingles (post-herpetic neuralgia), or multiple sclerosis can cause nerve damage, leading to persistent burning, shooting, or stabbing pain. Pain specialists may use medications such as anticonvulsants, antidepressants, or nerve blocks to help manage this type of pain.
4. Fibromyalgia
Fibromyalgia is a condition characterized by widespread muscle pain, fatigue, and sleep disturbances. Pain management specialists can treat fibromyalgia with a combination of medication, physical therapy, and cognitive behavioral therapy (CBT) to manage the condition and improve patients’ quality of life.
5. Cancer Pain
For cancer patients, pain can be caused by the tumor itself or as a side effect of cancer treatments. Pain management specialists work closely with oncologists to offer a comprehensive pain management plan that may include opioid therapy, nerve blocks, and other advanced pain relief strategies.
6. Headaches and Migraines
Chronic headaches, including migraines, can be debilitating and interfere with daily life. Pain management specialists may provide treatments such as Botox injections, nerve blocks, medications, and other non-pharmaceutical interventions to help reduce the frequency and intensity of these headaches.
How Pain Management Specialists Diagnose Chronic Pain
To effectively treat chronic pain, a pain management specialist first conducts a thorough evaluation to determine the underlying cause of the pain. This diagnostic process may involve:
1. Medical History Review
The specialist will review the patient's medical history, including any previous injuries, surgeries, or medical conditions that could be contributing to the pain. Understanding the patient’s overall health is essential to determine the most appropriate treatment options.
2. Physical Examination
A comprehensive physical exam helps the specialist assess the patient’s range of motion, posture, reflexes, and specific areas of pain. This allows the specialist to identify which structures in the body (muscles, joints, or nerves) are involved.
3. Diagnostic Tests
Diagnostic tests such as X-rays, MRIs, CT scans, and nerve conduction studies may be used to identify the source of pain. These tests help confirm the presence of conditions such as herniated discs, nerve damage, or inflammation.
4. Pain Mapping
In some cases, pain mapping may be used to pinpoint the exact location and intensity of pain. This method helps guide treatment options such as nerve blocks or injections.
Treatment Approaches Used by Pain Management Specialists
Once the source of pain is identified, pain management specialists use a variety of approaches to manage and alleviate the discomfort. These treatments often involve a combination of the following:
1. Medications
Medications are commonly used in the management of chronic pain, including:
Nonsteroidal anti-inflammatory drugs (NSAIDs): For reducing inflammation and pain.
Acetaminophen: For mild to moderate pain relief.
Opioids: For severe pain, but used with caution due to the potential for addiction and side effects.
Antidepressants and Anticonvulsants: For nerve-related pain.
Topical analgesics: Creams or patches applied to the skin for localized pain.
2. Injections and Nerve Blocks
Pain management specialists may administer steroid injections, nerve blocks, or trigger point injections to target the source of pain. These injections can provide temporary or long-term relief by reducing inflammation, blocking pain signals, or numbing nerves.
3. Physical Therapy
Physical therapy is often prescribed to strengthen muscles, improve flexibility, and reduce pain. A tailored exercise program may be designed to help patients regain mobility and function.
4. Cognitive Behavioral Therapy (CBT)
CBT is a form of psychotherapy that helps patients manage chronic pain by changing negative thought patterns and developing coping strategies. Pain management specialists may recommend CBT to help patients address the emotional and psychological components of chronic pain.
5. Surgical Interventions
In cases where conservative treatments are ineffective, surgical options such as spinal cord stimulation or minimally invasive surgeries may be considered. Pain management specialists work with surgical teams to ensure the patient is a good candidate for such procedures.
6. Complementary Therapies
Some pain management specialists may incorporate alternative therapies such as acupuncture, massage therapy, or biofeedback as part of a holistic pain management plan. These methods aim to alleviate pain and promote relaxation without the need for medications or invasive procedures.
The Importance of a Multidisciplinary Approach
Chronic pain is complex and requires a multifaceted treatment strategy. Pain management specialists often work with other healthcare professionals, such as physical therapists, psychologists, and dietitians, to provide a comprehensive treatment plan. By addressing all aspects of pain, including the physical, emotional, and lifestyle factors, a multidisciplinary approach can significantly improve the chances of achieving long-term pain relief and enhancing quality of life.
Conclusion
Pain management specialists play a crucial role in the treatment of chronic pain. Through their expertise, they help patients navigate the complexities of persistent pain, offering relief and improving their overall well-being. Whether through medication, injections, physical therapy, or psychological support, pain management specialists provide individualized care to help patients regain control over their lives and reduce the impact of chronic pain on daily activities. For those suffering from chronic pain, seeking the help of a pain management specialist can be a crucial step toward a better quality of life.
1 note
·
View note
Text
Rideshare Injury Lawyers Help Maximize Settlement After a Rideshare Accident
Los Angeles Rideshare Accident Surge: Avrek Law Firm Leads the Way in Securing Fair Compensation for Victims
With the increasing popularity of rideshare services like Uber and Lyft in Los Angeles, accidents involving these vehicles have become more common. When a rideshare accident occurs, determining liability and the expected type of settlement can be complicated. Avrek Law Firm, one of the best rideshare accident lawyers in Los Angeles, is here to help victims understand their legal options and ensure they receive fair compensation for their injuries.

Common Types of Settlements After a Rideshare Accident
When it comes to rideshare accidents, there are several types of settlements that injured parties may be entitled to receive. The settlement amount can vary depending on the severity of the injuries and the extent of the damages. Some of the most common types of settlements include:
Medical Expenses: Compensation for medical bills, including emergency care, surgery, hospital stays, rehabilitation, and future medical needs.
Lost Wages: If the accident causes the victim to miss work, a settlement can cover lost wages and may also include future earning potential if the injuries result in long-term disability.
Pain and Suffering: This type of settlement accounts for physical and emotional distress experienced as a result of the accident.
Property Damage: In cases where personal property, such as a vehicle, is damaged in the accident, compensation can be awarded for repair or replacement costs.
Understanding the types of compensation available is critical to ensure you receive the full benefits you’re entitled to. A skilled rideshare injury lawyer from Avrek Law Firm will work to secure maximum compensation across all these categories.
Factors That Influence Rideshare Settlement Amounts
The settlement amount a victim can expect after a rideshare accident depends on various factors that can complicate the process. Key elements that influence the value of a rideshare settlement include:
Severity of Injuries: More severe injuries, such as traumatic brain injuries, spinal cord damage, or broken bones, typically result in higher settlements due to the extensive medical treatment required.
Insurance Policies Involved: Rideshare drivers are covered by different insurance policies depending on the circumstances of the accident. Lyft and Uber offer $1 million in liability coverage when the driver is actively transporting passengers. However, if the driver was not logged into the app, their personal insurance may be the only coverage available.
Shared Liability: In some cases, both the rideshare driver and another party may share responsibility for the accident. The percentage of fault assigned to each party can impact the total settlement amount.
Legal Representation: Having the best rideshare accident attorney on your side can make a significant difference in the outcome of your settlement. An experienced attorney can handle the legal complexities and negotiate with insurance companies to ensure you receive the highest possible compensation.
Avrek Law Firm’s team of rideshare accident lawyers in Los Angeles has a proven track record of securing favorable settlements for their clients, ensuring that all factors are carefully evaluated to maximize payouts.
How the Best Rideshare Accident Attorney Can Help Maximize Your Settlement
The legal process after a rideshare accident can be overwhelming. The best course of action is to consult with a reputable rideshare injury lawyer to protect your rights. Avrek Law Firm’s Los Angeles-based attorneys have many years of experience handling rideshare accident claims and are well-versed in the complexities of rideshare insurance policies.
The benefits of working with one of the best rideshare accident attorneys include:
Thorough Investigation: An attorney will gather all necessary evidence, including police reports, witness statements, and medical records, to build a strong case.
Accurate Valuation of Your Claim: The attorney will ensure that all aspects of your losses are accounted for, including future medical costs and lost earning capacity.
Negotiation with Insurance Companies: Rideshare companies and their insurers often attempt to minimize payouts for injured parties. Avrek Law Firm’s legal experts have the skills and experience to negotiate aggressively on your behalf, ensuring that you receive fair compensation.
Litigation if Necessary: If a fair settlement cannot be reached through negotiation, Avrek Law Firm is prepared to take the case to court to fight for your rights.
By working with the best rideshare accident attorney, you can rest assured that your case is in capable hands and that every effort will be made to secure the maximum settlement possible.
Steps to Take After a Rideshare Accident to Protect Your Rights
To ensure that you receive the compensation you deserve after a rideshare accident, it’s essential to take the right steps immediately after the incident. Here are the actions you should take:
Seek Medical Attention: Your health should always be the top priority after an accident. Even if you don’t feel injured, some injuries may not be immediately apparent, making it important to get checked by a medical professional.
Document the Accident: Take photos of the accident scene, any vehicle damage, and any visible injuries sustained during the incident. Make sure to obtain contact information from all parties involved, including witnesses.
Report the Accident: Notify the rideshare company and your insurance provider about the accident.
Contact a Rideshare Accident Lawyer: Before speaking with any insurance adjusters or agreeing to a settlement, consult with an experienced rideshare accident attorney from Avrek Law Firm to discuss your legal options.
Following these steps will help safeguard your rights and strengthen your case for compensation.

Ensure You Receive Rightful Settlement With The Best Rideshare Accident Lawyers in Los Angeles: Avrek Law Firm
When you’ve been injured in a rideshare accident, navigating the legal process can be challenging. By working with Avrek Law Firm, one of the best rideshare accident lawyers in Los Angeles, you can ensure that your case is handled professionally and that you receive the maximum settlement possible. With their extensive experience, Avrek Law Firm’s team of rideshare accident attorneys is dedicated to helping victims receive fair compensation for their injuries. For more information or to schedule a consultation, contact Avrek Law Firm at (800) 800-9828.
Contact Information:
Avrek Law Firm
3415 South Sepulveda Blvd. Ste 1100 Los Angeles, CA 90034 United States
Avrek Law Firm * https://avrek.com
Original Source: https://www.avrek.com/blog/types-of-settlement-expected-after-a-rideshare-accident/
0 notes
Text
How Does a Denver Motorcycle Accident Lawyer Determine the Value of Your Claim?

After a motorcycle accident, one of the most pressing concerns for victims is understanding how much their claim is worth. The value of your claim can significantly impact the compensation you receive for your injuries, medical expenses, lost wages, and pain and suffering. A Denver motorcycle accident lawyer plays a vital role in determining this value by evaluating various factors related to the accident, your injuries, and the circumstances surrounding the cradenver motorcycle accident lawyer sh. Here's how a Denver motorcycle accident lawyer typically determines the value of your claim.
1. Evaluating the Severity of Your Injuries
The first factor that a Denver motorcycle accident lawyer will consider when determining the value of your claim is the severity of your injuries. Motorcycle accidents often result in severe injuries such as broken bones, head trauma, spinal cord injuries, road rash, and even wrongful death. The more serious your injuries, the higher the potential value of your claim. This is because severe injuries usually require more extensive medical treatment, long-term care, and can result in permanent disability.
Your lawyer will work closely with your medical providers to gather information about the type of injuries you've sustained, the medical treatments you've received, and the long-term prognosis for recovery. They will also take into account how the injury affects your ability to work, engage in everyday activities, and enjoy your quality of life. A Denver motorcycle accident lawyer will use all this information to build a compelling case that reflects the true value of your suffering.
2. Medical Expenses and Future Medical Costs
Medical bills are one of the most significant factors in determining the value of your claim. After a motorcycle accident, you may face immediate medical expenses, such as emergency room visits, surgeries, hospital stays, and rehabilitation. Additionally, you may need ongoing medical care, such as physical therapy, medication, and specialist visits, especially if your injuries are severe.
A Denver motorcycle accident lawyer will carefully review your medical records and work with medical experts to determine the cost of your current and future medical expenses. Future medical costs can be particularly challenging to estimate, especially if your injuries require long-term or permanent care. A lawyer will ensure that the projected costs for future medical treatment are included in your claim to ensure that you’re adequately compensated for all your medical needs.
3. Lost Wages and Lost Earning Potential
Another key component in determining the value of your claim is the impact of the accident on your ability to work. If you were employed at the time of the crash, your Denver motorcycle accident lawyer will consider the wages you’ve lost due to your injuries. This includes both short-term lost income while you’re recovering, as well as long-term wage losses if your injuries prevent you from returning to your previous job or career.
In cases where a motorcycle accident causes permanent disability, your lawyer will calculate the impact on your future earning potential. For example, if your injuries prevent you from working in the same capacity or force you to take a lower-paying job, your lawyer will work with economic experts to determine how this loss of income should be factored into your claim.
4. Pain and Suffering
Pain and suffering refer to the physical and emotional toll an injury takes on a person’s life. While it can be more difficult to quantify than medical bills or lost wages, pain and suffering are still a critical part of the compensation process. Motorcycle accidents often cause long-term physical pain, emotional distress, and psychological trauma. Victims may experience anxiety, depression, and post-traumatic stress disorder (PTSD) as a result of the accident.
A Denver motorcycle accident lawyer will take your pain and suffering into account by looking at the extent of your physical pain, emotional distress, and how the accident has affected your quality of life. They may also consider the psychological impact of the accident, such as fear of riding again, loss of enjoyment of life, or other emotional burdens.
To calculate pain and suffering, a lawyer may use a variety of methods, including multiplying your total economic damages (such as medical bills and lost wages) by a certain factor or using a per diem approach, which assigns a daily value to your pain and suffering. This can vary based on the severity of the injuries and the duration of the recovery process.
5. Property Damage
In addition to bodily injury, motorcycle accidents often result in significant property damage. Your Denver motorcycle accident lawyer will assess the extent of the damage to your motorcycle, helmet, protective gear, and any other personal property involved in the accident. The repair or replacement cost of your property will be included in your claim, helping to ensure that you are fully compensated for the financial losses caused by the accident.
Your lawyer will work with repair shops, appraisers, and insurance companies to determine the fair value of your damaged property. They will also consider whether your motorcycle is repairable or if it is a total loss, which can affect the total amount you are awarded for property damage.
6. Liability and Comparative Negligence
The amount of compensation you receive is also influenced by the degree of fault in the accident. In Denver, as in many other states, Colorado follows a comparative negligence rule. This means that if you are partially at fault for the accident, your compensation may be reduced based on the percentage of fault assigned to you.
For example, if you were speeding at the time of the crash but the other driver was also negligent, your lawyer will evaluate how the fault is divided between the parties involved. If you are found to be 20% at fault, your compensation will be reduced by that percentage. Your Denver motorcycle accident lawyer will carefully investigate the circumstances of the crash, review police reports, and gather evidence to support your claim of fault, aiming to minimize your liability and maximize your compensation.
7. Insurance Coverage and Policy Limits
Another crucial aspect in determining the value of your claim is the available insurance coverage. Motorcycle accident claims often involve complex insurance policies, including the at-fault driver’s insurance, your own motorcycle insurance, and possibly uninsured or underinsured motorist coverage. A Denver motorcycle accident lawyer will review all applicable insurance policies and determine the amount of coverage available to you.
If the at-fault driver is underinsured or uninsured, your lawyer may help you pursue additional claims through your own insurance coverage or take legal action against the driver. They will also ensure that the insurance companies involved do not undervalue your claim or pressure you into accepting a low settlement.
8. Expert Testimony and Evidence
In many motorcycle accident cases, expert witnesses may be needed to determine the full value of your claim. For instance, accident reconstruction experts can analyze the scene of the crash to establish fault, while medical experts can provide testimony regarding the severity of your injuries and the long-term effects on your health. Your Denver motorcycle accident lawyer will work with these experts to gather evidence that strengthens your case and ensures that the value of your claim accurately reflects your losses.
Conclusion
Determining the value of a motorcycle accident claim in Denver is a complex process that requires a thorough understanding of both the legal and medical aspects of the case. A Denver motorcycle accident lawyer will evaluate your injuries, medical expenses, lost wages, pain and suffering, and other damages to calculate a fair and just compensation amount. By leveraging their expertise, experience, and access to medical and economic experts, your lawyer will work tirelessly to ensure that you receive the compensation you deserve after a motorcycle accident.
0 notes